مداخلات جراحی در برابر مداخلات محافظهکارانه برای درمان دررفتگیهاي مفصل آکرومیوکلاویکولار شانه در بزرگسالان
Appendices
Appendix 1. Search strategies for this update (date of search: June 2019)
CENTRAL (CRS Web)
Search 1
1 MESH DESCRIPTOR Acromioclavicular Joint AND CENTRAL: TARGET (45)
2 (acromioclavic* or coracoclavic* or AC joint ): AB,EH,KW,KY,MC,MH,TI,TO AND 3 CENTRAL: TARGET (119)
3 #1 OR #2 (119)
Search 2 (top‐up search)
Lines 1 to 3 as above
4 20/08/2018_To_17/06/2019:CRSCREATED AND CENTRAL:TARGET (270097)
5 #4 AND #3 (42)
MEDLINE: Ovid MEDLINE(R)
Search 1
1 ACROMIOCLAVICULAR JOINT/ (1901)
2 (acromioclavic* or coracoclavic* or AC joint).tw. (2133)
3 1 or 2 (2641)
4 Randomized controlled trial.pt. (466407)
5 Controlled clinical trial.pt. (92552)
6 randomi?ed.ti,ab. (469940)
7 placebo.ab. (174425)
8 Clinical trials as topic/ (184490)
9 randomly.ab. (253639)
10 trial.ti. (161749)
11 4 or 5 or 6 or 7 or 8 or 9 or 10 (1091561)
12 exp Animals/ not Humans/ (4486177)
13 11 not 12 (997810)
14 3 and 13 (110)
15 ("2009*" or "2010*" or "2011*" or "2012*" or "2013*" or "2014*" or "2015*" or "2016*" or "2017*" or "2018*").ed,dc. (7648309)
16 14 and 15 (76)
Search 2 (top‐up search)
Lines 1 to 14 as above
15 (201808* or 201809* or 201810* or 201811* or 201812* or 2019*).ed,dt. (1738451)
16 14 and 15 (23)
Embase: Ovid Embase
Search 1
1 Acromioclavicular joint/ (2062)
2 Acromioclavicular dislocation/ (772)
3 (acromioclavic* or coracoclavic* or ac joint).tw. (2607)
4 1 or 2 or 3 (3405)
5 exp Randomized controlled trial/ (504384)
6 Clinical Trial/ (939186)
7 Double blind procedure/ (148573)
8 Single blind procedure/ (31924)
9 Crossover procedure/ (55868)
10 Randomization/ (78722)
11 Placebo/ (307097)
12 Prospective study/ (461060)
13 ((clinical or controlled or comparative or placebo or prospective$ or randomi#ed) adj3 (trial or study)).tw. (1091445)
14 (random* adj7 (allocat* or allot* or assign* or basis* or divid* or order*)).tw. (272957)
15 ((singl* or doubl* or trebl* or tripl*) adj7 (blind* or mask*)).tw. (209854)
16 (cross?over* or (cross adj1 over*)).tw. (92019)
17 ((allocat* or allot* or assign* or divid*) adj3 (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)).tw. (372499)
18 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 (2591375)
19 limit 18 to human (2238288)
20 4 and 19 (396)
21 (2009* or 2010* or 2011* or 2012* or 2013* or 2014* or 2015* or 2016* or 2017* or 2018*).dc,yr. (13296554)
22 20 and 21 (254)
Search 2 (top‐up search)
Lines 1 to 20 as above
21 (2018* or 2019*).dc,yr. (2680741)
22 20 and 21 (61)
LILACS (BIREME)
(mh:(“acromioclavicular joint”)) OR (tw:(acromioclavic*)) OR (tw:(coracoclavic*)) OR (tw:("AC joint")) AND (instance:"regional") AND ( db:("LILACS")) (159)
WHO ICTRP
Acromioclavicular Joint OR acromioclavic* OR coracoclavic* OR AC joint (54)
ClinicalTrials.gov
Acromioclavicular Joint OR acromioclavic* OR coracoclavic* OR AC joint | First posted from 02/01/2009 to 06/17/2019 (130)
Appendix 2. Report of search results in previous version of the review
2010, Issue 8 (Date of Search: February 2009)
We searched the Cochrane Bone, Joint andMuscle Trauma Group Specialised Register (to February 2009), the Cochrane Central Register of Controlled Trials (TheCochrane Library 2009, Issue 1), MEDLINE (1966 to February 2009), EMBASE (1988 to February 2009), and the Latin American andCaribbeanHealth Sciences database (LILACS) (1982 to February 2009). We also searched theWHO International Clinical Trials Registry Platform Search Portal (to February 2009), Current Controlled Trials (to February 2009), and the UK National Research Register (NRR) Archive (up to September 2007) for ongoing and recently completed trials.
Our search found 171 references. The numbers of records identified via our searches of individual databases for the first version of the review were as follows: Cochrane Bone, Joint andMuscle Trauma Group Specialised Register (6 records), The Cochrane Central Register of Controlled Trial (The Cochrane Library (Wiley InterScience)) (39 records), MEDLINE (PubMed) (35 records)), EMBASE (Elsevier) (76 records)), LILACS (Bireme) (14 records) and Grey Literture (1 record).
After removing duplicates and screening of titles and abstracts we excluded 165 articles. The remaining six potentially relevant studies were evaluated from full trial reports and one of these studies (Sehmisch 2008) was translated into English. We excluded three studies: two prospective studies (Sehmisch 2008; Sternick 1991) were neither randomised nor quasi‐randomised, and one study (Galpin 1985) was retrospective. The remaining three studies were either randomised or quasi‐randomised controlled trials that reported relevant outcomes (Bannister 1989; Imatani 1975; Larsen 1986). In addition, two ongoing trials were identified from trial registers.
Appendix 3. Previous 'Types of outcome measures' (Tamaoki 2010)
Types of outcome measures
Primary outcomes
-
Health‐related quality of life;
-
Pain;
-
Shoulder function (preferably patient‐reported);
-
Return to previous activities, including work, sport and activities of daily living;
-
Treatment failure and other serious adverse effects of treatment such as requirement for a subsequent operation.
Examples of validated patient‐assessed instruments for measuring the first three outcomes are:
-
Short Form‐36 (SF‐36) (Ware 1992) for health related quality of life;
-
VAS (visual analogue scale) (Revill 1976) for pain;
-
Disability of the Arm, Shoulder, and Hand (DASH) Questionnaire (Hudak 1996) for upper‐limb function.
A commonly used instrument for assessing shoulder function is the Constant score (Constant 1987), which is a composite score for shoulder function which includes pain and activities of daily living, and range of movement and strength.
Secondary outcomes
Clinical outcomes
-
Shoulder range of motion;
-
Strength;
-
Cosmetic appearance;
-
Patient satisfaction with treatment.
Radiological outcomes
-
Residual deformity (distance between coracoid and clavicle or acromion and clavicle).
Resource use
-
Hospital admission and length of stay, number of outpatient attendances and other costs of treatment;
-
Time off work or education.
Safety (success or failure of treatment and adverse events)
-
Complications:
-
-
Early (e.g. wound or skin breakdown or skin necrosis under strapping, fixation failure, migration of wires, residual deformity, infection, requirement for reoperation);
-
Late (e.g. traumatic arthritis, calcification of coracoclavicular ligament, requirement for reoperation).
-
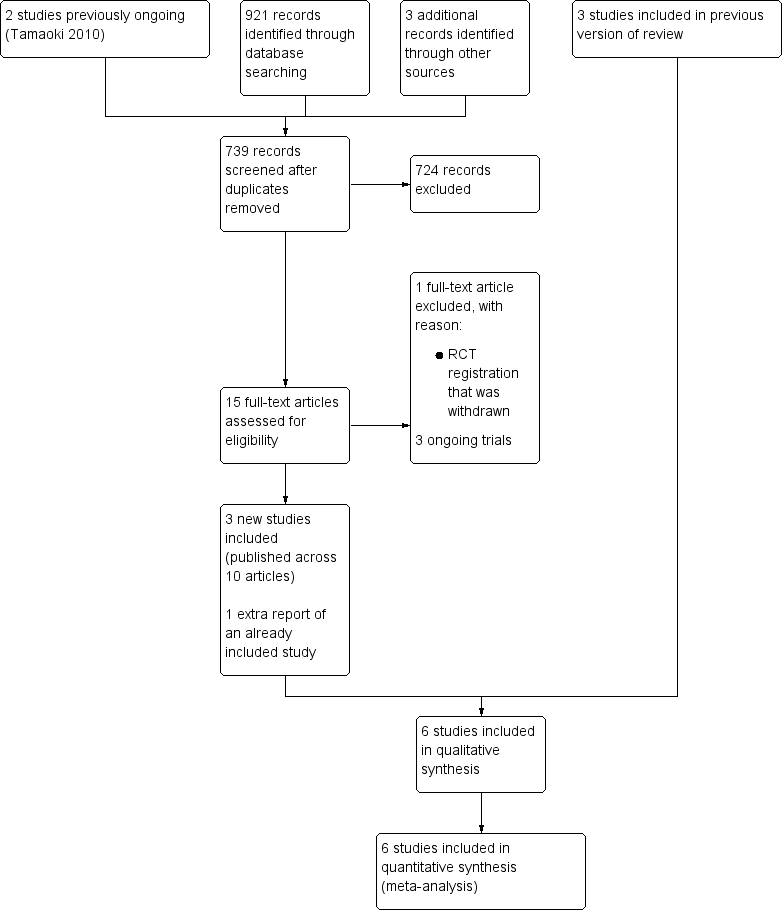
Study flow diagram for update.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Surgical intervention versus conservative intervention, Outcome 1 DASH questionnaire (0 (best function) to 100 (worst function)).

Comparison 1 Surgical intervention versus conservative intervention, Outcome 2 Constant score (0 (worst function) to 100 (best function)).
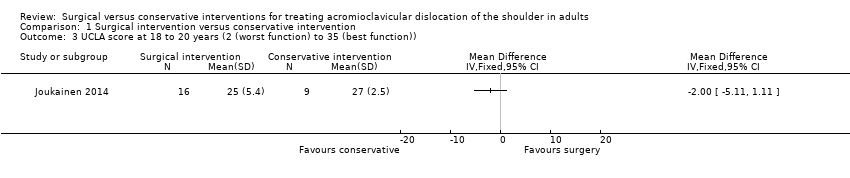
Comparison 1 Surgical intervention versus conservative intervention, Outcome 3 UCLA score at 18 to 20 years (2 (worst function) to 35 (best function)).

Comparison 1 Surgical intervention versus conservative intervention, Outcome 4 Oxford Shoulder Score (0 (worst function) to 48 (best function)).

Comparison 1 Surgical intervention versus conservative intervention, Outcome 5 Unsatisfactory function (only 'poor' or 'fair' category ) at 1 year.

Comparison 1 Surgical intervention versus conservative intervention, Outcome 6 Pain: presence of pain (slight or moderate).
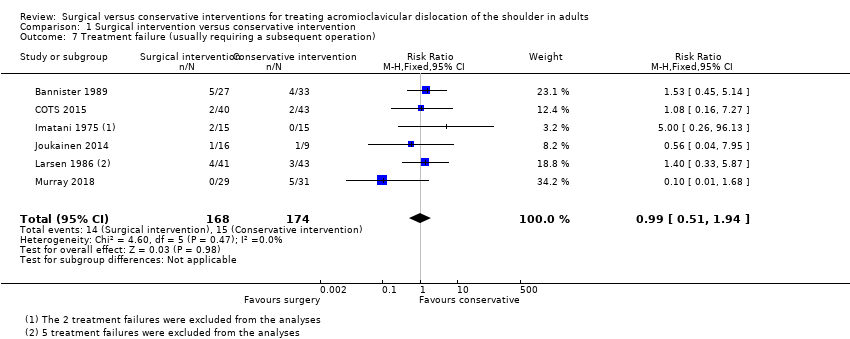
Comparison 1 Surgical intervention versus conservative intervention, Outcome 7 Treatment failure (usually requiring a subsequent operation).

Comparison 1 Surgical intervention versus conservative intervention, Outcome 8 Number of participants to return to work/sport.

Comparison 1 Surgical intervention versus conservative intervention, Outcome 9 Health‐related quality of life: SF‐36 or SF‐12 (0 (worst quality of life) to 100 (best quality of life)).
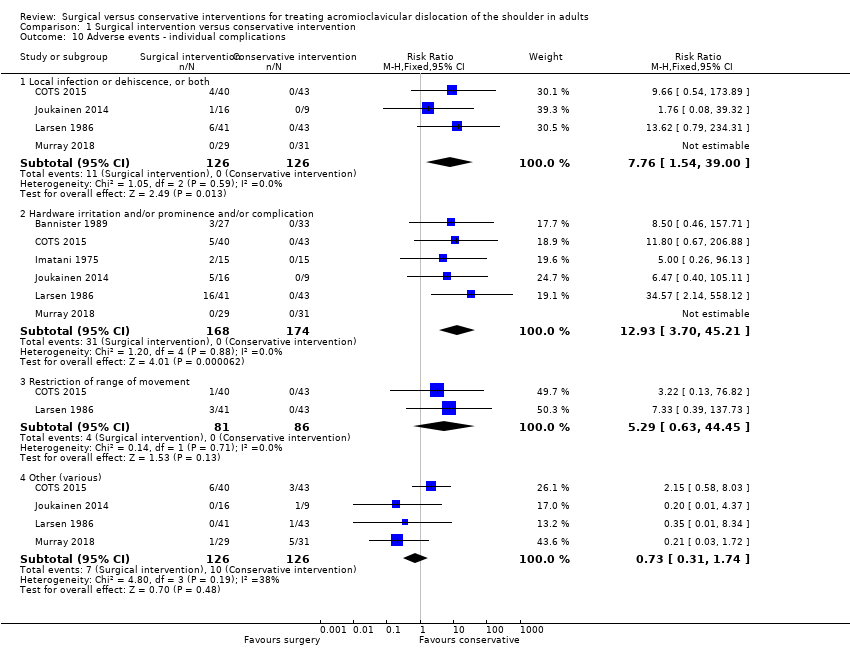
Comparison 1 Surgical intervention versus conservative intervention, Outcome 10 Adverse events ‐ individual complications.
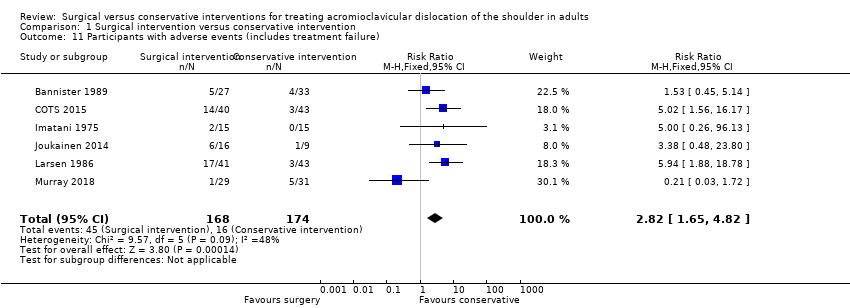
Comparison 1 Surgical intervention versus conservative intervention, Outcome 11 Participants with adverse events (includes treatment failure).
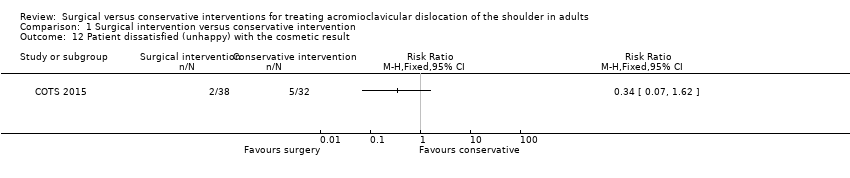
Comparison 1 Surgical intervention versus conservative intervention, Outcome 12 Patient dissatisfied (unhappy) with the cosmetic result.
| Surgical intervention compared to conservative intervention for treating acromioclavicular dislocation of the shoulder in adults | ||||||
| Patient or population: adults with acute acromioclavicular dislocation of the shouldera | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Risk with conservative intervention | Risk with surgical intervention | |||||
| DASH questionnaire (0 (best function) to 100 (worst function)) ‐ at 1 year | The mean DASH questionnaire score at 1 year ranged from 4.67 to 9.2. | MD 0.73 higher | ‐ | 112 (2 studies) | ⊕⊕⊝⊝b,c | This does not represent a clinically important difference. The MCID of the DASH questionnaire is 10 points.d |
| Pain: presence of pain (slight or moderate) at 1 year | Study population | RR 1.32 | 79 (1 study) | ⊕⊝⊝⊝b,c,f | None of the studies reported pain measured via a visual analogue scale. | |
| 175 per 1000e | 231 per 1000 | |||||
| Treatment failure (usually requiring a subsequent operation) at 1 year | Study population | RR 0.99 | 342 | ⊕⊝⊝⊝a,b | The main sources of treatment failure in the conservatively treated group were persistent symptoms and discomfort from acromioclavicular dislocation, and in the surgical group problems related to hardware. | |
| 87 per 1000e | 87 per 1000 | |||||
| Number of participants to return to work/sport ‐ at 1 year | Study population | RR 0.96 | 137 | ⊕⊕⊝⊝b,c low | There is, however, low‐quality but consistent evidence of an earlier recovery after conservative treatment compared with surgery. | |
| 886 per 1000e | 851 per 1000 | |||||
| Health‐related quality of life: SF‐36 or SF‐12 (0 (worst quality of life) to 100 (best quality of life)) ‐ physical component score at 1 year | The mean health‐related quality of life (SF‐36 or SF‐12) physical component scores at 1 year ranged from 52.61 to 55.1. | MD 0.63 lower | ‐ | 122 (2 studies) | ⊕⊕⊝⊝b,c | This does not represent a clinically important difference. The MCID of the overall SF‐36 ranges from 2.0 to 7.8 points (scale 0 to 100). |
| Participants with adverse events at 1 year | Study population | RR 2.82 (1.65 to 4.82) | 342 (6 studies) | ⊕⊝⊝⊝b,c,g | The derivation of this outcome (number of people with 1 or more adverse events), which includes people with treatment failure for whatever reason, varied across studies. Hardware complication or discomfort, or both, was the most frequent problem in the surgical group (31/168 (18.5%), range 0% to 39%; 6 studies) and persistent symptoms or discomfort, or both, in the conservatively treated group (9/126 (7.1%); 4 studies). Infection or dehiscence, or both, occurred only in the surgical group (11/126 (8.7%); 4 studies). The majority of surgical complications were in studies testing now‐outdated devices known for their high risk of complications. | |
| 92 per 1000e | 260 per 1000 (152 to 444) | |||||
| Patient dissatisfaction with the cosmetic result at 1 yearh | Study population | RR 0.34 (0.07 to 1.62) | 70 (1 study) | ⊕⊝⊝⊝b,i | One of the treatment failures in each of the conservatively treated groups of 2 other studies was for cosmetic reasons. | |
| 157 per 1000e | 54 per 1000 (11 to 255) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence Low quality: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. | ||||||
| aThe study populations were predominantly male and young adults; the mean ages in the trials ranged from 23.6 to 37.6 years. hAlthough our intended outcome was patient satisfaction, the study only reported on the numbers who were unhappy with their cosmetic result. iThere was very serious imprecision reflecting wide confidence intervals and very few events. | ||||||
| Type | Description |
| Type I | A mild injury involving spraining of the acromioclavicular ligaments while leaving the joint intact |
| Type II | Injury where the acromioclavicular ligaments are torn and acromioclavicular joint is disrupted, whilst the coracoclavicular ligaments are intact |
| Type III | Injury involves complete tearing of both the acromioclavicular and coracoclavicular ligaments with 100% dislocation of the joint. |
| Type IV | Injury is a complete acromioclavicular dislocation with posterior displacement of the clavicle through or into the trapezius fascia. |
| Type V | Injury is a complete acromioclavicular dislocation with 100% to 300% superior dislocation of the clavicle. It can involve significant disruption of the deltotrapezial fascia. |
| Type VI | Injury involves inferior displacement of the clavicle into a subacromial or subcoracoid position. |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 DASH questionnaire (0 (best function) to 100 (worst function)) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 At 6 weeks | 2 | 115 | Mean Difference (IV, Fixed, 95% CI) | 15.10 [7.87, 22.33] |
| 1.2 At 3 months | 2 | 112 | Mean Difference (IV, Fixed, 95% CI) | 8.38 [2.62, 14.14] |
| 1.3 At 6 months | 2 | 116 | Mean Difference (IV, Fixed, 95% CI) | 1.70 [‐2.98, 6.39] |
| 1.4 At 1 year | 2 | 112 | Mean Difference (IV, Fixed, 95% CI) | 0.73 [‐2.70, 4.16] |
| 1.5 At 2 years | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐1.61 [‐5.67, 2.45] |
| 2 Constant score (0 (worst function) to 100 (best function)) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 At 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 At 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 At 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 At 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 At 18 to 20 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 UCLA score at 18 to 20 years (2 (worst function) to 35 (best function)) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Oxford Shoulder Score (0 (worst function) to 48 (best function)) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Unsatisfactory function (only 'poor' or 'fair' category ) at 1 year Show forest plot | 3 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.75, 2.95] |
| 5.1 Score included pain, motion, and function | 2 | 81 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.76, 3.12] |
| 5.2 Score included pain, motion, and strength | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.07, 15.83] |
| 6 Pain: presence of pain (slight or moderate) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Treatment failure (usually requiring a subsequent operation) Show forest plot | 6 | 342 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.51, 1.94] |
| 8 Number of participants to return to work/sport Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 Return at 6 weeks | 2 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.37, 1.08] |
| 8.2 Return at 1 year | 2 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.85, 1.10] |
| 9 Health‐related quality of life: SF‐36 or SF‐12 (0 (worst quality of life) to 100 (best quality of life)) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Physical component score at 6 weeks | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | ‐4.60 [‐8.58, ‐0.62] |
| 9.2 Physical component score at 3 months | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | ‐6.38 [‐9.15, ‐3.61] |
| 9.3 Physical component score at 6 months | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | ‐2.89 [‐5.23, ‐0.55] |
| 9.4 Physical component score at 1 year | 2 | 122 | Mean Difference (IV, Fixed, 95% CI) | ‐0.63 [‐2.63, 1.37] |
| 9.5 Physical component score at 2 years | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 1.89 [‐0.78, 4.56] |
| 9.6 Mental component score at 6 weeks | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | 1.98 [‐3.66, 7.62] |
| 9.7 Mental component score at 3 months | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | 3.60 [‐1.14, 8.34] |
| 9.8 Mental component score at 6 months | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐3.10, 3.42] |
| 9.9 Mental component score at 1 year | 2 | 122 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐1.51, 2.44] |
| 9.10 Mental component score at 2 years | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐0.98 [‐4.24, 2.28] |
| 10 Adverse events ‐ individual complications Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Local infection or dehiscence, or both | 4 | 252 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.76 [1.54, 39.00] |
| 10.2 Hardware irritation and/or prominence and/or complication | 6 | 342 | Risk Ratio (M‐H, Fixed, 95% CI) | 12.93 [3.70, 45.21] |
| 10.3 Restriction of range of movement | 2 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.29 [0.63, 44.45] |
| 10.4 Other (various) | 4 | 252 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.31, 1.74] |
| 11 Participants with adverse events (includes treatment failure) Show forest plot | 6 | 342 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.82 [1.65, 4.82] |
| 12 Patient dissatisfied (unhappy) with the cosmetic result Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

