Gestão cirúrgica versus não‐cirúrgico da lesão abdominal
Abstract
Background
Injury to the abdomen can be blunt or penetrating. Abdominal injury can damage internal organs such as the liver, spleen, kidneys, intestine, and large blood vessels. There are controversies about the best approach to manage abdominal injuries.
Objectives
To assess the effects of surgical and non‐surgical interventions in the management of abdominal trauma in a haemodynamically stable and non‐peritonitic abdomen.
Search methods
We searched the Cochrane Injuries Group's Specialised Register, The Cochrane Library, Ovid MEDLINE(R), Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid OLDMEDLINE(R), EMBASE Classic+EMBASE (Ovid), ISI WOS (SCI‐EXPANDED, SSCI, CPCI‐S & CPSI‐SSH), CINAHL Plus (EBSCO), and clinical trials registers, and screened reference lists. We ran the most recent search on 17 September 2015.
Selection criteria
Randomised controlled trials of surgical interventions and non‐surgical interventions involving people with abdominal injury who were haemodynamically stable with no signs of peritonitis. The abdominal injury could be blunt or penetrating.
Data collection and analysis
Two review authors independently applied the selection criteria. Data were extracted by two authors using a standard data extraction form, and are reported narratively.
Main results
Two studies are included, which involved a total of 114 people with penetrating abdominal injuries. Both studies are at moderate risk of bias because the randomisation methods are not fully described, and the original study protocols are no longer available. The studies were undertaken in Finland between 1992 and 2002, by the same two researchers.
In one study, 51 people were randomised to surgery or an observation protocol. None of the participants in the study died. Seven people had complications: 5 (18.5%) in the surgical group and 2 (8.3%) in the observation group; the difference was not statistically significant (P = 0.42; Fischer's exact). Among the 27 people who had surgery, 6 (22.2%) surgeries were negative laparotomies, and 15 (55.6%) were non‐therapeutic.
In the other study, 63 people were randomised to diagnostic laparoscopy (surgery) or an observation protocol. There were no deaths and no unnecessary surgeries in either group. Four people did not receive the intervention they were assigned. There was no difference in therapeutic operations between the two groups: 3 of 28 in the diagnostic laparoscopy group versus 1 of 31 in the observation protocol group (P = 0.337).
Authors' conclusions
Based on the findings of 2 studies involving a total of 114 people, there is no evidence to support the use of surgery over an observation protocol for people with penetrating abdominal trauma who have no signs of peritonitis and are stable.
PICOs
Resumo para leigos
Cirurgia versus observação para pessoas com lesão abdominal
A lesão no abdómen é comum e pode ser sem corte, de acidentes de trânsito ou quedas, ou penetrante, de tiros ou facadas. Estas lesões estão normalmente associadas a lesões nos órgãos abdominais, tais como o fígado, baço, rins, intestino e o seu revestimento, e grandes vasos sanguíneos. Pode ocorrer um sangramento ou corrimento do conteúdo abdominal para a cavidade abdominal, que pode ameaçar a vida de uma pessoa. O exame do paciente pelo médico (exame físico), embora seja o método mais preciso para avaliar as pessoas, é insuficiente para determinar a extensão dos danos. Por outro lado, uma pessoa não deveria ser submetida a um procedimento cirúrgico, a menos que seja necessário. Há relatórios de que as lesões podem não ser encontradas, mesmo após uma cirurgia.
A observação de um paciente, esperando que a lesão tenha cicatrizado naturalmente e intervir cirurgicamente, caso exista essa necessidade, é conhecida como gestão seletiva não‐operatória (SNOM) ou observação. Um protocolo de observação é usado quando a pessoa não apresenta qualquer sinal de hemorragia interna ou infeção abdominal (peritonite). Recorre‐se à cirurgia se, durante a observação, forem observados sinais de hemorragia ou infeção.
Os autores desta revisão procuraram identificar os estudos, onde as pessoas com uma lesão abdominal foram aleatorizados para cirurgia ou para a observação. Os autores analisaram várias bases de dados médicas, mas identificaram apenas 2 estudos, envolvendo 51 e 63 pessoas respetivamente, ambos tiveram lugar na Finlândia e foram conduzidos pelos mesmos investigadores. Os estudos incluíam portadores de lesões abdominais penetrantes, provocadas por esfaqueamento. Os autores da revisão consideraram ambos os estudos como tendo um risco de viés moderado, uma vez que apenas uma parte do processo de aleatorização foi descrita e os protocolos do estudo não estavam disponíveis para permitir a avaliação completa da qualidade global.
Num estudo (1992‐1994), as pessoas receberam o tratamento segundo um protocolo de observação ou de cirurgia obrigatória. Nenhuma das pessoas no estudo morreu, e não houve diferença no número de pessoas com complicações médicas entre os grupos estudados. Um dos danos mencionados pelos autores do estudo foi a realização da cirurgia nalgumas pessoas que, na realidade, nem precisava disso. A cirurgia desnecessária pode submeter as pessoas a potenciais complicações.
Noutro estudo (1997‐2002), as pessoas receberam um protocolo de observação ou de laparoscopia de diagnóstico (cirurgia mínima). Ninguém morreu, em ambos os grupos, e não houve diferenças entre os grupos, no número de cirurgias necessárias. Não existiram cirurgias desnecessárias, em ambos os grupos.
Com base nas conclusões destes dois estudos pequenos, não há evidências para apoiar o uso do tratamento cirúrgico em detrimento de um protocolo de observação para pessoas com trauma abdominal, que não mostram sinais de hemorragia ou infeção.
Os autores recomendam que os futuros estudos controlados aleatorizados relatem claramente o tipo de lesão, número de órgãos danificados, extensão da lesão dos órgãos internos e complicações nas pessoas incluídas no estudos.
Authors' conclusions
Background
Description of the condition
Injury is a leading cause of morbidity and mortality worldwide. The most common causes of injury are falls from heights, road traffic crashes, and gun shot and stab wounds (Kahn 2006).
Injury to the abdomen can be blunt or penetrating. The most common cause of blunt abdominal trauma (BAT) is road traffic crashes (Kahn 2006). Other causes of BAT include pedestrian crashes and falls from heights (Anjum 2001). Penetrating abdominal trauma (PAT) may be caused by gun shots or stab wounds from piercing instruments. Most injuries to the abdomen are blunt injuries (Kahn 2006) and are associated with higher risk of death because the extent of injury is less obvious compared with penetrating injury (Anjum 2001).
Abdominal injuries are usually associated with injury to internal organs such as the liver, spleen, kidneys, the covering of the intestine and large blood vessels, and subsequent intra‐abdominal haemorrhage. Sometimes the extent of injury may not be readily obvious, particularly for blunt abdominal injuries. Severe bleeding may present with signs of haemodynamic instability: people may have a weak pulse, low blood pressure or be in a state of shock. Quite often these signs of internal injury may delay in manifesting clinically (Poletti 2004). Initial physical examination has been found to be unreliable for detecting people at risk of serious abdominal injury (Mackersie 1989; Hoff 2002). However, serial physical examination by experienced clinicians has been found to be reliable in detecting abdominal injuries in PAT (Como 2010).
Description of the intervention
The modality of management of people with abdominal injury depends on the severity of injuries incurred and the haemodynamic state of the person. Diagnosis of associated injuries in abdominal trauma presents a great challenge, even to the best of trauma surgeons (Hoff 2002; Radwan 2006). There are reports that physical examinations, though the most important assessment for intervention, are inaccurate (Hoff 2002). Consequently, clinically significant injuries may be missed. This dictates the need for active management of cases by surgical intervention. It has been observed, however, that injured organs may not be identified despite surgery (Jo 2007).
Recently, observation protocols have been adopted to avoid unnecessary surgery for both PAT (Demetriades 2006; Navsaria 2007) and BAT (Holmes 2005; Kahn 2006; Velmahos 2003). One approach involves selecting people based on their haemodynamic state and absence of peritonitis. People with signs of blood loss (haemodynamic instability) undergo surgery, while surgery is delayed for people in a stable condition until signs of blood loss or peritonitis are apparent.
Why it is important to do this review
Some experts oppose an observation protocol, arguing that this leads to delayed management of hollow viscous and mesenteric injuries (Yegiyants 2006). Other experts support this approach. They argue that avoiding unnecessary surgical intervention spares the person the consequences of metabolic response to surgical trauma and possible intra‐ and post‐operative complications (Basile 2006).
To have evidence for practice, there is a need for a synthesis of the evidence on the active surgical management and an observation protocol for the two types of abdominal trauma: blunt abdominal trauma (BAT) and penetrating abdominal trauma (PAT).
Objectives
To assess the effects of surgical interventions and non‐surgical interventions in the management of abdominal trauma in a haemodynamically stable and non‐peritonitic abdomen.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
Any person with abdominal trauma who is haemodynamically stable and with no sign of peritonitis. The abdominal injury could be blunt or penetrating.
Types of interventions
Surgical (operative) versus non‐surgical (observation) interventions.
Types of outcome measures
Primary outcomes
-
Mortality at final follow‐up.
Secondary outcomes
-
Need for rescue intervention (blood transfusion, surgical intervention, etc);
-
Morbidity (infection, shock, etc).
Search methods for identification of studies
In order to reduce publication and retrieval bias we did not restrict our search by language, date or publication status.
Electronic searches
The Cochrane Injuries Group's Trial Search Co‐ordinator searched the following:
-
Cochrane Injuries Group specialised register (17 September 2015);
-
Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library) (Issue 8 of 12, 2015);
-
Ovid MEDLINE(R), Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid OLDMEDLINE(R) (1946 to 17 September 2015);
-
EMBASE Classic + EMBASE (OvidSP) (1947 to 17 September 2015);
-
CINAHL Plus (EBSCO) (1937 to 17 September 2015);
-
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) (1970 to 17 September 2015);
-
ISI Web of Science: Conference Proceedings Citation Index‐Science (CPCI‐S) (1990 to 17 September 2015);
-
PubMed (17 September 2015).
Search strategies are reported in Appendix 1.
Searching other resources
We checked the reference lists of all relevant studies and reviews to identify further studies. We also searched the Internet and the following trial registers to January 2012:
-
Current Controlled Trials (www.controlled‐trials.com);
-
Clinicaltrials.gov (www.clinicaltrials.gov).
Data collection and analysis
The Cochrane Injuries Group's Trials Search Co‐ordinator ran the searches and collated the results before passing them on to the authors for screening.
Selection of studies
Two authors screened the results independently using the inclusion criteria published in this systematic review's protocol (Oyo‐Ita 2008), to identify eligible studies. There was no disagreement on the inclusion of studies. For the first version of the review UU and IAI screened the search results. For the 2015 update, PC and AO screened the search results.
Data extraction and management
Data extraction was carried out using a standard extraction form. Two authors (UU and IAI in 2012; PC in 2015) extracted the data and one author (AO) cross‐checked for errors and completion. As data from the two included studies could not be combined, data were not entered into Review Manager for meta‐analysis as had originally been planned.
Assessment of risk of bias in included studies
Two authors (UU and IAI in 2012; PC and AO in 2015) independently assessed the methodological quality of the included studies. Methodological quality was assessed based on the following criteria: method of generation of the randomisation sequence, concealment of the randomisation sequence, incomplete outcome data, selective reporting, and other sources of bias. The review authors gave a judgement of 'high', 'low' or 'unclear' risk of bias, as outlined in theCochrane Handbook (Higgins 2011). Blinding of participants and treating physicians is not possible for the interventions studied in this review, therefore blinding was not included in the 'Risk of bias' assessment.
Assessment of heterogeneity
Both studies had an observation protocol (which the study authors called 'expectant non‐operative management') as the control arm, but different intervention arms. Due to heterogeneity of the interventions, study results are presented separately and in narrative format.
Assessment of reporting biases
We contacted the study researcher (personal communication, Leppäniemi 2003b), who provided a full response to our request for information. According to Dr. Leppäniemi it was the policy of the hospital ethics committee that the study information and data be destroyed upon publication of the results. As the study protocols have been destroyed it is not possible to assess reporting bias.
Data synthesis
The results of the studies are presented separately, in narrative format.
Sensitivity analysis
There were insufficient data included in the review to enable a sensitivity analysis to be performed.
Results
Description of studies
Results of the search
The electronic search for studies identified 1635 records. Eight potentially‐eligible studies were evaluated in full‐text and two studies (Leppäniemi 1996 and Leppäniemi 2003b) met the inclusion criteria (Figure 1).
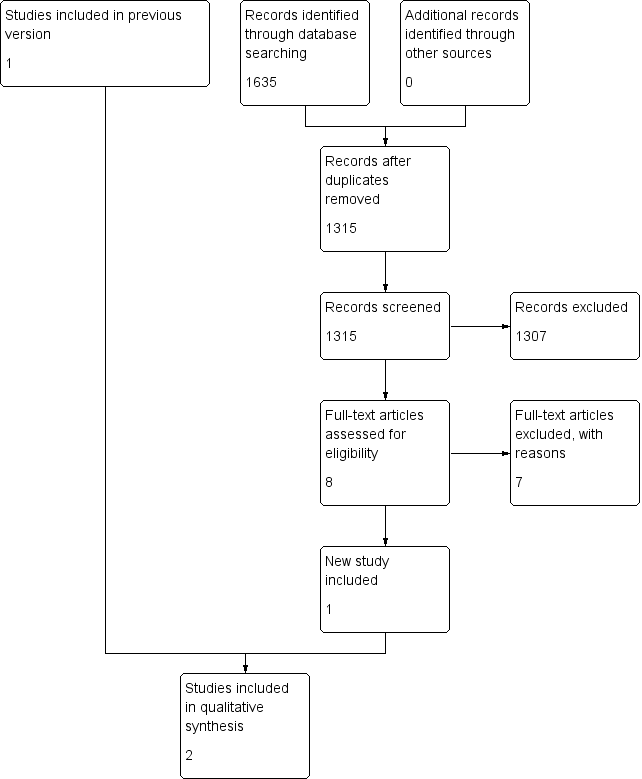
Study flow diagram.
Included studies
Two studies (Leppäniemi 1996; Leppäniemi 2003b) are included in this review.
The first (Leppäniemi 1996) was carried out between 1 March 1992 and 3 July 1994 in Finland and included any person with an abdominal or lower thoracic stab injury received in the preceding 48 hours. Abdominal or lower thoracic was defined as the area bounded anteriorly and laterally by the fifth intercostal space, posteriorly by the inferior tip of the scapular, caudally and anteriorly by the inguinal creases and laterally and posteriorly by the iliac bone crests. A person with suspected peritoneal penetration who did not require immediate laparotomy was randomised using a sealed opaque envelope to either mandatory laparotomy or the observation protocol. A person randomised to receive mandatory surgery was operated on immediately. A person in the observation protocol was physically examined every 2 hours for the first 6 hours, then every 12 hours for at least 48 hours. Twenty seven people were randomised to the surgery group and 24 to the observation group; 74% and 83% were males in the surgery and observation groups respectively.
On admission, the following tests were carried out on people in the observation group: haemoglobin level, urine amylase, urine blood, chest and plain abdominal radiographs. Investigations six hours after admission included haemoglobin level and contrast‐enhanced computed tomography. No antibiotics were given to either group except when wound contamination was suspected. A person was observed for 48 hours if there was no need for intervention. A person was required to return for follow up 4 to 6 weeks after the injury and later if necessary. The main outcomes studied included early morbidity (for complications within the initial hospital stay or within 90 days of the injury) and length of hospital stay (including readmission for complications within 90 days of the injury).
The second study (Leppäniemi 2003b) was carried out in Finland from May 1997 to January 2002. Fifty‐nine people with equivocal peritoneal violation on local wound exploration were randomised to diagnostic laparoscopy or an observation protocol. While the laparoscopy was restricted to diagnostic purposes, we considered it to be a surgical intervention as the technique of laparoscopy involves the making of an incision. (This study also included another arm not relevant to this review (Leppäniemi 2003a) in which people who were stable and without peritonitis but who had demonstrated peritoneal violation were randomised to one or other of two surgical interventions ‐ exploratory laparotomy or diagnostic laparoscopy). The number of people randomised to diagnostic laparotomy and observation were 28 and 31 respectively. Males accounted for 89% of people in the diagnostic laparoscopy group and 87% of people in the observation group.
The observation protocol (expectant non‐operative management) was performed according to the hospital's previously published guidelines. Diagnostic laparoscopy was performed in the operating room under general anaesthesia after insertion of a nasogastric tube and a Foley catheter. Pneumoperitoneum was created through an infra‐umbilical incision using a Veress needle or open technique, and air leakage from the stab wound was controlled with sutures, if needed. Special attention was paid to the possibility of a tension pneumothorax developing during the procedure. A 10‐mm port was inserted and a 30‐degree laparoscope used for abdominal exploration starting with the identification of peritoneal violation at the stab wound site followed by systematic exploration of the abdominal contents using the person's position.
Excluded studies
Ten studies (Bitseff 1984; Croce 1995; Demetriades 2006; Heyns 1992; Karateke 2013; Leppäniemi 2003a; Liebenberg 1988; Sherman 1994; Velmahos 2003; Yucel 2014) were excluded from the review; nine of them were prospective observational studies. One (Leppäniemi 2003a) was a randomised trial that compared two surgical interventions (diagnostic laparoscopy and exploratory laparotomy).
Risk of bias in included studies
Figure 2 shows the 'Risk of bias' assessments of the two included studies.
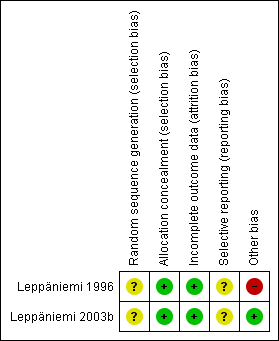
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Sequence generation (selection bias)
There was no mention of how the randomisation sequence was generated in either of the two included studies.
Allocation
Allocation was concealed by use of sealed opaque envelopes in the two included studies.
Incomplete outcome data
In Leppäniemi 1996 all 51 people who were randomised completed the study, and there were complete data on the outcomes sought for this review. Data were collected on people for 90 days following their injury.
In Leppäniemi 2003b of the 63 people randomised there were 4 dropouts; 3 were associated with protocol violation and 1 person refused consent. The published report states "two underwent a nontherapeutic laparotomy and one was treated nonoperatively; all three people recovered without complications." (p.637) As the report does not specify to which study group these people were randomised, it is not possible to analyse the data on an intention‐to‐treat basis. Data are presented for the remaining 59 people only, on a per‐protocol basis. The duration of the post‐injury follow‐up period is not reported in this study.
Selective reporting
We were unable to assess selective reporting as the protocols of both included studies were destroyed following publication of the results, which was stated as being in accordance with the requirements of the researchers' institutional review board.
Other potential sources of bias
In Leppäniemi 1996 people in the observation group were monitored more closely than people in the surgical group.
In Leppäniemi 2003b there were statistically significant differences between groups at baseline in terms of injury severity scores and abdominal trauma index, which were higher in the diagnostic laparoscopy group.
Effects of interventions
Primary outcome
Mortality
No one died in either of the included studies.
Secondary outcomes
Need for rescue intervention
Leppäniemi 1996: Four (16.7%) of the 24 people in the observation group required surgical intervention. (Therefore, 20 (83.3%) of the 24 people in the observation group were successfully managed conservatively). Two people developed peritonitis from a perforated colon 6 and 18 hours, respectively, after admission. One person had an intra‐abdominal haemorrhage from a lacerated liver 44 hours after admission. The fourth patient was initially discharged 3 days after admission but was readmitted 52 days after discharge with pleural empyema. At surgery, a perforated stomach that had herniated through a laceration in the diaphragm was seen.
Leppäniemi 2003b: There was no significant difference in therapeutic operations between the two groups: 3 of 28 in the diagnostic laparoscopy group versus 1 of 31 in the observation group (P = 0.337).
Morbidity
Leppäniemi 1996: Five of 27 (18.5%) people in the surgical group and 2 of 24 (8.3%) people in the observation group had early morbidity. The difference was not statistically significant, P = 0.42 (Fischer's exact). The complications in the surgical group were pulmonary atelectasis, intestinal obstruction, delirium, biliary fistula and pneumonia, delayed splenic rupture, pancreatic fistula and pleural effusion. Two people in the observation group had superficial thrombophlebitis, pleural empyema, candida pleuritis and wound infection.
Leppäniemi 2003b: There was no difference in morbidity between the two groups: 3 of 28 in the diagnostic laparoscopy group versus 0 of 31 in the observation group (P = 0.101).
Unnecessary surgeries
Leppäniemi 1996: In the surgical group, 15 of 27 (56%) laparotomies were non‐therapeutic. Non‐therapeutic laparotomy was defined as an operation involving the opening of the peritoneal cavity that indicated minimal injuries with no need for active surgical management. Also considered non‐therapeutic was evacuation of non‐contaminated blood from the peritoneal cavity. The management of stab injuries in the abdominal wall without the need for opening the peritoneal cavity does not meet the definition of laparotomy. Six of the 12 (50%) therapeutic surgeries were also said to be unnecessary as they involved arrest of minimal bleeding which could have been managed conservatively.
Leppäniemi 2003b: The surgical group in this study was the group in which diagnostic laparoscopy was performed. There were no unnecessary surgeries in either this or the observation group.
Discussion
Summary of main results
Two small studies involving 51 and 63 people respectively were identified through the systematic search for studies. Both studies were at moderate risk of bias as only part of the randomisation process was described and we could not obtain the study protocols.
In the first study (Leppäniemi 1996), people with penetrating abdominal stab wounds were randomised to surgery or an observation protocol, and follow‐up was for 90 days following injury. No one taking part in the study died, and there was no difference in the number of people with complications between treatment groups.
In the second study (Leppäniemi 2003b), people with equivocal peritoneal violation on local wound exploration were randomised to diagnostic laparoscopic surgery or an observation protocol. The follow‐up period was not stated. No one taking part in the study died, no unnecessary surgeries were performed, and there was no statistically significant difference between the groups in morbidity or therapeutic surgery.
Based on the findings of two small studies, there is no evidence to support the use of surgery (including diagnostic laparoscopy) over an observation protocol for people with asymptomatic abdominal stab wounds.
Overall completeness and applicability of evidence
With the help of the Cochrane Injuries Group, we searched a variety of biomedical science databases, conference abstracts, trial registers and the Internet, and identified only 2 studies involving a total of 114 people. Clinical evidence on this topic is therefore incomplete.
Despite the lack of evidence from randomised controlled trials, an observation protocol for people with blunt abdominal injuries has been accepted as routine practice in some centres (Como 2010; Gibson 2006; Lenzini 2006; Miller 2002; Ozturk 2004; Schroeppel 2007).
Quality of the evidence
We assessed the studies as being at moderate risk of bias. The method of generating the randomisation sequence was not reported, but allocation concealment was through use of opaque envelopes. Blinding was not possible due to the nature of surgical studies. There was no loss to follow up in 1 trial and a loss of 4 (out of 63) people in the second trial. We were unable to assess selective reporting as we could not obtain the study protocols.
Agreements and disagreements with other studies or reviews
There are only two RCTs on this topic, and we did not come across any other systematic reviews of RCTs on this topic when screening the search results.
Experts generally support observation as the management of choice for both blunt and penetrating abdominal injuries, provided patients are asymptomatic. This is particularly so with the emerging new technologies used in damage‐control resuscitation and transvascular interventions in the management of blunt abdominal injury with associated spleen or liver injury (Stengel 2015). Diagnostic accuracy is required to select patients who should be managed with an observation protocol. The Eastern Association for the Surgery of Trauma (EAST) has developed a guideline for the screening of people with blunt abdominal trauma into observation and surgical groups (Hoff 2002).
In another publication, the EAST Practice Mangement Committee searched in PubMed for data published in English from 1960 to 2007 on non‐operative management of penetrating abdominal trauma, for the development of a guideline on selective management of penetrating abdominal trauma. Evidence for the guideline was from observational studies and one RCT. The guideline supports an observation protocol for the management of abdominal stab wounds that are haemodynamically stable and without peritonitis, but is inconclusive on the management of non‐tangential gun shot wounds that are asymptomatic (Como 2010). In abdominal stab wounds with eviscerated omentum in the haemodynamically stable patient, arguments exist for and against laparotomy versus an observation protocol (Como 2010). Some experts have recommended observation for omental evisceration without peritoneal signs (Huizinga 1987). Management of thoracoabdominal trauma also remains controversial (Parreira 2008). Though the diagnosis of diaphragmatic injury may be made with the use of new generation computerised tomography, there are questions on managing patients with an observation protocol using these technologies in view of the low risk of herniation and high risk of strangulation among those with herniation (Parreira 2008).
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

