Levonorgestrel intrauterine system for endometrial protection in women with breast cancer on adjuvant tamoxifen
Abstract
Background
Adjuvant tamoxifen reduces the risk of breast cancer recurrence in women with oestrogen receptor‐positive breast cancer. Tamoxifen also increases the risk of postmenopausal bleeding, endometrial polyps, hyperplasia, and endometrial cancer. The levonorgestrel‐releasing intrauterine system (LNG‐IUS) causes profound endometrial suppression. This systematic review considered the evidence that the LNG‐IUS prevents the development of endometrial pathology in women taking tamoxifen as adjuvant endocrine therapy for breast cancer.
Objectives
To determine the effectiveness and safety of levonorgestrel intrauterine system (LNG‐IUS) in pre‐ and postmenopausal women taking adjuvant tamoxifen following breast cancer for the outcomes of endometrial and uterine pathology including abnormal vaginal bleeding or spotting, and secondary breast cancer events.
Search methods
We searched the following databases: Cochrane Menstrual Disorders and Subfertility Group Specialised Register (MDSG), Cochrane Breast Cancer Group Specialised Register (CBCG), Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Abstracts of Reviews of Effects (DARE), The Cochrane Library, clinicaltrials.gov, The World Health Organisation International Trials Registry, ProQuest Dissertations & Theses, MEDLINE, EMBASE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), PsycINFO, Web of Science, OpenGrey, LILACS, PubMed, and Google. The final search was performed in October 2015.
Selection criteria
Randomised controlled trials of women with breast cancer on adjuvant tamoxifen that compared endometrial surveillance alone (control condition) versus the LNG‐IUS with endometrial surveillance (experimental condition) on the incidence of endometrial pathology.
Data collection and analysis
Study selection, risk of bias assessment and data extraction were performed independently by two review authors. The primary outcome measure was endometrial pathology (including polyps, endometrial hyperplasia, or endometrial cancer) diagnosed at hysteroscopy or endometrial biopsy. Secondary outcome measures included fibroids, abnormal vaginal bleeding or spotting, breast cancer recurrence, and breast cancer‐related deaths. The overall quality of evidence was rated using GRADE methods.
Main results
Four randomised controlled trials involving 543 women were identified and are included in this review. In the included studies, the active treatment arm was the 20 μg/day levonorgestrel‐releasing intrauterine system (LNG‐IUS) plus endometrial surveillance; the control arm was endometrial surveillance alone. In tamoxifen users, the LNG‐IUS led to a reduction in the incidence of endometrial polyps over both a 12‐month period (Peto OR 0.22, 95% CI 0.08 to 0.64, 2 studies, n = 212, I² = 0%) and over a long‐term follow‐up period (24 to 60 months) (Peto OR 0.22, 95% CI 0.13 to 0.39, 4 studies, n = 417, I² = 0%, moderate quality evidence). Also the LNG‐IUS led to a reduction in the incidence of endometrial hyperplasia over a long‐term follow‐up period (24 to 60 months) (Peto OR 0.13, 95% CI 0.03 to 0.67, four studies, n = 417, I² = 0%, moderate quality evidence). However, it should be noted that the number of events of endometrial hyperplasia was low (n = 6). None of the trials were sufficiently powered to detect whether LNG‐IUS leads to significant changes in the incidence of endometrial cancer in tamoxifen users. At 12 months of follow‐up abnormal vaginal bleeding or spotting was more common in the LNG‐IUS treatment group (Peto OR 7.26, 95% CI 3.37 to 15.66, 3 studies, n = 376, I² = 0%, moderate quality evidence). By 24 months of follow‐up, abnormal vaginal bleeding or spotting occurred less frequently compared to 12 months of follow‐up in the LNG‐IUS treatment group but was still more common than the control group (Peto OR 2.72, 95% CI 1.04 to 7.10, 2 studies, n = 233, I² = 0%, moderate quality evidence). By 60 months of follow‐up, no cases of abnormal vaginal bleeding or spotting were reported in either group. The numbers of events for the following outcomes were low: fibroids (n = 13), breast cancer recurrence (n = 18), and breast cancer‐related deaths (n = 16). There was no evidence of a difference between the LNG‐IUS treatment group and controls for these outcomes. The quality of the evidence was judged as moderate, due to limited sample sizes and low event rates for the outcome comparisons.
Authors' conclusions
The LNG‐IUS reduces the incidence of benign endometrial polyps and endometrial hyperplasia in women with breast cancer taking tamoxifen. At 12 and 24 months of follow‐up, the LNG‐IUS increased abnormal vaginal bleeding or spotting among women in the treatment group compared to those in the control. There is no clear evidence from the available randomised controlled trials that the LNG‐IUS prevents endometrial cancer in these women. There is no clear evidence from the available randomised controlled trials that the LNG‐IUS affects the risk of breast cancer recurrence or breast cancer‐related deaths. Larger studies are necessary to assess the effects of the LNG‐IUS on the incidence of endometrial cancer, and to determine whether the LNG‐IUS might have an impact on the risk of secondary breast cancer events.
PICOs
Plain language summary
Levonorgestrel intrauterine system (LNG‐IUS) for endometrial protection in women with breast cancer taking tamoxifen to prevent recurrence
Review question:
Cochrane authors investigated whether the levonorgestrel‐releasing intrauterine system (LNG‐IUS) can reduce the risk of endometrial polyps, abnormal thickening of the lining of the uterus and endometrial cancer in women taking tamoxifen following breast cancer. The review also investigated whether use of the LNG‐IUS influences the risk of abnormal vaginal bleeding or spotting, fibroids, breast cancer recurrence or death in women taking tamoxifen following breast cancer.
Background:
Tamoxifen is commonly used by women to reduce the risk of breast cancer recurrence. Tamoxifen can also cause abnormal changes to the lining of the uterus (endometrium), including polyps and cancer. The LNG‐IUS is a uterine device that releases the synthetic hormone levonorgestrel into the endometrium and causes marked endometrial suppression. As levonorgestrel is a progestin, and many breast cancers are progesterone‐sensitive, it is important to study the safety of the LNG‐IUS in breast cancer survivors.
Study characteristics:
We included four randomised controlled trials involving 543 women. The studies took place in the United Kingdom, Turkey, Egypt and Hong Kong, and the primary outcome in all studies was abnormal changes in the lining of the uterus. Three studies reported on the outcome of fibroids. Three studies reported on abnormal vaginal bleeding or spotting. Two studies reported on the outcomes of breast cancer recurrence, and three studies reported on the outcomes of breast cancer‐related death. The evidence is current to October 2015.
Key results:
This review suggests that the LNG‐IUS can reduce the risk of endometrial polyps and endometrial hyperplasia over a long‐term follow‐up period (24 to 60 months) in women taking tamoxifen following breast cancer. At 12 and 24 months of follow‐up, more women in the LNG‐IUS group experienced abnormal vaginal bleeding or spotting. However by 60 months of follow‐up, no abnormal vaginal bleeding or spotting was reported in either group. There were insufficient data to show whether there is any effect on incidence of endometrial cancer (a cancer originating in glandular tissue), fibroids, breast cancer recurrence, or breast cancer‐related death.
Quality of the evidence:
The quality of the evidence was judged as moderate, due to limited sample sizes and low event rates for the outcome comparisons. Larger studies are necessary to assess the effects of the LNG‐IUS on the incidence of endometrial cancer, and the impact of the LNG‐IUS on the risk of secondary breast cancer events.
Authors' conclusions
Summary of findings
| The LNG‐IUS with endometrial surveillance compared to endometrial surveillance alone for endometrial protection in women with breast cancer on adjuvant tamoxifen | ||||||
| Patient or population: endometrial protection in women with breast cancer on adjuvant tamoxifen | ||||||
| Outcomes | Illustrated comparative risks* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Assumed Risk | Corresponding Riks | |||||
| Endometrial surveillance alone | LNG‐IUS with endometrial surveillance | |||||
| Endometrial Polyps | Moderate | OR 0.22 | 417 | ⊕⊕⊕⊝ | ||
| 235 per 1000 | 63 per 1000 | |||||
| Endometrial Hyperplasia | Moderate | OR 0.13 | 417 | ⊕⊕⊕⊝ | ||
| 28 per 1000 | 4 per 1000 | |||||
| Endometrial Cancer | Moderate | not estimable | 154 | ⊕⊕⊕⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Fibroids | Moderate | OR 0.48 | 314 | ⊕⊕⊕⊝ | ||
| 58 per 1000 | 29 per 1000 | |||||
| Abnormal Vaginal Bleeding or Spotting | Moderate | OR 7.26 | 376 | ⊕⊕⊕⊝ | ||
| 17 per 1000 | 113 per 1000 | |||||
| Abnormal Vaginal Bleeding or Spotting | Moderate | OR 2.72 | 233 | ⊕⊕⊕⊝ | ||
| 42 per 1000 | 107 per 1000 | |||||
| Abnormal Vaginal Bleeding or Spotting | Moderate | not estimable | 94 | ⊕⊕⊕⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Breast Cancer Recurrence | Moderate | OR 1.74 | 154 | ⊕⊕⊕⊝ | ||
| 80 per 1000 | 131 per 1000 | |||||
| Breast Cancer‐related Death | Moderate | OR 1.02 | 277 | ⊕⊕⊕⊝ | ||
| 69 per 1000 | 70 per 1000 | |||||
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 limited sample size and low event rate | ||||||
Background
Description of the condition
Breast cancer is the most common cancer in women, affecting up to one in eight women in developed countries (www.cancer.org). Most of these cancers express the oestrogen receptor (ER) and progesterone receptor (PR). Adjuvant treatment in most cases includes anti‐oestrogen therapy. For most premenopausal and many postmenopausal women this is with the selective ER modulator tamoxifen. Five‐year treatment with tamoxifen is associated with a 41% relative reduction in the annual risk of relapse and a 34% relative reduction in the annual risk of death among those women with ER‐positive breast cancer (EBCTCG 2005). Additionally, ten‐year treatment with tamoxifen is associated with significant reductions in the risk of breast cancer recurrence, breast cancer mortality and overall mortality in women with ER‐positive breast cancer (Davies 2013).
Tamoxifen is a selective ER modulator (SERM), which inhibits growth of breast cancer by competitive antagonism at the ER level. However, it has partial agonist effects on the skeletal system, lipid metabolism, the vagina, and the uterus. This oestrogenic effect in the uterus may promote the development of endometrial polyps, uterine fibroids, and endometrial hyperplasia (Cohen 2004; Kedar 1994) and causes a two‐fold increase in the relative risk of endometrial cancer (Van Leeuwen 1994). These effects appear to be largely confined to postmenopausal women. Premenopausal women do not appear to have an increased risk of endometrial cancer while taking tamoxifen (ACOG 2006; Davies 2013). Despite this adverse endometrial profile for tamoxifen, for most women with breast cancer the benefits of taking tamoxifen for 5 to 10 years outweigh the risks. However, benign and malignant uterine pathology in tamoxifen users is a significant clinical problem (Coates 2007).
Description of the intervention
The contraceptive levonorgestrel intrauterine system (LNG‐IUS) releases 20 μg of levonorgestrel daily from a central core. Systemic concentrations of levonorgestrel are low and most of the progestogen is delivered to the endometrial cavity (Xiao 1990), where it causes profound suppression and decidualisation of the endometrium and glandular atrophy (Scommegna 1970).
How the intervention might work
Because of the profound anti‐proliferative effect, the LNG‐IUS is thought to reduce the risk of endometrial hyperplasia and endometrial cancer, and may be effective in treating established endometrial hyperplasia. The LNG‐IUS has been used in women with breast cancer taking tamoxifen as a way of preventing endometrial proliferation. However, the safety of the LNG‐IUS following oestrogen or progesterone receptor‐positive breast cancer is unclear. A case control study from Finland suggested the LNG‐IUS is associated with an increased risk with breast cancer (Lyytinen 2009). Small observational studies suggest that the LNG‐IUS does not adversely impact breast cancer prognosis (Trinh 2008).
Why it is important to do this review
This systematic review evaluated all available data from randomised controlled trials to assess the effectiveness of the LNG‐IUS in preventing the development of endometrial pathology (polyps, hyperplasia, and cancer) in pre‐ and postmenopausal women taking adjuvant tamoxifen following breast cancer. Additionally, it is important to determine the effect of the LNG‐IUS in regards to developing fibroids, abnormal vaginal bleeding or spotting and secondary breast cancer events.
Objectives
To determine the effectiveness and safety of levonorgestrel intrauterine system (LNG‐IUS) in pre‐ and postmenopausal women taking adjuvant tamoxifen following breast cancer for the outcomes of endometrial and uterine pathology including abnormal vaginal bleeding or spotting, and secondary breast cancer events.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) were eligible for inclusion. Quasi‐randomised and non‐randomised studies were excluded.
Types of participants
Pre‐ and postmenopausal women with breast cancer on adjuvant tamoxifen were eligible for inclusion. Women were excluded if they had any of the following conditions: contraindications to the LNG‐IUS, evidence of recurrent breast cancer prior to LNG‐IUS insertion, or history of malignant disease other than breast cancer.
Types of interventions
Comparisons of the LNG‐IUS combined with endometrial surveillance (experimental condition) versus endometrial surveillance alone (control condition).
Types of outcome measures
Primary outcomes
1. Endometrial polyps
2. Endometrial hyperplasia
3. Endometrial cancer
Secondary outcomes
4. Fibroids
5. Abnormal vaginal bleeding or spotting
6. Breast cancer recurrence
7. Breast cancer‐related death
Search methods for identification of studies
Using a search strategy developed in consultation with the Trials Search Coordinator for the Cochrane Menstrual Disorders and Subfertility Group (MDSG), we searched the following databases for all published and unpublished RCTs that compared the LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, without language restrictions.
Electronic searches
The searches were conducted in October 2015 and designed for the following databases: the Cochrane Menstrual Disorders and Subfertility Group Specialised Register (MDSG), see Appendix 1; Cochrane Breast Cancer Group Specialised Register (CBCG), see Appendix 2; Cochrane Central Register of Controlled Trials (CENTRAL), see Appendix 3; Cochrane Database of Abstracts of Reviews of Effects (DARE); The Cochrane Library, see Appendix 4; clinicaltrials.gov; The World Health Organisation International Trials Registry; ProQuest Dissertations & Theses; MEDLINE (1946 to October 2015), see Appendix 5; EMBASE (1980 to October 2015), see Appendix 6; CINAHL (Cumulative Index to Nursing and Allied Health Literature) (1982 to October 2015), see Appendix 7; PsycINFO, see Appendix 8; Web of Science; OpenGrey; LILACS; PubMed (1946 to October 2015), see Appendix 9; and Google. The search strategies for databases without appendices used similar terms as the MDSG and PubMed search strategies.
Searching other resources
We searched references of relevant systematic reviews and RCTs.
Data collection and analysis
Selection of studies
Studies were selected in accordance with the described criteria. Two review authors (SD and HIS) independently and in a standardised method assessed eligibility of the studies retrieved from the search, see Figure 1. Disagreement was resolved by consensus.

Study flow diagram
Data extraction and management
All data were extracted independently by two authors (SD and HIS) using forms designed according to the Cochrane guidelines (Higgins 2011). For each included trial, information was collected regarding the location of the study, methods of the study (as per risk of bias assessment checklist), the participants (age range, eligibility criteria), the nature of the interventions, and data relating to the outcomes specified above.
Assessment of risk of bias in included studies
The risk of bias for all studies that were deemed eligible for the review was assessed independently by two review authors (SD and HIS) using the Cochrane 'Risk of bias' assessment tool (Higgins 2011). Discrepancies were resolved by discussion. Trials were screened and analysed for the following risk of bias criteria.
1. Selection bias (random sequence generation and allocation concealment)
2. Performance bias (blinding of participants and personnel)
3. Detection bias (blinding of outcome assessment)
4. Attrition bias (incomplete outcome data)
5. Reporting bias (selective reporting)
6. Other bias
Each domain was assigned a high, low or unclear risk of bias rating. This information is presented in 'Risk of bias' tables (see Figure 2; Figure 3) and the text of the review.

Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
Measures of treatment effect
For dichotomous data (all the outcome measures in this review), results for each study were expressed as Peto odds ratios (Peto OR) with 95% confidence intervals (CI) and combined for meta‐analysis with Review Manager 5 software using a fixed‐effect model. The Peto method was selected because it performs well when events are very rare (Higgins 2011).
Unit of analysis issues
No unit of analysis issues were identified due to the nature of the data generated.
Dealing with missing data
The data were analysed on a intent‐to‐treat basis. If there had been missing data, we would have sought further information directly from the authors of the RCTs. Where no additional information was forthcoming, we analysed only the available data.
Assessment of heterogeneity
Heterogeneity (variation) between the results of different studies was examined by inspecting the scatter in the data points on a graph and the overlap in their CIs; and, more formally, by considering the I² statistic and the Chi² test P value. We would have interpreted a low P value (or a large Chi² statistic relative to its number of degrees of freedom) as providing evidence of heterogeneity of intervention effects (a variation in effect estimates beyond chance). We would have interpreted the I² statistic, in conjunction with consideration of the magnitude and direction of the effects seen, as follows:
-
0% to 40%, might not be important;
-
30% to 60%, may represent moderate heterogeneity;
-
50% to 90%, may represent substantial heterogeneity;
-
75% to 100%, considerable heterogeneity.
Assessment of reporting biases
To minimise the potential impact of reporting biases, the authors conducted a comprehensive search for eligible articles and were alert for potential duplication of data. If 10 or more studies were included in an analysis, funnel plots would have been constructed to detect reporting biases.
Data synthesis
We pooled the results statistically for each comparison (endometrial polyps, endometrial hyperplasia, endometrial cancer, fibroids, abnormal vaginal bleeding or spotting, breast cancer recurrence and breast cancer‐related death). The meta‐analysis was carried out using Review Manager 5. We used the fixed‐effect method of synthesising the data for the combined analysis in accordance with the guidelines of the Cochrane Menstrual Disorders and Subfertility Group. We had no continuous data to consider; however, if we had had such data we would have used mean differences (MDs) or standardised mean differences (SMDs). If a large degree of heterogeneity had been detected, a random‐effects model would have been considered.
Subgroup analysis and investigation of heterogeneity
We did not pre‐specify any subgroups for analysis and due to the nature of our findings neither a post hoc subgroup analysis nor an investigation of heterogeneity was required.
Sensitivity analysis
We planned to conduct the following sensitivity analyses for the primary outcomes:
-
Eligibility was restricted to studies without high risk of bias
-
A random‐effects model had been adopted
-
The summary effect measure was relative risk rather than Peto odds ratio.
Overall quality of the body of evidence: Summary of findings table
We generated a summary of findings table using GRADEpro software. This table evaluated the overall quality of the body of evidence for the review outcomes (endometrial polyps, endometrial hyperplasia, endometrial cancer, fibroids, abnormal vaginal bleeding or spotting, breast cancer recurrence and breast cancer‐related death) using GRADE criteria: study limitations (i.e., risk of bias); consistency of effect; imprecision; indirectness and publication bias. Judgments about the quality of evidence (high, moderate or low) were justified, documented and incorporated into reporting of results for each outcome.
Results
Description of studies
Results of the search
The electronic search was run in October 2015 and a total of 315 references were retrieved: MDSG = 16; CBCG = 8; CENTRAL = 5; DARE = 0; The Cochrane Library = 6; clinicaltrials.gov = 1; The World Health Organisation International Trials Registry = 1; ProQuest Dissertations & Theses = 2; MEDLINE = 54; EMBASE = 162; CINAHL = 37; Web of Science = 8; PsycINFO = 1; OpenGrey = 0; LILACS = 7; PubMed = 6; and Google = 1. From those, we identified six potential studies, which were read in full; two of these six studies were included in the previously published review. No additional reference was retrieved from the manual search. See Figure 1 for details of the screening and selection process. See Characteristics of included studies; Table 1; Table 2; Table 3; Table 4 for detailed information.
| Treatment Group | Control | P value | |
| 6 months follow‐up | |||
| Randomised | 64 | 65 | |
| Completed | 55 | 58 | |
| Abnormal vaginal bleeding or spotting | 20 | 1 | <0.001 |
| 12 months follow‐up | |||
| Completed | 55 | 58 | |
| Abnormal vaginal bleeding or spotting | 6 | 1 | 0.06 |
| Endometrial polyps | 1 | 9 | 0.02 |
| Endometrial hyperplasia | 0 | 0 | |
| Fibroids | 1 | 2 | 1.0 |
| 24 months follow‐up | |||
| Completed | 55 | 57 | |
| Abnormal vaginal bleeding or spotting | 6 | 3 | 0.45 |
| 45 months follow‐up | |||
| Completed | 48 | 52 | |
| Abnormal vaginal bleeding or spotting | 0 | 0 | |
| 60 months follow‐up | |||
| Completed | 46 | 48 | |
| Abnormal vaginal bleeding or spotting | 0 | 0 | |
| Endometrial polyps | 2 | 16 | < 0.001 |
| Endometrial hyperplasia | 0 | 1 | 1.0 |
| Endometrial cancer | 0 | 0 | |
| Fibroids | 1 | 2 | 1.0 |
| Breast cancer recurrence | 10 | 6 | 0.25 |
| Breast cancer‐related deaths | 6 | 5 | 0.71 |
| Treatment Group | Control | P value | |
| 12 months follow‐up | |||
| Randomised | 64 | 58 | |
| Completed | 47 | 52 | |
| Endometrial polyps | 1 | 4 | 0.4 |
| Endometrial hyperplasia | 0 | 1 | |
| Fibroids | 1 | 3 | 0.2 |
| Final follow‐up (24, 36, or 48 months) | |||
| Completed at 24 months | 31 | 29 | |
| Completed at 36 months | 19 | 20 | |
| Completed at 48 months | 6 | 9 | |
| Endometrial polyps | 3 | 8 | |
| Endometrial hyperplasia | 0 | 1 | |
| Endometrial cancer | 0 | 0 | |
| Breast cancer recurrence | 1 | 1 | |
| Breast cancer‐related deaths | 2 | 2 |
| Treatment Group | Control | P value | |
| 5 months follow‐up | |||
| Randomised | 70 | 72 | |
| Completed | 70 | 72 | |
| Abnormal vaginal bleeding or spotting | 7 | 0 | |
| 12 months follow‐up | |||
| Randomised | 70 | 72 | |
| Completed | 70 | 72 | |
| Abnormal vaginal bleeding or spotting | 0 | 0 | |
| 36 months follow‐up | |||
| Randomised | 70 | 72 | |
| Completed | 70 | 72 | |
| Endometrial polyps | 4 | 14 | < 0.05 |
| Endometrial hyperplasia | 0 | 4 | < 0.05 |
| Treatment Group | Control | P value | |
| 12 months follow‐up | |||
| Randomised | 75 | 75 | |
| Completed | 60 | 63 | |
| Abnormal vaginal bleeding or spotting | 22 | 2 | <0.001 |
| Breast cancer‐related deaths | 0 | 1 | |
| 24 months follow‐up | |||
| Completed | 59 | 62 | |
| Abnormal vaginal bleeding or spotting | 7 | 2 | 0.08 |
| Endometrial polyps | 1 | 10 | 0.02 |
| Endometrial hyperplasia | 0 | 0 | |
| Fibroids | 2 | 4 | 1.0 |
Included studies
Study design and setting
The searches identified four randomised controlled trials for consideration in this review (Chan 2007; Gardner 2000; Kesim 2008; Omar 2010). These trials took place in Egypt (Omar 2010), Turkey (Kesim 2008), United Kingdom (Gardner 2000), and Hong Kong (Chan 2007). The Gardner 2000 and Chan 2007 trials published long‐term follow‐up of their trials (Gardner et al, 2009 and Wong et al, 2013 respectively).
Participants
The trials included 543 pre‐ and postmenopausal women with breast cancer on adjuvant tamoxifen; 273 women in the treatment group and 270 women in the control group.
Interventions
All four trials compared endometrial surveillance plus the LNG‐IUS, which releases 20 μg/day of the synthetic progestogen levonorgestrel, to endometrial surveillance alone. The Chan 2007 trial (follow up: 60 months) compared endometrial surveillance alone versus endometrial surveillance plus the LNG‐IUS insertion before the commencement of tamoxifen in pre‐ and postmenopausal women. The Gardner 2000 trial (follow up: 48 months) compared endometrial surveillance alone versus endometrial surveillance with insertion of the LNG‐IUS in postmenopausal women who had been taking adjuvant tamoxifen treatment for at least one year. The Kesim 2008 trial (follow up: 36 months) compared endometrial surveillance alone versus endometrial surveillance with insertion of the LNG‐IUS in postmenopausal women who had been taking adjuvant tamoxifen treatment for more than one year. The Omar 2010 trial (follow up: 24 months) compared endometrial surveillance alone versus endometrial surveillance with insertion of the LNG‐IUS before the commencement of tamoxifen in pre‐ and postmenopausal women who required postoperative adjuvant tamoxifen.
Outcomes
All four trials reported endometrial polyps diagnosed at hysteroscopy with endometrial biopsy (Chan 2007; Gardner 2000; Kesim 2008; Omar 2010).
All four trials reported endometrial hyperplasia diagnosed at hysteroscopy with endometrial biopsy (Chan 2007; Gardner 2000; Kesim 2008; Omar 2010).
Two of the four trials reported no cases of endometrial cancer (Chan 2007; Gardner 2000).
Three of the four trials reported fibroids (Chan 2007; Gardner 2000; Omar 2010).
Three of the four trials reported abnormal vaginal bleeding or spotting (Chan 2007; Kesim 2008; Omar 2010).
Two of the four trials reported breast cancer recurrence (Chan 2007; Gardner 2000).
Three of the four trials reported breast cancer‐related death (Chan 2007; Gardner 2000; Omar 2010).
Excluded studies
There were no excluded studies.
Risk of bias in included studies
See Figure 2 and Figure 3 for detailed information.
Allocation
Three trials were assessed as low risk of selection bias related to sequence generation as all used computer generated random number series for allocation (Chan 2007; Kesim 2008; Omar 2010). One trial did not describe the sequence generation method used and was rated as unclear risk of selection bias related to sequence generation (Gardner 2000).
All trials were rated as low risk of selection bias related to allocation concealment as all used pre‐prepared, serially‐numbered sealed envelopes (Chan 2007; Gardner 2000; Kesim 2008; Omar 2010).
Blinding
All trials were rated as low risk of detection and performance bias as the pathologists (i.e., outcome assessors) were blinded (Chan 2007; Gardner 2000; Kesim 2008; Omar 2010). Even though the provider and participant were not blinded given the clinical intervention (insertion of the LNG‐IUS), the blinding of providers and participants is considered unlikely to influence the outcomes.
Incomplete outcome data
Two trials were judged to be at low risk of attrition bias as the majority of randomised participants were included in the final analyses (Kesim 2008; Omar 2010). For both trials, there were no evidence of differences in baseline data between women who completed and did not complete the study.
One trial was judged as unclear risk of attrition bias (Chan 2007). At 12 months of follow‐up, 16/129 (12%) participants (7 in control group and 9 in treatment group) were lost to follow‐up or dropped out. At 60 months of follow‐up, 35/129 (27%) participants (17 in the control group and 18 in the treatment group) were lost to follow‐up.
One trial was judged as unclear risk of attrition bias (Gardner 2000). At 12 months of follow‐up, 23/122 (19%) of participants (6 in control group and 17 in treatment group) were lost to follow‐up or dropped out. There were no evidence of differences in baseline data between women who completed and did not complete the study; hence the 12 months follow‐up data are at low risk of attrition bias. However, the 24, 36 and 48 months follow‐up data are considered at high risk of attrition bias due to the high rate of attrition. At 24 months of follow‐up, 62/122 (51%) of participants were lost to follow‐up or dropped out. At 36 months of follow‐up, 83/122 (68%) of participants were lost to follow‐up or dropped out. At 48 months of follow‐up, 107/122 (88%) of participants were lost to follow‐up or dropped out.
Selective reporting
All four trials were considered at low risk of reporting bias (Chan 2007; Gardner 2000; Kesim 2008; Omar 2010). Due to the small number of included studies (less than 10), it was not considered appropriate to construct funnel plots to detect publication bias.
Other potential sources of bias
No other potential sources of bias were identified.
Effects of interventions
See: Summary of findings table 1 LNG‐IUS with endometrial surveillance compared to endometrial surveillance alone for endometrial protection in women with breast cancer on adjuvant tamoxifen.
1. LNG‐IUS with endometrial surveillance versus endometrial surveillance alone
Primary outcomes
1.1 Endometrial polyps
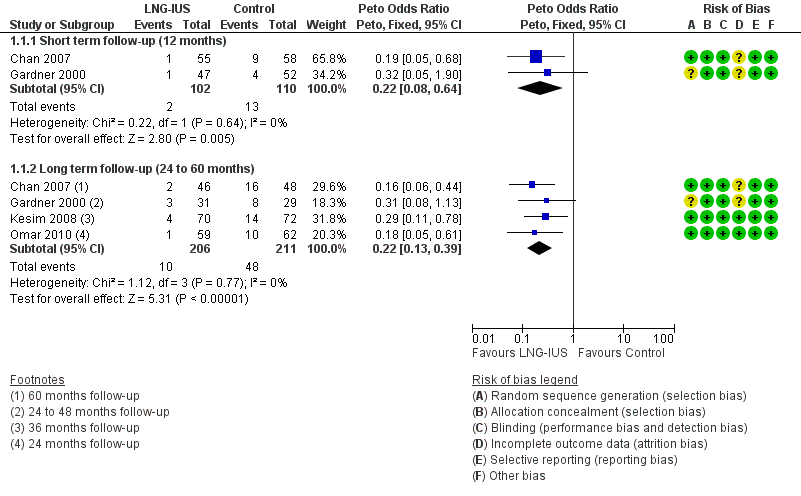
At short‐term follow‐up (12 months), the pooled data from two trials (Chan 2007; Gardner 2000) suggested a reduction in the incidence of endometrial polyps in the LNG‐IUS users group (2.0%) compared to endometrial surveillance alone (11.8%) (Peto OR 0.22, 95% CI 0.08 to 0.64, two RCTS, n = 212, I² = 0%) (Analysis 1.1,Figure 4).
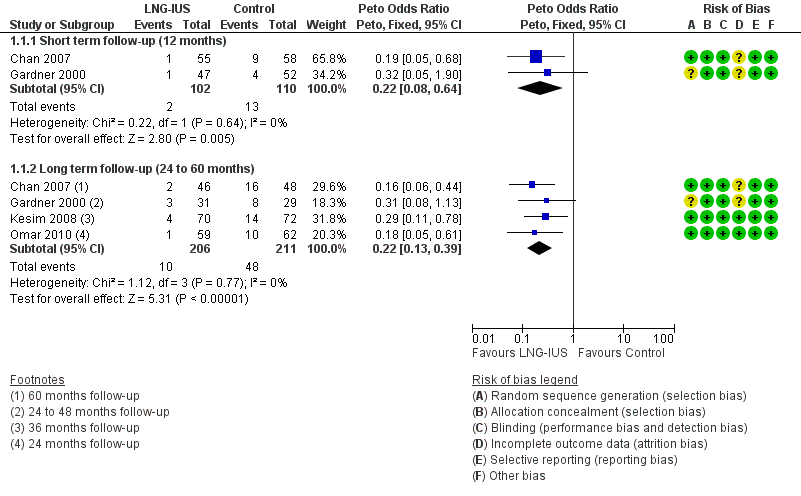
Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.1 Endometrial Polyps.
At long‐term follow‐up (24 to 60 months), the pooled data from all four trials (Chan 2007; Gardner 2000; Kesim 2008; Omar 2010) suggested a reduction in the incidence of endometrial polyps in the LNG‐IUS users group (4.9%) compared to endometrial surveillance alone (22.7%) (Peto OR 0.22, 95% CI 0.13 to 0.39, four RCTs, n = 417, I² = 0%, moderate quality evidence) (Analysis 1.1,Figure 4).
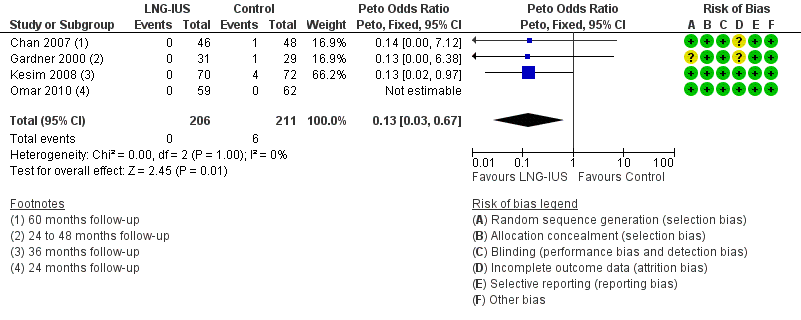
1.2 Endometrial hyperplasia
At long‐term follow‐up (24 to 60 months), the pooled data from all four trials (Gardner 2000; Chan 2007; Kesim 2008; Omar 2010) showed only six cases of endometrial hyperplasia in the control group, which suggests a reduction in the incidence of endometrial hyperplasia in the LNG‐IUS users compared to the control (Peto OR 0.13, 95% CI 0.03 to 0.67, four RCTs, n = 417, moderate quality evidence) (Analysis 1.2, Figure 5).
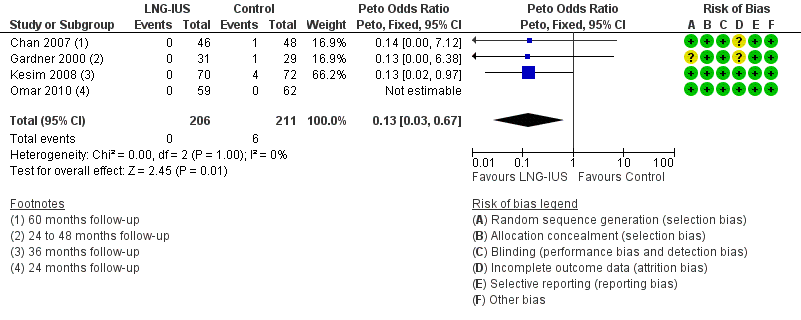
Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.2 Endometrial Hyperplasia.
1.3 Endometrial cancer
The included studies reported no cases of endometrial cancer. Hence, we could not calculate statistics for the endometrial cancer outcome.
Secondary outcomes
1.4 Fibroids
Pooled data from three trials (Chan 2007; Gardner 2000; Omar 2010) showed no evidence of a difference in the incidence of fibroids in LNG‐IUS users (2.6%) compared to the control group with endometrial surveillance (5.6%) (Peto OR 0.48, 95% CI 0.16 to 1.46, three RCTs, n = 314, I² = 0%, moderate quality evidence) (Analysis 1.4, Figure 6).

Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.4 Fibroids.
1.5 Abnormal vaginal bleeding or spotting
At 12 months of follow‐up, three trials reported on abnormal vaginal bleeding or spotting in the LNG‐IUS and control groups (Chan 2007;Kesim 2008; Omar 2010), and at 24 months of follow‐up two of these trials (Chan 2007; Omar 2010) reported on abnormal vaginal bleeding or spotting. Only 1 trial (Chan 2007) reported on findings at 45 and 60 months of follow‐up At 12 months of follow‐up, there was more abnormal vaginal bleeding or spotting in the LNG‐IUS treatment group (15.2%) compared to endometrial surveillance alone (1.6%) (Peto OR 7.26, 95% CI 3.37 to 15.66, three RCTs, n = 376, I² = 0%, moderate quality evidence) (Analysis 1.5, Figure 7). At 24 months of follow‐up, abnormal vaginal bleeding or spotting was reduced but still higher in the LNG‐IUS group (11.4%) compared to the control (4.2%) (Peto OR 2.72, 95% CI 1.04 to 7.10, two RCTs, n = 233, I² = 0%, moderate quality evidence) (Analysis 1.5, Figure 7). By 45 and 60 months of follow‐up, no cases of abnormal vaginal bleeding or spotting were reported in either group (Analysis 1.5, Figure 7).

Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.5 Abnormal Vaginal Bleeding or Spotting.
1.6 Breast cancer recurrence
Pooled data from two trials showed no evidence of a difference in breast cancer recurrence in LNG‐IUS users (14.3%) compared to the control group (9.1%) with endometrial surveillance (Peto OR 1.74, 95% CI 0.64 to 4.74, two RCTs, n = 154, I² = 0%, moderate quality evidence) (Analysis 1.6, Figure 8) (Chan 2007; Gardner 2000).

Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.6 Breast Cancer Recurrence.
1.7 Breast cancer‐related death
Pooled data from three trials showed no evidence of a difference in breast cancer‐related deaths in LNG‐IUS users (5.8%) compared to the control group (5.7%) with endometrial surveillance (Peto OR 1.02, 95% CI 0.36 to 2.84, three RCTs, n = 277, I² = 0%, moderate quality evidence) (Analysis 1.7, Figure 9) (Chan 2007; Gardner 2000; Omar 2010).

Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.7 Breast Cancer‐related Death.
Sensitivity analyses
We did not conduct the planned sensitivity analysis by risk of bias, because risk of bias was similar across the included studies.
We conducted the planned sensitivity analyses by statistical model and effect estimate. When switching the pooled estimate from Peto odds ratio to Mantel‐Haenszel risk ratio and fixed or random effects for all outcomes, only the pooled estimate for the endometrial hyperplasia outcome changed, to show no evidence of a difference between the groups (RR fixed effect 0.19, 95% CI 0.03 to 1.15, four RCTs, n = 417).
Discussion
Summary of main results
See Summary of findings table 1.
This review included four randomised controlled trials that compared endometrial protection by the 20 μg/day levonorgestrel‐releasing intrauterine system (LNG‐IUS) plus endometrial surveillance versus endometrial surveillance alone in women with breast cancer on adjuvant tamoxifen. The pooled data from the included studies found that the LNG‐IUS led to a significant reduction in the incidence of endometrial polyps over a 12‐month period and a long‐term follow‐up period (24 to 60 months) among women with breast cancer taking tamoxifen. Also the LNG‐IUS led to a reduction in endometrial hyperplasia over a long‐term follow‐up period (24 to 60 months). The pooled data showed there was more abnormal vaginal bleeding or spotting in the LNG‐IUS treatment group compared to the control at 12 months and 24 months of follow‐up. However, there was a gradual reduction of abnormal vaginal bleeding or spotting from 12 to 24 months, and no bleeding or spotting in either group was reported at 45 or 60 months of follow‐up. Additionally, there was no difference in the odds of fibroids (n = 13), breast cancer recurrence (n = 18), and breast cancer‐related deaths (n = 16) between the LNG‐IUS treatment groups and controls. Since none of the studies reported cases of endometrial cancer, there were insufficient data to show an effect on the incidence of endometrial cancer.
Overall completeness and applicability of evidence
All four included studies (Chan 2007; Gardner 2000; Kesim 2008; Omar 2010) used the 'gold standard' of hysteroscopy and endometrial biopsy to diagnose endometrial pathology. Endometrial pathology prior to randomisation was excluded by hysteroscopy and endometrial biopsy; any endometrial pathology detected at baseline was treated. Endometrial pathology was the primary end point for all four studies. However, the timing of the primary end point assessment varied by study, ranging from 12 to 60 months.
While the four included studies differed in patient selection, inclusion criteria, secondary outcomes assessed, and overall study design (see Characteristics of included studies), adequate information was provided to answer the review question. The findings of this review provide evidence that the LNG‐IUS prevents endometrial polyps and endometrial hyperplasia in women with breast cancer using tamoxifen. However, the data are insufficient to suggest that the LNG‐IUS protects tamoxifen users from endometrial cancer.
Quality of the evidence
Using the GRADE system, the quality of the evidence for all study outcomes (i.e., endometrial polyps, endometrial hyperplasia, endometrial cancer, fibroids, abnormal vaginal bleeding or spotting, breast cancer recurrence and breast cancer‐related death) was judged as moderate (see Summary of findings table 1). For all four studies, evidence was downgraded by one level because of limited sample sizes and low event rates for the study outcomes. Also it should be noted that none of the studies were sufficiently powered to address whether the LNG‐IUS protects women on tamoxifen against endometrial cancer.
Further, a potential limitation of this review is the inclusion of both pre‐ and postmenopausal women in two of the included studies (Chan 2007; Omar 2010). This may have underestimated the effect of the levonorgestrel intrauterine system (LNG‐IUS) in preventing endometrial pathology in postmenopausal women.
Potential biases in the review process
No potential biases were identified by the authors in the review process. Based on the comprehensive literature search and included search terms, we are confident that all relevant studies were identified and included in this review.
Agreements and disagreements with other studies or reviews
No other reviews were identified.

Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.1 Endometrial Polyps.
Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.2 Endometrial Hyperplasia.

Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.4 Fibroids.

Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.5 Abnormal Vaginal Bleeding or Spotting.

Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.6 Breast Cancer Recurrence.

Forest plot of comparison: 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, outcome: 1.7 Breast Cancer‐related Death.

Comparison 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, Outcome 1 Endometrial Polyps.

Comparison 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, Outcome 2 Endometrial Hyperplasia.

Comparison 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, Outcome 3 Endometrial Cancer.

Comparison 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, Outcome 4 Fibroids.

Comparison 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, Outcome 5 Abnormal Vaginal Bleeding or Spotting.

Comparison 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, Outcome 6 Breast Cancer Recurrence.

Comparison 1 LNG‐IUS with endometrial surveillance versus endometrial surveillance alone, Outcome 7 Breast Cancer‐related Death.
| The LNG‐IUS with endometrial surveillance compared to endometrial surveillance alone for endometrial protection in women with breast cancer on adjuvant tamoxifen | ||||||
| Patient or population: endometrial protection in women with breast cancer on adjuvant tamoxifen | ||||||
| Outcomes | Illustrated comparative risks* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Assumed Risk | Corresponding Riks | |||||
| Endometrial surveillance alone | LNG‐IUS with endometrial surveillance | |||||
| Endometrial Polyps | Moderate | OR 0.22 | 417 | ⊕⊕⊕⊝ | ||
| 235 per 1000 | 63 per 1000 | |||||
| Endometrial Hyperplasia | Moderate | OR 0.13 | 417 | ⊕⊕⊕⊝ | ||
| 28 per 1000 | 4 per 1000 | |||||
| Endometrial Cancer | Moderate | not estimable | 154 | ⊕⊕⊕⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Fibroids | Moderate | OR 0.48 | 314 | ⊕⊕⊕⊝ | ||
| 58 per 1000 | 29 per 1000 | |||||
| Abnormal Vaginal Bleeding or Spotting | Moderate | OR 7.26 | 376 | ⊕⊕⊕⊝ | ||
| 17 per 1000 | 113 per 1000 | |||||
| Abnormal Vaginal Bleeding or Spotting | Moderate | OR 2.72 | 233 | ⊕⊕⊕⊝ | ||
| 42 per 1000 | 107 per 1000 | |||||
| Abnormal Vaginal Bleeding or Spotting | Moderate | not estimable | 94 | ⊕⊕⊕⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Breast Cancer Recurrence | Moderate | OR 1.74 | 154 | ⊕⊕⊕⊝ | ||
| 80 per 1000 | 131 per 1000 | |||||
| Breast Cancer‐related Death | Moderate | OR 1.02 | 277 | ⊕⊕⊕⊝ | ||
| 69 per 1000 | 70 per 1000 | |||||
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 limited sample size and low event rate | ||||||
| Treatment Group | Control | P value | |
| 6 months follow‐up | |||
| Randomised | 64 | 65 | |
| Completed | 55 | 58 | |
| Abnormal vaginal bleeding or spotting | 20 | 1 | <0.001 |
| 12 months follow‐up | |||
| Completed | 55 | 58 | |
| Abnormal vaginal bleeding or spotting | 6 | 1 | 0.06 |
| Endometrial polyps | 1 | 9 | 0.02 |
| Endometrial hyperplasia | 0 | 0 | |
| Fibroids | 1 | 2 | 1.0 |
| 24 months follow‐up | |||
| Completed | 55 | 57 | |
| Abnormal vaginal bleeding or spotting | 6 | 3 | 0.45 |
| 45 months follow‐up | |||
| Completed | 48 | 52 | |
| Abnormal vaginal bleeding or spotting | 0 | 0 | |
| 60 months follow‐up | |||
| Completed | 46 | 48 | |
| Abnormal vaginal bleeding or spotting | 0 | 0 | |
| Endometrial polyps | 2 | 16 | < 0.001 |
| Endometrial hyperplasia | 0 | 1 | 1.0 |
| Endometrial cancer | 0 | 0 | |
| Fibroids | 1 | 2 | 1.0 |
| Breast cancer recurrence | 10 | 6 | 0.25 |
| Breast cancer‐related deaths | 6 | 5 | 0.71 |
| Treatment Group | Control | P value | |
| 12 months follow‐up | |||
| Randomised | 64 | 58 | |
| Completed | 47 | 52 | |
| Endometrial polyps | 1 | 4 | 0.4 |
| Endometrial hyperplasia | 0 | 1 | |
| Fibroids | 1 | 3 | 0.2 |
| Final follow‐up (24, 36, or 48 months) | |||
| Completed at 24 months | 31 | 29 | |
| Completed at 36 months | 19 | 20 | |
| Completed at 48 months | 6 | 9 | |
| Endometrial polyps | 3 | 8 | |
| Endometrial hyperplasia | 0 | 1 | |
| Endometrial cancer | 0 | 0 | |
| Breast cancer recurrence | 1 | 1 | |
| Breast cancer‐related deaths | 2 | 2 |
| Treatment Group | Control | P value | |
| 5 months follow‐up | |||
| Randomised | 70 | 72 | |
| Completed | 70 | 72 | |
| Abnormal vaginal bleeding or spotting | 7 | 0 | |
| 12 months follow‐up | |||
| Randomised | 70 | 72 | |
| Completed | 70 | 72 | |
| Abnormal vaginal bleeding or spotting | 0 | 0 | |
| 36 months follow‐up | |||
| Randomised | 70 | 72 | |
| Completed | 70 | 72 | |
| Endometrial polyps | 4 | 14 | < 0.05 |
| Endometrial hyperplasia | 0 | 4 | < 0.05 |
| Treatment Group | Control | P value | |
| 12 months follow‐up | |||
| Randomised | 75 | 75 | |
| Completed | 60 | 63 | |
| Abnormal vaginal bleeding or spotting | 22 | 2 | <0.001 |
| Breast cancer‐related deaths | 0 | 1 | |
| 24 months follow‐up | |||
| Completed | 59 | 62 | |
| Abnormal vaginal bleeding or spotting | 7 | 2 | 0.08 |
| Endometrial polyps | 1 | 10 | 0.02 |
| Endometrial hyperplasia | 0 | 0 | |
| Fibroids | 2 | 4 | 1.0 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Endometrial Polyps Show forest plot | 4 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 1.1 Short term follow‐up (12 months) | 2 | 212 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.22 [0.08, 0.64] |
| 1.2 Long term follow‐up (24 to 60 months) | 4 | 417 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.22 [0.13, 0.39] |
| 2 Endometrial Hyperplasia Show forest plot | 4 | 417 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.03, 0.67] |
| 3 Endometrial Cancer Show forest plot | 2 | 154 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Fibroids Show forest plot | 3 | 314 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.48 [0.16, 1.46] |
| 5 Abnormal Vaginal Bleeding or Spotting Show forest plot | 3 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 5.1 12 months | 3 | 376 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.26 [3.37, 15.66] |
| 5.2 24 months | 2 | 233 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.72 [1.04, 7.10] |
| 5.3 45 months | 1 | 100 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.4 60 months | 1 | 94 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Breast Cancer Recurrence Show forest plot | 2 | 154 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.74 [0.64, 4.74] |
| 7 Breast Cancer‐related Death Show forest plot | 3 | 277 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.02 [0.36, 2.84] |

