比较开放式与封闭式手术治疗上颚移位犬齿
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Trial design: quasi‐randomised, 2‐arm parallel groups, superiority. Setting: Jordan University of Science and Technology, Jordan. Number of centres: 1. Study duration: not reported. | |
| Participants | Inclusion criteria: patients with unilateral palatally impacted maxillary canines. Exclusion criteria: not reported. Other prognostic factors: bone removal required for some patients (open: 10; closed: 11). Age: open: mean age 17.3 (SD 4.5) years; closed: mean age 17.6 (SD 2.4) years. Gender: open: 14 females, 2 males; closed: 14 females, 2 males. Number randomised: 32 (open: 16; closed: 16). Number evaluated: 32 (open: 16; closed: 16). | |
| Interventions | Comparison: open surgical exposure technique versus closed surgical exposure technique All exposures carried out under local anaesthetic and by the same surgeon. In both groups, a standard mucoperiosteal flap was raised and if the crown of the canine was covered by bone, bone was removed with a rotary instrument. This was followed by:
All patients given co‐amoxiclav 625 mg and ibuprofen 400 mg every 8 hours for 5 days starting 1 hour after end of surgery and chlorhexidine 0.2% mouthwash 3 times daily for 7 days starting 24 hours after surgery. | |
| Outcomes | Patient response – pain: worst pain experienced each day for 1 week postoperatively measured on a 1 to 10 scale; reported as daily incidence of mild (1 to 3), moderate (4 to 7) and severe (8 to 10). Length of treatment – duration of surgery: measured from initial incision until final suture, reported in minutes. | |
| Notes | Sample size calculation: not reported. Adverse effects: not reported. Funding: not reported. Declarations/conflicts of interest: not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The exposure type was randomly selected". Comment: no details given on how random sequence was generated. Additional information from correspondence: quasi‐randomisation using alternate allocation. |
| Allocation concealment (selection bias) | High risk | Quote: "Half of the participants had closed‐eruption surgical exposure of the maxillary canine. The other half had open‐eruption exposure". Comment: not possible to conceal allocation when using alternate allocation. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: it was not possible to blind the participants or personnel. One surgeon operated, however it is not clear if they were equally proficient in both surgical techniques. |
| Blinding of outcome assessment (subjective outcomes) | Unclear risk | Comment: it was not possible to blind the participants, but as they only received one of the procedures it is unlikely that they were biased. |
| Blinding of outcome assessment (objective outcomes) | Unclear risk | Blinding was not mentioned for timing of surgical duration. |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses. |
| Selective reporting (reporting bias) | Unclear risk | Through correspondence with the author, we found out that data on periodontal health was recorded, but there is no mention of this in the paper and we are unsure if this was in the original protocol. The data are not yet available |
| Other bias | Low risk | None apparent. |
| Methods | Trial design: randomised, 2‐arm parallel groups, superiority trial. Setting: University of Sheffield, Sheffield, UK. Number of centres: 3 (1 teaching hospital, 2 district general hospitals the UK). Study duration: not reported (recruitment from August 2002 to January 2007). | |
| Participants | Inclusion criteria: patients with unilateral palatally ectopic maxillary canines who required surgical exposure and orthodontic alignment; age 20 years or younger; minimal orthodontic problems other than ectopic canine; good oral hygiene and motivated to wear affixed appliances for at least 2 years. Exclusion criteria: patients with bilateral palatally ectopic maxillary canines or ectopic mandibular canines; compromising medical conditions (require antibiotic prophylaxis to prevent infective endocarditis); periodontal disease (bleeding on probing, pocket probing depths > 3 mm and decreased bone levels diagnosed from baseline panoramic imaging; cases where canine is to be brought into the position of the lateral incisor. Other prognostic factors: all tests for pretreatment comparability of groups were nonsignificant (age, gender, severity of impaction) except for side of impaction, i.e. more right‐sided in the open group (P = 0.002). Age: open: mean age 14.3 years (SD 1.3) years; closed: mean age 14.1 years (SD 1.6) years. Gender: open: 27 female, 13 male; closed: 25 female, 16 male. Number randomised: 81 (open: 40; closed: 41). Number evaluated: 71 (open: 35; closed: 36) but this varied for each outcome. | |
| Interventions | Comparison: open surgical exposure technique versus closed surgical exposure technique All surgical procedures carried out under general anaesthetic by one of two specialist surgeons at each unit, all of whom had at least 10 years' experience using both techniques. In both groups, the primary canine was extracted if present. Bone was then surgically removed, exposing the largest diameter of the ectopic canine crown, which was followed by:
Chlorhexidine digluconate 0.2% mouthwash was prescribed for both groups after surgery (10 ml 3 times per day for 7 days, starting 4 hours after surgery). | |
| Outcomes | Success: assessed by whether or not re‐exposure was required. Aesthetics: multiple outcomes, assessed separately by both a panel of orthodontists and a panel of lay people using clinical photographs 3 months after debonding of the orthodontic appliance used to align the erupted canine. Patient response (assessed 10 days postoperatively):
Length of treatment: actual surgical time in minutes from incision to last suture. Any patient requiring an overnight stay was documented. Gum/periodontal health (assessed 3 months after debonding of orthodontic appliance):
| |
| Notes | Sample size calculation: 60 participants required to detect a mean difference of 0.5 mm loss of attachment at 90% power and 5% significance. Adverse effects: re‐exposure required in 4 participants, postoperative infection requiring antibiotics (n = 1), pain from traction due to chain being bonded too close to cementoenamel junction (n = 1), re‐exposure 2 years after initial exposure (n = 1) due to slow moving tooth. Funding: "This study was supported by a grant from the British Orthodontic Society Foundation". Declarations/conflicts of interest: none reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was allocated to 1 of 2 interventions...using computer generated random numbers in randomly allocated blocks". Comment: adequate method of random sequence generation. |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation concealment was with consecutively numbered, sealed, opaque envelopes held by 1 individual not involved in the trial…who was contacted by telephone by the consenting clinician". Comment: ideal method of allocation concealment. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "It was not possible to mask those administering the surgical treatment". Comment: it was not possible to blind the participants or personnel. Trial authors reported that operators were equally proficient with both techniques. |
| Blinding of outcome assessment (subjective outcomes) | Unclear risk | Patient pain response: participants had no experience of the alternative procedure. Aesthetics: panel were blinded. |
| Blinding of outcome assessment (objective outcomes) | Low risk | Blinded assessors were used for periodontal and aesthetic assessments. |
| Incomplete outcome data (attrition bias) | Low risk | Drop‐out varied by outcome, but reasons were stated and were not related to outcomes. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported. The study reported data for surgical treatment time. They measured two other aspects (time for canine to erupt and overall duration of treatment) that are still to be published. |
| Other bias | Low risk | None apparent. |
| Methods | Trial design: quasi‐randomised, 2‐arm parallel groups, superiority. Setting: Department of Orthodontics, The Lithuanian University of Health Sciences. Number of centres: 1. Study duration: June 2007 to January 2012. | |
| Participants | Inclusion criteria: nonsyndromic patients with unilateral palatally impacted maxillary canines; good oral hygiene (Oral Hygiene Index (OHI‐S) < 1.3). Exclusion criteria: previous orthodontic treatment; metabolic disorders or other medical conditions that might influence treatment. Age at baseline (years): open: mean age 15.46 years (SD 3.28) years; closed: 16.15 years (SD 2.79) years. Gender: 35 females, 8 males (not reported by group). Number randomised: 43 (open: 22; closed: 21). Number evaluated: 43 (open: 22; closed: 21). | |
| Interventions | Comparison: open surgical exposure technique versus closed surgical exposure technique Open and closed surgical techniques were performed according to the method described by Kokich and Mathews 1993 and Kokich 2010. All surgical procedures were undertaken by the same oral surgeon.
Each patient instructed in proper oral hygiene measures. | |
| Outcomes | Post‐treatment examination undertaken 3 to 6 months after fixed appliance removal (mean 4.19 (SD 1.44) months) Periodontal health: assessed by periodontal pocket depths, gingival recession, gingivitis (using Gingival Index ‒ Silness and Loe and Papilla Bleeding Index), oral hygiene (using Oral Hygiene Index), width of keratinized tissue (not an outcome for this review) and bone support assessed radiographically. Ease of treatment/economics: mean time required to achieve eruption of the impacted canine from surgical exposure to bonding a bracket on the labial surface, and duration of orthodontic treatment from bonding to debonding of the fixed appliances with both techniques. Patient response: participants evaluated the treatment results as either satisfactory or unsatisfactory. Aesthetics: visual examination of colour, shape, inclination, function (occlusal contacts in lateral and anterior protrusion) and position in dental arch of previously impacted canines. | |
| Notes | Sample size calculation: not reported. Adverse effects: not reported. Funding: not reported. Declarations/conflicts of interest: "The authors state no conflict of interest." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: “Every second patient was assigned to the open technique group”. Comment: alternate allocation, which is not random. |
| Allocation concealment (selection bias) | High risk | Quote: “Every second patient was assigned to the open technique group”. Comment: not possible to conceal allocation when using alternation. |
| Blinding of participants and personnel (performance bias) | Unclear risk | It was not possible to blind the participants or personnel. However, it is unlikely that this would introduce any performance bias that could affect the outcomes. |
| Blinding of outcome assessment (subjective outcomes) | Unclear risk | It was not possible to blind the participants so this may affect their satisfaction with treatment. |
| Blinding of outcome assessment (objective outcomes) | Unclear risk | Quote: “Periodontal examination was carried out by one calibrated periodontist”. Comment: unclear if periodontist was blinded to participant treatment group. Quote: “Radiographic bone support was diagnosed…by one of the authors without knowledge of the impaction side”. Comment: blinded assessor used. |
| Incomplete outcome data (attrition bias) | Unclear risk | After further correspondence with the author, we learned that one participant was excluded after randomisation, due to poor oral hygiene, which was not reported in the paper. |
| Selective reporting (reporting bias) | High risk | No clear statement about primary and secondary outcomes. |
| Other bias | High risk | The participants in the two groups were treated differently. Those in the open exposure group had their fixed appliance placed before surgery. Those in the closed exposure group had their fixed appliance placed after surgery. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| No information regarding randomisation. Buccally and palatally displaced canines. | |
| Consecutively treated participants. | |
| No information about randomisation, uncontrolled. | |
| Consecutively treated participants, split‐mouth design but technique compared to historical alternative technique. | |
| Not clear how participants were allocated or if the trial was prospective. | |
| Cohort study. |
All these studies were excluded in the previous version of the review. No additional studies were excluded in this version.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Open versus closed surgical exposure of impacted canine teeth |
| Methods | Randomised controlled trial. |
| Participants | Patients with palatally ectopic maxillary canines who required surgical exposure and orthodontic alignment 13 years to 25 years (child, adult). |
| Interventions |
|
| Outcomes | Primary outcome: measure of width of attached gingiva (time frame: 36 months). Many measures that assess the periodontal outcome like crown length, gingival recession, bone loss will be assessed. Secondary outcome: pain score on the visual analogue scale (time frame: 10 days post surgery). Many patient‐related outcomes like the number of times the bond failure took place, surgical time, pain associated with surgery will be assessed. |
| Starting date | January 2015. |
| Contact information | |
| Notes |
| Trial name or title | The impact of surgical technique on PDC (PDC) |
| Methods | Randomised clinical trial. |
| Participants | Patients with diagnosis of uni‐ or bilateral palatally impacted canine(s) planned for surgical exposure at start of treatment of the impacted canines. 8 years to 16 years (child). |
| Interventions | Procedure: closed surgical technique. Procedure: open surgical technique. |
| Outcomes | Primary outcomes: treatment success; the previous impacted canine is positioned in the dental arch (time frame: within 3 years after surgery). Secondary outcomes: duration from surgery until the previous impacted canine has erupted into the mouth (time frame: within 1.5 year from surgery). |
| Starting date | November 2013. |
| Contact information | |
| Notes |
| Trial name or title | Closed window vs. open window technique in management of palatally impacted canines. |
| Methods | Randomised clinical trial. |
| Participants | Inclusion criteria:
Exclusion criteria:
11 years to 17 years (child) |
| Interventions | Procedure: open window technique. Procedure: closed window technique. |
| Outcomes | Primary outcome: total duration of treatment (time frame: 24 to 36 months). Secondary outcomes:
|
| Starting date | October 2015. |
| Contact information | |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Success of surgery Show forest plot | 3 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.06] |
| Analysis 1.1  Comparison 1 Open surgical technique versus closed surgical technique, Outcome 1 Success of surgery. | ||||
| 2 Aesthetics Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.2 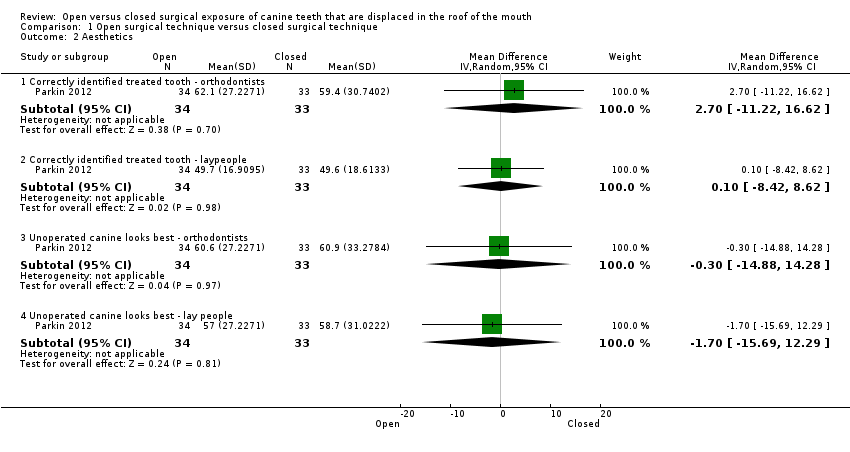 Comparison 1 Open surgical technique versus closed surgical technique, Outcome 2 Aesthetics. | ||||
| 2.1 Correctly identified treated tooth ‐ orthodontists | 1 | 67 | Mean Difference (IV, Random, 95% CI) | 2.70 [‐11.22, 16.62] |
| 2.2 Correctly identified treated tooth ‐ laypeople | 1 | 67 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐8.42, 8.62] |
| 2.3 Unoperated canine looks best ‐ orthodontists | 1 | 67 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐14.88, 14.28] |
| 2.4 Unoperated canine looks best ‐ lay people | 1 | 67 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐15.69, 12.29] |
| 3 Posttreatment aesthetics and morphology Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.3 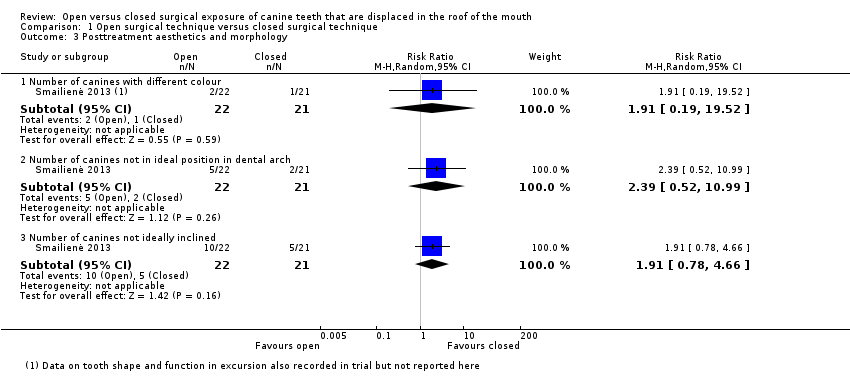 Comparison 1 Open surgical technique versus closed surgical technique, Outcome 3 Posttreatment aesthetics and morphology. | ||||
| 3.1 Number of canines with different colour | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.19, 19.52] |
| 3.2 Number of canines not in ideal position in dental arch | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 2.39 [0.52, 10.99] |
| 3.3 Number of canines not ideally inclined | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.78, 4.66] |
| 4 Patient response Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.4 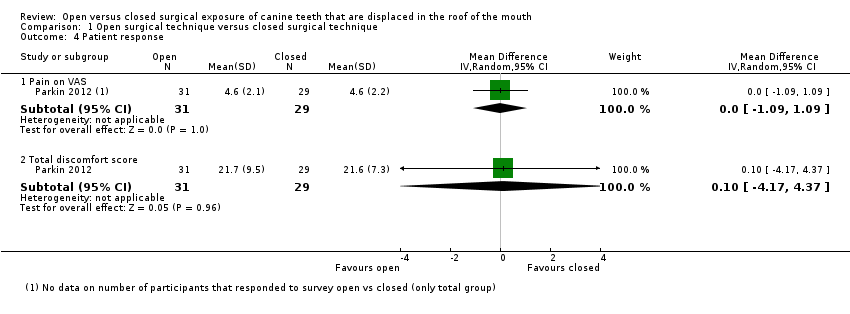 Comparison 1 Open surgical technique versus closed surgical technique, Outcome 4 Patient response. | ||||
| 4.1 Pain on VAS | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐1.09, 1.09] |
| 4.2 Total discomfort score | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐4.17, 4.37] |
| 5 Pain (dichotomous) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.5 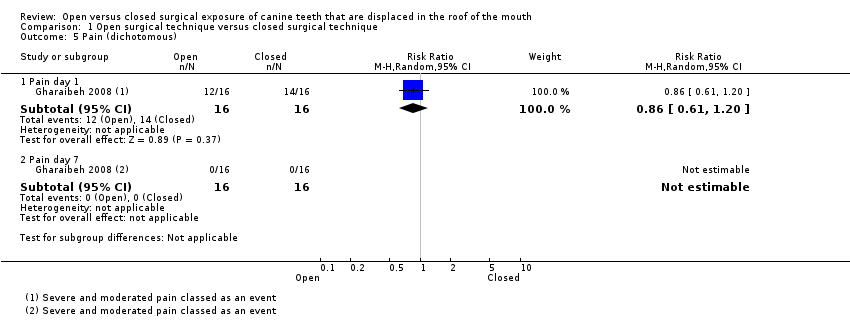 Comparison 1 Open surgical technique versus closed surgical technique, Outcome 5 Pain (dichotomous). | ||||
| 5.1 Pain day 1 | 1 | 32 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.61, 1.20] |
| 5.2 Pain day 7 | 1 | 32 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Gum health Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.6 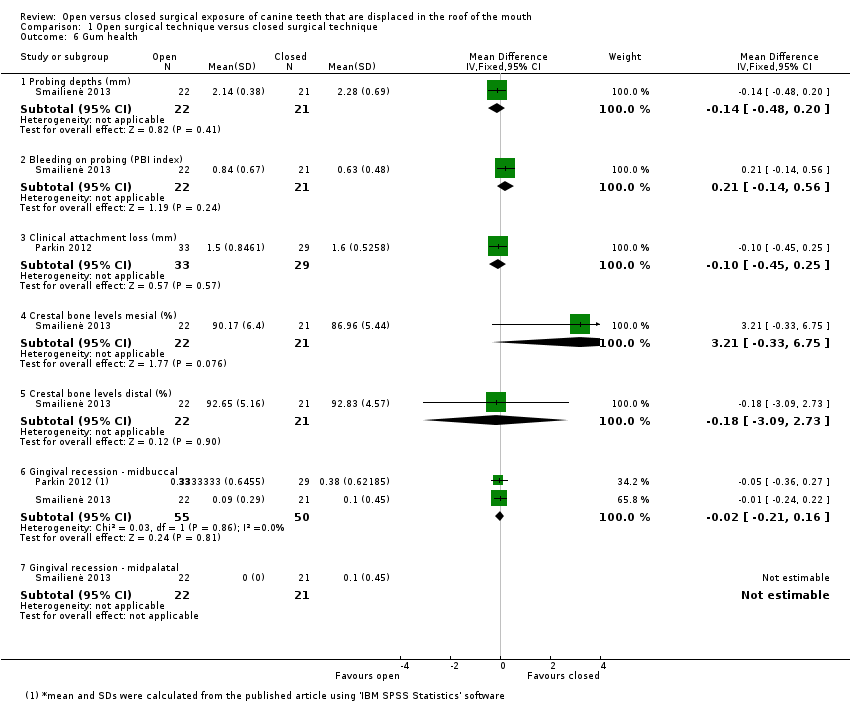 Comparison 1 Open surgical technique versus closed surgical technique, Outcome 6 Gum health. | ||||
| 6.1 Probing depths (mm) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.48, 0.20] |
| 6.2 Bleeding on probing (PBI index) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 0.21 [‐0.14, 0.56] |
| 6.3 Clinical attachment loss (mm) | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.45, 0.25] |
| 6.4 Crestal bone levels mesial (%) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 3.21 [‐0.33, 6.75] |
| 6.5 Crestal bone levels distal (%) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐3.09, 2.73] |
| 6.6 Gingival recession ‐ midbuccal | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.21, 0.16] |
| 6.7 Gingival recession ‐ midpalatal | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Gingival recession (dichotomous) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 Open surgical technique versus closed surgical technique, Outcome 7 Gingival recession (dichotomous). | ||||
| 7.1 Midpalatal recession | 1 | 62 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.63, 2.77] |
| 8 Treatment time Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.8  Comparison 1 Open surgical technique versus closed surgical technique, Outcome 8 Treatment time. | ||||
| 8.1 Length of time in surgery | 2 | 89 | Mean Difference (IV, Random, 95% CI) | ‐3.30 [‐9.97, 3.36] |
| 8.2 Time taken for eruption | 1 | 43 | Mean Difference (IV, Random, 95% CI) | ‐3.81 [‐5.80, ‐1.82] |
| 8.3 Length of fixed appliance phase | 1 | 43 | Mean Difference (IV, Random, 95% CI) | ‐3.77 [‐9.20, 1.66] |
| 9 Patient response (satisfaction) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.9 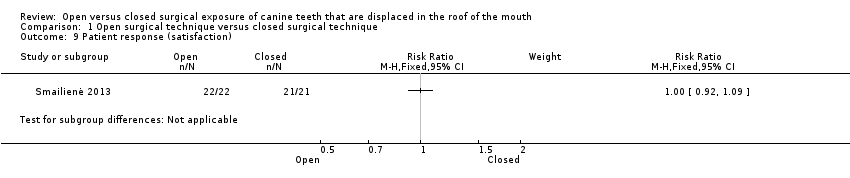 Comparison 1 Open surgical technique versus closed surgical technique, Outcome 9 Patient response (satisfaction). | ||||

Closed technique

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Study flow diagram of searches conducted for this update (2008 to 2017)

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 1 Success of surgery.

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 2 Aesthetics.
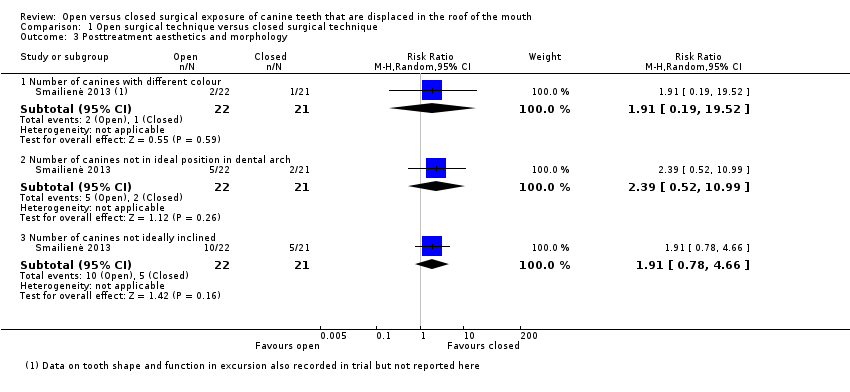
Comparison 1 Open surgical technique versus closed surgical technique, Outcome 3 Posttreatment aesthetics and morphology.
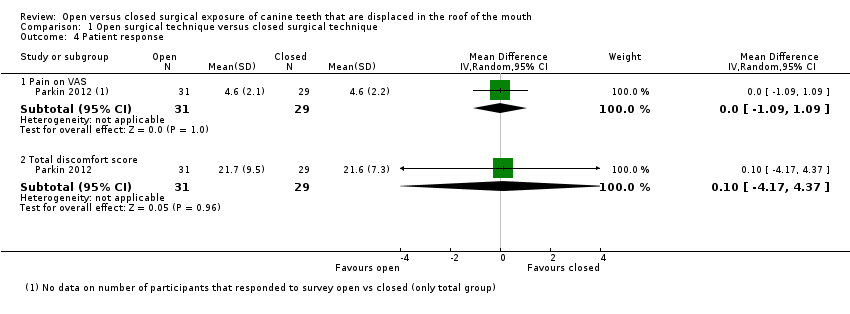
Comparison 1 Open surgical technique versus closed surgical technique, Outcome 4 Patient response.

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 5 Pain (dichotomous).

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 6 Gum health.

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 7 Gingival recession (dichotomous).

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 8 Treatment time.

Comparison 1 Open surgical technique versus closed surgical technique, Outcome 9 Patient response (satisfaction).
| Open surgical technique compared with closed surgical technique for palatally impacted canines | ||||||
| Patient or population: people with maxillary palatally impacted canines Settings: oral surgery departments Intervention: open surgical technique Comparison: closed surgical technique | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Closed surgery | Open surgery | |||||
| Success of surgery | 943 per 1000 | 934 per 1000 | RR 0.99 (0.93 to 1.06) | 141 | ⊕⊕⊝⊝ | The available evidence suggests that there is no difference in the success of surgery between the techniques and that both techniques have a high success rate. |
| Complications | One surgical failure was due to detachment of the gold chain (closed group). One study reported two complications following surgery, both in the closed group: a post‐operative infection requiring antibiotics and pain during alignment of the canine as the gold chain penetrated through the gum tissue of the palate. | |||||
| Aesthetics (reported in various manners at different time points) | This outcome was measured in a variety of ways in the studies that cannot be pooled. | ⊕⊝⊝⊝ | This outcome is subjective and can be measured and reported in many different ways. The current evidence suggests that there is no difference in aesthetic outcomes between the groups. | |||
| Patient response (pain and discomfort reported in different ways between 1 to 10 days postoperatively) | This outcome was measured in a variety of ways in the studies that cannot be pooled. | ⊕⊝⊝⊝ | This outcome is subjective and was measured and reported in different ways. The current evidence suggests that there is no difference in patient response outcomes between the groups. | |||
| Gum health (clinical attachment level (CAL); 3 months post‐debond) | Mean CAL in the closed group | Mean CAL in the intervention groups was 0.1 mm lower | 62 | ⊕⊕⊝⊝ | This outcome was measured and reported in different ways in different studies. The current evidence suggests that there is no difference in periodontal outcomes between the groups. | |
| Treatment time (length of time in operating theatre from first incision to final suture) | Mean of the closed group was 34.3 minutes in Parkin 2012; and 37.7 minutes in Gharaibeh 2008. | Mean of the open group was 3.18 minutes less (7.59 minutes less to 1.22 minutes more) | 89 (2 studies) | ⊕⊝⊝⊝ | The current evidence suggests that there is no difference in length of time in surgery between the groups. | |
| *The basis for the assumed risk is the Parkin 2012 closed group. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to high risk of bias in two studies. Downgraded one level as two studies had no failures. 2 Downgraded one level due to high risk of bias in one study. Downgraded one level as each outcome only reported by single studies. Downgraded one level as studies with few participants and large confidence intervals for some outcomes. 3 Downgraded two levels due to high risk of bias in two studies and subjective participant‐reported outcome with no blinding. Downgraded one level as each outcome only reported by single studies. 4 Downgraded two levels as single small study at high risk of bias. 5 Downgraded one level due to high risk of bias in one study. Downgraded one level as substantial heterogeneity between results. Downgraded one level as studies with few participants and large confidence intervals for some outcomes. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Success of surgery Show forest plot | 3 | 141 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.06] |
| 2 Aesthetics Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Correctly identified treated tooth ‐ orthodontists | 1 | 67 | Mean Difference (IV, Random, 95% CI) | 2.70 [‐11.22, 16.62] |
| 2.2 Correctly identified treated tooth ‐ laypeople | 1 | 67 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐8.42, 8.62] |
| 2.3 Unoperated canine looks best ‐ orthodontists | 1 | 67 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐14.88, 14.28] |
| 2.4 Unoperated canine looks best ‐ lay people | 1 | 67 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐15.69, 12.29] |
| 3 Posttreatment aesthetics and morphology Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Number of canines with different colour | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.19, 19.52] |
| 3.2 Number of canines not in ideal position in dental arch | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 2.39 [0.52, 10.99] |
| 3.3 Number of canines not ideally inclined | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.78, 4.66] |
| 4 Patient response Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Pain on VAS | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐1.09, 1.09] |
| 4.2 Total discomfort score | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐4.17, 4.37] |
| 5 Pain (dichotomous) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Pain day 1 | 1 | 32 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.61, 1.20] |
| 5.2 Pain day 7 | 1 | 32 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Gum health Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Probing depths (mm) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.48, 0.20] |
| 6.2 Bleeding on probing (PBI index) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 0.21 [‐0.14, 0.56] |
| 6.3 Clinical attachment loss (mm) | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.45, 0.25] |
| 6.4 Crestal bone levels mesial (%) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 3.21 [‐0.33, 6.75] |
| 6.5 Crestal bone levels distal (%) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐3.09, 2.73] |
| 6.6 Gingival recession ‐ midbuccal | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.21, 0.16] |
| 6.7 Gingival recession ‐ midpalatal | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Gingival recession (dichotomous) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Midpalatal recession | 1 | 62 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.63, 2.77] |
| 8 Treatment time Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Length of time in surgery | 2 | 89 | Mean Difference (IV, Random, 95% CI) | ‐3.30 [‐9.97, 3.36] |
| 8.2 Time taken for eruption | 1 | 43 | Mean Difference (IV, Random, 95% CI) | ‐3.81 [‐5.80, ‐1.82] |
| 8.3 Length of fixed appliance phase | 1 | 43 | Mean Difference (IV, Random, 95% CI) | ‐3.77 [‐9.20, 1.66] |
| 9 Patient response (satisfaction) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |


