Music interventions for preoperative anxiety
Abstract
Background
Patients awaiting surgical procedures often experience significant anxiety. Such anxiety may result in negative physiological manifestations, slower wound healing, increased risk of infection, and may complicate the induction of anaesthesia and impede postoperative recovery. To reduce patient anxiety, sedatives and anti‐anxiety drugs are regularly administered before surgery. However, these often have negative side effects and may prolong patient recovery. Therefore, increasing attention is being paid to a variety of non‐pharmacological interventions for reduction of preoperative anxiety such as music therapy and music medicine interventions. Interventions are categorized as 'music medicine' when passive listening to pre‐recorded music is offered by medical personnel. In contrast, music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process, and the use of personally tailored music experiences. A systematic review was needed to gauge the efficacy of both music therapy and music medicine interventions for reduction of preoperative anxiety.
Objectives
To examine the effects of music interventions with standard care versus standard care alone on preoperative anxiety in surgical patients.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 7), MEDLINE (1950 to August 2012), CINAHL (1980 to August 2012), AMED (1985 to April 2011; we no longer had access to AMED after this date), EMBASE (1980 to August 2012), PsycINFO (1967 to August 2012), LILACS (1982 to August 2012), Science Citation Index (1980 to August 2012), the specialist music therapy research database (March 1 2008; database is no longer functional), CAIRSS for Music (to August 2012), Proquest Digital Dissertations (1980 to August 2012), ClinicalTrials.gov (2000 to August 2012), Current Controlled Trials (1998 to August 2012), and the National Research Register (2000 to September 2007). We handsearched music therapy journals and reference lists, and contacted relevant experts to identify unpublished manuscripts. There was no language restriction.
Selection criteria
We included all randomized and quasi‐randomized trials that compared music interventions and standard care with standard care alone for reducing preoperative anxiety in surgical patients.
Data collection and analysis
Two review authors independently extracted the data and assessed the risk of bias. We contacted authors to obtain missing data where needed. Where possible, results were presented in meta analyses using mean differences and standardized mean differences. Post‐test scores were used. In cases of significant baseline differences, we used change scores.
Main results
We included 26 trials (2051 participants). All studies used listening to pre‐recorded music. The results suggested that music listening may have a beneficial effect on preoperative anxiety. Specifically, music listening resulted, on average, in an anxiety reduction that was 5.72 units greater (95% CI ‐7.27 to ‐4.17, P < 0.00001) than that in the standard care group as measured by the Stait‐Trait Anxiety Inventory (STAI‐S), and ‐0.60 standardized units (95% CI ‐0.90 to ‐0.31, P < 0.0001) on other anxiety scales. The results also suggested a small effect on heart rate and diastolic blood pressure, but no support was found for reductions in systolic blood pressure, respiratory rate, and skin temperature. Most trials were assessed to be at high risk of bias because of lack of blinding. Blinding of outcome assessors is often impossible in music therapy and music medicine studies that use subjective outcomes, unless in studies in which the music intervention is compared to another treatment intervention. Because of the high risk of bias, these results need to be interpreted with caution.
None of the studies included wound healing, infection rate, time to discharge, or patient satisfaction as outcome variables. One large study found that music listening was more effective than the sedative midazolam in reducing preoperative anxiety and equally effective in reducing physiological responses. No adverse effects were identified.
Authors' conclusions
This systematic review indicates that music listening may have a beneficial effect on preoperative anxiety. These findings are consistent with the findings of three other Cochrane systematic reviews on the use of music interventions for anxiety reduction in medical patients. Therefore, we conclude that music interventions may provide a viable alternative to sedatives and anti‐anxiety drugs for reducing preoperative anxiety.
PICO
Plain language summary
Can music interventions replace sedatives for reduction of preoperative anxiety?
People awaiting surgical procedures often experience high levels of anxiety. Such anxiety may result in negative bodily responses, such as increased blood pressure and heart rate, leading to slower wound healing and increased risk of infection. High anxiety may also affect the start of anaesthesia and slow down postoperative recovery. To reduce patient anxiety, sedatives and anti‐anxiety drugs are regularly administered before surgery. However, these often have negative side effects, such as causing drowsiness and breathing difficulties, and may interact with anaesthetic drugs to prolong patient recovery and discharge. Therefore, increasing attention is being paid to music therapy and music medicine interventions, amongst other non‐pharmacological interventions, for reduction of preoperative anxiety. Interventions are categorized as 'music medicine' when passive listening to pre‐recorded music is offered by medical personnel. In contrast, music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process, and the use of personally tailored music experiences. A systematic review was needed to gauge the efficacy of both music therapy and music medicine interventions for reduction of preoperative anxiety.
The review included 26 trials with a total of 2051 participants. The findings suggested that music listening may have a beneficial effect on preoperative anxiety. Most trials presented some methodological weakness. Therefore, these results need to be interpreted with caution. However, these findings are consistent with the findings of three other Cochrane systematic reviews on the use of music interventions for anxiety reduction in medical patients. Therefore, we conclude that music interventions may provide a viable alternative to sedatives and anti‐anxiety drugs for reducing preoperative anxiety.
Authors' conclusions
Summary of findings
| Patient or population: patients with preoperative anxiety | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Standard care | Music | |||||
| Preoperative anxiety (STAI) | The mean preoperative anxiety (stai) ranged across control groups from | The mean preoperative anxiety (stai) in the intervention groups was | 896 | ⊕⊕⊝⊝ | ||
| Preoperative anxiety (non‐STAI) | The mean preoperative anxiety (non‐stai) in the intervention groups was | 504 | ⊕⊕⊝⊝ | |||
| Heart rate | The mean heart rate ranged across control groups from | The mean heart rate in the intervention groups was | 1109 | ⊕⊝⊝⊝ | ||
| Heart rate variability | The mean heart rate variability ranged across control groups from | The mean heart rate variability in the intervention groups was | 241 | ⊕⊝⊝⊝ | ||
| Systolic blood pressure | The mean systolic blood pressure ranged across control groups from | The mean systolic blood pressure in the intervention groups was | 809 | ⊕⊝⊝⊝ | ||
| Diastolic blood pressure | The mean diastolic blood pressure ranged across control groups from | The mean diastolic blood pressure in the intervention groups was | 786 | ⊕⊝⊝⊝ | ||
| Respiratory rate | The mean respiratory rate ranged across control groups from | The mean respiratory rate in the intervention groups was | 375 | ⊕⊝⊝⊝ | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The majority of the trials were assessed as high risk of bias studies | ||||||
Background
Description of the condition
Patients awaiting surgical procedures often experience significant anxiety in anticipation of events that are uncomfortable, uncertain, and that may include a health risk. High levels of anxiety result in negative physiological manifestations, such as elevated blood cortisol levels, and increased blood pressure and heart rate, leading to slower wound healing, diminished immune response, and increased risk of infection (Scott 2004). High anxiety may also complicate presurgical drug administration, adversely affect the induction of anaesthesia, and impede postoperative recovery (Kain 2000; Kiecolt‐Glaser 1998; Maranets 1999; Ozalp 2003; Scott 2004). To reduce patient anxiety, sedatives or antianxiety drugs are regularly administered before surgery. However, sedatives often have negative side effects, such as drowsiness and respiratory depression, and may interact with anaesthetic agents prolonging patient recovery and discharge (Agarwal 2005). Therefore, increasing attention is being paid to a variety of non‐pharmacological interventions for reduction of preoperative anxiety (Agarwal 2005; Leroy 2003; Norred 2000; Wright 2007).
Description of the intervention
Music has been used in different medical fields to meet physiological, psychological, and spiritual needs of patients. Research on the effects of music and music therapy for medical patients has burgeoned during the past 20 years and has included a variety of outcome measures in a wide range of specialty areas (Dileo 2005). Specifically, the anxiolytic effects of music have been studied in a variety of medical patients, including surgical (Daub 1988Kaempf 1989Koch 1998Mok 2003), cardiac (Bolwerk 1990; Hamel 2001; White 1999), and oncology patients (Frank 1985; Pfaff 1989).
It is important to make a clear distinction between music interventions administered by medical or healthcare professionals (music medicine) and those implemented by trained music therapists (music therapy). A substantive set of data (Dileo 2005) indicates that music therapy interventions with medical populations are significantly more effective than music medicine interventions for a wide variety of outcomes. This difference might be attributed to the fact that music therapists individualize their interventions to meet patients' specific needs, more actively engage the patients in the music making, and employ a systematic therapeutic process that includes assessment, treatment, and evaluation. As defined by Dileo (Dileo 1999), interventions are categorized as 'music medicine' when passive listening to pre‐recorded music is offered by medical personnel. In contrast, music therapy requires the implementation of a music intervention by a trained music therapist, the presence of a therapeutic process, and the use of personally tailored music experiences. These music experiences include:
-
listening to live, improvised, or pre‐recorded music;
-
performing music on an instrument;
-
improvising music spontaneously using voice or instruments, or both;
-
composing music; and
-
music combined with other modalities (e.g., movement, imagery, art) (Dileo 2007).
How the intervention might work
A common theory regarding the anxiety‐reducing effects of music is that music can help patients focus their attention away from stressful events to something pleasant and soothing (Mitchell 2003; Nilsson 2008). Even though this is an important mechanism in preoperative anxiety reduction, it is important to emphasize that music does more than refocusing patients’ attention. It provides the patient with an aesthetic experience that can offer comfort and peace while awaiting surgery. In music interventions provided by a trained music therapist, the music therapist furthermore adapts the live music interactions to the in‐the‐moment needs of the patients. This often provides a deeply humanizing and validating experience for the patient. The act of making music together can provide a strong sense of support. Moreover, the active and creative engagement in music making (for example, singing songs, improvising music) stands in stark contrast to passively submitting oneself to surgical procedures. This may result in an increased sense of control and empowerment.
On a neurophysiological level, it has been postulated that music induces relaxation through its impact on automated and central nervous responses (Gillen 2008; Lai 2006). More specifically, it is believed that the anxiolytic effect of music is achieved through its suppressive action on the sympathetic nervous system, leading to decreased adrenergic activity and decreased neuromuscular arousal (Chlan 1998; Gillen 2008). Music furthermore triggers the limbic system in the brain to release endorphins; these neurotransmitters play an important role in enhancing a sense of well‐being (Arslan 2008; Lee 2005). However, Gillen (Gillen 2008) has suggested that more research is needed to examine the physiological mechanisms that explain the anxiolytic effects of music.
Why it is important to do this review
Most research studies examining the anxiety‐reducing effects of music in presurgical patients have used music listening as the primary intervention. Several of these studies have found that exposure to music reduces preoperative anxiety. Several studies, however, have suffered from small sample size, making it nearly impossible to achieve statistically significant results. In addition, a number of individual factors that are likely to influence responses to music, including age, gender, emotional state, music preference, personal associations with the music, prior musical training, and culture, are likely to influence the outcomes (Dileo 2005; Pelletier 2004; Standley 1986; Standley 2000). A systematic review was needed to more accurately gauge the efficacy of both music medicine and music therapy for reduction of preoperative anxiety as well as to identify variables that may moderate the effects.
Objectives
-
To identify randomized controlled trials examining the effects of music therapy or music medicine interventions (as defined by the authors) on preoperative anxiety in surgical patients.
-
To compare the efficacy of participation in standard care combined with music therapy or music medicine interventions with standard care alone.
-
To compare the efficacy of patient‐preferred music with researcher‐selected music.
-
To compare the efficacy of different types of music interventions (music therapy versus music medicine).
Methods
Criteria for considering studies for this review
Types of studies
We included all randomized controlled trials (RCT) and controlled clinical trials (CCTs) with quasi‐randomized or systematic methods of treatment allocation in any language, published and unpublished.
We conducted a sensitivity analysis to assess the impact of the randomization method.
Types of participants
This review included all surgical patients that were inpatients, outpatients, emergency, non‐emergency, undergoing major as well as minor surgical procedures. Dental surgical patients and patients undergoing non‐surgical procedures were excluded. This review did not include family members of the participants. There were no restrictions as to age, gender, or ethnicity.
Types of interventions
The review included all studies in which standard care combined with music therapy or music medicine interventions (as defined by the authors) delivered during the preoperative period was compared with standard treatment alone. Studies that included a combination of operative periods (for example, preoperative, perioperative, postoperative) were considered only if data on the effects of music on anxiety during the preoperative period were reported.
Types of outcome measures
Primary outcomes
The primary outcome for this review was preoperative anxiety. Measures of anxiety included the State Anxiety scale of the State‐Trait Anxiety Inventory (STAI‐S) (Spielberger 1983), visual analogue scales (VAS), numerical rating scales (NRS), and the Zung Self‐Rating Anxiety Scale. We only included scales with established reliability and validity (that is, as evidenced in at least one prior published study in a peer‐reviewed journal).
Secondary outcomes
The secondary outcomes for this review were:
-
preoperative sedative drug intake;
-
physiological outcomes (e.g., heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure, skin temperature) using post‐intervention or change scores to compare the treatment and control groups;
-
physical outcomes (e.g., infection rate, wound healing);
-
patient satisfaction.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases and trial registers:
-
Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 7);
-
MEDLINE (Ovid) (1950 to August 2012);
-
EMBASE (1980 to August 2012);
-
CINAHL (1982 to August 2012);
-
PsycINFO (1967 to August 2012);
-
LILACS (1982 to August 2012);
-
AMED (1985 to April 2011; we no longer had access to AMED after this date);
-
Science Citation Index (1980 to August 2012);
-
The specialist music therapy research database at www.musictherapyworld.net (database is no longer functional) (1 March 2008);
-
CAIRSS for Music (August 2012);
-
Proquest Digital Dissertations (1980 to August 2012);
-
ClinicalTrials.gov (http://www.clinicaltrials.gov/) (2000 to August 2012);
-
Current Controlled Trials (http://www.controlled‐trials.com/) (1998 to August 2012);
-
National Research Register (http://www.nihr.ac.uk/Pages/NRRArchive.aspx) (2000 to August 2012).
We used the search strategy found in Appendix 2 for MEDLINE (Ovid) and adapted it for the other databases.
Searching other resources
We handsearched the following journals from their first available date:
-
Australian Journal of Music Therapy (August 2012);
-
Canadian Journal of Music Therapy (August 2012);
-
The International Journal of the Arts in Medicine (December 2007, latest issue was published in 1999);
-
Journal of Music Therapy (August 2012);
-
Musik‐, Tanz‐, und Kunsttherapie (Journal for Art Therapies in Education, Welfare and Health Care)(August 2012);
-
Musiktherapeutische Umschau (online index available until 2010);
-
Music Therapy (February 2012; latest issue published 1996);
-
Music Therapy Perspectives (August 2012);
-
Nordic Journal of Music Therapy (August 2012);
-
Music Therapy Today (online journal of music therapy) (December 2007; latest issue published December 2007);
-
Voices (online international journal of music therapy) (August 2012);
-
New Zealand Journal of Music Therapy (online index available until 2009);
-
British Journal of Music Therapy (August 2012).
In an effort to identify further published, unpublished, and ongoing trials we searched the bibliographies of relevant studies and reviews, contacted experts in the field, and searched available proceedings of music therapy conferences.
We imposed no language restrictions for either searching or trial inclusion.
Data collection and analysis
Selection of studies
One author (JB) scanned the titles and abstracts of each record retrieved from the search. If information in the abstract clearly indicated that the trial did not meet the inclusion criteria, we rejected the trial. When a title or abstract could not be rejected with certainty, JB and MS independently obtained and inspected the full article. We used an inclusion criteria form to assess the trial's eligibility for inclusion. We resolved any disagreements by discussion. If a trial was excluded, we kept a record of both the article and the reason for its exclusion.
Data extraction and management
JB and MS independently extracted data from the selected trials using a standardized coding form. We discussed and were able to resolve any differences in data extraction. We extracted the following data.
General information
-
Author
-
Year of publication
-
Title
-
Journal (title, volume, pages)
-
If unpublished, source
-
Duplicate publications
-
Country
-
Language of publication
Intervention information
-
Type of intervention (e.g., singing, song‐writing, music listening, music improvisation)
-
Music selection (detailed information on music selection in case of music listening)
-
Music preference (patient‐preferred versus researcher‐selected in the case of music listening)
-
Level of intervention (music therapy versus music medicine as defined by the authors in the background section)
-
Length of intervention
-
Frequency of intervention
-
Comparison intervention
Participants information
-
Total sample size
-
Number in experimental group
-
Number in control group
-
Gender
-
Age
-
Ethnicity
-
Type of surgery
-
Setting
-
Inclusion criteria
Outcomes
Pre‐test means, post‐test means, standard deviations, and sample sizes were extracted for the treatment group and the control group for the following outcomes (if applicable). For some trials only change scores, instead of post‐test scores, were available.
-
Preoperative anxiety.
-
Preoperative sedative drug intake.
-
Physiological outcomes (e.g., heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure, skin temperature).
-
Physical outcomes (e.g., infection rate, wound healing).
-
Patient satisfaction.
Assessment of risk of bias in included studies
JB and MS assessed all included trials for risk of bias and were blinded to each other's assessments. Any disagreements were resolved by discussion. The authors used the following criteria for quality assessment.
Random sequence generation
-
Low risk
-
Unclear risk
-
High risk
Random sequence generation was rated as low risk if every participant had an equal chance to be selected for either condition and if the investigator was unable to predict which treatment the participant would be assigned to. Use of date of birth, date of admission, or alternation resulted in high risk of bias.
Allocation concealment
-
Low risk methods to conceal allocation include:
-
-
central randomization;
-
serially numbered, opaque, sealed envelopes;
-
other descriptions with convincing concealment.
-
-
Unclear risk, authors did not adequately report on method of concealment.
-
High risk (e.g., alternation methods were used).
Blinding of participants and personnel
-
Low risk
-
Unclear risk
-
High risk
Since participants cannot be blinded in a music intervention trial, studies were not downgraded for not blinding the participants. As for personnel, in music therapy studies music therapists cannot be blinded because they are actively making music with the patients. In contrast, in music medicine studies blinding of personnel is possible by providing control group participants with headphones but no music (e.g., blank CD). Therefore, downgrading for not blinding personnel was only applied in studies that used listening to pre‐recorded music.
Blinding of outcome assessors
-
Low risk
-
Unclear risk
-
High risk
Incomplete outcome data
We recorded the proportion of participants whose outcomes were analysed. We coded losses to follow‐up for each outcome as:
-
low risk, if fewer than 20% of patients were lost to follow‐up and reasons for loss to follow‐up were similar in both treatment arms;
-
unclear risk, if loss to follow‐up was not reported;
-
high risk, if more than 20% of patients were lost to follow‐up or reasons for loss to follow‐up differed between treatment arms.
Selective reporting
-
Low risk, reports of the study were free of suggestion of selective outcome reporting
-
Unclear risk
-
High risk, reports of the study suggest selective outcome reporting
Other sources of bias
-
Low risk
-
Unclear risk
-
High risk
Information on potential financial conflicts of interest was considered as a possible source of additional bias.
The above criteria were used to give each article an overall quality rating, based on the Cochrane Handbook for Systematic Reviews of Interventions Section 8.7 (Higgins 2011).
A. Low risk of bias: all criteria met.
B. Moderate risk of bias: one or more of the criteria only partly met.
C. High risk of bias: one or more criteria not met.
Studies were not excluded based on a low quality score. We planned to use the overall quality assessment rating for sensitivity analysis. However, since most trials were at high risk of bias, we could not carry out this analysis.
Measures of treatment effect
All outcomes in this review were presented as continuous variables. We calculated standardized mean differences with 95% confidence intervals (CI) for outcome measures using results from different scales. When there were sufficient data available from various studies using the same measurement instrument (for example, Spielberger's State Anxiety Inventory) we computed a mean difference (MD) with 95% CI.
Unit of analysis issues
In all studies included in this review, participants were individually randomized to the intervention or the standard care control group. Post‐test values or change values on a single measurement for each outcome from each participant were collected and analysed.
Dealing with missing data
We did not impute missing outcome data. We analysed data on an endpoint basis, including only participants for whom final data point measurements were obtained (available case analysis). It was not assumed that participants who dropped out after randomization had a negative outcome.
Assessment of heterogeneity
We investigated heterogeneity using visual inspection of the forest plots as well as the I2 statistic (Higgins 2002).
Assessment of reporting biases
Publication bias using preoperative anxiety as the outcome was examined visually in the form of a funnel plot (Figure 1). The funnel plot did not show evidence of publication bias.
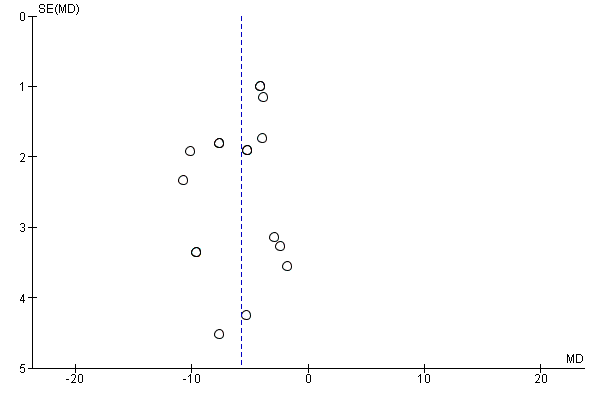
Funnel plot of comparison: 1 Music versus standard care, outcome: 1.1 State Anxiety STAI.
Data synthesis
We entered all trials included in the systematic review into Review Manager (RevMan 5.1). We anticipated that some individual studies would have used final scores whereas others might have used change scores. We combined these different types of analyses as mean difference (MD). We calculated pooled estimates using the more conservative random‐effects model. We determined the levels of heterogeneity by the I2 statistic (Higgins 2002).
The following treatment comparison was made: music interventions versus standard care alone.
Subgroup analysis and investigation of heterogeneity
The following subgroup analyses were determined a priori, but these could not be carried out because of insufficient numbers of trials per subgroup:
a. music medicine with music therapy interventions;
b. patient‐preferred music with researcher‐selected music;
d. comparison of different types of music interventions (e.g., listening to music, active music making).
Sensitivity analysis
We examined the impact of sequence generation by comparing the results of including and excluding trials that used inadequate or unclear randomization methods.
Results
Description of studies
See Figure 2
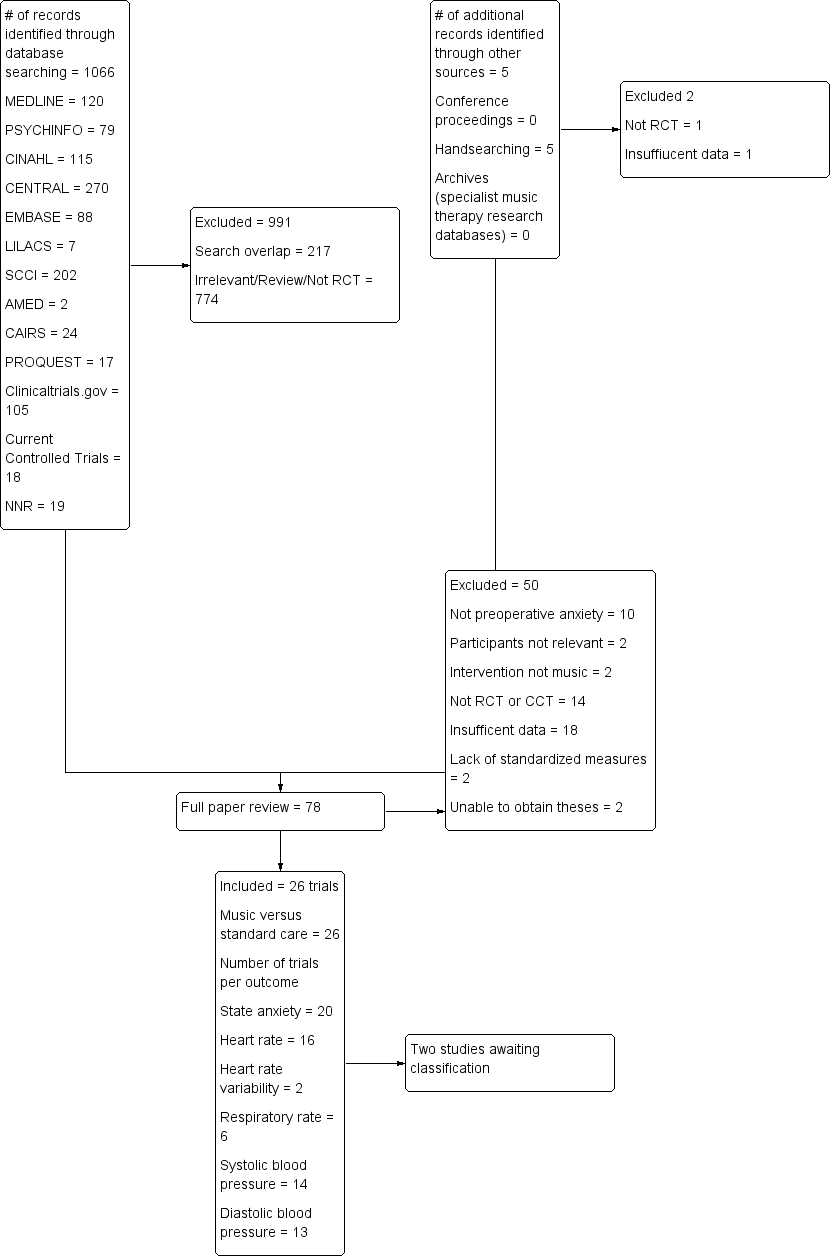
Excluded Study flow diagram.
Results of the search
The database searches and handsearching of conference proceedings, journals, and reference lists resulted in 1071 citations. Two authors (JB and MS) examined the titles and abstracts and identified 76 studies as potentially relevant, which were retrieved for further assessment. These were then independently screened by JB and MS.
We included 26 trials in this review (see Characteristics of included studies). Where necessary, we contacted the chief investigators to obtain additional information on study details and data.
Two studies (Berbel 2007; Dwita 2002) are awaiting classification. We were unable to obtain the study reports.
Included studies
We included 26 studies with a total of 2051 participants in this review. These studies examined the effects of music on preoperative anxiety in patients awaiting surgery. There was a balanced distribution of female (54%) and male (46%) participants in these studies. The mean age of participants was 48.74 years of age. Only five studies specified the ethnicity of the study participants (Augustin 1996; Hook 2008; Lee 2011; Yung 2002; Yung 2003). Nine studies were conducted in the USA (Allen 2001; Augustin 1996; Bringman 2009; Cassidy 2003; Cooke 2005; DeMarco 2012; Evans 1994; Gaberson 1995; Winter 1994); five in Taiwan (Chang 1996; Lee 2011; Lee 2012; Lin 2011; Ni 2011); three in Hong Kong (Szeto 1999; Yung 2002; Yung 2003); three in China (Guo 2005; Lee 2004; Li 2004); two in Poland (Miluk‐Kolasa 1996; Miluk‐Kolasa 2002); two in Turkey (Arslan 2008; Ganidagli 2005); one in Malaysia (Hook 2008); and one in Israel (Kushnir 2012). Trial sample size ranged from 9 to 327 participants with an average sample size of 78.9 (SD 64.36) participants.
The studies included many different types of surgery including general ambulatory (Augustin 1996), general (Bringman 2009; Cassidy 2003; Gaberson 1995; Hook 2008; Lee 2004; Lee 2011; Lee 2012; Miluk‐Kolasa 1996; Miluk‐Kolasa 2002; Ni 2011; Szeto 1999), endoscopic (Evans 1994), gynaecological or urogenital (Arslan 2008; Winter 1994; Yung 2002; Yung 2003), orthopaedic (Cooke 2005; Lin 2011), elective cosmetic (DeMarco 2012), elective caesarian (Kushnir 2012), cardiac (Chang 1996), ophthalmic (Allen 2001), septorhinoplastic (Ganidagli 2005), and gastric cancer (Li 2004).
Not all studies measured all outcomes identified for this review.
All included studies were categorized as music medicine studies (as defined by the review authors in the background section) and used listening to pre‐recorded music as the intervention. Some authors provided theoretical frameworks for the use of music to reduce anxiety including: (a) decreased adrenergic and sympathetic nervous system activity through entrainment of body rhythms with music (Arslan 2008; Lee 2004); (b) sedative music's capacity to reduce neuroendocrine activity (Lin 2011); (c) the influence of music listening on the limbic system of the brain by reducing the ability of neurotransmitters to relay uncomfortable feelings and by triggering the release of endorphins (Arslan 2008; Cooke 2005); (d) alteration of perceptual responses including the perception of time (Cooke 2005); and (e) music as a distracter, focusing the patient’s attention away from negative stimuli to something pleasant and encouraging (Lee 2011; Lee 2012). Robb and colleagues emphasize the need for researchers to specify a theoretical framework and "provide a rationale for the music selected and specify how qualities and delivery of the music are expected to impact targeted outcomes" (Robb 2011).
Most studies offered one 20 to 30‐minute music session to the participants during the preoperative waiting period. Two studies offered multiple music listening sessions, starting several days before surgery and continuing to the day of the surgery (Li 2004; Lin 2011).
Few studies provided detailed information about the music that was used (Bringman 2009; DeMarco 2012; Winter 1994). Most authors only reported the different styles of music that were offered to the participants (for example, jazz, easy listening, country and western, classical music) without any composition‐specific or performance‐specific information. Five studies indicated the tempo range of the music, namely between 60 to 80 beats per minute (bpm) (Chang 1996; Hook 2008; Lee 2011; Lee 2012; Lin 2011). The majority of the studies asked the participants to select their preferred music from a limited number of music offerings. In contrast, two studies used researcher‐selected music and did not take into account participant preference (DeMarco 2012; Li 2004). The decision to use patient‐selected music was based on the assumption that music preference plays an important part in the effectiveness of music relaxation. This assumption has been supported by a recent series of studies that found that music preference and familiarity with the music are positively correlated with the degree of relaxation obtained from listening to music (Tan 2012). It needs to be noted that, in the studies included in this review, participants could only select from a limited number of music styles presented by the researcher. It is likely that the preferred music of some of the participants was not included in the music selections offered and, even if it were, that they may not have liked the specific compositions or songs being played. In two studies, participants were asked to bring music of their own choice (Cassidy 2003; Ganidagli 2005).
Thirteen studies excluded patients who had received preoperative sedatives (Augustin 1996; Cooke 2005; DeMarco 2012; Evans 1994; Gaberson 1995; Lee 2004; Lee 2011; Lee 2012; Ni 2011; Szeto 1999; Winter 1994; Yung 2002; Yung 2003). In two studies, standard preoperative drugs, including midazolam hydrochloride and alfentanil hydrochloride, were administered to both the music intervention group and the standard care control group (Allen 2001; Ganidagli 2005). For a few studies, it was unclear whether participants received preoperative sedatives (Guo 2005; Hook 2008; Li 2004; Lin 2011). Five studies did not include any information on the use of preoperative drugs (Arslan 2008; Cassidy 2003; Kushnir 2012; Miluk‐Kolasa 1996; Miluk‐Kolasa 2002). Finally, one study compared a music intervention group who did not receive preoperative sedatives with a standard care control group who received midazolam (Bringman 2009). Because of the differences in preoperative drug administration between the two groups, this study could not be pooled with the other studies in this review. Instead, we included the results of this study in the narrative of this review.
One study's results (Miluk‐Kolasa 1996) could not be pooled with other studies because only percentage change scores were reported. These results are therefore presented in the narrative of the results section.
Details of the studies included in the review are shown in the table Characteristics of included studies.
Excluded studies
We excluded a total of 50 studies for the following reasons:
-
studies did not address preoperative anxiety; instead, the post‐test measurement of anxiety was administered after surgery (10 studies);
-
studies were not randomized controlled trials or controlled clinical trials (14 studies);
-
study participants did not meet the inclusion criteria (two studies);
-
insufficient data reporting (18 studies);
-
studies did not use standardized measures for anxiety (two studies);
-
studies did not use music (two studies); and
-
we were unable to obtain the studies (two studies).
The reasons for exclusion are listed in the table Characteristics of excluded studies.
Risk of bias in included studies
Allocation
We included 11 trials that used appropriate methods of randomization (for example, computer‐generated table of random numbers, a draw of lots, flip of coins), four trials that used alternate group assignment as the allocation method, four trials that used other forms of systematic allocation (for example, date of birth, day of surgery), and seven trials that reported using randomization but failed to state the randomization method.
Five trials used allocation concealment whereas eight trials did not. For the remainder of the trials, use of allocation concealment was not mentioned.
Blinding
In music intervention studies, participants cannot be blinded (unless they are in studies that compare different types of music interventions). Three studies reported blinding personnel. This was achieved by having both music group and control group participants wear headsets and listen to a CD. The control group listened to a blank CD. Twenty‐one studies did not blind personnel, and for two studies blinding of personnel was unclear.
Only seven trials reported blinding of the outcome assessors for objective measures. For 12 trials, the use of blinding was unclear. The other trials did not use blinding. However, it is important to point out that blinding of outcome assessors is not possible in the case of subjective measurement tools (for example, STAI (Spielberger 1983)) unless the participants are blinded to the intervention. We would like to point out that the assessment of risk of bias figure (Figure 3) lists three studies as having used blinding for subjective outcomes. However, these were studies that did not include subjective outcomes. A rating of low risk was assigned if studies did not include subjective outcomes.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Incomplete outcome data
The dropout rate was small for most trials, namely between 0% and 13%. Three trials reported dropout rates of more than 20%. For nine trials it was unclear whether there were any participant withdrawals. Most trials reported reasons for dropout. Detailed information on the dropout rate and reasons is included in the Characteristics of included studies table.
Selective reporting
We did not identify any issues related to selective reporting.
Other potential sources of bias
We did not identify any other potential sources of bias in the studies included in this review.
As a result of the risk of bias assessment, we concluded that two trials were at moderate risk of bias (Ganidagli 2005; Guo 2005). All other trials were at high risk of bias. The main reason for receiving a high risk of bias rating was the lack of blinding. As mentioned before, blinding is often impossible in music therapy and music medicine studies that use subjective outcomes, unless in studies where the music intervention is compared to another treatment intervention (for example, progressive muscle relaxation or different type of music intervention). Therefore, it appears impossible for these types of studies to receive a low or moderate risk of bias even if all other risk factors (for example, randomization, allocation concealment, etc.) have been adequately addressed.
It is worth noting that the Chinese trials were particularly problematic in terms of providing sufficient information regarding risk of bias. It is unclear, however, if this was due to incomplete translations or lack of detail in the original trial reports.
Risk of bias is detailed for each trial in the risk of bias tables included with the Characteristics of included studies table and the 'Risk of bias' summary (Figure 4). In addition, an overall assessment of risk of bias can be viewed in Figure 3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Effects of interventions
Primary outcome
Preoperative anxiety
Twenty trials (N = 1400) examined the effects of music interventions on preoperative anxiety. Thirteen trials measured anxiety by means of the Spielberger State‐Trait Anxiety Inventory ‐ State Anxiety scale (STAI‐S) (Allen 2001; Augustin 1996; Cassidy 2003; Cooke 2005; DeMarco 2012; Guo 2005; Lee 2004; Miluk‐Kolasa 2002; Ni 2011; Szeto 1999; Winter 1994; Yung 2002; Yung 2003). The STAI‐S is a validated and widely used instrument to measure patients' anxiety. It consists of 20 statements aimed at determining a patient's current anxiety level. The total score for STAI‐S ranges from 20 to 80. Seven trials reported mean anxiety measured by other scales such as a numeric rating scale and a visual analogue scale (Chang 1996; Gaberson 1995; Ganidagli 2005; Lee 2011; Lee 2012; Li 2004; Lin 2011). The data of one trial (Bringman 2009) could not be included in the meta‐analysis because, unlike the other studies, midazolam was withheld from participants in the music group but not from the control group. The results of this study are reported separately below.
A meta‐analysis of 13 trials that used the STAI‐S to examine state anxiety in 896 participants indicated significantly lower state anxiety in participants who received standard care combined with music interventions than those who received standard care alone (MD ‐5.72, 95% CI ‐7.27 to ‐4.17, P < 0.00001). The results were consistent across trials (I² = 43%) (Analysis 1.1). In the trial by Bringman (N = 327), participants in the non‐midazolam music listening group reported lower levels of anxiety at post‐test (mean 30, standard deviation (SD) 7.0) than those in the standard care midazolam group (mean 34, SD 7.0) and this difference was statistically significant (P < 0.001). A sensitivity analysis, removing those trials that used inadequate methods of randomization (Arslan 2008; Augustin 1996; Cassidy 2003; DeMarco 2012; Lee 2004) or for which the method of randomization was unclear (Miluk‐Kolasa 2002; Szeto 1999; Yung 2002; Yung 2003), resulted in similar findings (MD ‐5.76, 95% CI ‐7.94 to ‐3.57, P <.00001; I² = 38%) (Analysis 1.1).
The standardized mean difference (SMD) of those trials that reported post‐test anxiety scores on measures different than the STAI‐S (N = 504) also suggested a moderate anxiety‐reducing effect of music (SMD ‐0.60, 95% CI ‐0.90 to ‐0.31, P < 0.0001) (Analysis 1.2). Statistical heterogeneity across the trials (I² = 61%) was due to some trials (Chang 1996; Li 2004; Lin 2011) reporting much larger beneficial effects of music interventions than others. A sensitivity analysis to examine the impact of randomization method, excluding the data of four trials (Chang 1996; Lee 2012; Li 2004; Lin 2011), resulted in a smaller SMD of ‐0.41 (95% CI ‐0.71 to ‐0.12, P = 0.006), but improved the homogeneity of the results (I² = 0%) (Analysis 1.2).
Secondary outcomes
Preoperative sedative drug intake
None of the studies in this review included preoperative sedative drug intake as an outcome variable. Instead, for most studies sedative drug intake was an exclusion criterion: patients who had received preoperative sedative drugs could not participate in the studies. One study (Bringman 2009) compared a non‐midazolam music listening group directly with a midazolam group and found that music listening was more effective than midazolam for preoperative anxiety reduction (see preoperative anxiety section).
Physiological responses
Heart rate (HR)
The pooled estimate of 16 studies (Allen 2001; Augustin 1996; Cassidy 2003; Chang 1996; DeMarco 2012; Evans 1994; Guo 2005; Kushnir 2012; Lee 2004; Lee 2011; Lee 2012; Lin 2011; Ni 2011; Winter 1994; Yung 2002; Yung 2003) indicated that listening to music had a small effect on heart rate (MD ‐2.77, 95% CI ‐4.76 to ‐0.78, P = 0.006; I² = 79%). The results were inconsistent across studies (Analysis 1.3). Ten of these studies used inadequate methods of randomization or did not report the specific randomization method used. A sensitivity analysis excluding these studies from the analysis resulted in a similar MD of ‐2.44 (95% CI ‐5.95 to 1.07, P = 0.17). However, this effect size was no longer statistically significant and the heterogeneity of the studies increased (I² = 90%) (Analysis 1.3).
Two studies (Lee 2011; Lee 2012) examined the impact of music listening on heart rate variability (HRV) in patients awaiting surgery. HRV is gaining acceptance as a measurement of cardiac parasympathetic activity and, therefore, an indicator of a relaxation response (Friedman 2007). Lee stated that "in the frequency‐domain of HRV, low frequencies (LFs; frequencies between 0.04 and 0.15 Hz) reflect mixed sympathetic and parasympathetic activities. High frequencies (HFs; frequencies between 0.15 and 0.4 Hz) reflect parasympathetic activity. High values of the low to high (LF/HF) ratio indicate a dominance of sympathetic activity while low values indicate a dominance of parasympathetic activity. Activation of the sympathetic nerves, as in anxiety, can cause the HR to increase, high frequencies to decrease, and low frequencies and the low‐to‐high ratio to increase" (Lee 2011, p1182). The pooled estimate of these two studies did not show evidence for an effect of music listening on HRV (LF/HF ratio) (MD ‐0.37, 95% CI ‐1.16 to 0.42, P = 0.36; I² = 69%) (Analysis 1.4).
The study by Bringman (Bringman 2009) did not find a statistically significant difference for HR between the music listening group (mean post‐test value of 67 bpm, SD 11) and the midazolam control group (mean post‐test value of 68 bpm, SD 10). However, given that the music listening group did not receive a preoperative sedative whereas the control group did means that music listening was able to achieve the same sedative effects as preoperative sedative drugs.
Finally, one study (Miluk‐Kolasa 1996) reported a ‐2.2% (SD 1.4) reduction from baseline HR for the music listening group (n = 50) and an 11.1% (SD 1.1) increase for the standard care control group (n = 50). In addition, this study measured the impact of music on cardiac output, the volume of blood being pumped by the heart. An increase in cardiac output can be attributed to an increase in HR and sympathetic nervous system activity. A reduction of 3.5% (SD 2.0) was reported in cardiac output for the music group whereas the control group's results indicated an increase of 10.9% (SD 2.1).
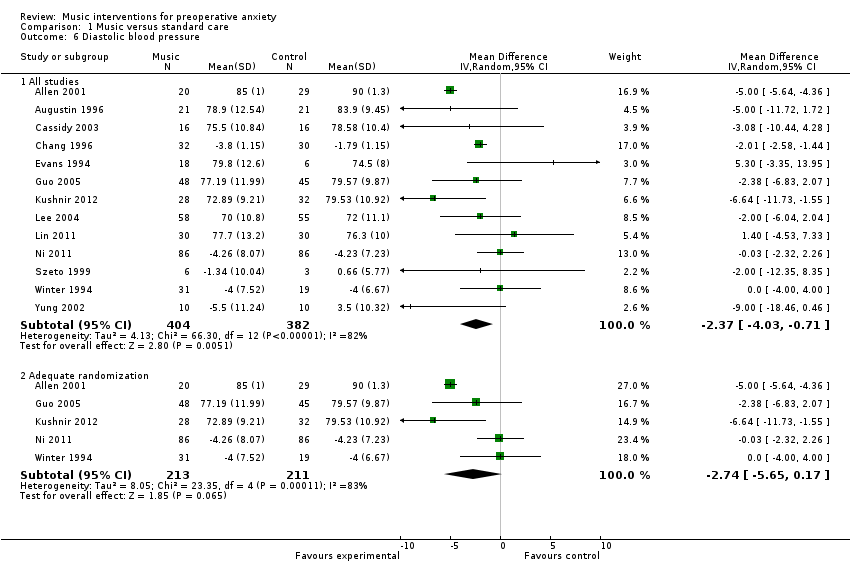
Blood pressure
Fourteen studies (Allen 2001; Augustin 1996; Cassidy 2003; Chang 1996; DeMarco 2012; Evans 1994; Guo 2005; Kushnir 2012; Lee 2004; Lin 2011; Ni 2011; Szeto 1999; Winter 1994; Yung 2002) examined the effects of music listening on systolic blood pressure (SBP). Their pooled estimate indicated no strong evidence of effect for music listening (MD ‐4.82, 95% CI ‐12.13 to 2.49, P = 0.20; I² = 98%) (Analysis 1.5). A pooled estimate of ‐2.37 mm Hg (95% CI ‐4.03 to ‐0.71; 13 studies) was found for diastolic blood pressure (DBP) and this effect was statistically significant (P = 0.005) (Allen 2001; Augustin 1996; Cassidy 2003; Chang 1996; Evans 1994; Guo 2005; Kushnir 2012; Lee 2004; Lin 2011; Ni 2011; Szeto 1999; Winter 1994; Yung 2002). However, the results were inconsistent across studies (I² = 98%) (Analysis 1.6).
We conducted sensitivity analyses to assess the impact of inadequate randomization methods on the results. For SBP, the effect size remained non‐significant and heterogeneity persisted (MD ‐5.80, 95% CI ‐18.96 to 7.36, P = 0.39; I² = 98%) (Analysis 1.5). Likewise, for DBP excluding studies because of inadequate randomization method did not influence the effect size but the results were no longer statistically significant (MD ‐2.74, 95% CI ‐5.65 to 0.17, P = 0.06; I² = 83%) (Analysis 1.6).
A large study (N = 327) by Bringman (Bringman 2009) suggested that music listening can result in similar reductions in SBP and DBP compared with the administration of midazolam. Music listening resulted in mean post‐test values of 131 (SD 16) and 81 (SD 12), respectively, whereas midazolam intake resulted in mean post‐test values of 129 (SD 18) and 81 (SD 14), respectively.
The study by Miluk‐Kolasa (Miluk‐Kolasa 1996) reported a SBP change from baseline of ‐2.0% (SD 0.7) for the music group and 4.9% (SD 0.8) for the standard care control group. Similarly, a reduction in DBP was found for the music group (‐0.8%, SD 1) whereas the DBP in the control group increased by 3.8% (SD 1).
Respiratory rate
Listening to music had a clinically insignificant effect on respiratory rate, namely listening to music increased participants' respiratory rate by one breath per minute compared to standard care (6 studies; MD 0.97, 95% CI 0.82 to 1.11, P < 0.00001). Furthermore, the results were inconsistent across studies (I² = 96%) (Analysis 1.7).
Skin temperature and skin conductivity
Two studies (Chang 1996; Miluk‐Kolasa 1996) included skin temperature as an outcome variable. Increased skin temperature is related to a greater state of relaxation. The two studies could not be pooled because one study (Miluk‐Kolasa 1996) only reported percentage change scores. No difference in skin temperature between the two groups was found in the Chang study (N = 62) (music group mean post‐test value 33.62, SD 0.11; control group mean post‐test value 33.66, SD 0.11). In contrast, Miluk‐Kolasa (N = 100) reported an increase in skin temperature for the music group (4.3%, SD 0.4) and a decrease for the control group (‐3.1%, SD 0.3).
Guo (Guo 2005) included skin conductivity in a study examining the impact of music listening on the anxiety of 93 participants awaiting laparoscopic surgery. Skin conductivity refers to the electrical conductance of the skin, which varies with its moisture level. Because the sweat glands are controlled by the sympathetic nervous system, skin conductance is used as an indication of psychological or physiological arousal or stress response. Even though music group participants reported significantly less anxiety after music listening than control group participants, this self‐reported anxiety reduction was not reflected in the skin conductivity results with a mean post‐test value of 4.54 (SD 0.12) for the music group and 4.03 (SD 1.53) for the control group.
Salivary cortisol
Salivary cortisol is frequently used as a biomarker for psychological stress yet only one study in this review included this as an outcome (Guo 2005). Music listening (mean 3.11, SD 0.92) had a small, statistically significant effect on post‐intervention cortisol levels compared to the standard care control group (mean 3.61, SD 1.08).
Glucose count
Miluk‐Kolasa (Miluk‐Kolasa 1996) included plasma glucose concentrations as an outcome related to stress response in preoperative patients. An increase in blood glucose may be a function of increased stress. Listening to music preoperatively resulted in an average decrease in blood glucose of 6.9% (SD 1.9). In contrast, an average increase of 10.2% (SD 2.0) was found in the standard care control group.
Physical outcomes
None of the studies in this review included physical outcomes such as infection rate or wound healing. Some studies measured the effect of music on pain, but this outcome was not included in this review because of overlap with a published Cochrane review on music interventions for pain (Cepeda 2006).
Patient satisfaction
None of the studies included in this review included patient satisfaction as an outcome.
Discussion
Summary of main results
Preoperative anxiety
The results of 20 trials suggest that music listening may have a beneficial effect on anxiety in people awaiting surgery. Music listening resulted, on average, in an anxiety reduction that was 5.72 units greater than that of the standard care group, as measured by the STAI‐S. At this time, there is no consensus on what constitutes a clinically significant change in anxiety as measured by the STAI‐S. However, assessment of clinical significance is often determined using 0.5 standard deviation (SD) of the baseline measure as a guideline (Sloan 2005). Baseline SDs of studies included in this review ranged from 5.7 to 10.66, with a mean SD of 8.77. Based on the 0.5 SD rule, the difference between the treatment group and control group found in this review could therefore be considered clinically significant. Studies that used anxiety scales other than the STAI‐S resulted in a difference of ‐0.60 standardized units. Although the magnitude of the effect differed across the studies that used non‐STAI anxiety scales, the trials agreed on the direction of the point estimates. These anxiety‐reducing results are considered moderate in size according to interpretation guidelines put forth by Cohen (Cohen 1988). Cohen suggested that an effect size of 0.2 be considered a small effect, an effect size of 0.5 medium, and an effect size of 0.8 large.
Preoperative sedative drug intake
None of the studies in this review included preoperative sedative drug intake as an outcome variable. However, the results of one study that compared a non‐midazolam music listening group directly with a midazolam group found that music listening was more effective than midazolam for preoperative anxiety reduction.
Physiological responses
As for the effect of music on physiological responses, the results of 16 studies suggest that music listening has a small effect on heart rate, but these results were inconsistent across studies. No evidence was found for an effect of music listening on heart rate variability (HRV). However, the HRV result is based on two studies and more research is needed. One study reported that music listening significantly reduced cardiac output compared to a standard care control group.
Mixed results were found for blood pressure. Whereas no support for an effect of music was found for systolic blood pressure, those same studies did find support for an effect of music on diastolic blood pressure, although again the results were inconsistent across studies.
Listening to music had a clinically insignificant effect on respiratory rate, namely listening to music resulted in a respiratory rate that was faster by one breath per minute compared to the control group. The results were highly inconsistent across studies.
The results on the effect of music listening on skin temperature and skin conductivity were inconclusive with one study finding support for a beneficial effect and two studies failing to demonstrate such support.
Finally, single studies found a small, statistically significant effect of music on cortisol levels and blood glucose levels.
No studies were identified that addressed the other secondary outcomes listed in the protocol, namely physical outcomes and patient satisfaction.
Overall completeness and applicability of evidence
This review included 26 randomized and quasi‐randomized controlled trials. All trials used listening to pre‐recorded music as the music intervention. No music therapy trials, as defined by the authors in the background section, were included in this review. Although we found several music therapy studies that measured preoperative anxiety, these studies could not be included because they did not use a control group, suffered from insufficient data reporting, or failed to use standardized measures of anxiety.
In general, the trials that used listening to pre‐recorded music included limited information about the music selections used, except for mentioning general music styles (for example new age, classical music, easy listening, etc.). Music within each of these styles can vary widely and more detailed information would help clinicians make well‐informed decisions regarding music selections. More research is needed to evaluate the effect of music that is truly patient‐preferred, as well as the effect of music with different characteristics (tempo, timbre, harmony, emotional intensity, etc.) on patients during high anxiety situations such as when awaiting surgery.
Most trials used one music intervention session of 20 to 30 minutes. This clinical uniformity adds to the strength of this review, but also leaves several questions unanswered. First, the relationship between the frequency and duration of treatment and treatment effect remains unclear. Could it be that multiple music sessions before the onset of surgery, where feasible, result in greater benefit? Two studies (Li 2004; Lin 2011) did offer multiple music sessions starting with the first session several days before surgery and continuing to the day of the surgery. Compared to other studies, these two studies resulted in greater anxiety reduction. We would like to suggest that offering multiple music listening sessions allows for the patient to give feedback about the music, select different music if needed, and become more skilled in using music for relaxation purposes. Further investigation into the optimal frequency and duration of music interventions for presurgical patients is needed. In addition, since no music therapy interventions that use live music to meet specific in‐the‐moment needs of the patients were included in these studies, we were unable to determine whether these would be more effective than listening to pre‐recorded music.
Presently, no data can be provided regarding cost or cost‐effectiveness of the use of music interventions in the presurgical arena as these data were not included in the trials reviewed.
Because little information was provided in these studies about the ethnic make‐up of the patient samples, one can question the generalizability of these results to various ethnic groups. Persons' cultures may influence their music preferences and their potential acceptance and use of music as a therapeutic agent, especially during high‐stress medical situations such as surgery. This in turn may influence the anxiety‐reducing potential of music, to a greater or lesser degree.
Quality of the evidence
In general the quality of reporting was poor, with only 11 studies detailing the methods of randomization and allocation concealment, and level of blinding. The chief investigators of many studies needed to be contacted to provide additional methodological and statistical information. All but two studies received a high risk of bias rating.
Because of the large number of trials at high risk of bias, the findings of this review need to be interpreted with caution. It is important to be mindful that many studies received a high risk of bias because of lack of blinding. Often blinding of participants is not possible in music medicine or music therapy studies unless a comparative design is used (for example, comparing listening to pre‐recorded music with interactive music making with a therapist). When participants cannot be blinded to the intervention, there is definitely an opportunity for bias when participants are asked to report on subjective outcomes such as anxiety. However, this also means that trials that meet all other requirements for a low risk of bias rating are assigned a high risk of bias because of the inability to meet the blinding requirement for subjective outcomes.
For anxiety, consistent effects were obtained across studies. For the other outcomes included in the protocol, inconsistent results were obtained or not enough studies were available.
In summary, the quality of evidence was low (summary of findings Table for the main comparison).
Potential biases in the review process
The strength of our review is that we searched all available databases and a large number of music therapy journals (English, German, and French language), checked reference lists of all relevant trials, contacted relevant experts for identification of unpublished trials, and included publications without restricting language. In spite of such a comprehensive search, it is still possible that we missed some published and unpublished trials. We requested additional data, where necessary, for all trials we considered for inclusion. This allowed us to get accurate information on the trial quality and data for most trials and helped us make well‐informed trial selection decisions.
It is possible that we did not identify some grey literature; however, it is doubtful that this would have had a significant impact on our results. Grey literature tends to include trials with relatively small numbers of participants and inconclusive results (McAuley 2000).
Agreements and disagreements with other studies or reviews
The findings of this review are consistent with the results of a review (26 studies) on the effects of music interventions on anxiety in patients awaiting minimally invasive procedures (Gillen 2008). Gillen and colleagues reported that music had a consistent and statistically significant effect on pre‐procedural anxiety. However, no consistent effects were found for physiological responses. Based on these results, they questioned the adequacy of current theories that link anxiety and the autonomic nervous system and the impact that music listening may have on these processes. Similarly, a review by Pittman and Kridli (Pittman 2011) (11 studies) found that music listening consistently reduced anxiety in patients awaiting surgery or invasive medical procedures. However, they reported inconsistent results regarding music’s effectiveness in lowering blood pressure, heart rate, and respiration in presurgical and pre‐procedural patients.
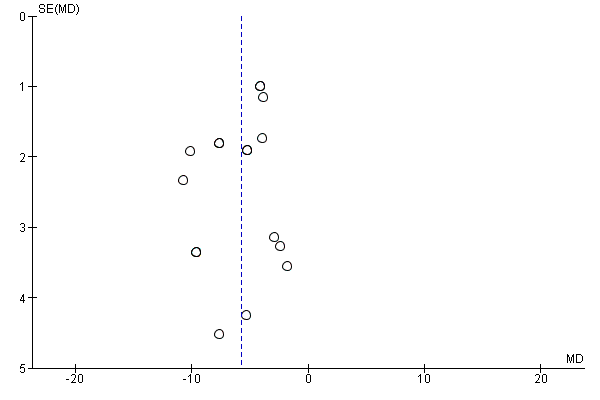
Funnel plot of comparison: 1 Music versus standard care, outcome: 1.1 State Anxiety STAI.

Excluded Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Music versus standard care, Outcome 1 State anxiety STAI).

Comparison 1 Music versus standard care, Outcome 2 Anxiety (non‐STAI).
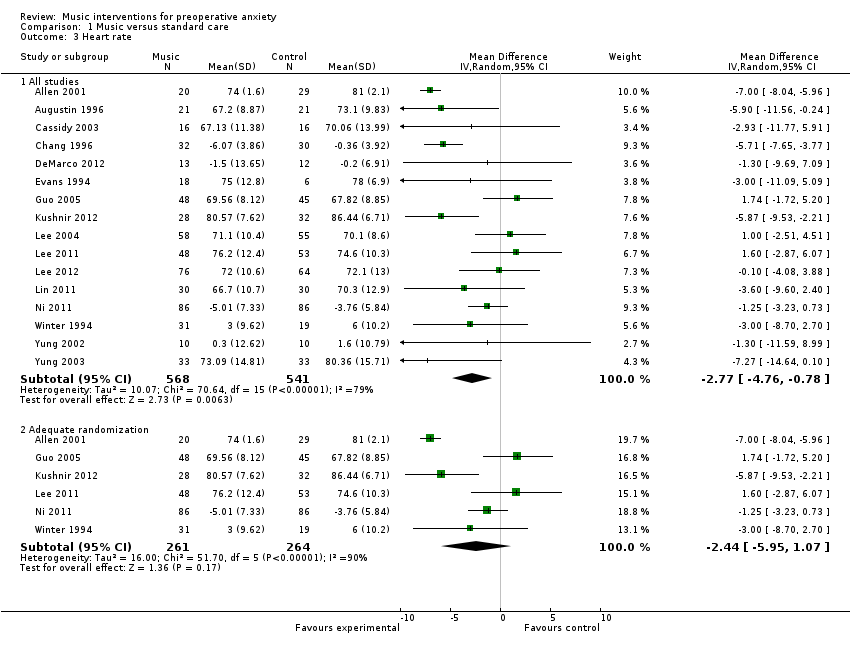
Comparison 1 Music versus standard care, Outcome 3 Heart rate.

Comparison 1 Music versus standard care, Outcome 4 Heart rate variability ‐ LF/HF ratio.

Comparison 1 Music versus standard care, Outcome 5 Systolic blood pressure.
Comparison 1 Music versus standard care, Outcome 6 Diastolic blood pressure.

Comparison 1 Music versus standard care, Outcome 7 Respiratory rate.
| Patient or population: patients with preoperative anxiety | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Standard care | Music | |||||
| Preoperative anxiety (STAI) | The mean preoperative anxiety (stai) ranged across control groups from | The mean preoperative anxiety (stai) in the intervention groups was | 896 | ⊕⊕⊝⊝ | ||
| Preoperative anxiety (non‐STAI) | The mean preoperative anxiety (non‐stai) in the intervention groups was | 504 | ⊕⊕⊝⊝ | |||
| Heart rate | The mean heart rate ranged across control groups from | The mean heart rate in the intervention groups was | 1109 | ⊕⊝⊝⊝ | ||
| Heart rate variability | The mean heart rate variability ranged across control groups from | The mean heart rate variability in the intervention groups was | 241 | ⊕⊝⊝⊝ | ||
| Systolic blood pressure | The mean systolic blood pressure ranged across control groups from | The mean systolic blood pressure in the intervention groups was | 809 | ⊕⊝⊝⊝ | ||
| Diastolic blood pressure | The mean diastolic blood pressure ranged across control groups from | The mean diastolic blood pressure in the intervention groups was | 786 | ⊕⊝⊝⊝ | ||
| Respiratory rate | The mean respiratory rate ranged across control groups from | The mean respiratory rate in the intervention groups was | 375 | ⊕⊝⊝⊝ | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The majority of the trials were assessed as high risk of bias studies | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 State anxiety STAI) Show forest plot | 13 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 All studies | 13 | 896 | Mean Difference (IV, Random, 95% CI) | ‐5.72 [‐7.27, ‐4.17] |
| 1.2 Adequate randomization | 4 | 435 | Mean Difference (IV, Random, 95% CI) | ‐5.76 [‐7.94, ‐3.57] |
| 2 Anxiety (non‐STAI) Show forest plot | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 All studies | 7 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐0.90, ‐0.31] |
| 2.2 Adequate randomization | 3 | 182 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 3 Heart rate Show forest plot | 16 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 All studies | 16 | 1109 | Mean Difference (IV, Random, 95% CI) | ‐2.77 [‐4.76, ‐0.78] |
| 3.2 Adequate randomization | 6 | 525 | Mean Difference (IV, Random, 95% CI) | ‐2.44 [‐5.95, 1.07] |
| 4 Heart rate variability ‐ LF/HF ratio Show forest plot | 2 | 241 | Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.16, 0.42] |
| 5 Systolic blood pressure Show forest plot | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 All studies | 14 | 809 | Mean Difference (IV, Random, 95% CI) | ‐4.82 [‐12.13, 2.49] |
| 5.2 Adequate randomization | 5 | 424 | Mean Difference (IV, Random, 95% CI) | ‐5.80 [‐18.96, 7.36] |
| 6 Diastolic blood pressure Show forest plot | 13 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 All studies | 13 | 786 | Mean Difference (IV, Random, 95% CI) | ‐2.37 [‐4.03, ‐0.71] |
| 6.2 Adequate randomization | 5 | 424 | Mean Difference (IV, Random, 95% CI) | ‐2.74 [‐5.65, 0.17] |
| 7 Respiratory rate Show forest plot | 6 | 375 | Mean Difference (IV, Fixed, 95% CI) | 0.97 [0.82, 1.11] |

