Intervencija glazbom kod mehanički ventiliranih pacijenata
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Cross‐over design | |
| Participants | Adults with diseases necessitating at least 3 days of invasive mechanical ventilation Diagnoses: respiratory (n = 20), cardiovascular (n = 20), neurological (n = 3), other (n = 6) Average length of mechanical ventilation before onset of study: group A: 11 days (8 to 17); group B: 12 days (6 to 30) Ventilator mode: self‐triggering mode Type of airway: not reported N randomized: 55 N analysed: 49 Sex: 17 F, 32 M Age: 62 (3) y Ethnicity: not reported Setting: critical care unit Country: Canada | |
| Interventions | Two study conditions: 1. music condition: listening to music via headphones of an MP3 player 2. placebo sham condition: wearing headphones of an MP3 player with nothing (no music) playing Music selections provided: Bach (Air from Suite for Orchestra No. 3, Bach (Air for G string), Beethoven (Moonlight Sonata), Beethoven (Pathetic Sonata), Brahms (Lullaby), Chopin (Nocturne in G), Debussy (Clair de Lune), Pachelbel (Canon in D), St‐Saens (The Swan), Tchaïkovsky (Panorama from Sleeping Beauty) Number of sessions: 4 (2 music, 2 sham) Length of session: 60 minutes Categorized as music medicine study | |
| Outcomes | Sedative drug intake (fentanyl, benzodiazepines, hypnotic propofol): post‐test scores Heart rate (HR), respiratory rate (RR), arterial pressure (AP): cannot be included in meta‐analysis since means and standard deviations (SD) are not reported Information was requested from the authors but was not received Blood cortisol: change scores Blood ACTH/cortisol ratio: change scores Blood prolactin: post‐test scores Blood leptin: post‐test scores IL‐6: post‐test scores C‐reactive protein (CRP): no statistical information methionine‐enkephalin content (MET‐enkephalin): post‐test scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated block randomization list was prepared by the investigators" (p. 443) |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was concealed using numbered, opaque sealed envelopes and was revealed by an ICU staff member not involved in the direct care of the randomized patient". (p. 443) |
| Blinding (performance bias and detection bias) | Low risk | Blinding of participants was not possible. Staff who administered music or sham were aware of group assignment but these staff were not involved in direct care of the participant |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Each apparatus [MP3 player] was blinded such that the nurse committed in sedative drug tapering was unable to perceive in which group the patient belonged to" (p.444) |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate: 10.9%. Quote: "Of the 55 randomized patients, 6 patients did not complete all of the requirements of the protocol (missing listening sessions, missing blood samples, non‐completion of the 3‐day MV experimental follow‐up), and their data were therefore excluded from the analyses" (p. 445) |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Free from financial conflict of interest | Low risk | Funded by dedicated grants from CRCEL‐CHUS (PAFI). This trial is registered in ClinicalTrials.gov: NCT00880035. The authors declare no conflict of interest and they were neither funded to select specific MP3 devices nor to select special music pieces. |
| Methods | Two‐arm parallel group design | |
| Participants | Adults necessitating mechanical ventilation Diagnoses: pulmonary‐related (80%), miscellaneous (20%) (e.g., cancer and kidney transplant) Average length of mechanical ventilation before onset of study: control group: 5.4 days; music group 14.5 days (due to one patient in music group with a ventilator length of 72 days) Ventilator mode: not reported Type of airway: not reported N randomized to music group: 11 N randomized to control group: 9 N analysed in music group: 11 N analysed in control group: 9 Sex: 7 F, 13 M Age: 59.95 y Ethnicity: not reported Setting: critical care units Country: USA | |
| Interventions | Two study groups:
Music selections provided: classical selections from Music for Relaxation (Helen Bonny) Number of sessions: 1 Length of session: 30 minutes Categorized as music medicine study | |
| Outcomes | Mood (Profile or Mood States): post‐test scores Heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure, oxygen saturation, airway pressure: change scores from pre‐test to post‐test | |
| Notes | No standard deviations were reported for post‐test scores. Additional data were obtained from the lead author. Change scores were computed by JB. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Flip of coin (personal communication with principle investigator (PI)) |
| Allocation concealment (selection bias) | Low risk | Achieved through use of flip of coin for each patient after consent was obtained |
| Blinding (performance bias and detection bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | The outcome assessor was not blinded (personal communication with PI) |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No subject loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Free from financial conflict of interest | Low risk | This study was supported in part by a grant, sponsored by the Medtronic Corporation, from the Greater Twin Cities Area Chapter ‐ American Association of Critical Care Nurses. |
| Methods | Two‐arm parallel group design | |
| Participants | Adults necessitating mechanical ventilation Diagnoses: pulmonary related (68%), cancer (4%), heart transplant (4%), trauma (5%), miscellaneous (19%) Average length of mechanical ventilation before onset of study: 7.39 days (SD 10.39) Most common ventilator mode: Synchronized Intermittent Mandatory Ventilation (SIMV) (70%). Other ventilator modes: pressure support (PS), positive end expiratory pressure (PEEP), continuous positive airway pressure (CPAP), assist/control (A/C) Type of airway: not reported N randomized to music group: 27 N randomized to control group: 27 N analysed in music group: 27 N analysed in control group: 27 Sex: 59% F, 41% M Age: 57.1y Ethnicity: 92.5% white, 5.5% black, and 2% Native American Setting: critical care units Country: USA | |
| Interventions | Two study groups:
Music selections provided: classical, new age, country/western, religious, and easy listening. Number of sessions: 1 Length of session: 30 minutes Categorized as music medicine study | |
| Outcomes | State anxiety: post‐test scores on the Spielberger State Anxiety Inventory (6‐item version) Heart rate: post‐test scores (at 30 minutes) Respiratory rate: post‐test scores (at 30 minutes) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were randomized using a table of random numbers, to either the control or treatment condition" (p.44) |
| Allocation concealment (selection bias) | Low risk | Confirmed through personal communication with author |
| Blinding (performance bias and detection bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were not blinded (personal communication with PI) |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate: 7% |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Free from financial conflict of interest | Low risk | Unfunded study |
| Methods | Two‐arm parallel group design | |
| Participants | Adults receiving mechanical ventilation in critical care unit Diagnoses: pneumonia (5), respiratory failure (2), shortness of breath (1), ventricular tachycardia (1), and ischaemic bowel (1) Average length of mechanical ventilation before onset of study: 14.2 (15) days Ventilator modes: A/C (6), SIMV (2), and pressure‐release (2) Type of airway: not reported N randomized to music group: 5 N randomized to control group: 5 N analysed in music group: 5 N analysed in control group: 5 Age: 64.9 (7.8) y Sex: 6 F, 4 M Ethnicity: 90% white, 10% black Setting: critical care unit Country: USA | |
| Interventions | Two study groups: 1. Music group: listening to patient‐selected music via headphone 2. Control group: rest quietly without headphones Number of sessions: 1 Length of session: 60 minutes Categorized as music medicine study | |
| Outcomes | Corticotropin, cortisol, epinephrine and norepinephrine blood samples were obtained from central venous catheter at 4 intervals: baseline, 15 minutes after baseline, 30 minutes after baseline, and 60 minutes after baseline Heart rate: at baseline, 15 minutes after baseline, 30 minutes after baseline, and 60 minutes after baseline | |
| Notes | The data of this study cannot be pooled with data from other studies in this review because of several confounding variables that likely impacted the outcomes at post‐test: wide variability in mean levels of biomarkers, a very small sample size, administration of intravenous morphine sulphate to 2 control subjects immediately prior to intervention, and 2 subjects in the experimental group needed endotracheal suctioning during the intervention. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Flip of coin (personal communication with PI) |
| Allocation concealment (selection bias) | Low risk | Achieved through use of flip of coin |
| Blinding (performance bias and detection bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were not blinded (personal communication with PI) |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not include subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No subject loss |
| Selective reporting (reporting bias) | Unclear risk | No evidence of selective reporting |
| Free from financial conflict of interest | Low risk | This study was supported in part by a grant‐in‐aid from the University of Minnesota Graduate School awarded to Dr Linda Chlan and in part by National Science Foundation grant IBN‐0112543 awarded to Dr William Engeland |
| Methods | Three‐arm parallel group design | |
| Participants | Adults receiving acute mechanical ventilatory support because of respiratory failure or distress Indication for mechanical ventilation: respiratory failure (n = 63, 63, 61, patient‐directed music group, noise‐cancelling headphones group, usual care group respectively), respiratory distress (n=32, 27, 36), pneumonia (n = 7, 5, 7), respiratory arrest (n = 3, 4, 4), airway protection (n = 2, 5, 4), postoperative (n = 2, 3, 4), COPD (n = 7, 4, 0), hypoxia (n = 2, 3, 2), ARDS (n = 1, 1, 0), tachypnoea (n = 1, 0, 1), cardiac arrest (n = 4, 2, 5), pulmonary edema (n = 1, 0, 0), asthma (n = 0, 0,1), and other or missing (n = 1, 5, 0) Average length of mechanical ventilation before onset of study: patient‐directed music group: 4.5 days (0‐35); noise‐cancelling headphones group: 6.0 days (1‐79), and usual care group: 6.0 days (0 to 38) Ventilator mode:not reported Type of airway: not reported N randomized to patient‐directed music group: 126 N randomized to noise‐cancelling headphones group: 122 N randomized to usual care group: 125 N analysed to music‐directed group: 82 for anxiety analysis, 87 for sedation analysis N analysed to noise‐cancelling headphones group: 76 for anxiety analysis, 90 for sedation analysis N analysed to usual care group:83 for anxiety analysis, 89 for sedation analysis Sex: 193 F, 180 M Age: 59 Ethnicity: White (86%); other ethnicities not reported Setting: critical care units at 5 hospitals in Minnesota Country: USA | |
| Interventions | Three study groups:
Music selections provided: starter set of 6 CDs were reviewed with the patient by the research nurse to provide for immediate listening upon randomization to the PDM group. The starter set included relaxing music played on piano, harp, guitar, and Native American flute. Within 24 hours of randomization, the music therapist completed a music preference assessment on each PDM patient using a tool designed to assess music preferences of mechanically ventilated patients with a simple yes or no format Number of sessions: the use of listening to music or noise‐cancelling headphones was patient‐directed. Nursing staff were encouraged to offer the music at least twice per shift but they were reminded that the decision to listen to music was determined by the patient Length of session: variable, determined by the patient. Average length of music listening was 79.8 (SD = 126) minutes per day. Average length of wearing noise‐cancelling headphones by the NCH group participants was 34 (89.6) minutes per day Categorized as music medicine study | |
| Outcomes | State anxiety (Visual Analogue Scale ‐ Anxiety), daily sedative drug intensity, daily sedative drug dose frequency: change scores compared to usual care group and mixed models analysis results are reported. Means and SDs per measurement point are not reported Extubation rate at end of study Mortality rate Urinary free cortisol (UFC) (from subsample of patients with intact renal function and not receiving medications known to influence cortisol levels (n = 65) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated random numbers list allocated patients to 1 of 3 groups" (p. 2336) |
| Allocation concealment (selection bias) | Low risk | Quote: "Group assignment was concealed in an opaque envelope" (p. 2336) |
| Blinding (performance bias and detection bias) | High risk | Blinding of the participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measure was used for the subjective outcomes |
| Incomplete outcome data (attrition bias) | High risk | Attrition rates for the PDM, NCH, and usual care group were 34.9%, 37.7%, and 33.6% respectively for anxiety analysis and 27.7%, 22.9%, and 28% for the sedation analysis. Reasons for attrition were: participants were not able to complete anxiety assessments each day due to fatigue, medical condition, state of sedation, inability or refusal to complete assessments, or were off the unit (p. 2338) |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Free from financial conflict of interest | Low risk | This study was funded by grant R01‐NR009295 from the National Institutes of Health, National Institute of Nursing Research. The study is registered on clinicaltrials.gov: NCT00440700. |
| Methods | Two‐arm parallel group design | |
| Participants | Critically ill adults on mechanical ventilation Average length of mechanical ventilation before onset of study: not reported Ventilator modes: not reported Type of airway: not reported N randomized to music group: 5 N randomized to control group: 5 N analysed in music group: 5 N analysed in control group: 5 Sex: 1 F, 9 M Age M: 59.9 y Ethnicity: not reported Setting: critical care unit Country: Germany | |
| Interventions | Two study groups:
Music selection: "slow‐moving" Mozart piano sonatas selected based on compositional elements of relaxation, according to the author: KV283, Andante; KV311, Andantino con espressione; KV330, Andante cantabile; KV332, Adagio; KV333, Andante cantabile; KV545, Andante; KV570, Adagio; and KV576, Adagio Number of sessions: 1 Length of session: 60 min | |
| Outcomes | Sedative drug intake, heart rate variability, arterial pressure, serum level of dehydroepiandrosterone (DHEAS), serum concentrations of growth hormone, interleukin‐6: for these variables, means and standard error of the mean (SEM) are given for the control group but not for the music group. Only general statements such as "serum levels of dehydroepiandrosterone remained unchanged during the music intervention" are provided for the music group. Exact P values of between‐group changes are given for mean arterial pressure, growth hormone, interleukin‐6, epinephrine, and DHEAS, but no mean differences are reported Prolactin, norepinephrine, adrenocorticotropic hormone (ACTH), cortisol, prolactin monomer: only P values are given Because of the limited data reporting, results of this study are only discussed in narrative form in this review | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate assignment (personal communication with PI) |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not possible because of the use of alternate assignment |
| Blinding (performance bias and detection bias) | Low risk | Participants could not be blinded. Nursing staff who performed outcome assessments were blinded as to whether the patient received music via the headphones |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded (personal communication with PI) |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not include subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No subject loss |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Free from financial conflict of interest | Low risk | "The authors did not disclose any conflicts of interest" (p. 2709) |
| Methods | Two‐arm parallel group design | |
| Participants | Adults in ICU who are mechanically ventilated Indications for mechanical ventilation: abdominal surgery (n = 5), pneumonia (n = 4), cardiovascular (n = 3), sepsis (n = 3), heart transplant (n = 1), lung transplant (n = 1), pancreatitis (n = 1), respiratory distress (n = 1), and trauma (n = 1) Average length of mechanical ventilation before onset of study: 24.6 (3 to 137) days Ventilator mode: pressure support ventilation or assisted spontaneous breathing Type of airway: not reported N randomized to music group: 10 N randomized to control group: 10 N analysed in music group: 10 N analysed in control group:10 Sex: 8 F, 12 M Age: 52.2 (15.3) y Ethnicity: not reported Setting: critical care units Country: the Netherlands | |
| Interventions | Two study groups:
Music selections provided: participants were asked to select from classical music or easy listening music. The types of music offered were classical (Anton Bruckner: Quintet F‐Dur: Adagio and Gustav Mahler: Symphony Nr. 4 G‐Dur: Ruhevoll) and easy listening (film music: Vangelis: 1492, songs without vocals were chosen). Both types of music had slow beats and were relaxing Number of sessions: 3 sessions spread over 2 days Length of session: 30 minutes Categorized as music medicine study | |
| Outcomes | HR, RR, AP, SBP, DBP, sedation scores: change scores Mortality | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"Twenty subjects were randomly assigned to either the experimental or control group by the researcher who used a manual method (drawing lots)" (p. 1032) |
| Allocation concealment (selection bias) | High risk | No allocation concealment was used. Lots were drawn by research team member but not in presence of the participant |
| Blinding (performance bias and detection bias) | High risk | Blinding of the participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "During the music intervention or rest periods, data on physiological parameters and sedation scores were recorded by the attending nurse. The nurse was unaware of the background of the study, to limit bias in the registration of parameters and sedation scores |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not address subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No participant loss. Missing values are clearly explained by the authors (p. 1034‐5) |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Free from financial conflict of interest | Low risk | Unfunded research study |
| Methods | Three‐arm parallel group design | |
| Participants | Adults necessitating mechanical ventilation through synchronized intermittent mandatory ventilation or pressure control mode, or both Diagnoses: cardiovascular disease (60%), respiratory problems (26%), and digestive system disease (13%) Average length of mechanical ventilation before onset of study: 3.47 (1 to 161) days Ventilator mode: most common type of ventilatory support was the synchronized intermittent mandatory ventilation mode (86.9%) Type of airway: oral endotracheal tube (89.1%), tracheotomy tube (10.9%) N randomized to music group: 44 N randomized to placebo group: 44 N randomized to control group: 49 N analysed in music group: 44 N analysed in placebo group: 44 N analysed in control group: 49 Sex: 77 F, 60 M Age: 46.18 y Ethnicity: 100% Chinese Setting: critical care units Country: China | |
| Interventions | Three study groups:
Music selections provided: participants were asked to select from investigator's selection. There were over 40 choices from four categories of relaxing music, including Western classical music (e.g. Moonlight Sonata, Appassionata), Western light music (e.g. Brahms Lullaby, Ballade pour Adeline), Chinese traditional music (e.g. Butterfly Lovers, Moonlight of Spring River) and Chinese folk songs with lyrics (e.g. Song of Jasmine, Rhythm of a Running Stream). All the musical options were of a relaxing nature containing slow, flowing rhythms that duplicate pulses of 60 to 80 beats per minute (Chlan 1998, 2000) and were familiar to Chinese people Number of sessions: 1 Length of session: 30 minutes Categorized as music medicine study | |
| Outcomes | State anxiety (STAI ‐ Chinese version), HR, RR, SBP, DBP, Sa02: change scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was generated from the Randomiser website of the Social Psychology Network (1997)" (p. 980) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Personnel were not blinded. Authors write that "participants were unaware about the design of the study and the groups assigned to them" (p. 980) |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "The researcher remained in the room to record the physiological measures across the three groups during the procedure" (p.980). The researcher knew whether participants were listening to music or not |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measure was used for subjective outcome |
| Incomplete outcome data (attrition bias) | Low risk | No participant loss |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Free from financial conflict of interest | Low risk | This research was funded by the Special Departmental Research Grant from the School of Nursing, The Hong Kong Polytechnic University |
| Methods | Cross‐over trial | |
| Participants | Adults on mechanical ventilation Diagnoses: post‐surgical (9), pancreatitis (2), respiratory issues (2), sepsis (2) Average length of mechanical ventilation before onset of study: not reported Ventilator mode: not reported Type of airway: oral endotracheal tube (87%), tracheostomy (13%) N analysed in music condition: 15 (ventilated patients only ‐ see notes) N analysed in control condition: 15 (ventilated patients only ‐ see notes) Age: 58 (7.8) y Sex: 7 F, 8 M Ethnicity: not reported Setting: critical care unit Country: France | |
| Interventions | Two conditions:
Music selection used: a compilation of patient‐preferred music was made by a music therapist according to the following tempo guidelines: the music started at 90 to 100 beats per minute (bpm), then slowed down to 50‐60 bpm. The last 5 minutes, the tempo was increased to 70 to 80 bpm to re‐energize the patient The music therapist did not implement the music intervention sessions Number of sessions: 1 Length of session: 20 minutes Categorized as music medicine study | |
| Outcomes | Heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure: at 15 minute intervals Because the music selections followed a U‐curve (decreasing the tempo and then increasing during the last 5 minutes to re‐energize the patient), the data of the 15‐minute interval was used The study report does not include standard deviations and precise data for each group. This information was obtained from the lead author. | |
| Notes | This study compared ventilated patients (n = 15) with non‐ventilated patients (n = 15). All patients were randomized to receive music listening followed by a period of rest or to first receive a period of rest followed by a period of music. Only data of the ventilated patients were used in this review. Group‐specific data were obtained from the author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers (personal communication with PI) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Blinding of the participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded to treatment (personal communication with author) |
| Blinding of outcome assessment (detection bias) | Unclear risk | This study did not include subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate for entire study sample (see notes) was 14%. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Free from financial conflict of interest | Unclear risk | Funding information is not provided. Conflict of interest statement is lacking |
| Methods | Two‐arm parallel group design | |
| Participants | Adults in ICU receiving mechanical ventilation Average length of mechanical ventilation before onset of study: 8.32 (SD = 1.37) days within a range of 1 to 30 days Medical diagnoses: pulmonary (n = 25), heart failure (n = 21), chronic kidney failure (n = 5), pancreatitis (n = 4) and liver failure (n = 5) Ventilator mode: positive end‐expiratory pressure Type of airway: not reported N randomized to music group: 30 N randomized to control group:30 N analysed in music group: not reported N analysed in control group:not reported Sex: 28 F, 32 M Age: 45.31 y Ethnicity: 100% Turkish Setting: critical care units Country: Turkey | |
| Interventions | Two study groups:
Music selections provided: Bach’s 19 trio sonatas played by James Galway on flute, 60 to 66 beats per minute Number of sessions: 1 Length of session: 60 minutes Categorized as music medicine study | |
| Outcomes | HR, RR, SBP, DBP, SaO2: only P values and visual graphs are reported. We contacted the authors to obtain means and SDs but no reply was received | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. We contacted the authors for additional information but no reply was received |
| Allocation concealment (selection bias) | Unclear risk | Not reported. We contacted the authors for additional information but no reply was received |
| Blinding (performance bias and detection bias) | Unclear risk | Not reported. We contacted the authors for additional information but no reply was received |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "The research nurse was not blinded as to the allocation of each group" (p.1033). All physiological responses were recorded from a monitoring device by the research nurse |
| Blinding of outcome assessment (detection bias) | Low risk | This study did not include subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported. We contacted the authors for additional information but no reply was received |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Free from financial conflict of interest | Low risk | This study was funded by Ege University Research Foundation |
| Methods | Two‐arm parallel group design | |
| Participants | Adults on mechanical ventilation Diagnoses: respiratory problems (39%) and postoperative surgical problems (34.3%) Average length of mechanical ventilation before onset of study: 2.5 (3.3) days Most frequently used ventilator mode: pressure support (PS) (89%) Most common type of airway: oral endotracheal tube (91%). Other: nasal (4%) and tracheostomy (4%) Ethnicity: Chinese N randomized to music group: unclear N randomized to control group: unclear N analysed in music group: 32 N analysed in control group: 32 Sex: 18 F, 46 M Age: 69.4 y Ethnicity: 100% Chinese Setting: critical care unit Country: China | |
| Interventions | Two study groups:
Music selections provided: Chinese classical music, religious music (Buddhist and Christian), Western classical music and music with "natural sounds" Number of sessions: 1 Length of session: 30 minutes Categorized as music medicine study | |
| Outcomes | State anxiety: change scores from pre‐test to post‐test on the Spielberger State Anxiety Inventory (6‐item version) Heart rate: change scores from pre‐test to post‐test Respiratory rate: change scores from pre‐test to post‐test Systolic blood pressure: change scores from pre‐test to post‐test Diastolic blood pressure: change scores from pre‐test to post‐test | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were randomly assigned to either experimental or control group by having a case nurse draw lots" (p. 613) |
| Allocation concealment (selection bias) | Low risk | Achieved through use of draw of lots by independent group assigner after consent was obtained |
| Blinding (performance bias and detection bias) | Low risk | Participants could not be blinded. Personnel were blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The researcher was blind to the treatment condition of both groups during the whole period of data collection" (p. 614) |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measure was used for subjective outcome |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analysed equals the number of participants recruited |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Free from financial conflict of interest | Unclear risk | Funding information is not provided. Conflict of interest statement is lacking |
| Methods | Randomized controlled trial Randomization method: alternate assignment Allocation concealment: inadequate Blinding: unclear Design: repeated measures control group design Intention to treat: adequate | |
| Participants | Adults with various diagnoses on mechanical ventilation: cardiac problems (56%), pulmonary issues (21%), traumatic injury (8%), other (15%) Average length of mechanical ventilation before onset of study: not reported Ventilator mode: not reported Type of airway: no tracheostomy N randomized to music group (medical): 10 N randomized to music group (cardiac): 10 N randomized to control group (medical): 10 N randomized to control group (cardiac): 10 N analysed in music group (medical): 10 N analysed in music group (cardiac): 9 (not included in this review) N analysed in control group (medical): 10 N analysed in control group (cardiac): 10 (not included in this review) Sex: 10 F, 10 M (for medical, non‐cardiac patients) Age: 57.5 y Ethnicity: not reported Setting: critical care unit Country: USA | |
| Interventions | Two study groups:
Patient‐selected live music used. Music therapist used guitar and voice Number of sessions: 1 Length of session: 25 minutes Categorized as music therapy study | |
| Outcomes | Hear rate: change scores from pre‐test to post‐test Respiratory rate: change scores from pre‐test to post‐test Oxygen saturation level: change scores from pre‐test to post‐test Rapid shallow breathing: change scores from pre‐test to post‐test | |
| Notes | Only the data of the medical, non‐cardiac patients are included in this review. The cardiac patients were treated immediately following cardiac artery bypass grafting surgery and their physiological responses were still suppressed by the anaesthesia. The SDs reported in this study are large. Large SDs were present at baseline, meaning that there was a large variety in physiological responses even before the start of the intervention. The author did not report standard deviations (SDs) for the reported change score so we computed these. Since we did not have information about the correlation coefficient, we used a conservative estimate of 0.5. This made the SD of the change score large (i.e., similar to SDs of pre‐ and post‐test scores). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate group assignment |
| Allocation concealment (selection bias) | High risk | Allocation concealment was not possible because of use of alternate group assignment |
| Blinding (performance bias and detection bias) | High risk | Participants could not be blinded. Personnel were blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Low risk | This study does not include subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate: 0% |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Free from financial conflict of interest | Low risk | Unfunded study (Master's thesis) |
| Methods | Cross‐over trial | |
| Participants | Adults receiving mechanical ventilation in critical care unit. Most frequent primary diagnosis: pulmonary disease (no further details reported) Average length of mechanical ventilation before onset of study: 6.05 (3.65) days Ventilator mode: PS (80%), SIMV + PS (20%) Type of airway: tracheostomy (60%), oral endotracheal tube (40%) Diagnosis: pulmonary diseases N randomized to music group: unclear N randomized to control group: unclear N analysed in music condition: 20 N analysed in control condition: 20 Age: 58.25 y Sex: 5 F, 15 M Ethnicity: Chinese Setting: inpatient critical care unit Country: China | |
| Interventions | Two study groups:
Music selection used: Chinese music (Chinese folk song, music played by Chinese instruments, Chinese music played by Western instruments, Buddhist music) and various Western music (classical, soundtrack, piano) Number of sessions: each subject participated in one music condition and one rest condition Length of condition: 30 minutes Categorized as music medicine study | |
| Outcomes | State anxiety (short form; data was converted to full score): post‐test score on the Spielberger State Anxiety Inventory (6‐item version) Respiratory rate: post‐test score Mean blood pressure: post‐test score | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization to different orderings of the interventions was done by drawing lots [...]" (p. 379) |
| Allocation concealment (selection bias) | Low risk | Achieved through use of draw of lots for each patient after consent was obtained |
| Blinding (performance bias and detection bias) | High risk | Participants could not be blinded. Personnel were blinded |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessor was not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether number of participants analysed equals the number of participants recruited |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting |
| Free from financial conflict of interest | Unclear risk | Funding information is not provided. Conflict of interest statement is lacking |
| Methods | Two‐arm parallel group design | |
| Participants | Adults necessitating mechanical ventilation Participants were suffering from lung‐related diseases (n = 39) and non‐lung related diseases (n = 21) Average length of mechanical ventilation before onset of study: 3.47 (1 to 161) days Ventilator mode: not reported Type of airway: oral endotracheal tube and tracheotomy tube N randomized to music group: 30 N randomized to control group: 30 N analysed in music group: 30 N analysed in control group: 30 Sex: 23 F, 37 M Age: mean age not reported Ethnicity: 100% Chinese Setting: critical care unit Country: Taiwan | |
| Interventions | Two study groups:
Music selections provided: participants were asked to select from Chinese, religious, New Age, hymn, classical or orchestral music with slow tempo. Most participants selected old Taiwanese popular songs without lyrics (n = 17) and religious music (n = 7, 24) Number of sessions: 1 Length of session: 30 minutes Categorized as music medicine study | |
| Outcomes | Anxiety (VAAS): change scores HR, RR, SBP, DBP, MAP, O2sa: change scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of coin flip |
| Allocation concealment (selection bias) | Low risk | Use of coin flip |
| Blinding (performance bias and detection bias) | High risk | Blinding of the participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Self‐report measures were used for subjective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No participant loss |
| Selective reporting (reporting bias) | Low risk | No indication of selective reporting |
| Free from financial conflict of interest | Low risk | Unfunded research study |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Insufficient data reporting | |
| Review article | |
| Commentary on Wong 2001 | |
| Not randomized controlled trial (RCT) or controlled clinical trial (CCT) | |
| Not RCT or CCT | |
| Not population of interest | |
| Programme description | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Not RCT or CCT. Report on analysis of anxiety patterns of subsample of the 2013 RCT included in this review | |
| Not RCT or CCT | |
| review article | |
| Programme description | |
| Not RCT or CCT | |
| Review article | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Not population of interest | |
| Commentary on Bradt 2010 | |
| Not population of interest | |
| Not population of interest | |
| Not randomized controlled trial. In the thesis author explicitly states that only 4 CD players were available. If all CD players were in use, the next group of patients were placed in the control group | |
| Not population of interest |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
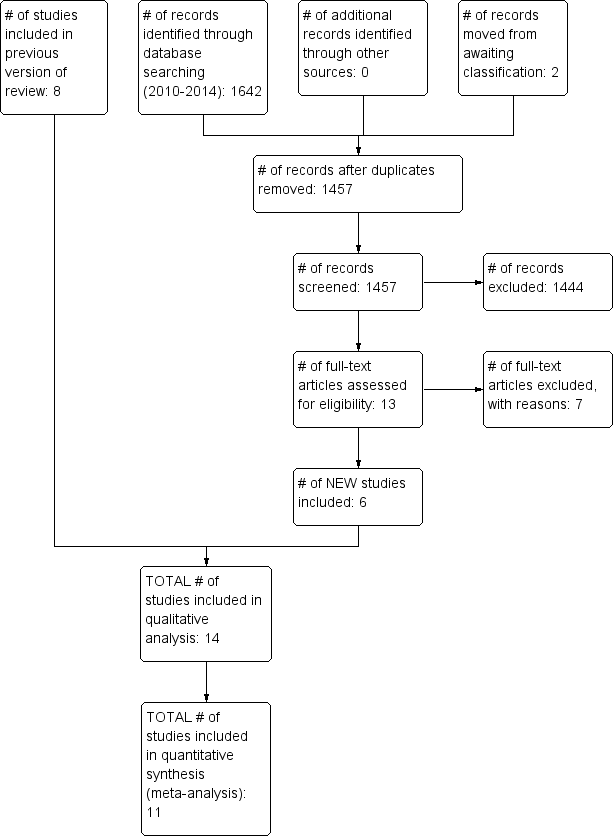
| 1 State Anxiety (change scores) Show forest plot | 5 | 288 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.11 [‐1.75, ‐0.47] |
| Analysis 1.1 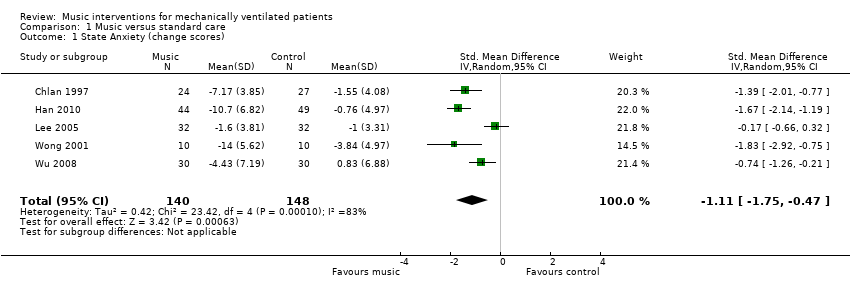 Comparison 1 Music versus standard care, Outcome 1 State Anxiety (change scores). | ||||
| 2 Heart Rate Show forest plot | 8 | 338 | Mean Difference (IV, Random, 95% CI) | ‐3.95 [‐6.62, ‐1.27] |
| Analysis 1.2 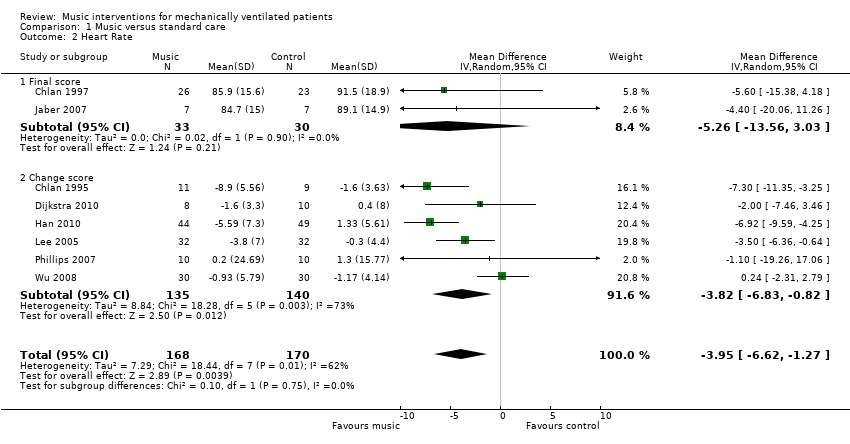 Comparison 1 Music versus standard care, Outcome 2 Heart Rate. | ||||
| 2.1 Final score | 2 | 63 | Mean Difference (IV, Random, 95% CI) | ‐5.26 [‐13.56, 3.03] |
| 2.2 Change score | 6 | 275 | Mean Difference (IV, Random, 95% CI) | ‐3.82 [‐6.83, ‐0.82] |
| 3 Heart Rate (adequate randomization) Show forest plot | 7 | 318 | Mean Difference (IV, Random, 95% CI) | ‐4.01 [‐6.80, ‐1.22] |
| Analysis 1.3 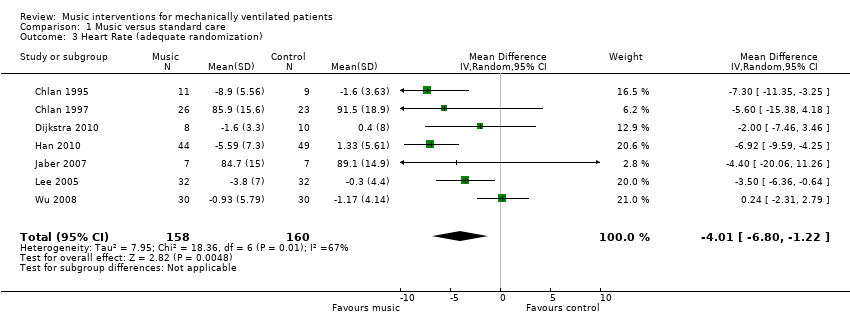 Comparison 1 Music versus standard care, Outcome 3 Heart Rate (adequate randomization). | ||||
| 4 Respiratory Rate Show forest plot | 9 | 357 | Mean Difference (IV, Random, 95% CI) | ‐2.87 [‐3.64, ‐2.10] |
| Analysis 1.4  Comparison 1 Music versus standard care, Outcome 4 Respiratory Rate. | ||||
| 4.1 Final score | 3 | 83 | Mean Difference (IV, Random, 95% CI) | ‐2.14 [‐4.06, ‐0.22] |
| 4.2 Change score | 6 | 274 | Mean Difference (IV, Random, 95% CI) | ‐3.01 [‐3.85, ‐2.17] |
| 5 Respiratory Rate (adequate randomization) Show forest plot | 8 | 337 | Mean Difference (IV, Random, 95% CI) | ‐2.87 [‐3.64, ‐2.09] |
| Analysis 1.5  Comparison 1 Music versus standard care, Outcome 5 Respiratory Rate (adequate randomization). | ||||
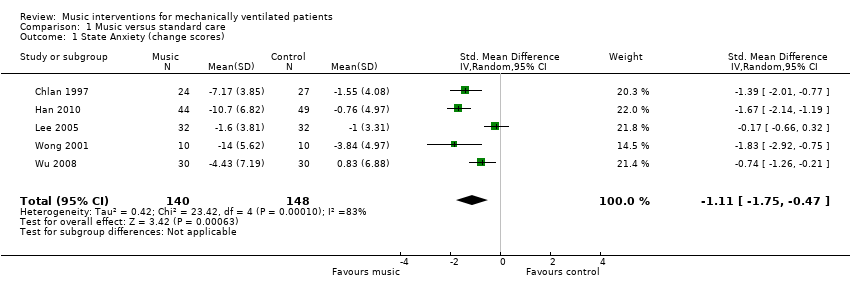
| 6 Systolic Blood Pressure Show forest plot | 6 | 269 | Mean Difference (IV, Random, 95% CI) | ‐4.22 [‐6.38, ‐2.06] |
| Analysis 1.6  Comparison 1 Music versus standard care, Outcome 6 Systolic Blood Pressure. | ||||
| 6.1 Final score | 1 | 14 | Mean Difference (IV, Random, 95% CI) | ‐9.0 [‐22.40, 4.40] |
| 6.2 Change score | 5 | 255 | Mean Difference (IV, Random, 95% CI) | ‐4.09 [‐6.28, ‐1.90] |
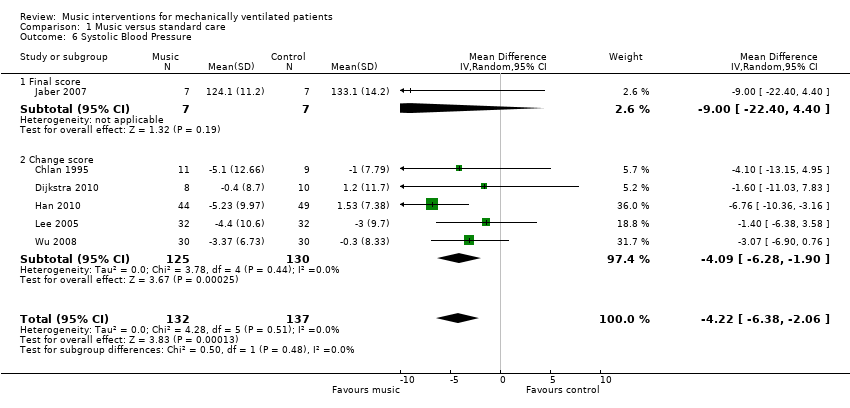
| 7 Diastolic Blood Pressure Show forest plot | 6 | 269 | Mean Difference (IV, Random, 95% CI) | ‐2.16 [‐4.40, 0.07] |
| Analysis 1.7 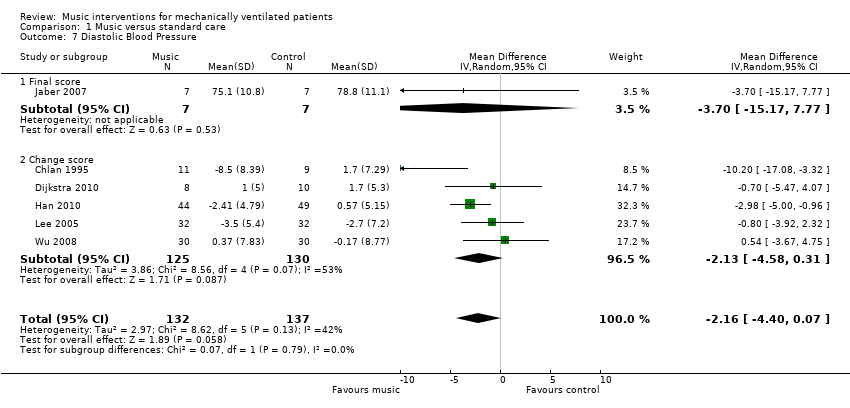 Comparison 1 Music versus standard care, Outcome 7 Diastolic Blood Pressure. | ||||
| 7.1 Final score | 1 | 14 | Mean Difference (IV, Random, 95% CI) | ‐3.70 [‐15.17, 7.77] |
| 7.2 Change score | 5 | 255 | Mean Difference (IV, Random, 95% CI) | ‐2.13 [‐4.58, 0.31] |
| 8 Mean Arterial Pressure Show forest plot | 3 | 98 | Mean Difference (IV, Random, 95% CI) | ‐1.79 [‐4.56, 0.99] |
| Analysis 1.8 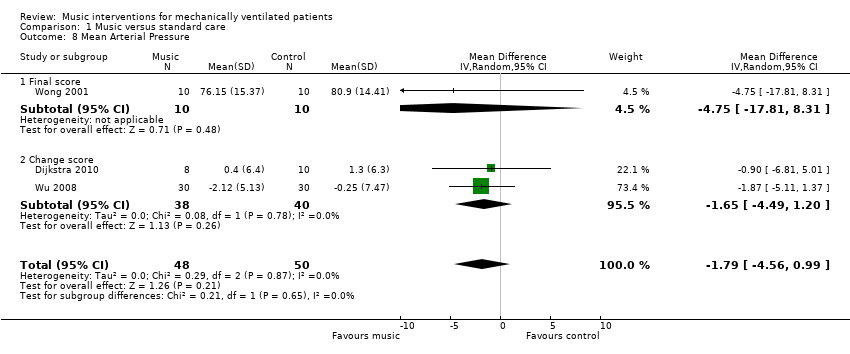 Comparison 1 Music versus standard care, Outcome 8 Mean Arterial Pressure. | ||||
| 8.1 Final score | 1 | 20 | Mean Difference (IV, Random, 95% CI) | ‐4.75 [‐17.81, 8.31] |
| 8.2 Change score | 2 | 78 | Mean Difference (IV, Random, 95% CI) | ‐1.65 [‐4.49, 1.20] |
| 9 Oxygen Saturation Level (change scores) Show forest plot | 4 | 193 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.67, 0.57] |
| Analysis 1.9 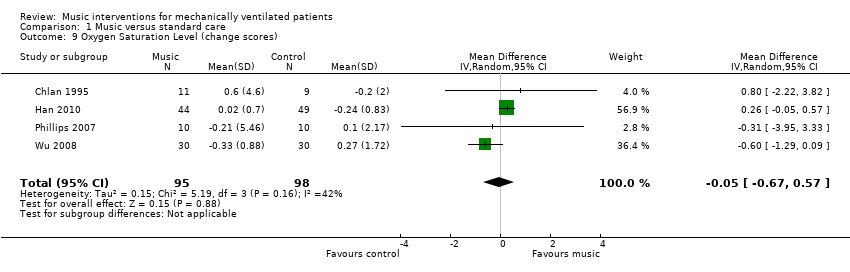 Comparison 1 Music versus standard care, Outcome 9 Oxygen Saturation Level (change scores). | ||||
| 10 Mortality Show forest plot | 2 | 271 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.38, 1.51] |
| Analysis 1.10 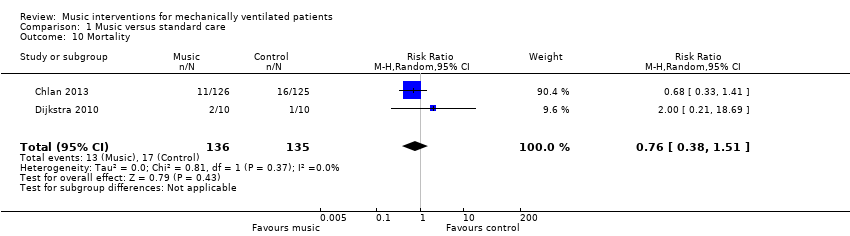 Comparison 1 Music versus standard care, Outcome 10 Mortality. | ||||
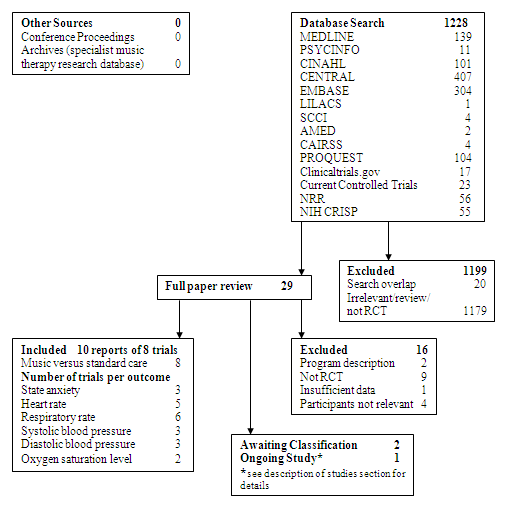
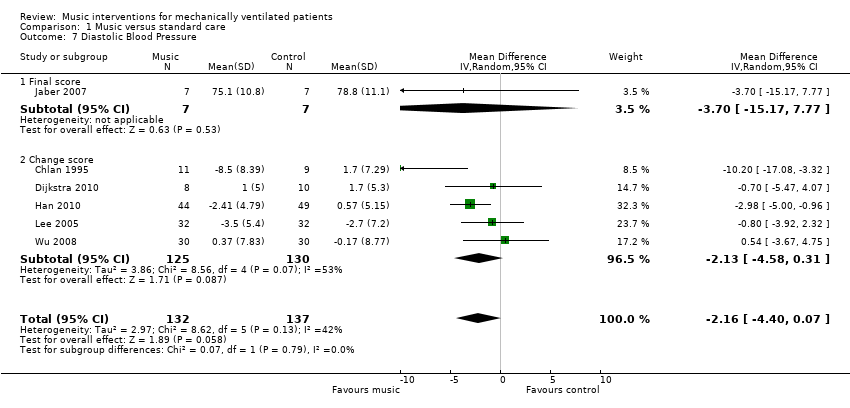
Study Flow Diagram ‐ Original Review.
Study flow diagram ‐ updated review.

Funnel plot of comparison: 1 Music versus standard care, outcome: 1.4 Respiratory rate.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Comparison 1 Music versus standard care, Outcome 1 State Anxiety (change scores).

Comparison 1 Music versus standard care, Outcome 2 Heart Rate.

Comparison 1 Music versus standard care, Outcome 3 Heart Rate (adequate randomization).

Comparison 1 Music versus standard care, Outcome 4 Respiratory Rate.

Comparison 1 Music versus standard care, Outcome 5 Respiratory Rate (adequate randomization).
Comparison 1 Music versus standard care, Outcome 6 Systolic Blood Pressure.
Comparison 1 Music versus standard care, Outcome 7 Diastolic Blood Pressure.

Comparison 1 Music versus standard care, Outcome 8 Mean Arterial Pressure.
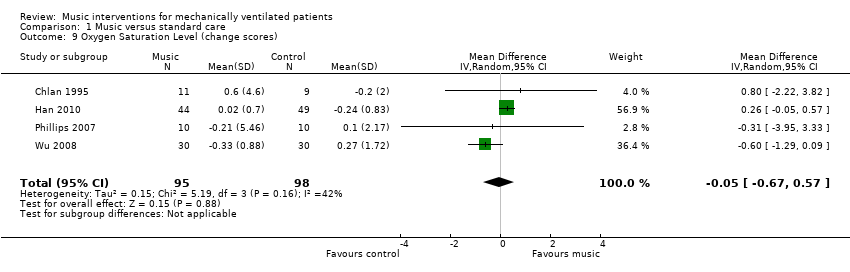
Comparison 1 Music versus standard care, Outcome 9 Oxygen Saturation Level (change scores).
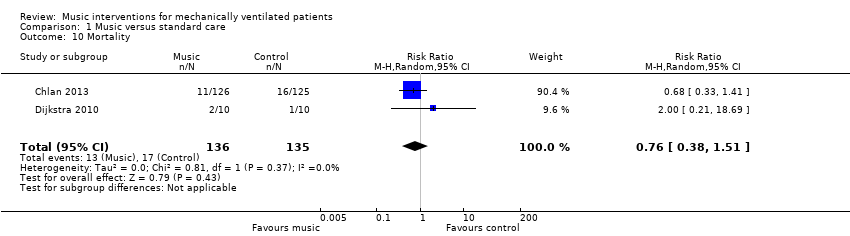
Comparison 1 Music versus standard care, Outcome 10 Mortality.
| Music compared to standard care for mechanically ventilated patients | |||
| Patient or population: mechanically ventilated patients | |||
| Outcomes | Relative effect | No of participants | Quality of the evidence |
| State anxiety | The mean state anxiety in the intervention groups was | 288 | ⊕⊕⊝⊝ |
| Heart rate | The mean heart rate in the intervention groups was | 338 | ⊕⊝⊝⊝ |
| Respiratory rate | The mean respiratory rate in the intervention groups was | 357 | ⊕⊝⊝⊝ |
| Systolic blood pressure mmHg | The mean systolic blood pressure in the intervention groups was | 269 | ⊕⊝⊝⊝ |
| Diastolic blood pressure mmHg | The mean diastolic blood pressure in the intervention groups was | 269 | ⊕⊝⊝⊝ |
| Mean arterial pressure mmHg | The mean arterial pressure in the intervention groups was | 98 | ⊕⊝⊝⊝ |
| Oxygen saturation level | The mean oxygen saturation level in the intervention groups was | 193 | ⊕⊕⊝⊝ |
| CI: Confidence interval | |||
| GRADE Working Group grades of evidence | |||
| 1 The majority of the trials were assessed as high risk of bias studies | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 State Anxiety (change scores) Show forest plot | 5 | 288 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.11 [‐1.75, ‐0.47] |
| 2 Heart Rate Show forest plot | 8 | 338 | Mean Difference (IV, Random, 95% CI) | ‐3.95 [‐6.62, ‐1.27] |
| 2.1 Final score | 2 | 63 | Mean Difference (IV, Random, 95% CI) | ‐5.26 [‐13.56, 3.03] |
| 2.2 Change score | 6 | 275 | Mean Difference (IV, Random, 95% CI) | ‐3.82 [‐6.83, ‐0.82] |
| 3 Heart Rate (adequate randomization) Show forest plot | 7 | 318 | Mean Difference (IV, Random, 95% CI) | ‐4.01 [‐6.80, ‐1.22] |
| 4 Respiratory Rate Show forest plot | 9 | 357 | Mean Difference (IV, Random, 95% CI) | ‐2.87 [‐3.64, ‐2.10] |
| 4.1 Final score | 3 | 83 | Mean Difference (IV, Random, 95% CI) | ‐2.14 [‐4.06, ‐0.22] |
| 4.2 Change score | 6 | 274 | Mean Difference (IV, Random, 95% CI) | ‐3.01 [‐3.85, ‐2.17] |
| 5 Respiratory Rate (adequate randomization) Show forest plot | 8 | 337 | Mean Difference (IV, Random, 95% CI) | ‐2.87 [‐3.64, ‐2.09] |
| 6 Systolic Blood Pressure Show forest plot | 6 | 269 | Mean Difference (IV, Random, 95% CI) | ‐4.22 [‐6.38, ‐2.06] |
| 6.1 Final score | 1 | 14 | Mean Difference (IV, Random, 95% CI) | ‐9.0 [‐22.40, 4.40] |
| 6.2 Change score | 5 | 255 | Mean Difference (IV, Random, 95% CI) | ‐4.09 [‐6.28, ‐1.90] |
| 7 Diastolic Blood Pressure Show forest plot | 6 | 269 | Mean Difference (IV, Random, 95% CI) | ‐2.16 [‐4.40, 0.07] |
| 7.1 Final score | 1 | 14 | Mean Difference (IV, Random, 95% CI) | ‐3.70 [‐15.17, 7.77] |
| 7.2 Change score | 5 | 255 | Mean Difference (IV, Random, 95% CI) | ‐2.13 [‐4.58, 0.31] |
| 8 Mean Arterial Pressure Show forest plot | 3 | 98 | Mean Difference (IV, Random, 95% CI) | ‐1.79 [‐4.56, 0.99] |
| 8.1 Final score | 1 | 20 | Mean Difference (IV, Random, 95% CI) | ‐4.75 [‐17.81, 8.31] |
| 8.2 Change score | 2 | 78 | Mean Difference (IV, Random, 95% CI) | ‐1.65 [‐4.49, 1.20] |
| 9 Oxygen Saturation Level (change scores) Show forest plot | 4 | 193 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.67, 0.57] |
| 10 Mortality Show forest plot | 2 | 271 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.38, 1.51] |

