音樂的介入用於後天性腦損傷
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT | |
| Participants | Participants with a severe head injury Diagnosis: post‐traumatic amnesia scoring less than or equal to 8 on the Westmead Post‐traumatic Amnesia Scale on the day prior to commencement of the experiment Time since onset: not stated N randomised: 22 N analysed in treatment group (live music): 22 | |
| Interventions | 3 study groups: 1: Music intervention (live): Participants listened to live music. The music selection was individualised for each participant and comprised 3 music pieces that were chosen from selections suggested by family members. All styles of music were permitted. The researcher was present in the room sitting opposite and facing the participant 2. Music intervention (recorded): Participants listened to recorded music. The same 3 pieces were played during the recorded music condition as were used in the live music condition, and played in the same order. The music was played free‐field on an audio cassette player. To avoid agitating the participant no headphones were used. The researcher was present in the room sitting opposite and facing the participant | |
| Outcomes | Agitation (Agitated Behavior Scale): effect size reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers |
| Allocation concealment (selection bias) | High risk | No allocation concealment used |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants was not possible. It was not possible to blind the personnel delivering the interventions. |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) | Low risk | 1 dropout because of early resolution of PTA |
| Selective reporting (reporting bias) | Low risk | There were no indications of selective reporting in this study |
| Free from financial conflict of interest | Low risk | No funding support reported |
| Methods | RCT Cross‐over trial | |
| Participants | Participants with first ischaemic CVA Time since onset: at least 6 months post‐CVA N randomised: 41 N analysed at baseline condition: 20 N analysed in RAS condition: 21 Mean age: 60.8 years (SD 19.8) Sex: 17 females (41.5%), 24 males (58.5%) Ethnicity: not reported Setting: rehabilitation centres Country: South Korea | |
| Interventions | All participants were studied under 5 conditions. Study compared walking with no intervention (baseline) with RAS at 4 different speeds (baseline‐matched RAS, ‐10%, +10%, and +20%). In this review we used baseline‐matched RAS and +20% Number of sessions: not clear Length of sessions: not stated | |
| Outcomes | Gait parameters: gait velocity (cm/second), gait cadence (steps per minute), stride length‐affected (cm), stride length‐unaffected (cm), stride symmetry. Post‐test scores used | |
| Notes | This study used rhythm delivered by a metronome without music | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Conditions were applied in random order" (p480) All participants received all conditions. We assessed randomisation bias to be low for this reason |
| Allocation concealment (selection bias) | Low risk | Allocation of treatment order not reported. However, all participants received all treatments |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or to blind the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The GAITRite system recorded the gait velocity, cadence, stride length, double limb support (% of cycle), and double single limb support (% of cycle)” (p480). As personnel were not involved in entering the data, we rated detection bias as low risk |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition was not reported. However, 41 participants were recruited, and the authors report 41 data sets included in the analysis |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support reported |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants with chronic hemiparetic stroke Diagnosis: ischaemic or haemorrhagic stroke Time since onset: at least 6 months N randomised to RAS and intense gait‐training treatment: 10 N randomised to intensive gait training alone (control): 10 N analysed in treatment group: 10 N analysed in control group: 10 Mean age: 61.4 years Sex: 8 females (40%), 12 males (60%) Ethnicity: not reported Setting: inpatient hospital Country: South Korea | |
| Interventions | 2 study groups: 1. Music intervention group: RAS with intensive gait training 2. Control group: intensive gait training alone Number of sessions: 30 sessions in total over 6 weeks Length of sessions: 30 minutes | |
| Outcomes | Gait velocity (cm/second), gait cadence (steps/minute), stride length‐affected side (cm), stride length‐unaffected side (cm), balance (Berg Balance Scale), quality of life (Stroke Specific Quality of Life Scale). Pre‐ and post‐test scores | |
| Notes | This study used rhythm delivered by a metronome in combination with recorded music | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned to either and [sic] RAS training or control group using sealed envelopes”. Method of randomisation was not reported (p682) |
| Allocation concealment (selection bias) | Low risk | Allocation using sealed envelopes. Quote: "randomly assigned to either and [sic] RAS training or control group using sealed envelopes" (p682) |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or to blind the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of the personnel involved in assessing outcomes was not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition was not reported, although 20 were randomised and 20 completed |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support reported. Quote: "The authors declared no potential conflicts of interest with respect to the authorship and/or publication of this article" (p687) |
| Methods | RCT 3‐arm parallel‐group design | |
| Participants | Participants with middle cerebral artery hemiparetic stroke Time since onset: discharged from hospital at least 3 months earlier N randomised to RAS and standard care: 15 N randomised to standard care: 15 N randomised to visual cueing and standard care: 15 (not included in this review) N analysed in RAS and standard care group: 15 N analysed in standard care (control) group: 15 N analysed in visual cueing and standard care group: 15 (not included in this review) Mean age: 57.40 years (SD 5.18) Sex: 9 females (20%), 36 males (80%) Ethnicity: not reported Setting: multispecialty hospital and research centre Country: India | |
| Interventions | 3 study groups: 1. Music intervention group: RAS plus conventional treatment 2. Other therapy intervention (not used in this review): visual cueing plus conventional treatment 3. Control group: conventional treatment Number of sessions: RAS given for 9 sessions in total over 3 weeks Length of sessions: 2 hours | |
| Outcomes | Upper extremity function (Fugl‐Meyer Assessment), general gait (Dynamic Gait Index). Post‐test scores used | |
| Notes | This study used rhythm delivered by a metronome without music | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The subjects selected for the study were randomly allocated using sealed envelopes into 3 groups." (p344). Method of randomisation was not stated |
| Allocation concealment (selection bias) | Low risk | Quote: "The subjects selected for the study were randomly allocated using sealed envelopes into 3 groups." (p396) |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or to blind the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of the personnel involved in assessing outcomes was not reported |
| Incomplete outcome data (attrition bias) | Low risk | Reported 0 withdrawals |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support reported |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants with acute stroke with mild to severe nonfluent aphasia Time since onset: most within 13 days, 2 control and 1 treatment participant were > 60 days N randomised to treatment group at baseline: 16 N randomised to control group at baseline: 14 N analysed in treatment group at visit 1: 14 N analysed in control group at visit 1: 10 N analysed in treatment group at visit 2: 9 N analysed in control group at visit 2: 8 Mean age: 61.51 years (SD 15.49) Sex: 14 females (47%), 16 males (53%) Ethnicity: not reported Setting: inpatient Country: USA | |
| Interventions | 2 study groups: 1. Music intervention group: received modified melodic intonation therapy (MMIT). This involved a 10‐ to 15‐minute session with the music therapist "consisting of the music therapist teaching the participant a melodic phrase." (p1466) 2. Control group: received a 10‐ to 15‐minute session with the music therapist "who discussed the participant’s impairment, different forms of treatment, different outcomes, and various issues that can result from aphasia, such as depression and withdrawal." (p1466) Number of sessions: 2 in total Length of sessions: 10 to 15 minutes | |
| Outcomes | 2 tasks similar to Western Aphasia Battery: adjusted total score. Change scores used | |
| Notes | Quote: "The Western Aphasia Battery has two subtests that were deemed appropriate, one for repetition and one for responsiveness; however, both sections are designed to elicit short answers. Because of the length of the phrases utilized in MMIT it was decided not to use the exact subtests from the Western Aphasia Battery, but instead to design two similar tasks that would elicit longer responses." (p465) Outcomes were measured for all 3 visits. However, due to high attrition for visit 3, we only reported change scores between visit 1 and visit 2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization table was generated by a biostatistician prior to the start of the study. Random assignment was performed by the music therapist after enrolment by the nursing manager, who had no prior knowledge of the ordering of participants." (p1466) |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants was not possible. It was not possible to blind the personnel delivering the interventions |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The evaluators were not present in the room when the treatment or control session was given, and the music therapist, being blinded to the test scores until after the post‐test was completed for each session, was not in the room when the test was administered." (pp1465‐6) |
| Incomplete outcome data (attrition bias) | High risk | Attrition from baseline to visits 1 and 2 higher than 20% for control group. Attrition from baseline to visit 2 higher than 20% for treatment group. Quote: "Out of the 14 controls, 10 had both pre and post scores at Visit 1, and eight had pre and post scores at Visit 2. For the treatment group, 14 out of the 16 had both pre and post scores at Visit 1, and nine had pre and post scores at Visit 2. Only patients who completed both components (responsive and repetitive) in both pre and post assessments were considered in the following analysis. Data are not given for Visit 3 due to the small number of participants (one control, three treatments)." (pp1466‐7) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support reported |
| Methods | Quasi‐RCT 2‐arm parallel‐group design | |
| Participants | Participants with severe cerebral damage in vegetative state Diagnosis: traumatic brain injury (38%), non‐traumatic origin hypoxic‐ischaemic encephalopathy (35%), acute cerebrovascular accident (20%), central nervous system infections (4%), and central nervous system tumours (4%). Time since onset: > 3 years, (mean 45.9 months; SD 20.5 months) N randomised to treatment group: 13 N randomised to control group: 13 N analysed in treatment group: 13 N analysed in control group: 13 Mean age: 54.05 years (SD 14.37) Sex: 13 females (50%), 13 males (50%) Ethnicity: not reported Setting: inpatient, "Irreversible cerebral damage unit" (p120) Country: Spain | |
| Interventions | 2 study groups: 1. Music intervention group: Participants were exposed to 3 types of musical/auditory stimuli: classical relaxing music (CRM), relaxing music with nature sounds (RMNS), and radio (various musical genres and commercial messages). CRM and RMNS were played individually using an MP3 player via headphones for a period of 20 minutes. The radio was played as environmental music via a stereo system for 1 hour Number of sessions: 18 sessions in total. The frequency of sessions is unclear: "18 sessions (six sessions for each musical stimulus), being performed once a day, twice weekly at the same hour" (p119) Length of sessions: CRM and RMNS were played for 20 minutes. "Radio ... was played as environmental music ... for one hour via a stereo system" (p119) | |
| Outcomes | Vital signs: systolic BP, diastolic BP, heart rate, respiratory rate, oxygen saturation (not included in this review). Facial expressions: muscular facial relaxation, eye opening, mouth movements, head movements, yawning, smiling, eyebrow movements, and sound emission (results not provided for control group) | |
| Notes | The outcomes of this study were not included in a meta‐analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was achieved using a computer‐generated list of random numbers (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Unclear risk | Allocation was not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding is not reported, however it may be assumed that personnel delivering the interventions were not blinded, as the part of the experimental intervention involved radio played as "environmental music ... via a stereo system" (p119) |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding is not reported, however it may be assumed that raters were not blind, as behavioural ratings were taken immediately after live music was played on headphones to heavily dependent participants |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition was not reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient data were reported to assess the effects of music listening on facial expressions. Objectives at the outset of the research were (quote): "to verify the influence of music listening on patients’ facial expressions" (p117). Although the authors state (quote): "Alterations in facial expression were displayed in each patient" (p117), inadequate information is presented to evaluate whether this outcome has been reported selectively |
| Free from financial conflict of interest | Low risk | Quote: "The authors declare no conflicts of interest." (p117) |
| Methods | Quasi‐RCT with alternate group allocation 2‐arm parallel‐group design | |
| Participants | Participants with chronic stroke and right hemiparesis Time since onset: mean 3.3 years (SD 2.1) N assigned to treatment group: 6 N assigned to control group: 4 N analysed in treatment group: 5 N analysed in control group: 3 Mean age: 60 years (8.74) Sex: 6 females (60%), 4 males (40%) Ethnicity: 70% Caucasian (understood to be white). Otherwise not reported Setting: Not reported. However, the setting seems to be a community outpatient setting. Quote: "Subjects were recruited by local rehabilitation therapists and by subject inquiry regarding current studies" (p729) Country: USA | |
| Interventions | 2 study groups: 1. Music intervention group: interactive metronome (IM) intervention. Consisted of occupational therapy treatment with 30 minutes of IM session embedded. Interactive metronome consisted of a computer‐based rhythmic and auditory training program. As the computer‐generated reference was heard through headphones, the participants attempted to match the rhythmic auditory beat with repeated limb movements, such as clapping their hands together with a switch in their hand. One IM session consisted of repetitive limb movement lasting 1 to 3 minutes. Sessions took place 3 times per week for 10 weeks. | |
| Outcomes | Upper extremity function (FMA, Arm Motor Ability Test, Box and Block Test, Canadian Occupational Performance Measure). Quality of life (Stroke Impact Scale 2.0) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Subjects were enrolled in the study groups by alternating group assignment (i.e. Subject 1 was in the OT group, Subject 2 was in the IM+OT group)" (p729) |
| Allocation concealment (selection bias) | Unclear risk | Allocation is not reported |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants was not possible. It was not possible to blind the personnel delivering the interventions. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It is unclear whether the SIS for quality of life involved self reports |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "All outcomes except the COPM were measured by the same blinded rater 1 week before intervention and within 1 week after intervention" (p729) |
| Incomplete outcome data (attrition bias) | High risk | Attrition reported at 20%. 1 participant was lost to follow‐up, and 1 withdrew from the study |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Equipment support reported. Quote: "We thank Interactive Metronome for providing the equipment and software for the study" (p737) |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants following infarct (60.6%) and haemorrhagic stroke (39.4%) Diagnosis: 17 with left stroke lesion (51.1%), 15 with right stroke lesion (45.5%), 1 with bilateral stroke lesion (3%) Time since onset: mean 6.39 years (SD 4.96) N randomised to treatment group: 18 N randomised to control group: 18 N received intended treatment in treatment group: 18 N received intended treatment in control group: 18 N analysed in treatment group: 16 N analysed in control group: 17 Mean age: 60.1 years (SD 7.88) Sex: 10 females (30.3%), 23 males (69.7%) Ethnicity: not reported Setting: outpatient. Follow‐up data collected at a "community setting" for experimental group and from individual households for the control group (p127) Country: South Korea | |
| Interventions | 2 study groups: 1. Music intervention group: RAS music‐movement exercise intervention, which consisted of 4 sections: (a) preparatory activities, (b) main activities, (c) wrap‐up activities, and (d) follow‐up. Quote: "The routines are composed of a series of dynamic rhythmic motions involving the whole body". Other types of dynamic rhythmic movements and rhythm tools that were used in the programme included shaking an egg shaker and playing percussion instruments, such as a small Korean drum or tambourine, to a rhythm after listening to it." (p127) 2. Control group: The intervention involved receiving referral information about available usual care services. Number of sessions: 8 weeks in total. Number of sessions per week unclear Length of sessions: 2 hours per week | |
| Outcomes | Physiological parameters: upper extremity function, shoulder flexion ROM (goniometer); lower extremity function, ankle flexion ROM (goniometer); lower extremity function, ankle extension ROM (goniometer); shoulder flexibility, upward in affected arm (back‐scratch test); shoulder flexibility, downward in affected arm (back‐scratch test): change scores Psychological outcomes: mood (POMS ‐ Korean version); interpersonal relationships (The Relationship Change Scale); Quality of life (Stroke Specific Quality of Life Scale): pre‐ and post‐scores | |
| Notes | Intervention described appears to be more similar to therapeutic instrumental performance or patterned sensory enhancement than RAS Total POMS scores reported only; subscale results not reported. Authors used the Korean version of the POMS. However, the total scores were very low (range 1.56 to 2.81 out of a possible 136). We repeatedly attempted to contact the authors to check the POMS data, but were unable to obtain more information. As these data seemed unreliable, we excluded them from the meta‐analysis Change scores were computed by 1 review author (JB) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list. Quote: "Using computer‐generated number cards, the participants were then randomly assigned to one of two groups" (p125) |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not reported |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of the outcome assessors for the objective outcomes was not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Although the numbers of withdrawals are reported as less than 20%, the reasons for withdrawal are not given. Quote: "Of the total 36 who were originally recruited, 33 completed the follow‐up data collection. Attrition is less than 20%" (p129) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "This study was supported by the BK21 project (Grant No. 0522‐20010002), the Korea Science and Engineering Foundation (Grant No. R04‐2001‐000‐00197‐0), and the Research Institute of Nursing Science at Seoul National University." (p131) |
| Methods | Quasi‐RCT with alternate group allocation | |
| Participants | People with stroke with chronic aphasia (Broca's aphasia and global aphasia) who were no longer receiving speech therapy N allocated to treatment group: 9 N analysed in treatment group: 8 N analysed in control group: 5 | |
| Interventions | 2 study groups: 1. Music intervention group: rhythmic‐melodic voice training (SIPARI) sessions. SIPARI is a music therapy technique based on specific use of the voice. It actively works with the remaining speech capabilities in the right hemisphere of people with aphasia, namely singing, intonation, prosody embedded in physiologically appropriate breathing. The SIPARI method also employs instrumental and vocal rhythmic exercises and music improvisations to practice communication scenarios. Length of sessions: group sessions 60 minutes, individual sessions 45 minutes | |
| Outcomes | Articulation and prosody, repetition, labelling, speech comprehension, total speech profile (Aachener Aphasie Test/Aachen Aphasia Test): effect size reported | |
| Notes | 1 review author (JB) computed change scores and SD from raw scores received from the principal investigator. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate group allocation |
| Allocation concealment (selection bias) | High risk | No allocation concealment was reported |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Low risk | Independent outcome assessors were used |
| Incomplete outcome data (attrition bias) | High risk | 23% attrition reported: 1 control and 1 experimental excluded as diagnosis of global or Broca's aphasia was unclear. 2 further participants excluded due to serious illness |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support reported |
| Methods | RCT | |
| Participants | Participants with stroke: 8 with severe hemiplegia, 2 with mild hemiplegia Mean age: not reported, age range: 61 to 73 years | |
| Interventions | 3 study groups: 1. Music intervention group: listening to recorded songs with lyrics 2. Music intervention group: listening to karaoke accompaniment without lyrics during upper extremities exercises Number of sessions: 8 sessions in total on a weekly basis Length of sessions: not reported | |
| Outcomes | Pain (Likert scale). No post‐test means or change scores were reported; only F statistic and significance level. | |
| Notes | The author informed us that she no longer had access to the raw data, therefore we could obtain no means or SD. We did not include extracted data from this study in our review as no other included studies examined pain as an outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers |
| Allocation concealment (selection bias) | Low risk | All participants underwent the 3 conditions in random order |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) | Low risk | No objective outcomes were used in this study |
| Incomplete outcome data (attrition bias) | High risk | 4 participants (28.5%) withdrew due to health condition or frequent absences (personal communication with author) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "The authors wish to thank the Kwanak Senior Center in Seoul, Korea for its generous support of this research." (p81) |
| Methods | RCT Cross‐over trial with 4 groups | |
| Participants | Participants with poststroke hemiparesis. No other diagnostic information provided Time since onset: mean 19.40 months (SD 19.49) N recruited: 18 N analysed: 15 Mean age: 60.07 years (SD 11.93) Sex: 7 females (47%), 8 males (53%) Ethnicity: not reported Setting: rehabilitation unit Country: Korea | |
| Interventions | 4 study groups: 1. Control group: visual locomotor imagery training (used as the control in this review) 2. Music intervention group: visual locomotor imagery training with auditory step rhythm (used as the experimental condition in this review) 3. Other therapy intervention (not used in this review): kinesthetic locomotor imagery training 4. Other therapy intervention (not used in this review): kinesthetic locomotor imagery training with auditory step rhythm Number of sessions: 4 sessions in total over 4 days, with 1 intervention presented in each session Length of sessions: 10 to 12 minutes | |
| Outcomes | Walking performance (Timed Up‐and‐Go Test, EMG data recorded from the quadriceps, hamstring, tibialis anterior, and gastrocnemius of the affected leg). Change scores were used | |
| Notes | We did not include EMG recording outcomes in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing of lots. Quote: "For randomization, we drew lots with four cards marked with 1, 2, 3 or 4 to determine the order of treatments" (p137) |
| Allocation concealment (selection bias) | Low risk | Drawing of lots. Quote: "Each subject had an envelope containing the four cards; without looking, each drew one card on each occasion" (p137) |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or to blind the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of the outcome assessors for the objective outcomes was not reported |
| Incomplete outcome data (attrition bias) | Low risk | Attrition reported at 16.6%. Quote: "Although initially 18 subjects were recruited, 3 subjects were excluded in data analysis owing to spontaneous refusal and irregular participation in intervention sessions" (p137) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support reported |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants with subacute stroke Diagnosis: 8 infarction (40%), 12 haemorrhage (60%) Time since onset: mean 5.22 months (SD 2.02) N randomised to treatment group: 10 N randomised to control group: 10 N analysed in treatment group: 9 N analysed in control group: 9 Mean age: 55.05 years (SD 12.88) Sex: 7 females (35%), 13 males (65%) Ethnicity: not reported Setting: inpatient rehabilitation Country: South Korea | |
| Interventions | 2 study groups: 1. Music intervention group: RAS 2. Control group: conventional therapy consisting of "one‐on‐one neurodevelopmental therapy between a patient and a therapist. Was composed of sitting up from lying down, sit to stand, and trunk and limb training aimed at learning normal gait patterns" (p1308) Number of sessions: 15 sessions in total with 3 sessions per week Length of sessions: 30 minutes | |
| Outcomes | Gait velocity (m/minute); gait cadence (steps/minute); stride length (affected side ‐ m); stride length (unaffected side ‐ m); functional gait ability (Dynamic Gait Index); dynamic balance (Four Square Step Test); gait ability (functional ambulation category), sit to stand, walking, stand to sit (Timed Up‐and‐Go Test); spatio‐temporal parameters of gait (up stair time ‐ step/second); spatio‐temporal parameters of gait (down stair time ‐ step/second). Change scores used for all of these outcomes Risk of falls (activities‐specific balance confidence scale). Change scores used Dynamic balance (Timed Up‐and‐Go Test). Post scores used | |
| Notes | This study used metronome pulse without music, delivered via a smart phone metronome application | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing of lots used (personal correspondence with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Participants drew lots (personal correspondence with principal investigator) |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or to blind the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of the outcome assessors for the objective outcomes was not reported |
| Incomplete outcome data (attrition bias) | Low risk | Attrition reported at 10% due to 1 participant from each group (N = 2) leaving the hospital halfway through the study |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support reported |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants with hemiplegic stroke Diagnosis: 14 infarction (70%), 6 haemorrhage (30%) Time since onset: mean 15.5 months N randomised to treatment group: 10 N randomised to control group: 10 N analysed in treatment group: 10 N analysed in control group: 10 Mean age: 64.85 years Sex: not reported Ethnicity: not reported Setting: outpatient Country: South Korea | |
| Interventions | 2 study groups: 1. Music intervention group: Auditory stimulation with metronome beat. Quote: "over the ground gait training with a metronome beat" (p775) 2. Control group: Quote: "over the ground gait training" (p775) Number of sessions: 18 in total, 3 sessions per week for 6 weeks Length of sessions: 10 minutes | |
| Outcomes | Gait velocity (km/h); stride length (affected side) (cm); stride length (unaffected side) (cm); stride length asymmetry ratio; single‐support‐time asymmetry; ratio; affected side single support time; non‐affected side single support time m/s. Pre‐ and post‐scores were used | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Contradictory reporting of randomisation procedures. Quote: "At the time of enrolment, the subjects were randomly assigned to the experimental or control groups by a computerized random‐number generator supervised by an independent researcher" (p776) Quote: "The limitations of this study were the lack of randomization" (p777) |
| Allocation concealment (selection bias) | Unclear risk | Quote: "the subjects were randomly assigned to the experimental or control groups by a computerized random‐number generator supervised by an independent researcher" (p776) |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or to blind the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of the outcome assessors for the objective outcomes was not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition not reported. Attempts to contact authors were unsuccessful |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support reported |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants with stroke Diagnosis: 15 thrombosis (50%), 15 haemorrhage (50%) Time since onset: mean 8.13 months (SD 2.16) N randomised to treatment group: 15 N randomised to control group: 15 N analysed in treatment group: 15 N analysed in control group: 15 Mean age: 67.4 years (range 40 to 80) Sex: 21 females (70%), 9 males (30%) Ethnicity: not reported Setting: nursing home Country: China | |
| Interventions | 2 study groups: 1. Music intervention group: RAS with conventional gait training 2. Control group: conventional gait training Number of sessions: 10 in total with 2 sessions per week over 5 weeks Length of sessions: 30 minutes | |
| Outcomes | Stride length (affected side ‐ cm), affected and unaffected stride difference (cm), stride frequency (steps per minute), max walking speed (m/min). Post scores used | |
| Notes | This study used rhythm delivered by a metronome in combination with live music | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing of lots (personal correspondence with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Drawing of lots (personal correspondence with principal investigator) |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or to blind the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | High risk | Blinding of the outcome assessors for the objective outcomes was not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition was not reported |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support reported |
| Methods | RCT 3‐arm parallel‐group design | |
| Participants | Participants with CVA (N = 1; 6.67%) and traumatic brain injury (N = 14; 93.33%) Time since onset: mean 21.56 years (SD 21.93) N randomised to experimental group: 5 N randomised to placebo singing group: 5 N randomised to control group: 4 N analysed in experimental group: 5 N analysed in placebo singing group: 5 N analysed in control group: 4 Mean age: 43.93 years (SD 10.41) Sex: 5 females (36%), 9 males (64%) Ethnicity: not reported Setting: rehabilitation Country: USA | |
| Interventions | 3 study groups: 1. Music intervention group (used in this review): endogenous shifting training within the context of neurologic music therapy tasks led by a board‐certified music therapist 2. Placebo singing group (not used in this review): group sing‐a‐long sessions, led by the same music therapist 3. Control group: standard care Number of sessions: 5 in total once per day over 5 days Length of sessions: 60 minutes | |
| Outcomes | Mental flexibility (Trail Making Test parts A and B); executive functioning (Dysexecutive Questionnaire (DEX) of the Behavioural Assessment of the Dysexecutive Syndrome and the Paced Auditory Serial Addition Test) Pre and post scores used | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used computer‐generated number list with stratified random sampling. Quote: "Random assignment was accomplished by assigning numbers to each participant using the online programme RANDOM.org. The numbers were then randomly sorted into three groups using the online randomisation programme, Research Randomizer" (p32) |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not reported |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Participants were provided with information in the consent form that could influence subjective outcomes. Quote: "We hope to show that music therapy makes a positive difference. We hope this research will help insurance companies decide to pay for future music therapy services" (p76) |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessment was adequate for the outcomes recommended for inclusion in this review (from the Trail Making Test Part B). Quote: "The psychometrist ... who remained blind to group membership, performed data collection on the Trail Making Test parts A & B scores (time and errors), and scores on the Paced Auditory Serial Addition Test (3 second and 2 second delivery rate). The researcher (neurologic music therapist) collected the data for the AMMA and also distributed and collected the DEX questionnaires" (pp39‐40). Outcomes from the Trail Making Test Part A, the Paced Auditory Serial Addition Test, and the Dysexecutive Questionnaire of the Behavioural Assessment of the Dysexecutive Syndrome were not used in this review |
| Incomplete outcome data (attrition bias) | Low risk | Attrition was 6.67%. Quote: "One participant dropped out due to scheduling conflicts" (p33 and p41) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support was reported |
| Methods | RCT Cross‐over trial Quote: "A multiple baseline within subjects protocol was chosen to provide data on a range of contrasting music therapy, and non‐music therapy auditory stimuli." (p38) | |
| Participants | Participants with disorders of consciousness, grouped into 2 cohorts: 1. Minimally consciousness state (N = 9; 43%) 2. Vegetative state (N = 12; 57%) Healthy normal participants were also included in another cohort not included in this review Cause of brain injury: hypoxic (N = 8; 38%); traumatic brain injury (N = 11; 52%); intracerebral haemorrhage (N = 2; 10%) Time since onset: mean 7.3 months (SD 2.8) N randomised: 21 N analysed: 21 Mean age: 45 years (SD 17.5) Sex: 10 females (48%), 11 males (52%) Ethnicity: not reported Setting: inpatient rehabilitation Country: UK | |
| Interventions | All participants were studied under 5 conditions on 1 occasion. Treatment order was randomised. 5 minutes of baseline silence was followed by the presentation of 4 contrasting conditions, each condition administered for 3 minutes with a 2‐minute period of silence between each. The 5 conditions were as follows. 1. Baseline (silence) 2. Liked music: live performance by a music therapist of a participant‐preferred song 3. Entrained improvisation: live performance of an improvised vocal melody singing "Hello" and the participant's name, entrained to the participant's respiration 4. Disliked music: recordings of music disliked by the participant 5. White noise Number of sessions: 1 Length of session: 22 minutes | |
| Outcomes | Behavioural outcomes were rated from video recordings in 10‐second segments: eye blinks per minute, eyes closed with body movements present, eyes closed with no body movements, eyes open with body movements present (not used in this review) Physiological outcomes: respiration rate per minute, respiration amplitude variance, respiration variance, heart rate, heart rate variability (not used in this review) Neurophysiological outcomes: electroencephalogram data across delta, theta, alpha, and beta bandwidths (not used in this review) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation through drawing of lots |
| Allocation concealment (selection bias) | Low risk | Quote: "To control for order effects, the order of stimuli was randomised, with order series placed in opaque sealed envelopes with envelopes selected by an independent observer for each participant." (p40). All participants underwent the 5 conditions in random order |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Behavioural data using video recordings of patient sessions were analysed by a trained volunteer, who was blinded by removing audio from recordings." (p41) |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition was not reported |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "The research detailed in this thesis was funded primarily through a three year full time PhD Mobility Fellowship from the Doctoral School of the Humanities within the Department of Psychology and Communication at Aalborg University. Additional funding was provided by the Royal Hospital for Neuro‐disability and the Music Therapy Charity." (piii) |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants with unilateral poststroke hemiparesis Diagnosis: haemorrhagic stroke (32%), infarction (68%) Time since onset: mean 15.5 months (SD 5) N randomised to experimental condition (fast‐tempo auditory stimulation (FTAS)): 13 N randomised to wait‐list control: 13 N analysed in FTAS: 13 N analysed in control: 12 Mean age: 59.55 years Sex: 16 females (64%), 9 males (36%) Ethnicity: not reported Setting: rehabilitation unit Country: South Korea | |
| Interventions | 2 study groups: 1. Music intervention group: FTAS 2. Control group: walking training with no specific auditory stimulation Number of sessions: 20 sessions in total, with sessions twice a day 5 days a week over 2 weeks Length of sessions: 30 minutes | |
| Outcomes | Gait parameters: gait velocity, gait cadence, stride length, Wisconsin Gait Scale: post‐test scores used. | |
| Notes | This study used rhythm delivered by a metronome in combination with recorded music. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation through drawing of lots (correspondence with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Allocation concealment through drawing of sealed envelopes (correspondence with principal investigator) |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving FTAS or the personnel involved in delivering FTAS |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | High risk | Blinding of the outcome assessors for the objective outcomes was not reported |
| Incomplete outcome data (attrition bias) | Low risk | 1 participant was eliminated from the data analysis due to a history of irregular participation in repeated trials. Attrition reported at 3.85%. Quote: "During the study, one CG subject was eliminated from data analysis due to a history of irregular participation in repeated trials" (p296) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support was reported |
| Methods | Quasi‐RCT | |
| Participants | Adults with stroke with unilateral cerebral hemiplegia determined to have reached their maximum capacity of physical function and subsequently discharged from occupational and physical therapies. All participants had at least 10 degrees of limitation in active shoulder flexion and elbow extension. Time since onset: mean 93.4 days (SD 49.5) N randomised to experimental group: 10 N randomised to control group: 10 | |
| Interventions | 2 study groups: 1. Music intervention group: participants engaged in active music improvisation sessions with the music therapist using electronic music devices that allowed for easy sound manipulation. Improvisations emphasised steady rhythmic pulses. | |
| Outcomes | Active shoulder flexion (Jamar goniometer); elbow extension (Jamar goniometer). Post‐test scores were used | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate group allocation |
| Allocation concealment (selection bias) | High risk | No allocation concealment used |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind the participants or professionals delivering this intervention |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Low risk | 2 occupational therapists who did the goniometric measurements were blinded. Quote: "The therapists were blind to the conditions of each participant” (p229) |
| Incomplete outcome data (attrition bias) | Low risk | There were no withdrawals |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "This project was funded by a research grant from the Institute for Music and Neurologic Function, New York, New York" (p236) |
| Methods | RCT Cross‐over trial with 2 groups | |
| Participants | TBI participants in subacute rehabilitation Diagnosis: haemorrhage (N = 5) 50%, stroke (N = 2) 20%, traumatic brain injury (N = 3) 30% Time since onset: mean 11.55 years (138.6 months) N randomised to experimental condition: 5 N randomised to control condition: 5 N analysed in experimental group: 3 N analysed in control group: 5 Mean age: 53.8 years Sex: 6 females (60%), 4 males (40%) Ethnicity: not reported Setting: community day centres Country: UK | |
| Interventions | 2 study groups: 1. Music intervention group: 8 sessions of music therapy followed by another 8 sessions of music therapy followed by 8 weeks of standard care/follow‐up 2. Control group: 8 weeks of standard care followed by 8 sessions of music therapy followed by another 8 sessions of music therapy followed by 8 weeks of follow‐up Music therapy intervention was musical attention‐training exercises and songwriting In this review we only used the first phase of this study (8 sessions), before the cross‐over Number of sessions: 8 sessions on a weekly basis Length of sessions: 60 minutes | |
| Outcomes | Cognitive function: Test of Everyday Attention, Immediate Recall subtest from the Rivermead Behavioural Memory Test‐Third Edition Mood: POMS‐Bipolar version, satisfaction of emotional needs (developed for this study) Change scores were used | |
| Notes | For mood outcomes, this study used the following POMS‐Bipolar form subscales: agreeable‐hostile, composed‐anxious, energetic‐tired, and elated‐depressed only. As total scores were not available, we could not include these outcomes in our meta‐analyses 1 review author (JB) computed change scores | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation through flipping of coin |
| Allocation concealment (selection bias) | Low risk | Allocation concealment through flipping of coin |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors for the objective outcomes were blinded. Quote: "The test administrators were not informed about which time‐point each participant was at in the treatment schedule. Therefore, the administrators were blinded to the treatment conditions for each participant" (p117) |
| Incomplete outcome data (attrition bias) | High risk | Attrition reported as 2 (20%). Reasons for attrition not given. Quote: "Two subjects dropped out from the total number of ten subjects recruited" (p337) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support was reported |
| Methods | Quasi‐RCT 2‐arm parallel‐group design | |
| Participants | People with stroke with moderate impairment of upper limb motor function. 20 (50%) with left extremity affected (10 in each group) and 20 (50%) with right extremity affected (10 in each group) Diagnosis: 34 (85%) ischaemic stroke, 6 (15%) haemorrhagic stroke Time since onset: mean 2 months N randomised to experimental group: 20 N randomised to control group: 20 N analysed in experimental group: 20 N analysed in control group: 20 Mean age: 56.3 years Sex: 13 females (33%), 27 males (67%) Ethnicity: all native German speakers Setting: inpatient Country: Germany | |
| Interventions | 2 study groups: 1. Music intervention group: Music‐supported training (MST). This involved playing either a MIDI keyboard (fine motor skills) or an electronic drum set consisting of 8 pads (gross motor skills), or both. The music exercises were adaptable to the needs of the participants and systematically increased in difficulty according to 10 set levels. All exercises were demonstrated by the instructor first and then repeated by the participant 2. Control group: Conventional therapy Number of sessions (experimental group only): 15 in total over 3 weeks Length of sessions: 30 minutes | |
| Outcomes | Upper extremity motor functions (Action Research Arm Test; Arm Paresis Score; Box and Block Test; Nine‐Hole Pegboard Test). Analysis of quality and velocity of finger‐tapping and hand‐tapping movements assessed using a computerised movement analysis system (frequency of full cycles per second; number of inversions of velocity profiles per movement segment; average maximum angular velocity) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients were assigned pseudo‐randomly" (p1340). We determined through correspondence with author that participants were assigned to groups in blocks using alternate assignment (20 to MST, followed by 20 to control, followed by 12 to MST, followed by 10 to control) |
| Allocation concealment (selection bias) | High risk | Quote: "Patients were assigned pseudo‐randomly by the occupational therapists not involved in the study to two groups" (p1340). However, we determined that there was a high risk of selection bias due to serial block allocation |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Subjective outcomes were not used in this study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "There were no drop outs" (p1340) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "Supported by grants from the DFG (AL 269/7‐1) and the BMBF" (p1345) |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants with hemiplegic stroke Diagnosis: 5 (31.25%) haemorrhagic stroke, 11 (68.75%) ischaemic stroke Time since onset: mean 305.32 days N randomised to experimental group: 8 N randomised to control group: 8 N analysed in experimental group: 8 N analysed in control group: 8 Mean age: 65.82 years Sex: 10 females (62.5%), 6 males (37.5%) Ethnicity: not reported Setting: rehabilitation unit Country: South Korea | |
| Interventions | 2 study groups: 1. Music intervention group: neurodevelopmental therapy (NDT) gait training with RAS 2. Control group: NDT gait training without RAS Number of sessions: 15 in total, once per day for 3 weeks Length of sessions: 15 minutes | |
| Outcomes | Gait parameters: gait velocity (m/minute), gait cadence (steps per minute), stride length (m), standing balance (overall stability index). Change scores used | |
| Notes | The RAS employed in this study did not use accompanying music. Quote: "The rhythm stimulation was composed of single tone series in 4/4 time signature" (p195) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list. Quote: "Patients were randomly assigned to either experimental (N = 8) or control (N = 8) group by a computerized random number generator" (p194) |
| Allocation concealment (selection bias) | Low risk | Allocation concealment reported. Quote: "Random numbers for the allocation‐to‐treatment sequence were concealed from the recruiter and the therapists. Patients were informed of the two possible treatment allocations, but not whether they are in the experimental or control arm." (p194) |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were blind to treatment allocations. Quote: "Random numbers for the allocation‐to‐treatment sequence were concealed from the recruiter and the therapists. Patients were informed of the two possible treatment allocations, but not whether they are in the experimental or control arm" (p194). It is not possible to blind the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | Low risk | Subjective outcomes were not used in this study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition was not reported |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "The work was supported by the Ewha Global Top 5 Grant 2012 of Ewha Womans University." (p198) |
| Methods | RCT 3‐arm parallel‐group design | |
| Participants | Participants with ischaemic stroke Time since onset: mean 6.2 days N randomised to music listening: 20 N randomised to audio book listening: 20 N randomised to standard care control: 20 N analysed in music listening: 19 N analysed in audio book listening: 19 N analysed in standard care control: 17 Mean age: 58.87 years Sex: 16 females (44%), 20 males (56%) Ethnicity: not reported Setting: neurology unit Country: Finland | |
| Interventions | 3 study groups: 1. Music intervention group: Music therapists provided participants with portable CD players and CDs of their own favourite music in any musical genre. 2. Language intervention group (not used in this review): Participants were provided with portable cassette players and narrated audio books on cassettes selected by the participants from a collection of the Finnish Celia library for the visually impaired (celia.fi) 3. Control group: No listening material. Number of sessions (experimental group): daily for 2 months Length of sessions: minimum of 60 minutes per day | |
| Outcomes | Communication function repetition and reading (subtests of the Finnish version of the Boston Diagnostic Aphasia Examination); verbal fluency and naming subtests (Consortium to Establish a Registry for Alzheimer’s Disease battery and a shortened version of the Token Test). Cognitive function (story recall subtest from the Rivermead Behavioural Memory Test, digit span subtest from the Wechsler Memory Scale‐Revised), and a memory interference task (Frontal Assessment Battery). Attention (CogniSpeed reaction time software). Mood (POMS). Change scores used | |
| Notes | The POMS used in this study was "the shortened Finnish version (Hänninen 1989) of the Profile of Mood States (POMS; McNair et al 1981). It contains 38 items that form following eight subscales: tension, depression, irritability, vigour, fatigue, inertia, confusion and forgetfulness." (p868). Scores for the subscales were available from published data, and total scores were made available by the principal investigator in unpublished data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation using computer‐generated number list. Quote: "Randomization was performed with a random number generator" (p867) |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was performed with a random number generator by a researcher not involved in the patient enrollment" (p867)Quote: "The researchers involved in these studies (authors TS and MM) were blinded to the group allocation of the patients" (p868) |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Clinical neuropsychological assessment was performed on all patients at the baseline (1 week from stroke onset), and repeated again 3 months and 6 months post‐stroke. The researchers involved in these studies (authors TS and MM) were blinded to the group allocation of the patients" (p868) |
| Incomplete outcome data (attrition bias) | Low risk | Attrition reported with reasons for withdrawal. Quote: "Of the 60 subjects originally recruited in to the study, 55 completed the study up to the 3‐month follow‐up (music group N = 19, language group N = 19 and control group N = 17). Of the five drop‐outs, one was due to false diagnosis (transient Ischaemic attack), one due to a new stroke, one due to dementia and two due to refusal. One further subject died from myocardial infarction before the 6‐month follow‐up (music group N = 18, language group N = 19, and control group N = 17 at the 6‐month stage)" (p867) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "This work was supported by Academy of Finland (project no 77322), Jenny and Antti Wihuri Foundation (Helsinki, Finland), National Graduate School of Psychology and Neurology Foundation (Helsinki, Finland). Funding to pay the Open Access publication charges for this article was provided by Cognitive Brain Research Unit, Department of Psychology, University of Helsinki, Finland." (p874) |
| Methods | RCT | |
| Participants | Participants with hemiparesis following stroke N randomised to experimental group: 10 N randomised to control group: 10 N analysed in experimental group: 10 N analysed in control group: 10 Mean age: 73 years (SD 7) experimental group, 72 years (SD 8) control group | |
| Interventions | 2 study groups: 1. Music intervention group: RAS | |
| Outcomes | Gait parameters: velocity, stride length, cadence, symmetry: pre‐test and post‐test values | |
| Notes | The RAS employed in this study used metronome beat in combination with recorded music. Quote: "The rhythmic stimulus in the training sessions consisted of music tapes played over headsets that were prerecorded on a synthesizer/sequencer module. Instrumental music in 4 different styles was prepared (classic, folk, country, jazz). The music was recorded in 2/4 meter to match the rhythm of the step patterns in gait. A metronome beat was overlaid on the strong beat of the music to enhance the rhythmic perception for the patient." (p209) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Recruiters did not know group conditions (personal communication with principal investigator) |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | Low risk | Subjective outcomes were not used in this study |
| Blinding of outcome assessment (detection bias) | Low risk | Participants were assessed by "a physical therapist blind to the experiment" (p208) |
| Incomplete outcome data (attrition bias) | Low risk | No participant loss (personal communication with principal investigator) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "This research was funded in part by a grant from the Poudre Valley Hospital Foundation and grants RR 07127‐20 and RR 07127‐23 from the National Institutes of Health (NIH)" (p211) |
| Methods | RCT | |
| Participants | Participants with left hemispheric stroke Time since onset: mean 11.4 months (SD 5.2) Diagnosis: 19 (90%) ischaemic stroke (15 in the middle cerebral artery distribution and 4 in the anterior cerebral artery distribution); 2 (10%) intracerebral haemorrhage related to a cerebral aneurysm N randomised: 21 N analysed: 21 Mean age: 52.7 years (SD 13.7) | |
| Interventions | 2 study groups: 1. Music intervention group: RAS | |
| Outcomes | Arm timing, variability of movement timing, wrist trajectories, wrist trajectory variability, elbow range of motion. Pre‐test and post‐test scores used | |
| Notes | The RAS employed in this study did not use accompanying music. Quote: "The auditory rhythm consisted of a metronome‐like 1000 Hz square wave tone with a 50 ms plateau time produced by a computerized MIDI‐sequencing sound software" (p1075) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers (personal communication with principal investigator) |
| Allocation concealment (selection bias) | Low risk | Serially numbered, opaque, sealed envelopes (personal communication with principal investigator) |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or the personnel involved in delivering RAS |
| Blinding of outcome assessment (detection bias) | Low risk | Subjective outcomes were not used in this study |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Participant withdrawals were not reported |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "This research was supported in part by a grant from the Deutsche Forschungsgesellschaft, Sonderforschungsbereich 194 to Thaut and Hoemberg (DFG: German Research Council, Special Research Section 194)" (p1079) |
| Methods | RCT | |
| Participants | Participants with subacute hemiparetic stroke Diagnosis: 65 (83%) middle cerebral artery stroke; 8 (11%) internal capsule stroke; 4 (5%) basal ganglia/thalamus stroke; 1 (1%) subdural haematoma Time since onset: approximately 21 days N randomised to experimental group: 43 N randomised to control group: 35 N analysed in experimental group: 43 N analysed in control group: 35 Mean age: 69.2 years (SD 11.5) experimental group; 69.7 years (SD 11.2) control group | |
| Interventions | 2 study groups: 1. Music intervention group: RAS | |
| Outcomes | Gait parameters: velocity, stride length, cadence, symmetry: post‐test scores were used | |
| Notes | The RAS employed in this study used metronome beat in combination with recorded music. Quote: "RAS training followed established protocols using a metronome and specifically prepared music tapes in digital MIDI format to ensure temporal precision and tempo stability as well as full capacity for frequency modulation of the stimulus based on patient needs" (p456) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers |
| Allocation concealment (selection bias) | Low risk | Serially numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | It is not possible to blind participants receiving RAS or the personnel involved in delivering RAS. Quote: "Therapists were not blinded to the treatment conditions of the study. However, because both conditions are considered full treatment conditions, no performance bias was expected." (p456) |
| Blinding of outcome assessment (detection bias) | Unclear risk | Subjective outcomes included participant satisfaction, however the measures used and the methods of data collection were not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: “Both groups were assessed by blinded physical therapists” (p456) |
| Incomplete outcome data (attrition bias) | High risk | 23% dropouts in German centre, 10% in US centre (absolute numbers are not reported) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | No funding support was reported |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants with light to moderate motor impairment in the upper extremity following stroke Diagnosis: 15 (50%) haemorrhagic stroke, 15 (50%), ischaemic stroke Time since onset: mean 5.35 months N randomised to experimental group: 15 N randomised to control group: 15 N analysed in experimental group: 15 N analysed in control group: 15 Mean age: 49.35 years Sex: 4 females (62.5%), 26 males (37.5%) Ethnicity: Chinese Setting: rehabilitation unit Country: China | |
| Interventions | 2 study groups: Music‐supported therapy involving 2 conditions: 1. Music intervention group: audible music group involving the playing of musical instruments that were audible/not muted 2. Control group: mute music group involving the playing of musical instruments that resembled the audible musical instruments used in the music intervention group but that were made of sponge Number of sessions: 20 in total over 4 weeks | |
| Outcomes | Upper extremity function (Wolf Motor Function Test, FMA): change scores used | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation using random number table. Quote: "Randomisation was performed by assigning random numbers from random number tables" (p2) |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not reported |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Subjective outcomes were not used in this study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of outcome assessors for the objective outcomes was not reported |
| Incomplete outcome data (attrition bias) | Low risk | Attrition was reported as 9%. Quote: "Three patients in the CG dropped out because of training boredom" (p4) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | The authors declare no conflict of interest. Quote: "This work was partially supported by China Rehabilitation Research Center (CRRC) fund (no. 2008‐19)." (p6) |
| Methods | RCT 3‐arm parallel‐group design | |
| Participants | Participants with stroke with light to moderate motor impairment in the upper extremity Diagnosis: stroke Time since onset: mean 9.37 weeks N randomised to modified bilateral arm training with rhythmic auditory cueing (mBATRAC) group: 19 N randomised to DMCT control group: 19 N randomised to modified constraint‐induced movement therapy (mCIMT) control group: 22 N analysed in mBATRAC group: 18 N analysed in DMCT control group: 16 N analysed in mCIMT control group: 21 Mean age: 59.75 years Sex: not reported Ethnicity: not reported Setting: rehabilitation unit Country: Netherlands | |
| Interventions | 3 study groups: 1. Music intervention group: mBATRAC, which involved a modification of the original bilateral arm training with rhythmic auditory cueing protocol that targeted rhythmic flexion and extension movements about the wrist rather than movements of proximal parts of the upper limb 2. Control group: Conventional treatment (DMCT) was an exercise therapy based on existing guidelines for upper limb rehabilitation after stroke, discarding specific elements of the 2 experimental conditions 3. 2nd intervention group (not used in this review): mCIMT, which involved repetitive task practices and shaping of the desired movements, with an emphasis on increased control of wrist and finger extensors Number of sessions: 18 sessions in total with 3 sessions per week over 6 weeks | |
| Outcomes | Upper extremity function (Action Research Arm Test, Motricity Index, Nine‐Hole Peg Test, Fugl‐Meyer Motor Assessment, Erasmus modifications of the Nottingham Sensory Assessment) Communication function, cognitive function, mood (all using the Stroke Impact Scale) Change scores used | |
| Notes | RAC in this study followed the protocol for mBATRAC, which was not defined in this article. However, the BATRAC protocol has been defined elsewhere as moving "in time to a metronome" (McCombe Waller 2005, p546) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomized in permuted blocks and allocated to 1 of the 3 intervention groups" (p2164) |
| Allocation concealment (selection bias) | Low risk | Quote: "Concealed allocation was effectuated online using the minimization method" (p2164) |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Althoughsubjective outcomes were examined in this study, these outcomes were not included in this systematic review, as they had not been specified as outcomes of interest at the outset of the study |
| Blinding of outcome assessment (detection bias) | Unclear risk | The study is reported as a single‐blind trial, so presumably the data collector was blind. However, blinding is not described and is therefore unclear |
| Incomplete outcome data (attrition bias) | Low risk | Attrition reported as 15.8%. 19 enrolled in mBATRAC; 19 enrolled in DMCT; follow‐up 17 in mBATRAC and 15 in DMCT groups. Descriptions of withdrawals: 1 refused after allocation; 3 moved away; 2 did not appear for follow‐up |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "This study was funded by the Dutch Scientific College of Physiotherapy of the Royal Dutch Society for Physical Therapy." (p2615) |
| Methods | RCT with a wait‐list control group | |
| Participants | Participants with stroke with aphasia Diagnosis: 1 (7%) haemorrhagic stroke, 14 (86%) ischaemic stroke, 1 (7%) stroke type unknown Time since onset: mean 10.6 months N randomised to melodic intonation therapy (MIT): 16 N randomised to wait‐list control: 11 N analysed in MIT: 11 N analysed in wait‐list control: 11 Mean age: 52.55 years Sex: 16 females (60%), 11 males (40%) Ethnicity: not reported Setting: hospitals, rehabilitation centres, and nursing homes Country: Netherlands | |
| Interventions | 2 study groups: 1. Music intervention group: intensive melodic intonation therapy (MIT) for the first 6‐week period (between T1 and T2), and then received "regular therapy" for the second 6‐week period (between T2 and T3) 2. Control group: received "intensive control treatment" between T1 and T2, and then received delayed MIT between T2 and T3 Number of sessions: unclear. 5 hours a week over 6 weeks | |
| Outcomes | Communication function (Aachen Aphasia Test, Amsterdam‐Nijmegen Everyday Language Test, Semantic Association Task, Sabadell story retelling task (connected speech), MIT repetition task). Change scores used | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated number list. Quote: "A computer‐generated random allocation sequence was used” (p537) |
| Allocation concealment (selection bias) | Low risk | Used opaque, sealed envelopes. Quote: "a computer‐generated random allocation sequence was used and the results placed in consecutively numbered sealed envelopes” (pp537‐8) |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention. Quote: "participants and speech‐language therapists (SLTs) could not be blinded for treatment condition" (p538) |
| Blinding of outcome assessment (detection bias) | Low risk | No subjective outcomes were included in this study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of the outcome assessors for the objective outcomes was not achieved in all cases. Quote: "The researchers administering and scoring the assessments at each test moment were blinded for group allocation. In a few cases, blinding could not be maintained because the patients spontaneously informed the researcher about their therapy allocation" (p538) |
| Incomplete outcome data (attrition bias) | Low risk | Exact attrition rate is unclear as there is a lack of congruence between the text and the CONSORT diagram. Text suggests that there was a 14.8% attrition rate, due to early discharge and refusal to participate. Quote: "A total number of 27 patients were included in the study: 16 were allocated to the experimental group and 11 to the control group. Four patients withdrew from MIT after 1 or 2 weeks, because they felt uncomfortable with the therapy or were disappointed by their progress." (p539) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | Low risk | Quote: "The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Stichting Rotterdams Kinderrevalidatie Fonds Adriaanstichting (Grant No. 2007/0168 JKF/07.08.31KFA)" (p543) |
| Methods | RCT 2‐arm parallel‐group design | |
| Participants | Participants with unilateral stroke Diagnosis: Locations of strokes reported as follows. Brainstem: 6 (6%) Cerebellar: 2 (2%) Cortex: 39 (42%) Multiple: 3 (3%) Subcortical: 19 (20%) Unknown/missing: 24 (26%) Time since onset: > 6 months N randomised to BATRAC group: 55 N randomised to control (dose‐matched therapeutic exercises (DMTE)): 56 N analysed in BATRAC group: 42 N analysed in control group: 50 Mean age: 59.8 years Sex: 42 females (46%), 50 males (54%) Ethnicity: not reported Setting: outpatient Country: USA | |
| Interventions | 2 study groups: 1. Music intervention group: BATRAC 2. Control group: dose‐matched therapeutic exercises (DMTE) consisting of 4 exercises based on neurodevelopmental principles including thoracic spine mobilisation with weight shifting, scapular mobilisation, weight bearing with the paretic arm (elbow fixed), and opening the hand with finger extension Number of sessions: 18 in total with 3 sessions per week over 6 weeks Length of sessions: 1 hour, which included 20 minutes active participation and 4 minutes rest | |
| Outcomes | Motor impairment (Fugl‐Meyer Assessment of the Upper Extremity, Wolf Motor Function Test (time), Stroke Impact Scale, isokinetic strength of elbow flexion/extension arm movements) | |
| Notes | Total N of participants adds up to 83, not 92 as reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized after B2 to receive either BATRAC or DMTE using a stratified block allocation scheme based on initial function (NIH Stroke Scale with 2 as cutoff) and motor dominance of stroke." (pp121‐2) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Low risk | It was not possible to blind the participants or professionals delivering the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Self report measures were used for subjective outcomes |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Testing was conducted in a separate location from the training site by trained testers blinded to group assignment." (p122) |
| Incomplete outcome data (attrition bias) | Low risk | Attrition at post‐training analysis (6‐week time point): 17%. 55 allocated to BATRAC; 56 allocated to DMTE. N analysed in BATRAC = 42; N analysed in DMTE = 50. Descriptions of withdrawals: 12 for medical reasons (BATRAC, N = 8; DMTE, N = 4); 7 for personal reasons (BATRAC, N = 5; DMTE, N = 2) |
| Selective reporting (reporting bias) | Low risk | There are no indications of selective reporting for this study |
| Free from financial conflict of interest | High risk | Quote: "The author(s) declared a potential conflict of interest (e.g. a financial relationship with the commercial organizations or products discussed in this article) as follows: As inventors of the subject technology, Jill Whitall and Sandy McCombe Waller anticipate receiving licensing income from their institution (UMB), under its Intellectual Property Policy." (p127) |
BATRAC: bilateral arm training with rhythmic auditory cueing
BP: blood pressure
COPM: Canadian Occupational Performance Measure
CVA: cerebrovascular accident
EMG: electromyography
FMA: Fugl‐Meyer Assessment
POMS: Profile of Mood States
PTA: post‐traumatic amnesia
RAC: rhythmic auditory cueing
RAS: rhythmic auditory stimulation
RCT: randomised controlled trial
ROM: range of motion
SD: standard deviation
SIS: Stroke Impact Scale
TBI: traumatic brain injury
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Insufficient reporting on intervention and design. Attempts to obtain additional data from authors were unsuccessful. | |
| Control group used healthy participants, and not RCT. | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Not RCT or CCT No control group | |
| Control group used healthy participants. | |
| Not RCT or CCT Single‐subject design | |
| Insufficient reporting of results: only means are reported, no SDs. Attempts to obtain additional data from authors were unsuccessful. The authors use a standardised measure (12‐Item Short Form Health Survey) for physical and mental health, but all other outcomes (e.g. body awareness, emotional awareness, relational quality) are measured by self developed questionnaires. | |
| The published results of this study examine outcomes not included in this review. | |
| Not RCT or CCT | |
| Not RCT or CCT Within‐subject design | |
| Not RCT or CCT | |
| Unacceptable treatment allocation method | |
| Compared rhythmically cued speech, melodically cued speech, and verbal speech of participants who had been receiving music therapy | |
| Not population of interest (multiple sclerosis) | |
| Control group used healthy participants. | |
| We could not locate any published results. Attempts to obtain additional data from authors were unsuccessful. | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Planned to be conducted as RCT, however only 2 participants enrolled | |
| Not RCT or CCT Within‐subject design | |
| Not RCT or CCT Within‐subject design | |
| Standardised outcome measures had been adapted, and adaptations had not been validated. | |
| Not RCT or CCT Wait‐list design with no control group | |
| Insufficient data collection (personal communication) | |
| Not RCT or CCT | |
| Not RCT or CCT Single‐subject design with healthy controls | |
| An intervention using rhythmic auditory stimulation was used as a control condition, therefore control condition did not qualify as a 'no‐music' condition. | |
| Extremely large standard deviations indicate that the data was not normally distributed. | |
| Not RCT or CCT | |
| Not RCT or CCT Protocol description | |
| No randomisation or quasi‐randomisation | |
| Not population of interest (cerebral palsy) | |
| Not RCT or CCT Within‐subject design using pre and post measures | |
| Single‐group design with no randomisation | |
| The research question was not relevant to this review. | |
| Not RCT or CCT | |
| Comparative study of 2 music therapy interventions | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Further details are required about the randomisation process. Attempts to obtain additional data from authors were unsuccessful. We could not locate the authors through an internet search for the facility. Given the age of this article, we have excluded it from our review. | |
| Not RCT or CCT | |
| Not RCT or CCT (personal communication with author's project advisor) | |
| Not RCT or CCT | |
| Cannot access this publication through interlibrary searching | |
| Cross‐over design that examined 2 conditions (preferred music with classical music) and used baseline data as the "control" No control data reported | |
| We could not determine whether randomisation had been used in this study. Attempts to obtain additional data from authors were unsuccessful as we were unable to obtain author contact information. | |
| Not RCT or CCT | |
| Inconsistent reporting of research design, treatment conditions, and dosage We contacted the authors on several occasions but received no response. | |
| Not RCT or CCT | |
| Not RCT or CCT No control group | |
| Control group used healthy participants. | |
| Not RCT or CCT No randomisation (personal communication with author) | |
| Control group used healthy participants. | |
| Inadequate methodological information | |
| Outcomes are not of interest to this review. | |
| Not RCT or CCT Study was designed as a 2‐group parallel study, and the control group was added to the research at a later stage. | |
| Unable to retrieve publication | |
| Used matched healthy controls | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| This study is part of the Särkämö 2008 study, however it only reports on brain imaging outcomes, which are not outcomes of interest to this review. | |
| Not RCT or CCT This study does not examine outcomes of interest to this review (amusia). | |
| Control group used healthy participants. | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Not RCT or CCT No randomisation or quasi‐randomisation Results present within‐group comparisons rather than between‐group comparisons. | |
| Not RCT or CCT Single‐subject design with multiple baselines Intervention does not seem to include a musical condition, and so is not an intervention of interest to this review. | |
| Not RCT or CCT Within‐subject design | |
| Not RCT or CCT Single‐subject design | |
| Not RCT or CCT Single‐subject design | |
| Not RCT or CCT No control intervention Comparison of 2 interventions: somatosensory stimulation and "exercise therapy on music" | |
| Not RCT or CCT | |
| Unable to determine methods of randomisation We contacted the authors on several occasions but received no response. | |
| Not RCT or CCT No randomisation or quasi‐randomisation | |
| Not RCT or CCT | |
| Not RCT or CCT | |
| Unable to retrieve publication | |
| Unable to retrieve publication |
CCT: controlled clinical trial
RCT: randomised controlled trial
SD: standard deviation
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT 4‐arm parallel‐group design |
| Participants | Participants with stroke with hemiparesis Time since onset: unknown N randomised: 60 Age range: unknown Sex: unknown Ethnicity: unknown Setting: unknown Country: Iran |
| Interventions | 4 study groups: 1. Program‐based computer software use 2. Listening to Mozart Sonata K448 3. Software use plus listening to Mozart Sonata K448 4. Control: no intervention Length of intervention: 6 months Number of sessions: unclear Length of sessions: 1 hour per night |
| Outcomes | Magnetic resonance spectroscopy Fugl‐Meyer Assessment of Physical Performance Mini Mental State Exam |
| Notes |
| Methods | RCT 3‐arm parallel‐group design |
| Participants | Participants with subacute stroke Time since onset: unknown N randomised: 60 Age range: 50 to 70 years, mean unknown Sex: 22 females (37%), 38 males (63%) Ethnicity: unknown Setting: unknown Country: unknown |
| Interventions | 3 study groups: 1: Listening to film and classical songs plus conventional management 2. Meditation plus conventional management 3. Conventional management only (control) Length of intervention: 6 weeks Number of sessions: total unknown Length of sessions: unknown |
| Outcomes | Hamilton Rating Scale for Depression Berg Balance Scale Barthel Activities of Daily Living Index Fatigue Severity Scale |
| Notes |
| Methods | RCT 3‐arm parallel‐group design |
| Participants | Participants with stroke Time since onset: unknown N randomised: 16 Mean age: unknown Sex: unknown Ethnicity: unknown Setting: tertiary inpatient medical centre Country: Philippines |
| Interventions | 3 study groups: 1. Control: white noise background 2. Rhythm: metronome ‐ 100 beats per minute 3. Music: "Pomp and Circumstance" Length of intervention: unknown Number of sessions: unknown Length of sessions: unknown |
| Outcomes | Functional Independence Measure Hand dynamometer |
| Notes |
| Methods | RCT 2‐arm parallel‐group design |
| Participants | Participants with stroke Time since onset: unknown N randomised to intervention: 8 N randomised to control: 11 Mean age: unknown Sex: unknown Ethnicity: unknown Setting: unknown Number of sessions: unknown Length of intervention: unknown Length of sessions: unknown |
| Interventions | Music therapy |
| Outcomes | Health‐related quality of life Anxiety, depression, irritation, and anger Quality of life (anxiety, acceptance of condition, sense of control) |
| Notes |
| Methods | RCT 2‐arm parallel‐group design |
| Participants | Adults following stroke Time since onset: first 12 weeks' poststroke N randomised: unknown Mean age: unknown Sex: unknown Ethnicity: unknown Setting: unknown Number of sessions: unknown Length of intervention: unknown Length of sessions: unknown |
| Interventions | 70 hours of preferred music listening over 12 weeks via MP3 players and logged in diaries |
| Outcomes | Not specified, but describes mood and cognition as primary outcomes, and function and quality of life as secondary outcomes |
| Notes | Prospective abstract describing study protocol |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Examining the effects of active music therapy on post‐stroke recovery: a randomised controlled cross‐over trial |
| Methods | RCT Cross‐over trial Computer‐generated randomisation |
| Participants | 45 participants with stroke |
| Interventions | Experimental music therapy condition: 2 (60‐minute) weekly sessions of active music therapy in individual setting over a period of 3 months |
| Outcomes | Functional disability and activities of daily living independency (BI), level of impairment (NIHSS), disability grade (mRS), neglect (BIT), and motor function of upper extremity (ARAT) |
| Starting date | |
| Contact information | Contact: Professor Esa Ala‐Ruona, email: esa.ala‐[email protected] |
| Notes |
| Trial name or title | Melodic‐intonation‐therapy and speech‐repetition‐therapy for patients with non‐fluent aphasia |
| Methods | RCT Parallel assignment |
| Participants | Adults with aphasia following first‐time ischaemic left‐hemispheric stroke or CVA |
| Interventions | Music condition: melodic intonation therapy Active comparator: speech repetition therapy Control: no therapy |
| Outcomes | Primary outcomes: language outcomes (correct information units) Secondary outcomes: language, speech, functional and structural brain changes |
| Starting date | February 2008 |
| Contact information | Contact: Gottfried Schlaug, MD, PhD, email: [email protected] Andrea Norton, email: [email protected] |
| Notes | This study is currently recruiting participants. Estimated study completion date: December 2016 |
| Trial name or title | The effects of a rhythm and music‐based therapy program and therapeutic riding in late recovery phase following stroke |
| Methods | RCT Parallel assignment |
| Participants | Adults aged 50 to 75 years who are 1 to 5 years' poststroke Estimated enrolment: 123 |
| Interventions | Music condition: rhythm and music therapy Active comparator: therapeutic riding Control: receives no intervention |
| Outcomes | Primary: degree of participation (Stroke Impact Scale, version 2) Secondary: self reported fatigue, perceived physical functioning, self rated perceived mental functioning, cognitive function, body function, environmental factors, personal factors |
| Starting date | January 2010 |
| Contact information | Contact: Lina Bunketorp Kall, PhD, email: Lina.Bunketorp‐[email protected] |
| Notes | The results of this study are being prepared for publication (correspondence with principal investigator). Estimated study completion date: December 2015 |
| Trial name or title | Creative therapy to affect stroke outcomes |
| Methods | RCT Parallel assignment |
| Participants | Adults with stroke more than 1 month prior |
| Interventions | Music condition: creative therapy (art and music therapy) Control condition: conventional physical therapy |
| Outcomes | Primary outcome: cognition (Abbreviated Mental Test Score) Secondary outcomes: physical function (BI), mood (Hospital Anxiety and Depression Scale), quality of life (Pictorial Thai Quality of Life) |
| Starting date | November 2011 |
| Contact information | Contact: Vilai Kuptniratsaikul, MD, email: [email protected] |
| Notes | The recruitment status of this study is unknown because the information has not been recently verified. Estimated study completion date: May 2014 |
| Trial name or title | Improving arm and hand functions in chronic stroke |
| Methods | RCT Parallel assignment |
| Participants | Adults who sustained first‐time unilateral middle cerebral artery stroke more than 6 months prior. Estimated enrolment: 60 |
| Interventions | Music condition: music‐supported rehabilitation using musical exercises to improve hand and arm motor functioning Control: conventional upper extremity therapy |
| Outcomes | Primary: arm and hand functions: ARAT; Chedoke Arm and Hand Activity Inventory; Stroke Impact Scale Secondary: brain structure and brain function |
| Starting date | November 2012 |
| Contact information | Contact: Deirdre R Dawson, PhD, email: [email protected] |
| Notes | This study is ongoing, but not recruiting participants. Estimated study completion date: December 2015 |
| Trial name or title | Music listening and stroke recovery |
| Methods | RCT Factorial assignment |
| Participants | Adults with stroke. Estimated enrolment: 60 |
| Interventions | Music condition 1: daily listening to instrumental music Music condition 2: daily listening to vocal music Control condition: standard rehabilitation |
| Outcomes | Primary outcomes: physiological stress indicators, neuropsychological performance, brain MRI |
| Starting date | December 2012 |
| Contact information | Contact: Seppo Soinila, MD, email: [email protected] |
| Notes | The recruitment status of this study is unknown because the information has not been recently verified. Estimated study completion date: December 2014 |
| Trial name or title | Influence of timing on motor learning |
| Methods | RCT Parallel assignment |
| Participants | Adults with CVA. Estimated enrolment: 40 |
| Interventions | Music condition: MusicGlove group Active comparator for MusicGlove: conventional hand exercise Experimental: resonating arm exerciser Active comparator for experimental: conventional arm exercise |
| Outcomes | Motor and strength: Box and Block Test; Fugl‐Meyer Assessment |
| Starting date | September 2012 |
| Contact information | Principal investigator: Steven Cramer, MD, University of California, Irvine |
| Notes | This study is ongoing, but not recruiting participants. Estimated study completion date: June 2015 |
| Trial name or title | Efficacy and neural basis of music‐based neurological rehabilitation for traumatic brain injury (MUBI) |
| Methods | RCT Cross‐over trial |
| Participants | Adults with traumatic brain injury. Estimated enrolment: 60 |
| Interventions | Music condition: music‐based neurological rehabilitation with standard care Control condition: standard care |
| Outcomes | Primary outcomes: cognition (executive functions; focused and sustained attention; verbal working memory and learning; verbal and non‐verbal reasoning) Secondary outcomes: upper extremity motor function; depression; quality of life; emotional well‐being; structural and functional neuroplasticity |
| Starting date | March 2014 |
| Contact information | Contact: Susanna Melkas, MD, PhD, email: [email protected] |
| Notes | This study is currently recruiting participants. Estimated study completion date: December 2017 |
| Trial name or title | Music therapy to restore motor deficits after stroke (NEUROMUSIC) |
| Methods | RCT Parallel assignment |
| Participants | Adults aged 30 to 75 with motor deficits following a first stroke |
| Interventions | Music condition 1: music‐supported therapy Music condition 2: home‐based music‐supported therapy Control condition: conventional treatment |
| Outcomes | Primary outcome: performance of movements with the paretic upper extremity (ARAT) Secondary outcomes: motor function; cognitive function; emotional and quality of life change; changes in brain activation |
| Starting date | November 2013 |
| Contact information | Contact: Antoni Rodríguez‐Fornells, PhD, email: [email protected] |
| Notes | Currently recruiting participants. Estimated study completion date: April 2016 |
| Trial name or title | Listening for leisure after stroke (MELLO) |
| Methods | RCT Parallel assignment |
| Participants | Adults with ischaemic stroke, ≤ 14 days poststroke at time of recruitment. Estimated enrolment: 100 |
| Interventions | Music condition: music listening with brief mindfulness Active comparator: music listening Placebo comparator: audio book intervention |
| Outcomes | Neuropsychological assessment of cognition and mood |
| Starting date | October 2014 |
| Contact information | Contact: Jonathan Evans, PhD, email: [email protected] Satu Baylan, PhD, email: [email protected] |
| Notes | Currently recruiting participants. Estimated study completion date: September 2016 |
| Trial name or title | Music therapy for the rehabilitation of upper limb with stroke patients |
| Methods | RCT Cross‐over trial |
| Participants | Estimated enrolment: 12 |
| Interventions | Experimental music condition: early‐intervention music therapy Active comparator: delayed‐intervention music therapy |
| Outcomes | Primary outcomes: ARAT Secondary outcomes: Nine‐Hole Peg Test |
| Starting date | January 2014 |
| Contact information | Contact: Alexander J Street, email: [email protected] |
| Notes | This study is currently recruiting participants. Estimated study completion date: September 2016 |
| Trial name or title | The impact of group singing on patients with stroke and their personal caregivers |
| Methods | RCT Parallel assignment |
| Participants | Adults with stroke. Estimated enrolment: 80 |
| Interventions | Music condition: communal singing Control: no intervention |
| Outcomes | Primary: change in mood and quality of life as indicated through saliva (cortisol and melatonin sampling) Secondary: change in language aphasia |
| Starting date | April 2014 |
| Contact information | Contact: Joanne Loewy, DA, email: [email protected] Marie Grippo, email: [email protected] |
| Notes | Currently recruiting participants. Estimated study completion date: April 2018 |
| Trial name or title | To determine the therapeutic effect of the Music Glove and conventional hand exercises to subacute stroke patients |
| Methods | RCT Cross‐over trial |
| Participants | Adults with CVA. Estimated enrolment: 40 |
| Interventions | Music condition: MusicGlove Active comparator: conventional hand exercise programme |
| Outcomes | Primary: Box and Block Test Secondary: Fugl‐Meyer Assessment of the Upper Extremity; ARAT; Nine‐Hole Peg Test |
| Starting date | March 2015 |
| Contact information | Contact: Vicky Chan, email: [email protected] Renee Augburger, email: [email protected] |
| Notes | Currently recruiting participants. Estimated study completion date: June 2016 |
| Trial name or title | The efficacy of Melodic Intonation Therapy (MIT) in aphasia rehabilitation |
| Methods | RCT |
| Participants | Adults with aphasia after left hemisphere stroke |
| Interventions | Music condition: melodic intonation therapy (MIT) Control condition (postacute group): non‐MIT condition Control condition (chronic group): no treatment |
| Outcomes | Primary outcome: language (Sabadell) Secondary outcomes: language (ANELT; Aachen Aphasia Test; repetition of trained and untrained items) |
| Starting date | October 2009 |
| Contact information | Contact: Dr van der Meulen, email: [email protected] |
| Notes | See van der Meulen 2014 for results of MIT in the postacute group. This study examined the efficacy of MIT in the chronic phase of stroke. The results of the chronic phase are being prepared for publication (correspondence with principal investigator). |
ANELT: Amsterdam‐Nijmegen Everyday Language Test
ARAT: Action Research Arm Test
BI: Barthel index
BIT: Behavioral Inattention Test
CVA: cerebrovascular accident
MRI: magnetic resonance imaging
mRS: modified Rankin Scale
NIHSS: National Institutes of Health Stroke Scale
RCT: randomised controlled trial
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gait velocity Show forest plot | 9 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.1 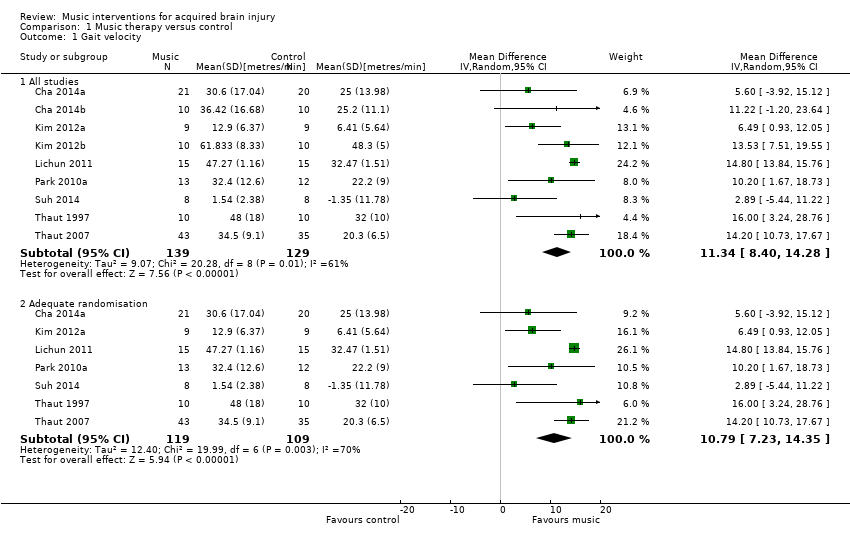 Comparison 1 Music therapy versus control, Outcome 1 Gait velocity. | ||||
| 1.1 All studies | 9 | 268 | Mean Difference (IV, Random, 95% CI) | 11.34 [8.40, 14.28] |
| 1.2 Adequate randomisation | 7 | 228 | Mean Difference (IV, Random, 95% CI) | 10.79 [7.23, 14.35] |
| 2 Gait velocity ‐ interventionist Show forest plot | 9 | 268 | Mean Difference (IV, Random, 95% CI) | 11.34 [8.40, 14.28] |
| Analysis 1.2  Comparison 1 Music therapy versus control, Outcome 2 Gait velocity ‐ interventionist. | ||||
| 2.1 Music therapist | 3 | 128 | Mean Difference (IV, Random, 95% CI) | 14.76 [13.84, 15.69] |
| 2.2 Non‐music therapist | 6 | 140 | Mean Difference (IV, Random, 95% CI) | 8.48 [5.16, 11.80] |
| 3 Gait velocity ‐ music type Show forest plot | 9 | 268 | Mean Difference (IV, Random, 95% CI) | 11.34 [8.40, 14.28] |
| Analysis 1.3 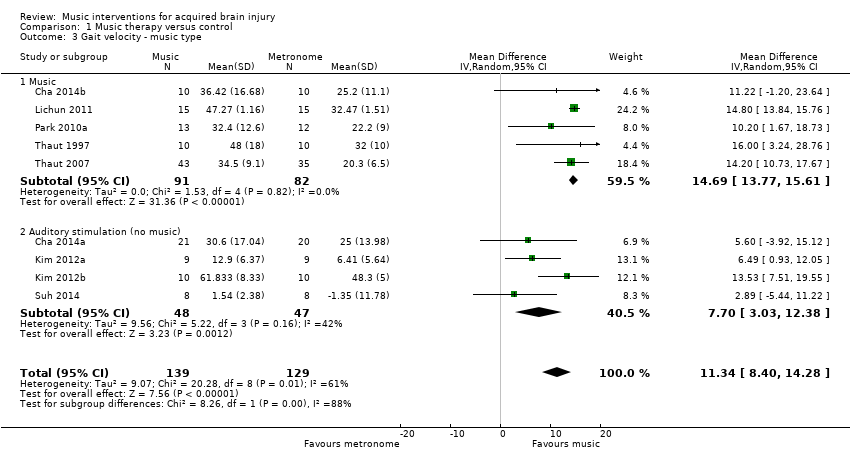 Comparison 1 Music therapy versus control, Outcome 3 Gait velocity ‐ music type. | ||||
| 3.1 Music | 5 | 173 | Mean Difference (IV, Random, 95% CI) | 14.69 [13.77, 15.61] |
| 3.2 Auditory stimulation (no music) | 4 | 95 | Mean Difference (IV, Random, 95% CI) | 7.70 [3.03, 12.38] |
| 4 Stride length (affected side) Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 Music therapy versus control, Outcome 4 Stride length (affected side). | ||||
| 4.1 All studies | 5 | 129 | Mean Difference (IV, Random, 95% CI) | 0.12 [0.04, 0.20] |
| 4.2 Adequate randomisation | 3 | 89 | Mean Difference (IV, Random, 95% CI) | 0.08 [0.05, 0.11] |
| 5 Stride length (affected side) ‐ music type Show forest plot | 5 | 129 | Mean Difference (IV, Random, 95% CI) | 0.12 [0.04, 0.20] |
| Analysis 1.5 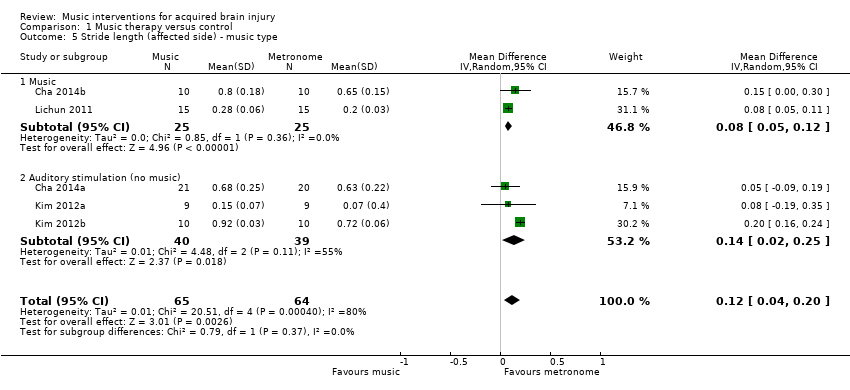 Comparison 1 Music therapy versus control, Outcome 5 Stride length (affected side) ‐ music type. | ||||
| 5.1 Music | 2 | 50 | Mean Difference (IV, Random, 95% CI) | 0.08 [0.05, 0.12] |
| 5.2 Auditory stimulation (no music) | 3 | 79 | Mean Difference (IV, Random, 95% CI) | 0.14 [0.02, 0.25] |
| 6 Stride length (unaffected side) [metres] Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.6 ![Comparison 1 Music therapy versus control, Outcome 6 Stride length (unaffected side) [metres].](/cdsr/doi/10.1002/14651858.CD006787.pub3/media/CDSR/CD006787/image_n/nCD006787-CMP-001-06.png) Comparison 1 Music therapy versus control, Outcome 6 Stride length (unaffected side) [metres]. | ||||
| 6.1 All studies | 4 | 99 | Mean Difference (IV, Random, 95% CI) | 0.11 [0.01, 0.22] |
| 6.2 Adequate randomisation | 2 | 59 | Mean Difference (IV, Random, 95% CI) | 0.06 [0.01, 0.12] |
| 7 Stride length (unspecified) [metres] Show forest plot | 3 | 186 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.01, 0.33] |
| Analysis 1.7 ![Comparison 1 Music therapy versus control, Outcome 7 Stride length (unspecified) [metres].](/cdsr/doi/10.1002/14651858.CD006787.pub3/media/CDSR/CD006787/image_n/nCD006787-CMP-001-07.png) Comparison 1 Music therapy versus control, Outcome 7 Stride length (unspecified) [metres]. | ||||
| 8 Gait cadence Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.8 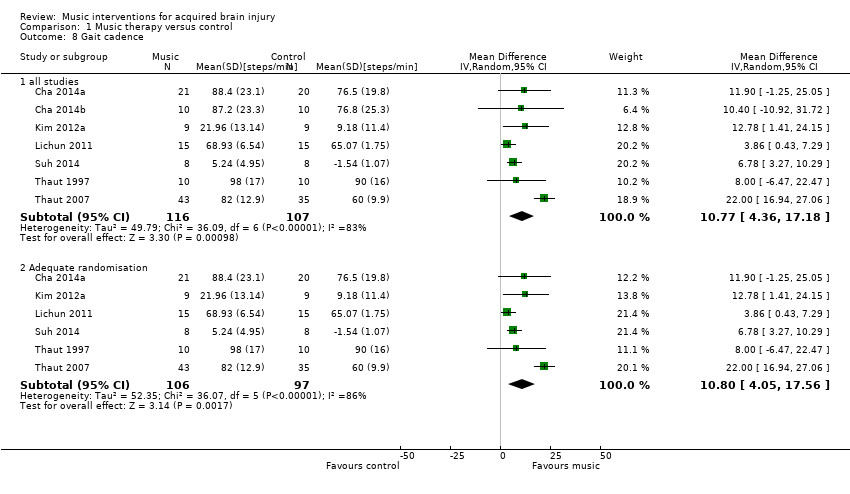 Comparison 1 Music therapy versus control, Outcome 8 Gait cadence. | ||||
| 8.1 all studies | 7 | 223 | Mean Difference (IV, Random, 95% CI) | 10.77 [4.36, 17.18] |
| 8.2 Adequate randomisation | 6 | 203 | Mean Difference (IV, Random, 95% CI) | 10.80 [4.05, 17.56] |
| 9 Gait cadence ‐ interventionist Show forest plot | 7 | 223 | Mean Difference (IV, Random, 95% CI) | 10.77 [4.36, 17.18] |
| Analysis 1.9  Comparison 1 Music therapy versus control, Outcome 9 Gait cadence ‐ interventionist. | ||||
| 9.1 Music therapist | 3 | 128 | Mean Difference (IV, Random, 95% CI) | 11.51 [‐2.57, 25.60] |
| 9.2 Non‐music therapist | 4 | 95 | Mean Difference (IV, Random, 95% CI) | 7.65 [4.43, 10.86] |
| 10 Gait cadence ‐ music type Show forest plot | 7 | 223 | Mean Difference (IV, Random, 95% CI) | 10.77 [4.36, 17.18] |
| Analysis 1.10  Comparison 1 Music therapy versus control, Outcome 10 Gait cadence ‐ music type. | ||||
| 10.1 Music | 4 | 148 | Mean Difference (IV, Random, 95% CI) | 11.34 [‐1.05, 23.74] |
| 10.2 Auditory stimulus (no music) | 3 | 75 | Mean Difference (IV, Random, 95% CI) | 7.58 [4.33, 10.83] |
| 11 Stride symmetry Show forest plot | 3 | 139 | Std. Mean Difference (IV, Random, 95% CI) | 0.94 [‐0.32, 2.20] |
| Analysis 1.11  Comparison 1 Music therapy versus control, Outcome 11 Stride symmetry. | ||||
| 12 General gait Show forest plot | 2 | 48 | Mean Difference (IV, Random, 95% CI) | 7.67 [5.67, 9.67] |
| Analysis 1.12 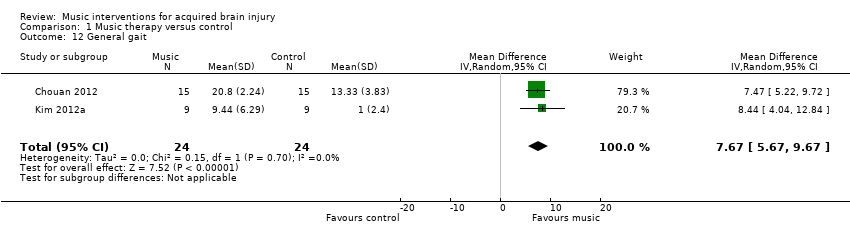 Comparison 1 Music therapy versus control, Outcome 12 General gait. | ||||
| 13 Balance Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.13  Comparison 1 Music therapy versus control, Outcome 13 Balance. | ||||
| 13.1 All studies | 3 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.48, 1.09] |
| 13.2 Adequate randomisation | 2 | 34 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐1.10, 1.37] |
| 14 Upper extremity functioning (general) Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.14 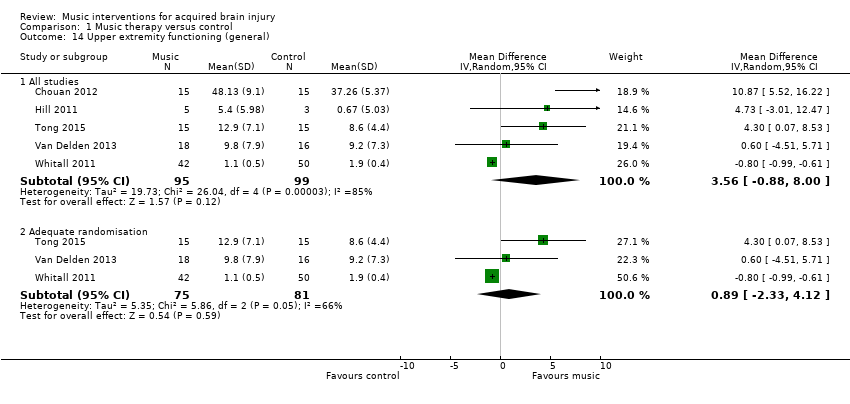 Comparison 1 Music therapy versus control, Outcome 14 Upper extremity functioning (general). | ||||
| 14.1 All studies | 5 | 194 | Mean Difference (IV, Random, 95% CI) | 3.56 [‐0.88, 8.00] |
| 14.2 Adequate randomisation | 3 | 156 | Mean Difference (IV, Random, 95% CI) | 0.89 [‐2.33, 4.12] |
| 15 Upper extremity functioning ‐ time Show forest plot | 2 | 122 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.69, ‐0.47] |
| Analysis 1.15  Comparison 1 Music therapy versus control, Outcome 15 Upper extremity functioning ‐ time. | ||||
| 16 Range of motion ‐ shoulder flexion Show forest plot | 2 | 53 | Mean Difference (IV, Random, 95% CI) | 9.81 [‐12.71, 32.33] |
| Analysis 1.16 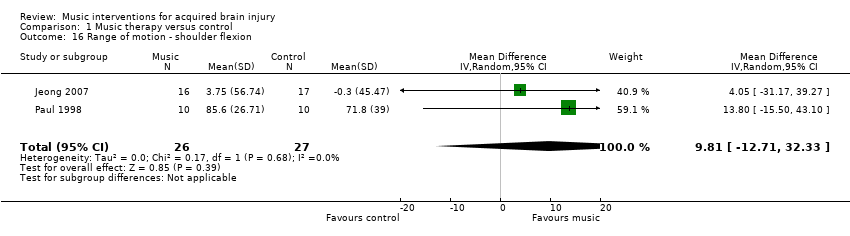 Comparison 1 Music therapy versus control, Outcome 16 Range of motion ‐ shoulder flexion. | ||||
| 17 Hand function Show forest plot | 2 | 113 | Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.91, 1.54] |
| Analysis 1.17  Comparison 1 Music therapy versus control, Outcome 17 Hand function. | ||||
| 18 Upper limb strength Show forest plot | 2 | 113 | Mean Difference (IV, Random, 95% CI) | 6.03 [‐2.52, 14.59] |
| Analysis 1.18 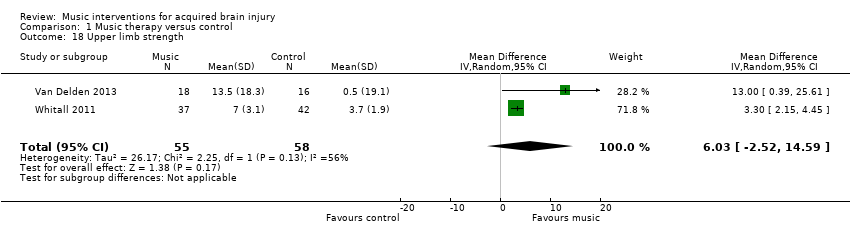 Comparison 1 Music therapy versus control, Outcome 18 Upper limb strength. | ||||
| 19 Manual dexterity Show forest plot | 2 | 74 | Mean Difference (IV, Random, 95% CI) | 0.47 [‐1.08, 2.01] |
| Analysis 1.19  Comparison 1 Music therapy versus control, Outcome 19 Manual dexterity. | ||||
| 20 Overall communication Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.20 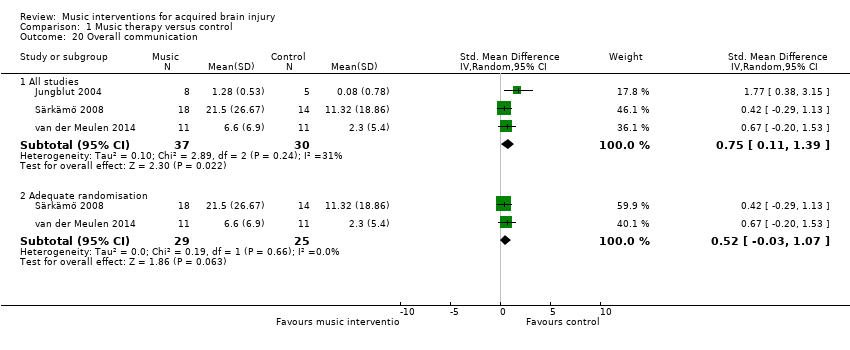 Comparison 1 Music therapy versus control, Outcome 20 Overall communication. | ||||
| 20.1 All studies | 3 | 67 | Std. Mean Difference (IV, Random, 95% CI) | 0.75 [0.11, 1.39] |
| 20.2 Adequate randomisation | 2 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 0.52 [‐0.03, 1.07] |
| 21 Naming Show forest plot | 2 | 35 | Mean Difference (IV, Random, 95% CI) | 9.79 [1.37, 18.21] |
| Analysis 1.21  Comparison 1 Music therapy versus control, Outcome 21 Naming. | ||||
| 22 Repetition Show forest plot | 2 | 35 | Mean Difference (IV, Random, 95% CI) | 8.90 [3.25, 14.55] |
| Analysis 1.22 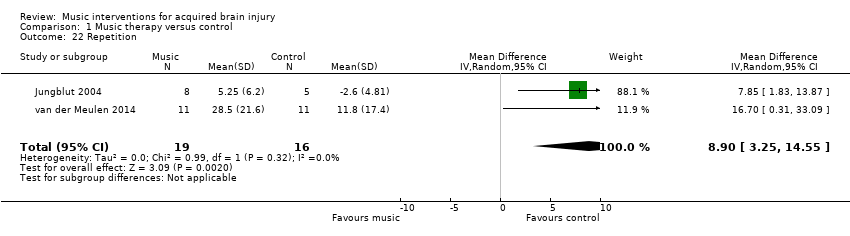 Comparison 1 Music therapy versus control, Outcome 22 Repetition. | ||||
| 23 Memory Show forest plot | 2 | 42 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [‐0.29, 0.95] |
| Analysis 1.23 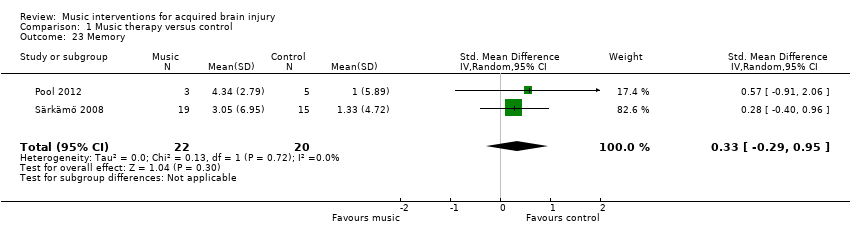 Comparison 1 Music therapy versus control, Outcome 23 Memory. | ||||
| 24 Attention Show forest plot | 2 | 39 | Std. Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.34, 0.94] |
| Analysis 1.24  Comparison 1 Music therapy versus control, Outcome 24 Attention. | ||||
| 25 Quality of life Show forest plot | 2 | 53 | Std. Mean Difference (IV, Random, 95% CI) | 0.89 [0.32, 1.46] |
| Analysis 1.25 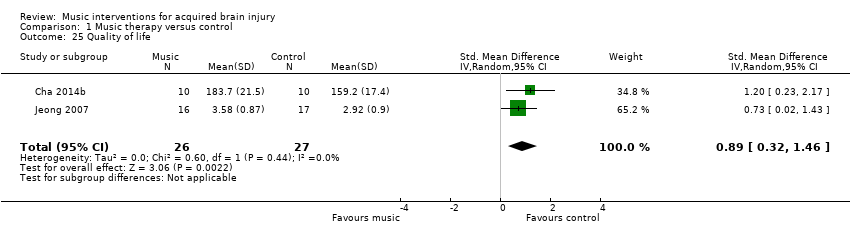 Comparison 1 Music therapy versus control, Outcome 25 Quality of life. | ||||
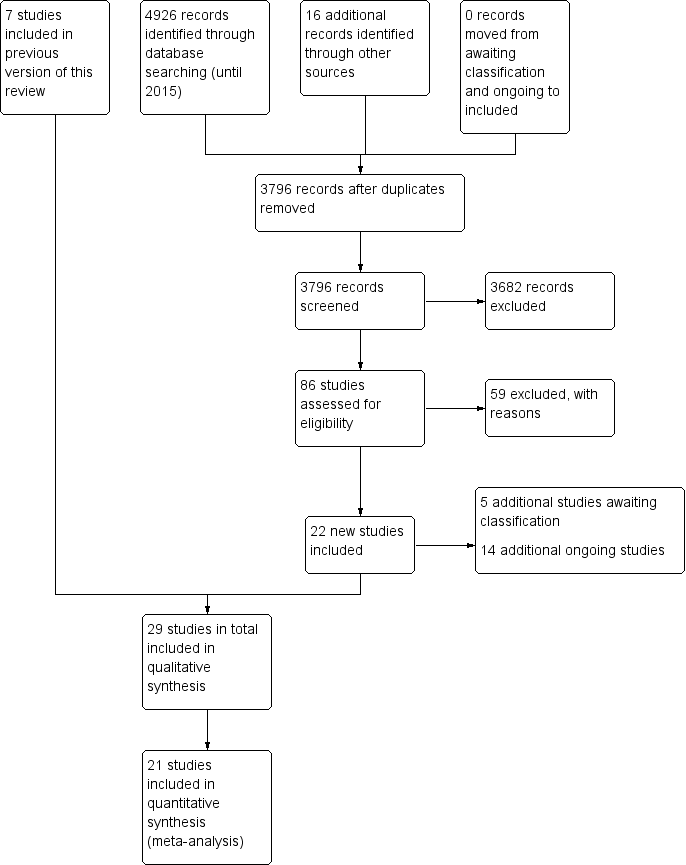
Study flow diagram for the updated review.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
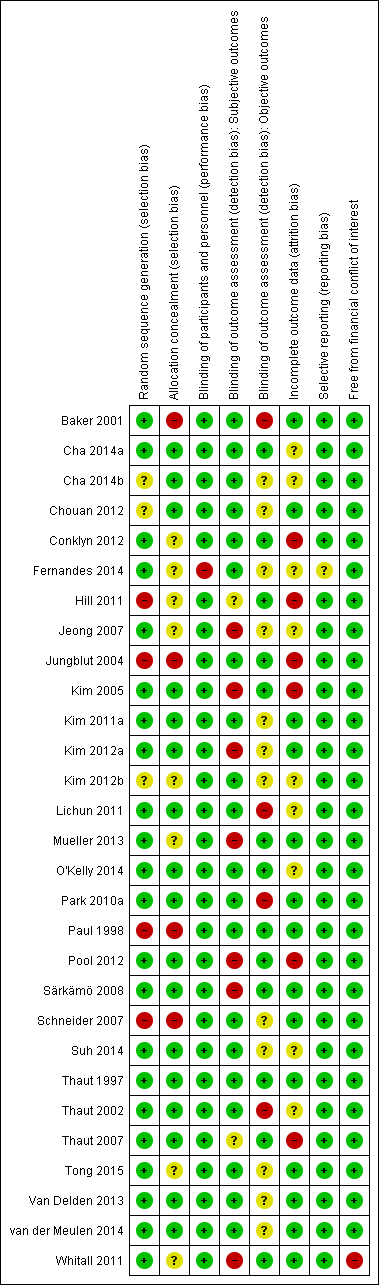
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
![Funnel plot of comparison: 1 Music therapy versus control, outcome: 1.1 Gait velocity [metres/min].](/es/cdsr/doi/10.1002/14651858.CD006787.pub3/media/CDSR/CD006787/image_n/nCD006787-AFig-FIG04.png)
Funnel plot of comparison: 1 Music therapy versus control, outcome: 1.1 Gait velocity [metres/min].

Comparison 1 Music therapy versus control, Outcome 1 Gait velocity.

Comparison 1 Music therapy versus control, Outcome 2 Gait velocity ‐ interventionist.

Comparison 1 Music therapy versus control, Outcome 3 Gait velocity ‐ music type.

Comparison 1 Music therapy versus control, Outcome 4 Stride length (affected side).

Comparison 1 Music therapy versus control, Outcome 5 Stride length (affected side) ‐ music type.
![Comparison 1 Music therapy versus control, Outcome 6 Stride length (unaffected side) [metres].](/es/cdsr/doi/10.1002/14651858.CD006787.pub3/media/CDSR/CD006787/image_n/nCD006787-CMP-001-06.png)
Comparison 1 Music therapy versus control, Outcome 6 Stride length (unaffected side) [metres].
![Comparison 1 Music therapy versus control, Outcome 7 Stride length (unspecified) [metres].](/es/cdsr/doi/10.1002/14651858.CD006787.pub3/media/CDSR/CD006787/image_n/nCD006787-CMP-001-07.png)
Comparison 1 Music therapy versus control, Outcome 7 Stride length (unspecified) [metres].
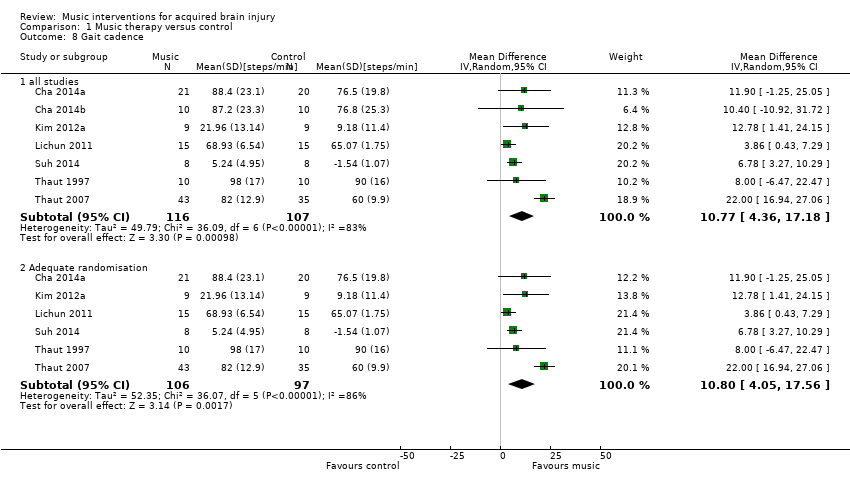
Comparison 1 Music therapy versus control, Outcome 8 Gait cadence.

Comparison 1 Music therapy versus control, Outcome 9 Gait cadence ‐ interventionist.

Comparison 1 Music therapy versus control, Outcome 10 Gait cadence ‐ music type.
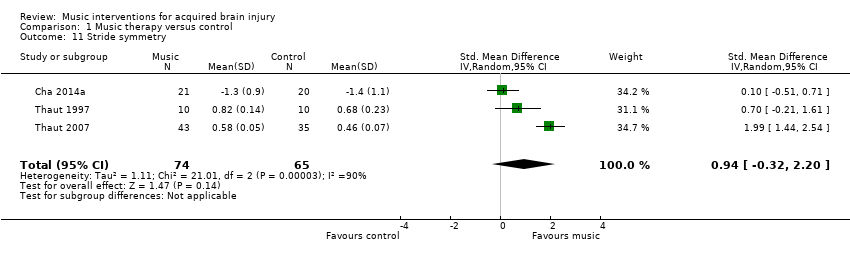
Comparison 1 Music therapy versus control, Outcome 11 Stride symmetry.
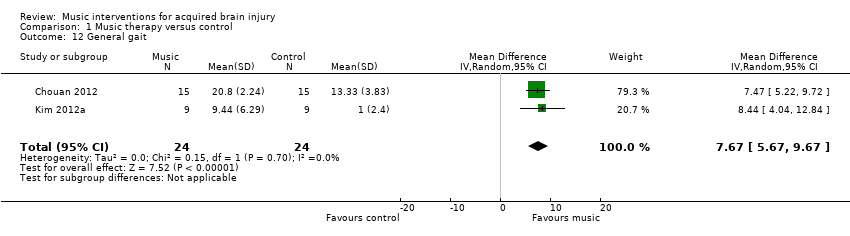
Comparison 1 Music therapy versus control, Outcome 12 General gait.

Comparison 1 Music therapy versus control, Outcome 13 Balance.

Comparison 1 Music therapy versus control, Outcome 14 Upper extremity functioning (general).
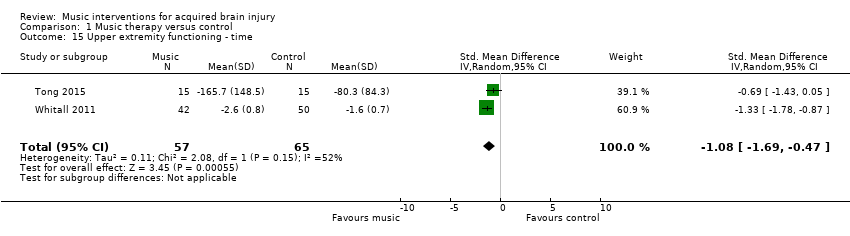
Comparison 1 Music therapy versus control, Outcome 15 Upper extremity functioning ‐ time.
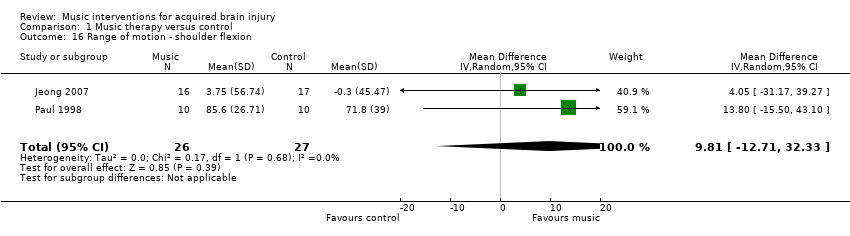
Comparison 1 Music therapy versus control, Outcome 16 Range of motion ‐ shoulder flexion.
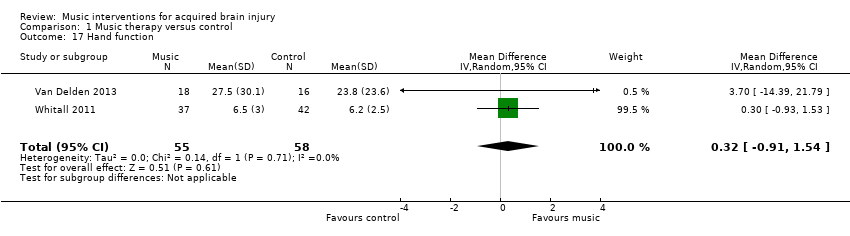
Comparison 1 Music therapy versus control, Outcome 17 Hand function.
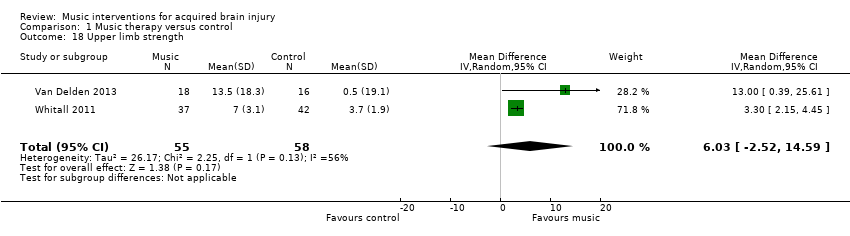
Comparison 1 Music therapy versus control, Outcome 18 Upper limb strength.
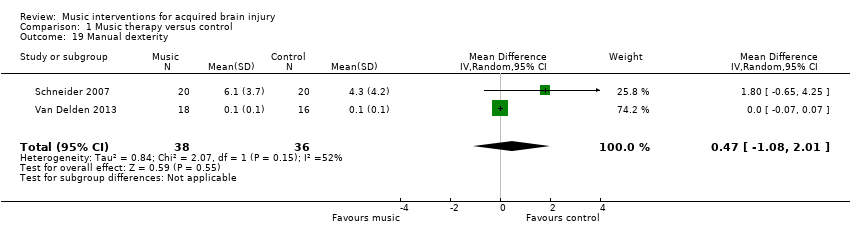
Comparison 1 Music therapy versus control, Outcome 19 Manual dexterity.
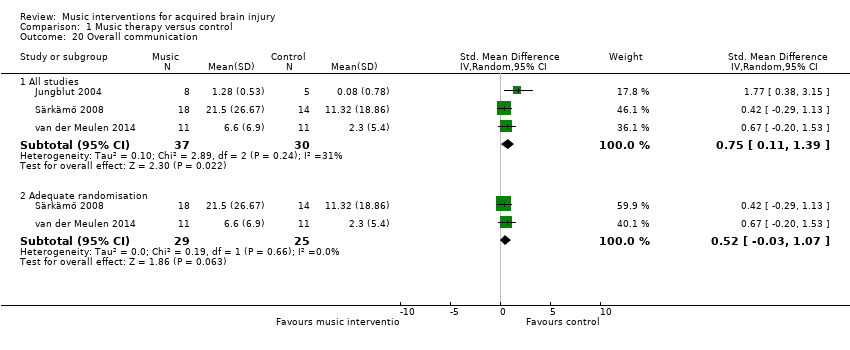
Comparison 1 Music therapy versus control, Outcome 20 Overall communication.
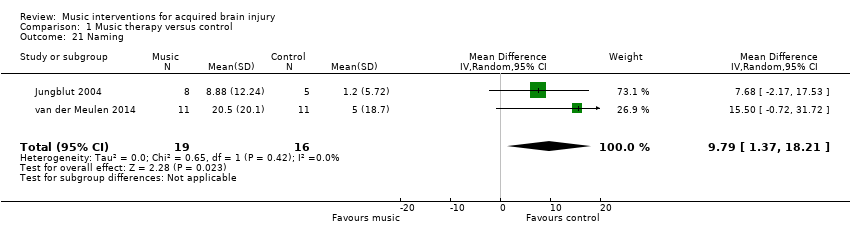
Comparison 1 Music therapy versus control, Outcome 21 Naming.
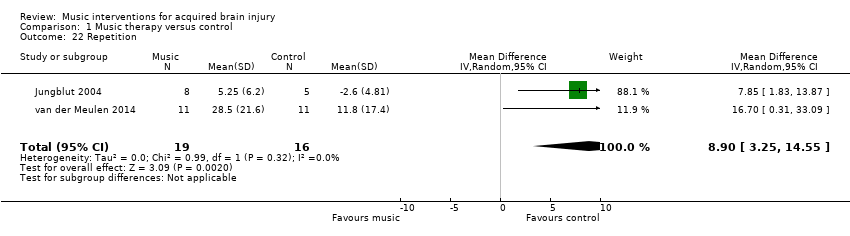
Comparison 1 Music therapy versus control, Outcome 22 Repetition.

Comparison 1 Music therapy versus control, Outcome 23 Memory.

Comparison 1 Music therapy versus control, Outcome 24 Attention.
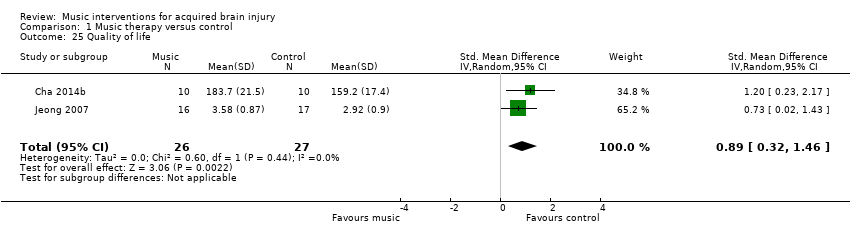
Comparison 1 Music therapy versus control, Outcome 25 Quality of life.
| Music compared with standard care for acquired brain injury | |||
| Patient or population: acquired brain injury | |||
| Outcomes | Relative effect | No of participants | Quality of the evidence |
| Gait velocity | The mean gait velocity in the intervention group was 11.34 metres more (8.4 more to 14.28 more). | 268 | ⊕⊕⊕⊝ |
| Stride length (affected side) | The mean stride length (affected side) in the intervention group was 0.12 metres more (0.04 more to 0.2 more). | 129 | ⊕⊕⊕⊝ |
| Gait cadence | The mean gait cadence in the intervention group was 10.77 steps/minute more (4.36 more to 17.18 more). | 223 | ⊕⊕⊝⊝ |
| Stride symmetry | The mean stride symmetry in the intervention group was 0.94 standard deviations more (0.32 fewer to 2.2 more). | 139 | ⊕⊕⊝⊝ |
| General upper extremity functioning assessed with: Fugl‐Meyer Assessment | The mean general upper extremity functioning in the intervention group was 3.56 units higher (0.88 lower to 8 higher). | 194 | ⊕⊝⊝⊝ |
| Overall communication | The mean overall communication in the intervention group was 0.75 standard deviations more (0.11 more to 1.39 more). | 67 | ⊕⊝⊝⊝ |
| Quality of life assessed with: Stroke Specific Quality of Life Scale | The mean quality of life in the intervention group was 0.89 standard deviations more (0.32 more to 1.46 more). | 53 | ⊕⊕⊝⊝ |
| CI: confidence interval; RCT: randomised controlled trial | |||
| GRADE Working Group grades of evidence | |||
| 1Most studies were rated as at unclear or high risk of bias | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gait velocity Show forest plot | 9 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 All studies | 9 | 268 | Mean Difference (IV, Random, 95% CI) | 11.34 [8.40, 14.28] |
| 1.2 Adequate randomisation | 7 | 228 | Mean Difference (IV, Random, 95% CI) | 10.79 [7.23, 14.35] |
| 2 Gait velocity ‐ interventionist Show forest plot | 9 | 268 | Mean Difference (IV, Random, 95% CI) | 11.34 [8.40, 14.28] |
| 2.1 Music therapist | 3 | 128 | Mean Difference (IV, Random, 95% CI) | 14.76 [13.84, 15.69] |
| 2.2 Non‐music therapist | 6 | 140 | Mean Difference (IV, Random, 95% CI) | 8.48 [5.16, 11.80] |
| 3 Gait velocity ‐ music type Show forest plot | 9 | 268 | Mean Difference (IV, Random, 95% CI) | 11.34 [8.40, 14.28] |
| 3.1 Music | 5 | 173 | Mean Difference (IV, Random, 95% CI) | 14.69 [13.77, 15.61] |
| 3.2 Auditory stimulation (no music) | 4 | 95 | Mean Difference (IV, Random, 95% CI) | 7.70 [3.03, 12.38] |
| 4 Stride length (affected side) Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 All studies | 5 | 129 | Mean Difference (IV, Random, 95% CI) | 0.12 [0.04, 0.20] |
| 4.2 Adequate randomisation | 3 | 89 | Mean Difference (IV, Random, 95% CI) | 0.08 [0.05, 0.11] |
| 5 Stride length (affected side) ‐ music type Show forest plot | 5 | 129 | Mean Difference (IV, Random, 95% CI) | 0.12 [0.04, 0.20] |
| 5.1 Music | 2 | 50 | Mean Difference (IV, Random, 95% CI) | 0.08 [0.05, 0.12] |
| 5.2 Auditory stimulation (no music) | 3 | 79 | Mean Difference (IV, Random, 95% CI) | 0.14 [0.02, 0.25] |
| 6 Stride length (unaffected side) [metres] Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 All studies | 4 | 99 | Mean Difference (IV, Random, 95% CI) | 0.11 [0.01, 0.22] |
| 6.2 Adequate randomisation | 2 | 59 | Mean Difference (IV, Random, 95% CI) | 0.06 [0.01, 0.12] |
| 7 Stride length (unspecified) [metres] Show forest plot | 3 | 186 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.01, 0.33] |
| 8 Gait cadence Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 all studies | 7 | 223 | Mean Difference (IV, Random, 95% CI) | 10.77 [4.36, 17.18] |
| 8.2 Adequate randomisation | 6 | 203 | Mean Difference (IV, Random, 95% CI) | 10.80 [4.05, 17.56] |
| 9 Gait cadence ‐ interventionist Show forest plot | 7 | 223 | Mean Difference (IV, Random, 95% CI) | 10.77 [4.36, 17.18] |
| 9.1 Music therapist | 3 | 128 | Mean Difference (IV, Random, 95% CI) | 11.51 [‐2.57, 25.60] |
| 9.2 Non‐music therapist | 4 | 95 | Mean Difference (IV, Random, 95% CI) | 7.65 [4.43, 10.86] |
| 10 Gait cadence ‐ music type Show forest plot | 7 | 223 | Mean Difference (IV, Random, 95% CI) | 10.77 [4.36, 17.18] |
| 10.1 Music | 4 | 148 | Mean Difference (IV, Random, 95% CI) | 11.34 [‐1.05, 23.74] |
| 10.2 Auditory stimulus (no music) | 3 | 75 | Mean Difference (IV, Random, 95% CI) | 7.58 [4.33, 10.83] |
| 11 Stride symmetry Show forest plot | 3 | 139 | Std. Mean Difference (IV, Random, 95% CI) | 0.94 [‐0.32, 2.20] |
| 12 General gait Show forest plot | 2 | 48 | Mean Difference (IV, Random, 95% CI) | 7.67 [5.67, 9.67] |
| 13 Balance Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 All studies | 3 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.48, 1.09] |
| 13.2 Adequate randomisation | 2 | 34 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐1.10, 1.37] |
| 14 Upper extremity functioning (general) Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 14.1 All studies | 5 | 194 | Mean Difference (IV, Random, 95% CI) | 3.56 [‐0.88, 8.00] |
| 14.2 Adequate randomisation | 3 | 156 | Mean Difference (IV, Random, 95% CI) | 0.89 [‐2.33, 4.12] |
| 15 Upper extremity functioning ‐ time Show forest plot | 2 | 122 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.69, ‐0.47] |
| 16 Range of motion ‐ shoulder flexion Show forest plot | 2 | 53 | Mean Difference (IV, Random, 95% CI) | 9.81 [‐12.71, 32.33] |
| 17 Hand function Show forest plot | 2 | 113 | Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.91, 1.54] |
| 18 Upper limb strength Show forest plot | 2 | 113 | Mean Difference (IV, Random, 95% CI) | 6.03 [‐2.52, 14.59] |
| 19 Manual dexterity Show forest plot | 2 | 74 | Mean Difference (IV, Random, 95% CI) | 0.47 [‐1.08, 2.01] |
| 20 Overall communication Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 20.1 All studies | 3 | 67 | Std. Mean Difference (IV, Random, 95% CI) | 0.75 [0.11, 1.39] |
| 20.2 Adequate randomisation | 2 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 0.52 [‐0.03, 1.07] |
| 21 Naming Show forest plot | 2 | 35 | Mean Difference (IV, Random, 95% CI) | 9.79 [1.37, 18.21] |
| 22 Repetition Show forest plot | 2 | 35 | Mean Difference (IV, Random, 95% CI) | 8.90 [3.25, 14.55] |
| 23 Memory Show forest plot | 2 | 42 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [‐0.29, 0.95] |
| 24 Attention Show forest plot | 2 | 39 | Std. Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.34, 0.94] |
| 25 Quality of life Show forest plot | 2 | 53 | Std. Mean Difference (IV, Random, 95% CI) | 0.89 [0.32, 1.46] |

