Cirugía de cataratas en pacientes con degeneración macular asociada a la edad
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Study design: parallel‐group RCT Number randomized: 54 participants (54 study eyes); 28 in immediate‐surgery group and 26 in delayed‐surgery group Unit of analysis: the individual (1 study eye per individual) Number analyzed: 49 participants completed the study; 27 in immediate‐surgery group and 22 in delayed‐surgery group Exclusions and loss to follow‐up: 5 lost to follow‐up (3 showed asymptomatic, occult CNV) Study follow‐up: 12 months | |
| Participants | Country: Austria Mean age: 80 years (range not reported) Gender: 12 men (24%) and 37 women (76%) Inclusion criteria: 18 years or older; cataract and non‐exudative AMD Exclusion criteria: retinal pathologies other than AMD; exudative AMD; progressive glaucoma; myopia > 10 diopters; panretinal laser treatment; former cataract or vitreoretinal surgery | |
| Interventions | Immediate surgery (n = 28): early cataract surgery Delayed surgery (n = 26): cataract surgery delayed 6 months General procedures: "standard small‐incision cataract surgery with intraocular lens implantation in the capsular bag under peribulbar anesthesia was performed. Ultraviolet radiation‐blocking acrylic lens material without blue light‐blocking components was used." | |
| Outcomes | Primary outcome, as defined in trial registry record: "AMD size (defined central region of interest)" at 6 months, "to evaluate AMD size progression, absolute and relative differences in pixels of the ROI were calculated by equivalent tests" Primary outcome, as defined in journal publication: "CDGAS [cumulated drusen or geographic atrophy area size] as primary outcome measure was determined by digitized color fundus photographs" Secondary outcome measures, as defined in trial registry record: functional ophthalmic assessments at 6 months, "cataract grade (LOCS‐III), visual acuity (distance/near), contrast acuity tests, Visual Function Index (VF‐14)" Secondary outcome measures, as defined in journal publication: "secondary outcome measures such as sex, age, cardiovascular risk factors, cataract grade (LOCS‐III charts), retinal fluorescein angiography (FLA), OCT scans, distance acuity (ETDRS charts), near acuity (Radner charts), contrast sensitivity (Pelli‐Robson charts), and patient’s subjective visual function (VF‐14 questionnaires) were assessed in all patients." Measurements taken: at baseline and 1, 6, and 12 months | |
| Notes | Study dates: January 2002 to July 2010 Trial registration: NCT01165801 Funding source(s): Scientific Fund of the Mayor of Vienna, Austria; "The authors have no conflicts of interest to declare and have no proprietary or commercial interest in any of the materials discussed in this article" Study name: ECAM–1 (Extracapsular Cataract surgery in Age‐related Macular degeneration) or EKAM‐1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "All 54 eyes were randomized into an early surgery group (ES = 28) with immediate cataract surgery and a control group (CO = 26) where surgery was performed after 6 months. Randomization was performed after baseline characteristics following fixed factors" |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment before randomization not reported |
| Masking of study personnel (performance bias) | Unclear risk | Surgeons and participants could not be masked. Masking of other study personnel not reported |
| Masking of outcome assessment (detection bias) | Unclear risk | "Consecutively, the slides were sent to an outside grading center, blinded for all other patient data." Participants were not masked when completing visual function questionnaires. Those refracting participants and evaluating visual acuity may or may not have known at 6 months whether surgery was performed. |
| Incomplete outcome data (attrition bias) | Unclear risk | 5 participants, 1 in the immediate‐surgery group and 4 in the delayed‐surgery group, were not included in the analysis |
| Selective reporting (reporting bias) | Low risk | The outcomes defined at the beginning of the study were all adequately reported |
| Other bias | Low risk | Study appeared to be well designed |
| Methods | Study design: parallel‐group RCT Number randomized: 68 eligible eyes; 60 participants (60 study eyes); 29 in immediate‐surgery group and 31 in delayed‐surgery group Unit of analysis: the individual (1 study eye per individual) Number analyzed: 56 participants completed the study; 27 in immediate‐surgery group and 29 in delayed‐surgery group Exclusions and loss to follow‐up: 4 lost to follow‐up, 2 from each group (1 died, 2 emigrated, and 1 refused follow‐up) Study follow‐up: 6 months | |
| Participants | Country: Australia Mean age: 78.9 years (range 67 to 92) Gender: 23 men (38%) and 37 women (62%) Inclusion criteria: 50 years or older; visually significant cataract and either bilateral AREDS category 3 AMD or 1 eye with advanced AMD and the second eye with AREDS category 2 or 3 Exclusion criteria: cataract too dense for clinical and angiographic evaluation, end‐stage AMD in study eye, fluorescein allergy, high myopia (greater than 8 diopter sphere), diabetic retinopathy, intermediate or posterior intraocular inflammatory disease, previous retinal laser treatment, or presence of another CNV‐associated disease | |
| Interventions | Immediate surgery (n = 29): cataract surgery within 2 weeks Delayed surgery (n = 31): cataract surgery delayed 6 months General procedures: "The baseline assessments involved detailed demographic and medical history; best‐corrected distance visual acuity (VA); contrast sensitivity; Impact of Vision Impairment (IVI) questionnaire; lens photography; laser retinometry; color fundus photography; and fundus fluorescein angiography (FFA) ... . The 6‐month follow‐up assessment followed a similar protocol, omitting lens photography and laser retinometry." All participants underwent phacoemulsification, however no details about the actual cataract surgery were reported. | |
| Outcomes | Outcomes as reported:
Measurements taken: at baseline and 6 months Primary and secondary outcomes were not clearly stated; one would expect visual acuity to improve more in participants with immediate surgery than in those awaiting surgery for visually significant cataract at 6 months. | |
| Notes | Study dates: not reported Trial registration: not reported Funding source(s): Leon Mow Foundation, Centre for Eye Research, Australia; National Health and Medical Research Council Public Health Fellowship and Medical Research Council, Australia; and Royal Victorian Eye and Ear Hospital Wagstaff Fellowship | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "All study participants had a baseline assessment performed and were then randomized to either a ‘treatment’ group, who underwent immediate (within 2 weeks) cataract extraction, or a ‘control’ group, who were randomized to deferred surgery after the 6‐month follow‐up visit." |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment before randomization not reported |
| Masking of study personnel (performance bias) | Unclear risk | Surgeons and participants could not be masked. Masking of other study personnel not reported. |
| Masking of outcome assessment (detection bias) | Unclear risk | "All examiners were masked to the randomization of the two groups." Participants were not masked when completing IVI questionnaires. Unknonwn whether those refracting participants and measuring visual acuity knew at 6 months whether surgery had been performed. |
| Incomplete outcome data (attrition bias) | Unclear risk | 4 participants, 2 from each group, were not included in the analysis |
| Selective reporting (reporting bias) | Low risk | The outcomes defined at the beginning of the study were all adequately reported |
| Other bias | Low risk | Study appeared to be well designed |
AMD: age‐related macular degeneration
AREDS: Age‐Related Eye Disease Study
CNV: choroidal neovascularization
ETDRS: Early Treatment Diabetic Retinopathy Study
LOCS‐III: Lens Opacities Classification System III
OCT: optical coherence tomography
RCT: randomized controlled trial
ROI: region of interest
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Review article about AMD and did not discuss cataract surgery | |
| Prospective cohort study comprised of (1) people with AMD who did not have surgery, (2) people with AMD who underwent cataract surgery, and (3) a control group of people without AMD who underwent cataract surgery | |
| Prospective cohort study comprised of (1) people with AMD scheduled to have cataract surgery and (2) a control group of people with AMD not having cataract surgery | |
| Commentary on the Age‐Related Eye Disease Study (AREDS). The AREDS itself was not included as it was not a randomized trial of cataract surgery in people with AMD; participants in AREDS were randomized to antioxidant or zinc supplements or both versus placebo | |
| Editorial on the treatment of AMD | |
| Case series of people undergoing cataract surgery | |
| Prospective cohort study of people undergoing cataract surgery, with and without AMD | |
| Observational study of eyes with AMD that had cataract surgery compared to fellow eyes that did not have surgery | |
| Observational study of people with AMD after cataract surgery in 1st eye, then 2nd eye | |
| Study was not limited to people with AMD | |
| Prospective cohort of people with advanced AMD versus those with moderate AMD; there was no comparison of cataract surgery versus no cataract surgery | |
| Retrospective case series of people over age 90; not all people had AMD | |
| Observational, cross‐sectional study; all included participants had cataract surgery | |
| Cross‐sectional study of cataract surgery. Although a subgroup of cataract surgery participants with AMD was noted, no comparison was made to people with AMD who did not have surgery. |
AMD: age‐related macular degeneration
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mean best‐corrected visual acuity Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1 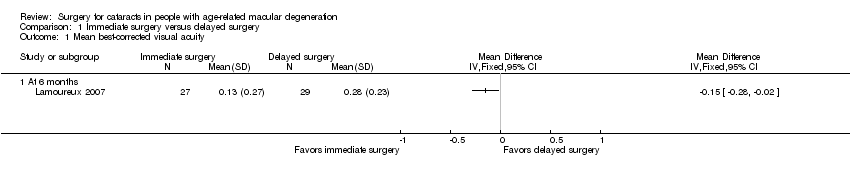 Comparison 1 Immediate surgery versus delayed surgery, Outcome 1 Mean best‐corrected visual acuity. | ||||
| 1.1 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Mean change in cumulative drusen and geographic atrophy size at 12 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Immediate surgery versus delayed surgery, Outcome 2 Mean change in cumulative drusen and geographic atrophy size at 12 months. | ||||
| 3 Development of choroidal neovascularization at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3 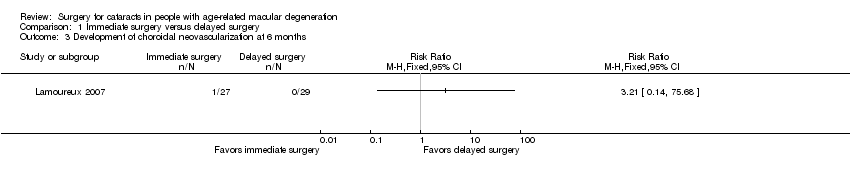 Comparison 1 Immediate surgery versus delayed surgery, Outcome 3 Development of choroidal neovascularization at 6 months. | ||||
| 4 Quality of life scores Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4 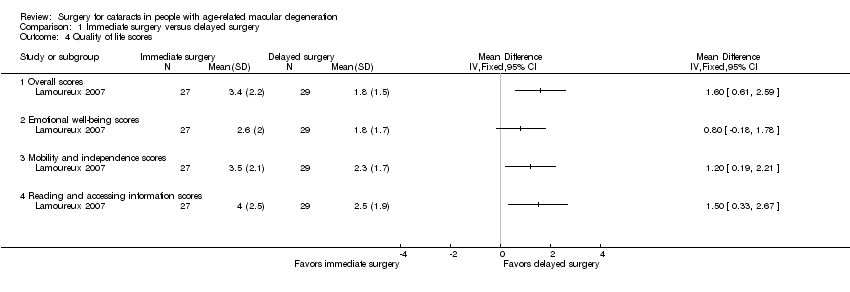 Comparison 1 Immediate surgery versus delayed surgery, Outcome 4 Quality of life scores. | ||||
| 4.1 Overall scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Emotional well‐being scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Mobility and independence scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Reading and accessing information scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
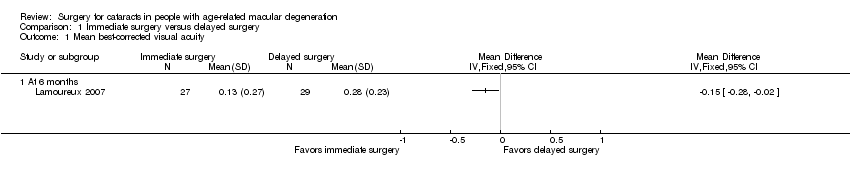
Comparison 1 Immediate surgery versus delayed surgery, Outcome 1 Mean best‐corrected visual acuity.

Comparison 1 Immediate surgery versus delayed surgery, Outcome 2 Mean change in cumulative drusen and geographic atrophy size at 12 months.
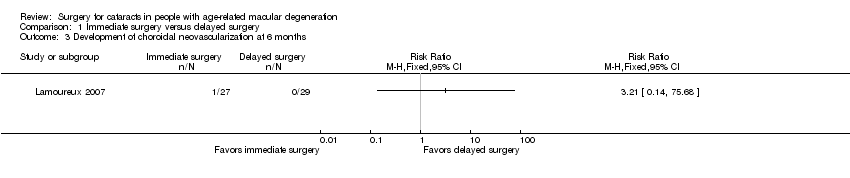
Comparison 1 Immediate surgery versus delayed surgery, Outcome 3 Development of choroidal neovascularization at 6 months.

Comparison 1 Immediate surgery versus delayed surgery, Outcome 4 Quality of life scores.
| Immediate cataract surgery compared with delayed cataract surgery in eyes with age‐related macular degeneration | ||||||
| Population: people with cataract and age‐related macular degeneration Settings: ophthalmology clinics Intervention: immediate cataract surgery (within 2 weeks) Comparison: delayed cataract surgery (after 6 months) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed cataract surgery | Immediate cataract surgery | |||||
| Mean best‐corrected visual acuity (BCVA) (measured on the LogMAR scale; 0 = good vision, higher scores = worse vision) | At 6 months' follow‐up | — | 56 | ⊕⊕⊕⊝ | Neither trial reported visual acuity outcomes as dichotomous or categorical outcomes. At 12 months, 1 trial reported mean distance visual acuity, but the unit of measure was not reported. | |
| Mean BCVA in the delayed‐cataract surgery group was 0.28 LogMAR units. | Mean BCVA in the immediate‐cataract surgery group was 0.15 LogMAR units lower (better) (0.28 lower to 0.02 lower). | |||||
| At 12 months' follow‐up | ||||||
| See comment | ||||||
| Mean change in cumulated drusen or geographic atrophy area size (CDGAS) | At 6 months' follow‐up | 1 trial did not report any outcome related to drusen or geographic atrophy. | ||||
| Not reported | ||||||
| At 12 months' follow‐up | — | 49 | ⊕⊕⊝⊝ | |||
| The mean change in CDGAS in the delayed‐cataract surgery group was ‐1.125 CDGAS units. | The mean change in CDGAS in the immediate‐cataract surgery group was 0.76 CDGAS units higher (8.49 lower to 10.00 higher). | |||||
| Development of choroidal neovascularization | At 6 months' follow‐up | RR 3.21 (0.14 to 75.68) | 56 | ⊕⊝⊝⊝ | At 6 months, none of 29 participants in the delayed‐cataract surgery group compared with 1 of 27 participants in the immediate‐cataract surgery group developed choroidal neovascularization. The other trial reported that no participant in either group developed exudative AMD up to 12 months' follow‐up. | |
| Not estimated (see comment) | ||||||
| At 12 months' follow‐up | ||||||
| See comment | ||||||
| Quality of life (measured by the Impact of Vision Impairment questionnaire; higher mean scores represent better quality of life in the analyses, scale of 0 to 5) | At 6 months' follow‐up | — | 56 | ⊕⊕⊝⊝ | The other trial measured quality of life using the Visual Function‐14 questionnaire to assess patient satisfaction at baseline and 12 months' follow‐up; however, no between‐group analysis of results could be performed. | |
| Mean overall score in the delayed‐cataract surgery group was 1.8. | Mean overall score in the immediate‐cataract surgery group was 1.60 higher (0.61 to 2.59 higher). | |||||
| At 12 months' follow‐up | ||||||
| See comment | ||||||
| Complications | Not reported | |||||
| *The basis for the assumed risk is the risk in the control group. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the control group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded (‐1) for unclear risks of bias such as selection bias (methods of randomization and allocation concealment not reported), performance and detection bias (effect of lack of masking on outcome unclear), and attrition bias (nine of 114 participants not included in analyses). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mean best‐corrected visual acuity Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Mean change in cumulative drusen and geographic atrophy size at 12 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Development of choroidal neovascularization at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Quality of life scores Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Overall scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Emotional well‐being scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Mobility and independence scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Reading and accessing information scores | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

