Guía ecográfica para el bloqueo del miembro superior e inferior
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT, parallel design | |
| Participants | 120 (ASA I ‐ III) participants scheduled for elbow, forearm, wrist, hand surgery Excluded: Pregnant women, patients < 18 yrs, those with contraindication to RA, such as known allergic reaction to LA, local infection at site of puncture and treatment or disease that severely affects coagulation | |
| Interventions | Ultrasound in‐plane (n = 40) versus ultrasound out‐of‐plane (n = 40) versus nerve stimulation (n = 40) Axillary brachial plexus block of 4 nerves (median, ulnar, radial, musculocutaneous); each blocked separately with no more than 40 ml in total of 1.5% mepivacaine Ultrasound: 8 ‐ 13 MHz probe (LOGIQe); endpoint ‐ visualisation of proper spread of the local anaesthetic around the targeted nerves. All 4 nerves blocked with 5‐7ml LA each. Neurostimulation: pulse duration of 100 µsec, frequency 1 Hz, initial current 1.5 mA. Nerves were located according to specific motor‐evoked muscular contractions. Current reduced to 0.5 mA. 15 ml of LA for median and radial nerves, and 5 ml for the musculocutaneous nerve. | |
| Outcomes |
| |
| Notes | 4 practitioners described as being experienced in both techniques For the purpose of analysis, we combined the data from the 2 groups ultrasound with in‐plane and ultrasound with out‐plane technique | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sealed envelopes used, but no further details |
| Allocation concealment (selection bias) | Unclear risk | As above |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias):Complications | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Anaesthetist not blinded. |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | Assume assessed by anaesthetist but no details reported |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | Assume assessed by anaesthetist but no details reported |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Assessed by independent observer |
| Blinding of outcome assessment (detection bias): Patient discomfort | Unclear risk | Assessed by independent observer. No details of whether participant is blinded but assume not |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought. Some expected outcomes not effectively reported – success of block, sensory testing |
| Baseline characteristics | Low risk | Largely equivalent. |
| Funding sources | Low risk | None, other departmental funding |
| Operator expertise | Unclear risk | “Four senior anaesthesiologists experienced in both neurostimulation and ultrasound techniques performed the block”. Unknown if experience was equivalent and whether participants stratified by anaesthetist. |
| Methods | RCT, parallel design | |
| Participants | 106 ASA I ‐ III participants scheduled for elbow, forearm, wrist or hand surgery Excluded: age < 18 or > 70 yr, language barrier, contraindication(s) to regional anaesthesia, weight > 100 kg, pre‐existing neurological deficit in the distribution to be anaesthetized, local infection, coagulopathy, chest or shoulder deformities, severe respiratory disease, or clavicle fracture. | |
| Interventions | Ultrasound (n = 53) versus nerve stimulation (n = 53) Intraclavicular brachial plexus block of radial, ulnar, median and musculocutaneous nerves. Total volume 30 ml local anaesthetic (2% lidocaine 15 mL and 0.5% bupivacaine 15 mL with epinephrine 1:200,000) Ultrasound: either linear probe 7 – 13 MHz (Philips/ATL HDI 5000) a 5 – 12 MHz (Philips HD11); endpoint ‐ visualization of lateral and posterior cord, LA injected incrementally to total volume of 30 ml. Nerve stimulation (Stimuplex): motor endpoints sought (elbow/ finger flexion, thumb opposition, wrist extension) at stimulating current of 0.3 ‐ 0.5 mA. 15 mL of LA injected incrementally at each position for a total of 30 mL. All participants given midazolam 2 – 4 mg iv as premedication. For nerve stimulation group, If 2 motor responses were not elicited within 20 min of needle insertion, procedure abandoned in favour of a different approach to brachial plexus blockade, and participant excluded from analysis. | |
| Outcomes |
| |
| Notes | One of 4 experienced regional anaesthesiologists ‐ no further details of whether experience is balanced between techniques Supported by grant funding, equipment received from manufacturers for purpose of study ‐ no interests declared. Time to perform block reported as median (interquartile range) and therefore not possible to combine in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization table |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding of participants and personnel (performance bias):Complications | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Anaesthetist not blinded |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Evaluated by blinded observer |
| Blinding of outcome assessment (detection bias): Complications | Low risk | Evaluated by blinded observer |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Evaluated by blinded observer |
| Blinding of outcome assessment (detection bias): Patient discomfort | Low risk | Participants blinded with use of 'sham' equipment |
| Incomplete outcome data (attrition bias) | Unclear risk | Small number of exclusions (5 participants) with clear reasons given. However, only 49% participants available for assessment of complications at postoperative day 7 |
| Selective reporting (reporting bias) | Unclear risk | No data available for pain on injection. Also published protocol not sought |
| Baseline characteristics | Low risk | Largely comparable, although some differences in types of surgery between groups |
| Funding sources | High risk | Funding from grants, equipment supplied by named manufacturers. Unclear whether any bias has been introduced |
| Operator expertise | Unclear risk | Anaesthetists described as experienced but no detail of whether experience is equivalent for both techniques |
| Methods | RCT, parallel design | |
| Participants | 59 patients, ASA I ‐ III, for scheduled forearm, wrist, or hand surgery | |
| Interventions | Ultrasound (n = 30) versus nerve stimulation (n = 29) Axillary brachial plexus block; 4 nerves located individually in both groups (ulnar, radial, median, musculocutaneous); each nerve blocked with 5 ml 0.75% bupivacaine in both groups | |
| Outcomes |
| |
| Notes | 2 practitioners with "substantial" experience Results for onset time presented in a graph, not possible to extract data for this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | "Sealed envelope technique" ‐ no further details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias):Complications | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Anaesthetist not blinded |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Assessed by blinded observer |
| Blinding of outcome assessment (detection bias): Complications | Low risk | Assessed by blinded observer |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Assessed by blinded observer |
| Blinding of outcome assessment (detection bias): Patient discomfort | High risk | Assessed by blinded observer, but participant aware of group allocation |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Largely equivalent |
| Funding sources | Low risk | From departmental sources only |
| Operator expertise | Unclear risk | Anaesthetists reported as having substantial experience in regional anaesthesia ‐ however, does not specify if experience is equivalent for both techniques. No details of which anaesthetist worked with which group |
| Methods | RCT, parallel design | |
| Participants | 70 participants, ASA I ‐ III scheduled for hallux vagus correction Excluded: patient refusal to procedure, neurologic or neuromuscular disease, acquired or congenital coagulopathy, skin infection at needle insertion site. | |
| Interventions | Ultrasound + nerve stimulation (n = 35) versus nerve stimulation (n = 35) Popliteal block of tibial and peroneal nerve; 20 ml LA (10 mL 0.75% ropivacaine and 10 mL 2% lidocaine without epinephrine) ‐ 12 ml close to tibial nerve, 8 ml close to peroneal nerve Ultrasound: 7.5 ‐ 12 Mhz linear probe; nerve stimulator turned on to confirm correct identification of nerves, then switched off for remaining procedure; endpoint ‐ stimulating current increased to obtain motor response Nerve stimulation (Stimuplex): pulse duration 100 µsec, initial current density 1 mA, frequency 2 Hz; endpoint ‐ stimulation at < 0.4 mA | |
| Outcomes |
| |
| Notes | All participants first given metatarsal osteotomy with ankle tourniquet. Blocks performed by 2 resident anaesthetists with prior experience of regional anaesthesia using nerve stimulator, but novices to ultrasound and to popliteal block | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized using sealed envelopes. No further details given |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetists |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetists |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetists |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Sensory block assessed by a blinded investigator |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Block performance time registered by senior staff not blinded to procedure, but blinded observer monitored onset and progression of sensory block |
| Blinding of outcome assessment (detection bias): Patient discomfort | Unclear risk | Blinded observer collected participant satisfaction levels in post‐op period, but unclear if participant blinded to group allocation |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Largely comparable. More women than men, but expected for this surgery |
| Funding sources | Low risk | No funding |
| Operator expertise | High risk | Anaesthetists had more experience in nerve stimulation use than ultrasound but none had experience of popliteal block |
| Methods | RCT, parallel design | |
| Participants | 188 patients, ASA I ‐ III, scheduled for hand surgery | |
| Interventions | Ultrasound (n = 64) versus ultrasound + nerve stimulation (n = 62) versus nerve stimulation (n = 62) Axillary brachial plexus block; 3 nerves targeted individually in each group (radial, ulnar, median); all groups received 21 ml 2% lidocaine with 1:200,000 epinephrine and 21 ml 0.5% bupivacaine (14 ml around each nerve) Ultrasound: linear 5 ‐ 12 MHz probe (Philips HDI 5000); endpoint ‐ local anaesthetic spread around each nerve | |
| Outcomes |
| |
| Notes | Multiple practitioners ‐ experience in technique not given, although some anaesthetists and some fellow/resident anaesthetists who were supervised Registered in clinicaltrials.gov | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number table |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes, but no further details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Not possible to blind anaesthetist, although use of "sham" equipment in order to ensure participant blinding |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | High risk | Need for rescue block assessed by anaesthetist who was not blinded |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details of who assessed this, possibly anaesthetist |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | Assessed by an independent observer, although unclear whether blinded |
| Blinding of outcome assessment (detection bias): Patient discomfort | Low risk | Assessed during follow‐up telephone conversation ‐ participant blinded to group allocation |
| Incomplete outcome data (attrition bias) | High risk | 30 participants (14%) not included as surgery commenced before 30‐minute assessment. Still possible to collect some outcome data for these participants |
| Selective reporting (reporting bias) | Low risk | Protocol details published in clinicaltrials.gov. NCT 00221884. Outcomes appear to be reported |
| Baseline characteristics | Low risk | Age, gender, weight, height, BMI, surgical time. All comparable |
| Funding sources | High risk | Funding sources reported, to include supply of ultrasound equipment by manufacturers |
| Operator expertise | High risk | Some blocks performed by supervised residents, which would have increased time to perform block and would introduce bias for this outcome |
| Methods | RCT, parallel design | |
| Participants | 40 participants, ASA I ‐ II scheduled for elective hand surgery under brachial plexus block. Excluded: Absolute contraindication of regional block, diabetes mellitus, or any other neurological disorder of the upper extremity | |
| Interventions | Ultrasound (n = 20) versus nerve stimulation (n = 20) Axillary brachial plexus block of radial, ulnar and median nerves; blocked with 40 ml 0.5% ropivacaine Ultrasound: 5 – 10 MHz linear probe (SonoAce 8000 SE); endpoint ‐ LA solution injected around each of the terminal branches of brachial plexus (median, ulnar and radial), 20 ml 0.5% ropivacaine in region of radial nerve, 10 ml ulnar, 10 ml median Nerve stimulation (Stimuplex): motor response to a current < 0.5 mA and > 0.2 mA Participants sedated with propofol TCI 1 ‐ 1.5 ng/ml | |
| Outcomes | 1. Supplementation rate (when 50 ‐ 100 µg fentanyl necessary to guarantee analgesia; or when conversion to GA required) 2. Complications (vascular puncture, paraesthesia) 3. Time to perform block (from palpation of axillary artery/ from transducer placed on the skin) 4. Participant discomfort | |
| Notes | No details given of number of practitioners and their experience | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Electronically‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details of who assessed outcomes |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details of who assessed outcomes |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | No details of who assessed outcomes |
| Blinding of outcome assessment (detection bias): Patient discomfort | Unclear risk | No details of who assessed outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Comparable |
| Funding sources | Low risk | No funding sources reported |
| Operator expertise | Unclear risk | No details given of practitioners and levels of experience |
| Methods | RCT, parallel design | |
| Participants | 50 participants, ASA I ‐ III, scheduled for elective coracoacromial ligament repair Excluded: < 18 yrs, > 85 yrs, unable to express informed consent, with known allergy to study medications, chronic opioid use, ipsilateral upper limb neurological deficits, or contraindications to continuous block placement | |
| Interventions | Ultrasound versus nerve stimulation. Interscalene brachial plexus block for nerve roots of brachial plexus; blocked with 20 ml 1% lidocaine Ultrasound: 10 – 12 MHz linear probe (LOGIQ E), in‐plane approach; endpoint ‐ direct visualization of LA spread around nerve roots. Catheter inserted after injection of LA Nerve stimulation: pulse duration 0.2 ms, initial current 1 mA, frequency 2 Hz; endpoint ‐ stimulation of deltoid muscle motor responses at 0.5 mA. Stimulating perineural catheter was then inserted through the needle and advanced to maintain the adequate motor response at ≤ 0.4 mA. LA injected in increments | |
| Outcomes |
| |
| Notes | 2 practitioners experienced in both techniques Registered in clinicaltrials.gov No numerical data presented for supplementation rate ‐ "There were no differences in the...requirements for GA" No denominator figures provided. Email request sent to authors, but as yet no reply. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence of random numbers |
| Allocation concealment (selection bias) | Unclear risk | “sealed envelope technique” but no further details given |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details of who assessed this outcome |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details of who assessed this outcome |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | Some outcomes recorded by a nurse, but no details as to whether nurse was blinded |
| Blinding of outcome assessment (detection bias): Patient discomfort | Unclear risk | No details of whether participant blinded to group allocation |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Low risk | Protocol details published in clinicaltrials.gov. NCT 00702416. Outcomes appear to be reported |
| Baseline characteristics | Low risk | Comparable |
| Funding sources | Low risk | None apparent |
| Operator expertise | Unclear risk | Only 2 practitioners, both experienced in both techniques |
| Methods | RCT, parallel design | |
| Participants | 67 participants, ASA I ‐ III, for elective hand surgery | |
| Interventions | Continous infraclavicular block (catheter) with ultrasound guidance + nerve stimulation (n = 23) versus nerve stimulation (catheter not stimulated) (n = 22) versus nerve stimulation with stimulation of catheter (n = 22) Ultrasound: 5 ‐ 10 MHz linear probe (Sonosite titan); position confirmed with nerve stimulation and agitated dextrose; catheter position confirmed visually with agitated dextrose | |
| Outcomes |
| |
| Notes | For analysis, we combined the 2 nerve stimulation groups and compared them against the ultrasound group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given |
| Allocation concealment (selection bias) | Unclear risk | Closed envelopes used; no further details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | High risk | Outcome assessment not blinded “the same anesthesiologist performed and evaluated |
| Blinding of outcome assessment (detection bias): Complications | High risk | Outcome assessment not blinded “the same anesthesiologist performed and evaluated |
| Blinding of outcome assessment (detection bias): time outcomes | High risk | Outcome assessment not blinded “the same anesthesiologist performed and evaluated |
| Incomplete outcome data (attrition bias) | Low risk | 2 participants excluded from analysis and details given. Low attrition rate |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Unclear risk | Age, height, weight, gender, ASA status. Significantly older participants in group with nerve stimulator with stimulating catheter. |
| Funding sources | Low risk | None apparent |
| Operator expertise | Unclear risk | No details |
| Methods | RCT, parallel design | |
| Participants | 61 patients, ASA I ‐ III scheduled foot or ankle surgery | |
| Interventions | Ultrasound + nerve stimulation (n = 30) versus nerve stimulation (n = 31) Midfemoral sciatic nerve block with 35 ml 0.5% ropivacaine in both groups Ultrasound: 7.5 ‐ 11 MHz linear probe (Toshiba Aplio); neurostimulation commenced when needle near nerve; endpoint ‐ neurostimulation at 0.5 mA | |
| Outcomes |
| |
| Notes | 1 radiologist and one anaesthetist for all blocks. Experience in technique not given Additional saphenous nerve block given as required for tourniquet pain Time to perform block and onset time presented as median (range) and therefore not possible to combine in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details of who assessed this outcome |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details of who assessed this outcome |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Quality of nerve block assessed by anaesthetist unaware of group allocation, but no details for other outcomes |
| Blinding of outcome assessment (detection bias): Patient discomfort | Unclear risk | No details |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Unclear risk | Some differences in types of surgery between groups |
| Funding sources | Low risk | No apparent external funding |
| Operator expertise | Unclear risk | Same anaesthetist performed both blocks |
| Methods | RCT, parallel design | |
| Participants | 51 patients, ASA I ‐ II, scheduled for foot surgery Exclusion criteria: type I and type II diabetes; history of abnormal bleeding; laboratory evidence of abnormal coagulation; infection at injection site; central or peripheral neurological disease; muscular disease | |
| Interventions | Ultrasound + nerve stimulation (n = 26) versus nerve stimulation (n = 25) Popliteal sciatic nerve block of tibial and common popliteal nerve with 20 ml 0.5% bupivacaine in both groups (10 ml tibial nerve; 10 ml common popliteal nerve) Ultrasound: 5 ‐ 10 MHz linear probe (GE LOGIQ book); endpoint ‐ neurostimulation < 0.5 mA; spread of local anaesthetic observed but no repositioning of needle to aid spread permitted Neurostimulation: pulse duration 0.1 msec; frequency 1 Hz; starting current 1.5 mA; endpoint‐ stimulation < 0.5 mA | |
| Outcomes |
| |
| Notes | Participants withdrawn from study if block not completed within 7 min Additional saphenous nerve block performed to prevent tourniquet pain 1 practitioner performed all US blocks while another performed all control blocks | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Evaluation of block by independent blinded observer |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details of who assessed complications at consultation 2 ‐ 4 weeks post‐surgery |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Evaluation of sensory nerve block done by independent observer |
| Blinding of outcome assessment (detection bias): Patient discomfort | High risk | Participants not blinded to group allocation |
| Incomplete outcome data (attrition bias) | High risk | High number of exclusions, although details provided |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Unclear risk | Some differences in ASA status, with twice as many ASAII participants in ultrasound group |
| Funding sources | Low risk | None apparent |
| Operator expertise | High risk | Different anaesthetists performed each block |
| Methods | RCT, parallel design | |
| Participants | 112 ASA I ‐ II participants scheduled for surgery on distal upper limb Exclusion criteria: poor general health, contraindications to regional anaesthesia | |
| Interventions | Ultrasound (n = 56) versus nerve stimulation (n = 56) Axillary brachial plexus block with single injection 50 ml 1% mepivacaine in both groups Ultrasound: 8 ‐ 13 MHz linear probe (Vivid i, Fa. GE); out‐of‐plane approach; Nerve stimulation (Stimuplex): pulse duration ≥ 0.1 msec; frequency 1 Hz; starting current not stated | |
| Outcomes |
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Use of sealed envelope. No further details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist to procedure technique |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist to procedure technique |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | No details |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Unclear risk | More women than men in the US group, but described as no difference by authors |
| Funding sources | Low risk | Assume none |
| Operator expertise | Unclear risk | No details |
| Methods | RCT, parallel design | |
| Participants | 80 ASA I or II patients, scheduled for hand, wrist and forearm surgery Excluded: Patients who could not co‐operate, those with disease that could prevent sensory block assessment in upper extremity, patients with coagulopathy, allergy to study drugs, known pregnancy or patients whose pervious surgery or trauma prevented anatomic localization of injection point | |
| Interventions | Ultrasound + nerve stimulation (n = 40) versus nerve stimulation (n = 40) Infraclavicular brachial plexus block of median, ulnar and radial nerves with 20 ml levobupivacaine, 5 mg/ml and 20 ml of lidocaine and 20 mg/ml with 5 µg/ml epinephrine (total vol 40 ml) Ultrasound: US probe (GE Logic) (8 ‐ 13 MHz) placed below clavicle about 0.5 ‐ 1 cm inferior to site of needle entry. After identification of axillary artery and cords, stimulating needle was positioned posterior to axillary artery. Electrical stimulator used to obtain motor response distal to elbow (ulnar, median or radial nerve responses). Needle repositioned if necessary to get motor response, then LA injected dorsal to axillary artery. LA distribution around cords and axillary artery observed with US Nerve stimulation (Stimuplex): 22 G, 100 mm insulated needle connected to negative pole of the nerve stimulator and set to deliver 1.5 mA current impulses of 0.1 ms duration at a frequency of 2 Hz. | |
| Outcomes |
| |
| Notes | Specialist anaesthesiologist and single senior resident. Experienced in block procedure. Does not indicate if experienced in US technique Results for onset time presented as median (range), therefore not possible to combine for this review. No difference between the 2 groups for this outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomized but no further details given |
| Allocation concealment (selection bias) | Unclear risk | “sealed envelope technique” – no further details. |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetists |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetists |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Assessed by a blinded anaesthetist. |
| Blinding of outcome assessment (detection bias): Complications | Low risk | Assessed by a blinded anaesthetist. |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | No details given as to who measured time to perform block. Possibly blinded anaesthetist? |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Published protocol sought |
| Baseline characteristics | Low risk | Mostly comparable |
| Funding sources | High risk | US device provided by General Electrics Company |
| Operator expertise | Unclear risk | Not clear if anaesthetists experienced in ultrasound techniques |
| Methods | RCT, parallel design | |
| Participants | 160 patients, ASA I ‐ II for scheduled trauma surgery of shoulder or upper arm Exclusion criteria: allergy to local anaesthetic; pre‐existing respiratory, metabolic or neurological diseases; history of cardiac, hepatic or renal failure; pregnancy | |
| Interventions | Ultrasound guidance (n = 80) versus nerve stimulation (n = 80) Interscalene brachial plexus block with 20 ml 0.75% bupivacaine in both groups Ultrasound: 5 ‐ 10 MHz linear probe (Sonosite); endpoint ‐ visualized spread local anaesthetic around all nerve roots (C5 ‐ T1), multiple injections permitted Nerve stimulation: pulse duration 0.1 msec, frequency 2 Hz; endpoint ‐ stimulation hand or forearm < 0.5 mA; single injection | |
| Outcomes |
| |
| Notes | All blocks performed by same 3 anaesthetists with experience in both guidance techniques Results for onset time given as median (range) therefore not possible to combine for this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | External preparation |
| Allocation concealment (selection bias) | Low risk | Sealed opaque sequentially‐numbered envelopes |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | Evaluation of nerve block by independent anaesthetist; no details if assessor is blinded |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details of who assessed this outcome |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | Evaluation of nerve block by independent anaesthetist; no details if assessor is blinded |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | baseline characteristics comparable |
| Funding sources | Low risk | No apparent external funding |
| Operator expertise | Unclear risk | All blocks by same experienced anaesthetists |
| Methods | RCT, parallel design | |
| Participants | 90 patients, ASA I ‐ II, scheduled for forearm, wrist or hand surgery | |
| Interventions | Ultrasound (double injection) (n = 30) versus ultrasound (single injection) (n = 30) versus nerve stimulation (double injection) (n = 30) Axillary brachial plexus block with 0.5 ml/kg 1.5% lignocaine with epinephrine (5 µg/kg) in nerve stimulation group and 30 ml 1.5% lignocaine with epinephrine (5 µg/kg) in ultrasound groups Ultrasound: 12 MHz probe (Hawk model 2102, B‐K medical); endpoint ‐ visualization of local anaesthetic spread around axillary artery. Either 1 injection (superior to artery) or 2 injections (superior and inferior to artery) | |
| Outcomes |
| |
| Notes | 1 practitioner performed all blocks, experience not given For the purpose of analysis of Adequacy of block and Supplementation rate, we combined the data for the double and single injection ultrasound groups For the purpose of analysis of Time to perform block, we took data only from ultrasound (double injection) versus nerve stimulation (double injection) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization table |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Assessment done by anaesthetist unaware of group allocation |
| Blinding of outcome assessment (detection bias): Complications | Low risk | Assessment done by anaesthetist unaware of group allocation |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Assessment done by anaesthetist unaware of group allocation |
| Incomplete outcome data (attrition bias) | Low risk | No withdrawals or exclusions |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Baseline characteristics comparable |
| Funding sources | Low risk | No apparent external funding |
| Operator expertise | Unclear risk | Same anaesthetist for all blocks |
| Methods | RCT, parallel design | |
| Participants | 230 patients, scheduled to undergo outpatient shoulder arthroscopy under interscalene block Excluded: < 18 yrs, > 75 yrs, patient refusal, pregnancy, dementia, severe pulmonary disease, and known pre‐existing neurological disorders involving the operative limb | |
| Interventions | Ultrasound (n = 115) vs nerve stimulation group (n = 115) Interscalene block of axillary, musculocutaneous, ulnar, radial and median nerves with mepivacaine 1.5% with 1:300,000 epinephrine and NaCO3 (1 meq/10mL); for participants < 50 kg, total dose of 45 ‐ 55 ml was used for patients ≥ 50 kg, total dose of 55 ‐ 65 mL was used Ultrasound: A linear 10 ‐ 13 MHz US probe was used to visualize the brachial plexus. Initial US visualization was at interscalene area. 5 cm 22 G needle placed through middle scalene muscle, into interscalene groove, in‐plane US guidance to visualize the entire needle. LA injected in divided doses with frequent aspiration under ultrasound visualization. Nerve stimulation (Stimuplex): 5 cm 22 G insulated needle placed into interscalene groove. Current decreased to range between 0.2 mA and 0.5 mA. If not still present then needle adjusted. LA injected in divided doses with frequent aspiration | |
| Outcomes |
| |
| Notes | No details of experience of anaesthetists giving nerve blocks | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number table |
| Allocation concealment (selection bias) | Unclear risk | Used a “sealed envelope sequence”. No further details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Adequacy of block assessed by an investigator who was unaware of group allocation |
| Blinding of outcome assessment (detection bias): Complications | Low risk | Neurological complications assessed and analyzed by blinded investigator |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | Time to perform block assessed by an investigator not performing block but no details as to whether they were blinded |
| Incomplete outcome data (attrition bias) | Low risk | Some losses to follow‐up but relatively small number and details given |
| Selective reporting (reporting bias) | Unclear risk | Pre‐published protocol not sought |
| Baseline characteristics | Low risk | All comparable |
| Funding sources | Low risk | None apparent |
| Operator expertise | Unclear risk | No details of who, how many and experience of anaesthetists giving blocks |
| Methods | RCT, parallel design | |
| Participants | 60 patients undergoing elective endoscopic carpal tunnel release Exclusions: none stated | |
| Interventions | Ultrasound (n = 30) versus nerve stimulation (n = 29) Median and ulnar nerve block (at wrist) with 4 ml 1.5% mepivacaine injected around each nerve in both groups Ultrasound: 13 MHz linear probe (GE LOGIQ e); endpoint ‐ local anaesthetic spread around each nerve. Needle repositioning to allow adequate spread Nerve stimulation (HNS 12, B Braun): pulse duration 0.1 msec; Freq 2 Hz; endpoint ‐ stimulation < 0.5 mA motor or sensory response | |
| Outcomes |
| |
| Notes | Palmaris radius blocked blindly in both groups Author contact attempted in original review for additional information for risk of bias table No details of experience of anaesthetist giving block Data for Block Performance time and Onset time presented as median (interquartile range), so not possible to combine in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomized but no details given |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | Sensory loss assessed by investigator not involved in block performance, but no details of whether blinded |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | No details of who assessed this outcome |
| Blinding of outcome assessment (detection bias): Patient discomfort | High risk | No details of whether participants blinded to group allocation, assume not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Only 1 withdrawal due to protocol violation ‐ low attrition rate |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Baseline characteristics largely equivalent |
| Funding sources | Low risk | No apparent funding sources |
| Operator expertise | Unclear risk | No details |
| Methods | RCT, parallel design | |
| Participants | 60 patients, ASA I ‐ II, scheduled for hand, forearm and elbow surgery Exlusion criteria: ASA > III, < 18 years and > 85 years, general contraindications for plexus block, known muscular or neurological deficits, pregnant or breastfeeding women, comprehension difficulties | |
| Interventions | Ultrasound (n = 30) versus nerve stimulation (n = 30) Axillary plexus block of median, radial, musculocutaneous, and ulnar nerve with 40 ‐ 50 ml 1.5% mepivacaine (plexus) and 5 ‐ 10 ml mepivacaine 0.5% (subcutaneous in medial skin of arm) Ultrasound: no details in paper Nerve stimulation (Braun): pulse duration 0.1 msec. Endpoint ‐ visible muscle contractions at current of 0.3 ‐ 0.5 mA | |
| Outcomes |
| |
| Notes | 5 practitioners with more than 5 years experience Participants given tourniquet block in both groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Assessor blinded from group allocation |
| Blinding of outcome assessment (detection bias): Complications | Low risk | Assessor blinded from group allocation |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Assessor blinded from group allocation |
| Blinding of outcome assessment (detection bias): Patient discomfort | Low risk | Assessor blinded from group allocation |
| Incomplete outcome data (attrition bias) | Low risk | Only 2 losses, clearly explained |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Age, gender, BMI, type of surgery, time length of surgery. All comparable |
| Funding sources | Low risk | None |
| Operator expertise | Unclear risk | 5 practitioners with more than 5 years experience |
| Methods | RCT, parallel design | |
| Participants | 129 ASA I ‐ II patients scheduled for elective orthopaedic surgery of elbow, forearm, wrist or finger Exclusion criteria: patient refusal, neurological disturbance, infection/inflammation of the upper extremity, coagulopathy, inability to communicate, those expected to have an axillary catheter | |
| Interventions | Ultrasound with nerve stimulation (n = 65) versus nerve stimulation only (n = 62) Axillary brachial plexus block of median, musculocutaneous, cubital and radial nerve Each nerve blocked with 10 ml 1% mepivacaine (40 ml in total) in each group Ultrasound: 5 ‐ 10 MHz linear probe (Titan, Sonosite) out‐of‐plane approach, once brachial plexus structures seen nerve stimulator used Nerve stimulation (Stimuplex): pulse duration 0.3 msec, Freq 2 Hz; endpoint ‐ stimulation of motor response at 0.4 mA | |
| Outcomes |
| |
| Notes | 2 anaesthesiologists with extensive experience in both techniques | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of random number table |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details of who assessed outcomes |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | No details of who assessed outcomes |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Age, gender, weight, height, ASA status reported. All comparable |
| Funding sources | Low risk | None apparent |
| Operator expertise | Unclear risk | Two anaesthesiologists with extensive experience in both techniques |
| Methods | RCT, parallel design | |
| Participants | 70 patients, ASA I ‐ II, scheduled for elective foot and ankle surgery Exclusions: contraindication to nerve block; significant peripheral neuropathy or neurological disease affecting lower extremity; pregnancy; history of alcohol or drug abuse; long‐standing opiate intake; significant psychiatric conditions | |
| Interventions | Ultrasound guidance (n = 37) versus nerve stimulation (n = 33) Popliteal fossa sciatic nerve block with 30 ml local anaesthetic mixture in both groups (15 ml 2% lignocaine and 15 ml 0.5% bupivacaine) Ultrasound: 4 ‐ 7 MHz or 4 ‐ 8 MHz linear probe (Philips Ultrasound); endpoint ‐ local anaesthetic spread around nerve; needle position adjustment permitted (Note: current required to elicit motor stimulation recorded once needle positioned with ultrasound but no further needle adjustment) Nerve stimulation (Stimuplex): duration 0.1 msec; frequency 2 Hz; endpoint ‐ stimulation of foot or toes at < 0.5 mA | |
| Outcomes |
| |
| Notes | Saphenous nerve block also given if required, for tourniquet pain Registered in clinicaltrials.gov | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number |
| Allocation concealment (selection bias) | Low risk | "group allocation not disclosed to patients" ‐ but no details given |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): Patient discomfort | Low risk | Sham ultrasound used, although relevant participant outcomes not reported |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Investigator blinded to group allocation assessed progress of block |
| Blinding of outcome assessment (detection bias): Complications | Low risk | Blinded anaesthetist responsible for all intraoperative care including induction of GA |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Investigator blinded to group allocation assessed progress of block |
| Incomplete outcome data (attrition bias) | Low risk | 4 participants excluded but low attrition rate |
| Selective reporting (reporting bias) | Low risk | Protocol details published in clinicaltrials.gov. NCT 00221920. Outcomes appear to be reported |
| Baseline characteristics | Low risk | Baseline characteristics largely comparable, although some differences in gender ratios |
| Funding sources | Low risk | Funding from university research award |
| Operator expertise | Unclear risk | Experienced anaesthetists in both techniques |
| Methods | RCT, parallel design | |
| Participants | 60 patients, ASA I ‐ III, scheduled for elbow, forearm, wrist and hand surgery under supraclavicular brachial plexus block without sedation Excluded: Patients refusing supraclavicular block, inability to obtain informed consent, hemidiaphragmatic dysfunction, coagulation disorders, neuropathy, pulmonary and cardiac disorders, BMI 35 kg/m² or higher, pregnancy, allergy to LA | |
| Interventions | Ultrasound (n = 30) vs neurostimulation (n = 30) Supraclavicular brachial plexus block of ulnar, median, radial and musculocutaneous nerves with 20 ml 0.75% ropivacaine Ultrasound: 38 mm 6 ‐ 13 MHz broadband linear array US probe to identify brachial plexus in short‐axis view located lateral to the subclavian artery. In‐plane approach Nerve stimulation (HNS 11, B. Braun):pulse duration 0.1 msec, frequency 2 Hz. Endpoint: Flexion of both fingers and wrist or extension of fingers at a stimulation current between 0.20 and 0.50 mA | |
| Outcomes |
| |
| Notes | For Supplementation rate we took data for intravenous fentanyl administration only. There were no participants requiring local anaesthetic or GA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No further details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details of who assessed this and whether blinded |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses after randomization |
| Selective reporting (reporting bias) | Unclear risk | Prepublished protocol not sought |
| Baseline characteristics | Low risk | Largely comparable |
| Funding sources | Low risk | None; department funding only |
| Operator expertise | Unclear risk | No details given of who gave anaesthetic and level of expertise |
| Methods | RCT, parallel design | |
| Participants | 60 patients scheduled for shoulder surgery Excluded: Hypersensitivity to local anaesthetics, neurologic deficits, bleeding tendency, respiratory failure, local infection, refusal to participate in the study or request for GA | |
| Interventions | Ultrasound + nerve stimulation (n = 30) vs nerve stimulation alone (n = 30) Interscalene brachial plexus block; In both cases, 30 ml of prilocaine was used followed by catheter insertion Ultrasound: Roots of brachial plexus sought between anterior and middle scalene muscles in an axial oblique plane. After sonographic plexus identification, injected glucose 5% to scan fluid around the plexus, then fixed needle. Nerve stimulation then switched on looking for muscle contractions as below Nerve stimulation (Stimuplex): pulse duration 0.1 msec, frequency 2 Hz, initial current mA. 5 ml sytrine with NaCl 0.9% through injection line inserted in a caudal slightly lateral and discrete dorsal orientation After 3 ‐ 4 cm, biceps contractions and then current reduced incrementally until 0.2 ‐ 0.3 mA was reached. Then needle retracted slightly and LA slowly injected | |
| Outcomes |
| |
| Notes | Study published in journal's 'short communication', therefore limited details Results for onset time presented as median and range, not possible to combine in this review. No statistically significant difference reported for this outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details of who assessed this outcome and whether blinded |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | No details of who assessed this outcome and whether blinded |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Comparable |
| Funding sources | Low risk | None apparent |
| Operator expertise | Unclear risk | 2 anaesthetic consultants with "over 10 years experience" |
| Methods | RCT, parallel design | |
| Participants | 80 patients, ASA I ‐ II, scheduled for elective forearm or hand surgery Exclusions: not detailed (inclusion criteria: ASA I or II; weight 50 ‐ 100 kg; normal neurological status; co‐operative) | |
| Interventions | Ultrasound (n = 40) versus peripheral nerve stimulation (n = 40) Interscalene brachial plexus block of musculocutaneous, radial, median, ulnar and antebrachial cutaneous nerves with 0.6 ml/kg mepivacaine with epinephrine in both groups Ultrasound: 5 ‐ 8 MHz curved probe (Sonosite); endpoint ‐ spread local anaesthetic around all cords or spread from 3 o'clock to 11 o'clock around artery. Multiple injections permitted Nerve stimulation (Stimuplex): 0.1 msec duration, frequency 2 Hz; starting current 1.5 mA; endpoint ‐ motor response in finger or hand from posterior or middle cord at 0.2 ‐ 0.5 mA. Single injection | |
| Outcomes |
| |
| Notes | Registered in clinicaltrials.gov Data for block performance time not presented as mean (SD) and therefore not possible to combine in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers; permuted blocks |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes opened immediately before block performed. No additional details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Assessed by blinded observer |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | Unclear who assessed this outcome and whether blinded |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | No details of who assessed these outcomes and whether blinded |
| Blinding of outcome assessment (detection bias): Patient discomfort | High risk | Participant not blinded to group allocation |
| Incomplete outcome data (attrition bias) | Low risk | Only 1 loss, low attrition rate |
| Selective reporting (reporting bias) | Low risk | Protocol details published in clinicaltrials.gov. NCT 00321425. Outcomes appear to be reported |
| Baseline characteristics | Low risk | Baseline characteristics comparable |
| Funding sources | Low risk | None apparent |
| Operator expertise | Unclear risk | 2 anaesthetists experienced in both techniques |
| Methods | Randomized, parallel design | |
| Participants | 250 ASA I ‐ III adult patients scheduled for orthopaedic foot surgery under tourniquet Exclusion criteria not given | |
| Interventions | Ultrasound (n = 125) versus nerve stimulation (n = 125); Distal sciatic block of sciatic, tibial and common peroneal nerves; each nerve blocked with 20 ml 1% prilocaine and 10 ml 0.75% ropivacaine Ultrasound: 6 ‐ 13 MHz linear probe (Sonosite); intraepineural needle position Nerve stimulation (Stimuplex): 0.1 msec duration, frequency 2 Hz; starting current 1.0 mA | |
| Outcomes |
| |
| Notes | Saphenous nerve block for tourniquet pain given to all participants Registered in clinicaltrials.gov Data for block onset time presented as log‐rank test results and therefore not possible to combine for this review Reported as significantly shorter onset time in US group, P value < 0.01 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Observer blinded from group allocation |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Observer blinded from group allocation |
| Incomplete outcome data (attrition bias) | Low risk | 7 participants in each group excluded from analysis, but low attrition rate |
| Selective reporting (reporting bias) | Low risk | Protocol details published in clinicaltrials.gov. NCT 01643616. Outcomes appear to be reported |
| Baseline characteristics | Low risk | Age, weight, height, gender, surgery time, diabetes mellitis. Some difference in gender balance but otherwise all comparable |
| Funding sources | Low risk | No conflicts of interest or funding declared |
| Operator expertise | Unclear risk | No details |
| Methods | RCT, parallel design | |
| Participants | 70 adult patients ASA I and II requiring upper arm surgery (wrist, forearm and hand) under axillary block Exclusion criteria: History of coagulopathy, allergy to drug, diabetes, local infection at site of block, patients requiring bilateral hand surgery, patients’ denial, cases that needed conversion to GA, surgery lasting more than 3.5 hours and patients beyond age of 20 ‐ 65 yrs, and body weight of 45 ‐ 65 kg | |
| Interventions | Ultrasound + nerve stimulation (n = 35) versus nerve stimulation (n = 35) Axillary brachial plexus block for ulnar, radial, median and musculocutaneous nerves Nerves blocked with a total of 24 ml of bupivacaine 0.5% with injection dexamethasone 4 mg, each individual nerve blocked with 6 ml Ultrasound: 8 MHz linear probe (Toshiba); endpoint ‐ nerve location confirmed by nerve stimulation and then local anaesthetic deposited under ultrasound guidance Nerve stimulation (Stimuplex): 0.2 msec duration, frequency 2 Hz; starting current 1.0 mA. Current reduced to 0.6 mA then 1 ml of LA injected to see if twitches disappeared. Then remaining 5 ml given | |
| Outcomes |
| |
| Notes | 1 anaesthetist performed all blocks, but no details of their experience in the 2 techniques Results for onset time reported as statistically significant difference between groups with shorter onset time in US group, P value < 0.01 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of a “lottery method” |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Data recorded by blinded observer |
| Blinding of outcome assessment (detection bias): Complications | Low risk | Data recorded by blinded observer |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Data recorded by blinded observer |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | All comparable |
| Funding sources | Low risk | None apparent |
| Operator expertise | Unclear risk | Only 1 person performing all blocks |
| Methods | RCT, parallel design | |
| Participants | 56 patients, ASA I ‐ III, scheduled for hand surgery | |
| Interventions | Ultrasound perivascular approach (n = 28) versus transarterial approach (n = 28) Axillary brachial plexus block with 30 ml 1.5% lidocaine in both groups Ultrasound: 3 ‐ 12 MHz probe (Philips EnVisor); endpoint ‐ circumferential spread of local anaesthetic around artery Separate musculocutaneous nerve block could be done at discretion of operator prior to study protocol (uncontrolled) | |
| Outcomes |
| |
| Notes | 7 practitioners performing blocks (3 trainees and 4 experienced) Musculocutaneous nerve block not controlled for and used at anaesthetist's preference 5 ml 1.5% lidocaine with 5 µg/ml epinephrine given to all participants for analgesia for tourniquet pain Study terminated early due to high level of block failure in transarterial group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of block randomization |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes but no further details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist/personnel |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Block assessed by blinded observer. Upgrade to GA etc. made by anaesthetist or surgeon not aware of group allocation |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details of who assessed this outcome |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Blinded research nurse |
| Incomplete outcome data (attrition bias) | High risk | Trial stopped early due to high failure rate in transarterial group |
| Selective reporting (reporting bias) | Unclear risk | Outcomes reported despite early stopping. Published protocol not sought |
| Baseline characteristics | Low risk | Baseline characteristics comparable |
| Funding sources | High risk | Ultrasound equipment provided by manufacturer during trial |
| Operator expertise | High risk | Some blocks performed by a supervised resident, some by an experienced anaesthetist |
| Methods | RCT, parallel design | |
| Participants | 40 patients for elective upper limb surgery Exclusion criteria: pre‐existing neurological deficit, local sepsis, respiratory failure, patient refusal | |
| Interventions | Ultrasound (n = 20) versus landmark technique (n = 20) Interscalene or axillary brachial plexus block with 3 mg/kg ropivacaine (0.75% for interscalene; 0.6% for axillary) Ultrasound: 13 MHz probe (Siemens sonoline); endpoint ‐ local anaesthetic spread around individual nerves/trunks. Needle position altered during injection to optimize local anaesthetic spread | |
| Outcomes |
| |
| Notes | 1 practitioner performed all blocks. Previous experience in ultrasound blocks and tuition from radiologist | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Details not given |
| Allocation concealment (selection bias) | Unclear risk | Details not given |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | Assessments done by independent investigator but no details of whether they were blinded. |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details of who assessed this and whether blinded to group allocation |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | No details of who assessed this and whether blinded to group allocation |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Unclear risk | No standard baseline characteristics reported |
| Funding sources | Low risk | No apparent additional funding sources |
| Operator expertise | Unclear risk | Same operator performed all blocks |
| Methods | RCT, parallel design | |
| Participants | 141 patients scheduled for hand surgery distal to the elbow with and estimated duration < 2 hrs Excluded: Those that declined to give informed consent, had known allergy to any anaesthetic substance, an infection in region of injection site, severe coagulopathy, pathological enlargement of axillary lymph nodes, those who had had previous surgery on the axilla | |
| Interventions | Ultrasound (n = 70) vs landmark technique (n = 71) Axillary brachial plexus block; dose of 20 ml LA deposited behind artery next to radial nerve; 10 ml LA then injected around mediocranial median nerve and mediocaudal ulnar nerve Ultrasound: cross‐section of axillary artery is imaged. Individual nerves are then identified. Cannula introduced under US. 20 G 105” bevelled needle. LA injected around all 4 nerves individually starting with radial nerve. Aim of infiltration is to see a circular perineural spread of the fluid in the ultrasound image. Bupivacaine hydrochloride (5 mg/ml) with 0.5% adrenaline and mepivacaine hydrochloride (10 mg/ml) in a ratio of 1:1 Neurostimulation: Anatomic landmarks used for orientation. Needle inserted in space between axillary artery and coracobrachial muscle, near to axillary fold. Needle at an angle to skin of 50 ‐ 90°, inserted past facial click and advanced cranially, caudally or transarterially past axillary artery | |
| Outcomes |
| |
| Notes | Training had been given to those conducting the ultrasound technique; baseline of 10 procedures with US before study, or 300 in conventional technique Not possible to combine data for Time to perform block or Onset time as no standard deviation reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):Complications | High risk | Surgeon not blinded |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Surgeon not blinded |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | High risk | “No blinding” reported at end of discussion |
| Blinding of outcome assessment (detection bias): Complications | High risk | “No blinding” reported at end of discussion |
| Blinding of outcome assessment (detection bias): time outcomes | High risk | “No blinding” reported at end of discussion |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | All comparable |
| Funding sources | Low risk | None |
| Operator expertise | High risk | Surgeon with limited experience (10 previous attempts) using ultrasound technique |
| Methods | RCT, parallel design | |
| Participants | 70 ASA I ‐ III patients scheduled for hand/wrist surgery Exclusion criteria: Patient refusal, neurologic or neuromuscular disease, anticoagulation, skin infection at site of needle insertion | |
| Interventions | Ultrasound (n = 35) versus nerve stimulation (n = 35) Coracoid infraclavicular brachial plexus block with single injection of 40 ml mepivacaine 1.5% Ultrasound: probe 6 ‐ 13 MHz (MicroMaxx); endpoint ‐ visualization under US of spread of local anaesthetic posterior to axillary artery Nerve stimulation (Pajunk Medizintechnologic): 0.1 msec duration, frequency 2 Hz; starting current 1.5 mA Current decreased to 0.5 mA or less when radial nerve stimulation could still be elicited. Then LA injected slowly | |
| Outcomes |
| |
| Notes | 2 practitioners performing blocks with long‐standing experience in performance of both nerve stimulator and US coracoid infraclavicular brachial plexus blocks Block considered a failure if taken more than 15 minutes to perform | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Computer‐generated random list |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias):Complications | High risk | Anaesthetist not blinded |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Anaesthetist not blinded |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details of who assessed this outcome – assume anaesthetists? |
| Blinding of outcome assessment (detection bias): Complications | Low risk | Assessed by an independent observer not aware of technique |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Assessed by an independent observer not aware of technique |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Prepublished protocol not sought |
| Baseline characteristics | Low risk | Some differences in type of surgery but unlikely to introduce bias, otherwise all comparable |
| Funding sources | Low risk | None |
| Operator expertise | Unclear risk | 2 experienced anaesthetists |
| Methods | RCT, parallel design | |
| Participants | 60 ASA I ‐ II patients scheduled for surgery of the upper limb (wrist, hand, elbow or distal arm) Exclusion criteria: none | |
| Interventions | Ultrasound (n = 30) versus nerve stimulation (n = 30) Infraclavicular brachial plexus block; nerves blocked with 15 ml 0.5% bupivacaine Ultrasound: 10 ‐ 12 MHz linear probe (Logiq 7) in‐plane approach; endpoint ‐ visualized LA injection around each brachial plexus cord with approximately 5 ml Nerve stimulation (Stimuplex): Initial stimulating current at 1 ‐ 1.5 mA; endpoint ‐ current gradually decreased until responses still present at 0.3 mA or less | |
| Outcomes |
| |
| Notes | Surgical tourniquet used in all participants Note: supplementary GA was used at discretion of attending anaesthetist and was not reported as an outcome. However, all participants were described as being awake during surgery Data for onset time of block reported as median (IQR), therefore not possible to combine in analysis. Onset time for motor block in US group 20 min (15 ‐ 26) vs 23 min (16 ‐ 32) in NS group; onset time for sensory block in US group 10 min (10 ‐ 15) vs 14 min (12 ‐ 25) in NS group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized by "distributing sealed, opaque envelopes". No further details |
| Allocation concealment (selection bias) | Unclear risk | As above. No further details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Low risk | Assessed by anaesthetist blinded to technique used |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | Assessed by anaesthetist blinded to technique used |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Age, gender, ASA status, weight, height, BMI, surgical duration. All comparable. |
| Funding sources | Low risk | None apparent |
| Operator expertise | Unclear risk | No details given |
| Methods | RCT, parallel design | |
| Participants | 40 ASA I ‐ III patients undergoing surgery of foot or ankle with distal sciatic nerve block in popliteal fossa Exclusion criteria: Patient refusal, pre‐existing neuropathy, kidney or liver disease, pregnancy, skin infection at site of needle insertion and inability to communicate | |
| Interventions | Ultrasound (n = 20) versus nerve stimulation (n = 20) Distal sciatic nerve block in the popliteal fossa with lignocaine 1.5% with adrenaline 5 µg/ml – at discretion of anaesthetist, min of 25 ml and max of 40 ml Ultrasound: with 7 ‐ 13 MHz 38 mm linear probe (Sonosite); endpoint ‐ visualization of LA distribution around nerve Nerve stimulation (HNS 11, Braun): 0.1 msec duration, frequency 2 Hz; starting current 1.0 mA. Initial current reduced until responses maintained with minimum of 0.2 mA and max 0.5 mA | |
| Outcomes |
| |
| Notes | Anaesthetists had extensive clinical experience with nerve stimulation guided popliteal sciatic nerve blocks but no experience with ultrasound guidance block Some participants also given saphenous nerve block if tourniquet required for surgery; no details in results of those that were given additional block | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomized using sealed envelopes. No further detail |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Anaesthestists not blinded |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Anaesthestists not blinded |
| Blinding of participants and personnel (performance bias): Patient discomfort | High risk | Anaesthestists not blinded |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details of who assessed this. Assume anaesthetist? |
| Blinding of outcome assessment (detection bias): time outcomes | Low risk | Assessor blinded to block technique |
| Blinding of outcome assessment (detection bias): Patient discomfort | Low risk | Assessor blinded to block technique |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Age, weight, height, ASAI‐III, gender, type of surgery. All comparable |
| Funding sources | High risk | Funding from dept sources. Study equipment supported was provided from Sonosite Inc, Bothell, WA, USA |
| Operator expertise | High risk | Anaesthetists had extensive clinical experience with nerve stimulation guided popliteal sciatic nerve blocks but no experience with ultrasound guidance block |
| Methods | RCT, parallel design | |
| Participants | 80 patients undergoing distal arm, forearm or hand surgery | |
| Interventions | Ultrasound + nerve stimulation (n = 40) versus nerve stimulation (n = 40) Supraclavicular brachial plexus block with 0.5 ml/kg of 0.5% bupivacaine/2% lidocaine and 1:200,000 epinephrine to maximum of 40 ml Ultrasound: 7.5 MHz probe (Aloka); endpoint ‐ neurostimulation at < 0.6 mA | |
| Outcomes |
| |
| Notes | All blocks attempted by 1 anesthesiology resident (limited experience of both techniques) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomized but no further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias): time outcomes | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details given of who assessed outcomes and whether blinded |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details given of who assessed outcomes and whether blinded |
| Blinding of outcome assessment (detection bias): time outcomes | Unclear risk | No details given of who assessed outcomes and whether blinded |
| Incomplete outcome data (attrition bias) | Low risk | No losses |
| Selective reporting (reporting bias) | Unclear risk | Published protocol not sought |
| Baseline characteristics | Low risk | Baseline characteristics comparable |
| Funding sources | Low risk | No apparent funding |
| Operator expertise | High risk | Performed by anesthesiology resident who had experience of blocks whilst under supervision by staff anaesthesiologist. This may have increased time to perform block and would introduce bias for this outcome |
| Methods | RCT, parallel design | |
| Participants | 34 adult ASA 1 ‐ III patients scheduled for surgery of upper limb Exclusions: Allergy to local anaesthetic, coagulopathy, infection at site of injection, pre‐existing neurological lesion | |
| Interventions | Ultrasound (n = 17) versus nerve stimulation (n = 17) Posterior approach to brachial plexus block of axillary, musculocutaneous, radial and median nerves; single injection of 30 ml 0.325% ropivacaine Ultrasound: 6 ‐ 13 mHz., cervical nerve root identified as a hypoechoic, circular image. Endpoint ‐ visualization of distribution of LA around nerve Nerve stimulation (Stimuplex): 0.1 msec duration, frequency 2 Hz; starting current 0.8 mA. Endpoint ‐ not stated | |
| Outcomes |
| |
| Notes | No details of experience of practitioners given | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding of participants and personnel (performance bias):adequacy of block, need for supplementation | High risk | Not possible to blind anaesthetist |
| Blinding of participants and personnel (performance bias):Complications | High risk | Not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias): adequacy of block, supplementation of block | Unclear risk | No details given |
| Blinding of outcome assessment (detection bias): Complications | Unclear risk | No details given |
| Incomplete outcome data (attrition bias) | Low risk | No apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Postoperative pain outcomes not reported. Published protocol not sought |
| Baseline characteristics | Low risk | Some differences in gender between groups, otherwise comparable |
| Funding sources | Low risk | No details. Assume no funding from external sources. |
| Operator expertise | Unclear risk | No details |
RCT = randomized controlled trials; RA = regional anaesthetic; LA = local anaesthetic; GA = general anaesthetic; ASA = American Society of Anesthesiologists; yr = year(s); min(s) = minute(s); BMI = body mass index; TCI = target controlled infusion; US = ultrasound; NS = nerve stimulation; SD = standard deviation; IQR = interquartile range
Note: The blank cells in the risk of bias tables are domains which are not applicable to the particular study.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Participants in both groups given GA after nerve block | |
| Included in 2009 version of review. Excluded in this update due to inclusion criteria changes (see Differences between review and current update). MEAV study design | |
| Included in 2009 version of review. Excluded in this update due to inclusion criteria changes (see Differences between review and current update). Aim to give femoral block to all participants following popliteal sciatic block | |
| MEAV study design | |
| Trunk block ‐ not upper or lower limb block | |
| Included in 2009 version of the review. Excluded in this update due to inclusion criteria changes (see Differences between review and current update). Assume participants given additional anaesthetic for knee/hip replacement surgery | |
| Trunk block ‐ not upper or lower limb block | |
| Participants in both groups given GA after nerve block | |
| Participants in both groups given a spinal‐epidural block | |
| Abstract published in 2010. No contact details available in abstract | |
| Included in 2009 version of review. Excluded in this update due to inclusion criteria changes (see Differences between review and current update). Aim to give spinal anaesthetic to all participants following nerve block | |
| Included in 2009 version of review. Excluded in this update due to inclusion criteria changes (see Differences between review and current update). Aim to give spinal anaesthetic to all participants following nerve block | |
| Nerve block given for postoperative analgesic. Assume further anaesthetic given | |
| Nerve block given for postoperative analgesic. Assume further anaesthetic given | |
| Nerve block given for postoperative analgesic. Assume further anaesthetic given | |
| Nerve block given for postoperative analgesic. Assume further anaesthetic given | |
| Nerve block given for postoperative analgesic. Assume further anaesthetic given | |
| Abstract only. Insufficient detail to include | |
| Abstract only. Results of study presented for some outcomes but no denominator figures and no details for risk of bias. No contact details available in abstract | |
| MEAV study design | |
| MEAV study design | |
| Abstract published in 2010. No contact details available in abstract | |
| MEAV study design | |
| Included in Characteristics of studies awaiting classification in 2009 version of review. Excluded in this update due to study enrolment of volunteers, not surgical patients | |
| Ultrasound used in all participants to initially identify needle entry point prior to group allocation to ultrasound or nerve stimulation technique | |
| Participants in both groups given GA after nerve block | |
| Abstract only. Insufficient detail to include | |
| Ultrasound is used pre‐puncture only | |
| Nerve block not used for sole operative anaesthesia | |
| Participants in both groups given GA after nerve block | |
| Abstract published in 2009. No contact details available in abstract | |
| MEAV study design | |
| Not described as randomized in full text |
MEAV = minimum effective anaesthetic volume; GA = general anaesthetic
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Identified in search run in May 2015. Full‐text review not yet completed |
| Methods | Randomized, parallel design |
| Participants | 210 patients undergoing elective hand or elbow surgery requiring infraclavicular plexus block |
| Interventions | US versus stimulating needle and catheter placement |
| Outcomes | Motor and sensory block success Complications Intraoperative analgesia requirement Time for catheter insertion |
| Notes | Study registered on clinicaltrials.gov (identifier: NCT 01136447). Completed but results not yet posted or study published |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Identified in search run in May 2015. Full‐text review not yet completed |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Unable to access study from British Library |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Identified in search run in May 2015. Full‐text review not yet completed |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Identified in search run in May 2015. Full‐text review not yet completed |
| Methods | Randomized, parallel design |
| Participants | 60 ASA I ‐ II patients scheduled for upper extremity procedures requiring supraclavicular brachial plexus block |
| Interventions | US versus NS |
| Outcomes | Haemodynamic responses Rate of complete block |
| Notes | Full text requires translation from Chinese |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Identified in search run in May 2015. Full‐text review not yet completed |
| Methods | Randomized, parallel design |
| Participants | Surgical patients aged over 18 years requiring lateral popliteal approach to the sciatic nerve block |
| Interventions | US versus NS |
| Outcomes | Procedural Time Number of Redirections |
| Notes | Clinical trials identifier: NCT 01579747. Results available on clinicaltrials.gov. Email sent to author to enquire about publications (awaiting reply at time of publication) |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Identified in search run in May 2015. Full‐text review not yet completed |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Identified in search run in May 2015. Full‐text review not yet completed |
US = ultrasound; NS = nerve stimulation
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Ultrasound guidance in nerve block anaesthesia |
| Methods | Randomized, parallel design |
| Participants | Patients aged over 18 years, scheduled for one of these blocks: interscalene, humeral, parasacral or lumbar blocks, for trauma or orthopaedic surgeries |
| Interventions | US + PNS versus PNS |
| Outcomes | Sensory and motor block quality Complications |
| Starting date | May 2005 |
| Contact information | Principal Investigator: Laurence Le Gourrier, MD., Unité d'Anesthésiologie et de Réanimation Chirurgicale, Hôpital de Hautepierre, Strasborg, France |
| Notes | Completion date: February 2009 |
| Trial name or title | Dual endpoint nerve stimulation versus ultrasound in infraclavicular block for hand surgery |
| Methods | Randomized, parallel design |
| Participants | Patients aged over 18 years, scheduled for upper limb surgery at or below the elbow |
| Interventions | US verus NS |
| Outcomes | Block success Ease of nerve location Speed of onset Duration of block Complications |
| Starting date | July 2009 |
| Contact information | Prinical investigator: Dr C McCartney, University Health Network, Toronto, Canada |
| Notes | Clinical trials identifier: NCT 009956683 |
| Trial name or title | Ultrasound visualization versus electrical nerve stimulation |
| Methods | Randomized design |
| Participants | Patients aged over 18 years undergoing unilateral elective surgical procedure requiring interscalene block |
| Interventions | US versus NS |
| Outcomes | Incidence of successful block Amount of sedation required for block |
| Starting date | February 2009 |
| Contact information | Principal Investigator: Nanette Schwann, M.D., Allentown Anesthesia Associates, Pensylvannia, US |
| Notes | Clinical trials identifier: NCT 01010412 |
| Trial name or title | Ultrasound plus nerve stimulator versus nerve stimulator guided lumbar plexus block |
| Methods | Randomized, parallel design |
| Participants | Patients 18 ‐ 70 years scheduled to undergo knee arthroscopy surgery |
| Interventions | US + NS versus NS |
| Outcomes | Time required to complete lumbar plexus block Total ultrasound visibility score Hymnody changes after skin incision Performance time of block |
| Starting date | 28 November 2013 |
| Contact information | Principal Investigator: Wei Mei, MD., PhD., Huazhong University of Science and Technology, China |
| Notes | Clinical trials identifier: NCT 02020096 |
US = ultrasound; (P)NS = (peripheral) nerve stimulation
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Predicted adequacy of block Show forest plot | 17 | 1346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.94 [2.14, 4.04] |
| Analysis 1.1  Comparison 1 Ultrasound technique versus other technique, Outcome 1 Predicted adequacy of block. | ||||
| 1.1 Ultrasound versus nerve stimulation | 15 | 1250 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.91 [2.08, 4.06] |
| 1.2 Ultrasound versus anatomical landmark technique | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.02 [0.20, 20.62] |
| 1.3 Ultrasound versus transarterial approach | 1 | 56 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 3.62 [1.19, 11.00] |
| 2 Supplementation of block Show forest plot | 18 | 1807 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.20, 0.39] |
| Analysis 1.2  Comparison 1 Ultrasound technique versus other technique, Outcome 2 Supplementation of block. | ||||
| 2.1 ultrasound versus nerve stimulation | 15 | 1570 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.21, 0.46] |
| 2.2 ultrasound versus anatomical landmark technique | 2 | 181 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.11, 0.44] |
| 2.3 ultrasound versus transarterial approach | 1 | 56 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.07, 0.85] |
| 3 Time to perform block Show forest plot | 10 | 690 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.41, ‐0.72] |
| Analysis 1.3  Comparison 1 Ultrasound technique versus other technique, Outcome 3 Time to perform block. | ||||
| 4 Paraesthesia Show forest plot | 6 | 471 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.23, 0.76] |
| Analysis 1.4  Comparison 1 Ultrasound technique versus other technique, Outcome 4 Paraesthesia. | ||||
| 5 Vascular puncture Show forest plot | 5 | 387 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.07, 0.57] |
| Analysis 1.5  Comparison 1 Ultrasound technique versus other technique, Outcome 5 Vascular puncture. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Predicted adequacy of block Show forest plot | 9 | 719 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.33 [2.13, 5.20] |
| Analysis 2.1  Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 1 Predicted adequacy of block. | ||||
| 2 Supplementation of block Show forest plot | 9 | 712 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.21, 0.56] |
| Analysis 2.2  Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 2 Supplementation of block. | ||||
| 3 Time to perform block Show forest plot | 7 | 587 | Mean Difference (IV, Fixed, 95% CI) | 0.76 [0.55, 0.98] |
| Analysis 2.3  Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 3 Time to perform block. | ||||
| 4 Paraesthesia Show forest plot | 3 | 178 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.30, 3.12] |
| Analysis 2.4  Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 4 Paraesthesia. | ||||
| 5 Vascular puncture Show forest plot | 2 | 143 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 0.90] |
| Analysis 2.5  Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 5 Vascular puncture. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 By type of intervention/comparison Show forest plot | 10 | 690 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.41, ‐0.72] |
| Analysis 3.1  Comparison 3 Time to perform block by subgroups US vs other, Outcome 1 By type of intervention/comparison. | ||||
| 1.1 nerve stimulation | 9 | 634 | Mean Difference (IV, Fixed, 95% CI) | ‐1.02 [‐1.37, ‐0.67] |
| 1.2 transarterial approach | 1 | 56 | Mean Difference (IV, Fixed, 95% CI) | ‐3.20 [‐5.76, ‐0.64] |
| 2 By type of nerve block/approach Show forest plot | 10 | 690 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.41, ‐0.72] |
| Analysis 3.2  Comparison 3 Time to perform block by subgroups US vs other, Outcome 2 By type of nerve block/approach. | ||||
| 2.1 axillary brachial plexus | 6 | 452 | Mean Difference (IV, Fixed, 95% CI) | ‐0.56 [‐0.98, ‐0.14] |
| 2.2 infraclavicular brachial plexus | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | ‐2.41 [‐3.10, ‐1.72] |
| 2.3 popliteal fossa sciatic | 2 | 108 | Mean Difference (IV, Fixed, 95% CI) | 1.00 [‐2.43, 0.44] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 By type of nerve block/approach Show forest plot | 7 | 587 | Mean Difference (IV, Fixed, 95% CI) | 0.76 [0.55, 0.98] |
| Analysis 4.1  Comparison 4 Time to perform block by subgroups US + PNS vs PNS, Outcome 1 By type of nerve block/approach. | ||||
| 1.1 Axillary brachial plexus block | 4 | 396 | Mean Difference (IV, Fixed, 95% CI) | 0.85 [0.62, 1.07] |
| 1.2 Interscalene brachial plexus | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.6 [‐2.12, 0.92] |
| 1.3 Supraclavicular brachial plexus | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐4.80 [‐7.24, ‐2.36] |
| 1.4 Popliteal fossa sciatic | 1 | 51 | Mean Difference (IV, Fixed, 95% CI) | 0.71 [‐0.07, 1.49] |
| 2 By catheter/no catheter placement Show forest plot | 7 | 587 | Mean Difference (IV, Fixed, 95% CI) | 0.76 [0.55, 0.98] |
| Analysis 4.2  Comparison 4 Time to perform block by subgroups US + PNS vs PNS, Outcome 2 By catheter/no catheter placement. | ||||
| 2.1 No catheter use | 6 | 527 | Mean Difference (IV, Fixed, 95% CI) | 0.79 [0.57, 1.01] |
| 2.2 Catheter placement | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.6 [‐2.12, 0.92] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 By type of intervention/comparison Show forest plot | 6 | 471 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.23, 0.76] |
| Analysis 5.1  Comparison 5 Paraesthesia by subgroups, Outcome 1 By type of intervention/comparison. | ||||
| 1.1 peripheral nerve stimulation | 5 | 431 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.25, 0.86] |
| 1.2 landmark technique | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.50] |
| 2 By type of nerve block/approach Show forest plot | 6 | 471 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.23, 0.76] |
| Analysis 5.2  Comparison 5 Paraesthesia by subgroups, Outcome 2 By type of nerve block/approach. | ||||
| 2.1 axillary brachial plexus | 3 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.19, 1.79] |
| 2.2 infraclavicular brachial plexus | 3 | 221 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.19, 0.76] |

Study flow diagram.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
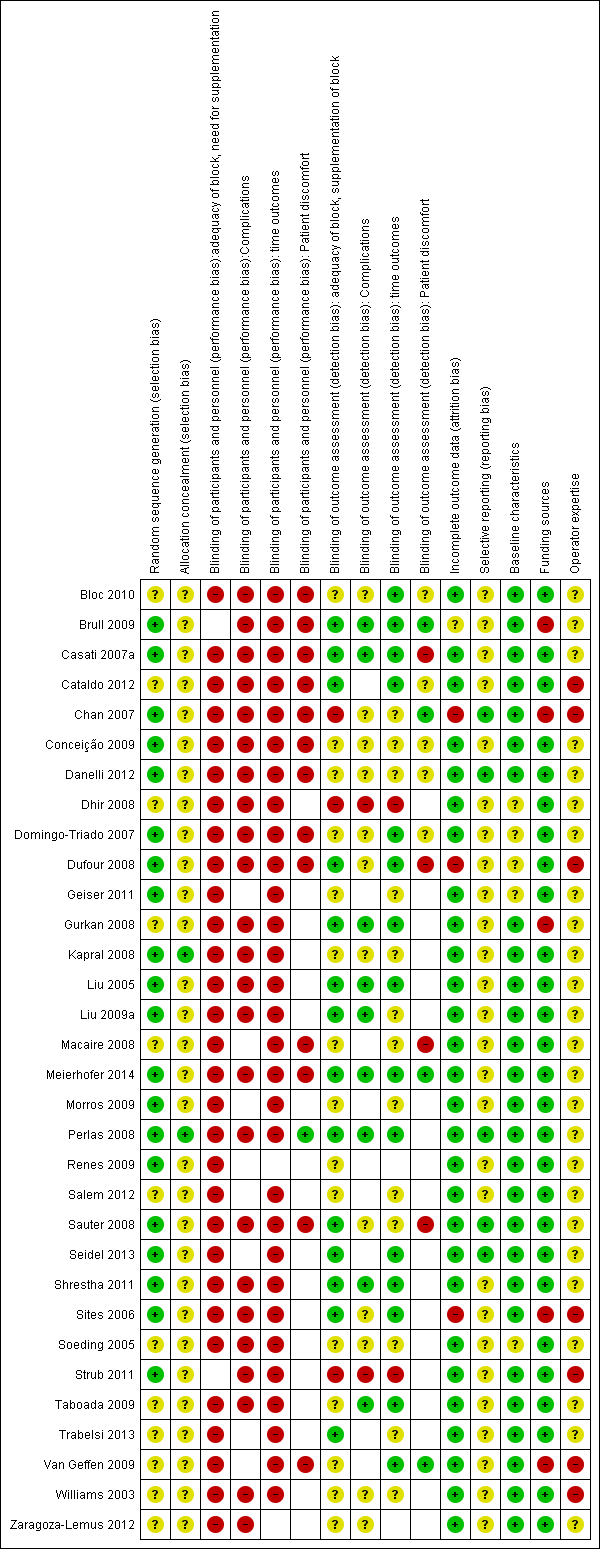
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Funnel plot of comparison: 1 Ultrasound technique versus other technique, outcome: 1.1 Predicted adequacy of block.
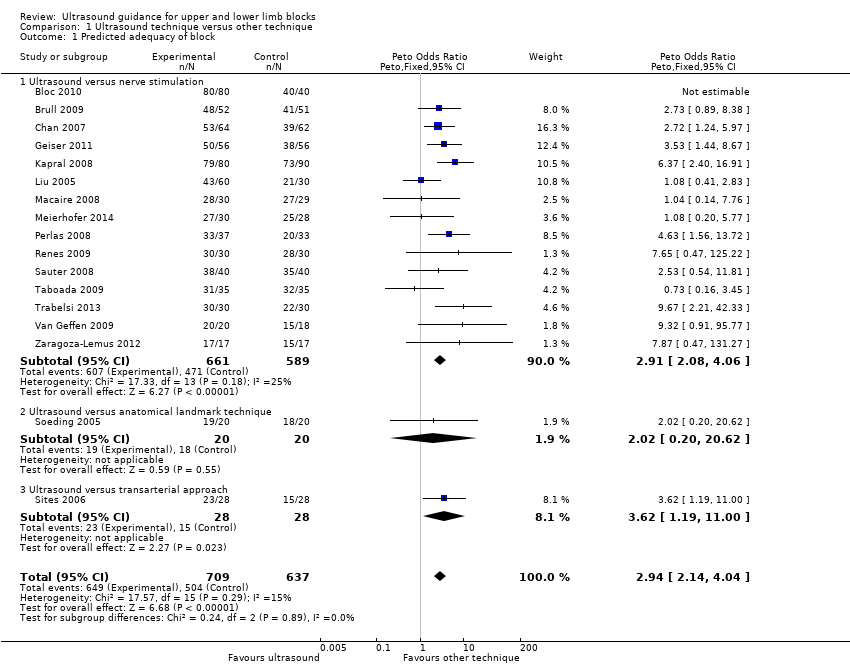
Comparison 1 Ultrasound technique versus other technique, Outcome 1 Predicted adequacy of block.

Comparison 1 Ultrasound technique versus other technique, Outcome 2 Supplementation of block.

Comparison 1 Ultrasound technique versus other technique, Outcome 3 Time to perform block.
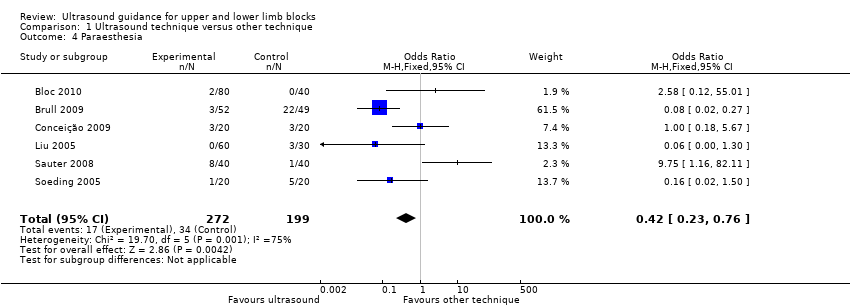
Comparison 1 Ultrasound technique versus other technique, Outcome 4 Paraesthesia.

Comparison 1 Ultrasound technique versus other technique, Outcome 5 Vascular puncture.

Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 1 Predicted adequacy of block.
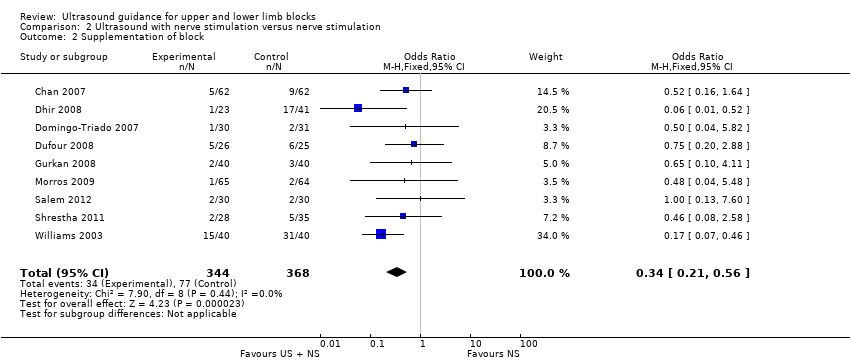
Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 2 Supplementation of block.
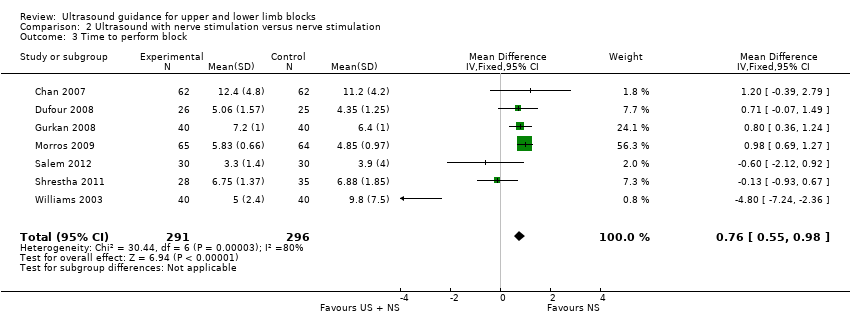
Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 3 Time to perform block.

Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 4 Paraesthesia.

Comparison 2 Ultrasound with nerve stimulation versus nerve stimulation, Outcome 5 Vascular puncture.

Comparison 3 Time to perform block by subgroups US vs other, Outcome 1 By type of intervention/comparison.

Comparison 3 Time to perform block by subgroups US vs other, Outcome 2 By type of nerve block/approach.

Comparison 4 Time to perform block by subgroups US + PNS vs PNS, Outcome 1 By type of nerve block/approach.

Comparison 4 Time to perform block by subgroups US + PNS vs PNS, Outcome 2 By catheter/no catheter placement.

Comparison 5 Paraesthesia by subgroups, Outcome 1 By type of intervention/comparison.
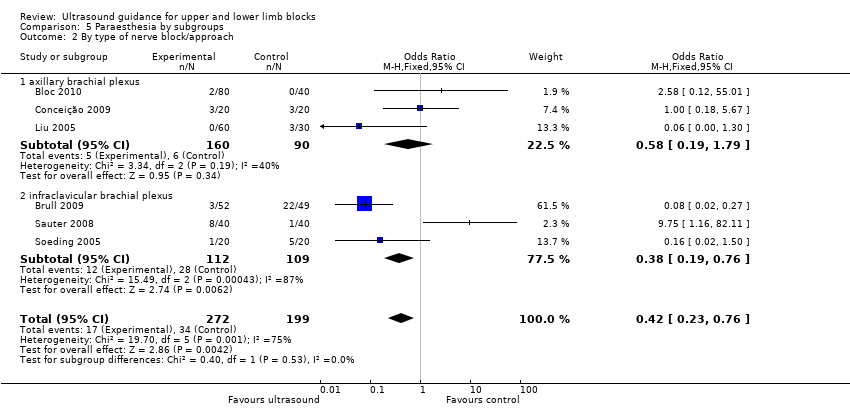
Comparison 5 Paraesthesia by subgroups, Outcome 2 By type of nerve block/approach.
| Ultrasound guidance for upper and lower limb blocks | ||||||
| Patient or population: People undergoing upper and lower limb blocks | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Ultrasound guidance | |||||
| Block success (predicted adequacy of block) | Study population | OR 2.49 (2.14 to 4.04) | 1346 | ⊕⊕⊕⊝ | ||
| 791 per 1000 | 902 per 1000 | |||||
| Moderate | ||||||
| Block success (supplementation or conversion to general anaesthesia | Study population | OR 0.28 (0.20 to 0.39) | 1807 | ⊕⊕⊕⊝ | ||
| 185 per 1000 | 73 per 1000 | |||||
| Moderate | ||||||
| Paraesthesia | Study population | OR 0.42 (0.23 to 0.76) | 471 | ⊕⊝⊝⊝ | ||
| 171 per 1000 | 80 per 1000 | |||||
| Moderate | ||||||
| Vascular puncture | Study population | OR 0.19 (0.07 to 0.57) | 387 | ⊕⊕⊝⊝ | ||
| 93 per 1000 | 20 per 1000 | |||||
| Moderate | ||||||
| Time to perform block | The mean time to perform block in the intervention groups was | 690 | ⊕⊝⊝⊝ | |||
| Number of attempts9 | See comment | See comment | Not estimable9 | 0 | ⊕⊕⊝⊝ | |
| Patient discomfort9 | See comment | See comment | Not estimable9 | 0 | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Unavoidable performance bias due to lack of blinding but does not appear to affect results. Not possible to fully explore potential for operator bias according to preference and/or experience of devices | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Predicted adequacy of block Show forest plot | 17 | 1346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.94 [2.14, 4.04] |
| 1.1 Ultrasound versus nerve stimulation | 15 | 1250 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.91 [2.08, 4.06] |
| 1.2 Ultrasound versus anatomical landmark technique | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.02 [0.20, 20.62] |
| 1.3 Ultrasound versus transarterial approach | 1 | 56 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 3.62 [1.19, 11.00] |
| 2 Supplementation of block Show forest plot | 18 | 1807 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.20, 0.39] |
| 2.1 ultrasound versus nerve stimulation | 15 | 1570 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.21, 0.46] |
| 2.2 ultrasound versus anatomical landmark technique | 2 | 181 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.11, 0.44] |
| 2.3 ultrasound versus transarterial approach | 1 | 56 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.07, 0.85] |
| 3 Time to perform block Show forest plot | 10 | 690 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.41, ‐0.72] |
| 4 Paraesthesia Show forest plot | 6 | 471 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.23, 0.76] |
| 5 Vascular puncture Show forest plot | 5 | 387 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.07, 0.57] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Predicted adequacy of block Show forest plot | 9 | 719 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.33 [2.13, 5.20] |
| 2 Supplementation of block Show forest plot | 9 | 712 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.21, 0.56] |
| 3 Time to perform block Show forest plot | 7 | 587 | Mean Difference (IV, Fixed, 95% CI) | 0.76 [0.55, 0.98] |
| 4 Paraesthesia Show forest plot | 3 | 178 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.30, 3.12] |
| 5 Vascular puncture Show forest plot | 2 | 143 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 0.90] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 By type of intervention/comparison Show forest plot | 10 | 690 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.41, ‐0.72] |
| 1.1 nerve stimulation | 9 | 634 | Mean Difference (IV, Fixed, 95% CI) | ‐1.02 [‐1.37, ‐0.67] |
| 1.2 transarterial approach | 1 | 56 | Mean Difference (IV, Fixed, 95% CI) | ‐3.20 [‐5.76, ‐0.64] |
| 2 By type of nerve block/approach Show forest plot | 10 | 690 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.41, ‐0.72] |
| 2.1 axillary brachial plexus | 6 | 452 | Mean Difference (IV, Fixed, 95% CI) | ‐0.56 [‐0.98, ‐0.14] |
| 2.2 infraclavicular brachial plexus | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | ‐2.41 [‐3.10, ‐1.72] |
| 2.3 popliteal fossa sciatic | 2 | 108 | Mean Difference (IV, Fixed, 95% CI) | 1.00 [‐2.43, 0.44] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 By type of nerve block/approach Show forest plot | 7 | 587 | Mean Difference (IV, Fixed, 95% CI) | 0.76 [0.55, 0.98] |
| 1.1 Axillary brachial plexus block | 4 | 396 | Mean Difference (IV, Fixed, 95% CI) | 0.85 [0.62, 1.07] |
| 1.2 Interscalene brachial plexus | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.6 [‐2.12, 0.92] |
| 1.3 Supraclavicular brachial plexus | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐4.80 [‐7.24, ‐2.36] |
| 1.4 Popliteal fossa sciatic | 1 | 51 | Mean Difference (IV, Fixed, 95% CI) | 0.71 [‐0.07, 1.49] |
| 2 By catheter/no catheter placement Show forest plot | 7 | 587 | Mean Difference (IV, Fixed, 95% CI) | 0.76 [0.55, 0.98] |
| 2.1 No catheter use | 6 | 527 | Mean Difference (IV, Fixed, 95% CI) | 0.79 [0.57, 1.01] |
| 2.2 Catheter placement | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.6 [‐2.12, 0.92] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 By type of intervention/comparison Show forest plot | 6 | 471 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.23, 0.76] |
| 1.1 peripheral nerve stimulation | 5 | 431 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.25, 0.86] |
| 1.2 landmark technique | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.50] |
| 2 By type of nerve block/approach Show forest plot | 6 | 471 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.23, 0.76] |
| 2.1 axillary brachial plexus | 3 | 250 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.19, 1.79] |
| 2.2 infraclavicular brachial plexus | 3 | 221 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.19, 0.76] |

