การให้การศึกษาเรื่องการเลี้ยงลูกด้วยนมแม่ในระหว่างการตั้งครรภ์เพื่อเพิ่มระยะเวลาการเลี้ยงลูกด้วยนมแม่
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT. Using a sealed envelope containing group allocation in blocks of 12, with 6 in the control and 6 in the experimental group. Random assignment was carried out by the lactation consultant giving the educational session. | |
| Participants | Number of women randomised: 75 Inclusion criteria Exclusion criteria Delivered less than 37 weeks | |
| Interventions | Experimental group (n = 37) An additional 1‐h teaching session for nulliparas more than 36 weeks pregnant. The teaching intervention was through a lactation consultant, not involved in the data collection. The content of the teaching session was correct positioning and attachment of the baby on the breast for feeding. Control group (n = 38) Standard educational programme of the study hospital | |
| Outcomes | Outcome measures (dichotomous) Primary
Secondary
Outcome measures (continuous) Primary
Secondary
| |
| Notes | Loss of participants to follow‐up: < 10% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelope (not described whether it was opaque or not) |
| Blinding of participants and personnel (performance bias) | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Only outcome assessors |
| Incomplete outcome data (attrition bias) | Unclear risk | No details available |
| Selective reporting (reporting bias) | Unclear risk | No information |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT | |
| Participants | Number of women randomised: 60 Inclusion criteria English speaking, pregnant, HIV negative women Exclusion criteria Not specified | |
| Interventions | Experimental group (n = 30) BF education by trained LC, incentive, instruction and discussion with handout Control group (n = 30) Prenatal educational regarding benefit and barriers to BF | |
| Outcomes |
| |
| Notes | This study was conducted in New York, USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information available |
| Allocation concealment (selection bias) | Unclear risk | No information available |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information available |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information available |
| Incomplete outcome data (attrition bias) | High risk | Loss to follow‐up in intervention group 36.7% (11/30), in control group 3.3% (1/30) |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Low risk | No other obvious biases |
| Methods | Cluster‐RCT | |
| Participants | Setting: microcredit meetings, Bauchi state, Nigeria, Africa 77 microcredit meeting groups with 461 pregnant women, aged 15‐45 years, attending monthly microcredit meetings for 7‐10 months 39 meeting groups including 229 women were randomised to receive the monthly group BF learning sessions 38 meeting groups including 232 women were randomised to receive standard microcredit group meeting with no BF learning sessions | |
| Interventions | Experimental group (229 women) Monthly group BF learning sessions including weekly cell phone BF text and voice messages to cell phone provided to each small microcredit group and monthly face‐to‐face BF information during microcredit monthly meeting. Information given included: exclusive BF to 6 months; initiation of BF within 1 h of birth; giving only breast milk not fluids during the first 3 days of life for 7‐10 months The messages were generated via songs and dramas by participants Adult learning techniques and participatory principles used with 1‐3 key messages each session including counselling cards for the intervention Control group (232 women) Women in the control clusters received only standard microcredit group meeting with no BF interventions | |
| Outcomes |
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomisation, process not described, other than it happened at the level of the monthly community meeting (clusters) |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not described, but highly unlikely that blinding was possible |
| Blinding of outcome assessment (detection bias) | Low risk | Baseline and final survey interviews were conducted by an independent team of trained data collectors unaware of the clients' study arm assignment |
| Incomplete outcome data (attrition bias) | Low risk | Eligible clients (n = 229 intervention, n = 232 control) were in the randomised meeting groups. At follow‐up, 196 (86%) and 194 (84%) clients remained in the intervention and control arms, respectively |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were published and reported on |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT Random allocation to a control group or 1 or 2 intervention groups, randomised by an external computerised system accessed by telephone by a research midwife | |
| Participants | Number of women randomised: 984 Inclusion criteria Exclusion criteria | |
| Interventions | Experimental group Group 1 (n = 327): 1.5‐h session on practical BF using teaching aids. Latch‐on technique demonstrated with dolls and knitted breasts, also BF complications and management. Plus access standard care available Group 2 (n = 329): two 1‐h sessions that focused on changing attitudes to BF. Women were encouraged to bring their partners or a significant other. Session 1 included information about BF advantages, views and attitudes of participants, their friends and families and society. For session 2, participants were encouraged to interview their own mother or her partner’s mother about attitudes of BF, which then was reflected and discussed in this session. Access standard care available Control group (n = 328) Able to access standard care, which included formal BF education sessions etc | |
| Outcomes | Duration of any BF at 2‐4 d, excluded babies not yet feeding. Duration of exclusive BF at 2‐4 days, excluded babies yet not feeding Number of mothers any BF at 6 months Number of mothers exclusive BF at 6 months | |
| Notes | Loss of participants to follow‐up and reasons: < 10% Blinding: unclear Intention‐to‐treat analysis: used Each intervention group was compared only with the group of women allocated to standard care; they were not compared with each other For this review we have presented separate intervention groups in Comparison 1; where we have totals in the analysis in Comparison 6 we have split the control group between the intervention arms Study was conducted in Melbourne, Australia | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computerized system of biased urn randomisation was accessed by telephone by the research midwife to ascertain women’s group allocation." |
| Allocation concealment (selection bias) | Low risk | "A computerized system of biased urn randomisation was accessed by telephone by the research midwife to ascertain women’s group allocation." |
| Blinding of participants and personnel (performance bias) | High risk | Not described, but very unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | The follow‐up rate in practical skill, attitudes, standard care we re 91%, 90% and 91%, respectively |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT | |
| Participants | 44 consecutive women from 2 upstate New York Women, Infants and Children (WIC) programmes, at least 18 years old, in 4th to 6th month of pregnancy, primigravida or women who had bottle‐fed previous children or who previously had an unsuccessful BF experience were randomly assigned to experimental (21 women) or control (23 women) groups. | |
| Interventions | Experimental group (21 women) 5 pamphlets providing information on the benefits of BF, basic physiology of lactation, proper nursing technique were mailed to the women's homes 1 at a time over 5 consecutive weeks. Control group (23 women) Did not receive pamphlets | |
| Outcomes |
These outcomes were not relevant to the review objective. | |
| Notes | This study was conducted in New York. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not described, but unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Unclear risk | Inadequate information |
| Methods | RCT | |
| Participants | Setting: At 4 participating prenatal clinics between the University of Virginia (UVA) Health System and the Virginia Commonwealth University (VCU) Health System, Virginia in the USA from 2009 to 2012 Inclusion criteria Pregnant women of 24‐41 weeks' gestation who were WIC‐eligible (income of 185% or less of the federal poverty income guidelines) Exclusion criteria Women with multiple‐gestation pregnancy, any known contraindication to BF (e.g. HIV infection, drug use, or receipt of chemotherapy), or their primary language was not English Total numbers of 522 eligible pregnant women were enrolled (459 at UVA, 63 at VCU). No information of how many randomised women of each group was reported | |
| Interventions | Experimental group A 25‐min educational BF video (Better Breastfeeding, Injoy Productions, 2008) provided general information about BF, including importance, latch, hunger cues, positioning, sore nipples, engorgement, how breast milk is made, and lifestyle issues. Total number analysed: 249 Control/Comparison intervention A 20‐min educational video about nutrition during pregnancy (Healthy Pregnancy Nutrition, Injoy Productions, 2007). It covered topics including healthy diet and the importance of exercise during pregnancy. Total number analysed: 248 | |
| Outcomes | Breastfeeding initiation Time of first feeding Any infant complication (hypoglycaemia, rule‐out sepsis, hypothermia, transient tachypnoea of the newborn, other breathing problems, cardiac problem, hyperbilirubinaemia, and others.) Unlikely to be related to the intervention. Also for maternal complications. Infant length of stay in newborn nursery only and never NICU and/or intermediate care Nursery (ICN) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated block randomisation sequence using random block sizes, stratified by prenatal clinic, was used. |
| Allocation concealment (selection bias) | Low risk | One member of the study team with no direct contact with participants prepared all of the consecutively‐numbered, sealed, opaque envelopes, which the research assistant opened just prior to loading the video for the participant to view. |
| Blinding of participants and personnel (performance bias) | High risk | Not described, but highly unlikely that blinding was possible |
| Blinding of outcome assessment (detection bias) | Low risk | Research assistants abstracting data were blinded to the group to which the participant was assigned. |
| Incomplete outcome data (attrition bias) | Low risk | Eligible women were 1580, 522 were randomised but there was no information of assigned number to each group. Analysis was done in 497 women (249 in intervention and 248 in control) account for 95% of the randomised women However, BF outcomes were analysed in 346 (70%; 174/249 for intervention and 69%; 172/248 for control) These were only those who gave BF |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were published and reported on. |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT Women in Monday clinic were randomised with a random number table into 2 intervention groups. Friday clinic became control group (not randomised, therefore data could not be used, both intervention groups data could be compared, as they were randomised) | |
| Participants | Number of women randomised: 74 Inclusion criteria Women 24 weeks' gestation or less Exclusion criteria None mentioned | |
| Interventions | 2 types of prenatal education. Individual BF and antenatal BF class Experimental groups Intervention group 1 (38 women): antenatal group BF class, 50‐80 min, at least 1 session discussing myths, problems and benefits of BF Intervention group 2 (36 women): individual pre‐counselling with a nurse practitioner or paediatrician, one‐to‐one, 15‐30 minutes, between 30‐40 weeks' gestation, similar topics discussed in IG1 Control group Normal antenatal care. No additional information but not randomised, therefore data were excluded, and not included in our analysis. | |
| Outcomes |
| |
| Notes | Loss of participants to follow‐up: 18.2% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers was used |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not described, but highly unlikely |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not enough information |
| Selective reporting (reporting bias) | Unclear risk | Information not available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT | |
| Participants | Number of women randomised: 209 Inclusion criteria Primiparous women who were planning to BF their infants. Exclusion criteria None mentioned | |
| Interventions | Experimental group: 111 women Usual care plus a self‐assessment pre‐workshop guide and an interactive, educational, antenatal workshop. Control group: 98 women Usual care | |
| Outcomes | BF at 3 and 6 months | |
| Notes | This study was conducted in Canada | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Not feasible to blind |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Comparable loss to follow‐up (< 20% at 6 months in both arms) |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Low risk | No other obvious biases |
| Methods | Cluster randomisation of 10 home healthcare centres. Coin flip determined which centres would receive intervention Clusters had comparable overall pre‐randomisation rates and sizes | |
| Participants | Number of women randomised: 781 Inclusion criteria Women considering BF Exclusion criteria Women with babies weighing < 2000 g | |
| Interventions | Experimental group 408 women received standard care and BF booklet, which was used and referred to by caregiver at each consultation (which included practical instructions on BF, discussion around how to cope with BF, motivational discussion to initiate and maintain BF and additional information if asked for). Opportunity to access 24‐hour free lactation consultant Control group 373 received standard antenatal care and BF booklet and phone number for BF questions or BF problems | |
| Outcomes |
| |
| Notes | Loss of participants to follow‐up: < 10% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin flip |
| Allocation concealment (selection bias) | Unclear risk | Coin flip was used |
| Blinding of participants and personnel (performance bias) | High risk | Not described.Not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Not described. Not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Minimal loss to follow‐up in experimental group and no loss to follow‐up in control group |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT | |
| Participants | Number of women randomised: 1193 Inclusion criteria 1193 nulliparous women were recruited before week 21 + 6 days of gestation, 603 were randomised to the intervention group, and 590 to the reference group. The inclusion criteria were nullipara registered at the Aarhus Midwifery Clinic, older than 18 years of age at enrolment,with a singleton pregnancy, and the ability to speak and understand Danish. | |
| Interventions | Experimental group Structured antenatal training programme for 9 h attended in mid‐pregnancy Control group Usual practice (no antenatal training) | |
| Outcomes |
| |
| Notes | This study was conducted in Denmark | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was assigned by one staff midwife using computer voice response system. Randomisation was through an algorithm generated by a data manager. Ratio of 1:1." |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not described, not possible |
| Blinding of outcome assessment (detection bias) | Low risk | Postnatal midwives (personnel) were blinded |
| Incomplete outcome data (attrition bias) | Low risk | 16 out of 603 and 15 out of 590 women in the intervention and reference groups were lost to follow‐up respectively |
| Selective reporting (reporting bias) | Low risk | Reported all outcomes as presented in methods |
| Other bias | Low risk | Baseline characteristics were quite comparable between intervention and reference groups. No other obvious biases |
| Methods | Cluster‐RCT Unit of randomisation: 8 electoral wards in 1 county, pairs were matched according to Jarman Underprivileged area score (UPA) Within‐pair randomised = 4 clusters each Opaque sealed envelopes | |
| Participants | Number of women randomised: 1312 Inclusion criteria Exclusion criteria Women with detected foetal abnormality | |
| Interventions | 1 antenatal BF education session with the woman’s attending community midwife. Midwives were trained for this intervention Experimental group (n = 633) Normal antenatal care plus during third trimester attendance of a single antenatal BF education session. Each session involved up to 8 women and was facilitated by a qualified infant feeding co‐ordinator Control group (n = 679) Received standard antenatal care that included BF advice from attending clinic midwives | |
| Outcomes |
| |
| Notes | Loss of participants to follow‐up: < 10% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes were used |
| Blinding of participants and personnel (performance bias) | High risk | The intervention was not feasible to be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up < 10% in both arms |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Low risk | No other obvious biases |
| Methods | Cluster‐RCT | |
| Participants | 66 antenatal clinics with 2511 pregnant women 33 clinics including 1140 women were randomised to receive the peer support worker service. 33 clinics including 1371 women were randomised to receive standard care. | |
| Interventions | Intervention group (1140 women) An antenatal peer support worker service planning a minimum of 2 contacts with women to provide advice, information, and support from approximately 24 weeks’ gestation within the antenatal clinic or at home. The trained peer support workers were of similar ethnic and socio‐demographic backgrounds to their clinic population. Control group (1371 women) Women in the control clusters received standard antenatal care, which included usual information and advice from midwives on BF without input from community peer support workers. | |
| Outcomes | Initiation of BF obtained from computerised maternity records of the hospitals where women from the primary care trust delivered | |
| Notes | This study was conducted in Birmingham, UK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | The intervention was not feasible to be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Data on outcome were supplied to the research team in an anonymous format |
| Incomplete outcome data (attrition bias) | Low risk | 113 out of 2511 women (4.5%) who participated in the trial were not available for primary outcome assessment |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Low risk | No other obvious biases |
| Methods | Cluster‐RCT A computer‐generated list was used to randomise the women into the 3 groups. Each woman was allocated to the intervention group next on the list after written informed consent had been obtained. Singapore | |
| Participants | Number of women randomised: 401 Inclusion criteria Singleton pregnancy, gestation of at least 36 weeks at recruitment, no uterine scar, and the absence of any obstetric complication that would contraindicate vaginal delivery, with informed consent. Exclusion criteria Not described | |
| Interventions | Multiple versus single Experimental group Group A (n = 123): received an information booklet describing the techniques and benefits of BF, which was written and published by the hospital’s BF support group. It contained practical advice on feeding techniques, expressing breast milk, and management of common BF problems. Participants also watched a 16‐min educational video entitled “14 Steps to Better BF” (InJoy Videos, Boulder, CO), in which the benefits of BF were introduced, correct positioning, latch‐on, and breast care were demonstrated, and common concerns (such as nipple pain) discussed. In addition, each woman had one 15‐minute session with a lactation counsellor who examined the woman’s nipples to assess adequacy for BF and answered questions on BF. Group B (n = 132) received the same booklet and watched the same video but did not have an individual session with the lactation counsellor. Control group Group C (n = 146) Did not watch the video, and did not have counselling. The primary report stated that the control group did not receive the booklet, video or counselling (Mattar 2007 p. 74) All women in all randomised groups had standard care during pregnancy, including access to postnatal BF support. | |
| Outcomes |
| |
| Notes | Loss of participants to follow‐up: 10% Comparison 4 includes the 2 treatment arms A and B | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list |
| Allocation concealment (selection bias) | Low risk | Each woman was allocated to the intervention group next on the list after written informed consent had been obtained. |
| Blinding of participants and personnel (performance bias) | High risk | The intervention was not feasible to be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up 10% |
| Selective reporting (reporting bias) | Unclear risk | Information not available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT | |
| Participants | Number of women randomised: 101 inclusion criteria Nulliparous women expecting a single child, an uncomplicated birth, and planning to BF The women had to read and write in English and have a telephone to complete the postpartum questionnaires. To remain in the study, a mother and her infant had to be discharged at the same time and be able to BF without restriction. Exclusion criteria Not described | |
| Interventions | Workshop Experimental group (n = 47) Standard care plus a 2.5‐h prenatal BF workshop designed using Bandura's theory of self‐efficacy and adult learning principles. The intervention involved the use of lifelike dolls, videos, and discussion in a comfortable atmosphere. Control group (n = 45) Standard care | |
| Outcomes |
| |
| Notes | This study was conducted in Ontario, Canada | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information not available |
| Allocation concealment (selection bias) | Low risk | Used sealed, sequentially numbered, opaque envelope containing a slip of paper stating either Control or Workshop |
| Blinding of participants and personnel (performance bias) | High risk | The intervention was not feasible to be blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Only outcome evaluators |
| Incomplete outcome data (attrition bias) | Low risk | Analysed the data with both the intention‐to‐treat assumption and using the actual workshop attendance. 101 randomised and 92 were available for analysis |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT | |
| Participants | Number of women randomised: 182 Inclusion criteria Pregnant women enrolled for prenatal care at 24 weeks (or beyond) who consented to participate. Exclusion criteria Age < 18 years, stated intention to bottle‐feed with formula, non‐English speaking, those for whom BF was medically contraindicated, those whose newborns would be anticipated to be incapable of BF, no access to telephone for follow‐up and those who were not planning to keep or raise their baby. | |
| Interventions | Experimental group 2‐h BF self‐efficacy theory‐based class (86 women) Control group No class (96 women) | |
| Outcomes |
| |
| Notes | This trial was conducted in Texas, USA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not feasible to blind |
| Blinding of outcome assessment (detection bias) | High risk | Quote "A research assistant was used for all postpartum data collection by phone. Although she did have access to the information regarding the subjects’ group assignment, she did not refer to this information when doing the phone interviews, in effect blinding her to their status. In this way, there was greater objectivity both by the interviewer and the interviewee." |
| Incomplete outcome data (attrition bias) | Low risk | Quote "The overall dropout rate was 7.7%." |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Low risk | No obvious baseline differences and other biases |
| Methods | RCT in parallel arms | |
| Participants | Setting: Arkansas department of Health USA Inclusion criteria Primiparous pregnant women on WIC with an expected due date greater than 2 months post‐enrolment, ages of 20 and 30, have access to email and the Internet and provide written consent to participate to completion. Exclusion Criteria Women identified as substance abusers on their ADH WIC‐5 record, received WIC in counties served by BF peer counsellors and BF contraindicated for any of the following reasons:
145 pregnant women on WIC were screened by Health Department nutritionists for eligibility and willingness to participate in the study. 23 participants completed consent and pre‐test forms, were randomly assigned to groups, and participated in the study. | |
| Interventions | Experimental group 6 weeks of peer counsellor‐guided web‐based education and support related to BF practices. In addition, the usual care of nursing and nutrition visits at the health department local health unit and written materials per Arkansas Department of Health (ADH) policy and procedure guidelines were given to the participants. Control group Usual care consisted of non‐web‐based interventions, such as face‐to‐face counselling and education and the distribution of written materials. | |
| Outcomes | Breastfeeding self‐efficacy None of our pre‐specified outcomes were reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Eligible subjects were randomly assigned to either the intervention group or the control group using a computer‐generated 2‐block random number generator in a 1:1 ratio. |
| Allocation concealment (selection bias) | Unclear risk | As above |
| Blinding of participants and personnel (performance bias) | High risk | Intervention could not be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information available |
| Incomplete outcome data (attrition bias) | Low risk | Data on all participants who were randomly assigned was analysed in the groups to which they were allocated on an intention‐to‐treat basis. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were published and reported |
| Other bias | Unclear risk | No information available |
| Methods | Single‐centre RCT | |
| Participants | 100 pregnant women and their partners randomised Inclusion criteria Women in the second trimester of pregnancy with no underlying disease or pregnancy complication. Exclusion criteria No details given | |
| Interventions | Intervention group The case group was provided with an educational package on promoting fathers’ participation. They attended 3 training sessions where they were trained by brochures. Control group Given no intervention | |
| Outcomes |
| |
| Notes | Trial conducted at family health research centre in Tehran, Iran | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was performed according to the table of random numbers." |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding of participants and personnel (performance bias) | High risk | Not described but very unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Results presented as text (no tables) but appears all data for all participants reported |
| Selective reporting (reporting bias) | Low risk | All outcomes reported and published |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT, did not describe how randomisation was done | |
| Participants | Number of women randomised: convenience sample of 194 pregnant women Inclusion criteria
Exclusion criteria Unforeseen circumstances (miscarriage, stillbirth, change of address) | |
| Interventions | Culture and language‐specific educational programme Experimental group A 25‐min videotape programme followed by a series of 3 x 2 h of small group discussion sessions conducted in Vietnamese. Control group BF and childbirth pamphlets | |
| Outcomes |
| |
| Notes | Loss of participants to follow‐up: < 10% Blinding: Intention‐to‐treat analysis: unclear This study was conducted in Sydney, Australia. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not described but highly unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Loss to follow‐up < 10% in both arms |
| Selective reporting (reporting bias) | Unclear risk | Information not available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT | |
| Participants | Total number of women randomised: 54 Pregnant women, at least 18 years old, English speaking, able to read and write, received prenatal care and could attend 4 visits before delivery, low income, having access to telephone, undecided about BF method during initial contact with researchers | |
| Interventions | Intervention group (26 women) Educational program (Best Start) included:
Control group (28 women) No exposure to the programme | |
| Outcomes |
| |
| Notes | This study was conducted in Houston, Texas, USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Women selected a sealed envelope. No information about envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Not described, unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT. Method of randomisation was not described | |
| Participants | Number of women randomised: 30 Inclusion criteria Low‐risk primigravida, Hispanic, in their third trimester, received care at Sedgwick, not planning to work outside the home for 6 months. Exclusion criteria Not described | |
| Interventions | Prenatal BF education Experimental group Level 1: the researcher approached the expectant mother. All participants confirmed that they planned to BF. Contents included benefits of BF. Charts and pictures were used to present supply‐and‐demand concept and prenatal breast preparation. Early and consistent BF practices were emphasised. A doll was used as a model for instruction about holding and positioning the baby and BF discreetly. Level 2: completed first level. Participants were introduced the concept of “baby quarantine” ( nothing enters the baby’s mouth except the mother’s breast for at least 40 days after birth. The benefits of avoiding bottles, pacifier and supplementation to promote establishment of milk for successful BF were reinforced. BF commitment was encouraged through the use of checklist Control group Standard care offered advice to BF and handouts were distributed during the initial prenatal visit | |
| Outcomes |
| |
| Notes | Loss of participants to follow‐up: 17%. This study was conducted in Kansas, USA. Schlickau 2005b is a thesis which included three parts: Part 1) Qualitative study Part 2) Multiple arm study of 30 women with a control group, a BF workshop (level 1), and a BF workshop with introduction to concept of 'baby quarantine' (level 2). Part 2 is reported in Schlickau 2005a. Part 3) 86 women randomised to either control or BF education workshop. Part 3 results are presented under Schlickau 2005b. Part 2 results are presented under Schlickau 2005a. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not described but unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Loss of participants to follow‐up: 17% |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Unclear risk | Not enough information |
| Methods | RCT | |
| Participants | Number of women randomised: 86 Inclusion criteria Primigravida, immigrant Hispanic women aged 15‐45 , 32‐36 weeks' gestation, stable family situation, had a work situation compatible with BF for 6 weeks, had normal nipple assessment Exclusion criteria Homeless, not in a temporary agencies or shelter, high‐risk pregnancies, serious illness of the newborn or mother that precluded BF, stillbirth, unforeseen family situation | |
| Interventions | Prenatal BF education Experimental group (44) BF education workshop Control group (42) Standard care | |
| Outcomes |
| |
| Notes | This study was conducted in Kansas, USA. Schlickau 2005b is a thesis which included three parts: Part 1) Qualitative study Part 2) Multiple arm study of 30 women with a control group, a BF workshop (level 1), and a BF workshop with introduction to concept of 'baby quarantine' (level 2). Part 2 is reported in Schlickau 2005a. Part 3) 86 women randomised to either control or BF education workshop. Part 3 results are presented under Schlickau 2005b. Part 2 results are presented under Schlickau 2005a. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Manila packet sealed envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Not described but unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up in intervention group (9.1%, 2/44), in control group (9.5 %, 4/42) |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT. Random number table was used. Method of randomisation (allocation) was not described. | |
| Participants | Number of women randomised: 156 Nulliparous women, 18 years or older, with a foetus of gestational age of 28 weeks or less, who had not yet selected a paediatrician or wanted their infants to receive paediatric care at the hospital‐based paediatric clinic | |
| Interventions | LC plus standard BF education (81 women) versus standard BF education (75 women) | |
| Outcomes |
| |
| Notes | This study was conducted in Baltimore, USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not described but unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up 7.7% |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT. Method of randomisation was not described | |
| Participants | Number randomised: not clear (59 couples completed study) 567 expectant mothers were approached during 1st and 2nd trimester, refused to participate 24%; lost during prenatal period 36%; lack of involvement with father 8%; fathers refusal to participate 11%; fathers’ failure after enrolling 9%, completed the study with 59 couples Inclusion criteria Women who sought prenatal care in the resident and faculty practices at Johns Hopkins Hospital Exclusion criteria Not described | |
| Interventions | Classroom discussion on infant care and BF for expectant fathers Experimental group (27 fathers) Groups of 4‐12 expectant fathers attending the classroom with open discussion about BF and support each other to be advocates for BF among fathers in the groups, facilitated by a man who was himself a father. 2‐h classes used a variety of teaching media were held approximately every 2 weeks Control group (32 fathers) The class covered topics related to infant care and safety only using the same facilitator, and methods of interactive and informal education as of those the intervention group. These subjects did not receive the intervention class that contained the BF content. | |
| Outcomes |
| |
| Notes | Loss of participants to follow‐up: 36% Blinding: Intention‐to‐treat analysis: not used This study was conducted in Baltimore, USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Not described but unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | Loss to follow‐up 36% |
| Selective reporting (reporting bias) | Unclear risk | No information available |
| Other bias | Low risk | No other obvious biases |
| Methods | RCT | |
| Participants | Setting: 2 study hospitals based on the geographic representativeness and high volume of eligible mothers in Hong Kong Inclusion criteria: pregnant women with 1) 18 years of age or older; 2) Cantonese‐speaking; 3) primiparous; 4) at least 35 weeks of gestation; 5) a singleton pregnancy; 6) no serious medical or obstetric complications; 7) intending to breastfeed; and 8) planning to stay in Hong Kong for at least 6 months after delivery Exclusion criteria: being not entitled to health benefits in Hong Kong, not a Hong Kong resident, or both Recruitment period: Jan‐June 2013 Follow‐up completed: Dec 2013 Total numbers of 469 eligible pregnant women were enrolled and randomised (233 to intervention and 236 to standard care) | |
| Interventions | Experimental group (233 women) Standard care plus one‐to‐one (20‐30 min) BF education and support session based on WHO guideline for baby‐friendly hospitals and evidence‐based maternity care. The intervention was given immediately after randomisation in a private room in the antenatal clinics to minimise contamination between the two treatment groups. Control group (236 women) Standard antenatal care: standard maternal and foetal health checks by either clinic midwives or obstetricians along with health education to promote a healthy pregnancy. | |
| Outcomes | Exclusive BF at 6 weeks, 3 and 6 months postpartum. Overall duration of any and exclusive BF (age in weeks when the infant first ingested formula and ceased BF completely, respectively) across the first 6 months postpartum. | |
| Notes | This study was conducted in Hong Kong. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent researcher who did not participate in participant recruitment or data collection generated the allocation sequence using the statistical software Stata13.1. |
| Allocation concealment (selection bias) | Low risk | Allocation sequences were kept in sequentially numbered, opaque, sealed envelopes. The research nurse opened up the next envelope in the sequence to determine the assigned group after a pregnant woman had agreed to participate and had signed the written consent form. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of the research nurse or the participants was not possible given the nature of the intervention. |
| Blinding of outcome assessment (detection bias) | Low risk | The BF follow‐up data were collected by a research assistant who was blinded to the participants’ group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | 443 (94.5% of 469), 222 (95.3% of 233) in intervention and 221 (93.6% of 236)in standard care, completed all follow‐up to 6 months postpartum or until weaned. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were published and reported on. |
| Other bias | Low risk | Comparable baseline characteristics between intervention and standard care groups presented |
BF: breastfeeding
LC: lactation consultation
NTI: nipple trauma index
RCT: randomised controlled trial
VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not RCT | |
| Not only antenatal BF education. 9 home visits were provided in the 6‐month postpartum period. | |
| Not only antenatal BF education. Peer counsellors also gave postpartum visits. | |
| Not only antenatal BF education. Home visits extended to 6 months postpartum. | |
| Not only antenatal BF education. Lactation consultants also made postpartum hospital or home visits. | |
| Included both pre and postnatal interventions. | |
| Not only antenatal BF education. Lactation consultants provided support in the postpartum period and until infants up to 1 year of age. | |
| Not only antenatal BF education. Peer counsellors followed up women in the postpartum period as long as they continued to breastfeed. | |
| Not only antenatal BF education. Peer counselling extended to postpartum period. | |
| Included both pre and postnatal interventions | |
| Not only antenatal BF education. Doula home visits extended to postpartum period. | |
| Animated computer agent used prenatally during a third trimester office visit and perinatally at discharge from the hospital plus usual care. The perinatal dialogue, delivered in the hospital, focused on essential information that mothers need the most in their first 3 days of BF (‘‘breastfeeding 101’’). The perinatal dialogue also focused on addressing the most commonly asked questions by new BF mothers and motivating adherence to the CDC‐recommended 6 months of exclusive BF goal. | |
| Not only antenatal BF education. Support was also provided at 3‐day, 3‐month and 9‐month postpartum. | |
| Not RCT, objective not relevant | |
| Not related to BF | |
| Not only antenatal BF education; a home visit was also provided postnatally. | |
| Not only antenatal BF education. Lactation counsellors provided postnatal support by telephone or home visits. | |
| Not RCT (letter to editor commenting on non‐RCT papers). | |
| Not RCT | |
| Not RCT | |
| Post‐natal interventions | |
| Intervention was not antepartum BF education | |
| Nutritional education not BF education | |
| Not RCT | |
| Not RCT | |
| Not only antenatal BF education. Home visits continued after delivery until the infant was 12 months | |
| Included pregnant and post‐partum women and 3‐month postpartum intervention | |
| Not antenatal BF education (only protocol) | |
| Included both pre and postnatal interventions (Only protocol) | |
| Not only antenatal BF education. Document on BF was provided, that affects BF behaviour of postpartum mothers. | |
| Not RCT | |
| Not RCT (letter to editor with comments on non‐RCT papers). | |
| Not RCT | |
| Not RCT, did not evaluate antenatal BF education | |
| Not only prenatal BF education intervention. Peer counsellors also visited mothers at 1st, 2nd, 4th and 8th week postpartum. | |
| Not only prenatal BF education intervention. Peer supporters provided support up to 16 weeks postpartum. | |
| Not only prenatal BF education intervention. Counseling during the antenatal period, at delivery and during the immunisation visits. | |
| Postnatal education intervention | |
| Included postnatal intervention | |
| Not RCT | |
| Not RCT | |
| Not only prenatal BF education intervention. Lactation consultant also provided support postnatally. | |
| Participants were not pregnant women. | |
| Not only antenatal BF educational intervention. Lactation counsellors also visited women after delivery. | |
| Not RCT | |
| Not RCT (systematic assignment) | |
| Not RCT | |
| Not only antenatal BF education. Following the birth of a prenatally enrolled target child, the Family Support Workers (FSW) typically made a visit to the newborn’s mother in the hospital. During this visit, the FSW assisted programme group mothers with any problems initiating BF. After hospital discharge, FSWs continued to offer programme group mothers information and support in the home on a weekly basis. | |
| Not only antenatal BF education. BF incentives were given pre and postnatally. | |
| Not RCT of antenatal BF education. | |
| Peer counsellor, the intervention was performed at pre and post delivery. | |
| Included antenatal and postnatal interventions. | |
| Included antenatal and postnatal interventions. | |
| Not only antenatal BF education. Lactation support was also provided in the postpartum period. | |
| Participants were not pregnant women. They were health professionals. | |
| Not yet recruited | |
| Not only antenatal BF education. Paraprofessional delivered home visit education during the postpartum period. | |
| Not RCT | |
| Not only antenatal BF education. Lactation consultant and peer counselling extended through 4 weeks postpartum. | |
| Included antenatal and postnatal interventions. | |
| Not antenatal BF education. | |
| Intervention was not antenatal BF education. | |
| Participants were not pregnant women. | |
| Not RCT | |
| Participants were not pregnant women. |
BF: breastfeeding
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting translation |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Awaiting translation |
BF: breastfeeding
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A study to prolong BF duration: design and rationale of the Parent Infant Feeding Initiative (PIFI) randomised controlled trial |
| Methods | Four‐arm, factorial randomised controlled trial of partners of pregnant women |
| Participants | Male partners of pregnant women |
| Interventions | Control group (CG) ‐ usual care Medium intensity intervention 1 (MI1) ‐ specialised antenatal classes for partners with supporting printed materials Medium intensity intervention 2 (MI2) ‐ antenatal and postnatal social support delivered via smartphone application (exclude‐ involves postnatal intervention) High intensity intervention ‐ specialised antenatal classes and antenatal and postnatal social support delivered via smartphone application (exclude‐ involves postnatal intervention) |
| Outcomes | Primary outcomes |
| Starting date | |
| Contact information | [email protected] |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of any breastfeeding Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1 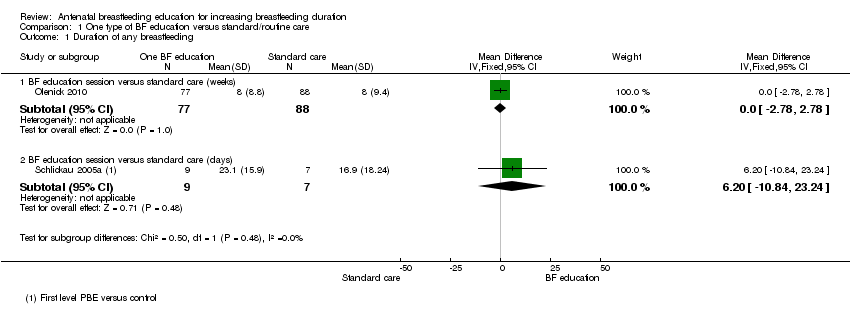 Comparison 1 One type of BF education versus standard/routine care, Outcome 1 Duration of any breastfeeding. | ||||
| 1.1 BF education session versus standard care (weeks) | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐2.78, 2.78] |
| 1.2 BF education session versus standard care (days) | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 6.20 [‐10.84, 23.24] |
| 2 Any breastfeeding at 3 months Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2 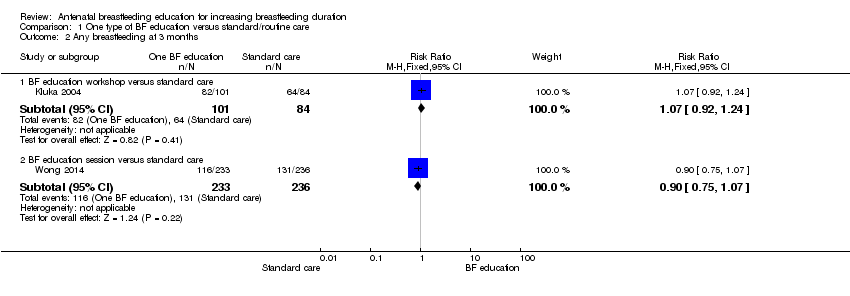 Comparison 1 One type of BF education versus standard/routine care, Outcome 2 Any breastfeeding at 3 months. | ||||
| 2.1 BF education workshop versus standard care | 1 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.92, 1.24] |
| 2.2 BF education session versus standard care | 1 | 469 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.75, 1.07] |
| 3 Any breastfeeding at 6 months Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 One type of BF education versus standard/routine care, Outcome 3 Any breastfeeding at 6 months. | ||||
| 3.1 BF education workshop versus standard care | 1 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.87, 1.51] |
| 3.2 BF practical skills versus standard care | 1 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.87, 1.17] |
| 3.3 BF attitude education versus standard care | 1 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.79, 1.07] |
| 3.4 BF education session versus standard care | 2 | 569 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.86, 1.19] |
| 4 Exclusive breastfeeding at 3 months Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 One type of BF education versus standard/routine care, Outcome 4 Exclusive breastfeeding at 3 months. | ||||
| 4.1 BF education workshop versus standard care | 1 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.84, 1.38] |
| 4.2 BF education session versus standard care | 2 | 637 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.85, 1.30] |
| 5 Exclusive breastfeeding at 6 months Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.5 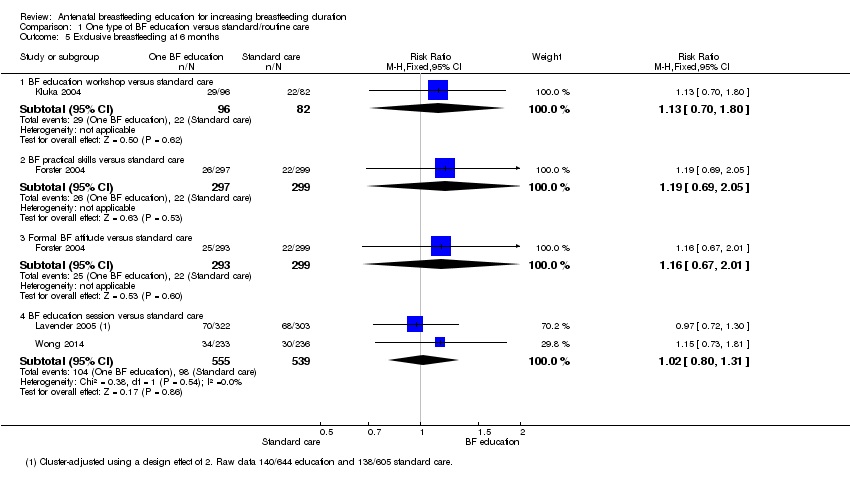 Comparison 1 One type of BF education versus standard/routine care, Outcome 5 Exclusive breastfeeding at 6 months. | ||||
| 5.1 BF education workshop versus standard care | 1 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.70, 1.80] |
| 5.2 BF practical skills versus standard care | 1 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.69, 2.05] |
| 5.3 Formal BF attitude versus standard care | 1 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.67, 2.01] |
| 5.4 BF education session versus standard care | 2 | 1094 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.80, 1.31] |
| 6 Initiation of breastfeeding Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.6 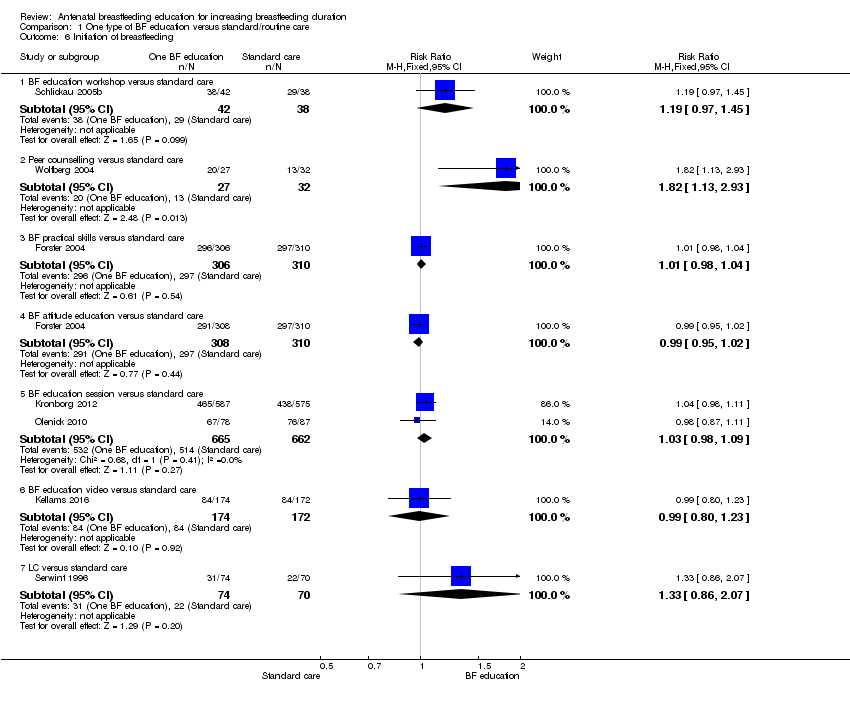 Comparison 1 One type of BF education versus standard/routine care, Outcome 6 Initiation of breastfeeding. | ||||
| 6.1 BF education workshop versus standard care | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.97, 1.45] |
| 6.2 Peer counselling versus standard care | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.82 [1.13, 2.93] |
| 6.3 BF practical skills versus standard care | 1 | 616 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.98, 1.04] |
| 6.4 BF attitude education versus standard care | 1 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.95, 1.02] |
| 6.5 BF education session versus standard care | 2 | 1327 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.98, 1.09] |
| 6.6 BF education video versus standard care | 1 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.80, 1.23] |
| 6.7 LC versus standard care | 1 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.86, 2.07] |
| 7 Initiation of BF (cluster‐randomised trial) Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 One type of BF education versus standard/routine care, Outcome 7 Initiation of BF (cluster‐randomised trial). | ||||
| 7.1 Peer counselling versus standard care | 1 | 2398 | Odds Ratio (Fixed, 95% CI) | 1.11 [0.86, 1.43] |
| 7.2 Group LC session versus standard care | 1 | 1249 | Odds Ratio (Fixed, 95% CI) | 1.20 [0.80, 1.80] |
| 8 Mastitis Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.8 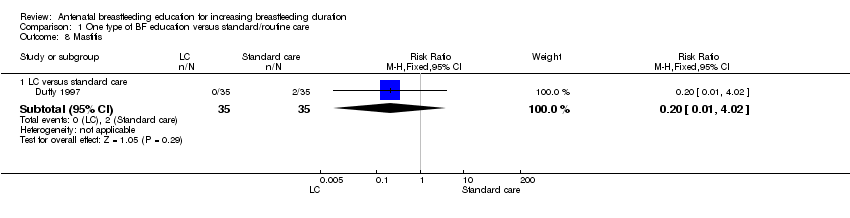 Comparison 1 One type of BF education versus standard/routine care, Outcome 8 Mastitis. | ||||
| 8.1 LC versus standard care | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 9 Breastfeeding complication (nipple pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.9  Comparison 1 One type of BF education versus standard/routine care, Outcome 9 Breastfeeding complication (nipple pain). | ||||
| 9.1 LC versus standard care | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐19.8 [‐23.23, ‐16.37] |
| 10 Breastfeeding complication (nipple trauma) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.10 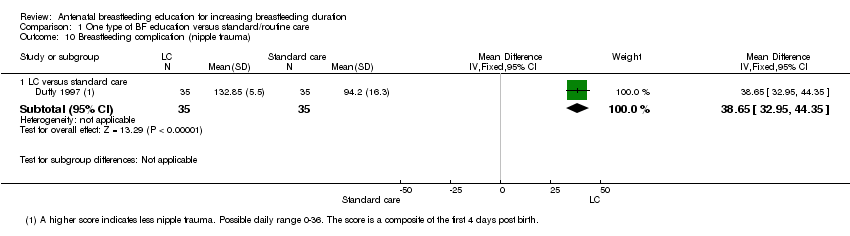 Comparison 1 One type of BF education versus standard/routine care, Outcome 10 Breastfeeding complication (nipple trauma). | ||||
| 10.1 LC versus standard care | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | 38.65 [32.95, 44.35] |
| 11 Breastfeeding problems Show forest plot | 1 | 1162 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.70, 1.43] |
| Analysis 1.11  Comparison 1 One type of BF education versus standard/routine care, Outcome 11 Breastfeeding problems. | ||||
| 11.1 BF education session versus standard care | 1 | 1162 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.70, 1.43] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any breastfeeding at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 One type of BF education versus a different type of BF education, Outcome 1 Any breastfeeding at 3 months. | ||||
| 1.1 Group education versus individual education | 1 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.84 [0.61, 13.18] |
| 2 Any breastfeeding at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.2 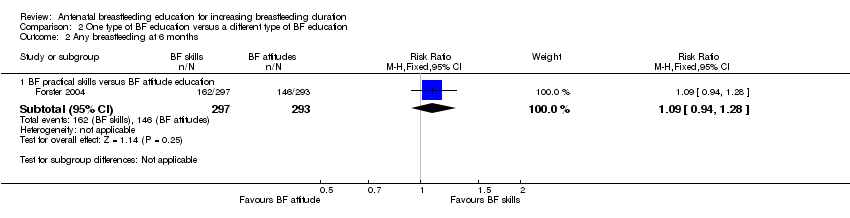 Comparison 2 One type of BF education versus a different type of BF education, Outcome 2 Any breastfeeding at 6 months. | ||||
| 2.1 BF practical skills versus BF attitude education | 1 | 590 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.94, 1.28] |
| 3 Exclusive breastfeeding at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2 One type of BF education versus a different type of BF education, Outcome 3 Exclusive breastfeeding at 6 months. | ||||
| 3.1 BF practical skills versus BF attitude education | 1 | 590 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.61, 1.73] |
| 4 Initiation of BF Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.4  Comparison 2 One type of BF education versus a different type of BF education, Outcome 4 Initiation of BF. | ||||
| 4.1 BF practical skills versus BF attitude education | 1 | 614 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.99, 1.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of any breastfeeding (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.1  Comparison 3 Multiple methods of BF education versus a single method of BF education, Outcome 1 Duration of any breastfeeding (days). | ||||
| 1.1 BF education session plus commitment to exclusive BF versus BF education session | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 8.0 [‐6.84, 22.84] |
| 2 Any breastfeeding at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 Multiple methods of BF education versus a single method of BF education, Outcome 2 Any breastfeeding at 6 months. | ||||
| 2.1 Video + education session versus pamphlets | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [0.86, 2.94] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any breastfeeding at 4 months (cluster‐randomised trial) Show forest plot | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| Analysis 4.1  Comparison 4 Different combinations of multiple methods of providing BF education, Outcome 1 Any breastfeeding at 4 months (cluster‐randomised trial). | ||||
| 1.1 LC + BF booklet + 24 h free LC versus BF booklet + phone number for BF questions and problems. | 1 | 698 | Odds Ratio (Fixed, 95% CI) | 0.82 [0.58, 1.16] |
| 2 Exclusive breastfeeding at 3 months Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| Analysis 4.2  Comparison 4 Different combinations of multiple methods of providing BF education, Outcome 2 Exclusive breastfeeding at 3 months. | ||||
| 2.1 LC + BF booklet + 24 hrs free LC versus BF booklet + phone number for BF questions and problems. | 1 | 698 | Odds Ratio (Fixed, 95% CI) | 0.79 [0.57, 1.09] |
| 2.2 BF booklet + video + LC versus BF booklet + video | 1 | 150 | Odds Ratio (Fixed, 95% CI) | 1.40 [0.70, 2.80] |
| 3 Exclusive breastfeeding at 6 months Show forest plot | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| Analysis 4.3  Comparison 4 Different combinations of multiple methods of providing BF education, Outcome 3 Exclusive breastfeeding at 6 months. | ||||
| 3.1 BF booklet + video + LC versus BF booklet + video | 1 | 169 | Odds Ratio (Fixed, 95% CI) | 2.50 [1.00, 6.25] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of any breastfeeding (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.1 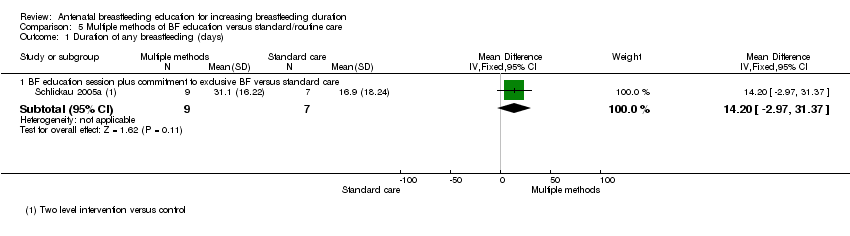 Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 1 Duration of any breastfeeding (days). | ||||
| 1.1 BF education session plus commitment to exclusive BF versus standard care | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 14.20 [‐2.97, 31.37] |
| 2 Exclusive breastfeeding at 3 months Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| Analysis 5.2  Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 2 Exclusive breastfeeding at 3 months. | ||||
| 2.1 BF booklet + video + LC versus standard care | 1 | 159 | Odds Ratio (Fixed, 95% CI) | 2.60 [1.25, 5.40] |
| 2.2 BF booklet + video versus standard care | 1 | 159 | Odds Ratio (Fixed, 95% CI) | 1.80 [0.80, 4.05] |
| 2.3 Monthly BF session + weekly cell phone message versus standard care | 1 | 390 | Odds Ratio (Fixed, 95% CI) | 1.80 [1.10, 2.95] |
| 3 Exclusive breastfeeding at six months Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| Analysis 5.3  Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 3 Exclusive breastfeeding at six months. | ||||
| 3.1 BF booklet + video + LC versus standard care | 1 | 175 | Odds Ratio (Fixed, 95% CI) | 2.40 [1.00, 5.76] |
| 3.2 BF booklet + video versus standard care | 1 | 184 | Odds Ratio (Fixed, 95% CI) | 0.90 [0.30, 2.70] |
| 3.3 Monthly BF session + weekly cell phone message versus standard care | 1 | 390 | Odds Ratio (Fixed, 95% CI) | 2.40 [1.40, 4.11] |
| 4 Initiation of breastfeeding Show forest plot | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| Analysis 5.4  Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 4 Initiation of breastfeeding. | ||||
| 4.1 Monthly BF session + weekly cell phone message versus standard care | 1 | 380 | Odds Ratio (Fixed, 95% CI) | 2.61 [1.61, 4.24] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Initiation of breastfeeding Show forest plot | 8 | 3505 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.94, 1.09] |
| Analysis 6.1  Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 1 Initiation of breastfeeding. | ||||
| 2 Exclusive breastfeeding at 3 months Show forest plot | 3 | 822 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.90, 1.25] |
| Analysis 6.2 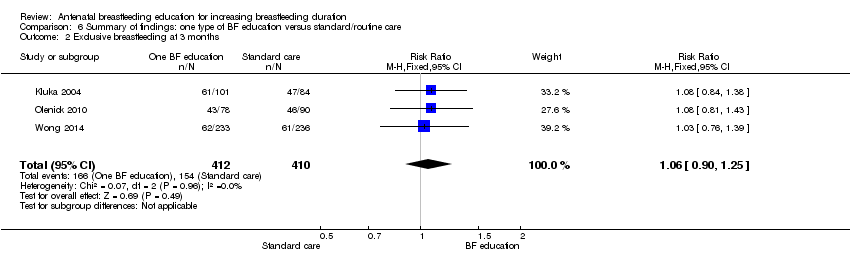 Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 2 Exclusive breastfeeding at 3 months. | ||||
| 3 Exclusive breastfeeding at 6 months Show forest plot | 4 | 2161 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.87, 1.30] |
| Analysis 6.3  Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 3 Exclusive breastfeeding at 6 months. | ||||
| 4 Any breastfeeding at 3 months Show forest plot | 2 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.82, 1.18] |
| Analysis 6.4  Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 4 Any breastfeeding at 3 months. | ||||
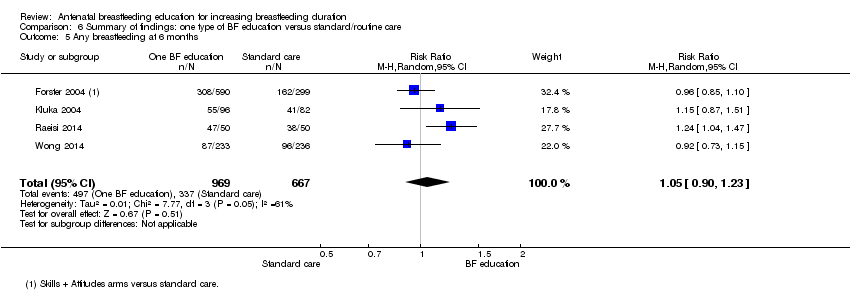
| 5 Any breastfeeding at 6 months Show forest plot | 4 | 1636 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.90, 1.23] |
| Analysis 6.5 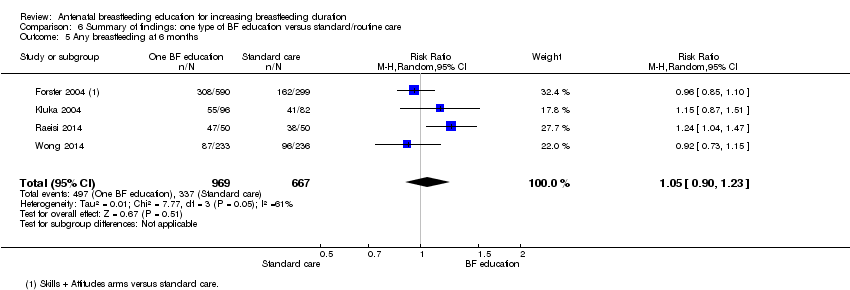 Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 5 Any breastfeeding at 6 months. | ||||
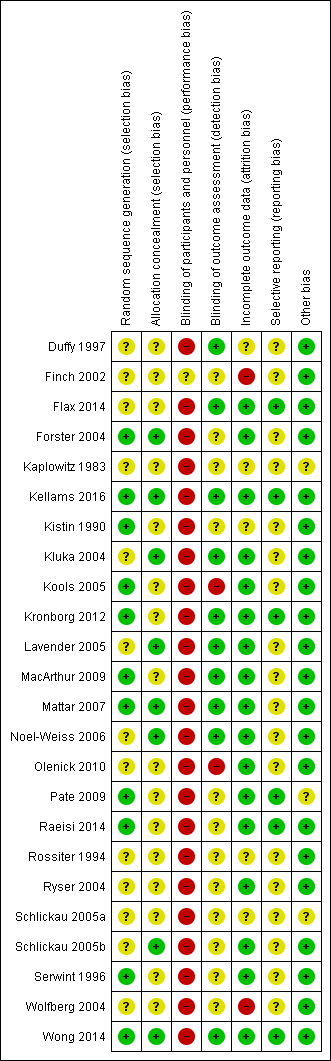
Methodological quality summary: review authors' judgements about each methodological quality item for each included study

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies

Comparison 1 One type of BF education versus standard/routine care, Outcome 1 Duration of any breastfeeding.

Comparison 1 One type of BF education versus standard/routine care, Outcome 2 Any breastfeeding at 3 months.
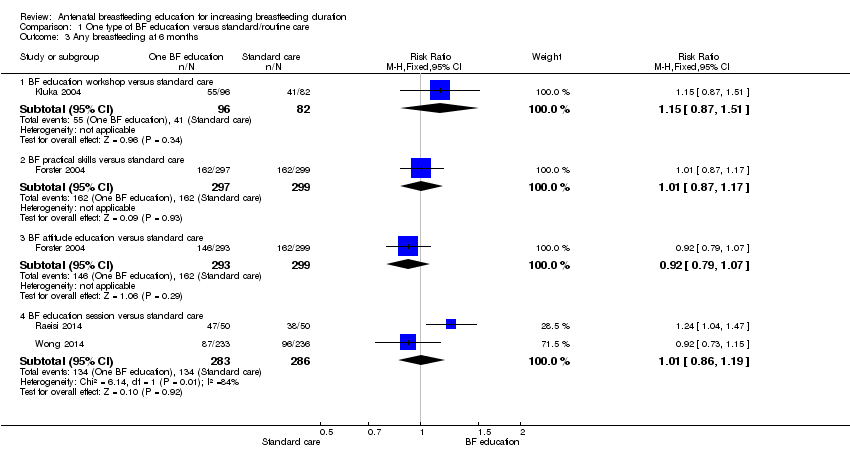
Comparison 1 One type of BF education versus standard/routine care, Outcome 3 Any breastfeeding at 6 months.
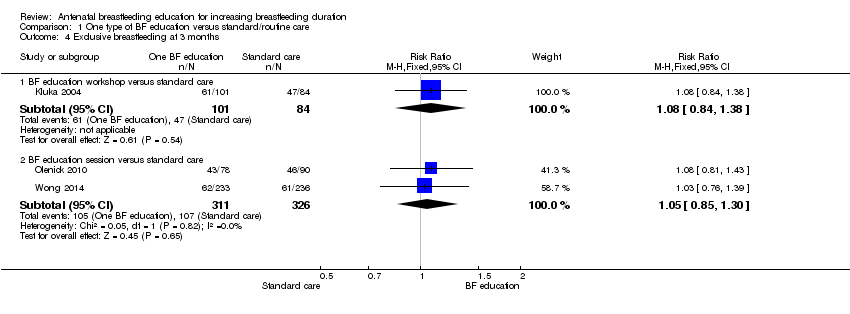
Comparison 1 One type of BF education versus standard/routine care, Outcome 4 Exclusive breastfeeding at 3 months.

Comparison 1 One type of BF education versus standard/routine care, Outcome 5 Exclusive breastfeeding at 6 months.

Comparison 1 One type of BF education versus standard/routine care, Outcome 6 Initiation of breastfeeding.

Comparison 1 One type of BF education versus standard/routine care, Outcome 7 Initiation of BF (cluster‐randomised trial).

Comparison 1 One type of BF education versus standard/routine care, Outcome 8 Mastitis.

Comparison 1 One type of BF education versus standard/routine care, Outcome 9 Breastfeeding complication (nipple pain).

Comparison 1 One type of BF education versus standard/routine care, Outcome 10 Breastfeeding complication (nipple trauma).
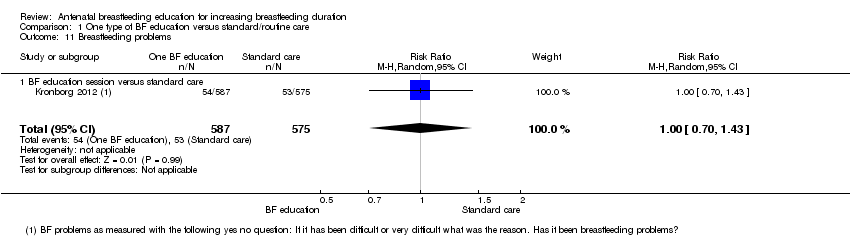
Comparison 1 One type of BF education versus standard/routine care, Outcome 11 Breastfeeding problems.

Comparison 2 One type of BF education versus a different type of BF education, Outcome 1 Any breastfeeding at 3 months.

Comparison 2 One type of BF education versus a different type of BF education, Outcome 2 Any breastfeeding at 6 months.

Comparison 2 One type of BF education versus a different type of BF education, Outcome 3 Exclusive breastfeeding at 6 months.
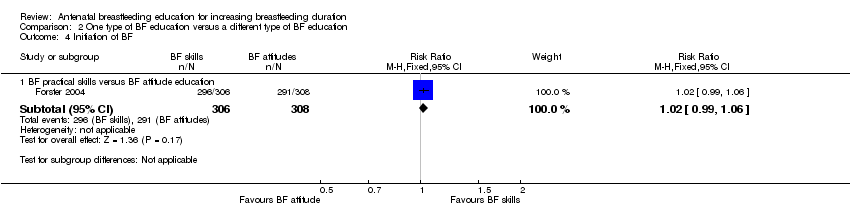
Comparison 2 One type of BF education versus a different type of BF education, Outcome 4 Initiation of BF.

Comparison 3 Multiple methods of BF education versus a single method of BF education, Outcome 1 Duration of any breastfeeding (days).

Comparison 3 Multiple methods of BF education versus a single method of BF education, Outcome 2 Any breastfeeding at 6 months.

Comparison 4 Different combinations of multiple methods of providing BF education, Outcome 1 Any breastfeeding at 4 months (cluster‐randomised trial).

Comparison 4 Different combinations of multiple methods of providing BF education, Outcome 2 Exclusive breastfeeding at 3 months.
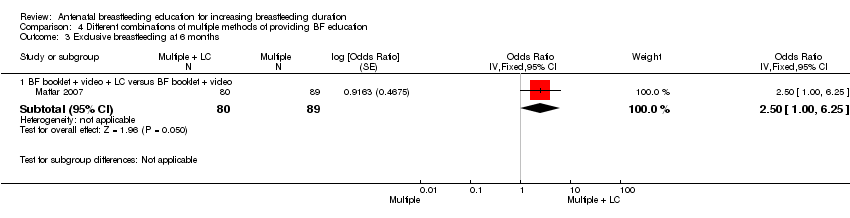
Comparison 4 Different combinations of multiple methods of providing BF education, Outcome 3 Exclusive breastfeeding at 6 months.
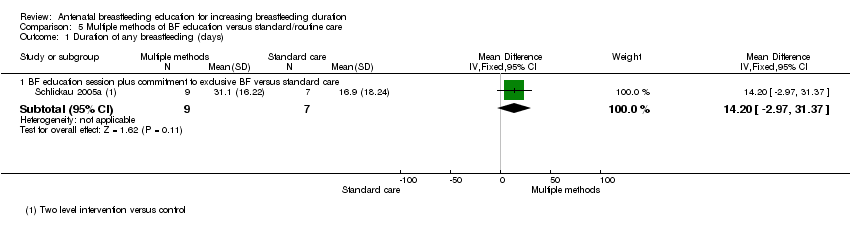
Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 1 Duration of any breastfeeding (days).

Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 2 Exclusive breastfeeding at 3 months.

Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 3 Exclusive breastfeeding at six months.
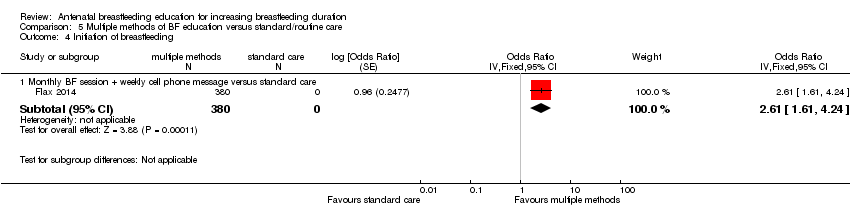
Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 4 Initiation of breastfeeding.
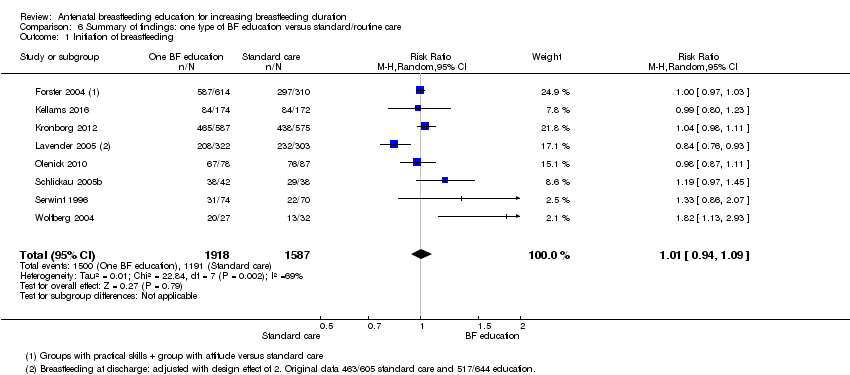
Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 1 Initiation of breastfeeding.
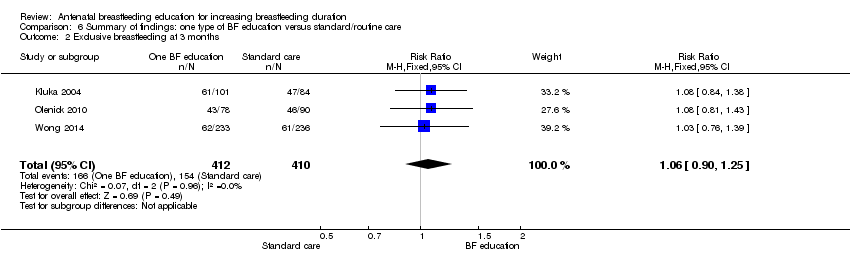
Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 2 Exclusive breastfeeding at 3 months.

Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 3 Exclusive breastfeeding at 6 months.

Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 4 Any breastfeeding at 3 months.
Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 5 Any breastfeeding at 6 months.
| BF education versus standard/routine care | ||||||
| Patient or population: pregnant women Comparison: standard/routine care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with Standard/routine care | Risk with Summary of findings: One BF education | |||||
| Initiation of BF | Study population | average RR 1.01 | 3505 | ⊕⊕⊕⊕ | We have not downgraded any outcome for lack of blinding. No trial contributing data had adequate blinding of staff and participants | |
| 750 per 1000 | 758 per 1000 | |||||
| Proportion of women exclusively BF at 3 months | Study population | RR 1.06 | 822 | ⊕⊕⊕⊝ | ||
| 376 per 1000 | 398 per 1000 | |||||
| Proportion of women exclusively BF at 6 months | Study population | RR 1.07 | 2161 | ⊕⊕⊕⊝ | ||
| 154 per 1000 | 165 per 1000 | |||||
| Proportion of women any BF at 3 months | Study population | average RR 0.98 | 654 | ⊕⊕⊝⊝ | ||
| 609 per 1000 | 597 per 1000 | |||||
| Proportion of women any BF at 6 months | Study population | average RR 1.05 | 1636 | ⊕⊕⊕⊕ | ||
| 505 per 1000 | 531 per 1000 | |||||
| Breastfeeding complications | Duffy 1997 (n = 70) reported no group differences for mastitis, but less nipple pain and less nipple trauma for women who had a lactation consultant.2 Kronborg 2012 (n = 1162) reported no group differences as to whether women responded yes when asked about BF problems.3 | (2 studies) | Moderate | Both trials compared the intervention with standard care | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Statistical heterogeneity I² = 69% (not downgraded) 2 Downgraded for imprecision due to small sample size (‐1). 3 Downgraded for imprecision due to wide confidence intervals crossing the line of no effect (‐1). 4 Statistical heterogeneity I² = 60% (not downgraded) 5 Wide confidence intervals crossing the line of no effect and small sample size (‐2) 6 Statistical heterogeneity I² = 61% (not downgraded) | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of any breastfeeding Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 BF education session versus standard care (weeks) | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐2.78, 2.78] |
| 1.2 BF education session versus standard care (days) | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 6.20 [‐10.84, 23.24] |
| 2 Any breastfeeding at 3 months Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 BF education workshop versus standard care | 1 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.92, 1.24] |
| 2.2 BF education session versus standard care | 1 | 469 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.75, 1.07] |
| 3 Any breastfeeding at 6 months Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 BF education workshop versus standard care | 1 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.87, 1.51] |
| 3.2 BF practical skills versus standard care | 1 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.87, 1.17] |
| 3.3 BF attitude education versus standard care | 1 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.79, 1.07] |
| 3.4 BF education session versus standard care | 2 | 569 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.86, 1.19] |
| 4 Exclusive breastfeeding at 3 months Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 BF education workshop versus standard care | 1 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.84, 1.38] |
| 4.2 BF education session versus standard care | 2 | 637 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.85, 1.30] |
| 5 Exclusive breastfeeding at 6 months Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 BF education workshop versus standard care | 1 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.70, 1.80] |
| 5.2 BF practical skills versus standard care | 1 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.69, 2.05] |
| 5.3 Formal BF attitude versus standard care | 1 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.67, 2.01] |
| 5.4 BF education session versus standard care | 2 | 1094 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.80, 1.31] |
| 6 Initiation of breastfeeding Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 BF education workshop versus standard care | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.97, 1.45] |
| 6.2 Peer counselling versus standard care | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.82 [1.13, 2.93] |
| 6.3 BF practical skills versus standard care | 1 | 616 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.98, 1.04] |
| 6.4 BF attitude education versus standard care | 1 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.95, 1.02] |
| 6.5 BF education session versus standard care | 2 | 1327 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.98, 1.09] |
| 6.6 BF education video versus standard care | 1 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.80, 1.23] |
| 6.7 LC versus standard care | 1 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.86, 2.07] |
| 7 Initiation of BF (cluster‐randomised trial) Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 7.1 Peer counselling versus standard care | 1 | 2398 | Odds Ratio (Fixed, 95% CI) | 1.11 [0.86, 1.43] |
| 7.2 Group LC session versus standard care | 1 | 1249 | Odds Ratio (Fixed, 95% CI) | 1.20 [0.80, 1.80] |
| 8 Mastitis Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 LC versus standard care | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 9 Breastfeeding complication (nipple pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 LC versus standard care | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐19.8 [‐23.23, ‐16.37] |
| 10 Breastfeeding complication (nipple trauma) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 LC versus standard care | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | 38.65 [32.95, 44.35] |
| 11 Breastfeeding problems Show forest plot | 1 | 1162 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.70, 1.43] |
| 11.1 BF education session versus standard care | 1 | 1162 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.70, 1.43] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any breastfeeding at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Group education versus individual education | 1 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.84 [0.61, 13.18] |
| 2 Any breastfeeding at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 BF practical skills versus BF attitude education | 1 | 590 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.94, 1.28] |
| 3 Exclusive breastfeeding at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 BF practical skills versus BF attitude education | 1 | 590 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.61, 1.73] |
| 4 Initiation of BF Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 BF practical skills versus BF attitude education | 1 | 614 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.99, 1.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of any breastfeeding (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 BF education session plus commitment to exclusive BF versus BF education session | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 8.0 [‐6.84, 22.84] |
| 2 Any breastfeeding at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Video + education session versus pamphlets | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [0.86, 2.94] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any breastfeeding at 4 months (cluster‐randomised trial) Show forest plot | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 1.1 LC + BF booklet + 24 h free LC versus BF booklet + phone number for BF questions and problems. | 1 | 698 | Odds Ratio (Fixed, 95% CI) | 0.82 [0.58, 1.16] |
| 2 Exclusive breastfeeding at 3 months Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 2.1 LC + BF booklet + 24 hrs free LC versus BF booklet + phone number for BF questions and problems. | 1 | 698 | Odds Ratio (Fixed, 95% CI) | 0.79 [0.57, 1.09] |
| 2.2 BF booklet + video + LC versus BF booklet + video | 1 | 150 | Odds Ratio (Fixed, 95% CI) | 1.40 [0.70, 2.80] |
| 3 Exclusive breastfeeding at 6 months Show forest plot | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 3.1 BF booklet + video + LC versus BF booklet + video | 1 | 169 | Odds Ratio (Fixed, 95% CI) | 2.50 [1.00, 6.25] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of any breastfeeding (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 BF education session plus commitment to exclusive BF versus standard care | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 14.20 [‐2.97, 31.37] |
| 2 Exclusive breastfeeding at 3 months Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 2.1 BF booklet + video + LC versus standard care | 1 | 159 | Odds Ratio (Fixed, 95% CI) | 2.60 [1.25, 5.40] |
| 2.2 BF booklet + video versus standard care | 1 | 159 | Odds Ratio (Fixed, 95% CI) | 1.80 [0.80, 4.05] |
| 2.3 Monthly BF session + weekly cell phone message versus standard care | 1 | 390 | Odds Ratio (Fixed, 95% CI) | 1.80 [1.10, 2.95] |
| 3 Exclusive breastfeeding at six months Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 3.1 BF booklet + video + LC versus standard care | 1 | 175 | Odds Ratio (Fixed, 95% CI) | 2.40 [1.00, 5.76] |
| 3.2 BF booklet + video versus standard care | 1 | 184 | Odds Ratio (Fixed, 95% CI) | 0.90 [0.30, 2.70] |
| 3.3 Monthly BF session + weekly cell phone message versus standard care | 1 | 390 | Odds Ratio (Fixed, 95% CI) | 2.40 [1.40, 4.11] |
| 4 Initiation of breastfeeding Show forest plot | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 4.1 Monthly BF session + weekly cell phone message versus standard care | 1 | 380 | Odds Ratio (Fixed, 95% CI) | 2.61 [1.61, 4.24] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Initiation of breastfeeding Show forest plot | 8 | 3505 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.94, 1.09] |
| 2 Exclusive breastfeeding at 3 months Show forest plot | 3 | 822 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.90, 1.25] |
| 3 Exclusive breastfeeding at 6 months Show forest plot | 4 | 2161 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.87, 1.30] |
| 4 Any breastfeeding at 3 months Show forest plot | 2 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.82, 1.18] |
| 5 Any breastfeeding at 6 months Show forest plot | 4 | 1636 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.90, 1.23] |

