L'éducation prénatale à l'allaitement pour augmenter la durée de l'allaitement maternel
Résumé scientifique
Contexte
Il est bien établi que le lait maternel est la meilleure source de nourriture pour les nourrissons. L'impact de l'éducation prénatale à l'allaitement sur la durée de l'allaitement n'a pas été évalué.
Objectifs
Évaluer l'efficacité de l'éducation prénatale à l'allaitement maternel (AM) pour augmenter le démarrage et la durée de celui‐ci.
Stratégie de recherche documentaire
Nous avons effectué des recherches dans le registre des essais du groupe Cochrane sur la grossesse et les accouchements le 1 mars 2016, CENTRAL (The Cochrane Library, 2016, numéro 3), MEDLINE (de 1966 au 1 mars 2016) et Scopus (de janvier 1985 au 1 mars 2016). Nous avons contacté des experts et consulté les références bibliographiques des articles trouvés.
Critères de sélection
Tous les essais contrôlés randomisés (ECR) identifiés, publiés, non publiés et en cours, évaluant l'effet de l'éducation prénatale formelle à l'allaitement ou comparant deux méthodes différentes d'éducation prénatale formelle à l'allaitement, sur la durée de l'allaitement. Nous avons inclus des ECR qui comprenaient uniquement des interventions prénatales et exclu ceux qui combinaient des éléments d'éducation prénatale, intrapartum ou postpartum. Les essais randomisés en grappes ont été inclus dans cette revue. Les essais quasi‐randomisés n'étaient pas éligibles pour l'inclusion.
Recueil et analyse des données
Nous avons évalué toutes les études identifiées au moyen de la stratégie de recherche. Deux auteurs de la revue ont extrait les données de chaque étude incluse à l'aide du formulaire agréé et évalué le risque de biais. Nous avons résolu les divergences par la discussion. Nous avons évalué la qualité des preuves en utilisant l'approche GRADE.
Résultats principaux
Cette revue mise à jour inclut 24 études (10 056 femmes). Vingt études (9789 femmes) ont fourni des données pour les analyses. La plupart des études ont été réalisées dans des pays à revenus élevés, tels que les États‐Unis, le Royaume‐Uni, le Canada et l'Australie. Dans les cinq premières comparaisons, nous présentons les essais inclus selon le type d'intervention sans combiner les données. Pour le « Résumé des résultats », nous avons combiné les données pour obtenir un effet global.
Cinq des études incluses étaient des essais randomisés en grappes : tous ceux‐ci ont ajusté des données et rapporté des ajustements sous forme de rapports des cotes (RC). Nous avons analysé les données à l'aide de la méthode de variance inverse générique et présenté les résultats sous forme de rapports de cotes, car nous ne sommes pas parvenus à trouver un risque relatif ajusté à partir des essais en grappes publiés. Nous reconnaissons que l'utilisation de rapport de cotes empêche la combinaison de ces essais en grappes dans nos principales analyses.
Une technique d'éducation à l'allaitement associée aux soins standard
Il n'y avait aucune différence quant à la durée de l'allaitement en termes de jours ou de semaines entre les groupes. Il n'y avait pas de preuves indiquant que les interventions amélioraient la proportion de femmes allaitant de manière exclusive ou non à trois ou à six mois. Des essais uniques de différentes interventions n'ont pas réussi à démontrer que l'éducation peut améliorer le démarrage de l'allaitement maternel, à l'exception d'un essai de petite taille à risque élevé de biais d'attrition. De nombreux résultats des essais étaient marginalement favorables à l'intervention, mais avaient de larges intervalles de confiance traversant la ligne d'absence d'effet. Les complications de l'allaitement maternel, telles que la mammite et d'autres problèmes étaient similaires dans les bras de traitement dans les essais uniques rendant compte de ces critères de jugement.
Plusieurs méthodes d'éducation à l'allaitement par rapport aux soins standard
Pour tous les essais inclus dans cette comparaison nous avons présenté les rapports de cotes des grappes ajustés, comme indiqué dans les essais publiés. Une étude à trois bras a montré qu'une brochure sur l'allaitement + une vidéo + une consultation pour l'allaitement par rapport aux soins standard mènent à une augmentation de la proportion de femmes allaitant exclusivement à trois mois (RC 2,60, IC à 95 % 1,25 à 5,40 ; nombre de femmes = 159) et légèrement à six mois (RC 2,40, IC à 95 % 1,00 à 5,76 ; nombre de femmes = 175). Dans le même essai, un bras d'intervention sans consultation d'un spécialiste de la lactation mais avec l'offre d'une brochure sur l'allaitement et d'une vidéo n'avait pas le même effet sur la proportion de femmes allaitant exclusivement à trois mois (RC 1,80, IC à 95 % 0,80 à 4,05 ; nombre de femmes = 159) ou à six mois (RC 0,90, IC à 95 % 0,30 à 2,70 ; nombre de femmes = 184). Une étude comparait les séances mensuelles d'allaitement et l'offre de messages téléphoniques hebdomadaires par rapport à des soins standard et a signalé des améliorations dans la proportion de femmes allaitant exclusivement à la fois à trois et six mois (trois mois RC 1,80, IC à 95 % 1,10 à 2,95 ; nombre de femmes = 390 ; six mois RC 2,40, IC à 95 % 1,40 à 4,11 ; nombre de femmes = 390). Une étude a trouvé que les séances mensuelles d'allaitement associées à des messages téléphoniques hebdomadaires amélioraient le démarrage de l'allaitement par rapport aux soins standard (RC 2,61, IC à 95 % 1,61 à 4,24 ; nombre de femmes = 380).
Les séances d'éducation à l'allaitement par rapport à des soins standard, analyses combinées pour le « Résumé des résultats » (SoF)
Cette comparaison n'a pas inclus les essais randomisés en grappes ne rapportant pas de rapports de cotes ajustés. Nous n'avons pas déclassé les preuves des essais lorsqu'il n'y avait pas de mise en aveugle ; aucun essai n'avait de mise en aveugle adéquate des participants et du personnel. Le tableau SoF présente les risques relatifs pour tous les critères de jugement analysés. Par rapport à la proportion de femmes allaitant exclusivement, il n'existe aucune preuve que l'éducation prénatale améliore l'allaitement à trois mois (RR 1,06, IC à 95 % 0,90 à 1,25 ; nombre de femmes = 822 ; nombre d'études = 3 ; preuves de qualité modérée) ou à six mois (RR 1,07, IC à 95 % 0,87 à 1,30 ; nombre de femmes = 2161 ; nombre d'études = 4 ; preuves de qualité modérée). Pour la proportion de femmes allaitant en général, il n'y avait aucune différence entre les groupes quant à l'allaitement à trois (RR moyen 0,98, IC à 95 % 0,82 à 1,18 ; nombre de femmes = 654 ; nombre d'études = 2 ; I² = 60 % ; preuves de faible qualité) ou à six mois (RR moyen 1,05, IC à 95 % 0,90 à 1,23 ; nombre de femmes = 1636 ; nombre d'études = 4 ; I² = 61 % ; preuves de qualité élevée). Il n'y avait aucune preuve soutenant que l'éducation prénatale à l'allaitement pourrait améliorer le démarrage de l'allaitement (RR moyen 1,01, IC à 95% 0,94 à 1,09 ; nombre de femmes = 3505 ; nombre d'études = 8 ; I² = 69 % ; preuves de qualité élevée). Lorsque nous avons rabaissé des preuves, cela était dû à des échantillons de petite taille ou de larges intervalles de confiance traversant la ligne d'absence d'effet, parfois les deux.
Il n'y avait pas suffisamment de données pour l'analyse en sous‐groupes selon la profession ou l'éducation de la mère.
Conclusions des auteurs
Il n'y avait pas de preuves concluantes soutenant une quelconque éducation prénatale à l'allaitement pour améliorer le démarrage de l'allaitement, la proportion de femmes allaitant ou allaitant exclusivement au bout de trois à six mois ou la durée de l'allaitement. Il existe un besoin urgent de mener des études contrôlées randomisées de haute qualité pour évaluer l'efficacité et les effets indésirables de l'éducation prénatale à l'allaitement, en particulier dans les pays à revenus faibles et intermédiaires. Les preuves contenues dans cette revue sont principalement pertinentes pour les contextes à revenus élevés.
PICO
Résumé simplifié
L'éducation prénatale à l'allaitement pour augmenter la durée de l'allaitement maternel
Quel est le problème?
L'allaitement maternel (AM) peut améliorer la santé de l'enfant, de la mère et la relation mère‐enfant. Les nourrissons ayant été allaités ont des taux plus faibles de problèmes respiratoires et gastriques, moins d'infections des organes de l'oreille et une meilleure élocution, vue et qualité globale du développement des compétences physiques et mentales. L'Organisation Mondiale de la Santé recommande que les nouveau‐nés soient exclusivement allaités de la naissance à l'âge de six mois et ensuite allaités en plus d'une alimentation adaptée à leur âge pendant deux ans et au‐delà. De nombreuses femmes ne sont pas en mesure de suivre ces recommandations, et il est ainsi pertinent de savoir comment aider les femmes à allaiter.
En quoi est‐ce important ?
L'éducation prénatale à l'allaitement correspond à l'enseignement de l'allaitement maternel offert durant la grossesse aux futures mères. L'une des raisons pour lesquelles les femmes n'allaitent pas est un manque d'éducation et de connaissances sur comment allaiter. Nous pensons que l'amélioration des connaissances des femmes enceintes sur l'allaitement pourrait les aider à allaiter plus longtemps, mais nous ne savons pas quels types d'éducation sont les plus utiles pour cette population.
Les preuves observées :
Nous avons inclus 24 études portant sur 10 056 femmes dans la revue, et 20 études portant sur 9789 femmes ont fourni des données pour les analyses. La plupart des études ont été réalisées dans des pays à revenus élevés, notamment aux États‐Unis, au Canada, au Royaume‐Uni et en Australie. Le soutien par les pairs, les consultations quant à l'allaitement et l'enseignement formel de l'allaitement pendant la grossesse ne semblent pas améliorer le recours à l'allaitement ou sa durée. Cependant, certains des essais à plus grande échelle dans différents contextes (un au Nigeria et un à Singapour) présentaient quelques preuves suggérant que l'éducation peut aider.
Qu'est‐ce que cela signifie ?
Nous ne savons pas encore si l'éducation prénatale à l'allaitement peut aider les femmes ; à l'heure actuelle, il n'existe pas suffisamment de preuves issues d'essais contrôlés randomisés permettant de suggérer que les mesures visant à éduquer les femmes enceintes se traduisent par un allaitement plus long et plus fréquent. Il y a presque autant de femmes ayant reçu des soins standard qui allaitent, comparé aux femmes qui ont reçu une éducation supplémentaire sur l'allaitement. Nous avons confiance dans les résultats des études mesurant le recours des femmes à l'allaitement au bout de trois et de six mois ; l'éducation ne semble pas affecter ces décisions. Nous avons quelques doutes sur l'impact de l'éducation sur l'allaitement exclusif à trois et six mois ; l'éducation ne semble pas aider les femmes, mais de futures études pourraient modifier cette conclusion. De futures études sont susceptibles de modifier nos connaissances sur l'impact de l'éducation à l'allaitement pendant la grossesse sur l'allaitement à trois mois. La plupart des études dans cette revue ont été réalisées dans des pays à revenus élevés, de sorte que nous ne sommes pas sûrs que nos conclusions soient pertinentes dans d'autres contextes.
Authors' conclusions
Summary of findings
| BF education versus standard/routine care | ||||||
| Patient or population: pregnant women Comparison: standard/routine care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with Standard/routine care | Risk with Summary of findings: One BF education | |||||
| Initiation of BF | Study population | average RR 1.01 | 3505 | ⊕⊕⊕⊕ | We have not downgraded any outcome for lack of blinding. No trial contributing data had adequate blinding of staff and participants | |
| 750 per 1000 | 758 per 1000 | |||||
| Proportion of women exclusively BF at 3 months | Study population | RR 1.06 | 822 | ⊕⊕⊕⊝ | ||
| 376 per 1000 | 398 per 1000 | |||||
| Proportion of women exclusively BF at 6 months | Study population | RR 1.07 | 2161 | ⊕⊕⊕⊝ | ||
| 154 per 1000 | 165 per 1000 | |||||
| Proportion of women any BF at 3 months | Study population | average RR 0.98 | 654 | ⊕⊕⊝⊝ | ||
| 609 per 1000 | 597 per 1000 | |||||
| Proportion of women any BF at 6 months | Study population | average RR 1.05 | 1636 | ⊕⊕⊕⊕ | ||
| 505 per 1000 | 531 per 1000 | |||||
| Breastfeeding complications | Duffy 1997 (n = 70) reported no group differences for mastitis, but less nipple pain and less nipple trauma for women who had a lactation consultant.2 Kronborg 2012 (n = 1162) reported no group differences as to whether women responded yes when asked about BF problems.3 | (2 studies) | Moderate | Both trials compared the intervention with standard care | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Statistical heterogeneity I² = 69% (not downgraded) 2 Downgraded for imprecision due to small sample size (‐1). 3 Downgraded for imprecision due to wide confidence intervals crossing the line of no effect (‐1). 4 Statistical heterogeneity I² = 60% (not downgraded) 5 Wide confidence intervals crossing the line of no effect and small sample size (‐2) 6 Statistical heterogeneity I² = 61% (not downgraded) | ||||||
Background
Description of the condition
Breastfeeding (BF) is well recognised as the best food source for infants (Sankar 2015). Complementary foods offered before six months of age tend to displace breast milk and do not confer any health advantage over exclusive BF (Kramer 2012). BF has been advocated to improve child health, maternal health and mother‐infant bonding (Ball 2001; Hanson 2002). BF has been associated with lower rates of gastrointestinal and respiratory diseases, otitis media and allergies, better visual acuity, and speech and cognitive development (Innis 2001; Quigley 2012; Renfrew 2012; Wold 2000). It is also cost effective (Renfrew 2012). Infants who are breastfed have a lower risk of developing insulin‐dependent diabetes in childhood (Horta 2015), sudden infant death syndrome (Renfrew 2012) and childhood cancer (Amitay 2016). Recent research indicates that the type of infant feeding may contribute to children becoming overweight and obese in early and late childhood. BF has been shown to protect against child obesity and cardiovascular risk outcomes and is dose related ‐ the longer the infant is breastfed, the lower the risk (Arenz 2004; Harder 2005; Owen 2005). A Cochrane Review by Kramer 2012 indicated that exclusive BF for six months has several advantages over exclusive BF for three to four months followed by mixed BF.
Delay in return of fertility has been associated with frequent and long periods of exclusive BF, as well as a lower risk of developing breast cancer (Chowdhury 2015). Women who had not breastfed their babies were four times more likely to have osteoporosis than women who had breastfed (Blaauw 1994). Better emotional health has also been attributed to women who breastfed. Virden 1988 found that, at one month postpartum, women who breastfed their infants had scores indicating less anxiety than women who had bottle fed their infants. The retrospective review of medical records of 800 pregnancies by Acheson 1995 revealed an association between lack of BF and physical and sexual abuse of the women or her children, or both. This was a small review, the results of which warrant further study. A recent published study found that women who breastfed for at least one year were less likely to develop Type 2 diabetes than women who did not breastfeed (Stuebe 2005). Some studies have shown a benefit of BF in enhancing couple and family relationships (Cohen 2002; Falceto 2004; Jordan 1993; Li 2004; Sullivan 2004).
In 1988, the World Health Organization (WHO) and UNICEF proposed the following standard terminology for the collection and description of data on BF behaviour; these were updated in 1991 (WHO 1991), and are now widely used (Dettwyler 1992). Breastfeeding means the infant receives breast milk but allows the infant to receive any food or liquid including non‐human milk. Exclusive BF is defined as an infant being fed only breast milk, with the possible exception of vitamin D in certain populations and iron in infants of relatively low birthweight (Dewey 2001). Predominant BF is when the infant receives breast milk as the predominant source of nourishment but allows the infant to receive liquids (water and water‐based drinks, fruit juice, oral dehydration solutions) and drops or syrups (vitamins, minerals, medicines) but does not allow the infant to receive anything else (in particular, non‐human milk and food‐based fluids). Complimentary BF is the situation when the infant receives breast milk and solid or semi‐solid foods and allows the infant to receive any food or liquid including non‐human milk.
Despite the many advantages and extensive promotion of BF, Susin 1999 reported that the trend towards BF in many countries has been increasing slowly. However, according to the UNICEF report (UNICEF 2005), six million lives a year are being saved by exclusive BF and global BF initiation rates have risen by at least 15% since 1990. At the same time, women breastfeed for a shorter time than they intended or wished to (Adams 2001; Wagner 2002). The World Health Organization recommends that infants should be exclusively breastfed from birth to six months and then breastfed alongside age‐appropriate, complementary feeding for two years and beyond (WHO 2001).
Description of the intervention
Antenatal BF education is defined as BF information being imparted during the pregnancy in a variety of forms. This could be on an individual or group basis, could include home visiting programmes, peer education programmes or clinic appointments specifically aimed at imparting BF knowledge and could involve prospective fathers or not. BF education is usually a formalised, defined, descriptive and goal‐orientated programme with a specific purpose and target audience.
BF education differs from BF support. BF support is usually aimed at the individual person as the need arises and is defined as a person, a group or an organisation providing support in many ways. This could be psychological support (affirming and encouraging the mother), physical support (providing meals, caring for her other children, house cleaning and gardening), financial support or BF information services available to be tapped into when a BF question arises. BF support usually starts in the postnatal period, not antenatally.
Although we recognise the potential importance of interventions in the postnatal period on BF outcomes, the focus of this review is on antenatal BF education only, and we have not included trials examining interventions that also involve intrapartum or postpartum BF education. Other Cochrane Reviews examine BF education and support interventions in the intrapartum and postnatal periods (Britton 2007; Dyson 2005; Sikorski 2002).
How the intervention might work
Another Cochrane Systematic Review provides evidence that various forms of BF education are effective at increasing rates of BF initiation among women on low incomes in the USA and initiation will, therefore, not be the main focus in this review (Dyson 2005). The impact of antenatal BF education on the duration of BF, however, has not been widely reported. In Australia, more than 90% of mothers initiate BF; however, only 48% of mothers are BF at one month postpartum and only 23% maintain any form of BF at six months (Lund‐Adams 1996). Similar BF duration rates have been reported in the USA (Raj 1998) and Britain (Griffiths 2005; Hoddinott 2000), as well as in low‐income countries (UNICEF 1998). A variety of BF promotion methods including educational programmes have been studied to support the trend to increase BF duration. It is generally believed that, by improving the mothers' knowledge of BF antenatally, the rates and duration of BF would increase (McLeod 2002). Lack of antenatal information and education about BF has been one factor attributed by New Zealand mothers interviewed about discontinuing BF (McLeod 2002).
Why it is important to do this review
This is an update of a Cochrane Review first published in 2011, and previously updated in 2012. The earlier version of the review indicated that there were significant methodological limitations and the observed effect sizes were small, and there was no clear evidence to support any specific antenatal BF education. This current update will provide the most up‐to‐date evidence on the effectiveness of antenatal BF education.
Objectives
-
To assess the effectiveness of antenatal breastfeeding (BF) education for increasing BF initiation and duration.
-
To compare the effectiveness of various forms of education; for example, peer support, educational programme, didactic teaching session, workshop, booklets, etc, or a combination of these interventions for increasing BF initiation and duration.
-
To assess the effects of antenatal BF education on other maternal and infant outcomes, for example, BF complications, maternal satisfaction and neonatal sepsis.
Methods
Criteria for considering studies for this review
Types of studies
All identified published, unpublished and ongoing randomised controlled trials (RCTs) comparing antenatal breastfeeding (BF) education programmes, with or without formal BF education. Randomised units could be clustered, for example, hospitals, communities or groups of pregnant women or individual women. We excluded quasi‐RCTs. We did not include studies published only as abstracts.
Types of participants
Pregnant women or their partners, or both.
Types of interventions
Any type of antenatal education with BF components. Antenatal BF education is defined as BF information being imparted during pregnancy in a variety of forms. This could be on an individual or group basis, include home visiting programmes; peer education programmes or clinic appointments specifically aimed at imparting BF knowledge; brochures or booklets; electronic education programmes; or a combination of these, and could involve prospective fathers or not. Formal BF education is defined as BF education that was given formally in addition to any BF education that was given as part of standard antenatal care. We excluded RCTs examining interventions that included intrapartum or postpartum BF education in addition to antenatal BF education.
We examined five comparisons.
-
One type of BF education versus standard/routine care
-
One type of BF education versus a different type of BF education
-
Multiple methods of BF education versus a single method of BF education
-
Different combinations of multiple methods of providing BF education
-
Multiple methods of BF education versus standard/routine care
Types of outcome measures
Primary outcomes
-
Duration of any BF
-
Duration of exclusive BF
-
Proportion of women with any BF at three and six months
-
Proportion of women exclusively BF at three and six months
-
Initiation of BF
Secondary outcomes
-
Maternal satisfaction
-
BF complications such as mastitis and breast abscess
-
Infant growth by weight and head circumference
-
Neonatal sepsis
-
Taking child to doctor
-
Hospital admission for child
Search methods for identification of studies
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
We searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (1 March 2016).
The Register is a database containing over 22,000 reports of controlled trials in the field of pregnancy and childbirth. For full search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link to the editorial information about the Cochrane Pregnancy and Childbirth Group in The Cochrane Library and select the ‘Specialized Register ’ section from the options on the left side of the screen.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by their Information Specialist and contains trials identified from:
-
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
-
weekly searches of MEDLINE (Ovid);
-
weekly searches of Embase (Ovid);
-
monthly searches of CINAHL (EBSCO);
-
handsearches of 30 journals and the proceedings of major conferences;
-
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set which has been fully accounted for in the relevant review sections (Included studies; Excluded studies; Studies awaiting classification; Ongoing studies).
In addition, we also searched CENTRAL (The Cochrane Library, 2016, Issue 3), MEDLINE (1966 to 1 March 2016) and Scopus (January 1985 to 1 March 2016). We contacted experts and searched reference lists of retrieved articles using the search strategies detailed in Appendix 1.
Searching other resources
We contacted investigators (identified from the retrieved articles) and other content experts known to us for unpublished studies. Furthermore, we looked for relevant studies in the references of the retrieved articles.
We did not apply any language or date restrictions.
Data collection and analysis
For methods used in the previous version of this review, seeLumbiganon 2012.
For this update, we used the following methods for assessing the 42 reports that we identified as a result of the updated search.
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Selection of studies
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted the third review author.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author. Data were entered into Review Manager (RevMan) software (RevMan 2014) and checked for accuracy.
When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We resolved any disagreement by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
-
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
-
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
-
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
-
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
-
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
-
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding was unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
-
low, high or unclear risk of bias for participants;
-
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
-
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
-
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
-
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
-
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
-
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
-
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
-
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Handbook (Higgins 2011a). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. In future updates, we will explore the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis.
Assessment of the quality of the evidence using the GRADE approach
For this update the quality of the evidence was assessed using the GRADE approach as outlined in the GRADE handbook, in order to assess the quality of the body of evidence relating to the following outcomes for comparison 6. Any BF education versus standard care:
-
Initiation of BF
-
Proportion of women exclusively BF at six months
-
Proportion of women exclusively BF at three months
-
Proportion of women with any BF at six months
-
Proportion of women with any BF at three months
-
BF complications such as mastitis and breast abscess
GRADEpro Guideline Development Tool was used to import data from RevMan (RevMan 2014) in order to create a ’Summary of findings’ table. A summary of the intervention effect and a measure of quality for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
For dichotomous data, we presented results as summary risk ratio (RR) with 95% confidence intervals (CI), with the exception of cluster‐randomised trials that reported adjusted odds ratios (OR) (see note below). For continuous data we used the mean difference (MD) if outcomes were measured in the same way between trials. In future updates, if appropriate, we will use the standardised mean difference to combine trials that measured the same outcome, but use different methods.
Unit of analysis issues
Cluster‐randomised trials
We included studies where individual women were randomised and cluster‐randomised studies where, for example, clinics were the unit of randomisation. Five included studies were cluster‐randomised trials (Flax 2014; Kools 2005; Lavender 2005; MacArthur 2009; Mattar 2007); all of these studies report results for review outcomes with adjustments made for clustering effects.
For trials where cluster‐adjusted data were reported as odds ratios (Flax 2014; Kools 2005; Lavender 2005; MacArthur 2009; Mattar 2007) we have analysed the data using the generic inverse variance method in RevMan 2014; we presented these results as odds ratios, because we were unable to derive a cluster‐adjusted risk ratio from the published, cluster‐adjusted odds ratio. We acknowledge that the use of odds ratios prevents the pooling of these cluster trials in our main analyses (comparison 6).
Where there was no adjustment for cluster design effect in the published report, or where raw data were available, we adjusted the data ourselves and have presented risk ratios, because we feel this statistic is more appropriate for BF outcomes. (For example, Lavender 2005 provides an intra‐cluster correlation co‐efficient (ICC) of 0.01, as well as mean cluster size and design effects for each BF outcome; we used these to adjust the sample size for outcome data in Analysis 1.5). If we adjusted data ourselves, we combined the adjusted data in analyses and report pooled risk ratios. We consider it reasonable to combine the results from both individual and cluster‐randomised trials if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
In future updates, if we identify any more cluster‐randomised trials we will include them in the analyses along with individually‐randomised trials. If adjustment for the cluster design effect has not already been made by the trial authors, we will adjust their sample sizes using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions; Section 16.3.4 or 16.3.6 (Higgins 2011b) using an estimate of the ICC derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC.
We will also acknowledge heterogeneity in the randomisation unit, and, if there are sufficient numbers of trials, we will perform a subgroup analysis to investigate the effects of the randomisation unit.
Cross‐over trials
Cross‐over trials were not eligible for this review.
Other unit of analysis issues
Multiple pregnancies
In the studies that contributed data to this review, four excluded multiple pregnancies from their trial (Kellams 2016; Kronborg 2012; Mattar 2007; Wong 2014). Of the remaining studies, 12 did not mention multiple pregnancies (Duffy 1997; Flax 2014; Forster 2004; Kistin 1990; Kluka 2004; Kools 2005; Lavender 2005; MacArthur 2009; Olenick 2010; Schlickau 2005a; Schlickau 2005b; Wolfberg 2004). Serwint 1996 was the only study that reported a twin pregnancy and only included data from twin A. We have not made adjustments to any analyses to account for correlated outcomes due to multiple pregnancy.
Multiple‐armed studies
Four studies contributing data to our review included multiple treatment arms (Forster 2004; Kistin 1990; Mattar 2007; Schlickau 2005a). Ryser 2004 also included multiple treatment arms but did not contribute any data to this review.
We treated trials with three arms as follows.
-
We included two intervention arms comparing one form of BF education versus another form (group antenatal BF class and individual antenatal counselling) in Comparison 2 (Kistin 1990). In this study, the third comparison arm was a control group which was not randomised and therefore not included in this review.
-
We included only the intervention arms comparing an information booklet, educational video and session with a lactation consultant versus the same information booklet and video without the lactation consultant session in Comparison 4 (Mattar 2007), the third comparison was a control group and was included in Comparison 5.
-
For comparisons 1 to 5, we included more than one intervention arm compared with control, so the study ID will appear in the forest plot twice (a footnote identifies the arms). We did not split the control groups for these analyses because the trials were not pooled.
-
We kept intervention arms separate and split the control group to avoid double counting for pooled data in Comparison 6 (Forster 2004).
-
Schlickau 2005a presented continuous data, and so we compared single intervention arms with control.
Dealing with missing data
For included studies, we noted levels of attrition. In future updates, if more eligible studies are included, we will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, that is, we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² (Higgins 2003) and Chi² statistics. We regarded heterogeneity as substantial if I² was greater than 30% and either Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. If we identified substantial heterogeneity (above 30%), we planned to explore it by pre‐specified subgroup analysis (Deeks 2011).
Assessment of reporting biases
In future updates, if there are 10 or more studies in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager (RevMan) software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: that is, where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar.
If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary was treated as the average range of possible treatment effects and we discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we planned not to combine trials. If we used random‐effects analyses, the results were presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
Where we identified substantial heterogeneity, we planned to investigate it using subgroup analyses and sensitivity analyses. We used a random‐effects model if the overall summary was meaningful.
We planned to carry out the following subgroup analyses.
-
Type of intervention
-
Study setting
-
Maternal education
-
Maternal occupation
We planned to restrict subgroup analysis to primary outcomes with sufficient numbers of trials in the relevant subgroups and to assess subgroup differences by interaction tests available within RevMan (RevMan 2014). We planned to report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
There were insufficient trials in relevant subgroups to analyse subgroups according to types of interventions or setting. There were insufficient trials reporting outcome data according to maternal education or maternal occupation to conduct these subgroup analyses.
Sensitivity analysis
We planned to explore the effect of trial quality assessed by concealment of allocation, high attrition rates, or both, with poor‐quality studies being excluded from the analyses in order to assess whether this made any difference to the overall result. There were no studies at high risk of bias for allocation concealment, so we did not conduct this analysis. When we removed one trial at high risk of bias for attrition (Wolfberg 2004) results did not change for Analysis 6.1 (analysis not shown).
Results
Description of studies
Results of the search
In the first published version of this review (Lumbiganon 2011) the search of the Pregnancy and Childbirth Group's Trials Register yielded 57 potential studies. Our additional search yielded one potential study. We explored the contents, and grouped together trial reports for the same study; from this we identified 17 studies (involving 7131 women) that met the inclusion criteria. We excluded 39 studies.
In the subsequent version (Lumbiganon 2012) of this review we searched the Pregnancy and Childbirth Group's Trials Register on 2 December 2011 and in addition, we searched CENTRAL (The Cochrane Library, 2011, Issue 11), MEDLINE (1966 to 30 November 2011) and Scopus (January 1985 to 30 November 2011) using the search strategies detailed in Appendix 1. We identified five additional potential studies, two studies (Kronborg 2012; Olenick 2010) were included, and three excluded (Kupratakul 2010; NCT01383070; Wockel 2009). We therefore included 19 studies involving 8506 women and excluded 42 studies in that update.
For this update (2016) we searched Pregnancy and Childbirth's Trials Register (1 March 2016), CENTRAL (The Cochrane Library, 2016, Issue 3), MEDLINE (1966 to 1 March 2016) and Scopus (January 1985 to 1 March 2016). We identified 42 citations of which there were nine potential included studies. We have included five more studies (Flax 2014; Kellams 2016; Pate 2009; Raeisi 2014; Wong 2014) at this update.
Two studies are awaiting translation and classification (Bahri 2013; Bastani 2009) and one study is ongoing (Maycock 2015). For the 2016 update we have included a total of 24 studies and excluded at total of 66 studies.
Included studies
We included 24 studies. We have provided full details of included studies in the Characteristics of included studies tables. Of these, 20 studies involving 9789 women contributed data to the analyses for primary and secondary outcomes; four included studies (Kaplowitz 1983; Noel‐Weiss 2006; Pate 2009; Ryser 2004) met our inclusion criteria but did not report data on any of our prespecified outcomes. Kaplowitz 1983 described women's attitudes towards breastfeeding (BF) before and after the intervention and we have not included results from this study in the review. Ryser 2004 and Noel‐Weiss 2006 report on BF at time points which we had not prespecified, and we have included a brief description of results from these studies following results for our primary and secondary outcomes. Pate 2009 reported self‐efficacy outcomes which were not prespecified outcomes in this review.
Study design
We included 19 randomised controlled trials and five cluster randomised trials (Flax 2014; Kools 2005; Lavender 2005; MacArthur 2009; Mattar 2007). Five studies included multiple treatment arms (Forster 2004; Kistin 1990; Mattar 2007; Ryser 2004; Schlickau 2005a).
Sample sizes
We included 24 studies with 10,056 women in the review, and 20 studies involving 9789 women contributed data to the analyses. The sample size of studies that contributed data to the review ranged from 30 (Schlickau 2005a) to 2511 (MacArthur 2009) with an average of 419 women. Six of these studies had fewer than 100 women taking part (Duffy 1997; Finch 2002; Kistin 1990; Schlickau 2005a; Schlickau 2005b; Wolfberg 2004).
Setting
Eleven studies were conducted in the USA (Finch 2002; Kaplowitz 1983; Kellams 2016; Kistin 1990; Olenick 2010; Pate 2009; Ryser 2004; Schlickau 2005a; Schlickau 2005b; Serwint 1996; Wolfberg 2004), three in Australia (Duffy 1997; Forster 2004; Rossiter 1994), two in the United Kingdom (Lavender 2005; MacArthur 2009), two in Canada (Kluka 2004; Noel‐Weiss 2006), one in Iran (Raeisi 2014), one in Nigeria (Flax 2014), one in the Netherlands (Kools 2005), one in Denmark (Kronborg 2012), one in Singpore (Mattar 2007), and one in Hong Kong (Wong 2014). Overwhelmingly the evidence in this review is relevant to higher income countries and settings.
Participants
All 24 studies recruited women in the antenatal period who were accessing antenatal care services with the exception of Flax 2014 who recruited women attending monthly microcredit meetings. Nine studies only recruited primigravida women (Forster 2004; Kluka 2004; Kronborg 2012; Noel‐Weiss 2006; Pate 2009; Schlickau 2005a; Schlickau 2005b; Serwint 1996; Wong 2014). Kaplowitz 1983 included primigravida women, women who had bottle‐fed previous children or who had previously had an unsuccessful BF experience.
The studies recruited at a range of gestations for example Rossiter 1994 recruited pregnant women who were at least 12 weeks' gestation, Forster 2004 and Kaplowitz 1983 at 16 to 24 weeks' gestation and Mattar 2007 at gestations above 36 weeks.
Kellams 2016; Pate 2009 and Ryser 2004 only recruited women on a low income, though only Kellams 2016 contributed data to the review.
None of the studies specified ethnicity except for Kistin 1990, who recruited only black women born in the USA, and Rossiter 1994, who only recruited Vietnamese or other women who were born and reared in Vietnam.
Four studies only recruited women with singleton pregnancies (Kronborg 2012; Mattar 2007; Noel‐Weiss 2006; Wong 2014).
Wolfberg 2004 and Raeisi 2014 recruited pregnant women's partners to antenatal BF education.
Interventions and comparisons
Interventions included BF education session, printed information, video, peer counselling and lactation consultation (LC), weekly cell phone BF text and voice messages to cell phone, web‐based education, and support related to BF practices.
There were a total of 20 comparisons from the included studies which are described below (some studies with more than two experimental arms are included in more than one comparison).
Sixteen studies compared a single method of BF education with standard care (Duffy 1997; Forster 2004; Kaplowitz 1983; Kellams 2016; Kluka 2004; Kronborg 2012; Lavender 2005; MacArthur 2009; Noel‐Weiss 2006; Olenick 2010; Raeisi 2014; Schlickau 2005a; Schlickau 2005b; Serwint 1996; Wolfberg 2004; Wong 2014). Two of these studies (Kaplowitz 1983; Noel‐Weiss 2006) compared BF education session versus standard care but did not provide any information about BF practices. Seven studies (Forster 2004; Kronborg 2012; Lavender 2005; Olenick 2010; Raeisi 2014; Schlickau 2005a; Wong 2014) compared BF education session versus standard care. Two studies (Duffy 1997; Serwint 1996) compared LC versus standard care. Two studies (Kluka 2004; Schlickau 2005b) compared BF workshop versus standard care. One study (Kellams 2016) compared BF video versus standard care. Two studies (MacArthur 2009; Raeisi 2014) compared BF peer support versus standard care. Raeisi 2014 and Wolfberg 2004 both aimed interventions at partners of pregnant women.
There were two studies (Forster 2004; Kistin 1990) comparing one form of BF education versus other form of BF education. One study (Kistin 1990) compared group education versus individual education. One study (Forster 2004) compared BF practical skills versus BF attitude education.
Three studies (Finch 2002; Rossiter 1994; Schlickau 2005a) examined programmes involving multiple methods of providing education compared to those using a single method. Finch 2002 compared LC plus incentive plus handout with BF education session. Rossiter 1994 examined the effect of a video and BF education session versus a BF pamphlet. One study (Schlickau 2005a) compared BF education session and baby quarantine versus BF education session.
Two studies (Kools 2005; Mattar 2007) compared different combinations of multiple interventions. One study (Mattar 2007) compared a BF booklet plus a video and LC versus a BF booklet and video only. Another study (Kools 2005) compared LC and a BF booklet with BF booklet and phone number for BF questions.
There were four studies (Flax 2014; Mattar 2007; Ryser 2004; Schlickau 2005a) that compared programmes involving multiple methods of providing education versus standard care. Flax 2014 compared weekly cell phone BF text and voice messages to cell phone and monthly face‐to‐face BF information versus standard care. Mattar 2007 compared a BF booklet, video and LC versus no formal BF education. Ryser 2004 compared a counselling session plus viewing a video plus the provision of written materials addressing common BF barriers perceived by low‐income women versus no formal BF education. This study did not provide any information on our proposed outcomes and has not been included in the analyses. Schlickau 2005a compared BF education session plus baby quarantine concept versus standard care.
In studies where BF education was compared with standard care, there was considerable variation in what was offered as part of usual care in terms of BF education. In many studies standard care was not described at all or the description was vague (e.g. provision of a leaflet or midwife advice). We have set out information about care for control groups in the Characteristics of included studies, and it is important that this is taken into account in the interpretation of results. Intrapartum and postpartum care could also have an impact on BF duration; these aspects of care also varied across included studies.
Comparisons in the studies were mostly reported as 'routine' or 'standard' antenatal care. In 13 studies standard/routine care included some form of BF education or support (Finch 2002; Forster 2004; Kluka 2004; Kools 2005; Lavender 2005; MacArthur 2009; Mattar 2007; Pate 2009; Rossiter 1994; Schlickau 2005a; Schlickau 2005b; Serwint 1996; Wong 2014). Two studies did not include any BF information (Flax 2014; Wolfberg 2004), and it was not clear in the remaining nine studies whether the control group participants received any BF education or support as part of standard care (Duffy 1997; Kaplowitz 1983; Kellams 2016; Kistin 1990; Kronborg 2012; Noel‐Weiss 2006; Olenick 2010; Raeisi 2014; Ryser 2004).
Excluded studies
We excluded 66 studies. Reasons for exclusion included: the intervention was not confined to the antenatal period only or was not an educational intervention, or the paper did not report on a randomised controlled study. For further details, see the Characteristics of excluded studies tables.
We have not considered educational and support interventions to promote BF in the intrapartum and postnatal periods in this review; related Cochrane Reviews (Britton 2007; Dyson 2005) examine these topics.
Risk of bias in included studies
We have provided details of risk of bias in each study in the Characteristics of included studies tables and the methodological quality summary (Figure 1) and methodological quality graph (Figure 2).
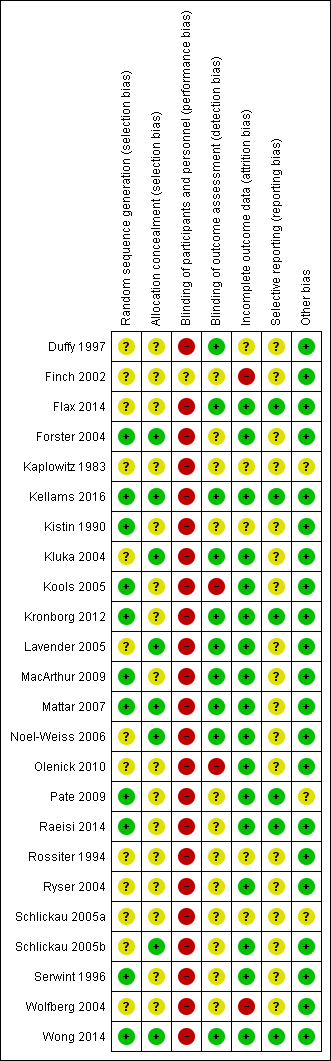
Methodological quality summary: review authors' judgements about each methodological quality item for each included study
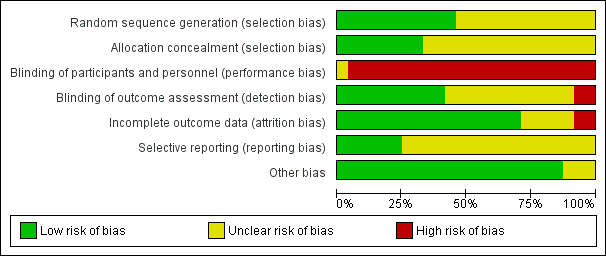
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies
Allocation
Eleven out of 24 included studies (Forster 2004; Kellams 2016; Kistin 1990; Kools 2005; Kronborg 2012; MacArthur 2009; Mattar 2007; Pate 2009; Raeisi 2014; Serwint 1996; Wong 2014) had adequate sequence generation for randomisation.
Eight out of 24 included studies (Forster 2004; Kellams 2016; Kluka 2004; Lavender 2005; Mattar 2007; Noel‐Weiss 2006; Schlickau 2005b; Wong 2014) had adequate allocation concealment.
Blinding
Only 10 included studies (Duffy 1997; Flax 2014; Kellams 2016; Kluka 2004; Kronborg 2012; Lavender 2005; MacArthur 2009; Mattar 2007; Noel‐Weiss 2006; Wong 2014) had implemented blinding; however, this blinding was only for the outcome assessors. This is perhaps mainly due to the nature of the interventions in that it was not possible to blind both women and educators. All studies were judged at high risk of performance bias except for Finch 2002 where blinding of participants and personnel was unclear.
Incomplete outcome data
Seventeen out of 24 included studies (Flax 2014; Forster 2004; Kellams 2016; Kluka 2004; Kools 2005; Kronborg 2012; Lavender 2005; MacArthur 2009; Mattar 2007; Noel‐Weiss 2006; Olenick 2010; Pate 2009; Raeisi 2014; Ryser 2004; Schlickau 2005b; Serwint 1996; Wong 2014) had low risk of attrition bias. Two studies (Finch 2002; Wolfberg 2004) had high risk of bias. Five studies (Duffy 1997; Kaplowitz 1983; Kistin 1990; Rossiter 1994; Schlickau 2005a) had unclear risk of bias.
Selective reporting
Since we did not have access to the protocols of most of the included studies, we assessed their risk of bias for selective reporting as unclear. In the current update, we assessed selective reporting as low risk of bias since all expected outcomes reported in the methods were reported in the results (Flax 2014; Kellams 2016; Pate 2009; Raeisi 2014; Wong 2014). We have also re‐assessed one trial (Kronborg 2012) for this update and have changed risk of bias from unclear to low risk for selective reporting.
Other potential sources of bias
Three out of 24 included studies (Kaplowitz 1983; Pate 2009; Schlickau 2005a) had unclear risk of other potential sources of biases. All other studies had low risk of other sources of bias.
Effects of interventions
This review includes 24 studies with 10,056 women. However, for our primary and secondary outcomes only 20 studies with 9789 women contributed data for analyses and for most comparisons, only single studies contributed outcome data. For the first five comparisons in this review we display the included trials according to type of intervention without pooling data. However, for the 'Summary of findings' table we pooled data in order to provide evidence for a summary effect for the main comparison of BF eduction versus standard care. Some studies had more than two treatment arms and are included in more than one comparison (Forster 2004; Kistin 1990; Mattar 2007; Schlickau 2005a) and some studies were cluster‐randomised trials (Flax 2014; Kools 2005; Lavender 2005; MacArthur 2009; Mattar 2007; Schlickau 2005a), and provided cluster‐adjusted odds ratios and have been analysed using the generic inverse variance method.
We have presented effects of interventions for each comparison as follows.
1. One type of BF education versus standard/routine care
For this comparison we have presented evidence according to the type of intervention. We have not pooled the totals for this comparison.
We have reported results from cluster trials that presented cluster‐adjusted odds ratios separately (Lavender 2005; MacArthur 2009).
Primary outcomes
Duration of any BF
One study (Olenick 2010) involving 165 women reported the comparison of BF education session with standard care. The mean difference (MD) in duration of any BF in the two groups was very similar in both groups (MD 0.0 weeks, 95% CI ‐2.78 to 2.78 weeks; Analysis 1.1). Another study (Schlickau 2005a) involving 16 women reported the comparison of BF education session with standard care. The intervention group had a slightly longer mean duration of BF compared with the standard care group but the CI was wide and crossed the line of no effect (MD 6.20 months, 95% CI ‐10.84 to 23.24 months; Analysis 1.1).
Proportion of women any BF at three and six months
Any BF at three months Analysis 1.2: Kluka 2004 compared a BF education workshop with standard care. This study reported data for 185 women and no increases were found in BF at three months (RR 1.07, 95% CI 0.92 to 1.24; women = 185). Wong 2014 found no group differences with a BF education session (RR 0.90, 95% CI 0.75 to 1.07; women = 469).
Any BF at six months Analysis 1.3: In Kluka 2004 there was very little difference in proportion of women exclusively BF at six months between the BF education group and the standard care group (RR 1.15, 95% CI 0.87 to 1.51; women = 178). Forster 2004 compared practical skills education with attitude education and standard care; there were no group differences in the intervention arms (skills: RR 1.01, 95% CI 0.87 to 1.17; women = 596; attitudes: RR 0.92, 95% CI 0.79 to 1.07; women = 592). Wong 2014 and Raeisi 2014 compared BF education session with standard care (Raeisi 2014 targeted the intervention at partners of pregnant women) and found no evidence of group differences (RR 1.01, 95% CI 0.86 to 1.19; women = 569; studies = 2).
Proportion of women exclusively BF at three and six months
Exclusive BF at three months Analysis 1.4: Kluka 2004 compared a BF education workshop with standard care. This study reported data for 185 women and no differences were found in exclusive BF at three months (RR 1.08, 95% CI 0.84 to 1.38; women = 185). Olenick 2010 and Wong 2014 both tested BF education sessions against standard care with no evidence of group differences (RR 1.05, 95% CI 0.85 to 1.30; women = 637; studies = 2).
Exclusive BF at six months Analysis 1.5: In Kluka 2004 there were 178 women remaining in the sample at six months and proportion of women exclusively BF in each group was very similar (RR 1.13, 95% CI 0.70 to 1.80; women = 178). Forster 2004 tested both skills education and attitudes education with no evidence for an impact on exclusive BF at this time point (skills: RR 1.19, 95% CI 0.69 to 2.05; women = 596; attitudes: RR 1.16, 95% CI 0.67 to 2.01; women = 592). Wong 2014 and Lavender 2005 did not detect group differences after an education session versus standard care (RR 1.02, 95% CI 0.80 to 1.31; women = 1094).
Initiation of BF
Single studies of different interventions were unable to show that education improved initiation of BF, apart from one small trial at high risk of attrition bias (Wolfberg 2004). Many trial results favoured the intervention but had wide confidence intervals crossing the line of no effect.
One study (Schlickau 2005b) involving 80 women compared a BF education workshop with standard care. There were no differences in initiation of BF between the two groups (RR 1.19, 95% CI 0.97 to 1.45; women = 80; Analysis 1.6). A study by Wolfberg 2004 involving partners of 59 women comparing peer counselling versus standard care showed an increase in the initiation of BF in the intervention group (RR 1.82, 95% CI 1.13 to 2.93; women = 59; Analysis 1.6). Another study (Forster 2004) compared BF practical skills education versus standard care and BF attitudes education versus standard care. Again, the number of women initiating BF was similar in both groups (skills: RR 1.01, 95% CI 0.98 to 1.04; women = 616; attitude: RR 0.99, 95% CI 0.95 to 1.02; women = 618; Analysis 1.6). Two further studies (Kronborg 2012; Olenick 2010) compared BF education sessions with standard care and showed no differences in initiation rate of BF between the two groups (pooled subtotal RR 1.03, 95% CI 0.98 to 1.09; women = 1327; Analysis 1.6). One study (Kellams 2016) with 346 women compared BF education video with standard care and, again, showed no difference in numbers of women initiating BF (RR 0.99, 95% CI 0.80 to 1.23; Analysis 1.6). Another study (Serwint 1996) with 144 women compared LC with standard care also showed no difference between the groups in initiation of BF (RR 1.33, 95% CI 0.86 to 2.07; Analysis 1.6).
Two cluster‐randomised trials reported adjusted odds ratios for this outcome, and reported peer counselling (MacArthur 2009) and group LC session (Lavender 2005) versus standard care. Both studies found women who received the intervention were slightly more likely to initiate BF, however both studies had wide confidence intervals, which crossed the line of no effect (MacArthur 2009 OR 1.11, 95% CI 0.86 to 1.43; women = 2398; Lavender 2005 OR 1.20, 95% CI 0.80 to 1.80; women = 1249; Analysis 1.7).
Duration of exclusive BF
This was not reported in any trials in this comparison.
Secondary outcomes
BF complications (mastitis, nipple trauma and pain)
Duffy 1997 compared LC versus standard care. There was no difference in numbers of women with mastitis between the groups (RR 0.20, 95% CI 0.01 to 4.02; women = 70; Analysis 1.8). However, a reduction in nipple pain as measured by visual analogue scale (VAS) scores was recorded (MD ‐19.80, 95% CI ‐23.23 to ‐16.37; women = 70; Analysis 1.9). The VAS ranged from 0 to 10 with a '0' representing 'no pain' and an increase to a maximum of 10 representing 'pain as bad as it could possibly be'. In the same study, less nipple trauma measured by nipple trauma index (NTI) scores was reported for the LC group (MD 38.65, 95% CI 32.95 to 44.35; women = 70; Analysis 1.10). The possible range of NTI was 0 to 34 with a higher NTI score indicating less trauma. One study (Kronborg 2012) with data for 1162 women compared group training programme with standard care and showed no differences in numbers of women reporting BF problems (RR 1.00, 95% CI 0.70 to 1.43; women = 1162; Analysis 1.11).
Secondary outcomes maternal satisfaction, neonatal sepsis, taking child to doctor, and hospital admission for child were not reported by any trials in this comparison. Raeisi 2014 reported no difference in infant weight gain between the intervention and control groups but the data was not in a format that could be included in an analysis.
Non‐prespecified outcomes
Two studies reported BF practices at time points not pre‐specified for this review. One study (Noel‐Weiss 2006) compared a BF education workshop with standard care. It involved 92 women and no significant increases were reported for BF at eight weeks (RR 0.91, 95% CI 0.75 to 1.11) and exclusive BF at eight weeks (RR 0.82, 95% CI 0.60 to 1.12) (data not shown in data and analyses tables). Another study (Ryser 2004) compared a BF education programme with standard care. It involved 54 women and outcomes were reported at seven days; at this time point significant increases were reported in BF (RR 1.21, 95% CI 1.03 to 1.42) (data not shown in data and analyses tables).
2. One type of BF education versus a different type of BF education
Primary outcomes
Proportion of women any BF at three and six months
Any BF at three months: one study (Kistin 1990) involving 74 women compared group discussion versus individual discussion and reported the women who received group discussion were very slightly more likely to be BF at three months but the CIs for this data were very wide and crossed the line of no effect (RR 2.84, 95% CI 0.61 to 13.18; Analysis 2.1).
Any BF at six months: Forster 2004 compared BF practical skills education versus BF attitudes education. This study reported data for 590 women and found similar proportions of women were BF at six months in each group (RR 1.09, 95% CI 0.94 to 1.28; Analysis 2.2).
Proportion of women exclusively BF at three and six months
No trial included in this comparison reported exclusive BF at three months.
Exclusive BF at six months: Forster 2004 also reported no differences between the women receiving practical skills education versus BF attitudes education who were exclusively BF at six months (RR 1.03, 95% CI 0.61 to 1.73; women = 590; Analysis 2.3).
Initiation of BF
One study (Forster 2004) involving 614 women compared BF practical skills education versus BF attitudes education. There was no difference between the numbers of women in each group who initiated BF (RR 1.02, 95% CI 0.99 to 1.06; women = 614; Analysis 2.4).
Duration of any BF, duration of exclusive BF, andproportion of women exclusively BFat three months were not reported in any trials in this comparison.
Secondary outcomes
No secondary outcomes were reported in this comparison.
3. Multiple methods of BF education versus a single method of BF education
There were limited trials available for this comparison, with most outcomes not reported.
Primary outcomes
Duration of any BF
One study (Schlickau 2005a) involving 18 women compared BF education session plus commitment to exclusive BF versus BF education session. Although women receiving multiple interventions appeared to breastfeed for slightly more days than those receiving a single intervention, the CI was wide and crossed the line of no effect (MD 8.00 days, 95% CI ‐6.84 to 22.84 days; Analysis 3.1).
Proportion of women any BF at three and six months
Any BF at six months: the study by Rossiter 1994, involving 175 women compared video plus BF education session with the provision of pamphlets. There was no evidence of a difference in BF at six months between the two groups (RR 1.59, 95% CI 0.86 to 2.94; Analysis 3.2).
Duration of exclusive BF, proportion of women any BF at three months, proportion of women exclusively BF at three and six months, and initiation of BF were not reported in any trials in this comparison.
Secondary outcomes
No secondary outcomes were reported in this comparison.
4. Different combinations of multiple methods of providing BF education
All trials contributing data for this comparison at this update were cluster‐randomised trials. We have presented the cluster‐adjusted odds ratios as reported (Kools 2005; Mattar 2007).
Primary outcomes
Proportion of women any BF at three and six months
Three months: Kools 2005, with 698 women, compared LC plus BF booklet plus 24‐hour free LC versus BF booklet plus phone number for BF questions and problems; the trial reported similar rates of BF in both groups (adjusted OR 0.82, 95% CI 0.58 to 1.16; Analysis 4.1).
Proportion of women exclusively BF at three and six months
Three months: Kools 2005 also reported no evidence of a difference in exclusive BF at three months (adjusted OR 0.79, 95% CI 0.57 to 1.09; women = 698; Analysis 4.2). Another study (Mattar 2007) compared BF booklet plus video plus LC versus BF booklet plus video. Again, the study reported no evidence of a difference in exclusive BF at three months (OR 1.40, 95% CI 0.70 to 2.80; women = 150; Analysis 4.2).
Six months: Mattar 2007 reported a marginal increase in exclusive BF in the group receiving a booklet plus video plus LC compared with the group who received a booklet plus video only (OR 2.50, 95% CI 1.00 to 6.25; women = 169; Analysis 4.3).
Duration of any BF, duration of exclusive BF, proportion of women any BF at six months, and initiation of BF were not reported in any trials in this comparison.
Secondary outcomes
No secondary outcomes were reported in this comparison.
5. Multiple methods of BF education versus standard/routine care
Two trials (Flax 2014; Mattar 2007) included in this comparison at this update were cluster‐randomised trials. For categorical variables we have presented the cluster‐adjusted odds ratios as reported in trial publications.
Primary outcomes
Duration of any BF
One study (Schlickau 2005a) involving 16 women compared BF education session plus commitment to BF versus standard care. Women in the BF education session plus commitment group breastfed for more days than those who only received standard care, however, the data for this outcome had a wide CI, which crossed the line of no effect (MD 14.20 days, 95% CI ‐2.97 to 31.37 days; Analysis 5.1).
One study (Finch 2002) involving 48 women compared LC plus incentive versus standard care; there were no significant differences in duration of BF between intervention and control group (median 12 versus six weeks, data not shown in the analysis).
Proportion of women exclusively BF at three and six months
Exclustive BF at three months Analysis 5.2: one three‐arm study (Mattar 2007) involving 234 women. We have reported each intervention arm compared with control, so Mattar 2007 appears twice in the forest plot. The intervention of BF booklet plus video plus LC versus standard care improved rates of exclusive BF (OR 2.60, 95% CI 1.25 to 5.40; women = 159). The intervention arm without a LC but with the BF booklet and video did not have the same effect on exclusive BF at three months (OR 1.80, 95% CI 0.80 to 4.05; women = 159). Flax 2014, involving 461 women, compared monthly BF sessions plus weekly cell phone message versus standard care and reported women in the intervention group were more likely than those in the standard care group to be exclusively BF at three months (OR 1.80, 95% CI 1.10 to 2.95; women = 390).
Exclusive BF at six months Analysis 5.3: at six months similar patterns of increase in exclusive BF of the three comparisons were presented. Mattar 2007 had marginal results for the intervention arm including an LC, but not otherwise (with LC OR 2.40, 95% CI 1.00 to 5.76; women = 175; without LC OR 0.90, 95% CI 0.30 to 2.70; women = 184). Flax 2014 found no group differences (OR 2.40, 95% CI 1.40 to 4.11; women = 390).
Initiation of BF
One study (Flax 2014), involving 461 women, compared monthly BF sessions plus weekly cell phone message versus standard care and reported that those in the intervention group were more likely to initiate of BF (OR 2.61, 95% CI 1.61 to 4.24; women = 380; Analysis 5.4).
Duration of exclusive BF andproportion of women any BF at three and six months were not reported in any trials in this comparison.
Secondary outcomes
No secondary outcomes were reported in this comparison.
6. Summary of findings: one type of BF education versus standard/routine care
There was no evidence that antenatal education of any sort could improve the initiation or duration of BF over the standard care offered to pregnant women. It is important to bear in mind that of the 20 studies contributing data to this review, 13 had BF education or support as part of the standard care comparator. Cluster trials presenting adjusted odds ratios were not included in this comparison. We expected substantial heterogeneity due to the different interventions and settings of trials. We used a random‐effects model for all analyses with high heterogeneity (Analysis 6.1; Analysis 6.4; and Analysis 6.5). For the summary of findings we used pooled effects of any BF education versus standard care.
No differences were observed between groups for any of the following outcomes.
-
Initiation of BF (average RR 1.01, 95% CI 0.94 to 1.09; women = 3505; studies = 8; I² = 69%; Analysis 6.1; high‐quality evidence)
-
Proportion of women exclusively BF at three months (RR 1.06, 95% CI 0.90 to 1.25; women = 822; studies = 3; I² = 0%; Analysis 6.2; moderate‐quality evidence)
-
Proportion of women exclusively BF at six months (RR 1.07, 95% CI 0.87 to 1.30; women = 2161; studies = 4; I² = 0%; Analysis 6.3; moderate‐quality evidence)
-
Proportion of women any BF at three months (average RR 0.98, 95% CI 0.82 to 1.18; women = 654; studies = 2; I² = 60%; Analysis 6.4; low‐quality evidence)
-
Proportion of women any BF at six months (average RR 1.05, 95% CI 0.90 to 1.23; women = 1636; studies = 4; I² = 61%; Analysis 6.5; high‐quality evidence)
-
Breastfeeding problems (Duffy 1997 (n = 70) reported no group differences for mastitis, but less nipple pain and less nipple trauma for women who had a lactation consultant. Kronborg 2012 (n = 1162) reported no group differences as to whether women responded 'yes' when asked about BF problems; Analysis 1.9; Analysis 1.10; Analysis 1.11; Analysis 1.8; moderate‐quality evidence)
Sensitivity analysis
For the outcomes included in our 'Summary of findings', there were no trials assessed to be of high risk of bias for allocation concealment. We did not, therefore, conduct sensitivity analysis based on removing trials of high risk of bias.
Subgroup analysis
There were insufficient trials reporting outcome data by maternal education or occupation for us to conduct this analysis. For type of intervention, all of the first five comparisons of this review displayed the type of intervention in forest plots. There were too few trials in each subgroup to compare the groups in a meaningful analysis. For this update, due to time constraints, we have not conducted subgroup analysis by trial setting.
Discussion
Summary of main results
In this update we have included 24 studies with 10,056 women. Twenty studies involving 9789 women contributed data to the analyses. There was no evidence that antenatal breastfeeding (BF) education of any sort could improve the initiation of BF, the proportion of women with any BF and exclusive BF at three or six months as well as duration of BF over the standard care. However, It is important to mention here that of the 20 studies contributing data to this review, 13 had BF education or support as part of the standard care comparator. We have presented cluster trials with adjusted odds ratios separately in comparisons 4 and 5; most cluster trials did not contribute to the pooled effects in summary of findings Table for the main comparison.
Overall completeness and applicability of evidence
Twenty‐two out of 24 studies were from high‐income countries, mainly the USA, Australia, Canada and the UK. The only two included studies not from a high‐income country were from Nigeria and Iran. Applying the results to low‐ and middle‐income countries should be done cautiously. Although we have 24 included studies, there were diverse interventions among these studies. The overall completeness of evidence in this review is therefore too limited to make any strong conclusions or generalisations.
Quality of the evidence
For the comparison BF education versus standard care, we assessed five outcomes according to GRADE methodology. We did not downgrade any trial for lack of blinding, and no included trial had adequate blinding of participants or staff. We did not downgrade for substantial heterogeneity, though we have noted this on the 'Summary of findings' (SoF) table. Evidence for two outcomes was of high quality (initiation rate of BF and proportion of women with any BF at six months). A grade of high quality suggests confidence that the result is robust to future studies. Future trials should also find that antenatal education does not appear to improve uptake of BF or BF at six months. We assessed evidence for two further outcomes as of moderate quality, suggesting some doubt about the robustness of the observed effect due to small sample size in one analysis (proportion of women exclusive BF at three months) and a wide confidence interval crossing the line of effect in another (proportion of women exclusive BF at six months). Future studies may improve our understanding of the impact of antenatal education on exclusive BF at these time points. Lastly, we assessed evidence for the outcome of proportion of women with any BF at three months as of low quality, having the most uncertainly. Please see summary of findings Table for the main comparison for further details.
Potential biases in the review process
We strictly followed the review process recommended by Cochrane (Higgins 2011c). We obtained all relevant studies identified from search results. We independently reviewed all potentially relevant studies and resolved disagreement by discussion. Potential bias in the review process should be minimal.
Agreements and disagreements with other studies or reviews
A systematic review of professional support interventions for BF concluded that interventions expanding from pregnancy to the intrapartum period and throughout the postnatal period were more effective than interventions concentrating on a shorter period. In addition, intervention packages using various methods of education and support from well‐trained professionals are more effective than interventions concentrating on a single method (Hannula 2008). However, this review included not only educational but also support interventions and did not restrict the included studies to randomised controlled trials.
Another Cochrane Review found that health education and peer support interventions can result in some improvements in the number of women beginning to breastfeed (Dyson 2005). This review is currently being updated (Dyson 2005). We we were unable to confirm if peer counselling was significantly better than formal BF education for initiation of BF due to small single trials in our subgroups.
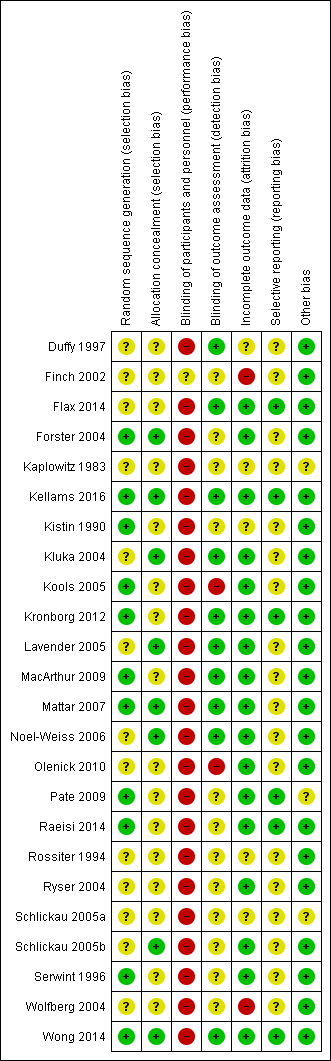
Methodological quality summary: review authors' judgements about each methodological quality item for each included study

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies

Comparison 1 One type of BF education versus standard/routine care, Outcome 1 Duration of any breastfeeding.

Comparison 1 One type of BF education versus standard/routine care, Outcome 2 Any breastfeeding at 3 months.
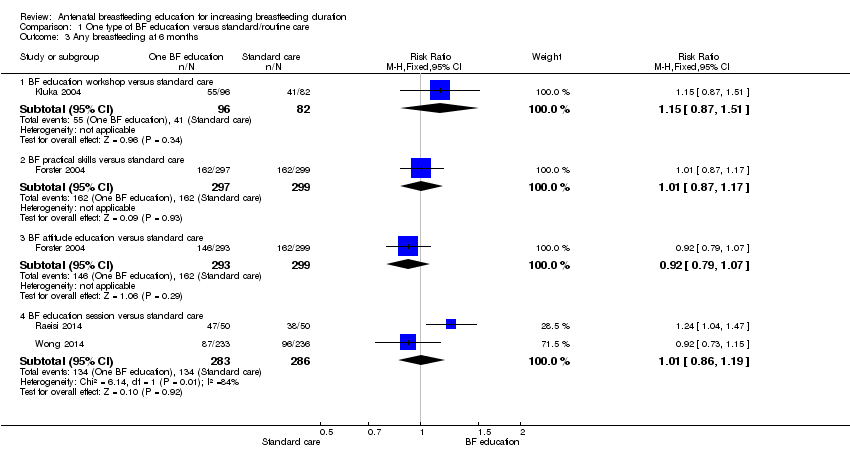
Comparison 1 One type of BF education versus standard/routine care, Outcome 3 Any breastfeeding at 6 months.
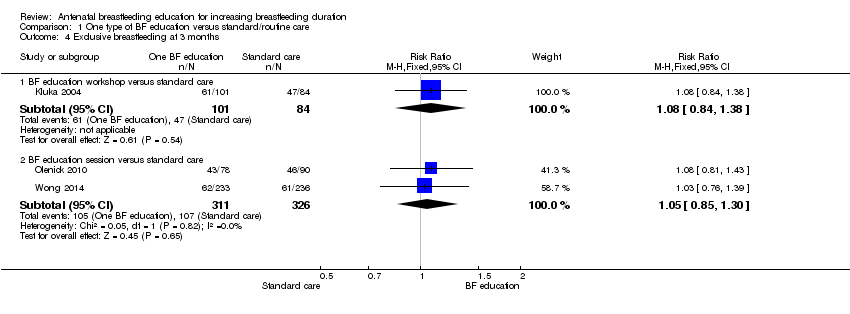
Comparison 1 One type of BF education versus standard/routine care, Outcome 4 Exclusive breastfeeding at 3 months.

Comparison 1 One type of BF education versus standard/routine care, Outcome 5 Exclusive breastfeeding at 6 months.

Comparison 1 One type of BF education versus standard/routine care, Outcome 6 Initiation of breastfeeding.

Comparison 1 One type of BF education versus standard/routine care, Outcome 7 Initiation of BF (cluster‐randomised trial).

Comparison 1 One type of BF education versus standard/routine care, Outcome 8 Mastitis.

Comparison 1 One type of BF education versus standard/routine care, Outcome 9 Breastfeeding complication (nipple pain).

Comparison 1 One type of BF education versus standard/routine care, Outcome 10 Breastfeeding complication (nipple trauma).
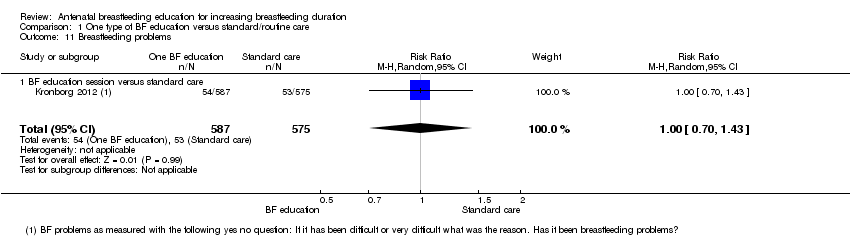
Comparison 1 One type of BF education versus standard/routine care, Outcome 11 Breastfeeding problems.

Comparison 2 One type of BF education versus a different type of BF education, Outcome 1 Any breastfeeding at 3 months.

Comparison 2 One type of BF education versus a different type of BF education, Outcome 2 Any breastfeeding at 6 months.

Comparison 2 One type of BF education versus a different type of BF education, Outcome 3 Exclusive breastfeeding at 6 months.
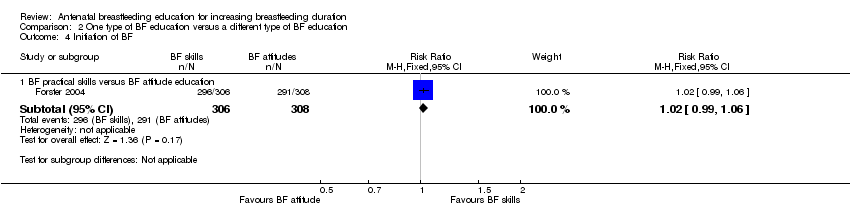
Comparison 2 One type of BF education versus a different type of BF education, Outcome 4 Initiation of BF.

Comparison 3 Multiple methods of BF education versus a single method of BF education, Outcome 1 Duration of any breastfeeding (days).

Comparison 3 Multiple methods of BF education versus a single method of BF education, Outcome 2 Any breastfeeding at 6 months.

Comparison 4 Different combinations of multiple methods of providing BF education, Outcome 1 Any breastfeeding at 4 months (cluster‐randomised trial).

Comparison 4 Different combinations of multiple methods of providing BF education, Outcome 2 Exclusive breastfeeding at 3 months.
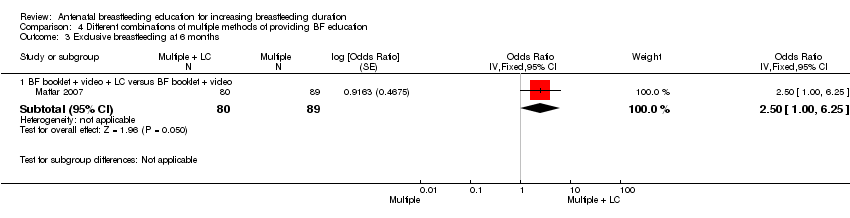
Comparison 4 Different combinations of multiple methods of providing BF education, Outcome 3 Exclusive breastfeeding at 6 months.
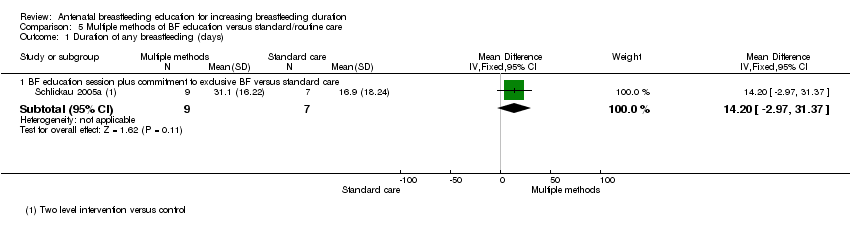
Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 1 Duration of any breastfeeding (days).

Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 2 Exclusive breastfeeding at 3 months.

Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 3 Exclusive breastfeeding at six months.
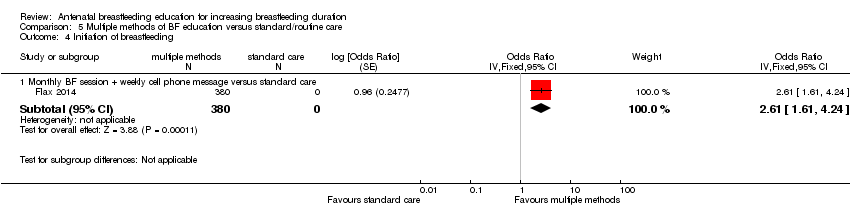
Comparison 5 Multiple methods of BF education versus standard/routine care, Outcome 4 Initiation of breastfeeding.
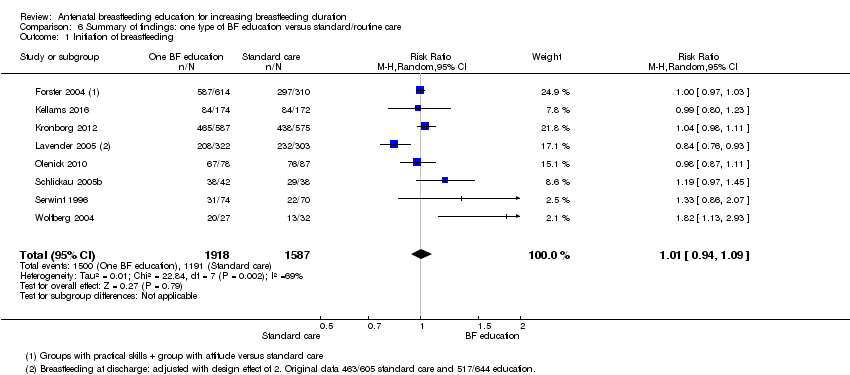
Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 1 Initiation of breastfeeding.
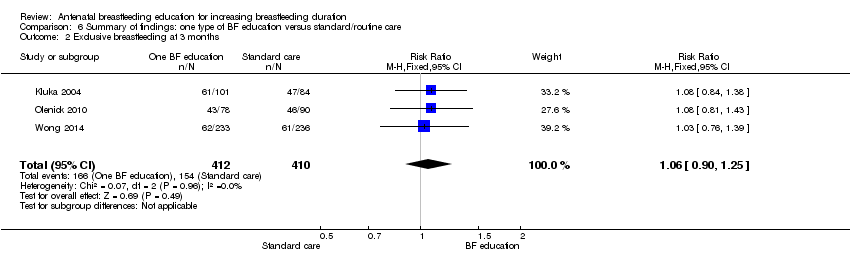
Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 2 Exclusive breastfeeding at 3 months.

Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 3 Exclusive breastfeeding at 6 months.

Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 4 Any breastfeeding at 3 months.
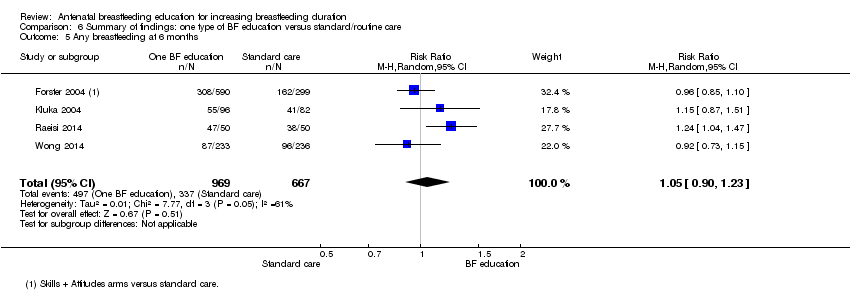
Comparison 6 Summary of findings: one type of BF education versus standard/routine care, Outcome 5 Any breastfeeding at 6 months.
| BF education versus standard/routine care | ||||||
| Patient or population: pregnant women Comparison: standard/routine care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with Standard/routine care | Risk with Summary of findings: One BF education | |||||
| Initiation of BF | Study population | average RR 1.01 | 3505 | ⊕⊕⊕⊕ | We have not downgraded any outcome for lack of blinding. No trial contributing data had adequate blinding of staff and participants | |
| 750 per 1000 | 758 per 1000 | |||||
| Proportion of women exclusively BF at 3 months | Study population | RR 1.06 | 822 | ⊕⊕⊕⊝ | ||
| 376 per 1000 | 398 per 1000 | |||||
| Proportion of women exclusively BF at 6 months | Study population | RR 1.07 | 2161 | ⊕⊕⊕⊝ | ||
| 154 per 1000 | 165 per 1000 | |||||
| Proportion of women any BF at 3 months | Study population | average RR 0.98 | 654 | ⊕⊕⊝⊝ | ||
| 609 per 1000 | 597 per 1000 | |||||
| Proportion of women any BF at 6 months | Study population | average RR 1.05 | 1636 | ⊕⊕⊕⊕ | ||
| 505 per 1000 | 531 per 1000 | |||||
| Breastfeeding complications | Duffy 1997 (n = 70) reported no group differences for mastitis, but less nipple pain and less nipple trauma for women who had a lactation consultant.2 Kronborg 2012 (n = 1162) reported no group differences as to whether women responded yes when asked about BF problems.3 | (2 studies) | Moderate | Both trials compared the intervention with standard care | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Statistical heterogeneity I² = 69% (not downgraded) 2 Downgraded for imprecision due to small sample size (‐1). 3 Downgraded for imprecision due to wide confidence intervals crossing the line of no effect (‐1). 4 Statistical heterogeneity I² = 60% (not downgraded) 5 Wide confidence intervals crossing the line of no effect and small sample size (‐2) 6 Statistical heterogeneity I² = 61% (not downgraded) | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of any breastfeeding Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 BF education session versus standard care (weeks) | 1 | 165 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐2.78, 2.78] |
| 1.2 BF education session versus standard care (days) | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 6.20 [‐10.84, 23.24] |
| 2 Any breastfeeding at 3 months Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 BF education workshop versus standard care | 1 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.92, 1.24] |
| 2.2 BF education session versus standard care | 1 | 469 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.75, 1.07] |
| 3 Any breastfeeding at 6 months Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 BF education workshop versus standard care | 1 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.87, 1.51] |
| 3.2 BF practical skills versus standard care | 1 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.87, 1.17] |
| 3.3 BF attitude education versus standard care | 1 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.79, 1.07] |
| 3.4 BF education session versus standard care | 2 | 569 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.86, 1.19] |
| 4 Exclusive breastfeeding at 3 months Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 BF education workshop versus standard care | 1 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.84, 1.38] |
| 4.2 BF education session versus standard care | 2 | 637 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.85, 1.30] |
| 5 Exclusive breastfeeding at 6 months Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 BF education workshop versus standard care | 1 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.70, 1.80] |
| 5.2 BF practical skills versus standard care | 1 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.69, 2.05] |
| 5.3 Formal BF attitude versus standard care | 1 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.67, 2.01] |
| 5.4 BF education session versus standard care | 2 | 1094 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.80, 1.31] |
| 6 Initiation of breastfeeding Show forest plot | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 BF education workshop versus standard care | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.97, 1.45] |
| 6.2 Peer counselling versus standard care | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.82 [1.13, 2.93] |
| 6.3 BF practical skills versus standard care | 1 | 616 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.98, 1.04] |
| 6.4 BF attitude education versus standard care | 1 | 618 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.95, 1.02] |
| 6.5 BF education session versus standard care | 2 | 1327 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.98, 1.09] |
| 6.6 BF education video versus standard care | 1 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.80, 1.23] |
| 6.7 LC versus standard care | 1 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.86, 2.07] |
| 7 Initiation of BF (cluster‐randomised trial) Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 7.1 Peer counselling versus standard care | 1 | 2398 | Odds Ratio (Fixed, 95% CI) | 1.11 [0.86, 1.43] |
| 7.2 Group LC session versus standard care | 1 | 1249 | Odds Ratio (Fixed, 95% CI) | 1.20 [0.80, 1.80] |
| 8 Mastitis Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 LC versus standard care | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.02] |
| 9 Breastfeeding complication (nipple pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 LC versus standard care | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐19.8 [‐23.23, ‐16.37] |
| 10 Breastfeeding complication (nipple trauma) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 LC versus standard care | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | 38.65 [32.95, 44.35] |
| 11 Breastfeeding problems Show forest plot | 1 | 1162 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.70, 1.43] |
| 11.1 BF education session versus standard care | 1 | 1162 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.70, 1.43] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any breastfeeding at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Group education versus individual education | 1 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.84 [0.61, 13.18] |
| 2 Any breastfeeding at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 BF practical skills versus BF attitude education | 1 | 590 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.94, 1.28] |
| 3 Exclusive breastfeeding at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 BF practical skills versus BF attitude education | 1 | 590 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.61, 1.73] |
| 4 Initiation of BF Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 BF practical skills versus BF attitude education | 1 | 614 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.99, 1.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of any breastfeeding (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 BF education session plus commitment to exclusive BF versus BF education session | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 8.0 [‐6.84, 22.84] |
| 2 Any breastfeeding at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Video + education session versus pamphlets | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [0.86, 2.94] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any breastfeeding at 4 months (cluster‐randomised trial) Show forest plot | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 1.1 LC + BF booklet + 24 h free LC versus BF booklet + phone number for BF questions and problems. | 1 | 698 | Odds Ratio (Fixed, 95% CI) | 0.82 [0.58, 1.16] |
| 2 Exclusive breastfeeding at 3 months Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 2.1 LC + BF booklet + 24 hrs free LC versus BF booklet + phone number for BF questions and problems. | 1 | 698 | Odds Ratio (Fixed, 95% CI) | 0.79 [0.57, 1.09] |
| 2.2 BF booklet + video + LC versus BF booklet + video | 1 | 150 | Odds Ratio (Fixed, 95% CI) | 1.40 [0.70, 2.80] |
| 3 Exclusive breastfeeding at 6 months Show forest plot | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 3.1 BF booklet + video + LC versus BF booklet + video | 1 | 169 | Odds Ratio (Fixed, 95% CI) | 2.50 [1.00, 6.25] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of any breastfeeding (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 BF education session plus commitment to exclusive BF versus standard care | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 14.20 [‐2.97, 31.37] |
| 2 Exclusive breastfeeding at 3 months Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 2.1 BF booklet + video + LC versus standard care | 1 | 159 | Odds Ratio (Fixed, 95% CI) | 2.60 [1.25, 5.40] |
| 2.2 BF booklet + video versus standard care | 1 | 159 | Odds Ratio (Fixed, 95% CI) | 1.80 [0.80, 4.05] |
| 2.3 Monthly BF session + weekly cell phone message versus standard care | 1 | 390 | Odds Ratio (Fixed, 95% CI) | 1.80 [1.10, 2.95] |
| 3 Exclusive breastfeeding at six months Show forest plot | 2 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 3.1 BF booklet + video + LC versus standard care | 1 | 175 | Odds Ratio (Fixed, 95% CI) | 2.40 [1.00, 5.76] |
| 3.2 BF booklet + video versus standard care | 1 | 184 | Odds Ratio (Fixed, 95% CI) | 0.90 [0.30, 2.70] |
| 3.3 Monthly BF session + weekly cell phone message versus standard care | 1 | 390 | Odds Ratio (Fixed, 95% CI) | 2.40 [1.40, 4.11] |
| 4 Initiation of breastfeeding Show forest plot | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 4.1 Monthly BF session + weekly cell phone message versus standard care | 1 | 380 | Odds Ratio (Fixed, 95% CI) | 2.61 [1.61, 4.24] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Initiation of breastfeeding Show forest plot | 8 | 3505 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.94, 1.09] |
| 2 Exclusive breastfeeding at 3 months Show forest plot | 3 | 822 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.90, 1.25] |
| 3 Exclusive breastfeeding at 6 months Show forest plot | 4 | 2161 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.87, 1.30] |
| 4 Any breastfeeding at 3 months Show forest plot | 2 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.82, 1.18] |
| 5 Any breastfeeding at 6 months Show forest plot | 4 | 1636 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.90, 1.23] |

