نقش ایزونیازید در پیشگیری از ابتلا به سل در کودکان مبتلا به HIV
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Trial design: double‐blind, randomized placebo‐controlled trial. Follow‐up: full blood count, liver function tests, urea and electrolyte tests, percentage of CD4 cells and viral load were measured at baseline and 6‐monthly. CXR was performed at baseline, and additional CXRs were taken if clinically indicated. Adverse events: symptoms of adverse reactions to INH were recorded at each study visit. | |
| Participants | Number of participants: 167 Median (IQR) age at baseline: 35 months (15 to 65) Inclusion criteria: age > 8 weeks, on ART for greater than 2 months, weight > 2.5 kg, adherence to ART of > 90%, prior history of TB treatment or prophylaxis, informed consent, resident in the area, access to transport. Exclusion criteria: chronic diarrhoea, currently using isoniazid prophylaxis, exposure to a TB contact, history of prior isoniazid hypersensitivity, severe anaemia (haemoglobin less than 7 gm/dL), neutropenia (absolute neutrophil count less than 400 cells/µL), thrombocytopenia (platelet count less than 50 000/µL), non‐reversible renal failure. | |
| Interventions |
All children were on ART and had adherence of at least 90% at baseline. | |
| Outcomes |
Not included in this review
| |
| Notes | Definitions: ‐ Definite TB: a microbiological or histological identification of Mycobacterium tuberculosis. ‐ Probable TB: based on a combination of typical clinical symptoms and signs, tuberculin skin testing, chest radiography, a history of close TB contact, and a documented response to antimycobacterial therapy. Country: South Africa Prevalence of isoniazid resistance: 0% Positive tuberculin test: 16% Funding: The study was funded by the Medical Research Council, South Africa; the National Research Foundation, Department of Health, South Africa; and the Discovery Foundation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization list was created using permuted blocks, stratified by HIV infection status and balanced by study site. |
| Allocation concealment (selection bias) | Low risk | Treatment groups were centrally allocated. |
| Blinding of participants and personnel (performance bias) | Low risk | "Placebo had an identical appearance to INH tablets and was administered in a double blind matter". |
| Blinding of outcome assessment (detection bias) | Low risk | "The chest radiographs were reported by a radiologist blinded to the prophylactic regimen to which the child was allocated. Diagnosis of TB was independently reviewed by an experienced clinician blinded to study randomisation". |
| Incomplete outcome data (attrition bias) | Low risk | Intention‐to‐treat analysis was followed. All participants randomized were included in analysis. |
| Selective reporting (reporting bias) | Low risk | Outcomes stated in the protocol were included in the published manuscript. |
| Other bias | Low risk | None suspected. |
| Methods | Trial design: multicentre, phase 2–3, randomized, double‐blind, placebo‐controlled trial. Follow‐up: TB disease‐free survival and incidence of TB disease at 96 weeks after randomization. Adverse events: liver enzyme tests, blood counts, clinical neurologic evaluations for peripheral neuropathy, at scheduled visits every 3 months. | |
| Participants | Number of participants: 547 Median (IQR) age at baseline: 3 months (3 to 4) Inclusion criteria: age of 91 to 120 days, received Bacille Calmette‐Guerin (BCG) vaccine, no history of TB in the infant, known exposure to a microbiological confirmed case of TB, or active anti‐TB treatment in the mother at the time of the infant's birth, no evidence of failure to thrive, recurrent pneumonia, chronic diarrhoea, or immunosuppressive conditions other than HIV infection. Exclusion criteria: previous diagnosis of TB infection, previous receipt of isoniazid, contact with a known acid fast bacilli (AFB) sputum smear or culture‐positive case of TB before study entry, current acute or recurrent (3 or more prior episodes) lower respiratory tract disease, chronic persistent diarrhoea, significant drop in weight or failure to gain weight appropriately during a 2‐ to 3‐month period, contraindications for use of isoniazid or SMX/TMP, require certain medications, known or suspected immune system diseases other than HIV, current or previous diagnosis of or treatment for cancer, current immunosuppressive therapy greater than 1 mg/kg/day of prednisone or equivalent, anticipated long‐term oral or intravenous corticosteroid therapy (greater than 3 weeks), those receiving nonsteroidal anti‐inflammatory agents and inhaled corticosteroids were not excluded, grade 3 or greater AST/SGOT, ALT/SGPT, ANC, haemoglobin, platelet count, rash, neuropathy, or myopathy at screening, any grade 4 clinical or laboratory toxicity within 14 days prior to study entry, other acute or chronic conditions that, in the opinion of the investigator, may interfere with the study. | |
| Interventions |
At baseline, 98.7% of the children were on ART. ART mainly included stavudine, lamivudine, and lopinavir‐ritonavir or zidovudine, lamivudine, and lopinavir– ritonavir, following per country‐specific guidelines. | |
| Outcomes |
Not included in this review
| |
| Notes | Definitions: ‐ Definite TB: a microbiological or histological identification of Mycobacterium tuberculosis. ‐ Probable TB: based on a combination of typical clinical symptoms and signs, tuberculin skin testing, chest radiography, a history of close TB contact, and a documented response to antimycobacterial therapy. All infants were enrolled in the first 6 months of life. The study included HIV‐uninfected children with outcomes defined differently for this subgroup, however, analysis of HIV‐uninfected children was not included in this review. All HIV‐infected children also received trimethoprim–sulfamethoxazole prophylaxis 5 mg/kg according to WHO guidelines. TB disease‐free survival was defined as the first occurrence of death from any cause or TB disease, 96 weeks after randomization. HIV disease progression, was defined as the first occurrence of worsening of the Centers for Diseases Control and Prevention (CDC) clinical categorization of HIV infection or death. Country: South Africa, Botswana Prevalence of isoniazid resistance (95% CI): 26% (9 to 51) Positive tuberculin test: not reported Funding: The study was supported by the Statistical and Data Analysis Center at the Harvard School of Public Health, under NIAID cooperative agreements with the Pediatric AIDS Clinical Trials Group (5 U01 AI41110) and the IMPAACT Group (1 U01 AI068616); NIAID and the NICHD International and Domestic Pediatric and Maternal HIV Clinical Trials Network (NICHD contract number N01‐DK‐9‐001/HHSN267200‐800001C); Secure the Future Fund, a philanthropy program sponsored by Bristol‐Myers Squibb. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization list was created using permuted blocks". |
| Allocation concealment (selection bias) | Low risk | Treatment groups were centrally allocated. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants, caregivers and investigators were blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | "End point review committee was unaware of study‐group assignments". |
| Incomplete outcome data (attrition bias) | Low risk | Intention‐to‐treat analysis was followed, however, its not clear if all enrolled participants were included in analysis. |
| Selective reporting (reporting bias) | Low risk | All important outcomes stated in the study protocol were reported in the published manuscript. |
| Other bias | Low risk | None suspected. |
| Methods | Trial design: double‐blind, placebo‐controlled trial. Follow‐up: children underwent a tuberculin skin test and chest radiography if clinically indicated. Adverse events: alanine transaminase were measured one and three months after randomization and thereafter six‐monthly or more frequently if clinically indicated. | |
| Participants | Number of participants: 277 Median (IQR) age at baseline: 25 months (9 to 52) Inclusion criteria: age > 8 weeks, weight > 2.5 kg, access to transport, informed consent, children stable on ART for two to three months. Exclusion criteria: chronic diarrhoea, current use of or need for isoniazid prophylaxis, previous hypersensitivity to isoniazid or sulphur containing drugs, haemoglobin < 70 g/L, neutrophil count < 400 cell/uL, platelet count < 50,000 x109/L, non‐reversible renal failure. | |
| Interventions |
ART was not widely available. Some children obtained treatment through participation in pharmaceutical trials or charitable donations. 23 of 263 (9%) were on ART at enrolment and 58 (22%) started treatment during the trial. | |
| Outcomes |
Not included in this review: none | |
| Notes | Definitions: ‐ Definite TB: a microbiological or histological identification of Mycobacterium tuberculosis. ‐ Probable TB: based on a combination of typical clinical symptoms and signs, tuberculin skin testing, chest radiography, a history of close TB contact, and a documented response to antimycobacterial therapy. Cotrimoxazole (5 mg/kg/dose of the trimethoprim component): Given to all children < 12 months and those older with clinical CDC category B or C disease, in those with severe immunological impairment (CD4 count of < 15% of total lymphocyte count), or in those with previous episode of Pneumocystis jirovecii pneumonia. Study was planned to run for 2 years, however, the placebo arm was terminated early on the recommendation of the data safety monitoring board on the basis of the results of interim analyses. About 30% of the children received ART during the trial with similar percentages in isoniazid and placebo groups. Adverse events were graded 1 to 4 according to the toxicity criteria of the National Institutes of Health's division of AIDS (DAIDS). Grade 3 and 4 events were reported. Country: South Africa Prevalence of isoniazid resistance: 0% Positive tuberculin test: 9% Funding: The study was supported by Rockefeller Foundation, USA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A variable block random list was used. Generation of allocation sequence was achieved by variable blocked randomization lists prepared by the trial statistician and sent to each trial site pharmacist in a sealed opaque envelope. |
| Allocation concealment (selection bias) | Low risk | Central allocation (pharmacists labelled trial drugs with sequential numbers). The participants were allocated study numbers sequentially by the study nurse at enrolment. They were then sequentially allocated to treatment group by the pharmacist according to the prepared list. |
| Blinding of participants and personnel (performance bias) | Low risk | Placebo was manufactured to have an identical appearance to isoniazid, participants and personnel were blinded to study assignment. |
| Blinding of outcome assessment (detection bias) | Low risk | Investigators assessing the outcome and were blinded, the diagnosis of probable TB was subject to independent review by a blinded investigator. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate was very low, < 20%. |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the study protocol were the same as those in the published manuscript. |
| Other bias | Unclear risk | The data safety monitoring board recommended randomization into placebo to be stopped after 277 of the planned 432 were enrolled. The placebo arm was ended on 17 May 2004 on the recommendation of the data safety monitoring board on the basis of the results of interim analyses. |
Abbreviations:
ALT/SGPT: Alanine aminotransferase (serum glutamic pyruvic transaminase)
ANC: Absolute neutrophil count
ART: Antiretroviral therapy
AST/SGOT: Aspartate aminotransferase (serum glutamic‐oxaloacetic transaminase)
CDC: Centers for Diseases Control and Prevention
CXR: Chest x‐rays
INH: Isoniazid
SMX/TMP: Trimethoprim/Sulfamethoxazole
TB: Tuberculosis
WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| A cohort study. | |
| Secondary analysis of Madhi 2011. | |
| Commentary. | |
| Not addressing review outcomes; secondary analysis of Zar 2007. | |
| Cohort study. Secondary analysis of Zar 2007. | |
| Commentary. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Active TB Show forest plot | 3 | 737 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.50, 1.14] |
| Analysis 1.1  Comparison 1 Isoniazid prophylaxis versus placebo for HIV‐positive children on antiretroviral therapy (ART), Outcome 1 Active TB. | ||||
| 2 Death Show forest plot | 3 | 737 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.78, 2.72] |
| Analysis 1.2  Comparison 1 Isoniazid prophylaxis versus placebo for HIV‐positive children on antiretroviral therapy (ART), Outcome 2 Death. | ||||

Study flow diagram.
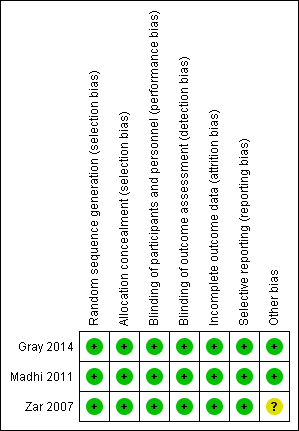
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.

'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies.

Forest plot of comparison: 1 Isoniazid prophylaxis versus placebo, outcome: 1.1 Active TB, HIV‐positive children on ART.

Forest plot of comparison: 1 Isoniazid prophylaxis versus placebo, outcome: 1.2 Death, HIV‐positive children on ART.

Comparison 1 Isoniazid prophylaxis versus placebo for HIV‐positive children on antiretroviral therapy (ART), Outcome 1 Active TB.

Comparison 1 Isoniazid prophylaxis versus placebo for HIV‐positive children on antiretroviral therapy (ART), Outcome 2 Death.
| Isoniazid prophylaxis compared to placebo for HIV‐positive children not on antiretroviral therapy (ART) | ||||||
| Patient or population: HIV‐positive children not taking ART | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comment | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Isoniazid prophylaxis | |||||
| Active TB | 10 per 100 | 3 per 100 (1 to 9) | HR 0.31 (95% CI 0.11 to 0.87) | 240 (1 trial) | ⊕⊕⊝⊝ due to serious indirectness and imprecision | Isoniazid prophylaxis may reduce active TB |
| Death | 17 per 100 | 8 per 100 (8 per 17) | HR 0.46 (95% CI 0.22 to 0.95) | 240 (1 trial) | ⊕⊕⊝⊝ due to serious indirectness and imprecision | Isoniazid prophylaxis may reduce death |
| The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1No serious risk of bias: this trial was at low risk of selection bias, and adequately blinded study participants and personnel. However, the study was stopped early on the recommendation of the data safety monitoring board after only 277 of the planned 432 were enrolled. Not downgraded. | ||||||
| Isoniazid prophylaxis compared to placebo for HIV‐positive children on antiretroviral therapy (ART) | ||||||
| Patient or population: HIV‐positive children on ART | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Isoniazid prophylaxis | |||||
| Active TB | 13 per 100 | 9 per 100 | RR 0.76 | 737 | ⊕⊝⊝⊝ due to serious indirectness and imprecision | We don't know if Isoniazid prophylaxis reduce active TB |
| Death | 4 per 100 | 6 per 100 | RR 1.45 (0.78 to 2.72) | 737 | ⊕⊝⊝⊝ due to serious indirectness and imprecision | We don't know if Isoniazid prophylaxis reduce death |
| The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1No serious risk of bias: trials were at low risk of selection bias. Both studies adequately blinded study participants and personnel. | ||||||
| Number of children with adverse events | Number of adverse events | |||||||
| Children not on ART | Children on ART | Children on ART | Children on ART | |||||
| Isoniazid prophylaxis group N = 91 | Placebo group N = 91 | Isoniazid prophylaxis group N = 41 | Placebo group N = 40 | Isoniazid prophylaxis group N = 273 | Placebo group N = 274 | Isoniazid prophylaxis group N= 85 | Placebo group N = 82 | |
| Clinical adverse events | ||||||||
| Peripheral neuropathy | Not reported | Not reported | Not reported | Not reported | 3 | 2 | Not reported | Not reported |
| Other clinical adverse events | Not reported | Not reported | Not reported | Not reported | 14 | 23 | 1 | 1 |
| Laboratory adverse events | ||||||||
| Haematological (neutropenia, thrombocytopenia, anaemia) | 5 | 6 | 0 | 0 | 10 | 9 | Not reported | Not reported |
| Liver enzyme abnormalities | 0 | 2 | 0 | 0 | 12 | 12 | 3 | 1 |
| Other laboratory adverse events | Not reported | Not reported | 0 | 0 | Not reported | Not reported | Not reported | Not reported |
| Abbreviations: ART: antiretroviral therapy; N: number of participants. | ||||||||
| Outcome | Assumed risk | Source | Clinically important relative reduction | Sample size required1,2 |
| Active TB | 46/366 (13%) | 25% | 2990 | |
| Death | 15/366 (4%) | 50% | 2282 | |
| 1We based all calculations on: 2‐sided tests, with a ratio of 1:1, power of 0.8, and confidence level of 0.05. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Active TB Show forest plot | 3 | 737 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.50, 1.14] |
| 2 Death Show forest plot | 3 | 737 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.78, 2.72] |

