Fisioterapia torácica para la neumonía en adultos
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised, parallel‐group trial | |
| Participants | In‐patient setting; relevant details of health status of participants; age; sex; country 50 treatment, 48 control 16 to 95 years old (mean 65) Male/female: 84 /61 Conducted in Sweden | |
| Interventions | The physiotherapy was positive expiratory pressure (PEP). In this study a bottle containing 10 cm of tap water was used. Patients were asked to sit up with their feet on the floor and blow bubbles at a calm speed into the bottle through a plastic tube (10 mm in diameter) with an air pressure just sufficient to overcome the resistance of the water. This method was used 20 times per hour from 9 am to 8 pm and continued after discharge. This study consisted of three group (A, B, C). Group A was control which underwent early mobilisation and "huffing". Group B members were given the same as A and deep breaths. Group C members were given the same as A and the method of bottle‐blowing | |
| Outcomes | Primary outcomes: death Secondary outcomes: duration of hospital stay (days); fever clearance time; CRP; VC; FEV1; PEF | |
| Notes | The study was supported financially by the Orebro County Council Research Committee and the Orebro Medical Center Research Foundation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The randomised method was not clearly reported |
| Allocation concealment (selection bias) | Low risk | "Sealed envelopes" were used |
| Blinding (performance bias and detection bias) | High risk | No blinding |
| Incomplete outcome data (attrition bias) | Low risk | 19 (13%) patients were drop‐outs. However, ITT analysis was performed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
| Methods | Randomised, parallel‐group, single‐blind trial | |
| Participants | In‐patient setting; relevant details of health status of participants; age; sex; country 83 treatment, 88 control 15 to 75 years old (control: 47.2, treatment: 47.4) Male/female: 74/97 Conducted in Sweden | |
| Interventions | The chest physiotherapy consisted of postural drainage, external help with breathing, percussion and vibration. The placebo was to receive advice on expectoration, deep breathing and how to exercise to avoid thrombosis | |
| Outcomes | Primary outcomes: death; cure rate Secondary outcomes: duration of hospital stay (days); healing time (days); fever clearance time; FEV1 | |
| Notes | The study was approved by the ethical committee of the Karolinska Hospital, Stockholm Sources of funding were not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The randomised method was not clearly reported |
| Allocation concealment (selection bias) | Low risk | "Sealed envelopes" were used |
| Blinding (performance bias and detection bias) | Low risk | Outcome assessor was blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | High risk | The standard deviations of duration of hospital stay and fever were not reported |
| Methods | Randomised, parallel‐group trial | |
| Participants | In‐patient setting; relevant details of health status of participants; age; sex; country 27 treatment, 27 control Age (mean ± SD): control: 63 ± 3 years old, treatment: 61 ± 4 years old Male/female: control 13/14, treatment 14/13 Conducted in Sweden | |
| Interventions | The chest physiotherapy consisted of postural drainage, chest percussion and vibration, with encouragement of deep breathing and coughing. This therapy was used concomitantly with intermittent positive pressure breathing every 4 hours during the first 24 hours. Therapy was given for at least 3 days to all the treated participants, with an average duration of 5 days | |
| Outcomes | Primary outcomes: death; cure rate Secondary outcomes: duration of hospital stay (days); rate of clearing of X‐ray film; fever clearance time | |
| Notes | The study was supported by a grant (PHS 17292) to the Vermont Lung Center from the National Heart, Lung, and Blood Institute, National Institutes of Health Sources of funding not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomisation was not described |
| Allocation concealment (selection bias) | Low risk | "Sealed envelopes" were used |
| Blinding (performance bias and detection bias) | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
| Methods | Randomised, parallel‐group, double‐blind trial | |
| Participants | In‐patient setting; relevant details of health status of participants; age; sex; country 11 in treatment group, 10 in control group The mean age was 78.7 in the control group, 82.5 in the treatment group Male/female: control 3/7, treatment 3/8 The trial was conducted in the United States | |
| Interventions | Patients in the treatment group received a standardised osteopathic manipulative treatment protocol treatment consisting of 7 osteopathic manipulative techniques and non‐standardised osteopathic manipulative treatments from an osteopathic manipulative treatment specialist, while participants in the control group received a standardised light touch protocol treatment (sham treatment), with care taken not to move myofascial structures or to articulate joints. The session was 10 to 15 minutes, and the frequency of treatment was 2 sessions per day | |
| Outcomes | Primary outcomes: death; cure rate Secondary outcomes: duration of hospital stay (days); rate of clearing of X‐ray film; duration of antibiotic therapy; duration of leukocytosis | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomisation was not described |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | Low risk | Patients and outcome assessors were blinded |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
| Methods | Randomised, double‐blind, parallel trial | |
| Participants | In‐patient setting; relevant details of health status of participants; age; sex; country 28 in treatment group; 30 in control group Age (mean ± SD): control group: 77.0 ± 17.2 years old; treatment group: 77.7 ± 17.1 years old Male/female: control group: 16/14; treatment group: 14/14 The trial was conducted in the United States | |
| Interventions | Patients in the treatment group received a standardised osteopathic manipulative treatment protocol treatment consisting of 7 osteopathic manipulative techniques and non‐standardised osteopathic manipulative treatments from an osteopathic manipulative treatment specialist, while participants in the control group received a standardised light touch protocol treatment (sham treatment), with care taken not to move myofascial structures or to articulate joints. The session was 10 to 15 minutes, and the frequency of treatment was 2 sessions per day | |
| Outcomes | Primary outcomes: death; cure rate Secondary outcomes: duration of hospital stay (days); rate of clearing of X‐ray film; duration of antibiotic therapy; change in leukocyte count; mean leukocyte count | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomisation was not described |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | Low risk | Patients and outcome assessors were blinded |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
| Methods | Randomised, parallel‐group trial | |
| Participants | In‐patient setting; relevant details of health status of participants; age; sex; country 12 treatment, 20 control Age (mean ± SD): control: 36.80 ± 16.91 years old, treatment: 42.08 ± 15.59 years old Male/female: control 10/10, treatment 9/3 Conducted in UK | |
| Interventions | The physiotherapy was active cycle of breathing techniques, which consisted of breathing control using the diaphragm; localised expansion exercises; postural drainage; thoracic expansion exercises with vibrations on expiration; percussion. The first 2 methods were continued to discharge and the other methods were used when participants became productive of sputum. The dose of the therapy was dependent on the patient's tolerance and the sputum production | |
| Outcomes | Primary outcomes: death; cure rate Secondary outcomes: duration of hospital stay (days); rate of clearing of X‐ray film; duration of all antibiotic therapy; duration of production of sputum; in‐patient sputum weight | |
| Notes | This study was under the funding of Norwich Health Authority and the East Anglian Regional Health Authority Research Committee | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomisation was not described |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | High risk | Blinding was not performed |
| Incomplete outcome data (attrition bias) | Low risk | Only 4 (11%) patients did not complete the study. Among them, 1 patient died, 2 patients were re‐diagnosed as having other disease and 1 patient could not attend sufficient assessments |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
CRP: C‐reactive protein
VC: vital capacity
FEV1: forced expiratory volume in the first second
ITT: intention‐to‐treat
PEF: peak expiratory flow
OMT: osteopathic manipulative treatment
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Physical agent; no control | |
| Secondary publications under Britton 1985 | |
| Secondary publications under Britton 1985 | |
| The participants had diffuse panbronchiolitis | |
| This study was not a RCT or quasi‐RCT. It covered mechanical ventilation for patients with acute respiratory failure caused by pneumonia | |
| Study was about mechanical ventilation for patients with pneumonia | |
| Study was about respiratory failure caused by pneumonia | |
| Study was about respiratory failure caused by pneumonia | |
| It was a prevention study | |
| In addition to pneumonia, the participants also had asthma, chronic bronchitis or bronchiectasis. Not a RCT or quasi‐RCT | |
| In addition to pneumonia, the participants had atelectasis. Not a RCT or quasi‐RCT | |
| Not a RCT or quasi‐RCT | |
| Some participants with pneumonia also had congestive heart failure or diabetes mellitus. Not a RCT or quasi‐RCT | |
| Some participants with pneumonia also had COPD or asthma. A before‐and‐after study in the same participants | |
| It was a study protocol | |
| Some participants in the study were less than 18 years old. There was no subgroup analysis for adults provided in the study | |
| The participants also had asthma, lung cancer, COPD or pulmonary embolism | |
| Participants had lower respiratory tract infections, not only pneumonia. Not a RCT or quasi‐RCT | |
| The participants also had chronic bronchitis or acute bronchitis, not only pneumonia. Not a RCT or quasi‐RCT | |
| Participants had a pulmonary infection, not only pneumonia. Not a RCT or quasi‐RCT | |
| Participants had a pulmonary infection, not only pneumonia. Not a RCT or quasi‐RCT | |
| Participants had pneumonia caused by chronic bronchitis. Not a RCT or quasi‐RCT | |
| Participants had a pulmonary infection, not only pneumonia. Not a RCT or quasi‐RCT | |
| Participants had lower respiratory tract infections, not only pneumonia. Not a RCT or quasi‐RCT | |
| The participants had acute lung abscesses. Not a RCT or quasi‐RCT | |
| Participants had pneumonia caused by COPD, not only pneumonia. Not a RCT or quasi‐RCT |
COPD: chronic obstructive pulmonary disease
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Unclear |
| Participants | Unclear |
| Interventions | Unclear |
| Outcomes | Unclear |
| Notes | — |
| Methods | Unclear |
| Participants | Unclear |
| Interventions | Unclear |
| Outcomes | Unclear |
| Notes | — |
| Methods | Unclear |
| Participants | Unclear |
| Interventions | Unclear |
| Outcomes | Unclear |
| Notes | — |
| Methods | Unclear |
| Participants | Unclear |
| Interventions | Unclear |
| Outcomes | Unclear |
| Notes | — |
| Methods | Unclear |
| Participants | Unclear |
| Interventions | Unclear |
| Outcomes | Unclear |
| Notes | — |
| Methods | Unclear |
| Participants | Unclear |
| Interventions | Unclear |
| Outcomes | Unclear |
| Notes | — |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Multi‐Center Osteopathic Pneumonia Study in the Elderly (MOPSE) |
| Methods | Randomised, double‐blind, placebo‐controlled trial |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | The first group: osteopathic manipulative treatment (OMT) The second group: light touch control The third group: conventional care only |
| Outcomes | Primary outcome measures: length of hospital stay, time to clinical stability, rate of symptomatic and functional recovery |
| Starting date | March 2004 |
| Contact information | Not available |
| Notes | The trial had been completed when we were drafting this review, however it has not yet been published |
IV: intravenous
WBC: white blood cell
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.15, 7.13] |
| Analysis 1.1  Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 1 Mortality. | ||||
| 2 Cure rate Show forest plot | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.91, 1.04] |
| Analysis 1.2  Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 2 Cure rate. | ||||
| 3 Duration of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3 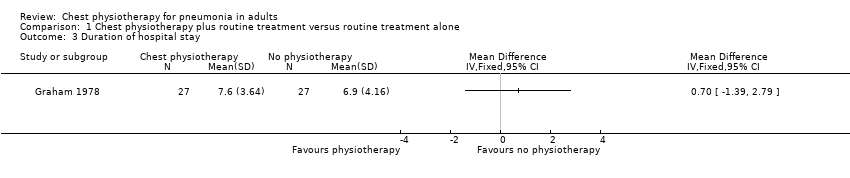 Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 3 Duration of hospital stay. | ||||
| 4 Duration of fever Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 4 Duration of fever. | ||||
| 5 Rate of improvement of chest X‐ray Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 5 Rate of improvement of chest X‐ray. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cure rate Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 1 Cure rate. | ||||
| 2 Duration of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 2 Duration of hospital stay. | ||||
| 3 Rate of improvement of chest X‐ray Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 3 Rate of improvement of chest X‐ray. | ||||
| 4 Duration of antibiotic therapy Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.4  Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 4 Duration of antibiotic therapy. | ||||
| 5 Duration of sputum production Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.5  Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 5 Duration of sputum production. | ||||
| 5.1 In‐patient | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Out‐patient | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Total | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 In‐patient sputum weight Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.6  Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 6 In‐patient sputum weight. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 2 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.05, 1.57] |
| Analysis 3.1 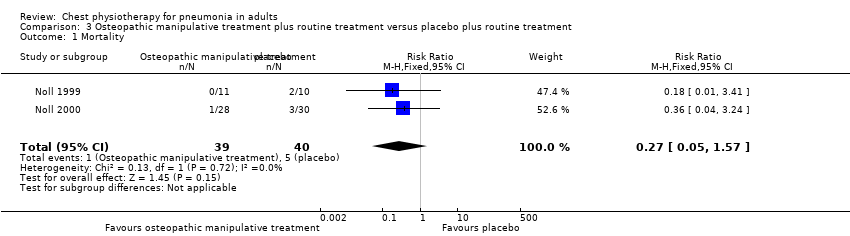 Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 1 Mortality. | ||||
| 2 Cure rate Show forest plot | 2 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.97, 2.46] |
| Analysis 3.2 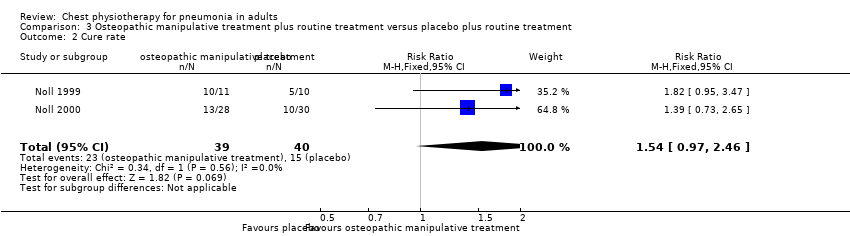 Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 2 Cure rate. | ||||
| 3 Duration of hospital stay Show forest plot | 2 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐2.02 [‐3.46, ‐0.58] |
| Analysis 3.3 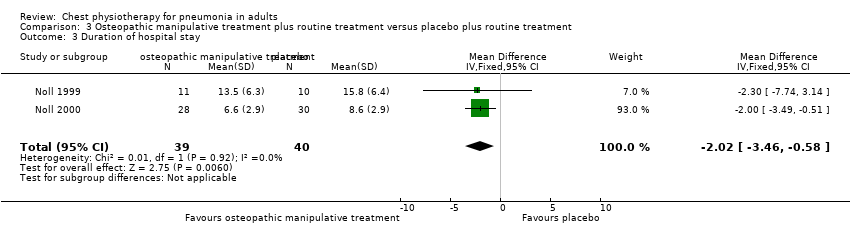 Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 3 Duration of hospital stay. | ||||
| 4 Duration of fever Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.4  Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 4 Duration of fever. | ||||
| 5 Rate of improvement of chest X‐ray Show forest plot | 2 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.77, 1.73] |
| Analysis 3.5 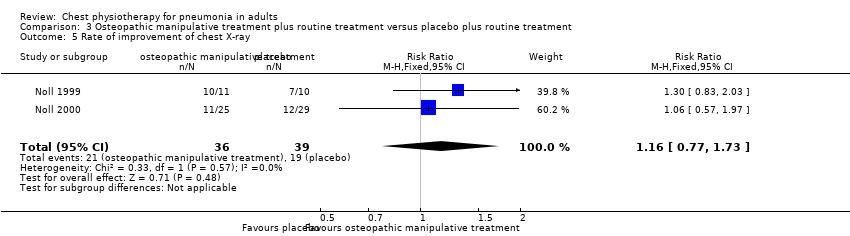 Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 5 Rate of improvement of chest X‐ray. | ||||
| 6 Duration of oral antibiotic therapy Show forest plot | 2 | 79 | Mean Difference (IV, Random, 95% CI) | 0.97 [‐1.25, 3.20] |
| Analysis 3.6  Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 6 Duration of oral antibiotic therapy. | ||||
| 7 Duration of intervenous therapy Show forest plot | 2 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐2.11 [‐3.36, ‐0.87] |
| Analysis 3.7  Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 7 Duration of intervenous therapy. | ||||
| 8 Duration of total antibiotic therapy Show forest plot | 2 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐1.93 [‐3.12, ‐0.74] |
| Analysis 3.8  Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 8 Duration of total antibiotic therapy. | ||||
| 9 Duration of leukocytosis Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.9  Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 9 Duration of leukocytosis. | ||||
| 10 Change in leukocyte count Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.10  Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 10 Change in leukocyte count. | ||||
| 10.1 Change between Day 3 and 1 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Change between Day 5 and 1 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Mean leukocyte count Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.11  Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 11 Mean leukocyte count. | ||||
| 11.1 Day 3 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Day 5 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.1  Comparison 4 Positive expiratory pressure plus routine treatment versus routine treatment alone, Outcome 1 Duration of hospital stay. | ||||
| 2 Duration of fever Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.2 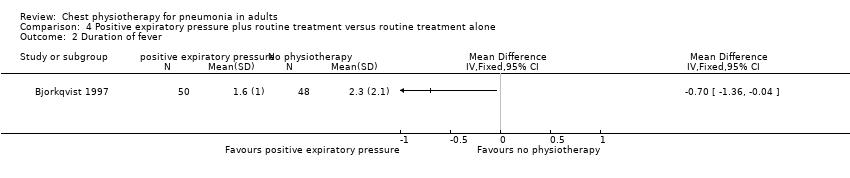 Comparison 4 Positive expiratory pressure plus routine treatment versus routine treatment alone, Outcome 2 Duration of fever. | ||||
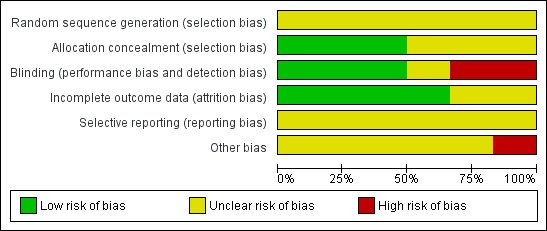
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Chest physiotherapy plus routine treatment versus routine treatment alone, outcome: 1.1 Mortality.

Forest plot of comparison: 1 Chest physiotherapy plus routine treatment versus routine treatment alone, outcome: 1.2 Cure rate.

Forest plot of comparison: 3 OMT plus routine treatment versus placebo plus routine treatment, outcome: 3.1 Mortality.

Forest plot of comparison: 3 OMT plus routine treatment versus placebo plus routine treatment, outcome: 3.2 Cure rate.

Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 1 Mortality.

Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 2 Cure rate.

Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 3 Duration of hospital stay.
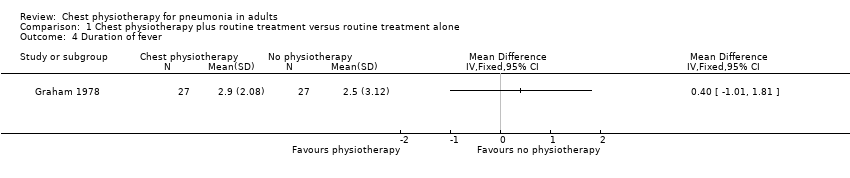
Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 4 Duration of fever.

Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 5 Rate of improvement of chest X‐ray.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 1 Cure rate.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 2 Duration of hospital stay.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 3 Rate of improvement of chest X‐ray.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 4 Duration of antibiotic therapy.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 5 Duration of sputum production.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 6 In‐patient sputum weight.
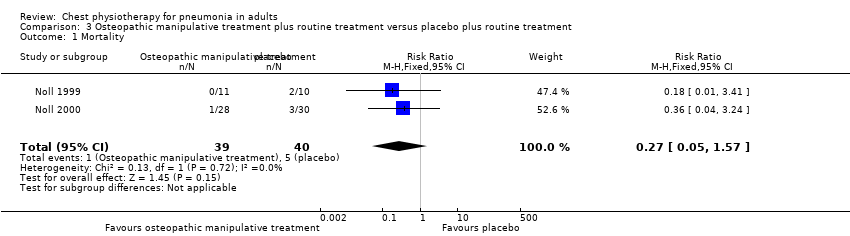
Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 1 Mortality.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 2 Cure rate.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 3 Duration of hospital stay.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 4 Duration of fever.
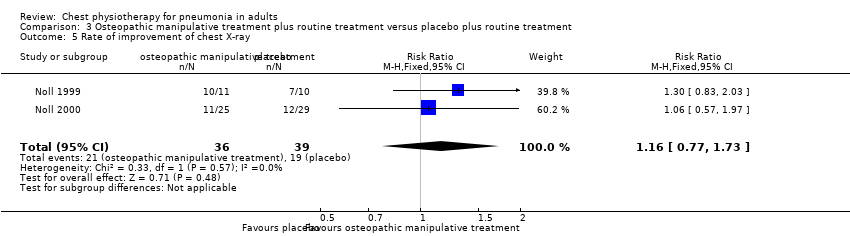
Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 5 Rate of improvement of chest X‐ray.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 6 Duration of oral antibiotic therapy.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 7 Duration of intervenous therapy.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 8 Duration of total antibiotic therapy.
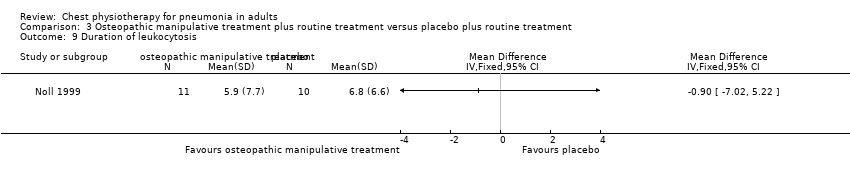
Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 9 Duration of leukocytosis.
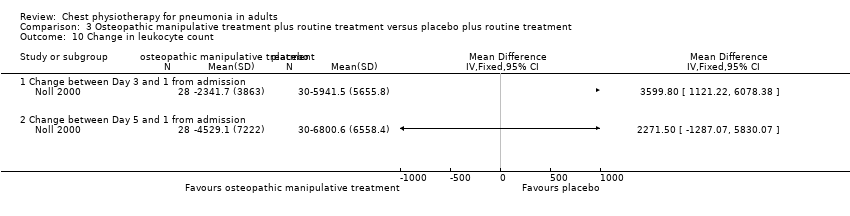
Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 10 Change in leukocyte count.
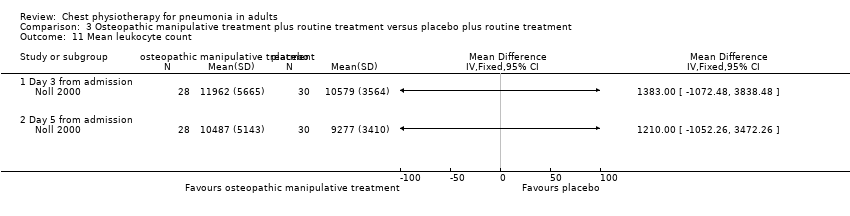
Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 11 Mean leukocyte count.
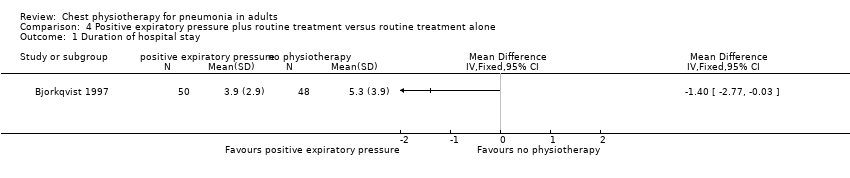
Comparison 4 Positive expiratory pressure plus routine treatment versus routine treatment alone, Outcome 1 Duration of hospital stay.

Comparison 4 Positive expiratory pressure plus routine treatment versus routine treatment alone, Outcome 2 Duration of fever.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.15, 7.13] |
| 2 Cure rate Show forest plot | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.91, 1.04] |
| 3 Duration of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Duration of fever Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Rate of improvement of chest X‐ray Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cure rate Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Duration of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Rate of improvement of chest X‐ray Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Duration of antibiotic therapy Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Duration of sputum production Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 In‐patient | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Out‐patient | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Total | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 In‐patient sputum weight Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 2 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.05, 1.57] |
| 2 Cure rate Show forest plot | 2 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.97, 2.46] |
| 3 Duration of hospital stay Show forest plot | 2 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐2.02 [‐3.46, ‐0.58] |
| 4 Duration of fever Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Rate of improvement of chest X‐ray Show forest plot | 2 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.77, 1.73] |
| 6 Duration of oral antibiotic therapy Show forest plot | 2 | 79 | Mean Difference (IV, Random, 95% CI) | 0.97 [‐1.25, 3.20] |
| 7 Duration of intervenous therapy Show forest plot | 2 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐2.11 [‐3.36, ‐0.87] |
| 8 Duration of total antibiotic therapy Show forest plot | 2 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐1.93 [‐3.12, ‐0.74] |
| 9 Duration of leukocytosis Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10 Change in leukocyte count Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Change between Day 3 and 1 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Change between Day 5 and 1 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Mean leukocyte count Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 Day 3 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Day 5 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Duration of fever Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |

