Fisioterapia torácica para la neumonía en adultos
Resumen
Antecedentes
A pesar de que la evidencia es contradictoria, la fisioterapia torácica se ha usado ampliamente como tratamiento adyuvante para los adultos con neumonía.
Objetivos
Evaluar la efectividad y seguridad de la fisioterapia torácica para el tratamiento de la neumonía en adultos.
Métodos de búsqueda
Se hicieron búsquedas en CENTRAL 2012, número 11, MEDLINE (1966 hasta noviembre, semana 2, 2012), EMBASE (1974 hasta noviembre 2012), Physiotherapy Evidence Database (PEDro) (1929 hasta noviembre 2012), CINAHL (2009 hasta noviembre 2012) y CBM (1978 hasta noviembre 2012).
Criterios de selección
Ensayos controlados aleatorizados (ECA) que evaluaran la eficacia de la fisioterapia torácica para el tratamiento de la neumonía en adultos.
Obtención y análisis de los datos
Dos autores de la revisión, de forma independiente, evaluaron la elegibilidad de los ensayos, extrajeron los datos y evaluaron la calidad de los ensayos. Los resultados primarios fueron la mortalidad y la tasa de curación. Se utilizaron los riesgos relativos (RR) y la diferencia de medias (DM) para los resultados de los ensayos individuales en el análisis de datos. Se realizó el metanálisis y se midieron todos los resultados con intervalos de confianza (IC) del 95%.
Resultados principales
Seis ECA (434 participantes) evaluaron cuatro tipos de fisioterapia torácica (fisioterapia torácica convencional; tratamiento con manipulación osteopática (que incluye inhibición paraespinal, elevación de costillas y liberación miofascial); ciclo activo de técnicas de respiración (que incluye control activo de la respiración, ejercicios de expansión torácica y técnicas de espiración forzada); y presión espiratoria positiva).
Ninguna de las fisioterapias (versus ninguna fisioterapia o placebo) mejoró las tasas de mortalidad en los adultos con neumonía.
La fisioterapia torácica convencional (versus ninguna fisioterapia), el ciclo activo de técnicas respiratorias (versus ninguna fisioterapia) y el tratamiento de manipulación osteopática (versus placebo) no aumentaron la tasa de curación o la tasa de mejoría en las radiografías de tórax.
El tratamiento con manipulación osteopática (versus placebo) y la presión respiratoria positiva (versus ninguna fisioterapia) redujeron la duración media de la estancia hospitalaria en 2,0 días (diferencia de medias [DM] ‐2,0 días; IC del 95%: ‐3,5 a ‐0,6) y 1,4 días (DM ‐1,4 días; IC del 95%: ‐2,8 a ‐0,0), respectivamente. No fue así con la fisioterapia torácica convencional y el ciclo activo de técnicas respiratorias.
La presión expiratoria positiva (versus ninguna fisioterapia) redujo la duración de la fiebre (DM ‐0,7 días; IC del 95%: ‐1,4 a ‐0,0). No fue así con el tratamiento con manipulación osteopática.
El tratamiento con manipulación osteopática (versus placebo) redujo la duración del tratamiento con antibióticos intravenoso (DM ‐2,1 días; IC del 95%: ‐3,4 a ‐0,9) y completo (DM ‐1,9 días; IC del 95%: ‐3,1 a ‐0,7).
Las limitaciones de esta revisión son que los estudios que consideraron el tratamiento con manipulación osteopática fueron pequeños, y que los seis estudios publicados que parecen reunir los criterios de inclusión están a la espera de clasificación.
Conclusiones de los autores
Sobre la base de la evidencia limitada actual, la fisioterapia torácica no puede recomendarse como tratamiento adicional sistemático para la neumonía en los adultos.
PICOs
Resumen en términos sencillos
Fisioterapia torácica para la neumonía en adultos
La neumonía es uno de los problemas de salud más frecuentes que afecta a todos los grupos etarios en todo el mundo. Los antibióticos representan la base del tratamiento de la neumonía, mientras otros tratamientos son principalmente de apoyo. La fisioterapia torácica se ha usado ampliamente como tratamiento adyuvante para la neumonía en los adultos sin evidencia fiable.
Se incluyeron seis ensayos controlados aleatorizados que evaluaron a 434 participantes. Los estudios evaluaron cuatro tipos de fisioterapia torácica: la fisioterapia torácica convencional, el tratamiento con manipulación osteopática (que incluye inhibición paraespinal, elevación de costillas y liberación miofascial diafragmática o blanda), el ciclo activo de técnicas respiratorias (que incluye control respiratorio activo, ejercicios de expansión torácica y técnica de espiración forzada) y la presión expiratoria positiva. Ninguna de estas técnicas (versus ninguna fisioterapia o tratamiento con placebo) reduce la mortalidad. En tres de las técnicas (fisioterapia torácica convencional, ciclo activo de técnicas respiratorias y tratamiento con manipulación osteopática), no existe evidencia que apoye una mejor tasa de curación en comparación con ninguna fisioterapia o tratamiento con placebo. La evidencia limitada indica que la presión expiratoria positiva (versus ninguna fisioterapia) y el tratamiento con manipulación osteopática (versus tratamiento con placebo) pueden reducir levemente la duración de la estancia hospitalaria (en 2,02 y 1,4 días, respectivamente). Además, la presión expiratoria positiva (versus ninguna fisioterapia) puede reducir levemente la duración de la fiebre por 0,7 días; y el tratamiento con manipulación osteopática (versus tratamiento con placebo) puede reducir la duración del uso de antibióticos en 1,93 días. No se encontraron eventos adversos graves.
En resumen, la fisioterapia torácica no debe recomendarse como tratamiento adicional sistemático para la neumonía en los adultos. La limitación de la revisión es que los seis estudios publicados que parecen satisfacer los criterios de inclusión están a la espera de clasificación (cinco de los cuales están publicados en idioma ruso).
Authors' conclusions
Background
Description of the condition
Pneumonia is caused most commonly by bacteria but occasionally by viruses, fungi, parasites and other infectious agents. It is the leading cause of death from infectious disease (Niederman 2001). Pneumonias are typically classified as community‐acquired pneumonia, hospital‐acquired pneumonia (nosocomial pneumonia) and ventilator‐associated pneumonia (the most serious form of nosocomial pneumonia, infecting patients who are mechanically ventilated for other reasons). It is estimated that community‐acquired pneumonia costs the United States USD 12.2 billion in treatment per year (Colice 2004), with an average mortality rate of 14% (Fine 1990). Nosocomial pneumonia is the second most common nosocomial infection and the leading cause of death from hospital‐acquired infection (Bowton 1999).
Description of the intervention
Antibiotics represent the mainstay of pneumonia treatment, while other therapies are mostly supportive. These adjunctive therapies include supplementary oxygen, intravenous hydration and chest physiotherapy (George 1995). Chest physiotherapy is an airway clearance technique that combines manual percussion of the chest wall by a caregiver, strategic positioning of the patient for mucous drainage, and teaching cough and breathing techniques.
Conventional chest physiotherapy includes postural drainage, percussion, chest shaking, huffing and coughing. Recently, several new physiotherapy techniques have been developed, including the active cycle of breathing techniques, positive expiratory pressure and osteopathic manipulative treatment. Active cycle of breathing techniques include active breathing control, thoracic expansion exercises and forced expiration technique, and sometimes postural drainage and chest clapping. Positive expiratory pressure uses devices to provide a positive expiratory pressure of 10 to 25 cmH20 during expiration. It may stabilise airways by keeping them open during expiration, which may facilitate airway clearance. Osteopathic manipulative treatment includes bilateral paraspinal inhibition, bilateral rib raising, diaphragmatic myofascial release and soft myofascial release to the anterior thoracic inlet. It may improve chest wall mobility and enhance exercise tolerance.
How the intervention might work
Chest physiotherapy assists in treating some of the symptoms of respiratory disorders, such as airflow obstruction, alterations in ventilatory pump functions and impaired exercise performance. The aim is to improve the patient's respiratory status and expedite recovery by enhancing airway clearance in lung diseases associated with hypersecretion and reduced airway resistance. Increased airway clearance enhances gas exchange and reduces the work of breathing (Wallis 1999). Chest physiotherapy is best used for patients with copious secretions (more than 30 ml/day) and reduced ability to cough (Cochrane 1977; Graham 1978).
Why it is important to do this review
Chest physiotherapies for cystic fibrosis, acute bronchiolitis and patients undergoing mechanical ventilation have been reviewed (Flenady 2010; Roqué i Figuls 2012; Van der Schans 2009). However, the clinical effectiveness of chest physiotherapy for pneumonia is controversial. Some clinical studies have concluded that chest physiotherapy did not hasten the resolution of pneumonia (Graham 1978) or was not useful (Britton 1983; Britton 1985). Two studies suggested that larger or multi‐centre trials were needed to confirm the findings (Ntoumenopoulos 2002; Tydeman 1989). Others concluded that chest physiotherapy had beneficial effects in patients with pulmonary infection (Hanying 2005). However, chest physiotherapy may be ineffective and even harmful. It may cause an increase in oxygen consumption (Horiuchi 1997; Weissman 1991; Weissman 1993), bronchospasm (Campbell 1975), induce hypertension, increase oxygen demand (Horiuchi 1997; Weissman 1993), cause hypoxaemia (Connors 1980; Poelaert 1991) and even lead to rib fractures (Chalumeau 2002).
To our knowledge, no systematic review or meta‐analysis of chest physiotherapy for pneumonia has been published. This review aims to systematically review all randomised controlled trials (RCTs) which examine the effectiveness of chest physiotherapy for pneumonia in adults.
Objectives
To assess the effectiveness and safety of chest physiotherapy for pneumonia in adults.
Methods
Criteria for considering studies for this review
Types of studies
We considered all randomised controlled trials (RCTs) assessing the efficacy of chest physiotherapy for adult participants with any type of pneumonia. We included trials which also included other basic respiratory diseases, once pneumonia was diagnosed; we analysed such trials separately. We excluded trials in which physiotherapy was administered for the prevention of pneumonia, as pneumonia could occur in many conditions, such as trauma, cerebral vessels disease and postoperative conditions. We included both published and unpublished trials.
Types of participants
Adult participants (older than 18 years of age) of either gender, with any type of pneumonia. Pneumonia was defined by each original trial author. We included intubated or non‐intubated participants.
Types of interventions
Chest physiotherapy of any type was compared with no chest physiotherapy. We included trials using traditional chest physiotherapy. We included trials using mechanical devices which have the same effect as traditional chest physiotherapy. We considered the following methods: postural drainage, chest percussion, vibration, thoracic oscillation, chest shaking, huffing, directed coughing, thoracic expansion, forced exhalation or expiration techniques and manual hyperinflation.
Types of outcome measures
Primary outcomes
-
Mortality.
-
Cure rate (the definitions of 'cure' and the 'time to cure' were determined by original trial authors).
Secondary outcomes
-
Duration of hospital stay (days).
-
Healing time (days) (subjective or objective assessment of time to complete recovery).
-
Duration of fever (days) (fever defined as more than 37.5 degrees).
-
Rate of improvement of chest X‐ray (chest X‐ray improvement was defined as any improvement on chest X‐ray after treatment compared with before treatment. The assessment could be made by radiologists or clinicians).
-
Duration of antibiotic therapy (days).
-
Duration of sputum production (days).
-
In‐patient sputum weight.
-
Duration of leukocytosis (days).
-
Change in leukocyte count.
-
Mean leukocyte count.
Adverse events
We defined serious adverse events according to the International Conference on Harmonisation (ICH) Guidelines (ICH 1997) as any event that: leads to death, is life‐threatening, requires in‐patient hospitalisation or prolongation of existing hospitalisation, results in persistent or significant disability, and any important medical event which may harm the patient or requires intervention to prevent it. All other adverse events were considered non‐serious.
Search methods for identification of studies
Electronic searches
For this update we searched the Cochrane Central Register of Controlled Trials (CENTRAL) 2012, Issue 11, part of The Cochrane Library, www.thecochranelibrary.com (accessed 21 November 2012), which contains the Cochrane Acute Respiratory Infections (ARI) Group's Specialised Register, MEDLINE (August 2009 to November week 2, 2012), EMBASE (August 2009 to November 2012), Physiotherapy Evidence Database (PEDro) (August 2009 to November 2012), CINAHL (2009 to November 2012) and CBM (1978 to November 2012). Please see Appendix 1 for details of the previous search.
We used the following search strategy to search CENTRAL and MEDLINE. We combined the MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision), Ovid format (Lefebvre 2011). We adapted these search terms to search EMBASE (see Appendix 2), PEDro (see Appendix 3) and CINAHL (see Appendix 4).
MEDLINE (OVID)
1 exp Pneumonia/
2 pneumon*.tw.
3 (bronchopneumon* or pleuropneumon*).tw.
4 Respiratory Tract Infections/
5 (lower respiratory tract infection* or lower respiratory infection* or lrti).tw.
6 (lung adj3 (inflamm* or infect*)).tw.
7 empyema, pleural/ or pleural effusion/ or exp pleurisy/
8 (pleural adj3 (empyema or effusion*)).tw.
9 pleurisy.tw.
10 or/1‐9
11 exp Physical Therapy Modalities/
12 (physiotherap* or physical therap* or physical treatment*).tw.
13 Vibration/
14 exp Respiratory Therapy/
15 exp Positive‐Pressure Respiration/
16 postural drain*.tw.
17 (patient* adj3 position*).tw.
18 (oscillat* or vibrat* or percuss* or huff*).tw.
19 ((chest or thora*) adj3 (clap* or shak* or compress*)).tw.
20 (forced adj2 (exhal* or expir*)).tw.
21 (cough* adj2 (directed or maneuver* or manoeuver* or techniqu*)).tw.
22 (breath* adj2 (control* or techni* or train* or exercis*)).tw.
23 positive pressure ventilation*.tw.
24 positive expiratory pressure*.tw.
25 electrostimulat*.tw.
26 massag*.tw.
27 ((respirat* or ventilat*) adj2 muscle train*).tw.
28 (osteopath* adj3 (manipulat* or treatment* or therap* or techniq*)).tw.
29 or/11‐28
30 10 and 29
Searching other resources
We handsearched related journals. We did not impose any language or publication restrictions.
Data collection and analysis
Selection of studies
Two review authors (XLY, BYW) independently searched the databases. Two review authors (BYW, YPY) independently assessed the titles and abstracts to identify potentially relevant articles. We excluded the trials which failed to meet the inclusion criteria. Differences were resolved by the arbitrator (BRD).
Data extraction and management
Two review authors (XLY, BYW) independently extracted data using a standardised form. A third review author (MY) checked the extracted data. Extracted data included, where possible:
-
description of participants (including age, gender, type of pneumonia);
-
severity of pneumonia;
-
basic conditions and setting;
-
description of intervention (details of chest physiotherapy, including type, frequency, intensity and time);
-
description of control therapy;
-
methodological details (including design and recruitment);
-
method of randomisation;
-
sample size;
-
trial inclusion and exclusion criteria;
-
withdrawals;
-
description of outcomes (including mortality, duration of hospital stay, adverse events, cure, healing time, rate of clearing of X‐ray film and duration of fever); and
-
source of funding.
Assessment of risk of bias in included studies
Two review authors (XLY, BYW) independently assessed trial quality based on the generation of the allocation sequence, allocation concealment, blinding and follow‐up. Finally, we assessed the risks of bias as follows: A = low risk of bias (all of the criteria met); B = moderate risk of bias (one or more criteria partly met); C = high risk of bias (one or more criteria not met). Differences were resolved by the arbitrator (BRD).
The detailed quality components were as follows.
Generation of the allocation sequence
Adequate: computer‐generated random numbers, table of random numbers, or similar.
Unclear: the trial was described as randomised, but the generation of the allocation sequence was not described. Inadequate: the allocation sequence was generated by some rules based on date of admission, record number, date of birth, and so on.
Allocation concealment
Adequate: concealed up to the point of treatment by central randomisation, sealed envelopes or similar.
Unclear: the allocation concealment procedure was not described.
Inadequate: open table of random numbers or similar.
Blinding
Adequate: since the intervention of chest physiotherapy was extremely difficult to mask completely, it was rare to have double‐blinding. Hence, we considered single‐blinding as adequate.
Unclear: if the method of blinding was not described.
Not performed: if the trial was not blinded.
Follow‐up
Adequate: if the numbers and reasons for drop‐outs and withdrawals in all intervention groups were described or if it was specified that there were no drop‐outs or withdrawals.
Unclear: if the report gave the impression that there had been no drop‐outs or withdrawals, but this was not specifically stated.
Inadequate: if the number or reasons for drop‐outs and withdrawals were not described.
Measures of treatment effect
We expressed dichotomous data, such as cure rate or mortality, as risk ratios (RR). We expressed continuous data, such as duration of fever, as mean differences (MD). We reported all outcomes with 95% confidence intervals (CIs).
Unit of analysis issues
The unit of analysis was the individual, because all RCTs included in this review were simple parallel‐group trials in which participants were randomly allocated to several groups and a single result for each outcome from each individual was collected and analysed. There were no complicated designs, such as cross‐over or cluster‐randomisation, used in the included RCTs.
Dealing with missing data
We contacted trial authors (by e‐mail, letter or fax) to search for additional papers, and to confirm data extraction and obtain missing data.
Assessment of heterogeneity
We assessed heterogeneity in trial results by inspecting the forest plots to detect non‐overlapping CIs, applying the Chi2 test with a P value of 0.10 indicating statistical significance, and implementing the I2 statistic (with a value of 50% to denote moderate levels of heterogeneity). In the case of heterogeneity between studies, we made efforts to explore sources of heterogeneity due to various factors, such as type of pneumonia and type of physiotherapy.
Assessment of reporting biases
We could not perform a funnel plot analysis to identify reporting biases because of the small number of included studies.
Data synthesis
We used RevMan (version 5.0) (RevMan 2011) to combine some outcomes. We used a fixed‐effect model unless significant heterogeneity was noted; in which case we used a random‐effects model. We calculated both the effect sizes and the summary measures with their 95% CIs.
Subgroup analysis and investigation of heterogeneity
We performed a subgroup analysis for different types of chest physiotherapies and outcomes.
Sensitivity analysis
We did not perform a sensitivity analysis in this review.
Results
Description of studies
See the 'Characteristics of included studies' and 'Characteristics of excluded studies' tables.
Results of the search
In this 2012 update we retrieved a total of 835 records from the electronic databases after duplicates had been removed. After screening the titles and abstracts we identified two publications (Dangour 2011; Noll 2008) as potentially eligible, which we retrieved in full text. However, both of them were excluded.
In the 2009 search we retrieved 1329 articles by electronic database searching (383 in MEDLINE, 452 in EMBASE, 105 in CBM, 378 in CENTRAL, six in PEDro and five in the National Research Register). After screening the titles and abstracts we identified 68 trials as potentially relevant, which we retrieved in full text. Among those, six trials (Bjorkqvist 1997; Britton 1985; Graham 1978; Noll 1999; Noll 2000; Tydeman 1989) met the inclusion criteria (see 'Characteristics of included studies' table). Seven trials which appeared to meet the inclusion criteria have not yet been included or excluded in this review, as five of them (Kuznetsov 1976; Kuznetsov 1980a; Kuznetsov 1980b; Sedov 1975; Vorob'ev 1984) are published in Russian, one (Facto 1947) was published in 1947 and we have not yet managed to retrieve the full text, and the seventh trial (Noll) is as yet unpublished.
Included studies
Six trials (Bjorkqvist 1997; Britton 1985; Graham 1978; Noll 1999; Noll 2000; Tydeman 1989) were included in this review, of which three (Graham 1978; Noll 1999; Noll 2000) were conducted in the United States, two (Bjorkqvist 1997; Britton 1985) in Sweden, and one (Tydeman 1989) in the United Kingdom. All of them were randomised, parallel‐group controlled trials.
Participants
In total, 434 participants (215 males, 219 females) were involved in the six trials, with 211 participants in the treatment group and 223 participants in the control group. The participants' ages ranged from 15 to 94 years. The included trials involved participants with acute pneumonia. Two trials (Bjorkqvist 1997; Tydeman 1989) included community‐acquired pneumonia only, two trials (Noll 1999; Noll 2000) included community‐acquired pneumonia, nosocomial pneumonia and nursing home‐acquired pneumonia. The remaining two trials (Britton 1985; Graham 1978) did not describe the type of pneumonia. The severity of pneumonia was mild to moderate in two trials (Graham 1978; Tydeman 1989), and not stated in the other four trials (Bjorkqvist 1997; Britton 1985; Noll 1999; Noll 2000). The baseline characteristics of the experiment and control groups of each included trial were comparable.
Interventions
Two trials (Noll 1999; Noll 2000) compared chest physiotherapy and routine treatment to placebo and routine treatment. In the other four trials (Bjorkqvist 1997; Britton 1985; Graham 1978; Tydeman 1989) chest physiotherapy and routine treatment was compared with routine treatment alone. Among these trials, the types of chest physiotherapies were significantly different to each another, including conventional chest physiotherapy, osteopathic manipulative treatment, active cycle of breathing techniques and positive expiratory pressure. Both treatment groups and control groups were given routine treatments such as antibiotics, oxygen therapy and other drug therapies, if necessary.
Outcome measures
The primary outcomes were mortality and cure rate. Mortality could be calculated from data from all included trials. However, cure rate was calculated from five included trials (Britton 1985; Graham 1978; Noll 1999; Noll 2000; Tydeman 1989). The following secondary outcomes were reported in some of the included trials:
-
duration of hospital stay (Bjorkqvist 1997; Britton 1985; Graham 1978; Noll 1999; Noll 2000; Tydeman 1989);
-
healing time (Britton 1985);
-
duration of fever (Bjorkqvist 1997; Britton 1985; Graham 1978);
-
rate of improvement of chest X‐ray (Graham 1978; Noll 1999; Noll 2000; Tydeman 1989);
-
duration of antibiotic therapy (Noll 1999; Noll 2000; Tydeman 1989);
-
duration of sputum production (Tydeman 1989);
-
in‐patient sputum weight (Tydeman 1989);
-
duration of leukocytosis (Noll 1999);
-
change in leukocyte count (Noll 2000);
-
mean leukocyte count (Noll 2000); and
-
adverse effects: one trial (Noll 2000) reported adverse effects, another trial (Bjorkqvist 1997) stated no side effects were reported during the period of study, and the remaining trials did not discuss this outcome.
Excluded studies
For reasons for excluding studies please see the 'Characteristics of excluded studies' table.
Risk of bias in included studies
The detailed risk of biases and quality of each study are explained in the Characteristics of included studies table. We identified none of the included trials as 'low risk of bias', we assessed three trials (Graham 1978; Noll 1999; Noll 2000) as 'moderate risk of bias', and we assessed three trials (Bjorkqvist 1997; Britton 1985; Tydeman 1989) as 'high risk of bias' (Figure 1; Figure 2). None of the studies were supported by pharmaceutical company funding.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All six trials explicitly stated that randomisation was used in their studies. However, none mentioned the method of randomisation. Only three studies clearly described the method of allocation concealment (Bjorkqvist 1997; Britton 1985; Graham 1978).
Blinding
Participants and outcome assessors were blinded in two studies (Noll 1999; Noll 2000). In one trial (Britton 1985) only participants were blinded. Two studies (Bjorkqvist 1997; Tydeman 1989) clearly stated that blinding was not conducted. One study (Graham 1978) did not describe whether blinding was used or not.
Incomplete outcome data
Each of the included studies had a statement on drop‐outs or withdrawals. Two studies (Noll 1999; Noll 2000) had no drop‐outs, and four studies (Bjorkqvist 1997; Britton 1985; Graham 1978; Tydeman 1989) had more than 10% drop‐outs. An intention‐to‐treat (ITT) analysis was not used in these four studies (Bjorkqvist 1997; Britton 1985; Graham 1978; Tydeman 1989).
Selective reporting
There was no evidence of selective outcome reporting.
Other potential sources of bias
One trial (Britton 1985) did not report the standard deviation of duration of hospital stay and fever.
Effects of interventions
Because of the obvious clinical heterogeneity between different chest physiotherapies, we presented the results as comparisons between:
-
conventional chest physiotherapy plus routine treatment versus routine treatment alone;
-
active cycle of breathing techniques plus routine treatment versus routine treatment alone;
-
osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment; and
-
positive expiratory pressure plus routine treatment versus routine treatment alone.
We only used a placebo with the osteopathic manipulative treatment because in the two trials (Noll 1999; Noll 2000) using this therapy, participants in the control group received standardised light touch treatment as placebo, in addition to the routine treatment. In the remaining trials, participants in the control group received routine treatment alone.
1. Conventional chest physiotherapy plus routine treatment versus routine treatment alone
Two trials (Britton 1985; Graham 1978) including 225 participants, with 110 participants in the treatment group and 115 participants in the control group, appraised the effect of conventional chest physiotherapy.
1.1 Primary outcomes
1.1.1 Mortality
The meta‐analysis of the two trials (Britton 1985; Graham 1978) using a fixed‐effect model indicated that there was no significant difference between conventional chest physiotherapy plus routine treatment and routine treatment alone (risk ratio (RR) 1.03, 95% confidence interval (CI) 0.15 to 7.13) (Figure 3).
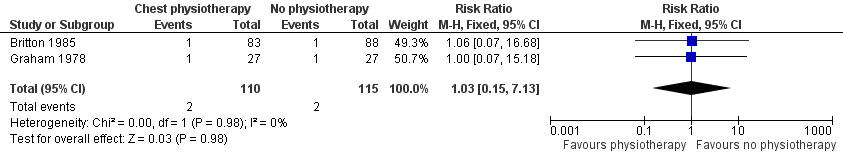
Forest plot of comparison: 1 Chest physiotherapy plus routine treatment versus routine treatment alone, outcome: 1.1 Mortality.
1.1.2. Cure rate
Among the two included trials (Britton 1985; Graham 1978), all participants were cured in both treatment group and control group in one trial (Britton 1985); the other trial (Graham 1978) reported that cure rates in the treatment group and control group were 59.26% and 70.37%, respectively. However, there was no significant difference between the two groups (RR 0.84, 95% CI 0.57 to 1.25) (Figure 4).

Forest plot of comparison: 1 Chest physiotherapy plus routine treatment versus routine treatment alone, outcome: 1.2 Cure rate.
1.2 Secondary outcomes
1.2.1 Duration of hospital stay
Meta‐analysis could not be performed, as one of the included trials (Britton 1985) did not report the standard deviation of duration of hospital stay. This study (Britton 1985) found that "there was no significant difference between the treatment and control groups" (P value was not available). The other trial (Graham 1978) reached a similar result (mean difference (MD) 0.7 day, 95% CI ‐1.39 to 2.79).
1.2.2 Duration of fever
One of the included trials (Britton 1985) did not report the standard deviation of duration of fever, therefore meta‐analysis could not be carried out. Britton (Britton 1985) found the mean duration of fever in the treatment group and control group was 6.8 and 4.9 days, respectively (P < 0.01). The other trial (Graham 1978) reported the mean duration of fever in treatment group and control group was 2.9 and 2.5 days, respectively. However, there was no statistical significance between the groups (P = 0.64).
1.2.3 Rate of improvement of chest X‐ray
Only one trial (Graham 1978) reported this outcome, which indicated that conventional chest physiotherapy had no benefit on improvement of chest X‐ray (RR 0.85, 95% CI 0.59 to 1.22).
1.2.4 Healing time
One trial (Britton 1985) reported healing time as a secondary outcome. The mean healing time was 30.6 days in the treatment group, and 31.3 days in the control group. However, it reported "there was no significant difference between groups" (P value was unavailable).
2. Active cycle of breathing techniques plus routine treatment versus routine treatment alone
Only one trial (Tydeman 1989) including 32 participants (12 in the treatment group and 20 in the control group) was included in this review.
2.1 Primary outcomes
2.1.1 Mortality
No participants died during the study period.
2.1.2 Cure rate
The cure rates in the treatment group and the control group were 41.67% and 70.00% respectively, with no statistical significance between groups (RR 0.60, 95% CI 0.29 to 1.23).
2.2 Secondary outcomes
2.2.1 Duration of hospital stay
The duration of hospital stay (mean ± SD) was 6.67 ± 3.26 days in the treatment group, and 5.27 ± 2.26 days in the control group. However, there was no significant difference between groups (MD 1.40 days, 95% CI ‐0.69 to 3.49).
2.2.2 Rate of improvement of chest X‐ray
Active cycle of breathing techniques had no benefit for rate of improvement of chest X‐ray (RR 0.60, 95% CI 0.29 to 1.23).
2.2.3 Duration of antibiotic therapy
The duration of antibiotic therapy (mean ± SD) was 15.17 ± 6.70 days in the treatment group, and 15.02 ± 5.53 days in the control group. No significant difference was identified between groups (MD 0.15 day, 95% CI ‐4.39 to 4.69).
2.2.4 Duration of sputum production
The mean duration of sputum production seemed to be 0.37 days longer in the treatment group than in the control group, but there was no significant difference between groups (MD ‐0.37, 95% CI ‐3.74 to 3.00). The subgroup analysis indicated that there were no significant differences in both in‐patient and out‐patient populations in terms of duration of sputum production (MD 0.83 day, 95% CI ‐1.57 to 3.23; MD ‐1.20 days, 95% CI ‐3.28 to 0.88, respectively).
2.2.5 In‐patient sputum weight
Active cycle of breathing techniques did not improve the in‐patient sputum weight either (MD 4.9 g, 95% CI ‐1.82 to 11.62).
3. Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment
We identified two trials (Noll 1999; Noll 2000), involving 79 participants in total, with 39 in the treatment group and 40 in the control group.
3.1 Primary outcomes
3. 1.1 Mortality
Compared with placebo, osteopathic manipulative treatment did not improve mortality (RR 0.27, 95% CI 0.05 to 1.57) (Figure 5).

Forest plot of comparison: 3 OMT plus routine treatment versus placebo plus routine treatment, outcome: 3.1 Mortality.
3.1.2 Cure rate
Osteopathic manipulative treatment did not increase cure rate in comparison with placebo (RR 1.54, 95% CI 0.97 to 2.46) (Figure 6).
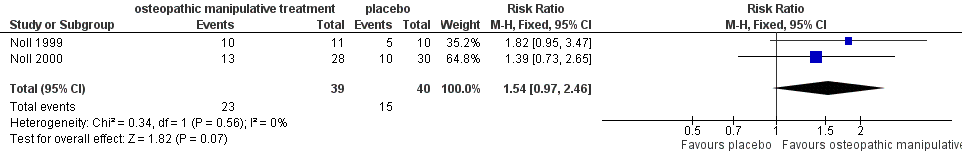
Forest plot of comparison: 3 OMT plus routine treatment versus placebo plus routine treatment, outcome: 3.2 Cure rate.
3.2 Secondary outcomes
3.2.1 Duration of hospital stay
Osteopathic manipulative treatment, compared with placebo, significantly reduced the mean duration of hospital stay by 2.0 days (weighted mean difference (WMD) ‐2.0, 95% CI ‐3.46 to ‐0.58).
3.2.2 Duration of fever
Only one trial (Noll 1999) with 21 participants assessed this outcome, which suggested that osteopathic manipulative treatment could not decrease the duration of fever in comparison with placebo (MD 0.6 day, 95% CI ‐1.60 to 2.80).
3.2.3 Rate of improvement of chest X‐ray
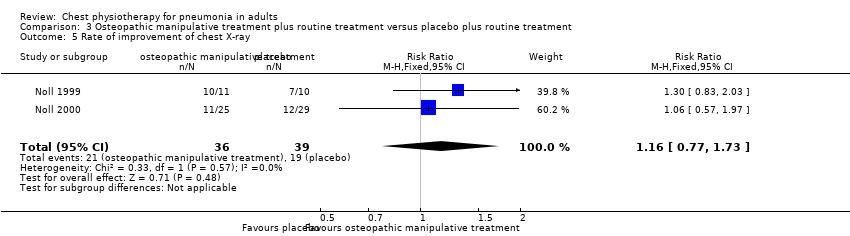
Two trials (Noll 1999; Noll 2000) appraised this outcome. Pooled data showed that osteopathic manipulative treatment, compared with placebo, had no benefit on improvement of chest X‐ray (RR 1.16, 95% CI 0.77 to 1.73).
3.2.4 Duration of antibiotic therapy
Compared with placebo, osteopathic manipulative treatment decreased the mean duration of antibiotic therapy by 1.9 days (MD ‐1.9, 95% CI ‐3.12 to ‐0.74). In addition, the subgroup analysis found that osteopathic manipulative treatment could decrease the mean duration of intravenous antibiotic therapy by 2.1 days (MD ‐2.1, 95% CI ‐3.36 to ‐0.87), but it had no benefit for decreasing the mean duration of oral antibiotic therapy (MD 0.9 day, 95% CI ‐1.25 to 3.20).
3.2.5 Duration of leukocytosis
Only one trial (Noll 1999) with 21 participants assessed this outcome, and found that osteopathic manipulative treatment did not decrease the mean duration of leukocytosis in comparison with placebo (MD ‐0.90 day, 95% CI ‐7.02 to 5.22).
3.2.6 Change in leukocyte count
One trial (Noll 2000) with 58 participants assessed the change in leukocytosis count. There was a significant difference in leukocyte count changes between days one and three (MD 3599.8, 95% CI 1121.22 to 6078.38). However, by day five these differences were no longer statistically significant (MD 2271.5, 95% CI ‐1287.07 to 5830.07).
3.2.7 Mean leukocyte count
One trial (Noll 2000) also assessed the mean leukocyte count on day three and five after admission, and it identified no significant differences between groups for mean white blood cell count on days three and five (day three: MD 1383, 95% CI ‐1072 to 3838; day five: MD 1210, 95% CI ‐1052 to 3472, respectively).
3.2.8 Adverse effects
Only one trial (Noll 2000) reported adverse effects, as transient muscle tenderness emerged after treatment in two individuals during the period of study.
4. Positive expiratory pressure plus routine treatment versus routine treatment alone
One trial (Bjorkqvist 1997) including 98 participants, with 50 in the treatment group and 48 in the control group, focused on this technique.
4.1 Primary outcomes
4. 1.1 Mortality
No participants died during the period of study.
4.1.2 Cure rate
Not reported.
4.2 Secondary outcomes
4.2.1 Duration of hospital stay
Compared with the routine treatment alone, positive expiratory pressure plus routine treatment reduced the mean duration of hospital stay by 1.4 days and there was a significant difference between groups (MD ‐1.4, 95% CI ‐2.77 to ‐0.03).
4.2.2 Duration of fever
Positive expiratory pressure could reduce the mean duration of fever by 0.7 day with a significant difference between groups (MD ‐0.7, 95% CI ‐1.36 to ‐0.04).
4.2.3 Adverse effects
No side effects were found during the study period.
Discussion
Summary of main results
Six randomised controlled trials (RCTs) with 434 participants were included in this review, which appraised four types of chest physiotherapies (i.e. conventional chest physiotherapy, active cycle of breathing techniques, osteopathic manipulative treatment and positive expiratory pressure). None of the techniques were found to improve mortality of pneumonia in adults. Conventional chest physiotherapy, active cycle of breathing techniques and osteopathic manipulative treatment did not increase the cure rate of pneumonia nor the rate of chest X‐ray improvement. Osteopathic manipulative treatment and positive expiratory pressure did reduce the mean duration of hospital stay by 2.02 and 1.4 days, respectively, whereas conventional chest physiotherapy and active cycle of breathing techniques did not. Positive expiratory pressure might reduce the duration of fever, while osteopathic manipulative treatment might not. In addition, osteopathic manipulative treatment might have an effect on reducing the duration of intravenous and total antibiotic treatments.
Overall completeness and applicability of evidence
Most of the included RCTs were conducted around 10 to 30 years ago. The main positive conclusions (a decrease in duration of hospital stay, fever and antibiotic treatment) were based on two trials with small sample sizes, conducted more than 10 years ago. There have been advances in chest physiotherapies which have not yet been appraised in randomised controlled trials. The authors of Noll 2008 are conducting a RCT which evaluates the effect of osteopathic manipulative treatment for elderly patients with pneumonia. The results are supposed to offer valuable information for this special population. Moreover, to a large extent, the effects of physiotherapy depend upon the skills of the practitioners. It has been reported that the duration, sessions and quality of chest physiotherapies vary from case to case (Guessous 2008). Misleading results may occur if the treatments are administered by unskilled practitioners. However, information on the experience and training of the physiotherapists who implemented the treatments was not available in most of the included trials. The techniques, the number and duration of sessions and the duration of the intervention period also varied across trials. We therefore recommend that caution is required when interpreting the results of this review and applying them to current practice.
Quality of the evidence
All included studies were of poor to moderate methodological quality. Firstly, although all studies stated that randomisation was used, none mentioned the method of randomisation. Secondly, only two of the six studies (Noll 1999; Noll 2000) were double‐blinded trials (in which participants and outcome assessors were blinded), and one (Britton 1985) was a single‐blinded trial. Lack of blinding might cause overestimation of the effects. It should be noted that chest physiotherapy was performed by a physiotherapist, so it might be difficult to blind the practitioners. Thirdly, four of the six studies (Bjorkqvist 1997; Britton 1985; Graham 1978; Tydeman 1989) had more than 10% drop‐outs, but none used an intention‐to‐treat (ITT) analysis, which aims to maintain the unbiased group comparison afforded by randomisation and to resolve the problem of non‐compliance. Absence of an ITT analysis might lead to potential biases. Finally, the sample sizes of the six trials were too small to permit adequate assessment of this intervention. Moreover, there were challenges in obtaining high‐quality evidence for physiotherapy interventions because of the difficulties in blinding the intervention, standardising the method of chest physiotherapy and defining clinically meaningful outcomes.
Potential biases in the review process
Six published studies appeared to meet the inclusion criteria but have not yet been included or excluded. Five papers are published in Russian and one was published in 1947 and we have not yet managed to retrieve a copy of the trial. This is the major limitation in our review and may lead to selective reporting bias. It was impossible to perform a funnel plot analysis to assess potential publication bias because of the limited number of trials for each outcome. Another limitation of our review is that none of the included studies were recent publications; most trials reported on participants treated in the 1980s and 1990s. Moreover, the publication date of the included studies varied from 1978 to 2000, which leads us to consider that definitions of care and cure in the different studies, plus medical management (including the methods of chest physiotherapy) may have differed. For these reasons, clinical heterogeneity was inevitable, although we had performed subgroup analyses on different types of chest physiotherapies and outcomes to minimise the effect of heterogeneity. Clinical heterogeneity might lead to bias if we combined the results of different studies by meta‐analysis.
Agreements and disagreements with other studies or reviews
Although chest physiotherapy has been widely used in pneumonia, there is little evidence of any benefit (Guessous 2008). To our knowledge, this is the first systematic review to examine chest physiotherapy for pneumonia in adults. According to our results, chest physiotherapy has no benefit for mortality and cure rate. It can be costly as it requires equipment and experienced respiratory therapists, physiotherapists or clinicians to perform (Guessous 2008). Therefore, we recommend caution when prescribing chest physiotherapy for pneumonia in adults.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
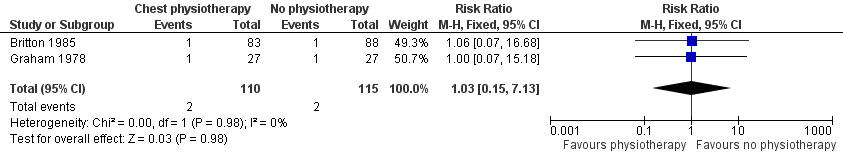
Forest plot of comparison: 1 Chest physiotherapy plus routine treatment versus routine treatment alone, outcome: 1.1 Mortality.

Forest plot of comparison: 1 Chest physiotherapy plus routine treatment versus routine treatment alone, outcome: 1.2 Cure rate.

Forest plot of comparison: 3 OMT plus routine treatment versus placebo plus routine treatment, outcome: 3.1 Mortality.
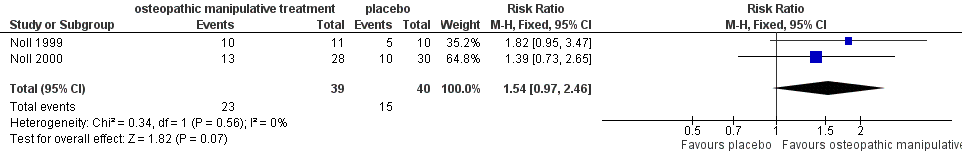
Forest plot of comparison: 3 OMT plus routine treatment versus placebo plus routine treatment, outcome: 3.2 Cure rate.

Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 1 Mortality.

Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 2 Cure rate.
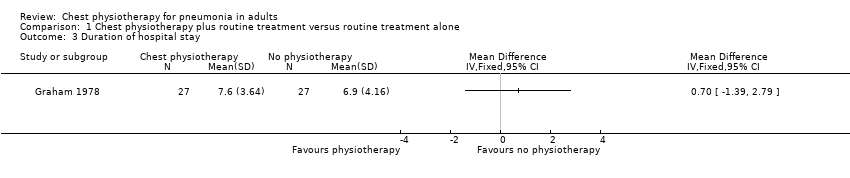
Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 3 Duration of hospital stay.

Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 4 Duration of fever.

Comparison 1 Chest physiotherapy plus routine treatment versus routine treatment alone, Outcome 5 Rate of improvement of chest X‐ray.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 1 Cure rate.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 2 Duration of hospital stay.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 3 Rate of improvement of chest X‐ray.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 4 Duration of antibiotic therapy.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 5 Duration of sputum production.

Comparison 2 Active cycle of breathing techniques plus routine treatment versus routine treatment alone, Outcome 6 In‐patient sputum weight.
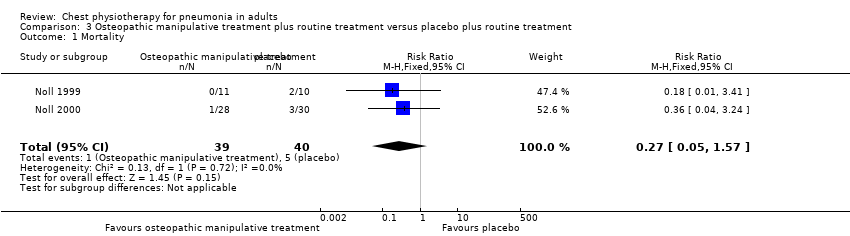
Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 1 Mortality.
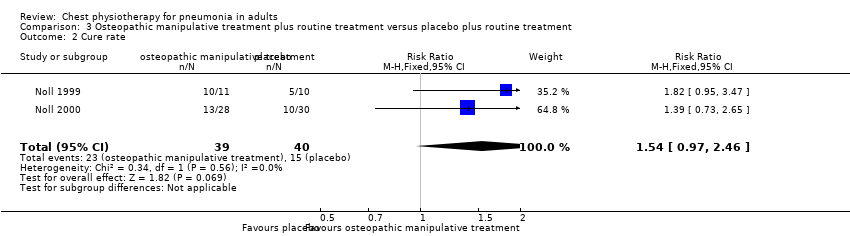
Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 2 Cure rate.
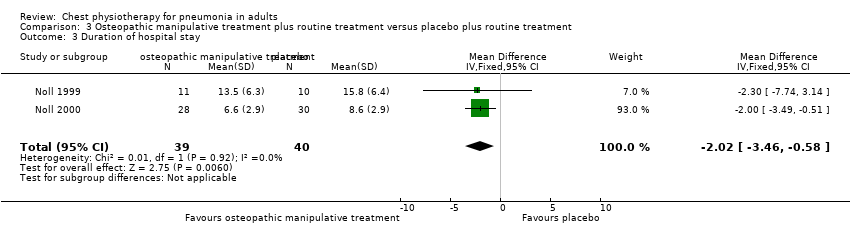
Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 3 Duration of hospital stay.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 4 Duration of fever.
Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 5 Rate of improvement of chest X‐ray.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 6 Duration of oral antibiotic therapy.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 7 Duration of intervenous therapy.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 8 Duration of total antibiotic therapy.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 9 Duration of leukocytosis.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 10 Change in leukocyte count.

Comparison 3 Osteopathic manipulative treatment plus routine treatment versus placebo plus routine treatment, Outcome 11 Mean leukocyte count.

Comparison 4 Positive expiratory pressure plus routine treatment versus routine treatment alone, Outcome 1 Duration of hospital stay.
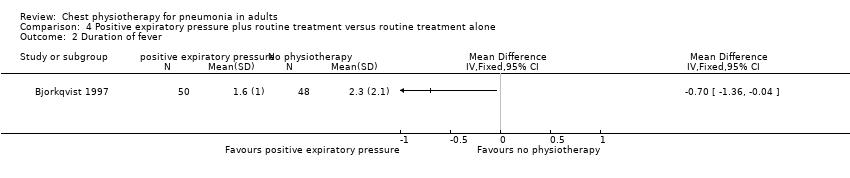
Comparison 4 Positive expiratory pressure plus routine treatment versus routine treatment alone, Outcome 2 Duration of fever.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.15, 7.13] |
| 2 Cure rate Show forest plot | 2 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.91, 1.04] |
| 3 Duration of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Duration of fever Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Rate of improvement of chest X‐ray Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cure rate Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Duration of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Rate of improvement of chest X‐ray Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Duration of antibiotic therapy Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Duration of sputum production Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 In‐patient | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Out‐patient | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Total | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 In‐patient sputum weight Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 2 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.05, 1.57] |
| 2 Cure rate Show forest plot | 2 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.97, 2.46] |
| 3 Duration of hospital stay Show forest plot | 2 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐2.02 [‐3.46, ‐0.58] |
| 4 Duration of fever Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 Rate of improvement of chest X‐ray Show forest plot | 2 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.77, 1.73] |
| 6 Duration of oral antibiotic therapy Show forest plot | 2 | 79 | Mean Difference (IV, Random, 95% CI) | 0.97 [‐1.25, 3.20] |
| 7 Duration of intervenous therapy Show forest plot | 2 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐2.11 [‐3.36, ‐0.87] |
| 8 Duration of total antibiotic therapy Show forest plot | 2 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐1.93 [‐3.12, ‐0.74] |
| 9 Duration of leukocytosis Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10 Change in leukocyte count Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Change between Day 3 and 1 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Change between Day 5 and 1 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Mean leukocyte count Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 Day 3 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Day 5 from admission | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Duration of hospital stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Duration of fever Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |

