Sub‐Tenon anestezija ili anestezija kapima (topikalna) za operaciju katarakte
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomized controlled trial | |
| Participants | 303 participants undergoing their first cataract surgery by phacoemulsification | |
| Interventions | Treatment group: topical anaesthesia with oxybuprocaine 0.4% drops (n = 100) Control group: sub‐Tenon's anaesthesia with lidocaine 2% with 1 in 200,000 epinephrine plus bupivacaine 0.75% (n = 105) Phacoemulsification was performed by the same surgeon throughout Study includes a third group with peribulbar anaesthesia | |
| Outcomes | Pain during anaesthetic administration and pain during surgery | |
| Notes | We did not retain the results of this study for analysis because data are provided only as a sum of subjective scores (0 to 5) plus VAS scores (0 to 10) for anaesthesia and surgery. This study was published in abstract form only, and study authors provided no contact information | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized"; no details |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not mentioned |
| Blinding of outcome assessment (detection bias) | Low risk | "Patients scored the severity of the components of their pain by verbal responses to the SF‐MPQ, administered by a masked investigator" |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up mentioned |
| Selective reporting (reporting bias) | Low risk | No cross‐over mentioned |
| Other bias | Unclear risk | Not enough details; published in abstract form only |
| Methods | Randomized controlled trial | |
| Participants | Inclusion criterion: patient listed for cataract surgery | |
| Interventions | Treatment group: Topical anaesthesia was provided by 0.4% oxybuprocaine hydrochloride (Benoxinate), instilled onto the cornea and the conjunctiva (n = 16) A superior rectus fixation suture was used in the sub‐Tenon’s group but not in the topical group. The operative technique for both groups was otherwise identical and was performed by 1 surgeon | |
| Outcomes | Pain felt intraoperatively (median VAS scores taken as P value) | |
| Notes | No pre‐medication was used, and no sedation or other analgesia was required during surgery Complications were not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "allocated randomly"; no details |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Pain assessor blinded to participant group: not stated |
| Incomplete outcome data (attrition bias) | Low risk | No participants excluded |
| Selective reporting (reporting bias) | Low risk | No cross‐over mentioned |
| Other bias | Unclear risk | Characteristics of participants not provided |
| Methods | Randomized controlled trial | |
| Participants | 119 patients undergoing elective clear corneal phacoemulsification Inclusion criterion: patient listed for cataract surgery Mean age (years) in topical anaesthesia: 76.4, sub‐Tenon's: 75.9. Age range (years) in topical anaesthesia was 46 to 93 years, in sub‐Tenon's, range was 54 to 92 years | |
| Interventions | Treatment group:: proparacaine 0.5% (n = 46) | |
| Outcomes | Pain felt on administration of anaesthesia | |
| Notes | Complications not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Method not stated. Three groups with unequal numbers. Diffferent surgeon for each group |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) | High risk | Participants were randomly assigned to 1 of the sub‐Tenon’s anaesthesia groups and were informed about which type of local anaesthesia they were to receive |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) | Low risk | "Two patients were excluded from the study for incomplete data entry" |
| Selective reporting (reporting bias) | High risk | Not in intention‐to‐treat: "Two patients were excluded from the study for incomplete data entry" |
| Other bias | Low risk | Groups well balanced |
| Methods | Randomized double‐blind controlled trial | |
| Participants | 28 participants with single eye surgery; patients listed for cataract surgery in a single unit, first eye operation | |
| Interventions | Treatment group: topical anaesthesia with 2 drops of proxymetacaine 0.5% followed by 4 drops of amethocaine 1% (tetracaine). Intracameral local anaesthesia was not used (n = 14) | |
| Outcomes | Participant satisfaction with anaesthesia care (ISAS) (total score from ‐3 to + 3). Some items had nothing to do with the anaesthetic technique used or with the surgery itself (too hot or too cold) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated permuted block randomization was obtained from the Department of Biostatistics via telephone |
| Allocation concealment (selection bias) | Low risk | "obtained from the Department of Biostatistics via telephone" |
| Blinding of participants and personnel (performance bias) | Low risk | Participants and surgeons were formally masked regarding the method of anaesthesia, but no sham injections were given in the topical anaesthesia group. All local anaesthesia was administered by anaesthetists or surgeons who were not otherwise involved in the care of that participant nor with analysis of satisfaction scores |
| Blinding of outcome assessment (detection bias) | Low risk | Participants and surgeons were formally masked regarding the method of anaesthesia, but no sham injections were given in the topical anaesthesia group. All local anaesthesia was administered by anaesthetists or surgeons who were not otherwise involved in the care of that participant nor with analysis of satisfaction scores |
| Incomplete outcome data (attrition bias) | High risk | Dropout criteria included the following: participant voices wanting to drop out of the study, participant expresses uncontrolled pain and participant becomes restless. It was decided that participants who drop out should receive a top‐up, or an injection of local anaesthetic block and midazolam sedation, Two of the 28 questionnaires contained unanswered questions ‐ both in the topical anaesthesia group |
| Selective reporting (reporting bias) | High risk | One participant dropped out after randomization (topical anaesthesia). Ten minutes into the operation, the participant expressed severe pain and was moving too much for the surgeon to continue operating. The participant was given 1 mg midazolam and a peribulbar block so surgery could be completed Not intention‐to‐treat |
| Other bias | Low risk | Groups well balanced: "Both groups were comparable regarding age, sex, waiting time, ASA status, access to hospital transport" |
| Methods | Randomized controlled trial | |
| Participants | 100 participants listed for cataract surgery on single eye | |
| Interventions | Treatment group: Topical anaesthesia with oxybuprocaine 0.4% 1 drop, xylocaine 2% jelly, 2 applications over 7 to 10 minutes, lignocaine 1% 1 drop on bare sclera, lignocaine 1% 0.5 mL intracamerally (n = 50) All surgeries performed by the same surgeon | |
| Outcomes | Pain felt intraoperatively (this score included the anaesthetic technique), measured on a 10‐point VAS scale | |
| Notes | No intraoperative complications occurred in any of the study groups. One case of postoperative iritis (cells and flare in the anterior chamber) was encountered in each group postoperatively. Both cases resolved with intensified topical steroids without sequelae | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly assigned"; no details |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) | High risk | Surgeon not blinded; unclear for participants |
| Blinding of outcome assessment (detection bias) | Low risk | Independent investigator |
| Incomplete outcome data (attrition bias) | Low risk | No lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Intention‐to‐treat for pain scores |
| Other bias | Low risk | Groups well balanced |
| Methods | Randomized controlled trial Approved by the ethics committee; written informed consent obtained | |
| Participants | 210 participants listed for cataract surgery on a single eye by a single surgeon | |
| Interventions | Treatment group: topical anaesthesia with proxymetacaine 0.5% 4+2 drops; 5 minutes apart (n = 70) | |
| Outcomes | Pain during anaesthesia Pain felt intraoperatively (VAS score 0 to 10) | |
| Notes | Surgeon blinded to participant group: yes Pain assessor blinded to participant group: yes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "An independent researcher provided the hospital pharmacy with an individual randomization schedule of 250 allocations" |
| Allocation concealment (selection bias) | Low risk | "The randomization schedule was retained in the hospital pharmacy and was not seen by the investigators until the trial was completed" |
| Blinding of participants and personnel (performance bias) | Low risk | "A customized pack was prepared from this schedule for each patient. The pack comprised a syringe containing either 3 mL of local anaesthetic lidocaine 2% (2 mL) and bupivacaine 0.75% (1 mL) or placebo, a minims dropper containing either placebo or proxymethocaine 0.5%, and a separate minims dropper containing proxymethocaine 0.5%. These packs were sequentially labelled 1 to 210. All patients received a sub‐Tenon’s injection and topical eyedrops. In this way the patients, the ophthalmologist administering the anaesthetic, the surgeon and the nurse measuring the pain score were fully masked from the identity of the contents of the pack" |
| Blinding of outcome assessment (detection bias) | Low risk | "A customized pack was prepared from this schedule for each patient. The pack comprised a syringe containing either 3 mL of local anaesthetic lidocaine 2% (2 mL) and bupivacaine 0.75% (1 mL) or placebo, a minims dropper containing either placebo or proxymethocaine 0.5%, and a separate minims dropper containing proxymethocaine 0.5%. These packs were sequentially labelled 1 to 210. All patients received a sub‐Tenon’s injection and topical eyedrops. In this way the patients, the ophthalmologist administering the anaesthetic, the surgeon and the nurse measuring the pain score were fully masked from the identity of the contents of the pack" |
| Incomplete outcome data (attrition bias) | Low risk | Nine participants (5 in sub‐Tenon’s group and 5 in topical anaesthesia group) were excluded from the analysis, as their pain scores were not recorded |
| Selective reporting (reporting bias) | Low risk | No cross‐over |
| Other bias | Low risk | Groups well balanced |
| Methods | Randomized cross‐over trial | |
| Participants | 25 participants with both eyes operated on within 24 hours | |
| Interventions | Treatment group: topical anaesthesia with tetracaine 1% 1+1+1 drop; 10 minutes apart (n = 25) | |
| Outcomes | Pain felt intraoperatively (5‐point scale) | |
| Notes | 64% of participants preferred sub‐Tenon's anaesthesia, 8% preferred topical anaesthesia and the rest expressed no preference | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Technique for first eye chosen at random; method unspecified |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not mentioned |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No cross‐over |
| Other bias | Low risk | Same participants |
| Methods | Randomized cross‐over trial | |
| Participants | 100 participants with surgery on both eyes 1 to 2 months apart; listed for bilateral cataract surgery | |
| Interventions | Treatment group: topical anaesthesia with diclofenac 0.1% 2+2 drops 20 minutes apart, phenylephrine 5% 2+2+2 drops 5 minutes apart, tropicamide 0.5% 2+2+2 drops 5 minutes apart, proparacaine hydrochloride 0.5% 2+2+2+2 drops 3 minutes apart (n = 100) | |
| Outcomes | Pain felt on administration of anaesthesia (VAS score 0 to 10) Pain assessed: immediately (30 minutes) after surgery (VAS score 0 to 10) Patient co‐operation measured on a 10‐point scale (10 excellent to 0 extremely poor) | |
| Notes | Pain was assessed at 24 hours postoperatively | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Technique for the first eye chosen at random; no details on the method used |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not mentioned |
| Blinding of outcome assessment (detection bias) | Low risk | "After surgery, patients were taken to the post‐operative area, where they were asked to complete a |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | No cross‐over |
| Other bias | Low risk | Same participants |
Abbreviations:
ASA: American Society of Anesthesiologists
D: Diopter.
ISAS: Iowa Satisfaction with Anaesthesia Scale (‐3 totally dissatisfied, +3 totally satisfied).
mL: millilitres.
SF‐MPQ: Short Form McGill Pain Questionnaire.
VAS: visual analogue pain scale (0 = no pain, 10 = worst pain ever).
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Different population. Study was performed on participants with potentially difficult cataract surgery | |
| No outcomes of interest | |
| All participants were given standard intravenous (IV) pre‐medication with midazolam (0.02 mg/kg) and alfentanil (0.005 mg/kg) | |
| Study included 3 groups of participants; all were operated on under monitored anaesthesia care with lidocaine‐propofol‐remifentanil mixture |
Abbreviations:
IV: intravenous.
RCT: randomized controlled trial.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Topical Jelly and Intracameral Anesthesia Versus Sub‐Tenon's Anesthesia, in Cataract Surgery |
| Methods | Randomized, double‐blind (participant, investigator, outcomes assessor) |
| Participants | Inclusion criteria: Bilateral cataract, 18 years and older Exclusion criteria: Refusal to participate, high surgical risk (ASA 4 or 5), allergy to lidocaine or other amide local anaesthetics, inability to understand informed consent, coagulation abnormalities, prior ophthalmologic surgery, small pupil, Fuchs dystrophy, lens luxation, uveitis |
| Interventions | Treatment group: topical jelly and intracameral anaesthesia Control group: sub‐Tenon's anaesthesia |
| Outcomes | Primary outcome measures: number of participants who prefer topical anaesthesia measured at 1 month Secondary outcome measures: intraoperative pain measured at 1 hour |
| Starting date | April 2011 |
| Contact information | Contact: Tomás‐Ortiz Basso ([email protected]), MD, and Contact: Diego Giunta, MD ([email protected]) |
| Notes |
Abbreviations:
ASA: American Society of Anesthesiologists.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during surgery Show forest plot | 6 | 705 | Std. Mean Difference (Random, 95% CI) | 0.64 [0.43, 0.84] |
| Analysis 1.1  Comparison 1 Topical anaesthesia versus sub‐Tenon's anaesthesia, Outcome 1 Pain during surgery. | ||||
| 1.1 Low risk for outcome assessor blindness | 3 | 501 | Std. Mean Difference (Random, 95% CI) | 0.47 [0.29, 0.66] |
| 1.2 Unclear risk for outcome assessor blindness | 3 | 204 | Std. Mean Difference (Random, 95% CI) | 0.90 [0.61, 1.20] |
| 2 Pain during anaesthesia administration Show forest plot | 3 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Topical anaesthesia versus sub‐Tenon's anaesthesia, Outcome 2 Pain during anaesthesia administration. | ||||
| 2.1 Cross‐over trial | 1 | 200 | Std. Mean Difference (Random, 95% CI) | ‐2.21 [‐2.57, ‐1.86] |
| 2.2 Parallel trial | 2 | 320 | Std. Mean Difference (Random, 95% CI) | ‐0.20 [‐0.43, 0.04] |
| 3 Pain at 30 minutes after surgery Show forest plot | 2 | Std. Mean Difference (Fixed, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Topical anaesthesia versus sub‐Tenon's anaesthesia, Outcome 3 Pain at 30 minutes after surgery. | ||||
| 3.1 Cross‐over trial | 1 | 200 | Std. Mean Difference (Fixed, 95% CI) | 0.96 [0.67, 1.26] |
| 3.2 Parallel trial | 1 | 201 | Std. Mean Difference (Fixed, 95% CI) | 0.54 [0.24, 0.84] |

Flow diagram of study selection for the updated review.
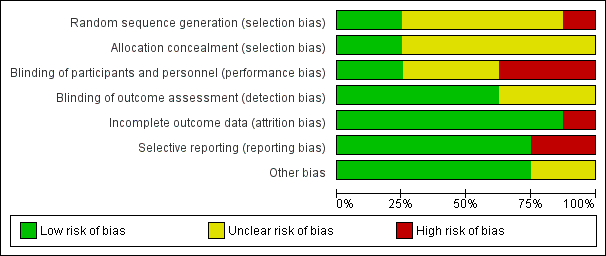
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Topical anaesthesia versus sub‐Tenon's anaesthesia, Outcome 1 Pain during surgery.
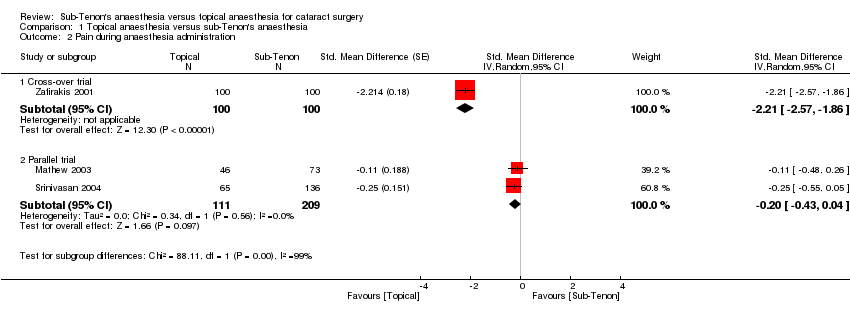
Comparison 1 Topical anaesthesia versus sub‐Tenon's anaesthesia, Outcome 2 Pain during anaesthesia administration.

Comparison 1 Topical anaesthesia versus sub‐Tenon's anaesthesia, Outcome 3 Pain at 30 minutes after surgery.
| Topical anaesthesia compared with sub‐Tenon's anaesthesia for cataract surgery | ||||||
| Patient or population: patients with cataract surgery | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Sub‐Tenon's anaesthesia | Topical anaesthesia | |||||
| Intraoperative pain | Mean intraoperative pain in the intervention groups was | 501 | ⊕⊕⊕⊕ | Equivalent to 1.1 on a score from 0 to 10 | ||
| Pain during administration of anaesthesia | Mean pain during administration of anaesthesia in the intervention groups was | 184 | ⊕⊕⊝⊝ | |||
| Pain at 24 hours | Mean pain at 24 hours in the intervention groups was | 200 | ⊕⊕⊕⊝ | Equivalent to 0.2 on a score from 0 to 10 | ||
| Surgeon's satisfaction | Mean surgeon satisfaction in the intervention groups was | 200 | ⊕⊕⊝⊝ | |||
| Participant satisfaction | Mean participant satisfaction in the intervention groups was | 26 | ⊕⊕⊕⊝ | |||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aWe retained only studies in which the outcome assessor was blinded to the anaesthetic technique. | ||||||
| Study ID | Subconjunctival haemorrhage T vs ST | Chemosis T vs ST | Transient increase in intraocular pressure T vs ST | Posterior capsular tear T vs ST | Iris prolapsus T vs ST | Conversion to ST | Iritis T vs ST | Comments |
| 0 | Complications not reported | |||||||
| 0 | Complications not reported | |||||||
| 1/14 | Complications not reported | |||||||
| 0/50 vs 0/50 | 0/50 vs 0/50 | 5/50 | 1/50 vs 1/50 | The topical anaesthesia group felt pain during cauterization of the episcleral vessels | ||||
| 3/65 vs 2/136 | 0/65 vs 1/136 | 0 | No participant required supplemental analgesia after surgery | |||||
| 25/25 vs 25/25a | 0/25 vs 15/25 | 0/25 vs 0/25 | 0/25 vs 0/25 | 0 | ||||
| 0/100 vs 22/100 | 0/100 vs 76/100 | 0 | ||||||
| T: topical anaesthesia ST: sub‐Tenon's anaesthesia vs: versus aAny amount | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during surgery Show forest plot | 6 | 705 | Std. Mean Difference (Random, 95% CI) | 0.64 [0.43, 0.84] |
| 1.1 Low risk for outcome assessor blindness | 3 | 501 | Std. Mean Difference (Random, 95% CI) | 0.47 [0.29, 0.66] |
| 1.2 Unclear risk for outcome assessor blindness | 3 | 204 | Std. Mean Difference (Random, 95% CI) | 0.90 [0.61, 1.20] |
| 2 Pain during anaesthesia administration Show forest plot | 3 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 2.1 Cross‐over trial | 1 | 200 | Std. Mean Difference (Random, 95% CI) | ‐2.21 [‐2.57, ‐1.86] |
| 2.2 Parallel trial | 2 | 320 | Std. Mean Difference (Random, 95% CI) | ‐0.20 [‐0.43, 0.04] |
| 3 Pain at 30 minutes after surgery Show forest plot | 2 | Std. Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 3.1 Cross‐over trial | 1 | 200 | Std. Mean Difference (Fixed, 95% CI) | 0.96 [0.67, 1.26] |
| 3.2 Parallel trial | 1 | 201 | Std. Mean Difference (Fixed, 95% CI) | 0.54 [0.24, 0.84] |

