백내장수술시 테논낭밑마취(sub‐Tenon‘s anesthesia)와 점안마취(topical anesthesia) 비교
Información
- DOI:
- https://doi.org/10.1002/14651858.CD006291.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 27 agosto 2015see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Anestesia
- Copyright:
-
- Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Updated review:
Joanne Guay (JG), Karl Sales (KS).
Co‐ordinating the review: JG.
Undertaking manual searches: JG.
Screening search results: JG, KS.
Organizing retrieval of papers: JG.
Screening retrieved papers against inclusion criteria: JG, KS.
Appraising quality of papers: JG, KS.
Abstracting data from papers: JG, KS.
Managing data for the review: JG.
Entering data into Review Manager: JG.
Analysing RevMan statistical data: JG.
Performing other statistical analyses not using RevMan: JG.
Interpreting data: JG, KS.
Making statistical inferences: JG.
Writing the review: JG, KS.
Securing funding for the review: departmental resources only.
Serving as guarantor for the review (one review author): JG.
Taking responsibility for reading and checking the review before submission: JG, KS.
Designing the literature search: Karen Hovhannisyan (KH).
Sources of support
Internal sources
-
University of Sherbrooke, Canada.
Access to medical journals
-
University of Quebec in Abitibi‐Temiscamingue, Canada.
Access to medical journals
External sources
-
Cochrane Anaesthesia Review Group, Denmark.
Search strategy and list of abstracts
Declarations of interest
Joanne Guay: I have had no direct relationship with any pharmaceutical company or equipment manufacturer in the past five years. I have not acted as a witness expert in the past five years. I am not an author of any of the included or excluded studies. I do not hold stock other than mutual funds. During the past five years, I have received fees as speaker for two lectures given at the University of Dalhousie: one on regional anaesthesia for carotid endarterectomy, and the other on local anaesthetic‐related methaemoglobinaemia. My fees were paid by the University of Dalhousie. I am the editor of a multi‐author textbook on anaesthesia (including notions on general and regional anaesthesia). I receive fees for a course on airway management from University of Quebec in Abitibi‐Temiscamingue.
Karl Sales: I have had no direct relationship with any pharmaceutical company or equipment manufacturer in the past five years. I have not acted as a witness expert in the past five years. I am not an author of any of the included or excluded studies.
Acknowledgements
The first version of this review was prepared by Marc Davison, Sara Padroni, Catey Bunce and Heinrich Rüschen (Davison 2007). We would like to thank Karen Hovhannisyan for preparing the search strategy for the original review and the updated review, and for providing abstracts for this update. Relevant references for this update were provided by University of Sherbrooke and University of Quebec in Abitibi‐Temiscamingue.
We would also like to thank Cochrane Anaesthesia, Critical and Emergency Care editors ‐ Nathan Pace, Andrew Smith and Janet Wale ‐ for providing help with this updated review.
Version history
| Published | Title | Stage | Authors | Version |
| 2015 Aug 27 | Sub‐Tenon's anaesthesia versus topical anaesthesia for cataract surgery | Review | Joanne Guay, Karl Sales | |
| 2007 Jul 18 | Sub‐Tenon's anaesthesia versus topical anaesthesia for cataract surgery | Review | Marc Davison, Sara Padroni, Catey Bunce, Heinrich Rüschen | |
| 2006 Oct 18 | Sub‐Tenon's anaesthesia versus topical anaesthesia for cataract surgery | Protocol | Marc Davison, Sara Padroni, Catey Bunce, Heinrich Rüschen | |
Notes
Updated review February 2015
Despite using the same studies, we have had to change the conclusions from those of the original review (Davison 2007) on the basis of the following.
-
We were able to pool the data of more studies (different techniques of data extraction). As a result of this, the new analysis shows that the higher level of pain with topic anaesthesia was overestimated by the inclusion of studies in which outcome assessors were not blinded to the anaesthetic technique used.
-
The original review stated that surgeons had a small preference for the sub‐Tenon's technique. Possibly because they are now more familiar with topical anaesthesia, surgeons in various countries are telling us by their numbers that they are using almost exclusively topic anaesthesia, or at least in the majority of their patients. We can no longer say that they prefer sub‐Tenon's anaesthesia despite the results of RCTs performed years ago; this seems no longer true.
-
The original review stated that topical anaesthesia was associated with a higher rate of intraoperative complications. We have calculated that the number of participants included in our review was insufficient to allow us to present conclusions on this.
Therefore, with the new analysis and integration of actual literature on the topic (up to 2014), we have had to change the conclusions, despite the fact that we did not add new studies to the analysis.
The original review (Davison 2007) was edited by Andrew Smith, Marialena Trivella, Anders Behndig and Maurizio Solca.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Aged; Aged, 80 and over; Female; Humans; Male;
PICO

Flow diagram of study selection for the updated review.
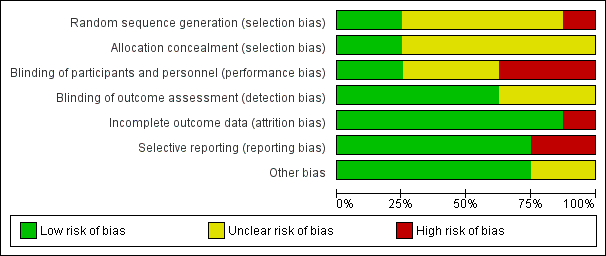
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Topical anaesthesia versus sub‐Tenon's anaesthesia, Outcome 1 Pain during surgery.
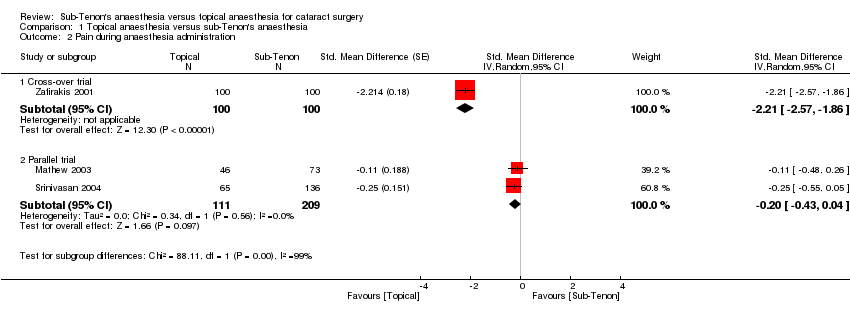
Comparison 1 Topical anaesthesia versus sub‐Tenon's anaesthesia, Outcome 2 Pain during anaesthesia administration.

Comparison 1 Topical anaesthesia versus sub‐Tenon's anaesthesia, Outcome 3 Pain at 30 minutes after surgery.
| Topical anaesthesia compared with sub‐Tenon's anaesthesia for cataract surgery | ||||||
| Patient or population: patients with cataract surgery | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Sub‐Tenon's anaesthesia | Topical anaesthesia | |||||
| Intraoperative pain | Mean intraoperative pain in the intervention groups was | 501 | ⊕⊕⊕⊕ | Equivalent to 1.1 on a score from 0 to 10 | ||
| Pain during administration of anaesthesia | Mean pain during administration of anaesthesia in the intervention groups was | 184 | ⊕⊕⊝⊝ | |||
| Pain at 24 hours | Mean pain at 24 hours in the intervention groups was | 200 | ⊕⊕⊕⊝ | Equivalent to 0.2 on a score from 0 to 10 | ||
| Surgeon's satisfaction | Mean surgeon satisfaction in the intervention groups was | 200 | ⊕⊕⊝⊝ | |||
| Participant satisfaction | Mean participant satisfaction in the intervention groups was | 26 | ⊕⊕⊕⊝ | |||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aWe retained only studies in which the outcome assessor was blinded to the anaesthetic technique. | ||||||
| Study ID | Subconjunctival haemorrhage T vs ST | Chemosis T vs ST | Transient increase in intraocular pressure T vs ST | Posterior capsular tear T vs ST | Iris prolapsus T vs ST | Conversion to ST | Iritis T vs ST | Comments |
| 0 | Complications not reported | |||||||
| 0 | Complications not reported | |||||||
| 1/14 | Complications not reported | |||||||
| 0/50 vs 0/50 | 0/50 vs 0/50 | 5/50 | 1/50 vs 1/50 | The topical anaesthesia group felt pain during cauterization of the episcleral vessels | ||||
| 3/65 vs 2/136 | 0/65 vs 1/136 | 0 | No participant required supplemental analgesia after surgery | |||||
| 25/25 vs 25/25a | 0/25 vs 15/25 | 0/25 vs 0/25 | 0/25 vs 0/25 | 0 | ||||
| 0/100 vs 22/100 | 0/100 vs 76/100 | 0 | ||||||
| T: topical anaesthesia ST: sub‐Tenon's anaesthesia vs: versus aAny amount | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during surgery Show forest plot | 6 | 705 | Std. Mean Difference (Random, 95% CI) | 0.64 [0.43, 0.84] |
| 1.1 Low risk for outcome assessor blindness | 3 | 501 | Std. Mean Difference (Random, 95% CI) | 0.47 [0.29, 0.66] |
| 1.2 Unclear risk for outcome assessor blindness | 3 | 204 | Std. Mean Difference (Random, 95% CI) | 0.90 [0.61, 1.20] |
| 2 Pain during anaesthesia administration Show forest plot | 3 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 2.1 Cross‐over trial | 1 | 200 | Std. Mean Difference (Random, 95% CI) | ‐2.21 [‐2.57, ‐1.86] |
| 2.2 Parallel trial | 2 | 320 | Std. Mean Difference (Random, 95% CI) | ‐0.20 [‐0.43, 0.04] |
| 3 Pain at 30 minutes after surgery Show forest plot | 2 | Std. Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 3.1 Cross‐over trial | 1 | 200 | Std. Mean Difference (Fixed, 95% CI) | 0.96 [0.67, 1.26] |
| 3.2 Parallel trial | 1 | 201 | Std. Mean Difference (Fixed, 95% CI) | 0.54 [0.24, 0.84] |

