Ejercicio para los síntomas menopáusicos vasomotores
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | 3‐group RCT: exercise, yoga, control | |
| Participants | Low active or sedentary women 42 to 58 years of age who were experiencing vasomotor menopausal symptoms in the past month and had no history of surgical menopause and no hormone therapy use in the previous 6 months A total of 164 participants were randomly assigned (exercise n = 63, yoga n = 62, control n = 39). At four‐month follow‐up, 16 were lost to follow‐up (exercise n = 6, yoga n = 7, control n = 3). However, only 1 participant (yoga group) was excluded from the analyses (used HT); thus 163 participants were included in the analyses (161 for primary outcome). At 2‐year follow‐up, data were available for 134/164 randomly assigned participants. Of these, 102/134 agreed to take part in the 2‐year follow‐up study and 99/134 returned a follow‐up questionnaire (response rate of 74%; 99/134) (exercise n = 41, yoga n = 35, control n = 23). Overall, 60.4% (99/164) provided follow‐up questionnaire data 2 years after randomisation | |
| Interventions |
The intervention period was 4 months | |
| Outcomes | Vasomotor menopausal symptoms using the Greene Climacteric Scale. Adverse events were not reported | |
| Notes | Inclusion criteria stipulated that women had to be vasomotor symptomatic at baseline, but results indicate that based on classification of bleeding patterns (by self‐report), 17% of participants would be considered premenopausal Most of the sample (70%) were overweight or obese More participants were purposefully randomly assigned to the exercise (n = 63) and yoga (n = 62) groups than to the control group (n = 39). Trial authors intentionally oversampled in the exercise and control groups to increase the probability of detecting a difference between outcomes in these groups, and because resources for physician cover for physiological testing were limited in the control group Intervention compliance: Compliance between yoga (63%) and exercise (70%) groups did not differ significantly during the 4‐month intervention period. At 2‐year follow‐up, physical activity was assessed in terms of energy expenditure/METs per week, but no data according to group were reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned to trial groups by a computer‐based statistical package |
| Allocation concealment (selection bias) | High risk | Contact with trial authors indicates that allocation was not concealed from the research team |
| Blinding of participants and personnel (performance bias) | Unclear risk | It is not possible to blind exercise interventions to participants nor to trial personnel |
| Blinding of outcome assessment (detection bias) | Low risk | Study states that all medical and testing staff were blind to group allocation at outcome assessment |
| Incomplete outcome data (attrition bias) | Low risk | 161/164 women were analysed for the primary outcome |
| Selective reporting (reporting bias) | Unclear risk | Study does not report adverse events |
| Other bias | Unclear risk | Trial groups were not balanced at baseline with regard to age, socioeconomic status and number of children. High rate of refusal to participate among eligible women (204/462 refused) could potentially affect applicability of findings |
| Methods | 3‐group RCT: exercise plus soy milk (n = 12 analysed), soy milk only (n = 15 analysed) and control (n = 10 analysed) Study authors analysed 37 participants (exercise plus soy milk n = 12; soy milk only n = 15; control n = 10), but no data regarding dropouts or loss to follow‐up were reported. Study authors did not respond to our request for further information regarding loss to follow‐up. Therefore it is unclear how many women were randomly assigned | |
| Participants | Non‐smoking postmenopausal women, free from disease, not taking any form of hormone treatment in the previous 12 months and not currently using soybean‐derived products or herbal medications, with intact uterus and experiencing hot flushes | |
| Interventions |
| |
| Outcomes | Vasomotor menopausal symptoms assessed using the Kupperman Index. Adverse events not reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study states it is a randomised trial and provides no other details |
| Allocation concealment (selection bias) | Unclear risk | No information was given in the trial report to allow a judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | It is not possible to blind exercise interventions to participants or to trial personnel |
| Blinding of outcome assessment (detection bias) | Unclear risk | Reports of the trial do not state whether outcome assessors were blinded from knowledge of which intervention participants received |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether the 37 women analysed included all who were randomly assigned |
| Selective reporting (reporting bias) | Unclear risk | Outcomes were reported in narrative form and on graphs; no raw data were suitable for analysis. Adverse events were not reported |
| Other bias | Unclear risk | Poor reporting: Control intervention was not described. Baseline characteristics are similar in the 2 groups |
| Methods | 2‐group RCT: exercise, HT | |
| Participants | Women 48 to 63 years, with vasomotor symptoms and spontaneous menopause at least 6 months previously and exercising less than 1 hour per week at baseline. Contact with the study author revealed that participants were not taking HT at baseline Study originally included 75 women who were randomly assigned to exercise, 2 modes of acupuncture, oestrogen therapy (HT) or applied relaxation (n = 15 per group). We describe data here from the report that compared exercise with HT (Lindh‐Åstrand 2004). Results from the other groups are presented elsewhere (Nedstrand 2005; Wyon 2004), but none of these are compared with exercise. Of women randomly assigned to exercise, 4/15 did not start the exercise programme, and 1 participant dropped out during the intervention, resulting in 10/15 receiving follow‐up at 12 weeks. Only 5 of the participants randomly assigned to exercise completed follow‐up at 24 week and 36 weeks. Among women randomly assigned to HT (n = 15), all completed follow‐up at 12 weeks, and 9/15 completed 24‐week follow‐up. It is not entirely clear from the report how many women in the HT completed follow‐up at 9 months, but it appears to be 9/15. In summary, 14 participants provided follow‐up data at 24 weeks; therefore the Lindh‐Åstrand 2004 trial was judged likely to contain high attrition bias because dropout at follow‐up was substantial | |
| Interventions |
| |
| Outcomes | Number of hot flushes per 24 hours using a diary/log book. Climacteric symptoms assessed by the Kupperman Index, although scores for vasomotor symptoms subscale were not reported. Total climacteric symptom intensity and distress experienced from symptoms, although this outcome was not vasomotor symptom specific and was focused on all menopausal symptoms | |
| Notes | This trial report is part of a larger trial in which women were also randomly assigned to 3 other treatment groups; data from these groups are reported separately | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study reports it is a randomised trial and provides no other details |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed with the use of identical, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) | Unclear risk | It is not possible to blind exercise interventions to participants or to trial personnel |
| Blinding of outcome assessment (detection bias) | Unclear risk | Reports of the trial do not state whether outcome assessors were blinded from knowledge of which intervention participants received |
| Incomplete outcome data (attrition bias) | High risk | Data are incomplete for all outcomes and were unbalanced across groups at each follow‐up. Reason for missing data is likely to be related to true outcome. Only 10/15 (66%) women in exercise arm were included in the analysis |
| Selective reporting (reporting bias) | Unclear risk | Adverse effects were not reported |
| Other bias | Unclear risk | High rate of cross‐overs was seen in the exercise arm—only 5 women completed protocol and follow‐up; 5/10 included in analysis started HT during study |
| Methods | 2‐group RCT: exercise vs control | |
| Participants | Symptomatic women experiencing daily hot flushes, 40 to 63 years of age, not taken HT in the previous 3 months, sedentary and 6 to 36 months since less menstruation. All participants were of white ethnicity Study randomly assigned 176 women equally to the exercise group or the control group; 154 received follow‐up (exercise group n = 74; control group n = 80). Both trial groups received 1‐hour lectures once or twice per month from the principal investigator on physical activity and general health | |
| Interventions |
All participants also attended lectures (60‐75 minutes) once or twice per month, which covered topics such as physical activity and general health | |
| Outcomes | Vasomotor symptoms measured by the Women's Health Questionnaire. Hot flushes and night sweats recorded by diary. Adverse events not reported | |
| Notes | Control group attended lectures once or twice per month, which covered topics such as physical activity and general health | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation list was computer generated |
| Allocation concealment (selection bias) | Unclear risk | Envelopes were used to randomly assign participants, but no details were provided about whether they were sealed or consecutively numbered |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information about blinding is given |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information about blinding is given |
| Incomplete outcome data (attrition bias) | Unclear risk | 154/176 (88%) women were included in the analysis. Dropouts were potentially related to efficacy or adverse effects (e.g. 2 dropouts in exercise group crossed over to HT, 2 dropped out because of musculoskeletal problems, no reason was given for 9). Significant differences in age and weight were noted between dropouts and non‐dropouts |
| Selective reporting (reporting bias) | Unclear risk | Adverse effects were not reported |
| Other bias | Low risk | This study appears free of other sources of bias |
| Methods | 3‐group RCT: exercise, yoga and usual care control group | |
| Participants | Women 42 to 62 years of age, late perimenopausal or postmenopausal or having a hysterectomy with FSH > 20 mlU/mL and oestradiol ≥ 50 pg/mL. To be eligible, women must have been experiencing 14 or more vasomotor symptoms per week in each of 3 consecutive weeks, as measured by daily diaries. Vasomotor symptom frequency between visits 1 and 2 no less than 50% of weekly mean in the 2 weeks before Visit 1, and symptoms rated as severe or bothersome on at least 4 occasions. Women taking HT or contraceptives in past 2 months were excluded, as were women with BMI > 37. Women taking omega‐3 and participating in yoga in the previous 3 months were excluded 355 women were randomly assigned to exercise (n = 106), usual activity (n = 142) or yoga (n = 107). Of these, 338 received follow‐up (exercise n = 101, yoga n = 102, control group n = 135) | |
| Interventions |
Women were further randomly assigned (1:1) within each arm to 1.8 g/d U‐3 fish oil or identically appearing placebo capsules | |
| Outcomes | Vasomotor symptom frequency as measured by daily diaries. Bother of symptoms as measured by daily diaries. Adverse events reported for both groups | |
| Notes | This was a multi‐site trial. Data for the yoga group were extracted for this review from the second trial publication (Newton 2013) Intervention compliance: Participants attended 8.5 (3.5) (mean (SD)) of 12 scheduled yoga sessions (ranging from 0 to 13). Women practiced at home 4.1 (2.3) times per week. On average, women did poses 2.6 (1.1) times per week and Yoga Nidra 2.3 (1.2) times per week. Adherence to the exercise intervention was assessed in several ways: attendance at 80% or more of training sessions; achievement of 80% or more of weekly energy expenditure goal; and achievement of target heart rate (+10 beats/min) for 50% or more of exercise time. Documented home‐based training sessions were counted for women who were unable to attend a facility‐based session. Study authors reported that 74 women adhered to the intervention (defined by training sessions), 66 women achieved the energy expenditure goal and 75 achieved the target heart rate goal. Activity behaviour outside exercise training decreased by 1.5 steps/min in the exercise group compared with an increase of 0.22 steps/min in the usual activity group (P value 0.02) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated dynamic randomisation algorithm was used to maintain comparability between groups |
| Allocation concealment (selection bias) | Low risk | Randomisation was conducted using a secure Web‐based database |
| Blinding of participants and personnel (performance bias) | Unclear risk | Data collectors were blinded to participants' group allocation |
| Blinding of outcome assessment (detection bias) | Unclear risk | Local access to information on group assignment was limited to site staff involved in delivery of the intervention |
| Incomplete outcome data (attrition bias) | Low risk | 241/248 (97%) women in exercise vs usual care group and 237/249 in yoga vs usual care group (95%) were included in the analysis |
| Selective reporting (reporting bias) | Low risk | Report includes all expected outcomes and data on adverse events |
| Other bias | Low risk | Women were further randomly assigned (1:1) within each arm to 1.8 g/d U‐3 fish oil or identically appearing placebo capsules. This appears unlikely to be associated with bias |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not all participants were symptomatic at baseline | |
| Participants were not vasomotor symptomatic at baseline | |
| Participants were not vasomotor symptomatic at baseline | |
| Not all participants were symptomatic at baseline | |
| Not an RCT | |
| Not all participants were vasomotor symptomatic at baseline | |
| Not all participants were symptomatic at baseline | |
| Not an RCT | |
| Nor an RCT | |
| Not an RCT | |
| No measure of vasomotor symptoms | |
| Not an RCT | |
| Participants were not vasomotor symptomatic at baseline | |
| Case control study | |
| 12.3% of participants were taking HT at baseline. Not possible to obtain data for those participants not taking HT at baseline | |
| 29% of participants were taking HT at the time of the study. Not clear whether all participants were vasomotor symptomatic at baseline | |
| Participants were not vasomotor symptomatic at baseline | |
| Not an RCT | |
| No measure of vasomotor symptoms | |
| No measure of vasomotor symptoms | |
| Not clear whether all participants were symptomatic at baseline, and the study author could not be located for clarification | |
| Not an RCT (systematic review) | |
| No measure of vasomotor symptoms | |
| Not all participants were symptomatic at baseline | |
| Unclear whether participants were symptomatic at baseline | |
| Participants were not vasomotor symptomatic at baseline | |
| Not an RCT | |
| Most participants were taking HT at baseline | |
| Not all participants were symptomatic at baseline | |
| No measure of vasomotor symptoms | |
| Participants were not vasomotor symptomatic at baseline | |
| Study not traceable by the British Library | |
| Not all participants were symptomatic at baseline | |
| Unclear whether participants were symptomatic at baseline | |
| No measure of vasomotor symptoms | |
| Not an RCT | |
| Not an RCT | |
| Not all participants were symptomatic at baseline | |
| Not an RCT | |
| Not an RCT | |
| Participants were not vasomotor symptomatic at baseline | |
| No measure of vasomotor symptoms | |
| Not an RCT | |
| Not an RCT | |
| Did not include an exercise intervention | |
| Not all participants were symptomatic at baseline |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Aerobic exercise as a treatment for vasomotor menopausal symptoms: randomised controlled trial |
| Methods | RCT |
| Participants | 261 inactive perimenopausal and menopausal symptomatic women not using HT |
| Interventions | 2 exercise interventions: (1) exercise consultations plus DVD and written literature; (2) exercise consultations plus exercise social support groups |
| Outcomes | Hot flushes, night sweats, other menopausal symptoms, quality of life, depression, anxiety |
| Starting date | January 2012 |
| Contact information | |
| Notes | Principal investigator of this trial is also the first author of this review |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||
| 1 Change in hot flushes/night sweats Show forest plot | 3 | 454 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.33, 0.13] | ||||||||||||||||||
| Analysis 1.1  Comparison 1 Exercise versus control, Outcome 1 Change in hot flushes/night sweats. | ||||||||||||||||||||||
| 2 Additional data: decrease in hot flushes Show forest plot | Other data | No numeric data | ||||||||||||||||||||
| Analysis 1.2
Comparison 1 Exercise versus control, Outcome 2 Additional data: decrease in hot flushes. | ||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in hot flushes/night sweats Show forest plot | 2 | 279 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.45, 0.38] |
| Analysis 2.1  Comparison 2 Exercise versus yoga, Outcome 1 Change in hot flushes/night sweats. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in mean number of flushes in 24 hours Show forest plot | 1 | 14 | Mean Difference (IV, Random, 95% CI) | 5.80 [3.17, 8.43] |
| Analysis 3.1  Comparison 3 Exercise versus HT, Outcome 1 Change in mean number of flushes in 24 hours. | ||||
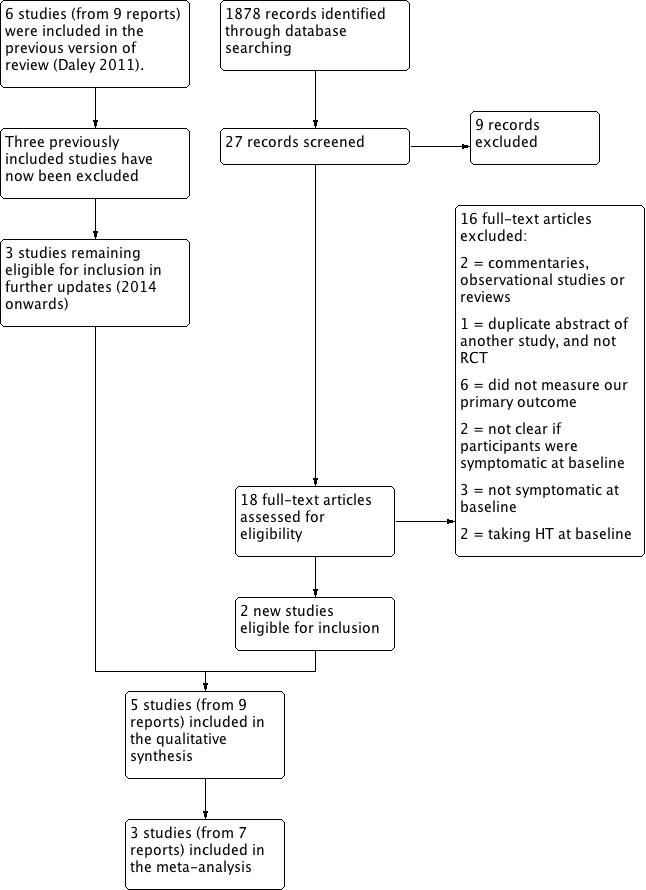
Study flow diagram.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
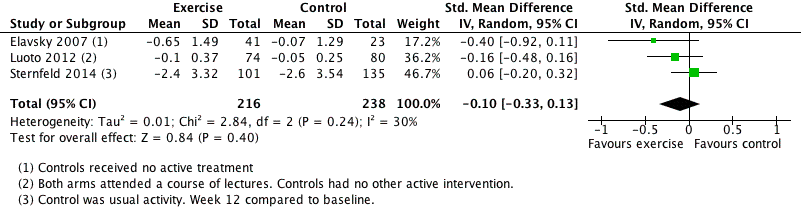
Forest plot of comparison. Exercise versus control, outcome: 1.1 Change in hot flushes/night sweats.

Forest plot of comparison. Exercise versus yoga, outcome: 1.2 Change in hot flushes/night sweats.
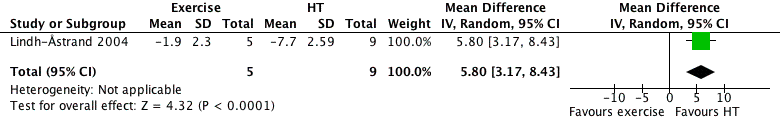
Forest plot of comparison. 3 Exercise versus HT, outcome: 3.1 Change in mean number of flushes in 24 hours.

Comparison 1 Exercise versus control, Outcome 1 Change in hot flushes/night sweats.
| Study | Outcome | Intervention | Comparison | Result | Statistical significance |
| Hanachi 2008 | Decrease in hot flushes | 1. Exercise + soymilk | 2. Soymilk only 3. Control (no details) | Group 1. Hot flushes decreased by 83% relative to Group 3 Group 2. Hot flushes decreased by 72% relative to Group 3 | Significant benefit for Group 1 and Group 2 versus Group 3 p<0.05 |
Comparison 1 Exercise versus control, Outcome 2 Additional data: decrease in hot flushes.
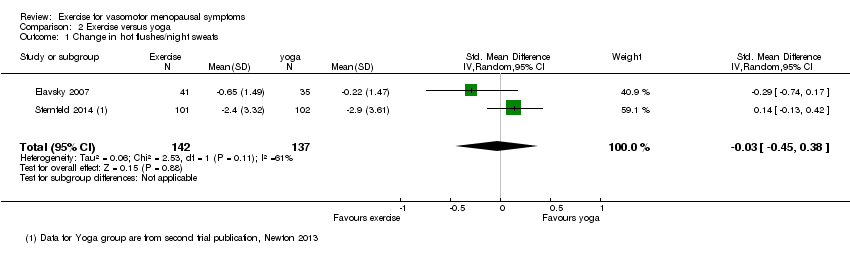
Comparison 2 Exercise versus yoga, Outcome 1 Change in hot flushes/night sweats.
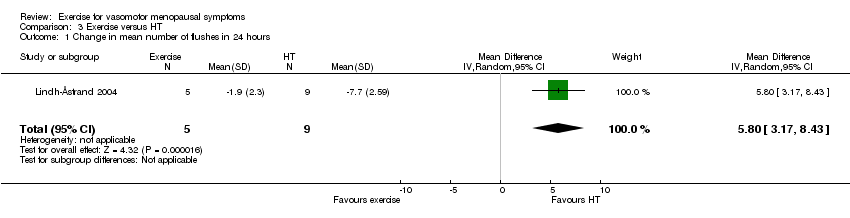
Comparison 3 Exercise versus HT, Outcome 1 Change in mean number of flushes in 24 hours.
| Exercise versus control for vasomotor menopausal symptoms | ||||
| Population: women with vasomotor menopausal symptoms | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | Number of participants | Quality of the evidence | Comments |
| Exercise versus no active treatment | ||||
| Change in hot flushes/night sweats | Mean change in hot flushes/night sweats is | 454 | ⊕⊝⊝⊝ Lowa,b,c | SMD ‐0.10 (‐0.33 to 0.13) |
| *The basis for the assumed risk is the mean control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||
| GRADE Working Group grades of evidence. | ||||
| aEvidence self‐reported: validated scales or logs/diaries used. | ||||
| Exercise versus yoga for vasomotor menopausal symptoms | ||||
| Population: women with vasomotor menopausal symptoms | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | Number of participants | Quality of the evidence | Comments |
| Corresponding risk | ||||
| Exercise versus yoga | ||||
| Change in hot flushes/night sweats | Mean change in hot flushes/night sweats | 279 | ⊕⊝⊝⊝ | SMD ‐0.03 (‐0.45 to 0.38) |
| *The basis for the assumed risk is the mean control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||
| GRADE Working Group grades of evidence. | ||||
| aEvidence self‐reported: validated scales or logs/diaries used. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in hot flushes/night sweats Show forest plot | 3 | 454 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.33, 0.13] |
| 2 Additional data: decrease in hot flushes Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in hot flushes/night sweats Show forest plot | 2 | 279 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.45, 0.38] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in mean number of flushes in 24 hours Show forest plot | 1 | 14 | Mean Difference (IV, Random, 95% CI) | 5.80 [3.17, 8.43] |

