Druck auf den Gebärmuttergrund während der Austreibungsphase
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised, controlled, single‐blind prospective study | |
| Participants | Trial conducted in Obstetrics and Gynecology Unit, San Giuseppe Hospital, Empoli, Italy from January 24‐March 24, 2011. 80 women randomised Inclusion criteria: primiparous women in active labour at term, maternal age 23–42 years, singleton pregnancy, cephalic presentation of the fetus Exclusion criteria: preterm delivery (gestational age < 37 weeks), breech or transverse position of the fetus, gestational diabetes mellitus, pregnancy‐induced hypertension, fetal macrosomia, placental abnormalities (low‐lying placenta or placental abruption), uterine anatomic abnormalities, previous uterine scar, fetal heart‐rate anomalies at the time of enrolment (bradycardia, tachycardia, or prolonged variable decelerations). | |
| Interventions | Intervention: 40 women allocated to having Baby‐guard Belt inflated to optimal pressures (80–150 mm Hg) during the second stage of labour. "During the second stage of labor, the operator inflated the ergonomic belt for 30 seconds at every contraction according to the pressures prescribed in the study protocol. Uterine fundal pressure through the inflatable belt was set at a 30°–40° angle to the spine toward the pelvic outlet, standardizing the force and surface area of application (980 cm2). The frequency of inflation was limited to fewer than 6 times (each time for 30 seconds) for a total period of 20 minutes, followed by a pause of 10 minutes." Control: 40 women allocated to having Baby‐guard Belt inflated with minimal pressures (10–20 mm Hg). All participants received standard management of the second stage of labour, which included fetal heart rate monitoring and care from the attending physician or midwife. | |
| Outcomes |
| |
| Notes | Baby‐guard Belt: “The Baby‐guard system consists of a disposable ergonomic 3‐chamber inflatable belt and a detector of electro‐physiologic signals of myographic uterine activity from the maternal abdomen (i.e. fetal and maternal heart signals). The 3 chambers of the belt can be inflated individually in order to reposition the fetus. These chambers are filled according to the pressures set by the operator (midwife or clinician) and allow gentle positioning of the fetus in the correct position toward the pelvis. Once the correct fetal position has been attained, all 3 chambers are inflated synchronously during uterine contraction. The maternal and fetal heart monitoring unit comprises a medical touch‐screen computer that records electro‐physiologic signals collected by a medical signal amplifier deriving from the mother (uterine contractions and maternal heart rate) and the fetus (fetal heart rate). There is also the possibility to record Doppler parameters of the fetal heart from the cardiotocograph.“ 27 out of 40 women in the low pressure group had Kristeller manoeuvre. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Eligible participants were assigned to 1 of 2 groups and randomisation was performed using numbered envelopes during full dilatation of the cervix.” No information on generation of random sequence |
| Allocation concealment (selection bias) | Unclear risk | Envelopes numbered, but not discussed if opaque/sealed |
| Blinding of participants and personnel (performance bias) | High risk | "The obstetrician, midwife, and participants were blind to whether the belt was inflated with sufficient pressure or not. During the second stage of labor, the operator inflated the ergonomic belt for 30 seconds at every contraction according to the pressures prescribed in the study protocol." The operator inflated the belt every 30 seconds for study group, so blinding was likely easy to ascertain. |
| Blinding of outcome assessment (detection bias) | High risk | Insufficient information provided. Unlikley to be feasible to blind this type of intervention |
| Incomplete outcome data (attrition bias) | Unclear risk | Difficult to assess, several outcomes are reported as continuous outcomes, and dichotomous outcomes do not report missing rates. |
| Selective reporting (reporting bias) | Unclear risk | Apgar score was not pre‐specified outcome, but its inclusion is reasonable. Other pre‐specified outcomes all reported |
| Other bias | Low risk | No evidence of other bias. Baseline demographics similar in both groups. 27/40 in the low pressure group had Kristeller manoeuvre. |
| Methods | Prospective randomised controlled trial. Individual randomisation | |
| Participants | Trial conducted at Kayseri Education and Training Hospital of Medicine, Turkey 295 women randomised Inclusion criteria: all participants were between 37 and 40 weeks of gestation with singleton cephalic presentation and none had any medical or obstetrical problems. Neither epidural nor combined spinal epidural analgesia was used. Exclusion criteria: pregnant women who required oxytocin augmentation, multiple gestations, pregnancy with medical problems (such as asthma, thyroid, cardiac, liver, kidney disease, pre‐eclampsia and diabetes), pregnancy with previous caesarean and pregnancy with estimated fetal weight < 2500 g or > 4000 g were not included into the study. | |
| Interventions | Intervention: fundal pressure (Kristeller manoeuvre) in second stage. No further detail given Control: no fundal pressure. No further detail given | |
| Outcomes |
| |
| Notes | Not clear what outcome was used for power calculation Conducted between 25 July 2012‐01 March 2013 at Kayseri Education and Training Hospital of Medicine, Turkey | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a computer‐generated random number chart |
| Allocation concealment (selection bias) | Unclear risk | Not well described. "In all consecutive patients, numbers were written on envelopes, while the allocation data were entered on separate papers that were put into the numbered envelopes which were then sealed." Envelopes not opened until women reached second stage. A quarter of the women were excluded between admission and before they reached the 2nd stage |
| Blinding of participants and personnel (performance bias) | High risk | Women and caregivers aware of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Many of the outcomes reported were subjective and may have been influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | "As a result of inadequate sample collection, 4 volunteers in the control group and 2 volunteers in the intervention group were excluded from the study. Because of blood clotting, 2 volunteers in the study and 2 volunteers in the control group were excluded from study." There was no clear information re when exactly randomisation took place and a quarter of the sample recruited were lost before the 2nd stage. A small number of women were lost to follow‐up or excluded post randomisation 10/295). |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available. It was not stated what outcome was used for the power calculation. |
| Other bias | High risk | Control group had more multiparous women 98/140. Intervention group had less 63/145. Mean age of women also differed The study was conducted only during daylight hours by the same obstetrician and fundal pressure was applied by the same obstetric staff. This may have affected which women were enrolled. |
| Methods | Randomised controlled trial. Participants individually randomised | |
| Participants | Trial took place in Turkey ‐ no further details given 197 women randomised Inclusion criteria: pregnant women between 37‐42 weeks' gestation, singleton cephalic presentation, none had any medical or obstetrical problems. Exclusion criteria: neither epidural nor combined spinal epidural analgesia was used. “excluded before the second stage by cesarean section, three were post‐ term pregnancies, seven were preeclamptic and one was a diabetic mother.” | |
| Interventions | Intervention: 94 women allocated to fundal pressure (Kristeller manoeuvre) Fundal pressure was applied manually with 1 of the provider’s forearms pressed on the uppermost part of the uterus at a 30°‐45° angle to the maternal spine in the direction of the pelvis. Fundal pressure was applied by obstetricians concomitant with each uterine contraction when the cervix was fully dilated and the woman felt a spontaneous urge to push down, until delivery of the fetal head. Control: 103 women had no fundal pressure | |
| Outcomes | Primary: duration of the second stage Secondary
| |
| Notes | Vaginal examinations were done every 30 min when the cervix reached 8 cm dilatation. If the woman felt a strong urge to push down, the examination was performed earlier. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number chart |
| Allocation concealment (selection bias) | Unclear risk | Opaqueness of envelopes was not discussed. “numbers were written on envelopes, while the allocation data were entered on separate papers that were put into the numbered envelopes which were then sealed. When the woman was admitted to the delivery ward and met the inclusion criteria, she signed the informed consent form and was given her participation number. When the woman had reached the second stage, the envelope with the participation number on its cover was opened to reveal the randomization.” |
| Blinding of participants and personnel (performance bias) | High risk | When the woman had reached the second stage, the envelope with the participation number on its cover was opened to reveal the randomisation and the obstetrician was informed whether fundal pressure was to be applied or not. |
| Blinding of outcome assessment (detection bias) | High risk | Not specified, presumably unblinded |
| Incomplete outcome data (attrition bias) | High risk | 1 participant lost to follow‐up Some missing data in both arms on umbilical cord blood analysis, disproportionately worse in intervention group |
| Selective reporting (reporting bias) | Unclear risk | Several outcomes did not have numerical data reported. |
| Other bias | Unclear risk | Control group were slightly older (26.68 ± 5.69 versus 24.41 ± 5.33, P = 0.007) and contained more nulliparous woman (54% (56/103) versus 36% (34/94) 0.009) than the study group. No other sources of bias evident |
| Methods | Simple randomisation by computer‐generated random numbers held within opaque sealed envelopes. Recruitment during first stage of labour, randomised at full dilatation. No blinding | |
| Participants | Trial conducted in Queen Charlotte's and Chelsea Hospital, London, UK 500 women randomised Inclusion criteria: nulliparous women, singleton cephalic at term, functioning epidural anaesthesia, ruptured membranes, maternal weight < 100 kg, maternal age between 20 and 40 | |
| Interventions | Intervention: routine care plus inflatable obstetric belt, to produce fundal pressure synchronised with the contractions. Applied immediately after randomisation, at full dilatation. Switched off when head was crowning/before instrumentation Control: routine care: 1 h passive second stage, 1 h pushing after which instrumental delivery if delivery not imminent | |
| Outcomes |
| |
| Notes | Non‐blinding appears to have had a significant impact on the outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Women who had given their consent to participate were randomised at full dilatation by means of computer‐ generated random numbers held within sealed, opaque, sequentially numbered envelopes.” |
| Allocation concealment (selection bias) | Low risk | “Women who had given their consent to participate were randomised at full dilatation by means of computer‐ generated random numbers held within sealed, opaque, sequentially numbered envelopes.” “No randomisation envelopes were lost during the study.” |
| Blinding of participants and personnel (performance bias) | High risk | Not feasible to blind this intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | “Participants were reviewed by the research registrar after delivery and asked about their second stage of labour by grading their levels of satisfaction using visual analogue scores. Women who used the belt were also asked to grade whether the belt was comfortable, restricted movement and gave them confidence.” Self‐reported outcomes at high risk of bias due to lack of blinding of participants and the researchers collecting the data. “Information about fetal wellbeing was obtained from the routine 24‐hour paediatric check (paediatricians were blind to allocation group).” Fetal wellbeing outcomes low risk of detection bias. |
| Incomplete outcome data (attrition bias) | Low risk | Difficult to assess for some outcomes, but does not appear to be a missing data problem. |
| Selective reporting (reporting bias) | Unclear risk | Unable to locate protocol. |
| Other bias | Unclear risk | “Both groups were homologous with regard to demographic and obstetric details at entry into the second stage of labour, except that women in the belt group had had their epidural in situ for significantly shorter than the control group (435 vs 526 min, P = 0.03).” |
| Methods | Randomised, controlled, prospective study. Women individually randomised | |
| Participants | 123 women randomised during first stage of labour between November 2006‐August 2007 Trial conducted in hospital in Seoul, Korea Inclusion criteria: nulliparous women, 20‐35 years of age, term (37 + 0 to 41 + 6 weeks' gestation), singleton cephalic presentation, with a clinically adequate pelvis, cervical dilatation < 10 cm on admission, and the estimated fetal body weight was > 2.8 kg and < 3.8 kg Exclusion criteria:
| |
| Interventions | Intervention: 62 women randomised to Labor Assister "Upon full dilation of the cervix, indicating the onset of the second stage of labor, the Labor AssisterTM was switched on in the active group. As a uterine contraction started, the inflatable obstetric belt was inflated synchronously and maintained at 200 mmHg for 30 sec. The Labor AssisterTM was not used for more than 3 hr and was discontinued when delivery was imminent, when the obstetrician decided to remove the device, or when the patient requested removal of the device." Control: 61 women randomised to standard care Both arms: all participants wore the belt in the first stage of labour, but were unable to see the belt due to a draped screen. In addition, all the women, whether randomised to the belt or the control group, received standard management of the second stage of labour, which included 1‐to‐1 support, continuous electronic fetal heart rate monitoring, and care from midwife. All of the participants had continuous external fetal heart monitoring. | |
| Outcomes | NB: outcomes were not pre‐specified. Below list is based on reported results.
| |
| Notes | The Labor AssisterTM consists of a toco transducer, a control unit, and an inflatable belt. The toco transducer on the inflatable belt detects uterine contractions and sends the signal to the control unit, which then injects 200 mmHg of air into the belt for 30 sec. The frequency of inflation was limited to fewer than 7 times per 15 min. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | They were divided into 2 groups by randomly numbered envelopes. |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding of participants and personnel (performance bias) | High risk | “All patients wore the belt in the first stage of labor, but were unable to see the belt due to a draped screen.” Blinding likely to be broken |
| Blinding of outcome assessment (detection bias) | High risk | Not stated; based on protocol of LA use, blinding was unlikely |
| Incomplete outcome data (attrition bias) | Unclear risk | Difficult to assess, as insufficient information provided |
| Selective reporting (reporting bias) | Unclear risk | Difficult to assess, as outcomes were not pre‐specified in methods text |
| Other bias | Low risk | No evidence of this ‐ baseline data similar in both groups |
| Methods | Randomised, controlled, and prospective study | |
| Participants | Trial conducted in university hospital and medical centre in Korea from July 2009‐December 2010 188 women randomised Inclusion criteria: nulliparous women, gestation between 37 + 0 and 41 + 6 weeks, singleton cephalic presentation, less than 10 cm of cervical dilatation on admission, with a clinically adequate pelvis, and between 2.8 kg and 4.0 kg of estimated fetal birthweight. Exclusion criteria:
| |
| Interventions | Intervention: 97 women randomised to multi‐function inflatable belt (The Labor Assister). "Upon full dilation of the cervix, indicating the onset of the second stage of labor, the Labor Assister was switched on in the active group. It was begun in 10 min after the start of the second stage of labor. As a uterine contraction started, the inflatable obstetric belt was inflated synchronously and maintained at 200 mmHg for 30s. The Labor Assister was not used for more than 3h and was discontinued when delivery was imminent, when the obstetrician decided to remove the device, or when the patient requested removal of the device." Control: 91 women randomised to standard care. Both arms: all patients wore the belt in the first stage of labour, but were unable to see the belt due to a draped screen. In addition, all the women, whether randomised to the belt or the control group, received standard management of the second stage of labour, which included 1‐to‐1 support, continuous electronic fetal heart rate monitoring and care from doctor. | |
| Outcomes |
| |
| Notes | "The Labor Assister (Baidy M‐520/Curexo, Inc., Seoul, Korea) consists of a toco transducer, a control unit, an air hose and an inflatable belt (Figure 1). The toco transducer on the inflatable belt detects uterine contractions and sends the signal to the control unit, which then injects 200 mmHg of air into the belt for 30 sec." "The frequency of inflation was limited to fewer than 7 times per 15 min when oxytocin was administered." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “For all participants, numbers were written on envelopes, and the allocation data were entered on separate papers that were put into the numbered envelopes which were then sealed. When the woman was admitted to the delivery ward and met the inclusion criteria, she signed the informed consent form and was given her participation number. When the woman reached the second stage, the envelope with the participation number on its cover was opened to reveal the randomization and the obstetrician was informed whether inflatable obstetric belt was to be applied or not.” Does not specify opaque envelopes or not, or where randomisation sequence was generated from. |
| Allocation concealment (selection bias) | Unclear risk | See above ‐ not described |
| Blinding of participants and personnel (performance bias) | High risk | Belt was draped so that participant could not see inflation, this blinding is likely to be broken |
| Blinding of outcome assessment (detection bias) | High risk | Obstetrician controlled belt and given the nature of intervention, blinding is very unlikely |
| Incomplete outcome data (attrition bias) | High risk | Duration of the second stage was the primary outcome measure. It was not measured in 14 women who had caesarean sections and 1 woman who delivered precipitously. |
| Selective reporting (reporting bias) | Unclear risk | No protocol seen |
| Other bias | Low risk | No evidence of other bias – similar baseline characteristics in both groups |
| Methods | Pilot randomised controlled trial | |
| Participants | 209 women individually randomised Trial took place Maharishi Markendeshwar Institute of Medical Sciences and Research, Mullana, Ambala, India Inclusion criteria: healthy primigravidae women (aged 20‐27 years), singleton fetus in cephalic presentation, having spontaneous onset of labour, between 37‐40 weeks, pelvis being average adequate gynaecoid with no clinical evidence of cephalo‐ pelvic disproportion Exclusion criteria
| |
| Interventions | Intervention: 101 women received manual pressure applied to the uterine fundus during the second stage of labour "Fundal pressure was applied manually at a 30‐to 40‐degree angle to the spine in the direction of the pelvis by the same doctor and three applications at the most in group‐I patients after the clinical confirmation of full cervical dilatation with the vertex below the level of the ischial spines (plus‐station) and occipito‐anterior position." Control: 108 women received no fundal pressure Both arms: "to observe uniformity, right medio‐ lateral episiotomy was employed at the instance of crowning of the vertex in all the cases and the placenta was delivered by modified Brandt‐ Andrew’s technique (controlled cord traction) at the clinical confirmation of its separation following delivery of the baby". | |
| Outcomes |
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised table of numbers |
| Allocation concealment (selection bias) | Unclear risk | “Index cards with the random assignment were prepared and placed in sealed envelopes and a researcher who was blinded to the baseline examination findings opened the envelope, approximately at the onset of the second stage of labour, and the proceedings were done according to the group assignment.” Does not specify opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Not stated, but blinding unlikely given nature of intervention |
| Blinding of outcome assessment (detection bias) | High risk | Not stated, but blinding unlikely given nature of intervention |
| Incomplete outcome data (attrition bias) | Unclear risk | Difficult to assess, insufficient information |
| Selective reporting (reporting bias) | Unclear risk | Difficult to assess, but all outcomes appear to be reported. Protocol not seen |
| Other bias | Low risk | No evidence of other bias – similar baseline characteristics in both groups |
| Methods | Pilot randomised control trial. Individual randomisation | |
| Participants | Trial undertaken at Frere and Cecilia Makiwane Hospitals, East London, South Africa 120 women randomised Inclusion criteria: healthy nulliparous women singleton pregnancy and cephalic presentation and gestational age of 35 weeks and above, who had not given birth after 15 min of bearing down. Exclusion criteria: obstetric or medical complications | |
| Interventions | Intervention: 58 women allocated to planned controlled fundal pressure during the second stage. Women randomised after 15 minutes of bearing down if they had not yet delivered. "During contractions steady firm fundal pressure was applied using the palms of both hands in the direction of the pelvis using only the strength of her forearms. Steady, sustained pressure was maintained for the full duration of each contraction or 30 seconds, whichever was shorter. Forceful or rapid pressure and the use of body weight to apply pressure were avoided." Comparison: 62 women allocated to no fundal pressure. "The attendant assumed the same supportive position, but no fundal pressure was applied." In both groups women were encouraged to bear down | |
| Outcomes | Primary outcome:
Other outcomes:
| |
| Notes | Additional information was provided by the authors. Pilot study underpowered to identify any but very large differences between groups for study outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation was ordered using a computer‐generated random sequence in balanced blocks of variable size in a 1:1 ratio |
| Allocation concealment (selection bias) | Low risk | Consented women…were enrolled in the trial by research midwives, by entering the name in a recruitment register, then opening the next in a consecutively numbered series of sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Blinding women or staff to this intervention was not feasible |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessment and recording would mainly be by staff aware of the allocation |
| Incomplete outcome data (attrition bias) | Low risk | Data appears complete. Analysis by intention to treat |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Other bias | Low risk | Other bias not apparent. Groups appeared similar at baseline |
| Methods | Described as double‐blind clinical trial | |
| Participants | Trial took place in hospitals related to the Azad University in Tehran 2236 women randomised Inclusion criteria: active labour at term with a singleton fetus in vertex presentation Exclusion criteria:
| |
| Interventions | Intervention: 1171 women randomised to receive fundal pressure “Fundal pressure often was applied manually by impatient obstetricians or midwifes on part of the uterus at a 30_45 angle to the maternal spine in the direction of the pelvis with each uterine contraction when the cervix was fully diluted.” Control: 1065 women randomised to receive no fundal pressure | |
| Outcomes |
| |
| Notes | Additional information provided by trial authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Experienced group and control group were formed by randomized selection.“ Insufficient information provided |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information provided |
| Blinding of participants and personnel (performance bias) | High risk | “ Physicians, hospital personnel and mothers did not know that Researchers oversee the delivery process.” Blinding with this intervention is unlikely |
| Blinding of outcome assessment (detection bias) | High risk | Blinding with this intervention is unlikely |
| Incomplete outcome data (attrition bias) | Unclear risk | There are some errors in the totals for various tables |
| Selective reporting (reporting bias) | High risk | Difficult to assess, outcomes not well specified. Errors in reporting of certain outcomes such as duration of active second stage meant that data could not be used in this review. Protocol not seen |
| Other bias | Unclear risk | Trial reporting lacked clarity. Difficult to assess other sources of bias |
CTG: cardiotocogram
FBS: fetal blood sampling
NICU: neonatal intensive care unit
SCBU: special care baby unit
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| The studied intervention of fundal pressure was performed by choice of the clinician, and not as a result of allocation. Therefore, the risk of confounding factors is too high. This study cannot be considered as (quasi‐) randomised. | |
| This is a poor methodological quality study, with a high risk of bias. The description of allocation, "these women were allocated into the groups according to the order they came to the hospital", does not give adequate confirmation that serious allocation bias was excluded. Given that several studies with well‐described random allocation are available for the abdominal belt analysis, the reason for considering quasi‐randomised trials (paucity of randomized data) does not apply. |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised controlled trial (more information needed to ascertain) |
| Participants | 100 primiparous women, with normal vaginal delivery |
| Interventions | Intervention group: 50 women used multi‐functional abdominal pressure belt during the second and third stages of labour Control group: 50 women did not use the belt in labour |
| Outcomes |
|
| Notes | Trial conducted in Guangzhou, China Unable to find contact details of trial authors |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | The Gentle Assisted Pushing study (GAP). A multi‐centre randomised controlled trial of gentle assisted pushing in the upright posture (GAP) or upright posture alone compared with routine practice to reduce prolonged second stage of labour |
| Methods | Randomised, controlled, unblinded, clinical trial with 3 parallel arms across 4 hospital sites in South Africa |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Intervention arm 1: Gentle Assisted Pushing. The woman will be assisted to assume an upright kneeling or squatting posture on the bed. The trained birth attendant will kneel behind her on the bed or stand behind her with the woman positioned at right angles to the length of the bed and back close to the side of the bed. The trained birth attendant will wrap her arms around the woman passing below her axillae, and place both open palms, overlapping, on the fundus of her uterus. Steady pressure in the long axis of the uterus will be applied only during contractions. The duration of pressure will be limited to 30 s with a minimum of 30 s rest before the next pressure Intervention arm 2: upright crouching or kneeling position for second stage Control: recumbent/supine posture only |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Starting date | March 2015 |
| Contact information | Correspondence to [email protected] |
| Notes | Likely to finish June 2017 |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 No spontaneous vaginal birth within a specified time, as defined by the trial authors Show forest plot | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.71, 1.28] |
| Analysis 1.1  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 1 No spontaneous vaginal birth within a specified time, as defined by the trial authors. | ||||
| 2 Instrumental birth Show forest plot | 1 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.28 [0.14, 79.65] |
| Analysis 1.2  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 2 Instrumental birth. | ||||
| 3 Caesarean section Show forest plot | 1 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.07, 17.27] |
| Analysis 1.3 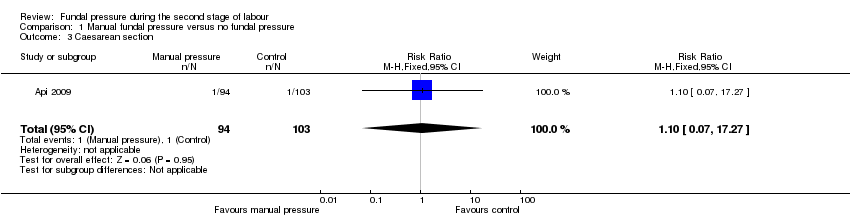 Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 3 Caesarean section. | ||||
| 4 Operative birth ‐ instrumental or caesarean Show forest plot | 2 | 317 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.12, 3.55] |
| Analysis 1.4  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 4 Operative birth ‐ instrumental or caesarean. | ||||
| 5 Low arterial cord pH Show forest plot | 2 | 297 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.72, 1.58] |
| Analysis 1.5 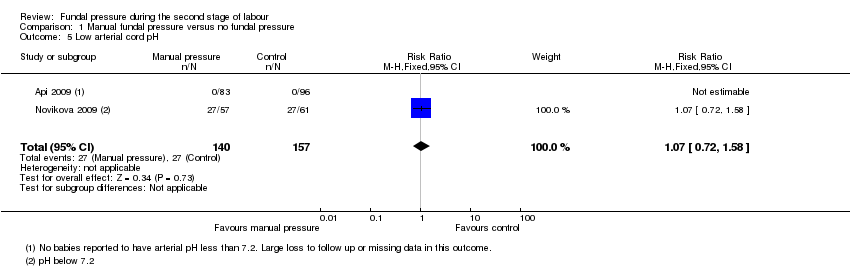 Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 5 Low arterial cord pH. | ||||
| 6 Apgar score less than 7 at 5 minutes Show forest plot | 4 | 2759 | Risk Ratio (M‐H, Random, 95% CI) | 4.48 [0.28, 71.45] |
| Analysis 1.6  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 6 Apgar score less than 7 at 5 minutes. | ||||
| 7 Duration of active second stage Show forest plot | 1 | 194 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐3.66, 2.06] |
| Analysis 1.7  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 7 Duration of active second stage. | ||||
| 8 Episiotomy Show forest plot | 2 | 317 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.92, 1.50] |
| Analysis 1.8  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 8 Episiotomy. | ||||
| 9 Soft tissue damage ‐ perineal Show forest plot | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.42 [0.79, 52.37] |
| Analysis 1.9 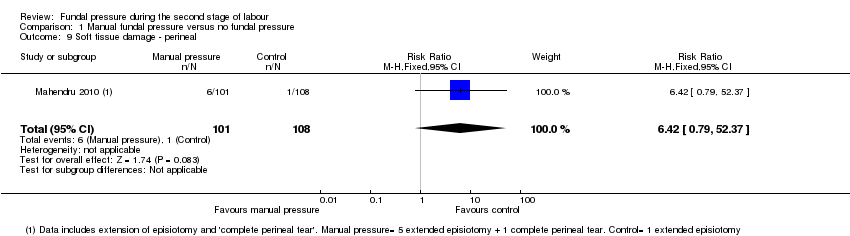 Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 9 Soft tissue damage ‐ perineal. | ||||
| 10 Soft tissue damage ‐ vaginal laceration Show forest plot | 1 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.75, 2.03] |
| Analysis 1.10  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 10 Soft tissue damage ‐ vaginal laceration. | ||||
| 11 Soft tissue damage ‐ cervical Show forest plot | 1 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.90 [1.09, 21.98] |
| Analysis 1.11 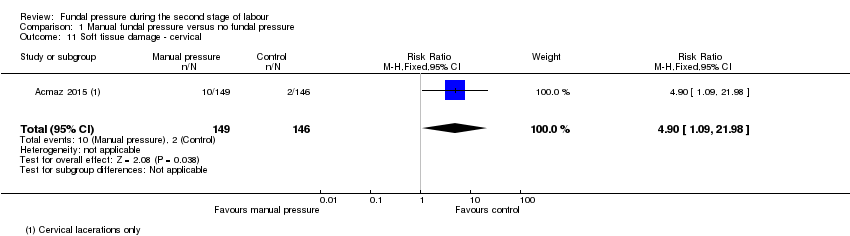 Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 11 Soft tissue damage ‐ cervical. | ||||
| 12 Postpartum haemorrhage Show forest plot | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.87 [0.58, 6.06] |
| Analysis 1.12  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 12 Postpartum haemorrhage. | ||||
| 13 Pain after enrolment as defined by trial authors Show forest plot | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.54 [2.21, 9.34] |
| Analysis 1.13 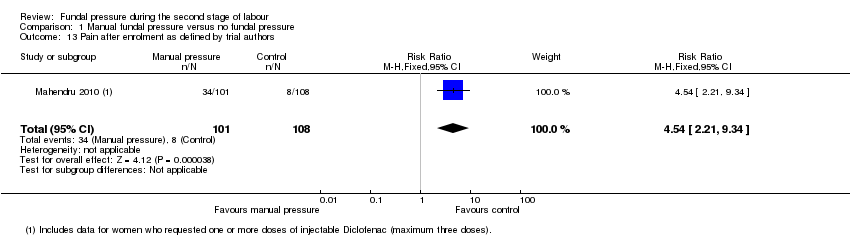 Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 13 Pain after enrolment as defined by trial authors. | ||||
| 14 Neonatal trauma ‐ fractures Show forest plot | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.14  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 14 Neonatal trauma ‐ fractures. | ||||
| 15 Neonatal trauma ‐ haematoma Show forest plot | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.15  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 15 Neonatal trauma ‐ haematoma. | ||||
| 16 Admission to neonatal intensive care unit Show forest plot | 1 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.40, 6.71] |
| Analysis 1.16 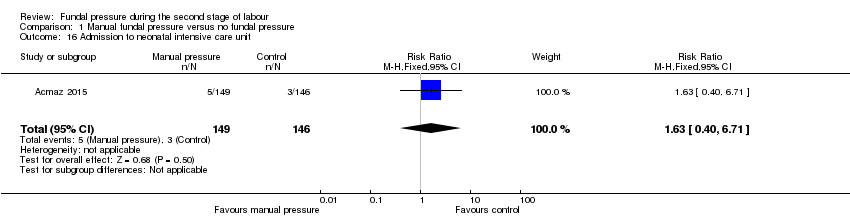 Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 16 Admission to neonatal intensive care unit. | ||||
| 17 Neonatal death Show forest plot | 2 | 2445 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.17  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 17 Neonatal death. | ||||
| 18 Sensitivity analysis: low arterial cord pH Show forest plot | 1 | 118 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.72, 1.58] |
| Analysis 1.18  Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 18 Sensitivity analysis: low arterial cord pH. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Instrumental birth Show forest plot | 4 | 891 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.52, 1.02] |
| Analysis 2.1  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 1 Instrumental birth. | ||||
| 2 Caesarean section Show forest plot | 4 | 891 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.14, 2.26] |
| Analysis 2.2  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 2 Caesarean section. | ||||
| 3 Operative birth ‐ instrumental or caesarean section Show forest plot | 4 | 891 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.38, 1.01] |
| Analysis 2.3 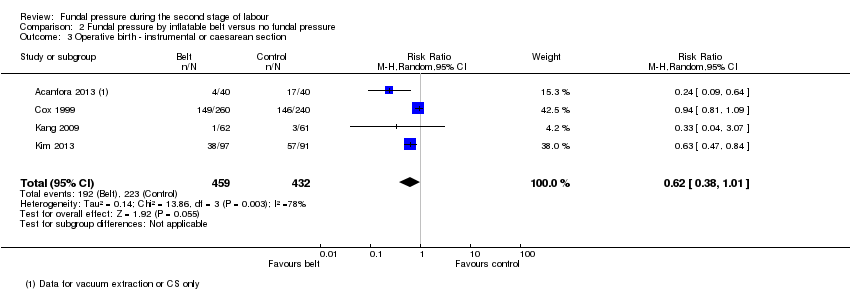 Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 3 Operative birth ‐ instrumental or caesarean section. | ||||
| 4 Low arterial cord pH Show forest plot | 1 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.09, 2.55] |
| Analysis 2.4 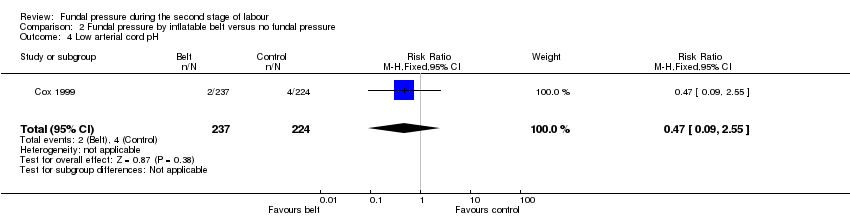 Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 4 Low arterial cord pH. | ||||
| 5 Apgar score less than 7 after 5 minutes Show forest plot | 1 | 500 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.62 [0.22, 95.68] |
| Analysis 2.5  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 5 Apgar score less than 7 after 5 minutes. | ||||
| 6 Duration of second stage Show forest plot | 2 | 253 | Mean Difference (IV, Random, 95% CI) | ‐50.80 [‐94.85, ‐6.74] |
| Analysis 2.6 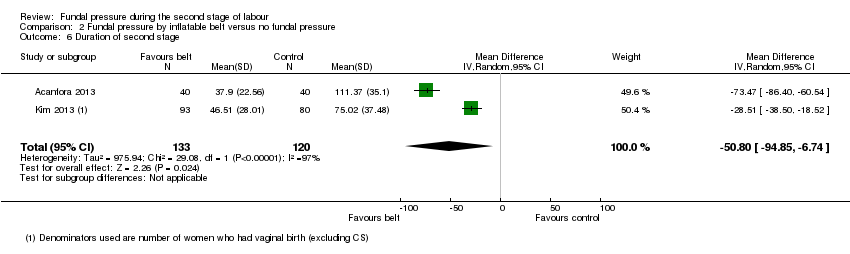 Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 6 Duration of second stage. | ||||
| 7 Episiotomy Show forest plot | 3 | 811 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.86, 1.12] |
| Analysis 2.7 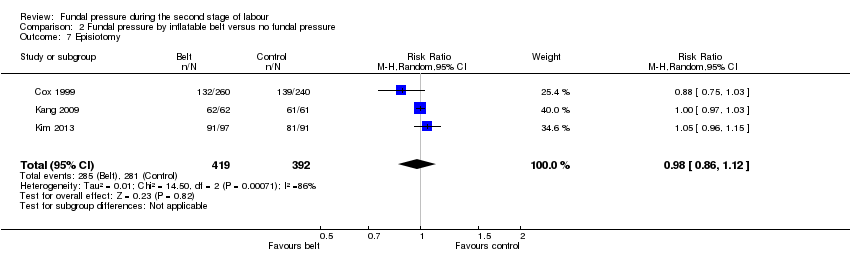 Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 7 Episiotomy. | ||||
| 8 Soft tissue damage ‐ perineal Show forest plot | 4 | 897 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.20, 1.38] |
| Analysis 2.8  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 8 Soft tissue damage ‐ perineal. | ||||
| 9 Soft tissue damage ‐ vaginal Show forest plot | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.27, 2.00] |
| Analysis 2.9 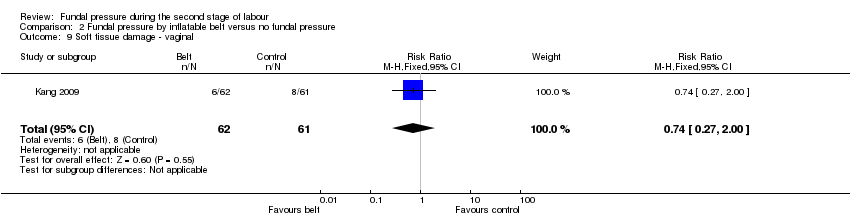 Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 9 Soft tissue damage ‐ vaginal. | ||||
| 10 Soft tissue damage ‐ anal sphincter Show forest plot | 1 | 500 | Risk Ratio (M‐H, Fixed, 95% CI) | 15.69 [2.10, 117.02] |
| Analysis 2.10  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 10 Soft tissue damage ‐ anal sphincter. | ||||
| 11 Soft tissue damage ‐ cervical/uterine Show forest plot | 2 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.06, 2.82] |
| Analysis 2.11  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 11 Soft tissue damage ‐ cervical/uterine. | ||||
| 12 Postpartum haemorrhage Show forest plot | 1 | 500 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.09, 1.29] |
| Analysis 2.12  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 12 Postpartum haemorrhage. | ||||
| 13 Neonatal trauma ‐ haematoma Show forest plot | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.90] |
| Analysis 2.13  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 13 Neonatal trauma ‐ haematoma. | ||||
| 14 Admission to neonatal intensive care unit Show forest plot | 4 | 891 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.19, 2.14] |
| Analysis 2.14 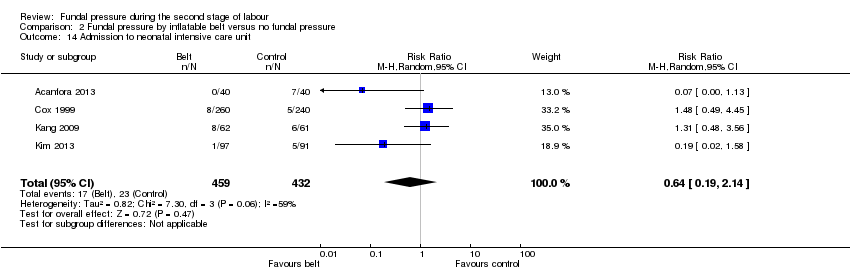 Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 14 Admission to neonatal intensive care unit. | ||||
| 15 Sensitivity analysis: instrumental birth Show forest plot | 3 | 811 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.63, 1.04] |
| Analysis 2.15  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 15 Sensitivity analysis: instrumental birth. | ||||
| 16 Sensitivity analysis: caesarean section Show forest plot | 3 | 811 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.20, 3.19] |
| Analysis 2.16  Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 16 Sensitivity analysis: caesarean section. | ||||
| 17 Sensitivity analysis: operative delivery ‐ instrumental or caesarean section Show forest plot | 3 | 811 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.52, 1.13] |
| Analysis 2.17 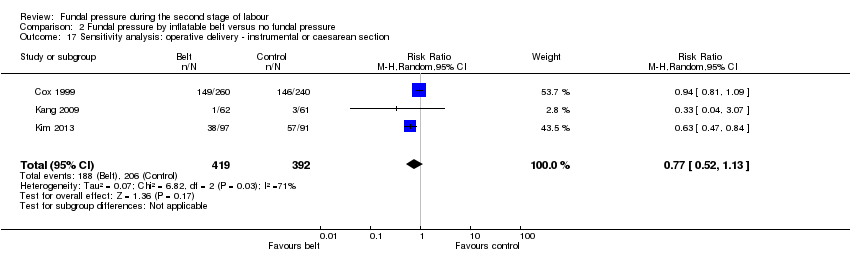 Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 17 Sensitivity analysis: operative delivery ‐ instrumental or caesarean section. | ||||

Study flow diagram

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 1 No spontaneous vaginal birth within a specified time, as defined by the trial authors.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 2 Instrumental birth.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 3 Caesarean section.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 4 Operative birth ‐ instrumental or caesarean.
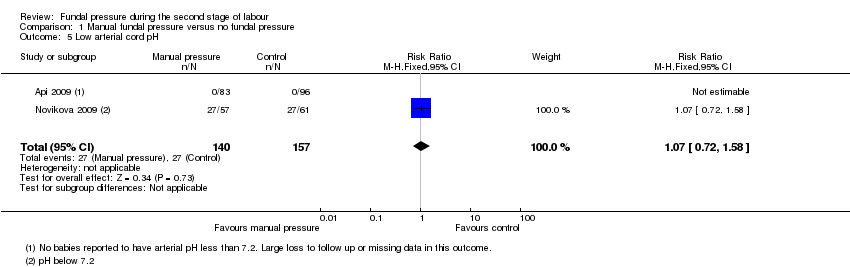
Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 5 Low arterial cord pH.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 6 Apgar score less than 7 at 5 minutes.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 7 Duration of active second stage.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 8 Episiotomy.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 9 Soft tissue damage ‐ perineal.
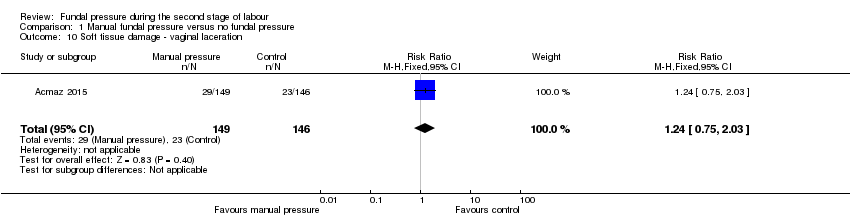
Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 10 Soft tissue damage ‐ vaginal laceration.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 11 Soft tissue damage ‐ cervical.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 12 Postpartum haemorrhage.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 13 Pain after enrolment as defined by trial authors.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 14 Neonatal trauma ‐ fractures.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 15 Neonatal trauma ‐ haematoma.
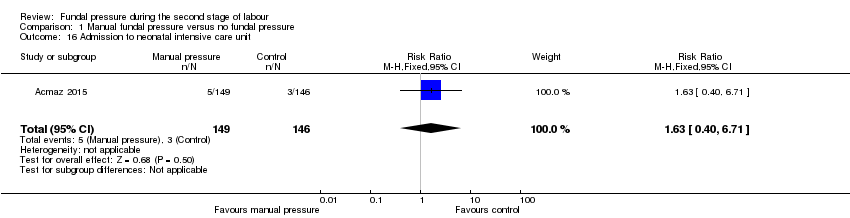
Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 16 Admission to neonatal intensive care unit.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 17 Neonatal death.

Comparison 1 Manual fundal pressure versus no fundal pressure, Outcome 18 Sensitivity analysis: low arterial cord pH.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 1 Instrumental birth.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 2 Caesarean section.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 3 Operative birth ‐ instrumental or caesarean section.
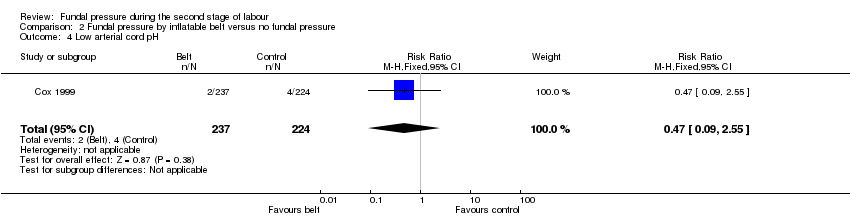
Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 4 Low arterial cord pH.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 5 Apgar score less than 7 after 5 minutes.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 6 Duration of second stage.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 7 Episiotomy.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 8 Soft tissue damage ‐ perineal.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 9 Soft tissue damage ‐ vaginal.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 10 Soft tissue damage ‐ anal sphincter.
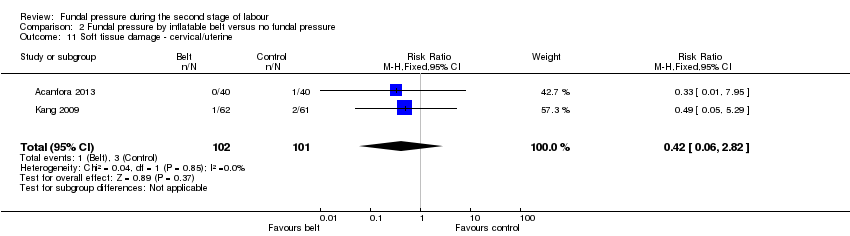
Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 11 Soft tissue damage ‐ cervical/uterine.
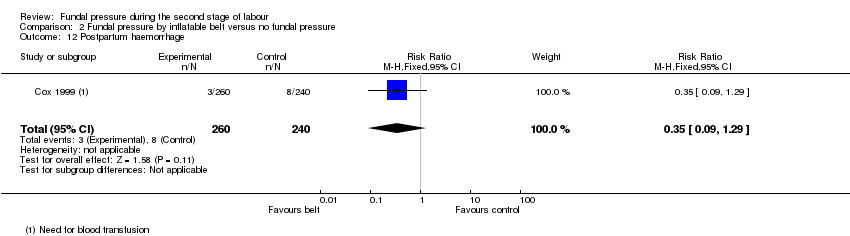
Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 12 Postpartum haemorrhage.
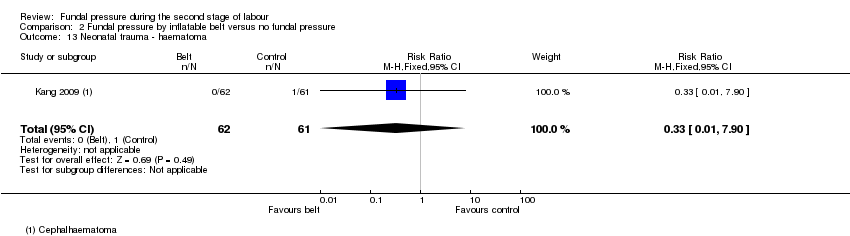
Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 13 Neonatal trauma ‐ haematoma.
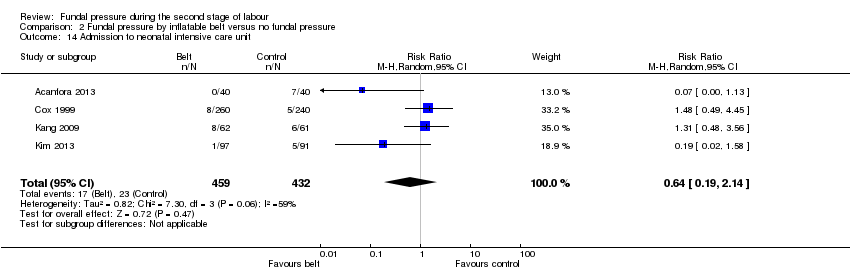
Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 14 Admission to neonatal intensive care unit.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 15 Sensitivity analysis: instrumental birth.

Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 16 Sensitivity analysis: caesarean section.
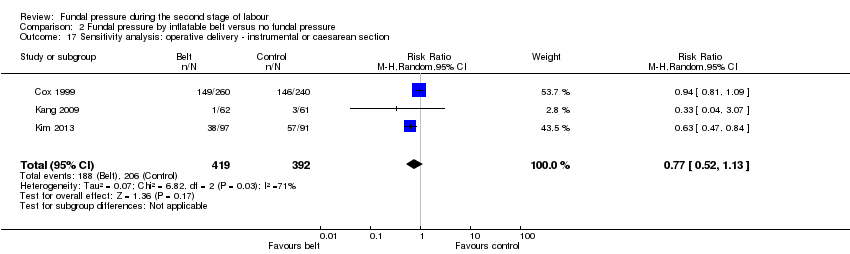
Comparison 2 Fundal pressure by inflatable belt versus no fundal pressure, Outcome 17 Sensitivity analysis: operative delivery ‐ instrumental or caesarean section.
| Manual fundal pressure compared to no fundal pressure for the second stage of labour | ||||||
| Patient or population: women with singleton pregnancy in vertex position in second stage of labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no fundal pressure | Risk with manual fundal pressure | |||||
| No spontaneous vaginal birth within a specified time, as defined by the trial authors | Study population | RR 0.96 | 120 | ⊕⊝⊝⊝ | Reported as "Time from bearing down to birth of head =/>30 min or operative delivery". Data may contain instrumental births and should be interpreted with due caution | |
| 613 per 1000 | 588 per 1000 | |||||
| Operative birth ‐ Instrumental or caesarean birth | Study population | Average RR 0.66 (0.12 to 3.55) | 317 (2 RCTs) | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 33 per 1000 (12 to 92) | |||||
| Low arterial cord pH | Study population | RR 1.07 | 297 | ⊕⊝⊝⊝ | ||
| 172 per 1000 | 184 per 1000 | |||||
| APGAR score less than 7 at 5 minutes | Study population | Average RR 4.48 | 2759 | ⊕⊝⊝⊝ | ||
| 5 per 1000 | 23 per 1000 | |||||
| Duration of active second stage | No absolute effects Mean duration of labour 16.6 minutes | No absolute effects Mean duration of labour 17.4 minutes | The mean duration of second stage was 0.8 minutes shorter in the fundal pressure group (3.66 minutes shorter to 2.06 minutes longer) | 194 | ⊕⊝⊝⊝ | |
| Severe maternal morbidity or death | Study population | ‐ | (0 study) | ‐ | No trial reported this outcome | |
| See comment | See comment | |||||
| Neonatal death | Study population | ‐ | 2445 | ⊕⊝⊝⊝ | Zero neonatal deaths reported in both trials | |
| See comment | See comment | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Wide confidence interval crossing the line of no effect, few events and small sample size (‐2). | ||||||
| Fundal pressure by inflatable belt compared to no fundal pressure for second stage of labour | ||||||
| Patient or population: women with singleton pregnancy in vertex position in second stage of labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no fundal pressure | Risk with fundal pressure by inflatable belt | |||||
| No spontaneous vaginal birth within a specified time | Study population | ‐ | (0 study) | ‐ | No trial reported this outcome | |
| See comment | See comment | |||||
| Operative birth ‐ instrumental or caesarean section | Study population | Average RR 0.62 | 891 | ⊕⊝⊝⊝ | ||
| 516 per 1000 | 320 per 1000 | |||||
| Low arterial cord pH | Study population | RR 0.47 | 461 | ⊕⊕⊝⊝ | ||
| 18 per 1000 | 8 per 1000 | |||||
| Apgar score less than 7 after 5 minutes | Study population | RR 4.62 | 500 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Duration of second stage (minutes) | No absolute effects | No absolute effects | The average mean duration of second stage was 50.8 minutes shorter in the inflatable belt group (94.85 minutes shorter to 6.74 minutes shorter) | 253 (2 RCTs) | ⊕⊝⊝⊝ | Acanfora 2013: mean duration of second stage was 73.47 minutes shorter for women in the inflatable belt group (86.40 minutes shorter to 60.54 minutes shorter) Kim 2013: mean duration of second stage was 28.51 minutes shorter for women in the inflatable belt group (38.50 minutes shorter to 18.52 minutes shorter) |
| Severe maternal morbidity and death | Study population | ‐ | (0 study) | ‐ | No trial reported these outcomes | |
| See comment | See comment | |||||
| Neonatal death | Study population | ‐ | (0 study) | ‐ | No trial reported this outcome | |
| See comment | See comment | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Most studies contributing data had design limitations (‐1). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 No spontaneous vaginal birth within a specified time, as defined by the trial authors Show forest plot | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.71, 1.28] |
| 2 Instrumental birth Show forest plot | 1 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.28 [0.14, 79.65] |
| 3 Caesarean section Show forest plot | 1 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.07, 17.27] |
| 4 Operative birth ‐ instrumental or caesarean Show forest plot | 2 | 317 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.12, 3.55] |
| 5 Low arterial cord pH Show forest plot | 2 | 297 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.72, 1.58] |
| 6 Apgar score less than 7 at 5 minutes Show forest plot | 4 | 2759 | Risk Ratio (M‐H, Random, 95% CI) | 4.48 [0.28, 71.45] |
| 7 Duration of active second stage Show forest plot | 1 | 194 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐3.66, 2.06] |
| 8 Episiotomy Show forest plot | 2 | 317 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.92, 1.50] |
| 9 Soft tissue damage ‐ perineal Show forest plot | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.42 [0.79, 52.37] |
| 10 Soft tissue damage ‐ vaginal laceration Show forest plot | 1 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.75, 2.03] |
| 11 Soft tissue damage ‐ cervical Show forest plot | 1 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.90 [1.09, 21.98] |
| 12 Postpartum haemorrhage Show forest plot | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.87 [0.58, 6.06] |
| 13 Pain after enrolment as defined by trial authors Show forest plot | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.54 [2.21, 9.34] |
| 14 Neonatal trauma ‐ fractures Show forest plot | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Neonatal trauma ‐ haematoma Show forest plot | 1 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Admission to neonatal intensive care unit Show forest plot | 1 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.40, 6.71] |
| 17 Neonatal death Show forest plot | 2 | 2445 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Sensitivity analysis: low arterial cord pH Show forest plot | 1 | 118 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.72, 1.58] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Instrumental birth Show forest plot | 4 | 891 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.52, 1.02] |
| 2 Caesarean section Show forest plot | 4 | 891 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.14, 2.26] |
| 3 Operative birth ‐ instrumental or caesarean section Show forest plot | 4 | 891 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.38, 1.01] |
| 4 Low arterial cord pH Show forest plot | 1 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.09, 2.55] |
| 5 Apgar score less than 7 after 5 minutes Show forest plot | 1 | 500 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.62 [0.22, 95.68] |
| 6 Duration of second stage Show forest plot | 2 | 253 | Mean Difference (IV, Random, 95% CI) | ‐50.80 [‐94.85, ‐6.74] |
| 7 Episiotomy Show forest plot | 3 | 811 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.86, 1.12] |
| 8 Soft tissue damage ‐ perineal Show forest plot | 4 | 897 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.20, 1.38] |
| 9 Soft tissue damage ‐ vaginal Show forest plot | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.27, 2.00] |
| 10 Soft tissue damage ‐ anal sphincter Show forest plot | 1 | 500 | Risk Ratio (M‐H, Fixed, 95% CI) | 15.69 [2.10, 117.02] |
| 11 Soft tissue damage ‐ cervical/uterine Show forest plot | 2 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.06, 2.82] |
| 12 Postpartum haemorrhage Show forest plot | 1 | 500 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.09, 1.29] |
| 13 Neonatal trauma ‐ haematoma Show forest plot | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.90] |
| 14 Admission to neonatal intensive care unit Show forest plot | 4 | 891 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.19, 2.14] |
| 15 Sensitivity analysis: instrumental birth Show forest plot | 3 | 811 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.63, 1.04] |
| 16 Sensitivity analysis: caesarean section Show forest plot | 3 | 811 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.20, 3.19] |
| 17 Sensitivity analysis: operative delivery ‐ instrumental or caesarean section Show forest plot | 3 | 811 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.52, 1.13] |

