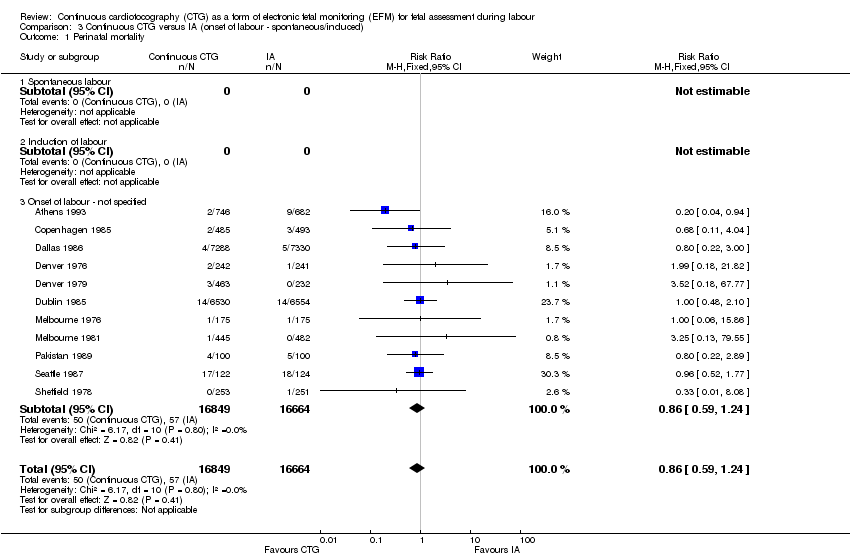
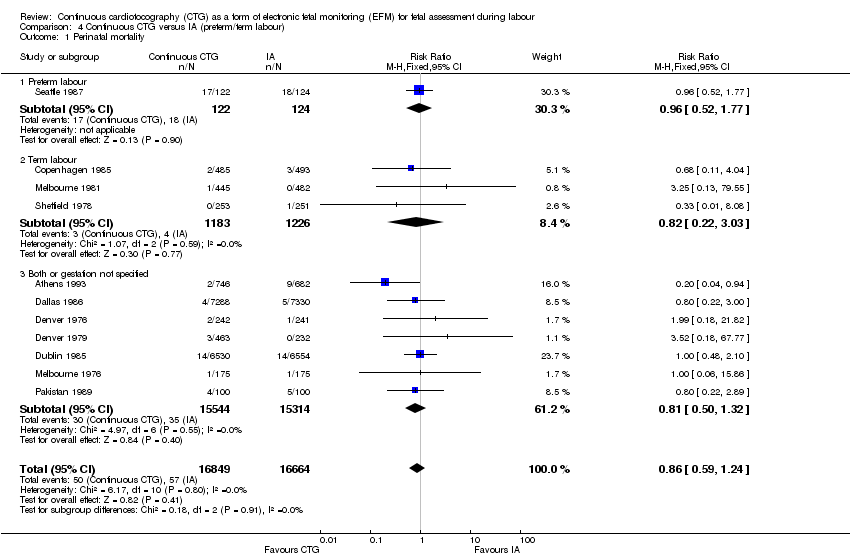
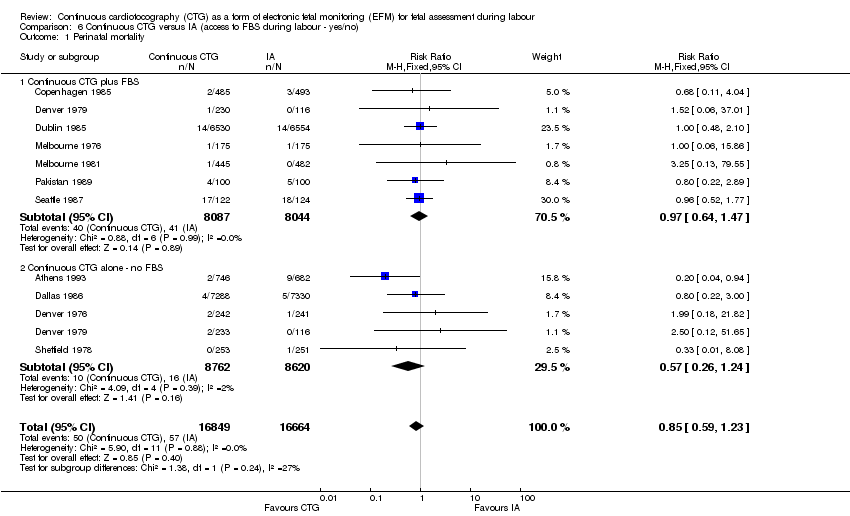
| 1 Perinatal mortality (primary outcome) Show forest plot | 11 | 33513 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.59, 1.24] |
|
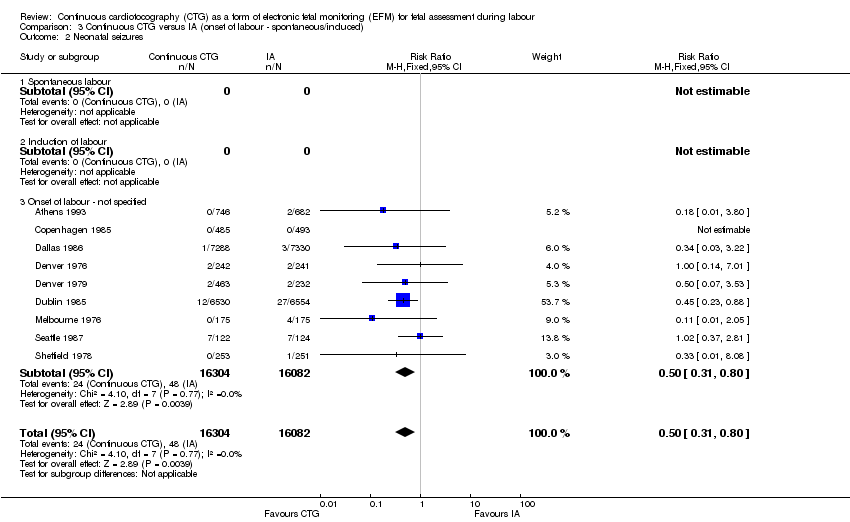
| 2 Neonatal seizures (primary outcome) Show forest plot | 9 | 32386 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.31, 0.80] |
|
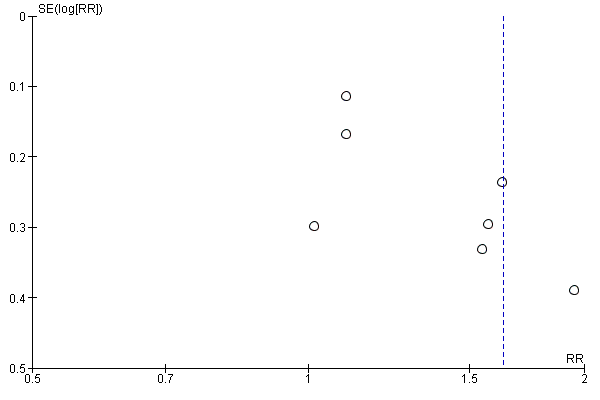
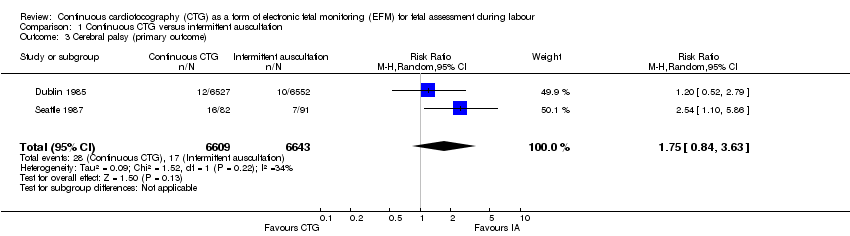
| 3 Cerebral palsy (primary outcome) Show forest plot | 2 | 13252 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.84, 3.63] |
|
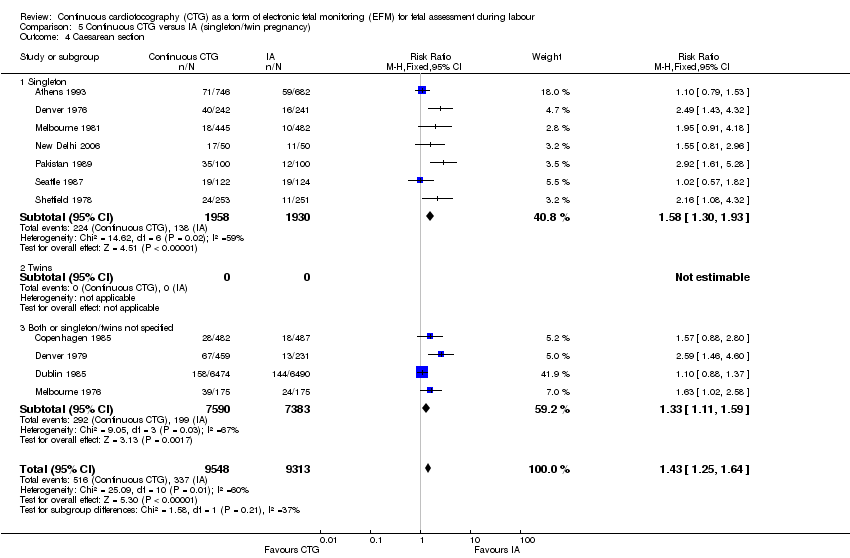
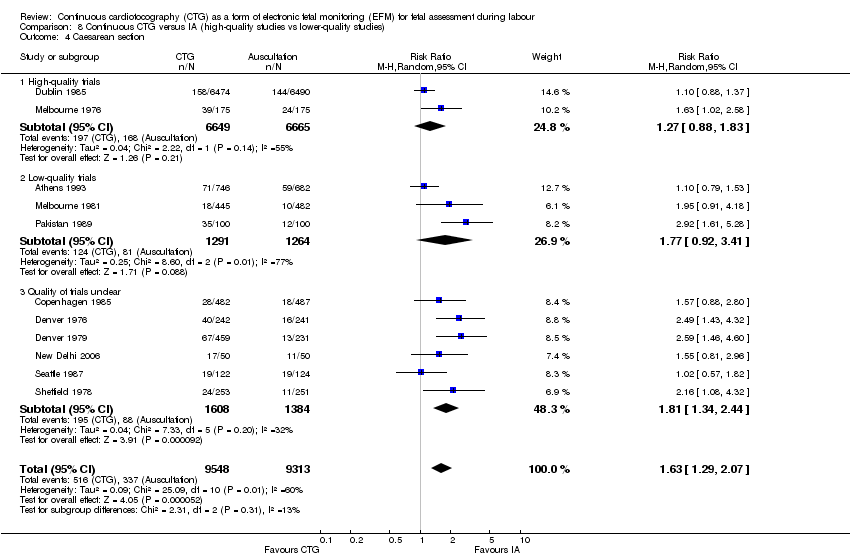
| 4 Caesarean section (primary outcome) Show forest plot | 11 | 18861 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [1.29, 2.07] |
|
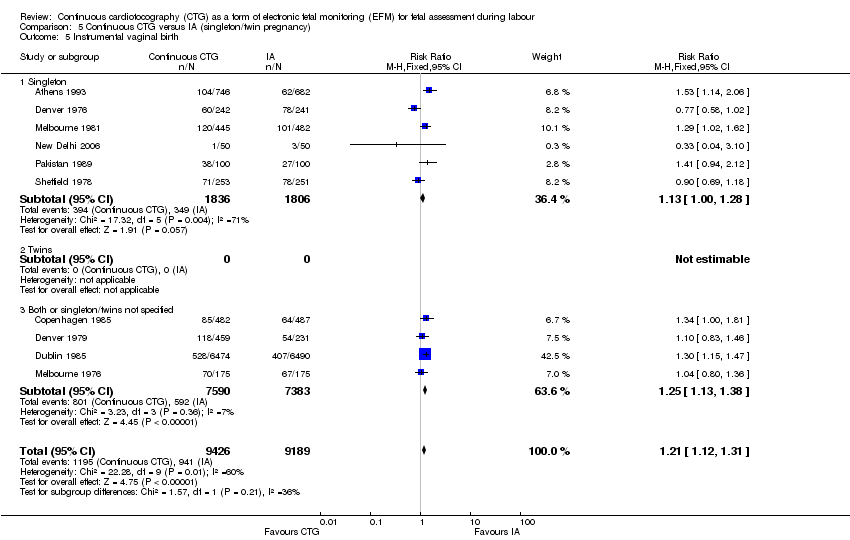
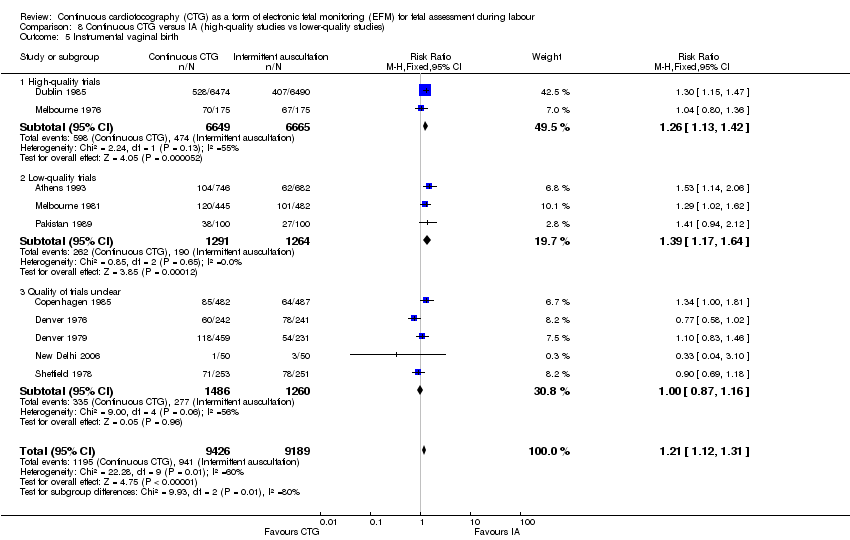
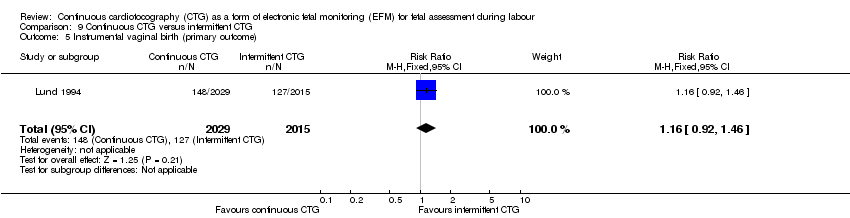
| 5 Instrumental vaginal birth (primary outcome) Show forest plot | 10 | 18615 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.01, 1.33] |
|
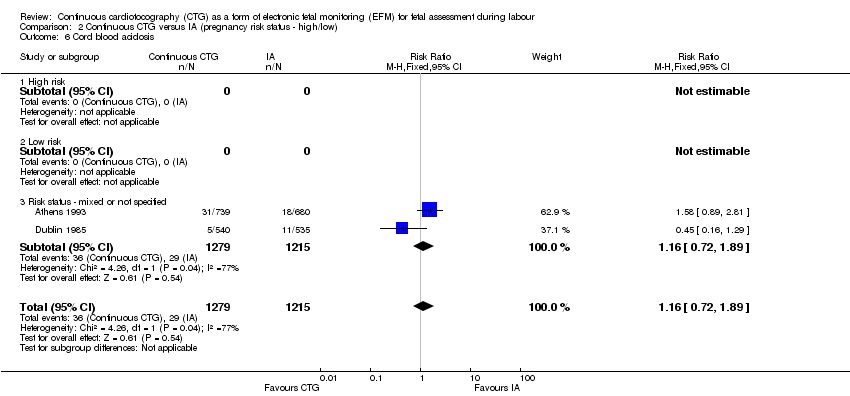
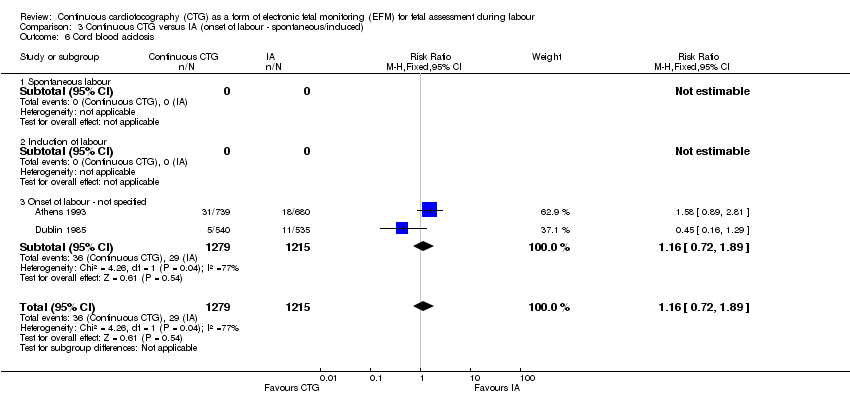
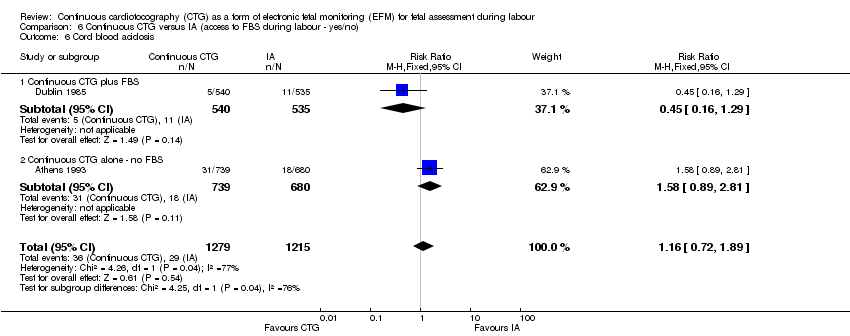
| 6 Cord blood acidosis (primary outcome) Show forest plot | 2 | 2494 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.27, 3.11] |
|
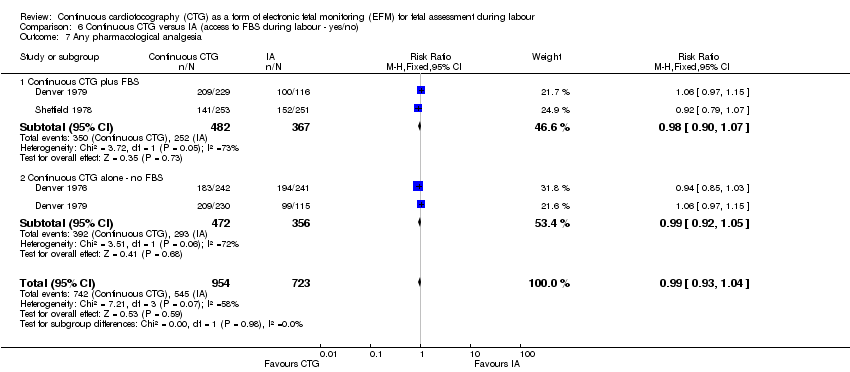
| 7 Any pharmacological analgesia (primary outcome) Show forest plot | 3 | 1677 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.88, 1.09] |
|
| 8 Hypoxic ischaemic encephalopathy Show forest plot | 1 | 1428 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.04, 5.03] |
|
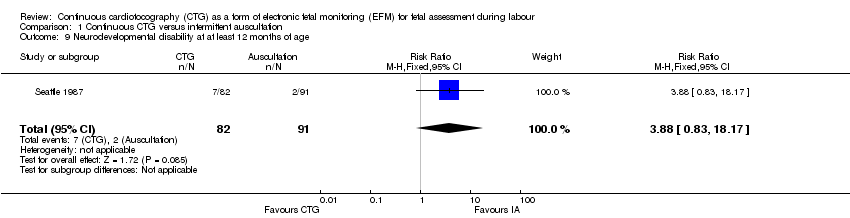
| 9 Neurodevelopmental disability at at least 12 months of age Show forest plot | 1 | 173 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.88 [0.83, 18.17] |
|
| 10 Apgar score < 7 at 5 minutes Show forest plot | 6 | 4137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.71, 1.27] |
|
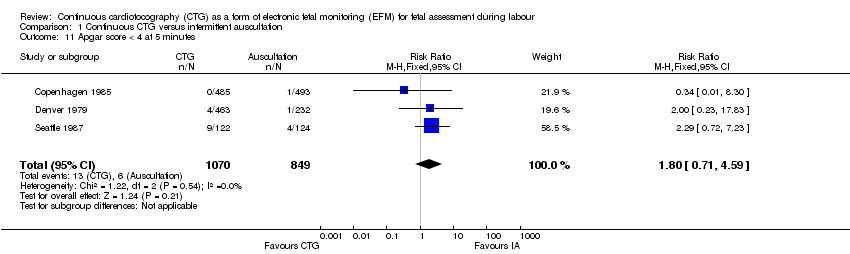
| 11 Apgar score < 4 at 5 minutes Show forest plot | 3 | 1919 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.80 [0.71, 4.59] |
|
| 12 Neonatal ICU admissions Show forest plot | 10 | 33167 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.86, 1.18] |
|
| 13 Fetal blood sampling Show forest plot | 2 | 13929 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [1.05, 1.47] |
|
| 14 Damage/infection from scalp electrode or scalp sampling Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.12, 72.77] |
|
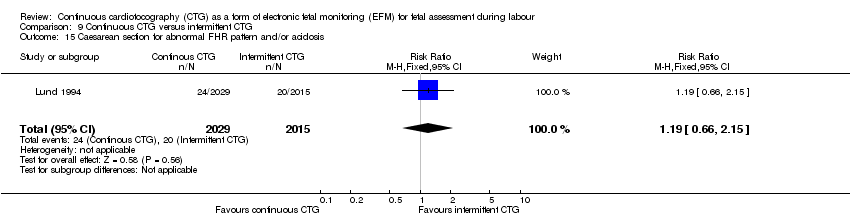
| 15 Caesarean section for abnormal FHR pattern and/or acidosis Show forest plot | 11 | 33379 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [1.89, 3.01] |
|
| 16 Instrumental vaginal birth for abnormal CTG or fetal acidosis Show forest plot | 1 | 12964 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.54 [1.95, 3.31] |
|
| 17 Spontaneous vaginal birth Show forest plot | 11 | 18861 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.86, 0.96] |
|
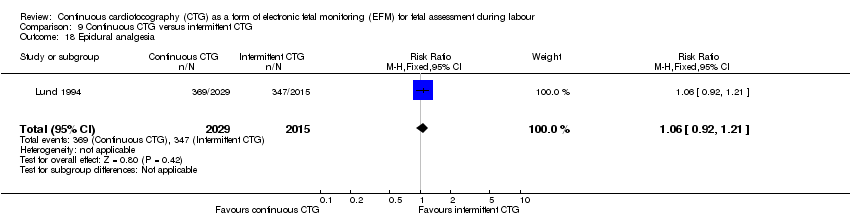
| 18 Epidural analgesia Show forest plot | 8 | 17630 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.12] |
|
| 19 Use of non pharmacological methods of coping with labour | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Amniotomy | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
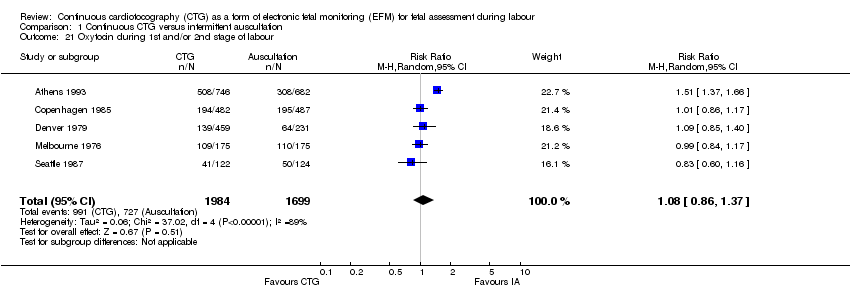
| 21 Oxytocin during 1st and/or 2nd stage of labour Show forest plot | 5 | 3683 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.86, 1.37] |
|
| 22 Perineal trauma needing repair | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Inability to adopt preferred position in labour | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 24 Dissatisifaction with labour and/or perceived loss of control | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Postpartum depression | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Exclusive breastfeeding at discharge | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
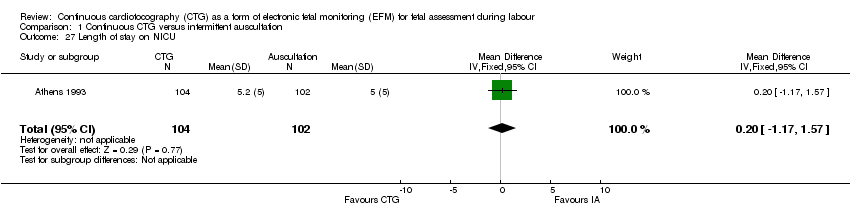
| 27 Length of stay on NICU Show forest plot | 1 | 206 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐1.17, 1.57] |
|