مداخلات برای پیشگیری یا درمان خونریزی شدید قاعدگی یا درد مرتبط با استفاده از دستگاه داخل‐رحمی
چکیده
پیشینه
خونریزی شدید قاعدگی و درد از دلایل شایعی است که زنان استفاده از دستگاه داخل‐رحمی (intrauterine device; IUD) را متوقف میکنند. استفادهکنندگان از IUD مسی (Cu IUD) با افزایش خونریزی قاعدگی روبهرو میشوند، در حالی که استفادهکنندگان از IUD لوونورژسترل (levonorgestrel) (LNG IUD) عادت ماهانه نامنظمی دارند. درمانهای داروی مورد استفاده برای کاهش خونریزی شدید قاعدگی یا درد مرتبط با استفاده از IUD نوع Cu و LNG شامل داروهای غیر‐استروئیدی ضد‐التهابی (non‐steroidal anti‐inflammatory drugs; NSAIDs)، ضد‐فیبرینولیتیکها (anti‐fibrinolytics) و پاراستامول (paracetamol) هستند. مداخلات درمانی و پیشگیرانه را جداگانه آنالیز کردیم زیرا پیامدهای مورد انتظار برای مداخلات درمانی و پیشگیرانه متفاوت هستند. کلاسهای دارویی مختلف را در آنالیز ترکیب نکردیم، چرا که مکانیسمهای اثر متفاوتی دارند. این یک نسخه بهروز شده از مروری است که ابتدا در مورد NSAIDها انجام شد. دامنه مرور گسترده شده و شامل تمام مداخلات برای درمان یا پیشگیری از خونریزی شدید قاعدگی یا درد مرتبط با استفاده از IUD میشود.
اهداف
ارزیابی همه کارآزماییهای تصادفیسازی و کنترل شده (randomised controlled trials; RCTs) که استراتژیهای درمان و پیشگیری را از خونریزی شدید قاعدگی یا درد مرتبط با استفاده از IUD ارزیابی کردند، به عنوان مثال، درمان دارویی و درمانهای جایگزین.
روشهای جستوجو
تا ژانویه 2021 به جستوجو در CENTRAL؛ MEDLINE؛ Embase و CINAHL پرداختیم.
معیارهای انتخاب
RCTهایی را به هر زبانی وارد کردیم که استراتژیهای درمان یا پیشگیری از خونریزی شدید قاعدگی یا درد مرتبط را با استفاده از IUD (Cu IUD؛ LNG IUD یا IUD دیگر) تست کردند. مقایسه میتوانست شامل عدم‐مداخله، دارونما (placebo) یا مداخله فعال دیگری باشد.
گردآوری و تجزیهوتحلیل دادهها
دو نویسنده مرور بهطور مستقل از هم به ارزیابی کارآزماییها برای ورود و خطر سوگیری (bias) آنها پرداختند، و دادهها را استخراج کردند. پیامدهای اولیه شامل حجم خونریزی در دوره قاعدگی، طول دوره قاعدگی و قاعدگی دردناک بود. از مدل اثرات‐تصادفی در تمام متاآنالیزها (meta‐analysis) استفاده کردیم. نویسندگان مرور، قطعیت شواهد را با استفاده از رویکرد درجهبندی توصیه، ارزیابی، توسعه و ارزشیابی (GRADE) ارزیابی کردند.
نتایج اصلی
این مرور شامل 21 کارآزمایی با 3689 شرکتکننده از کشورهایی با سطح درآمد متوسط و بالا است. زنان 18 تا 45 سال بودند که یا قبلا از IUD استفاده کرده یا به تازگی یک IUD را برای پیشگیری از بارداری گذاشته بودند. کارآزماییهای وارد شده NSAIDها و دیگر مداخلات را بررسی کردند. یازده کارآزمایی از نوع درمانی بودند، هفت مورد روی استفادهکنندگان از Cu IUD، یک مورد بر LNG IUD و سه مورد بر یک نوع ناشناخته انجام شدند. تعداد ده کارآزمایی از نوع پیشگیرانه بودند، شش مورد بر استفادهکنندگان از Cu IUD و چهار مورد بر استفادهکنندگان از LNG IUD متمرکز بودند. شانزده کارآزمایی به دلیل ارزیابی ذهنی از درد و خونریزی، با خطر بالای سوگیری (bias) تشخیص روبهرو بودند.
درمان خونریزی شدید قاعدگی
Cu IUD
ویتامین B1 در مقایسه با دارونما منجر به استفاده کمتر از پد (pad) در روز (تفاوت میانگین (MD): 7.00‐؛ 95% فاصله اطمینان (CI): 8.50‐ تا 5.50‐) و روزهای کمتر همراه با خونریزی (MD: ‐2.00؛ 95% CI؛ 2.38‐ تا 1.62‐؛ 1 کارآزمایی؛ 110 زن؛ شواهد با قطعیت پائین) شد. شواهد در مورد تاثیر ناپروکسن (naproxen) در مقایسه با دارونما بر حجم خونریزی قاعدگی بسیار نامطمئن است (نسبت شانس (OR): 0.09؛ 95% CI؛ 0.00 تا 1.78؛ 1 کارآزمایی، 40 زن، شواهد با قطعیت بسیار پائین).
درمان با مفنامیک اسید (mefenamic acid) در مقایسه با ترانکسامیک اسید (tranexamic acid) منجر به کاهش حجم خون از دسترفته شد (MD: ‐64.26؛ 95% CI؛ 105.65‐ تا 22.87‐؛ 1 کارآزمایی، 94 زن؛ شواهد با قطعیت پائین). با این حال، هیچ تفاوتی در طول مدت خونریزی با درمان مفنامیک اسید یا ترانکسامیک اسید وجود نداشت (MD: 0.08 روز، 95% CI؛ 0.27‐ تا 0.42، 2 کارآزمایی، 152 زن؛ شواهد با قطعیت پائین).
LNG IUD
استفاده از اولیپریستال استات (ulipristal acetate) در مقایسه با دارونما در LNG IUD ممکن است تعداد روزهای خونریزی را در 90 روز کاهش ندهد (MD؛ 9.30‐ روز، 95% CI؛ 26.76‐ تا 8.16؛ 1 کارآزمایی، 24 زن، شواهد با قطعیت پائین).
نوع ناشناخته IUD
مفنامیک اسید ممکن است حجم خونریزی را در مقایسه با وایتکس آگنوس (Vitex agnus) بر اساس اندازهگیری انجام شده با نمودار تصویری ارزیابی خون (pictorial blood assessment chart) کاهش ندهد (MD: ‐2.40؛ 95% CI؛ 13.77‐ تا 8.97؛ 1 کارآزمایی؛ 84 زن؛ شواهد با قطعیت پائین).
درمان درد
Cu IUD
درمان با ترانکسامیک اسید و سدیم دیکلوفناک (sodium diclofenac) ممکن است منجر به تفاوتی اندک یا عدم تفاوت در وقوع درد شود (OR: 1.00؛ 95% CI؛ 0.06 تا 17.25؛ 1 کارآزمایی، 38 زن؛ شواهد با قطعیت بسیار پائین).
نوع ناشناخته IUD
ناپروکسن ممکن است درد را کاهش دهد (MD: 4.10؛ 95% CI؛ 0.91 تا 7.29؛ 1 کارآزمایی، 33 زن، شواهد با قطعیت پائین).
پیشگیری از خونریزی شدید قاعدگی
Cu IUD
شواهدی را با قطعیت بسیار پائین پیدا کردیم مبنی بر اینکه تولفنامیک اسید (tolfenamic acid) ممکن است در مقایسه با دارونما از بروز خونریزی شدید پیشگیری کند (OR: 0.54؛ 95% CI؛ 0.34 تا 0.85؛ 1 کارآزمایی، 310 زن). هیچ تفاوتی میان ایبوپروفن (ibuprofen) و دارونما در کاهش حجم خون از دسترفته (MD: ‐14.11؛ 95% CI؛ 36.04‐ تا 7.82) و طول دوره خونریزی (MD؛ 0.2‐ روز، 95% CI؛ 1.40‐ تا 1.0؛ 1 کارآزمایی، 28 زن، شواهد با قطعیت پائین) دیده نشد.
آسپرین (aspirin) ممکن است در مقایسه با پاراستامول از بروز خونریزی شدید پیشگیری نکند (MD: ‐0.30؛ 95% CI؛ 26.16‐ تا 25.56؛ 1 کارآزمایی، 20 زن؛ شواهد با قطعیت بسیار پائین).
LNG IUD
اولیپریستال استات در مقایسه با دارونما ممکن است درصد روزهای خونریزی را افزایش دهد (MD: 9.50؛ 95% CI؛ 1.48 تا 17.52؛ 1 کارآزمایی، 118 زن، شواهد با قطعیت پائین). دادههای کافی برای آنالیز در یک کارآزمایی واحد در مقایسه با میفپریستون (mifepristone) و ویتامین B به دست نیامد.
برای آنالیز کارآزمایی واحد به منظور مقایسه ترانکسامیک اسید و مفنامیک اسید و در کارآزمایی دیگری که ناپروکسن را با استرادیول (estradiol) مقایسه کرد، نیز دادههای کافی وجود نداشت.
پیشگیری از بروز درد
Cu IUD
شواهدی را با قطعیت پائین یافتیم مبنی بر اینکه تولفنامیک اسید ممکن است در مقایسه با دارونما در پیشگیری از قاعدگی دردناک موثر نباشد (OR: 0.71؛ 95% CI؛ 0.44 تا 1.14؛ 1 کارآزمایی، 310 زن). ایبوپروفن احتمالا کرامپهای قاعدگی را در مقایسه با دارونما کاهش نمیدهد (OR: 1.00؛ 95% CI؛ 0.11 تا 8.95؛ 1 کارآزمایی، 20 زن، شواهد با قطعیت پائین).
نتیجهگیریهای نویسندگان
یافتههای این مرور باید با احتیاط تفسیر شوند، زیرا شواهدی با قطعیت پائین و بسیار پائین دارند. کارآزماییهای وارد شده محدود بودند؛ اکثر شواهد از کارآزماییهای واحد با تعداد کمی شرکتکننده به دست آمدند. پژوهشهای بیشتر نیاز به انجام کارآزماییهای بزرگتر و گزارشدهی بهتر از کارآزمایی دارند. تاثیر استفاده از ویتامین B1 و مفنامیک اسید برای درمان قاعدگیهای شدید و تولفنامیک اسید برای پیشگیری از بروز قاعدگی شدید مرتبط با Cu IUD باید بررسی شوند. برای ایجاد شواهدی برای درمان و پیشگیری از قاعدگی شدید و دردناک مرتبط با LNG IUD، به انجام کارآزماییهای بیشتری نیاز است.
PICO
خلاصه به زبان ساده
داروهای مورد استفاده در مدیریت بالینی خونریزی شدید قاعدگی و درد مرتبط با دستگاههای داخل‐رحمی کنترل بارداری
پیشینه
خونریزی شدید قاعدگی (heavy menstrual bleeding) و کرامپ شایعترین دلایلی است که باعث میشوند زنان استفاده از دستگاه داخل‐رحمی (intrauterine device; IUD) را برای کنترل بارداری متوقف کنند. مطالعات را مرور کردیم تا بدانیم که تسکین درد یا دیگر داروها، یا روشهای دیگر میتوانند خونریزی و درد مرتبط با استفاده از IUD را کاهش دهند یا خیر.
ویژگیهای مطالعه
شواهد تا ژانویه 2021 بهروز است. مطالعاتی را وارد کردیم که درمان یا پیشگیری از خونریزی شدید قاعدگی یا درد مرتبط با استفاده از IUD را مورد بررسی قرار دادند. درمان میتوانست با داروی دیگر، عدم‐درمان یا دارونما (placebo) (داروی ساختگی) مقایسه شده باشد.
نتایج کلیدی
این مرور شامل 21 مطالعه با 3689 شرکتکننده زن است. یازده مطالعه درمان را بررسی کردند، در حالی که 10 مطالعه به پیشگیری از بروز خونریزی و درد شدید پرداختند. بیشتر شواهد از مطالعات واحد با تعداد کمی شرکتکننده به دست آمدند. اطمینانی اندک یا عدم‐اطمینان نسبت به این نتایج داریم. قطعیت شواهد محدود است زیرا برخی از مطالعات فقط شامل چند نفر بودند، مداخلات مختلفی داشتند یا گزارش روشنی را در مورد نحوه انجام مطالعه ارائه ندادند.
درمان خونریزی شدید قاعدگی
IUD مسی
ویتامین B1 ممکن است طول دوره خونریزی، تعداد روزهای لکهبینی و تعداد پدهای مورد استفاده را در روز کاهش دهد. مفنامیک اسید (mefenamic acid) در مقایسه با ترانکسامیک اسید (tranexamic acid) میتواند حجم خون از دسترفته را کاهش دهد اما تاثیری بر طول دوره خونریزی ندارد. ناپروکسن (naproxen) ممکن است حجم خونریزی قاعدگی مرتبط با IUD مسی را کاهش ندهد.
IUD لوونورژسترل (levonorgestrel)
اولیپریستال استات (ulipristal acetate) ممکن است خونریزی را میان استفادهکنندگان از IUD لوونورژسترل کاهش ندهد.
نوع ناشناخته IUD
در یک مطالعه با نوع ناشناخته IUD، متوجه شدیم که مفنامیک اسید ممکن است حجم خونریزی قاعدگی را کاهش ندهد.
درمان قاعدگی دردناک
IUD مسی
درمان با ترانکسامیک اسید و دیکلوفناک سدیم (sodium diclofenac) ممکن است باعث کاهش وقوع قاعدگی دردناک مرتبط با IUD مسی نشود.
نوع ناشناخته IUD
ناپروکسن (naproxen) شاید درد مرتبط با نوع ناشناخته IUD را کاهش دهد
پیشگیری از خونریزی شدید قاعدگی
IUD مسی
تولفنامیک اسید (tolfenamic acid) ممکن است از خونریزی شدید قاعدگی پیشگیری کند، در حالی که ایبوپروفن (ibuprofen) در مقایسه با دارونما تفاوتی اندک تا عدم تفاوت در حجم و مدت خونریزی قاعدگی ایجاد میکند. آسپرین (aspirin) در مقایسه با پاراستامول (paracetamol) ممکن است از وقوع خونریزی شدید قاعدگی پیشگیری نکند.
IUD لوونورژسترل (levonorgestrel)
مطالعات انجام شده بر ترانکسامیک اسید، استرادیول، ناپروکسن و میفپریستون (mifepristone) نمیتوانند به ما بگویند که خونریزی شدید قاعدگی مرتبط با استفاده از IUD لوونورژسترل پیشگیری میکنند یا خیر.
پیشگیری از بروز قاعدگی دردناک
IUD مسی
تولفنامیک اسید و ایبوپروفن در مقایسه با دارونما ممکن است برای پیشگیری از قاعدگی دردناک موثر نباشند.
نتیجهگیریهای نویسندگان
خونریزی شدید قاعدگی در استفادهکنندگان از IUD مسی ممکن است با ویتامین B و مفنامیک اسید درمان شود در حالی که ترانکسامیک اسید و دیکلوفناک ممکن است قاعدگی دردناک را کاهش ندهند. در مورد استفادهکنندگان از IUD لوونورژسترل، اولیپریستال ممکن است خونریزی شدید قاعدگی را کاهش ندهد یا از آن پیشگیری نکند. تولفنامیک اسید ممکن است از خونریزی شدید قاعدگی پیشگیری کند اما از بروز درد همراه با IUD لوونورژسترل پیشگیری نمیکند. اطمینان ما به شواهد در سطح پائین تا بسیار پائین است. برای تولید شواهدی با کیفیت بالاتر در مورد داروهای موثر برای درمان و پیشگیری از خونریزی شدید قاعدگی و قاعدگی دردناک مرتبط با استفاده از IUD، انجام مطالعات بیشتری در آینده مورد نیاز است. دسترسی به شواهد حاصل از مطالعات بیشتر به احتمال زیاد نتایج ما را تغییر خواهند داد.
Authors' conclusions
Summary of findings
| Interventions versus comparisons | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Vitamin B1 vs placebo | |||||
| Menstrual blood loss Number of pads (diary record) Follow‐up: 1 month after completion of intervention for 3 months | The mean number of pads was 19 pads | MD 7 pads fewer | ‐ | 110 | ⨁⨁◯◯ |
| Duration of bleeding Number of bleeding days (diary record)
Follow‐up: 1 month after completion of intervention for three months | The mean duration of bleeding was 8 days | MD 2 days fewer | ‐ | 110 | ⨁⨁◯◯ |
| Adverse events or side effects | None reported |
|
|
|
|
| Mefenamic acid vs tranexamic acid | |||||
| Menstrual blood loss Volume blood loss (pictorial chart in mL)
Follow‐up: after 3rd month of intervention | The mean volume of menstrual blood loss was 160 mL | MD 64.26 mL lower | ‐ | 94 | ⨁⨁◯◯ |
| Duration of bleeding Number of bleeding days (menstrual record)
Follow‐up: after 3rd month of intervention Recorded on daily diary | The mean number of bleeding days was 3.5 to 6.4 days | MD 0.08 days more | ‐ | 152 | ⨁⨁◯◯ |
| Adverse events or side effects | No data available |
|
|
|
|
| Mefenamic acid vs desmopressin | |||||
| Menstrual blood loss Mean reduction of PBAC score Follow‐up: after 3rd month of intervention | The mean reduction of PBAC score was 40.5% in desmopressin and 45.7% in mefenamic acid |
| 24 | ⨁◯◯◯ | |
| Tranexamic acid vs sodium diclofenac | |||||
| Menstrual blood loss Volume of blood loss (alkaline hematin method) Follow‐up: each intervention cycle (cross‐over) for 5 menstrual cycles | The mean blood loss was 102mL | MD 42.7mL lower | ‐ | 38 | ⨁◯◯◯ |
| Duration of bleeding
Follow‐up: each intervention cycle (cross‐over) for 5 menstrual cycles | The mean duration of bleeding was 5.1 days | MD 0 days | ‐ | 38 | ⨁◯◯◯ |
| Side effects: gastrointestinal disturbances (diarrhoea, lower abdominal pain), headache and sweating | 316 per 1000 | 684 per 1000 (356 to 895) | OR 4.69 (1.2 to 18.44) | 38 (1 RCT) | ⨁◯◯◯ |
| Tranexamic acid vs flavonoids | |||||
| Menstrual blood loss PBAC score Follow‐up: each cycle for 3 menstrual cycles | The mean PBAC score was 125 | MD 32 lower | ‐ | 100 | ⨁⨁◯◯ |
| Menstrual blood loss Number of pads per day Follow‐up: each cycle for 3 menstrual cycles | The mean number of pads was 3 pads per day | MD 0.5 pads lower | ‐ | 100 | ⨁⨁◯◯ |
| Duration of bleeding Number of bleeding days Follow‐up: each cycle for 3 menstrual cycles | The mean number of bleed days was 6.8 days | MD 1.4 days lower | ‐ | 100 | ⨁⨁◯◯ |
| Side effects: headache Follow‐up: each cycle for 3 menstrual cycles | 160 per 1000 | 99 per 1000 (33 to 268) | OR 0.58 (0.18 to 1.92) | 100 | ⨁⨁◯◯ |
| Side effects: vomiting Follow‐up: each cycle for 3 menstrual cycles | 180 per 1000 | 140 per 1000 (33 to 268) | OR 0.74 (0.25 to 2.18) | 100 | ⨁⨁◯◯ |
| Tranexamic acid vs active comparators (mefenamic acid, flavonoid, sodium diclofenac) | |||||
| Duration of bleeding Number of bleeding days Follow‐up: 2‐5 menstrual cycles
| The mean number of bleeding days was 5.1 to 6.8 days | MD 0.27 days lower | ‐ | 290 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; PBAC: pictorial blood assessment chart; RCT: randomized controlled trial; vs: versus aDowngraded one level due to unclear risk of selection bias. | |||||
| Interventions vs comparisons | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Ulipristal acetate vs placebo | |||||
| Duration of bleeding Total bleeding in 90 days (bleeding calendar) Follow‐up: 30, 60 and 90 days after treatment initiation | The mean total of bleeding days in 90 days was 29.8 to 39.1 days | MD 9.3 days lower | ‐ | 24 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded one level due to high risk of detection bias. | |||||
| Interventions vs comparisons | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |||
|---|---|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||||
| Mefenamic acid vs Vitex agnus | |||||||
| Menstrual blood loss PBAC score Follow‐up: monthly for 4 months | The mean PBAC score was 89.7 | 2.4 lower | ‐ | 84 | ⨁⨁◯◯ | ||
| Side effects: nausea Follow‐up: monthly for 4 months | 24 per 1000 | 24 per 1000 (1 to 287) | OR 1.00 (0.06 to 16.53) | 84 | ⨁⨁◯◯ | ||
| Side effects: abdominal pain Follow‐up: monthly for 4 months | 24 per 1000 | 8 per 1000 (0 to 167) | OR 0.33 (0.01 to 8.22) | 84 | ⨁⨁◯◯ | ||
| CI: confidence interval; MD: mean difference; OR: odds ratio; PBAC: pictorial blood assessment chart; RCT: randomized controlled trial; vs: versus aDowngraded one level due to unclear reporting bias. | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Tranexamic acid vs sodium diclofenac | |||||
| Pelvic pain Follow‐up: each intervention cycle (cross over) for 5 menstrual cycles | 53 per 1000 | 53 per 1000 | OR 1.00 | 38 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded two levels due to unclear risk of selection, performance and reporting bias and high risk of detection bias. | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Naproxen vs placebo | |||||
| Overall pain relief score (4‐point scale) Follow‐up: each cycle for 3 menstrual cycles | The mean overall pain relief score was 7.9 | MD 4.1 higher | ‐ | 33 | ⨁⨁◯◯ |
| Daily pain relief score (6‐point scale) Follow‐up: each cycle for 3 menstrual cycles | The mean daily pain relief score was 10.8 | 3.1 higher | ‐ | 33 | ⨁⨁◯◯ |
| Need for additional analgesia (self‐recorded) Follow‐up: each cycle for 3 menstrual cycles | 313 per 1000 | 116 per 1000 | OR 0.29 | 33 | ⨁⨁◯◯ |
| Side effects: gastrointestinal symptoms Follow‐up: each cycle for 3 menstrual cycles | 48 per 1000 | 95 per 1000 (9 to 557) | OR 2.11 (0.18 to 25.17) | 33 | ⨁⨁◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded two levels due to unclear risk of selection, performance and reporting bias as well as high risk of detection bias. | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Outcomes |
|---|---|---|---|---|---|
| Ibuprofen vs placebo | |||||
| Menstrual blood loss (alkaline hematin method) Follow‐up: 3 months | The mean menstrual blood loss was 44.7 to 109.2 mL | MD 14.11 mL lower | ‐ | 40 | ⨁◯◯◯ |
| Duration of bleeding (menstrual diary) Follow‐up: 3 months | The mean duration of bleed was 6.4 days | MD 0.2 days lower | ‐ | 28 | ⨁◯◯◯ |
| Side effects: eye and mouth swelling, stomach cramps, fatigue, irritability (diary record) Follow‐up: 3 months | 38 per 1000 | 79 per 1000 (20 to 271) | OR 2.15 (0.5 to 9.31) | 68 (2 RCTs) | ⨁⨁◯◯ |
| Tolfenamic acid vs placebo | |||||
| Menstrual blood loss Menstruation "more abundant than normal" (questionnaire) Follow‐up: 3 months | 658 per 1000 | 510 per 1000 | OR 0.54 | 310 | ⨁◯◯◯ |
| Side effects: dyspepsia, diarrhoea, headache, fatigue (questionnaire) Follow‐up: 3 months | 129 per 1000 | 66 per 1000 | OR 0.48 | ⨁◯◯◯ | |
| Aspirin vs paracetamol | |||||
| Menstrual blood loss (alkaline hematin method) Follow‐up: 3 cycles | The mean menstrual blood loss was 49.5 mL | MD 0.3mL lower | ‐ | 20 | ⨁◯◯◯ |
| Adverse events or side effects | Not reported | ||||
| 2 g tranexamic acid vs 1 g tranexamic acid | |||||
| Menstrual blood loss % occurrence of heavy menstrual bleeding (alkaline hematin method) Follow‐up: each cycle for 3 menstrual cycles | 2 g tranexamic acid: 20 1 g tranexamic acid: 11.76 | 64 | ⨁◯◯◯ | ||
| Menstrual blood loss % occurrence heavy menstrual bleeding (PBAC score) Follow‐up: each cycle for 3 menstrual cycles | 2 g tranexamic acid: 26.79 1 g tranexamic acid: 45.83 | 175 | ⨁◯◯◯ | ||
| Adverse events or side effects | Not reported | ||||
| CI: confidence interval; MD: mean difference; OR: odds ratio; PBAC: pictorial blood assessment chart; RCT: randomized controlled trial; vs: versus aDowngraded one level due to unclear risk of selection and reporting bias. | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Ulipristal acetate vs placebo | |||||
| Percentage days bleeding or spotting (questionnaire) Follow‐up: 1, 3 and 6 months after IUD insertion | The mean percentage days bleeding or spotting was 20.7 | MD 9.5% higher (1.48 higher to 17.52 higher) | ‐ | 118 | ⨁⨁◯◯ |
| Adverse events or side effects | Not reported | ||||
| Tranexamic acid vs mefenamic acid | |||||
| Menstrual blood loss | No data reported | ||||
| Duration of bleeding Median number of bleed days (diary) Follow‐up: 90 days of study assessment followed by 30 days | Tranexamic acid: 8 Mefenamic acid: 10 | 168 | ⨁⨁◯◯ | ||
| Side effects: gastrointestinal disorders, headache, breast tenderness, musculoskeletal disorders Follow‐up: 90 days of study assessment followed by 30 days | 468 per 1000 | 468 per 1000 | OR 1.00 (0.49 to 2.02) | 168 | ⨁⨁◯◯ |
| Mifepristone vs vitamin B | |||||
| Menstrual blood loss | No data reported | ||||
| Duration of bleeding % spotting and bleeding days Follow‐up: 1, 3 and 6 months after IUD insertion | Mifepristone: fewer women reported bleeding or spotting. Fewer days with normal or heavy intensity bleeding Vitamin B: more bleeding or spotting days | 58 | ⨁◯◯◯ | ||
| Adverse events or side effects | Not reported | ||||
| Naproxen vs estradiol | |||||
| Menstrual blood loss | Not reported | ||||
| Duration of bleeding Median number of bleeding and spotting days (diary) Follow‐up: every 4 weeks for 16 weeks | Naproxen: 27.5 Estradiol: 44 | 106 | ⨁◯◯◯ | ||
| Side effects: gastroesophageal reflux Follow‐up: every 4 weeks for 16 weeks | 0 per 1000 | 0 per 1000 | OR 3.22 (0.13 to 81.19) | 86 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded one level for imprecision as effects were measured from one trial. | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Ibuprofen vs placebo | |||||
| Reduction in painful menstruation Follow‐up: end of 1st, 2nd and 3rd months | 200 per 1000 | 200 per 1000 | OR 1.00 | 20 | ⨁⨁◯◯ |
| Tolfenamic acid vs placebo | |||||
| Menstruation "more painful than normal" Follow‐up: 3 months | 387 per 1000 | 310 per 1000 | OR 0.71 | 310 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded one level due to unclear risk of selection and reporting bias. | |||||
Background
The intrauterine device (IUD) is one of the most commonly used methods of reversible contraception worldwide, accounting for 17% of contraceptive use. In 2019, it was used by 159 million women worldwide, up from 133 million women in 1994 (United Nations 2019). The estimated prevalence of IUD use among women of reproductive age (15 to 49 years) in 2019 was 10.7% in Asia, 8.1% in Europe and 4.6% in Latin America and the Caribbean. The highest prevalence of IUD use in 2019 is in the Democratic People’s Republic of Korea (46.9%) and Uzbekistan (36.9%). Among women of reproductive age, IUDs are used by 151 million married women (20%) in contrast to eight million (6%) unmarried women (United Nations 2019).
Two types of IUD are commonly available: copper‐containing IUDs (Cu IUD) and levonorgestrel‐releasing IUDs (LNG IUD). Adolescent and adult women who desire a highly effective contraceptive method, which is long term and reversible, are eligible for IUD use (Francis 2017). IUD use has no restrictions for women who may have co‐morbidities including but not limited to benign ovarian tumours, breast disease, cervical cancer, cirrhosis, history of deep vein thrombosis, diabetes mellitus, epilepsy, migraine, hypertension, ischaemic heart disease, inflammatory bowel disease, multiple sclerosis, obesity, ovarian cancer, active smoking, thyroid disorders, tuberculosis and valvular heart disease (Gaffield 2016; Tepper 2016).
Benefits of IUDs include highly effective pregnancy prevention. IUDs are long‐acting and rapidly reversible, with few side effects, few contraindications, reduced risk of cervical and ovarian cancer and do not require regular adherence to maintain their effectiveness (Cortessis 2017; Heinemann 2015; WHO 2015). However, despite their many benefits, IUD use is also associated with side effects such as heavier menstrual bleeding, prolonged or unscheduled bleeding, spotting, amenorrhoea and cramping (Bayer 2017). These side effects contribute to fear among women wanting to initiate IUD use as well as discontinuation among existing IUD users, as these effects are disturbing and affect quality of life (Diedrich 2015).
Description of the condition
Use of IUDs is associated with heavy menstrual bleeding and pain and these are the most commonly reported reasons for IUD removal within the first six months after insertion (Grunloh 2013). Heavy menstrual bleeding is defined based on a woman’s perception of increased daily or total menstrual volume or flow regardless of the duration, frequency and regularity (NICE 2018). This definition is subjective but a volume that impedes a woman’s physical, social, emotional or material quality of life is truly heavy.
Previously, heavy menstrual bleeding was defined as a menstrual blood loss of more than 80 mL. However, in 2011, the International Federation of Gynaecology and Obstetrics (FIGO) developed new definitions and terminology for abnormal uterine bleeding symptoms as well as a new classification of underlying causes of abnormal uterine bleeding in the reproductive years (Munro 2011).
Normal menstruation is defined as a frequency of 24 to 38 days, regularity of seven to nine days or less, duration of eight days or less and a subjective clinical definition of volume, which does not interfere with a woman’s physical, social, emotional or material quality of life. Research definition for normal volume is 80 mL vaginal blood loss per cycle or less. Any symptomatic variation from normal menstruation is thus, abnormal uterine bleeding (Munro 2011; NICE 2018).
Heavy menstrual bleeding can be specified more objectively for research reasons by direct or indirect methods for determining menstrual blood loss. The volumetric description of heavy menstrual bleeding is less than 80 mL per cycle and can be assessed using the alkaline hematin method from menstrual sanitary pads and tampons after careful collection or a semi‐quantitative method using pictorial blood loss assessment charts (PBAC; Hallberg 1964; Higham 1990; Newton 1977).
Description of the intervention
Several interventions have been studied for the treatment of heavy menstrual bleeding and pain associated with IUD use, among which are nonsteroidal anti‐inflammatory drugs (NSAIDs), such as mefenamic acid; naproxen; indomethacin; aspirin; and antifibrinolytics, such as tranexamic acid. Other interventions studied include hormones such as desmopressin and estradiol, vitamins, flavonoids, paracetamol, and alternative therapies.
How the intervention might work
Increased fibrinolytic activity and increased prostaglandin release play a role in bleeding and pain associated with Cu IUD use (Godfrey 2013; Ylikorkala 1994). Endometrial concentrations of some prostaglandin metabolites correlate with measured blood loss in Cu IUD users (Ylikorkala 1994). As for LNG IUD, it has been hypothesized that progesterone causes increased fragility of the superficial vessels of the endometrium as well as endometrial atrophy (Hickey 2002).
NSAIDs act as inhibitors of prostaglandin synthetase and decrease the release of endometrial prostaglandin, while tranexamic acid exerts its antifibrinolytic effect by inhibiting the endometrial plasminogen activator, preventing fibrinolysis and the breakdown of clots (Alanwar 2018; Saharkhiz 2017). NSAIDs and fibrinolytic agent such as tranexamic acid have been recommended by the World Health Organization's (WHO) Selected Practice Recommendations for Contraceptive Use as possible treatments for heavy menstrual bleeding among Cu IUD users (WHO 2015).
Flavonoids have been shown to inhibit the release of the inflammatory mediators prostaglandin E2, prostaglandin F2a, thromboxane A2 and prostacyclin and thus reduce capillary hyper‐fragility, increase lymphatic drainage, normalize capillary permeability and strengthen capillary resistance (Lyseng‐Williamson 2003; Manthey 2000). These mechanisms of action are thought to reduce heavy menstrual bleeding and pain associated with Cu and LNG IUD use.
Why it is important to do this review
IUD users give the reasons for discontinuation of IUD use as heavy menstrual bleeding and pain associated with IUDs. The discontinuation of IUD use due to pain was 28% (LNG IUD) to 35% (Cu IUD), while due to heavy bleeding it was 9% (LNG IUD) and 19% (Cu IUD) (Grunloh 2013). This percentage is large and in turn affects many women, given the current use of IUDs worldwide (159 million women; United Nations 2019). As IUDs are highly effective, safe, cost‐effective and well tolerated by most women, strategies to treat and prevent heavy menstrual bleeding and pain associated with its use should be sought to ensure uptake of this contraceptive method and reduce discontinuation rates.
Objectives
To evaluate all randomized controlled trials (RCTs) that have assessed strategies for treatment and prevention of heavy menstrual bleeding or pain associated with IUD use, for example, pharmacotherapy and alternative therapies.
Methods
Criteria for considering studies for this review
Types of studies
We included all RCTs in any language that compared any intervention for treating heavy menstrual bleeding or pain associated with any IUD use. We excluded cohort trials and before‐after trials. Interventions for pain during IUD insertion have been examined in another Cochrane Review (Lopez 2015). The intervention could be compared with no intervention, placebo or another active intervention. We excluded pathological causes of heavy menstrual bleeding and post‐menopausal bleeding.
Types of participants
We included women of reproductive age (15 to 49 years) of any gravidity and parity who were using an IUD for contraception.
Types of interventions
We included any pharmacological or other interventions used either for the treatment or the prevention of heavy menstrual bleeding or pain, or both, associated with IUD use. Comparisons included placebo, no intervention or another active intervention. Types of intervention may include NSAIDs, antifibrinolytics, hormones, other drugs or complementary alternative therapies.
Types of outcome measures
Primary outcomes
We searched the Core Outcome Measures in Effectiveness Trials (COMET) database (www.comet-initiative.org), to see if a core outcome set had been developed for the outcomes in heavy menstrual bleeding. We found one ongoing trial in the Core Outcomes in Women’s and Newborn health (CROWN) initiative (www.comet-initiative.org/Studies/Details/789). Therefore, after discussion between the review authors, we have chosen the primary and secondary outcomes below.
-
Volume of menstrual blood loss: outcome measures for bleeding included quantitative measurements of blood loss (Hallberg 1964), semi‐quantitative assessments of blood loss by PBAC scores (Higham 1990; Reid 2000), or IUD discontinuation (Hubacher 2006) and number of sanitary pads used for bleeding. Participant perceptions of bleeding being more abundant than usual using categorical scales or menstrual diary cards could also be included.
-
Duration of bleeding: duration of bleeding in number of bleeding or spotting days
-
Painful menstruation: level of pain could be reported on Likert scales, pain scores, qualitatively or any pain reduction
Secondary outcomes
-
IUD removal
-
Haemoglobin levels
-
Need for additional analgesia
-
Quality of life measured by any validated scales
-
Side effects and adverse events
Search methods for identification of studies
The Cochrane Fertility Regulation Information Specialist conducted a search for all published, unpublished, and ongoing trials, without restrictions on language or publication status till 28 January 2021. The search strategies for each database were modelled on the search strategy designed for MEDLINE Ovid (Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations and Daily), available in Appendix 1.
Electronic searches
We searched the following databases from their inception.
-
EBM Reviews Ovid (1974 to 28 January 2021)
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 12)
-
MEDLINE Ovid (Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations and Daily) (1946 to 28 January 2021)
-
Embase.com (1974 to 28 January 2021)
-
CINAHL (1982 to 28 January 2021)
-
LILACs lilacs.bvsalud.org/en/ (1982 to 28 January 2021)
-
Global Health Ovid (inception to 28 January 2021)
-
Scopus (inception to 28 January 2021)
We searched the following trials registries:
-
The World Health Organization International Clinical Trials Registry Platform (www.who.int/trialsearch) (up to 28 January 2021)
-
ClinicalTrials.gov (www.clinicaltrials.gov) (up to 28 January 2021)
We searched the following grey literature sites:
-
Guttmacher Institute (www.guttmacher.org/united-states/abortion) (up to 28 January 2021)
-
International Planned Parenthood Federation (www.ippf.org/) (up to 28 January 2021)
-
Ibis Reproductive Health (ibisreproductivehealth.org/) (up to 28 January 2021)
-
Women on Waves (www.womenonwaves.org/) (up to 28 January 2021)
-
Marie Stopes International (www.mariestopes.org/) (up to 28 January 2021)
-
Population Council (www.popcouncil.org/) (up to 28 January 2021)
-
Population Services International (www.psi.org/) (up to 28 January 2021)
-
Ipas (www.ipas.org/) (up to 28 January 2021)
Searching other resources
We checked the bibliographies of included trials and any relevant systematic reviews identified for further references to relevant trials. We contacted experts and organizations in the field to obtain additional information on relevant trials. We wrote to authors of published trial reports to solicit other published or unpublished trials that we may have missed. We also contacted trial report authors as needed to supplement published information.
Data collection and analysis
For this update, we applied the techniques below to evaluate the reports that we discovered as a result of the updated search, and we went back over the trial reports in the 2011 publication to assign them to the proper comparison and to revise their risk of bias.
Selection of studies
Two review authors independently assessed and abstracted data from the trials identified to improve accuracy. We resolved any discrepancies or disagreements through discussion or by involving a third review author if needed.
Data extraction and management
Two review authors extracted the data for the eligible trials. We solved inconsistencies through discussion or, if necessary, we sought advice from the third review author. We entered data into Review Manager 5 software (Review Manager 2020), and checked accuracy. When any information was doubtful, we tried to contact authors of the original reports for further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each trial using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). We resolved any disagreement by discussion, or by involving a third review author. The biases related to this review were: selection bias (random sequence generation; allocation concealment); performance bias (blinding of participants and personnel); detection bias (blinding of outcome assessors); attrition bias (incomplete outcome data); reporting bias (selective reporting); and other forms of bias (such as baseline imbalance, selective reporting of subgroups, or potential influence from funders). Conclusions were assigned to each of these domains (Higgins 2017). We graded each risk of bias domain as 'low', 'unclear' or 'high', We described all judgements fully and presented the conclusions in the Risk of bias in included studies. We assessed the likely magnitude and direction of the bias and whether it was likely to impact the findings. We explored impact of bias by performing sensitivity analysis. We also noted funding source for trials and declaration of interest by trial authors.
Measures of treatment effect
For continuous variables, we computed the mean difference (MD) with 95% confidence interval (CI). We used standardized mean difference (SMD) if trials in the meta‐analysis used different measurement scales. We would interpret SMD as 0.2 small effect, 0.5 moderate effect and 0.8 a large effect (Cohen 1988). For dichotomous outcomes, we calculated odds ratio (OR) with 95% CI. We used a random‐effects model in meta‐analysis. We presented data as provided by the trial authors, for trials that reported in medians, ranges and percentages.
Unit of analysis issues
We checked included trials for unit of analysis errors, and we did not encounter any of these. If we had encountered any cluster‐RCTs we intended to adjust the results from trials showing unit of analysis errors based on the mean cluster size and intra‐cluster correlation coefficient (Higgins 2021a).
Dealing with missing data
For included trials, we noted levels of attrition. We had proposed to investigate the influence of including trials with high levels of missing data in the whole assessment of treatment effect by using sensitivity analysis.
For all outcomes, we conducted analyses, as far as feasible, on an intention‐to‐treat basis.
Assessment of heterogeneity
We deemed whether the clinical and methodological qualities of the included trials were adequately similar for meta‐analysis to provide a meaningful summary. Where we were able to carry out meta‐analyses, we checked for heterogeneity by visually inspecting the forest plots for evidence of poor overlap of the 95% CIs. More accurately, we used the Chi2 test (with a P value less than 0.10 being evidence of significance) and the I2 statistic value (Higgins 2003). The Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2021), suggested a rough guide for interpretation of I2 statistic values:
-
0% to 40% might not be important;
-
30% to 60% may represent moderate heterogeneity;
-
50% to 90% may represent substantial heterogeneity;
-
75% to 100% was considerable heterogeneity.
Where we found substantial heterogeneity (I2 statistic > 50%), we aimed to look at possible sources involving variations in trial quality, inclusion criteria or intervention regimes among trials.
Assessment of reporting biases
We aimed to minimize the likelihood of reporting bias by conducting a comprehensive search for eligible trials with no restriction to language or publication status and by being alert to duplication of data. Despite these efforts, it is still possible that we may have missed some trials, so our conclusions should be interpreted with some caution. If we found 10 or more trials for the primary outcomes, we planned to use a funnel plot to explore the possibility of small‐trial effects.
Data synthesis
We carried out statistical analysis using Review Manager 5 software (Review Manager 2020). We applied a random‐effects model in meta‐analysis for merging data as we believed it was acceptable to presume that there was clinical heterogeneity due to the huge difference in the type of intervention used (Deeks 2021). There was also variation in the subjective assessment of volume of menstrual blood loss and level of pain. These variations directed us to believe that the underlying treatment effects would differ between trials. Cross‐over trials are a suitable design to evaluate stable, chronic conditions (Higgins 2021b). We therefore anticipated trials with cross‐over design in this review, as bleeding or pain associated with IUD use is a recurrent condition. However, to date, the reporting of cross‐over trials is variable, and the data needed to include a paired analysis in a meta‐analysis is often unpublished. We made an a priori decision to include only data from the first period if available and to report the rest of the cross‐over data in the review.
Subgroup analysis and investigation of heterogeneity
Where data were available, we planned to undertake subgroup analyses according to type and dose of interventions. However, there were insufficient trials to undertake subgroup analyses.
Sensitivity analysis
Akin to the previous review, we did not perform sensitivity analyses due to the inability to aggregate the included trials. We intended to do sensitivity analysis when there was high risk of bias for sequence generation and allocation concealment of included trials. Future updates may undertake this analysis if there are an adequate number of relevant trials.
Summary of findings and assessment of the certainty of the evidence
Assessing the certainty of evidence using the GRADE approach
We used the GRADE approach to assess the certainty of the body of evidence for this update, relating to the following outcomes for the main comparisons.
-
Menstrual blood loss
-
Duration of bleeding
-
Level of pain
We used the GRADEPro GDT development tool (GRADEpro GDT), to import data from Review Manager 5 (Review Manager 2020), to create the summary of findings tables. Using the GRADE approach, we generated a summary of the intervention effect and measure of certainty for each of the above outcomes.
The GRADE approach uses five considerations (trial limitations, consistency of effect, indirectness, imprecision and publication bias) to assess the certainty of the body of evidence for each outcome. We downgraded the evidence from 'high certainty' by one level for serious (or by two levels for very serious) weaknesses, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; Characteristics of ongoing studies; Table 1; Table 2.
| Trial | Experimental Intervention | Comparison Intervention | IUD type | Duration of intervention | Follow‐up | Outcome |
|---|---|---|---|---|---|---|
| Effectiveness trials | ||||||
| Bleeding trials | ||||||
| RCT with cross‐over | Oral naproxen 1250 mg/day | Oral naproxen 500 mg on 1st day then 750 mg on subsequent days Placebo | Unknown | 4 cycles Each participant took 2 of the 3 treatments, each for 2 menstrual cycles. Each regimen was begun on the 1st day of menstrual bleeding and continued for a total of 5 days. | After every 2 menstrual cycles | Percentage reduction in menstrual blood loss |
| RCT | Oral ulipristal acetate 5 mg/day for 5 days | Oral placebo | LNG IUD | 5 days, bleeding was assessed at 30 days, 60 days and 70 days | 90 days | Total bleeding days |
| RCT | Oral vitamin B1 100 mg/day during the 2nd, 3rd and 4th months following insertion of the IUD | Oral placebo during the 2nd, 3rd and 4th months following insertion of the IUD | Cu IUD | 3 cycles | 1 month after completion of intervention | Number of pads used Number of spotting days Duration of bleeding |
| Pain trials | ||||||
| RCT | Oral naproxen sodium 550 mg initially, then 275 mg every 6 hours as needed for uterine pain | Placebo (lactose) | Unknown IUD type | 3 cycles | No details | Overall and daily pain relief score (6‐point Likert scale) |
| RCT with cross‐over | Oral naproxen 500 mg followed by 250 mg 2‐4 times a day, with a maximum of 1250 mg, taken at the first sign of menstrual distress. | Oral placebo taken at the first sign of menstrual distress. | Cu IUD | 4 cycles Participant took an intervention for 2 cycles then crossed over to the other intervention for 2 cycles | After 2nd and 4th menstrual cycle | Pain relief (5‐point Likert scale) |
| Comparative effectiveness trials | ||||||
| Bleeding trials | ||||||
| RCT | Oral tranexamic acid 500 mg, 1 tablet 6‐hourly during the 1st 3 days of menstrual bleeding | Oral micronized flavonoid 500 mg, 1 tablet 6‐hourly during the 1st 3 days of menstrual bleeding | Cu IUD | 3 cycles | No details | PBAC score Number of pads used/day Number of bleeding days |
| RCT | Oral mefenamic acid, 250 mg; 1 capsule every 8 hours on the first 3 days of menstruation | Oral tranexamic acid, 250 mg; 1 capsule every 8 hours on the first 3 days of menstruation | Cu IUD | 2 cycles | No details | PBAC score Number of bleeding days |
| RCT | Desmopressin 300 mcg intranasal spray each morning for the first 5 days after start of menstruation | Oral mefenamic acid 1500 mg/day for the first 5 days after the start of menstruation. | Cu IUD | 3 months | Monthly for 3 months | PBAC score |
| RCT | Oral tranexamic acid 500 mg 3 times/day for 3‐5 days based on the duration of bleeding | Oral mefenamic acid 500 mg 3 times/day for 3‐5 days based on the duration of bleeding | Cu IUD | 3 months | Monthly for 3 months | Volume of blood loss Duration of bleeding |
| RCT | Oral mefenamic acid 250 mg 3 times/day from the 1st day of menstruation until day 8 | Oral Vitex agnus 3 times/day from the 1st day of menstruation until day 8 | Unknown IUD type | 4 months | No details | PBAC score |
| RCT with cross‐over | Oral tranexamic acid 4.5 g/day for 5 days | Oral sodium diclofenac 150 mg on day 1 then 75 mg/day on days 2‐4 Placebo | Cu IUD | 5 months Each participant received placebo for 1 month, 2 months of tranexamic acid, and 2 months of sodium diclofenac | No details | Menstrual blood loss (alkaline hematin) Duration of bleeding |
| Cu IUD: copper intrauterine device; HMB: heavy menstrual bleeding; IUD: intrauterine device; LNG IUD: levonorgestrel intrauterine device; PBAC: pictorial blood loss assessment chart | ||||||
| Trial | Experimental intervention | Comparison intervention | IUD type | Duration of intervention | Follow‐up | Outcomes |
|---|---|---|---|---|---|---|
| Effectiveness trials | ||||||
| Bleeding trials | ||||||
| RCT | Oral ibuprofen 1200 mg/day at the beginning of menstruation and to continue to end of bleeding for a maximum of 10 days. | Oral placebo at the beginning of menstruation and to continue to end of bleeding for a maximum of 10 days. | Cu IUD | 3 cycles | No details | Menstrual blood loss (alkaline hematin) Length of menstruation |
| RCT with cross‐over | Oral ibuprofen 1600 mg/day starting with bleeding and continuing until end of bleeding or maximum of 7 days | Placebo starting with bleeding and continuing until end of bleeding or maximum of 7 days | Cu IUD Cu Lippes loop | 3 cycles Each participant had 1 month of observation, 1 month on ibuprofen or placebo, and 1 month crossed over to the alternative treatment. | End of month 1, 2, 3 | Menstrual blood loss (alkaline hematin) |
| RCT | Oral CDB‐2914 50 mg/day | Oral placebo | LNG IUD | Intervention taken for 3 consecutive days with separate treatments starting 21, 49 and 77 days after LNG IUD insertion | 1,3 and 6 months after IUD insertion | Percentage days bleeding/ spotting, removal of LNG IUD within 6 months; the longest run of amenorrhoea in the 64 days after third treatment, side effects |
| Bleeding and pain trials | ||||||
| RCT | Oral ibuprofen 1200 mg/day to be taken with the first 6 menstruations after IUD insertion and for a maximum of 5 days at a time. | Oral placebo to be taken with the first 6 menstruations after IUD insertion and for a maximum of 5 days at a time. | Cu IUD | 6 cycles | 6, 13, 26 and 52 weeks after IUD insertion | IUD removal within 12 months of insertion due to HMB/pain |
| RCT | Oral tolfenamic acid 600 mg/day starting at IUD insertion and continuing for 7 days; this was to be repeated during the next 3 menstruations. | Placebo starting at IUD insertion and continuing for 7 days; this was to be repeated during the next 3 menstruations | Cu IUD | 3 cycles | No details | Number of pads used, menstruation more abundant than normal, clots, menstruation more painful than normal |
| Comparative effectiveness trials | ||||||
| Bleeding trials | ||||||
| RCT with cross‐over | Oral aspirin 1500 mg/day | Oral paracetamol 1500 mg/day Placebo | Cu IUD | 3 cycles Interventions taken on day 1 of menstruation and continued for the duration of bleeding. Each participant received each treatment in alternating order. | No details | Menstrual blood loss (alkaline hematin) |
| RCT | Oral tranexamic acid 2 g/day, taken for the 1st 5 days of 3 consecutive cycles after IUD insertion | Oral tranexamic acid 1 g/day, taken for the 1st 5 days of 3 consecutive cycles after IUD insertion | Cu IUD | 3 cycles | No details | Percentage occurrence of HMB by alkaline hematin and PBAC |
| RCT | Oral naproxen 500 mg twice a day first 5 days of a 4‐week period | Transdermal estradiol 0.1 mg on day after insertion of IUD, changing it weekly Oral placebo twice a day | LNG IUD | First 12 weeks of IUD use | Telephone surveys at 4, 8, and 16 weeks and an in‐person follow‐up visit at 12 weeks | Median bleed days, patient satisfaction, continuation rates of IUD |
| RCT | Oral 50 mg mifepristone every other day starting on the 1st day of the menstrual cycle for the pre‐treatment period | Oral vitamin B every other day starting on the 1st day of the menstrual cycle for the pre‐treatment period | LNG IUD | 2 months (corresponding to 2 menstrual cycles i.e. 2 × 28 days) prior to insertion and until 3 days (± 2 days) following the LNG IUD insertion | Monthly for the first 3 months, 6 months post‐LNG IUD insertion and 12 months end‐of‐trial evaluation | Bleeding and spotting days |
| RCT | Oral tranexamic acid 1500 mg/day, taken on the 1st day of a bleeding or spotting episode until bleeding or spotting stopped | Oral mefenamic acid 1500 mg/day, taken on the 1st day of a bleeding or spotting episode until bleeding or spotting stopped Oral placebo (lactose and magnesium stearate), taken on the 1st day of a bleeding or spotting episode until bleeding or spotting stopped | LNG IUD | 90 days | No details | Median reduction of bleed days and length of bleed days, satisfaction with drug/placebo, occurrence of pain, number of days pain medication used to alleviate pain, adverse effects |
| Cu IUD: copper intrauterine device; HMB: heavy menstrual bleeding; IUD: intrauterine device; LNG IUD: levonorgestrel intrauterine device; PBAC: pictorial blood loss assessment chart | ||||||
Results of the search
For this update, we retrieved 591 records from the search conducted in January 2021.
We also re‐examined trials from the previous version of the review (Grimes 2006): there were 15 included trials, 10 excluded trials, and two ongoing trials.
We excluded 11 trials (Figure 1). Eight trials were awaiting classification due to inability to retrieve full texts; six from the previous review (Di Lieto 1987; Jensen 1998; Massey 1974; Toppozada 1982; Wu 2000; Yarkoni 1984), and two from our new search (Bayer 2013; Wang 2013). There were no ongoing trials.
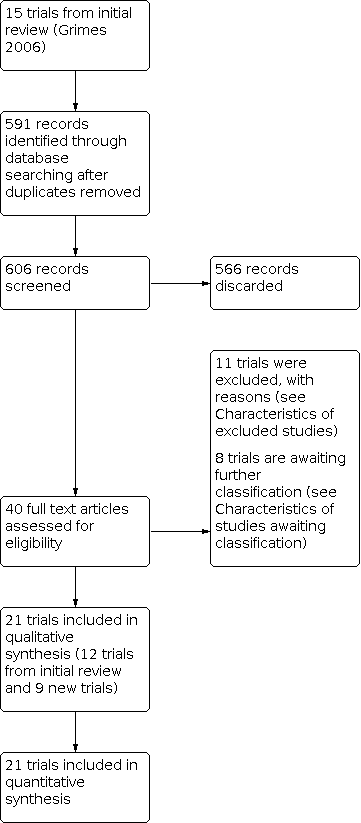
Trial flow diagram
Included studies
This update includes 21 trials with a total of 3689 participants. Of those, 11 trials were included in the previous review (Buttram 1979; Davies 1981; Hahn 1979; Hubacher 2006; Lalos 1983; Lin 2007; Mercorio 2003; Roy 1981; Warner 2010; Ylikorkala 1978; Ylikorkala 1983). One trial was excluded from the previous review (Makarainen 1986), and we included nine new trials from the updated search (Alanwar 2018; Fava 2020; Jafari 2014; Kaviani 2013; Madden 2012; Papaikonomou 2018; Saharkhiz 2017; Sordal 2013; Yavarikia 2013). See Figure 1 for the PRISMA flow diagram (Page 2021).
Of the 20 included trials, five trials with a total of 104 participants were randomized controlled trials (RCTs) with cross‐over design (Davies 1981; Hahn 1979; Lalos 1983; Roy 1981; Ylikorkala 1983). The number of participants in each trial ranged from 19 to 2019. The 20 trials were undertaken in 10 countries. Four trials were conducted in Iran (Jafari 2014; Kaviani 2013; Saharkhiz 2017; Yavarikia 2013), three in the USA (Buttram 1979; Madden 2012; Roy 1981), three in Sweden (Hahn 1979; Lalos 1983; Papaikonomou 2018), three in Finland (Makarainen 1986; Ylikorkala 1978; Ylikorkala 1983), two in the UK (Davies 1981; Warner 2010), one in Egypt (Alanwar 2018), one in Chile (Hubacher 2006), one in China (Lin 2007), one in Brazil (Fava 2020) and one in Italy (Mercorio 2003). One trial (Sordal 2013), involved three countries, which were Denmark, Ireland and Norway. Six trials were multi‐centre trials (Hubacher 2006; Jafari 2014; Kaviani 2013; Lin 2007; Saharkhiz 2017; Sordal 2013).
Participants’ age ranged from 15 to 49 years old. Cu IUD was used by participants in 12 trials (Alanwar 2018; Hahn 1979; Hubacher 2006; Jafari 2014; Kaviani 2013; Lalos 1983; Lin 2007; Makarainen 1986; Mercorio 2003; Saharkhiz 2017; Ylikorkala 1978; Ylikorkala 1983), Cu IUD and Lippes Loop in one trial (Roy 1981), and LNG IUD in five trials (Fava 2020; Madden 2012; Papaikonomou 2018; Sordal 2013; Warner 2010). Three trials did not state the type of IUD used (Buttram 1979; Davies 1981; Yavarikia 2013). See Characteristics of included studies.
Treatment trials
Seven trials were among Cu IUD users. There were two effectiveness trials (Jafari 2014; Lalos 1983), and five comparative effectiveness trials (Alanwar 2018; Kaviani 2013; Mercorio 2003; Saharkhiz 2017; Ylikorkala 1983). Five trials focused on the treatment of heavy menstrual bleeding associated with IUD use (Alanwar 2018; Jafari 2014; Kaviani 2013; Mercorio 2003; Saharkhiz 2017), one trial on the treatment of pain associated with IUD use (Lalos 1983), and one trial on treatment of pain and bleeding associated with IUD use (Ylikorkala 1983).
LNG IUD was used in one treatment of bleeding effectiveness trial (Fava 2020). Details are in Characteristics of included studies.
The IUD type was uncertain in two treatment of bleeding effectiveness trials (Davies 1981; Yavarikia 2013), and one treatment of pain comparative effectiveness trial (Buttram 1979).
Table 1 summarizes the experimental and comparison interventions for the treatment trials. Additional details are given in Characteristics of included studies.
The following are the interventions for the treatment of bleeding and pain.
Cu IUD
-
Treatment of heavy menstrual bleeding
-
Vitamin B1 versus placebo
-
Naproxen versus placebo
-
Mefenamic acid versus tranexamic acid
-
Mefenamic acid versus desmopressin
-
Tranexamic acid versus diclofenac
-
Tranexamic acid versus flavonoids
-
Tranexamic acid versus active comparators (mefenamic acid, flavonoids, diclofenac)
-
-
Treatment of pain
-
Tranexamic acid versus diclofenac
-
LNG IUD
-
Treatment of heavy menstrual bleeding
-
Ulipristal versus placebo
-
-
Treatment of pain ‐ none
Unknown IUD type
-
Treatment of heavy menstrual bleeding
-
Higher dose versus lower dose naproxen
-
Mefenamic acid versus Vitex agnus
-
-
Treatment of pain
-
Naproxen versus placebo
-
Treatment of heavy bleeding associated with IUD use
Cu IUD
The five treatment of bleeding trials included a total of 544 Cu IUD users, with sample size ranging from 24 to 210 women. The age of the women ranged from 18 to 49 years old.
One trial studied oral vitamin B1 compared to placebo (dried starch; Jafari 2014). The dose of vitamin B was 100 mg per day taken during the second through fourth month of menstruation.
Three trials studied NSAIDs (Kaviani 2013; Mercorio 2003; Saharkhiz 2017). Two trials compared mefenamic acid to tranexamic acid (Kaviani 2013; Saharkhiz 2017). The dose of mefenamic acid used was 750 mg per day in comparison tranexamic acid 750 mg per day for the first three days of menstruation for a total of two menstrual cycles (Kaviani 2013), while the other trial used 1500 mg mefenamic acid compared to 1500 mg tranexamic acid for three to five days, depending on the duration of bleeding, for three cycles (Saharkhiz 2017). An Italian RCT compared oral mefenamic acid 1500 mg per day to intranasal desmopressin 300 mcg per day for the first five days of menstruation for a duration of three cycles (Mercorio 2003).
One trial studied oral tranexamic acid at a dose of 2 g per day compared to oral flavonoids at a dose of 2 g per day, taken on the first three days of menstruation for duration of three cycles (Alanwar 2018).
Five trials assessed menstrual blood loss by applying PBAC (Alanwar 2018; Jafari 2014; Kaviani 2013; Mercorio 2003). One trial (Saharkhiz 2017), evaluated menstrual blood loss using a different pictorial chart, where each pad was perceived as lightly (10 mL), mildly (20 mL), moderately (30 mL), or completely saturated (40 mL).
LNG IUD
One trial among 30 LNG IUD users compared 5 mg oral ulipristal acetate per day, taken for five days, to oral placebo (Fava 2020). Duration of bleeding was reported as the number of days until bleeding stopped as well as the number of bleeding days in 90 days.
Unknown IUD type
One trial compared naproxen sodium at 1250 mg to 500 mg on the first day then 750 mg on subsequent days or placebo on day one to five of menstruation, for a total of two menstrual cycles per intervention (Davies 1981). No method of blood loss quantification was reported.
Another trial compared oral mefenamic acid 750 mg per day to oral Vitex agnus 750 mg per day for the first eight days of menstruation for a duration of four months (Yavarikia 2013). Blood loss was assessed using a PBAC.
Treatment of pain associated with IUD use
Cu IUD
One trial involving 21 Cu IUD users examined the use of naproxen sodium against placebo for the treatment of pain (Lalos 1983). This trial was a cross‐over design that compared oral naproxen at a dose of 500 mg initially followed by 250 mg two to four times per day as needed for two cycles followed by placebo for two cycles or vice versa. Pain was assessed using a Likert scale with scale of five being excellent relief and scale of one being worst pain.
Unknown IUD type
One trial with an unknown IUD type randomized 35 women to receive either naproxen sodium (550 mg initially, then 275 mg every six hours as needed) versus a placebo (lactose) for three consecutive menstrual cycles (Buttram 1979). Pain was assessed by a self‐administered six‐point Likert scale with 6 being excellent relief and 1 being no relief.
Treatment of bleeding and pain associated with IUD use
Cu IUD
One trial assessed treatment of heavy menstrual bleeding and pain associated with IUD use (Ylikorkala 1983). The trial consisted of 19 women on Cu IUD, studied during five cycles. In randomized order, they received for two cycles oral tranexamic acid, 1.5 g three times daily for five days; in another two cycles they received sodium diclofenac, 50 mg three times daily on the first day followed by 25 mg three times daily for four days and placebo for five days in another cycle. Ylikorkala 1983 assessed menstrual blood loss using the alkaline hematin method, but did not describe the method for pain assessment.
Prevention trials
There were 10 prevention trials (Hahn 1979; Hubacher 2006; Lin 2007; Madden 2012; Makarainen 1986; Papaikonomou 2018; Roy 1981; Sordal 2013; Warner 2010; Ylikorkala 1978). Six were effectiveness trials, while four were comparative effectiveness, as detailed below (see Characteristics of included studies and Table 2).
Four trials in women with Cu IUD were effectiveness trials (Hubacher 2006; Makarainen 1986; Roy 1981; Ylikorkala 1978), while two were comparative effectiveness trial (Hahn 1979; Lin 2007). Three trials examined prevention of heavy menstrual bleeding associated with Cu IUD (Hahn 1979; Lin 2007; Makarainen 1986), while another three trials looked at the prevention of both bleeding and pain (Hubacher 2006; Roy 1981; Ylikorkala 1978).
Four trials assessed the prevention of bleeding associated with LNG IUD use (Madden 2012; Papaikonomou 2018; Sordal 2013; Warner 2010). Only one was an effectiveness trial (Warner 2010).
Table 2 summarizes the experimental and comparison interventions for the 10 prevention trials. Additional details are given in Characteristics of included studies.
Prevention of pain ‐ There were 11 treatment trials. Five were effectiveness trials, while six were comparative effectiveness, as detailed below (see Characteristics of included studies; Table 1)
The following are the interventions for the prevention of bleeding and pain:
Cu IUD
-
Prevention of heavy menstrual bleeding
-
Ibuprofen versus placebo
-
Tolfenamic acid versus placebo
-
Aspirin versus paracetamol
-
2 g tranexamic acid versus 1 g tranexamic acid
-
-
Prevention of pain
-
Ibuprofen versus placebo
-
Tolfenamic acid versus placebo
-
LNG IUD
-
Prevention of heavy menstrual bleeding
-
CDB‐2914 (ulipristal) versus placebo
-
Tranexamic acid versus mefenamic acid
-
Mifepristone versus vitamin B1
-
Naproxen versus estradiol
-
-
Prevention of pain ‐ none
Prevention of heavy menstrual bleeding associated with IUD use
Cu IUD
One trial examined oral ibuprofen (1200 mg per day) against placebo for three cycles (Makarainen 1986), while another trial compared different doses of oral tranexamic acid (2 g per day versus 1 g per day; Lin 2007).
One trial compared aspirin to paracetamol for the prevention of heavy bleeding (Hahn 1979). Aspirin, 1500 mg per day was compared to 1500 mg paracetamol taken from day one of menstruation and continued for the duration of bleeding for a total of three menstrual cycles.
Two trials assessed menstrual blood loss using the alkaline hematin method (Hahn 1979; Makarainen 1986), while another trial utilized a PBAC and the alkaline hematin method (Lin 2007).
LNG IUD
Two trials examined NSAIDs for the prevention of bleeding associated with LNG IUD (Madden 2012; Sordal 2013). One trial compared the use of oral mifepristone, 50 mg every other day, to vitamin B, starting on the first day of the menstrual cycle for the pre‐treatment period until three days (± 2 days) following the LNG IUD insertion (Papaikonomou 2018). One trial compared a selective progesterone receptor modulator, Ulipristal acetate to placebo (Warner 2010). Women were randomized to receive oral ulipristal acetate 50 mg per day or placebo, taken for three consecutive days, with separate treatments starting 21, 49 and 77 days after IUD insertion.
One trial compared oral naproxen 1 g per day for the first five days to transdermal estradiol 0.1 mg weekly or oral placebo (Madden 2012), while the other trial utilized oral tranexamic acid 1500 mg per day against oral mefenamic acid 1500 mg per day and placebo (Sordal 2013). The duration of the intervention in both trials was for three menstrual cycles.
Four trials used diaries to record bleeding days and pattern (Madden 2012; Papaikonomou 2018; Sordal 2013; Warner 2010).
Prevention of bleeding and pain associated with IUD use
Cu IUD
Three trials, with a total of 2199 participants, evaluated prevention of bleeding and pain associated with Cu IUD use (Hubacher 2006; Roy 1981; Ylikorkala 1978). Two trials compared ibuprofen to placebo; Hubacher 2006 utilized oral ibuprofen at a dose of 1200 mg per day and Roy 1981 at a dose of 1600 mg per day. One prevention trial compared oral tolfenamic acid 600 mg to placebo (Ylikorkala 1978).
One trial assessed menstrual blood loss using the alkaline hematin method (Roy 1981). Subjective assessment of pain in diaries (Roy 1981) and bleeding pattern records (Ylikorkala 1978) were reported.
Sources of trial funding
Fifteen trials reported their sources of funding (Fava 2020; Hubacher 2006; Jafari 2014; Kaviani 2013; Lin 2007; Madden 2012; Makarainen 1986; Papaikonomou 2018; Roy 1981; Saharkhiz 2017; Sordal 2013; Warner 2010; Yavarikia 2013; Ylikorkala 1978; Ylikorkala 1983). Four trials received funding from universities (Jafari 2014; Kaviani 2013; Saharkhiz 2017; Yavarikia 2013), four trials were funded by pharmaceutical companies (Lin 2007; Roy 1981; Sordal 2013; Warner 2010), three from government research funding bodies (Hubacher 2006; Papaikonomou 2018; Ylikorkala 1983), and one from a charitable private trust (Ylikorkala 1978). Two trials received funding from both a pharmaceutical company and government research funding body (Madden 2012; Makarainen 1986), and one trial partially from a grant and research council (Fava 2020). Six trials did not report their funding (Alanwar 2018; Buttram 1979; Davies 1981; Hahn 1979; Lalos 1983; Mercorio 2003).
Declaration of interests
Seven trials reported their declaration of interests as ‘none’ (Alanwar 2018; Jafari 2014; Kaviani 2013; Madden 2012; Papaikonomou 2018; Saharkhiz 2017; Yavarikia 2013). One trial (Fava 2020), reported a conflict of interest for being a member of a foundation and receiving honorarium by a pharmaceutical company as a speaker. Thirteen trials did not report on declarations of interest by researchers (Buttram 1979; Davies 1981; Hahn 1979; Hubacher 2006; Lalos 1983; Lin 2007; Makarainen 1986; Mercorio 2003; Roy 1981; Sordal 2013; Warner 2010; Ylikorkala 1978; Ylikorkala 1983). See Characteristics of included studies.
Excluded studies
In this update, we excluded 11 trials for several reasons, including seven trials which were non‐randomized controlled trials (Batar 1978; Dreher 1980; Grunloh 2013; Guillebaud 1978; Hidalgo 2002; Lal 2010; Toppozoda 1987). We excluded four trials as they did not meet the inclusion criteria. Abbas 2018, Baldwin 2016, and Tavakolian 2015 reported pain perception during IUD insertion, while Van der Heijden 2017 did not fulfil the inclusion criteria for type of intervention. See Characteristics of excluded studies.
Risk of bias in included studies
Summaries of assessments of bias in included studies are shown in Figure 2 and Figure 3. Details of the appraisals made on risk of bias are described below.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials

Risk of bias summary: review authors' judgements about each risk of bias item for each included trial
Allocation
Twelve trials described the method they used to generate the randomization sequence, thus meeting the criteria for low risk of bias (Alanwar 2018; Fava 2020; Hubacher 2006; Jafari 2014; Kaviani 2013; Madden 2012; Mercorio 2003; Papaikonomou 2018; Saharkhiz 2017; Sordal 2013; Warner 2010; Yavarikia 2013). Randomization was mostly undertaken by a computer‐generated list of random numbers. For allocation concealment, we found 10 trials to have low risk of bias (Alanwar 2018; Fava 2020; Madden 2012; Makarainen 1986; Mercorio 2003; Papaikonomou 2018; Saharkhiz 2017; Warner 2010; Yavarikia 2013; Ylikorkala 1978). Eight out of 21 trials met the criteria for low risk of selection bias (both random sequence generation and allocation concealment; Alanwar 2018; Fava 2020; Madden 2012; Mercorio 2003; Papaikonomou 2018; Saharkhiz 2017; Warner 2010; Yavarikia 2013). Nine trials had unclear random sequence generation (Buttram 1979; Davies 1981; Hahn 1979; Lalos 1983; Lin 2007; Makarainen 1986; Roy 1981; Ylikorkala 1978; Ylikorkala 1983), while 11 trials had unclear allocation concealment (Buttram 1979; Davies 1981; Hahn 1979; Hubacher 2006; Jafari 2014; Kaviani 2013; Lalos 1983; Lin 2007; Roy 1981; Sordal 2013; Ylikorkala 1983). There were no trials with high risk of selection bias.
Blinding
Performance bias
Ten trials met the criteria for low risk of performance bias that ensured blinding of participants and investigators because the control groups had treatment regimens identical in appearance to the experimental intervention (Alanwar 2018; Buttram 1979; Fava 2020; Hubacher 2006; Jafari 2014; Kaviani 2013; Roy 1981; Saharkhiz 2017; Sordal 2013; Yavarikia 2013). We found two trials to have high risk of performance bias because the route of administration of the experimental intervention was transdermal (Madden 2012), and intranasal (Mercorio 2003), without similar route of administration in the controls. We judged nine other trials to have unclear risk of performance bias because there were insufficient details to infer who was blinded (Davies 1981; Hahn 1979; Lalos 1983; Lin 2007; Makarainen 1986; Papaikonomou 2018; Warner 2010; Ylikorkala 1978; Ylikorkala 1983).
Detection bias
We considered 16 trials to have high risk of detection bias because their assessments of bleeding and pain outcomes were subjective (Alanwar 2018; Buttram 1979; Fava 2020; Jafari 2014; Kaviani 2013; Lalos 1983; Lin 2007; Madden 2012; Makarainen 1986; Mercorio 2003; Papaikonomou 2018; Saharkhiz 2017; Sordal 2013; Warner 2010; Ylikorkala 1978; Ylikorkala 1983). In these trials, the participants assessed the outcome by filling in the questionnaires and PBACs and recording their symptoms in diaries. Four trials met the criteria for low risk of detection bias, with the use of alkaline hematin tests in laboratories (Hahn 1979; Hubacher 2006; Roy 1981; Yavarikia 2013). One trial had unclear risk of detection bias because they did not describe their methods of outcome measurement and there were no other details regarding blinding of outcome assessors (Davies 1981).
Incomplete outcome data
Eighteen trials had low risk of attrition bias because there were either no missing data or they excluded the missing data from analysis, or they applied the intention‐to‐treat principle (Alanwar 2018; Buttram 1979; Fava 2020; Hahn 1979; Hubacher 2006; Jafari 2014; Kaviani 2013; Lalos 1983; Lin 2007; Madden 2012; Makarainen 1986; Papaikonomou 2018; Roy 1981; Saharkhiz 2017; Sordal 2013; Warner 2010; Yavarikia 2013; Ylikorkala 1983). Three trials had unclear risk of attrition bias because they did not provide details regarding missing data (Davies 1981; Mercorio 2003; Ylikorkala 1978).
Selective reporting
The majority of the included trials published only data. There was no access to the trial registration reports or trial protocols. Under these conditions, we were not able to evaluate whether trial authors had overlooked reporting findings for all their pre‐specified outcomes. Thus, we considered 13 trials to have an unclear risk of reporting bias (Buttram 1979; Davies 1981; Hahn 1979; Hubacher 2006; Kaviani 2013; Lalos 1983; Lin 2007; Makarainen 1986; Mercorio 2003; Roy 1981; Yavarikia 2013; Ylikorkala 1978; Ylikorkala 1983). The remaining eight trials met the criteria for low risk of reporting bias because they listed their pre‐specified outcomes in their protocols or trial registration reports (Alanwar 2018; Fava 2020; Jafari 2014; Madden 2012; Papaikonomou 2018; Saharkhiz 2017; Sordal 2013; Warner 2010).
Other potential sources of bias
We deemed most of the included trials to have low risk of bias in this domain as they appeared free from other sources of bias. We judged one trial, which was a cross‐over design, to be high risk due to differences in baseline characteristics because four out of 10 participants on IUD had prolonged bleeding time, increased capillary fragility or a history of bleeding tendencies prior to intervention (Hahn 1979). Two trials had unclear risk of bias because the baseline characteristics were not available (Davies 1981; Mercorio 2003).
Effects of interventions
See: Summary of findings 1 Interventions (vitamin B1, mefenamic acid, tranexamic acid) compared to placebo or active comparators (desmopressin, sodium diclofenac, flavonoids) for the treatment of heavy menstrual bleeding associated with Cu IUD; Summary of findings 2 Ulipristal acetate compared to placebo for the treatment of heavy menstrual bleeding associated with LNG IUD; Summary of findings 3 Mefanamic acid compared to Vitex agnus for the treatment of heavy menstrual bleeding associated with unknown IUD type; Summary of findings 4 Tranexamic acid compared to sodium diclofenac for the treatment of pain associated with Cu IUD; Summary of findings 5 Naproxen compared to placebo for the treatment of pain associated with unknown IUD type; Summary of findings 6 Interventions (ibuprofen, tolfenamic acid, aspirin, tranexamic acid) compared to placebo or active comparators (paracetamol, tranexamic acid) for the prevention of heavy menstrual bleeding associated with Cu IUD; Summary of findings 7 Interventions (ulipristal acetate, tranexamic acid, mifepristone, naproxen) compared placebo or active comparators (mefenamic acid, vitamin B, estradiol) for the prevention of heavy menstrual bleeding associated with LNG IUD; Summary of findings 8 Interventions (ibuprofen, tolfenamic acid) compared to placebo for the prevention of pain associated with Cu IUD
Primary outcomes
Treatment trials
Treatment of heavy menstrual bleeding associated with IUD use
Cu IUD
-
Vitamin B1 versus placebo: vitamin B1 may reduce the number of pads used per day (MD −7.0 pads, 95% CI −8.50 to −5.50, P < 0.001; 1 trial, 110 participants; Analysis 1.1), number of spotting days (MD −1.60 days, 95% CI −1.94 to −1.26, P < 0.001; 1 trial, 110 participants; Analysis 1.2) and number of bleeding days in comparison to placebo (MD −2.00 days, 95% CI −2.38 to −1.62; P < 0.001; 1 trial, 110 participants; Analysis 1.3). This evidence was low certainty, downgraded for serious risk of bias and imprecision.
-
Naproxen versus placebo: there may be little or no difference between naproxen and placebo for heavier menstrual flow (OR 0.09, 95% CI 0.00 to 1.78; P = 0.11; 1 trial; 40 participants; Analysis 2.1) but the evidence is uncertain. The result was assessed as very low certainty, downgraded for very serious risk of bias and serious imprecision.
-
Mefenamic acid versus tranexamic acid: mefenamic acid may reduce the volume of menstrual blood loss in comparison to tranexamic acid (MD −64.26 mL, 95% CI −105.65 to −22.87; P = 0.002; 1 trial, 94 participants; Analysis 1.1). The certainty of evidence was low, downgraded for very serious risk of bias and serious imprecision (summary of findings Table 1). Mefenamic acid may have lower pictorial blood loss assessment chart (PBAC) score in contrast to tranexamic acid (MD −8.19, 95% CI −25.24 to 8.86; P = 0.35; 1 trial, 58 participants; Analysis 3.2) but the evidence is very uncertain. The certainty of evidence was very low, downgraded for very serious risk of bias and serious imprecision. There may be little or no difference in the number of bleeding days between mefenamic acid and tranexamic acid (MD 0.08 days, 95% CI −0.27 to 0.42; P = 0.66, I2 = 0; 2 trials, 152 participants; Analysis 3.3). Evidence was of low certainty, downgraded for serious imprecision (summary of findings Table 1).
-
Mefenamic acid versus desmopressin: the evidence is very uncertain about the effect of mefenamic acid compared to desmopressin and there were insufficient data available for analysis. It was reported that the mean reduction in PBAC score was 45.7% in the mefenamic acid group and 40.5% in the desmopressin group (1 trial, 24 participants; Analysis 4.1). Evidence was very low certainty, downgraded due to very serious risk of bias and serious imprecision (summary of findings Table 1).
-
Tranexamic acid versus sodium diclofenac: tranexamic acid may reduce the volume of menstrual blood loss in comparison to sodium diclofenac (MD −42.70 mL, 95% CI −73.33 to −12.07; P = 0.006; 1 trial, 38 participants; Analysis 5.1) but the evidence is very low certainty, downgraded for serious risk of bias and imprecision (summary of findings Table 1). There may be little or no difference in the duration of bleeding between tranexamic acid and sodium diclofenac (MD 0.00 95% CI −0.62 to 0.62; P = 1.0; 1 trial, 38 participants; Analysis 5.2) but the evidence is very uncertain. Evidence was of very low certainty, downgraded for serious risk of bias and imprecision (summary of findings Table 1).
-
Tranexamic acid versus flavonoids: tranexamic acid may be associated with a modest reduction in PBAC score compared with oral flavonoids (MD −32.0, 95% CI −39.84 to −24.16; P < 0.001; 1 trial, 100 participants; Analysis 6.1). The certainty of evidence was low, downgraded for serious risk of bias and imprecision (summary of findings Table 1). Tranexamic acid may result in fewer pads used per day (MD −0.50 pads, 95% CI −0.91 to −0.09; P = 0.02; 1 trial, 100 participants; Analysis 6.2) and fewer bleeding days in comparison to flavonoids (MD −1.40 days, 95% CI −1.93 to −0.87; 1 trial, 100 participants; Analysis 6.3). The certainty of evidence was assessed as low, downgraded for serious risk of bias and imprecision (summary of findings Table 1).
-
Tranexamic acid versus active comparators (mefenamic acid, flavonoid, sodium diclofenac): the evidence is very uncertain about the effect of tranexamic acid compared to controls in the number of bleeding days (MD −0.27 95% CI −1.14 to 0.60; P = 0.54, I2 = 87%; 4 trials, 290 participants; Analysis 7.1). The certainty of evidence was very low, downgraded for serious risk of bias and inconsistency (summary of findings Table 1). This was a composite analysis as other trials had different interventions and outcomes, which could not be analysed together.
LNG IUD
-
Ulipristal acetate versus placebo: the evidence is very uncertain about the effect of ulipristal acetate compared with placebo on the duration of bleeding (MD −3.30 days, 95% CI −9.07 to 2.47; P = 0.26, 1 trial, 24 participants; Analysis 8.1) and number of bleeding days in 90 days (MD −9.30 days, 95% CI −26.76 to 8.16; P = 0.30, 1 trial, 24 participants; Analysis 8.2). This evidence was very low certainty, downgraded for serious risk of bias and serious imprecision as well as inconsistency (summary of findings Table 2).
Unknown IUD type
-
High‐dose naproxen versus low‐dose naproxen: the evidence is very uncertain about the effect of different naproxen doses on menstrual blood loss; there were insufficient data available for analysis. One trial involving 34 users of an unknown type of IUD reported that naproxen 1250 mg per day for five days had higher percentage (31.6%) of menstrual blood loss in comparison to 500 mg on day one then 750 mg per day for five days (9.5%) (Davies 1981; Analysis 9.1).
-
Mefenamic acid versus Vitex agnus: mefenamic acid may not differ from Vitex agnus in PBAC score (MD −2.40, 95% CI −13.77 to 8.97; P = 0.68; 1 trial, 84 participants; Analysis 10.1). The certainty of evidence was low, downgraded due to serious risk of bias and imprecision (summary of findings Table 3).
Treatment of pain associated with IUD use
Cu IUD
-
Tranexamic acid versus sodium diclofenac: there may be little or no difference between tranexamic acid and sodium diclofenac for the occurrence of pelvic pain (OR 1.0, 95% CI 0.06 to 17.25; P = 1.00; 1 trial, 38 participants; Analysis 11.1) but the evidence is very uncertain. The evidence was very low certainty, downgraded for serious risk of bias and imprecision (summary of findings Table 4).
Unknown IUD type
-
Naproxen versus placebo: compared to placebo, naproxen may be associated with lower overall pain relief scores (MD 4.1, 95% CI 0.91 to 7.29; P = 0.01; 1 trial, 33 participants; Analysis 12.1) and lower daily pain relief score (MD 3.1, 95% CI 0.27 to 5.93; P = 0.03; 1 trial, 33 participants; Analysis 12.2). Evidence for both outcomes was low certainty, downgraded for serious risk of bias and imprecision (summary of findings Table 5).
Prevention trials
Prevention of heavy menstrual bleeding associated with IUD use
Cu IUD
-
Ibuprofen versus placebo: the trial arms did not differ significantly in reduction of blood loss volume, measured by alkaline hematin method, for ibuprofen and placebo (MD −14mL.11, 95% CI −36.04 to 7.82; P = 0.21; 2 trials, 40 participants; Analysis 13.1). Subgroup analysis by type of IUD (Lippes loop and Cu IUD) also revealed no difference. The evidence was of low certainty, downgraded for serious risk of bias and imprecision (summary of findings Table 6). In another trial (Makarainen 1986), there was no difference in duration of bleeding between ibuprofen and placebo (MD −0.20 days, 95% CI −1.40 to 1.00; P = 0.74; 1 trial; 28 participants; Analysis 13.2). The evidence was of very low certainty, downgraded for very serious risk of bias and serious imprecision (summary of findings Table 6). The median blood loss in this trial was 51 mL in the ibuprofen group with Fincoid IUD and 47 mL with the multiload copper‐375 IUD in comparison to 49 mL in the placebo group with Fincoid IUD and 62 mL with the multiload copper‐375 IUD (Analysis 13.3).
-
Tolfenamic acid versus placebo: tolfenamic acid resulted in fewer pads used per day (MD −1.00 pads, 95% CI −1.57 to −0.43; P < 0.001; 1 trial, 122 participants; Analysis 14.1), fewer occurrences of menstruation that were "more abundant than normal" in comparison to placebo (OR 0.54, 95% CI 0.34 to 0.85; P = 0.008; 1 trial, 181 events; Analysis 14.2) and fewer blood clots (OR 0.43, 95% CI 0.27 to 0.68, P < 0.001; 1 trial, 150 events; Analysis 14.3). Evidence was very low certainty; downgraded for serious risk of bias and imprecision (summary of findings Table 6).
-
Aspirin versus paracetamol: there was no evidence of a difference between aspirin and paracetamol to reduce the volume of menstrual blood loss (MD −0.30, 95% CI −26.16 to 25.56; P = 0.98; 1 trial, 20 participants; Analysis 15.1). This evidence was of very low certainty, downgraded for very serious risk of bias and serious imprecision (summary of findings Table 6).
-
Higher dose of tranexamic acid versus lower dose of tranexamic acid: one trial conducted among 175 Cu IUD users compared 1 g tranexamic acid to 2 g tranexamic acid for the prevention of bleeding (Lin 2007). The percentage occurrence of heavy menstrual bleeding was 20% in the 2 g tranexamic acid arm versus 11.76% in the 1 g tranexamic acid arm as measured by the alkaline hematin method (Analysis 16.1). The PBAC score was also lower in the 2 g tranexamic acid group (26.79%) in comparison to 1 g tranexamic acid (45.83%; Analysis 16.1). The evidence was very low certainty, downgraded for serious risk of bias and imprecision (summary of findings Table 6).
LNG IUD
-
Ulipristal acetate (CBD‐2914) versus placebo: ulipristal acetate may increase the percentage bleeding or spotting days in comparison to placebo (MD 9.50, 95% CI 1.48 to 17.52; P = 0.02; 1 trial, 118 participants; Analysis 17.1). However, the certainty of evidence was low, downgraded for serious risk of bias and very serious imprecision (summary of findings Table 7).
-
Tranexamic acid versus mefenamic acid and placebo: one trial that compared tranexamic acid, mefenamic acid and placebo had insufficient data for analysis (Sordal 2013). The median number of bleed days reported was 8 days in the tranexamic acid group, 10 in the mefenamic acid group and 11.5 in the placebo group (Analysis 18.1). Evidence was low certainty, downgraded for serious risk of bias and imprecision (summary of findings Table 7).
-
Mifepristone versus vitamin B: there were insufficient data for analysis in the trial comparing mifepristone and vitamin B, which reported that fewer participants in the mifepristone group reported bleeding or spotting (Papaikonomou 2018; Analysis 20.1). The evidence was of very low certainty, downgraded for very serious risk of bias and imprecision (summary of findings Table 7).
-
Naproxen versus estradiol: one trial provided insufficient data for analysis of number of bleeding days for naproxen compared with estradiol (Madden 2012). The median number of bleeding days in the naproxen arm was 27.5 in comparison to 44 days in the estradiol arm (Analysis 19.1). Evidence was very low certainty, downgraded for very serious risk of bias and imprecision (summary of findings Table 7).
Prevention of pain
Cu IUD
-
Tolfenamic acid versus placebo: there may be little or no difference between tolfenamic acid and placebo in reduction of the occurrence of menstruation that was "more painful than normal" but the evidence is very uncertain (OR 0.71, 95% CI 0.44 to 1.14; P = 0.15; 1 trial, 108 events; Analysis 21.1). Evidence was very low certainty, downgraded for serious risk of bias and imprecision (summary of findings Table 8).
-
Ibuprofen versus placebo: there may be little or no difference between ibuprofen and placebo in the reduction of menstrual cramps (OR 1.0, 95% CI 0.11 to 8.95, P = 1.00; 1 trial, 4 events; Analysis 22.1). The evidence was low certainty, downgraded for serious risk of bias and imprecision (summary of findings Table 8).
Secondary outcomes
Treatment trials
IUD removal
No treatment trials assessed IUD removal due to bleeding or pain.
Haemoglobin levels
One trial reported on pre‐ and post‐haemoglobin levels of all Cu IUD participants, but data were insufficient for analysis because the trial did not compare tranexamic acid and sodium diclofenac (Ylikorkala 1983). The mean (standard error) for pre‐intervention blood haemoglobin concentrations was 124.8 (1.9) g/L while for post‐intervention it was 124.7 (1.8) g/L.
Need for additional analgesia
One trial that compared naproxen to placebo for the treatment of pain associated with IUD use (unknown type of IUD) reported the use of additional analgesia (Buttram 1979). There was no difference between naproxen and placebo for the use of additional analgesia (OR 0.29, 95% CI 0.05 to 1.80; P = 0.19; 1 trial, 33 participants, 7 events; Analysis 12.4).
Quality of life
No treatment trial reported quality of life.
Side effects
Four treatment trials among Cu IUD users reported side effects but it was not possible to analyze the data due to differences in various side effects, interventions and control. In a small trial by Mercorio 2003, it was difficult to estimate the difference between mefenamic acid and desmopressin, with no effect on the occurrence of headache and insomnia (OR 0.11, 95% CI 0.00 to 2.36, P = 016; 1 trial, 24 participants, 3 events; Analysis 4.2).
In another trial that compared tranexamic acid and sodium diclofenac for the occurrence of side effects (gastrointestinal symptoms, headache, sweating), tranexamic acid increased the odds of the occurrence of side effects compared to sodium diclofenac (OR 4.69, 95% CI 1.20 to 18.44; P = 0.03; 1 trial, 38 participants, 19 events; Analysis 5.3; Ylikorkala 1983).
The occurrence of headache (OR 0.58, 95% CI 0.18 to 1.92; P = 0.38; 1 trial, 100 participants, 13 events; Analysis 6.4) and vomiting (OR 0.74, 95% CI 0.25 to 2.18; P = 0.59; 1 trial, 100 participants, 16 events; Analysis 6.4) also did not differ in a trial comparing tranexamic acid and oral flavonoids (Alanwar 2018).
There was also no difference in the occurrence of side effects in a trial that compared naproxen and placebo (OR 1.91, 95% CI 0.72 to 5.06; P = 0.19; 1 trial, 336 participants, 16 events; Analysis 2.2; Lalos 1983).
In another trial comparing mefenamic acid and Vitex agnus (Yavarikia 2013), where the IUD type was not known, the occurrence of nausea (OR 1.00, 95% CI 0.06 to 16.53; P = 1.0; 1 trial, 84 participants, 2 events; Analysis 10.2) and abdominal pain (OR 0.33, 95% CI 0.01 to 8.22; P = 0.50; 1 trial; 84 participants, 1 event; Analysis 10.2) did not differ.
Prevention trials
IUD removal
One prevention trial assessed the effect of ibuprofen and placebo among Cu IUD users on IUD removal due to pain or increased blood loss (Hubacher 2006). There was no difference between ibuprofen and placebo on IUD removal due to pain or increased blood loss by 26 weeks (OR 0.96, 95% CI 0.66 to 1.38; P = 0.81; 1 trial, 1962 participants, 120 events; Analysis 23.1) and by 52 weeks (OR 1.25, 95% CI 0.39 to 1.69; P = 0.14; 1 trial, 1962 participants, 190 events; Analysis 23.2).
Haemoglobin levels
No prevention trial assessed haemoglobin levels.
Need for additional analgesia
No prevention trial assessed need for analgesia.
Quality of life
No prevention trial assessed quality of life.
Side effects
Four prevention trials provided data for side effects but it was not feasible to pool data for analysis due to differences in side effects, interventions and control. Three trials were in Cu IUD users (Makarainen 1986; Roy 1981; Ylikorkala 1978), while one trial was among LNG IUD users (Madden 2012). There was no difference in the occurrence of side effects between ibuprofen and placebo in two trials (OR 2.15, 95% CI 0.5 to 9.31; P = 0.30, I2 = 0%; 2 trials, 108 participants, 8 events; Analysis 13.4; Makarainen 1986; Roy 1981).
In another trial comparing tolfenamic acid and placebo (Ylikorkala 1978), there was no difference in the occurrence of side effects (OR 0.42, 95% CI 0.02 to 9.29; P = 0.58; 1 trial, 366 participants, 14 events; Analysis 21.2). The occurrence of dyspepsia and diarrhoea (OR 9.96, 95% CI 0.52 to 189.04; P = 0.13; 1 trial, 122 participants, 4 events; Analysis 21.2) were more common with tolfenamic acid but the estimate was not statistically significant and the confidence interval was wide. The occurrence of headache (OR 0.09, 95% CI 0.00 to 1.60; P = 0.10; 1 trial, 122 participants, 5 events; Analysis 21.2) and depression (OR 0.09, 95% CI 0.00 to 1.60, P = 0.10; 1 trial, 122 participants, 5 events; Analysis 21.2) did not differ between tolfenamic acid and placebo.
There was no difference in the occurrence of gastroesophageal reflux between naproxen and estradiol among LNG IUD users (OR 3.22, 95% CI 0.13 to 81.19; P = 0.48; 1 trial, 86 participants, 1 event; Analysis 19.3).
Discussion
Summary of main results
This updated review includes 21 trials involving 3689 participants. Trials were mostly conducted in upper‐middle‐ to high‐income countries. There were 11 treatment trials (seven Cu IUD, one LNG IUD, three unknown IUD type), involving 767 participants, and 10 prevention trials (six Cu IUD, four LNG IUD), involving 2922 participants. This review has also extended its interventions to not just include NSAIDs but any interventions that were assessed to treat or prevent heavy menstrual bleeding or pain, or both, induced by IUD.
Treatment trials
Treatment of heavy menstrual bleeding associated with Cu IUD use
-
Vitamin B1 versus placebo: in one trial involving 126 participants, 100 mg vitamin B1 may reduce the number of pads used per day, number of spotting days and duration of bleeding in comparison to placebo (Jafari 2014). Since the evidence was from one trial, we cannot draw definitive conclusions.
-
Naproxen versus placebo: there may be little or no difference between oral naproxen (500 mg followed by 250 mg two to four times per day as needed) and oral placebo in the amount of menstrual flow according to one small trial involving 40 participants but the effect is very uncertain (Lalos 1983).
-
Mefenamic acid versus tranexamic acid: oral mefenamic acid at 1500 mg per day may reduce the volume of menstrual blood loss in comparison to oral tranexamic acid 1500 mg per day but this evidence is based on one trial with 94 participants, thus, we cannot draw definitive conclusions (Saharkhiz 2017). Mefenamic acid and tranexamic acid may not reduce the duration of bleeding (Kaviani 2013; Saharkhiz 2017). This evidence however, was based on two trials involving a total of 152 participants.
-
Mefenamic acid versus desmopressin: there were insufficient data for analysis.
-
Tranexamic acid versus sodium diclofenac: based on one trial involving 38 participants (Ylikorkala 1983), oral tranexamic acid at 4.5 g per day for five days may reduce the volume of menstrual blood loss but not the duration of bleeding in comparison to oral sodium diclofenac 150 mg on day 1 then 75 mg for four days.
-
Tranexamic acid versus flavonoids: oral tranexamic acid 500 mg, six‐hourly, taken for the first three days of menstruation, had a lower PBAC score, fewer number of pads used per day and fewer bleeding days in comparison to flavonoids. This evidence was also from a single trial involving 100 participants (Alanwar 2018).
-
Tranexamic acid versus comparisons: oral tranexamic acid (at various doses and regimes) may reduce the number of bleeding days in comparison to control (Alanwar 2018; Kaviani 2013; Saharkhiz 2017; Ylikorkala 1983). There was substantial heterogeneity due to the various doses of tranexamic acid and type of comparisons used (mefenamic acid, flavonoid, sodium diclofenac).
Treatment of heavy menstrual bleeding associated with LNG IUD use
-
Ulipristal acetate versus placebo: oral ulipristal acetate 5 mg per day taken for five days made no difference in comparison to placebo to the duration of days until bleeding stops and total bleeding days in 90 days for bleeding associated with LNG IUD use. However, this evidence was also from one small trial involving 30 participants (Fava 2020).
Treatment of heavy menstrual bleeding associated with unknown IUD type
-
Higher dose naproxen versus lower dose naproxen: there were insufficient data for analysis. One trial (Davies 1981), compared oral naproxen 1250 mg per day for five days to 500 mg then 750 mg for five days and reported that the higher dose of naproxen reduced menstrual blood loss more than the lower dose (32% versus 22%).
-
Mefenamic acid versus Vitex agnus: the PBAC score did not differ significantly between oral mefenamic acid and Vitex agnus for the treatment of bleeding associated with LNG IUD based on one trial involving 84 participants (Yavarikia 2013).
Treatment of pain associated with Cu IUD use
-
Tranexamic acid versus sodium diclofenac: there was no difference between oral tranexamic acid and oral sodium diclofenac for pain in one trial involving 38 participants (Ylikorkala 1983).
Treatment of pain associated with unknown IUD type
-
Naproxen versus placebo: oral naproxen may provide overall and daily pain relief in comparison to placebo, but this evidence was also based on one trial with 33 participants thus definitive conclusions can’t be drawn (Buttram 1979).
Prevention trials
Prevention of heavy menstrual bleeding associated with Cu IUD use
-
Ibuprofen versus placebo: prophylactic oral ibuprofen did not reduce menstrual blood loss (Roy 1981) or duration of bleeding (Makarainen 1986). There were insufficient data to pool these two trials together for further analysis.
-
Tolfenamic acid versus placebo: prophylactic tolfenamic acid at a dose of 600 mg per day may be effective to reduce the number of pads used, the number of occurrences of menstruation that were "more abundant than normal" and blood clots compared to placebo. The evidence was from one trial with 160 participants (Ylikorkala 1978).
-
Aspirin versus paracetamol: there was no significant difference between oral aspirin and oral paracetamol for the prevention of bleeding associated with Cu IUD, based on one small trial involving 20 participants (Hahn 1979).
-
Higher dose of tranexamic acid versus lower dose of tranexamic acid: there were insufficient data for analysis. One trial, involving 175 participants, compared 2 g prophylactic oral tranexamic acid versus 1 g and reported a lower percentage of heavy menstrual bleeding occurrence in the 2 g arm than in the 1 g arm (20% versus 11.76% via alkaline hematin method and 26.79% versus 45.83% via PBAC score; Lin 2007).
Prevention of bleeding associated with LNG IUD
-
Ulipristal acetate (CBD‐2914) versus placebo: ulipristal acetate, a selective progesterone receptor modulator at a dose of 50 mg per day taken for three consecutive days with separate treatments starting from 21, 49 and 77 days after IUD insertion may not be effective to reduce the percentage bleeding/spotting days. This evidence was generated from a single trial involving 118 participants (Warner 2010).
-
Tranexamic acid versus mefenamic acid and placebo: there were insufficient data for analysis. One trial including 187 participants (Sordal 2013), reported that the median number of bleed days in the prophylactic tranexamic acid group was 8 days while in the mefenamic acid group it was 10 days, and 11.5 days with placebo.
-
Mifepristone versus vitamin B: there were insufficient data for analysis in the trial comparing prophylactic mifepristone and vitamin B (Papaikonomou 2018).
-
Naproxen versus estradiol: there were insufficient data for analysis. The median number of bleeding days in the naproxen arm was 27.5 in comparison to 44 days in the estradiol arm from the trial conducted by Madden 2012 involving 129 women. The occurrence of gastroesophageal reflux was more common in the naproxen group but findings were not statistically significant with a wide confidence interval.
Prevention of pain associated with Cu IUD use
-
Tolfenamic acid versus placebo: there was no difference between prophylactic oral tolfenamic acid and placebo in the occurrence of more painful menstruation among 160 Cu IUD users in one trial conducted by Ylikorkala 1978.
-
Ibuprofen versus placebo: there was also no difference in oral ibuprofen and placebo to prevent menstrual cramps associated with Cu IUD use. This evidence was from one small trial involving 20 participants (Roy 1981) thus, further research is necessary.
Overall completeness and applicability of evidence
This review included a heterogeneous literature due to the broad review objective and scope. The heterogeneity related to the intent of the intervention either for prophylaxis or treatment, the various interventions and comparators, the different intervention regimens, reporting of outcomes and limited number of trials, and the different IUD types studied. Due to the considerable heterogeneity we could not combine the data using meta‐analysis. Therefore, the overall completeness of evidence in this review is limited.
In terms of applicability in clinical practice based on evidence in this review, there is still insufficient evidence to draw conclusions regarding a specific drug or regimen for the treatment or prevention of heavy menstrual bleeding or pain associated with IUD use. In agreement with the previous review, mefenamic acid and tranexamic acid may reduce heavy menstrual bleeding associated with Cu IUD use. Vitamin B1 may reduce heavy menstrual bleeding while naproxen may reduce pain among Cu IUD users. Prophylactic tolfenamic acid could possibly reduce heavy menstrual bleeding associated with Cu IUD use. There was no evidence for the effectiveness of ulipristal and Vitex agnus to treat bleeding and pain associated with LNG IUD and ulipristal acetate to prevent heavy menstrual bleeding.
With regard to side effects, there were only two trials that had sufficient data for analysis. The occurrence of dyspepsia and headache was more frequent with tolfenamic acid while gastroesophageal reflux was more common with naproxen. The evidence for side effects was limited, with wide confidence intervals. It was not possible to rule out possible harms and establish the side effects of treatments.
Quality of the evidence
We used GRADE to evaluate the certainty of evidence for each primary and secondary outcome, as reported in the summary of findings tables. The methodological quality of the evidence varied from very low to low. The major limitations were risk of bias and imprecision. Risk of bias was mostly serious due to unclear selection (allocation concealment), detection (unclear blinding of outcome assessors and self‐reporting of subjective assessments such as pain) and reporting bias (unpublished protocols). Most of the evidence had serious imprecision as effect measures were mostly obtained from a single trial for each of the comparisons. Larger, properly designed trials of the interventions are essential in order to achieve conclusions on the comparative efficacy of treatments.
Potential biases in the review process
We are mindful of possible biases in the reviewing process and have undertaken several measures to curb bias, such as having two review authors independently extracting data. Publication of an updated protocol prior to undertaking this review would have been better but all review authors have approved the protocol changes prior to initiating the review. We deem that all relevant trials are now incorporated but cannot dismiss the likelihood that additional trials may be unpublished or published in sources not accessible to our search. Hence, publication bias cannot be wholly disregarded.
Agreements and disagreements with other studies or reviews
There are several systematic reviews previously published for pain and bleeding unrelated to IUD use. There was insufficient evidence to determine whether NSAIDs reduced volumes of menstrual blood loss in comparison to combined oral contraceptives for heavy menstrual bleeding unrelated to IUD use (Lethaby 2019). In another systematic review for participants with primary pain, NSAIDs were effective for pain relief but had more side effects particularly gastrointestinal symptoms (Marjoribanks 2015). We found low‐ to very low‐certainty evidence that mefenamic acid, tranexamic acid and vitamin B1 may reduce heavy menstrual bleeding associated with Cu IUD use, while naproxen may relieve pain.
Trials investigating NSAIDs in this review had various interventions and outcome measures. Thus, no conclusions can be drawn regarding the preferred NSAID. There is limited evidence in terms of the possible effectiveness of NSAIDs, or whether a specific NSAID or regimen might be most effective to reduce pain associated with IUD use. Therefore, the choice of NSAID might be driven by other considerations such as cost, dosage and regimen, drug interactions, and patient’s preference, as well as side effects.
Research regarding the interventions to treat and prevent heavy bleeding and pain associated with LNG IUD use remains limited.
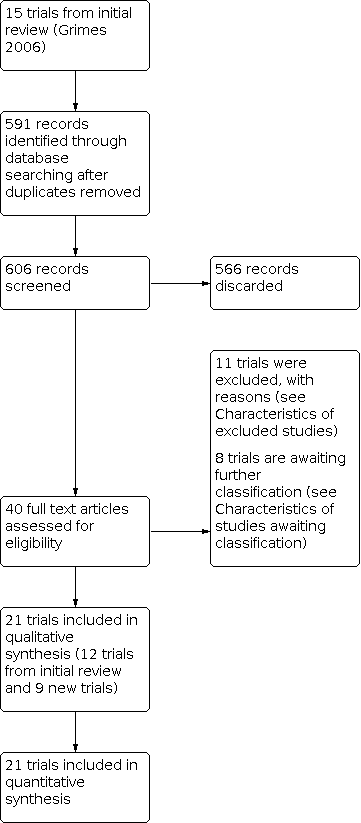
Trial flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials

Risk of bias summary: review authors' judgements about each risk of bias item for each included trial

Comparison 1: Vitamin B1 vs placebo (Cu IUD, treatment for HMB), Outcome 1: Number of pads/day

Comparison 1: Vitamin B1 vs placebo (Cu IUD, treatment for HMB), Outcome 2: Number of spotting days

Comparison 1: Vitamin B1 vs placebo (Cu IUD, treatment for HMB), Outcome 3: Number of bleeding days

Comparison 2: Naproxen vs placebo (Cu IUD, treatment for HMB), Outcome 1: "More" menstrual flow

Comparison 2: Naproxen vs placebo (Cu IUD, treatment for HMB), Outcome 2: Side effects

Comparison 3: Mefenamic acid vs tranexamic acid (Cu IUD, treatment for HMB), Outcome 1: Volume of blood loss

Comparison 3: Mefenamic acid vs tranexamic acid (Cu IUD, treatment for HMB), Outcome 2: PBAC score

Comparison 3: Mefenamic acid vs tranexamic acid (Cu IUD, treatment for HMB), Outcome 3: Number of bleeding days
| Mean reduction of PBAC score (%) | ||
| Study | desmopressin | mefenamic acid |
|---|---|---|
| Mercorio 2003 | 40.5 | 45.7 |
Comparison 4: Mefenamic acid vs desmopressin (Cu IUD, treatment for HMB), Outcome 1: Mean reduction of PBAC score (%)

Comparison 4: Mefenamic acid vs desmopressin (Cu IUD, treatment for HMB), Outcome 2: Side effects: headache and insomnia

Comparison 5: Tranexamic acid vs sodium diclofenac (Cu IUD, treatment for HMB), Outcome 1: Menstrual blood loss (alkaline hematin)

Comparison 5: Tranexamic acid vs sodium diclofenac (Cu IUD, treatment for HMB), Outcome 2: Duration of menstruation

Comparison 5: Tranexamic acid vs sodium diclofenac (Cu IUD, treatment for HMB), Outcome 3: Side effects

Comparison 6: Tranexamic acid vs flavonoids (Cu IUD, treatment for HMB), Outcome 1: PBAC score

Comparison 6: Tranexamic acid vs flavonoids (Cu IUD, treatment for HMB), Outcome 2: Number of pads/day

Comparison 6: Tranexamic acid vs flavonoids (Cu IUD, treatment for HMB), Outcome 3: Number of bleeding days

Comparison 6: Tranexamic acid vs flavonoids (Cu IUD, treatment for HMB), Outcome 4: Side effects

Comparison 7: Tranexamic acid vs active comparators (mefenamic acid, flavonoids, diclofenac) (Cu IUD, treatment for HMB), Outcome 1: Number of bleeding days

Comparison 8: Ulipristal acetate vs placebo (LNG IUD, treatment of HMB), Outcome 1: Duration of days until bleeding stops

Comparison 8: Ulipristal acetate vs placebo (LNG IUD, treatment of HMB), Outcome 2: Total bleeding in 90 days
| Blood loss reduction (%) | ||
| Study | High dose naproxen | Low dose naproxen |
|---|---|---|
| Davies 1981 | 31.6 | 9.5 |
Comparison 9: High‐dose naproxen vs low‐dose naproxen (unknown IUD, treatment of HMB), Outcome 1: Blood loss reduction (%)

Comparison 10: Mefenamic acid vs Vitex agnus (unknown IUD, treatment for HMB), Outcome 1: PBAC score

Comparison 10: Mefenamic acid vs Vitex agnus (unknown IUD, treatment for HMB), Outcome 2: Side effects

Comparison 11: Tranexamic acid vs sodium diclofenac (Cu IUD, treatment for pain), Outcome 1: Pelvic pain

Comparison 12: Naproxen vs placebo (unknown IUD, treatment for pain), Outcome 1: Overall pain relief score

Comparison 12: Naproxen vs placebo (unknown IUD, treatment for pain), Outcome 2: Daily pain relief score

Comparison 12: Naproxen vs placebo (unknown IUD, treatment for pain), Outcome 3: Pain relief

Comparison 12: Naproxen vs placebo (unknown IUD, treatment for pain), Outcome 4: Need for analgesia

Comparison 13: Ibuprofen vs placebo (Cu IUD, prevention of HMB), Outcome 1: Menstrual blood loss (alkaline hematin)

Comparison 13: Ibuprofen vs placebo (Cu IUD, prevention of HMB), Outcome 2: Duration of bleeding
| Median menstrual blood loss (alkaline hematin) | ||
| Study | Ibuprofen | Placebo |
|---|---|---|
| Fincoid | ||
| Makarainen 1986 | 51 | 49 |
| ML Cu 375 | ||
| Makarainen 1986 | 47 | 62 |
Comparison 13: Ibuprofen vs placebo (Cu IUD, prevention of HMB), Outcome 3: Median menstrual blood loss (alkaline hematin)

Comparison 13: Ibuprofen vs placebo (Cu IUD, prevention of HMB), Outcome 4: Side effects

Comparison 14: Tolfenamic vs placebo (Cu IUD, prevention of HMB), Outcome 1: Number of pads/day

Comparison 14: Tolfenamic vs placebo (Cu IUD, prevention of HMB), Outcome 2: Menstruation "more abundant than normal"

Comparison 14: Tolfenamic vs placebo (Cu IUD, prevention of HMB), Outcome 3: Clots in menstrual blood

Comparison 15: Aspirin vs paracetamol (Cu IUD, prevention of HMB), Outcome 1: Menstrual blood loss (alkaline hematin)
| Occurence of HMB (%) | ||
| Study | 2g tranexamic | 1g tranexamic |
|---|---|---|
| Alkaline hematin | ||
| Lin 2007 | 20 | 11.76 |
| PBAC | ||
| Lin 2007 | 26.79 | 45.83 |
Comparison 16: 2 g tranexamic vs 1 g tranexamic (Cu IUD, prevention HMB), Outcome 1: Occurence of HMB (%)

Comparison 17: Ulipristal acetate (CDB‐2914) vs placebo (LNG IUD, prevention of HMB), Outcome 1: Percentage days bleeding or spotting

Comparison 17: Ulipristal acetate (CDB‐2914) vs placebo (LNG IUD, prevention of HMB), Outcome 2: Longest consecutive run of days without bleeding or spotting
| Median number of bleeding days | |||
| Study | tranexamic acid (n=55) | mefenamic acid (n=57) | placebo (n=56) |
|---|---|---|---|
| Sordal 2013 | 8 | 10 | 11.5 |
Comparison 18: Tranexamic acid vs mefenamic acid (LNG IUD, prevention of HMB), Outcome 1: Median number of bleeding days
| Median number of bleeding and spotting days | |||
| Study | Naproxen (n=35) | Estradiol (n=34) | Placebo (n=37) |
|---|---|---|---|
| Madden 2012 | 27.5 | 44 | 32 |
Comparison 19: Naproxen vs estradiol (LNG IUD, prevention of HMB), Outcome 1: Median number of bleeding and spotting days

Comparison 19: Naproxen vs estradiol (LNG IUD, prevention of HMB), Outcome 2: Satisfied with bleeding pattern at 12 weeks

Comparison 19: Naproxen vs estradiol (LNG IUD, prevention of HMB), Outcome 3: Side effects
| Percentage bleeding and spotting days | ||
| Study | Mifepristone | Vitamin B |
|---|---|---|
| Papaikonomou 2018 | Fewer women reported bleeding or spotting. Less days with normal or heavy intensity bleeding | More bleeding or spotting days. |
Comparison 20: Mifepristone vs vitamin B (LNG IUD, prevention of HMB), Outcome 1: Percentage bleeding and spotting days

Comparison 21: Tolfenamic acid vs placebo (Cu IUD, prevention of pain), Outcome 1: Menstruation "more painful than normal"

Comparison 21: Tolfenamic acid vs placebo (Cu IUD, prevention of pain), Outcome 2: Side effects

Comparison 22: Ibuprofen vs placebo (Cu IUD, prevention of pain), Outcome 1: Reduction in menstrual cramps

Comparison 23: Ibuprofen vs placebo (Cu IUD,prevention of bleed and pain, IUD removal), Outcome 1: IUD removal by 26 weeks due to pain or increased blood loss

Comparison 23: Ibuprofen vs placebo (Cu IUD,prevention of bleed and pain, IUD removal), Outcome 2: IUD removal due to pain or increased blood loss by 52 weeks
| Interventions versus comparisons | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Vitamin B1 vs placebo | |||||
| Menstrual blood loss Number of pads (diary record) Follow‐up: 1 month after completion of intervention for 3 months | The mean number of pads was 19 pads | MD 7 pads fewer | ‐ | 110 | ⨁⨁◯◯ |
| Duration of bleeding Number of bleeding days (diary record)
Follow‐up: 1 month after completion of intervention for three months | The mean duration of bleeding was 8 days | MD 2 days fewer | ‐ | 110 | ⨁⨁◯◯ |
| Adverse events or side effects | None reported |
|
|
|
|
| Mefenamic acid vs tranexamic acid | |||||
| Menstrual blood loss Volume blood loss (pictorial chart in mL)
Follow‐up: after 3rd month of intervention | The mean volume of menstrual blood loss was 160 mL | MD 64.26 mL lower | ‐ | 94 | ⨁⨁◯◯ |
| Duration of bleeding Number of bleeding days (menstrual record)
Follow‐up: after 3rd month of intervention Recorded on daily diary | The mean number of bleeding days was 3.5 to 6.4 days | MD 0.08 days more | ‐ | 152 | ⨁⨁◯◯ |
| Adverse events or side effects | No data available |
|
|
|
|
| Mefenamic acid vs desmopressin | |||||
| Menstrual blood loss Mean reduction of PBAC score Follow‐up: after 3rd month of intervention | The mean reduction of PBAC score was 40.5% in desmopressin and 45.7% in mefenamic acid |
| 24 | ⨁◯◯◯ | |
| Tranexamic acid vs sodium diclofenac | |||||
| Menstrual blood loss Volume of blood loss (alkaline hematin method) Follow‐up: each intervention cycle (cross‐over) for 5 menstrual cycles | The mean blood loss was 102mL | MD 42.7mL lower | ‐ | 38 | ⨁◯◯◯ |
| Duration of bleeding
Follow‐up: each intervention cycle (cross‐over) for 5 menstrual cycles | The mean duration of bleeding was 5.1 days | MD 0 days | ‐ | 38 | ⨁◯◯◯ |
| Side effects: gastrointestinal disturbances (diarrhoea, lower abdominal pain), headache and sweating | 316 per 1000 | 684 per 1000 (356 to 895) | OR 4.69 (1.2 to 18.44) | 38 (1 RCT) | ⨁◯◯◯ |
| Tranexamic acid vs flavonoids | |||||
| Menstrual blood loss PBAC score Follow‐up: each cycle for 3 menstrual cycles | The mean PBAC score was 125 | MD 32 lower | ‐ | 100 | ⨁⨁◯◯ |
| Menstrual blood loss Number of pads per day Follow‐up: each cycle for 3 menstrual cycles | The mean number of pads was 3 pads per day | MD 0.5 pads lower | ‐ | 100 | ⨁⨁◯◯ |
| Duration of bleeding Number of bleeding days Follow‐up: each cycle for 3 menstrual cycles | The mean number of bleed days was 6.8 days | MD 1.4 days lower | ‐ | 100 | ⨁⨁◯◯ |
| Side effects: headache Follow‐up: each cycle for 3 menstrual cycles | 160 per 1000 | 99 per 1000 (33 to 268) | OR 0.58 (0.18 to 1.92) | 100 | ⨁⨁◯◯ |
| Side effects: vomiting Follow‐up: each cycle for 3 menstrual cycles | 180 per 1000 | 140 per 1000 (33 to 268) | OR 0.74 (0.25 to 2.18) | 100 | ⨁⨁◯◯ |
| Tranexamic acid vs active comparators (mefenamic acid, flavonoid, sodium diclofenac) | |||||
| Duration of bleeding Number of bleeding days Follow‐up: 2‐5 menstrual cycles
| The mean number of bleeding days was 5.1 to 6.8 days | MD 0.27 days lower | ‐ | 290 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; PBAC: pictorial blood assessment chart; RCT: randomized controlled trial; vs: versus aDowngraded one level due to unclear risk of selection bias. | |||||
| Interventions vs comparisons | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Ulipristal acetate vs placebo | |||||
| Duration of bleeding Total bleeding in 90 days (bleeding calendar) Follow‐up: 30, 60 and 90 days after treatment initiation | The mean total of bleeding days in 90 days was 29.8 to 39.1 days | MD 9.3 days lower | ‐ | 24 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded one level due to high risk of detection bias. | |||||
| Interventions vs comparisons | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |||
|---|---|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||||
| Mefenamic acid vs Vitex agnus | |||||||
| Menstrual blood loss PBAC score Follow‐up: monthly for 4 months | The mean PBAC score was 89.7 | 2.4 lower | ‐ | 84 | ⨁⨁◯◯ | ||
| Side effects: nausea Follow‐up: monthly for 4 months | 24 per 1000 | 24 per 1000 (1 to 287) | OR 1.00 (0.06 to 16.53) | 84 | ⨁⨁◯◯ | ||
| Side effects: abdominal pain Follow‐up: monthly for 4 months | 24 per 1000 | 8 per 1000 (0 to 167) | OR 0.33 (0.01 to 8.22) | 84 | ⨁⨁◯◯ | ||
| CI: confidence interval; MD: mean difference; OR: odds ratio; PBAC: pictorial blood assessment chart; RCT: randomized controlled trial; vs: versus aDowngraded one level due to unclear reporting bias. | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Tranexamic acid vs sodium diclofenac | |||||
| Pelvic pain Follow‐up: each intervention cycle (cross over) for 5 menstrual cycles | 53 per 1000 | 53 per 1000 | OR 1.00 | 38 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded two levels due to unclear risk of selection, performance and reporting bias and high risk of detection bias. | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Naproxen vs placebo | |||||
| Overall pain relief score (4‐point scale) Follow‐up: each cycle for 3 menstrual cycles | The mean overall pain relief score was 7.9 | MD 4.1 higher | ‐ | 33 | ⨁⨁◯◯ |
| Daily pain relief score (6‐point scale) Follow‐up: each cycle for 3 menstrual cycles | The mean daily pain relief score was 10.8 | 3.1 higher | ‐ | 33 | ⨁⨁◯◯ |
| Need for additional analgesia (self‐recorded) Follow‐up: each cycle for 3 menstrual cycles | 313 per 1000 | 116 per 1000 | OR 0.29 | 33 | ⨁⨁◯◯ |
| Side effects: gastrointestinal symptoms Follow‐up: each cycle for 3 menstrual cycles | 48 per 1000 | 95 per 1000 (9 to 557) | OR 2.11 (0.18 to 25.17) | 33 | ⨁⨁◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded two levels due to unclear risk of selection, performance and reporting bias as well as high risk of detection bias. | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Outcomes |
|---|---|---|---|---|---|
| Ibuprofen vs placebo | |||||
| Menstrual blood loss (alkaline hematin method) Follow‐up: 3 months | The mean menstrual blood loss was 44.7 to 109.2 mL | MD 14.11 mL lower | ‐ | 40 | ⨁◯◯◯ |
| Duration of bleeding (menstrual diary) Follow‐up: 3 months | The mean duration of bleed was 6.4 days | MD 0.2 days lower | ‐ | 28 | ⨁◯◯◯ |
| Side effects: eye and mouth swelling, stomach cramps, fatigue, irritability (diary record) Follow‐up: 3 months | 38 per 1000 | 79 per 1000 (20 to 271) | OR 2.15 (0.5 to 9.31) | 68 (2 RCTs) | ⨁⨁◯◯ |
| Tolfenamic acid vs placebo | |||||
| Menstrual blood loss Menstruation "more abundant than normal" (questionnaire) Follow‐up: 3 months | 658 per 1000 | 510 per 1000 | OR 0.54 | 310 | ⨁◯◯◯ |
| Side effects: dyspepsia, diarrhoea, headache, fatigue (questionnaire) Follow‐up: 3 months | 129 per 1000 | 66 per 1000 | OR 0.48 | ⨁◯◯◯ | |
| Aspirin vs paracetamol | |||||
| Menstrual blood loss (alkaline hematin method) Follow‐up: 3 cycles | The mean menstrual blood loss was 49.5 mL | MD 0.3mL lower | ‐ | 20 | ⨁◯◯◯ |
| Adverse events or side effects | Not reported | ||||
| 2 g tranexamic acid vs 1 g tranexamic acid | |||||
| Menstrual blood loss % occurrence of heavy menstrual bleeding (alkaline hematin method) Follow‐up: each cycle for 3 menstrual cycles | 2 g tranexamic acid: 20 1 g tranexamic acid: 11.76 | 64 | ⨁◯◯◯ | ||
| Menstrual blood loss % occurrence heavy menstrual bleeding (PBAC score) Follow‐up: each cycle for 3 menstrual cycles | 2 g tranexamic acid: 26.79 1 g tranexamic acid: 45.83 | 175 | ⨁◯◯◯ | ||
| Adverse events or side effects | Not reported | ||||
| CI: confidence interval; MD: mean difference; OR: odds ratio; PBAC: pictorial blood assessment chart; RCT: randomized controlled trial; vs: versus aDowngraded one level due to unclear risk of selection and reporting bias. | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Ulipristal acetate vs placebo | |||||
| Percentage days bleeding or spotting (questionnaire) Follow‐up: 1, 3 and 6 months after IUD insertion | The mean percentage days bleeding or spotting was 20.7 | MD 9.5% higher (1.48 higher to 17.52 higher) | ‐ | 118 | ⨁⨁◯◯ |
| Adverse events or side effects | Not reported | ||||
| Tranexamic acid vs mefenamic acid | |||||
| Menstrual blood loss | No data reported | ||||
| Duration of bleeding Median number of bleed days (diary) Follow‐up: 90 days of study assessment followed by 30 days | Tranexamic acid: 8 Mefenamic acid: 10 | 168 | ⨁⨁◯◯ | ||
| Side effects: gastrointestinal disorders, headache, breast tenderness, musculoskeletal disorders Follow‐up: 90 days of study assessment followed by 30 days | 468 per 1000 | 468 per 1000 | OR 1.00 (0.49 to 2.02) | 168 | ⨁⨁◯◯ |
| Mifepristone vs vitamin B | |||||
| Menstrual blood loss | No data reported | ||||
| Duration of bleeding % spotting and bleeding days Follow‐up: 1, 3 and 6 months after IUD insertion | Mifepristone: fewer women reported bleeding or spotting. Fewer days with normal or heavy intensity bleeding Vitamin B: more bleeding or spotting days | 58 | ⨁◯◯◯ | ||
| Adverse events or side effects | Not reported | ||||
| Naproxen vs estradiol | |||||
| Menstrual blood loss | Not reported | ||||
| Duration of bleeding Median number of bleeding and spotting days (diary) Follow‐up: every 4 weeks for 16 weeks | Naproxen: 27.5 Estradiol: 44 | 106 | ⨁◯◯◯ | ||
| Side effects: gastroesophageal reflux Follow‐up: every 4 weeks for 16 weeks | 0 per 1000 | 0 per 1000 | OR 3.22 (0.13 to 81.19) | 86 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded one level for imprecision as effects were measured from one trial. | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
|---|---|---|---|---|---|
| Risk with comparisons | Risk with interventions | ||||
| Ibuprofen vs placebo | |||||
| Reduction in painful menstruation Follow‐up: end of 1st, 2nd and 3rd months | 200 per 1000 | 200 per 1000 | OR 1.00 | 20 | ⨁⨁◯◯ |
| Tolfenamic acid vs placebo | |||||
| Menstruation "more painful than normal" Follow‐up: 3 months | 387 per 1000 | 310 per 1000 | OR 0.71 | 310 | ⨁◯◯◯ |
| CI: confidence interval; MD: mean difference; OR: odds ratio; RCT: randomized controlled trial; vs: versus aDowngraded one level due to unclear risk of selection and reporting bias. | |||||
| Trial | Experimental Intervention | Comparison Intervention | IUD type | Duration of intervention | Follow‐up | Outcome |
|---|---|---|---|---|---|---|
| Effectiveness trials | ||||||
| Bleeding trials | ||||||
| RCT with cross‐over | Oral naproxen 1250 mg/day | Oral naproxen 500 mg on 1st day then 750 mg on subsequent days Placebo | Unknown | 4 cycles Each participant took 2 of the 3 treatments, each for 2 menstrual cycles. Each regimen was begun on the 1st day of menstrual bleeding and continued for a total of 5 days. | After every 2 menstrual cycles | Percentage reduction in menstrual blood loss |
| RCT | Oral ulipristal acetate 5 mg/day for 5 days | Oral placebo | LNG IUD | 5 days, bleeding was assessed at 30 days, 60 days and 70 days | 90 days | Total bleeding days |
| RCT | Oral vitamin B1 100 mg/day during the 2nd, 3rd and 4th months following insertion of the IUD | Oral placebo during the 2nd, 3rd and 4th months following insertion of the IUD | Cu IUD | 3 cycles | 1 month after completion of intervention | Number of pads used Number of spotting days Duration of bleeding |
| Pain trials | ||||||
| RCT | Oral naproxen sodium 550 mg initially, then 275 mg every 6 hours as needed for uterine pain | Placebo (lactose) | Unknown IUD type | 3 cycles | No details | Overall and daily pain relief score (6‐point Likert scale) |
| RCT with cross‐over | Oral naproxen 500 mg followed by 250 mg 2‐4 times a day, with a maximum of 1250 mg, taken at the first sign of menstrual distress. | Oral placebo taken at the first sign of menstrual distress. | Cu IUD | 4 cycles Participant took an intervention for 2 cycles then crossed over to the other intervention for 2 cycles | After 2nd and 4th menstrual cycle | Pain relief (5‐point Likert scale) |
| Comparative effectiveness trials | ||||||
| Bleeding trials | ||||||
| RCT | Oral tranexamic acid 500 mg, 1 tablet 6‐hourly during the 1st 3 days of menstrual bleeding | Oral micronized flavonoid 500 mg, 1 tablet 6‐hourly during the 1st 3 days of menstrual bleeding | Cu IUD | 3 cycles | No details | PBAC score Number of pads used/day Number of bleeding days |
| RCT | Oral mefenamic acid, 250 mg; 1 capsule every 8 hours on the first 3 days of menstruation | Oral tranexamic acid, 250 mg; 1 capsule every 8 hours on the first 3 days of menstruation | Cu IUD | 2 cycles | No details | PBAC score Number of bleeding days |
| RCT | Desmopressin 300 mcg intranasal spray each morning for the first 5 days after start of menstruation | Oral mefenamic acid 1500 mg/day for the first 5 days after the start of menstruation. | Cu IUD | 3 months | Monthly for 3 months | PBAC score |
| RCT | Oral tranexamic acid 500 mg 3 times/day for 3‐5 days based on the duration of bleeding | Oral mefenamic acid 500 mg 3 times/day for 3‐5 days based on the duration of bleeding | Cu IUD | 3 months | Monthly for 3 months | Volume of blood loss Duration of bleeding |
| RCT | Oral mefenamic acid 250 mg 3 times/day from the 1st day of menstruation until day 8 | Oral Vitex agnus 3 times/day from the 1st day of menstruation until day 8 | Unknown IUD type | 4 months | No details | PBAC score |
| RCT with cross‐over | Oral tranexamic acid 4.5 g/day for 5 days | Oral sodium diclofenac 150 mg on day 1 then 75 mg/day on days 2‐4 Placebo | Cu IUD | 5 months Each participant received placebo for 1 month, 2 months of tranexamic acid, and 2 months of sodium diclofenac | No details | Menstrual blood loss (alkaline hematin) Duration of bleeding |
| Cu IUD: copper intrauterine device; HMB: heavy menstrual bleeding; IUD: intrauterine device; LNG IUD: levonorgestrel intrauterine device; PBAC: pictorial blood loss assessment chart | ||||||
| Trial | Experimental intervention | Comparison intervention | IUD type | Duration of intervention | Follow‐up | Outcomes |
|---|---|---|---|---|---|---|
| Effectiveness trials | ||||||
| Bleeding trials | ||||||
| RCT | Oral ibuprofen 1200 mg/day at the beginning of menstruation and to continue to end of bleeding for a maximum of 10 days. | Oral placebo at the beginning of menstruation and to continue to end of bleeding for a maximum of 10 days. | Cu IUD | 3 cycles | No details | Menstrual blood loss (alkaline hematin) Length of menstruation |
| RCT with cross‐over | Oral ibuprofen 1600 mg/day starting with bleeding and continuing until end of bleeding or maximum of 7 days | Placebo starting with bleeding and continuing until end of bleeding or maximum of 7 days | Cu IUD Cu Lippes loop | 3 cycles Each participant had 1 month of observation, 1 month on ibuprofen or placebo, and 1 month crossed over to the alternative treatment. | End of month 1, 2, 3 | Menstrual blood loss (alkaline hematin) |
| RCT | Oral CDB‐2914 50 mg/day | Oral placebo | LNG IUD | Intervention taken for 3 consecutive days with separate treatments starting 21, 49 and 77 days after LNG IUD insertion | 1,3 and 6 months after IUD insertion | Percentage days bleeding/ spotting, removal of LNG IUD within 6 months; the longest run of amenorrhoea in the 64 days after third treatment, side effects |
| Bleeding and pain trials | ||||||
| RCT | Oral ibuprofen 1200 mg/day to be taken with the first 6 menstruations after IUD insertion and for a maximum of 5 days at a time. | Oral placebo to be taken with the first 6 menstruations after IUD insertion and for a maximum of 5 days at a time. | Cu IUD | 6 cycles | 6, 13, 26 and 52 weeks after IUD insertion | IUD removal within 12 months of insertion due to HMB/pain |
| RCT | Oral tolfenamic acid 600 mg/day starting at IUD insertion and continuing for 7 days; this was to be repeated during the next 3 menstruations. | Placebo starting at IUD insertion and continuing for 7 days; this was to be repeated during the next 3 menstruations | Cu IUD | 3 cycles | No details | Number of pads used, menstruation more abundant than normal, clots, menstruation more painful than normal |
| Comparative effectiveness trials | ||||||
| Bleeding trials | ||||||
| RCT with cross‐over | Oral aspirin 1500 mg/day | Oral paracetamol 1500 mg/day Placebo | Cu IUD | 3 cycles Interventions taken on day 1 of menstruation and continued for the duration of bleeding. Each participant received each treatment in alternating order. | No details | Menstrual blood loss (alkaline hematin) |
| RCT | Oral tranexamic acid 2 g/day, taken for the 1st 5 days of 3 consecutive cycles after IUD insertion | Oral tranexamic acid 1 g/day, taken for the 1st 5 days of 3 consecutive cycles after IUD insertion | Cu IUD | 3 cycles | No details | Percentage occurrence of HMB by alkaline hematin and PBAC |
| RCT | Oral naproxen 500 mg twice a day first 5 days of a 4‐week period | Transdermal estradiol 0.1 mg on day after insertion of IUD, changing it weekly Oral placebo twice a day | LNG IUD | First 12 weeks of IUD use | Telephone surveys at 4, 8, and 16 weeks and an in‐person follow‐up visit at 12 weeks | Median bleed days, patient satisfaction, continuation rates of IUD |
| RCT | Oral 50 mg mifepristone every other day starting on the 1st day of the menstrual cycle for the pre‐treatment period | Oral vitamin B every other day starting on the 1st day of the menstrual cycle for the pre‐treatment period | LNG IUD | 2 months (corresponding to 2 menstrual cycles i.e. 2 × 28 days) prior to insertion and until 3 days (± 2 days) following the LNG IUD insertion | Monthly for the first 3 months, 6 months post‐LNG IUD insertion and 12 months end‐of‐trial evaluation | Bleeding and spotting days |
| RCT | Oral tranexamic acid 1500 mg/day, taken on the 1st day of a bleeding or spotting episode until bleeding or spotting stopped | Oral mefenamic acid 1500 mg/day, taken on the 1st day of a bleeding or spotting episode until bleeding or spotting stopped Oral placebo (lactose and magnesium stearate), taken on the 1st day of a bleeding or spotting episode until bleeding or spotting stopped | LNG IUD | 90 days | No details | Median reduction of bleed days and length of bleed days, satisfaction with drug/placebo, occurrence of pain, number of days pain medication used to alleviate pain, adverse effects |
| Cu IUD: copper intrauterine device; HMB: heavy menstrual bleeding; IUD: intrauterine device; LNG IUD: levonorgestrel intrauterine device; PBAC: pictorial blood loss assessment chart | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Number of pads/day Show forest plot | 1 | 110 | Mean Difference (IV, Random, 95% CI) | ‐7.00 [‐8.50, ‐5.50] |
| 1.2 Number of spotting days Show forest plot | 1 | 110 | Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐1.94, ‐1.26] |
| 1.3 Number of bleeding days Show forest plot | 1 | 110 | Mean Difference (IV, Random, 95% CI) | ‐2.00 [‐2.38, ‐1.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 "More" menstrual flow Show forest plot | 1 | 40 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.00, 1.78] |
| 2.2 Side effects Show forest plot | 1 | 336 | Odds Ratio (M‐H, Random, 95% CI) | 1.91 [0.72, 5.06] |
| 2.2.1 Irregular flow | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 2.24 [0.36, 13.78] |
| 2.2.2 Fluor | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 3.15 [0.12, 81.74] |
| 2.2.3 Tender vagina | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 3.15 [0.12, 81.74] |
| 2.2.4 Gastrointestinal symptoms | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 2.11 [0.18, 25.17] |
| 2.2.5 Dizziness | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 3.15 [0.12, 81.74] |
| 2.2.6 Trembling legs | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 3.15 [0.12, 81.74] |
| 2.2.7 Blurry vision | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.06, 17.12] |
| 2.2.8 Sore lips | 1 | 42 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.01, 8.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Volume of blood loss Show forest plot | 1 | 94 | Mean Difference (IV, Random, 95% CI) | ‐64.26 [‐105.65, ‐22.87] |
| 3.2 PBAC score Show forest plot | 1 | 58 | Mean Difference (IV, Random, 95% CI) | ‐8.19 [‐25.24, 8.86] |
| 3.3 Number of bleeding days Show forest plot | 2 | 152 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.27, 0.42] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Mean reduction of PBAC score (%) Show forest plot | 1 | Other data | No numeric data | |
| 4.2 Side effects: headache and insomnia Show forest plot | 1 | 24 | Odds Ratio (M‐H, Random, 95% CI) | 0.11 [0.00, 2.36] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 Menstrual blood loss (alkaline hematin) Show forest plot | 1 | 38 | Mean Difference (IV, Random, 95% CI) | ‐42.70 [‐73.33, ‐12.07] |
| 5.2 Duration of menstruation Show forest plot | 1 | 38 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.62, 0.62] |
| 5.3 Side effects Show forest plot | 1 | 38 | Odds Ratio (M‐H, Random, 95% CI) | 4.69 [1.20, 18.44] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 PBAC score Show forest plot | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐32.00 [‐39.84, ‐24.16] |
| 6.2 Number of pads/day Show forest plot | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.91, ‐0.09] |
| 6.3 Number of bleeding days Show forest plot | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐1.40 [‐1.93, ‐0.87] |
| 6.4 Side effects Show forest plot | 1 | 200 | Odds Ratio (M‐H, Random, 95% CI) | 0.67 [0.30, 1.48] |
| 6.4.1 Headache | 1 | 100 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.18, 1.92] |
| 6.4.2 Vomiting | 1 | 100 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.25, 2.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Number of bleeding days Show forest plot | 4 | 290 | Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐1.14, 0.60] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 8.1 Duration of days until bleeding stops Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐3.30 [‐9.07, 2.47] |
| 8.2 Total bleeding in 90 days Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐9.30 [‐26.76, 8.16] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 9.1 Blood loss reduction (%) Show forest plot | 1 | Other data | No numeric data | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 10.1 PBAC score Show forest plot | 1 | 84 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐13.77, 8.97] |
| 10.2 Side effects Show forest plot | 1 | 168 | Odds Ratio (M‐H, Random, 95% CI) | 0.62 [0.07, 5.13] |
| 10.2.1 Nausea | 1 | 84 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.06, 16.53] |
| 10.2.2 Abdominal pain | 1 | 84 | Odds Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 8.22] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 11.1 Pelvic pain Show forest plot | 1 | 38 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.06, 17.25] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 12.1 Overall pain relief score Show forest plot | 1 | 33 | Mean Difference (IV, Random, 95% CI) | 4.10 [0.91, 7.29] |
| 12.2 Daily pain relief score Show forest plot | 1 | 33 | Mean Difference (IV, Random, 95% CI) | 3.10 [0.27, 5.93] |
| 12.3 Pain relief Show forest plot | 1 | 40 | Odds Ratio (M‐H, Random, 95% CI) | 2.79 [0.77, 10.04] |
| 12.4 Need for analgesia Show forest plot | 1 | 33 | Odds Ratio (M‐H, Random, 95% CI) | 0.29 [0.05, 1.80] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 13.1 Menstrual blood loss (alkaline hematin) Show forest plot | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐14.11 [‐36.04, 7.82] |
| 13.1.1 Cu IUD | 1 | 20 | Mean Difference (IV, Random, 95% CI) | ‐9.47 [‐34.45, 15.51] |
| 13.1.2 Lippes Loop | 1 | 20 | Mean Difference (IV, Random, 95% CI) | ‐29.68 [‐75.44, 16.08] |
| 13.2 Duration of bleeding Show forest plot | 1 | 28 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.40, 1.00] |
| 13.3 Median menstrual blood loss (alkaline hematin) Show forest plot | 1 | Other data | No numeric data | |
| 13.3.1 Fincoid | 1 | Other data | No numeric data | |
| 13.3.2 ML Cu 375 | 1 | Other data | No numeric data | |
| 13.4 Side effects Show forest plot | 2 | 108 | Odds Ratio (M‐H, Random, 95% CI) | 2.15 [0.50, 9.31] |
| 13.4.1 Eye and mouth swelling | 1 | 40 | Odds Ratio (M‐H, Random, 95% CI) | 3.15 [0.12, 82.16] |
| 13.4.2 Stomach cramps | 1 | 40 | Odds Ratio (M‐H, Random, 95% CI) | 3.15 [0.12, 82.16] |
| 13.4.3 Tired, irritable | 1 | 28 | Odds Ratio (M‐H, Random, 95% CI) | 1.67 [0.25, 11.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 14.1 Number of pads/day Show forest plot | 1 | 122 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐1.57, ‐0.43] |
| 14.2 Menstruation "more abundant than normal" Show forest plot | 1 | 310 | Odds Ratio (M‐H, Random, 95% CI) | 0.54 [0.34, 0.85] |
| 14.3 Clots in menstrual blood Show forest plot | 1 | 310 | Odds Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.68] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 15.1 Menstrual blood loss (alkaline hematin) Show forest plot | 1 | 20 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐26.16, 25.56] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 16.1 Occurence of HMB (%) Show forest plot | 1 | Other data | No numeric data | |
| 16.1.1 Alkaline hematin | 1 | Other data | No numeric data | |
| 16.1.2 PBAC | 1 | Other data | No numeric data | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 17.1 Percentage days bleeding or spotting Show forest plot | 1 | 118 | Mean Difference (IV, Random, 95% CI) | 9.50 [1.48, 17.52] |
| 17.2 Longest consecutive run of days without bleeding or spotting Show forest plot | 1 | 118 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐6.93, 3.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 18.1 Median number of bleeding days Show forest plot | 1 | Other data | No numeric data | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 19.1 Median number of bleeding and spotting days Show forest plot | 1 | Other data | No numeric data | |
| 19.2 Satisfied with bleeding pattern at 12 weeks Show forest plot | 1 | 73 | Odds Ratio (M‐H, Random, 95% CI) | 1.10 [0.40, 3.03] |
| 19.3 Side effects Show forest plot | 1 | 86 | Odds Ratio (M‐H, Random, 95% CI) | 3.22 [0.13, 81.19] |
| 19.3.1 Gastroesophageal reflux disease (GERD) | 1 | 86 | Odds Ratio (M‐H, Random, 95% CI) | 3.22 [0.13, 81.19] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 20.1 Percentage bleeding and spotting days Show forest plot | 1 | Other data | No numeric data | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 21.1 Menstruation "more painful than normal" Show forest plot | 1 | 310 | Odds Ratio (M‐H, Random, 95% CI) | 0.71 [0.44, 1.14] |
| 21.2 Side effects Show forest plot | 1 | 366 | Odds Ratio (M‐H, Random, 95% CI) | 0.42 [0.02, 9.29] |
| 21.2.1 Dyspepsia and diarrhoea | 1 | 122 | Odds Ratio (M‐H, Random, 95% CI) | 9.96 [0.52, 189.04] |
| 21.2.2 Headache | 1 | 122 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.00, 1.60] |
| 21.2.3 Depression | 1 | 122 | Odds Ratio (M‐H, Random, 95% CI) | 0.09 [0.00, 1.60] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 22.1 Reduction in menstrual cramps Show forest plot | 1 | 20 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.11, 8.95] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 23.1 IUD removal by 26 weeks due to pain or increased blood loss Show forest plot | 1 | 1962 | Odds Ratio (M‐H, Random, 95% CI) | 0.96 [0.66, 1.38] |
| 23.2 IUD removal due to pain or increased blood loss by 52 weeks Show forest plot | 1 | 1962 | Odds Ratio (M‐H, Random, 95% CI) | 1.25 [0.93, 1.69] |

