درمان ارتودنسی برای دیپ بایت (deep bite) و عقبرفتگی دندانهای فوقانی جلویی در کودکان
چکیده
پیشینه
اختلال در بسته شدن (malocclusion) کلاس II گروه 2 (Class II division 2) دهان، که با دندانهای فوقانی جلویی که به عقب کشیده میشوند (به سمت سقف دهان کشیده شدهاند) و افزایش اووربایت (overbite) شناخته میشود، میتواند باعث مشکلات دهانی شده و بر ظاهر افراد تاثیر بگذارد.
این مشکل را میتوان با استفاده از بریسهای دندانی مخصوص (وسایل فانکشنال) که دندانهای فوقانی جلویی را حرکت داده و رشد فک بالا یا پائین، یا هر دو، را تغییر میدهند، اصلاح کرد. اکثر انواع وسایل فانکشنال متحرک هستند و این روش درمانی اغلب نیازی به کشیدن هیچیک از دندانهای دائمی ندارد. برای اطمینان از بهترین نتیجه، ممکن است درمان بیشتر با بریسهای ثابت لازم باشد.
یک رویکرد جایگزین این است که با حرکت دادن دندانهای مولر به عقب، فضایی را برای اصلاح دندانهای جلویی ایجاد کنیم. این کار با اعمال نیرو به دندانها از پشت سر با استفاده از یک بریس سر (headgear) و انتقال این نیرو به بخشی از یک بریس دندانی ثابت یا متحرک که به دندانهای عقب متصل است، انجام میشود. درمان مذکور ممکن است با یا بدون کشیدن دندان دائمی انجام شود.
اگر امکان استفاده از headgear وجود نداشته باشد، دندانهای عقبی ممکن است با بندهای متصل به یک بار (bar) ثابت در پشت سقف دهان یا در تماس با جلوی سقف دهان در جای خود نگه داشته شوند. این درمان معمولا نیاز به دو دندان دائمی دارد که از میانه آرک (arch) بالایی کشیده شوند (از هر طرف یک دندان).
اهداف
تعیین اینکه درمان ارتودنسی که در آن نیازی به کشیدن هیچیک از دندانهای دائمی نباشد، نتیجهای را ارائه میکند که تفاوتی با عدم‐استفاده از درمانهای ارتودنسی یا درمان ارتودنسی با کشیدن دندانهای دائمی در کودکان مبتلا به اختلال در بسته شدن کلاس II گروه 2 دهان نداشته باشد یا خیر.
روشهای جستوجو
متخصص اطلاعات پایگاه سلامت دهان در کاکرین بانکهای اطلاعاتی زیر را جستوجو کرد: پایگاه ثبت کارآزماییهای گروه سلامت دهان در کاکرین (تا 13 نوامبر 2017)، پایگاه ثبت مرکزی کارآزماییهای کنترل شده کاکرین (CENTRAL) (کتابخانه کاکرین، شماره 10، 2017)؛ MEDLINE Ovid (1946 تا 13 نوامبر 2017)، و Embase Ovid (1980 تا 13 نوامبر 2017). برای شناسایی کارآزماییهای منتشر نشده یا در حال انجام، پایگاه ثبت کارآزماییهای بالینی در حال انجام مؤسسات ملی سلامت ایالات متحده (ClinicalTrials.gov) و پلتفرم بینالمللی پایگاه ثبت کارآزماییهای بالینی سازمان جهانی بهداشت (apps.who.int/trialsearch) جستوجو شدند. همچنین با محققان بینالمللی که ممکن بود در هر کارآزمایی بالینی مربوط به کلاس II گروه 2 حضور داشته باشند تماس گرفتیم.
معیارهای انتخاب
کارآزماییهای تصادفیسازی و کنترل شده (randomised controlled trials; RCTs) و کارآزماییهای بالینی کنترل شده (controlled clinical trials; CCTs) مربوط به درمانهای ارتودنسی جهت اصلاح دندانهای deep bite و عقبرفتگی دندانهای فوقانی جلویی در کودکان.
گردآوری و تجزیهوتحلیل دادهها
دو نویسنده مرور بهطور مستقل از هم نتایج جستوجو را برای یافتن مطالعات واجد شرایط غربالگری کردند، و دادهها را استخراج و خطر سوگیری (bias) کارآزماییهای وارد شده را ارزیابی کردند. هدف این بود که از متاآنالیز اثرات‐تصادفی برای موارد زیر استفاده کنیم؛ نشان دادن تخمین اثرگذاری درمان بر اساس میانگین تفاوتها برای پیامدهای پیوسته و خطر نسبی برای پیامدهای دو‐حالتی، با 95% فاصله اطمینان (CI)؛ و بررسی هر گونه ناهمگونی بالینی یا روششناسی.
نتایج اصلی
ما هیچ RCT یا CCT را شناسایی نکردیم که درمان اختلال در بسته شدن کلاس II گروه 2 دهان را در کودکان ارزیابی کرده باشد.
نتیجهگیریهای نویسندگان
هیچ شواهدی برگرفته از کارآزماییهای بالینی برای توصیه به یا رد استفاده از هر نوع درمان ارتودنسی در اصلاح اختلال در بسته شدن کلاس II گروه 2 دهان در کودکان وجود ندارد. این وضعیت بعید است که تغییر کند، زیرا طراحی و انجام کارآزماییها برای ارزیابی بهترین مدیریت اختلال در بسته شدن کلاس II گروه 2 دهان چالشبرانگیز هستند، چرا که شیوع این وضعیت پائین بوده، و مشکلاتی در ورود افراد به مطالعات و مسائل اخلاقی با تصادفیسازی کردن آنها وجود دارد.
PICO
خلاصه به زبان ساده
درمان ارتودنسی برای دیپ بایت (deep bite) و عقبرفتگی دندانهای فوقانی جلویی در کودکان
پیشینه
ارتودنسی با رشد فکها و صورت، رشد دندانها، و نحوه متصل شدن دندانها و فکها مرتبط است. در حالت ایدهآل، دندانهای bite پائین جلویی به وسط سطح پشتی دندانهای فوقانی جلویی قفل میشوند. هنگامی که دندانهای bite پائین جلویی نسبت به حالت ایدهآل جلوتر از سطح پشتی دندانهای فوقانی قرار گیرند، به عنوان deep bite کلاس II شناخته میشود. اختلال در بسته شدن کلاس II گروه 2 دهان با دندانهای جلویی فوقانی که رو به عقب هستند (به سمت سقف دهان کشیده شدهاند) و افزایش اووربایت (overbite) (همپوشانی عمودی دندانهای جلویی) شناخته میشود، که میتواند باعث مشکلات دهانی شده و روی ظاهر افراد تاثیر بگذارد.
این مشکل را میتوان با استفاده از بریسهای دندانی مخصوص (وسایل فانکشنال) که دندانهای فوقانی جلویی را حرکت داده و رشد فک بالا یا پائین، یا هر دو، را تغییر میدهند، اصلاح کرد. این بریسها را میتوان از دهان خارج کرد و این روش معمول نیازی به حذف هیچ یک از دندانهای دائمی ندارد. برای اطمینان از بهترین نتیجه، ممکن است درمان بیشتر با بریسهای ثابت لازم باشد.
یک رویکرد جایگزین این است که با حرکت دادن دندانهای مولر به عقب، فضایی را برای اصلاح دندانهای جلویی ایجاد کنیم. این کار با اعمال نیرو به دندانها از پشت سر با استفاده از یک بریس سر (headgear) و انتقال این نیرو به بخشی از یک بریس دندانی ثابت یا متحرک که به دندانهای عقب متصل است، انجام میشود. درمان مذکور ممکن است با یا بدون کشیدن دندان دائمی انجام شود.
اگر استفاده از headgear امکانپذیر نباشد، دندانهای عقبی را میتوان با بندهای متصل به یک قوس ثابت در پشت سقف دهان یا در تماس با جلوی سقف دهان نگاه داشت. این درمان معمولا نیاز به دو دندان دائمی دارد که از میانه آرک (arch) بالایی کشیده شوند (از هر طرف یک دندان).
هدف
این مطالعه مروری کاکرین را انجام دادیم تا ببینیم درمان ارتودنسی بدون حذف دندان دائمی اثرات متفاوتی نسبت به عدم استفاده از درمانهای ارتودنسی یا درمان ارتودنسی با حذف دندانهای دائمی، در کودکان مبتلا به اختلال در بسته شدن کلاس II گروه 2 دهان دارد یا خیر.
روش انجام
متون علمی را تا 13 نوامبر 2017 جستوجو کرده و هیچ مطالعهای را مربوط به این مطالعه مروری نیافتیم.
نتایج
هیچ شواهد علمی برای نشان دادن اینکه درمان ارتودنسی، که بدون حذف دندانهای دائمی انجام میشود، بهتر یا بدتر از عدم استفاده از درمان ارتودنسی یا درمان ارتودنسی با کشیدن دندانهای دائمی، در کودکان مبتلا به اختلال در بسته شدن کلاس II گروه 2 دهان است، وجود ندارد.
نتیجهگیریهای نویسندگان
در حال حاضر هیچ شواهدی از کارآزماییهای بالینی وجود ندارد که هر یک از انواع درمان ارتودنسی را برای اصلاح دندانهای کودکانی که دارای deep bite بوده و دندانهای جلویی فوقانی آنها به سمت سقف دهان کشیده شده، توصیه یا آن را رد کند. بعید به نظر میرسد که کارآزماییهایی برای بررسی این درمان انجام شوند، زیرا طراحی و انجام چالشبرانگیزی دارند.
Authors' conclusions
Summary of findings
| Orthodontic intervention (without extraction) compared with extraction or no orthodontic intervention for treating deep bite and retroclined upper front teeth in children | ||||||
| Patient or population: children with deep bite and retroclined upper front teeth Settings: orthodontic clinic Intervention: orthodontic treatment Comparison: extraction or no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Extraction or no treatment | Orthodontic treatment | |||||
| Dento‐occlusal results of treatment, measured with the PAR index | No data are available as no RCTs or CCTs have been conducted. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
Background
Orthodontics is the branch of dentistry concerned with the growth of the jaws and face, the development of the teeth, and the way the teeth and jaws bite together. It also involves treatment of the teeth and jaws when they are irregular or bite in an abnormal way, or both. Teeth may not bite together correctly due to any combination of problems in the positioning of the teeth, jaws, lips, tongue or cheeks; these can be affected in some cases by a habit, such as thumb sucking, or by the way in which people breathe (Shaw 1991). The need for orthodontic treatment can be determined by looking at the effect any particular tooth position has on the life expectancy of the teeth or by the effect that the appearance of the teeth has on how people feel about themselves, or both (Shaw 1991).
Description of the condition
Ideally the lower front teeth bite in the middle of the back surface of the upper front teeth. When the lower front teeth bite further behind the upper front teeth than ideal, this is known as a Class II malocclusion. The upper jaw can be too far forward or, more usually, the lower jaw is too far back. The upper front teeth may stick out (Class II division 1 malocclusion) if the lower lip catches behind them or as a result of a habit, such as thumb‐sucking (Shaw 1980). Management of prominent upper front teeth (Class II division 1 malocclusion) in children is the subject of a separate systematic review (Thiruvenkatachari 2013).
A Class II division 2 malocclusion is a type of orthodontic problem characterised by retroclined (tilted toward the roof of the mouth) upper front teeth and an increased overbite (vertical overlap of the front teeth), although there is variation in the severity of each of these (Millett 2012; Bilgic 2015; Dimberg 2015). Aesthetic impairments and trauma to the palatal or lower labial gingivae are frequently reported by people with this problem. Sometimes the deep overbite is so severe that the front teeth bite into the gums either behind the upper front teeth or in front of the lower front teeth producing damage (traumatic overbite) (Wragg 1990). The incidence of Class II division 2 malocclusion is reported to be about 10% within the UK population (Houston 1996), but prevalence of 18% has been reported in the Croatian population (Legovic 1999). Recent Swedish and Turkish studies have reported lower prevalence, from 1.8% to 4.7% (Bilgic 2015; Dimberg 2015). This type of malocclusion has a strong genetic link (Markovic 1992; Mossey 1999).
The appearance of the upper front teeth and the deep bite of the upper and lower front teeth are reasons why people with this type of problem seek orthodontic treatment (O'Brien 1993). Class II division 2 malocclusion is also associated with a greater percentage of upper permanent canines failing to erupt as a result of them following an abnormal pathway towards the palate/roof of the mouth (Mossey 1999; Al‐Nimri 2005).
Correction of the Class II division 2 malocclusion may be carried out using several types of orthodontic (dental brace) treatment, but the evidence regarding management is weak and highly biased (Millett 2012). People with severe Class II division 2 malocclusions may require surgery to the jaws in combination with orthodontics.
Description of the intervention
In growing children, treatment may sometimes be carried out using special upper and lower dental braces (functional appliances) that can be removed from the mouth (Dyer 2001). They usually work by correcting the position of the upper and lower front teeth and modifying the growth of the upper or lower jaws, or both (growth modification). In many cases this treatment does not involve taking out any permanent teeth but often further treatment is needed with fixed braces to get the best result; such braces are glued to the teeth.
In other cases, treatment aims to move the molar teeth backwards to provide space for the correction of the front teeth. This may be carried out by applying a force to the teeth and jaws from the back of the head using a head brace (headgear) and transmitting this force to part of a fixed or removable dental brace that is attached to the back teeth (Litt 1984). This treatment may or may not involve the removal of permanent teeth.
Other options do exist and may include fixed brace treatment without extraction of permanent teeth, with neither functional appliances nor headgear (Selwyn‐Barnett 1996).
As an alternative to headgear, the back teeth can be held back in other ways such as with an arch across the roof of the mouth or in contact with the front of the roof of the mouth which links the two back teeth. Often in these cases, two permanent teeth are taken out from the middle of the upper arch (one on each side) to provide room to correct the position of the upper front teeth (Paquette 1992).
In severe cases, particularly in adults, treatment may require a combination of dental braces and surgery to the jaws to correct the position of the teeth and the bite (Arvystas 1979). Our review does not evaluate this treatment option, which is not generally used for children.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were considered most clinically important to maintain on the Cochrane Library (Worthington 2015). The orthodontic expert panel identified this review as a priority title (Cochrane Oral Health priority review portfolio).
It is important for orthodontists to establish whether orthodontic treatment alone, carried out without the removal of permanent teeth, in children with a Class II division 2 malocclusion, produces a result that is any different from no orthodontic treatment or orthodontic treatment involving extraction of permanent teeth.
We did not consider combined orthodontic treatment and surgery to the jaws in this review.
Objectives
To evaluate the effectiveness of:
(1) orthodontic treatment only for Class II division 2 malocclusion in children (aged ≤ 16 years) versus no treatment in terms of:
-
dento‐occlusal results of treatment, measured with the Peer Assessment Rating (PAR) index;
-
cephalometric measurements (A Point‐Nasion‐B Point (ANB) change and front teeth inclination changes);
-
participant discomfort;
-
gingival and temporomandibular joint (TMJ) symptoms;
-
side effects;
-
quality of life;
(2) orthodontic treatment only for Class II division 2 malocclusion in children (aged ≤ 16 years) that does not involve extraction of permanent teeth versus orthodontic treatment involving extraction of permanent teeth in terms of:
-
dento‐occlusal results of treatment, measured with the PAR index;
-
number of visits to complete treatment;
-
duration of treatment;
-
cephalometric measurements (ANB change and front teeth inclination changes);
-
participant discomfort;
-
gingival and TMJ symptoms;
-
side effects;
-
quality of life.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and controlled clinical trials (CCTs) of orthodontic treatments to correct deep bite and retroclined upper front teeth in children.
Types of participants
We planned to include trials that recruited participants (80% aged ≤ 16 years) receiving orthodontic treatment to correct deep bite and retroclined upper front teeth.
We planned to exclude trials of participants with a cleft lip or palate, or both, or other craniofacial deformity/syndrome, and trials in which participants had received surgical treatment for their Class II malocclusion.
Types of interventions
Active interventions: orthodontic braces (removable, fixed, functional) or head braces with or without extraction of permanent teeth.
Control: no treatment or delayed treatment.
Types of outcome measures
Primary outcomes
-
Dento‐occlusal results of treatment, measured with the PAR index
Secondary outcomes
-
Number of visits required to complete treatment and the duration of treatment (for objective 2)
-
Cephalometric measurements (ANB change and front teeth inclination changes)
-
Participant discomfort
-
Gingival and TMJ symptoms
-
Side effects
-
Quality of life
Where appropriate, we planned to group outcome data into those measured post‐phase I (growth modification phase) and post‐phase II (fixed brace phase), to record and report post‐retention outcomes and to consider examining outcome data reported at other time points.
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches in the following databases for RCTs and CCTs:
-
Cochrane Oral Health's Trials Register (searched 13 November 2017) (see Appendix 1);
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 10) in the Cochrane Library (searched 13 November 2017) (see Appendix 2);
-
MEDLINE Ovid (1946 to 13 November 2017) (see Appendix 3);
-
Embase Ovid (1980 to 13 November 2017) (see Appendix 4).
No language, publication year or publication status restrictions were imposed.
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, we combined these strategies with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying RCTs and CCTs, as described in Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011).
Searching other resources
The following resources were searched for ongoing trials:
-
US National Institutes of Health Trials Register (ClinicalTrials.gov; searched 13 November 2017) (see Appendix 5);
-
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 13 November 2017) (see Appendix 6).
We planned to contact all first authors of trials in an attempt to identify any unpublished studies and clarify information about published trials (including missing data, method of randomisation, blinding and withdrawals). We intended to screen the references cited in the included studies for any further trials. We wrote to international researchers potentially involved in Class II division 2 malocclusion clinical trials in an attempt to identify unpublished/ongoing RCTs or CCTs.
A separate search for the adverse effects of interventions used was not performed.
Data collection and analysis
Selection of studies
Two review authors (DTM and CMO or SC) independently scanned the titles and abstracts (when available) of all reports identified. When studies appeared to meet the inclusion criteria, or there was insufficient information in the title and abstract to make a decision, we obtained the full report and two review authors assessed it independently to establish whether the inclusion criteria were met or not. We planned to resolve any disagreements by discussion, consulting a third review author if necessary. We had planned to carry out 'Risk of bias' assessments of all studies meeting the inclusion criteria, to extract relevant data and to record all studies rejected at this or subsequent stages in a table of excluded studies, together with the reasons for exclusion. The review authors were not to be blinded to author(s), institution or site of publication.
Data extraction and management
For each trial, we planned to enter the following information on a customised data collection form.
-
Year of publication, country of origin, setting and source of study funding.
-
Details on the type of interventions including appliance type.
-
Details of the participants including demographic characteristics, criteria for inclusion and exclusion, and sample size by study group.
-
Details of the outcomes reported, including method of assessment and time intervals.
-
Details of withdrawals by study group.
-
Details of outcomes, including measures and timepoints.
Assessment of risk of bias in included studies
We planned for two review authors to independently assess random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessors, incomplete outcome data, selective outcome reporting and 'other issues' for each study, using the 'Risk of bias' tool recommended for Cochrane Reviews (Higgins 2011). For blinding, we would have noted any outcomes where participants self‐assessed. We would have categorised the overall risk of bias for each study as follows.
| Risk of bias | Interpretation | Within a study | Across studies |
| Low risk of bias | Plausible bias unlikely to seriously alter the results | Low risk of bias for all key domains | Most information is from studies at low risk of bias |
| Unclear risk of bias | Plausible bias that raises some doubt about the results | Unclear risk of bias for one or more key domains | Most information is from studies at low or unclear risk of bias |
| High risk of bias | Plausible bias that seriously weakens confidence in the results | High risk of bias for one or more key domains | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results |
Measures of treatment effect
We planned to calculate risk ratios, the number needed to treat for an additional beneficial/harmful outcome and corresponding 95% confidence intervals, for dichotomous data, and the mean difference and 95% confidence intervals for continuous data. We would have used the fixed‐effect model for all meta‐analyses unless there were more than three trials included, in which case we would have used a random‐effects model.
Assessment of heterogeneity
We planned to assess heterogeneity using Cochran's test and the I2 statistic, which describes the percentage of total variation across studies that is due to heterogeneity rather than chance. We planned to assess clinical heterogeneity by examining the types of participants and interventions for all outcomes in each study.
Data synthesis
We planned to follow Cochrane statistical guidelines. We would have included only studies of similar comparisons reporting the same outcome measures in meta‐analyses. We planned to analyse the data using Review Manager software (RevMan 2014).
Subgroup analysis and investigation of heterogeneity
We planned a subgroup analysis based on the age (stage of dental development) at which treatment was undertaken.
Sensitivity analysis
We planned to conduct sensitivity analysis based on risk of bias (i.e. including studies at low risk of bias only).
Results
Description of studies
Results of the search
Through our searches and enquiries, we identified 928 references that were potentially relevant to our review. Two review authors (DTM and CMO or SC) screened these records and rejected them all. We were involved in a trial that we mentioned in a previous version of this review, but this was discontinued due to difficulties with patient recruitment (Cunningham 2011). Therefore, we have been unable to identify any RCTs or CCTs for inclusion in this review (Figure 1).
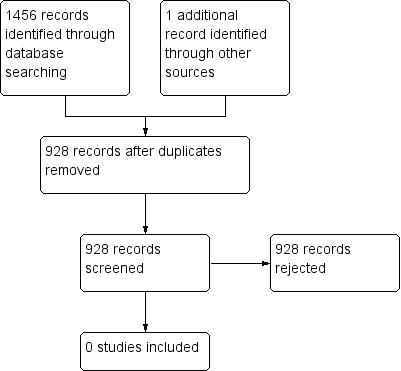
Study flow diagram
Risk of bias in included studies
No RCTs or CCTs were included in this review.
Effects of interventions
No RCTs or CCTs were included in this review (summary of findings Table for the main comparison).
Discussion
We found no RCTs or CCTs assessing i) orthodontic treatment without the removal of permanent teeth versus no treatment or ii) orthodontic treatment involving removal of permanent teeth versus treatment without the removal of permanent teeth. There is no evidence from clinical trials to guide the management of this malocclusion in children. It is unlikely that this situation will change as no trials have been conducted since we first identified the need for trials in the original version of this review, which was published in 2006.

Study flow diagram
| Orthodontic intervention (without extraction) compared with extraction or no orthodontic intervention for treating deep bite and retroclined upper front teeth in children | ||||||
| Patient or population: children with deep bite and retroclined upper front teeth Settings: orthodontic clinic Intervention: orthodontic treatment Comparison: extraction or no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Extraction or no treatment | Orthodontic treatment | |||||
| Dento‐occlusal results of treatment, measured with the PAR index | No data are available as no RCTs or CCTs have been conducted. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||

