Progestogen for treating threatened miscarriage
Abstract
Background
Miscarriage is a common complication encountered during pregnancy. It is defined as spontaneous pregnancy loss before 20 weeks' gestation. Progesterone's physiological role is to prepare the uterus for the implantation of the embryo, enhance uterine quiescence and suppress uterine contractions, hence, it may play a role in preventing rejection of the embryo. Inadequate secretion of progesterone in early pregnancy has been linked to the aetiology of miscarriage and progesterone supplementation has been used as a treatment for threatened miscarriage to prevent spontaneous pregnancy loss. This update of the Cochrane Review first published in 2007, and previously updated in 2011, investigates the evidence base for this practice.
Objectives
To determine the efficacy and the safety of progestogens in the treatment of threatened miscarriage.
Search methods
We searched Cochrane Pregnancy and Childbirth’s Trials Register, ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP) (8 August 2017) and reference lists of retrieved trials.
Selection criteria
Randomised, quasi‐randomised or cluster‐randomised controlled trials, that compared progestogen with placebo, no treatment or any other treatment for the treatment of threatened miscarriage in women carrying singleton pregnancy.
Data collection and analysis
At least two review authors assessed the trials for inclusion in the review, assessed trial quality and extracted the data and graded the body of evidence.
Main results
We included seven trials (involving 696 participants) in this update of the review. The included trials were conducted in different countries, covering the full spectrum of the World Bank's economic classification, which enhances the applicability of evidence drawn from this review. Two trials were conducted in Germany and Italy which are high‐income countries, while four trials were conducted in upper‐middle income countries; two in Iran, one in Malaysia and the fourth in Turkey, and the seventh trial was conducted in Jordan, which is a lower‐middle income country. In six trials all the participants met the inclusion criteria and in the seventh study, we included in the meta‐analysis only the subgroup of participants who met the inclusion criteria. We assessed the body of evidence for the main outcomes using the GRADE tool and the quality of the evidence ranged from very low to moderate. Downgrading of evidence was based on the high risk of bias in six of the seven included trials and a small number of events and wide confidence intervals for some outcomes.
Treatment of miscarriage with progestogens compared to placebo or no treatment probably reduces the risk of miscarriage; (risk ratio (RR) 0.64, 95% confidence interval (CI) 0.47 to 0.87; 7 trials; 696 women; moderate‐quality evidence). Treatment with oral progestogen compared to no treatment also probably reduces the miscarriage rate (RR 0.57, 95% CI 0.38 to 0.85; 3 trials; 408 women; moderate‐quality evidence). However treatment with vaginal progesterone compared to placebo, probably has little or no effect in reducing the miscarriage rate (RR 0.75, 95% CI 0.47 to 1.21; 4 trials; 288 women; moderate‐quality evidence). The subgroup interaction test indicated no difference according to route of administration between the oral and vaginal subgroups of progesterone.
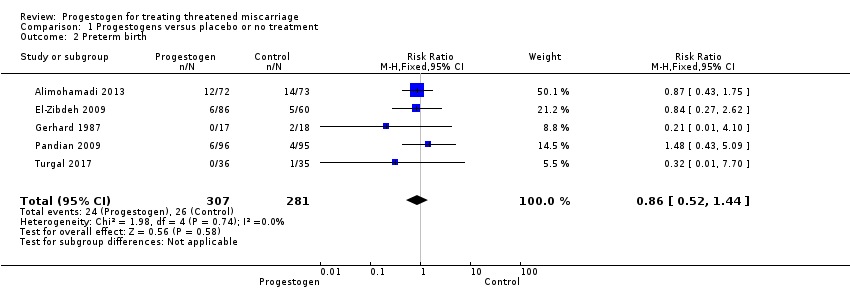
Treatment of miscarriage with the use of progestogens compared to placebo or no treatment may have little or no effect in reducing the rate of preterm birth (RR 0.86, 95% CI 0.52 to 1.44; 5 trials; 588 women; low‐quality evidence).
We are uncertain if treatment of threatened miscarriage with progestogens compared to placebo or no treatment has any effect on the rate of congenital abnormalities because the quality of the evidence is very low (RR 0.70, 95% CI 0.10 to 4.82; 2 trials; 337 infants; very‐low quality evidence).
Authors' conclusions
The results of this Cochrane Review suggest that progestogens are probably effective in the treatment of threatened miscarriage but may have little or no effect in the rate of preterm birth. The evidence on congenital abnormalities is uncertain, because the quality of the evidence for this outcome was based on only two small trials with very few events and was found to be of very low quality.
PICO
Plain language summary
Progestogen for treating threatened miscarriage
What is the issue?
Spontaneous miscarriage occurs in about 15% to 20% of pregnancies. Threatened miscarriage occurs when a mother might be losing her baby at less than 20 weeks' gestation. The symptoms of threatened miscarriage are vaginal bleeding, with or without abdominal pain, while the cervix of the womb is closed and the baby inside the womb is alive. Progesterone is a hormone that is known to prepare the uterus for implantation of the fertilized egg and suppress uterine contractions until term. Medications that mimic the action of progesterone are known as progestogens. Treatment with progestogens may be effective in reducing the rate of miscarriage in women who have threatened miscarriage. This Cochrane Review examines whether progestogens could reduce miscarriage for women with threatened miscarriage, and also addresses the safety of these medications for mother and baby.
Why is this important?
We were interested to investigate if progestogens are effective and safe in the treatment of threatened miscarriage, which may increase the women's chances of having a successful pregnancy and a live birth.
What evidence did we find?
In this review of the literature, up to August 2017, we identified seven randomised trials involving 696 women that compared the use of progestogens in the treatment of threatened miscarriage with either placebo or no treatment. We found that the use of a progestogen probably reduces the rate of spontaneous miscarriage and this was supported by moderate‐quality evidence. Five trials, involving 588 women, reported on the effectiveness of progestogens given for threatened miscarriage in reducing the rate of preterm delivery and showed little or no effect, with low‐quality evidence. Two trials, involving 337 women, reported on the effect of treatment with progestogens given for threatened miscarriage on the rate of occurrence of congenital abnormalities in the newborns. The evidence on congenital abnormalities is uncertain, because the quality of the evidence for this outcome was based on only two small trials with very few events and was found to be of very low quality.
What does this mean?
The evidence suggests that progesterone probably reduces the rate of spontaneous miscarriage but may make little or no difference to the number of preterm deliveries. The evidence for congenital abnormalities is uncertain because the quality of the evidence for this outcome was based on only two small trials with very few events and was found to be of very low quality.
Authors' conclusions
Summary of findings
| Progesterone compared to placebo or no treatment for treating threatened miscarriage | ||||||
| Patient or population: women with threatened miscarriage | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with placebo or no treatment | Risk with progesterone | |||||
| Miscarriage | Study population | RR 0.64 | 696 | ⊕⊕⊕⊝ | ||
| 242 per 1000 | 138 per 1000 | |||||
| Preterm birth | Study population | RR 0.86 | 588 | ⊕⊕⊝⊝ | ||
| 91 per 1000 | 84 per 1000 | |||||
| Congential abnormalities | Study population | RR 0.70 | 337 | ⊕⊝⊝⊝ | ||
| 13 per 1000 | 9 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation and/or allocation concealment had a high or unclear risk of bias in the majority of the trials (methodological quality of trials) (‐1). | ||||||
Background
Description of the condition
"Miscarriage is pregnancy loss before 20 weeks' gestation based on the first day of the last menstrual period or, if gestation age is unknown, it is the loss of an embryo or a fetus of less than 400 g" (Zegers‐Hochschild 2009). Threatened miscarriage is manifested by vaginal bleeding, with or without abdominal pain, while the cervix is closed and the fetus is viable and inside the uterine cavity (Cunningham 2001a). Once the cervix begins to dilate, miscarriage and pregnancy loss are inevitable. When the fetus is non‐viable and the cervix is closed, this is known as missed miscarriage or missed abortion (Cunningham 2001a). The presence of a short cervix or funnelling of the internal cervical os in the gestation period between 16 and 24 weeks has been found to indicate increased risk or threat to miscarriage (Owen 2004; Rust 2005).
Miscarriage is a common complication of pregnancy occurring in 15% to 20% of all clinically recognised pregnancies (Blohm 2008; Cohain 2017). As many as 50% of the miscarried fetuses and embryos have normal chromosomes (Suzumori 2010; Vorsanova 2005). In many cases, the cause of miscarriage cannot be identified, however, among the recognised risk factors of miscarriage are maternal age over 34 years and paternal age over 40 years (De La Rochebrochard 2002), previous history of two or more miscarriages (Sugiura‐Ogasawara 2009), and maternal autoimmune factors such as phospholipids antibodies (Check 2011). In addition, many modifiable risk factors were recognised including maternal obesity (Hahn 2014), maternal infection such as genital herpes simplex, HIV‐1 and vaginal colonisation of group B streptococci (Nigro 2011; Rocchetti 2011; Temmerman 1992). Maternal endocrine abnormalities such as uncontrolled diabetes mellitus (Galindo 2006), polycystic ovary syndrome (Arredondo 2006) and insufficient production of progesterone are other known risk factors. Progesterone insufficiency is due to corpus luteum (CL) deficiency, which is a group of cells in the ovary that are formed after the release of the ovum (Cunningham 2001b). The main function of the CL is to produce sufficient progesterone to prepare and support the lining of the uterus and facilitate implantation of the ovum (Cunningham 2001b). It is suggested that progesterone deficiency in early pregnancy may be an aetiological factor for miscarriage, hence, treatment with progesterone may prevent miscarriage. However the evidence support for the effectiveness and safety of such treatment is uncertain based on the results of recently published trials (Coomarasamy 2015; Saccone 2017).
Description of the intervention
Progestogens are a group of hormones that bind to the progesterone receptors; they include both the natural female sex hormone progesterone and the synthetic forms. Medications that mimic the action of progesterone are known as progestational agents. Progesterone and progestational agents are known as progestogens. Progesterone is secreted during early pregnancy from the ovary by CL (Cunningham 2001b). It is an essential hormone for the establishment and maintenance of pregnancy. Progestogens can be given to women with threatened miscarriage orally, as intramuscular injection or in the form of vaginal suppositories. Due to the wide range of doses, preparations and types of progestogens used for the treatment of threatened miscarriage (Carp 2012; Mirza 2016), it is uncertain what is the best type, dose and route of administration for the treatment of threatened miscarriage.
How the intervention might work
Progesterone induces secretory changes in the lining of the uterus, which are important for implantation of the fertilised ovum (Jin 2006). In addition, it modulates the immune response of the mother to prevent rejection of the embryo through a protein called progesterone induced blocking factor (PIBF), which is produced by the lymphocytes (white blood cells) of the pregnant woman (Szekeres‐Bartho 2010), and it enhances uterine quiescence and suppresses uterine contractions (Szekeres‐Bartho 2008; Szekeres‐Bartho 2009). Low progesterone levels have been linked to increased risk of first trimester miscarriage (Osmanağaoğlu 2010).
Owing to the documented physiological role of progesterone in maintaining pregnancy, it has been used to treat women with threatened miscarriage and presumed progesterone deficiency to improve expectations for continuity of pregnancy (Palagiano 2004). The therapeutic value of progesterone in preventing or treating threatened miscarriage has not been established (Kalinka 2005), although more recent evidence suggests that it may be effective in preventing miscarriage in women with a history of recurrent miscarriage of unclear etiology (Haas 2018). This might be due to the poor designs of the trials done to evaluate its effectiveness (Kalinka 2005), and the inclusion of women in these trials with different aetiologies for threatened miscarriage.
Why it is important to do this review
Miscarriage is associated with considerable physical and psychological morbidity. Women who had threatened miscarriage were found to have increased rate of antepartum haemorrhage, pre‐labour rupture of the membranes, preterm delivery, and intrauterine growth restriction when compared with women who did not have threatened miscarriage (Saraswat 2010). The emotional response to miscarriage can be profound; it includes depression, sleep disturbance, anger, and marital disturbances (Marcinko 2011). The introduction of ultrasound scans in the management of bleeding in early pregnancy has improved the diagnosis by rapid confirmation of viability and has improved the management by introducing prognostic factors such as fetal bradycardia and discrepancy between gestational age and crown‐to‐rump length (Dede 2010; Makrydimas 2003). This has rationalised the management of threatened miscarriage, as attempts to maintain a pregnancy are likely to be effective only if the fetus is viable and has no chromosomal abnormalities (Lede 2005).
The importance of progesterone on the maintenance of pregnancy was demonstrated by the successful use of progesterone antagonists, such as mifepristone (RU 486) in the elective induction of abortion (Dabash 2015). In a recently published systematic review vaginally administered progesterone was more effective in the prevention of preterm birth compared to the injectable progesterone (Oler 2017). This raised the question about the importance of the route of administration and the type of progestogen used to prevent preterm labour (Di Renzo 2005). These same questions might apply to the use of progestogens in the treatment of threatened miscarriage.
In earlier reports progestogen therapy has been linked to the development of hypospadias (deformity of the penis) in the male fetus (Silver 1999); however, recent reports did not show an increase in rate of hypospadias in infants of mothers who received progestogens in early pregnancy (Källén 2010).
The aim of this review is to study all the available data on the effectiveness of administration of progestogens for the treatment of threatened miscarriage.
Objectives
To determine the efficacy and the safety of progestogens in the treatment of threatened miscarriage.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised, quasi‐randomised or cluster‐randomised controlled trials, that assessed the effectiveness and safety of progestogens in the treatment of threatened miscarriage compared to placebo, no treatment or other intervention, if viability of the embryo or the fetus was confirmed before the commencement of treatment.
Types of participants
We included pregnant women, with threatened miscarriage at or less than 23 weeks, with singleton embryo or fetus, and who had a confirmed viable pregnancy. Fetal viability was to ensure that we excluded from this review trials that included women with bleeding in early pregnancy due to missed miscarriage. We have placed no restriction on the age of the woman or past obstetric history.
Types of interventions
We included any type of progestogens, natural or synthetic, used in the treatment of threatened miscarriage regardless of the dose, duration or route of administration compared with placebo, no treatment or other intervention.
Types of outcome measures
Primary outcomes
-
Miscarriage
Secondary outcomes
Mother
-
Pain relief (as defined by the study authors)
-
Thromboembolism
-
Preterm birth
-
Depression (as defined by the study authors)
-
Any other adverse outcomes that were reported (pregnancy‐induced hypertension; antepartum haemorrhage)
Child
-
Preterm birth
-
Stillbirth
-
Neonatal death
-
Congenital abnormalities, including genital malformations
-
Any other adverse neonatal outcomes that were reported (intrauterine growth restriction; respiratory distress syndrome)
-
Low birthweight (not prespecified)
-
Birthweight (not prespecified)
Search methods for identification of studies
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
We searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (8 August 2017)
The Register is a database containing over 23,000 reports of controlled trials in the field of pregnancy and childbirth. For full search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link to the editorial information about the Cochrane Pregnancy and Childbirth in the Cochrane Library and select the ‘Specialized Register ’ section from the options on the left side of the screen.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by their Information Specialist and contains trials identified from:
-
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
-
weekly searches of MEDLINE (Ovid);
-
weekly searches of Embase (Ovid);
-
monthly searches of CINAHL (EBSCO);
-
handsearches of 30 journals and the proceedings of major conferences;
-
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Two people screen the search results and review the full text of all relevant trial reports identified through the searching activities described above. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set that has been fully accounted for in the relevant review sections (Included studies; Excluded studies; Studies awaiting classification; Ongoing studies).
In addition, we searched ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP) for unpublished, planned and ongoing trial reports (8 August 2017) using the search terms given in Appendix 1.
Searching other resources
We scanned bibliographies of identified papers.
We did not apply any language restrictions.
Data collection and analysis
We have outlined the methods of data collection and analysis that we used to assess Gerhard 1987 and Palagiano 2004 in the previous version of this review, Wahabi 2011.
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Selection of studies
Three review authors independently assessed for inclusion all the potential trials we identified as a result of the search strategy. We resolved any disagreement through discussion.
Data extraction and management
For methods used in the previous version of this review, see Wahabi 2011.
For this update, we used the following methods for assessing the 29 reports that the Information Specialist identified as a result of the updated search.
Assessment of risk of bias in included studies
The four review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). We resolved any disagreement by discussion.
(1) Random sequence generation (checking for possible selection bias)
We described the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
For each included study we assessed the method as being at:
-
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
-
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
-
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
For each included study we described the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as being at:
-
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
-
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
-
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
For each included study we described the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that trials were at low risk of bias if they were blinded, or if we judged that the lack of blinding was unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as being at:
-
low, high or unclear risk of bias for participants;
-
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
For each included study we described the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as being at:
-
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
For each included study, and for each outcome or class of outcomes, we described the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses that we undertook.
We assessed methods as being at:
-
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
-
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
-
unclear risk of bias.
We excluded trials where more than 20% of participants were lost to follow‐up.
(5) Selective reporting (checking for reporting bias)
For each included study we described how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as being at:
-
low risk of bias (where it was clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review have been reported);
-
high risk of bias (where not all the study’s prespecified outcomes were reported; one or more reported primary outcomes were not prespecified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
-
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
For each included study we described any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether trials were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it was likely to have an impact on the findings. In future updates, we will explore the impact of the level of bias through undertaking sensitivity analyses (Sensitivity analysis).
Assessment of the quality of the evidence using the GRADE approach
For this update of the review, we used the GRADE approach, as outlined in the GRADE handbook (GRADE 2013), to assess the quality of the body of evidence relating to the following outcomes for the main comparisons, progesterone versus placebo or no treatment.
-
Miscarriage
-
Preterm birth
-
Congenital abnormalities
We used the GRADEpro Guideline Development tool (GRADEpro GDT 2015) to import data from Review Manager 5 (RevMan 5) (RevMan 2014) in order to create 'Summary of findings' tables. We produced a summary of the intervention effect and using the GRADE approach, a measure of quality for each of the above outcomes. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we present results as summary risk ratio (RR) with 95% confidence intervals (CIs).
Continuous data
None of the outcomes were reported as continuous data in this update. In future updates, if trials measure outcomes in the same way, we will use the mean difference. We will use the standardised mean difference to combine trials that measure the same outcome, but use different methods.
Unit of analysis issues
Cluster‐randomised trials
We did not identify any cluster‐randomised trials for inclusion. If we identify any cluster‐randomised trials in future updates of this review, we will include them in the analyses along with individually randomised trials. We will adjust their sample sizes using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions, using an estimate of the intra‐cluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population (Higgins 2011c). If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a subgroup analysis to investigate the effects of the randomisation unit.
Dealing with missing data
For included trials, we noted levels of attrition. For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, that is, we attempted to include all participants randomised to each group in the analyses, and analysed all participants in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² (Higgins 2003) and Chi² statistics (Deeks 2011). We regarded heterogeneity as substantial if I² was greater than 30% and either Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity.
Assessment of reporting biases
In future updates of this review, if there are 10 or more trials in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it (Sterne 2011).
Data synthesis
We carried out statistical analysis using the RevMan 5 software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that trials were estimating the same underlying treatment effect: that is, where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar. In future updates, if there is clinical heterogeneity sufficient to expect that the underlying treatment effects would differ between trials, or if we detect substantial statistical heterogeneity, we will use random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials is considered clinically meaningful. We will treat the random‐effects summary as the average range of possible treatment effects and we will discuss the clinical implications of treatment effects differing between trials. If the average treatment effect is not clinically meaningful we will not combine trials (Deeks 2011).
If we use random‐effects analyses, we will present the results as the average treatment effect with 95% CIs, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
We did not identify substantial heterogeneity. However, we carried out the following subgroup analyses for the primary outcome.
-
Route of administration
If we identify substantial heterogeneity in future updates of this review, we will investigate it using subgroup analyses and sensitivity analyses. We will consider whether an overall summary is meaningful, and if it is, use random‐effects analysis to produce it. We will include the following subgroups, in addition to route of administration.
-
Type of progestogen
-
Progestogen dose
-
Effect of progestogens in early (no more than 12 weeks) and late (more than 12 weeks) threatened miscarriage
We will restrict subgroup analysis to the primary outcome. We will assess subgroup differences by interaction tests available within RevMan 5 (RevMan 2014). We will report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value (Deeks 2011).
Sensitivity analysis
We included seven trials in this review. All but one were similar in terms of risk of bias. For future updates of this review, we will carry out sensitivity analysis to explore the effect of risk of bias. This will involve analysis based on our 'Risk of bias' judgements for allocation concealment, performance bias and attrition bias. We will compare the results of those trials assessed as being rated 'low' risk of bias for these domains with those rated as 'high' or 'unclear' risk of bias.
Results
Description of studies
Results of the search
We assessed 29 new trial reports of potential relevance identified by the updated search (see: Figure 1).
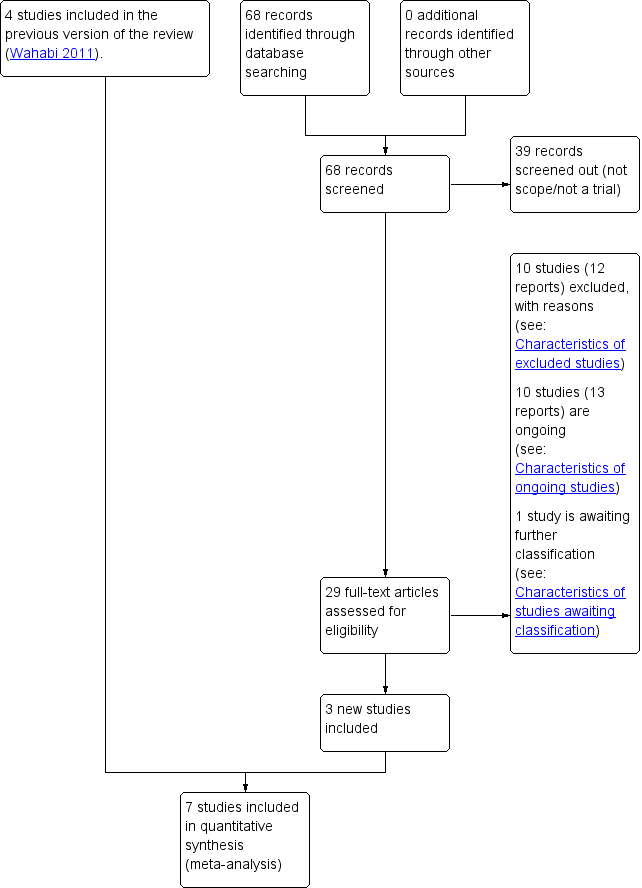
Trial flow diagram
Included studies
Trial location
We included seven trials (involving 696 participants) in this update of the review. The included trials were conducted in different countries, covering the full spectrum of the World Bank's economic classification (World Bank 2017), which may enhance the applicability and generalisation of evidence drawn from this review. Two trials were conducted in Germany and Italy (Gerhard 1987; Palagiano 2004), which are high‐income countries, while four trials were conducted in upper‐middle income countries; two in Iran (Alimohamadi 2013; Yassaee 2014), one in Malaysia (Pandian 2009) and the fourth in Turkey (Turgal 2017). The seventh trial was conducted in Jordan (El‐Zibdeh 2009), which is a lower‐middle income country. All trials were conducted in hospital settings.
Trial design
We included six randomised controlled trials (Alimohamadi 2013; Gerhard 1987; Palagiano 2004; Pandian 2009; Turgal 2017; Yassaee 2014) and one quasi‐randomised controlled trial (El‐Zibdeh 2009).
Sample size
A total of 696 women were included in this review. The largest trial involved 191 women (Pandian 2009) and the smallest involved 35 women (Gerhard 1987).
Participants
We included pregnant women, with threatened miscarriage at or less than 23 weeks and who had a confirmed viable pregnancy. Fetal viability was to ensure that we excluded from this review trials that included women with bleeding in early pregnancy due to missed miscarriage. We placed no restriction on the age of the woman or past obstetric history.
Type of intervention
The seven included trials compared progestogens to either placebo (Alimohamadi 2013; Gerhard 1987; Palagiano 2004; Turgal 2017) or no treatment (El‐Zibdeh 2009; Pandian 2009; Yassaee 2014). Three trials investigated oral progestogen (El‐Zibdeh 2009; Pandian 2009; Turgal 2017) and four investigated vaginal progesterone (Alimohamadi 2013; Gerhard 1987; Palagiano 2004; Yassaee 2014).
Outcome measure
Primary outcome
Miscarriage
All the included trials investigated this primary outcome. Three trials investigated oral progestogen (El‐Zibdeh 2009; Pandian 2009; Turgal 2017), and four trials investigated vaginal progesterone (Alimohamadi 2013; Gerhard 1987; Palagiano 2004; Yassaee 2014).
Secondary outcomes
Pain relief
Two trials (Palagiano 2004; Yassaee 2014) reported pain relief as an outcome of treatment with progesterone.
Preterm birth
Five trials (Alimohamadi 2013; El‐Zibdeh 2009; Gerhard 1987, Pandian 2009; Turgal 2017); with 588 women, reported the effect of oral or vaginal progestogens on preterm birth.
Pregnancy‐induced hypertension
Two trials (El‐Zibdeh 2009; Pandian 2009) reported pregnancy‐induced hypertension as a maternal adverse outcome.
Antepartum haemorrhage
Two trials (El‐Zibdeh 2009; Pandian 2009) reported antepartum haemorrhage as a maternal adverse outcome.
Perinatal death
One trial investigated the effect of progestogens on neonatal death (Alimohamadi 2013) and two trials investigated the effect of progestogens on stillbirth (Pandian 2009; Turgal 2017).
Congenital abnormalities
Two trials (El‐Zibdeh 2009; Pandian 2009) reported congenital abnormalities as an outcome.
Intrauterine growth restriction and low birthweight
Two trials (Turgal 2017, El‐Zibdeh 2009) reported on the frequency of intrauterine growth restriction in the intervention and control groups. Another trial (Alimohamadi 2013) reported on the frequency of low birthweight in the progesterone and the placebo group.
Respiratory distress syndrome
One trial (Alimohamadi 2013) investigated the rate of respiratory distress syndrome in the progesterone and the placebo group.
Birthweight
Only one trial (Turgal 2017) reported the difference in birthweight as an outcome.
Date of trials
Six trials were published between 2004 and 2017 (Alimohamadi 2013; El‐Zibdeh 2009; Palagiano 2004; Pandian 2009; Turgal 2017; Yassaee 2014). One trial was published in 1987 (Gerhard 1987).
Funding source
Solvay Pharmaceuticals funded two trials (El‐Zibdeh 2009; Pandian 2009). The rest of the trials did not mention the source of funding.
Delcaration of interest
None of the study authors reported any conflict of interest.
For further details, see Characteristics of included studies.
Excluded studies
In this update of the review, we excluded 10 (plus two duplicate) full‐text trials, in addition to the 32 excluded from the previous version. The reasons for exclusion of the 42 trials was as follows: 18 trials had a different population to this review' criteria (Brenner 1962; Corrado 2002; El Zibdeh 2000; El Zibdeh 2002; El Zibdeh 2005; Fuchs 1966; Goldzieher 1964; Johnson 1975; Klopper 1965; Le Vine 1964; Nyboe 2002; Porcaro 2015; Prietl 1992; Reijnders 1988; Shearman 1963; Smitz 1992; Swyer 1953; Turner 1966); 14 trials, either compared progesterone to another type of progesterone or used it in combination with another therapy (Beigi 2016; Berle 1977; Check 1995; Chye 2014 (and duplicate); Czajkowski 2007; Famina 2015; Hui 2015; Luz 1988 [pers comm]; Pustotina 2018; Siew 2014; Siew 2015; Song 2007; Vincze 2006; Zhang 2000); seven trials did not use a reliable method to confirm the viability of the fetus (Berle 1980; Crowder 1950; Govaerts‐Videtzky 1965; Moller 1965; Sondergaard 1985; Souka 1980; Tognoni 1980); one study (and duplicate) had a mixed group of participants and we could not obtain separate results for the threatened‐miscarriage group (Costantino 2016); one was not an RCT (Akhtar 2012); and one study had a high rate of attrition, more than 20% (Omar 2005).
For further details, see Characteristics of excluded studies.
Risk of bias in included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included trial
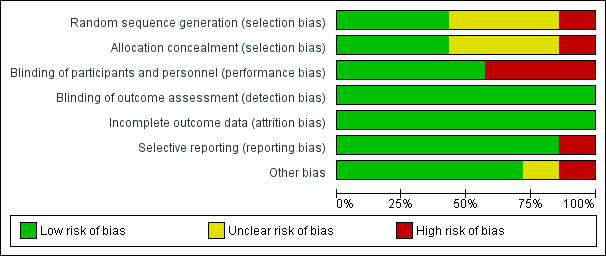
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials
We judged only three of the seven included trials (42%) to be at low risk of bias for random sequence generation and allocation concealment, and four trials (57%) to be at low risk for performance bias. We judged all trials (100%) at low risk of detection bias and attrition bias. We judged six trials at low risk of selective reporting bias (85%), and five trials (71%) at low risk of other biases.
Allocation
In three trials (Alimohamadi 2013; Pandian 2009; Turgal 2017), the investigators described a random component in the sequence‐generation process by using computer random‐number generators, so we judged these trials to have low risk of selection bias. In three trials (Gerhard 1987; Palagiano 2004; Yassaee 2014), there was insufficient information about the sequence‐generation process to permit judgement of low or high risk, so we judged them as unclear risk of selection bias. We judged one study (El‐Zibdeh 2009) as high risk for selection bias, as the investigators described a non‐random component in the sequence‐generation process, which was based on the day of the week that women presented to the clinic.
Participants and investigators enrolling participants could not foresee assignment to intervention or control group in three trials because Alimohamadi 2013 and Palagiano 2004 used sequentially numbered drug containers of identical appearance and Pandian 2009 used sequentially numbered concealed envelopes; we judged these trials at low risk of selection bias. Three trials (Gerhard 1987; Turgal 2017; Yassaee 2014), did not describe the method of concealment sufficiently to allow a definite judgement, so we judged them at unclear risk of selection bias. In El‐Zibdeh 2009, participants and investigators enrolling participants could foresee assignments, as the allocation was performed by the attending physician based on the day of the week the women visited the clinic, and thus the risk of selection bias introduction was high.
Blinding
Four trials (Alimohamadi 2013; Gerhard 1987; Palagiano 2004; Turgal 2017) ensured blinding of participants and key study personnel, and it is unlikely that the blinding could have been broken, so we judged the risk of performance bias to be low. Three trials did not use placebo for the control group. Two of these (El‐Zibdeh 2009; Pandian 2009) did not blind either personnel or women to the treatment received and one (Yassaee 2014) was a single‐blind study, in which the researchers were unaware which woman had received progesterone. Although outcomes such as miscarriage, preterm birth and fetal structural malformations are not likely to be influenced by lack of blinding, lack of blinding of participants or personnel could have introduced performance bias if participants inadvertently took a different type of progestogen than the one in the trial or exaggerated their reports of subjective outcomes, such as pain.
Five of the seven trials blinded outcome assessors to the treatment the women had received (Alimohamadi 2013; El‐Zibdeh 2009; Gerhard 1987; Palagiano 2004; Yassaee 2014). Pandian 2009 did not blind the assessors, and Turgal 2017 did not give any information about blinding. Outcomes such as miscarriage, preterm birth and fetal structural malformations are not likely to be influenced by lack of assessor's blinding, so we judged all seven trials as having low risk of detection bias.
Incomplete outcome data
There was no missing outcome data in five of the seven included trials (Alimohamadi 2013;El‐Zibdeh 2009; Palagiano 2004; Pandian 2009; Yassaee 2014); Gerhard 1987 excluded two women (5.7%) from the study after randomisation, and Turgal 2017 reported incomplete outcome data for 12 women (14.5%), equal in both groups. We judged all seven trials to be at low risk of attrition bias.
Selective reporting
All the included trials, except one (Palagiano 2004), reported all of the expected prespecified (primary and secondary) outcomes, so we assessed these at low risk of reporting bias. In Palagiano 2004, the study authors mentioned in the methods that they would report all the adverse effects, but in the results there was no explicit mention of the absence or presence of any adverse effects, so we judged it to be at high risk of reporting bias.
Other potential sources of bias
We assessed one study at high risk of other biases due to the difference in the number of participants recruited to the experimental and the control groups (86 versus 60; El‐Zibdeh 2009). In another study (Gerhard 1987), the risk of other bias was not clear because we included only participants with evidence of fetal viability, which amounts to only half of the participants.
Effects of interventions
Seven trials met the inclusion criteria, involving 696 participants. We performed subgroup analysis for the effect of progestogens by route of administration; however, due to paucity of data we could not carry out subgroup analysis for type and dose of progestogen. We undertook a total of six meta‐analyses.
Primary outcome
Miscarriage
The seven included trials, with 696 participants, compared progestogens to either placebo (Alimohamadi 2013; Gerhard 1987; Palagiano 2004: Turgal 2017) or no treatment (El‐Zibdeh 2009; Pandian 2009; Yassaee 2014). Treatment of miscarriage with progestogens compared to placebo or no treatment probably reduces the risk of miscarriage; (risk ratio (RR) 0.64, 95% confidence interval (CI) 0.47 to 0.87; 7 trials; 696 women; moderate‐quality evidence).
Subgroup analysis by route of administration
Three trials investigated treatment with oral progestogen (El‐Zibdeh 2009; Pandian 2009; Turgal 2017), and showed that treatment with oral progestogen compared to no treatment probably reduces the miscarriage rate (RR 0.57, 95% CI 0.38 to 0.85; 3 trials; 408 women; moderate‐quality evidence; Analysis 1.1.1). Four trials investigated treatment with vaginal progesterone compared to placebo (Alimohamadi 2013; Gerhard 1987; Palagiano 2004; Yassaee 2014), which probably has little or no effect in reducing the miscarriage rate (RR 0.75, 95% CI 0.47 to 1.21; 4 trials; 288 women; moderate‐quality evidence; Analysis 1.1.2). However, It should be noted that there were no differences between these two subgroups according to the subgroup interaction test (test for subgroup differences: Chi² = 0.76, df = 1 (P = 0.38), I² = 0%).
Secondary outcomes
Maternal outcomes
Pain relief
Two trials (Palagiano 2004; Yassaee 2014) reported pain relief as an outcome of treatment with progesterone. Palagiano 2004 reported reduction on the mean pain score with the use of progesterone from 2.6 ± 0.9 before treatment to 0.4 ± 0.7 (mean ± standard deviation) after treatment (P < 0.01), while no change in pain score was observed in women who received placebo from 2.5 ± 1.0 before treatment to 2.4 ± 0.8 (mean ± standard deviation) after treatment (P > 0.05). They reported pain using a progressive score from 0 to 4, where a score of 0 indicated 'no pain' and a score of 4 indicated 'extreme pain'. In Yassaee 2014, nine (30%) of the women in the progesterone and seven (23.3%) of the control group, continued to have pain after intervention (P = 0.55). We could not pool the results of these two trials due to the different types of data (dichotomous and continuous).
Preterm birth
Five trials (Alimohamadi 2013; El‐Zibdeh 2009; Gerhard 1987, Pandian 2009; Turgal 2017); reported the effect of progestogens on preterm birth. Treatment of preterm birth with the use of progestogens compared to placebo or no treatment may have little or no effect in reducing the rate of preterm birth (RR 0.86, 95% CI 0.52 to 1.44; 5 trials; 588 women; low‐quality evidence; Analysis 1.2).
Other maternal adverse outcomes
Pregnancy‐induced hypertension
Two trials (El‐Zibdeh 2009; Pandian 2009) reported pregnancy‐induced hypertension as a maternal adverse outcome. There was no difference in the occurrence of pregnancy‐induced hypertension between the progestogen and the control group (RR 1.00, 95% CI 0.54 to 1.88; 2 trials; 337 women; Analysis 1.3).
Antepartum haemorrhage
Two trials (El‐Zibdeh 2009; Pandian 2009) reported antepartum haemorrhage as maternal adverse outcome. Progestogens have little or no difference in the occurrence of antepartum haemorrhage (RR 0.76, 95% CI 0.30 to 1.94; 2 trials; 337 women; Analysis 1.4).
Child outcomes
Stillbirth
Two trials investigated the effect of progestogens on the stillbirth rate (Pandian 2009; Turgal 2017). Progestogens have little or no difference effects on the rate of stillbirth (RR 1.94, 95% CI 0.18 to 20.49; 2 trials; 262 women; Analysis 1.5).
Congenital abnormalities
Two trials (El‐Zibdeh 2009; Pandian 2009) reported congenital abnormalities as an outcome. We are uncertain if treatment of threatened miscarriage with progestogens compared to placebo or no treatment has any effect on the rate of congenital abnormalities, (RR 0.70, 95% CI 0.10 to 4.82; 2 trials; 337 infants; very low‐quality evidence; Analysis 1.6).
Neonatal death
Only one trial reported the effect of progestogens on neonatal death (Alimohamadi 2013). Progestogens have little or no effect in the neonatal death rate (RR 1.35, 95% CI 0.31 to 5.83; 1 trial; 145 women).
Other neonatal adverse outcomes
Intrauterine growth restriction and low birthweight
One trial (Turgal 2017) reported on the frequency of intrauterine growth restriction in the intervention and control group and showed no difference between the two groups; 0 (0%) in the progestogen group, one (3.5%) in the control group. Another trial (Alimohamadi 2013) reported on the frequency of low birthweight in the progesterone and the placebo group and showed no difference between the two groups; five (7%) for the progesterone group and seven (9.8%) for the placebo group.
Birthweight
Only one trial (Turgal 2017) reported the difference in birthweight as an outcome. It showed no difference in the mean birthweight between the progestogen and the control group; 3.1156 ± 0.643 kg for the intervention group and 3.2076 ± 0.500 kg for the control group.
Respiratory distress syndrome
One trial (Alimohamadi 2013) investigated the rate of respiratory distress syndrome in the progesterone and the placebo groups, and showed no difference between the two groups; there were two neonates with respiratory distress syndrome (2.8%) in the progesterone group and one (1.4%) in the placebo group.
Outcomes not reported in the primary trials
Due to paucity of data, we could not evaluate the following secondary outcomes.
-
Thromboembolism
-
Depression
In addition we could not perform the following subgroup analyses.
-
Route of progestogen administration
-
Type of progestogen
-
Progestogen dose
-
Effect of progestogens in early and late miscarriage
Discussion
Summary of main results
We included seven trials (involving 696 participants) in this update of the review. The included trials were conducted in different countries, covering the full spectrum of the World Bank's economic classification (World Bank 2017), which enhances the applicability of evidence drawn from this review. Two trials were conducted in Germany and Italy which are high‐income countries, while four trials were conducted in upper‐middle income countries; two in Iran, one in Malaysia and the fourth in Turkey, and the seventh trial was conducted in Jordon, which is a lower‐middle income country. In six trials all the participants met the inclusion criteria and in the seventh study, we included only the subgroup of participants who met the inclusion criteria in the meta‐analysis. Using the GRADE tool, we assessed the body of evidence for the main outcomes as ranging from very low‐quality to moderate‐quality evidence. Downgrading of evidence was based on the high risk of bias in six of the seven included trials and imprecision for some of the outcomes.
Treatment of miscarriage with progestogens compared to placebo or no treatment probably reduces the risk of miscarriage. Subgroup analysis by route of administration showed that treatment with oral progestogen compared to no treatment probably reduces the miscarriage rate, although treatment with vaginal progesterone compared to placebo, probably has little or no effect in reducing the miscarriage rate. However, the subgroup interaction test indicated no difference according to route of administration between the oral and vaginal subgroups of progesterone. Treatment of preterm birth with the use of progestogens compared to placebo or no treatment may have little or no effect in reducing the rate of preterm birth. We are uncertain if treatment of threatened miscarriage with progestogens compared to placebo or no treatment has any effect on the rate of congenital abnormalities.
Overall completeness and applicability of evidence
Threatened miscarriage is a common health problem. In a longitudinal study by Blohm 2008, one in four multiparous women had experienced a miscarriage and more than 7% of the studied population had experienced three or more miscarriages. In a large population‐based study by Cohain 2017, more than 40% of parous women reported having experienced one or more first trimester spontaneous miscarriages.
This update of the review includes seven trials, with a relatively small number of women (696), from six countries. All trials were conducted in hospital settings. Two trials were conducted in high‐income countries (Gerhard 1987; Palagiano 2004), four in upper‐middle income countries (Alimohamadi 2013; Pandian 2009; Turgal 2017; Yassaee 2014) and one in lower‐middle income country (El‐Zibdeh 2009). Although no trial was conducted in a low‐income country, the participants in the trials of the review have diverse ethnic and economic backgrounds (World Bank 2017). This may make the evidence in this review applicable to a large sector of women with threatened miscarriage.
Quality of the evidence
In this updated review we assessed the body of evidence for miscarriage as moderate quality, mainly due to limitations in study design of the included trials. From the seven included trials we judged only three (42%) to be at low risk of bias for random sequence generation and allocation concealment. Four trials (57%) were at low risk for performance bias, and all were at low risk of detection bias. We assessed all trials at low risk for attrition bias and six were at low risk of selective reporting bias. Only five trials (71%) trials were at low risk for other biases (summary of findings Table for the main comparison).
For preterm birth we assessed the body of evidence as low quality due to imprecision (wide confidence intervals crossing the no‐effect line) and limitations with study design of the included trials. From the five included trials, three (60%) were at low risk of bias for random sequence generation, while three (60%) were at low risk of performance bias and all trials were at low risk of detection bias. In addition, one study randomised different numbers of participants to the two arms of the study, which we considered as additional bias and in one study we included the results of only 50% of the participants who met the inclusion criteria.
For the outcome congenital abnormality, we assessed the body of evidence as very low due to imprecision (wide confidence intervals crossing the no‐effect line), small number of trials (two trials) and participants (337 women) and limitations with study design. We assessed one of the two included trials to be at high risk of selection bias and performance bias and the other study at high risk of performance bias.
Potential biases in the review process
In this review, we took steps to minimise bias, although we are aware that bias may be present in our review: two review authors independently assessed trials for eligibility and extracted the data as necessary. We resolved discrepancies through discussion or, if required, we consulted a third review author; two review authors also performed GRADE assessments independently and resolved discrepancies though discussion; and we conducted a comprehensive search in order to identify all relevant published and unpublished literature.
Agreements and disagreements with other studies or reviews
Our assessment of the body of evidence in this update of the review did not differ much from the previous version of the review (Wahabi 2011). For the main comparison, we have included three additional trials, however, neither the magnitude nor the direction of evidence changed markedly from the earlier version of the review. We have used the recent methodology introduced for Cochrane Reviews in 2008, which assesses risk of bias in the individual trials more carefully than in the past (Higgins 2011b). In addition, we assessed the quality of the evidence using the GRADE approach as outlined in the GRADE Handbook (GRADE 2013).
The results of this review agree with a recently published systematic review of randomised and non‐randomised controlled trials of dydrogesterone (oral progestogen) for the treatment of threatened miscarriage (Carp 2012) and with non‐randomised controlled trials (Akhtar 2012), which investigated the effectiveness of oral progestogens in the treatment of threatened miscarriage. The results of this trial showed that a larger proportion of women who received progestogen continued to be pregnant compared to the control group, however, the difference was not significant.
Recently published trials suggested that the route of administration and the type of progestogen influence its effectiveness in the prevention of miscarriage. In a multicenter, randomised, placebo‐controlled trial on women with unexplained recurrent miscarriages, vaginal progesterone was found not to be significantly different from placebo in the prevention of miscarriage (Coomarasamy 2015). However, the results of a review of randomised trials on the use of progestogen in the prevention of recurrent miscarriage, concluded that synthetic progestogens, but not natural progesterone, were associated with a lower risk of recurrent miscarriage, nevertheless, the conclusion was limited by the low quality of evidence (Saccone 2017).
Our results suggested that progestogen may not be as effective in the prevention of preterm birth (Analysis 1.2). There are conflicting published reports about the effectiveness of progestational agents in the prevention of preterm birth with apparent influence of type of progestogen and route of administration, as well as different subgroups of women, on the effectiveness of treatment (Facchinetti 2017; Heyborne 2016; O'Brien 2016).
Our results relating to the safety of progestogen use for the mother and infant are limited by the small number of trials and participants in addition to the low quality of the evidence. However, our systematic review is in agreement with other systematic reviews, which also suggest that there are no increased risks of adverse outcomes to the mother or the infant from the use of progestogen compared to the control group (Haas 2018).
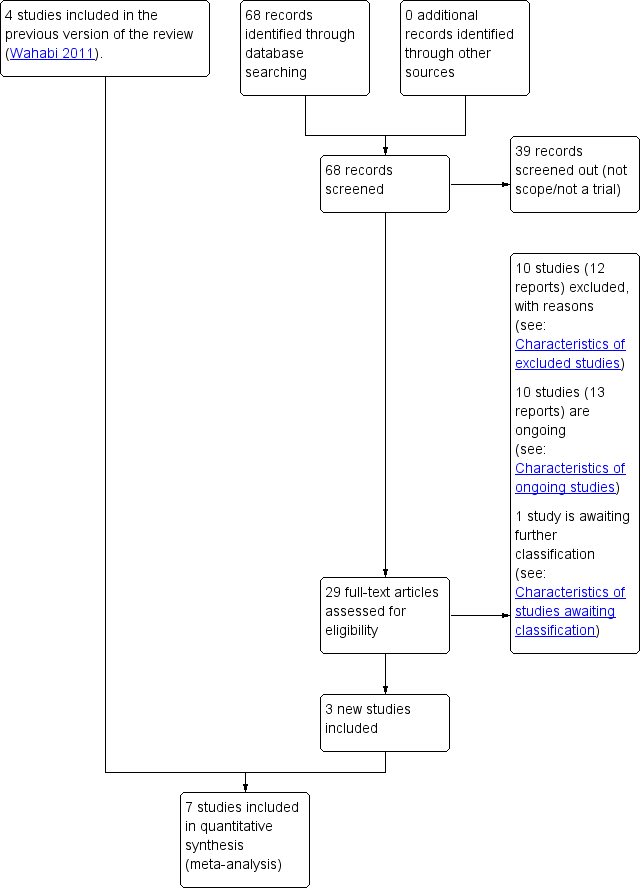
Trial flow diagram
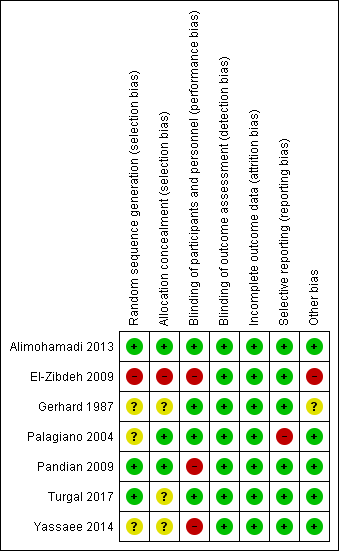
Risk of bias summary: review authors' judgements about each risk of bias item for each included trial

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials

Comparison 1 Progestogens versus placebo or no treatment, Outcome 1 Miscarriage.
Comparison 1 Progestogens versus placebo or no treatment, Outcome 2 Preterm birth.

Comparison 1 Progestogens versus placebo or no treatment, Outcome 3 Pregnancy‐induced hypertension.

Comparison 1 Progestogens versus placebo or no treatment, Outcome 4 Antepartum haemorrhage.

Comparison 1 Progestogens versus placebo or no treatment, Outcome 5 Stillbirth.

Comparison 1 Progestogens versus placebo or no treatment, Outcome 6 Congential abnormalities.
| Progesterone compared to placebo or no treatment for treating threatened miscarriage | ||||||
| Patient or population: women with threatened miscarriage | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with placebo or no treatment | Risk with progesterone | |||||
| Miscarriage | Study population | RR 0.64 | 696 | ⊕⊕⊕⊝ | ||
| 242 per 1000 | 138 per 1000 | |||||
| Preterm birth | Study population | RR 0.86 | 588 | ⊕⊕⊝⊝ | ||
| 91 per 1000 | 84 per 1000 | |||||
| Congential abnormalities | Study population | RR 0.70 | 337 | ⊕⊝⊝⊝ | ||
| 13 per 1000 | 9 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Random sequence generation and/or allocation concealment had a high or unclear risk of bias in the majority of the trials (methodological quality of trials) (‐1). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Miscarriage Show forest plot | 7 | 696 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.47, 0.87] |
| 1.1 Oral progestogen versus no treatment | 3 | 408 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.38, 0.85] |
| 1.2 Vaginal progesterone versus placebo | 4 | 288 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.47, 1.21] |
| 2 Preterm birth Show forest plot | 5 | 588 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.52, 1.44] |
| 3 Pregnancy‐induced hypertension Show forest plot | 2 | 337 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.54, 1.88] |
| 4 Antepartum haemorrhage Show forest plot | 2 | 337 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.30, 1.94] |
| 5 Stillbirth Show forest plot | 2 | 262 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.94 [0.18, 20.49] |
| 6 Congential abnormalities Show forest plot | 2 | 337 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.10, 4.82] |

