Infusión continua de insulina subcutánea versus inyecciones diarias múltiples de insulina para embarazadas con diabetes
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | "Randomly divided". | |
| Participants | 10 women recruited from 8 weeks to 'term'. | |
| Interventions | CSII versus MDI. | |
| Outcomes | Gestational age at birth, caesarean section, weight gain during pregnancy, preterm birth, hyperbilirubinaemia, and maternal days hospitalised. | |
| Notes | Single‐centre trial in Italy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of the type of intervention from clinician and participant for the trials was not possible because of the nature of the study. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of assessors not reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported. |
| Selective reporting (reporting bias) | Unclear risk | Pre‐specified outcomes not reported. |
| Other bias | Unclear risk | Small trial group, limited reporting. |
| Methods | "Randomly assigned" no other information reported. | |
| Participants | 15 women with type 1 diabetes (13 on conventional insulin therapy, 2 on continuous insulin therapy) and 14 women with type 2 diabetes (4 were on oral hypoglycaemics, 10 diet‐controlled). Recruitment occurred in the first trimester, 2 women allocated to CSII had already been using a CSII pump pre‐conceptually. | |
| Interventions | CSII versus MDI. Participants were hospitalised initially in order to achieve optimal glycaemic control, diet was prescribed according to individual needs. A Microject MC 20 portable syringe pump was used with porcine insulin (Actrapid MC) 40 U/mL, adjustments were made to the dosage in order to obtain strict glycaemic control (fasting BG < 80 + 10 mg/dL, postprandial BG < 120 mg/dL). Participants randomised to the MDI dose were given Actrapid MC split into 4 boluses. | |
| Outcomes | Maternal and neonatal mortality, large‐for‐gestational age, fetal anomaly and hypoglycaemia, weight gain during pregnancy, mean 24‐hour BG, mean HbA1c, gestational age at delivery, preterm birth, birthweight and rate of instrumental delivery. | |
| Notes | Single‐centre trial in Italy. Participants and their neonates were followed up at delivery and for the first 2 days postnatally. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of the type of intervention from clinician and participant for the trials was not possible because of the nature of the study. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of assessors not reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | The numbers of women included in analysis across pregnancy comparing maternal 24‐hour mean glucose and mean HbA1c varied from 13 to 15 in the CSII group and from 8 to 14 in the MDI group. |
| Selective reporting (reporting bias) | Unclear risk | Pre‐specified outcomes not reported. |
| Other bias | Unclear risk | Small trial group, limited reporting of methods. |
| Methods | "Randomly assigned". | |
| Participants | 71 women with type 1 diabetes. | |
| Interventions | MDI versus CSII. | |
| Outcomes | Daily glucose levels, 24‐hour glycaemic profiles, infant abdominal fat deposition. | |
| Notes | Raw and mean data not reported, therefore could not be included in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of the type of intervention from clinician and participant for the trials was not possible because of the nature of the study. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of assessors not reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported. |
| Selective reporting (reporting bias) | Unclear risk | Pre‐specified outcomes not reported. |
| Other bias | Unclear risk | Single‐centre trial in Italy, small trial group, limited reporting of methods. |
| Methods | "Randomly allocated", using sealed envelopes. | |
| Participants | 31 women with type 1 insulin‐dependent diabetes included undergoing 32 pregnancies, 1 woman included twice for separate pregnancies. 4 women were recruited in the pre‐conception period, 28 women recruited during their first trimester. The women were described as highly motivated and referred to their centre for intensive therapy. | |
| Interventions | Allocated either CSII or MDI. Microject MC 20 and Daedi B.V. portable battery‐powered syringe infusion pumps, participants receiving MDI had 4 daily insulin injections (regular insulin at each meal and intermediate acting insulin at night, type of insulin used was not stated). | |
| Outcomes | Maternal and neonatal mortality, large‐for‐gestational age, fetal anomaly and hypoglycaemia, mean 24‐hour BG, mean HbA1c, gestational age at delivery, preterm birth, Apgar score < 7 at 5 minutes, respiratory distress syndrome, birthweight and rate of instrumental delivery. | |
| Notes | No losses to follow‐up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Low risk | Used sealed envelopes to conceal allocation of their participants. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of the type of intervention from clinician and participant for the trials was not possible because of the nature of the study. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of assessors not reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided. |
| Selective reporting (reporting bias) | Unclear risk | Pre‐specified outcomes not reported. |
| Other bias | High risk | Small trial group, described as "highly motivated". Single‐centre trial in Italy, limited reporting of methods. |
| Methods | "Randomly assigned". | |
| Participants | 12 women with type 1 diabetes. | |
| Interventions | MDI versus CSII. | |
| Outcomes | Perinatal mortality, large‐for‐gestational age, maternal weight gain during pregnancy, mean 24‐hour BG in each trimester, and respiratory distress syndrome. | |
| Notes | Several data outcomes described as comparable rather than reported as statistics. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of the type of intervention from clinician and participant for the trials was not possible because of the nature of the study. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding of assessors not reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported. |
| Selective reporting (reporting bias) | Unclear risk | Pre‐specified outcomes not reported. |
| Other bias | Unclear risk | Not reported. |
BG: blood glucose
CSII: continuous subcutaneous insulin infusion
HbA1c: glycated haemoglobin
MDI: multiple daily injection
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Exclusion of MDI group participants from analysis if normoglycaemia not achieved (number not reported). | |
| Wrong intervention: conventional versus intensive therapy, rather than CSII versus MDI. Women using CSII and MDI therapy included in the intensive therapy group. | |
| 21 women randomised antenatally (1 randomised twice for separate pregnancies), gestation at randomisation not stated, therefore length of treatment may be inconsistent. 7 women randomised in the pre‐conceptual period, conceiving between 2 weeks and 1 year. The differences in time to conceive and treatment length is likely to lead to inconsistency of treatment effects. | |
| Probably not a randomised study: 41 women were "divided" into 2 groups. Number of women included in the study and by study group inconsistently reported (41 women included and 21 in each of the 2 groups). | |
| 30 women randomised, 9 declined CSII, so did not receive the allocated intervention and were reported as a separate group, thus potentially confounding the results. | |
| Wrong intervention: 2‐arm cross‐over trial comparing closed‐loop versus conventional CSII. | |
| No methods or data provided by trial authors, therefore assessment of the trial is not possible. |
CSII: continuous subcutaneous insulin infusion
MDI: multiple daily injection
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | CLIP‐03. |
| Methods | 2‐arm cross‐over trial comparing closed‐loop CSII overnight with not closed‐loop (continuous glucose monitor and insulin pump but not closed‐loop) CSII overnight. |
| Participants | Pregnant women with type 1 diabetes, 8‐24 weeks GA. Setting: UK. |
| Interventions | Closed‐loop CSII overnight versus continuous glucose monitor and insulin pump but not closed‐loop. |
| Outcomes | Overnight time spent in the target glucose range (3.5‐7.8 mmol/L), number of episodes of nocturnal hypoglycaemia, duration and outcome of events. Frequency and duration of use of the closed‐loop system, users’ responses (lifestyle change and diabetes self‐management). Overnight time above and below target range, metabolic control, trends in CGM data. |
| Starting date | 01/04/2014. |
| Contact information | Dr Zoe Stewart. |
| Notes | This study may not be eligible for inclusion, because it does not compare CSII with MDI. |
| Trial name or title | |
| Methods | 2‐arm randomised trial, comparing insulin pump with multiple daily insulin injection. Single‐blind (outcome assessor). The information indicates that allocation is “randomized”, there is no description of the method. |
| Participants | Pregnant women with type 1 or type 2 diabetes prior to pregnancy. First trimester, singleton pregnancy, receiving intensive insulin therapy of less than 100 unit of insulin per day. Setting: Canada. |
| Interventions | Insulin pump versus multiple daily insulin injections. |
| Outcomes | Composite obstetric/perinatal morbidity or mortality, mean maternal HbA1c during pregnancy, number of episodes of severe hypoglycaemia. |
| Starting date | April 2014. |
| Contact information | Dr David Thompson [email protected] |
| Notes |
CGM: continuous glucose monitor
CSII: continuous subcutaneous insulin infusion
GA: gestational age
HbA1c: glycated haemoglobin
MDI: multiple daily injection
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hypertensive disorders of pregnancy (including pre‐eclampsia, pregnancy‐induced hypertension, eclampsia) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Caesarean section Show forest plot | 3 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.66, 1.77] |
| Analysis 1.2  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 2 Caesarean section. | ||||
| 3 Development of type 2 diabetes | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Large‐for‐gestational age Show forest plot | 3 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.15 [0.49, 34.95] |
| Analysis 1.4  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 4 Large‐for‐gestational age. | ||||
| 5 Perinatal mortality Show forest plot | 4 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.33 [0.38, 14.32] |
| Analysis 1.5  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 5 Perinatal mortality. | ||||
| 6 Mortality or morbidity composite | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neurosensory disability | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Induction of labour | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Perineal trauma | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Weight gain during pregnancy Show forest plot | 3 | 51 | Mean Difference (IV, Fixed, 95% CI) | 0.52 [‐1.12, 2.17] |
| Analysis 1.10  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 10 Weight gain during pregnancy. | ||||
| 11 Maternal 24‐hour mean blood glucose (mg/dL) first trimester Show forest plot | 3 | 67 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐7.19, 7.43] |
| Analysis 1.11  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 11 Maternal 24‐hour mean blood glucose (mg/dL) first trimester. | ||||
| 12 Maternal 24‐hour mean blood glucose (mg/dL) second trimester Show forest plot | 3 | 73 | Mean Difference (IV, Fixed, 95% CI) | 1.77 [‐5.02, 8.56] |
| Analysis 1.12  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 12 Maternal 24‐hour mean blood glucose (mg/dL) second trimester. | ||||
| 13 Maternal 24‐hour mean blood glucose (mg/dL) third trimester Show forest plot | 3 | 69 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐5.57, 5.72] |
| Analysis 1.13  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 13 Maternal 24‐hour mean blood glucose (mg/dL) third trimester. | ||||
| 14 Mean HbA1c first trimester Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐2.13, 1.73] |
| Analysis 1.14  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 14 Mean HbA1c first trimester. | ||||
| 15 Mean HbA1c second trimester Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐2.29, 3.69] |
| Analysis 1.15  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 15 Mean HbA1c second trimester. | ||||
| 16 Mean HbA1c third trimester Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐2.38, 2.58] |
| Analysis 1.16  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 16 Mean HbA1c third trimester. | ||||
| 17 Maternal hypoglycaemia Show forest plot | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.35, 25.87] |
| Analysis 1.17  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 17 Maternal hypoglycaemia. | ||||
| 18 Maternal hyperglycaemia Show forest plot | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.39, 125.44] |
| Analysis 1.18  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 18 Maternal hyperglycaemia. | ||||
| 19 Postnatal depression | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Postnatal weight retention or return to pre‐pregnancy weight | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Gestational age at birth Show forest plot | 3 | 71 | Mean Difference (IV, Fixed, 95% CI) | ‐1.18 [‐2.92, 0.57] |
| Analysis 1.21  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 21 Gestational age at birth. | ||||
| 22 Preterm birth < 37 weeks' gestation Show forest plot | 3 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.18, 3.24] |
| Analysis 1.22  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 22 Preterm birth < 37 weeks' gestation. | ||||
| 23 Preterm birth < 32 weeks' gestation Show forest plot | 3 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.62] |
| Analysis 1.23  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 23 Preterm birth < 32 weeks' gestation. | ||||
| 24 Apgar score < 7 at 5 minutes Show forest plot | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.24  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 24 Apgar score < 7 at 5 minutes. | ||||
| 25 Macrosomia Show forest plot | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.2 [0.14, 72.62] |
| Analysis 1.25  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 25 Macrosomia. | ||||
| 26 Small‐for‐gestational age Show forest plot | 2 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.10, 18.71] |
| Analysis 1.26  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 26 Small‐for‐gestational age. | ||||
| 27 Mean birthweight grams Show forest plot | 2 | 61 | Mean Difference (IV, Fixed, 95% CI) | 220.56 [‐2.09, 443.20] |
| Analysis 1.27  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 27 Mean birthweight grams. | ||||
| 28 Adiposity (infant) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Respiratory distress syndrome Show forest plot | 2 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 68.57] |
| Analysis 1.29  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 29 Respiratory distress syndrome. | ||||
| 30 Neonatal hypoglycaemia Show forest plot | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 14.64] |
| Analysis 1.30  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 30 Neonatal hypoglycaemia. | ||||
| 31 Neonatal hyperbilirubinaemia Show forest plot | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.02, 6.65] |
| Analysis 1.31  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 31 Neonatal hyperbilirubinaemia. | ||||
| 32 Fetal anomaly Show forest plot | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.07, 15.54] |
| Analysis 1.32  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 32 Fetal anomaly. | ||||
| 33 Diabetes (infant) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 34 Length of postnatal stay (mother) Show forest plot | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | 9.40 [‐6.04, 24.84] |
| Analysis 1.34  Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 34 Length of postnatal stay (mother). | ||||

Study flow diagram.
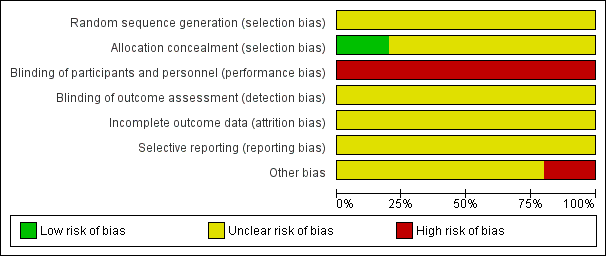
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
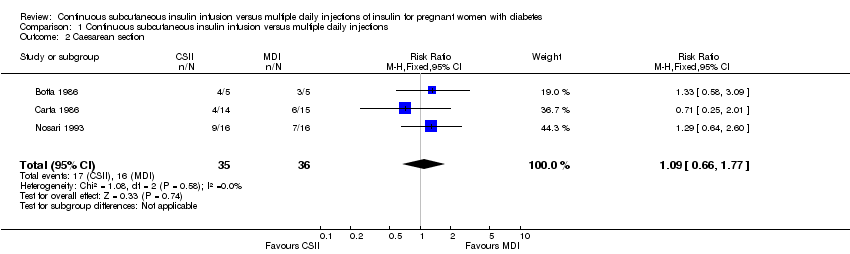
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 2 Caesarean section.
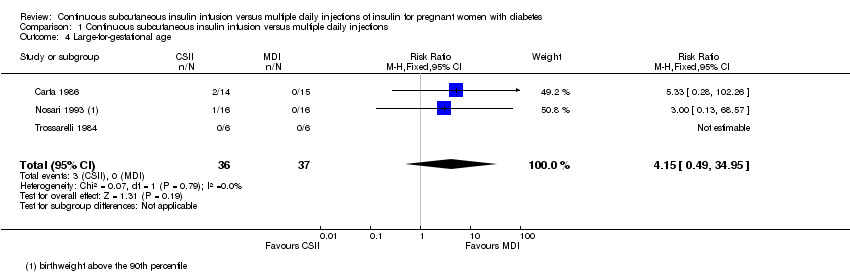
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 4 Large‐for‐gestational age.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 5 Perinatal mortality.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 10 Weight gain during pregnancy.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 11 Maternal 24‐hour mean blood glucose (mg/dL) first trimester.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 12 Maternal 24‐hour mean blood glucose (mg/dL) second trimester.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 13 Maternal 24‐hour mean blood glucose (mg/dL) third trimester.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 14 Mean HbA1c first trimester.
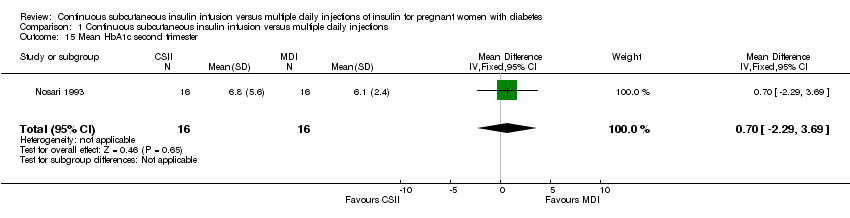
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 15 Mean HbA1c second trimester.
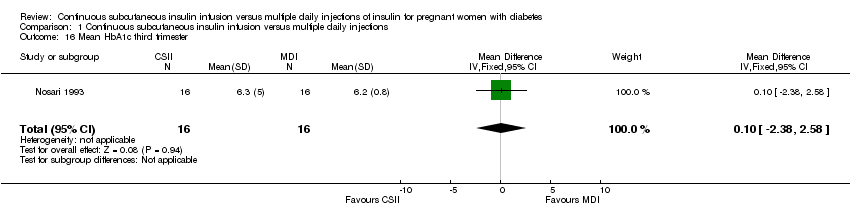
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 16 Mean HbA1c third trimester.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 17 Maternal hypoglycaemia.
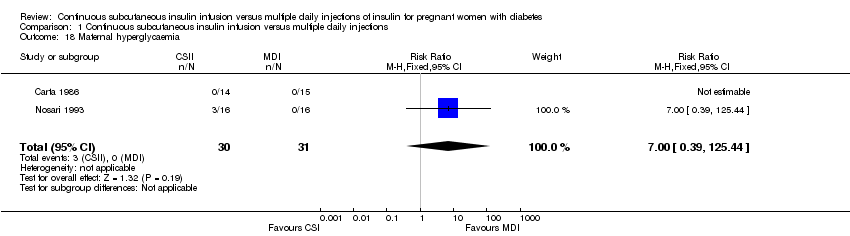
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 18 Maternal hyperglycaemia.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 21 Gestational age at birth.
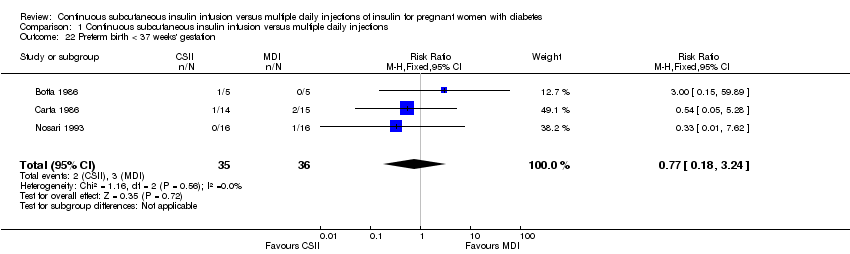
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 22 Preterm birth < 37 weeks' gestation.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 23 Preterm birth < 32 weeks' gestation.
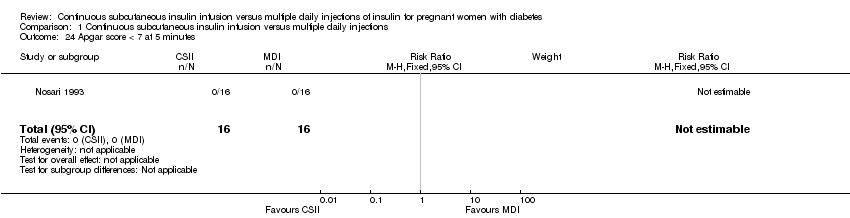
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 24 Apgar score < 7 at 5 minutes.
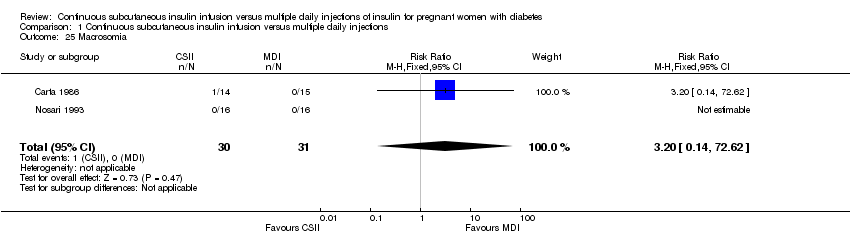
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 25 Macrosomia.
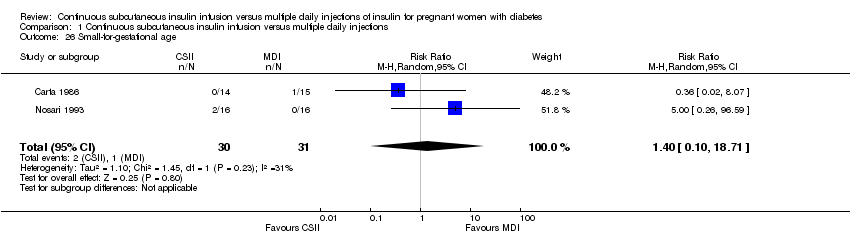
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 26 Small‐for‐gestational age.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 27 Mean birthweight grams.

Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 29 Respiratory distress syndrome.
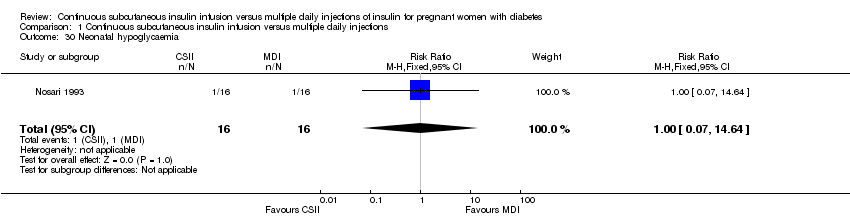
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 30 Neonatal hypoglycaemia.
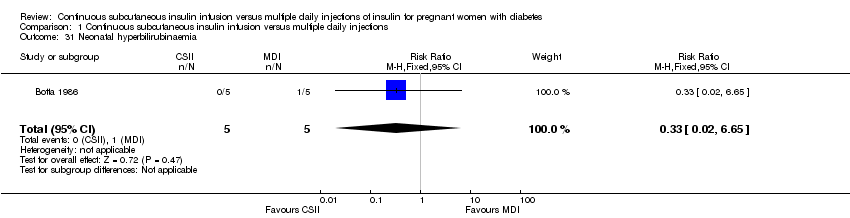
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 31 Neonatal hyperbilirubinaemia.
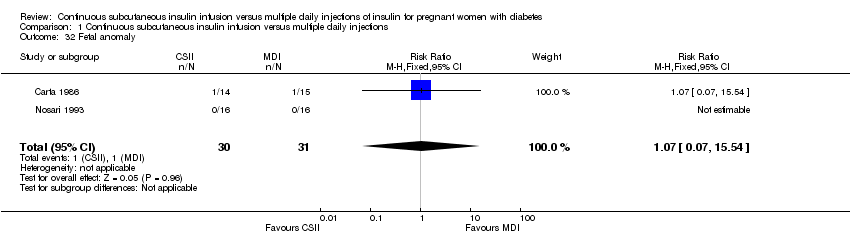
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 32 Fetal anomaly.
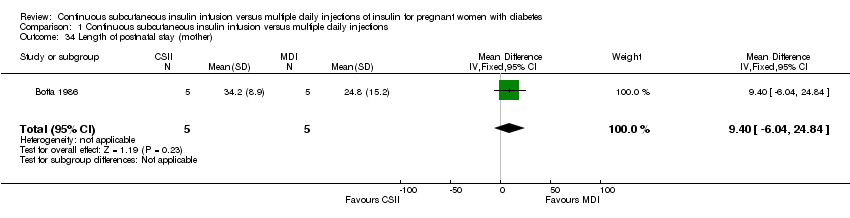
Comparison 1 Continuous subcutaneous insulin infusion versus multiple daily injections, Outcome 34 Length of postnatal stay (mother).
| Continuous subcutaneous insulin infusion (CSII) versus multiple daily injections (MDI) of insulin for pregnant women with diabetes | ||||||
| Patient or population: pregnant women with diabetes | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with MDI | Risk with GRADE CSII | |||||
| Hypertensive disorders of pregnancy (including pre‐eclampsia, pregnancy‐induced hypertension, eclampsia) | (0 studies) | outcome not reported | ||||
| Caesarean section | Study population | RR 1.09 | 71 | ⊕⊝⊝⊝ | ||
| 444 per 1000 | 484 per 1000 | |||||
| Moderate | ||||||
| 438 per 1000 | 477 per 1000 | |||||
| Development of Type 2 diabetes | (0 studies) | outcome not reported | ||||
| Perineal trauma | (0 studies) | outcome not reported | ||||
| Return to pre‐pregnancy weight | (0 studies) | outcome not reported | ||||
| Postnatal depression | (0 studies) | outcome not reported | ||||
| Induction of labour | (0 studies) | outcome not reported | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 All studies contributing data had design limitations. 2 Wide confidence interval crossing the line of no effect, and small sample size. | ||||||
| Continuous subcutaneous insulin infusion (CSII) versus multiple daily injections (MDI) of insulin for pregnant women with diabetes | ||||||
| Patient or population: infants of pregnant women with diabetes | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with MDI | Risk with GRADE CSII | |||||
| Large‐for‐gestational age | Study population | RR 4.15 | 73 | ⊕⊝⊝⊝ | Study population and moderate risks were not calculated, due to the small sample size, few events, and no events in the MDI group. | |
| 0 per 1000 | 0 per 1000 | |||||
| Perinatal mortality (stillbirth and neonatal mortality) | Study population | RR 2.33 | 83 | ⊕⊝⊝⊝ | Moderate risks were not calculated, due to the small sample size and few events. | |
| 24 per 1000 | 55 per 1000 | |||||
| Mortality or morbidity composite | (0 studies) | outcome not reported | ||||
| Neonatal hypoglycaemia | Study population | RR 1.00 | 32 | ⊕⊝⊝⊝ | ||
| 63 per 1000 | 63 per 1000 | |||||
| Adiposity (infant) | (0 studies) | outcome not reported | ||||
| Type 1 and type 2 diabetes (infant) | (0 studies) | outcome not reported | ||||
| Neurosensory disability | (0 studies) | outcome not reported | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 All studies contributing data had design limitations. 2 Wide confidence interval crossing the line of no effect, small sample size and few events. 3 One study with design limitations. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hypertensive disorders of pregnancy (including pre‐eclampsia, pregnancy‐induced hypertension, eclampsia) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Caesarean section Show forest plot | 3 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.66, 1.77] |
| 3 Development of type 2 diabetes | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Large‐for‐gestational age Show forest plot | 3 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.15 [0.49, 34.95] |
| 5 Perinatal mortality Show forest plot | 4 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.33 [0.38, 14.32] |
| 6 Mortality or morbidity composite | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Neurosensory disability | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Induction of labour | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Perineal trauma | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Weight gain during pregnancy Show forest plot | 3 | 51 | Mean Difference (IV, Fixed, 95% CI) | 0.52 [‐1.12, 2.17] |
| 11 Maternal 24‐hour mean blood glucose (mg/dL) first trimester Show forest plot | 3 | 67 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐7.19, 7.43] |
| 12 Maternal 24‐hour mean blood glucose (mg/dL) second trimester Show forest plot | 3 | 73 | Mean Difference (IV, Fixed, 95% CI) | 1.77 [‐5.02, 8.56] |
| 13 Maternal 24‐hour mean blood glucose (mg/dL) third trimester Show forest plot | 3 | 69 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐5.57, 5.72] |
| 14 Mean HbA1c first trimester Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐2.13, 1.73] |
| 15 Mean HbA1c second trimester Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐2.29, 3.69] |
| 16 Mean HbA1c third trimester Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐2.38, 2.58] |
| 17 Maternal hypoglycaemia Show forest plot | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.35, 25.87] |
| 18 Maternal hyperglycaemia Show forest plot | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.39, 125.44] |
| 19 Postnatal depression | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Postnatal weight retention or return to pre‐pregnancy weight | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Gestational age at birth Show forest plot | 3 | 71 | Mean Difference (IV, Fixed, 95% CI) | ‐1.18 [‐2.92, 0.57] |
| 22 Preterm birth < 37 weeks' gestation Show forest plot | 3 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.18, 3.24] |
| 23 Preterm birth < 32 weeks' gestation Show forest plot | 3 | 71 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.62] |
| 24 Apgar score < 7 at 5 minutes Show forest plot | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Macrosomia Show forest plot | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.2 [0.14, 72.62] |
| 26 Small‐for‐gestational age Show forest plot | 2 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.10, 18.71] |
| 27 Mean birthweight grams Show forest plot | 2 | 61 | Mean Difference (IV, Fixed, 95% CI) | 220.56 [‐2.09, 443.20] |
| 28 Adiposity (infant) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Respiratory distress syndrome Show forest plot | 2 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 68.57] |
| 30 Neonatal hypoglycaemia Show forest plot | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 14.64] |
| 31 Neonatal hyperbilirubinaemia Show forest plot | 1 | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.02, 6.65] |
| 32 Fetal anomaly Show forest plot | 2 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.07, 15.54] |
| 33 Diabetes (infant) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 34 Length of postnatal stay (mother) Show forest plot | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | 9.40 [‐6.04, 24.84] |

