Orthodontic and orthopaedic treatment for anterior open bite in children
Abstract
This is a protocol for a Cochrane Review (Intervention). The objectives are as follows:
(1) To determine whether orthodontic and/or orthopaedic treatment in children with anterior open bite is effective at correcting the anterior open bite.
(2) To determine whether any one treatment is more effective than another.
(3) To determine whether treatment:
(a) reduces or cures snoring or sleep apnoea;
(b) reduces signs and symptoms of masticatory and swallowing dysfunction;
(c) changes other dentofacial characteristics ‐ maxillo‐mandibular width, height, length and dental position.
Background
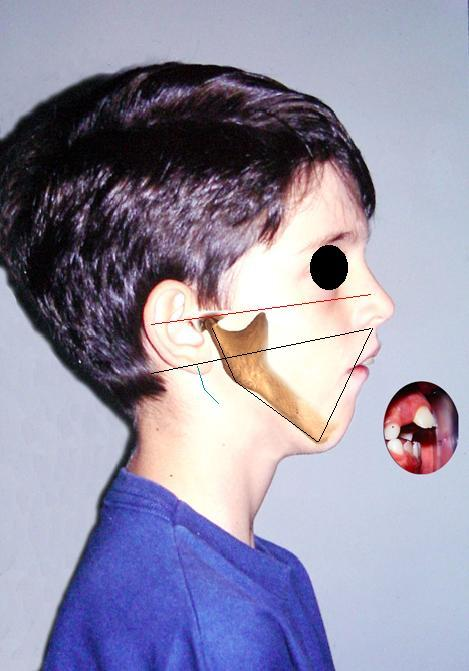
An anterior open bite can be defined as failure of the upper and lower anterior teeth to meet and overlap each other in the vertical plane. The cause of an anterior open bite is generally multifactorial and can be due to a combination of skeletal, dental and soft tissue effects (Figure 1). Many potential aetiological factors have been considered, including unfavourable growth patterns (Bell 1971; Nahoum 1977), digit sucking habits (Atkinson 1966; Mizrahi 1978; Subtelny 1964), enlarged lymphatic tissue (Atkinson 1966; Linder‐Aronson 1970), heredity (Mizrahi 1978; Sassouni 1969) and oral functional matrices (Moss 1971).

The characteristics of individuals with an anterior open bite include one or more of the following: excessive gonial, mandibular and occlusal plane angles, small mandibular body and ramus, increased lower anterior facial height, decreased upper anterior facial height, retrusive mandible, increased anterior and decreased posterior facial height, class II tendency, divergent cephalometric planes, steep anterior cranial base (Lopez‐Gavito 1985), inadequate lip seal (Bell 1971).
Some studies (Proffit 1983; Straub 1960) have found a correlation between orofacial musculature and facial structure suggesting a relationship between weak musculature and a long face/anterior open bite pattern.
The interaction between an anterior open bite and non‐nutritive sucking habits, e.g. thumb or dummy sucking, is clear. Persistence of open bite is probably associated with neuromuscular imbalance or divergent growth pattern, although this is not well understood.
Although some studies have found that mouth breathing has an effect on the facial characteristics by increasing the vertical pattern of facial growth, open bites and crossbites (Harvold 1972; Linder‐Aronson 1970; Linder‐Aronson 1974; Ricketts 1968), data from one longitudinal study indicate that the effects of the mode of breathing on facial morphology are unsupported (Shanker 2004).
In addition, cephalometric studies of individuals with obstructive sleep apnoea (Kikuchi 2002) and mouth breathing (Juliano 2004), have found a characteristic cephalometric pattern which includes: long face and increased lower anterior facial height suggesting a hyper divergent pattern of skeletal open bite (Frankel 1983). Individuals with narrow airways and craniofacial anomalies may have increased risk for obstructive sleep apnoea (Jureyda 2004). However, the interactions between oral breathing, maxillofacial growth and clinical symptoms associated with sleep‐related breathing disorders are not clearly understood.
Due to the variety of theories on cause, a wide variety of treatments have been advocated for correcting anterior open bite (Erbay 1995; Frankel 1983; Kim 1987; Kuster 1992; Simões 2003) by either eliminating the cause or correcting dentofacial changes, with the objective of improving mastication, respiratory function and swallowing. However some studies have reported high relapse rates (Lopez‐Gavito 1985; Nemeth 1974).
Despite the existence of extensive literature on anterior open bite, interventions are not supported by strong scientific evidence. There is a need to investigate the anterior open bite literature due to the variety of treatments available and to determine if there is an association between open bite, respiratory pattern, respiratory disturbance and snoring because critical systemic disorders can occur (Ali 1993; Gottlieb 2003; Marcus 1998; O'Brien 2004; Smedje 2001).
Objectives
(1) To determine whether orthodontic and/or orthopaedic treatment in children with anterior open bite is effective at correcting the anterior open bite.
(2) To determine whether any one treatment is more effective than another.
(3) To determine whether treatment:
(a) reduces or cures snoring or sleep apnoea;
(b) reduces signs and symptoms of masticatory and swallowing dysfunction;
(c) changes other dentofacial characteristics ‐ maxillo‐mandibular width, height, length and dental position.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) of orthodontic and/or orthopaedic treatments to correct anterior open bite.
Trials using quasi‐random methods of allocation (such as alteration, date of birth, record number) will be included and subjected to a sensitivity analysis.
Types of participants
Children and adolescents in which over 80% of included participants are 16 years old or younger at the start of treatment, with anterior open bite (lack of contacts between upper and lower front teeth) ,who have stopped any sucking habits 1 year or more before treatment, do not have a class III skeletal relationship, cleft lip and/or palate or other syndrome associated with cranio‐facial anomalies.
Types of interventions
Orthodontic or orthopaedic treatment (not surgical) which have been used to correct anterior open bite. The main interventions of interest for this review are:
-
Orthopaedic functional appliances e.g.: Simões Network 2 (SN2), Simões Network 3 (SN3), Frankel's function regulator (RF4) and others.
-
Fixed orthodontic appliances e.g. Multiloop edgewise archwire (MEAW), Mcloughlin, Bennett, Trevisi techniques.
-
Removable orthodontic appliances e.g. tongue crib appliances, fixed intraoral habit appliances, removable habit‐breaker and others.
These interventions may be compared to: no intervention, or another technique.
Types of outcome measures
Primary
(1) Correction of the anterior open bite measured by contacts between upper and lower central incisors ‐ measured in plaster models, and/or cephalometric data as well as clinical assessment.
Secondary
(1) Stability of anterior open bite correction measured 1 year after treatment ‐ clinical assessment.
(2) Expansion of the upper and lower jaw measured,in plasters models, as changes in the width between the molars and/or canines.
(3) Incisors position and inclination measured in cephalometric data.
(4) Alteration of hyper divergent growth pattern measured in cephalometric data or facial analysis.
(5) Mandibular ramus growth measured in cephalometric data.
(6) Reduction of snoring measured by standard polysomnography.
(7) Signs and symptoms of respiratory disease: mouth breathing, nasal airway resistance measured by rhinomanometry, fibroscopy, clinical assessment.
(8) Signs and symptoms of atypical swallowing, and speech production disturbances measured by clinical assessment, validated tests for speech production, videofluoroscopy.
(9) Reduction or treatment of obstructive sleep apnoea syndrome (OSAS) or upper airway resistance syndrome (UARS), measured by standard polysomnography and body‐weight development curve compared by graphic of body mass index for age percentiles.
(10) Economic evaluation ‐ costs.
(11) Drop outs.
(12) Side effects ‐ tolerability ‐ patients' self report.
(13) Patients satisfaction measured by patients' self report.
Search methods for identification of studies
Studies will be searched independently of language and source of information. Non‐English language papers will be translated.
Electronic search
For identification of studies included or considered for this review detailed search strategies will be developed for each database searched. These will be based on the search strategy developed for MEDLINE but will be revised appropriately for the following databases:
-
Cochrane Oral Health Group Trials Register;
-
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, current Issue);
-
PubMed (1966 to present);
-
EMBASE (1980 to present);
-
Lilacs (1982 to present);
-
BBO (Bibliografia Brasileira de Odontologia) (1986 to present);
-
SciELO (1997 to present).
The Cochrane sensitive search strategy for RCTs (as published in Appendix 5c in the Cochrane Handbook for Systematic Reviews of Interventions) will be combined with specific phases 1 and 2. The combination of controlled vocabulary and free text terms will be used. MeSH terms are presented in upper case and free terms in lower case.
Phase 1
(OPEN BITE) OR MALOCCLUSION OR (TONGUE HABITS) OR (MOUTH BREATHING) OR (DEGLUTITION DISORDERS)
Phase 2
(ORTHODONTIC APPLIANCE* FUNCTIONAL) OR (ORTHODONTIC APPLIANCE* REMOVABLE) OR (ORTHOPEDIC APPLIANCE*) OR (ORTHODONTIC* PREVENTIVE) OR (ORTHODONTIC* INTERCEPTIVE) OR (ORAL APPLIANCE*) OR (Simões network*) OR (multi loop edgewise archwire) OR (straight wire technique*) OR (Frankel appliance*) OR (function* regulator) OR (bite blocks) OR (magnetic active corrector) OR (crib therapy) OR (tongue crib appliance*) OR (tongue thrust therapy) OR (lip seal training) OR (myofunctional therapy) OR (fixed intraoral habit appliance*) OR (removable habit* breaker) OR (thera spoon) OR (intruder molar) OR (dental device*) OR (intraoral device*) OR (dental appliance*) OR (oral device)
Search strategy for PubMed
PHASE 1
OPEN BITE OR MALOCCLUSION OR TONGUE HABITS OR MOUTH BREATHING OR DEGLUTITION DISORDERS OR maxil* OR mandibul* OR SWALLOW*
PHASE 2
ORTHODONTIC APPLIANCES FUNCTIONAL OR orthodontic appliances, functional OR ORTHODONTIC APPLIANCES REMOVABLE OR orthodontic appliances, removable OR ORTHOPEDIC APPLIANCE OR (ORTHODON* AND PREVENTIVE) OR (ORTHODON* AND INTERCEPTIVE) OR ORAL APPLIANCE OR Simões network* OR multiloop edgewise archwire OR straight wire technique* OR Frankel appliance* OR function* regulator* OR bite blocks OR magnetic active corrector OR crib therapy OR tongue crib appliance* OR tongue thrust therapy OR lip seal training OR myofunctional therapy OR fixed intraoral habit appliance* OR removable habit* breaker OR thera spoon OR intruder molar OR dental device* OR intraoral device* OR dental appliance* OR oral device
PHASE 3
randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized controlled trials [mh] OR random allocation [mh] OR double‐blind method [mh] OR single‐blind method [mh] OR clinical trial [pt] OR clinical trials [mh] OR ("clinical trial" [tw]) OR ((singl* [tw] OR doubl* [tw] OR trebl* [tw] OR tripl* [tw]) AND (mask* [tw] OR blind* [tw])) OR ( placebos [mh] OR placebo* [tw] OR random* [tw] OR research design [mh:noexp] OR comparative study [mh] OR evaluation studies [mh] OR follow‐up studies [mh] OR prospective studies [mh] OR control* [tw] OR prospectiv* [tw] OR volunteer* [tw]) NOT (animals [mh] NOT human [mh])
This search strategy should be linked together to run the search:
#1 (phase 1)
#2 (phase 2)
#3 (phase 3)
#4 (#1 AND #2 AND #3)
Search strategies for others databases are included in an additional table.
Cross‐checking references
References from original papers and review articles will be checked.
Personal communication
First authors of included studies and specialists will be contacted to identify further information about unpublished studies.
Handsearching
The following journals will be handsearched by two authors (Ye Qingsong (YQ) and Luo Junjie(LJ)):
-
Chinese Journal of Stomatology (1953 to 2005)
-
West China Journal of Stomatology (1983 to 2005)
-
Journal of Clinical Stomatology (1985 to 2005)
-
Stomatology (1981 to 2005)
-
Shangai Journal of Stomatology (1992 to 2005)
-
Journal of Modern Stomatology (1987 to 2005)
-
Journal of Practical Stomatology (1985 to 2005)
-
Journal of Comprehensive Somatology (1985 to 2005)
-
Chinese Journal of Dental Materials and Devices (1992 to 2005)
-
Chinese Journal of Orthodontics (1994 to 2005).
Data collection and analysis
Study selection
Titles and abstracts of all reports identified through the searches will be scanned by six authors (Debora Lentini‐Oliveira (DLO), Fernando Carvalho (FRC), Marco Machado (MAM), Lucila Prado (LBP),YE, LJ) and two authors (DLO, FRC) will independently assess the eligibility of all reports identified to this review. Agreement between authors will be assessed using the Kappa statistic (Landis 1977). Disagreements will be resolved by discussion with the main supervisor (Gilmar Prado (GFP)).
Data extraction
Data will be extracted by two authors (DLO, FRC) who will independently and in duplicate record :
(a) year of publication, author;
(b) methods: randomisation procedure, blindness, design, analysis (intention‐to‐treat), allocation and duration;
(c) participants:
-
sample size
-
age of individuals
-
gender
-
diagnosis (criteria)
-
diagnosis (characteristics: anterior open bite, anterior open bite and crossbite, anterior open bite and overjet, anterior open bite with crossbite and overjet)
-
history;
(d) interventions: intervention, duration and sample size;
(e) outcomes.
Quality assessment:
The quality assessment of the included trials will be undertaken independently and in duplicate by two authors (DLO , FRC) as part of the data extraction process. The agreement between the authors will be assessed by calculating the Kappa score (Landis 1977). If there is disagreement, the main supervisor (GFP) will be consulted.
Four main quality criteria will be examined:
(1) Allocation concealment, recorded as:
(A) adequate;
(B) unclear;
(C) inadequate;
(D) not used;
as described in the Cochrane Handbook for Systematic Reviews of Interventions.
The items 2, 3 and 4 will be assessed with the following criteria:
met: criteria were described in the publication or acquired from the author and properly applied;
unclear: not described and impossible to be acquired from the author;
not met: criteria were described in the publication or acquired from the author, but improperly applied.
(2) Blind outcome assessment.
(3) Completeness of follow up.
Did the study consider no more than 20% of withdrawals and /or substantial difference between two comparison groups?
(4) Intention‐to‐treat analysis.
All randomised participants were analysed?
Methodological judgements will be applied according to criteria 2, 3, and 4 as follows.
Studies will be classified as low bias risk when all of the criteria met, moderate bias risk when all criteria are at least partly met and high bias risk when one or more criteria not met (Green 2005).
Data analysis
The Cochrane Oral Health Group statistical guidelines will be followed. The data will be analysed using RevMan and reported according to Cochrane Collaboration criteria.
Risk ratios, the number needed to treat and corresponding 95% confidence intervals will be calculated for dichotomous data and expressed by individual study. In cases where the included studies present results as continuous data, we will express the results as weighted mean difference and 95% confidence intervals. For both continuous and dichotomous data we will carry out a meta‐analysis, when appropriate.
Heterogeneity will be assessed using Cochran's test. If significant heterogeneity (P < 0.1) is detected, regarding the methodological and clinical diversity inherent to the clinical question of this systematic review), the significance of the treatment effects will be assessed using a random‐effects model.
An assessment of publication bias, will be attempted by using data to plot a funnel graph (trial effect versus trial size).
Subgroup analysis
-
Subgroup analysis will be carried out on the age (stage of dental development) that treatment was carried out.
-
Different characteristics (anterior open bite, anterior open bite and crossbite, anterior open bite and overjet, anterior open bite with crossbite and overjet) will be analysed and presented separately.
-
Different interventions will be analysed and presented separately.
Sensitivity analysis will be made according to the methodological judgements of included studies.