Tratamiento ortodóntico y ortopédico para la mordida abierta anterior en niños
Resumen
Antecedentes
La mordida abierta anterior se produce cuando no hay superposición vertical de los incisivos superiores e inferiores. La etiología es multifactorial e incluye: hábitos orales, patrones de crecimiento desfavorables, tejido linfático agrandado con respiración bucal. Se han propuesto varios tratamientos para corregir esta maloclusión, pero las intervenciones no están respaldadas por evidencia científica sólida.
Objetivos
El objetivo de esta revisión sistemática fue evaluar los tratamientos ortodónticos y ortopédicos para corregir la mordida abierta anterior en niños.
Métodos de búsqueda
Se realizaron búsquedas en las siguientes bases de datos: el Registro de Ensayos del Grupo Cochrane de Salud Oral (Cochrane Oral Health Group) (hasta el 14 de febrero de 2014); el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL) (la Cochrane Library 2014, número 1); MEDLINE vía OVID (1946 hasta el 14 de febrero de 2014); EMBASE vía OVID (1980 hasta el 14 de febrero de 2014); LILACS vía BIREME Virtual Health Library (1982 hasta el 14 de febrero de 2014); BBO vía BIREME Virtual Health Library (1980 hasta el 14 de febrero de 2014) y SciELO (1997 hasta el 14 de febrero de 2014). Se buscaron los ensayos en curso a través de ClinicalTrials.gov (hasta el 14 de febrero de 2014). Se hicieron búsquedas manuales en revistas chinas y se recuperaron las bibliografías de los trabajos.
Criterios de selección
Todos los ensayos controlados aleatorizados o cuasialeatorizados de tratamientos ortodónticos u ortopédicos o ambos para corregir la mordida abierta anterior en los niños.
Obtención y análisis de los datos
Dos autores de la revisión, de forma independiente, evaluaron la elegibilidad de todos los informes identificados.
Para los datos dicotómicos se calcularon los riesgos relativos (RR) y los correspondientes intervalos de confianza (IC) del 95%. Los datos continuos se expresaron tal como los describió el autor.
Resultados principales
Se incluyeron tres ensayos controlados aleatorizados que compararon: los efectos del regulador de la función de Frankel‐4 (RF‐4) con el entrenamiento de sellado labial versus ningún tratamiento; imanes de repulsión versus placas de mordida; y rejilla palatina con mentonera de tracción occipital versus ningún tratamiento.
El estudio que comparó imanes de repulsión versus placas de mordida no se pudo analizar porque los autores interrumpieron el tratamiento antes de lo previsto debido a los efectos secundarios en cuatro de diez pacientes.
El RF‐4 asociado con el entrenamiento de sellado labial (RR 0,02 [IC del 95%: 0,00 a 0,38]) y la rejilla palatina extraíble asociada con la mentonera de tracción occipital (RR 0,23 [IC del 95%: 0,11 a 0,48]) pudieron corregir la mordida abierta anterior.
Ningún estudio describió el proceso de asignación al azar, el cálculo del tamaño de la muestra, no hubo cegamiento en el análisis cefalométrico y los dos estudios evaluaron dos intervenciones al mismo tiempo. Por consiguiente, estos resultados se deben considerar con cautela.
Conclusiones de los autores
Hay evidencia débil de que las intervenciones RF‐4 con entrenamiento de sellado labial y la rejilla palatina asociada con la mentonera de tracción occipital son capaces de corregir la mordida abierta anterior. Debido a que los ensayos incluidos tienen un sesgo potencial, estos resultados se deben observar con cautela. Las recomendaciones para la práctica clínica no se pueden hacer sólo sobre la base de los resultados de estos ensayos. Se necesitan más ensayos controlados aleatorizados para dilucidar las intervenciones para el tratamiento de la mordida abierta anterior.
Resumen en términos sencillos
Tratamiento ortodóntico y ortopédico para la mordida abierta anterior en niños
Las intervenciones pudieron corregir la mordida abierta anterior, pero este hallazgo se basó en los datos de dos estudios con problemas de calidad.
La mordida abierta se caracteriza por la falta de superposición vertical de los incisivos superiores e inferiores. Este problema tiene varias causas posibles como la respiración bucal, los hábitos de succión, la alteración del desarrollo de la mandíbula y el maxilar. Puede dificultar el habla, la deglución, la masticación y la estética. Se han utilizado varios tratamientos para corregir la mordida abierta anterior. Los autores de la revisión evaluaron tres estudios con los siguientes tratamientos: El regulador de la función de Frankel‐4 (RF‐4) con entrenamiento de sellado labial, rejilla palatina con mentonera de tracción occipital e imanes de repulsión versus placas de mordida. Este último estudio no se pudo analizar porque el autor interrumpió el tratamiento antes de lo previsto debido a los efectos secundarios.
Authors' conclusions
Background
Open bite is a lack of vertical overlap or contact of the upper and lower incisors. It may occur with an underlying class I, class II or class III skeletal pattern. The cause of an anterior open bite is generally multifactorial and can be due to a combination of skeletal, dental and soft tissue effects (Figure 1). Many potential aetiological factors have been considered, including unfavourable growth patterns (Bell 1971; Nahoum 1977), digit sucking habits (Mizrahi 1978; Subtelny 1964), enlarged lymphatic tissue (Subtelny 1964), heredity (Mizrahi 1978; Sassouni 1969) and oral functional matrices (Moss 1971). The prevalence ranges from 17% to 18% of children in the mixed dentition (Cozza 2005; Silva Filho 1989; Tausche 2004). When associated with sucking habits, the prevalence increases to 36.3% (Cozza 2005).

Characteristics of skeletal anterior open bite
1. Anterior open bite
2. Frankfurt plane
3. Mandibular plane
4. Maxillary plane
5. Gonial angle
6. Lower anterior facial height
The characteristics of individuals with an anterior open bite include one or more of the following: excessive gonial, mandibular and occlusal plane angles, small mandibular body and ramus, increased lower anterior facial height, decreased upper anterior facial height, retrusive mandible, increased anterior and decreased posterior facial height, class II tendency, divergent cephalometric planes, steep anterior cranial base (Lopez‐Gavito 1985), and inadequate lip seal (Bell 1971).
Some studies (Proffit 1983; Straub 1960) have found a correlation between orofacial musculature and facial structure suggesting a relationship between weak musculature and a long face or between tongue position and anterior open bite pattern.
The interaction between an anterior open bite and non‐nutritive sucking habits, e.g. thumb or dummy sucking, is clear. Persistence of open bite is probably associated with neuromuscular imbalance or divergent growth pattern, although this is not well understood.
Although some studies have found that mouth breathing has an effect on the facial characteristics by increasing the vertical pattern of facial growth, open bites and crossbites (Harvold 1972; Linder‐Aronson 1970; Linder‐Aronson 1974; Ricketts 1968), data from one longitudinal study indicate that the effects of the mode of breathing on facial morphology are unsupported (Shanker 2004).
In addition, cephalometric studies of individuals with obstructive sleep apnoea (Kikuchi 2002) and mouth breathing (Juliano 2005), have found a characteristic cephalometric pattern which includes: long face and increased lower anterior facial height suggesting a hyper divergent pattern of skeletal open bite (Frankel 1983). Individuals with narrow airways and craniofacial pattern may have increased risk for obstructive sleep apnoea (Jureyda 2004). However, the interactions between oral breathing, maxillofacial growth and clinical symptoms associated with sleep‐related breathing disorders are not clearly understood.
Due to the variety of theories on cause, a wide variety of treatments have been advocated for correcting anterior open bite (Erbay 1995; Frankel 1983; Kim 1987; Kuster 1992; Simões 2003) by either eliminating the cause or correcting dentofacial changes, with the objective of improving mastication, respiratory function and swallowing. However some studies have reported high relapse rates (Lopez‐Gavito 1985; Nemeth 1974).
Despite of the existence of extensive literature on anterior open bite, interventions are not supported by strong scientific evidence. There is a need to investigate the anterior open bite literature due to the variety of treatments available. And to determine if there is an association between open bite, respiratory pattern, sleep respiratory disturbance and snoring due to critical systemic disorders that can occur when these diseases occur (Ali 1993; Gottlieb 2003; O'Brien 2004; Smedje 2001).
Objectives
(1) To determine whether orthodontic or orthopaedic treatment or both in children with anterior open bite is effective at correcting the anterior open bite (dental, dento‐alveolar and/or skeletal).
(2) To determine whether any one treatment is more effective than another.
(3) To determine whether treatment:
(a) reduces or cures snoring or sleep apnoea;
(b) reduces signs and symptoms of masticatory and swallowing dysfunction;
(c) changes other dentofacial characteristics ‐ maxillo‐mandibular width, height, length and dental position.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) of orthodontic or orthopaedic treatments or both to correct anterior open bite.
Trials using quasi‐random methods of allocation (such as alternation, date of birth, record number) were included and subjected to a sensitivity analysis.
Types of participants
Children and adolescents of which over 80% of included participants are 16 years old or younger at the start of treatment, with anterior open bite (lack of contact or vertical overlap between upper and lower front teeth), who have stopped any sucking habits 1 year or more before treatment, do not have a class III skeletal relationship, cleft lip or palate or both, or other syndrome associated with craniofacial anomalies.
Types of interventions
Orthodontic or orthopaedic treatment (not surgical) which has been used to correct anterior open bite. The main interventions of interest for this review were.
-
Orthopaedic functional appliances e.g. Simões Network 2 (SN2), Simões Network 3 (SN3), Frankel's function regulator‐4 (FR‐4) and others.
-
Fixed orthodontic appliances e.g. multiloop edgewise archwire (MEAW), Mcloughlin, Bennett, Trevisi techniques.
-
Removable orthodontic appliances e.g. tongue crib appliances, fixed intraoral habit appliances, removable habit‐breaker and others.
These interventions may be compared to: no intervention, or another technique.
Types of outcome measures
Primary
(1) Correction of the anterior open bite measured by contacts/overlap between upper and lower central incisors ‐ measured in plaster models, and/or cephalometric data as well as clinical assessment.
Secondary
(1) Stability of anterior open bite correction measured 1 year after treatment by clinical assessment.
(2) Expansion of the upper and lower jaws measured in plaster models, as changes in the width between the molars or canines or both.
(3) Incisors position and inclination measured in cephalometric data.
(4) Alteration of hyper divergent growth pattern measured in cephalometric data or by facial analysis.
(5) Mandibular ramus growth measured in cephalometric data.
(6) Reduction of snoring measured by standard polysomnography.
(7) Signs and symptoms of respiratory disease: mouth breathing, nasal airway resistance measured by rhinomanometry, fibroscopy, clinical assessment.
(8) Signs and symptoms of atypical swallowing, and speech production disturbances measured by clinical assessment, validated tests for speech production, videofluoroscopy.
(9) Reduction or treatment of obstructive sleep apnoea syndrome (OSAS) or upper airway resistance syndrome (UARS), measured by standard polysomnography and body‐weight development curve compared by graphic of body mass index for age percentiles.
(10) Economic evaluation ‐ costs.
(11) Drop outs.
(12) Side effects ‐ tolerability ‐ patients' self report.
(13) Patient satisfaction measured by patients' self report.
Search methods for identification of studies
The search attempted to identify all relevant studies, regardless of the language and source. Duplicate records were identified and removed.
Electronic searches
For the identification of studies included or considered for this review, we developed detailed search strategies for each database searched. These were based on the search strategy developed for MEDLINE (OVID) but revised appropriately for each database. The search strategy used a combination of controlled vocabulary and free text terms and was linked with the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials (RCTs) in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 (updated March 2011) (Higgins 2011). Details of the MEDLINE search are provided in Appendix 3. The search of EMBASE was linked to the Cochrane Oral Health Group filter for identifying RCTs, and the search of LILACS and BBO were linked to the Brazilian Cochrane Center filter.
The following databases were searched:
-
the Cochrane Oral Health Group's Trials Register (to 14 February 2014) (Appendix 1);
-
the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2014, Issue 1) (Appendix 2);
-
MEDLINE via OVID (1946 to 14 February 2014) (Appendix 3);
-
EMBASE via OVID (1980 to 14 February 2014) (Appendix 4);
-
LILACS via BIREME Virtual Health Library (1982 to 14 February 2014) (Appendix 5);
-
Brazilian Bibliography of Odontology (BBO) via BIREME Virtual Health Library (1980 to 14 February 2014) (Appendix 6);
-
SciELO (1997 to 14 February 2014) (Appendix 7)
-
ClinicalTrials.gov (to 14 February 2014) (Appendix 8).
Searching other resources
Cross‐checking references
References from original papers and reviewed articles were checked and no further randomised controlled trials were found.
Personal communication
The first authors of included studies and specialists were contacted to identify further information about unpublished or ongoing studies.
Handsearching
The following journals were handsearched by two authors of this review (QY, JL) until 2005 and updated by two review authors (QY, RH):
-
Chinese Journal of Stomatology (1953 to April 2013)
-
West China Journal of Stomatology (1983 to April 2013)
-
Journal of Clinical Stomatology (1985 to April 2013)
-
Stomatology (1981 to 2005)
-
Shangai Journal of Stomatology (1992 to April 2013)
-
Journal of Modern Stomatology (1987 to April 2013)
-
Journal of Practical Stomatology (1985 to April 2013)
-
Journal of Comprehensive Somatology (1985 to April 2013)
-
Chinese Journal of Dental Materials and Devices (1992 to April 2013)
-
Chinese Journal of Orthodontics (1994 to April 2013).
Language
There were no language restrictions in the electronic searches.
Data collection and analysis
Study selection
The titles and abstracts of all reports identified through the searches were scanned by five authors of this review (Debora Lentini‐Oliveira (DLO), Fernando Carvalho (FC), Lucila Prado (LP), Qingsong Ye (QY) and Rongdang Hu (RH) and three authors (DLO, FC, HMS) assessed the eligibility of all identified reports independently. Disagreements about the eligibility of these reports were resolved by discussion and consensus.
Data extraction
Data were extracted by two review authors who independently and in duplicate recorded:
(a) year of publication, author;
(b) methods: randomisation procedure, blindness, design, analysis (intention‐to‐treat), allocation and duration;
(c) participants:
-
sample size
-
age of individuals
-
gender
-
diagnosis (criteria)
-
diagnosis (characteristics: anterior open bite, anterior open bite and crossbite, anterior open bite and overjet, anterior open bite with crossbite and overjet)
-
history;
(d) interventions: intervention, duration and sample size;
(e) outcomes.
Quality assessment
The quality assessment of the included trials was undertaken independently and in duplicate by two review authors as part of the data extraction process. There was agreement between the review authors (Kappa = 1).
The following parameters of methodological quality were assessed.
(1) Allocation concealment, recorded as:
(A) adequate;
(B) unclear;
(C) inadequate;
as described in the Cochrane Handbook for Systematic Reviews of Interventions 4.2.6.
(2) Blind outcome assessment.
(3) Completeness of follow up.
Did the study consider no more than 20% of withdrawals or substantial difference between two comparison groups or both?
(4) Intention‐to‐treat analysis.
Were all randomised participants analysed?
Parameters (2), (3) and (4) were assessed with the following criteria:
met: criteria were described in the publication or acquired from the author and properly applied;
unclear: not described and impossible to be acquired from the author;
not met: criteria were described in the publication or acquired from the author, but improperly applied.
Studies were classified as low bias risk when all criteria were met, as moderate bias risk when all criteria were at least partly met and as high bias risk when one or more criteria were not met (Higgins 2006).
Data analysis
The Cochrane Collaboration statistical guidelines were followed. The data were analysed using RevMan and reported according to Cochrane Collaboration criteria.
Risk ratios and corresponding 95% confidence intervals were calculated for dichotomous data and expressed by individual study. In cases where the included studies presented results as continuous data, the results were presented as described by the author.
Data synthesis
The following data synthesis was planned, but the number of studies was insufficient and they evaluated different interventions for a meta‐analysis or any of the other procedures below to be conducted:
(1) to assess heterogeneity by Cochran's test;
(2) to undertake a sensitivity analysis excluding low quality studies;
(3) subgroup analysis carried out on age (stage of dental development), different characteristics (anterior open bite, anterior open bite and crossbite, anterior open bite and overjet, anterior open bite with crossbite and overjet) and dental, dento‐alveolar or skeletal anterior open bite;
(4) to investigate publication and other biases by drawing a funnel plot.
Despite the existence of sufficient data to calculate the mean difference (MD) we decided only to describe data because of the poor quality of the trials. We think that to calculate MD or the number needed to treat (NNT) could confound readers and not help them.
Results
Description of studies
Results of the search
Through search strategy, we retrieved 576 records from the electronic database search: 75 from the Cochrane Oral Health Group's Trial Register, 56 from CENTRAL, 368 from MEDLINE via OVID, 30 from EMBASE, via OVID, 26 from LILACS, 21 from BBO via BIREME. After removing duplicates this number was reduced to 453. Following screening, 21 records were considered to be potentially eligible, and sought for further detailed assessment. Ten studies: three thesis (Cassis 2009; Ferreira 2008; Torres 2008) and seven articles (Bennett 1999; Cassis 2010; Cozza 2007b; Giuntini 2008; Kuster 1992; Moore 1989; Sharma 2009) were excluded due to the reasons outlined in the Characteristics of excluded studies table. Three studies (one thesis and two articles) were included (Almeida 2005; Erbay 1995; Kiliaridis 1990). One study is awaiting assessment (Doshi 2010).
Two review authors handsearched all the related Chinese dental journals until 2005 independently, then combined the results (first publication). Both authors identified five clinical studies from the indexes related to interventions for open bite (Hu 2003; Hu 2004; Li 2002; Wang 2003; Zou 2003) but after reading the complete articles, none were found to be relevant. To check it again, they handsearched together for a third time, with no change in the outcome. In the update (2006 to present), two review authors identified two more studies (Hu 2009; Liu 2007) but neither of them was an RCT and therefore both were excluded.
We contacted the authors of the three excluded thesis (Cassis 2009; Ferreira 2008; Torres 2008) and three publications derived from these three thesis were identified but they were not included because they were retrospective studies.
Included studies
Characteristics of trial setting and investigators
Of the three included studies, one was conducted in Sweden (Kiliaridis 1990), one in Turkey (Erbay 1995) and one in Brazil (Almeida 2005). This last study was published as a thesis in 2005.
None of them described the method of randomisation, allocation concealment and the calculation of sample size. None described ethical approval and only one (Almeida 2005) accounted that informed consent was obtained.
None of the three included studies had drop outs and only one had blind outcome assessment (Kiliaridis 1990).
The randomisation process was obtained after contact with only one of the authors (Almeida 2005) that informed that all the patients were divided, without any criteria, in two folders. All children in the first folder were treated and all patients in the second folder were controlled without treatment. After 1 year, 30 patients in each group were chosen at random by one of the authors. Then, these patients were analysed.
Characteristics of participants
Two studies had skeletal anterior open bite in their inclusion criteria, but with differences. Kiliaridis 1990 established as criterion that participants showed a vertical skeletal dysplasia, verified at least by one of the following cephalometric values, i.e. a steep mandibular plane, increased lower anterior facial height and a large gonial angle, but the cut off point was not defined.
Erbay 1995 defined this cut off point as a steep mandibular plane angle (SN/GoMe angle > 37 degrees) and Almeida 2005 did not include skeletal anterior open bite as criterion. The inclusion criterion of Almeida 2005 was anterior open bite independently of the type.
The ages of the participants were similar in Erbay 1995 and Almeida 2005. They respectively included children between 7 years and 5 months and 9 years and 3 months; and children between 7 years and 9 years and 11 months. In Kiliaridis 1990, the age ranged between 8 years and 9 months and 16 years and 1 month.
Anterior open bite of at least 1 mm was inclusion criterion to Erbay 1995 and Almeida 2005. Kiliaridis 1990 did not include this criterion.
Only one study considered in its criteria that they had no record of sucking habits.
Sexual dimorphism was evaluated and not found in Erbay 1995 and Almeida 2005.
The sample size was 20 participants in Kiliaridis 1990, 40 participants in Erbay 1995 and 60 participants in Almeida 2005.
Characteristics of interventions
One study compared the effects of Frankel's function regulator‐4 with lip‐seal training versus no treatment (Erbay 1995), another trial compared repelling‐magnet splints versus bite‐blocks (Kiliaridis 1990) and the other compared removable appliance with palatal crib associated with high‐pull chincup versus no treatment (Almeida 2005).
All three trials provided a clear description of the type and duration of the intervention for both the test and control groups.
Description of interventions
(1) Frankel's function regulator‐4 (FR‐4) and lip‐seal training (Erbay 1995).
The FR‐4 appliance had two buccal shields, two lower lip pads, a palatal bow, an upper labial wire, and four occlusal rests on the upper permanent first molars and upper deciduous first molars. Lip‐seal training consisted of holding a plastic spatula between the lips during homework and while watching television.
Duration of treatment: 2 years.
(2) Repelling‐magnet splints versus bite‐blocks (Kiliaridis 1990).
The components of repelling‐magnet splints consisted of two posterior occlusal splints, one for the upper, and one for the lower jaw. Samarium cobalt magnets have been incorporated into the acrylic splints, over the occlusal region of the teeth planned to be intruded. The two appliances had posterior acrylic of the same thickness. Both appliances provided intrusion of the posterior teeth.
Duration of treatment: 6 months.
(3) Removable appliances with palatal crib associated with high‐pull chincup (Almeida 2005).
The palatal crib was constituted of retention brace in first permanent molars or second deciduous molars, vestibular arch, palatal crib and resin plaque covering the palate.
The high‐pull chincup was a vertical chincup constituted of a casket and a chin support. The direction of strength was 45 degrees and the intensity was 450 force grams.
Duration of treatment: 12 months.
Characteristics of outcome measures
Of the outcomes proposed in this systematic review, five were evaluated in the included studies:
(1) Anterior open bite correction (Almeida 2005; Erbay 1995; Kiliaridis 1990)
(2) Incisors position and inclination (Almeida 2005; Erbay 1995)
(3) Alteration of hyper divergent growth pattern (Almeida 2005; Erbay 1995)
(4) Mandibular ramus growth (Almeida 2005; Erbay 1995)
(5) Expansion of the upper and lower jaw (Almeida 2005).
In Kiliaridis 1990 the outcomes were measured by cephalometric growth analysis with cephalograms superimposed on the anterior cranial base. Dental casts, intraoral photographs and lateral cephalograms were taken before and after treatment and used to assess dental and skeletal changes.
The two other studies measured outcomes by different cephalometric measures compared before and after treatment.
Excluded studies
Reasons for exclusion of a trial from the review are given in the Characteristics of excluded studies table. The 24 studies were excluded for the following reasons: non‐random, retrospective studies, different outcomes. Although described as randomised, one trial (Bennett 1999) was excluded because the age of the patients was not recorded and it was not possible to obtain it from the author.
Risk of bias in included studies
The quality of the analysed trials has been assessed according to criteria in the Cochrane Handbook for Systematic Reviews of Interventions 4.2.6.
In Erbay 1995 the groups were similar (age, open bite type, gender); there was completeness of follow up; all cephalometric radiographs were traced by a single investigator, but it is unclear if there was blinding evaluation. Two interventions were tested at the same time: Frankel's function regulator‐4 and lip‐seal training. They were not measured separately, so there is potential bias: the results can be attributed either to the appliance or to lip‐seal exercises. It was not possible to obtain the randomisation process from the author. For these reasons, this study was classified as B for allocation concealment and of moderate bias risk.
Kiliaridis 1990 had similar groups, except intervention (age, open bite type, gender); the size of the combined error method in locating, superimposing and measuring the changes of the different landmarks was calculated and did not exceed 0.8 mm for any of the cephalometric measurements used or 0.4 mm for the measurements of the vertical overbite on the dental casts; the analysis was performed by one of the authors without knowing the group to which the patients belonged; there was a small sample size and there was interruption of the treatment earlier than planned because of side effects. The fact that the authors were forced to change the experimental design in one group did not allow them to evaluate statistically the results of the two treatments tested. This study was therefore classified as B for allocation concealment and of high bias risk.
Almeida 2005 had similar groups (age, skeletal maturation, open bite type, gender); the authors examined random and systematic error when measuring cephalogram radiographs; there was completeness of follow up. The method used to allocate the participants was inadequate. Two interventions were tested at the same time: removable appliance with palatal crib and high‐pull chincup. Their effects were not measured separately. Considerations should be made in relation to the results that can be attributed either to removable appliance or to high‐pull chincup. Oral habits were not evaluated. There was no blinding in the cephalometric analysis. This information was obtained from the author. The sample size calculation was not made. The study was classified as C for allocation concealment and of high bias risk.
Effects of interventions
The search strategy identified over 1895 titles and abstracts and from these we obtained 28 full reports. Only three studies were included.
Frankel's function regulator‐4 (FR‐4) and lip‐seal training versus no treatment
(Erbay 1995)
Thirty cephalometric measurements in the sagittal and vertical planes were used to evaluate the outcomes. Of these 30 parameters, only 16 parameters had results which were determined to be essentially related to the treatment. Of the outcomes proposed by this systematic review, the results of the four evaluated by the author are described as following.
Open bite correction
The mean overbite changed from ‐3.9 (standard deviation (SD) 1.3) mm before treatment to 1.1 (SD 0.9) mm after treatment in the intervention group; with difference of 5.0 (SD 1.3), P < 0.001, indicating that skeletal anterior open bite was successfully corrected in all patients. However, overbite remained negative in the control group, ranging from ‐3.5 (SD 1.4) mm initially to ‐2.1 (SD 1.8) mm in the end; with difference of 1.4 (SD 1.8) mm, P < 0.01. Risk ratio (RR) = 0.02 (95% confidence interval (CI) 0.00 to 0.38).
Position of the incisors
The angulation of the upper incisors with the palatal plane (1/ANSPNS) remained almost constant during the study period, decreasing an average of 0.3 (SD 4.6) degrees in the control group whereas in the treated group the mean degree of retrusion was 4 (SD 4.6) degrees, P < 0.01. There was significant improvement in the degree of retrusion of the upper incisors in the treated group.
Alteration of hyper divergent growth pattern
In the treated group total anterior facial height (N‐Me) and upper anterior facial height (N‐ANS) showed an increment of 3.9 (SD 1.8) mm and 3.3 (SD 1.2) mm respectively. However, the control group demonstrated significantly greater increase in total anterior facial height (N‐Me = 7.3 (SD 2.6) mm, P < 0.001), but a similar change in upper anterior facial height (N‐ANS = 3.0 (SD 1.7) mm).
Measurement of lower anterior facial height (ANS‐Me) indicated that significant growth increment occurred in the control group (4.2 (SD 2.3) mm, P < 0.001), but remained almost constant in the treated group (0.6 (SD 1.6) mm).
The rate of growth in total posterior facial height (S‐Go) in the treated group (4.5 (SD 1.6) mm) exceeded that of the control group (3.6 (SD 2.5) mm, P < 0.05).
There was reduction in mandibular plane angles in the treated group (SN/GoMe = 2.8 (SD 1.1) degrees, P < 0.001; ANSPNS/GoMe = 4.6 (SD 2.6) degrees, P < 0.001), and in the control group respectively (0.7(SD 1.9) and 0.8 (SD 1.5) degrees, P < 0.05).
All these results indicate that the development pattern of the mandible was altered through upward and forward mandibular rotation in the treated group.
Mandibular ramus growth
The author reported no difference between groups in the mandibular ramus growth.
Repelling‐magnet splints versus bite‐blocks
(Kiliaridis 1990)
After 4 months the open bite was observed to close in the magnet group, but in four out of these ten patients, transverse problems were observed (unilateral crossbite) which led to the interruption of the treatment earlier than planned. These patients had used their appliances for 24 hours daily.
The authors reported that the bite‐blocks group showed improvement in the dental vertical relation, but it is not clear how many patients had their anterior open bite closed.
Removable appliances with palatal crib associated with high‐pull chincup versus no treatment
Open bite correction
The treatment group did not have closure of the anterior open bite in six patients, and the control group had spontaneous closure of the open bite in four patients. So, in the control group, 26 patients did not have closure of the anterior open bite (RR = 0.23 (95% CI 0.11 to 0.48)).
Position of the incisors
The author reported that data (1.NA, 1‐NA, 1‐PP, 1.NB, 1‐NB, 1‐GoMe) showed statistically significant difference. There was palatal inclination of the upper incisors in the intervention group that contributed to the closure of the anterior open bite. There was protrusion of the upper incisors in the control group.
Alteration of hyper divergent growth pattern and mandibular ramus growth
The author reported that the angles (SN.GoGN, SN.PP and NS.Gn) and linear measures (AFA, AFP and AFAI) did not demonstrate significant alterations between groups.
And also the cephalometric data (SNA, Co‐A, SNB, Ar‐Go, Ar.GoMe, Co‐Gn, ANB) were reported by the author to be not significantly different between groups.
The results indicate that interventions did not produce significant changes on the skeletal maxillary or mandibular components. The effects were dento‐alveolar.
Discussion
Methodology
There is a great number of controlled trials evaluating anterior open bite treatment, however many do not randomise participants, but divide them following criteria such as: growing patients versus not growing patients (Kim 2000) or matched for age, sex, amount of open bite (Iscan 1997; Ngan 1992; Sankey 2000). Therefore only three randomised controlled trials (RCTs) were included in this review.
None of the three included trials described the method of randomisation or the calculation of sample size.
The randomisation is described in the three studies by only one phrase. First named authors were written to about this and only one author answered and provided information on the randomisation process (Almeida 2005). The process was inadequate, without allocation concealment.
The methods used to create a sequence of aleatory allocation such as random numbers table, random sequence created by computer, besides allocation concealment, prevent that voluntarily or involuntarily investigators influence the process of allocation. This is an important bias found in these studies.
None of these studies calculated sample size. Although the results had been significant statistically, the studies analysed did not evaluate the probably (power) to detect if important statistical and clinical differences exist. Pilot studies can collaborate to define the adequate sample size.
In the results analyses, only Kiliaridis 1990 was concerned with blind outcomes assessment. The other studies had outcomes evaluated by one of the investigators that may have involuntarily influenced the results.
Besides, sucking habits may have been an important confounder of the results. Almeida 2005 and Erbay 1995 did not consider this question.
In Almeida 2005 and Erbay 1995, two interventions were used at the same time. It is possible that the simultaneous use of these interventions results in a number of desirable treatment effects greater than those induced by each appliance separately, but the effective changes can only be known if these interventions were compared separately.
Results
Outcomes
Cephalometric data have frequently been used to evaluate treatments. In the clinical experience, other instruments have been used such as facial analysis (Suguino 1996), gnatosthatic cast (Planas 1994) or other non‐validated instruments.
Each author used different cephalometric analyses to evaluate the changes, comparing data before and after treatment or through superimposition on the anterior cranial base. There are not standardizing or validity of measures. Although, cephalograms are traditionally used, they have limitations because most orthodontics planes and angles do not represent actual, key sites of remodeling or growth activity (Enlow 1983).
Only five outcomes proposed in this systematic review were found in the three included studies: open bite correction, alteration of hyper divergent growth pattern, incisors position and inclination, mandibular ramus growth and expansion of the upper and lower jaw.
Anterior open bite correction
The measurement of overbite was not defined by Kiliaridis 1990 and it was different for the two other studies. Erbay 1995 defined it as the distance between incisal points of the upper and lower central incisors when these points are projected onto N‐Me line and Almeida 2005 defined it as the vertical distance from the upper incisal face to the lower incisal face.
Alteration of hyper divergent growth pattern
Each author used different cephalometric data to evaluate the changes. Erbay 1995 established a cut off point of steep mandibular plane > 37 degrees and Kiliaridis 1990 defined this skeletal plane when the participant had one of three representative measures of skeletal pattern, i.e. a steep mandibular plane, increased lower anterior facial height and a large gonial angle. In literature, the cut off point to the skeletal open bite pattern was defined by Ngan 1992 as ratio of posterior facial height (sella‐gonion) to anterior facial height (nasion‐menton) of less than 62%. There is not concordance among authors.
Position of the incisors
Erbay 1995 used the angles 1/ANSPNS and 1/GoMe and Almeida 2005 used the measures 1.NA, 1‐NA, 1‐PP, 1.NB, 1‐GoMe.
Mandibular ramus growth
Almeida 2005 and Erbay 1995 used the same linear measure: Ar‐Go.
The other outcomes proposed in this review were not found: stability of anterior open bite correction; reduction of snoring; signs and symptoms of respiratory disease: mouth breathing, nasal airway resistance; signs and symptoms of atypical swallowing, and speech production disturbances; reduction or treatment of obstructive sleep apnoea syndrome (OSAS) or upper airway resistance syndrome (UARS); economic evaluation ‐ costs; side effects ‐ tolerability; and patients satisfaction.
Interactions between mouth breathing and facial morphology, including anterior open bite, have been discussed for many years (Linder‐Aronson 1970; Linder‐Aronson 1974; Ricketts 1968; Sankey 2000) and only recently has there been concern about the interrelation between malocclusion and sleep respiratory disturbance.
Due to critical systemic disorders that can occur, the outcomes of treatment of anterior open bite should be extended, considering implications to the global health of individuals and clinically relevant questions such as interaction with mouth breathing, or sleep‐disordered breathing. On the other hand, outcomes of treatment of sleep‐disordered breathing should include facial morphology evaluation. In spite of that, neither orthodontists, orthopaedists or sleep researchers have included these outcomes in their studies.
Results
The results of the included studies demonstrated weak evidence that the interventions Frankel's function regulator‐4 (FR‐4) with lip‐seal training and removable palatal crib with high‐pull chincup are able to correct open bite in children through skeletal or dento‐alveolar effects. However, studies show a lack of standardization of diagnostic criteria, inclusion criteria, validity measures to evaluate outcomes and important methodological limitations.
There are many other interventions to correct anterior open bite that are frequently used in orthodontic and orthopaedic clinical practice such as Simões Network 2 (SN2), Simões Network 3 (SN3), multiloop edgewise archwire (MEAW), bite‐blocks and others. These interventions should be tested in randomised controlled clinical trials and later compared, to define which is or which are the best interventions.
It is suggested that the Consolidated Standards of Reporting Trials (CONSORT) guidelines (Moher 2001) are followed to improve the reliability and the quality of these studies that take a long time, are expensive and relevant.
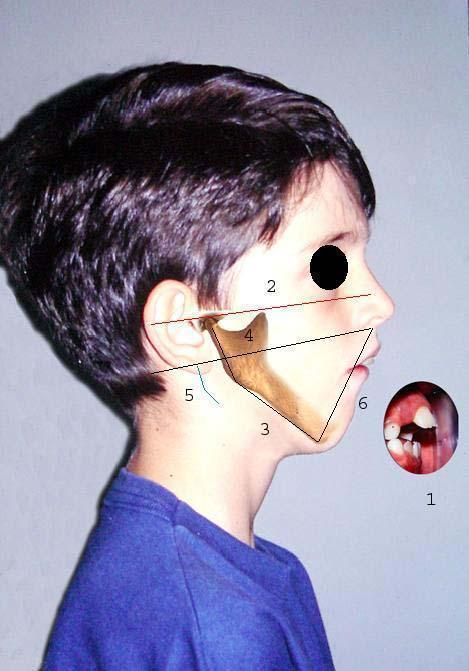
Characteristics of skeletal anterior open bite
1. Anterior open bite
2. Frankfurt plane
3. Mandibular plane
4. Maxillary plane
5. Gonial angle
6. Lower anterior facial height
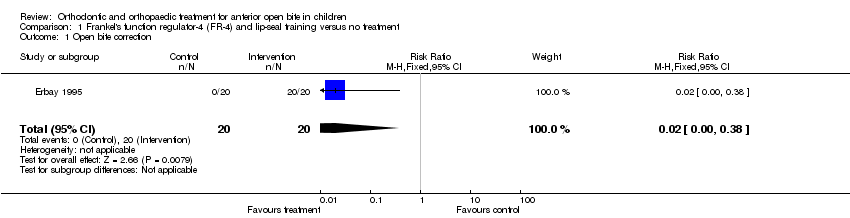
Comparison 1 Frankel's function regulator‐4 (FR‐4) and lip‐seal training versus no treatment, Outcome 1 Open bite correction.

Comparison 3 Removable appliances with palatal crib associated with high‐pull chincup versus no treatment, Outcome 1 Open bite correction.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Open bite correction Show forest plot | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.02 [0.00, 0.38] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Open bite correction Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.11, 0.48] |

