Acupuntura para la esquizofrenia
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with auditory hallucinations (CCMD‐3). History: average duration of illness (5.85 ± 4.80) months (acupoint catgut treatment + low dose risperidone group); (4.92 ± 3.69) years (risperidone group). Country: China. Inclusion criteria: had a CCMD‐3 diagnosis of schizophrenia; the duration of illness more than 3 months and auditory hallucinations continued longer than 1 month; never received any antipsychotics or washout period was longer than 1 week; age between 18 and 60 years. Exclusion criteria: elderly and frail; pregnant women; severe somatic diseases; cerebral organic diseases. | |
| Interventions | 1. Acupoint catgut treatment + low dose risperidone: acupoint catgut treatment (Tinggong; opened mouth; once 7‐10 days; 6 weeks as a treatment course) + low dose risperidone (1 to 2 mg/d; average dose (1.38 ± 0.52) mg/d). N = 88. 2. Risperidone: initial dose 1 mg, adjusted the dose according to treatment courses and side effects and achieved to 4 to 10 mg/d within 2 weeks; average dose (5.95 ± 1.76) mg/d. N = 92. Combination therapy: could add artane, propranolol and benzodiazepine drugs and could not received any other antipsychotics. | |
| Outcomes | Global state: no clinically important change in global state1. Mental state2: PANSS; SAPS. Behaviour: leaving the study early. Adverse effects: TESS; skin infection. Unable to use: Adverse effects: lab test (kidney function; blood sodium; blood chloride; blood glucose; stool routine test) (reported no impact in both groups but no data). Lab test: EEG (not clinical outcome). | |
| Notes | 1. Assessment criteria (according to traditional criteria): recovery; marked improvement; improvement; no effect. 2. The ratings were assessed before treatment and, 1 week after treatment, 2 weeks after treatment, 4 weeks after treatment and 6 weeks after treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report stated ‐ "using random sampling". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Not used sham acupoint catgut treatment. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Unclear risk | This study was supported by the Health Department of Shanxi Province. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with auditory hallucinations (CCMD‐2‐R). Age: between 15 and 60 years (mean age (36.4 ± 2.1) years) (acupoint catgut treatment + antipsychotics group); between 20 and 58 years (mean age (35.7 ± 1.2) years) (antipsychotics group). History: duration of illness between 1 and 8 years (average duration 2.3 years) (acupoint catgut treatment + antipsychotics group); between 0.6 and 9.0 years (average duration 2.1 years) (antipsychotics group). Country: China. Inclusion criteria: had a CCMD‐2‐R diagnosis of schizophrenia; auditory hallucinations still existed after 8‐weeks treatment with equivalent chlorpromazine dose 400 to 600 mg/d. | |
| Interventions | 1. Acupoint catgut treatment + antipsychotics: acupoint catgut treatment (Tinggong [double]; opened mouth; 10 days as a treatment course; total 3 treatment courses) + antipsychotics (no further details). N = 108. 2. Antipsychotics: no further details. N = 108. | |
| Outcomes | Mental state: no clinically important change in specific symptoms (auditory hallucinations)1. Behaviour: leaving the study early. Unable to use: Adverse effects: local pain when eating (existed in acupoint catgut treatment + antipsychotics group but no data). | |
| Notes | 1. Assessment criteria: marked improvement (auditory hallucinations disappeared within 10 days); improvement (auditory hallucinations disappeared within 20 days); no effect (auditory hallucinations still existed after 30 days). 2. The equivalent chlorpromazine dose of two compared groups was no difference. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into treatment group and control group according to admission order". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not used; sham acupoint catgut treatment. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. Follow‐up: 2 years. | |
| Participants | Diagnosis: schizophrenia (CCMD‐2‐R). History1: duration of illness between 3 and 240 months (average duration (54.72 ± 58.75) months) (acupoint injection + chlorpromazine group); between 3 and 304 months (average duration (65.81 ± 67.98) months) (chlorpromazine group). Sex: women and men. Country: China. Inclusion criteria: had a CCMD‐2‐R diagnosis of schizophrenia; BPRS > 36. Exclusion criteria: severe somatic and haemorrhagic diseases; acupuncture syncope and had aggressive behaviour. Follow‐up: participants with effective treatment. N = 144/170. History: duration of illness between 3 and 232 months (average duration (55.87 ± 59.76) months (acupoint injection + chlorpromazine group); between 3 and 301 months (average duration (53.02 ± 58.32) months) (chlorpromazine group). | |
| Interventions | 1. Acupoint injection + low dose chlorpromazine: acupoint injection* (Salviae Miltiorrhizae; acupoints choice according to the type of TCM**) + low dose chlorpromazine (Wintermin; less than 300 mg/d; average dose (253.92 ± 42.25) mg/d1). N = 105. 2. Chlorpromazine: Wintermin; over 400 mg/d; average dose was (465.29 ± 72.92) mg/d1. N = 65. Combination therapy: dose could be adjusted within the provision range or added anticholinergic drugs when adverse reactions took place; could add benzodiazepine drugs when needed. Follow‐up: 1. Acupoint injection + chlorpromazine: Wintermin; maintained the same antipsychotics; average dose (149 ± 55) mg/d. N = 92/105. 2. Chlorpromazine: Wintermin; maintained the same antipsychotics; average dose (160 ± 58) mg/d. N = 52/65. Combination therapy: the same as treatment period. * Acupoint injection: two side acupoints in turn; once a day; 10 days as a treatment course; 7‐day interval between two courses. ** Acupoints choice according to type of TCM: Type of phlegm‐fire attacking upwards: Shangqiu, Fenglong, Yangjiao, Ququan, Baihui. Type of internal retention of phlegm and dampness; Sanjingjiao, Shangqiu, Fenglong, Yanglingquan, Baihui. Type of Qi stagnation and Blood stasis: Ligou, Benshen, Yangjiao, Ququan, Baihui. Type of Yin deficiency and fire excess: Shaohai, Zhizheng, Zhubing, Feiyang, Baihui. Type of Yang deficiency: Sanyingjiao, Zusanli, Dazhong, Feiyang, Baihui. | |
| Outcomes | Mental state: BPRS2,3. Behaviour: leaving the study early. Adverse effects: TESS4. Follow‐up: Global state: relapse. Mental state:BPRS5 (BPRS score was assessed continuously during follow‐up). | |
| Notes | 1. Data reported from only 160 participants. 2. The rating was assessed before treatment and after each treatment course. 3. Another assessment standard (according to reduced rate): recovery (≥ 75%); marked improvement (≥ 50%); improvement (≥ 25%); no effect (< 25%). 4. The rating was assessed after each treatment course. 5. The rating was assessed before follow‐up, one year and two years; we used data of two years. 6. Contact made with author as there was little difference between two references. Author Yufeng Pan had retired and author Yuying Pan clarified that the two references referred to the same study. For those outcomes containing different data from the two papers we did not extract the data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into the two groups". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham acupoint injection not used. |
| Blinding of outcome assessment (detection bias) | Low risk | Report stated ‐ "the assessors were blind to the drug allocation". |
| Incomplete outcome data (attrition bias) | High risk | Ten participants left the study early during the study and the follow‐up period. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | High risk | There were inconsistencies in the data between the 2 reports of the same study. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with auditory hallucinations (CCMD‐2‐R). Age: between 18 and 59 years (mean age (39.54 ± 10.93) years) (acupoint injection + antipsychotics group); between 18 and 58 years (mean age (38.27 ± 9.78) years) (antipsychotics group). History: duration of illness (12.70 ± 8.31) years (acupoint injection + antipsychotics group); (11.5 ± 8.31) years (antipsychotics group). Country: China. Inclusion criteria: had a CCMD‐2‐R diagnosis of schizophrenia; existed all kinds of auditory hallucinations and the scores of the twelfth item of BPRS ≥ 3; auditory hallucinations did not disappear after 2 months systemic treatment with one antipsychotics. Exclusion criteria: organic diseases and other hallucinations. | |
| Interventions | 1. Acupoint injection + antipsychotics: acupoint injection (clonazepam 1.0 mg; Tinggong [double], opened mouth, once two days, 7 times) + antipsychotics (remained previous antipsychotics treatment; equivalent chlorpromazine dose (685 ± 240) mg/d). N = 45. 2. Antipsychotics: remained previous antipsychotics treatment; equivalent chlorpromazine dose (633 ± 247) mg/d. N = 45. | |
| Outcomes | Mental state: BPRS (the scores of the twelfth item). Behaviour: leaving the study early. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report stated ‐ "randomly divided into experimental group and control group using draw lots method". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham acupoint injection not used. |
| Blinding of outcome assessment (detection bias) | Low risk | Report stated ‐ " two doctors with extensive clinical experience and not attending the trial assessed outcomes before treatment and 2 weeks after treatment". |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | High risk | One author worked for drug industry. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with auditory hallucinations (CCMD‐2). Age: mean age 30.7 years (acupoint injection + antipsychotics group); 28.8 years (antipsychotics group). History: average duration of illness 5.2 years (acupoint injection + antipsychotics group) and 5.8 years (antipsychotics group). Country: China. Inclusion criteria: had CCMD‐2‐R diagnosis of schizophrenia; > 2 hospitalisations; systemic treatments of multiple antipsychotics but persistent auditory hallucinations; after other treatments (acupuncture and Chinese herbs) persistent auditory hallucinations or reappeared; current auditory hallucinations > 8 weeks; BPRS < 30. | |
| Interventions | 1. Acupoint injection + antipsychotics: acupoint injection (sulpiride 50 mg; Tinggong [double], once a day, 5 times as a treatment course, 2 intermittent treatment courses each month, total half a year) + antipsychotics (remained antipsychotics treatment; equivalent chlorpromazine dose (668.4 ± 221.6) mg/d). N = 34. 2. Antipsychotics: remained antipsychotics treatment (except some cases reduced dose or added artane for extrapyramidal reaction); equivalent chlorpromazine dose (651 ± 20.84) mg/d. N = 30. | |
| Outcomes | Mental state: BPRS1; no clinically important change in specific symptoms (auditory hallucinations)2. Behaviour: leaving the study early. | |
| Notes | 1. The rating was assessed 1 week before treatment and, 3 months and half a year after treatment. 2. Criteria: recovery (auditory hallucinations disappeared completely; did not reappear about half a year); improvement (times of auditory hallucinations reduced; had insight of auditory hallucinations; did not effect daily life; or auditory hallucinations appeared occasionally after disappeared); no effect (auditory hallucination still existed or appeared frequently after disappeared). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into two groups". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham acupoint injection not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia. Age: between 19 and 37 years (electric acupuncture convulsive therapy group) and between 17 and 48 years (electroconvulsive therapy group); most of them were middle‐aged patients. Country: China. | |
| Interventions | 1. Electric acupuncture convulsive therapy: Renzhong and Baihui; average electricity consumption 1.27 Joule/331 times; once every two days; 12 times as a treatment course. N = 34. 2. Electric convulsive therapy: electrode position of two temporal; average electricity consumption 34.97 Joule/286 times; once every two days; 12 times as a treatment course. N = 34. | |
| Outcomes | Behaviour: leaving the study early. Adverse effects: back pain; spinal fracture1. Unable to use: Physical exam: tendon reflexes; patellar clonus (not clinical outcomes). | |
| Notes | 1. Twelve patients suffered a spinal fracture during the treatment period and their data could not be used. 2. Authors compared three groups (electric acupuncture convulsive therapy group, electroconvulsive therapy group and grand mal epilepsy group) but only patients with schizophrenia randomly divided into electric acupuncture convulsive therapy group and electroconvulsive therapy group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into two groups". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Author compared two groups and used electrodes with different positions. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: post‐schizophrenic depression1 (CCMD‐3). N = 67. History: average duration of illness (5.6 ± 2.9) years (electroacupuncture + antipsychotics group) and (4.9 ± 3.8) years (antipsychotics group). Setting: both inpatients and outpatients. Country: China. | |
| Interventions | 1. Electroacupuncture + antipsychotics: electroacupuncture* (Baihui and Yingtang) + antipsychotics (remained previous medication). N = 33. 2. Antipsychotics: remained previous medication. N = 34. * Electroacupuncture: continuous wave; 2‐4 Hz, 50 minutes, once a day. | |
| Outcomes | Mental state: HAMD3,4. Behaviour: leaving the study early. Adverse effects: TESS3. | |
| Notes | 1. Diagnosis of post‐schizophrenia depression: diagnosed with schizophrenia in the last 1 year; symptoms of depression appeared when the condition improved but not cured; the depression continued at least two weeks; HAMD > 20. 2. Although the author reported that there was no significant age difference between the two groups the table appears to contain a typographical error in the antipsychotics' group. 3. The rating was assessed before treatment and at 2 weeks, 4 weeks and 6 weeks after treatment. 4. Another assessment standard (according to reduced rate): recovery (≥ 75%); marked improvement (≥ 50%); improvement (≥ 50%); no effect (< 25%, reduced rate = [total scores before treatment‐total scores after treatment]/total scores before treatment*100%). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with negative symptoms (type II schizophrenia) (CCMD‐3; Andreasen's diagnosis standard of type II schizophrenia) . N = 62. History: duration of illness between 3 and 24 years1 (electroacupuncture + aripiprazole group); between 2 and 19 years (aripiprazole group). Setting: hospitalised patients. Country: China. Inclusion criteria: had a CCMD‐3 and a type II diagnosis of schizophrenia; with mainly negative symptoms and PANSS > 60, the scores of negative factors > 30; age between 16 and 60 years and duration of illness more than 1 year; liver and kidney function test, lipids test, blood glucose test, ECG, blood routine test, urine routine test, and stool routine test normal; patients or family members gave their consent. Exclusion criteria: combined with other diseases; had serious physical illnesses or brain organic diseases or epilepsy and alcohol or drug abuse; pregnant or lactating women; with similar drug allergic history and unable to adapt electroacupuncture history. | |
| Interventions | 1. Electroacupuncture + aripiprazole: electroacupuncture* (Baihui and Neiguan [double] group or Shuigou and Sanyingjiao [double] group) + aripiprazole (Bosiqing; initial dosage 5 mg/d; gradually added to the therapeutic dosage 10 to 30 mg/d within two weeks; average dosage (18.4 ± 6.2) mg/d). N = 32. 2. Aripiprazole: Bosiqing; initial dosage 5 mg/d; gradually added to the therapeutic dosage 10 to 30 mg/d within two weeks; average dosage (20.1 ± 4.3) mg/d. N = 30. Washout period: those treated with other antipsychotics or mood stablisers needed 2‐weeks' washout period. Combination therapy: could not receive any other antipsychotics during the observation period; symptomatic treatment drugs could be used according to patient's condition when with adverse drug reactions and could receive benzodiazepines when with poor sleep. * Electroacupuncture: used two acupoints groups in turn; once for 45 minutes; once a day; five days a week (except Saturday and Sunday); 12 weeks as a treatment course. | |
| Outcomes | Mental state: PANSS2,3. Behaviour: leaving the study early. Adverse effects: TESS2 (mainly reported insomnia; myotonia; tremor; akathisia; blurred vision; sweating; headache; tachycardia). Unable to use: Adverse effects: lab test (kidney function test, lipids test, blood glucose test, stool routine test) (reported no obvious abnormal before or after treatment in both groups and no data). | |
| Notes | 1. Two patients in the electroacupuncture + aripiprazole group left the study early and author reported the age, sex and duration of illness of this group excluding those two patients. 2. The ratings were assessed before treatment and at 2 weeks, 4 weeks, 8 weeks and 12 weeks after treatment. 3. Another assessment standard (according to reduced rate): recovery (≥ 75%); marked improvement (51% to 75%); improvement (25% to 50%); no effect (< 25%, reduced rate = [scores before treatment‐scores after treatment]/scores before treatment*100%). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report stated ‐ "random systematic sampling according to admission order". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | Two participants (electroacupuncture + aripiprazole group) left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. Duration: 4‐week baseline evaluation and risperidone run‐in phase + 6 weeks treatment period. | |
| Participants | Diagnosis: schizophrenia with auditory hallucinations (DSM IV) . N = 60. History: average duration of auditory hallucinations (10.13 ± 2.89) years (electroacupuncture + risperidone group) and (9.03 ± 2.94) years (sham electroacupuncture + risperidone group). Setting: hospitalised patients. Country: China. Inclusion criteria: were 18‐60 years of age; had a DSM IV diagnosis of schizophrenia using Structured Clinical Interview for DSM IV; had previously been treated with risperidone following documented treatment failure after two antipsychotics were administered for an adequate duration with sufficient dose; demonstrated a documented failure to show a satisfactory clinical response to an adequate trial of risperidone (three or more months of at least 4 mg/day of oral risperidone); had persistent and distressing auditory hallucinations, evidenced by a score of 11 or more on the total of PSYRATS‐AH; gave informed consent. Exclusion criteria: mental retardation; seizure disorder; substance abuse/dependence; pregnant; severe and unstable physical illnesses; danger of attack or extreme agitation; or previously received acupuncture (to maximise blinding). | |
| Interventions | 1. Electroacupuncture + risperidone: electroacupuncture* (Tinggong, Tinghui, Yifeng, Daling, Neiguan and Sanyijiao) + risperidone (before initiation of the baseline observation period all patients had been on a stable dose of risperidone for at least 4 weeks and baseline doses of risperidone remained stable throughout the study; the average initial risperidone dosage (5.15 ± 0.46) mg/d). N = 30. 2. Sham electroacupuncture + risperidone: sham electroacupuncture (20 mm away from each corresponding acupoint) + risperidone (before initiation of the baseline observation period all patients had been on a stable dose of risperidone for at least 4 weeks and baseline doses of risperidone remained stable throughout the study; the average initial risperidone dosage (5.22 ± 0.47) mg/d). N = 30. Combination therapy: lorazepam (< 4 mg) was allowed to counteract sleep problems; antidepressants, mood stabilisers and antipsychotic drugs other than risperidone were not allowed during the study. * Electroacupuncture: needled bilaterally; depth 15to 30 mm; once the 'De‐Qi' sensation was elicited, the handles of the needles inserted into Tinggong, Tinghui and Yifeng were connected to an electrical input via an electroacupuncture machine (sparse dense wave; frequency 2 to 10 Hz; intensity 2 to 3 mA); for 20 minutes; 5 times a week; total 30 times (6 weeks). ** Sham electroacupuncture: depth less than 5 mm; the handles of the needles inserted into points near Tinggong, Tinghui and Yifeng were connected to the electroacupuncture machine with no electrical current; for 20 minutes; 5 times a week; total 30 times (6 weeks) (simulated a real electroacupuncture procedure and the acupuncturist did not manipulate the needles and no 'De‐Qi' sensation was elicited). | |
| Outcomes | Mental state: PSYRATS‐AH1,2; PANSS1. Behaviour: leaving the study early. | |
| Notes | 1.The ratings were assessed at baseline, 2 weeks, 4 weeks and 6 weeks. 2. Another assessment standard: (according to reduction scores from baseline): a treatment response (≥ 20%). 3. This study is a part of Bai's study (see the reference) and they only reported this study (obtained the information from author Jing Chen). 4. Author analysed data using intention‐to‐treat method. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report stated ‐ "randomly assigned to either the real electroacupuncture group or the sham electroacupuncture group by the SAS program". |
| Allocation concealment (selection bias) | Low risk | Report stated ‐ "maintained using opaque sealed envelopes". |
| Blinding of participants and personnel (performance bias) | Low risk | Report stated ‐ "blinded to the treatment allocation"; the acupuncturist was "instructed not to communicate with the patients and the clinical investigators"; the participants were "acupuncture‐naive patients" and "there was also limited contact between the study participants and restricted conversation between acupuncturist and participants during treatment". |
| Blinding of outcome assessment (detection bias) | Low risk | Report stated ‐ "blinded to the treatment allocation" and the acupuncturist was "instructed not to communicate with the patients and the clinical investigators". |
| Incomplete outcome data (attrition bias) | Low risk | Though seven participants left the study early the author analysed data using intention‐to‐treat method. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Unclear risk | This study was supported by the Stanley Medical Research Institue (SMRI), Chevy Chase, Maryland. |
| Methods | Allocation: randomised. Duration: 6 weeks. | |
| Participants | Diagnosis: schizophrenia (CCMD‐2‐R) . N = 60. History: duration of illness between 5 and 10 years. Setting: hospitalised patients. Country: China. Inclusion criteria: had a CCMD‐2‐R diagnosis of schizophrenia; without severe heart, liver and kidney dysfunction or other severe somatic diseases; without chlorpromazine allergic history. | |
| Interventions | 1. Electroacupuncture + chlorpromazine: electroacupuncture* (acupoint choice according to different symptoms) + chlorpromazine (100 to 300 mg/d). N = 30. 2. Chlorpromazine: 400 to 500 mg/d. N = 30. Combination therapy: not combined with any other antipsychotics; could received symptomatic treatment when with extrapyramidal reactions, tachycardia or elevated transaminase. * Electroacupuncture: with mainly positive symptoms used Xinshu, Ganshu, Pishu, Shenmen, Fenglong; with mainly negative symptoms used Dazhui, Fengfu, Neiguan, Fenglong; with both positive and negative symptoms added or removed acupoints according to the symptoms; refusing to eat added Hegu and Zusanli; not speaking added Lianquan and Yamen; excitement and hyperactivity added Renzhong and Quchi; intensity according to patients feeling; frequency 20 to 40 times/second ; for 30 minutes; once two days; 20 times as a treatment course. | |
| Outcomes | Mental state: BPRS1,2. Behaviour: leaving the study early. Adverse effects: TESS3 (mainly reported extrapyramidal symptoms; tachycardia; dry mouth; blurred vision; sleepiness). Others4: adding medication. | |
| Notes | 1.The rating was assessed before treatment and, 2 weeks, 4 weeks and 6 weeks after treatment. 2. Another assessment standard (according to reduced rate): improvement (≥ 30%); marked improvement (≥ 50%); recovery (≥ 80%); no effect (< 30%). 3. The ratings were assessed at 2 weeks, 4 weeks and 6 weeks after treatment. 4. Author reported this outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report state ‐ "randomly divided into two groups according to age and gender matching". Contacted the author who said she used coin‐tossing method . |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. Duration: 2 months. | |
| Participants | Diagnosis: chronic schizophrenia (CCMD‐3). N = 50. History: duration of illness between 19 and 39 years (average duration (32.25 ± 6.31) years); duration of continued hospitalisation between 11 and 22 years (average duration (18.17 ± 7.35) years); received antipsychotics more than 10 years. Setting: hospitalised patients. Country: China. | |
| Interventions | 1. Electroacupuncture + antipsychotics: electroacupuncture* (Tanzhong, Zhongwan, Shenmen, Fenglong [double], Taichong [double], Neiguan [double]) + antipsychotics (remained previous medication). N = 25. 2. Antipsychotics: remained previous medication. N = 25. * Electroacupuncture: reinforcing‐reducing method for deficiency syndrome and reducing method for excess syndrome; connected needles to the electroacupuncture machine once the sensation was elicited; pulse current; 5 minutes; once two days. | |
| Outcomes | Mental state: BPRS; PANSS. Behaviour: leaving the study early. | |
| Notes | 1. Contact made with the author, Fenggang Li, and no participants left the study early. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into treatment group and control group". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Not used sham electroacupuncture and doctors often told patients (electroacupuncture + antipsychotics group) the importance and treatment mechanism of acupuncture. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Unclear risk | Participants were men and unsure if gender selection bias occurred and the study lasted longer than 20 years. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with negative symptoms (type II schizophrenia) (CCMD‐3; Andreasen's diagnosis standard of type II schizophrenia). Age: mean age (41.7 ± 10.6) years (electroacupuncture + risperidone group); (39.3 ± 9.2) years (risperidone group). History: duration of illness (11.7 ± 6.5) years (electroacupuncture + risperidone group) and (13.2 ± 7.4) years (risperidone group); average number of hospitalisations (4.2 ± 2.5) times (electroacupuncture + risperidone group) and (3.9 ± 2.2) times (risperidone group) . Country: China. Inclusion criteria: had a CCMD‐3 diagnosis of schizophrenia; had an Andreasen's diagnosis of type II schizophrenia; PANSS > 60; the scores of negative factors > 30; women and men; age between 18 and 55 years; patients receiving any other antipsychotics, mood stabilisers or antidepressants needed 2 weeks washout period and total scores of PANSS decreased < 20. Exclusion criteria: had cerebral organic diseases or severe physical illnesses; combined with other psychotic diseases; with similar drugs allergic history; drug or alcohol dependence or abuse; pregnant or lactating women. | |
| Interventions | 1. Electroacupuncture + risperidone: electroacupuncture* (Baihui, Shangxing, Yingtang, Sanyingjiao [double], Neiguan [double]) + risperidone (Weisitong; initial dose 1 mg/d and added to therapeutic dose 3 to 6 mg/d in 10 days according to patient's conditions and adverse reactions; average dose (4.9 ± 1.4) mg/d). N = 40. 2. Risperidone: Weisitong; initial dose 1 mg/d and added to therapeutic dose 3 to 6 mg/d in 10 days according to patient's conditions and adverse reactions; average dose (5.3 ± 1.2) mg/d. N = 35. Combination therapy: could add artane, propranolol when extrapyramidal reactions appeared; could add benzodiazepine drugs to treat patients with pool sleep. * Electroacupuncture: frequency 20 to 40 times/minute; intermittent wave; for 45 minutes; 5 times a week; 20 times as a treatment course; added Zhongwan and Zusanli when with gastrointestinal uncomfortable symptoms and added Fenglong when with symptoms of the type of stagnation of phlegm and Qi. | |
| Outcomes | Mental state: PANSS1,2. Behaviour: leaving the study early. Adverse effects: TESS1 (main: extrapyramidal symptoms; dry mouth; insomnia; blurred vision; dizziness; constipation; weight gain; nausea and vomiting); lab test (blood routine test; urine routine test; liver function and kidney function; and ECG). Others3: adding medication. | |
| Notes | 1. The ratings were assessed at the end of 0 week, 4 weeks and 8 weeks. 2. Another assessment standard (according to reduced rate): recovery (≥ 75%); marked improvement (51% to 75%); improvement (25% to 50%); no effect (< 25%). 3. Author reported this outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into experimental group and control group". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: refractory schizophrenia (CCMD‐3, the defined standard of refractory schizophrenia1). Age: mean age (29.4 ± 11.3) years (electroacupuncture + low dose clozapine group); (28.1 ± 12.2) years (clozapine group). History: average duration of illness (35.2 ± 12.2) months (electroacupuncture + low dose clozapine group); (36.3 ± 13.2) months (clozapine group). Country: China. Inclusion criteria: had a CCMD‐3 diagnosis of schizophrenia; had a diagnosis of refractory schizophrenia; age between 14 and 60 years; women and men; patients already receiving antipsychotics needed 7 days' washout period; gave informed consent. Exclusion criteria: had severe heart, liver and kidney primary diseases. | |
| Interventions | 1. Electroacupunture + low dose clozapine: electroacupuncture* (Baihui and Taiyang [double]) + low dose clozapine (initial dose 50 mg/d; added to 100 to 150 mg/d within 1 week). N = 40. 2.Clozapine: initial dose 50 to 100 mg/d, added to 200 to 500 mg/d within 1 week. N = 40. * Electroacupuncture: 10 voltage; continuous wave; frequency 60Hz; current intensity was limited when neck and facial muscles cramped and breath‐hold and hypoxia appeared; firstly continued to stimulate strongly 3 to 4 seconds then reduced the strength and frequency quickly, after patient's breath and face returned to normal and continued 30 to 60 seconds stimulated again; continued to stimulate 8 to 10 times; 3 times a week, total 8 weeks. | |
| Outcomes | Mental state: PANSS2,3. Behaviour: leaving the study early. Adverse effects: TESS4. | |
| Notes | 1. The defined standard of refractory schizophrenia: no effect after receiving at least 2 or more different antipsychotic chemical drugs with enough doses and enough treatment courses; no effect after receiving electric shock 7 to 12 times enough treatment courses' treatments; PANSS ≥ 60. 2. The rating was assessed before treatment and, 2 weeks, 4 weeks and 8 weeks after treatment. 3. Another assessment standard (according to reduced rate): recovery (≥80%); marked improvement (≥ 50%, < 80%); improvement (≥ 30%, < 50%); no effect (< 30%, reduced rate = [scores before treatment‐scores after treatment]/scores before treatment*100%). 4. The rating was assessed 8 weeks after treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomised into" two groups. No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Low risk | Report stated ‐ "two doctors who were blind the drug allocation assessed outcomes". |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. Duration: 8 weeks. Follow‐up: 6 months (effective case). | |
| Participants | Diagnosis: schizophrenia (CCMD‐3) . N = 90. History: duration of this episodes between 1 and 16 months (average duration (8 ± 5) years) (electroacupuncture + clozapine group), between 1.5 and 15 months (average duration (9 ± 3) months) (clozapine group). Type: paranoid type 31cases, undifferentiated type 9 cases, hebephrenic type 5 cases and 8 cases with positive family history (electroacupuncture + clozapine group); paranoid type 29 cases, undifferentiated type 12 cases, hebephrenic 4 cases and 10 cases with positive family history (clozapine group). Setting: hospitalised patients. Country: China. Inclusion criteria: had a CCMD‐3 diagnosis of schizophrenia; not received any antipsychotics within the last two weeks. Exclusion criteria: severe heart, brain, blood vessels and other physical illnesses; drug or alcohol dependence; pregnant or lactating women. | |
| Interventions | 1. Electroacupuncture + clozapine: electroacupuncture* (Baihui, Fenglong, Houxi, Ganshu) + clozapine (total dose 200‐300 mg/d; twice a day). N = 45. 2. Clozapine: total dose 200 to 300 mg/d; twice a day. N = 45. * Electroacupuncture: sparse dense wave; for 30 minutes; once a day; 20 to 30 times as a treatment course; total 2 treatment courses. | |
| Outcomes | Mental state: PANSS1.2. Behaviour: leaving the study early. Adverse effects: TESS1,3. Follow‐up: Mental state: PANSS2,4. | |
| Notes | 1. The ratings were assessed before treatment and, 2 weeks, 4 weeks, 6 weeks and 8 weeks after treatment. 2. Another assessment standard (according to reduced rate): recovery (> 95%); marked improvement (60% to 94%); improvement (30‐59%); no effect (< 30%). 3. Lab test included in TESS was tested before treatment and after treatment. 4. Effective cases included recovery cases, marked improvement cases and improvement cases. Effective cases were assessed 6 weeks of follow‐up period (converted to dichotomous data). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Reported state ‐ " randomly divided into two group using draw lots method". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | No participants left the study early but only followed up effective cases and six participants left the study early at follow‐up period. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia. First stage: History: mostly first admissions. Country: China. Inclusion criteria: as for readmitted patients only those who experienced marked improvement or cure at the end of the previous course of treatment were included. Second stage: N = 99. History: duration of illness within 2 years 66 cases and over 2 years 33 cases; first admissions 32 cases, second admissions 21 cases and more than 3 hospitalisation times 9 cases. Country: China. Inclusion criteria: as for readmitted patients only those who experienced marked improvement or cure at the end of the previous course of treatment were included. Ecliusion criteria: those whose illness had lasted over two years were included; others were the same as the first stage. | |
| Interventions | First stage: 1. Electroacupuncture + Dang Gui Cheng Qi Tang: electroacupuncture* (Yifeng, Tinggong, Tounjie, Chengling, Linqi, Baihui, Dingshen) + Dang Gui Cheng Qi Tang**. N = 49. 2. Decoction of herbs: Dang Gui Cheng Qi Tang**. N = 45. 3. Electrocupuncture*: Yifeng, Tinggong, Tounjie, Chengling, Linqi, Baihui, Dingshen. N = 43. 4. Chlorpromazine (Thorazine): any dose when necessary; 300‐600 mg/day; not combined with other antipsychotics. N = 45. Second stage: 1. Electroacupuncture + Dang Gui Cheng Qi Tang: electroacupuncture* (Yifeng, Tinggong, Chengling and Tounie) + Dang Gui Cheng Qi Tang**. N = 26. 2. Electroacupuncture + Dang Gui Cheng Qi Tang (with additives): electroacupuncture* (Yifeng, Tinggong, Chengling and Tounie) + Dang Gui Cheng Qi Tang** (with additives***). N = 25. 3. Electroacupuncture*: Tounie, Chengling and Linqi. N = 23. 4. Electroacupuncture*: Yifeng, Tinggong, Chengling and Tounie. N = 25. * Electroacupuncture: successive waves of 120cycles (Hz)/sec and 500 μsec pulse width; the intensity of stimulation varied with the individual and could be generalised into three grades (strong stimulation, moderate stimulation and mild stimulation); twice a day; adjustment of treatment depended upon the condition of the patient. ** Dang Gui Cheng Qi Tang: Radix Angelicae Sinensis 30 g, Radix et Rhizoma Rhei 30 g, Natrii Sulfas 15 g, Poncirus Trifoliata (L) Raf 12 g and Fruetus Trichosanthis 150 mL; all herbs except the Natrii Sulfas were decocted into a 100 mL solution, then the Natrii Sulfas was added and dissolved in it; usually 50 mL two times a day but the dose maybe increased to 150 to 200 mL daily when necessary. *** Additional herbs of Dang Gui Cheng Qi Tang (with additives): Swmen Persicae, Radix Curcumae, Radix Paeoniae Rubrae, Radix Bupleuri, Radix Scutellariae, Flos Carthami, Rhizoma Ligustici Chuanxiong, Radix Srephaniae tetrandrae, Radix Ledebouriellae, Poria, Radix Polygalae, Fructus Ziziphi Jujubae, Radix Rehmanniae, Rhizoma Acori Graminei, Os Draconis, Concha Osreeae, Haematitum, Herba Leonuri, Parata, Cortex Cinnamoni, Rhizoma Coptidis; according to the different condition of patient. Combination therapy: 10% chloral hydrate 10 to 20 mL orally, hyminal 0.1 to 0.2 g orally, phenobarbital 0.03 to 0.1 g or paraldehyde 4 to 5 mL orally or intramuscularly for patient who could not fall asleep at night and could not to be used for a long time. | |
| Outcomes | Global state: no clinically important change in global state1. Behaviour: leaving the study early. Unable to use; Adverse effects: reported electroacupuncture relative adverse effects (holding breath, facial cyanosis, arrhythmia, transient increase of blood pressure, injury of teeth, tongue and lips, epileptic attacks with strong stimulation) and TCM relative adverse effects (diarrhoea) existed but no data. | |
| Notes | 1. Assessment criteria: recovery (disappearance of all symptoms); marked improvement (50% relief of symptoms with moderate insight); mild improvement (25% relief of symptoms with no insight); no effect (no change in symptoms). 2. Only included the first stage of the study and could not include the second stage of the study because of interventions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "divided into groups randomly". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture or any other dummy treatments not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: refractory schizophrenia (CCMD‐2‐R). Age: both references reported mean age. History: both references reported average duration of illness. Country: China. Inclusion criteria: had a CCMD‐2‐R diagnosis of schizophrenia; after at least 2 times hospitalisations and systemic treatments of multiple antipsychotics most of the psychiatric symptoms disappeared but auditory hallucinations appeared repeatedly; after other treatments (acupuncture and Chinese herbs) auditory hallucinations still existed or reappeared after disappeared; auditory hallucinations this time continued more than 8 weeks; BPRS < 30. | |
| Interventions | 1. Electroacupuncture + antipsychotics: electroacupuncture* (CCEA; group one [Yingtang and Baihui] and group two [Shenting and Yamen]) + antipsychotics** (remained unchanged doses and kinds of medicines). 2. Antipsychotics**: remained unchanged doses and kinds of medicines. * Electroacupuncture: both groups were alternately used; sine‐wave; frequency 12, 10, 8, 6 Hz respectively for 10, 10, 10 and 15 minutes; frequency of fundamental waves 250 Hz and 750 Hz; maxim voltage 2 to 9 V; for 45 minutes; once a day; 8 weeks as a treatment course. ** From the date of two months before dividing into two groups to the end of the study the doses and kinds of medicines taken remained unchanged. | |
| Outcomes | Mental state2: SANS; SAPS. Unable to use: Global state: no clinically important change in global state3 (data could not to be used). Mental state: BPRS (data could not to be used). Behaviour: leaving the study early (data could not to be used). Adverse effects: TESS2(only reported no adverse effects in electroacupuncture + antipsychotics group and compared ECG no difference between two groups). Lab test: EEG; T3; T4; RUR; FT4I; TSH; rT3; TG; TM; LH; FSH; T (not clinical outcomes). | |
| Notes | 1. Two references with different participants' numbers but some data were the same and only extracted the same data with the same participants' number which could be used. No further detail. 2. The ratings were assessed before treatment, in 2nd, 4th, 6th and 8th week after treatment. 3. The effects were assessed after treatment with four degree which were worked out in Nanjing in 1958 (recovery, remarkable improvement, improvement and inefficacy). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "divided at random into two groups". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | Some of the graph showed data of 100 participants and some showed data of 69 participants. No further details. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | High risk | Some important data were the same but with different participants' number in two references. No further details. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with depressive symptoms (ICD‐10; CCMD‐2‐R). History: duration of illness between 7 months and 16 years (average (6.83 ± 4.77) years). Setting: hospitalised patients. Education level: higher than high school. Country: China. Inclusion criteria: had a CCMD‐2‐R and ICD‐10 diagnosis of schizophrenia; HAMD ≥ 20 and without severe tendency of suicide; without severe somatic diseases; without extreme excited, stupor, silent and any other uncooperative state; all the patients received simple antipsychotics and without receiving any antidepressants and anxiolytics. | |
| Interventions | 1. Electroacupuncture + antipsychotics: electroacupuncture (Intelligent electroacupuncture; Baihui and Yingtang; peak voltage 3‐10 VP; for 45 minutes; once a day; 5 days a week except Saturday and Sunday; 6 weeks as a treatment course) + antipsychotics (no further details). N = 22. 2. Antipsychotics: no further details. N = 20. | |
| Outcomes | Mental state: HAMD1, SDS. Behaviour: leaving the study early. | |
| Notes | 1. Another assessment standard (according to reduced rate): marked improvement (≥ 50%); improvement (≥ 25%); no effect (< 25%, reduced rate = [scores before treatment‐scores after treatment]/scores before treatment*100%). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report stated ‐ "randomly sampled". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (DSM III; CCMD). History: average duration of illness (8.2 ± 7.0) years. Country: China. Inclusion criteria: scores higher than 35 points on BPRS1. | |
| Interventions | 1. Electroacupuncture + low dose antipsychotics: electroacupuncture* (acupoints choice according to TCM types) + antipsychotics (a reduction of ˜60% of their previously daily levels). N = 25. 2. Antipsychotics: continued to receive their usual antipsychotics; equivalent chlorpromazine dose (560 ± 71.2) mg/day. N = 15. * Electroacupuncture: main acupoints (Yintang tou xinqu, Daling, Neiguan, Taiyang) and supplemental acupoints (Zusanli [Yang deficiency], Sanyinjiao [Yin deficiency], Fenglong [ Persistent Phlegm]);180 cycles/second; 500 ms pulse width; up to 60 mA; once a day except Sunday; 36 times as a treatment course (6 weeks). | |
| Outcomes | Global state: no clinically important change in global state1; CGI (CGI‐SI, CGI‐GI, EI). Behaviour: leaving the study early. Unable to use: Lab test: cAMP; cGMP; the neuropeptide beta‐endorphin (not clinical outcome). | |
| Notes | 1. Results were classified as: marked improvement (the majority of symptoms were eliminated and orientation was recovered); improvement (some of the symptoms were eliminated and orientation was partly recovered); no effect (symptoms and orientation showed no change). 2.This rating scale was written in Chinese and was assessed before treatment and at 2 weeks, 4 weeks and 6 weeks after treatment. 3. Another assessment criteria (according to reduced rate): marked improvement (≥ 80%); improvement (50%to 80%); slight improvement (20% to 50%); no effect (≤ 20%). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into two study groups". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Author compared two groups and did not use sham electroacupuncture. |
| Blinding of outcome assessment (detection bias) | Low risk | Report stated ‐ "The subjects were evaluated clinically before and after the study course by specialists in psychiatry who were blinded as to which group the subjects belonged". |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with auditory hallucinations. N = 60. History: average duration of illness 5.1 years (He‐Ne laser irradiation group (Ermen)); 6.2 years (chlorpromazine + sham laser irradiation group); 7.3 years (He‐Ne laser irradiation group (non‐acupoint)). Country: China. Inclusion criteria: had auditory hallucinations definitely schizophrenic in origin for more than one month. | |
| Interventions | 1. He‐Ne laser irradiation (Ermen): Ermen (double); irradiated with mouths partially open; the tube of the emitter held 30 cm away; power 4.7 hw; patch of red light 0.5 cm; wavelength 6328 Å; optimal current output 6 to 7.5 mA; for 15 minutes; once a day except Sunday; 30 times as a treatment course. N = 20. 2. Chlorpromazine + sham laser irradiation: chlorpromazine (average dosage 450 mg/d) + sham laser irradiation (the tube of the laser emitter pointed in the direction of the ear without real irradiation; once a day except Sunday; for 15 minutes; 30 times as a treatment course). N = 20. 3. He‐Ne laser irradiation (non‐acupoint): laser irradiation was thrown on the inner aspect of earlobe where no acupoint was located; once a day except Sunday; for 15 minutes; 30 times as a treatment course. N = 20. Combination therapy: not received any supplementary medication. | |
| Outcomes | Behaviour: leaving the study early. Adverse effects: numbness over the ear, upper extremity and chest on the treated side (only reported the data of the He‐Ne laser irradiation group (Ermen)). Unable to use: Mental state: rating scale of auditory hallucinations (for this particular trial). Adverse effects: sensation of heat at irradiated site and a feeling of plugged auditory canal (equivocal data). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly numbered and treated as three groups". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Author reported that three groups all used laser irradiation (two real and one sham) and one group combined with chlorpromazine but did not reported the other two groups used dummy drug. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with auditory hallucinations (CCMD‐2). N = 120. History: duration of illness ≥ 15 days (He‐Ne laser irradiation + chlorpromazine group); ≥ 10 days (chlorpromazine group). Setting: hospitalised patients. Country: China. Inclusion criteria: had a CCMD‐2 diagnosis of schizophrenia; BPRS ≥ 35. Exclusion criteria: brain organic diseases or brain organic diseases. | |
| Interventions | 1. He‐Ne laser irradiation + chlorpromazine: He‐Ne laser irradiation (Tinggong and Tinghui; wavelength 6328 Å; optimal current output 10 ± mA; negative ion generator 10‐4 A; output total laser power 14‐28 mµ; guided beam Φ3ⅹ300; focus divergent optical lens; for 30 minutes; once a day except Sunday) + chlorpromazine (dose 300 to 550 mg/d; average dose (395 ± 55) mg/d). N = 60. 2. Chlorpromazine: dose 300 to 600 mg/d; average dose (400 ± 85 mg/d). N = 60. Patients receiving antipsychotics before the study commenced needed a 2‐week washout period. Combination therapy: not combined with any other antipsychotics. | |
| Outcomes | Global state: no clinically important change in global state1. Mental state: BPRS (4 weeks); no clinically important change in specific symptoms (auditory hallucinations)2. Behaviour: leaving the study early (4 week). Service outcome: time to hospitalisation. Others3: Time to auditory hallucinations disappeared. | |
| Notes | 1. Assessment criteria: according to usual used 4 evaluation clinical criteria (recovery, marked improvement, improvement, no effect). 2. Assessment criteria: auditory hallucinations disappeared completely (disappeared completely); marked improvement (frequency of auditory hallucinations reduced obviously; clarity was significantly reduced; essentially no effect on patient's thinking or behaviour); improvement (frequency of auditory hallucinations reduced slightly; clarity was slightly reduced; partly effect on patient's thinking or behaviour); no effect (no change of auditory hallucinations). 3. Author reported this outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into two groups". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Sham laser irradiation not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (paranoid type) (DSM III; CCMD‐2‐R). History: duration of illness between 3 months and 22 years (average duration (6.2 ± 5) years). Country: China. Exclusion criteria: somatic diseases. | |
| Interventions | 1. Laser acupuncture*: group 1 (Dazhui and Shenting); group 2 (Taiyang [double]). N = 11. 2. Laser acupuncture + low dose chlorpromazine: laser acupuncture* (group 1 [Dazhui and Shenting] and group 2 [Taiyang [double]]) + chlorpromazine (150 to 300 mg/day). N = 10. 3. Sham laser acupuncture + chlorpromazine: sham laser acupuncture (needles fixed with tape on acupoints) + chlorpromazine (350 to 600 mg/day). N = 10. *Laser acupuncture: using the two acupoints groups every other day alternately; needles inserted acupoints; for 15 minutes; once a day (except Sunday); 5 weeks as a treatment course; optical fibre output power > 2 MW, output laser distributing angle < 20°; core diameter of optical fibre 300 micron. Combination therapy (laser acupuncture group and laser acupuncture + low dose chlorpromazine group): only could use diazepam or chloral hydrate when patient with insomnia. | |
| Outcomes | Global state: no clinically important change in global state1,2. Mental state: BPRS3. Behaviour: leaving the study early. Adverse effects: RESES3. Global state: CGI3 (no useful data). | |
| Notes | 1. The rating was assessed after treatment. 2. Assessment criteria (according to traditional criteria): recovery; marked improvement; improvement; no effect. 3. The ratings were assessed before treatment and each week after treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "divided into laser acupuncture group, laser acupuncture and low dose chlorpromazine group and sham laser acupuncture and high dose chlorpromazine group using random allocation method". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Though author compared 3 groups and used sham laser acupuncture did not use dummy medications. |
| Blinding of outcome assessment (detection bias) | Low risk | Report stated ‐ "two experience doctors assessed outcomes using blind evaluation method". |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia or schizoaffective disorder (DSM IV). N = 36. History1: duration of disorders between 1 year and 37 years (average duration (12.68 ± 9.39) years) and the number of previous hospitalisations ranged from 0 to 28 times (average number (6.19 ± 7.02) times). Country: Tunisia. Inclusion criteria: patient who met DSM IV diagnosis of schizophrenia and who gave their consent. | |
| Interventions | 1. Traditional acupuncture + antipsychotics: traditional acupuncture* (local points, distal points diagnosed by TCM) + antipsychotics (no further details). N = 151. 2. Sham acupuncture + antipsychotics: no further details. N = 161. * Traditional acupuncture: a simple manipulation; once for 20 minutes and 3 times a week; total 10 times. | |
| Outcomes | Mental state: PANSS; SAPS; SANS. Unable to use: Behaviour: leaving the study early (no useful data) (no further details). | |
| Notes | 1. These data were from 31 participants. 2. The author reported outcomes of 31 hospitalised patients and reported that four other participants left the study before completing the 10 sessions and another patient left study after the first session, thus there were a total of 36 participants and we did not know which group the five participants who left the study early came from. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "a clinical randomised trial". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Low risk | Reports stated ‐ "double‐blind". The author reported that both the patient and the psychiatrist did not know if it was a true traditional acupuncture treatment or a placebo (sham acupuncture). |
| Blinding of outcome assessment (detection bias) | Low risk | Report stated ‐ "outcome assessments were performed by the same treating psychiatrist and the psychiatrist did not know patient treated by a true traditional acupuncture treatment or sham acupuncture". |
| Incomplete outcome data (attrition bias) | High risk | Five participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with refractory auditory hallucinations (CCMD‐3). History: average duration of illness (4.27 ± 3.70) years (traditional acupuncture + risperidone group); (4.02 ± 3.91) years (risperidone group). Country: China. Inclusion criteria: had a CCMD‐3 diagnosis of schizophrenia and agreed to receive treatment; hospitalised and received systematic therapy with various antipsychotics, at least two, and the majority of psychiatric symptoms disappeared but the auditory hallucinations appeared repeatedly; had received other treatments (such as electric shock, acupuncture or Chinese herbs) but auditory hallucinations remained or reappeared; the duration of auditory hallucinations>8 weeks; BPRS < 30; expected length of hospitalisations > 3 months. | |
| Interventions | 1. Traditional acupuncture + risperidone: traditional acupuncture* (used main acupoints** and adjunct acupoints*** according to the TCM syndrome differentiation) + risperidone (Weisitong; initial dosage 1 mg [before breakfast]; gradually increased to the therapeutic dosage [2 to 6 mg/d] within 2 weeks; average dosage (2.3 ± 0.8) mg/d; daily total dosage less than 3 mg once a day before breakfast; otherwise twice a day before breakfast and dinner). N = 50. 2. Risperidone: Weisitong; initial dosage 1 mg (before breakfast); gradually increased to the therapeutic dosage (2 to 6 mg/d) within 2 weeks; daily total dosage less than 3 mg once a day before breakfast; otherwise twice a day before breakfast and dinner. N = 50. combination therapy: could not combine with any other antipsychotics, antidepressants, mood stabilisers or electric shock; could add artane, scopolamine injections and propranolol with temporary therapeutic dosage according to the condition to enhance patient's compliance and stopped to use when patient's somatic complaints alleviated. * Traditional acupuncture: manipulated needles every 10 minutes; for 30 minutes; 4 to 5 times a week and no less than 4 times; 1 month as 1 treatment course. ** Main acupoints: Shenmen (double); Daling (double); Taichong (double); Tinggong(double); Yifeng (double); Baihui. *** Adjunct acupoints: Type of stagnation of phlegm and Qi: Fenglong (double) and Tanzhong (double). Type of failure of the heart and kidney integrating: Taixi (double) and Laogong (double). Type of phlegm‐fire attacking upwards: Yongquan (double) and Houxi (double) Type of deficiency of both the heart and spleen: Zusanli (double) and Sanyinjiao (double). | |
| Outcomes | Global state: no clinically important change in global state1. Mental state2: BPRS; SAHS. Behaviour: leaving the study early. Adverse effects: TESS3. | |
| Notes | 1. Assessment criteria: recovery (auditory hallucinations disappeared completely; without any other psychiatric symptoms; insight recovered completely); marked improvement (the majority of auditory hallucinations disappeared; other psychiatric symptoms improved; insight partly recovered); improvement (the number of auditory hallucinations reduced; voice clarity was fuzzy; partly affected patient's daily life; insight was not complete); no effect (the number, duration and content of auditory hallucinations without marked change or became worse). 2. The ratings were assessed before treatment and at the end of 1, 2 and 3 treatment courses. 3. The rating was assessed at the end of 1, 2 and 3 treatment courses but lab test repeated twice (before and after third treatment). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report stated ‐ "randomly into two groups using the random number table according to the admission order". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | High risk | Four participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Unclear risk | This study was the Lanzhou's 2008 second batch technology program. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: type II syndrome of schizophrenia (CCMD‐3). History: duration of illness between 1.5 and 18 years (average duration (6.81 ± 5.42) years) (traditional acupuncture + risperidone group); between 1.5 and 20 years (average duration (7.73 ± 5.18) years) (risperidone group). Country: China. Inclusion criteria: had a CCMD‐3 diagnosis of schizophrenia; BPRS > 35; SANS ≥ 60; SAPS < 8. Exclusion criteria: severe somatic diseases; cerebral organic psychosis; ethyl alcohol and drug dependence. | |
| Interventions | 1. Traditional acupuncture + risperidone: traditional acupuncture* (two acupoints groups** in turn) + risperidone (initial dose 1 mg/d; added to 4 to 6 mg/d within 10 days; twice a day). N = 30. 2.Risperidone: initial dose 1 mg/d; added to 4 to 6 mg/d within 10 days; twice a day. N = 30. Combination therapy: supporting symptomatic treatment, psychological and occupational and recreational rehabilitation. * Traditinal acupuncture: for 30 minutes; once a day; 20 days as a treatment course and began another treatment course after 10 non‐treatment days. ** Acupoints group: Group A: Baihui (reinforcing method); Shenting Tou Shangxing (reinforcing method); Zusanli (left), Yanglingquan (left), Neiguan (left), Shenmen (left), Yongquan (left) (reinforcing‐reducing method). Group B: Sishencong (reinforcing method); Yingtang Tou face acupuncture heart area (reinforcing method); Zusanli (right), Yanglingquan (right), Neiguan (right), Shenmen (right), Yongquan (right) (reinforcing‐reducing method). | |
| Outcomes | Global state: no clinically important change in global state2. Mental state3: BPRS; SANS. Behaviour: leaving the study early. | |
| Notes | 1. Contact made with author Cheng Luo, however, still unclear about single‐blind method. 2. Assessment criteria (according to criteria of Neuropsychiatric Association of Chinese Medical Association): recovery; marked improvement; effect; no effect. 3. The ratings were assessed before treatment and at 1 month, 2 moths and 3 months after treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into two groups". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Report stated ‐ "using single‐blind method". No further details. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Report stated ‐ "using single‐blind method". No further details. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (type of stagnation of phlegm and Qi) (CCMD‐3, diagnosis of TCM). History: duration of illness between 1 month and 9 years (average duration (4.6 ± 3.42) years) (traditional acupuncture + risperidone group); between 2 months and 11 years (average duration (5.3 ± 3.6) years) (risperidone group). Country: China. Inclusion criteria: had a CCMD‐3 diagnosis of schizophrenia; PANSS ≥ 60; had a TCM diagnosis of type of stagnation of phlegm and Qi. Exclusion criteria: pregnant or lactating women; severe organic diseases; alcohol and drug dependence. | |
| Interventions | 1. Traditional acupuncture + risperidone: traditional acupuncture* (Juque, Tanzhong, Taichong, Jianshi, Fenglong, Daling, Yingtang) + risperidone (Silishu; initial dose 1 mg/d; added to 2 to 4 mg/d within 2 weeks). N = 30. 2.Risperidone: Silishu; initial dose 1 mg/d; added to 2 to 6 mg/d within 2 weeks. N = 30. * Traditional acupuncture: reducing by rotating needles; for 30 minutes; once a day; 5 days treatment with 2 days non‐treatment interval. | |
| Outcomes | Mental state: PANSS1,2. Behaviour: leaving the study early. Adverse effects: TESS1. Unable to use: Adverse effects: lab test (kidney function test ‐not reported. | |
| Notes | 1. The ratings were assessed before treatment and at 2 weeks, 4 weeks and 6 weeks after treatment. 2. Another assessment standard (according to reduced score): recovery (≥ 75%); marked improvement (50% to 74%); improvement (25% to 49%); no effect (< 25%). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into two groups". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | 1.We were unable to locate the protocol, unsure if selective reporting occurred. 2. Kidney function tests were completed but not reported and we are unsure of the reason for this omission. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia with auditory hallucinations (CCMD‐3). Country: China. Inclusion criteria: had a CCMD‐3 diagnosis of schizophrenia; duration of hospitalisation>6 months; received antipsychotics with good compliance but auditory hallucinations did not disappear. | |
| Interventions | 1. Traditional acupuncture + antipsychotics: traditional acupuncture* (acupoints choice according to the type of TCM**) + antipsychotics (remained previous antipsychotics treatment). N = 42. 2. Antipsychotics: remained previous antipsychotics treatment. N = 42. Combination therapy: could add artane, propranolol and benzodiazepine drugs and could not received any other antipsychotics. * Traditional acupuncture: acupoint near ear and on the head used transport point needling method and twisting and reducing method; acupoint on the limbs used quick‐slow supplementation and draining method and directional supplementation and draining method; manipulated needles every 10 minutes; for 30 minutes; 3 to 4 times a week and not less than 3 times; 3 weeks as a treatment course and 1‐week interval between two treatment courses; total 3 treatment courses. ** Acupoints choice according to type of TCM: Type of stagnation of phlegm and Qi: Taichong, Fenglong, Tinggong, Yifeng, Baihui, Daling, Tanzhong. Type of failure of the heart and kidney integrating: Tinggong, Taixi, Shenmen, Sanyingjiao, Baihui, Tongtian. Type of phlegm‐fire attacking upwards: Laogong, Yongquan, Daling, Taixi, Yifeng, Shenmen, Quchi. Type of deficiency of both the heart and spleen: Baihui, Pishu, Xinshu, Shenshu, Sanyingjiao, Zusanli. | |
| Outcomes | Global state: no clinically important change in global state1. Behaviour: leaving the study early. | |
| Notes | 1. Assessment criteria: marked improvement (auditory hallucinations disappeared; psychiatric symptoms cause by auditory hallucinations improved markedly); improvement (times of auditory hallucinations reduced or sound was fuzzy; other psychiatric symptoms improved); no effect (auditory hallucinations and psychiatric symptoms did not improve). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided into two groups". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: hebephrenic schizophrenia (CCMD‐2‐R). Age: mean age (15.87 ± 2.48) years (traditional acupuncture + low dose antipsychotics group); (16.11 ± 2.73 years (traditional acupuncture group); (15.74 ± 2.89) years (traditional antipsychotics group). History: average duration of illness (1.54 ± 1.29) years (traditional acupuncture + low dose antipsychotics group); (1.60 ± 1.21) years (traditional acupuncture group); (1.52 ± 1.17) years (traditional antipsychotics group). Country: China. Inclusion criteria: had a CCMD‐2‐R diagnosis of hebephrenic schizophrenia; BPRS ≥ 35. Exclusion criteria: had a CCMD‐2‐R diagnosis of hebephrenic schizophrenia but BPRS < 35; with different treatments caused by combining with other diseases; could not continue to receive treatment during the study period; changed to other treatments. | |
| Interventions | 1. Traditional acupuncture + low dose antipsychotics: traditional acupuncture* (Taichong [reducing method], Hegu [reducing method], Neiguan [straight inserted], Daling [straight inserted], Renzhong [reducing method], Dazhui [straight inserted] + acupoints choice according to type of TCM**) + low dose antipsychotics (≤equivalent chlorpromazine dose 0.2 g/d). N = 16. 2. Traditional acupuncture*:Taichong (reducing method), Hegu (reducing method), Neiguan (straight inserted), Daling (straight inserted), Renzhong (reducing method), Dazhui (straight inserted) + acupoints choice according to type of TCM**. N = 16. 3. Antipsychotics: enough dose antipsychotics (equivalent chlorpromazine dose 0.4 to 0.6 g/d). N = 16. Combination therapy: psychological counsel every day with parents according to patient's condition. * Traditional acupuncture: continued to manipulate needles 3 to 5 minutes every ten minutes; for 45 minutes; once a day; 15 times as a treatment course; 2 treatment courses. ** Acupoints choice according to type of TCM: Type of Qi stagnation and blood stasis: Yanglingquan, Sanyingjiao. Type of Internal retention of phlegm and dampness; Fenglong. Type of internal disturbance of pyrophlegm: Fenglong, Xingjian. Type of Yin deficiency and fire excess: Fuliu. Type of Yang deficiency: Shenshu (moxibustion), Pishu, Guanyuan (moxibustion). | |
| Outcomes | Global state: no clinically important change in global state1,2. Mental state3: BPRS, SAPS, SANS. Behaviour: leaving the study early. Adverse effects3: TESS. | |
| Notes | 1. Assessment criteria: recovery (psychiatric symptoms disappeared completely; insight recovered); effect (marked improvement [psychiatric symptoms disappeared completely or the majority main psychiatric symptoms disappeared; insight partly recovered or not recovered]; improvement [symptoms disappeared partly; insight did not recover); no effect (no symptoms improved obviously and insight did not recover). 2. The rating was assessed 30 days after treatment. 3. The ratings were assessed before treatment and each 15 days after treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report stated ‐ "randomly divided into 3 groups using random allocation table according to the admission date and case number". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (CCMD‐2‐R). Age: mean age (31.74 ± 10.23) years (traditional acupuncture + low dose antipsychotics group); (30.12 ± 8.06) years (antipsychotics group). History: average duration of illness (5.53 ± 6.08) years (start age (25.33 ± 8.12) years) (traditional acupuncture + low dose antipsychotics group); (6.04 ± 3.47) years (start age (26.17 ± 7.32) years) (antipsychotics group). Type: hebephrenic schizophrenia 2 cases, paranoid type 28 cases, simple schizophrenia 1 case, undifferentiated type 9 cases (traditional acupuncture + low dose antipsychotics group); hebephrenic schizophrenia 1 case, paranoid type 26 cases, simple schizophrenia 2 cases, catatonic type 1 case, undifferentiated type 10 cases (antipsychotics group) Country: China. Inclusion criteria: had a CCMD‐2‐R diagnosis of schizophrenia; BPRS ≥ 35. Exclusion criteria: had a CCMD‐2‐R diagnosis of schizophrenia but BPRS < 35 or had diseases which would affect trial results. | |
| Interventions | 1. Traditional acupuncture + low dose antipsychotics: traditional acupuncture* (used main acupoints** and adjunct acupoints*** [according to the TCM type of schizophrenia] and special acupoints**** [according to symptoms]) + low dose antipsychotics (equivalent chlorpromazine dose ≤ 0.2 g/d). N = 40. 2. Antipsychotics: maximum daily dose equivalent chlorpromazine dose 0.4 to 0.7 g/d. N = 40. Combination therapy: added artane when patient with severe extrapyramidal side effects; added propranolol when patient with severe palpitation and heart rate > 100 times/minute. * Traditional acupuncture: used lifting‐thrusting supplementation and draining method and twirling supplementation and draining method according to patient's condition; manipulated needles about 3 minutes and once ten minutes; total for about 30 minutes; at first once a day then reduced to once every two days when patient was in stable condition and once a week after psychiatric symptoms disappeared. ** Main acupoints: Shuigou, Baihui, Neiguan, Sanyingjiao. ***Adjunct acupoints (according to the CTM type of schizophrenia): Type of internal disturbance of pyrophlegm: Zhongwan, Fenglong, Xingjian. Type of Internal Retention of phlegm and dampness: Fenglong, Yinglingquan, Zusanli. Type of Qi stagnation and Blood stasis: Xuehai, Geshu. Type of Yin deficiency and fire excess: Shenmen, Fuliu. Type of Yang deficiency: Taixi, Guanyuan (moxibustion). Other miscellaneous types such as deficiency of both heart and spleen: Anmian, Shenmen. **** Special acupoints (according to symptoms): Zhongzhu, Tinggong (auditory hallucinations); Yuyao (phosphenes); Hegu, Laogong (agitation). | |
| Outcomes | Mental state1: BPRS; SAPS; SANS. Behaviour: leaving the study early. Adverse effects: TESS2. Unable to use: | |
| Notes | 1. The ratings were assessed before treatment and each 20 days after treatment. 3. Assessment criteria: recovery (psychiatric symptoms disappeared completely; insight recovered); marked improvement (psychiatric symptoms disappeared completely or the majority main psychiatric symptoms disappeared; insight partly recovered or not recovered); improvement (symptoms disappeared partly; insight did not recover); no effect (no symptoms improved obviously and insight did not recover). 4. The rating was assessed after treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report stated ‐ "randomly divided into experimental group and control group using random allocation table according to the admission date and case number". |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Sham electroacupuncture not used. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | Three participants left the study early but results graphs (BPRS, SAPS, SANS, TESS) showed that author analysed 40 cases in each group. |
| Selective reporting (reporting bias) | Unclear risk | We were unable to locate the protocol, unsure if selective reporting occurred. |
| Other bias | Unclear risk | Participants were men and unsure if gender selection bias occurred. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (type I; Kuang type) (CCMD‐2‐R; Diagnosis and Effect Standard of Diseases in TCM [1994]) . History: longer than 3 months. Setting: outpatients. Country: China. Inclusion criteria: had a CCMD‐2‐R diagnosis of schizophrenia; had a TCM diagnosis of Kuang type of phlegm‐fire disturbing mind; stopped to receive relative drug treatment more than 1 month. Exclusion criteria: cerebral organic mental disorders; mental disorders caused by somatic diseases; mental disorders caused by psychoactive substances and non‐dependent substances; had both schizophrenia and mood disorders symptoms but the duration of illness of disruptive symptoms was shorter than that of mood disorder symptoms or no longer than 2 weeks; with severe cardiovascular and cerebrovascular, liver and haematopoietic system diseases. | |
| Interventions | 1. Fuyuankang capsule: 5 capsules (0.4 g/capsule) every time; 3 times a day; with warm water. N = 90. 2. Traditional acupuncture: Shuigou, Shaoshang, Yingbai, Fengfu, Daling, Quchi, Fenglong; once a day; for 30 minutes. N = 90. 3. Traditional acupuncture + Fuyankang capsule: traditional acupuncture (Shuigou, Shaoshang, Yingbai, Fengfu, Daling, Quchi, Fenglong; once a day; for 30 minutes) + Fuyuankang capsule (5 capsules every time; 3 times a day; with warm water). N = 90. 4. Weisitong (risperidone tablet): initial dose 1 mg/d (after dinner); added 1 mg after 3 days then added 0.1 mg every week until daily dose 4 mg. N = 30. * Author used placebo with therapeutic medications; no further details. | |
| Outcomes | Global state: no clinically important change in global state1. Behaviour: leaving the study early. Unable to use: Global state: TCM Syndromes Scale2(no useful data). Mental state: BPRS (no data). Adverse effects: lab test (ECG; blood routine test; urine routine test; stool test; liver function; kidney function); blood pressure; adverse reaction (only reported data for traditional acupuncture + Fuyuankang group). Lab test: SOD (not clinical outcomes). | |
| Notes | 1. Assessment criteria: recovery (talk, behaviour and expression all returned to normal state; could deal with daily affairs; the reduction of BPRS ≥ 95%; improvement (talk, behaviour and expression returned to normal state approximately or obviously improved; the reduction of BPRS 30% to 94%); no effect (talk, behaviour and expression still existed as before; the reduction of BPRS < 29%). 2. Author also reported the global state of TCM. 3. The study of 'Zhao 2005' consisted of two parts ‐ 'traditional ‐ Zhao 2005a' (type I schizophrenia) and 'traditional ‐ Zhao 2005b' (type II schizophrenia). 4. The allocation rate of groups of each type schizophrenia was 3:3:3:1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Used placebo but did not use sham acupuncture. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | High risk | Although the protocol was not located, the author reported that BPRS was one of the outcomes, however, only reported global state. |
| Other bias | Low risk | Not obvious. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (type II; Dian type) (CCMD‐2‐R; Diagnosis and Effect Standard of Diseases in TCM [1994]) . History: longer than 3 months. Setting: outpatients. Country: China. Inclusion criteria: had a CCMD‐2‐R diagnosis of schizophrenia; had a TCM diagnosis of Dian type of phlegm‐Qi stagnation and blinding; stopped to receive relative drug treatment more than 1 month. Exclusion criteria: cerebral organic mental disorders; mental disorders caused by somatic diseases; mental disorders caused by psychoactive substances and non‐dependent substances; had both schizophrenia and mood disorders symptoms but the duration of illness of disruptive symptoms was shorter than that of mood disorder symptoms or no longer than 2 weeks; with severe cardiovascular and cerebrovascular, liver and haematopoietic system diseases. | |
| Interventions | 1. Fuyuankang capsule: 5 capsules (0.4 g/capsule) every time; 3 times a day; with warm water. N = 90. 2. Traditional acupuncture: Xinshu, Ganshu, Pishu, Shenmen, Fenglong; once a day; for 30 minutes. N = 90. 3. Traditional acupuncture + Fuyankang capsule: traditional acupuncture (Xinshu, Ganshu, Pishu, Shenmen, Fenglong; once a day; for 30 minutes) + Fuyuankang capsule (5 capsules every time; 3 times a day; with warm water). N = 90. 4. Weisitong (risperidone tablet): initial dose 1 mg/d (after dinner); added 1 mg after 3 days then added 0.1 mg every week until daily dose 4 mg. N = 30. * Author used placebo with therapeutic medications; no further details. | |
| Outcomes | Global state: no clinically important change in global state1. Behaviour: leaving the study early. Unable to use: Global state: TCM Syndromes Scale2(no useful data). Mental state: BPRS. Adverse effects: lab test (ECG; blood routine test; urine routine test; stool test; liver function; kidney function); blood pressure; adverse reaction (only reported data of traditional acupuncture + Fuyuankang group). Lab test: SOD (not clinical outcomes). | |
| Notes | 1. Criteria: recovery (talk, behaviour and expression all returned to normal state; could deal with daily affairs; the reduction of BPRS ≥ 95%; improvement (talk, behaviour and expression returned to normal state approximately or obviously improved; the reduction of BPRS 30% to 94%); no effect (talk, behaviour and expression still existed as before; the reduction of BPRS < 29%). 2. Author also reported the global state of TCM. 3. The study of 'Zhao 2005' consisted of two part ‐ 'traditional ‐ Zhao 2005a' (type I schizophrenia) and 'traditional ‐ Zhao 2005b' (type II schizophrenia). 4. The allocation rate of groups of each type schizophrenia was 3:3:3:1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report stated ‐ "randomly divided". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Not stated. |
| Blinding of participants and personnel (performance bias) | High risk | Used placebo but did not use sham acupuncture. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | No participants left the study early. |
| Selective reporting (reporting bias) | High risk | Although the protocol was not located, the author reported that BPRS was one of the outcomes, however, only reported global state. |
| Other bias | Low risk | Not obvious. |
Diagnostic tools and scales:
DSM: Diagnostic and Statistical Manual.
ICD 10: International Classification of Diseases.
CCMD: Chinese Classification of Mental Disorders.
Global state:
CGI: Clinical Global Impression Scale.
CGI‐SI: Clinical Global Impression ‐ Severity of illness.
CGI‐GI: Clinical Global Impression ‐ Improvement scale.
CGI‐EI: Clinical Global Impression ‐ Efficacy Index.
Mental state:
BPRS: Brief Psychiatric Rating Scale.
PANSS: Positive and Negative Syndrome Scale.
SANS: Scale for the Assessment of Negative Symptoms.
SAPS: Scale for the Assessment of Positive Symptoms.
SAHS: Specific Auditory Hallucination Scale.
HAMD: Hamilton Rating Scale for Depression.
SDS: Zung Self‐Rating Depression Scale.
PSYRATS‐AH: Psychotic Symptom Rating Scales Auditory Hallucination Subscale.
Adverse effects:
TESS: Treatment Emergent Symptom Scale.
RESES: Rating Scale for Extrapyramidal Side Effects.
Test:
ECG: electrocardiogram.
EEG: electroencephalogram.
cAMP: cyclic adenosine monophosphate.
cGMP: cyclic guanosine monophosphate.
T3: triiodothyronine.
T4: thyroid hormone.
RUR: T Resin Test.
FT4I: free T index.
TSH: thyroid‐stimulation hormone.
rT3: trans triiodothyronine.
TG: thyroglobulin antibody.
TM: thyroid microsome.
LH: luteinizing hormone.
FSH: follicle stimulating hormone.
T: testosterone.
SOD: superoxide dismutase.
Others:
TCM: Traditional Chinese Medicine.
CCEA: Computer‐Controlled Electric Acupuncture.
mg/d: mg per day.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Allocation: randomised. Participants: people with schizophrenia or mood disorders (affective disorders) manic episode. Interventions: acupuncture + antipsychotics vs antipsychotics. Outcomes: not reported by diagnostic group. | |
| Allocation: randomised. Participants: people with chronic schizophrenia. Interventions: antipsychotics + electroacupuncture (Yingtang and Baihui) versus antipsychotics + electroacupuncture (Baihui and Spiritual and emotional movement area) (compared electroacupuncture with different acupoints), not acupuncture vs other treatments. | |
| Allocation: not randomised. | |
| Allocation: not randomised, case series. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: acupoint injection + low dose chlorpromazine (Wintermin) versus chlorpromazine (Wintermin). Outcomes: BPRS (mental state); TESS (adverse effects). * Some important data from this study (conducted in same institution as acupoint inj ‐ Pan 2002) were the same as acupoint inj ‐ Pan 2002 (baseline and endpoint total BPRS), but numbers allocated, the acupoint method, and BPRS' factor data were different; we could not contact author of Wu 2004 but author of acupoint inj ‐ Pan 2002 had no knowledge of this study. | |
| Allocation: not randomised, quasi‐randomised (according to the admission order; patient with odd number into electroacupuncture group and with even number into MECT group). | |
| Allocation: divided randomly to three intervention groups but unclear how allocated within one key intervention group Participants: people with schizophrenia. Interventions: Electroacupuncture/acuclip convulsive therapy (EACT) (involved mixture of techniques ‐ not all of which are acupuncture ‐ several of which could be applied in a single person) versus electroconvulsive therapy (ECT) versus ECT or EACT (unclear how allocation to EACT undertaken within this group), not acupuncture versus none/other treatment. | |
| Allocation: randomised. | |
| Allocation: not randomised, allocated according to age and sex. |
Mental state:
BPRS: Brief Psychiatric Rating Scale.
Adverse effects:
TESS: Treatment Emergent Symptom Scale.
Test:
ECT: electroconvulsive therapy.
EACT: electric acupuncture convulsive therapy.
Other:
MECT: modified electroconvulsive therapy
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Allocation: randomised. Design: parallel. |
| Participants | Diagnosis: schizophrenia with obesity (ICD). N = 86 (estimated enrolment). Sex: women and men. Inclusion criteria: ICD:295, living in chronic ward for more than 2 months; body mass index (BMI) > or = 24; aged between 20 to 60; psychotic status stable and can communicate. Exclusion criteria: unstable psychotic status; participants who have endocrine disease; participants who have cardiac disease; participants who have immunological disease; participants who have liver or renal function impairment; pregnant or lactating woman; cerebrovascular accident (CVA) stroke and disability; participants who attend weight control programs in last 3 months; any conditions that treating doctors refuse to join in this study. |
| Interventions | 1. Auricular acupressure: with a 0.5 mm x 0.5 mm seed on the specific positions on the ear and press these specific positions 3 times a day. 2. Placebo: no further details. |
| Outcomes | Metabolic: Body weight scale, waste circumference, fat percentage by BIA. |
| Notes | Contacted with Han‐Yi Ching using the email address from the ClinicalTrials.gov but no feedback. No further details and unable to confirm whether the study has finished and unable to locate the full text. |
BIA: Bio‐Impedance Analysis
ICD: International Classification of Diseases.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 Global state: Not improved, endpoint Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.1  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 1 Global state: Not improved, endpoint. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.1 medium‐term (various similar criteria) | 3 | 244 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.28, 0.57] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.2 duration unclear | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.08] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse) Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.2  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 2 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.1 short‐term | 4 | 327 | Mean Difference (IV, Fixed, 95% CI) | ‐4.32 [‐5.28, ‐3.36] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.2 medium‐term | 3 | 220 | Mean Difference (IV, Fixed, 95% CI) | ‐5.51 [‐6.71, ‐4.30] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, medium‐term) ‐ subgroup analysis Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.3 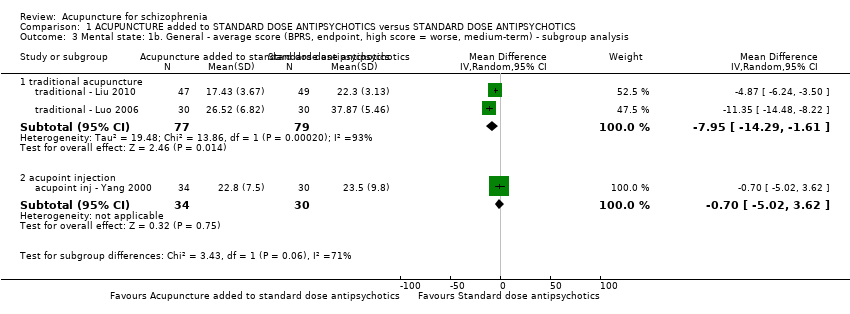 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 3 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, medium‐term) ‐ subgroup analysis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3.1 traditional acupuncture | 2 | 156 | Mean Difference (IV, Random, 95% CI) | ‐7.95 [‐14.29, ‐1.61] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3.2 acupoint injection | 1 | 64 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐5.02, 3.62] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4 Mental state: 2a. General ‐ average score (PANSS, endpoint, high score = worse) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.4  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 4 Mental state: 2a. General ‐ average score (PANSS, endpoint, high score = worse). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4.1 short‐term | 4 | 245 | Mean Difference (IV, Fixed, 95% CI) | ‐2.47 [‐4.31, ‐0.63] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4.2 medium‐term | 2 | 135 | Mean Difference (IV, Fixed, 95% CI) | ‐3.79 [‐6.43, ‐1.15] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5 Mental state: 2b. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ subgroup analysis Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.5  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 5 Mental state: 2b. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ subgroup analysis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5.1 traditional acupuncture | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 1.30 [‐1.56, 4.16] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5.2 electroacupuncture | 3 | 185 | Mean Difference (IV, Random, 95% CI) | ‐5.64 [‐10.93, ‐0.35] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6 Mental state: 2c. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ electroacupuncture subgroup analysis Show forest plot | 2 | 135 | Mean Difference (IV, Fixed, 95% CI) | ‐3.79 [‐6.43, ‐1.15] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.6 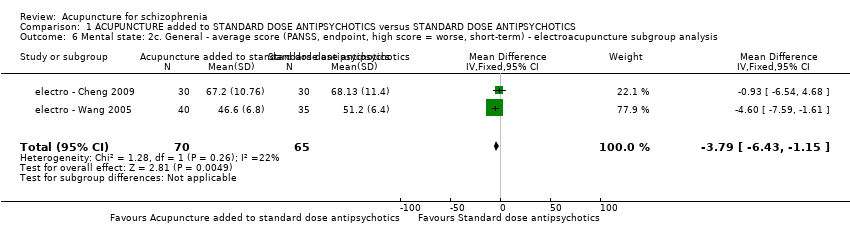 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 6 Mental state: 2c. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ electroacupuncture subgroup analysis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7 Mental state: 2d. General ‐ average score (PANSS, endpoint, high score = worse) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.7
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 7 Mental state: 2d. General ‐ average score (PANSS, endpoint, high score = worse) ‐ Skewed data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7.1 short‐term | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7.2 medium‐term | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8 Mental state: 2e. General ‐ not improved (PANSS), endpoint Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.8 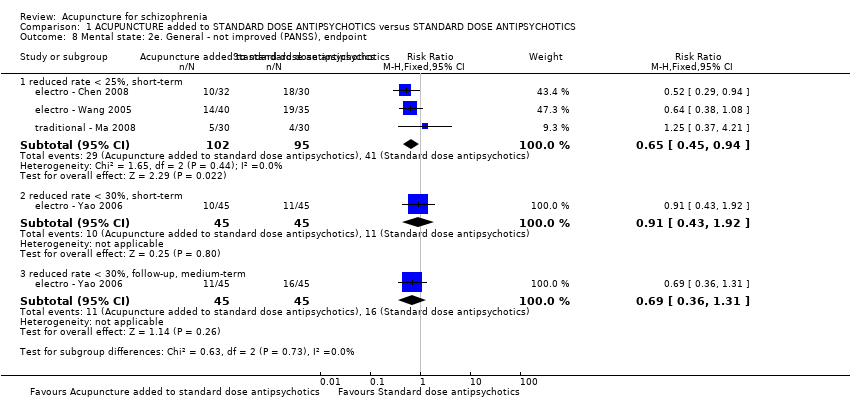 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 8 Mental state: 2e. General ‐ not improved (PANSS), endpoint. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8.1 reduced rate < 25%, short‐term | 3 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.45, 0.94] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8.2 reduced rate < 30%, short‐term | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.43, 1.92] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8.3 reduced rate < 30%, follow‐up, medium‐term | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.36, 1.31] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9 Mental state: 3. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.9
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 9 Mental state: 3. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10 Mental state: 4a.Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.10  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 10 Mental state: 4a.Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10.1 short‐term | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐7.66 [‐13.05, ‐2.27] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10.2 medium‐term | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐12.35 [‐17.54, ‐7.16] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.11
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 11 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11.1 traditional acupuncture | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11.2 electroacupuncture | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12 Mental state: 5a. Specific ‐ average score ‐ depression (HAMD, endpoint, high score = worse, short‐term) Show forest plot | 2 | 109 | Mean Difference (IV, Random, 95% CI) | ‐8.66 [‐12.10, ‐5.22] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.12 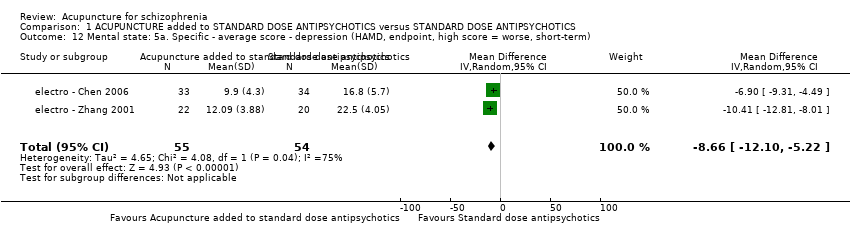 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 12 Mental state: 5a. Specific ‐ average score ‐ depression (HAMD, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13 Mental state: 5b. Specific ‐ not improved ‐ depression (HAMD, reduced rate < 25%, short‐term) Show forest plot | 2 | 109 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.08, 0.34] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.13 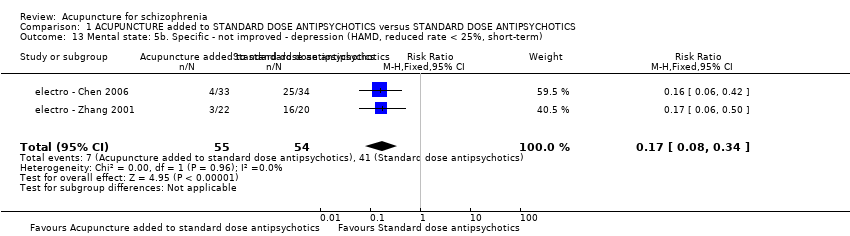 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 13 Mental state: 5b. Specific ‐ not improved ‐ depression (HAMD, reduced rate < 25%, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14 Mental state: 7b. Specific ‐ not improved ‐ auditory hallucinations (PSYRAS‐AH, reduction < 20%, short‐term) Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.14, 0.52] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.14  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 14 Mental state: 7b. Specific ‐ not improved ‐ auditory hallucinations (PSYRAS‐AH, reduction < 20%, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15 Mental state: 7a. Specific ‐ average score ‐ auditory hallucinations (PSYRAS‐AH,endpoint, high score = worse, short‐term) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.17 [‐4.16, ‐0.18] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.15  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 15 Mental state: 7a. Specific ‐ average score ‐ auditory hallucinations (PSYRAS‐AH,endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16 Mental state: 6. Specific ‐ average score ‐ depression (SDS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | ‐24.25 [‐28.01, ‐20.49] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.16  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 16 Mental state: 6. Specific ‐ average score ‐ depression (SDS, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17 Mental state: 8. Specific ‐ not improved (auditory hallucinations, endpoint) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.17  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 17 Mental state: 8. Specific ‐ not improved (auditory hallucinations, endpoint). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17.1 still existed after 30 days, short‐term | 1 | 216 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.13, 0.44] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17.2 still existed or appeared frequently after disappeared, medium‐term | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.17, 0.61] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17.3 no change of auditory hallucinations, duration unclear | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.17] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18 Mental state: 9. Specific ‐ average score ‐ auditory hallucinations (SAHS, endpoint, high score = worse) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.18
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 18 Mental state: 9. Specific ‐ average score ‐ auditory hallucinations (SAHS, endpoint, high score = worse) ‐ Skewed data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18.1 short‐term | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18.2 medium‐term | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 19 Mental state: 10. Specific ‐ average score ‐ hallucinations (BPRS [12th item], endpoint, high score = worse, short‐term) Show forest plot | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.73 [‐1.28, ‐0.18] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.19 ![Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 19 Mental state: 10. Specific ‐ average score ‐ hallucinations (BPRS [12th item], endpoint, high score = worse, short‐term).](/cdsr/doi/10.1002/14651858.CD005475.pub2/media/CDSR/CD005475/image_n/nCD005475-CMP-001-19.png) Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 19 Mental state: 10. Specific ‐ average score ‐ hallucinations (BPRS [12th item], endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20 Behaviour: Leaving the study early Show forest plot | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.20  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 20 Behaviour: Leaving the study early. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20.1 short‐term | 10 | 870 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.33, 5.45] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20.2 medium‐term | 5 | 370 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.58 [0.60, 21.27] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 21 Service outcomes: Time in hospital (days) Show forest plot | 1 | 120 | Mean Difference (IV, Fixed, 95% CI) | ‐16.0 [‐19.54, ‐12.46] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.21 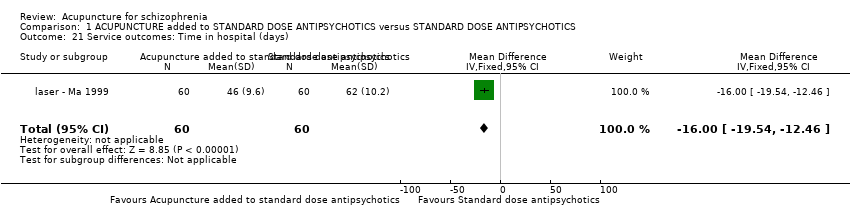 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 21 Service outcomes: Time in hospital (days). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 22 Adverse effects: 1. General ‐ average score (TESS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐2.80 [‐3.09, ‐2.51] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.22  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 22 Adverse effects: 1. General ‐ average score (TESS, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23 Adverse effects: 2a. Specific ‐ extrapyramidal symptoms Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.23 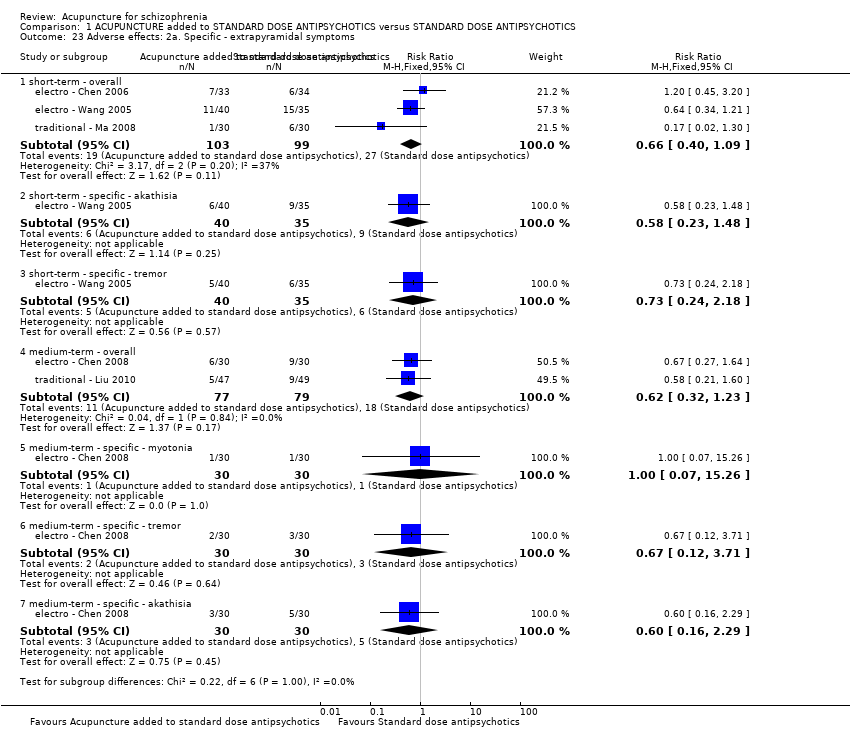 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 23 Adverse effects: 2a. Specific ‐ extrapyramidal symptoms. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23.1 short‐term ‐ overall | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.40, 1.09] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23.2 short‐term ‐ specific ‐ akathisia | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.23, 1.48] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23.3 short‐term ‐ specific ‐ tremor | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.24, 2.18] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23.4 medium‐term ‐ overall | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.32, 1.23] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23.5 medium‐term ‐ specific ‐ myotonia | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 15.26] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23.6 medium‐term ‐ specific ‐ tremor | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.71] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23.7 medium‐term ‐ specific ‐ akathisia | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.16, 2.29] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24 Adverse effects: 2b. Specific ‐ extrapyramidal symptoms ‐overall (short‐term) ‐ subgroup analysis Show forest plot | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.40, 1.09] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.24  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 24 Adverse effects: 2b. Specific ‐ extrapyramidal symptoms ‐overall (short‐term) ‐ subgroup analysis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24.1 traditional acupuncture | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.02, 1.30] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24.2 electroacupuncture | 2 | 142 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.47, 1.34] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25 Adverse effects: 3. Specific ‐ Central Nervous System Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.25 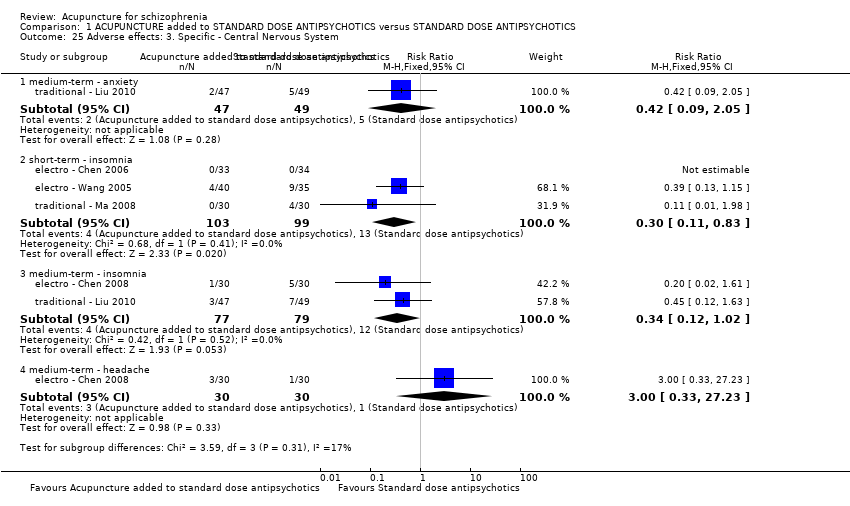 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 25 Adverse effects: 3. Specific ‐ Central Nervous System. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25.1 medium‐term ‐ anxiety | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.09, 2.05] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25.2 short‐term ‐ insomnia | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.11, 0.83] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25.3 medium‐term ‐ insomnia | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.12, 1.02] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25.4 medium‐term ‐ headache | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.33, 27.23] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26 Adverse effects: 4. Specific ‐ anticholinergic symptoms Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.26 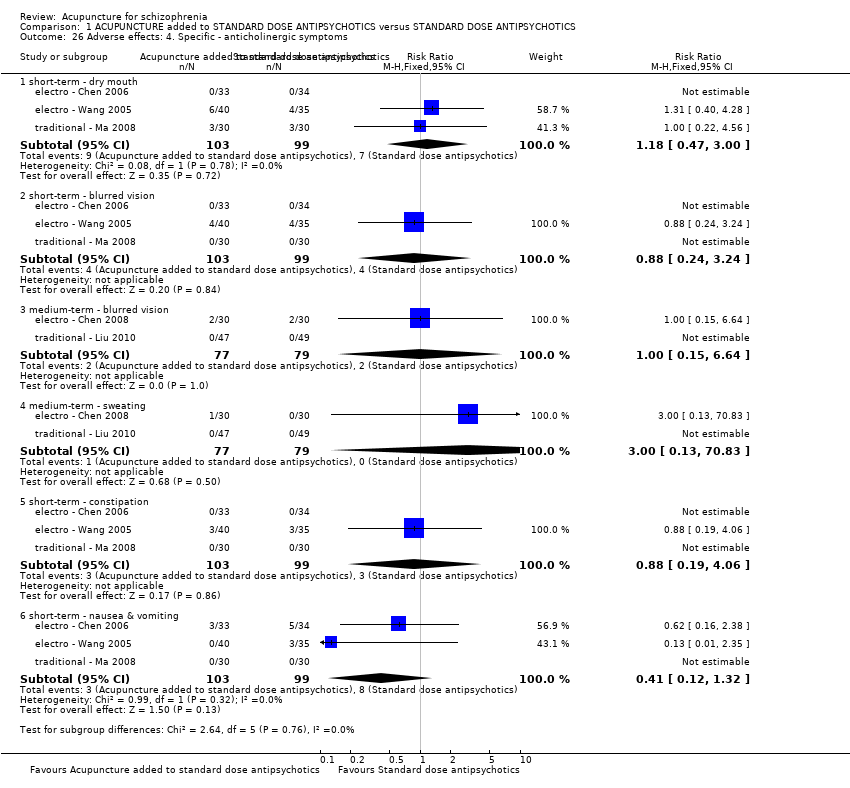 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 26 Adverse effects: 4. Specific ‐ anticholinergic symptoms. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26.1 short‐term ‐ dry mouth | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.47, 3.00] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26.2 short‐term ‐ blurred vision | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.24, 3.24] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26.3 medium‐term ‐ blurred vision | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.64] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26.4 medium‐term ‐ sweating | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.83] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26.5 short‐term ‐ constipation | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.19, 4.06] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26.6 short‐term ‐ nausea & vomiting | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.12, 1.32] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 27 Adverse effects: 5. Specific ‐ gastrointestinal system Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.27  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 27 Adverse effects: 5. Specific ‐ gastrointestinal system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 27.1 medium‐term ‐ unspecified gastrointestinal symptoms | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.10, 2.71] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 27.2 short‐term ‐ constipation | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.19, 4.06] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 27.3 short‐term ‐ nausea & vomiting | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.12, 1.32] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28 Adverse effects: 6. Specific ‐ cardiovascular symptoms (or headache) Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.28 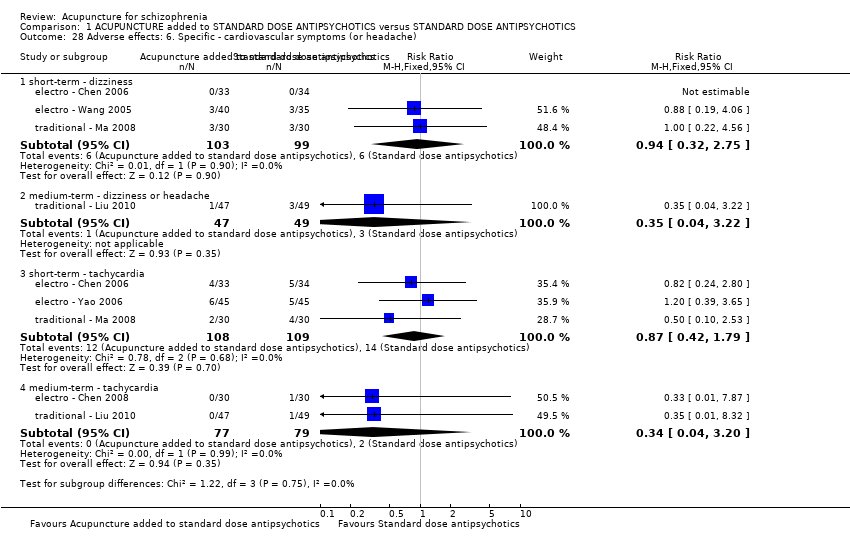 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 28 Adverse effects: 6. Specific ‐ cardiovascular symptoms (or headache). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28.1 short‐term ‐ dizziness | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.32, 2.75] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28.2 medium‐term ‐ dizziness or headache | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.04, 3.22] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28.3 short‐term ‐ tachycardia | 3 | 217 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.42, 1.79] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28.4 medium‐term ‐ tachycardia | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.04, 3.20] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29 Adverse effects: 7a. Specific ‐ metabolic system Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.29 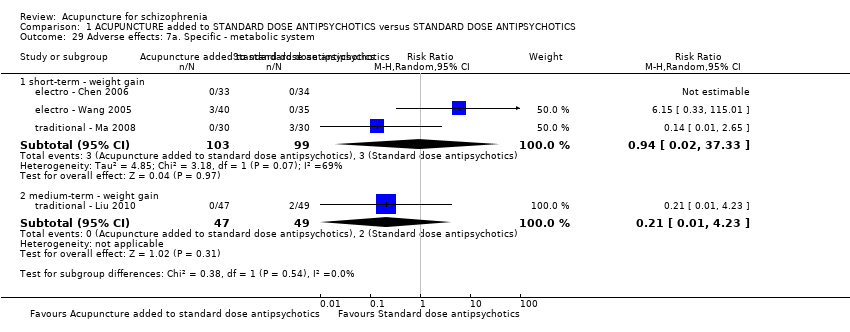 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 29 Adverse effects: 7a. Specific ‐ metabolic system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29.1 short‐term ‐ weight gain | 3 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.02, 37.33] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29.2 medium‐term ‐ weight gain | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.01, 4.23] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 30 Adverse effects: 7b. Specific ‐ metabolic system ‐ weight gain (short‐term) ‐ subgroup analysis Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.30  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 30 Adverse effects: 7b. Specific ‐ metabolic system ‐ weight gain (short‐term) ‐ subgroup analysis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 30.1 traditional acupuncture | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.65] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 30.2 electroacupuncture | 2 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 6.15 [0.33, 115.01] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31 Adverse effects: 8. Specific ‐ endocrine system Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.31 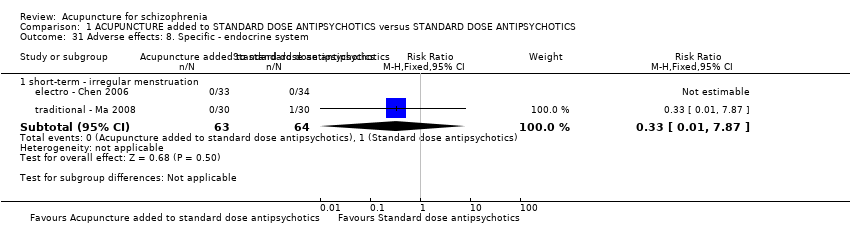 Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 31 Adverse effects: 8. Specific ‐ endocrine system. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 31.1 short‐term ‐ irregular menstruation | 2 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.87] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 32 Adverse effects: 9. Specific ‐ lab test Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.32  Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 32 Adverse effects: 9. Specific ‐ lab test. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 32.1 short‐term ‐ liver function abnormal | 4 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.26, 3.90] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 32.2 medium‐term ‐ liver function abnormal | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.12, 3.98] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 32.3 short‐term ‐ ECG abnormal (myocardial ischaemia) | 4 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.05, 5.32] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 32.4 short‐term ‐ blood routine test abnormal (leukocyte change) | 4 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.32, 5.62] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||||||||||||||||||||||||||
| 1 Global state: 1. Relapse (follow‐up, long‐term) Show forest plot | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.37, 0.89] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.1 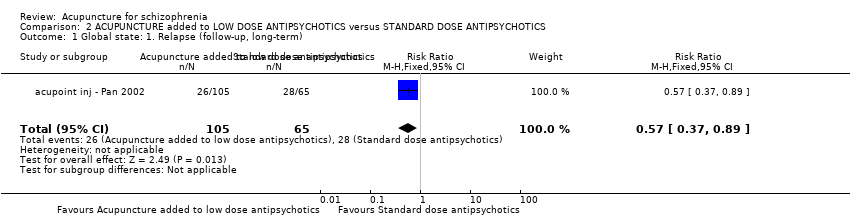 Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 1 Global state: 1. Relapse (follow‐up, long‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 Global state: 2. Not improved (various similar criteria), endpoint (short‐term) Show forest plot | 4 | 272 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.40, 1.72] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.2  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 2 Global state: 2. Not improved (various similar criteria), endpoint (short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.1 no symptoms improved obviously and insight did not recover | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.86] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 2.2 symptoms and orientation showed no change | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.9 [0.30, 2.68] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 2.3 according to traditional criteria | 2 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.35, 3.02] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 3 Global state: 3a. CGI ‐ average score ‐ CGI‐SI (endpoint, high score = worse, short‐term) Show forest plot | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐1.08, 0.28] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.3  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 3 Global state: 3a. CGI ‐ average score ‐ CGI‐SI (endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4 Global state: 3b. CGI ‐ average score ‐ CGI‐GI (endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.4
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 4 Global state: 3b. CGI ‐ average score ‐ CGI‐GI (endpoint, high score = worse, short‐term) ‐ Skewed data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5 Global state: 3c. CGI ‐ average score ‐ CGI‐EI (endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.5
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 5 Global state: 3c. CGI ‐ average score ‐ CGI‐EI (endpoint, high score = worse, short‐term) ‐ Skewed data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse) Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.6 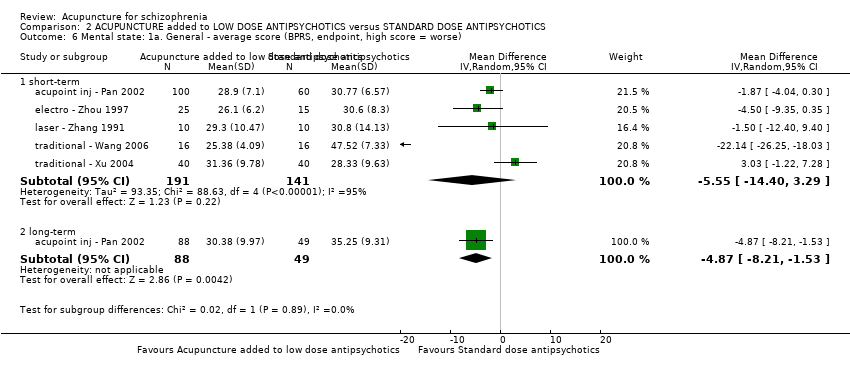 Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 6 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6.1 short‐term | 5 | 332 | Mean Difference (IV, Random, 95% CI) | ‐5.55 [‐14.40, 3.29] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 6.2 long‐term | 1 | 137 | Mean Difference (IV, Random, 95% CI) | ‐4.87 [‐8.21, ‐1.53] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 7 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, short‐term) ‐ subgroup analysis Show forest plot | 4 | 300 | Mean Difference (IV, Fixed, 95% CI) | ‐1.36 [‐3.13, 0.41] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.7  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 7 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, short‐term) ‐ subgroup analysis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7.1 traditional acupuncture | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 3.03 [‐1.22, 7.28] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 7.2 electroacupuncture | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐4.5 [‐9.35, 0.35] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 7.3 acupoint injection | 1 | 160 | Mean Difference (IV, Fixed, 95% CI) | ‐1.87 [‐4.04, 0.30] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 7.4 laser acupuncture | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐12.40, 9.40] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 8 Mental state: 1c. General ‐ not improved (BPRS, short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.8 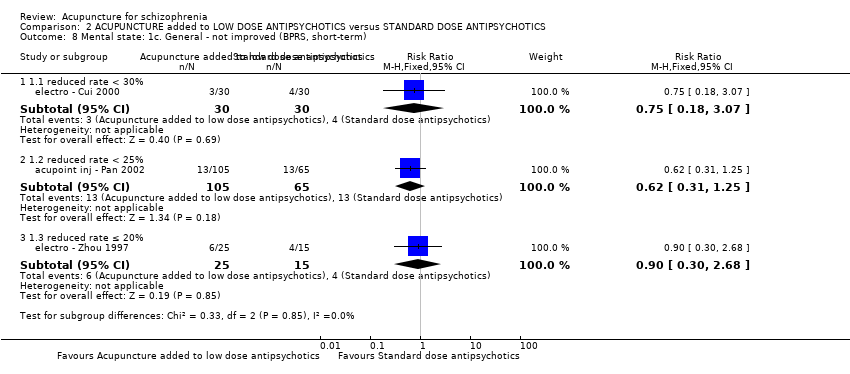 Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 8 Mental state: 1c. General ‐ not improved (BPRS, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8.1 1.1 reduced rate < 30% | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.07] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 8.2 1.2 reduced rate < 25% | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.31, 1.25] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 8.3 1.3 reduced rate ≤ 20% | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.9 [0.30, 2.68] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 9 Mental state: 1d. General ‐ average change scores (BPRS, low score = worse, short‐term) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.81 [‐3.17, 4.79] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.9  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 9 Mental state: 1d. General ‐ average change scores (BPRS, low score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10 Mental state: 2a. General ‐ Average score (PANSS, endpoint, high score = worse, short‐term) ‐ Skew data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.10
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 10 Mental state: 2a. General ‐ Average score (PANSS, endpoint, high score = worse, short‐term) ‐ Skew data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11 Mental state: 2b. General ‐ not improved (PANSS, reduced rate < 30%, short‐term) Show forest plot | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.57, 2.62] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.11 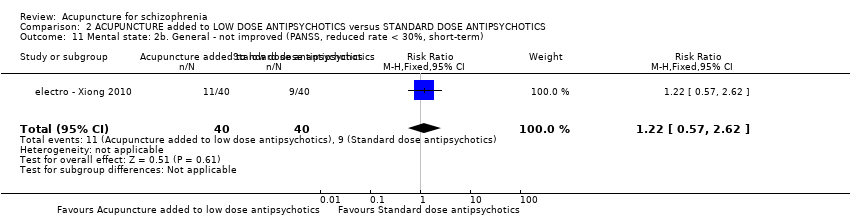 Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 11 Mental state: 2b. General ‐ not improved (PANSS, reduced rate < 30%, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12 Mental state: 3a. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.12  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 12 Mental state: 3a. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12.1 traditional acupuncture | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐13.34 [‐16.94, ‐9.74] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 12.2 acupoint catgut treatment | 1 | 180 | Mean Difference (IV, Random, 95% CI) | 1.21 [0.96, 1.46] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 13 Mental state: 3b. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.13
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 13 Mental state: 3b. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14 Mental state: 4a. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 0.61 [‐3.30, 4.52] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.14  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 14 Mental state: 4a. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.15
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 15 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16 Behaviour: Leaving the study early (short‐term) Show forest plot | 8 | 662 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.29, 2.29] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.16  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 16 Behaviour: Leaving the study early (short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17 Adverse effects: 1a. General ‐ average score (TESS, endpoint, high score = worse, short‐term) Show forest plot | 2 | 200 | Mean Difference (IV, Fixed, 95% CI) | ‐0.56 [‐0.86, ‐0.26] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.17 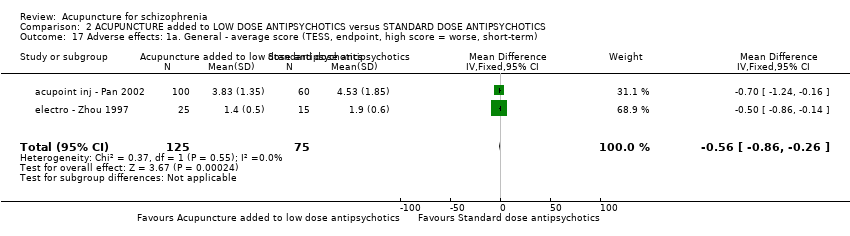 Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 17 Adverse effects: 1a. General ‐ average score (TESS, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18 Adverse effects: 1b. General ‐ average score (TESS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.18
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 18 Adverse effects: 1b. General ‐ average score (TESS, endpoint, high score = worse, short‐term) ‐ Skewed data. | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 19 Adverse effects: 2. Specific ‐ average score (RESES, endpoint, high score = worse, short‐term) Show forest plot | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐0.6 [‐0.73, ‐0.47] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.19 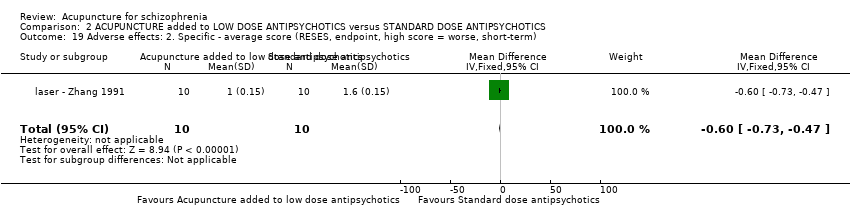 Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 19 Adverse effects: 2. Specific ‐ average score (RESES, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20 Adverse effects: 3. Specific ‐ extrapyramidal symptoms (short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.20  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 20 Adverse effects: 3. Specific ‐ extrapyramidal symptoms (short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20.1 overall | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.16, 0.46] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 20.2 specific ‐ myotonia | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.29] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 20.3 specific ‐ tremor | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.69] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 20.4 specific ‐ akathisia | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.49] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 21 Adverse effects: 4. Specific ‐ Central Nervous System (short‐term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.21  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 21 Adverse effects: 4. Specific ‐ Central Nervous System (short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 21.1 activity increasing | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.85] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 21.2 insomnia | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.00, 1.20] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 21.3 sleepiness | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.03] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 22 Adverse effects: 5. Specific ‐ anticholinergic symptoms (short‐term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.22  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 22 Adverse effects: 5. Specific ‐ anticholinergic symptoms (short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 22.1 dry mouth | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.09, 0.58] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 22.2 nasal congestion | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.69] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 22.3 blurred vision | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.06, 0.83] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 22.4 constipation | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.00, 1.20] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 23 Adverse effects: 6. Specific ‐ cardiovascular symptoms (short‐term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.23 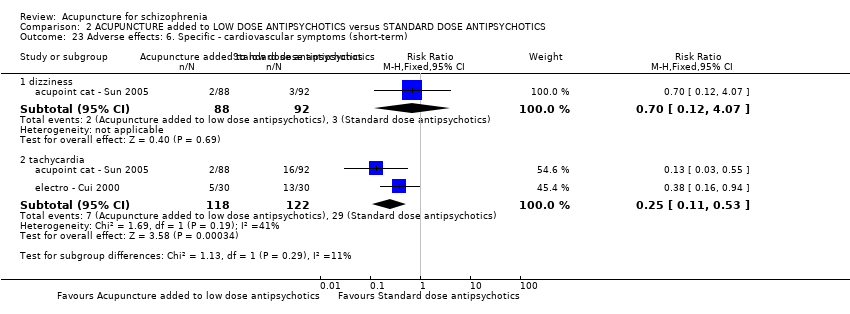 Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 23 Adverse effects: 6. Specific ‐ cardiovascular symptoms (short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23.1 dizziness | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.12, 4.07] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 23.2 tachycardia | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.11, 0.53] | ||||||||||||||||||||||||||||||||||||||||||||||||
| 24 Adverse effects: 7. Specific ‐ skin infection (short‐term) Show forest plot | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.24  Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 24 Adverse effects: 7. Specific ‐ skin infection (short‐term). | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||
| 1 Global state: Not improved, endpoint (short‐term) Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||
| Analysis 3.1  Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 1 Global state: Not improved, endpoint (short‐term). | ||||||||||||||||||||||||||||
| 1.1 various similar criteria | 3 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.53, 1.48] | ||||||||||||||||||||||||
| 1.2 talk, behaviour and expression still existed as before + reduction of BPRS < 29% | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.19, 0.59] | ||||||||||||||||||||||||
| 2 Mental state: 1. General ‐ average score (BPRS, endpoint, high score = worse, short‐term) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |||||||||||||||||||||||||
| Analysis 3.2  Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 2 Mental state: 1. General ‐ average score (BPRS, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||
| 2.1 traditional acupuncture | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐11.56 [‐16.36, ‐6.76] | ||||||||||||||||||||||||
| 2.2 laser acupuncture | 1 | 21 | Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐11.19, 9.05] | ||||||||||||||||||||||||
| 3 Mental state: 2. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | ‐5.24 [‐9.06, ‐1.42] | ||||||||||||||||||||||||
| Analysis 3.3  Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 3 Mental state: 2. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||
| 4 Mental state: 3. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | ‐7.92 [‐17.01, 1.17] | ||||||||||||||||||||||||
| Analysis 3.4  Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 4 Mental state: 3. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term). | ||||||||||||||||||||||||||||
| 5 Behaviour: Leaving the study early (short‐term) Show forest plot | 6 | 421 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||
| Analysis 3.5  Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 5 Behaviour: Leaving the study early (short‐term). | ||||||||||||||||||||||||||||
| 6 Adverse effects: 1. General ‐ average scores (TESS, endpoint, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||
| Analysis 3.6
Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 6 Adverse effects: 1. General ‐ average scores (TESS, endpoint, short‐term) ‐ Skewed data. | ||||||||||||||||||||||||||||
| 7 Adverse effects: 2. Specific ‐ extrapyramidal symptoms (short‐term) Show forest plot | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.00, 0.83] | ||||||||||||||||||||||||
| Analysis 3.7  Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 7 Adverse effects: 2. Specific ‐ extrapyramidal symptoms (short‐term). | ||||||||||||||||||||||||||||
| 8 Adverse effects: 3. Specific ‐ numbness over the ear, upper extremity and chest on the treated side (short‐term) Show forest plot | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.52] | ||||||||||||||||||||||||
| Analysis 3.8 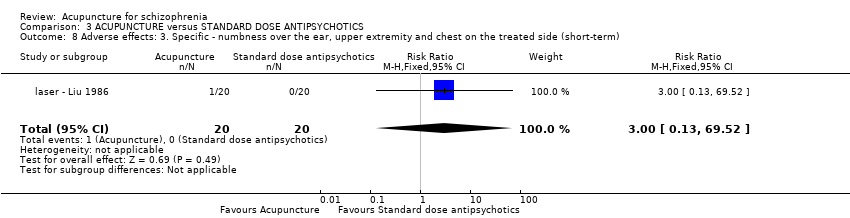 Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 8 Adverse effects: 3. Specific ‐ numbness over the ear, upper extremity and chest on the treated side (short‐term). | ||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint (short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.1  Comparison 4 ACUPUNCTURE added to TCM DRUG versus TCM DRUG, Outcome 1 Global state: Not improved, endpoint (short‐term). | ||||
| 1.1 talk, behaviour and expression still existed as before + reduction of BPRS < 29% | 2 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.02, 0.59] |
| 1.2 no change in symptoms | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.57, 1.06] |
| 2 Behaviour: Leaving the study early (short‐term) Show forest plot | 3 | 454 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 4.2  Comparison 4 ACUPUNCTURE added to TCM DRUG versus TCM DRUG, Outcome 2 Behaviour: Leaving the study early (short‐term). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint (short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.1 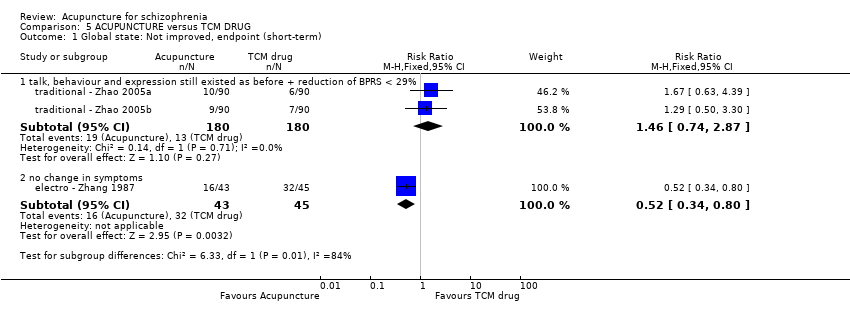 Comparison 5 ACUPUNCTURE versus TCM DRUG, Outcome 1 Global state: Not improved, endpoint (short‐term). | ||||
| 1.1 talk, behaviour and expression still existed as before + reduction of BPRS < 29% | 2 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.74, 2.87] |
| 1.2 no change in symptoms | 1 | 88 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.34, 0.80] |
| 2 Behaviour: Leaving the study early (short‐term) Show forest plot | 3 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 5.2  Comparison 5 ACUPUNCTURE versus TCM DRUG, Outcome 2 Behaviour: Leaving the study early (short‐term). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Behaviour: Leaving the study early (short‐term) Show forest plot | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 6.1  Comparison 6 ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTROCONVULSIVE THERAPY, Outcome 1 Behaviour: Leaving the study early (short‐term). | ||||
| 2 Adverse effects: 1. Specific ‐ back pain (short‐term) Show forest plot | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.74] |
| Analysis 6.2 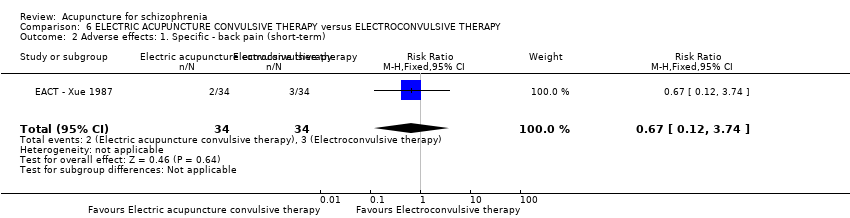 Comparison 6 ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTROCONVULSIVE THERAPY, Outcome 2 Adverse effects: 1. Specific ‐ back pain (short‐term). | ||||
| 3 Adverse effects: 2. Spinal fracture (short‐term) Show forest plot | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.14, 0.81] |
| Analysis 6.3 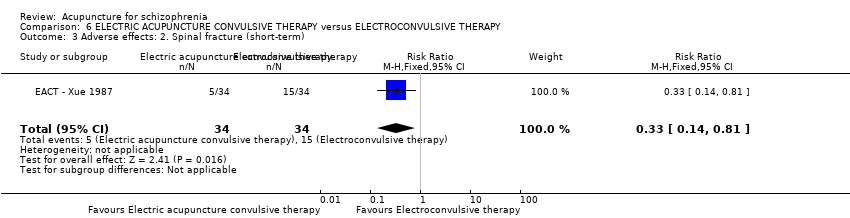 Comparison 6 ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTROCONVULSIVE THERAPY, Outcome 3 Adverse effects: 2. Spinal fracture (short‐term). | ||||

Study flow diagram.
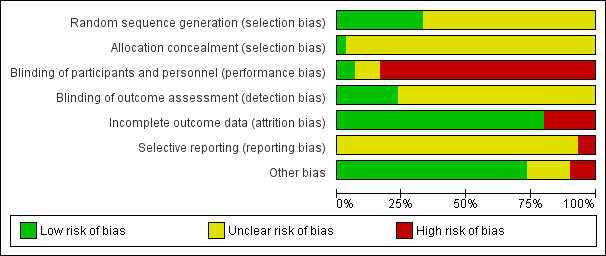
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
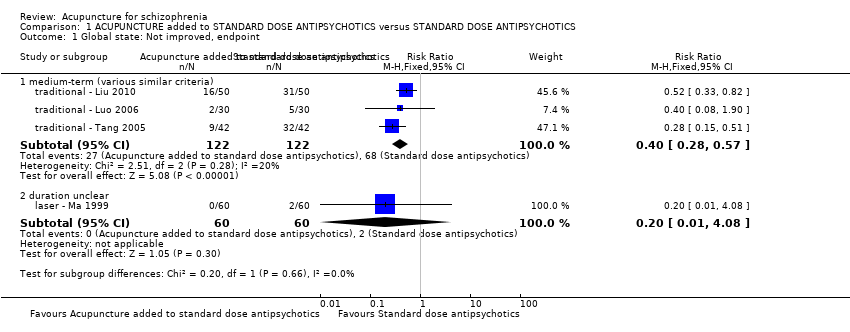
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 1 Global state: Not improved, endpoint.
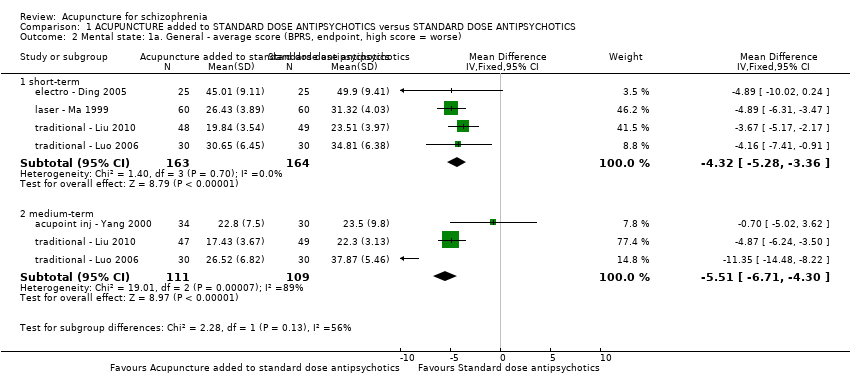
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 2 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 3 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, medium‐term) ‐ subgroup analysis.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 4 Mental state: 2a. General ‐ average score (PANSS, endpoint, high score = worse).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 5 Mental state: 2b. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ subgroup analysis.
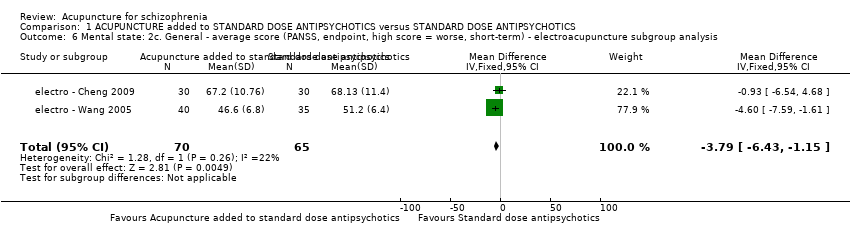
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 6 Mental state: 2c. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ electroacupuncture subgroup analysis.
| Study | Intervention | Mean | SD | N | Note |
| short‐term | |||||
| electro ‐ Chen 2008 | Electroacupuncture added to standard dose antipsychotics | 50.73 | 13.32 | 30 | Compared with the score before treatment P < 0.05 |
| electro ‐ Chen 2008 | Standard dose antipsychotics | 72.30 | 7.01 | 30 | |
| electro ‐ Yao 2006 | Electroacupuncture added to standard dose antipsychotics | 46.51 | 17.10 | 45 | Compared with the score before treatment P < 0.01 |
| electro ‐ Yao 2006 | Standard dose antipsychotics | 46.45 | 17.23 | 45 | Compared with the score before treatment P < 0.01 |
| traditional ‐ Bouhlel 2011 | Traditional acupuncture added to standard dose antipsychotics | 77.40 | 25.73 | 15 | P = 0.501 |
| traditional ‐ Bouhlel 2011 | Standard dose antipsychotics | 77.81 | 26.77 | 16 | |
| medium‐term | |||||
| electro ‐ Chen 2008 | Electroacupuncture added to standard dose antipsychotics | 32.02 | 11.21 | 30 | Compared with the score before treatment P < 0.01 |
| electro ‐ Chen 2008 | Standard dose antipsychotics | 52.10 | 10.32 | 30 | Compared with the score before treatment P < 0.01 |
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 7 Mental state: 2d. General ‐ average score (PANSS, endpoint, high score = worse) ‐ Skewed data.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 8 Mental state: 2e. General ‐ not improved (PANSS), endpoint.
| Study | Intervention | Mean | SD | N | Note |
| electro ‐ Zhang 1993 | Electroacupuncture added to standard dose antipsychotics | 6.71 | 6.15 | 38 | P < 0.01 |
| electro ‐ Zhang 1993 | Standard dose antipsychotics | 10.65 | 6.95 | 31 | |
| traditional ‐ Bouhlel 2011 | Traditional acupuncture added to standard dose antipsychotics | 42.00 | 28.69 | 15 | P = 0.539 |
| traditional ‐ Bouhlel 2011 | Standard dose antipsychotics | 46.75 | 25.05 | 16 | |
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 9 Mental state: 3. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 10 Mental state: 4a.Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse).
| Study | Intervention | Mean | SD | N | Note |
| traditional acupuncture | |||||
| traditional ‐ Bouhlel 2011 | Traditional acupuncture added to standard dose antipsychotics | 55.60 | 24.71 | 15 | P = 0.406 |
| traditional ‐ Bouhlel 2011 | Standard dose antipsychotics | 52.81 | 30.88 | 16 | |
| electroacupuncture | |||||
| electro ‐ Zhang 1993 | Electroacupuncture added to standard dose antipsychotics | 24.97 | 20.86 | 38 | P < 0.005 |
| electro ‐ Zhang 1993 | Standard dose antipsychotics | 37.26 | 16.02 | 31 | |
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 11 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 12 Mental state: 5a. Specific ‐ average score ‐ depression (HAMD, endpoint, high score = worse, short‐term).
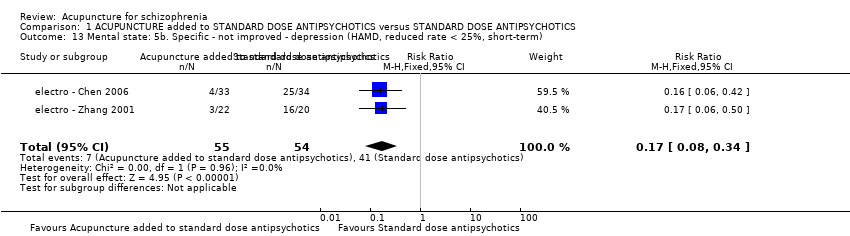
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 13 Mental state: 5b. Specific ‐ not improved ‐ depression (HAMD, reduced rate < 25%, short‐term).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 14 Mental state: 7b. Specific ‐ not improved ‐ auditory hallucinations (PSYRAS‐AH, reduction < 20%, short‐term).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 15 Mental state: 7a. Specific ‐ average score ‐ auditory hallucinations (PSYRAS‐AH,endpoint, high score = worse, short‐term).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 16 Mental state: 6. Specific ‐ average score ‐ depression (SDS, endpoint, high score = worse, short‐term).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 17 Mental state: 8. Specific ‐ not improved (auditory hallucinations, endpoint).
| Study | Intervention | Mean | SD | N | Note |
| short‐term | |||||
| traditional ‐ Liu 2010 | Traditional acupuncture added to standard dose antipsychotics | 9.26 | 5.37 | 48 | P < 0.05 |
| traditional ‐ Liu 2010 | Standard dose antipsychotics | 13.24 | 5.07 | 49 | |
| medium‐term | |||||
| traditional ‐ Liu 2010 | Traditional acupuncture added to standard dose antipsychotics | 5.12 | 3.64 | 47 | P < 0.01 |
| traditional ‐ Liu 2010 | Standard dose antipsychotics | 12.63 | 2.89 | 49 | |
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 18 Mental state: 9. Specific ‐ average score ‐ auditory hallucinations (SAHS, endpoint, high score = worse) ‐ Skewed data.
![Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 19 Mental state: 10. Specific ‐ average score ‐ hallucinations (BPRS [12th item], endpoint, high score = worse, short‐term).](/es/cdsr/doi/10.1002/14651858.CD005475.pub2/media/CDSR/CD005475/image_n/nCD005475-CMP-001-19.png)
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 19 Mental state: 10. Specific ‐ average score ‐ hallucinations (BPRS [12th item], endpoint, high score = worse, short‐term).
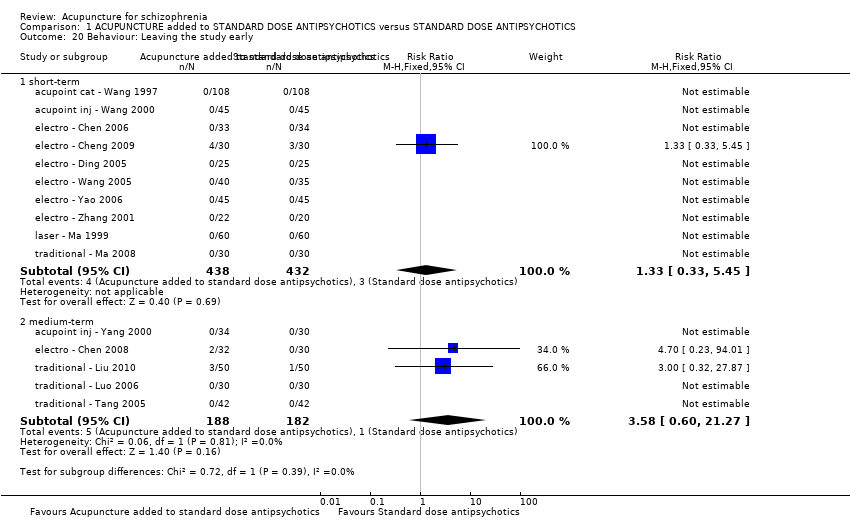
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 20 Behaviour: Leaving the study early.
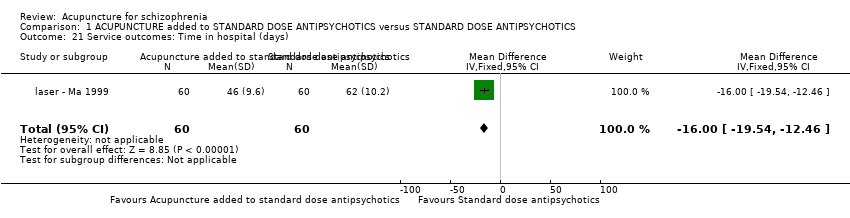
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 21 Service outcomes: Time in hospital (days).
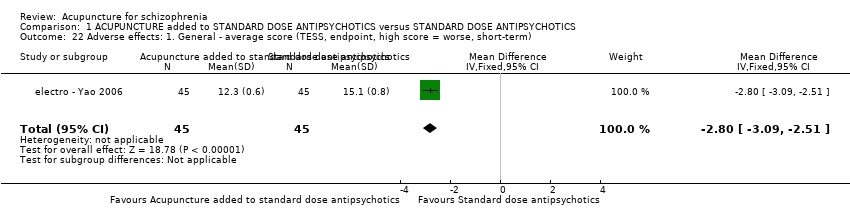
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 22 Adverse effects: 1. General ‐ average score (TESS, endpoint, high score = worse, short‐term).
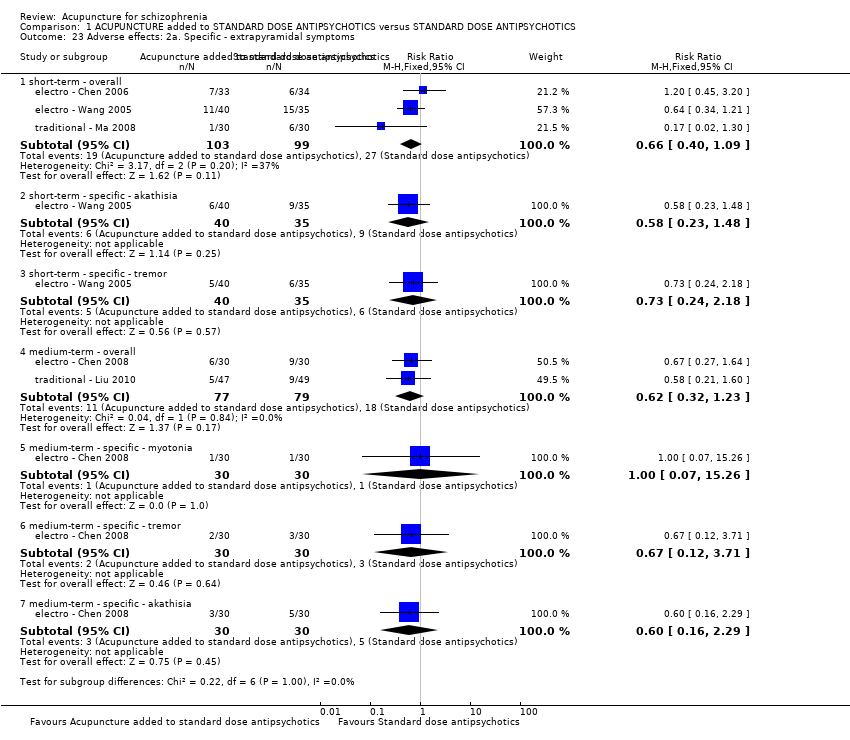
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 23 Adverse effects: 2a. Specific ‐ extrapyramidal symptoms.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 24 Adverse effects: 2b. Specific ‐ extrapyramidal symptoms ‐overall (short‐term) ‐ subgroup analysis.
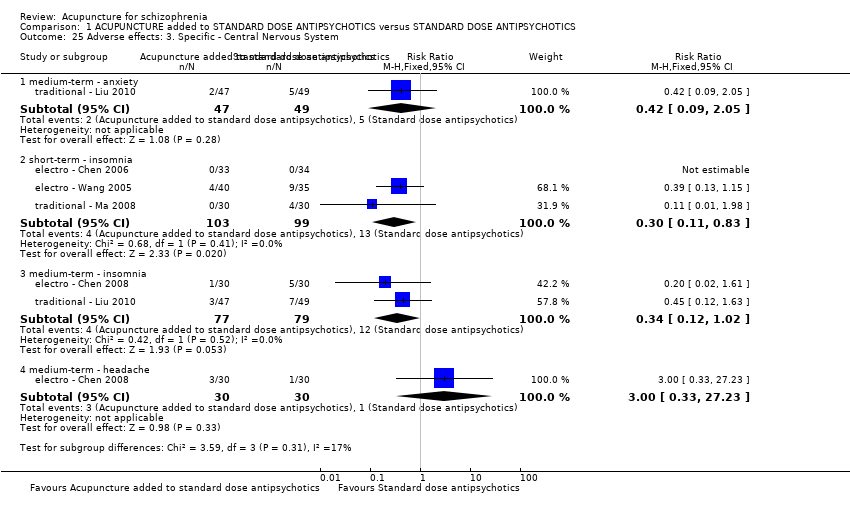
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 25 Adverse effects: 3. Specific ‐ Central Nervous System.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 26 Adverse effects: 4. Specific ‐ anticholinergic symptoms.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 27 Adverse effects: 5. Specific ‐ gastrointestinal system.
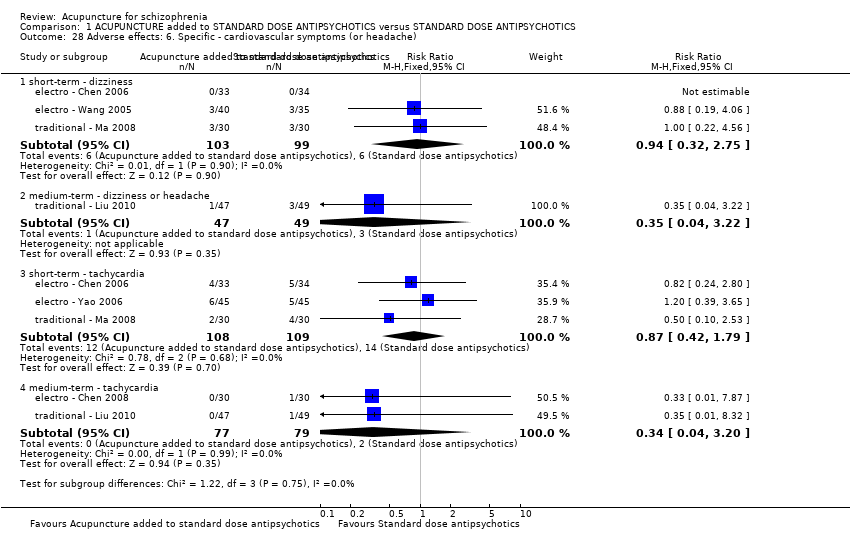
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 28 Adverse effects: 6. Specific ‐ cardiovascular symptoms (or headache).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 29 Adverse effects: 7a. Specific ‐ metabolic system.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 30 Adverse effects: 7b. Specific ‐ metabolic system ‐ weight gain (short‐term) ‐ subgroup analysis.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 31 Adverse effects: 8. Specific ‐ endocrine system.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 32 Adverse effects: 9. Specific ‐ lab test.
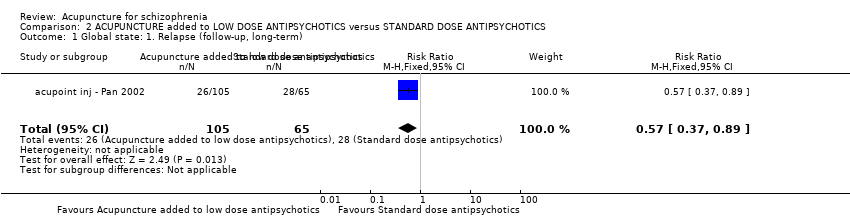
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 1 Global state: 1. Relapse (follow‐up, long‐term).
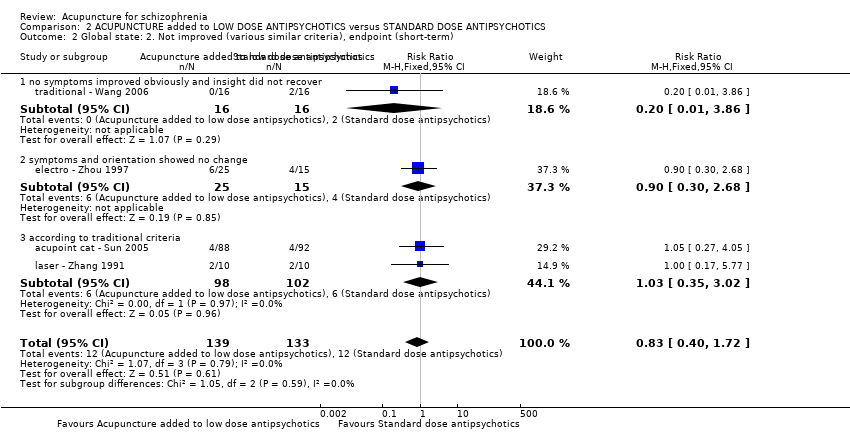
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 2 Global state: 2. Not improved (various similar criteria), endpoint (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 3 Global state: 3a. CGI ‐ average score ‐ CGI‐SI (endpoint, high score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| electro ‐ Zhou 1997 | Electroacupuncture added to low dose antipsychotics | 2.2 | 1.1 | 25 | No significant difference |
| electro ‐ Zhou 1997 | Standard dose antipsychotics | 2.3 | 1.3 | 15 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 4 Global state: 3b. CGI ‐ average score ‐ CGI‐GI (endpoint, high score = worse, short‐term) ‐ Skewed data.
| Study | Intervention | Mean | SD | N | Note |
| electro ‐ Zhou 1997 | Electroacupuncture added to low dose antipsychotics | 2.5 | 1.3 | 25 | P < 0.05 |
| electro ‐ Zhou 1997 | Standard dose antipsychotics | 1.5 | 0.8 | 15 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 5 Global state: 3c. CGI ‐ average score ‐ CGI‐EI (endpoint, high score = worse, short‐term) ‐ Skewed data.
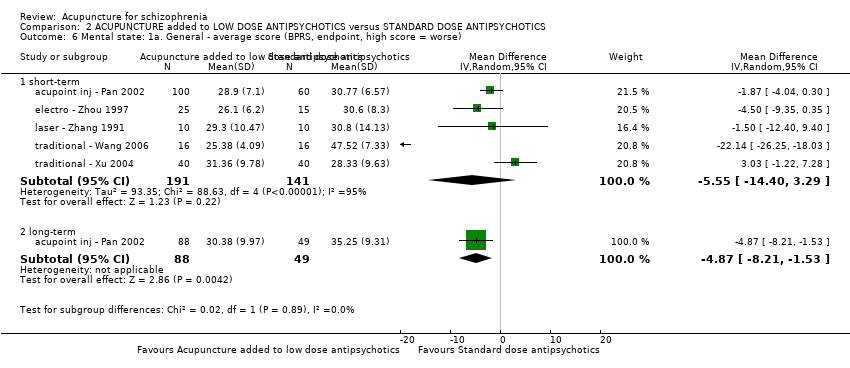
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 6 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse).
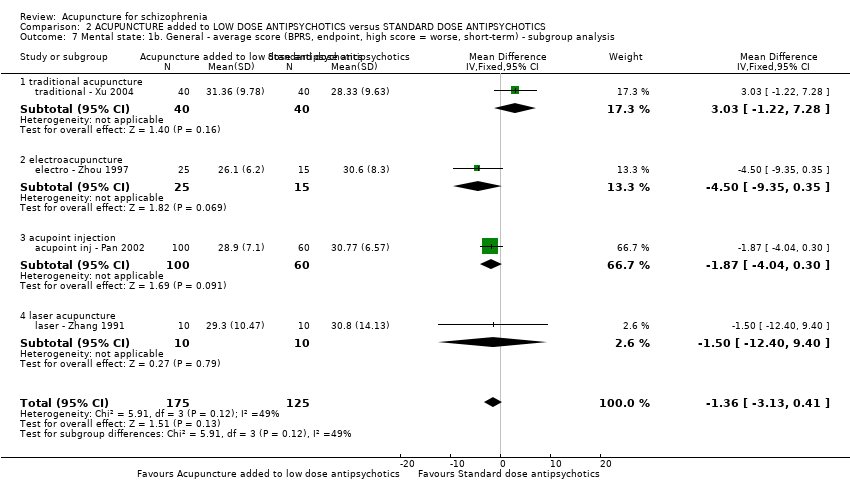
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 7 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, short‐term) ‐ subgroup analysis.
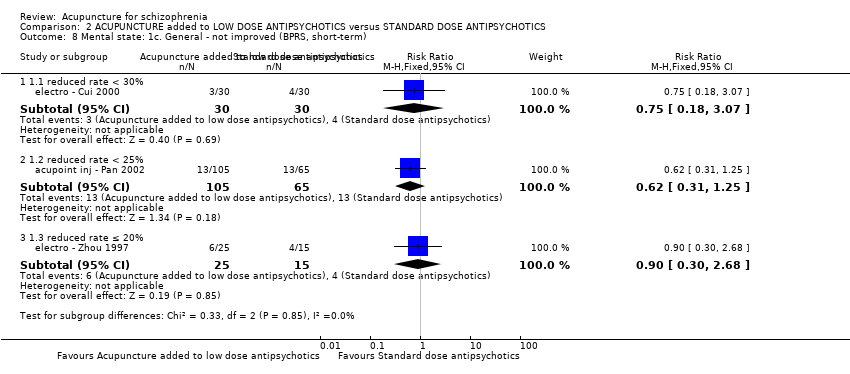
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 8 Mental state: 1c. General ‐ not improved (BPRS, short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 9 Mental state: 1d. General ‐ average change scores (BPRS, low score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| acupoint cat ‐ Sun 2005 | Acupoint catgut treatment added to low dose antipsychotics | 52.85 | 15.86 | 88 | P > 0.05 |
| acupoint cat ‐ Sun 2005 | Standard dose antipsychotics | 49.75 | 12.77 | 92 | |
| electro ‐ Xiong 2010 | Electroacupuncture added to low dose antipsychotics | 46.34 | 11.10 | 40 | Cmpared with score before treatment P < 0.01 |
| electro ‐ Xiong 2010 | Standard dose antipsychotics | 45.21 | 11.36 | 40 | Cmpared with score before treatment P < 0.01 |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 10 Mental state: 2a. General ‐ Average score (PANSS, endpoint, high score = worse, short‐term) ‐ Skew data.
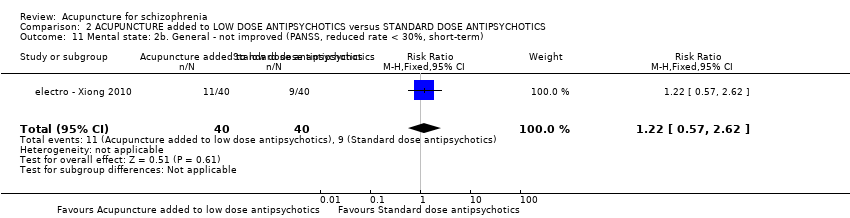
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 11 Mental state: 2b. General ‐ not improved (PANSS, reduced rate < 30%, short‐term).
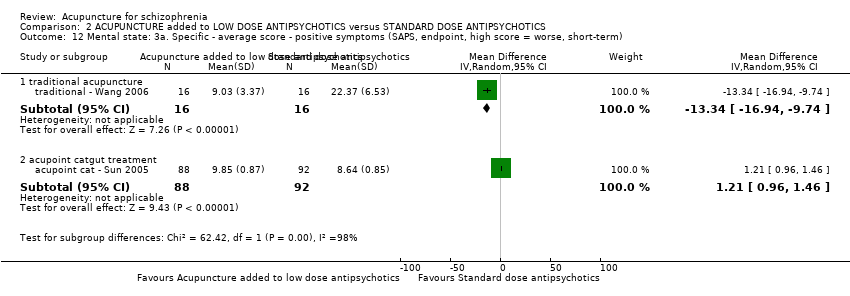
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 12 Mental state: 3a. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| traditional ‐ Xu 2004 | Traditional acupuncture added to low dose antipsychotics | 11.86 | 11.41 | 40 | No significant difference |
| traditional ‐ Xu 2004 | Standard dose antipsychotics | 11.12 | 9.87 | 40 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 13 Mental state: 3b. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data.

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 14 Mental state: 4a. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| traditional ‐ Wang 2006 | Traditional acupuncture added to low dose antipsychotics | 14.23 | 8.68 | 16 | P < 0.01 |
| traditional ‐ Wang 2006 | Standard dose antipsychotics | 30.56 | 13.31 | 16 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 15 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data.
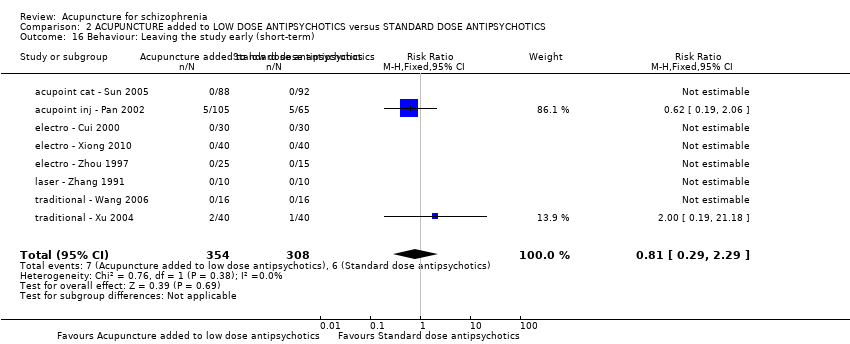
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 16 Behaviour: Leaving the study early (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 17 Adverse effects: 1a. General ‐ average score (TESS, endpoint, high score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| electro ‐ Xiong 2010 | Electroacupuncture added to low dose antipsychotics | 5.08 | 4.56 | 40 | P < 0.01 |
| electro ‐ Xiong 2010 | Standard dose antipsychotics | 10.38 | 6.52 | 40 | |
| traditional ‐ Wang 2006 | Traditional acupuncture added to low dose antipsychotics | 2.57 | 3.28 | 16 | P < 0.01 |
| traditional ‐ Wang 2006 | Standard dose antipsychotics | 6.93 | 5.28 | 16 | |
| traditional ‐ Xu 2004 | Traditional acupuncture added to low dose antipsychotics | 2.65 | 3.47 | 40 | P < 0.01 |
| traditional ‐ Xu 2004 | Standard dose antipsychotics | 10.12 | 8.12 | 40 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 18 Adverse effects: 1b. General ‐ average score (TESS, endpoint, high score = worse, short‐term) ‐ Skewed data.
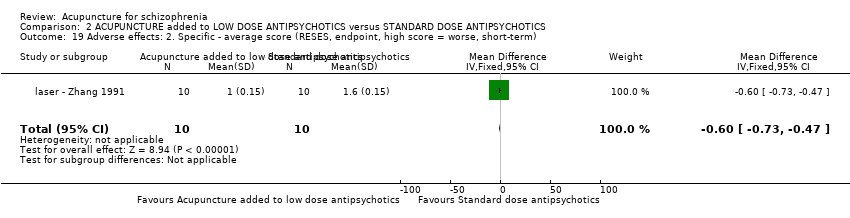
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 19 Adverse effects: 2. Specific ‐ average score (RESES, endpoint, high score = worse, short‐term).
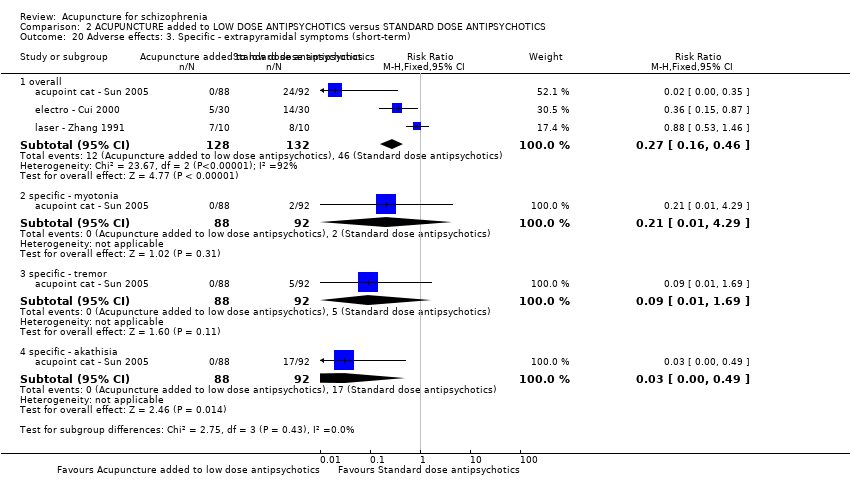
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 20 Adverse effects: 3. Specific ‐ extrapyramidal symptoms (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 21 Adverse effects: 4. Specific ‐ Central Nervous System (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 22 Adverse effects: 5. Specific ‐ anticholinergic symptoms (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 23 Adverse effects: 6. Specific ‐ cardiovascular symptoms (short‐term).
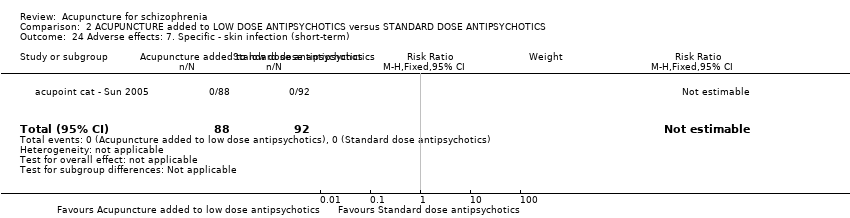
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 24 Adverse effects: 7. Specific ‐ skin infection (short‐term).

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 1 Global state: Not improved, endpoint (short‐term).

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 2 Mental state: 1. General ‐ average score (BPRS, endpoint, high score = worse, short‐term).
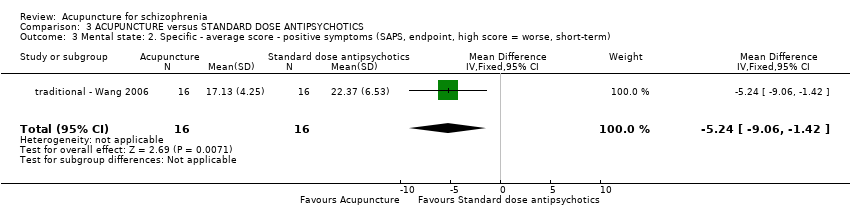
Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 3 Mental state: 2. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term).
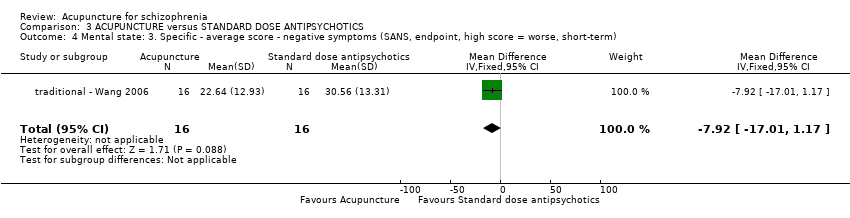
Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 4 Mental state: 3. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term).

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 5 Behaviour: Leaving the study early (short‐term).
| Study | Intervention | Mean | SD | N | Note |
| traditional ‐ Wang 2006 | Traditional acupuncture | 2.43 | 3.17 | 16 | P < 0.01 |
| traditional ‐ Wang 2006 | Antipsychotics | 6.93 | 5.28 | 16 | |
Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 6 Adverse effects: 1. General ‐ average scores (TESS, endpoint, short‐term) ‐ Skewed data.

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 7 Adverse effects: 2. Specific ‐ extrapyramidal symptoms (short‐term).

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 8 Adverse effects: 3. Specific ‐ numbness over the ear, upper extremity and chest on the treated side (short‐term).

Comparison 4 ACUPUNCTURE added to TCM DRUG versus TCM DRUG, Outcome 1 Global state: Not improved, endpoint (short‐term).
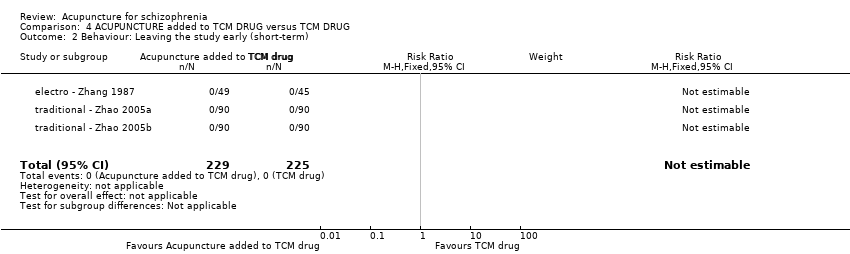
Comparison 4 ACUPUNCTURE added to TCM DRUG versus TCM DRUG, Outcome 2 Behaviour: Leaving the study early (short‐term).
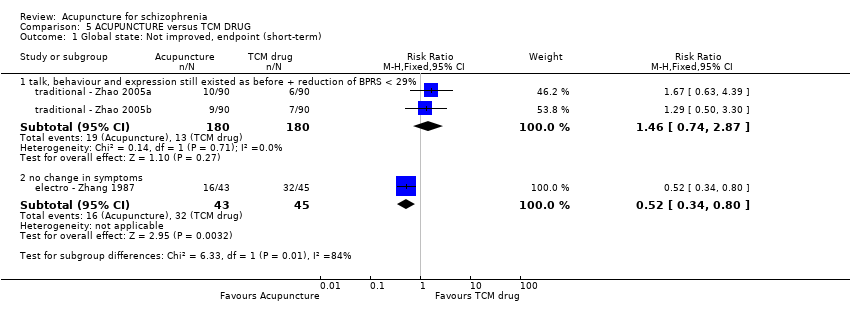
Comparison 5 ACUPUNCTURE versus TCM DRUG, Outcome 1 Global state: Not improved, endpoint (short‐term).

Comparison 5 ACUPUNCTURE versus TCM DRUG, Outcome 2 Behaviour: Leaving the study early (short‐term).

Comparison 6 ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTROCONVULSIVE THERAPY, Outcome 1 Behaviour: Leaving the study early (short‐term).

Comparison 6 ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTROCONVULSIVE THERAPY, Outcome 2 Adverse effects: 1. Specific ‐ back pain (short‐term).

Comparison 6 ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTROCONVULSIVE THERAPY, Outcome 3 Adverse effects: 2. Spinal fracture (short‐term).
| Comparison | Trial |
| Different acupoints | |
| Acupoints vs non‐acupoints |
| Methods | Allocation: randomised, clearly described, concealed. Follow‐up: 2 years. |
| Participants | Diagnosis: schizophrenia (DSM V) with one TCM type according to TCM diagnosis standard. |
| Interventions | 1. Electroacupuncture: N = 150. The acupoints and relative parameters clearly described. |
| Outcomes | 1. Death 2. Global state 3. Mental state 4. Behaviour 5. Service outcomes 6. Adverse effects 7. Engagement with service 8. Satisfaction with treatment 9. Quality of life 10. Economic outcome |
| Notes | * Powered to be able to identify a difference of ˜20% between groups for primary outcome with adequate degree of certainty. ** This is to maximise blinding. |
| ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS | |||||
| Global state: Not improved, endpoint ‐ medium‐term (various similar criteria) | 557 per 1000 | 223 per 1000 | RR 0.4 | 244 | ⊕⊝⊝⊝ | Relapse was not reported but 'no clinically important change in global state' was reported and another outcome without clear duration indicated no difference between two comparison groups. |
| Mental state: PANSS (not improved, reduced rated < 25%, short‐term) | 432 per 1000 | 281 per 1000 | RR 0.65 | 197 | ⊕⊝⊝⊝ | Data from PANSS were equivocal because of different criteria. Other mental state findings were mostly consistent with this finding. |
| Behaviour: Leaving the study early (short‐term) | 7 per 1000 | 9 per 1000 | RR 1.33 | 870 | ⊕⊝⊝⊝ | Similar outcomes at medium‐term. |
| Service outcomes: Time in hospital (days) | The mean service outcomes: time in hospital (days) in the intervention groups was | 120 | ⊕⊕⊕⊝ | 0nly one study reported service outcomes ‐ time in hospital. | ||
| Adverse effects: Central Nervous System ‐ insomnia (short‐term) | 131 per 1000 | 39 per 1000 | RR 0.30 | 202 | ⊕⊕⊝⊝ | Only insomnia rate indicated difference between two compared groups. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'very serious' ‐ Unblinding of participants and personnel and incomplete outcome data. | ||||||
| ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS | |||||
| Global state: Relapse (follow‐up, long‐term) | 431 per 1000 | 246 per 1000 | RR 0.57 | 170 | ⊕⊝⊝⊝ | Only one study reported this outcome. Other global state findings reported no difference between the two comparison groups. |
| Mental state: BPRS (not improved, reduced rate < 30%, short‐term) | 133 per 1000 | 100 per 1000 | RR 0.75 | 60 | ⊕⊝⊝⊝ | Though measured with different criteria of 'no clinically important change in general mental state', there was no difference between the two comparison groups at short‐term and mostly similar results from other mental state findings. |
| Behaviour: Leaving the study early (short‐term) | 19 per 1000 | 16 per 1000 | RR 0.81 | 662 | ⊕⊝⊝⊝ | |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Extrapyramidal symptoms ‐ specific ‐ akathisia (short‐term) | 185 per 1000 | 6 per 1000 | RR 0.03 | 180 | ⊕⊕⊝⊝ | Similar to the akathisia data, acupuncture added to low dose antipsychotics reduced participants experiencing dry mouth, blurred vision, tachycardia at short‐term. Only one study focused on acupoint catgut treatment relative adverse effects but did not find skin infection in either groups. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'very serious' ‐ Unblinding of participants and personnel and incomplete outcome data. | ||||||
| ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE versus ANTIPSYCHOTICS | |||||
| Global state: Not improved (talk, behaviour and expression still existed as before; the reduction of BPRS < 29%), endpoint (short‐term) | 317 per 1000 | 104 per 1000 | RR 0.33 | 240 | ⊕⊝⊝⊝ | Relapse was not reported but 'no clinically important change in global state' was reported and another three outcomes with different but similar criteria indicated no difference between the two comparison groups in the short‐term. |
| Mental state: BPRS, endpoint (high score = worse, short‐term) ‐ traditional acupuncture | The mean mental state: BPRS, endpoint (high score = worse, short‐term) ‐ traditional acupuncture in the intervention groups was | 32 | ⊕⊝⊝⊝ | The outcome of 'no clinically important change in general mental state' was not reported but average endpoint BPRS data were reported as was the SAPS score. There was no difference between the two comparison groups in the short‐term using either score. | ||
| Behaviour: Leaving the study early (short‐term) | See comment | See comment | Not estimable | 421 | ⊕⊕⊝⊝ | No participants left each compared group early. |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Extrapyramidal symptoms (short‐term) | 800 per 1000 | 40 per 1000 | RR 0.05 | 21 | ⊕⊕⊝⊝ | One study reported laser acupuncture relative adverse effects ‐ numbness over ear, upper extremity and chest on the treated side, but no difference between the two comparison groups. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'serious' ‐ Unblinding of participants and personnel. | ||||||
| ACUPUNCTURE plus TCM DRUG versus TCM DRUG for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE added to TCM DRUG versus TCM DRUG | |||||
| Global state: Not improved (talk, behaviour and expression still existed as before, the reduction of BPRS < 29%), endpoint (short‐term) | 72 per 1000 | 8 per 1000 | RR 0.11 | 360 | ⊕⊕⊝⊝ | Relapse was not reported but 'no clinically important change in global state' was reported and the other outcome with different criteria of 'no clinically important change in global state' indicated no difference between the two comparison groups in the short‐term. |
| Mental state: No clinically important change in mental state | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Behaviour: Leaving the study early (short‐term) | See comment | See comment | Not estimable | 454 | ⊕⊕⊝⊝ | No participants left either group early. |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Clinically important general adverse effects | See comment | See comment | Not estimable | 0 | See comment | Three studies reported this outcome, however, two studies only reported one group's data and the other one study did not report the data. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'serious' ‐ Unblinding of participants and personnel. | ||||||
| ACUPUNCTURE versus TCM DRUG for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE versus TCM DRUG | |||||
| Global state: Not improved, endpoint (short‐term) ‐ Not improved (no change in symptoms) ‐ Electroacupuncture | 711 per 1000 | 370 per 1000 | RR 0.52 | 88 | ⊕⊕⊝⊝ | Relapse was not reported but 'no clinically important change in global state' was reported and other outcomes with different criteria of 'no clinically important change in global state' indicated no difference between the two comparison groups in the short‐term. |
| Mental state: No clinically important change in general mental state | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Behaviour: Leaving the study early (short‐term) | See comment | See comment | Not estimable | 328 | See comment | No participants left either group early. |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Clinically important general adverse effects | See comment | See comment | Not estimable | ‐ | See comment | Three studies reported this outcome, however, two studies only reported one group's data and the other one study did not report the data. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'serious' ‐‐ Unblinding of participants and personnel. | ||||||
| ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTRIC CONVULSIVE THERAPY for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTRIC CONVULSIVE THERAPY | |||||
| Global state: Relapse | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Mental state: No clinically important change in general mental state | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Behaviour: Leaving the study early (short‐term) | See comment | See comment | Not estimable | 68 | ⊕⊕⊝⊝ | No participants in either group left early. |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Spinal fracture (short‐term) | 441 per 1000 | 146 per 1000 | RR 0.33 | 68 | ⊕⊕⊝⊝ | Data from a single study where there was no difference in back pain between the two groups. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias; rated 'serious' ‐ Unblinding of participants and personnel. | ||||||
| Global state: Adding medication | |||
| Study | Drug | Events/Acupuncture group (n/N) | Events/Control group (n/N) |
| Artane | 6/30 | 11/30 | |
| Promethazine | 3/30 | 6/30 | |
| Propranolol | 2/30 | 4/30 | |
| Chlorpheniramine | 0/30 | 1/30 | |
| Propranolol | 7/40 | 7/35 | |
| Artane | 6/40 | 9/35 | |
| Benzodiazepine drugs | 4/40 | 7/35 | |
| Mental state: Time to auditory hallucinations disappeared (days) | |||
| Study | Intervention | Mean | SD |
| Laser acupuncture added to standard dose antipsychotics | 19 | 4.1 | |
| Standard dose antipsychotics | 31 | 4.4 | |
| Intervention | Term | Adverse effects | Adverse effects/Intervention group (n/N) | Study | |
| Traditional acupuncture | |||||
| Traditional acupuncture added to standard dose antipsychotics versus standard dose antipsychotics | Short term | Extrapyramidal symptoms | Overall | 1/30 | |
| Anticholinergic symptoms | Dry mouth | 3/30 | |||
| Cardiovascular | Dizziness | 3/30 | |||
| Tachycardia | 2/30 | ||||
| Medium term | Extrapyramidal symptoms | Overall | 5/47 | ||
| Central Nervous System | Anxiety | 2/47 | |||
| Insomnia | 3/47 | ||||
| Cardiovascular symptoms (or headache) | Dizziness or headache | 1/47 | |||
| Gastrointestinal system | Unspecifid gastrointestinal symptoms | 2/47 | |||
| Lab test | Liver function abnormal | 2/47 | |||
| Electroacupuncture | |||||
| Electroacupuncture (or added to TCM drug) versus TCM drug | Short term | Hold breath, facial cyanosis, arrhythmia, transient increase of blood pressure, injury of teeth, tongue and lips, epileptic attacks with strong stimulation | not reported | ||
| Electroacupuncture added to standard dose antipsychotics versus standard dose antipsychotics | Short term | Extrapyramidal symptoms | Overall | 18/73 | |
| Tremor | 5/40 | ||||
| Akathisia | 6/40 | ||||
| Central Nervous System | Insomnia | 4/73 | |||
| Anticholinergic symptoms | Dry mouth | 6/73 | |||
| Blurred vision | 4/73 | ||||
| Constipation | 3/73 | ||||
| Nausea and vomiting | 3/73 | ||||
| Cardiovascular symptoms | Dizziness | 3/73 | |||
| Tachycardia | 10/78 | ||||
| Metabolic system | Weight gain | 3/73 | |||
| Lab test | Liver function abnormal | 4/118 | electro ‐ Chen 2006; electro ‐ Wang 2005; electro ‐ Yao 2006 | ||
| ECG abnormal (myocardial ischaemia) | 1/118 | ||||
| blood routine test abnormal (leukocyte change) | 4/118 | ||||
| Medium term | Extrapyramidal symptoms | Overall | 6/30 | ||
| Myotonia | 1/30 | ||||
| Tremor | 2/30 | ||||
| Akathisia | 3/30 | ||||
| Central Nervous System | Insomnia | 1/30 | |||
| Headache | 2/30 | ||||
| Anticholinergic symptoms | Blurred vision | 1/30 | |||
| Sweating | 3/30 | ||||
| Electroacupuncture added low dose antipsychotics versus standard dose antipsychotics | Short term | Extrapyramidal symptoms | Overall | 5/30 | |
| Central Nervous System | Sleepiness | 1/30 | |||
| Anticholinergic symptoms | Dry mouth | 4/30 | |||
| Blurred vision | 2/30 | ||||
| Cardiovascular symptoms | Tachycardia | 5/30 | |||
| Laser acupuncture | |||||
| Laser acupuncture versus standard dose antipsychotics | Short term | Numbness over the ear, upper extremity and chest on the treated side | 1/20 | ||
| Sensation of heat at irradiated site and a feeling of plugged auditory canal | one third of participants of He‐Ne laser irradiation group | ||||
| Laser acupuncture added to low dose antipsychotics versus standard dose antipsychotics | Short term | Extrapyramidal symptoms | Overall | 7/10 | |
| Acupoint catgut treatment | |||||
| Acupoint catgut treatment added to standard dose antipsychotics versus standard dose antipsychotics | Short term | Local pain when eating | not reported | ||
| Acupoint catgut treatment added to low dose antipsychotics versus standard dose antipsychotics | Short term | Cardiovascular symptoms | Dizziness | 2/88 | |
| Tachycardia | 2/88 | ||||
| Electric acupuncture convulsive therapy | |||||
| Electric acupuncture convulsive therapy versus electroconvulsive therapy | Short term | Back pain | 2/34 | ||
| Spinal fracture | 5/34 | ||||
| Study | Kind of acupuncture | Acupoints choice | Fequency and duration | Sham acupuncture (yes/no) |
| Traditional acupuncture | Local points, distal points diagnosed by TCM | Once for 20 minutes and 3 times a week; total 10 times | Yes | |
| Main acupoints and adjunct acupoints according to the TCM syndrome differentiation | Manipulated needles every 10 minutes; for 30 minutes; 4 to 5 times a week and no less than 4 times; 1 month as 1 treatment course, 3 treatment course | No | ||
| Two acupoint groups in turn | For 30 minutes; once a day; 20 days as a treatment course and began another treatment course after 10 non‐treatment days; 3 months treatment courses | No | ||
| Juque, Tanzhong, Taichong, Jianshi, Fenglong, Daling, Yingtang | For 30 minutes; once a day; 5 days treatment with 2 days non‐treatment interval; 6 weeks | No | ||
| According to the type of TCM | Manipulated needles every 10 minutes; for 30 minutes; 3 to 4 times a week and not less than 3 times; 3 weeks as a treatment course and 1 week interval; total 3 treatment courses | No | ||
| Taichong (reducing method), Hegu (reducing method), Neiguan (straight inserted), Daling (straight inserted), Renzhong (reducing method), Dazhui (straight inserted) + other acupoints choice according to type of TCM | Continued to manipulate needles 3 to 5 minutes every ten minutes; for 45 minutes; once a day; 15 times as a treatment course; 2 treatment courses | No | ||
| Main acupoints and adjunct acupoints (according to the TCM type of schizophrenia) and special acupoints (according to symptoms) | Manipulated needles about 3 minutes and once ten minutes; total for about 30 minutes; at first once a day then reduced to once every two days when patient was in stable condition and once a week after psychiatric symptoms disappeared; 80 days | No | ||
| Shuigou, Shaoshang, Yingbai, Fengfu, Daling, Quchi, Fenglong | Once a day; for 30 minutes; 60 days | No | ||
| Xinshu, Ganshu, Pishu, Shenmen, Fenglong | Once a day; for 30 minutes; 60 days | No | ||
| Electroacupuncture | Baihui and Yingtang | For 50 minutes, once a day, 6 weeks | No | |
| Two acupoints groups in turn ‐ Baihui and Neiguan (double) group or Shuigou and Sanyingjiao (double) group | For 45 minutes; once a day; five days a week (except Saterday and Sunday); 12 weeks as a treatment course | No | ||
| Tinggong, Tinghui, Yifeng, Daling, Neiguan and Sanyijiao | For 20 minutes; 5 times a week; total 30 times (6 weeks) | Yes; needles were inserted less than 5 mm superficially and about 20 mm away from each corresponding acupoint and electroacupuncture connected was with no electrical current for 20 minutes | ||
| According to different symptoms | For 30 minutes; once two days; 20 times as a treatment course | No | ||
| Tanzhong, Zhongwan, Shenmen, Fenglong (double), Taichong (double), Neiguan (double) | For 5 minutes; once two days | No | ||
| Baihui, Shangxing, Yingtang, Sanyingjiao (double), Neiguan (double); added Zhongwan and Zusanli when with gastrointestinal uncomfortable symptoms and added Fenglong when with symptoms of the type of stagnation of phlegm and Qi | For 45 minutes; 5 times a week; 20 times as a treatment course; 8 weeks | No | ||
| Baihui and Taiyang (double) | Firstly continued to stimulate strongly 3 to 4 seconds then reduced the strength and frequency quickly, after patient's breath and face returned to normal and continued 30 to 60 seconds stimulated again; continued to stimulate 8 to 10 times; 3 times a week, total 8 weeks | No | ||
| Baihui, Fenglong, Houxi, Ganshu | For 30 minutes; once a day; 20 to 30 times as a treatment course; total 2 treatment courses | No | ||
| Yifeng, Tinggong, Tounjie, Chengling, Linqi, Baihui, Dingshen | Twice a day; adjustment of treatment depended upon the condition of the patient; 20 days | No | ||
| Group one [Yingtang and Baihui] and group two [Shenting and Yamen] | For 45 minutes; once a day; 8 weeks as a treatment course | No | ||
| Baihui and Yingtang | For 45 minutes; once a day; 5 days a week except Saturday and Sunday; 6 weeks as a treatment course | No | ||
| According to TCM types; main acupoints (Yintang tou xinqu, Daling, Neiguan, Taiyang) and supplemental acupoints (Zusanli [Yang deficiency] | Once a day except Sunday; 36 times as a treatment course (6 weeks) | No | ||
| Acupoint injection | According to the type of TCM (with Salviae Miltiorrhizae) | Two side acupoints in turn; once a day; 10 days as a treatment course; 7 days interval between two courses; 3 treatment courses | No | |
| Tinggong (double) (with Clonazepam) | Once two days; 7 times | No | ||
| Tinggong (double) (Sulpiride) | Once a day; 5 times as a treatment course; 2 intermittent treatment courses each month; total half a year | No | ||
| Laser acupuncture | Ermen (double) (He‐Ne laser irradiation) | For 15 minutes; once a day except Sunday; 30 times as a treatment course | Yes; sham laser irradiation; the tube of the laser emitter pointed in the direction of the ear without real irradiation | |
| Tinggong and Tinghui (He‐Ne laser irradiation) | For 30 minutes; once a day except Sunday | No | ||
| Two acupoint groups were used every other day alternately ‐ group 1 (Dazhui and Shenting); group 2 (Taiyang [double]) | For 15 minutes; once a day (except Sunday); 5 weeks as a treatment course | Yes; needles fixed with tape on acupoints | ||
| Acupoint catgut treatment | Tinggong | Once 7‐10 days; 6 weeks as a treatment course | No | |
| Tinggong (double) | 10 days as a treatment course; total 3 treatment courses | No | ||
| Electric acupuncture convulsive therapy | Renzhong and Baihui | Once every two days; 12 times as a treatment course | No |
| Comparison | Missing outcomes |
| ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS | Death, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS | Death, service outcomes, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ACUPUNCTURE versus STANDARD ANTIPSYCHOTICS | Death, service outcomes, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ACUPUNCTURE added to TCM DRUG versus TCM DRUG | Death, mental state, service outcomes, adverse effects, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ACUPUNCURE versus TCM DRUG | Death, mental state, service outcomes, adverse effects, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ELECTRIC ACUPUCNTURE CONVULSIVE THERAPY versus ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY | Death, global state, mental state, service outcomes, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 medium‐term (various similar criteria) | 3 | 244 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.28, 0.57] |
| 1.2 duration unclear | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.08] |
| 2 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse) Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 short‐term | 4 | 327 | Mean Difference (IV, Fixed, 95% CI) | ‐4.32 [‐5.28, ‐3.36] |
| 2.2 medium‐term | 3 | 220 | Mean Difference (IV, Fixed, 95% CI) | ‐5.51 [‐6.71, ‐4.30] |
| 3 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, medium‐term) ‐ subgroup analysis Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 traditional acupuncture | 2 | 156 | Mean Difference (IV, Random, 95% CI) | ‐7.95 [‐14.29, ‐1.61] |
| 3.2 acupoint injection | 1 | 64 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐5.02, 3.62] |
| 4 Mental state: 2a. General ‐ average score (PANSS, endpoint, high score = worse) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 short‐term | 4 | 245 | Mean Difference (IV, Fixed, 95% CI) | ‐2.47 [‐4.31, ‐0.63] |
| 4.2 medium‐term | 2 | 135 | Mean Difference (IV, Fixed, 95% CI) | ‐3.79 [‐6.43, ‐1.15] |
| 5 Mental state: 2b. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ subgroup analysis Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 traditional acupuncture | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 1.30 [‐1.56, 4.16] |
| 5.2 electroacupuncture | 3 | 185 | Mean Difference (IV, Random, 95% CI) | ‐5.64 [‐10.93, ‐0.35] |
| 6 Mental state: 2c. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ electroacupuncture subgroup analysis Show forest plot | 2 | 135 | Mean Difference (IV, Fixed, 95% CI) | ‐3.79 [‐6.43, ‐1.15] |
| 7 Mental state: 2d. General ‐ average score (PANSS, endpoint, high score = worse) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 7.1 short‐term | Other data | No numeric data | ||
| 7.2 medium‐term | Other data | No numeric data | ||
| 8 Mental state: 2e. General ‐ not improved (PANSS), endpoint Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 reduced rate < 25%, short‐term | 3 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.45, 0.94] |
| 8.2 reduced rate < 30%, short‐term | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.43, 1.92] |
| 8.3 reduced rate < 30%, follow‐up, medium‐term | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.36, 1.31] |
| 9 Mental state: 3. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 10 Mental state: 4a.Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 short‐term | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐7.66 [‐13.05, ‐2.27] |
| 10.2 medium‐term | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐12.35 [‐17.54, ‐7.16] |
| 11 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 11.1 traditional acupuncture | Other data | No numeric data | ||
| 11.2 electroacupuncture | Other data | No numeric data | ||
| 12 Mental state: 5a. Specific ‐ average score ‐ depression (HAMD, endpoint, high score = worse, short‐term) Show forest plot | 2 | 109 | Mean Difference (IV, Random, 95% CI) | ‐8.66 [‐12.10, ‐5.22] |
| 13 Mental state: 5b. Specific ‐ not improved ‐ depression (HAMD, reduced rate < 25%, short‐term) Show forest plot | 2 | 109 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.08, 0.34] |
| 14 Mental state: 7b. Specific ‐ not improved ‐ auditory hallucinations (PSYRAS‐AH, reduction < 20%, short‐term) Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.14, 0.52] |
| 15 Mental state: 7a. Specific ‐ average score ‐ auditory hallucinations (PSYRAS‐AH,endpoint, high score = worse, short‐term) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.17 [‐4.16, ‐0.18] |
| 16 Mental state: 6. Specific ‐ average score ‐ depression (SDS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | ‐24.25 [‐28.01, ‐20.49] |
| 17 Mental state: 8. Specific ‐ not improved (auditory hallucinations, endpoint) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 still existed after 30 days, short‐term | 1 | 216 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.13, 0.44] |
| 17.2 still existed or appeared frequently after disappeared, medium‐term | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.17, 0.61] |
| 17.3 no change of auditory hallucinations, duration unclear | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.17] |
| 18 Mental state: 9. Specific ‐ average score ‐ auditory hallucinations (SAHS, endpoint, high score = worse) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 18.1 short‐term | Other data | No numeric data | ||
| 18.2 medium‐term | Other data | No numeric data | ||
| 19 Mental state: 10. Specific ‐ average score ‐ hallucinations (BPRS [12th item], endpoint, high score = worse, short‐term) Show forest plot | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.73 [‐1.28, ‐0.18] |
| 20 Behaviour: Leaving the study early Show forest plot | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 short‐term | 10 | 870 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.33, 5.45] |
| 20.2 medium‐term | 5 | 370 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.58 [0.60, 21.27] |
| 21 Service outcomes: Time in hospital (days) Show forest plot | 1 | 120 | Mean Difference (IV, Fixed, 95% CI) | ‐16.0 [‐19.54, ‐12.46] |
| 22 Adverse effects: 1. General ‐ average score (TESS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐2.80 [‐3.09, ‐2.51] |
| 23 Adverse effects: 2a. Specific ‐ extrapyramidal symptoms Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 23.1 short‐term ‐ overall | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.40, 1.09] |
| 23.2 short‐term ‐ specific ‐ akathisia | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.23, 1.48] |
| 23.3 short‐term ‐ specific ‐ tremor | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.24, 2.18] |
| 23.4 medium‐term ‐ overall | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.32, 1.23] |
| 23.5 medium‐term ‐ specific ‐ myotonia | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 15.26] |
| 23.6 medium‐term ‐ specific ‐ tremor | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.71] |
| 23.7 medium‐term ‐ specific ‐ akathisia | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.16, 2.29] |
| 24 Adverse effects: 2b. Specific ‐ extrapyramidal symptoms ‐overall (short‐term) ‐ subgroup analysis Show forest plot | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.40, 1.09] |
| 24.1 traditional acupuncture | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.02, 1.30] |
| 24.2 electroacupuncture | 2 | 142 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.47, 1.34] |
| 25 Adverse effects: 3. Specific ‐ Central Nervous System Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 25.1 medium‐term ‐ anxiety | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.09, 2.05] |
| 25.2 short‐term ‐ insomnia | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.11, 0.83] |
| 25.3 medium‐term ‐ insomnia | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.12, 1.02] |
| 25.4 medium‐term ‐ headache | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.33, 27.23] |
| 26 Adverse effects: 4. Specific ‐ anticholinergic symptoms Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 26.1 short‐term ‐ dry mouth | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.47, 3.00] |
| 26.2 short‐term ‐ blurred vision | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.24, 3.24] |
| 26.3 medium‐term ‐ blurred vision | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.64] |
| 26.4 medium‐term ‐ sweating | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.83] |
| 26.5 short‐term ‐ constipation | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.19, 4.06] |
| 26.6 short‐term ‐ nausea & vomiting | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.12, 1.32] |
| 27 Adverse effects: 5. Specific ‐ gastrointestinal system Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 27.1 medium‐term ‐ unspecified gastrointestinal symptoms | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.10, 2.71] |
| 27.2 short‐term ‐ constipation | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.19, 4.06] |
| 27.3 short‐term ‐ nausea & vomiting | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.12, 1.32] |
| 28 Adverse effects: 6. Specific ‐ cardiovascular symptoms (or headache) Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 28.1 short‐term ‐ dizziness | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.32, 2.75] |
| 28.2 medium‐term ‐ dizziness or headache | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.04, 3.22] |
| 28.3 short‐term ‐ tachycardia | 3 | 217 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.42, 1.79] |
| 28.4 medium‐term ‐ tachycardia | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.04, 3.20] |
| 29 Adverse effects: 7a. Specific ‐ metabolic system Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 29.1 short‐term ‐ weight gain | 3 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.02, 37.33] |
| 29.2 medium‐term ‐ weight gain | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.01, 4.23] |
| 30 Adverse effects: 7b. Specific ‐ metabolic system ‐ weight gain (short‐term) ‐ subgroup analysis Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 30.1 traditional acupuncture | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.65] |
| 30.2 electroacupuncture | 2 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 6.15 [0.33, 115.01] |
| 31 Adverse effects: 8. Specific ‐ endocrine system Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 31.1 short‐term ‐ irregular menstruation | 2 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.87] |
| 32 Adverse effects: 9. Specific ‐ lab test Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 32.1 short‐term ‐ liver function abnormal | 4 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.26, 3.90] |
| 32.2 medium‐term ‐ liver function abnormal | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.12, 3.98] |
| 32.3 short‐term ‐ ECG abnormal (myocardial ischaemia) | 4 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.05, 5.32] |
| 32.4 short‐term ‐ blood routine test abnormal (leukocyte change) | 4 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.32, 5.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: 1. Relapse (follow‐up, long‐term) Show forest plot | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.37, 0.89] |
| 2 Global state: 2. Not improved (various similar criteria), endpoint (short‐term) Show forest plot | 4 | 272 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.40, 1.72] |
| 2.1 no symptoms improved obviously and insight did not recover | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.86] |
| 2.2 symptoms and orientation showed no change | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.9 [0.30, 2.68] |
| 2.3 according to traditional criteria | 2 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.35, 3.02] |
| 3 Global state: 3a. CGI ‐ average score ‐ CGI‐SI (endpoint, high score = worse, short‐term) Show forest plot | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐1.08, 0.28] |
| 4 Global state: 3b. CGI ‐ average score ‐ CGI‐GI (endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 5 Global state: 3c. CGI ‐ average score ‐ CGI‐EI (endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 6 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse) Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 short‐term | 5 | 332 | Mean Difference (IV, Random, 95% CI) | ‐5.55 [‐14.40, 3.29] |
| 6.2 long‐term | 1 | 137 | Mean Difference (IV, Random, 95% CI) | ‐4.87 [‐8.21, ‐1.53] |
| 7 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, short‐term) ‐ subgroup analysis Show forest plot | 4 | 300 | Mean Difference (IV, Fixed, 95% CI) | ‐1.36 [‐3.13, 0.41] |
| 7.1 traditional acupuncture | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 3.03 [‐1.22, 7.28] |
| 7.2 electroacupuncture | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐4.5 [‐9.35, 0.35] |
| 7.3 acupoint injection | 1 | 160 | Mean Difference (IV, Fixed, 95% CI) | ‐1.87 [‐4.04, 0.30] |
| 7.4 laser acupuncture | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐12.40, 9.40] |
| 8 Mental state: 1c. General ‐ not improved (BPRS, short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 1.1 reduced rate < 30% | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.07] |
| 8.2 1.2 reduced rate < 25% | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.31, 1.25] |
| 8.3 1.3 reduced rate ≤ 20% | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.9 [0.30, 2.68] |
| 9 Mental state: 1d. General ‐ average change scores (BPRS, low score = worse, short‐term) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.81 [‐3.17, 4.79] |
| 10 Mental state: 2a. General ‐ Average score (PANSS, endpoint, high score = worse, short‐term) ‐ Skew data Show forest plot | Other data | No numeric data | ||
| 11 Mental state: 2b. General ‐ not improved (PANSS, reduced rate < 30%, short‐term) Show forest plot | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.57, 2.62] |
| 12 Mental state: 3a. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 traditional acupuncture | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐13.34 [‐16.94, ‐9.74] |
| 12.2 acupoint catgut treatment | 1 | 180 | Mean Difference (IV, Random, 95% CI) | 1.21 [0.96, 1.46] |
| 13 Mental state: 3b. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 14 Mental state: 4a. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 0.61 [‐3.30, 4.52] |
| 15 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 16 Behaviour: Leaving the study early (short‐term) Show forest plot | 8 | 662 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.29, 2.29] |
| 17 Adverse effects: 1a. General ‐ average score (TESS, endpoint, high score = worse, short‐term) Show forest plot | 2 | 200 | Mean Difference (IV, Fixed, 95% CI) | ‐0.56 [‐0.86, ‐0.26] |
| 18 Adverse effects: 1b. General ‐ average score (TESS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 19 Adverse effects: 2. Specific ‐ average score (RESES, endpoint, high score = worse, short‐term) Show forest plot | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐0.6 [‐0.73, ‐0.47] |
| 20 Adverse effects: 3. Specific ‐ extrapyramidal symptoms (short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 overall | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.16, 0.46] |
| 20.2 specific ‐ myotonia | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.29] |
| 20.3 specific ‐ tremor | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.69] |
| 20.4 specific ‐ akathisia | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.49] |
| 21 Adverse effects: 4. Specific ‐ Central Nervous System (short‐term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 21.1 activity increasing | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.85] |
| 21.2 insomnia | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.00, 1.20] |
| 21.3 sleepiness | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.03] |
| 22 Adverse effects: 5. Specific ‐ anticholinergic symptoms (short‐term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 22.1 dry mouth | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.09, 0.58] |
| 22.2 nasal congestion | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.69] |
| 22.3 blurred vision | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.06, 0.83] |
| 22.4 constipation | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.00, 1.20] |
| 23 Adverse effects: 6. Specific ‐ cardiovascular symptoms (short‐term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 23.1 dizziness | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.12, 4.07] |
| 23.2 tachycardia | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.11, 0.53] |
| 24 Adverse effects: 7. Specific ‐ skin infection (short‐term) Show forest plot | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint (short‐term) Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 various similar criteria | 3 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.53, 1.48] |
| 1.2 talk, behaviour and expression still existed as before + reduction of BPRS < 29% | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.19, 0.59] |
| 2 Mental state: 1. General ‐ average score (BPRS, endpoint, high score = worse, short‐term) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 traditional acupuncture | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐11.56 [‐16.36, ‐6.76] |
| 2.2 laser acupuncture | 1 | 21 | Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐11.19, 9.05] |
| 3 Mental state: 2. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | ‐5.24 [‐9.06, ‐1.42] |
| 4 Mental state: 3. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | ‐7.92 [‐17.01, 1.17] |
| 5 Behaviour: Leaving the study early (short‐term) Show forest plot | 6 | 421 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Adverse effects: 1. General ‐ average scores (TESS, endpoint, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 7 Adverse effects: 2. Specific ‐ extrapyramidal symptoms (short‐term) Show forest plot | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.00, 0.83] |
| 8 Adverse effects: 3. Specific ‐ numbness over the ear, upper extremity and chest on the treated side (short‐term) Show forest plot | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.52] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint (short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 talk, behaviour and expression still existed as before + reduction of BPRS < 29% | 2 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.02, 0.59] |
| 1.2 no change in symptoms | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.57, 1.06] |
| 2 Behaviour: Leaving the study early (short‐term) Show forest plot | 3 | 454 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint (short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 talk, behaviour and expression still existed as before + reduction of BPRS < 29% | 2 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.74, 2.87] |
| 1.2 no change in symptoms | 1 | 88 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.34, 0.80] |
| 2 Behaviour: Leaving the study early (short‐term) Show forest plot | 3 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Behaviour: Leaving the study early (short‐term) Show forest plot | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Adverse effects: 1. Specific ‐ back pain (short‐term) Show forest plot | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.74] |
| 3 Adverse effects: 2. Spinal fracture (short‐term) Show forest plot | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.14, 0.81] |


