Acupuntura para la esquizofrenia
Appendices
Appendix 1. Previous type of interventions (2005)
1. Acupuncture/electro‐acupuncture with or without moxibustion (a Traditional Chinese Medicine technique that involves the burning of mugwort to facilitate healing) or laser treatment, administered solely or in conjunction with antipsychotic drugs.
2. Placebo (sham acupuncture) or no treatment.
3. Antipsychotic drugs produced by pharmaceutical companies: any compound, dose, pattern or means of administration.
Appendix 2. Previous search strategy (2005)
1. Electronic searches
We searched the Cochrane Schizophrenia Group's Trials Register (April 2005) using the phrase: [(*acup* OR *moxibustion*) in REFERENCE and (*acupuncture* OR *moxibustion*) in STUDY]
This register is compiled by systematic searches of major databases (Biological Abstracts CINAHL, The Cochrane Library, EMBASE, MEDLINE, RUSSMED, LILACS, PSYNDEX and PsycLIT) hand searches and conference proceedings (see Group Module).
2. We also inspected the references of all identified studies (included and excluded) for further relevant trials.
Appendix 3. Previous data collection and analysis methods (2005)
1. Selection of studies
We (JR, JX) inspected all reports of studies identified from the search. A randomly selected sample of 10% of all the reports were re‐inspected in order to ensure that the selection was reliable. Where disagreement occurred, we resolved this by discussion and if there was still doubt we acquired the full article for further inspection. Once the full articles were obtained, we independently decided whether or not they met the review criteria. Again, where disagreement occurred, we resolved this by discussion and when this was not possible we sought further information from first authors and added these trials to the list of those awaiting assessment.
2. Assessment of methodological quality
We allocated trials to three quality categories, as described in the Cochrane Collaboration Handbook (Alderson 2004). When disputes arose as to which category a trial was allocated, again, we attempted resolution by discussion. When this was not possible and further information was necessary to clarify into which category to allocate the trial, we did not enter data but allocated the trial to the list of those awaiting assessment. We only included trials in Category A or B in the review.
A. Low risk of bias (adequate allocation concealment)
B. Moderate risk of bias (some doubt about the results)
C. High risk of bias (inadequate allocation concealment). For the purpose of the analysis in this review, trials were included if they met the Cochrane Handbook criteria A or B.
3. Data extraction
3.1 Reliable extraction
We independently extracted data from selected trials. When disputes arose, we attempted resolution by discussion. When this was not possible and further information was necessary to resolve the dilemma, we did not enter data but added this outcome of the trial to the list of those awaiting assessment.
3.2 Intention to treat analysis
We excluded data from studies where more than 50% of participants in any group were lost to follow‐up, except for the outcome of 'leaving the study early'. In studies with less than 50% dropout rate, everyone allocated to the intervention was counted whether or not they completed follow‐up. We considered those leaving early to have had the negative outcome, except for the event of death and adverse effects.
Where attrition rates were high (25% to 50%), we analysed the impact of including this type of data in a sensitivity analysis. If inclusion of high attrition data resulted in a substantive change in the estimate of effect, then we did not pool this data, but presented the data separately.
4. Data analysis
4.1 Dichotomous/binary data
In the review we used relative risk (RR), (fixed‐effect) and 95% confidence interval (CI). Where possible, we made efforts to convert relevant categorical or continuous outcome measures to dichotomous data by identifying cut off points on rating scales and dividing them into groups accordingly i.e.. 'moderate or severe impairment' and 'no better or worse'.
4.1.1 Summary statistic: For binary outcomes we calculated a standard estimate of the relative risk (RR) and its 95% confidence intervals (CI) (fixed‐effect). Where possible, we estimated the number needed to treat (NNT) using an on‐line calculator (http://www.nntonline.net/). If heterogeneity was found (see section 5) we used a random‐effects model.
4.2 Continuous data
4.2.1 Skewed data: continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data, the following standards are applied to all data before inclusion: (a) standard deviations and means were reported in the paper or were obtainable from the authors; (b) when a scale started from the finite number zero, the standard deviation, when multiplied by two, was less than the mean (as otherwise the mean was unlikely to be an appropriate measure of the centre of the distribution, (Altman 1996); (c) if a scale started from a positive value (such as PANSS which can have values from 30‐210) the calculation described above in (b) was modified to take the scale starting point into account. In these cases skewness is present if 2SD>(S‐Smin), where S is the mean score and Smin is the minimum score. Endpoint scores on scales often have a finite start and end point and these rules can be applied to them.
4.2.2 Summary statistic: For continuous outcomes we calculated weighted mean differences (WMD) and respective 95% CI (fixed‐effect). If heterogeneity was found (see section 5) we used a random‐effects model.
4.2.3 Valid scales: A wide range of instruments are available to measure mental health outcomes. These instruments vary in quality and it has been shown that the use of rating scales which have not been described in a peer‐reviewed journal (Marshall 2000) are associated with bias, or may not be valid, or even ad hoc. Therefore, some minimum standards were set: (a) the psychometric properties of the instrument should have been described in a peer‐reviewed journal; (b) the instrument should either be a self‐report, or completed by an independent rater or relative (not the therapist); and (c) the instrument should be a global assessment of an area of functioning.
4.2.4 Endpoint versus change data: where possible, we presented endpoint data and if both endpoint and change data were available for the same outcomes then we only reported the former in this review.
4.2.5 Cluster trials
Studies increasingly employ 'cluster randomisation' (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems. Firstly, authors often fail to account for intra class correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992) whereby P values are spuriously low, confidence intervals unduly narrow and statistical significance overestimated. This causes type I errors (Bland 1997, Gulliford 1999).
Where clustering was not accounted for in primary studies, we presented the data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review we will seek to contact first authors of studies to obtain intra‐class correlation co‐efficients of their clustered data and to adjust for this using accepted methods (Gulliford 1999). Where clustering has been incorporated into the analysis of primary studies, we will also present these data as if from a non‐cluster randomised study, but adjusted for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a 'design effect'. This is calculated using the mean number of participants per cluster (m) and the intraclass correlation co‐efficient (ICC) [Design effect = 1+(m‐1)*ICC] (Donner 2002). If the ICC was not reported it was assumed to be 0.1 (Ukoumunne 1999).
5. Test for heterogeneity
Firstly, we considered all of the included studies within any comparison to judge clinical heterogeneity. Then we visually inspected graphs used to investigate the possibility of statistical heterogeneity and supplemented this by using, primarily, the I‐squared statistic. This provides an estimate of the percentage of variability due to heterogeneity rather than chance alone. Where the I‐squared estimate was greater than or equal to 75%, we interpreted this as indicating the presence of high levels of heterogeneity (Higgins 2003). If inconsistency was high, we did not summate the data, but presented it separately and reasons for heterogeneity were investigated.
6. Addressing publication bias
We entered all data from the included studies into a funnel graph (trial effect against trial size) in an attempt to investigate the likelihood of overt publication bias (Egger 1997).
Appendix 4. Previous description of studies
1. Excluded studies
We excluded three studies. Xue 1985 and Zhuge 1993 were not randomised. Zhong 1995 compared electro‐acupuncture to computerised electrode.
2. Awaiting assessment
No studies are awaiting assessment.
3. Ongoing studies
We are not aware of any ongoing studies.
4. Included studies
We included five studies all of which were randomised. Only electro ‐ Zhou 1997 reported on blinding, in which the raters were blind to treatment allocation.
4.1 Length of trials
All included studies were short‐term (less than three months). The shortest study electro ‐ Zhang 1987 lasted for 20 days. laser ‐ Zhang 1991 was for five weeks, electro ‐ Zhou 1997 and electro ‐ Zhang 2001 were six week studies and Zhang 1994 was the longest study lasting eight weeks.
4.2 Participants
All participants were diagnosed with schizophrenia. electro ‐ Zhou 1997, laser ‐ Zhang 1991 and electro ‐ Zhang 2001 used operationalised criteria (DSM/ICD/CCMD). electro ‐ Zhang 1987, Zhang 1994 did not report using predefined diagnostic criteria. electro ‐ Zhou 1997, electro ‐ Zhang 1987, laser ‐ Zhang 1991 and electro ‐ Zhang 2001 used male and female participants, whilst Zhang 1994 did not report on gender.
4.3 Setting
All five trials were undertaken in a hospital setting.
4.4 Study size
The numbers of participants randomised ranged between 31 laser ‐ Zhang 1991 to 88 electro ‐ Zhang 1987. Forty people were randomised by electro ‐ Zhou 1997, 69 by Zhang 1994 and 42 by electro ‐ Zhang 2001.
4.5 Interventions
The treatment groups received acupuncture exclusively or in combination with antipsychotics. All the comparator groups received antipsychotics. electro ‐ Zhou 1997 used electro‐acupuncture in combination with reduced dose antipsychotics versus chlorpromazine equivalents (˜560mg/day). The treatment group in electro ‐ Zhang 1987 received electro‐acupuncture and the comparator group were given chlorpromazine (300‐600 mg/day). laser ‐ Zhang 1991 randomised people into three comparator groups, laser‐acupuncture with moxibustion, laser acupuncture with moxibustion and reduced dose chlorpromazine (150‐300 mg/day), or chlorpromazine (350‐600 mg/day). Zhang 1994 compared electro‐acupuncture to chlorpromazine equivalents (˜458 mg/day). electro ‐ Zhang 2001 compared electro‐acupuncture combined with antipsychotics to antipsychotics alone but did not report on the acupoints used or dosages. Details of acupuncture points, needles and electro‐acupuncture frequencies used (when reported) are listed in the included studies table.
4.6 Outcomes
All data outcomes were reported as short‐term (less than three months). Data from some studies were unusable because raw scores were not presented. Instead outcomes were reported as P values without means and standard deviations being provided, or the scale used was not identified. electro ‐ Zhang 2001 predefined no clinical improvement as HAMD scores reduced by </ = 25%. electro ‐ Zhou 1997 predefined no clinical improvement as BPRS scores reduced by </ = 20%.
4.6.1 Outcome scales: details of scales that provided usable data are shown below. Reasons for exclusion of data from instruments are given under 'outcomes' in the included studies table.
4.6.1.1 Global state scales
4.6.1.1.1 Clinical Global Impression Scale ‐ CGI (Guy 1970)
The CGI is a three‐item scale commonly used in studies on schizophrenia that enables clinicians to quantify severity of illness and overall clinical improvement. The items are: severity of illness, global improvement and efficacy index. A seven‐point scoring system is usually used with low scores indicating decreased severity and/or greater recovery. electro ‐ Zhou 1997 and laser ‐ Zhang 1991 reported CGI data.
4.6.1.2 Mental state
4.6.1.2.1 Brief Psychiatric Rating Scale ‐ BPRS (Overall 1962)
The BPRS is an 18‐item scale measuring positive symptoms, general psychopathology and affective symptoms. The original scale has sixteen items, but a revised eighteen‐item scale is commonly used. Scores can range from 0 ‐126. Each item is rated on a seven‐point scale, with high scores indicating more severe symptoms. electro ‐ Zhou 1997, laser ‐ Zhang 1991and Zhang 1994 all reported BPRS data.
4.6.1.2.2 Scale for the Assessment of Negative Symptoms ‐ SANS (Andreasen 1982)
This scale allows a global rating of the following negative symptoms: alogia (impoverished thinking), affective blunting, avolition‐apathy, anhedonia‐asociality and attention impairment. Assessments are made on a six‐point scale (0 = not at all to 5 = severe). Higher scores indicate more symptoms. Data for this scale were reported by Zhang 1994.
4.6.1.2.3 Scale for the Assessment of Positive Symptoms ‐ SAPS (Andreasen 1982)
This six‐point scale gives a global rating of positive symptoms such as delusions, hallucinations and disordered thinking. Higher scores indicate more symptoms. Zhang 1994 was the only study to report SAPS data.
4.6.1.2.4 Hamilton Rating Scale for Depression ‐ HAMD (Hamilton 1967)
This instrument is designed to be used only on patients already diagnosed as suffering from affective disorder of the depressive type. It is used for quantifying the results of an interview, and its value depends entirely on the skill of the interviewer in eliciting the necessary information. The scale contains 17 variables measured on either a five‐point or a three‐point rating scale, the latter being used where quantification of the variable is either difficult or impossible. Among the variables are: depressed mood, suicide, work and loss of interest, retardation, agitation, gastro‐intestinal symptoms, general somatic symptoms, hypochondriasis, loss of insight, and loss of weight. It is useful to have two raters independently scoring a patient at the same interview. The scores of the patient are obtained by summing the scores of the two physicians. A score of 11 is generally regarded as indicative of a diagnosis of mild depression, 14‐17 mild to moderate depression and >17 moderate to severe depression. electro ‐ Zhang 2001 reported data for this scale.
4.6.1.2.5 Zung Depression Scale ‐ ZDS (Zung 1965)
The Zung Self‐Rating Depression Scale is a 20‐item self‐rated scale that is widely used as a screening tool, covering affective, psychological and somatic symptoms associated with depression. The questionnaire takes approximately ten minutes to complete and items are framed in terms of positive and negative statements. It can be effectively used in a variety of settings, including primary care, psychiatric clinics, drug trials and various research situations. Each item is scored on a Likert scale ranging from one to four. Most people with depression score between 50 and 69, while a score of 70 and above indicates severe depression. electro ‐ Zhang 2001 reported data from this scale.
4.6.1.3 Adverse events
4.6.1.3.1 Treatment Emergent Symptom Scale/Form ‐ TESS/F (Guy 1976)
This checklist assesses a variety of characteristics for each adverse event, including severity, relationship to the drug, temporal characteristics (timing after a dose, duration and pattern during the day), contributing factors, course and action taken to counteract the effect. Symptoms can be listed a priori or can be recorded as observed by the investigator. Zhang 1994 reported data for this scale.
Appendix 5. Previous effects of interventions
1. The search
The electronic search identified 18 reports. We were able to include five trials and we added three trials to the excluded studies table.
2. COMPARISON 1. ACUPUNCTURE versus ANTIPSYCHOTICS
2.1. Global state
Two studies electro ‐ Zhang 1987 and laser ‐ Zhang 1991 reported on global state (not improved) with equivocal results.
2.2. Leaving the study early
There were no losses to follow‐up in either group from two trials electro ‐ Zhang 1987 and laser ‐ Zhang 1991 by five weeks.
2.3. Adverse effects
Extrapyramidal symptoms reported by laser ‐ Zhang 1991 were lower in the acupuncture group with no participants experiencing this adverse effect. The control group had significantly higher numbers with eight out of ten people reported as having extrapyramidal symptoms (n = 21, RR 0.05 CI 0.0 to 0.8, NNT 2 CI 2 to 8).
3. COMPARISON 2. ACUPUNCTURE + ANTIPSYCHOTICS versus ANTIPSYCHOTICS
3.1. Global state
One study laser ‐ Zhang 1991 reported global state (not improved at five weeks) with equivocal results. Clinical Global Impression (severity of illness) scores were reported by electro ‐ Zhou 1997 with equivocal scores. electro ‐ Zhou 1997 also reported on Clinical Global Impression (global improvement) but data were skewed.
3.2. Leaving the study early
Four trials (laser ‐ Zhang 1991, Zhang 1994, electro ‐ Zhou 1997, electro ‐ Zhang 2001) reported as short‐term outcomes that no participants left the study early (up to eight weeks).
3.3. Mental state
Dichotomised BPRS data were reported by electro ‐ Zhou 1997 (not improved </ = 20% reduction at endpoint) with equivocal results. Continuous BPRS data (Zhang 1994, electro ‐ Zhou 1997) were significant in favour of the acupuncture group (n = 109, WMD ‐4.31 CI ‐7.0 to ‐1.6). Mental state SANS and SAPS score were reported by Zhang 1994, but data were skewed and cannot be displayed graphically. Depression scores from the HAMD scale were reported by electro ‐ Zhang 2001 with scores from this smaller study being significantly lower in the acupuncture group (n = 42, WMD ‐10.41 CI ‐12.8 to ‐8.0). When the HAMD scores were dichotomised to 'not improved', again, by electro ‐ Zhang 2001 results significantly favoured the acupuncture group (n = 42, RR 0.17 CI 0.1 to 0.5, NNT 2 CI 2 to 3). electro ‐ Zhang 2001 also reported on depression using the Zung Depression Scale with results at five weeks significantly favouring the acupuncture group (n = 42, WMD ‐24.25 CI ‐28.0 to ‐20.5).
3.4. Adverse effects
electro ‐ Zhou 1997 reported TESS scores at six weeks, with results significantly favouring the acupuncture group (n = 40, WMD ‐0.50 CI ‐0.9 to ‐0.1). laser ‐ Zhang 1991 found the incidences of extrapyramidal symptoms to be similar for both treatment groups.

Study flow diagram.
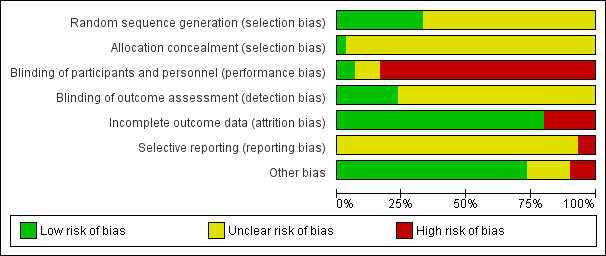
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
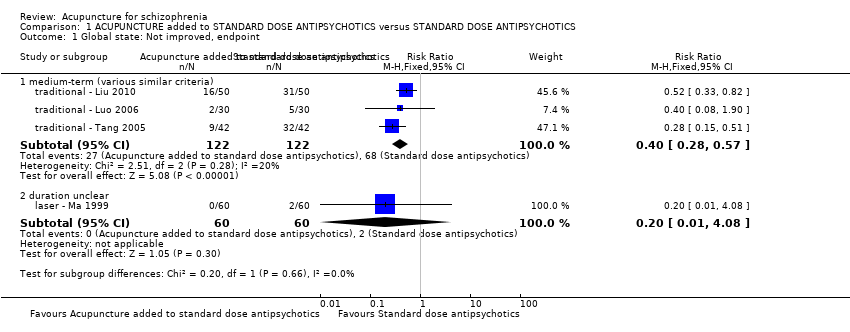
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 1 Global state: Not improved, endpoint.
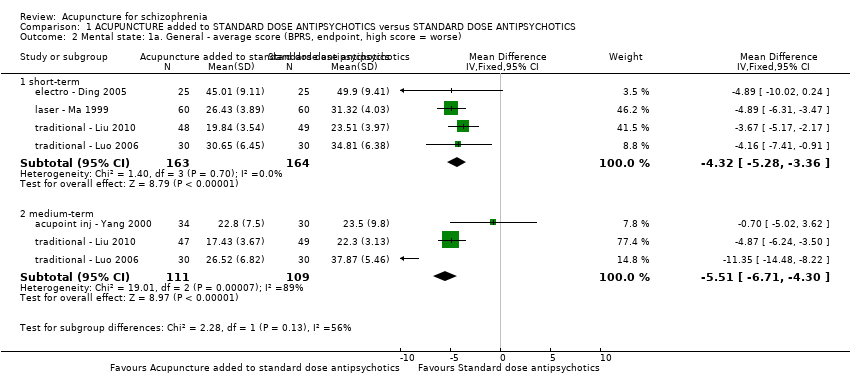
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 2 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 3 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, medium‐term) ‐ subgroup analysis.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 4 Mental state: 2a. General ‐ average score (PANSS, endpoint, high score = worse).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 5 Mental state: 2b. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ subgroup analysis.
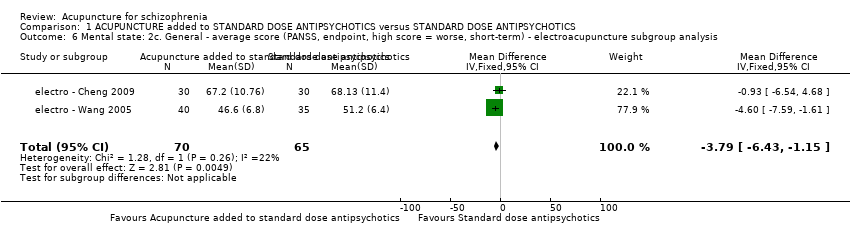
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 6 Mental state: 2c. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ electroacupuncture subgroup analysis.
| Study | Intervention | Mean | SD | N | Note |
| short‐term | |||||
| electro ‐ Chen 2008 | Electroacupuncture added to standard dose antipsychotics | 50.73 | 13.32 | 30 | Compared with the score before treatment P < 0.05 |
| electro ‐ Chen 2008 | Standard dose antipsychotics | 72.30 | 7.01 | 30 | |
| electro ‐ Yao 2006 | Electroacupuncture added to standard dose antipsychotics | 46.51 | 17.10 | 45 | Compared with the score before treatment P < 0.01 |
| electro ‐ Yao 2006 | Standard dose antipsychotics | 46.45 | 17.23 | 45 | Compared with the score before treatment P < 0.01 |
| traditional ‐ Bouhlel 2011 | Traditional acupuncture added to standard dose antipsychotics | 77.40 | 25.73 | 15 | P = 0.501 |
| traditional ‐ Bouhlel 2011 | Standard dose antipsychotics | 77.81 | 26.77 | 16 | |
| medium‐term | |||||
| electro ‐ Chen 2008 | Electroacupuncture added to standard dose antipsychotics | 32.02 | 11.21 | 30 | Compared with the score before treatment P < 0.01 |
| electro ‐ Chen 2008 | Standard dose antipsychotics | 52.10 | 10.32 | 30 | Compared with the score before treatment P < 0.01 |
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 7 Mental state: 2d. General ‐ average score (PANSS, endpoint, high score = worse) ‐ Skewed data.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 8 Mental state: 2e. General ‐ not improved (PANSS), endpoint.
| Study | Intervention | Mean | SD | N | Note |
| electro ‐ Zhang 1993 | Electroacupuncture added to standard dose antipsychotics | 6.71 | 6.15 | 38 | P < 0.01 |
| electro ‐ Zhang 1993 | Standard dose antipsychotics | 10.65 | 6.95 | 31 | |
| traditional ‐ Bouhlel 2011 | Traditional acupuncture added to standard dose antipsychotics | 42.00 | 28.69 | 15 | P = 0.539 |
| traditional ‐ Bouhlel 2011 | Standard dose antipsychotics | 46.75 | 25.05 | 16 | |
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 9 Mental state: 3. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 10 Mental state: 4a.Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse).
| Study | Intervention | Mean | SD | N | Note |
| traditional acupuncture | |||||
| traditional ‐ Bouhlel 2011 | Traditional acupuncture added to standard dose antipsychotics | 55.60 | 24.71 | 15 | P = 0.406 |
| traditional ‐ Bouhlel 2011 | Standard dose antipsychotics | 52.81 | 30.88 | 16 | |
| electroacupuncture | |||||
| electro ‐ Zhang 1993 | Electroacupuncture added to standard dose antipsychotics | 24.97 | 20.86 | 38 | P < 0.005 |
| electro ‐ Zhang 1993 | Standard dose antipsychotics | 37.26 | 16.02 | 31 | |
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 11 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 12 Mental state: 5a. Specific ‐ average score ‐ depression (HAMD, endpoint, high score = worse, short‐term).
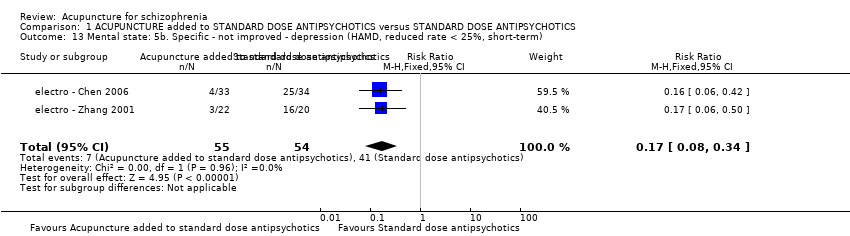
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 13 Mental state: 5b. Specific ‐ not improved ‐ depression (HAMD, reduced rate < 25%, short‐term).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 14 Mental state: 7b. Specific ‐ not improved ‐ auditory hallucinations (PSYRAS‐AH, reduction < 20%, short‐term).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 15 Mental state: 7a. Specific ‐ average score ‐ auditory hallucinations (PSYRAS‐AH,endpoint, high score = worse, short‐term).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 16 Mental state: 6. Specific ‐ average score ‐ depression (SDS, endpoint, high score = worse, short‐term).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 17 Mental state: 8. Specific ‐ not improved (auditory hallucinations, endpoint).
| Study | Intervention | Mean | SD | N | Note |
| short‐term | |||||
| traditional ‐ Liu 2010 | Traditional acupuncture added to standard dose antipsychotics | 9.26 | 5.37 | 48 | P < 0.05 |
| traditional ‐ Liu 2010 | Standard dose antipsychotics | 13.24 | 5.07 | 49 | |
| medium‐term | |||||
| traditional ‐ Liu 2010 | Traditional acupuncture added to standard dose antipsychotics | 5.12 | 3.64 | 47 | P < 0.01 |
| traditional ‐ Liu 2010 | Standard dose antipsychotics | 12.63 | 2.89 | 49 | |
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 18 Mental state: 9. Specific ‐ average score ‐ auditory hallucinations (SAHS, endpoint, high score = worse) ‐ Skewed data.
![Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 19 Mental state: 10. Specific ‐ average score ‐ hallucinations (BPRS [12th item], endpoint, high score = worse, short‐term).](/es/cdsr/doi/10.1002/14651858.CD005475.pub2/media/CDSR/CD005475/image_n/nCD005475-CMP-001-19.png)
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 19 Mental state: 10. Specific ‐ average score ‐ hallucinations (BPRS [12th item], endpoint, high score = worse, short‐term).
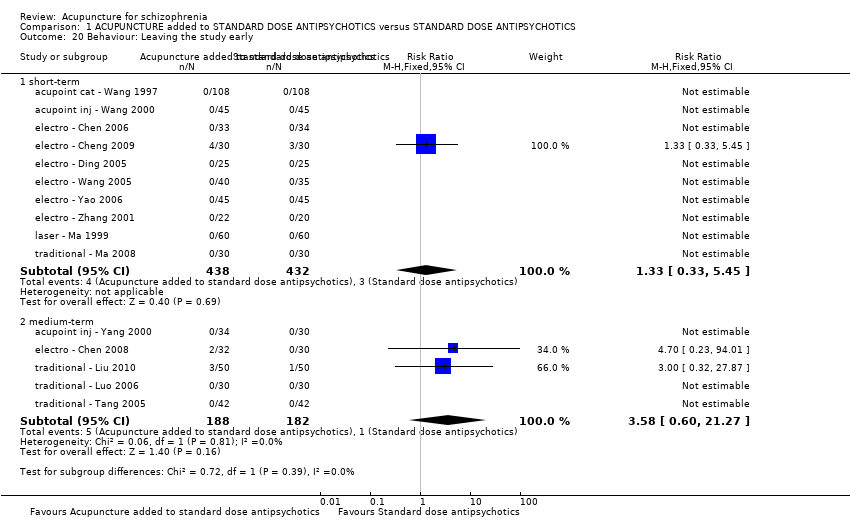
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 20 Behaviour: Leaving the study early.
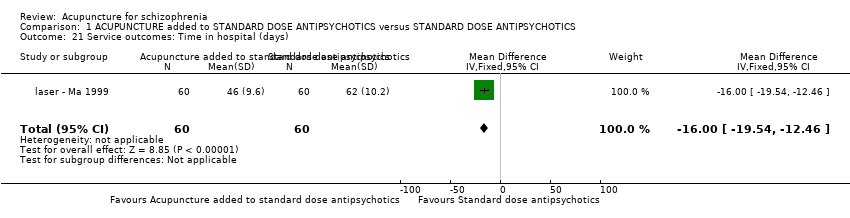
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 21 Service outcomes: Time in hospital (days).
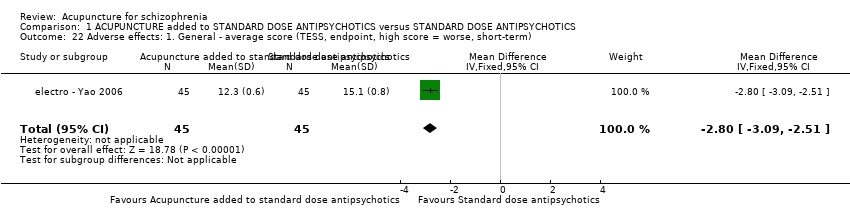
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 22 Adverse effects: 1. General ‐ average score (TESS, endpoint, high score = worse, short‐term).
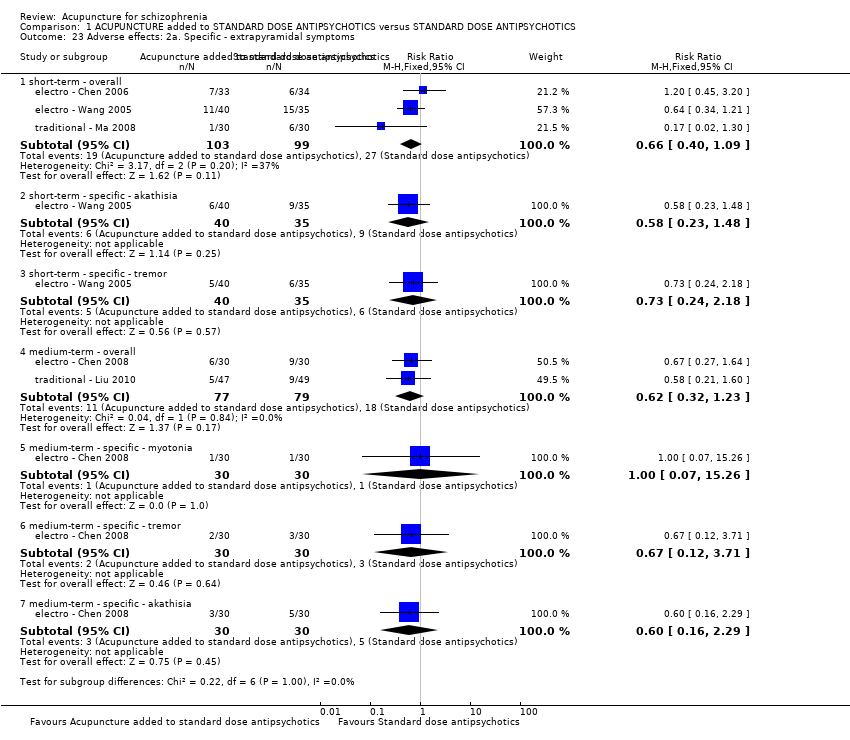
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 23 Adverse effects: 2a. Specific ‐ extrapyramidal symptoms.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 24 Adverse effects: 2b. Specific ‐ extrapyramidal symptoms ‐overall (short‐term) ‐ subgroup analysis.
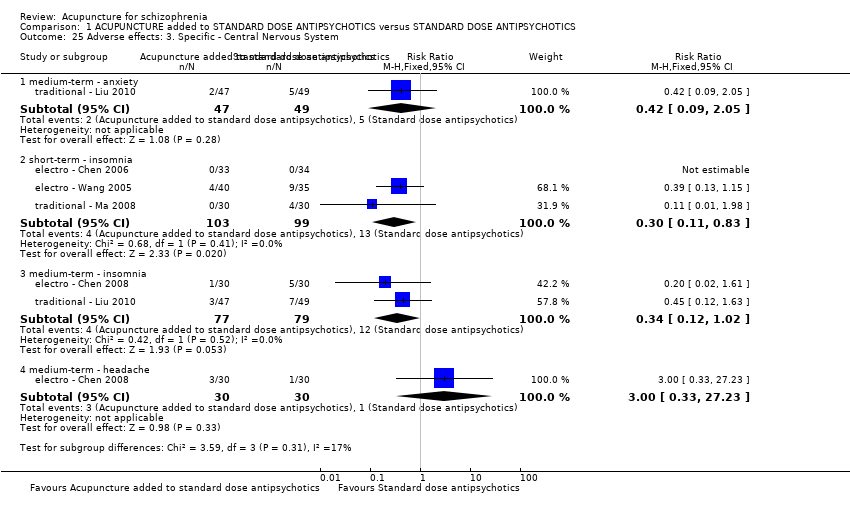
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 25 Adverse effects: 3. Specific ‐ Central Nervous System.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 26 Adverse effects: 4. Specific ‐ anticholinergic symptoms.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 27 Adverse effects: 5. Specific ‐ gastrointestinal system.
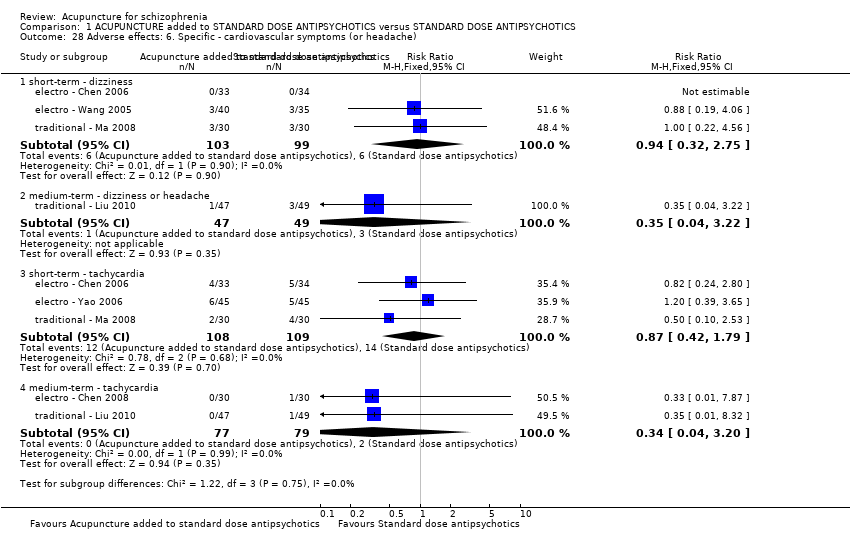
Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 28 Adverse effects: 6. Specific ‐ cardiovascular symptoms (or headache).

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 29 Adverse effects: 7a. Specific ‐ metabolic system.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 30 Adverse effects: 7b. Specific ‐ metabolic system ‐ weight gain (short‐term) ‐ subgroup analysis.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 31 Adverse effects: 8. Specific ‐ endocrine system.

Comparison 1 ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 32 Adverse effects: 9. Specific ‐ lab test.
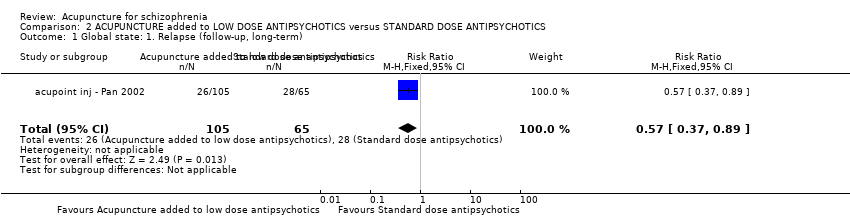
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 1 Global state: 1. Relapse (follow‐up, long‐term).
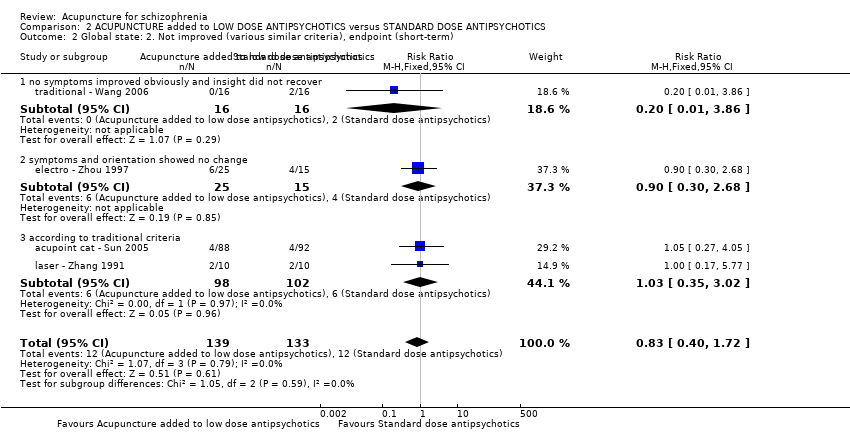
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 2 Global state: 2. Not improved (various similar criteria), endpoint (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 3 Global state: 3a. CGI ‐ average score ‐ CGI‐SI (endpoint, high score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| electro ‐ Zhou 1997 | Electroacupuncture added to low dose antipsychotics | 2.2 | 1.1 | 25 | No significant difference |
| electro ‐ Zhou 1997 | Standard dose antipsychotics | 2.3 | 1.3 | 15 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 4 Global state: 3b. CGI ‐ average score ‐ CGI‐GI (endpoint, high score = worse, short‐term) ‐ Skewed data.
| Study | Intervention | Mean | SD | N | Note |
| electro ‐ Zhou 1997 | Electroacupuncture added to low dose antipsychotics | 2.5 | 1.3 | 25 | P < 0.05 |
| electro ‐ Zhou 1997 | Standard dose antipsychotics | 1.5 | 0.8 | 15 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 5 Global state: 3c. CGI ‐ average score ‐ CGI‐EI (endpoint, high score = worse, short‐term) ‐ Skewed data.
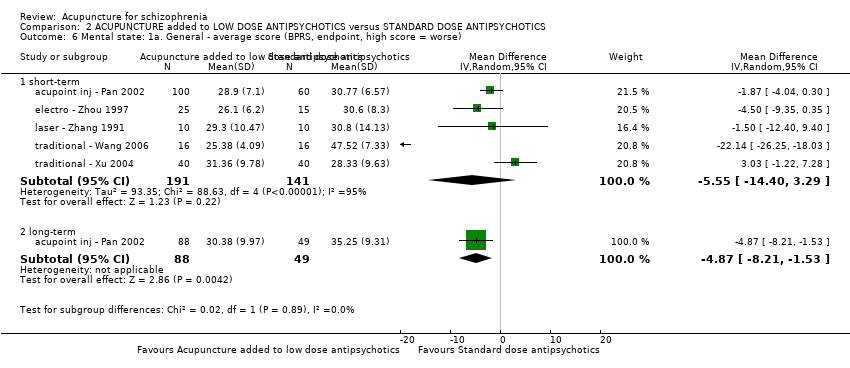
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 6 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse).
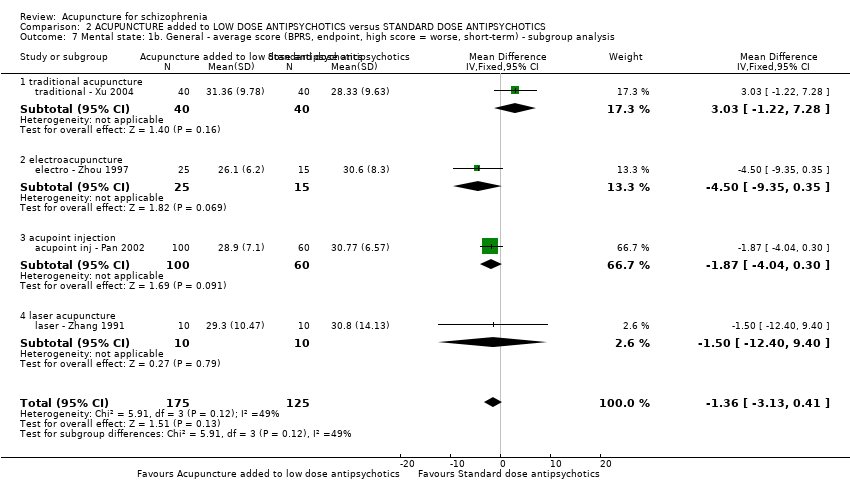
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 7 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, short‐term) ‐ subgroup analysis.
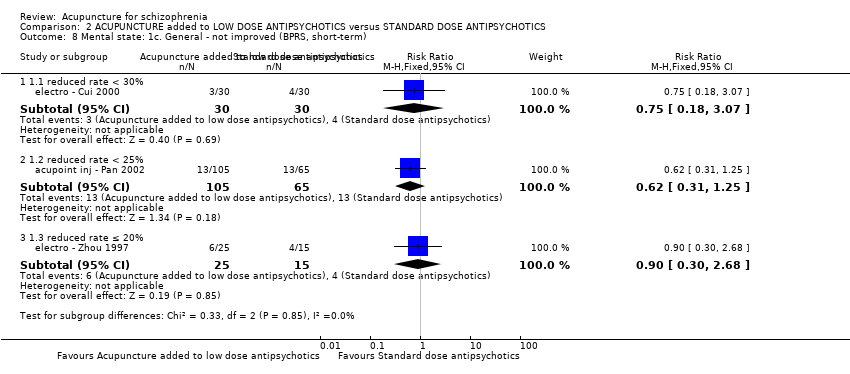
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 8 Mental state: 1c. General ‐ not improved (BPRS, short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 9 Mental state: 1d. General ‐ average change scores (BPRS, low score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| acupoint cat ‐ Sun 2005 | Acupoint catgut treatment added to low dose antipsychotics | 52.85 | 15.86 | 88 | P > 0.05 |
| acupoint cat ‐ Sun 2005 | Standard dose antipsychotics | 49.75 | 12.77 | 92 | |
| electro ‐ Xiong 2010 | Electroacupuncture added to low dose antipsychotics | 46.34 | 11.10 | 40 | Cmpared with score before treatment P < 0.01 |
| electro ‐ Xiong 2010 | Standard dose antipsychotics | 45.21 | 11.36 | 40 | Cmpared with score before treatment P < 0.01 |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 10 Mental state: 2a. General ‐ Average score (PANSS, endpoint, high score = worse, short‐term) ‐ Skew data.
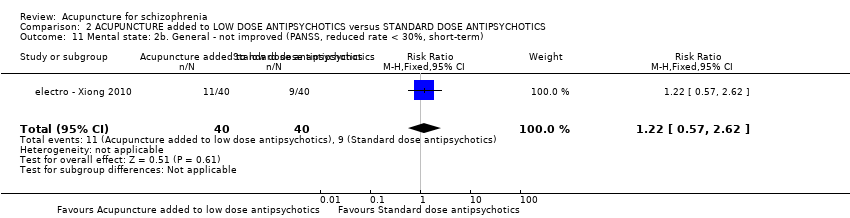
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 11 Mental state: 2b. General ‐ not improved (PANSS, reduced rate < 30%, short‐term).
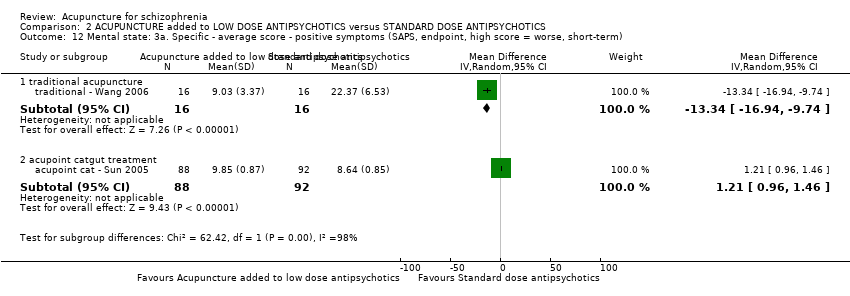
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 12 Mental state: 3a. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| traditional ‐ Xu 2004 | Traditional acupuncture added to low dose antipsychotics | 11.86 | 11.41 | 40 | No significant difference |
| traditional ‐ Xu 2004 | Standard dose antipsychotics | 11.12 | 9.87 | 40 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 13 Mental state: 3b. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data.

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 14 Mental state: 4a. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| traditional ‐ Wang 2006 | Traditional acupuncture added to low dose antipsychotics | 14.23 | 8.68 | 16 | P < 0.01 |
| traditional ‐ Wang 2006 | Standard dose antipsychotics | 30.56 | 13.31 | 16 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 15 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data.
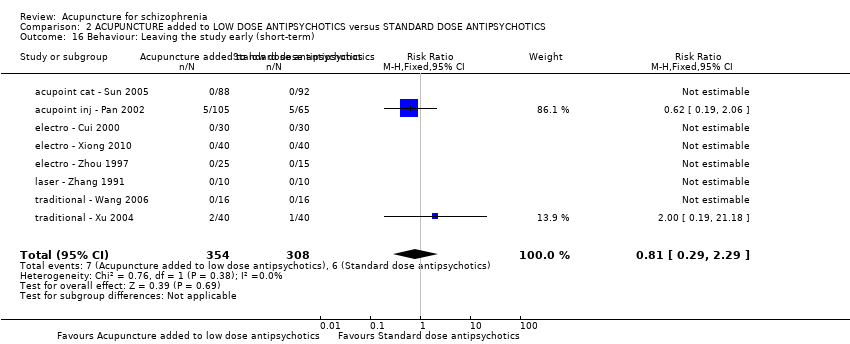
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 16 Behaviour: Leaving the study early (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 17 Adverse effects: 1a. General ‐ average score (TESS, endpoint, high score = worse, short‐term).
| Study | Intervention | Mean | SD | N | Note |
| electro ‐ Xiong 2010 | Electroacupuncture added to low dose antipsychotics | 5.08 | 4.56 | 40 | P < 0.01 |
| electro ‐ Xiong 2010 | Standard dose antipsychotics | 10.38 | 6.52 | 40 | |
| traditional ‐ Wang 2006 | Traditional acupuncture added to low dose antipsychotics | 2.57 | 3.28 | 16 | P < 0.01 |
| traditional ‐ Wang 2006 | Standard dose antipsychotics | 6.93 | 5.28 | 16 | |
| traditional ‐ Xu 2004 | Traditional acupuncture added to low dose antipsychotics | 2.65 | 3.47 | 40 | P < 0.01 |
| traditional ‐ Xu 2004 | Standard dose antipsychotics | 10.12 | 8.12 | 40 | |
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 18 Adverse effects: 1b. General ‐ average score (TESS, endpoint, high score = worse, short‐term) ‐ Skewed data.
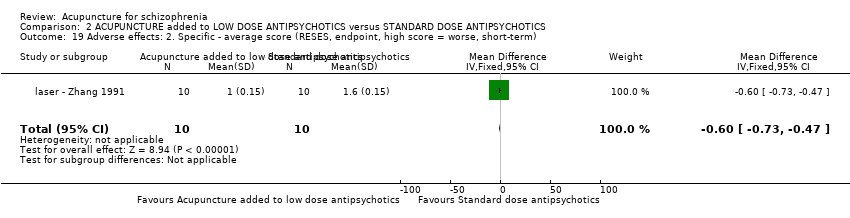
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 19 Adverse effects: 2. Specific ‐ average score (RESES, endpoint, high score = worse, short‐term).
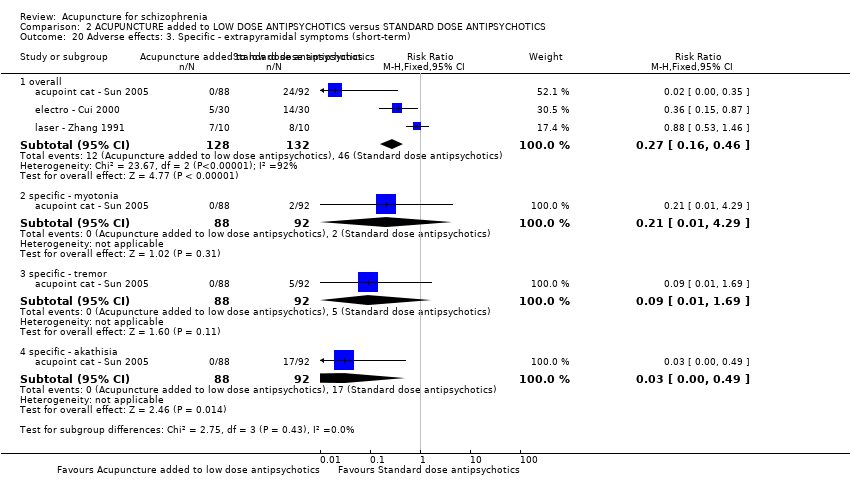
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 20 Adverse effects: 3. Specific ‐ extrapyramidal symptoms (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 21 Adverse effects: 4. Specific ‐ Central Nervous System (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 22 Adverse effects: 5. Specific ‐ anticholinergic symptoms (short‐term).

Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 23 Adverse effects: 6. Specific ‐ cardiovascular symptoms (short‐term).
Comparison 2 ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 24 Adverse effects: 7. Specific ‐ skin infection (short‐term).

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 1 Global state: Not improved, endpoint (short‐term).

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 2 Mental state: 1. General ‐ average score (BPRS, endpoint, high score = worse, short‐term).
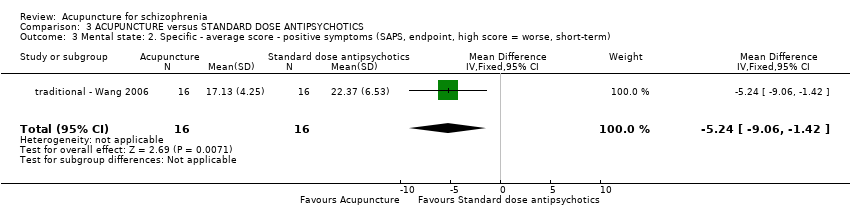
Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 3 Mental state: 2. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term).
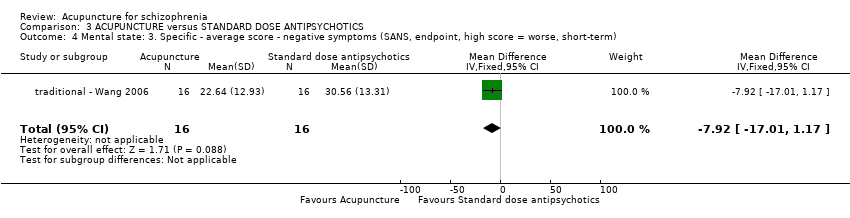
Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 4 Mental state: 3. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term).

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 5 Behaviour: Leaving the study early (short‐term).
| Study | Intervention | Mean | SD | N | Note |
| traditional ‐ Wang 2006 | Traditional acupuncture | 2.43 | 3.17 | 16 | P < 0.01 |
| traditional ‐ Wang 2006 | Antipsychotics | 6.93 | 5.28 | 16 | |
Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 6 Adverse effects: 1. General ‐ average scores (TESS, endpoint, short‐term) ‐ Skewed data.

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 7 Adverse effects: 2. Specific ‐ extrapyramidal symptoms (short‐term).

Comparison 3 ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS, Outcome 8 Adverse effects: 3. Specific ‐ numbness over the ear, upper extremity and chest on the treated side (short‐term).

Comparison 4 ACUPUNCTURE added to TCM DRUG versus TCM DRUG, Outcome 1 Global state: Not improved, endpoint (short‐term).
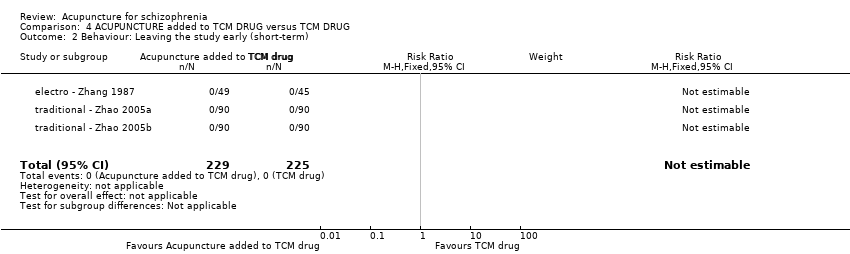
Comparison 4 ACUPUNCTURE added to TCM DRUG versus TCM DRUG, Outcome 2 Behaviour: Leaving the study early (short‐term).
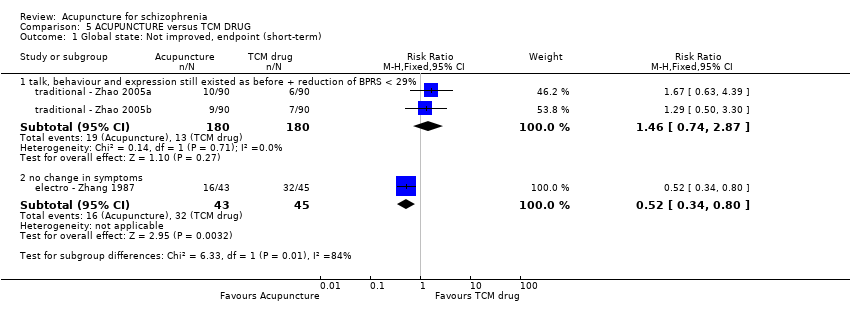
Comparison 5 ACUPUNCTURE versus TCM DRUG, Outcome 1 Global state: Not improved, endpoint (short‐term).

Comparison 5 ACUPUNCTURE versus TCM DRUG, Outcome 2 Behaviour: Leaving the study early (short‐term).

Comparison 6 ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTROCONVULSIVE THERAPY, Outcome 1 Behaviour: Leaving the study early (short‐term).

Comparison 6 ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTROCONVULSIVE THERAPY, Outcome 2 Adverse effects: 1. Specific ‐ back pain (short‐term).

Comparison 6 ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTROCONVULSIVE THERAPY, Outcome 3 Adverse effects: 2. Spinal fracture (short‐term).
| Comparison | Trial |
| Different acupoints | |
| Acupoints vs non‐acupoints |
| Methods | Allocation: randomised, clearly described, concealed. Follow‐up: 2 years. |
| Participants | Diagnosis: schizophrenia (DSM V) with one TCM type according to TCM diagnosis standard. |
| Interventions | 1. Electroacupuncture: N = 150. The acupoints and relative parameters clearly described. |
| Outcomes | 1. Death 2. Global state 3. Mental state 4. Behaviour 5. Service outcomes 6. Adverse effects 7. Engagement with service 8. Satisfaction with treatment 9. Quality of life 10. Economic outcome |
| Notes | * Powered to be able to identify a difference of ˜20% between groups for primary outcome with adequate degree of certainty. ** This is to maximise blinding. |
| ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS | |||||
| Global state: Not improved, endpoint ‐ medium‐term (various similar criteria) | 557 per 1000 | 223 per 1000 | RR 0.4 | 244 | ⊕⊝⊝⊝ | Relapse was not reported but 'no clinically important change in global state' was reported and another outcome without clear duration indicated no difference between two comparison groups. |
| Mental state: PANSS (not improved, reduced rated < 25%, short‐term) | 432 per 1000 | 281 per 1000 | RR 0.65 | 197 | ⊕⊝⊝⊝ | Data from PANSS were equivocal because of different criteria. Other mental state findings were mostly consistent with this finding. |
| Behaviour: Leaving the study early (short‐term) | 7 per 1000 | 9 per 1000 | RR 1.33 | 870 | ⊕⊝⊝⊝ | Similar outcomes at medium‐term. |
| Service outcomes: Time in hospital (days) | The mean service outcomes: time in hospital (days) in the intervention groups was | 120 | ⊕⊕⊕⊝ | 0nly one study reported service outcomes ‐ time in hospital. | ||
| Adverse effects: Central Nervous System ‐ insomnia (short‐term) | 131 per 1000 | 39 per 1000 | RR 0.30 | 202 | ⊕⊕⊝⊝ | Only insomnia rate indicated difference between two compared groups. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'very serious' ‐ Unblinding of participants and personnel and incomplete outcome data. | ||||||
| ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS | |||||
| Global state: Relapse (follow‐up, long‐term) | 431 per 1000 | 246 per 1000 | RR 0.57 | 170 | ⊕⊝⊝⊝ | Only one study reported this outcome. Other global state findings reported no difference between the two comparison groups. |
| Mental state: BPRS (not improved, reduced rate < 30%, short‐term) | 133 per 1000 | 100 per 1000 | RR 0.75 | 60 | ⊕⊝⊝⊝ | Though measured with different criteria of 'no clinically important change in general mental state', there was no difference between the two comparison groups at short‐term and mostly similar results from other mental state findings. |
| Behaviour: Leaving the study early (short‐term) | 19 per 1000 | 16 per 1000 | RR 0.81 | 662 | ⊕⊝⊝⊝ | |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Extrapyramidal symptoms ‐ specific ‐ akathisia (short‐term) | 185 per 1000 | 6 per 1000 | RR 0.03 | 180 | ⊕⊕⊝⊝ | Similar to the akathisia data, acupuncture added to low dose antipsychotics reduced participants experiencing dry mouth, blurred vision, tachycardia at short‐term. Only one study focused on acupoint catgut treatment relative adverse effects but did not find skin infection in either groups. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'very serious' ‐ Unblinding of participants and personnel and incomplete outcome data. | ||||||
| ACUPUNCTURE versus STANDARD DOSE ANTIPSYCHOTICS for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE versus ANTIPSYCHOTICS | |||||
| Global state: Not improved (talk, behaviour and expression still existed as before; the reduction of BPRS < 29%), endpoint (short‐term) | 317 per 1000 | 104 per 1000 | RR 0.33 | 240 | ⊕⊝⊝⊝ | Relapse was not reported but 'no clinically important change in global state' was reported and another three outcomes with different but similar criteria indicated no difference between the two comparison groups in the short‐term. |
| Mental state: BPRS, endpoint (high score = worse, short‐term) ‐ traditional acupuncture | The mean mental state: BPRS, endpoint (high score = worse, short‐term) ‐ traditional acupuncture in the intervention groups was | 32 | ⊕⊝⊝⊝ | The outcome of 'no clinically important change in general mental state' was not reported but average endpoint BPRS data were reported as was the SAPS score. There was no difference between the two comparison groups in the short‐term using either score. | ||
| Behaviour: Leaving the study early (short‐term) | See comment | See comment | Not estimable | 421 | ⊕⊕⊝⊝ | No participants left each compared group early. |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Extrapyramidal symptoms (short‐term) | 800 per 1000 | 40 per 1000 | RR 0.05 | 21 | ⊕⊕⊝⊝ | One study reported laser acupuncture relative adverse effects ‐ numbness over ear, upper extremity and chest on the treated side, but no difference between the two comparison groups. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'serious' ‐ Unblinding of participants and personnel. | ||||||
| ACUPUNCTURE plus TCM DRUG versus TCM DRUG for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE added to TCM DRUG versus TCM DRUG | |||||
| Global state: Not improved (talk, behaviour and expression still existed as before, the reduction of BPRS < 29%), endpoint (short‐term) | 72 per 1000 | 8 per 1000 | RR 0.11 | 360 | ⊕⊕⊝⊝ | Relapse was not reported but 'no clinically important change in global state' was reported and the other outcome with different criteria of 'no clinically important change in global state' indicated no difference between the two comparison groups in the short‐term. |
| Mental state: No clinically important change in mental state | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Behaviour: Leaving the study early (short‐term) | See comment | See comment | Not estimable | 454 | ⊕⊕⊝⊝ | No participants left either group early. |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Clinically important general adverse effects | See comment | See comment | Not estimable | 0 | See comment | Three studies reported this outcome, however, two studies only reported one group's data and the other one study did not report the data. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'serious' ‐ Unblinding of participants and personnel. | ||||||
| ACUPUNCTURE versus TCM DRUG for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ACUPUNCTURE versus TCM DRUG | |||||
| Global state: Not improved, endpoint (short‐term) ‐ Not improved (no change in symptoms) ‐ Electroacupuncture | 711 per 1000 | 370 per 1000 | RR 0.52 | 88 | ⊕⊕⊝⊝ | Relapse was not reported but 'no clinically important change in global state' was reported and other outcomes with different criteria of 'no clinically important change in global state' indicated no difference between the two comparison groups in the short‐term. |
| Mental state: No clinically important change in general mental state | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Behaviour: Leaving the study early (short‐term) | See comment | See comment | Not estimable | 328 | See comment | No participants left either group early. |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Clinically important general adverse effects | See comment | See comment | Not estimable | ‐ | See comment | Three studies reported this outcome, however, two studies only reported one group's data and the other one study did not report the data. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias: rated 'serious' ‐‐ Unblinding of participants and personnel. | ||||||
| ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTRIC CONVULSIVE THERAPY for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY versus ELECTRIC CONVULSIVE THERAPY | |||||
| Global state: Relapse | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Mental state: No clinically important change in general mental state | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Behaviour: Leaving the study early (short‐term) | See comment | See comment | Not estimable | 68 | ⊕⊕⊝⊝ | No participants in either group left early. |
| Service outcomes: Hospitalisation | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Adverse effects: Spinal fracture (short‐term) | 441 per 1000 | 146 per 1000 | RR 0.33 | 68 | ⊕⊕⊝⊝ | Data from a single study where there was no difference in back pain between the two groups. |
| Quality of life: No clinically important change in quality of life | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| Economic outcomes: Cost of care | See comment | See comment | Not estimable | ‐ | See comment | Not reported. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Risk of bias; rated 'serious' ‐ Unblinding of participants and personnel. | ||||||
| Global state: Adding medication | |||
| Study | Drug | Events/Acupuncture group (n/N) | Events/Control group (n/N) |
| Artane | 6/30 | 11/30 | |
| Promethazine | 3/30 | 6/30 | |
| Propranolol | 2/30 | 4/30 | |
| Chlorpheniramine | 0/30 | 1/30 | |
| Propranolol | 7/40 | 7/35 | |
| Artane | 6/40 | 9/35 | |
| Benzodiazepine drugs | 4/40 | 7/35 | |
| Mental state: Time to auditory hallucinations disappeared (days) | |||
| Study | Intervention | Mean | SD |
| Laser acupuncture added to standard dose antipsychotics | 19 | 4.1 | |
| Standard dose antipsychotics | 31 | 4.4 | |
| Intervention | Term | Adverse effects | Adverse effects/Intervention group (n/N) | Study | |
| Traditional acupuncture | |||||
| Traditional acupuncture added to standard dose antipsychotics versus standard dose antipsychotics | Short term | Extrapyramidal symptoms | Overall | 1/30 | |
| Anticholinergic symptoms | Dry mouth | 3/30 | |||
| Cardiovascular | Dizziness | 3/30 | |||
| Tachycardia | 2/30 | ||||
| Medium term | Extrapyramidal symptoms | Overall | 5/47 | ||
| Central Nervous System | Anxiety | 2/47 | |||
| Insomnia | 3/47 | ||||
| Cardiovascular symptoms (or headache) | Dizziness or headache | 1/47 | |||
| Gastrointestinal system | Unspecifid gastrointestinal symptoms | 2/47 | |||
| Lab test | Liver function abnormal | 2/47 | |||
| Electroacupuncture | |||||
| Electroacupuncture (or added to TCM drug) versus TCM drug | Short term | Hold breath, facial cyanosis, arrhythmia, transient increase of blood pressure, injury of teeth, tongue and lips, epileptic attacks with strong stimulation | not reported | ||
| Electroacupuncture added to standard dose antipsychotics versus standard dose antipsychotics | Short term | Extrapyramidal symptoms | Overall | 18/73 | |
| Tremor | 5/40 | ||||
| Akathisia | 6/40 | ||||
| Central Nervous System | Insomnia | 4/73 | |||
| Anticholinergic symptoms | Dry mouth | 6/73 | |||
| Blurred vision | 4/73 | ||||
| Constipation | 3/73 | ||||
| Nausea and vomiting | 3/73 | ||||
| Cardiovascular symptoms | Dizziness | 3/73 | |||
| Tachycardia | 10/78 | ||||
| Metabolic system | Weight gain | 3/73 | |||
| Lab test | Liver function abnormal | 4/118 | electro ‐ Chen 2006; electro ‐ Wang 2005; electro ‐ Yao 2006 | ||
| ECG abnormal (myocardial ischaemia) | 1/118 | ||||
| blood routine test abnormal (leukocyte change) | 4/118 | ||||
| Medium term | Extrapyramidal symptoms | Overall | 6/30 | ||
| Myotonia | 1/30 | ||||
| Tremor | 2/30 | ||||
| Akathisia | 3/30 | ||||
| Central Nervous System | Insomnia | 1/30 | |||
| Headache | 2/30 | ||||
| Anticholinergic symptoms | Blurred vision | 1/30 | |||
| Sweating | 3/30 | ||||
| Electroacupuncture added low dose antipsychotics versus standard dose antipsychotics | Short term | Extrapyramidal symptoms | Overall | 5/30 | |
| Central Nervous System | Sleepiness | 1/30 | |||
| Anticholinergic symptoms | Dry mouth | 4/30 | |||
| Blurred vision | 2/30 | ||||
| Cardiovascular symptoms | Tachycardia | 5/30 | |||
| Laser acupuncture | |||||
| Laser acupuncture versus standard dose antipsychotics | Short term | Numbness over the ear, upper extremity and chest on the treated side | 1/20 | ||
| Sensation of heat at irradiated site and a feeling of plugged auditory canal | one third of participants of He‐Ne laser irradiation group | ||||
| Laser acupuncture added to low dose antipsychotics versus standard dose antipsychotics | Short term | Extrapyramidal symptoms | Overall | 7/10 | |
| Acupoint catgut treatment | |||||
| Acupoint catgut treatment added to standard dose antipsychotics versus standard dose antipsychotics | Short term | Local pain when eating | not reported | ||
| Acupoint catgut treatment added to low dose antipsychotics versus standard dose antipsychotics | Short term | Cardiovascular symptoms | Dizziness | 2/88 | |
| Tachycardia | 2/88 | ||||
| Electric acupuncture convulsive therapy | |||||
| Electric acupuncture convulsive therapy versus electroconvulsive therapy | Short term | Back pain | 2/34 | ||
| Spinal fracture | 5/34 | ||||
| Study | Kind of acupuncture | Acupoints choice | Fequency and duration | Sham acupuncture (yes/no) |
| Traditional acupuncture | Local points, distal points diagnosed by TCM | Once for 20 minutes and 3 times a week; total 10 times | Yes | |
| Main acupoints and adjunct acupoints according to the TCM syndrome differentiation | Manipulated needles every 10 minutes; for 30 minutes; 4 to 5 times a week and no less than 4 times; 1 month as 1 treatment course, 3 treatment course | No | ||
| Two acupoint groups in turn | For 30 minutes; once a day; 20 days as a treatment course and began another treatment course after 10 non‐treatment days; 3 months treatment courses | No | ||
| Juque, Tanzhong, Taichong, Jianshi, Fenglong, Daling, Yingtang | For 30 minutes; once a day; 5 days treatment with 2 days non‐treatment interval; 6 weeks | No | ||
| According to the type of TCM | Manipulated needles every 10 minutes; for 30 minutes; 3 to 4 times a week and not less than 3 times; 3 weeks as a treatment course and 1 week interval; total 3 treatment courses | No | ||
| Taichong (reducing method), Hegu (reducing method), Neiguan (straight inserted), Daling (straight inserted), Renzhong (reducing method), Dazhui (straight inserted) + other acupoints choice according to type of TCM | Continued to manipulate needles 3 to 5 minutes every ten minutes; for 45 minutes; once a day; 15 times as a treatment course; 2 treatment courses | No | ||
| Main acupoints and adjunct acupoints (according to the TCM type of schizophrenia) and special acupoints (according to symptoms) | Manipulated needles about 3 minutes and once ten minutes; total for about 30 minutes; at first once a day then reduced to once every two days when patient was in stable condition and once a week after psychiatric symptoms disappeared; 80 days | No | ||
| Shuigou, Shaoshang, Yingbai, Fengfu, Daling, Quchi, Fenglong | Once a day; for 30 minutes; 60 days | No | ||
| Xinshu, Ganshu, Pishu, Shenmen, Fenglong | Once a day; for 30 minutes; 60 days | No | ||
| Electroacupuncture | Baihui and Yingtang | For 50 minutes, once a day, 6 weeks | No | |
| Two acupoints groups in turn ‐ Baihui and Neiguan (double) group or Shuigou and Sanyingjiao (double) group | For 45 minutes; once a day; five days a week (except Saterday and Sunday); 12 weeks as a treatment course | No | ||
| Tinggong, Tinghui, Yifeng, Daling, Neiguan and Sanyijiao | For 20 minutes; 5 times a week; total 30 times (6 weeks) | Yes; needles were inserted less than 5 mm superficially and about 20 mm away from each corresponding acupoint and electroacupuncture connected was with no electrical current for 20 minutes | ||
| According to different symptoms | For 30 minutes; once two days; 20 times as a treatment course | No | ||
| Tanzhong, Zhongwan, Shenmen, Fenglong (double), Taichong (double), Neiguan (double) | For 5 minutes; once two days | No | ||
| Baihui, Shangxing, Yingtang, Sanyingjiao (double), Neiguan (double); added Zhongwan and Zusanli when with gastrointestinal uncomfortable symptoms and added Fenglong when with symptoms of the type of stagnation of phlegm and Qi | For 45 minutes; 5 times a week; 20 times as a treatment course; 8 weeks | No | ||
| Baihui and Taiyang (double) | Firstly continued to stimulate strongly 3 to 4 seconds then reduced the strength and frequency quickly, after patient's breath and face returned to normal and continued 30 to 60 seconds stimulated again; continued to stimulate 8 to 10 times; 3 times a week, total 8 weeks | No | ||
| Baihui, Fenglong, Houxi, Ganshu | For 30 minutes; once a day; 20 to 30 times as a treatment course; total 2 treatment courses | No | ||
| Yifeng, Tinggong, Tounjie, Chengling, Linqi, Baihui, Dingshen | Twice a day; adjustment of treatment depended upon the condition of the patient; 20 days | No | ||
| Group one [Yingtang and Baihui] and group two [Shenting and Yamen] | For 45 minutes; once a day; 8 weeks as a treatment course | No | ||
| Baihui and Yingtang | For 45 minutes; once a day; 5 days a week except Saturday and Sunday; 6 weeks as a treatment course | No | ||
| According to TCM types; main acupoints (Yintang tou xinqu, Daling, Neiguan, Taiyang) and supplemental acupoints (Zusanli [Yang deficiency] | Once a day except Sunday; 36 times as a treatment course (6 weeks) | No | ||
| Acupoint injection | According to the type of TCM (with Salviae Miltiorrhizae) | Two side acupoints in turn; once a day; 10 days as a treatment course; 7 days interval between two courses; 3 treatment courses | No | |
| Tinggong (double) (with Clonazepam) | Once two days; 7 times | No | ||
| Tinggong (double) (Sulpiride) | Once a day; 5 times as a treatment course; 2 intermittent treatment courses each month; total half a year | No | ||
| Laser acupuncture | Ermen (double) (He‐Ne laser irradiation) | For 15 minutes; once a day except Sunday; 30 times as a treatment course | Yes; sham laser irradiation; the tube of the laser emitter pointed in the direction of the ear without real irradiation | |
| Tinggong and Tinghui (He‐Ne laser irradiation) | For 30 minutes; once a day except Sunday | No | ||
| Two acupoint groups were used every other day alternately ‐ group 1 (Dazhui and Shenting); group 2 (Taiyang [double]) | For 15 minutes; once a day (except Sunday); 5 weeks as a treatment course | Yes; needles fixed with tape on acupoints | ||
| Acupoint catgut treatment | Tinggong | Once 7‐10 days; 6 weeks as a treatment course | No | |
| Tinggong (double) | 10 days as a treatment course; total 3 treatment courses | No | ||
| Electric acupuncture convulsive therapy | Renzhong and Baihui | Once every two days; 12 times as a treatment course | No |
| Comparison | Missing outcomes |
| ACUPUNCTURE added to STANDARD DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS | Death, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ACUPUNCTURE added to LOW DOSE ANTIPSYCHOTICS versus STANDARD DOSE ANTIPSYCHOTICS | Death, service outcomes, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ACUPUNCTURE versus STANDARD ANTIPSYCHOTICS | Death, service outcomes, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ACUPUNCTURE added to TCM DRUG versus TCM DRUG | Death, mental state, service outcomes, adverse effects, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ACUPUNCURE versus TCM DRUG | Death, mental state, service outcomes, adverse effects, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| ELECTRIC ACUPUCNTURE CONVULSIVE THERAPY versus ELECTRIC ACUPUNCTURE CONVULSIVE THERAPY | Death, global state, mental state, service outcomes, engagement with services, satisfaction with treatment, quality of life, economic outcomes |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 medium‐term (various similar criteria) | 3 | 244 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.28, 0.57] |
| 1.2 duration unclear | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.08] |
| 2 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse) Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 short‐term | 4 | 327 | Mean Difference (IV, Fixed, 95% CI) | ‐4.32 [‐5.28, ‐3.36] |
| 2.2 medium‐term | 3 | 220 | Mean Difference (IV, Fixed, 95% CI) | ‐5.51 [‐6.71, ‐4.30] |
| 3 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, medium‐term) ‐ subgroup analysis Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 traditional acupuncture | 2 | 156 | Mean Difference (IV, Random, 95% CI) | ‐7.95 [‐14.29, ‐1.61] |
| 3.2 acupoint injection | 1 | 64 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐5.02, 3.62] |
| 4 Mental state: 2a. General ‐ average score (PANSS, endpoint, high score = worse) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 short‐term | 4 | 245 | Mean Difference (IV, Fixed, 95% CI) | ‐2.47 [‐4.31, ‐0.63] |
| 4.2 medium‐term | 2 | 135 | Mean Difference (IV, Fixed, 95% CI) | ‐3.79 [‐6.43, ‐1.15] |
| 5 Mental state: 2b. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ subgroup analysis Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 traditional acupuncture | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 1.30 [‐1.56, 4.16] |
| 5.2 electroacupuncture | 3 | 185 | Mean Difference (IV, Random, 95% CI) | ‐5.64 [‐10.93, ‐0.35] |
| 6 Mental state: 2c. General ‐ average score (PANSS, endpoint, high score = worse, short‐term) ‐ electroacupuncture subgroup analysis Show forest plot | 2 | 135 | Mean Difference (IV, Fixed, 95% CI) | ‐3.79 [‐6.43, ‐1.15] |
| 7 Mental state: 2d. General ‐ average score (PANSS, endpoint, high score = worse) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 7.1 short‐term | Other data | No numeric data | ||
| 7.2 medium‐term | Other data | No numeric data | ||
| 8 Mental state: 2e. General ‐ not improved (PANSS), endpoint Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 reduced rate < 25%, short‐term | 3 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.45, 0.94] |
| 8.2 reduced rate < 30%, short‐term | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.43, 1.92] |
| 8.3 reduced rate < 30%, follow‐up, medium‐term | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.36, 1.31] |
| 9 Mental state: 3. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 10 Mental state: 4a.Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 short‐term | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐7.66 [‐13.05, ‐2.27] |
| 10.2 medium‐term | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐12.35 [‐17.54, ‐7.16] |
| 11 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 11.1 traditional acupuncture | Other data | No numeric data | ||
| 11.2 electroacupuncture | Other data | No numeric data | ||
| 12 Mental state: 5a. Specific ‐ average score ‐ depression (HAMD, endpoint, high score = worse, short‐term) Show forest plot | 2 | 109 | Mean Difference (IV, Random, 95% CI) | ‐8.66 [‐12.10, ‐5.22] |
| 13 Mental state: 5b. Specific ‐ not improved ‐ depression (HAMD, reduced rate < 25%, short‐term) Show forest plot | 2 | 109 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.08, 0.34] |
| 14 Mental state: 7b. Specific ‐ not improved ‐ auditory hallucinations (PSYRAS‐AH, reduction < 20%, short‐term) Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.14, 0.52] |
| 15 Mental state: 7a. Specific ‐ average score ‐ auditory hallucinations (PSYRAS‐AH,endpoint, high score = worse, short‐term) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.17 [‐4.16, ‐0.18] |
| 16 Mental state: 6. Specific ‐ average score ‐ depression (SDS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | ‐24.25 [‐28.01, ‐20.49] |
| 17 Mental state: 8. Specific ‐ not improved (auditory hallucinations, endpoint) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 still existed after 30 days, short‐term | 1 | 216 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.13, 0.44] |
| 17.2 still existed or appeared frequently after disappeared, medium‐term | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.17, 0.61] |
| 17.3 no change of auditory hallucinations, duration unclear | 1 | 120 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.17] |
| 18 Mental state: 9. Specific ‐ average score ‐ auditory hallucinations (SAHS, endpoint, high score = worse) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 18.1 short‐term | Other data | No numeric data | ||
| 18.2 medium‐term | Other data | No numeric data | ||
| 19 Mental state: 10. Specific ‐ average score ‐ hallucinations (BPRS [12th item], endpoint, high score = worse, short‐term) Show forest plot | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.73 [‐1.28, ‐0.18] |
| 20 Behaviour: Leaving the study early Show forest plot | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 short‐term | 10 | 870 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.33, 5.45] |
| 20.2 medium‐term | 5 | 370 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.58 [0.60, 21.27] |
| 21 Service outcomes: Time in hospital (days) Show forest plot | 1 | 120 | Mean Difference (IV, Fixed, 95% CI) | ‐16.0 [‐19.54, ‐12.46] |
| 22 Adverse effects: 1. General ‐ average score (TESS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐2.80 [‐3.09, ‐2.51] |
| 23 Adverse effects: 2a. Specific ‐ extrapyramidal symptoms Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 23.1 short‐term ‐ overall | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.40, 1.09] |
| 23.2 short‐term ‐ specific ‐ akathisia | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.23, 1.48] |
| 23.3 short‐term ‐ specific ‐ tremor | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.24, 2.18] |
| 23.4 medium‐term ‐ overall | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.32, 1.23] |
| 23.5 medium‐term ‐ specific ‐ myotonia | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 15.26] |
| 23.6 medium‐term ‐ specific ‐ tremor | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.71] |
| 23.7 medium‐term ‐ specific ‐ akathisia | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.6 [0.16, 2.29] |
| 24 Adverse effects: 2b. Specific ‐ extrapyramidal symptoms ‐overall (short‐term) ‐ subgroup analysis Show forest plot | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.40, 1.09] |
| 24.1 traditional acupuncture | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.02, 1.30] |
| 24.2 electroacupuncture | 2 | 142 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.47, 1.34] |
| 25 Adverse effects: 3. Specific ‐ Central Nervous System Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 25.1 medium‐term ‐ anxiety | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.09, 2.05] |
| 25.2 short‐term ‐ insomnia | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.11, 0.83] |
| 25.3 medium‐term ‐ insomnia | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.12, 1.02] |
| 25.4 medium‐term ‐ headache | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.33, 27.23] |
| 26 Adverse effects: 4. Specific ‐ anticholinergic symptoms Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 26.1 short‐term ‐ dry mouth | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.47, 3.00] |
| 26.2 short‐term ‐ blurred vision | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.24, 3.24] |
| 26.3 medium‐term ‐ blurred vision | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.64] |
| 26.4 medium‐term ‐ sweating | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.83] |
| 26.5 short‐term ‐ constipation | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.19, 4.06] |
| 26.6 short‐term ‐ nausea & vomiting | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.12, 1.32] |
| 27 Adverse effects: 5. Specific ‐ gastrointestinal system Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 27.1 medium‐term ‐ unspecified gastrointestinal symptoms | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.10, 2.71] |
| 27.2 short‐term ‐ constipation | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.19, 4.06] |
| 27.3 short‐term ‐ nausea & vomiting | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.12, 1.32] |
| 28 Adverse effects: 6. Specific ‐ cardiovascular symptoms (or headache) Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 28.1 short‐term ‐ dizziness | 3 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.32, 2.75] |
| 28.2 medium‐term ‐ dizziness or headache | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.04, 3.22] |
| 28.3 short‐term ‐ tachycardia | 3 | 217 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.42, 1.79] |
| 28.4 medium‐term ‐ tachycardia | 2 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.04, 3.20] |
| 29 Adverse effects: 7a. Specific ‐ metabolic system Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 29.1 short‐term ‐ weight gain | 3 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.02, 37.33] |
| 29.2 medium‐term ‐ weight gain | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.01, 4.23] |
| 30 Adverse effects: 7b. Specific ‐ metabolic system ‐ weight gain (short‐term) ‐ subgroup analysis Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 30.1 traditional acupuncture | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.65] |
| 30.2 electroacupuncture | 2 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 6.15 [0.33, 115.01] |
| 31 Adverse effects: 8. Specific ‐ endocrine system Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 31.1 short‐term ‐ irregular menstruation | 2 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.87] |
| 32 Adverse effects: 9. Specific ‐ lab test Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 32.1 short‐term ‐ liver function abnormal | 4 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.26, 3.90] |
| 32.2 medium‐term ‐ liver function abnormal | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.12, 3.98] |
| 32.3 short‐term ‐ ECG abnormal (myocardial ischaemia) | 4 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.05, 5.32] |
| 32.4 short‐term ‐ blood routine test abnormal (leukocyte change) | 4 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.32, 5.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: 1. Relapse (follow‐up, long‐term) Show forest plot | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.37, 0.89] |
| 2 Global state: 2. Not improved (various similar criteria), endpoint (short‐term) Show forest plot | 4 | 272 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.40, 1.72] |
| 2.1 no symptoms improved obviously and insight did not recover | 1 | 32 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 3.86] |
| 2.2 symptoms and orientation showed no change | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.9 [0.30, 2.68] |
| 2.3 according to traditional criteria | 2 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.35, 3.02] |
| 3 Global state: 3a. CGI ‐ average score ‐ CGI‐SI (endpoint, high score = worse, short‐term) Show forest plot | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐1.08, 0.28] |
| 4 Global state: 3b. CGI ‐ average score ‐ CGI‐GI (endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 5 Global state: 3c. CGI ‐ average score ‐ CGI‐EI (endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 6 Mental state: 1a. General ‐ average score (BPRS, endpoint, high score = worse) Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 short‐term | 5 | 332 | Mean Difference (IV, Random, 95% CI) | ‐5.55 [‐14.40, 3.29] |
| 6.2 long‐term | 1 | 137 | Mean Difference (IV, Random, 95% CI) | ‐4.87 [‐8.21, ‐1.53] |
| 7 Mental state: 1b. General ‐ average score (BPRS, endpoint, high score = worse, short‐term) ‐ subgroup analysis Show forest plot | 4 | 300 | Mean Difference (IV, Fixed, 95% CI) | ‐1.36 [‐3.13, 0.41] |
| 7.1 traditional acupuncture | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 3.03 [‐1.22, 7.28] |
| 7.2 electroacupuncture | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐4.5 [‐9.35, 0.35] |
| 7.3 acupoint injection | 1 | 160 | Mean Difference (IV, Fixed, 95% CI) | ‐1.87 [‐4.04, 0.30] |
| 7.4 laser acupuncture | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐12.40, 9.40] |
| 8 Mental state: 1c. General ‐ not improved (BPRS, short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 1.1 reduced rate < 30% | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.07] |
| 8.2 1.2 reduced rate < 25% | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.31, 1.25] |
| 8.3 1.3 reduced rate ≤ 20% | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.9 [0.30, 2.68] |
| 9 Mental state: 1d. General ‐ average change scores (BPRS, low score = worse, short‐term) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.81 [‐3.17, 4.79] |
| 10 Mental state: 2a. General ‐ Average score (PANSS, endpoint, high score = worse, short‐term) ‐ Skew data Show forest plot | Other data | No numeric data | ||
| 11 Mental state: 2b. General ‐ not improved (PANSS, reduced rate < 30%, short‐term) Show forest plot | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.57, 2.62] |
| 12 Mental state: 3a. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 traditional acupuncture | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐13.34 [‐16.94, ‐9.74] |
| 12.2 acupoint catgut treatment | 1 | 180 | Mean Difference (IV, Random, 95% CI) | 1.21 [0.96, 1.46] |
| 13 Mental state: 3b. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 14 Mental state: 4a. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 0.61 [‐3.30, 4.52] |
| 15 Mental state: 4b. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 16 Behaviour: Leaving the study early (short‐term) Show forest plot | 8 | 662 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.29, 2.29] |
| 17 Adverse effects: 1a. General ‐ average score (TESS, endpoint, high score = worse, short‐term) Show forest plot | 2 | 200 | Mean Difference (IV, Fixed, 95% CI) | ‐0.56 [‐0.86, ‐0.26] |
| 18 Adverse effects: 1b. General ‐ average score (TESS, endpoint, high score = worse, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 19 Adverse effects: 2. Specific ‐ average score (RESES, endpoint, high score = worse, short‐term) Show forest plot | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐0.6 [‐0.73, ‐0.47] |
| 20 Adverse effects: 3. Specific ‐ extrapyramidal symptoms (short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 overall | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.16, 0.46] |
| 20.2 specific ‐ myotonia | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.29] |
| 20.3 specific ‐ tremor | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.69] |
| 20.4 specific ‐ akathisia | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.49] |
| 21 Adverse effects: 4. Specific ‐ Central Nervous System (short‐term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 21.1 activity increasing | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.85] |
| 21.2 insomnia | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.00, 1.20] |
| 21.3 sleepiness | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.03] |
| 22 Adverse effects: 5. Specific ‐ anticholinergic symptoms (short‐term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 22.1 dry mouth | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.09, 0.58] |
| 22.2 nasal congestion | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.69] |
| 22.3 blurred vision | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.06, 0.83] |
| 22.4 constipation | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.00, 1.20] |
| 23 Adverse effects: 6. Specific ‐ cardiovascular symptoms (short‐term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 23.1 dizziness | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.12, 4.07] |
| 23.2 tachycardia | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.11, 0.53] |
| 24 Adverse effects: 7. Specific ‐ skin infection (short‐term) Show forest plot | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint (short‐term) Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 various similar criteria | 3 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.53, 1.48] |
| 1.2 talk, behaviour and expression still existed as before + reduction of BPRS < 29% | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.19, 0.59] |
| 2 Mental state: 1. General ‐ average score (BPRS, endpoint, high score = worse, short‐term) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 traditional acupuncture | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐11.56 [‐16.36, ‐6.76] |
| 2.2 laser acupuncture | 1 | 21 | Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐11.19, 9.05] |
| 3 Mental state: 2. Specific ‐ average score ‐ positive symptoms (SAPS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | ‐5.24 [‐9.06, ‐1.42] |
| 4 Mental state: 3. Specific ‐ average score ‐ negative symptoms (SANS, endpoint, high score = worse, short‐term) Show forest plot | 1 | 32 | Mean Difference (IV, Fixed, 95% CI) | ‐7.92 [‐17.01, 1.17] |
| 5 Behaviour: Leaving the study early (short‐term) Show forest plot | 6 | 421 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Adverse effects: 1. General ‐ average scores (TESS, endpoint, short‐term) ‐ Skewed data Show forest plot | Other data | No numeric data | ||
| 7 Adverse effects: 2. Specific ‐ extrapyramidal symptoms (short‐term) Show forest plot | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.00, 0.83] |
| 8 Adverse effects: 3. Specific ‐ numbness over the ear, upper extremity and chest on the treated side (short‐term) Show forest plot | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.52] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint (short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 talk, behaviour and expression still existed as before + reduction of BPRS < 29% | 2 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.02, 0.59] |
| 1.2 no change in symptoms | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.57, 1.06] |
| 2 Behaviour: Leaving the study early (short‐term) Show forest plot | 3 | 454 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: Not improved, endpoint (short‐term) Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 talk, behaviour and expression still existed as before + reduction of BPRS < 29% | 2 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.74, 2.87] |
| 1.2 no change in symptoms | 1 | 88 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.34, 0.80] |
| 2 Behaviour: Leaving the study early (short‐term) Show forest plot | 3 | 328 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Behaviour: Leaving the study early (short‐term) Show forest plot | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Adverse effects: 1. Specific ‐ back pain (short‐term) Show forest plot | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.12, 3.74] |
| 3 Adverse effects: 2. Spinal fracture (short‐term) Show forest plot | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.14, 0.81] |


