Ambiente sensorial para mejorar los desenlaces relacionados con la salud en pacientes hospitalizados
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ‘‘Patients were sequentially selected from the patient rosters of two ophthalmic surgeons. [...] On each day data collection surgeons were randomly assigned to have their patients in the experimental or control group.’’ Method of randomisation not stated. |
| Allocation concealment (selection bias) | High risk | "Office assistants were unaware of the study prepared patient rosters. On each day data collection surgeons were randomly assigned to have their patients in the experimental or control group. Patients were then approached in the waiting room and asked to participate in the study." Patients approached after allocation. |
| Blinding (performance bias and detection bias) | High risk | Not extracted for review (validity of measurement scales unclear). |
| Blinding (performance bias and detection bias) | Low risk | Automated measurement of physiological data via Propaq Monitor. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. Physiological outcomes reported for all included patients. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Music allocated on an individual basis via headphones. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subsequently, patients were divided randomly into the experimental group or the control group by the flip of a coin." |
| Allocation concealment (selection bias) | High risk | Patients were randomised after consent by the flip of a coin. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of their group allocation. "During the procedure, patients did not inform either the explorer of assistant whether they belonged to the experiemental group or the control group." |
| Blinding (performance bias and detection bias) | Low risk | Patients aware of their group allocation. "During the procedure, patients did not inform either the explorer of assistant whether they belonged to the experiemental group or the control group." |
| Incomplete outcome data (attrition bias) | Unclear risk | Description of withdrawals and drop‐outs: 3 patients excluded as had taken anxiolytic drugs within 72 hours prior to procedure. Missing data unclear. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Music allocated to individuals via headphones. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not descibed. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear whether measurements of physiological outcomes were automated. |
| Incomplete outcome data (attrition bias) | Low risk | Description of withdrawals and drop‐outs: 7 patients were excluded due to incomplete outcome data. Outcomes reported for > 80% of participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Music allocated to individuals via headphones. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomized into three groups." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | "The research team consisted of a nonblinded member who randomized participants and administered the intervention" Allocation concealment not described. |
| Blinding (performance bias and detection bias) | Low risk | "An external power switch was connected to the opaque box and power was temporarily turned off before each OAA/S was determined to assure blindness of the outcomes assessor". |
| Blinding (performance bias and detection bias) | Low risk | "Vital signs [...], propofol consumption, and OAA/S score were documented every 5 min by the blinded researcher". |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Individuals allocated to groups and all wore headphones. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients who consented were immediately randomized [...] by selecting a randomly generated group number [...]" |
| Allocation concealment (selection bias) | Low risk | "randomly generated group number sealed in an opaque envelope" |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | Outcome assessors aware of group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | "113 (87.6%) agreed to participate [...].We have complete data on 107 patients. Six patients (4 controls, 2 experimental) were not included because the procedure was cancelled after their enrolment or they could not complete all the questionnaires because of complications." |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR and BP. |
| Protection from contamination? | Low risk | Individuals allocated to the music group listened via headphones. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The researcher randomly assigned subjects to one of the three intervention groups by drawing lots" |
| Allocation concealment (selection bias) | High risk | "After written consent was obtained from the subject, the researcher randomly assigned subjects [...]. A slip of paper was drawn out of the box before requesting participation. If the subject consented to participate, the slip of paper was thrown away; if the subject did not agree to participate, the slip of paper was put back in the box." |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Physiological data not described in enough detail for use in review. |
| Incomplete outcome data (attrition bias) | Unclear risk | "All participants enrolled in the study participated in both sessions". Missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: BP and HR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients who met the study criteria were assigned to the control or experimental groups by using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear if the anaesthetist was blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, drop‐outs and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly assigned to one of three groups." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Length of stay and narcotics usage ‐blinding unclear. |
| Incomplete outcome data (attrition bias) | Low risk | "100 patients were enrolled. Two patients who died in hospital were excluded from the final data analysis. Three patients whose hospitalization following surgery lasted longer 14 days were also excluded from the final data analysis." Data presented for 95 remaining participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by drawing lots in a blinded fashion. |
| Allocation concealment (selection bias) | Low risk | Randomised by drawing lots in a blinded fashion. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | HR and BP automated measurement with Hewlett‐Packard Component Monitoring System or a DINAMAP. Healthcare staff removing chest tubes were blinded to which tape patients were listening to. |
| Incomplete outcome data (attrition bias) | Low risk | 4 participants withdrew (reasons and group allocation not described), 3 participants had cancelled surgery, 11 had chest tube removal prior to baseline data collection, 3 participants were suffering from confusion, 9 had an unstable condition preventing chest tube removal, 2 had equipment failure, and one person died. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were assigned using a table of random numbers to either group" |
| Allocation concealment (selection bias) | Unclear risk | "Patients who consented to participate were then given a number that had been preassigned [...]. Patients became aware of their assigned group after they signed the consent." No description of whether the person recruiting patients knew the assignments in advance. |
| Blinding (performance bias and detection bias) | High risk | "The patients and staff were not blinded to assignment" |
| Blinding (performance bias and detection bias) | High risk | "The patients and staff were not blinded to assignment" |
| Incomplete outcome data (attrition bias) | Low risk | "A total of 190 persons were recruited, 20 refused, and 170 persons completed the study." Does not describe if the 20 refusals occurred before or after randomisation, or reasons for refusal. Data reported for 170 participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomized to either the treatment or control group by means of a table of random numbers." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) | High risk | Outcome assessors aware of group assignment. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomly allocated by the nurse to two groups using a computer‐generated list" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear if patients were aware of the difference between the two groups. Patients in the control group were played music after the outcome measures had been taken, for 10 minutes at the conclusion of the procedure. |
| Blinding (performance bias and detection bias) | Low risk | Anaesthesiologist blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | "There were no drop‐outs." |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The subjects were randomly assigned to either a music or no‐music group by the research nurse using a computer‐generated random number series [...]" |
| Allocation concealment (selection bias) | Low risk | "computer‐generated random number series contained within closed opaque envelopes." |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Objective outcomes not addressed by this study. |
| Incomplete outcome data (attrition bias) | Low risk | "all subjects completed the STAI form again and assessed their degree of pain" "220 women were entered into the trial and all of them completed the study" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Forty six participants were included in the study, using a random digit generated by research randomizer (Research Randomizer 2005)." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear if physiological outcome measures were automated. |
| Incomplete outcome data (attrition bias) | Unclear risk | "Three participants in the music group expressed a dislike of the music that they had chosen. They refused to continue to participate and their data were withdrawn from the analysis" "Missing values were replaced by the group mean" Amount of missing data values not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly allocated to experimental and control groups." Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients in the control group were not aware they had not had the opportunity to listen to music. |
| Blinding (performance bias and detection bias) | Low risk | Physiological outcomes were measured via automated system. |
| Incomplete outcome data (attrition bias) | Low risk | 6 withdrew from the music group for the following reasons:"(a) lost interest (n = 2), (b) received nitrous oxide or sedative (n=2), (c) had a newborn with imperforate anus (n = 1) or had failure of local anesthesia (n = 1)" 6 withdrew from the control group for the following reasons: "(a) had emergency caesarean section (n = 2) and (b) received nitrous oxide or sedative (n = 4)" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Unclear risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Each subject was randomized." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | Physiological measures recorded via range of means, some automated others not. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR, BP, and RR. |
| Protection from contamination? | Unclear risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "With use of a table of random numbers, subjects were randomized to either a control group or to an experimental group" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | Respiration rate measured via observation. Outcome assessor not blinded. Heart rate measured via bedside monitor. |
| Incomplete outcome data (attrition bias) | Low risk | "Among the 54 subjects who signed consent forms, two withdrew after instrument administration for personal reasons. Three subjects withdrew at various times during the assigned treatment conditions, two in the experimental group and one from the control group. Reasons given for with‐drawal were personal (i.e., tired of lying still or were too anxious) or, in one instance, because the subject was scheduled for a diagnostic test." |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR and RR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects who consented to participate in the study were randomized by a coin‐flip to either an experimental condition or control condition" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. "All subjects completed the NRS‐discomfort instrument, followed by the state anxiety scale" ‐implies no missing data. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "They were randomly assigned to experimental [...] and control [...] group" Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Unclear risk | This study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) | Unclear risk | Method of collecting blood pressure data not described. Unclear if automated. Heart rate variability measured via electrocardiogram (ECG). |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "using a random‐numbers table" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Data in tables presented for all included participants. Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer‐generated list was used for permuted block random assignment" |
| Allocation concealment (selection bias) | Low risk | "A biostatistician and research assistant who did not participate in data collection conducted the randomization procedures and prepared sequentially numbered sealed envelopes containing the random assignment for each consenting patient" |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "there were no drop‐outs" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was by patients selecting from a bag one of four different tapes in a blinded fashion" |
| Allocation concealment (selection bias) | Low risk | "Randomization was by patients selecting from a bag one of four different tapes in a blinded fashion" |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear if outcome assessor of vital signs was blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, HR, BP, and RR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety. |
| Protection from contamination? | Low risk | Intervention administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "With the use of a Latin square design, the three musical selections (A, B, C) were randomly assigned to be presented to the patients in one of three different orders. Whether patients listened to either the music or the control period first was also randomly varied." Method of random sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Questionairre not fully validated; not extracted for review. Patients aware of group assignment. |
| Blinding (performance bias and detection bias) | High risk | Automated recording of heart rate and respiratory rate, but data then determined from graphs by investigator ("the taped waveforms were off the scale because of a malfunction of the indicator needle"). |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: RR. |
| Protection from contamination? | High risk | Cross‐over study. Duration of wash‐out period unclear. "The patients were continuously monitored for two 42‐minute periods in the same day." |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The unit of assignment to intervention or control status was an entire day of FB procedures. The allocation schedule was generated by having a study member place equal numbers of intervention and control assignments in opaque envelopes. Each day at 4:00 PM, two other study members (not those who filled the envelopes) opened one of the envelopes to determine the next day’s assignment.’’ |
| Allocation concealment (selection bias) | Unclear risk | No information is given on concealment of allocation for patients. However “bronchoscopists could not know the assignment at the time that they scheduled their patients’’ |
| Blinding (performance bias and detection bias) | High risk | For this intervention, it was not possible to blind patients. |
| Blinding (performance bias and detection bias) | Unclear risk | The study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. Paper reports more than 10% of data for the outcome pain was missing (unclear exactly how much data was missing), and an imputation algorithm was used. Analyses were repeated with and without imputation, and the results were similar in both. Other outcomes had no more than 10% missing data; for these outcomes, missing values were substituted with the median (for ordinal and continuous outcomes) or mode (for nominal outcomes). |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Pain. |
| Protection from contamination? | Low risk | Interventions administered for an entire day. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects were then randomized, according to a computer‐generated random‐numbers table" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "Six subjects withdrew consent before randomization for the following reasons: one was late for a meeting, one did not want to be in a control group, one stated that reading the questions made her “feel depressed,” one changed her mind, one did not have enough time before being called in for the mammography, and one did not like the wording of the consent form. A seventh subject was not included in data analysis because she later reported that she did indeed have a current psychiatric illness, thus making her ineligible." |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 20 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Pre‐stratification of patients was achieved by a simple nine‐question risk score [...] This was designed empirically by one of us (KP), and had face validity, but has not been subjected to any other validation. This provided a score from 0 (low risk) to 9 (high risk), and was used to stratify patients into low (0‐2), medium (3‐4) or high (>4) perceived risk of falling prior to randomization. Using randomized envelopes for each risk group, patients were assigned to a floor group (carpet or vinyl) and a physiotherapy group [...]." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Study was not blinded. |
| Blinding (performance bias and detection bias) | High risk | Study was not blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Linoleum floor‐ 1 patient died, 2 were transferred, 7 did not comply with repeated therapy‐related outcome measurements; Carpet floor‐ 5 died, 1 patient was transferred, 6 patients did not comply with repeated therapy‐related outcome measurements. There is not a problem with the flooring‐related outcomes (falls) in this study, but 40% missing data for therapy‐related outcomes (not included in review). |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: length of stay. |
| Protection from contamination? | High risk | "two patients allocated to carpet were nursed on vinyl becasue they required side‐rooms" |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 6 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly placed in the hospital rooms by the hospital administration upon their admission to the hospital" ‐ Method of randomisation not described. |
| Allocation concealment (selection bias) | High risk | Patients were recruited into the study on their final day of hospital stay (after they had been allocated to a room). |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | Length of stay and drug requests objectively recorded. |
| Incomplete outcome data (attrition bias) | Unclear risk | "Eleven patients who were approached could not be used in the study. Three patients explained that they would just prefer not to participate. Two of the patients were considered legally colorblind. [...] One patient was extremely confused and could not understand the information being explained to him. [...] One patient felt uncomfortable with having the principal investigator examine his medical records [...]. One patient was considered extremely depressed by the nurse manager and was not approached to participate in the study and two patients could not speak English [...]. Lastly, one patient was extremely nervous and worried that the anxiety test would reveal that that she should have to stay in the hospital for an extended amount of time. It was therefore the researcher’s opinion that she altered her answers on the test to make it appear as though she had no anxiety in her life." It is unclear from which rooms withdrawals came. Data of remaining included patients appears complete. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, pain medication, and length of stay. |
| Protection from contamination? | Low risk | Patients assigned to individual rooms. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The study was a randomized, controlled trial." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) | High risk | Blood pressure was nurse‐assessed (not blinded). Heart rate was automated. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and dropouts not described. Data presented for all included participants. "The study examined the anxiety of 56 patients. [...] Fifty‐six subjects completed the study." |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 15 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Cases of Invasive aspergillosis were recorded as suspected or proven. Staff would have been aware of intervention. |
| Blinding (performance bias and detection bias) | High risk | Staff would have been aware of presence or absence of portable air filtration units. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. It is unclear if outcome data are complete. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Intervention assigned to patient rooms. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were assigned randomly." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | Unclear who assessed vomiting. There was no blinding of healthcare personnel, patients, or researchers. |
| Incomplete outcome data (attrition bias) | High risk | "Three control group patients were dropped from the study because measurements were not taken at baseline or at a minimum of four of the other six data collection points. A fourth patient requested to learn relaxation therapy in addition to the music and therefore was not included. An additional two patients in the music intervention group were dropped from the study because they did not listen to music at the prescribed time intervals." (15% of participants withdrawn). Outcomes were obtained for >80% of included participants at 8 hours follow‐up but not at 16 hours follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were randomly assigned." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | Vital signs measurement automated. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, HR, BP, and RR. |
| Protection from contamination? | Unclear risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 28 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Assignment to rooms was not controlled or formally randomized but was based on scheduling rules and OR availability" |
| Allocation concealment (selection bias) | High risk | Rule‐based system. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear level of blinding for assessment of outcomes. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear level of blinding for assessment of outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Participants assigned to rooms on individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were assigned randomly to one of the three groups." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | WIthdrawals and drop‐outs not described. Data reported for all 15 included participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Each research assistant randomly assigned subjects by lottery to one of three groups" Method of randomisation not clearly described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, dropouts, and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "they were assigned, using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) | Low risk | All patients wore headphones. "no hospital personnel were allowed to communicate with the patient. [...] scores were measured [...] by a blinded observer. To test observer blinding, the observer was asked whether he recognized the patient's group at any stage during the study period. [...] four patients were excluded because of failure in observer blinding after a technical problem." |
| Incomplete outcome data (attrition bias) | Unclear risk | "Four patients (three in the music and one in the control group) were excluded from the study because of technical problems related to the music player." Missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Random assignment [...]” Method of randomisation not described. |
| Allocation concealment (selection bias) | Low risk | “Random assignment was conducted by telephone to a separate data management centre. Patients and physicians were blinded to product allocation.” |
| Blinding (performance bias and detection bias) | High risk | Blinding was not done for non‐fragrant 'placebo' group, but was done for the pure essential oil and fragrant placebo groups. Although patients were not told their group allocation, only 9% of the non‐fragrant placebo group believed they had received the essential oil, compared to 25% of the fragrant placebo and 24% of the pure essential oil (P = 0.006). Therefore the non‐fragrant 'placebo' was not a true placebo control. |
| Blinding (performance bias and detection bias) | Unclear risk | The study did not assess this outcome. |
| Incomplete outcome data (attrition bias) | Low risk | Withdraws or dropouts: “The reason for not receiving the full number of possible aromatherapy treatments included research assistant illness and absence, failure to complete the planned radiotherapy course, and withdraw from receiving aromatherapy. Of the 313 patients who were randomly assigned, 285, 286, and 295 completed baseline, HADS anxiety (HADSA), HADS depression (HADSD), and SPHERE questionnaire, respectively providing 91% to 94% questionnaire compliance for analysis of these scores. There was no significant difference in missing data by allocated arms.” |
| Selective reporting (reporting bias) | Unclear risk | There may be a risk of bias from selective outcome reporting, given that the results are presented as the proportion of participants whose score on an ordinal variable exceeded a cut‐off point (> 7); the data could instead have been reported as mean and SD. Normative data for the HAD suggest ≤7 is normal, 8 to 10 is borderline, and ≥11 may indicate clinically relevant anxiety (Millar 1995); this presents a rationale for the cut‐off. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation via computer generated list. |
| Allocation concealment (selection bias) | High risk | Not done. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | Automated outcome assessment. |
| Incomplete outcome data (attrition bias) | Unclear risk | 5 in the control group and 2 in the music group were excluded after moving to other room. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were allocated into two groups using computer‐generated random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | Recovery room nurse who was "unaware of the group allocation" assessed time to recovery. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, dropouts, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiolytic medication |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomized using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | "Patients were unaware of their group assignment until they signed the consent form" Unclear if person recruiting patients had allocation concealment. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear if measurement of physiological outcomes was automated. |
| Incomplete outcome data (attrition bias) | Low risk | "Two hundred persons were enrolled and two were dropped due to incomplete data" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The subjects were randomly placed into three groups." Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | BP and HR monitored via automated machine. RR measured via counting rate for 1 minute. "The nurse caring for the subject was partially blinded and only knew whether the subject had headphones, but did not know which subjects received music." |
| Incomplete outcome data (attrition bias) | Unclear risk | Missing data not described. "A total of 60 subjects were studied, 20 in each study group. An additional three patients consented but were excluded. Two patients were non‐complaint with the study protocol and one patient had extended surgery." |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR, BP, and RR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | “The communal area of the unit was diffused [...], on alternate days [...].” |
| Allocation concealment (selection bias) | High risk | Not described‐ although CCT design means the sequence was predictable. |
| Blinding (performance bias and detection bias) | Low risk | Agitation measured by "an experienced independent blinded (using nose callipers prior to entry onto the ward) rater, unaware of the study design" |
| Blinding (performance bias and detection bias) | Unclear risk | The study did not address this outcome. |
| Incomplete outcome data (attrition bias) | Low risk | "Fifteen patients were recruited [...]. For each subject 10 total PAS scores were obtained." Results were obtained from all the patients that were recruited and therefore it is indicated that there were no dropouts or withdrawals. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | High risk | Cross‐over trial. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were assigned randomly." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | "The CDs were unmarked, and the content was unknown to the nurse starting the CD player. [...] All were told [...] that the investigators were to remain blinded as to which CD was used. [...] HR, noninvasive BP, mid RR were measured by an attending nurse who was unaware of the CD's content." |
| Incomplete outcome data (attrition bias) | Low risk | "Five patients ‐ three from M group and two from C group ‐ were excluded from the calculations because of extended surgery or various technical problems on the ward" |
| Selective reporting (reporting bias) | High risk | Reports systolic blood pressure but not diastolic blood pressure. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects wishing to participate were assigned to 1 of the 3 treatment groups by a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "One subject withdrew after consenting, but before data collection." Group allocation or reason not described. Data described for all included participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 33 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The Ss were randomly assigned to the eight experimental conditions‐with the one constraint that the experimental room randomly assigned to one E‐S pair dictate the room to be used by the other E‐S pair. Within that constraint, time of ratings by Ss was randomized." ("E‐S pair" refers to psychiatrist‐participant pair). This has been interpreted to mean that although 'time of data collection' is reported as randomised, the variable 'room' was not randomly allocated, as it was dependent on the previous allocation. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Study was not blinded. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: mood. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "One of three numbered but unlabelled tapes was randomly assigned to the patient by computer‐generated random number table. The randomisation was stratified according to estimated length of stay (less than 2 days and more than this)." |
| Allocation concealment (selection bias) | Unclear risk | Unclear if the person recruiting patients was aware of the randomisation schedule. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address subjective outcomes |
| Blinding (performance bias and detection bias) | Low risk | Fentanyl requirements: "throughout the study, the anaesthetist remained unaware of the nature of the tape" |
| Incomplete outcome data (attrition bias) | Low risk | "Eighty‐three of these gave their informed consent but seven later revoked this in the induction room" Description of reasons and group allocation not given. Data presented on all remaining included participants. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomized into either control or a music group using a Table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Unclear risk | This study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) | High risk | "Thus, the observer was not blinded to group assignment." |
| Incomplete outcome data (attrition bias) | Low risk | "Two patients were removed from the study secondary to the need for general anaesthesia and inadvertent departure from the study design." |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned." Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear if physiological measures were automated. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and dropouts not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States that participants were randomly assigned but does not say how the sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Low risk | Patients were unaware of which study group they were in. Intervention took place during surgery. |
| Blinding (performance bias and detection bias) | Low risk | Clinical staff and experimenter were blinded to study groups. |
| Incomplete outcome data (attrition bias) | Unclear risk | "Sämtliche Patientinnen (N = 163) konnten in die Auswertung aufgenommen werden. Von 23 Patientinnen liegt kein vollständiges Protokoll des Analgetikaverbrauchs in der Aufwachphase vor. Die Auswertung des Analgetikaverbrauchs bezieht sich daher auf eine Stichprobe von n = 140." All 163 patients were included in the analysis. However, there is incomplete data on analgesic consumption for 23 patients, so this outcome is based on 140 patients (unclear how many patients per group). |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions were administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly assigned" Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear how physiological outcomes were measured and if these were automated. |
| Incomplete outcome data (attrition bias) | High risk | Withdrawals and dropouts not described. "Blood pressure and heart rate were recorded in all the patients in the music as well as without music group. Respiratory rate was recorded in 34 and 29 patients in the music and without music group respectively." (RR measured for < 80% of participants) |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization was completed within categories of procedures [...] to ensure that the different types of procedures were distributed equally among the three study groups" Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | This study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "Data from two participants were excluded from analyses because experimental conditions had been contaminated. One participant assigned to the distraction group had an unusually long wait on the procedure table and requested music in addition to the distraction stimulus. One participant assigned to the control group was exposed to music when the surgeon requested that it be played while he was in the room" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Two participants were excluded due to "contamination" |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomly assigned by using computer generated numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | "All assessors were blinded as to the group to which patients were assigned" |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and dropouts not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ‘‘Participants were randomly assigned using computer‐generated numbers into three groups’’ |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients could not be blinded to this intervention. Patients reported pain and satisfaction and controlled the level of sedation. |
| Blinding (performance bias and detection bias) | Low risk | "Group 1 patients wore the same Eyetrek system with earphones even though they had no music to listen to. As a result, the endoscopists did not know whether patients were in group 1 or group 2". Endoscopists were not blinded to patients in group 3 (patient‐controlled sedation alone). Unclear who assessed number of hypotensive episodes and oxygen desaturation. Recovery nurses assessed recovery time. "All recovery nurses were blinded as to the sedation group to which patients had been assigned". |
| Incomplete outcome data (attrition bias) | Low risk | ‘‘Eight patients were excluded after randomization: four patients had incomplete assessment forms and four patients did not receive proper PCS due to mechanical failure during the procedure.’’ Unclear from which groups participants were withdrawn, but reasons given. More than 80% of outcome data were obtained. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects were randomly assigned to either experiment or control groups by having a case nurse draw lots" |
| Allocation concealment (selection bias) | Low risk | "After the subjects agreed to take part in the study, the case nurse drew lots to assign subjects" |
| Blinding (performance bias and detection bias) | High risk | Patients were aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | "The case nurse also helped the subjects choose the preferred music from the researcher's collection so that researcher would be blind to the conditions of treatment. [...] The researcher then entered the patient's cubicle and collected data. The researcher was blind to the treatment conditions of both groups during the whole period of data collection." |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and dropouts not described. |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomized" Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, drop‐outs, and missing data not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Patients aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Method of recorded physiological outcomes unclear. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals, dropouts, and missing data not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR, BP, and RR. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 17 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation not described (likely to be rule‐based, e.g. room availability). |
| Allocation concealment (selection bias) | High risk | Unlikely to have allocation concealment, as likely to have a rule‐based allocation system. |
| Blinding (performance bias and detection bias) | Unclear risk | Level of blinding not described. |
| Blinding (performance bias and detection bias) | Unclear risk | Level of blinding not described. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Infection. |
| Protection from contamination? | Unclear risk | Unclear if patients were moved between rooms. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 15 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly distributed" ‐ method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) | Unclear risk | Death ‐ objective outcome. Unclear blinding for bacterial infections and remission. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. It is unclear if patients with psychological problems were removed from the study or included on an ITT basis. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Infection. |
| Protection from contamination? | Low risk | Intervention administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random assignment of subjects [...] using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "A total of 5 patients were transferred to other hospitals during the study, leaving 18 patients in the nonmusic group and 17 patients in the music group" |
| Selective reporting (reporting bias) | Unclear risk | Unknown if selective outcome reporting. |
| Protection from contamination? | Unclear risk | It is possible that patients in the control group listened to their own music over the 3 day experiment, however it is unlikely that they would have been exposed to the structured intervention used for the study. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly divided" ‐method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR and BP. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Using a table of random numbers” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Low risk | Automated physiological outcome assessment |
| Incomplete outcome data (attrition bias) | Low risk | “None of the patients refused any of the measurements.” |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Participants then were assigned to one of the four groups by drawing of lots.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Low risk | Automated measurement of BP and HR. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Low risk | Appears to report on all major outcomes. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Patients were randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | High risk | Physiological data collected by (non‐blinded) nurses although methods of data collection are unclear. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Low risk | Appears to report on all major outcomes. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Patients were randomly assigned” Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Low risk | "After intubation, headphones were placed on the patient's ears in both groups. [...].The CD player was covered so that the investigator remained blinded to the study group." |
| Blinding (performance bias and detection bias) | Low risk | "After intubation, headphones were placed on the patient's ears in both groups. [...].The CD player was covered so that the investigator remained blinded to the study group." |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Patients were randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Patients were randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | “only 11 patients were able to complete the rating scales on the first evening [...]. By the second postoperative evening, all study patients were able to complete the pain and anxiety ratings”. Data extracted for review on the 2nd post‐operative day. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A computer generated the randomisation list.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Low risk | "The patient, anaesthetists, surgeon and nurses were blinded to the tape selection." |
| Blinding (performance bias and detection bias) | Low risk | "The patient, anaesthetists, surgeon and nurses were blinded to the tape selection." |
| Incomplete outcome data (attrition bias) | High risk | “One patient was withdrawn from the study because of a technical error with the cassette player.” Missing data for 1 patient on day of surgery (1%), 5 patients on first day after surgery (6%), and 34 patients on second day after surgery (38%). 25% of data is missing for the mobilisation outcome. Missing data appears evenly distributed between groups, however, the reasons for missing data are not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Computer generated randomisation” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: anxiety |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A computer generated the randomization list.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Low risk | "The anaesthesiologist, nurse anaesthetists, surgeon, physicians and nurses at the PACU were blinded to tape selection." |
| Incomplete outcome data (attrition bias) | Low risk | "One patient was withdrawn because of change of diagnosis intraoperatively, i.e. lipoma instead of inguinal hernia.” Otherwise, data appears to be complete. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A computer generated the randomization list. A block randomisation was used [...] block size was 25.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Low risk | "Sham and regular music CDs were thus indistinguishable [...] The anaesthesiologist, nurse anaesthetists, surgeon, physicians and nurses in the operating theatre and the PACU were blinded to the CD selection. All CD‐players were set to the same audio settings and were not audible to anyone in the immediate area." |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Low risk | Appears to report on all major outcomes. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Subjects were then allocated to one of three groups according to a predetermined computer‐generated random sequence.” |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Two study groups were unaware if they were receiving music alone, or music with binaural beats. The control group (standard care) was not blinded. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | “Of the 108 subjects who participated in the study, four were excluded as they were unable to complete the process. One participant disliked the music provided (Audio Group) and three subjects (one from each group) did not complete the second STAI‐S questionnaire for logistical reasons.” |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "participants were randomly assigned to the study groups by the flip of a coin." |
| Allocation concealment (selection bias) | High risk | "After voluntary consent was obtained, the sample participants were randomly assigned to the study groups by the flip of a coin." |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Low risk | Physiological outcomes were measure through automated assessment. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, HR and BP. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomly assigned to groups using a computer minimization program." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | High risk | "Of the 110 women enrolled, the researcher withdrew those who were unable to complete the three posttests (n = 33; 23%). These women had false labor pain (n = 8), received oxytocin between enrollment and starting the study at 3 cm dilation (n = 3), had caesarean section (n = 3), or rapid progress of labor and delivery (n = 19, 13%). Only one woman in the control group chose to withdraw from the study, and the reason given was too much pain." |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized" ‐ method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | Study was not blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomised". Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear whether physiological outcomes (BP and HR) were automated ‐ "non‐invasive system". |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Anxiety, HR and BP. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "flip of a coin" |
| Allocation concealment (selection bias) | High risk | "flip of a coin" |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | HR was automated by bedside monitor. BP was measured using a cuff (not blind). |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Low risk | Appears to report on major outcomes. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A biostatistician prepared a randomization list using a computer" |
| Allocation concealment (selection bias) | Low risk | "Only one member of the research team had access to this list of case numbers and randomization assignments, which was maintained in a locked filing cabinet. The nursing staff [...] presented the study to potential participants. At the time the patient agreed to participate in the study and the consent form was signed, the research associate called the registrar to obtain the patient's assigned case number and randomizaion group." |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "Two patients, one from each group, were excluded from final analysis because of incomplete data". |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Unclear risk | "patients in both groups may have interacted with each other or nonstudy individuals in the waiting room before or after treatment" |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Randomly assigned”. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group assignment. |
| Blinding (performance bias and detection bias) | Low risk | BP and HR measured using Critikon Model SNK9935 automated device. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After the clinicians performed a clinical assessment of hospitalised patients, the list of nominated patients was sent to us one day before the concert; we randomised the names of patients, thus ensuring that no bias was introduced when dividing the patients into two groups". Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) | Unclear risk | This is one of a series of studies. At the beginning of the report it is stated that: "they were all done as controlled, blind or double‐blind studies" but it is unclear from the report who was blinded in this particular study. |
| Incomplete outcome data (attrition bias) | High risk | "Initially, this study aimed to recruit 30 to 40 patients. The complexity of the clinic, including unforeseen problems with staff resources in taking blood samples, and the nature of the disease that can unpredictably incapacitate some patients to move from the ward reduced the total number studied to 17 patients. In spite of some patients' willingness to come from the ward to the ground floor where the concert was taking place, some patients felt unwell before the event or might have fallen asleep. Some patients changed their minds about participating, even after having signed the consent form." |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | "contol group formed by patients who remained on the ward at the time of the live performance" |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | Automated assessment of outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random assignment was made equally to one of three groups by drawing slips of paper indicating the group to which the subject would be assigned." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals described: "one subject was eliminated from the study because she was unable to cooperate with data collection". It is unclear if there is any missing data. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomly assigned to one of the three groups in the study, by drawing a slip of paper with group assignment" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | "Physiological measures [...] were taken manually for 1 min on all participants by the same research assistant." |
| Incomplete outcome data (attrition bias) | Low risk | "Nine subjects (17%) withdrew resulting in incomplete data, as they were sent to CC before completion of data collection at either time‐one or time‐two. A total of 45 subjects [...] completed the study, results reported are from these subjects." |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Prospective, randomized trail" ‐ method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Method of data collection not described. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer generated random numbers" |
| Allocation concealment (selection bias) | Low risk | Patients were blinded throughout study period. In a personal exchange with the study author (unpublished) they stated: "The person recruiting patients did not know the randomization." |
| Blinding (performance bias and detection bias) | Low risk | Patients were blinded to group allocation. |
| Blinding (performance bias and detection bias) | Low risk | Automated measurement of physiological outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "Five patients were excluded from the study due to changes in operation method, blood transfusion or insufficient epidural analgesia level" |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: HR and BP. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomized [...] by picking a slip of paper from one of two boxes (one for women and one for men so that gender could be matched)" |
| Allocation concealment (selection bias) | Low risk | "After signing informed consent, participants were randomized into control and experimental groups by picking a slip of paper". Informed consent was taken prior to randomisation. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear if intubation time was assessed blind or was automated. |
| Incomplete outcome data (attrition bias) | High risk | "There were 44 participants in the control group and 42 in the experimental group. [...]. Participants for this study continued to be recruited as others dropped out until a total of 60 participants completed the study. [...]. The elimination of 26 participants because of unforeseen complications during and after surgery is a limitation in this study and threat to the internal validity of results. These complications required extended intubation periods and eliminated participants from the normal weaning protocol or were unable to complete the state anxiety measure on the third postoperative day." 30% of participants were withdrawn (14 from the music group, and 12 from the control group). |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 33 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "The patient allocation [...] followed a predetermined rule: they were admitted to the wing with fewest patients, or with even numbers to the wing that did not receive the previous admittance." |
| Allocation concealment (selection bias) | High risk | Rule‐based system. |
| Blinding (performance bias and detection bias) | High risk | Blinding was not possible. |
| Blinding (performance bias and detection bias) | High risk | Blinding was not possible. |
| Incomplete outcome data (attrition bias) | Unclear risk | "One patient was excluded (senile dementia). [...]. Missing items on the PANSS ratings were evenly distributed in the groups with an average of 18.2% (14.3 ‐ 35.7%) for first and 7.2% (0 ‐ 20.1%) for the second and third rating. There were no missing items in the other rating scales." |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Unclear risk | Unclear if patients were free to move between wings of the ward. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned [...] using sealed envelopes with a varied block size prepared by the statistician" |
| Allocation concealment (selection bias) | Low risk | "using sealed envelopes with a varied block size [...] The investigator was blind to the block size and could not anticipate group assignment" |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "Although all patients who were enrolled completed the study, one participant in the music group was identified as an outliner for extreme pain and mild respiratory distress and was dropped from the analyses" |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 25 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Patients were held in the PACU and then discharged when a room on the unit became available. The unit director followed normal hospital protocol and assigned patients to either side of the unit depending on room availability." |
| Allocation concealment (selection bias) | High risk | Assignment used rule‐based system (room availability). |
| Blinding (performance bias and detection bias) | Unclear risk | "Patients were blind to the study's intervention as well as whether their room was located on the bright or dim side of the unit." It is unclear how blinding was acheived when: "Beginning on the afternoon of postoperative day 1 and continuing throughout hospitalization, light intensity (lux) was measured twice daily in the rooms of all study participants at approximately 9:30am and 3:30pm. Before measurement, the door of the room was closed, all artificial sources of light extinguished, and the window blinds were opened to permit maximum sunlight to enter the room." |
| Blinding (performance bias and detection bias) | Low risk | "A registered nurse, who was blind to the patient group assignment, abstracted the daily use of all opiod and opiod‐equivalent medications from the patient's medical records. [...] A hospital administrator, who was blind to patient group assignment, determined the total pain medication cost for each study patient from the hospital billing system." Unclear how blinding was acheived. |
| Incomplete outcome data (attrition bias) | Low risk | "The study used the intent‐to‐treat model and no patients were dropped after signing the consent. [...] no missing value procedures were used." Outcomes were obtained for >80% of participants on the day of sugery and post‐operative days 1 and 2, but not post‐operative days 3‐5 (participants were discharged). |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Rooms were assigned on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were randomly assigned" ‐ Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | Automated measurement of outcomes (HR, skin conductance). Method of measuring BP unclear. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly distributed" ‐ Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | HR and RR measured by auscultation for 30 seconds (not blind). |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Assigned randomly" ‐ Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | Measured by investigator (not blind) |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 15 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Patients (including emergency admissions) were received into both the open‐plan wards on Tuesday, Thursday, Saturday and on alternate Sundays" |
| Allocation concealment (selection bias) | High risk | Rule‐based allocation system. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address subjective outcomes. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear who assessed infections and level of blinding. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Participants assigned to rooms. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 22 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "a random number table" |
| Allocation concealment (selection bias) | Low risk | "Research staff not otherwise involved in the study generated a random‐number table and made sealed enrollment packets using these numbers" |
| Blinding (performance bias and detection bias) | High risk | "Patients were not told that the study was intended to primarily evaluate the pain associated with the gurney or chair". However, the study nurse who asked patients about their pain was not blinded to the study, and the patients were aware if they were on a gurney or a chair. Also: "The study nurse specifically instructed patients to rate the pain associated with the gurney, rather than pain from other sources" |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | "Four were discharged (two in each group) before the primary outcome could be measured [...]. Twenty‐four enrolled patients were discharged before t2 [...]." Outcomes were obtained for more than 80% of participants at time 1 but not at time 2. Outcome for review extracted at time 1. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | High risk | "Six patients in the chair group did not receive the allocated intervention, as they refused to get in the chair, and two patients in the gurney group demanded the chair." These patients were analysed on an intention‐to‐treat basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 20 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized" ‐ method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Study was not blinded. |
| Blinding (performance bias and detection bias) | High risk | Study was not blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | High risk | Insufficient data provided for extraction: Gait speed, and step length. |
| Protection from contamination? | High risk | Cross‐over trial. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer generated random groupings" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear if measurement of physiological outcomes was automated. |
| Incomplete outcome data (attrition bias) | High risk | "Twelve subjects in the latter [control] group did not complete the second questionnaire for a variety of reasons: 6 refused to complete the second questionnaire, 4 were taken to the Operating Room before the questionnaire could be completed, and 2 administered midazolam while in the Surgical Holding Area." (19.4% withdrawn, all from the control group). |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization [...] by drawing lots" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | High risk | RR measured via observation (not blind). BP measure via bedside cardiac monitor (automated). |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | High risk | Cross‐over design. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned". Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Low risk | BP and HR measured with automated system. RR measured via observation (not blind). |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer‐generated randomisation list" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | Unclear risk | Level of alertness was scored on the OAA/S with which the observer was unaware as to the significance of the score but not blinded to group allocation. It is unclear as to whether patients were blinded to group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | It is unclear as to the level of blinding in this study. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned." Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants in the control group were told the study was for gaining information on new admissions, so were unaware of the true purpose of the study. However, participants were not blind to whether they received music, white noise, or standard care. |
| Blinding (performance bias and detection bias) | Low risk | Physiological data obtained by automated measurements. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | See Table 8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned" ‐ Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) | High risk | Participants aware of group allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Study did not address objective outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop‐outs not described. |
| Selective reporting (reporting bias) | Unclear risk | Not known. |
| Protection from contamination? | Low risk | Interventions administered on an individual basis. |
ASA = American Society of Anesthesiologists; BP = blood pressure; bpm = beats per minute; CC = Cardiac catheterization; CD = compact disc; EGD = Esophagogastroduodenoscopy; FB = Flexible Bronchoscopy; FS = Flexible Sigmoidoscopy; HEPA = High energy particular air; HR = Heart rate; ICU = intensive care unit; IV = intravenous; MI = Myocardial Infarction; NRS = Numerical Rating Scale; OAA/S = Observer's assessment of alertness/sedation; OR = Operating Room; PACU = Post Anaesthesia Care Unit; PCS = Patient controlled sedation; POMS = Profile of Mood States; RCT = randomised controlled trial; RR = respiration rate; SD = Standard deviation; SE = Standard Error; STAI = State Trait Anxiety Inventory; UK = United Kingdom; USA = United States of America; VAS = visual analogue scale; VRS = Verbal rating scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| No intervention‐ observational study | |
| Summary paper, no data presented | |
| Study design | |
| Intervention | |
| Descriptive article | |
| Pediatric hospital | |
| Intervention | |
| Study design | |
| Descriptive article | |
| Review article | |
| Music CCT ‐ Post‐hoc exclusion | |
| Setting | |
| Outcomes | |
| No intervention | |
| No intervention | |
| No intervention | |
| Review article | |
| Not health‐related outcomes; policy changes | |
| Study design | |
| Study design | |
| Validity of outcomes | |
| Descriptive article | |
| Not health‐related outcome; query validity. | |
| Retrospective study | |
| Duplicate of Beauchemin 1998b | |
| Retrospective study | |
| Intervention music therapy at home | |
| Outcome measure not validated | |
| Other systematic review in this area (Cullum 2004) | |
| Retrospective study | |
| Participants (students) | |
| No intervention | |
| Overview‐ not a study | |
| Review article | |
| Music CCT ‐ Post‐hoc exclusion | |
| No intervention | |
| Study design (no control) | |
| Study design (matched pairs) | |
| Validity of outcomes | |
| Outcomes not reported for relevant groups; data collection methods unclear. | |
| Could not obtain article‐ not assessed for inclusion | |
| Qualitative report | |
| Study design | |
| Descriptive article | |
| Intervention provided outside of hospital | |
| Music CCT ‐ Post‐hoc exclusion | |
| Study design; outcomes | |
| Participants | |
| Study design | |
| Study design | |
| Study design | |
| Setting | |
| Study design | |
| Setting and population | |
| Setting and population | |
| Intervention | |
| Intervention | |
| Study design | |
| Not a study | |
| Intervention excluded‐ relaxation technique | |
| Cross‐sectional survey and qualitative interviews | |
| Qualitative | |
| Intervention‐ interactive music therapy | |
| Policy confounding (sterile versus clean attire). | |
| Study design (computer modelling) | |
| CBA‐ Control sites and 'before' sites not clearly defined | |
| Review article | |
| Questionable validity of outcome, relevant data not presented | |
| Setting | |
| Setting | |
| Review article | |
| Review article | |
| Qualitative | |
| Qualitative | |
| Included in Cochrane review by Cullum 2004 | |
| Setting | |
| Policy confound | |
| Outcome measure | |
| Policy confound | |
| Outcome measures | |
| Study design | |
| Study design | |
| Setting | |
| Participants | |
| Intervention | |
| Confounding | |
| Patients‐ mix of adults and children. Data inseparable. | |
| Setting | |
| Descriptive article | |
| Setting not hospital | |
| Study design | |
| Setting | |
| Study design | |
| Retrospective study | |
| Review article | |
| Review article | |
| Intervention not well‐defined | |
| Not a research study | |
| Music CCT ‐ Post‐hoc exclusion | |
| Policy changes | |
| Intervention provided during education programme | |
| Music CCT ‐ Post‐hoc exclusion | |
| Study design | |
| Study design | |
| Not hospital setting | |
| Music therapist confound; group differences in timing of data collection | |
| Music CCT ‐ Post‐hoc exclusion | |
| No intervention | |
| Intervention entailed coaching patients | |
| Setting not hospital | |
| Intervention interactive | |
| Qualitative | |
| Study design | |
| Editorial | |
| Study design | |
| Intervention interactive music therapy | |
| Study design | |
| Preliminary report of Rodriguez 1978; policy confound | |
| Sham operations | |
| One patient health‐related outcome reported (surgical site infections), but not enough detail on how it was assessed or if it was noted on an 'ad hoc' basis. | |
| Interventions not suitable for inclusion | |
| Study design | |
| No intervention in patients | |
| Setting; study design | |
| Study design | |
| Editorial | |
| Qualitative | |
| Intervention group provided 20 mins coaching | |
| Intervention group provided reinforncement and training‐ bias | |
| Intervention group provided coaching on relaxing | |
| Secondary analysis of Good 1999 | |
| Secondary analysis of previous study. | |
| Duplicate study‐ secondary analysis of Good 1999. | |
| Duplicate of study included in Cochrane review by Cullum 2004 | |
| News article | |
| Descriptive report | |
| Other systematic review in this area (Cullum 2004) | |
| Discussion article | |
| Qualitative | |
| Not research | |
| Outcomes | |
| Descriptive case study | |
| Relaxation (psychological) technique used in music group | |
| Music CCT ‐ Post‐hoc exclusion | |
| Qualitative, setting | |
| Qualitative | |
| Study design | |
| Study design | |
| Study design | |
| Music CCT ‐ Post‐hoc exclusion | |
| Study design | |
| Study design | |
| Outcomes | |
| Study design | |
| Review article | |
| Study design | |
| Study design | |
| Study design | |
| Music CCT ‐ Post‐hoc exclusion | |
| Intervention‐ taught techniques | |
| Music CCT ‐ Post‐hoc exclusion | |
| Outcomes | |
| Study design | |
| Study design and outcomes | |
| Study design | |
| Study design | |
| No intervention | |
| Not a study | |
| Intervention interactive virtual reality | |
| Intervention excluded‐ interactive distraction | |
| Experimental environment (not clinical situation), policy change | |
| Outcomes | |
| Outcomes | |
| Intervention‐ patient education video | |
| Descriptive article | |
| Case study | |
| Intervention not well defined | |
| Study design | |
| Outcomes | |
| Intervention not well defined | |
| Study design | |
| Qualitative; setting | |
| Setting | |
| Study design | |
| Study design | |
| Participants | |
| Policy confound (restraints use) | |
| Policy confound (restraints use) | |
| Policy confound (restraints use) | |
| Outcome measure | |
| Outcome measure | |
| Study design | |
| Outcome measure | |
| Participants | |
| Conference abstract‐ not enough information | |
| Literature review | |
| Study design | |
| Music CCT ‐ Post‐hoc exclusion | |
| Inadequate description of intervention | |
| Study design | |
| Review article | |
| Data unsuitable for cross‐over study | |
| Design; Outcomes | |
| Descriptive article | |
| Study design | |
| Study design; confounding | |
| Not health‐related outcome | |
| Setting not hospital | |
| Setting | |
| Commentary | |
| Descriptive article | |
| Setting | |
| Intervention not well defined | |
| Setting | |
| Intervention | |
| Validity of outcomes | |
| Study design‐ selection of participants by matching, different wards assigned to different conditions. | |
| Unable to clarify discrepancies in data with author | |
| Study design | |
| Setting | |
| Setting; Duplicate | |
| Intervention | |
| No intervention | |
| Policy confound | |
| Study design | |
| Intervention began before admission | |
| Study design (same study as Lawson 2003) | |
| Study design (same study as Lawson 2003) | |
| Study design (before‐and‐after no contemporaneous control) | |
| Study design | |
| Unclear methods and data | |
| Study design | |
| Music CCT ‐ Post‐hoc exclusion | |
| Not patient outcomes; test scenario | |
| Setting | |
| Study design | |
| Intervention relaxation training | |
| Policy confounding | |
| Study 1: inappropriate control; Study 2: intervention | |
| Study design | |
| Study design | |
| Test scenario, not patient outcomes | |
| Study design | |
| Some relevant subgroups within study however cannot separate data (number of re‐operations in each subgroup). Additionally, there are discrepancies in reporting with Lidwell 1984 with 185 patients switching subgroups. | |
| Same study as Lidwell 1982. Non‐transparant reporting of findings‐ data not usable. Discrepancies between Lidwell 1982 and Lidwell 1984. | |
| Study design | |
| Narrative article | |
| Intervention not well described (CCT) | |
| Intervention not well described (CCT) | |
| Could not obtain article, not assessed for inclusion | |
| Outcomes | |
| Setting | |
| Population‐ age | |
| Preliminary report of Lidwell 1982/Lidwell 1984 | |
| Policy confound | |
| Inadequate information provided (Ulrich study) | |
| Study design | |
| Study design‐ inappropriate data | |
| Outcomes not validated/reliable | |
| Study design; Intervention unclear | |
| Study design | |
| Study design | |
| Qualitative study | |
| Study design | |
| Study design | |
| Commentary | |
| Music CCT ‐ Post‐hoc exclusion | |
| Music CCT ‐ Post‐hoc exclusion | |
| No intervention | |
| Confounding | |
| Lack of information | |
| Participants; study design | |
| Confounding | |
| Intervention not well described | |
| Intervention not well described | |
| Music CCT ‐ Post‐hoc exclusion | |
| Policy change | |
| Setting | |
| Study design | |
| Commentary | |
| Music CCT ‐ Post‐hoc exclusion | |
| Intervention not well described, no data presented (CCT) | |
| Study design | |
| Setting and outcomes | |
| Study design | |
| Policy changes (confounding) | |
| Setting; outcomes | |
| Other systematic review in this area (Cullum 2004) | |
| Study design | |
| Literature review | |
| Study design | |
| Study design | |
| Not health‐related outcomes | |
| Study design | |
| Outcomes; unclear study design | |
| Intervention interactive with patient | |
| Policy confound | |
| Outcomes data not provided | |
| Patients‐ 38% <10 years old | |
| No intervention; comparison with healthy controls | |
| Study design | |
| Confounding staffing differences | |
| Policy (decontamination) changes | |
| Outcomes (validity and relevance) | |
| Study design (cross‐sectional, no intervention/control) | |
| Intervention | |
| Study design | |
| Study design (not enough data points to be included as ITS) | |
| Other systematic review in this area (Cullum 2004) | |
| Validity of outcomes | |
| Mock setting | |
| Descriptive article | |
| Setting and outcomes | |
| Inappropriate methods and analysis | |
| Aromas administered via nasal cannula, judged to be too invasive to constitute an 'environmental' intervention. | |
| Intervention (non‐environmental changes) | |
| Outcomes | |
| Policy confounding | |
| Intervention | |
| Not patient outcomes | |
| Literature review | |
| Intervention (care delivery systems) | |
| Intervention‐ relaxation tape | |
| Intervention | |
| Intervention not well described | |
| Policy confounding | |
| Intervention excluded as interactive | |
| Intervention excluded as interactive | |
| Intervention | |
| Policy change | |
| Data collection tool not validated | |
| Music CCT ‐ Post‐hoc exclusion | |
| Study design | |
| Intervention | |
| Study design | |
| Outcomes not validated | |
| Policy change‐ staff asked to remain quiet on intervention days | |
| Study design | |
| Policy change | |
| Intervention as treatment | |
| Compilation of studies, insufficient detail presented | |
| Setting | |
| Study design (no control) | |
| Study design | |
| Population, < 90% over 18 years old. | |
| Study design | |
| Follow‐up to Smylie 1971 and Davidson 1971; study design | |
| Study design | |
| Study design | |
| Overview‐ insufficient detail | |
| Music not well described; cross‐over trial with and without vibration. | |
| Study design (gender differences) | |
| Setting not hospital | |
| Study design | |
| Study design (block periods) | |
| Music CCT ‐ Post‐hoc exclusion | |
| Study design | |
| Study design | |
| Study design | |
| Intervention not well defined | |
| Confounding | |
| Staffing confound | |
| Study design | |
| Outcomes not validated | |
| Study design | |
| Setting not hospital | |
| Study design | |
| Intervention psychogical | |
| Music CCT ‐ Post‐hoc exclusion | |
| Patients allocated retrospectively to music or control, depending on whether or not they had noticed/heard any music. | |
| Music CCT ‐ Post‐hoc exclusion | |
| Intervention not well described | |
| Intervention; outcome not validated | |
| Study design | |
| Outcomes not validated | |
| Study design | |
| Qualitative evaluation | |
| Intervention | |
| Study design; outcomes | |
| Setting not in hospital | |
| Music CCT ‐ Post‐hoc exclusion | |
| Description of intervention/control unclear | |
| Insufficient info (intervention and data) | |
| Study design‐ retrospective matched pairs | |
| Conference abstract‐ unable to obtain further details from author | |
| Setting not a hospital | |
| Study design | |
| Study design | |
| Setting; Study design | |
| Literature review | |
| Study design, validity of outcomes | |
| Study design | |
| Test not clinical situation, healthy controls. | |
| Setting not a hospital | |
| Qualitative interviews | |
| Policy changes | |
| Intervention not well defined, query outcomes validity | |
| Not health‐related outcomes; conversation confounding | |
| Overview article | |
| Setting | |
| Study design | |
| Not patient outcomes | |
| Setting not a hospital | |
| Setting not a hospital | |
| Study design | |
| Study design; policy changes | |
| Study design‐ no control | |
| Music CCT ‐ Post‐hoc exclusion | |
| Study design‐ retrospective | |
| Qualitative; participants | |
| Descriptive case studies | |
| Participants not adults | |
| Music CCT ‐ Post‐hoc exclusion | |
| validity of outcomes | |
| Participants not patients | |
| Staff outcomes | |
| Music CCT ‐ Post‐hoc exclusion | |
| Policy confounding | |
| Inappropriate control‐ drugs | |
| Study design | |
| Music CCT ‐ Post‐hoc exclusion | |
| Duplicate study (Lee 2005) |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Review is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Published in Korean; we have not been able to assess this report yet due to translation difficulties. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Review is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | All patients 18 years and older with a diagnosis of cancer undergoing a BMBx in the Johns Hopkins Oncology Center will be screened for enrolment in the study. Based on power calculation, it was planned to enrol 40 patients in each group (total n = 120) to compensate for study withdrawal and missing data. |
| Interventions | All participants will have pain managed by the physicians responsible for their clinical care as dictated by those physicians. Participants assigned to Nature Sights and Sounds will have Bedscapes fabric panels depicting a scene of a mountain stream placed by the procedure table at a location where it will be visible throughout the procedure. An accompanying audiotape of complementary nature sounds will be played on portable tape players through headphones or speakers. They will be instructed to listen to the tape and look at the nature scene as frequently and for as long as they desire. The standard care group will have pain managed according to current oncology centre protocols but will not be allowed to use the distraction interventions. The Music/Photo group will be played a tape of typical city sounds and will have a poster of a city skyline placed by the procedure table. The city skyline poster will be similar in size to the Bedscapes mural. The skyline image is a daytime photograph without water, trees or other nature elements. The participants will be asked to listen to the music and view the picture during the procedure. |
| Outcomes | Pain; Profile of Mood States; Brief Symptom Index 18; Salivary cortisol; HR; BP; RR; overall satisfaction with care. Adverse events will be monitored. |
| Notes | Details obtained from ClinicalTrials.gov Final report not yet obtained. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Published in Korean; we have not been able to assess this report yet due to translation difficulties. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Study is being assessed as part of review update |
HR: heart rate; BP: blood pressure; RR: respiration rate
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | The HIP‐HOP Flooring Study: Helping Injury Prevention in Hospitalised Older People |
| Methods | Pilot cluster randomised controlled trial. |
| Participants | 8 elderly care wards in England (each ward has one bay, the 'study area', included in the study of 4 to 8 beds in size). |
| Interventions | 8.3mm thick floor covering (Omnisports EXCEL) versus standard floor covering |
| Outcomes | Fall‐related injuries; Falls; Adverse events; Cost‐effectiveness; User views; Slip resistance and shock absorbency of floor. |
| Starting date | April 2010 |
| Contact information | |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 2 | 87 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐1.05, 0.56] |
| Analysis 1.1  Comparison 1 Audiovisual distraction versus music, Outcome 1 Anxiety. | ||||
| 2 Pain Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Audiovisual distraction versus music, Outcome 2 Pain. | ||||
| 2.1 Endoscopic procedural pain | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 post‐operative pain | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Audiovisual distraction versus standard care, Outcome 1 Anxiety. | ||||
| 2 Pain Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Audiovisual distraction versus standard care, Outcome 2 Pain. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 3.1  Comparison 3 Music versus blank tape / headphones only, Outcome 1 Anxiety. | ||||
| 1.1 Pre‐procedural anxiety | 4 | 361 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.82 [‐1.03, ‐0.60] |
| 1.2 Procedural anxiety | 3 | 183 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.47, 0.23] |
| 1.3 Post‐operative anxiety | 3 | 220 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.52, 0.44] |
| 1.4 ICU anxiety | 1 | 64 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.32, 0.66] |
| 2 Heart rate Show forest plot | 8 | 543 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐1.02, 1.82] |
| Analysis 3.2  Comparison 3 Music versus blank tape / headphones only, Outcome 2 Heart rate. | ||||
| 3 Blood pressure Show forest plot | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 3.3  Comparison 3 Music versus blank tape / headphones only, Outcome 3 Blood pressure. | ||||
| 3.1 Systolic | 7 | 533 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐2.48, 1.67] |
| 3.2 Diastolic | 6 | 478 | Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐2.08, 1.39] |
| 3.3 Arterial | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 4.0 [‐5.33, 13.33] |
| 4 Respiration rate: with choice of outcomes Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 3.4  Comparison 3 Music versus blank tape / headphones only, Outcome 4 Respiration rate: with choice of outcomes. | ||||
| 4.1 Post‐operative period for Ikonomidou 2004 and final scores (both studies) | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐1.72 [‐1.00, ‐0.44] |
| 4.2 Post‐operative period for Ikonomidou 2004 and change score for Lee 2005 | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐2.48 [‐3.85, ‐1.11] |
| 4.3 Pre‐operative period for Ikonomidou 2004 and final scores (both studies) | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.92, 0.09] |
| 4.4 Pre‐operative period for Ikonomidou 2004 and change scores for Lee 2005 | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐2.09 [‐4.51, 0.34] |
| 5 Skin conductance Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 3.5  Comparison 3 Music versus blank tape / headphones only, Outcome 5 Skin conductance. | ||||
| 6 Stress hormones Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 3.6  Comparison 3 Music versus blank tape / headphones only, Outcome 6 Stress hormones. | ||||
| 6.1 Cortisol | 3 | 216 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.73, 0.09] |
| 6.2 Epinephrine | 2 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.38, 0.33] |
| 6.3 Norepinephrine | 2 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.44, 0.27] |
| 6.4 Adrenocorticotropic hormone (ACTH) | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐1.17, 0.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 8 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.1  Comparison 4 Music versus scheduled rest, Outcome 1 Anxiety. | ||||
| 1.1 Procedural anxiety | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 ICU/CCU anxiety | 7 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Heart rate Show forest plot | 4 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.76 [‐6.65, 1.13] |
| Analysis 4.2  Comparison 4 Music versus scheduled rest, Outcome 2 Heart rate. | ||||
| 3 Blood pressure Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 4.3  Comparison 4 Music versus scheduled rest, Outcome 3 Blood pressure. | ||||
| 3.1 Systolic | 3 | 140 | Mean Difference (IV, Random, 95% CI) | ‐1.51 [‐6.65, 3.63] |
| 3.2 Diastolic | 2 | 110 | Mean Difference (IV, Random, 95% CI) | ‐5.29 [‐8.78, ‐1.79] |
| 3.3 Arterial | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐4.75 [‐13.98, 4.48] |
| 4 Respiration rate Show forest plot | 3 | 110 | Mean Difference (IV, Random, 95% CI) | ‐2.04 [‐3.43, ‐0.66] |
| Analysis 4.4  Comparison 4 Music versus scheduled rest, Outcome 4 Respiration rate. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 29 | 1812 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.74, ‐0.36] |
| Analysis 5.1  Comparison 5 Music versus standard care, Outcome 1 Anxiety. | ||||
| 1.1 Pre‐procedural anxiety | 9 | 744 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.62, ‐0.12] |
| 1.2 Procedural anxiety | 15 | 865 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.02, ‐0.36] |
| 1.3 ICU/post‐operative anxiety | 5 | 203 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.01, ‐0.15] |
| 2 Heart rate Show forest plot | 21 | 1653 | Mean Difference (IV, Random, 95% CI) | ‐2.72 [‐4.70, ‐0.74] |
| Analysis 5.2  Comparison 5 Music versus standard care, Outcome 2 Heart rate. | ||||
| 3 Blood pressure Show forest plot | 20 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 5.3  Comparison 5 Music versus standard care, Outcome 3 Blood pressure. | ||||
| 3.1 Systolic | 18 | 1437 | Mean Difference (IV, Random, 95% CI) | ‐1.76 [‐5.09, 1.56] |
| 3.2 Diastolic | 17 | 1407 | Mean Difference (IV, Random, 95% CI) | ‐0.97 [‐2.58, 0.63] |
| 3.3 Arterial | 2 | 186 | Mean Difference (IV, Random, 95% CI) | ‐9.86 [‐12.06, ‐7.65] |
| 4 Respiration rate Show forest plot | 9 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.4  Comparison 5 Music versus standard care, Outcome 4 Respiration rate. | ||||
| 5 Sedation requirements (anxiolytics) Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.5  Comparison 5 Music versus standard care, Outcome 5 Sedation requirements (anxiolytics). | ||||
| 5.1 Midazolam (aka: Versed, Hypnovel, Dormicum, Dormonid), mg | 3 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Peripheral skin temperature Show forest plot | 4 | 298 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.08, 0.37] |
| Analysis 5.6  Comparison 5 Music versus standard care, Outcome 6 Peripheral skin temperature. | ||||
| 7 Oxygen saturation Show forest plot | 3 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.75, 0.32] |
| Analysis 5.7  Comparison 5 Music versus standard care, Outcome 7 Oxygen saturation. | ||||
| 8 Mood state Show forest plot | 2 | 170 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐2.17, ‐0.19] |
| Analysis 5.8  Comparison 5 Music versus standard care, Outcome 8 Mood state. | ||||
| 9 Satisfaction Show forest plot | 2 | 174 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.16, 0.76] |
| Analysis 5.9  Comparison 5 Music versus standard care, Outcome 9 Satisfaction. | ||||
| 10 Length of stay / Examination time Show forest plot | 2 | 153 | Mean Difference (IV, Random, 95% CI) | ‐6.00 [‐10.72, ‐1.28] |
| Analysis 5.10  Comparison 5 Music versus standard care, Outcome 10 Length of stay / Examination time. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Heart rate Show forest plot | 2 | 144 | Mean Difference (IV, Random, 95% CI) | 4.67 [‐0.76, 10.10] |
| Analysis 6.1  Comparison 6 Music versus white noise, Outcome 1 Heart rate. | ||||
| 2 Blood pressure Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 6.2  Comparison 6 Music versus white noise, Outcome 2 Blood pressure. | ||||
| 2.1 Systolic | 2 | 144 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐8.59, 5.00] |
| 2.2 Diastolic | 2 | 144 | Mean Difference (IV, Random, 95% CI) | 0.99 [‐7.60, 9.58] |

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Funnel plot of comparison: 5 Music versus standard care, outcome: 5.1 Anxiety.

Comparison 1 Audiovisual distraction versus music, Outcome 1 Anxiety.

Comparison 1 Audiovisual distraction versus music, Outcome 2 Pain.

Comparison 2 Audiovisual distraction versus standard care, Outcome 1 Anxiety.

Comparison 2 Audiovisual distraction versus standard care, Outcome 2 Pain.

Comparison 3 Music versus blank tape / headphones only, Outcome 1 Anxiety.

Comparison 3 Music versus blank tape / headphones only, Outcome 2 Heart rate.

Comparison 3 Music versus blank tape / headphones only, Outcome 3 Blood pressure.
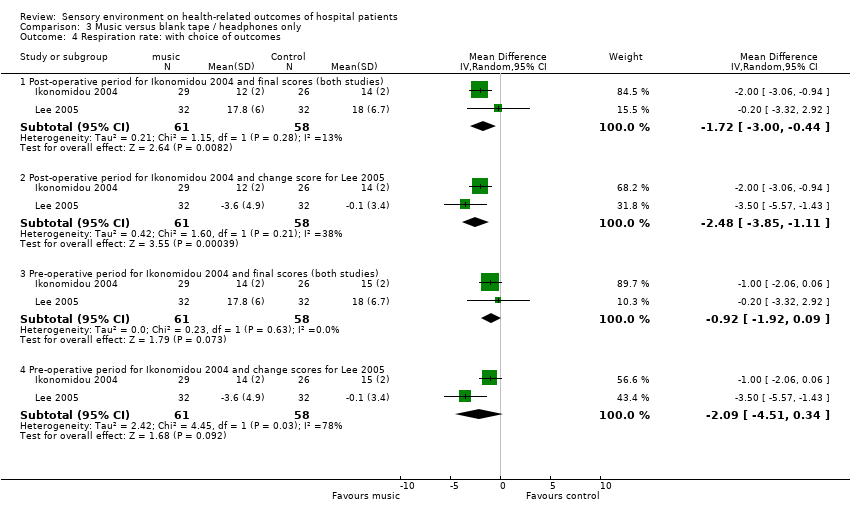
Comparison 3 Music versus blank tape / headphones only, Outcome 4 Respiration rate: with choice of outcomes.

Comparison 3 Music versus blank tape / headphones only, Outcome 5 Skin conductance.

Comparison 3 Music versus blank tape / headphones only, Outcome 6 Stress hormones.
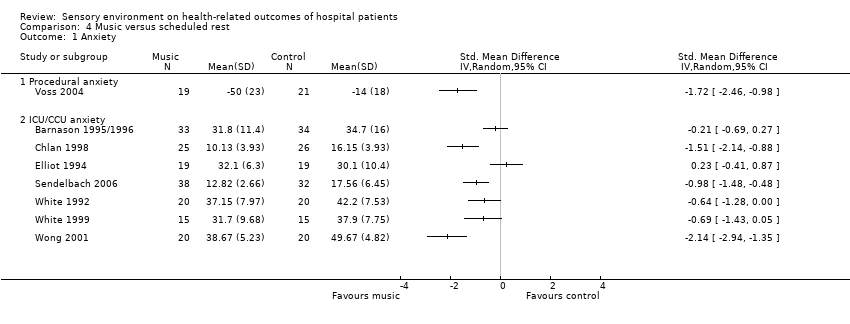
Comparison 4 Music versus scheduled rest, Outcome 1 Anxiety.
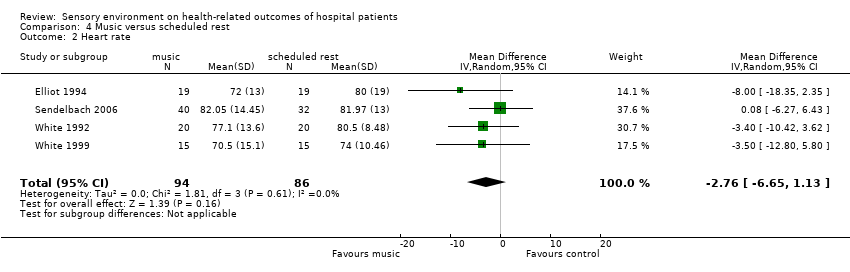
Comparison 4 Music versus scheduled rest, Outcome 2 Heart rate.

Comparison 4 Music versus scheduled rest, Outcome 3 Blood pressure.

Comparison 4 Music versus scheduled rest, Outcome 4 Respiration rate.

Comparison 5 Music versus standard care, Outcome 1 Anxiety.

Comparison 5 Music versus standard care, Outcome 2 Heart rate.

Comparison 5 Music versus standard care, Outcome 3 Blood pressure.
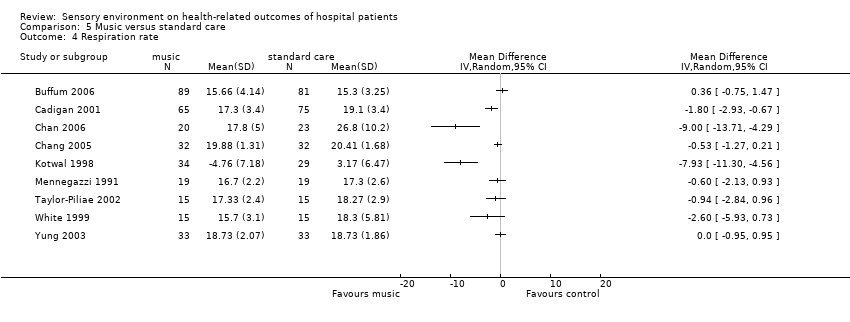
Comparison 5 Music versus standard care, Outcome 4 Respiration rate.

Comparison 5 Music versus standard care, Outcome 5 Sedation requirements (anxiolytics).

Comparison 5 Music versus standard care, Outcome 6 Peripheral skin temperature.

Comparison 5 Music versus standard care, Outcome 7 Oxygen saturation.

Comparison 5 Music versus standard care, Outcome 8 Mood state.
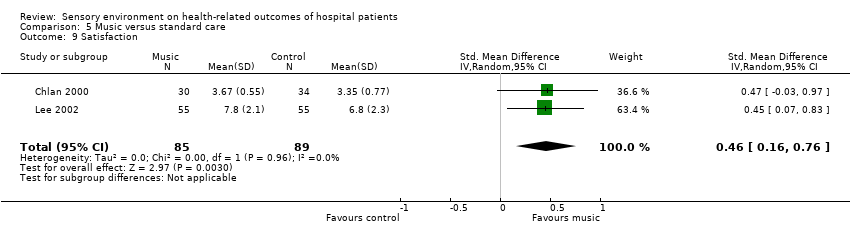
Comparison 5 Music versus standard care, Outcome 9 Satisfaction.

Comparison 5 Music versus standard care, Outcome 10 Length of stay / Examination time.
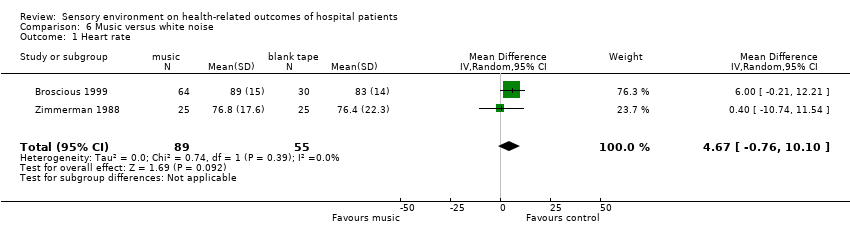
Comparison 6 Music versus white noise, Outcome 1 Heart rate.

Comparison 6 Music versus white noise, Outcome 2 Blood pressure.
| Study ID | Methods | Participants | Interventions | Outcomes |
| RCT; 3 parallel groups. | DESCRIPTION: 313 patients undergoing radiotherapy, in Australia. | FRAGRANT PLACEBO: Patients were administered the carrier oil with low‐grade essential oils. The carrier oil was sweet almond cold‐pressed pure vegetable oil. The low‐grade fractionated oils (lavender, bergamot, and cedarwood) were of unknown purity (supplied by Naturistics, Hornsby, Australia). These fractionated oils were diluted with the carrier oil in a ratio of 1:2. | ANXIETY, DEPRESSION, and FATIGUE: Measured via the Hospital Anxiety and Depression Scale (HADS), and the Somatic and Psychological Health Report (SPHERE), which is composed of the General Health Questionnaire (GHQ) and Symptoms of Fatigue and Anergia (SOFA) scales. | |
| CCT; Cross‐over trial, 2 conditions. | DESCRIPTION: 15 psychiatric inpatients in the communal area of a long‐stay hospital psychogeriatric ward for patients with behavioural problems, in England. | LAVENDER: The communal area of the unit was diffused with a standard concentration of lavender oil (2%), using three aroma‐streams for a period of two hours between the period of 4pm and 6pm. | AGITATION: Measured on the 16‐point Pittsburgh Agitation Scale by a blinded observer for the final hour of each two hour study period. Outcomes are presented as median scores for each patient in each condition. | |
| SD: standard deviation | ||||
| Study ID | Reason for exclusion |
| Intervention | |
| Study design | |
| Study design | |
| Study design | |
| Setting and population | |
| Editorial | |
| Study design | |
| Outcomes | |
| Study design | |
| Data unsuitable for cross‐over study | |
| Commentary | |
| Setting | |
| Setting | |
| Aromas administered via nasal cannula, judged to be too invasive to constitute an 'environmental' intervention. | |
| Intervention; outcome not validated |
| Study ID | Reason for exclusion |
| Qualitative report | |
| Descriptive article | |
| Participants | |
| Intervention interactive | |
| Qualitative report | |
| News article | |
| Qualitative | |
| Descriptive article | |
| Narrative article | |
| Commentary | |
| No group comparisons presented, unable to obtain further details from authors | |
| Study design | |
| Study design (part of same study as Staricoff 2001) | |
| Conference abstract, unable to obtain further details from author | |
| Setting | |
| Setting |
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| RCT; 3 parallel groups. | DESCRIPTION: 96 in‐patients in the cardiovascular ICU and progressive care units having undergone elective coronary artery bypass grafting, in USA. | MUSIC GROUP: Choice of 5 tapes: 'Country Western Instrumental' or 'Fresh Aire' by Mannheim Steamroller, 'Winter into Spring' by George Winston, or 'Prelude' or 'Comfort Zone' by Steven Halpern. Played via headphones for 30 minutes. | Barnason 1995 reports: | Data extracted for state anxiety (STAI measure). Pain data are extracted for the end values on the VRS. | |
| RCT; 2 parallel groups. | DESCRIPTION: 80 in‐patients and out‐patients undergoing FB in Mariland, USA. | BEDSCAPES GROUP: Countryside river scene with associated sounds of nature played through headphones. Intervention available before, during, and after FB procedure. The scene was mounted by the bedside in the recovery area and on the ceiling in the procedure room. | ANXIETY: State anxiety via STAI; | SDs for anxiety have been estimated from P value of a t‐test. | |
| RCT; 3 parallel groups. | DESCRIPTION: 157 day‐patients undergoing colonoscopy in an Endoscopy Suite in Hong Kong, China. | VISUAL DISTRACTION: Eyetreck system (olympus) with preset home made movie (mainly scenic views), patient wears earphones but with no sound. | PAIN: scored using 10 cm VAS; | ||
| RCT; 3 parallel groups. | DESCRIPTION: 37 patients undergoing flexible sigmoidoscopy in Calfornia, USA. | AUDIOVISUAL: Virtual‐i glasses, personal display system showing an ocean shoreline with corresponding sounds (via headphones) | DISCOMFORT: Measured via VAS which asked patients to rate their level of abdominal discomfort from faint to severly intense. | Data for discomfort entered as pain scores. | |
| RCT; 2 parallel groups. | DESCRIPTION: 17 in‐patients undergoing burns care treatment and dressings change in a Burn Special Care Unit, Cincinnati, USA. | AUDIOVISUAL GROUP: "Muralvision" (Muralvision Studios, Inc., Eugene, Ore.)‐ on a bedside television, video programmes composed of scenic beauty (ocean, desert, forest, flowers, waterfalls, and wildlife) with accompanying music. | PAIN: Measured via the McGill Pain Questionnaire, with the Pain Rating Index and Present Pain Intensity scales. | For data extraction in the review, change scores from baseline were calculated and associated estimated standard deviations, using the F statistics provided. | |
| SD: standard deviation; STAI: State Trait Anxiety Inventory; VAS: visual analogue scale | |||||
| Study ID | Reason for exclusion |
| Intervention | |
| Study design | |
| Study design | |
| Intervention‐ interactive virtual reality | |
| Intervention‐ interactive virtual reality | |
| Intervention‐ patient education video | |
| Inadequate information provided (Ulrich study) | |
| Intervention interactive | |
| Unclear validity of outcomes | |
| Intervention interactive | |
| Intervention interactive | |
| Intervention‐ snoezelen | |
| Population, < 90% over 18 years old. | |
| Setting | |
| Setting | |
| Participants not adults |
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| RCT; 4 parallel groups. | DESCRIPTION: 39 in‐patients (10 post‐operative for cardiac surgery, 29 undergoing cardiac observations) in a cardiac care unit in Florida, USA. | BEIGE: Walls remained original colour of beige (similar to Sherwin Williams colour SW6658) in four rooms. | ANXIETY: Measured via STAI on day of discharge (after 2 to 5 days in hospital). Presented as mean (SD). No significant differences reported. | Partients in this study were not approached for informed consent until Day 3 of the study. | |
| STAI: State Trait Anxiety Inventory | |||||
| Study ID | Reason for exclusion |
| Outcomes not validated | |
| Qualitative report | |
| Setting | |
| Study design | |
| Study design | |
| Participants | |
| Descriptive article | |
| Study design | |
| Descriptive article | |
| Outcomes | |
| Counfounding | |
| Staffing confound |
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| RCT; 2 parallel groups. | DESCRIPTION: 40 day‐patients undergoing ophthalmic surgery in New York, USA. | MUSIC GROUP: Patient choice of 22 types of music (e.g. soft hits, classical guitar, chamber music, folk music, popular singers from 1940's and 1950's), played via headphones throughout pre‐operative, surgical, and post‐operative periods. | PHYSIOLOGICAL: HR and BP measured via Propaq Monitor (Protocol Systems, Inc., Beaverton, OR) every 5 minutes during pre‐operative, surgical, and post‐operative period. Averages for the last three recorded measures within each time period were used for analysis in the paper. For purposes of review, data is extracted for the mean post‐operative scores only. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 118 out‐patients undergoing colonoscopy in a Digestive Endoscopy Unit in Spain. | MUSIC GROUP: Series of classical tracks (e.g. Bach, Grieg, Mozart, Delibe, Faure, and Mendelssohn) played via headphones during procedure. | ANXIETY: State anxiety measure pre and post procedure using the STAI; Reported as post ‐ pre difference with 95% CI. | There were no significant differences between groups regarding abnormal events. This data has not been extracted for the review. | |
| RCT; 3 parallel groups. | DESCRIPTION: 83 in‐patients undergoing cardiac catheterization in Germany. | MUSIC GROUP: Music was played via headphones, which were worn half on so patients could still hear the medical personnel, during the cardiac catheterization. A music therapist was present only to control the volume. Music played was "Entspannung" [relaxation] by Markus Rummel, composed specially for relaxation. | ANXIETY: Measured via the STAI before and after cardiac catheterization. Unclear whether post measurements were taken on the following day after cardiac catheterization. | ||
| RCT; 3 parallel groups. | DESCRIPTION: 90 patients undergoing urological surgery with spinal anaesthesia and PCS in Connecticut (USA) and Beirut (Lebonon). | MUSIC GROUP: Patients brought own music from home. | PROPOFOL REQUIREMENTS: Recorded as mg/kg/min and % of patients not using any propofol. Unclear if data presented are the SDs, and if the data presented as mg/kg/min is based on the total N or % of patients who used propofol. | Data not extracted for meta‐analysis. | |
| RCT; 2 parallel groups. | DESCRIPTION: 107 patients undergoing diagnostic coronary angiography or a percutaneous intervention procedure, in Ontario, Canada. | MUSIC GROUP: patient selected music (classical, soft rock, relaxation, country, own/other) played via headphones before, during, and after procedure, continued as the patient desired. | ANXIETY: State Anxiety via STAI pre and post procedure; | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 3 parallel groups. | DESCRIPTION: 96 in‐patients in the cardiovascular ICU and progressive care units having undergone elective coronary artery bypass grafting, in USA. | MUSIC GROUP: Choice of 5 tapes: 'Country Western Instrumental' or 'Fresh Aire' by Mannheim Steamroller, 'Winter into Spring' by George Winston, or 'Prelude' or 'Comfort Zone' by Steven Halpern. Played via headphones for 30 minutes. | Barnason 1995 reports: | Data extracted for state anxiety (STAI measure). See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 20 patients undergoing regional anaesthesia in North Carolina, USA. | NATURE TAPES: choice of sounds of birds, the ocean, a lagoon, or deeply resonant chimes, played for the duration of the surgery. | STATE ANXIETY: STAI administered pre‐operatively and one hour post‐operatively to calculate the change score. | Scores given for state anxiety are outside of the normal range for this questionnaire (20‐80). Method of calculating scores is not described. | |
| RCT; 3 parallel groups. | DESCRIPTION: 95 in‐patients undergoing coronary artery bypass (n = 92) or valvular heart surgery (n = 3) in Ohio, USA. | TAPED THERAPEUTIC SUGGESTIONS: excluded from review. | POST‐OPERATIVE STAY (days); Data extracted for analyses. | See Cepeda 2006 for details on music for pain relief. | |
| RCT: 3 parallel groups. | DESCRIPTION: 156 in‐patients undergoing chest tube removal after open heart surgery in Virginia, USA. | MUSIC GROUP: Patients preselected music they would prefer to hear from a library of 10 pre‐recorded music cassettes with no lyrics. Cassettes were produced by students in a music therapy programme under the supervision of a music therapist. Patients listened to the music via headphones for 10 minutes prior to and then during chest tube removal. | PAIN INTENSITY: Measured using a 10 cm NRS at 3 time points: (1) 10 minutes prior to chest tube removal, (2) immediately after chest tube removal, (3) 15 minutes after chest tube removal. | Report states that 18 participants had missing physiological data. Unclear from which groups these belonged, so for purposes of data extraction, it has been assumed that 6 participants were missing from each group. See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 170 pre‐operative patients to undergo vascular angiography in California, USA. | MUSIC GROUP: Selection of 5 categories (classical, jazz, rock, country western, easy listening), played via headphones for 15 minutes prior to angiography. Patients could continue to listen to music during the angiography after collection of outcomes. | ANXIETY: Measured via STAI before and after 15 minute study period. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 140 in‐patients in the cardiac units with intravascular sheaths or an intra‐aortic balloon pump (IABP) in place, in USA. | MUSIC GROUP: 30 minutes of music through headphones. Mixture of symphonic music and nature sounds selected by the researchers. Same music played to all those in the music group. | PAIN PERCEPTION: measured via 10 mm VAS pre‐ and post‐intervention. | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 193 day‐patients undergoing lithotripsy for renal stones (America). | MUSIC GROUP: Music of type preferred by patient played via headphones, starting 10 minutes prior to procedure and continuing until 10 minutes after lithotripsy is complete. Patients wore additional ear protectors to protect patients from the noise of the lithotriptor. | PAIN INTENSITY: rated verbally every 5 minutes throughout the lithotripsy on a NRS (0‐10). | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 220 female out‐patients undergoing colposcopy in China. | MUSIC GROUP: CD compilation of slow‐rhythm music (instrumental ballad). Patients could choose to listen to any song(s) within the compilation. Music played through speakers during the examination. Prior to onset of study women attending the clinic were surveyed on musical preferences to inform compilation disc. | ANXIETY: State anxiety via Chinese version of STAI measured pre and post colposcopy; | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 43 in‐patients undergoing application of a C‐clamp (which applies pressure to stop bleeding when sheaths are removed after percutaneous coronary interventions), in an ICU, Hong Kong, China. | MUSIC GROUP: 3 choices of soft, slow music without lyrics (slow rhythmic songs, Chinese slow rhythmic music, Western slow rhythmic music). Music played via headphones during the application of the C‐clamp (approximately 45 minutes). | VITAL SIGNS: BP, HR, RR, and oxygen saturation, recorded at baseline, 15, 30, and 45 minutes via a bedside monitor. | Outcomes extracted for end time‐point only. See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 64 patients undergoing cesarean section in Taiwan. | MUSIC GROUP: Choice of western classical, new age, or Chinese religious music, played via headphones. Participants listened to music for at least 30 minutes from start of anaesthesia to end of surgery. Volume low enough to allow mutual conversation with the researcher. | ANXIETY: measured via a 10 cm VAS, researcher filled it in after asking participant to indicate how they were feeling. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 20 in‐patients receiving mechanical ventilation in private patient room areas in critical care units in Midwest USA. | MUSIC GROUP: Selection of classical music played for 30 minutes via headphones. Patients instructed to close eyes and concentrate on the music. | MOOD: Short‐form POMS. | No SDs are presented for the post‐intervention physiological outcomes. Significant differences were found for HR and RR in favour of music. Other variables did not differ significantly. | |
| RCT; 2 parallel groups. | DESCRIPTION: 54 in‐patients receiving mechanical ventilation in one of 4 Intensive Care Units, USA. | MUSIC GROUP: choice of non‐lyric tapes 60‐80 bpm, classical, new age, country western, religious, and easy listening (30 mins). | ANXIETY: State anxiety via short form STAI (6 items); | Due to the lack of clarity over withdrawals and drop‐outs, it is unclear how many people were analysed in each group for the outcome anxiety. The degrees of freedom stated (49) suggests 51 observations were made, and we have assumed that N = 25 in the music group and N = 26 in the control group, based on the descriptions given for 3 of the withdrawals in the paper. | |
| RCT; 2 parallel groups. | DESCRIPTION: 64 out‐patients undergoing flexible sigmoidoscopy (FS) in Midwest USA. | MUSIC GROUP: choice of music (classical, country‐western, new‐age, easy listening, pop, rock, religious, jazz, era‐specific, motion picture soundtracks), played via headphones during FS procedure. Patients instructed to concentrate on music and that the investigator would meet with them afterwards to discuss their experiences. | ANXIETY: State anxiety measured via STAI | ||
| RCT; 2 parallel groups. | DESCRIPTION: 68 pre‐operative patients undergoing extracorporeal shock wave lithotripsy (ESWL) in Taiwan. | MUSIC GROUP: listened to natural music via headphones for 5 minutes prior to ESWL. | BLOOD PRESSURE: Method of data collection unclear. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 60 in‐patients and out‐patients undergoing flexible fibreoptic bronchoscopy (FB) in California, USA. | MUSIC GROUP: "Relax" (Expansion Records, Manchester, UK) consisting of piano improvisations (60bpm), played via headphones during FB procedure. | ANXIETY: State and Trait anxiety measure via STAI. | ||
| RCT; 3 parallel groups. | DESCRIPTION: 180 pre‐operative day patients scheduled for day surgery in Australia. | MUSIC GROUP: Choice of classical, jazz, country & western, new age, easy‐listening, and "other" mostly by contemporary artists. Music played for 30 minutes via headphones. | ANXIETY: State anxiety measured via STAI. | 95% Confidence Intervals are presented in the paper based on logarithmically transformed scores. Standard deviations were calculated by first back‐translating data to a log scale before utilising the CIs to estimate the SDs. Data entered into the review analysis are expressed as the natural log. | |
| RCT; 4 parallel groups. | DESCRIPTION: 121 patients undergoing elective cataract extraction in Canada. | MUSIC GROUP: Classical music accompanied by soothing sounds of nature, played via headphones intra‐operatively. | ANXIETY: Measured via STAI before and after surgery. | Data reporting unclear. Cannot extract SDs. | |
| RCT; 3 parallel groups. | DESCIPTION: 90 pre‐operative in‐patients waiting for dental restoration surgery under general anaesthesia, or orthopedic surgery, in Germany. | MUSIC GROUP: listened to 45 minutes of music pre‐operatively. Choice of music arranged the evening before surgery. 11 patients chose classical, 19 chose pop music. | ANXIETY: Measure via STAI and a tick‐box anxiety scale tailored for the clinic. There was a significant decrease in state anxiety from pre‐treatment to post‐treatment in the music group (change score = 2.2). There was no significant change in anxiety for the 'no medication' control group (change score = 0.633). | Not enough information for data extraction. | |
| RCT; Cross‐over study. | DESCRIPTION: 24 in‐patients with MI (N = 12) and other cardiac conditions (N=12) in a Critical Care Unit, Ontario, Canada. | MUSIC: 3 pieces each lasting approximately 12 minutes played in randomised Latin square design via headphones. a) Symphony no.6 by Beethoven; b) Eine Kleine Nachtmusik by Mozart; and c) The Moldau by Smetana. | PSYCHOLOGIC: Questionnaire not fully validated (content validity only). Not extracted for review. | Significant order effects for HR variability (P = 0.03) and heart rhythm (ectopy). | |
| RCT; 3 parallel groups. | DESCRIPTION: 143 out‐patients (93 included in present review) undergoing screening mammography in a clinic of a tertiary care hospital in Massachusetts, USA. | RELAXATION GROUP: excluded from review, as taped instructions constitute a psychological therapy. | ANXIETY: recorded before and after study period using the STAI, and at the end of the study with a Likert scale (1‐10) asking to rate level of anxiety felt during the procedure. | Investigator identified a possible floor effect. See Cepeda 2006 for details on music for pain relief (this study is not yet included in Cepeda 2006). | |
| RCT; 3 parallel groups. | DESCRIPTION: 56 in‐patients with unstable angina pectoris or acute MI at coronary care unit in Australia. | MUSIC GROUP: Received two or three 30‐minute sessions of light classical music (Bonny,Music Rx) played via headphones. | ANXIETY: Measured at pre and post test with three psychologic scales, 1) STAI, 2) Hospital Anxiety and Depression Scale, and 3) Linear Analogue Anxiety Scale (VAS). STAI scores extracted for review. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 33 in‐patients undergoing bone marrow transplant chemotherapy, in Columbus, USA. | MUSIC GROUP: Listened to 45 minute recording of self‐selected music via headphones at 6, 9, and 12 hours after the start of each infusion as an adjunct to antiemetic therapy. A variety of music selections was available and patients were encouraged to bring their favourite music. | NAUSEA: Measured on a VAS in the pictorial form of a thermometer (questionable validity). | Data not in sufficient detail for extraction. | |
| RCT; 2 parallel groups. | DESCRIPTION: 11 patients undergoing range‐of‐motion exercises as part of acute care rehabilitation for burns, Virginia, USA. | MUSIC GROUP: Choice of 6 cassette tapes (Lifescapes series) that met the guidelines for music in medical settings. Music was played during the range‐of‐motion exercises. | PAIN: Measured via VAS before and after rehabilitation exercises. There was a statistically significant increase in pain from pre‐treatment to post‐treatment in both groups (P = 0.04). There was no significant difference between groups (P = 0.38). | Data not in sufficient detail for extraction. See Cepeda 2006 for details on music for pain relief. | |
| RCT (post‐test only); 3 parallel groups. | DESCRIPTION: 15 pre‐operative patients in the waiting room for elective same‐day surgery in Pittsburgh, USA. | HUMOUR GROUP: excluded from review. | ANXIETY: Measured via a VAS after the intervention period. | ||
| RCT (post‐test only); 3 parallel groups. | DESCRIPTION: 46 pre‐operative patients scheduled for same‐day surgery in Pittsburgh, USA. | HUMOUR GROUP: excluded from review. | ANXIETY: Measure post‐intervention via VAS. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 50 pre‐operative patients to undergo septorhinoplastic surgery in Turkey. | MUSIC GROUP: Patients brought own CD or tape from home, those who forgot were provided with a 'suitable replacement', played via headphones during pre‐operative period, as patients were being sedated. | "modified" OAA/S: not included in review. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 93 in‐patients scheduled for laparoscope surgery, in Beijing, China. | MUSIC GROUP: Choice of 6 types of music (Western classical; light; pop; folk; folksong; opera) with 30 minutes listening time. Patients listened to music via headphones 1‐2 hours before their operation, whilst lying in bed. | ANXIETY: Measured via STAI before and after intervention period. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 78 patients undergoing colonoscopy in Kerala, India. | MUSIC GROUP: Choice of 6 tapes played via headphones during colonoscopy. Selection of: popular film songs (based on carnatic classical ragas), classical music, devotional songs, folk songs, soft instrumental music, bioacoustics (soft instrumental music with nature sounds). | SEDATION: Dose of midazolam (2 mg given on demand). | Data reported as median and range. See Cepeda 2006 for details on music for pain relief (this study is not yet included in Cepeda 2006). | |
| RCT; 2 parallel groups. | DESCRIPTION: 198 out‐patients awaiting gastrointestinal procedures (colonoscopy or esophagogastroduodenoscopy [EGD]) in California, USA. | MUSIC GROUP: Patient selected music (classical, rock, jazz, country western, easy listening) for 15 minutes prior to medical procedure. Were allowed to continue listening to music after outcome measures were taken. | ANXIETY: state anxiety measured via STAI. | This study has questionable clinical relevance: "To avoid introducing more anxiety with the explanation of the [gastrointestinal] procedure, the consent process for the [gastrointestinal] procedure was delayed until after the patients completed the music study". | |
| RCT; 3 parallel groups. | DESCRIPTION: 60 in‐patients who have undergone surgery with general anaesthesia, in a PACU in Iowa, USA. | MUSIC GROUP: Choice of three instrumental tapes: Calm classical (e.g. Bach, Debussy, Pachelbel), Stimulative classical (e.g. Strauss, Tschaikovsky), and calm popular music (e.g. piano solos by George Winston, guitar solos by William Ackerman and Steve Halpern). Patients decided which music they would like to listen to in the PACU in the pre‐operative visit. Played via headphones until discharge from PACU. | PAIN: Measured via 10cm VAS every 15 minutes while in the PACU. | Data insufficient for extraction. See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 55 day‐patients undergoing laparoscopic sterilization or laparoscopic tubal dyeing as part of a fertility programme in Sweden. | MUSIC GROUP: Panpipe music played via headphones for 30 minutes pre‐operatively and 30 minutes post operatively. | PHYSIOLOGICAL MEASURES: RR, BP, and HR, were measured by an attending nurse blinded to group allocation, before and after each 30 minute session (pre‐ and post‐surgery). | Sensitivity analyses conducted using data extracted for pre‐operative and post‐operative scores for anxiety, RR, BP, and HR. See Cepeda 2006 for details on music for pain relief. | |
| RCT; 3 parallel groups. | DESCRIPTION: 110 in‐patients and out‐patients undergoing IV catheter insertion in Southwestern public and private hospitals, USA. | SALINE GROUP: excluded from review as confounding non‐environmental intervention. | PAIN INTENSITY: measured via 100mm VAS. | See Cepeda 2006 for details on music for pain relief. Insertion difficulty is not included in the present review as a health‐related outcome. | |
| RCT; 3 parallel groups. | DESCRIPTION: 76 in‐patients undergoing surgery with general anaesthetic, in Sidcup, UK. | MUSIC GROUP: Classical music ('Adagio' Karajan, Deutsche Grammophon, 445 282‐4). Played via headphones during surgery. | FENTANYL REQUIIREMENTS: This served as an indication of the adequacy of nociception control provided during the operation. Fentanyl (ųg) was given intravenously if intra‐operative BP or HR increased by 20% or more above baseline values for more than 5 minutes. | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 34 out‐patients undergoing urologic procedures using spinal anaesthesia, USA. | MUSIC GROUP: All patients requested to bring their favourite CD to hospital on morning of surgery. A suitable substitution was provided to those who did not have access to their favourite CD. Music played via occlusive headphones intraoperatively. | BP (mm Hg), HR (bpm), PROPOFOL REQUIREMENTS (mg/min): recorded every 10 minutes for duration of surgery; | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 43 patients undergoing lithotripsy, USA. | MUSIC GROUP: Patients brought own music from home to listen to via occlusive headphones during surgery. | BP (mm Hg), HR (bpm), ALFENTANIL REQUIREMENTS: recorded every 15 mins. | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 3 parallel groups. | DESCRIPTION: 163 in‐patients undergoing hysterectomy in Vienna, Austria. | MUSIC GROUP: Patient choice of classical (Bach), Entertainment ("Musik zum Träumen" [Music for Dreaming]), or Relaxation (Oliver Shanti "Rainbow Way"). Played via headphones for 45 minutes beginning at the start of the operation (at the abdominal incision). | PAIN: Pain intensity measured via 10 cm VAS once a day for 5 days. There were no differences between groups. | Where means and SDs are presented (for length of stay), there are missing data from 23 participants so it is unclear how many people are in each group. See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 104 patients undergoing gastrointestinal endoscopy in India. | MUSIC GROUP: Classical Indian instrumental music played for 10 minutes prior to procedure and then throughout the procedure. | PHYSIOLOGICAL OUTCOMES: BP, HR, and RR measured at beginning of the consultation and at the end of the procedure. Methods unclear. Data presented as change scores. | ||
| RCT; 3 parallel groups. | DESCRIPTION: 58 patients undergoing noxious medical procedures (e.g. tissue biopsy, vascular port placement) at an oncology clinic in Midwestern USA. | MUSIC GROUP: Patient choice from selection of CDs (pop, rock, easy listening, classical, religious hymns, jazz or blues, country), listened via headphones prior to and during procedure. | PAIN: Pain intensity measured via a NRS prior to treatment, during treatment (retrospectively), and post treatment. | Values provided are adjusted scores (from analysis of covariance), adjusted for baseline scores, medications, and gender. Numbers reported as SDs in the text although too small so assumed to be the standard errors, which reflect the non‐significant findings described. See Cepeda 2006 for details on music for pain relief | |
| RCT; 3 parallel groups. | DESCRIPTION: 165 out‐patients undergoing elective colonoscopy in Hong Kong, China. | MUSIC ALONE: excluded from review as no appropriate control (i.e. music with no PCS). | PAIN SCORE: 10 mm VAS; | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 64 in‐patients on mechanical ventilation in an Intensive Care Unit in Hong Kong, China. | MUSIC GROUP: Choice of Chinese classical music, religious music (Buddhist and Christian), Western classical, natural sounds with slow beats. Played via headphones. | ANXIETY: State anxiety using Chinese STAI ‐short version (6 items). Participants responded to questions by holding up corresponding number of fingers. | ||
| RCT; 3 parallel groups. | DESCRIPTION: 37 patients undergoing flexible sigmoidoscopy in Calfornia, USA. | AUDIOVISUAL: Virtual‐i glasses, personal display system showing an ocean shoreline with corresponding sounds (via headphones) | DISCOMFORT: Measured via VAS which asked patients to rate their level of abdominal discomfort from faint to severely intense. | Data extracted for review on anxiety and anger. Arousal and attention not considered health‐related outcomes. | |
| RCT; 2 parallel groups. | DESCRIPTION: 50 in‐patients and out‐patients undergoing non‐oncologic surgery under spinal anaesthesia in Canada. | MUSIC GROUP: Choice of pop, jazz, classical, and new age played via non‐occlusive headset. Patients received the music prior to, during and after surgery. | PCS: Amount of midazolam consumed during the perioperative period was recorded. Data extracted for total midazolam consumed (mg). | Estimated anxiety data extracted. | |
| RCT; 2 parallel groups. | DESCRIPTION: 35 in‐patients in one of 5 Intensive Care Units having had an acute myocardial infarction, Midwestern USA. | MUSIC GROUP: 3 sessions of music listening on 1st, 2nd, and 3rd day (or 2nd‐4th day) of hospitalisation. Music session consisted of listening to 3 pieces of music each session: Bach's 'Largo', Beethoven's 'Largo', and Dubussy's 'Prelude to the Afternoon Faun'. Each session lasted approximately 22 minutes. | STATE ANXIETY: measured with the STAI at two time points: (1) during the first 48 hours of admission, and (2) on the 3rd or 4th day of hospitalisation. For the music group, these measurements were taken prior to the first music session and at the end of the 3rd music session. | ||
| RCT; 3 parallel groups. | DESCRIPTION: 45 patients undergoing femoral angiography in Boston, USA. | RELAXATION TAPE: Progressive muscle relaxation. Excluded from review. | STATE ANXIETY: Measured via STAI immediately pre‐ and post‐procedure. | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 44 post‐operative in‐patients in an Orthopaedic Department, Japan. | MUSIC GROUP: Choice of: Western classical music, Gagaku (Japanese traditional court music), Noh songs, or Enka. All participants choose Enka (a melodramatic and representative genre of Japanese popular songs, usually about sad aspects of life, irrecoverable destiny, and desertion by a lover, sung with a slow tempo), which is popular among elderly Japanese people. There were 10 Enka CDs to choose from. Music played via headphones for 20 minutes whilst lying in bed. | PAIN: Measured via 10 cm VAS and the Wong/Baker Faces Pain Rating Scale (includes 6 categories of facial expressions ranging from '0, a happy smiling face' and '5, a tearful face'). | See Cepeda 2006 for details on music for pain relief (study not yet included in Cepeda 2006). | |
| RCT; 4 parallel groups. | DESCRIPTION: 52 in‐patients undergoing various surgical procedures in USA. | MASSAGE THERAPY: excluded from review. | STATE ANXIETY: measured via the short‐form STAI‐6 in the PACU (after surgical procedure). | See Cepeda 2006 for details on music for pain relief (study not included in Cepeda 2006). | |
| RCT; 2 parallel groups. | DESCRIPTION: 38 emergency department admissions undergoing laceration repair in Pittsburgh, USA. | MUSIC GROUP: Listened to music via headset. Choice of 50 styles and artists to choose from. | ANXIETY: State anxiety measured via STAI before and after laceration repair. SDs presented in graphical format. Estimated figures extracted for purposes of review. | SDs for pain and anxiety are estimates from graphs. See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 30 patients undergoing surgery with general anaesthesia, Canada. | MUSIC GROUP: Selected a CD preoperatively from a choice of 4: classical, jazz, new‐age, popular piano music. Selected listening volume. Anesthesiologist started CD once patients were anaesthetised. Music played via headphones. | Repeated measures observations (4 time points)‐ T1: immediately after arterial line insertion, T2: 5 min after peritoneal incision, T3: at skin closer, T4: 30 min after arrival in the recovery area. | Data extracted for end time points only. See Cepeda 2006 for details on music for pain relief | |
| RCT; 2 parallel groups. | DESCRIPTION: 28 post‐operative in‐patients who have undergone elective abdominal hysterectomy, USA. | MUSIC GROUP: Four easy listening selections (out of an original 10) were selected by nursing graduate students to be harmonious, pleasant, and calming. Patients listened to music for 10 minutes via headphones and were requested to close eyes on the first and second post‐operative day. | PAIN: measured via VAS on first and second post‐operative day (pre and post 10 minute intervention period). | Outcomes extracted for 2nd post‐operative day as only 6 and 5 outcome measures were obtained for the intervention and control group on the 1st post‐operative day (all 28 participants completed the 2nd day of testing). See Cepeda 2006 for details on music for pain relief. | |
| RCT; 3 parallel groups. | DESCRIPTION: 90 (58 included in present review) in‐patients undergoing elective hysterectomy in Sweden. | MUSIC GROUP: relaxing music accompanied by sea waves (ref: Uneståhl L‐E. Avslappningmusik. Träningsprogram för kropp och själ. [Relaxation music. Training programme for body and soul]. Örebro, Sweden Veje International AB: 1970). Played through headphones from time of skin incision to time of wound closure. | PAIN INTENSITY: 10‐point VAS used every hour for the first 24 post‐operative hours, and every 3 hours after that until the patient felt no pain. Data presented as group mean score of patients' median score. | Data extracted for responses given on the day of surgery. See Cepeda 2006 for details on music for pain relief. | |
| RCT; 3 parallel groups. | DESCRIPTION: 151 day patients undergoing surgery of varicose veins or inguinal hernia repair under general anaesthesia, in Sweden. | INTRA‐OPERATIVE MUSIC GROUP: Music played via headphones from end of induction of anaesthesia until wound dressing via headphones. Music was soft instrumental comprising 7 melodies of a new‐age synthesizer. Post‐operatively, in the PACU, patients were exposed for 1 hour to a blank (silent) disc via headphones. | PAIN INTENSITY: Post‐operatively on a NRS (0 to10), every 30 minutes for 2 hours in the PACU. | Anxiety and fatigue not presented in enough detail. Findings on night sleep not reported at all. See Cepeda 2006 for details on music for pain relief. | |
| RCT; 3 parallel groups. | DESCRIPTION: 182 (125 included in present review) day patients undergoing surgery for varicose veins or inguinal hernia repair under general anaesthesia, from two hospitals in Sweden. | MUSIC GROUP: Soft classical music via headphones which allow conversation to take place. Played on auto‐reverse from the time of arrival at the PACU until the patient wanted to stop listening. | PAIN INTENSITY: taken every 30 minutes until patient reports a pain level of ≤ 3 on a VAS (0 to 10). Data presented as the mean of median scores in 120 minutes. | There was a significant difference in the length of time patients listened to their allocated tape. See Cepeda 2006 for details on music for pain relief. | |
| RCT; 3 parallel groups. | DESCRIPTION: 75 day patients undergoing surgery of open Lichtenstein inguinal hernia repair, in Sweden. | INTRA‐OPERATIVE MUSIC GROUP: exposed to new‐age synthesizer music during operation, and a sham (silent) CD for 1 hour post‐operatively in the PACU. | PAIN: assessed by NRS (0 to 10), 30 minutes before anaesthesia and 1 hour after admission to PACU. | Data extracted for post‐operative music group versus control group. See Cepeda 2006 for details on music for pain relief (study not yet included in Cepeda 2006). | |
| RCT; 2 parallel groups. | DESCRIPTION: 36 in‐patients with bronchial asthma, in Poland. | MUSIC GROUP: Underwent 10 day rehabilitation programme, including 45 minutes each day of: exercise of breath control, correction of respiratory pattern, training of diaphragm and additional respiratory muscles, plus an additional 15 minutes of music listening (C.M. Weber "Adagio"; J.S. Bach "Air on a G‐string"; V.A. Mozart "Andante z Divertimenta D‐dur"). | ANXIETY: Measured via the STAI at baseline and after the 10th session. | Data not provided in sufficient detail for extraction. | |
| RCT; 3 parallel groups. | DESCRIPTION: 104 day‐patients scheduled for elective surgical procedures (gynaecology, general surgery, urology) in a Day Surgery Unit in England. | MUSIC + BINAURAL BEAT: taken to a quiet environment pre‐operatively and asked to listen to music with their eyes closed; 30 minute soundtrack (Holosync Solution, 'Awakening Prologue', Centerpointe Research Institute, Beaverton, OR) which produces binaural beats (through two similar pure tones being presented separately to each other). | STATE ANXIETY: measured via the STAI before and after intervention period. Results converted to percentages instead of presenting STAI score. | It is unclear if > 90% of participants are 18 years old or over. | |
| RCT; 2 parallel groups. | DESCRIPTION: 50 out‐patients undergoing flexible sigmoidoscopy in Maryland, USA. | MUSIC GROUP: Choice of 20 tapes (classical/country‐western/popular/rhythm and blues/gospel) played via headphones throughout the procedure. | ANXIETY: Measured via STAI. An analysis of variance identified a significant difference between groups (P < 0.002): | No SDs reported. Insufficient data for extraction. | |
| RCT; 2 parallel groups. | DESCRIPTION: 110 in‐patients giving birth for the first time (to a singleton fetus), in Southern Thailand. | MUSIC: patient choice of western music without lyrics, including synthesizer, harp, piano, orchestra, and jazz (60‐80 bpm). Patients listened to their choice via headphones for the first 3 hours of the active phase of labour, starting when cervical dilation was 3 or 4 cm with uterine contraction of 30 to 60 seconds. Women could stop listening to music for 10 minutes if they wished. | PAIN SENSATION: measured using 100 mm VAS at four time points‐ once at the start of the study before the treatment period, and then every hour for 3 hours. | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 119 patients undergoing diagnostic endoscopy in Germany. | MUSIC GROUP: Played Radio Arabella (105.2 MHz) throughout the procedure. This is a well‐known regional broadcasting company in Munich, and plays various trends of pop, rock, soul, and 'Deutsche Schlager' music, specialising in 'oldies'. | SEDATION & ANALGESIA: Number of patients requiring midazolam and pethidine, and amount administered. It is unclear from the report if sedation is an outcome measure or baseline characteristic. | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 2 parallel groups. | DESCRIPTION: 30 patients undergoing cerebral angiography in Hannover, Germany. | MUSIC GROUP: Choice of nine tapes (international pop, German pop, oldies, meditation, rock, techno, instrumental, classic, and traditional). Played via stereo speakers throughout the angiogram; patients could adjust the volume. | ANXIETY: Measured via STAI the evening before the angiography and during the angiography. | Data not sufficient for extraction. | |
| RCT; 2 parallel groups. | DESCRIPTION: 86 post‐operative in‐patients who have undergone cardiac surgery, in cardiovascular units, Midwest USA. | MUSIC GROUP: Participants advised to clear minds and allow muscles to relax. They were given a choice of easy listening, classical, or jazz music, played via headphones, for 20 minutes whilst participant remained in bed. Music qualities were: no dramatic changes, consonance, instrumental, 60 to 70 bpm. The environment was made conducive to rest. | HR: Recorded on bedside monitor. No differences between groups. | Paper only reports data for the first 3 sessions due to missing data. SDs obtained from authors (unpublished). Data extracted for morning session of the first post‐operative day. See Cepeda 2006 for details on music for pain relief (study not yet included in Cepeda 2006). | |
| RCT; 2 parallel groups. | DESCRIPTION: 42 male out‐patients undergoing radiation therapy in a Veterans Affairs Hospital in Southeastern USA. | MUSIC GROUP: Patient choice of rock and roll, big band, country and western, classical, easy listening, Spanish, religious. Four to six tapes were available in each category. Each patient could choose one category for the duration of the study. Patients listened via headphones to the music before and during the radiation simulation appointment, and during daily radiation treatments for the duration of course of therapy. | STATE ANXIETY: measured using the STAI at 5 time points: (1) time of evaluation; (2) post simulation appointment; (3) end of first week of treatment; (4) end of third week of treatment; and (5) end of the fifth week or end of radiation therapy. | Data extracted for end time point. | |
| RCT; 2 parallel groups. | DESCRIPTION: 32 out‐patients undergoing colonoscopy, USA. | MUSIC GROUP: Patient choice of classical, jazz, pop rock, easy listening, played via headphones throughout pre‐sedation and procedure. | SEDATION REQUIREMENTS (mg). Amount of Versed and Demerol administered was recorded (not a primary outcome). | State anxiety data extracted from graph in article, bars taken as standard errors and converted into SD. | |
| RCT; 2 parallel groups. | DESCRIPTION: 17 in‐patients with HIV/AIDS staying in the HIV/AIDS ward, London, UK. | MUSIC GROUP: Attended a live music concert played in the public area on the hospital ground floor. Unclear what type of music was played. | LEVELS OF CD4 AND CD8 LYMPHOCYTES (cells/mm3): measured within one hour before and after the study period. | Data insufficient detail. | |
| RCT; 2 parallel groups. | DESCRIPTION: 120 in‐patients undergoing surgery with epidural anaesthesia in Taiwan. | MUSIC GROUP: Walkman music via headphones. Choice of 5 types (Manderin pop song, local Taiwanese folksong, Western, Classical, Buddhist hymn). Music played throughout operation. | Subjective feelings of anxiety and sedation: Method of assessment unclear (data EXCLUDED from review). | ||
| RCT; 3 parallel groups. | DESCRIPTION: 61 in‐patients who have had an elective abdominal hysterectomy using general anaesthesia in Arizona, USA. | MUSIC GROUP: patient choice brought from home or from selection provided (classical; jazz; light rock; country; rock and roll; easy listening; gospel), played via headphones. | PAIN INTENSITY: Two measures used: a 9‐inch VAS, and a 10‐point NRS. Measures were taken every 15 minutes for the duration of PACU stay (unspecified). Results of VAS are reported as a mean value for each group; results of NRS are reported as mean rating at 1 hour and at discharge from PACU. | See Cepeda 2006 for details on music for pain relief. | |
| RCT; 3 parallel groups. | DESCRIPTION: 30 pre‐operative in‐patients scheduled to undergo cardiac catheterization (CC) in Hong Kong, China. | SENSORY INFORMATION: excluded from review. | STATE ANXIETY: measured via STAI before and after intervention period; | Outcomes extracted for T1 ‐ after the study intervention but before cardiac catheterization, as the study has been categorised in the "pre‐procedure" subgroup. | |
| RCT; 2 parallel groups. | DESCRIPTION: 200 patients undergoing flexible bronchoscopy in Slovenia. | MUSIC GROUP: Easy listening and relaxation ambient music selected by the investigator, started immediately after the beginning of the procedure and stopped when the procedure is over. | PHYSIOLOGICAL: HR and BP recorded before and after the procedure, method of data collection not described. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 59 in‐patients undergoing elective laparoscopic cholecystectomy in an operating theatre in Japan. | NATURE SOUNDS: Patients were played their choice of nature sounds via headphones throughout operation, after induction of anaesthesia until the last suture of surgery. | PHYSIOLOGICAL MEASURES: BP and HR was recorded through 'non‐invasive' methods using the Philips patient monitoring system for anaesthesia [unpublished]. Outcomes were measured pre‐anaesthesia, at the start of surgery, at gallbladder removal, at the end of surgery, at extubation, at the end of anaesthesia, and in the PACU. | Data insufficient detail for extraction. Authors unable to provide means and SDs for physiological measures. | |
| RCT; 2 parallel groups. | DESCRIPTION: 60 in‐patients undergoing coronary artery bypass graft or vascular surgery, in the OR and ICU, Florida, USA. | MUSIC GROUP: Choice of 6 discs played during surgery and post‐operatively. Family encouraged to bring in additional music choices post‐operatively. Music selection from Prescriptive Music Inc., ('Clarity'‐ melodies from classical motion pictures; 'Timeless'‐ heartfelt originals, 'Towards'‐ piano improvisation, 'Interlude'‐ piano music by Mozart, 'Universe'‐ synthesized compositions, 'Essence'‐ cello and piano). | ANXIETY: Measured via the STAI on the 3rd post‐operative day. | ||
| RCT; 3 parallel groups. | DESCRIPTION: 61 post‐operative in‐patients following open heart surgery undergoing 30 minutes chair rest, in the surgical intensive care unit of a rural Midwestern hospital, USA. | MUSIC GROUP: Instructed to listen and follow music and allow it to distract and relax. Played through headphones. 6 choices: synthesizer, harp, piano, orchestra ,slow jazz, flute. 30 second excerpts provided for choice. Phone unplugged, blinds closed, lights dimmed and door closed. Do not disturb sign placed on door. | ANXIETY: Anxiety about chair rest measured via 100 mm VAS. | Change scores extracted for anxiety. | |
| RCT; 2 parallel groups. | DESCRIPTION: 93 pre‐surgical out‐patients, to undergo elective surgery (ear‐nose‐throat; orthopedics; plastics; or other general minor surgery), in USA. | MUSIC GROUP: Music played for 30 minutes via headphones prior to surgery in a hospital isolation room. Participants brought their own choice of music from home. | ANXIETY: Measured via STAI before and after experiment. | Outcomes are expressed as a percentage of the baseline score (mean and SD). | |
| RCT; 2 parallel groups. | DESCRIPTION: 40 in‐patients in acute care unit for acute myocardial infarction in Midwest USA. | MUSIC GROUP: listened to 4 adagios selected by the investigator for 25 minutes. Primarily string composition, low‐pitched, simple and direct musical rhythm, tempo approximately 60 bpm. Played via headphones. | ANXIETY: state anxiety measured via STAI. | ||
| RCT; 3 parallel groups. | DESCRIPTION: 45 in‐patients who had an acute MI, in private rooms in an ICU in Midwest USA. | MUSIC GROUP: Experimenter selected classical music, played via headphones. Asked to assume a comfortable position in bed, lights lowered, telephones unplugged, curtains drawn, doors closed, advised to clear mind and let muscles relax. 20 minutes. | PHYSIOLOGICAL: HR (chart extraction), RR (auscultation with a stethoscope for 30 seconds), BP (non‐invasive automatic oscillometric BP cuff), measured pre, immediately post and at 1 and 2 hours post the intervention period. Heart rate variability determined using power spectral analysis and fast Fourier transform from 3 hours of continuous electrocardiographic data (30 minutes pre to 2 hours post intervention period). | Data presented as mean and SE. SEs converted into SDs for purposes of review. | |
| RCT; 2 parallel groups. | DESCRIPTION: 50 day patients scheduled for elective same‐day surgery of gynaecological procedures (e.g. exploratory laparoscopies, laparoscopic tubal ligation, ovarian cysts excision, and intrauterine device removal), in New Jersey, USA. | MUSIC GROUP: Choice of classical, country, jazz, popular, or show music, played via headphones. | ANXIETY: State and trait anxiety via STAI on entry and exit of holding area. Results reported as Mean +/‐ SEM. | Anxiety data presented as mean and SEs. SEs converted into SDs for purposes of review. | |
| RCT; cross‐over study (2 allocation groups). | DESCRIPTION: 20 ventilator‐dependent in‐patients in an ICU in Hong Kong, China. | MUSIC GROUP: Choice of 7 cassettes (Chinese folk song; Chinese instrumental music; Chinese music with western instruments; Buddhist music; Western classic; Western movie music; piano music). Participants instructed to close eyes and focus on the flow of the music. | STATE ANXIETY: short‐form STAI, patients held up appropriate number of fingers in response to questions. Taken before and after each intervention. | This cross‐over study has not reported patient‐specific differences between the two intervention measurements. Therefore, the data has been extracted as if it is independent groups (as there was not enough data to calculate a correlation coefficient). | |
| RCT; 2 parallel groups. | DESCRIPTION: 39 patients undergoing eye operations with anaesthetics and analgesics in China. | MUSIC GROUP: Given a choice of 3 musical styles (pop, light, classical) with each type including 4 songs. Patients were asked to listen to the music 2 to 3 times the night before the operation and relax (not clear if patients were in‐patients). Patients then listened to the music throughout their operation. | ANXIETY: STAI presented as change scores. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 66 pre‐operative surgical patients in the OR holding area in Hong Kong, China. | MUSIC GROUP: Slow music played via headphones for 20 minutes pre‐operatively. Participants had a choice of 3 tapes‐ Chinese instrumental, Western instrumental, or Western and Chinese slow songs. | ANXIETY: State anxiety measured via C‐STAI pre‐ and post‐intervention period. | ||
| RCT; 2 parallel groups. | DESCRIPTION: 110 in‐patients undergoing abdominal hysterectomy in China. | MUSIC GROUP: Patient choice of music they felt to be calming and comforting, played via headphones intraoperatively, from 6 minutes before skin incision and 1 minute before the loading dose of anaesthesia to wound closure | PHYSIOLOGICAL: BP, HR, Bispectral Index recorded at 10‐minute intervals during surgery. Results reported as baseline and mean score during surgery (during target sedation period). | See Cepeda 2006 for details on music for pain relief (study not yet included in Cepeda 2006). | |
| RCT; 3 parallel groups. | DESCRIPTION: 75 in‐patients with suspected myocardial infarction in a coronary care unit in Midwest USA. | MUSIC GROUP: 30 minutes of self‐selected music choice of instrumental tapes: Halpern relaxation tape, classical music, country and western. Played via headphones. | ANXIETY: state anxiety measured via STAI | ||
| RCT; 2 parallel groups. | DESCRIPTION: 40 in‐patients with chronic cancer pain in acute care, Midwestern USA. | MUSIC GROUP: Choice of 10 relaxing instrumental tapes. Participants without a preference were given a Halpern antifrantic tape. The researcher suggested to the participant that the music would help them relax and reduce their pain. Participants listened to the music for 30 minutes via headphones. Participants lay on their beds and the lights were dimmed. | PAIN: Measured before and after 30 minute test period via McGill Pain Questionnaire (Pain Rating Index, Number of Words Chosen, and Present Pain Index). Additionally, pain intensity was measured via a 10 mm [sic] VAS. | See Cepeda 2006 for details on music for pain relief. | |
| BP: blood pressure; HR: heart rate; PACU: post‐operative care unit; POMS: Profile of Mood States; RR: respiration rate; SD: standard deviation; STAI: State Trait Anxiety Inventory; VAS: visual analogue scale; VRS: verbal rating scale; | |||||
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| CCT; 2 parallel groups; | DESCRIPTION: 42 pre‐operative patients scheduled for ambulatory surgery in a Midwestern city hospital, USA. | MUSIC GROUP: Choice of 20 tapes (classical, environmental, new age, country‐western, general easy listening), played via headphones whilst resting in recliner chairs. Intervention lasted 15‐30 minutes depending on how long patient had left before surgery. | PHYSIOLOGICAL MEASURES: measured using "standard noninvasive technology" before and after the intervention period. | ||
| CCT; 2 parallel groups; | DESCRIPTION: 301 outpatients and inpatients undergoing colonoscopy or esophagogastroduodenoscopy (EGD) in Switzerland. | MUSIC GROUP: Patients could choose between "light" and "classical" music which was played in the background during the examination. | GENERAL EVALUATION: Not extracted for review. | Paper reports outcomes as medians. Authors provided means and standard deviations on request for purposes of review. | |
| CCT; 2 parallel groups; | DESCRIPTION: 44 pre‐operative in‐patients in the holding area before total joint replacement, in Florida, USA. | MUSIC GROUP: Listened to music via headphones for a minimum of 30 minutes in the pre‐operative holding area. Music consisted of music‐enhanced nature sounds (sea, thunder, rainstorms, wind, and waterfalls). | The paper provides descriptive statistics only. | ||
| CCT; 2 parallel groups; | DESCRIPTION: 49 out‐patients undergoing bronchoscopy, USA. | MUSIC GROUP: Played new wave music 'Reflections of Passion' by Yanni, via headphones for the duration of bronchoscopy procedure. | PHYSIOLOGICAL: Methods of obtaining data unclear. There were no significant differences between groups on any of the physiological parameters. | ||
| CCT; 2 parallel groups; | DESCRIPTION: 158 inpatients with cardiovascular and respiratory illnesses participating in a therapeutic exercise programme, in the Republic of Uzbekistan. | MUSIC GROUP: Were played classical and pop music during the two week exercise programme. | PULSE: Assessed increase in pulse rate during exercise in the first and second weeks of the exercise programme. Method of data collection unclear. In week one, the music group worked harder, as demonstrated by increased pulse. | Authors conclude that cardiovascular patients should use music from the 1st week of exercise, and respiratory patients should use music from the 2nd week of exercise for better adaptation. | |
| CCT; 2 parallel groups; | DESCRIPTION: 24 pre‐operative day surgery patients waiting for surgery under general anaesthesia, in Texas, USA. | MUSIC GROUP: Choice of "easy listening" music selections recorded by the medical staff played via headphones for 20 minutes pre‐operatively. | ANXIETY: Measured via the STAI and a VAS. There was no significant difference between groups on either measure. STAI: | ||
| CCT; 2 parallel groups; | DESCRIPTION: 65 in‐patients undergoing rehabilitation (physiotherapy, balneotherapy, re‐education, and physical exercise) for lower back pain, France. | MUSIC GROUP: Music provided for first 4 days of 12 day hospitalisation. Music played for 20 minutes in the afternoon after physical therapy via headphones in a silent room. Patients were given a choice of music, with each choice arranged to have progressive relaxation with re‐awakening period at the end. | PAIN: Measured via VAS at baseline, day 5, and day 12, plus immediately pre and post therapy sessions. Day 5 outcomes did not significantly differ between groups: | ||
| CCT; 2 parallel groups; | DESCRIPTION: 101 in‐patients and out‐patients waiting for cardiac catheterizations in a cardiac telemetry unit, USA. | MUSIC GROUP: Listened to 20 minutes of 'Trance‐Zendance' by Halpern. Played via headphones prior to cardiac catheterization. | ANXIETY: Measured via STAI pre‐ and post‐ 20‐minute intervention period. There was a significant difference in anxiety scores in favour of the music group: | ||
| CCT; 2 parallel groups; | DESCRIPTION: 20 pre‐operative patients scheduled for breast biopsy in a holding area in Kentucky, USA. | MUSIC GROUP: Choice from selection of "new age" music listened to via headphones for 20 minutes pre‐operatively. No other music types were offered and patients' preferences were not solicited. | ANXIETY: Measured via the STAI pre‐ and post‐ 20‐minute study period. | ||
| CCT; 2 parallel groups; | DESCRIPTION: 34 in‐patients undergoing elective lumbar microdiscectomy procedures consented to participate (although only 10 analysed), Kentucky, USA. | MUSIC GROUP: Participants had a choice of 3 cassettes (country, instrumental, classical), with music 60‐80 bpm, played via headphones at a volume pre‐selected by participants. Music began 30 minutes before the end of the surgery and continued without interruption for one hour in PACU. | No data reported in paper. The paper reports there were no differences between the two groups on any of the outcome measures. | ||
| CCT; 2 parallel groups; | DESCRIPTION: 33 out‐patients awaiting arthroscopic procedures in Philadelphia, USA. | MUSIC GROUP: 20 minutes of classical music (tape 3 of Music Rx, developed by Bonny), played via audiocassette played placed 1 foot away during the waiting period. | BP: Measured via a Dinamap monitor before and after the 20 minute study period. There were no significant differences between the groups. Standard deviations are not provided. | ||
| CCT; 2 parallel groups; | DESCRIPTION: 113 pre‐operative day patients undergoing cytoscopy, cauterisation, or endoscopy, in China (Hong Kong).NUMBERS: Music group = 58, Control group = 55.AGE, mean (SD): Music group = 50.0 (15.5), Control group = 51.9 (14.4) years old.GENDER (male/female): Music group = 31/27, Control group = 27/28.ETHNICITY: not described.INCLUSION CRITERIA: 18 years or older; undertaking noninvasive day procedures with regional or local anaesthetic.EXCLUSION CRITERIA: Cognitive disability; hearing impairment; received preoperative sedatives; received a colon preparation; pre‐existing co‐morbid illness; did not have sufficient time to participate. | MUSIC GROUP: Choice of eastern and western style easy listening music and Chinese pop music (10 CDs and 10 mini‐discs) played via headphones in reclining chairs for 20‐40 minutes pre‐operatively.CONTROL GROUP: Undertook usual pre‐procedural relaxing activities (e.g. reading, watching TV) in the waiting room. | STATE ANXIETY: Measured via STAI pre‐ and post‐intervention period. Only the music group had a significant drop in anxiety. Post‐intervention scores:Music group = 42.5 (5.7) Control group = 46.4 (6.5) PHYSIOLOGICAL OUTCOMES: Measured via "standard non‐invasive instruments" pre‐ and post‐intervention period. There were no significant differences between groups.BP scores: Music group: Systolic BP = 124.2 (21.1), Diastolic BP = 70.0 (10.8) Control group: Systolic BP = 129.4 (25.6), Diastolic BP = 72.0 (11.1) PULSE scores: Music group = 71.1 (10.4) Control group = 70.1 (8.6) RR:Music group = 16.6 (1.0) Control group = 16.7 (1.0) | ||
| CCT; 2 groups (non‐parallel), intervention group was cross‐over (2 types of music played in same order for all participants), control group may have been recruited post‐hoc (UNCLEAR). | DESCRIPTION: 45 patients with disease of the lungs or chest being treated at the Department of Chest Surgery in Zakopane, Poland. | MUSIC GROUP: Cross‐over study. Music was played via headphones. Patients were played Debussy's 3rd part of Bergamasque Suite (Clair de Lune) on the piano (soothing music), and then Bartok's Wonderful Mandarin (nerve racking/exciting music). First, there was a 3‐minute rest in the recumbent position then, before, in between, and after each musical piece was a 3‐minute pause. | Parameters were measured at 5 time points in the music group: 1) Following 3‐min rest; 2) Following soothing music; 3) Following 3‐min pause; 4) Following exciting music; 5) Following 3‐min pause. Parameters were measured at 4‐time points in the control group (to follow same time scale as the music group)‐ a final 5th measurement was not taken for the control group. | Data not sufficient for extraction. No SDs reported. Paper reports significance as P < 0.1. | |
| CCT; 2 groups (non‐parallel), intervention group was cross‐over (2 types of music played in same order for all participants), control group may have been recruited post‐hoc (UNCLEAR). | DESCRIPTION: 45 patients with disease of the lungs or chest being treated at the Department of Chest Surgery in Zakopane, Poland. | MUSIC GROUP: Cross‐over study. Music was played via headphones. Patients were played Debussy's 3rd part of Bergamasque Suite (Clair de Lune) on the piano (soothing music), and then Bartok's finale of the Wonderful Mandarin (nerve racking/exciting music). First there was a 3‐minute rest in the recumbent position, then a 3‐minute pause before the first musical piece. After the first piece of music, there was a 4‐minute pause before the second musical piece was played. | Parameters of airway resistance were measured at three time points in both groups: 1) Following 3‐min rest; 2) Following relaxing music; 3) Following exciting music. | Data not sufficient for extraction. | |
| CCT; 2 parallel groups; | DESCRIPTION: 80 patients undergoing minor surgery in a day‐surgery ward in China. | MUSIC GROUP: Choice of 3 types of music with slow rhythms: classical music (concertos and sonatas), contemporary popular music (e.g. "The heart will go on"), Chinese popular music (e.g. "Night plane"). Music had 45 minutes running time and played via headphones for duration of surgery. | ANXIETY: measured via C‐STAI post‐surgery. Patients were asked to fill out the questionnaire by thinking retrospectively over procedure. | ||
| CCT; 2 parallel groups; | DESCRIPTION: 17 day‐patients undergoing arthroscopic surgery, USA. | MUSIC GROUP: Choice of 4 musical tapes (classical tapes from 'Music Rx', Bonny; popular tapes from 'Music Rx'; New Age tape by Steven Halpern called "Dawn"; easy listening selections assembled by investigator). Music played via headset and auto‐reverse cassette player. From administration of pre‐operative medication to PACU. Participants were told to restart the music if they desired after their return to the ambulatory surgery unit. | ANXIETY: state anxiety measured via STAI approximately 2 hours post‐operatively. Non‐significant. | SDs are estimated from the t‐value. | |
| CCT; 2 parallel groups; | DESCRIPTION: 63 patients undergoing dialysis, Florida, USA. | MUSIC GROUP: Choice of classical, pop, rock, jazz, country/western, gospel, easy listening, swing, and bluegrass played via headphones during dialysis treatment. Music was played for 1 hour beginning 30 minutes after the onset of dialysis treatment, there then was an hour of no music, followed by another hour of music. | BP: Measured after each hour of dialysis treatment. BP was recorded daily from each patient's chart for a 2‐week baseline period and a 3‐week treatment period. The two groups did not significantly differ on systolic and diastolic BP readings for onset through final readings during the treatment period. | Data not sufficient for extraction. | |
| CCT; 2 parallel groups; | DESCRIPTION: 88 pregnant women attending a high‐risk antenatal clinic, London, UK. | MUSIC GROUP: One or two musicians playing in one corner of the waiting room with the chairs arranged in a semi‐circle around them. Harp, clarinet, or guitar were preferred, violin and cello not welcomed. Does not explain in depth what was played. | BP: Obtained by the clinician (method unclear) at the beginning of the consultation (after the waiting room experience). There was no significant difference between the groups. | This is one of a series of studies. Two more studies were conducted in the antenatal clinic that do not need inclusion criteria for the review due to the study design (before and after). | |
| CCT; 2 parallel groups; | DESCRIPTION: 9 in‐patients waiting for elective surgery in a theatre holding area, China. | MUSIC GROUP: Choice of: slow rhythmical songs; Chinese slow rhythmical music; Western slow rhythmical music. Played via headphones for 20 minutes pre‐operatively. | BP: Measured via a calibrated Dinamap BP monitor before and after 20 minute study period. No significant differences between groups. | ||
| CCT; 3 parallel groups; | DESCRIPTION: 76 patients presenting to an emergency department with minor musculoskeletal trauma, in Midwest USA. | MUSIC GROUP: Provided with a Walkman tape player and choice of music (classical, country, rock, pop, and jazz), or were allowed to listen to the radio if they preferred. Patients also received standard care. | PAIN: Pain intensity measured at 0, 30, and 60 minutes via 10‐point NRS. There was no statistical differences between groups at any time interval. All groups showed significant improvement from baseline. | No SDs provided. | |
| CCT; 2 parallel groups; | DESCRIPTION: 57 post‐operative in‐patients who have undergone elective nasal surgery. | MUSIC GROUP: Choice of Chinese and Western various music types and patients encouraged to bring music of their own choice. Listened for 30 minutes on four occasions: post‐operatively (T1), again 4 hours later (T2), on the first post‐operative day at 8am (T3) and again at noon (T4). | PAIN: Measured via VRS at baseline and after each intervention session. Music group gave significantly lower pain ratings at all four time points. T4 data: | ||
| CCT; 2 parallel groups; | DESCRIPTION: 60 post‐operative in‐patients after coronary artery bypass graft in a progressive care area, USA. | SOUNDS GROUP: Marsona Sound Conditioner (providing white noise in the form of rain, ocean waves, or a waterfall). 56/60 patients chose ocean sounds. Sounds were played at the bedside throughout the night (switched on between 20.30 and 21.00 hours). Sounds played for 3 nights. | SLEEP: Pre‐test evaluated for patients on their usual sleep at home, data collected on admission, prior to surgery. Assessed on the fourth day post‐transfer for the quality of sleep the previous night. Measured via the Richards‐Campbell Sleep Questionnaire, which includes VAS for sleep depth, latency to sleep onset, awakening, return to sleep, quality of sleep, and a total sleep score. No SDs reported. | ||
| CCT; 2 parallel groups; | DESCRIPTION: 50 patients undergoing surgery with local anaesthetic, Poland. | MUSIC GROUP: Played music before during and after surgery. Patients chose music from a selection of instrumental tapes (music was soft, bright, avoiding high‐pitched sounds, classical). | ANXIETY: Measured via STAI the day before and directly after surgery in the recovery room. | Data not in sufficient detail for extraction. | |
| CCT; 2 parallel groups; | DESCRIPTION: 57 in‐patients undergoing surgery with local anaesthetic, Japan. | MUSIC GROUP: Were played a set piece (by Elgar) from when they entered the theatre to the end of surgery. | ANXIETY: Measured via STAI before and after surgery. Participants were requested to think back to how they felt during surgery in the post‐treatment questionnaire. | ||
| CCT; 3 parallel groups; | DESCRIPTION: 30 pre‐operative patients waiting for transurethral resection of the prostate, in a theatre holding area, Hong Kong, China. | MUSIC GROUP: 20 minutes of slow rhythm soft music played pre‐operatively via headphones. Choice of three tapes that had been judged by a panel of 3 musicians (slow rhythm songs, Chinese slow rhythm music, Western slow rhythm music). No nurse presence. | PHYSIOLOGICAL: BP and HR recorded on an automated BP monitor (Dinamap 1846‐SX) before and after 20 minute study period. Paper reports no significant differences between groups (Kruskal‐Wallis test) | ||
| BP: blood pressure; HR: heart rate; RR: respiration rate; STAI: State Trait Anxiety Inventory; VAS: visual analogue scale | |||||
| Study ID | Reason for exclusion |
| No data presented‐ summary paper | |
| Validity of outcomes | |
| Setting | |
| Validity of outcomes | |
| Outcomes not reported for relevant groups; data collection methods unclear. | |
| Study design | |
| Intervention provided outside of hospital | |
| Study design | |
| Setting and population | |
| Intervention | |
| Intervention | |
| Intervention‐ relaxation technique | |
| Intervention | |
| Questionable validity of outcome, relevant data not presented | |
| Setting | |
| Setting | |
| Qualitative report | |
| Outcome measure | |
| Outcomes | |
| Setting | |
| Intervention | |
| Setting | |
| Intervention not well defined | |
| Intervention provided during education programme | |
| Study design | |
| Music therapist confound; group differences in timing of data collection | |
| Intervention included coaching of participants | |
| Setting not hospital | |
| Study design | |
| Study design | |
| Intervention interactive music therapy | |
| Interventions not suitable for inclusion | |
| Invention group provided 20mins coaching. | |
| Intervention group provided reinforcement and training‐ bias | |
| Intervention group provided coaching on relaxing | |
| Secondary analysis of previous study | |
| Secondary analysis of previous study | |
| Secondary analysis of previous study | |
| Setting; qualitative | |
| Qualitative | |
| Relaxation (psychological) technique use with intervention | |
| Outcomes not health‐related | |
| Intervention‐ taught techniques | |
| Outcomes | |
| Case study | |
| Intervention not well defined | |
| Intervention not well defined | |
| Policy confound (restraints use) | |
| Policy confound (restraints use) | |
| Policy confound (restraints use) | |
| Outcome measure | |
| Outcome measure | |
| Study design | |
| Conference abstract‐ not enough detail | |
| Study design | |
| Intervention not well defined | |
| Data unsuitable for cross‐over study | |
| Setting | |
| Setting | |
| Intervention not well defined | |
| Validity of outcomes | |
| Study design‐ selection of participants by matching, different wards assigned to different conditions. | |
| Unable to clarify discrepancies in data with author | |
| Setting | |
| Setting; Duplicate | |
| Intervention began before admission | |
| Unclear methods and data | |
| Study design | |
| Intervention not well described (CCT) | |
| Intervention not well described (CCT) | |
| Outcomes not validated/reliable | |
| Study design | |
| Lack of information | |
| Confounding | |
| Intervention not well described | |
| Intervention not well described | |
| Intervention not well described, no data presented (CCT) | |
| Setting |
| Study ID | Reason for exclusion |
| Study design | |
| Study design | |
| Setting | |
| Inappropriate methods and analysis | |
| Outcomes not patient‐related | |
| Intervention | |
| Patients allocated retrospectively to music or control, depending on whether or not they had noticed or heard any music playing (unpublished information). | |
| Intervention not well described | |
| Data collection tool not validated | |
| Outcomes not validated | |
| Policy change‐ staff asked to remain quiet on intervention days | |
| Therapy as treatment | |
| Setting | |
| Overview‐ insufficient detail | |
| Music not well described; cross‐over trial with and with‐out vibration | |
| Setting | |
| Study design | |
| Study design | |
| Study design | |
| Study design | |
| Intervention not well defined | |
| Outcomes not validated | |
| Study design | |
| Setting | |
| Intervention | |
| Outcomes not validated | |
| Study design | |
| Study design; outcomes | |
| Insufficient information (intervention and data) | |
| Study design | |
| Study design | |
| Test (not clinical) situation, healthy controls | |
| Setting | |
| Intervention not well defined; validity of outcomes unclear | |
| Inappropriate control‐ drugs | |
| Duplicate study (Lee 2005) |
| Outcome | Detailed RCTs (N) | Participants (N) | Heterogeneity (%) | Results | Other RCTs | Participants (N) | Findings |
| Oxygen saturation | N = 1 | Total = 50 | N/A | MD 1.60, 95% CI 0.05 to 3.15, P value = 0.04 | N = 1 | Total = 20 | No significant difference between groups. |
| Airway pressure | None | N/A | N/A | N/A | N = 1 | Total = 20 | No significant differences between groups. |
| Skin conductance | Total = 186 | I2 = 81.7% (one study significant, one study non‐significant) | SMD 0.13, 95% CI −0.55 to 0.80, P value = 0.71 (Analysis 3.5). | None | N/A | N/A | |
| Heart rate variability (RR intervals, low and high frequency bands, total power, low/high frequency ratio) | None | N/A | N/A | N/A | N = 1 | Total = 68 | Heart rate variability data (high frequency power, logarithm of low frequency, and high/low frequency ratio) showed significant positive changes in the music group but not control group. Other variables (RR intervals, low and high frequency bands, low frequency power, and logarithm of high frequency) were non‐significant. |
| Bispectral index (mean, time to reach BIS 60) | N = 2 | Total = 160 | N/A (studies reported different outcomes) | Bispectral index: MD 1.00, 95% CI −1.27 to 3.27, P value = 0.39; | None | N/A | N/A |
| Stress hormones (Cortisol, epinephrine, norepinephrine, adrenocorticotropic hormone‐ ACTH) | N = 3 | Total = 216 | Cortisol I2 = 51.8% (3 studies) | Cortisol: SMD −0.32, 95% CI 0.73 to 0.09, P value = 0.13; | N = 1 | Total = 75 | No differences in cortisol levels at any time between groups. Change scores at 2 hours post‐operatively were significantly greater in the post‐operative music group than control. Blood glucose levels did not differ between groups at any time. |
| Mood | N = 1 | Total = 20 | N/A | MD −8.50, 95% CI −18.55 to 1.55, P value = 0.10 | None | N/A | N/A |
| Abnormal events (hypoxaemia, hypotension, hypertension, bradycardia, tachycardia, respiratory depression, pruritis) | N = 1 | Total = 118 | N/A | Cardio‐respiratory incidents = 0; | N = 1 | Total = 193 | Vomiting (Intra‐operatively/PACU): Music = 0/0%, Control = 2.2/0% Unclear missing data as presented in % values. |
| Headache | N = 1 | Total = 115 | N/A | MD 0.00, 95% CI −0.15 to 0.15, P value = 1.00 | None | N/A | N/A |
| Fatigue | N = 1 | Total = 115 | N/A | MD −0.30, 95% CI −0.78 to 0.18, P value 0.22 | N = 1 | Total = 151 | There were no significant differences between groups. |
| Urinary problems | N = 1 | Total = 115 | N/A | MD −0.10, 95% CI −0.40 to 0.20, P value = 0.51 | None | N/A | N/A |
| Well‐being | N = 1 | Total = 115 | N/A | MD 0.30, 95% CI 0.02 to 0.58, P value = 0.03 in favour of music group. | None | N/A | N/A |
| Nausea | N = 2 | Total = 308 | N/A (different methods of measurement) | MD −0.20, 95% CI −0.50 to 0.10, P value = 0.19 | N = 1 | Total = 151 | There were no significant differences between groups. |
| Satisfaction | N = 1 | Total = 110 | N/A | MD 1.60, 95% CI 1.29 to 1.91, P value < 0.00001 | N = 2 | Total = 344 | There were no significant differences between groups. |
| Length of stay | N = 1 | Total = 61 | N/A | MD 0.00, 95% CI −0.99 to 0.99, P value = 1.00 | N = 2 | Total = 118 | Harikumar 2006 reports that recovery time was significantly longer (difference in medians = 10 minutes) in the control group. Heitz 1992 reports no significant differences between groups. |
| Activities of daily living | N = 1 | Total = 61 | N/A | MD −0.30, 95% CI −2.63 to 2.03, P value 0.80 | None | N/A | N/A |
| Serum interleukins (IL‐6) | N = 1 | Total = 110 | N/A | MD −7.40, 95% CI −22.61 to 7.81, P value = 0.34 | None | N/A | N/A |
| Induction time of sedation (minutes) | N = 1 | Total 110 | N/A | MD −6.00, 95% CI −10.49 to −1.51, P value = 0.009 in favour of music. | None | N/A | N/A |
| CI: confidence interval; MD: mean difference; SMD: standardised mean difference; PACU: post‐operative care unit; RR: respiration rate | |||||||
| Outcome | Detailed RCTs (N) | Participants (N) | Heterogeneity (%) | Results | Other RCTs | Participants (N) | Findings | Comments |
| Skin temperature | N = 4 | Total = 298 | I2 = 0% | SMD 0.15, 95% CI −0.08 to 0.37, P value = 0.21; | None | N/A | N/A | |
| Oxygen saturation | N = 3 | Total = 150 | I2 = 79%; | MD −0.71% | None | N/A | N/A | |
| Requirement for oxygen supplementation | N = 1 | Total = 119 | N/A | OR 0.49, | None | N/A | N/A | |
| Blood flow characteristics | N = 1 | Total = 44 | N/A | Blood flow: MD −2.40 ml/min/100g, 95% CI −7.45 to 2.65, P value = 0.35; | None | N/A | N/A | |
| Bispectral index | N = 1 | Total = 39 | N/A | MD 0.22 BIS value, | None | N/A | N/A | It is unclear if this study meets the review inclusion criteria. Music group may have received intervention prior to coming to hospital. |
| Lung Function: (dyspnoea, tidal volume, minute ventilation, oxygen consumption, airway resistance). | None | N/A | N/A | N/A | N = 1 | Total = 36 | No significant differences. | |
| Stress hormones (Cortisol, Prolactin). | N = 1 | Total = 26 | N/A | Cortisol: MD 7.29, 95% CI −7.37 to 21.95, P value = 0.33; | N = 1 | Total = 30 | Cortisol significantly increased in the control group and remained unchanged in the music group. Catecholamines were non‐significant. | |
| Mood | N = 2 | Total = 170 | I2 = 0% | MD −1.18, | None | N/A | N/A | |
| Anger | N = 1 | Total = 24 | N/A | MD −1.80, | None | N/A | N/A | |
| Depression | N = 1 | Total = 39 | N/A | MD −3.29, | None | N/A | N/A | It is unclear if this study meets the review inclusion criteria. Music group may have received intervention prior to coming to hospital. |
| Fatigue | None | N/A | N/A | N/A | N= 1 | Total = 24 | No significant difference between groups. | |
| Uncertainty | N = 1 | Total = 30 | N/A | MD −3.53, 95% CI −12.15 to 5.09, P value = | None | N/A | N/A | |
| Satisfaction | N = 2 | Total = 174 | I2 = 0% | MD 0.46, 95% CI 0.16 to 0.76, | None | N/A | N/A | |
| Nausea | None | N/A | N/A | N/A | N = 1 | Total = 33 | The paper reports that the music group had significantly less nausea and vomiting than the control group (Mann‐Whitney U test, P < 0.017). | |
| Length of stay | N = 2 | Total = 153 | I2 = 0% | MD −6.00 minutes, 95% CI −10.72 to −1.28, P value = 0.01 in favour of music group (Analysis 5.10). | N = 1 | Total = 60 | Findings were non‐significant. | |
| Intubation time | N = 1 | Total = 60 | N/A | MD −200.20 minutes, 95% CI −391.03 to −9.37, P value = 0.04 in favour of music group. | None | N/A | N/A | |
| CI: confidence interval; MD: mean difference; SMD: standardised mean difference | ||||||||
| Study ID | Reason for exclusion |
| Setting | |
| Commentary | |
| Outcomes | |
| Study design | |
| Study design‐ retrospective matched pairs |
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| CCT; 2 parallel groups. | DESCRIPTION: In‐patients, predominantly with leukaemia, multiple myeloma, and malignant non‐Hodgkins lymphoma, admitted to the haematology‐oncology unit in Bonn, Germany. | AIR FILTRATION: 3 rooms (single or double) were fitted with portable air filtration units (NSA model 7100A/B Environment Air System, National Safety Association Ltd., Memphis, USA). These units have a 95% filtering capacity for particles > 0.3 micrometers. They have two settings (high/low). Flow rate: High = 168, Low = 112 cubic m/hr. | INVASIVE ASPERGILLOSIS: Counts of cases (confirmed and suspected) were achieved via ward liaison, targeted chart reviews, and consultation with medical staff. | Compliance to the air filtration units was low; they were generally run on low due to the noise generated, and sometimes stopped during the night. | |
| RCT; 2 parallel groups. | DESCRIPTION: 45 inpatients undergoing treatment for acute leukaemia or bone marrow aplasia, in Belgium. | ISOLATION: Patients were isolated in a laminar air flow room. The isolation unit consisted of a normal bed enclosed in a plastic tent. The area available for the patient was about 5 sq metres. Air was pumped vertically through high‐efficiency filters positioned on the ceiling. All procedures on the patient were done through plastic gloves on the sides of the tent. All items entering the unit were either gas or steam sterilized, passing through locks irradiated by ultraviolet light. The tent was only opened when absolutely necessary. Any person approaching the isolated patients wore sterile boots, gloves, gown, and mask. Patients remained in isolation until either the bone marrow showed haematologic remission or myeloid proliferation and maturation. The study period ended when the patient was no longer in isolation. | BACTERIAL INFECTIONS: Fungal cultures of stools were performed at least once a week. Data is reported as a count of the number of patients in which suppression of bacterial growth from stool cultures was achieved. Cultures were also obtained from the nose, gingiva, throat, ear, and axilla. Results report the number of days with infection (per 1000 days with severe neutropenia). | ||
| CCT; 2 parallel groups. | DESCRIPTION: 1726 in‐patients residing in the wards of a surgical unit (urological surgery/general surgery), in Scotland, UK. | OPEN WARDS: Two wards (one male, one female) with natural ventilation (and no mechanical ventilation). The male ward had partitioned 4‐6 bedded bays, housing a total of 28 beds, and female ward was completely open plan with 29 beds. | STAPHYLOCOCCUS AUREUS (Staph. aureus): Nasal acquisition of Staph. aureus was monitored via swabs taken on admission, and then every Monday and Thursday thereafter. Data reported as the number of acquisitions, and the rate per 100 patient‐week. The number of tetracycline‐resistant strains of Staph. aureus and delayed acquisitions was also determined. |
| Study ID | Reason for exclusion |
| Study design | |
| Setting | |
| Outcomes | |
| Study design (no control) | |
| Study design (matched pairs) | |
| Policy confound (sterile versus clean attire) | |
| Study design (computer modelling) | |
| Confounding | |
| Patients‐ mix of adults and children, data inseparable | |
| Preliminary report of Rodriguez 1978; policy confound | |
| Sham operations | |
| One patient health‐related outcome reported (surgical site infections), but not enough detail on how it was assessed or if it was noted on an 'ad hoc' basis. | |
| Not patient outcomes | |
| Study design | |
| Not patient outcomes; test scenario | |
| Not patient outcomes; test scenario | |
| Study design | |
| Some relevant subgroups within study however cannot separate data (number of re‐operations in each subgroup). Additionally, there are discrepancies in reporting with Lidwell 1984 with 185 patients switching subgroups. | |
| Same study as Lidwell 1982. Non‐transparant reporting of findings‐ data not usable. Discrepancies between Lidwell 1982 and Lidwell 1984. | |
| Population‐ age | |
| Preliminary report of Lidwell 1982 and Lidwell 1984 | |
| Study design | |
| Retrospective study; population (age) | |
| Policy (decontamination) changes | |
| Mock setting | |
| Policy confounding | |
| Policy confounding | |
| Study design | |
| Study design | |
| Not patient outcomes | |
| Policy confounding |
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| CCT; 2 parallel groups. | DESCRIPTION: 3327 patient‐weeks were analysed. Participants were in‐patients on one of two medical wards in the UK. | OPEN WARD: Two identical wards each containing 6 four‐bed rooms, which opened up on to the corridor. The four‐bed rooms each had three proper walls with the fourth side being open to the corridor except for low dividing walls (3 ft.) on each side of the entrance. | PATIENT NASAL AQUISITION OF STAPHYLOCOCCUS AUREUS: A nasal swab was taken from patients as soon as possible after arriving on the ward (within 3 days). Subsequently a swab was taken from each patient on a set day of the week. | Ratio of nasal carriage rates in single rooms to 4‐bed bays: |
| Study ID | Reason for exclusion |
| Review article | |
| Participants (age) | |
| Cross‐sectional survey and qualitative interviews | |
| Confounding | |
| Retrospective study | |
| Policy changes | |
| Preliminary report of Rodriguez 1978; policy confound | |
| Healthy participants received intervention | |
| Study design | |
| Study design | |
| Study design | |
| Study design, outcomes | |
| Study design | |
| Outcome measure | |
| Participants | |
| Study design | |
| Study design; confounding | |
| Intervention | |
| Study design | |
| Confounding | |
| Study 1: inappropriate control; Study 2: intervention | |
| Study design | |
| Study design | |
| Study design; unclear intervention | |
| Participants; Study design | |
| Setting | |
| Study design | |
| Policy changes | |
| Patients‐ 38% <10 years old | |
| Study design | |
| Intervention (non‐environmental changes) | |
| Policy confounding | |
| Policy confounding | |
| Policy change | |
| Study design | |
| Study design | |
| Policy changes | |
| Study design | |
| Study design | |
| Study design‐ no control | |
| Validity of outcomes | |
| Policy confounding |
| Study ID | Reason for exclusion |
| Participants (students) | |
| Study design |
| Study ID | Methods | Participants | Interventions | Outcomes |
| RCT; 2 x 2 design (2 x flooring, 2 x therapy). | DESCRIPTION: 54 in‐patients in an elderly care rehabilitation ward, in England. | LINOLEUM FLOOR: Patient admitted to one of two four‐bed bays with latex vinyl square tile flooring. | NUMBER OF FALLERS: obtained from the accident report forms. | |
| RCT, cross‐over design, 2 conditions. | DESCRIPTION: 58 elderly hospital patients in England. | CARPETED CORRIDOR: Each patient walked along the corridor towards a staff member standing 15 m ahead. Chalk marks were drawn at an interval of 10 m. | GAIT SPEED and STEP LENGTH: The number of steps taken was counted from the time the patient crossed the first chalk line until the distal line was crossed by the leading forefoot, and elapsed time was measured by a stopwatch. |
| Study ID | Reason for exclusion |
| Paediatric hospital | |
| Study design; outcomes | |
| Qualitative | |
| Study design | |
| Study design | |
| Study design | |
| Qualitative evaluation |
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| RCT; 2 parallel groups. | DESCRIPTION: 132 elderly out‐patients admitted to the emergency department, in Ohio, USA. | CHAIR GROUP: Remained on the gurney until initial physician and nursing evaluations complete. Patients were then assisted to a reclining chair. Patients were told "it is now time to move to the chair" and if they asked why, they were told they had the option of now moving to the chair. Patients were assisted to a position of comfort. Patients can sit on the reclining chairs with the hips and knees flexed. | PAIN: "The study nurse specifically instructed patients to rate pain associated with the gurney, rather than other sources." Measured on a NRS at three time points (time 0 = baseline; time 1 = one hour after randomisation; time 2 = two hours after randomisation). This outcome was dichotomised as favourable outcome (yes/no). A favourable outcome was considered as the patient having no pain at time 0 or time 1, or a decrease in pain from time 0 to time 1. An unfavourable outcome was defined as an increase in pain from time 0 to time 1, or no change in pain score if the patient complained of pain at time 0. | SDs for satisfaction were estimated from the 95% confidence interval (1.4, 2.8), assuming 66 patients per group. |
| Study ID | Reason for exclusion |
| Outcomes and policy changes | |
| Other systematic review in this area (Cullum 2008) | |
| Other systematic review in this area (Cullum 2008) | |
| Study design | |
| Not a research study | |
| Other systematic review in this area (Cullum 2008) | |
| Other systematic review in this area (Cullum 2008) | |
| Study design | |
| Test (not clinical) situation, policy change | |
| Study design | |
| Study design‐ inappropriate data | |
| Other systematic review in this area (Cullum 2008) | |
| Not health‐related outcomes | |
| Outcomes (validity and relevance) | |
| Other systematic review in this area (Cullum 2008) | |
| Policy change | |
| Study design | |
| Intervention | |
| Policy changes with cleaning of blankets |
| Study ID | Reason for exclusion |
| No intervention‐ observational study | |
| No intervention | |
| No intervention | |
| No intervention | |
| Review article | |
| Study design | |
| Review article | |
| Study design; outcomes | |
| No intervention | |
| No intervention in patients | |
| Study design | |
| Discussion article | |
| Study design | |
| Study design | |
| Study design | |
| Study design | |
| No intervention | |
| Review article | |
| No intervention | |
| Policy confound | |
| Policy change | |
| Study design (cross‐sectional, no intervention) | |
| Study design |
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| CCT; 2 parallel groups. | DESCRIPTION: 89 post‐operative in‐patients recovering from elective cervical and lumbar spinal surgeries in single patient rooms, Pittsburgh, USA. | BRIGHT ROOM: On west side of the corridor. Received approximately 46% more natural sunlight than dim rooms (received on average 73,537 lux‐hours per day). | ANALGESIC CONSUMPTION: obtained via chart extraction and standardised to morphine equivalent mg/hr. | Analgesic consumption data extracted for entire LOS mg/hr. | |
| POMS: Profile of Mood States | |||||
| Study ID | Reason for exclusion |
| Retrospective study | |
| Duplicate of Beauchemin 1998b | |
| Retrospective study | |
| Retrospective study | |
| Study design | |
| Study design | |
| Study design | |
| Setting | |
| Intervention | |
| Intervention | |
| Study design | |
| Setting; Study design | |
| Literature review |
| Study ID | Reason for exclusion |
| Setting; study design | |
| Setting; outcomes | |
| Intervention |
| Study ID | Methods | Participants | Interventions | Outcomes |
| CCT; 2 parallel groups. | DESCRIPTION: 97 surgical in‐patients undergoing lower extremity vascular reconstruction in an ORa in Maryland, USA. | WARM OR: Patient underwent operation in one of a group of ORs with the ambient room temperature maintained at 24.5 (0.4) degrees Celsius. | ORAL TEMPERATURE: Measured with an electronic digital thermometer, pre‐operatively (before being transported to the OR), immediately post‐operatively, on arrival at the ICU, and every hour for 24 hours. | |
| aOR = Operating Room. | ||||
| Study ID | Reason for exclusion |
| Study design | |
| Study design | |
| Study design | |
| Intervention‐ temperature of equipment not ambient room temperature | |
| Staff outcomes |
| Study ID | Reason for exclusion |
| Not health‐related outcomes; policy changes | |
| Not health‐related outcomes; query validity | |
| Not a hospital setting | |
| Qualitative | |
| Design; outcomes | |
| Not health‐related outcome | |
| Outcomes | |
| Study design | |
| Confounding staffing differences | |
| Qualitative; participants |
| Study ID | Reason for exclusion |
| Setting | |
| Study design | |
| Setting | |
| Study design‐ inappropriate data | |
| No intervention; comparison with healthy controls | |
| Not health‐related outcomes; conversation confounding | |
| Setting | |
| Participants not patients |
| Study ID | Reason for exclusion |
| Study design | |
| Study design, validity of outcomes | |
| Study design‐ retrospective |
| Study ID | Methods | Participants | Interventions | Outcomes | Notes |
| CCT; 8 parallel groups (2 x rooms, 2 x psychiatrists, 2 x time of data collection). | DESCRIPTION: 115 applicants for out‐patient psychiatric treatment at the Neuropsychiatric Institute, Los Angeles, USA. | 'BEAUTIFUL ROOM': Carpeted in burnt‐yellow carpeting and contained an abstract picture on one wall, a floor‐sized artificial plant, a wooden waste‐basket, and indirect lighting provided by a contemporary desk lamp. The room was neat and well kept.'UGLY ROOM': Carpetless, with beige asphalt floor tiling, overhead fluorescent lighting and was unkempt, with work papers strewn over the furniture and an overflowing grey metal wastebasket and ashtray. Both rooms were windowless offices of identical size (6 x 8 x 8 feet), wall covering, and colour. The furniture was the same (brown metal desks with beige formica tops, green leatherette desk chairs, and green and yellow leatherette side chairs. The offices varied only in decor. | ROOM RATINGS: not included in review. | Data not presented in enough detail for extraction. | |
| CCT; 2 parallel groups. | DESCRIPTION: 56 psychiatric in‐patients in the seclusion area of an acute psychiatric ward in Norway. | REFURBISHED WING: Redecorated and refurbished with the aim of looking, as much as security permitted, like an ordinary Norwegian home: Wainscoting walls, colourful wallpaper and paintings, lowered ceilings, multiple lighting spots, tasteful curtains, wardrobes, chairs, flowers, personal items, Italian ceramic‐tiled bathroom. | SYMPTOMS AND PSYCHOPATHOLOGY: Scored on the Positive And Negative Syndrome Scale (PANSS) for schizophrenia, with the time criterion of the last 24 hours. Scale has scores for total, positive, negative, and general symptoms. Assessed on admittance, day 3, and at discharge from seclusion. | Data extracted for change from baseline (beginning and end time‐points only).PANSS score for 'total' extracted for review. No significant difference was found on any of the subscales. |
| Study ID | Reason for exclusion |
| Descriptive article | |
| Descriptive article | |
| Study design | |
| Descriptive article | |
| No intervention | |
| No intervention | |
| CBA‐ Control sites and 'before' sites not clearly defined | |
| Review article | |
| Setting | |
| Policy confound | |
| Policy confound | |
| Study design | |
| Descriptive article | |
| Study design | |
| Review article | |
| Review article | |
| Study design | |
| Descriptive article | |
| Descriptive case study | |
| Study design | |
| Review article | |
| Study design | |
| Outcomes | |
| Outcomes | |
| Qualitative; setting | |
| Setting | |
| Literature review | |
| Setting | |
| Intervention | |
| Study design (same study as Lawson 2003) | |
| Study design (same study as Lawson 2003) | |
| Study design (before‐and‐after no contemporaneous control) | |
| Study design | |
| Study design (before‐and‐after no contemporaneous control) | |
| Study design | |
| Policy confound | |
| Qualitative study | |
| Study design | |
| Study design | |
| No intervention | |
| Confounding | |
| Literature review | |
| Study design | |
| Study design | |
| Study design | |
| Outcomes; unclear study design | |
| Policy confound | |
| Confounding staffing differences | |
| Literature review | |
| Intervention (care delivery systems) | |
| Study design | |
| Follow‐up study (Smylie 1971, Davidson 1971); study design | |
| Study design | |
| Study design (gender differences) | |
| Study design | |
| Unclear intervention/control | |
| Study design | |
| Qualitative interviews | |
| Overview article | |
| Study design | |
| Descriptive case studies |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 2 | 87 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐1.05, 0.56] |
| 2 Pain Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Endoscopic procedural pain | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 post‐operative pain | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Pain Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Pre‐procedural anxiety | 4 | 361 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.82 [‐1.03, ‐0.60] |
| 1.2 Procedural anxiety | 3 | 183 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.47, 0.23] |
| 1.3 Post‐operative anxiety | 3 | 220 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.52, 0.44] |
| 1.4 ICU anxiety | 1 | 64 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.32, 0.66] |
| 2 Heart rate Show forest plot | 8 | 543 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐1.02, 1.82] |
| 3 Blood pressure Show forest plot | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Systolic | 7 | 533 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐2.48, 1.67] |
| 3.2 Diastolic | 6 | 478 | Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐2.08, 1.39] |
| 3.3 Arterial | 1 | 30 | Mean Difference (IV, Random, 95% CI) | 4.0 [‐5.33, 13.33] |
| 4 Respiration rate: with choice of outcomes Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Post‐operative period for Ikonomidou 2004 and final scores (both studies) | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐1.72 [‐1.00, ‐0.44] |
| 4.2 Post‐operative period for Ikonomidou 2004 and change score for Lee 2005 | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐2.48 [‐3.85, ‐1.11] |
| 4.3 Pre‐operative period for Ikonomidou 2004 and final scores (both studies) | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.92, 0.09] |
| 4.4 Pre‐operative period for Ikonomidou 2004 and change scores for Lee 2005 | 2 | 119 | Mean Difference (IV, Random, 95% CI) | ‐2.09 [‐4.51, 0.34] |
| 5 Skin conductance Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Stress hormones Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Cortisol | 3 | 216 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.73, 0.09] |
| 6.2 Epinephrine | 2 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.38, 0.33] |
| 6.3 Norepinephrine | 2 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.44, 0.27] |
| 6.4 Adrenocorticotropic hormone (ACTH) | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐1.17, 0.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 8 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Procedural anxiety | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 ICU/CCU anxiety | 7 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Heart rate Show forest plot | 4 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.76 [‐6.65, 1.13] |
| 3 Blood pressure Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Systolic | 3 | 140 | Mean Difference (IV, Random, 95% CI) | ‐1.51 [‐6.65, 3.63] |
| 3.2 Diastolic | 2 | 110 | Mean Difference (IV, Random, 95% CI) | ‐5.29 [‐8.78, ‐1.79] |
| 3.3 Arterial | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐4.75 [‐13.98, 4.48] |
| 4 Respiration rate Show forest plot | 3 | 110 | Mean Difference (IV, Random, 95% CI) | ‐2.04 [‐3.43, ‐0.66] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Anxiety Show forest plot | 29 | 1812 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.74, ‐0.36] |
| 1.1 Pre‐procedural anxiety | 9 | 744 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.62, ‐0.12] |
| 1.2 Procedural anxiety | 15 | 865 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.02, ‐0.36] |
| 1.3 ICU/post‐operative anxiety | 5 | 203 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.01, ‐0.15] |
| 2 Heart rate Show forest plot | 21 | 1653 | Mean Difference (IV, Random, 95% CI) | ‐2.72 [‐4.70, ‐0.74] |
| 3 Blood pressure Show forest plot | 20 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Systolic | 18 | 1437 | Mean Difference (IV, Random, 95% CI) | ‐1.76 [‐5.09, 1.56] |
| 3.2 Diastolic | 17 | 1407 | Mean Difference (IV, Random, 95% CI) | ‐0.97 [‐2.58, 0.63] |
| 3.3 Arterial | 2 | 186 | Mean Difference (IV, Random, 95% CI) | ‐9.86 [‐12.06, ‐7.65] |
| 4 Respiration rate Show forest plot | 9 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Sedation requirements (anxiolytics) Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Midazolam (aka: Versed, Hypnovel, Dormicum, Dormonid), mg | 3 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Peripheral skin temperature Show forest plot | 4 | 298 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.08, 0.37] |
| 7 Oxygen saturation Show forest plot | 3 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.75, 0.32] |
| 8 Mood state Show forest plot | 2 | 170 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐2.17, ‐0.19] |
| 9 Satisfaction Show forest plot | 2 | 174 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [0.16, 0.76] |
| 10 Length of stay / Examination time Show forest plot | 2 | 153 | Mean Difference (IV, Random, 95% CI) | ‐6.00 [‐10.72, ‐1.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Heart rate Show forest plot | 2 | 144 | Mean Difference (IV, Random, 95% CI) | 4.67 [‐0.76, 10.10] |
| 2 Blood pressure Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Systolic | 2 | 144 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐8.59, 5.00] |
| 2.2 Diastolic | 2 | 144 | Mean Difference (IV, Random, 95% CI) | 0.99 [‐7.60, 9.58] |

