旧大陆皮肤利什曼病的干预措施
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Omdurman Hospital for Tropical Diseases, Sudan Study period: August 2007 to March 2008 (7 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: people with cutaneous leishmaniasis, confirmed microscopically by finding amastigotes in slit skin smears, if they had not received any previous treatment (Antimonial) Exclusion criteria: pregnant women, people weighing < 10 kg, malnourished people and those with a history of allergy to sulphonamides or artemisinins N randomised: 41 (group 1: n = 20, group 2: n = 21) Withdrawals: 0 N assessed: 41 (100%) (group 1: n = 20, group 2: n = 21) Mean age (SD): group 1: 30.6 years (18.0), group 2: 28.5 years (15.3) Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 8 weeks Co‐interventions: pentosan was administered to participants who failed treatment with the study drug as well as to participants who had received placebo tablets | |
| Outcomes | Healing rates: disappearance and/or shrinkage of the lesions. Lesions were identified, measured and numbered by their specific location on the participant's body before treatment and after 36 days and 72 days. Reported at the end of treatment. Adverse effects: participants were questioned about expected adverse effects for 3 days (days 5–7) following administration of the doses. These were considered drug‐related if they were not reported at presentation. | |
| Notes | Study funding sources: Dafra Pharma NV/SA, Turnhout, Belgium Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated block‐randomisation, blinded to the treating physician, was used to allocate patients to the two treatment arms" |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "a double‐blind, placebo controlled clinical trial"; "blinded to the treating physician…" Comment: not fully reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Unclear risk | Dropouts are unclear |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available; not registered in a prospective clinical trial registry |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised, prospective clinical trial Setting/location: outpatient clinic of Basra teaching hospital, south Iraq Study period: April 2004 to March 2005 (11 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania major and L tropica Inclusion criteria: all patients with cutaneous leishmaniasis who were diagnosed clinically by the same dermatologist Exclusion criteria: ≥ 20 lesions; pregnancy, lactation; hypersensitivity to pentavalent antimonials or local anaesthetic; serious medical illness, lesion in proximity to mucous membranes, face, or cartilage; implanted metallic devices; unwillingness to avoid procreation for at least 2 months N randomised: 38 participants, 70 lesions: group 1 = 35, group 2 = 35 Withdrawals: group 1: 14 lesions; group 2: 8 lesions N assessed: lesions assessed: group 1: 21 (60%); group 2: 27 (77%) Age range: 1.5 to 64 years (1.5–45 years in group 1 and 3–64 years in group 2) with a mean of 21.1 years Sex: 52.5% males, 47.5% females Baseline data:
| |
| Interventions | Type of interventions:
Both drugs were injected into the lesions in amounts of 0.1–0.5 mL according to the size of the lesion Duration of intervention: 8 weeks | |
| Outcomes | Clinical cure: resolution of active lesion with or without scarring. A scoring system was specially designed as follows. The diameter of lesions was recorded in mm using a ruler and scored as: 0 (total healing); 1 (0 cm to < 0.5 cm); 2 (0.5 cm to < 1 cm); 3 (1 cm to < 1.5 cm); 4 (1.5 cm to < 2 cm); 5 (2 cm to < 2.5 cm); or 6 (≥ 2.5 cm). The degree of induration was assessed by palpation in comparison with the participant's normal skin and given the following scores: 0, 0.5, 1, 1.5, 2, or 3. The degree of erythema was assessed visually and scored as: 0, 0.5, 1, 1.5, 2, or 3. Ulceration was scored as: 1 (present) or 0 (absent). The scores of these 4 parameters were added to give a total score for each lesion. Time points reported: the changes in total score between weeks: lesions were assessed at the start and again at 2‐week intervals after treatment for 8 weeks: 0, 2, 4, 6, and 8 weeks of treatment. Follow‐up continued for 8 weeks until complete healing took place | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Not reported; probably an open trial |
| Blinding of outcome assessment (detection bias) | High risk | Not reported; probably an open trial. No information on how lesions were assessed |
| Incomplete outcome data (attrition bias) | Unclear risk | After excluding participants who defaulted on treatment, 21/35 lesions were analysed in group 1 (HSCS) and 27/35 in group 2 (ciprofloxacin) |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Not registered in a clinical trial registry. Pre‐specified outcomes of the review were reported. Tables were not available in the links of the journal, and .pdf does not work. No adverse effects reported in the text |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Kuwait Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica or L major in the area Inclusion criteria: positive for leishmanial parasites (amastigotes) on microscopic examination. Women of childbearing age were instructed to use potent and adequate contraceptive measures before the initiation of treatment. Exclusion criteria: not described N randomised: 24. Oral itraconazole: 15; placebo: 9 Withdrawals: 0 N assessed: N = 24. Oral itraconazole: 15; placebo: 9 Age range: 12‐52 years Sex: male/female: 13/11 Baseline data: single or multiple lesions, active being nodule, nodule‐ulcerative, or ulcerative. The site of lesions including both groups was 75% on upper limbs; 46% on lower limbs; 25% on the face, and 4% on the trunk. The duration of the lesion varied between 1 and 14 months. | |
| Interventions | Type of interventions:
Duration of intervention: 6‐8 weeks Duration of follow‐up: 12 weeks post‐treatment | |
| Outcomes | Primary outcome: percentage of participants 'cured' 2 months after treatment. The response to treatment was graded as excellent (reduction in size of lesion by 80% up to complete clearance); good (reduction in size of lesion by 50%) and poor when there is minimal or no change of lesion. Secondary outcomes: duration of remission and percentage of people with treated lesions that recur within 6 months and 1, 2, and 3 years (for a period up to 3 months after suspension of the drug) Adverse effects Time points reported: 8 weeks and 12 weeks post‐treatment | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The participants were randomly divided into two groups" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The patients were randomly divided into two groups" No further information about allocation concealment was provided |
| Blinding of participants and personnel (performance bias) | Low risk | The drug and the placebo were supplied in capsules with the same shape. No information about blinding of personnel was provided but it is not likely to add risk of bias being oral administration |
| Blinding of outcome assessment (detection bias) | Unclear risk | No blinding of outcome assessment was described |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Al‐Ahssa, Saudi Arabia Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L major in the area Inclusion criteria: only a few (1‐3) simple lesions, on a non‐facial site; clinically confirmed CL by direct slit smears and/or in skin‐punch biopsies of the active, infiltrated edge of a representative lesion. Exclusion criteria: multiple or disseminated lesions, lesions aged > 6 months, pregnancy, chronic illness, immunologically compromised condition, hyperallergic reaction to the trial drugs, treatment with regular medications which may affect specific therapy, treatment with antileishmanial drugs within the previous 6 months, the presence of scars of previously healed lesions N participants (lesions) randomised: 80. IMMA group: 40 (77); ILMA group: 40 (70) Withdrawals: 13 (13). IMMA group: 9 (9); ILMA group: 4 (4) N assessed: 67. IMMA group: 31 (68); ILMA group: 36 (66) Mean age (range): range 13‐42 years. IMMA group: 29.8 years (15‐41); ILMA group: 31.5 years (13‐42) Sex: male: 48, female: 19 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention:
Duration of follow‐up: 1 month post‐treatment | |
| Outcomes | Primary outcome: percentage of lesions 'cured' at the end of treatment Secondary outcomes: prevention of scarring Adverse effects Time points reported: days 15, 30 | |
| Notes | Study funding sources: none described Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "enrolled patients were randomly assigned to one of two treatment groups" Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Quote: "enrolled patients were randomly assigned to one of two treatment groups" Comment: no further information about allocation concealment was provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information about blinding of participants and personnel was provided but the different administration via of the drug is impossible to blind, although it is unlikely to add risk of bias |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Lesions were assessed, whenever a patient came for his or her injection (s), by an observer who was unaware of the treatment the patient was receiving." |
| Incomplete outcome data (attrition bias) | Unclear risk | No information about dropouts |
| Selective reporting (reporting bias) | Unclear risk | No information about adverse effects was provided |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Al‐Ahsaa and Ryyadh, Saudi Arabia Study period: 15 months Sample size calculation: to detect a difference of 22% in the rate of healing between the placebo group and the treatment group, assuming a healing rate of 45% in the placebo group, with a power of 90% and a two‐sided type I error of 5%, 101 subjects were needed in each group. To compensate for loss to follow‐up, 25% more participants were to be enrolled in each group. | |
| Participants | Type of Leishmania:L major 56 participants (27%) Inclusion criteria: age > 12 years, presence of lesions parasitologically confirmed leishmaniasis, non‐use of antileishmanial therapy during previous 2 months Exclusion criteria: pregnancy, potential for pregnancy, breastfeeding; presence of lesions on the face or ears; presence of more than 10 lesions; history of liver disease; elevated serum, creatinine concentration, abnormal results on liver‐function tests; allergy to fluconazole N randomised: 209. 106 were assigned to the fluconazole group, and 103 were assigned to the placebo group Withdrawals: 63 received the container of capsules at the first visit and never returned for follow‐up: 37 participants assigned to receive placebo and 26 participants of fluconazole group One participant in the placebo group, who was therefore excluded from the analyses. N assessed: 145. Fluconazole group: 80, placebo group: 65 Age and sex: not described Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks Co‐interventions: SSG was offered during follow‐up if oral therapy was considered to have failed (14 participants in the fluconazole group and 33 in the placebo group) Duration of follow‐up: 1 year post‐treatment | |
| Outcomes | Healing rates:
Adverse effects Time points reported: 6 weeks, 3 months of follow‐up, 1 year post‐treatment | |
| Notes | Baseline imbalances: because of the criteria for inclusion and the limited number of women at risk for Leishmania in the study areas, there was only one female participant. Most of the participants were foreign construction workers or farmers originally from countries where CL is not endemic. One of 5 participants was a local national. Study funding sources: supported in part by a grant (no. 146‐1414) from Pfizer and the Ministry of Health of Saudi Arabia Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the randomisation sequence was generated from a random‐number table" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The randomisation sequence was generated from a random‐number table" Comment: no further information about allocation concealment was provided |
| Blinding of participants and personnel (performance bias) | Low risk | Quotes: "assigned to receive either fluconazole (Diflucan, Pfizer, New York) in the form of a 200‐mg capsule once daily for six weeks or a matching placebo" "An independent observer evaluated the rates of compliance and side effects by interviewing patients and counting their remaining capsules." |
| Blinding of outcome assessment (detection bias) | Unclear risk | No further information about blinding of outcome assessment was provided |
| Incomplete outcome data (attrition bias) | High risk | High rate of drops out: 63/209 (30.14%). Missing outcome data imbalanced in numbers across groups. Fluconazole orally 200 mg: 26. Placebo group: 37. An ITT analysis was performed |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Kuwait Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania spp not specified Inclusion criteria: only the smear‐positive cases included in the study Exclusion criteria: participants younger than 14 years and pregnant nursing women N randomised: 33. Group 1, ketoconazole 600 mg: 18; Group 2, ketoconazole 800 mg: 15 Withdrawals: 7. Group 1: 3, Group 2: 4 N assessed: 26. Group 1: 15, Group 2: 11 Age range: 14‐66 years Sex (male/female): 26/7 Severity of illness: 1‐8 lesions. Site of the lesions in the ketoconazole 600 mg group: 46% on the upper extremities and 24/% on the lower extremities. In the ketoconazole 800 mg: 58% on the upper extremities; 21% on the lower extremities and 21% on head and neck Ketoconazole 600 mg: MNL: 3.56 (range 2‐8). MDLBT: 3.4 months (range 1.5‐7) Ketoconazole 800 mg: MNL: 3.27 (range 1‐6). MDLBT: 4.5 months (range 1‐12) | |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks or until the participant was cured (whatever occurred early) Duration of follow‐up: 6 months | |
| Outcomes | Healing rates: percentage of participants 'cured' at the end of treatment ( If there was more than 90% improvement of these parameters: re‐epithelisation and decrease in the size and inflammation of the lesions, with a negative smear for Leishmania parasites) Secondary outcomes: duration of remission and percentage of people with treated lesions that recur within 6 months Adverse effects Time points reported: 1, 2, 4, 6, 8 weeks post‐treatment | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment was provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information about blinding was provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information about blinding was provided |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data balanced in numbers across intervention groups |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge. |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Walter Reed Army Medical Center (WRAMC) in Washington Study period: 24 months (2004‐6) Sample size calculation: a sample size of 27 participants per treatment group was planned, assuming a 73% cure rate for ThermoMed (TM), 99% for SSG, controlling for a probability of a type I error at alpha = 0.05 and was predicted to have 80% power to determine a 26% difference in outcome. | |
| Participants | Type of Leishmania: L major Inclusion criteria: eligible participants were Department of Defense healthcare beneficiaries with parasitologically confirmed cutaneous leishmaniasis. At Walter Reed Army Medical Center (WRAMC) in Washington. All participants were likely infected in Iraq or Kuwait. All were treatment naive. Exclusion criteria: 20 lesions; pregnancy, lactation; hypersensitivity to pentavalent antimonials or local anaesthetic; serious medical illness; lesion in proximity to mucous membranes, face, or cartilage; implanted metallic devices; unwillingness to avoid procreation for at least 2 months N randomised: 56, IVSSG: 28. Localised TM device heat treatment: 28 Participants with clinical failure at 2 months were offered cross‐over treatment. Afer 2 months: SSG: 29 (−1, +3), TM: 25 (−3, +1). Withdrawals: 2. TM: 1 (lesion not amenable to heat), SSG: 1 (not confirmed L major) N assessed: 54 (96.43%) completed treatment: TM: 27 (96.43%), SSG: 27 (96.43%). 53 (94.64%) completed 12 months follow‐up: TM: 27 (96.43%), SSG: 26 (92.86%) Median age (range): TM: 25 years (20‐53); SSG: 24 years (18‐57) Sex: TM: males: 28 (100%), SSG: males: 27 (96%), females: 1 (4%) Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: TM: 1 session. SSG: 10 days. Co‐interventions: participants randomised to thermotherapy received oral antibiotics for secondary bacterial infections of the leishmaniasis lesion(s) prior to treatment. SSG arm participants were treated concurrently with antibiotics. Follow‐up: 2, 6, and 12–24 months post‐treatment. | |
| Outcomes | Clinical cure of the lesions: clinical cure was defined as complete epithelialisation or visually healed at 2 ± 1 month after completion of therapy and no reactivation in 12 months after the start of treatment. Clinical failure was less than complete epithelialisation or visually not healed at 2 ± 1 month after treatment completion. Relapse failure was defined as skin lesion persistence at the treatment site or elsewhere in the period up to 12 months after start of therapy, regardless of appearance at 2 ± 1 month after treatment completion Laboratory cure of the lesions: microbiological cure: they looked for an eradication of the infection Time to healing: survival analysis of time to healing for the 2 treatment arms Adverse effects: toxicity profile Time points reported: 2, 6, 12 months. Toxicity profile: daily physician evaluations | |
| Notes | Study funding sources: this trial was supported by Walter Reed Army Medical Center, The North Atlantic Regional Medical Command, and the US Army Medical and Materiel Development Agency. Possible conflicts of interest: the authors have declared that no competing interests exist | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The statistician (RH) generated the randomisation plan in blocks of 4 subjects using www.randomization.com. The research pharmacist made assignments using the randomisation plan in sequential order. |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was unavailable to investigators until completion of the trial |
| Blinding of participants and personnel (performance bias) | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Sequential photographs were independently assessed by blinded leishmaniasis experts, who were clinicians experienced in the treatment of CL, with a tiebreaker assessment when needed. |
| Incomplete outcome data (attrition bias) | Low risk | 2/56 withdrawals. An ITT analysis was performed |
| Selective reporting (reporting bias) | Low risk | Clinical Trial Registration: ClinicalTrials.gov NCT 00884377; all prespecified outcomes were reported |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: 8 primary health centres around Borkhar, north of Isfahan, Iran Study period: 14 months Sample size calculation: not described | |
| Participants | Type of Leishmania: infections here were thought to be caused entirely by L major parasites, although there is probably some L tropica infection within the city of Isfahan Inclusion criteria: 2 years or older, single lesion that was parasitologically positive, < 5 cm in diameter, at least 3 cm from the eyes, lesion present < 4 months Exclusion criteria: pregnant or nursing mothers, previously treated for leishmaniasis, intercurrent illness or a history of allergy to aminoglycoside N randomised: 251, aminosidine group: 126 (134 lesions); placebo group: 125 (134 lesions) Withdrawals: not described N assessed: aminosidine group: 123 lesions; placebo group: 123 lesions Age (years): aminosidine group: < 15 years: 114, >15 years: 12; placebo group: < 15 years: 105, > 15 years: 20 Sex (male/female): aminosidine group: 64/62; placebo group: 67/58 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 14 days Co‐interventions: additional treatment, usually parenteral antimony, was given if lesions were judged to have worsened (25 participants in the PR‐treated group and 28 in the placebo group) Duration of follow‐up: 105 days after starting treatment | |
| Outcomes | Healing rates: percentage of participants 'cured' 2.5 months after treatment. Definite cure was defined as complete epithelialisation on days 45 or 105 Adverse effects Tertiary outcomes: microbiological or histopathological cure of skin lesion Time points reported: 15, 45, 105 days | |
| Notes | Study funding sources: this work was supported in part by he UNDP/World Bank/WHO Special Program for Research and Training in Tropical Diseases (TDR) and Isfahan University of Medical Sciences Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation of treatment was carried out in Geneva (Switzerland) but did not state how that was done. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Identical ointment tubes were numbered and allocated to consecutive eligible participants. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups (16 drops out of 251, 10%) |
| Selective reporting (reporting bias) | Unclear risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were pre‐specified |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: 3 primary health centres around Borkhar district north of Isfahan, Iran Study period: not described Sample size calculation: determined on the basis of a 2‐week cure rate of 50% at day 45 and unexpected 4‐week cure rate of 70% | |
| Participants | Type of Leishmania: L major Inclusion criteria: participants with a single parasitologically confirmed lesion, < 5 cm in diameter Exclusion criteria: lesions duration > 4 months and < 2 years, pregnant or nursing mothers, treated previously, any intercurrent illness or history of allergy to aminoglycoside N randomised: 233. 117 were allocated to receive 4 weeks of active treatment and 116 to receive 2 weeks of active treatment Withdrawals: 17, 9 in 4 weeks of active treatment and 8 in 2 weeks of active treatment N assessed: 216, 108 in each group. Mean age (SD): 4 weeks of active treatment: 9.2 years (8.9); 2 weeks of active treatment: 9.0 years (8.8) Sex ratio (male/female): 4 weeks of active treatment: 47/53; 2 weeks of active treatment: 44/56 Baseline data: ulcerated lesion (SD): 4 weeks of active treatment 85 (79); 2 weeks of active treatment 95 (88) | |
| Interventions | Type of interventions:
Co‐interventions: if lesions were bad enough, they were treated with antimonate Duration of follow‐up: 105 days after starting treatment | |
| Outcomes | Healing rates: 'Clinical cure' was defined as > 50% re‐epithelialisation of the original lesion, and 'clinical and parasitological cure' as either complete re‐epithelialisation or clinical cure plus a parasitologically negative smear. The primary study endpoints were clinical cure and clinical and parasitological cure at day 29, when the 4 weeks of active treatment ended Adverse effects Tertiary outcomes: microbiological or histopathological cure of skin lesions Time points reported: days 29, 45, 105 | |
| Notes | Study funding sources: this investigation was supported by the UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list after participants returned their first used tube after 2 weeks |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgment |
| Blinding of participants and personnel (performance bias) | Low risk | The vehicle and active ointments looked and smelled identical. Outcome is not likely to be influenced by the lack of blinding. |
| Blinding of outcome assessment (detection bias) | High risk | The clinical and parasitological evaluators were blinded to each other's assessment. All efforts were made to reduce the introduction of bias into this study; however, duration of the lesion, which was self‐reported by the participants or their guardians, could introduce bias if the durations were significantly different in the 2 arms by chance. |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were pre‐specified |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Skin Diseases and Leishmania Research Center of Isfahan (Iran) Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania but spp not declared Inclusion criteria: confirmed diagnosis parasitologically and clinically, lesions with duration of < 8 weeks Exclusion criteria: participants with a history of > 8 weeks, those with allergy to antimonials, lactating or pregnant women N randomised participants (lesions): 400 (539). Combined cryotherapy and ILMA: 100 (149), cryotherapy alone: 200 (230), ILMA alone: 100 (160) Withdrawals: 30 participants (46 lesions) N assessed (lesions): 370 (493). Group 1: 93 (132); group 2: 185 (210); group 3: 92 (151) Age: range 2‐65 years. Mean: group 1, 32 years; group 2, 27 years; group 3, 25 years Sex (male/female): 186/184. Group 1, 46/47; group 2, 95/90; group 3, 45/47 Baseline data: not described | |
| Interventions | Type of interventions:
Different modalities of treatment were not given to the same participant in different lesions (i.e. each participant received ILMA alone, cryotherapy alone, or combined cryotherapy and ILMA). Duration of intervention: fortnightly until complete cure or for up to 6 weeks Duration of follow‐up: 6 months | |
| Outcomes | Healing rates: percentage of participants 'cured' 2.5 months after treatment Adverse effects: mild adverse side effects, such as postinflammatory hypopigmentation and hyperpigmentation Tertiary outcomes: microbiological or histopathological cure of skin lesions | |
| Notes | Baseline imbalances: in number of participants and lesions among the groups Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The 400 patients were randomly divided into three groups" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The 400 patients were randomly divided into three groups" Comment: no further information was provided. |
| Blinding of participants and personnel (performance bias) | High risk | Treatment doesn't appear as blinded and the different treatments are difficult to blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information about blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) | Unclear risk | No good information about adverse effects. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Skin and Leishmaniasis Research Center of Isfahan (Iran) Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: not reported Inclusion criteria: age 7‐70 years, disease confirmed clinically and by laboratory methods, lesions present, surface area of lesions ≤ 5 cm² Exclusion criteria: disease duration > 4 months; pregnant or breastfeeding; chronic disease; immune suppression; and sporotrichoid forms N participants randomised (lesions): 233 (433). 123 (183) were included in the CO₂ laser group and 110 (250) in the IMMA group Withdrawals: 59 (112). CO₂ laser group: 40 (72), IMMA group: 19 (40) N assessed (lesions): 174 (321). CO₂ laser group: 83 (111), IMMA group: 91 (210) Age: range 12‐60 years Sex (male/female): 55/68 included in the CO₂ laser group; 40/70 in the IMMA group (control group) Baseline imbalances: no Severity Illness: in 47% of cases, participants had one lesion and in 53% of cases they had 2‐5 lesions. There were more lesions on the upper limbs (43%), and lesions were < 5 cm². In the remaining, the lesion duration was 2‐4 months. Mean number of lesions: CO₂ laser group: 1.49; IMMA group: 2.27 | |
| Interventions | Type of interventions:
Co‐interventions: in the first group, lesions were locally anaesthetised by injection of 1%–2% lidocaine Duration of follow‐up: 24 weeks | |
| Outcomes | Healing rates:
Adverse effects | |
| Notes | Study funding sources: none declared Possible conflicts of interest: none described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: the author was contacted. The randomisation was through coin flip method. |
| Allocation concealment (selection bias) | Unclear risk | Comment: the author was contacted. The randomisation was through coin flip method, but the method to conceal the allocation was not described. |
| Blinding of participants and personnel (performance bias) | High risk | No data provided, but the treatment is unlikely to be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided about blinding of outcome assessment |
| Incomplete outcome data (attrition bias) | High risk | Imbalance in the missing data between the groups |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Unclear risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Department of Dermatology, Isfahan University of Medical Sciences (Iran) Study period: September 2004 to May 2005 (8 months) Sample size calculation: after following a formula, sample size and number of lesions would be a maximum of 20 participants and 40 lesions, respectively, for each group | |
| Participants | Type of Leishmania: L major Inclusion criteria: confirmation of typical CL by positive Giemsa‐stained direct smear for Leishman‐Donovan bodies Exclusion criteria: > 2 lesions, lesions with > 20 mm induration diameter, duration of the disease > 2 months, previous use of any anti‐leishmanial treatments, pregnant or nursing women, children < 5 years of age, serious concomitant medical problems, history of seizure, photosensitivity N participants randomised (lesions): 60 (99). Photodynamic therapy (PDT): 20 (31); topical paromomycin: 20 (35); vehicle: 20 (33) Withdrawals (n = 3): 1 participant with one lesion in topical paromomycin group and 2 participants with 3 lesions (one participant had 2 lesions and the other had one) in vehicle group did not complete the study because they used the ointment irregularly N assessed (lesions): 57 (95). Photodynamic therapy (PDT): 20 (31); topical paromomycin: 19 (34); placebo: 18 (30) Age: range 5‐59 years. Mean (SD): PDT 22.2 years (15); topical paromomycin: 24.2 years (17); vehicle 22.3 years (15) Sex (n, (%)): PDT: female: 12 (60)/male: 8 (40); topical paromomycin: female: 8 (42.1)/male: 11 (57.9); vehicle: female: 11 (61.1)/male: 7 (38.9) Severity of illness: the most common sites of lesions (< 10) were on the extremities. Total number of lesions: PDT 31; topical paromomycin 34; vehicle 30 MNL: PDT 1.55; topical paromomycin 1.75, vehicle 1.65 Mean duration of lesions (SD): PDT 38 days (11); topical paromomycin 35 days (11); vehicle 36 days (11.6) | |
| Interventions | Type of interventions:
Duration of intervention: 4 weeks Duration of follow‐up: these groups were followed for 2 months after the end of treatment | |
| Outcomes | Healing rates: percentage of lesions 'cured' 2 months after treatment; prevention of scarring Scale: 'complete improvement' was defined as loss of induration and other signs of inflammation, complete re‐epithelialisation and return to normal skin texture as well as 'parasitological cure', i.e. a negative Giemsa‐stained direct smear. 'Partial improvement' was considered as flattening, reduction in size and induration without complete re‐epithelialisation. All lesions showing no decrease in size or induration were regarded as 'treatment failures'. Adverse effects Tertiary outcomes: microbiological or histopathological cure of skin lesions Time points reported: days 7, 14, 21, 28, 90 | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The participants were randomly divided into three groups of 20 subjects each, using computer‐based randomisation." |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "Subjects in both the paromomycin and placebo groups and the clinician treating them were blinded with respect to the topical treatment received. However, it was not possible to blind subjects in the PDT group." |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The dermatologist was not aware of the type of the treatment that the patient was receiving." |
| Incomplete outcome data (attrition bias) | High risk | No defaults were included in the analyses. No good information about adverse effects. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised, prospective, clinical trial Setting/location: Skin and Leishmaniasis Research Center of Isfahan, Barkhar Health Center and Department of Dermatology, Isfahan University of Medical Sciences (Iran) Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: fewer than 4 lesions of < 1 month old and < 3 cm, lesions not located on the face, > 15 years of age, lesions located neither on muscles nor were sporotrichoid lesions; receiving no medication for leishmaniasis Exclusion criteria: history of susceptibility to MA or miltefosine; pregnant or breastfeeding; immunosuppressed; had taken systemic medication interfering with p‐450 enzyme; or history of kidney, liver, and heart failure N randomised: 64. Topical miltefosine: 32, ILMA: 32 Withdrawals: 0 N assessed: 64 (100%). Topical miltefosine: 32, ILMA: 32 Mean age (SD): 23.12 years (13.30) Sex: topical miltefosine: 17 males (53%) and 15 females (47%). ILMA: 16 males (50%) and 16 females (50%) Baseline data: mean (SD) size of the lesions before treatment in the group treated with miltefosine and ILMA was 4.4 cm (3.1) and 2.3 cm (2.2), respectively. | |
| Interventions | Type of interventions:
Duration of intervention: 28 days | |
| Outcomes | Clinical cure: cure of cutaneous leishmaniasis was defined as follows:
Adverse effects: participants were questioned about expected adverse effects for 3 days (days 5–7) following administration of the doses. These were considered drug‐related if they were not reported at presentation. Time points reported: at the end of treatment, 1 month after treatment | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly divided into two groups" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Unclear risk | Open trials. Photography was done from all the lesions both at the first visit and all the follow‐up visits |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | High risk | Protocol not available; not registered; in clinical trial registry; adverse effects not reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Sidi‐ Bouzid. Tunisia Study period: 9 months Sample size calculation: the ideal sample size was estimated to be 120 based on a rate of success of treatment of 80%, 30%‐45% self‐healing in the vehicle group (type I error = 0.01and type II error = 0.10), and 10%‐20% loss to follow‐up | |
| Participants | Type of Leishmania: L major Inclusion criteria: aged 2‐60 years, single lesion diagnosed by the presence of parasite in stained dermal smears, no previous anti‐leishmanial treatment Exclusion criteria: known allergy, adverse reactions to aminoglycoside antibiotics, multiple lesions, an active lesion measuring > 5 cm in diameter, if their ulcerated lesion had already persisted for more than 4 months, lesions < 3 cm from the eye, who by the physician's judgment required systemic antimonial treatment: participants with serious concomitant diseases, under medication for other illnesses likely to interfere with this study; pregnant women or nursing mothers. N randomised: 132. Paromomycin group: 66; vehicle: 66 Withdrawals: 17. Paromomycin group: 9; vehicle: 8 N assessed: 115. Paromomycin group: 57; vehicle: 58 Mean age (SD): paromomycin group: 19.2 years ( 2.31); vehicle: 18.2 years (1.65) Sex (ratio M:F): paromomycin group: 1.04; vehicle: 1.07 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: twice daily for 14 days Duration of follow‐up: 105 days | |
| Outcomes | Healing rates: percentage of participants with complete re‐epithelisation of the lesion, 2.5 months after treatment initiation (105 days) Parasitological cure: percentage of lesions with negative smear and culture, 2.5 months after treatment initiation (105 days) Adverse effects Time points reported: days 15, 45, 105 | |
| Notes | Study funding sources: this investigation received funding from the United Nations Development Program/World Bank/World Health Organization Special Program for Research and TraininginTropical Diseases(grant ID:TDK910677) Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The tubes containing drug or placebo were supplied by the WHO/TDR, randomly numbered, and were given in numerical order to patients as they were admitted into the study." |
| Allocation concealment (selection bias) | Low risk | Quote: "The tubes containing drug or placebo were supplied by the WHO/TDR, randomly numbered, and were given in numerical order to patients as they were admitted into the study." |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "The code remained unknown to patients and investigators until the study had been completed" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The code remained unknown to patients and investigators until the study had been completed" |
| Incomplete outcome data (attrition bias) | High risk | No defaults were included in the analysis |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Sidi Bouzid,Tunisia, and Paris, France Study period: 22 months Sample size calculation: the protocol calculated a sample size of 50 participants per group with 80 percent power and a Type I error rate of 5 percent to detect a 30% difference in the proportion of participants achieving CCR, assuming a CCR proportion of 35% in the vehicle group and 65 percent in WR279, 396 participants, with a 5% expected rate of loss to follow‐up | |
| Participants | Type of Leishmania: L major, L tropica, L infantum Inclusion criteria: aged 5‐75 years, presence of parasitologically confirmed CL, lesions that were primarily ulcerative (i.e. not purely verrucous or nodular) and measured ≥ 1 cm² and ≤ 5 cm². Exclusion criteria: history of known or suspected hypersensitivity or idiosyncratic reactions to aminoglycoside; previous use of antileishmanial drugs (within 3 months) or nephrotoxic or ototoxic drugs; prior diagnosis of leishmaniasis; more than 5 lesions, or a lesion in the face that in the opinion of the attending dermatologist could potentially cause significant disfigurement; significant medical problems as determined by history or laboratory studies; breastfeeding and pregnancy N randomised: 92. WR279,396: 50; vehicle: 42 Withdrawals (n = 2): WR279,396: 1; vehicle: 1 N assessed (%): 90 (95.7). WR279,396: 49 (94.2), vehicle: 41 (97.6) Age < 18 years ‐ n (%): WR278,396: 47 (94), vehicle: 33 (79) Sex: male: 54, female: 38 Severity of illness: N lesions: 1: 54, 2: 16, 3: 13, 4 or 5: 9 Total lesion area (median, IQR): WR279,396: 128 (85 to 223), vehicle: 154 (70 to 264) Index lesion area (median, IQR): WR279,396: 92 (55 to 141), vehicle: 115 (50 to 172) Leishmania spp ‐ n (%): L major: WR279,396: 32 (64), vehicle: 24 (57). L Infantum: WR279,396: 1 (2), placebo: 0 (0). L tropica: WR279,396: 1 (2), vehicle: 0 (0). Unidentified: WR279,396: 16 (32), placebo: 18 (43) | |
| Interventions | Type of interventions:
Duration of intervention: 20 days | |
| Outcomes | Clinical cure: defined as complete re‐epithelialisation (i.e. length 6 width of ulceration = 060) of the index lesion by day 50 or a 50% re‐epithelialisation by day 50 followed by complete re‐epithelialisation on or before day 100 with no relapse ever having occurred from day 50 through day 180. Relapse was defined as an increase in the area of ulceration relative to the previous measurement. Participants who did not complete the 180‐day period of observation were considered to have failed to achieve complete clinical response (CCR) because relapse could not be fully assessed. Complete clinical response at the index lesion according to baseline characteristics: influence of baseline factors on effect of treatment. Time to healing: time course of complete re‐epithelialisation measured at 20, 50, 100, 180 days since start of treatment. Adverse effects: immediate: observed within 30 min of application. Delayed: observed just prior to next application | |
| Notes | Study funding sources: the Office of the Surgeon General (OTSG), Chief, Human Subjects Protection Division, U.S. Army MRMC, Fort Detrick, MD 21702‐5012. IND50,098 HSRRB Protocol#1791. Co‐sponsor: Institute Pasteur, Rue du Dr. Roux, Paris, France Possible conflicts of interest: MG has no financial competing interests | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A sequence of genuine random numbers for the randomisation procedure was obtained from the 'fourmilab.ch/hotbits' website by a member of the Department of Chemical Information, Walter Reed Army Institute of Research, Silver Spring, Maryland and purged of duplicates. The random numbers are generated by a process which takes advantage of the inherent uncertainty in the quantum mechanical laws of nature. Specifically, they are generated by timing successive pairs of radioactive decays detected by a Geiger‐Muëller tube interfaced to a computer. This process is better than the pseudo‐random number algorithms typically used in computer programs. The randomisation of the study drugs was done by an independent group, Fischer BioServices, Rockville, Maryland a contractor to The U.S. Army Medical Research Acquisition Activity (USAMRAA), Ft. Detrick, Maryland." |
| Allocation concealment (selection bias) | Low risk | The randomisation of the study drugs was done by an independent group; however, allocation concealment is not fully described. |
| Blinding of participants and personnel (performance bias) | Low risk | The vehicle lacked the active components and trace amounts of colorings agents to match the appearance and maintain the blind. |
| Blinding of outcome assessment (detection bias) | Low risk | "Investigators, who were blinded to whether participants received WR279,396 or placebo‐vehicle, evaluated lesions for clinical response on D20 (i.e. the end of the treatment period), D50 (i.e., 30 days after the conclusion of treatment), D100, and D180". Investigators measured all lesions in 2 perpendicular directions and took photographs at the following time points: prior to therapy, at the end of therapy |
| Incomplete outcome data (attrition bias) | Low risk | 49 of 50 participants randomised to WR279,396 and 41 of 42 participants randomised to placebo‐vehicle completed the study. With one exception, applications of study drugs were conducted according to the protocol |
| Selective reporting (reporting bias) | Low risk | ClinicalTrials.gov NCT00703924. Pre‐specified outcomes were reported |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Sidi Bouzid, Tunisia Study period: January 2008 to July 2011 (42 months) Sample size calculation: the sample size of 375 participants was based on estimated rates of final clinical cure of 94% in the paromomycin – gentamicin group and 71% in the vehicle‐control group, as shown in a previous study. On the basis of these rates, a sample size of 125 participants in each of these 2 groups provided a statistical power of 99% to detect a significant difference in the rates of final clinical cure rates (94% vs 71%). | |
| Participants | Type of Leishmania: L major Inclusion criteria: aged 5‐65 years; good health besides cutaneous leishmaniasis if female; absence of pregnancy and lactation; the presence of ≤ 5 lesions, with an index lesion that was ulcerative; lesions measured 1‐5 cm in diameter; lesions confirmed to contain Leishmania by means of culture or microscopical examination of lesion material Exclusion criteria: included clinically significant lymphadenopathy or mucosal involvement, against which a topical agent would not be expected to be effective N randomised: 383 (129 were assigned to paromomycin–gentamicin; 128 were assigned to paromomycin; 126 were assigned to vehicle control) Withdrawals: 8 participants (4, paromomycin–gentamicin; 3, paromomycin; 1, vehicle control) N assessed: 375 participants (125 in each of the 3 groups) Mean age (SD): 24 years (16) (paromomycin–gentamicin, 23 years (16); paromomycin, 25 years (16); vehicle 23 years (15) Sex: male 193 (51%) (paromomycin–gentamicin, 56 (45%); paromomycin, 68 (54%); vehicle control, 69 (55%)) Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 20 days | |
| Outcomes | Final cure of index lesion Total re‐epithelialisation of ulcerated lesions at 42 days Adverse effects Time points reported: 168 days | |
| Notes | Study funding sources: the study was sponsored by the Office of the Surgeon General, Department of the Army Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A permuted block randomisation schema was generated using nQuery, employing random block sizes, for the first 330 randomisation numbers. As 7 subjects were randomised that did not receive treatment at the time when the new randomisation list was generated, the plan in generating the new list was to balance the assignments in the new list for these 7 subjects to achieve the 1:1:1 allocation balance overall. The second randomisation was performed using SAS Version 9.2." |
| Allocation concealment (selection bias) | Low risk | The randomisation of the study drugs was done by an independent group. |
| Blinding of participants and personnel (performance bias) | Low risk | The placebo consisted of the vehicle without the active components and trace amounts of colorings agents to match the appearance and maintain the blind. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "The modified intention‐to‐treat population consisted of patients who received at least one dose of study treatment. We tested two hypotheses using a fixed testing‐sequence procedure with an overall two‐sided alpha level of 0.05 or less." |
| Selective reporting (reporting bias) | Low risk | ClinicalTrials.gov number, NCT00606580. Pre‐specified outcomes were reported |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised, phase I, open‐label, clinical trial Setting/location: Department of Dermatology at SP Medical College and PBM Hospital, Bikaner, India Study period: June 2009 to December 2010 (19 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: aged ≥ 4 years, 4 or fewer lesions, a parasitologically confirmed diagnosis of CL by demonstration of organisms (L tropica bodies) in the lesion smear or biopsy Exclusion criteria: included lesion size > 5 cm diameter, prior treatment failure with SSG, treatment for CL within 2 months of enrolment into the study, any chronic condition that might prevent the patient from completing the study therapy and subsequent follow‐up N randomised: 100; radiofrequency‐induced heat therapy (RFHT): 50; ILSSG: 50 Withdrawals: not described N assessed: 100 Median (range) age: RFHT: 20 years (4‐70); ILSSG: 20.5 years (4‐85) Sex: RFHT: male 27, female 23; ILSSG: male 20, female 30 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: RFHT, 5 days; ILSSG, 4 weeks Co‐interventions: all participants were prescribed oral nonsteroidal anti‐inflammatory drugs and topical antibacterial cream (fusidic acid cream) for 5 days | |
| Outcomes | Cure rate, assessed as follows:
Time points reported: 6, 8, 10, 12, 16, and 20 weeks after the initiation of treatment, and at 5, 6, 9, 12 and 18 months post‐treatment | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were N randomised in a 1:1 ratio" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "The clinician who recorded healing was blinded to the modality of treatment." Comment: not clear how the assessor was blinded |
| Incomplete outcome data (attrition bias) | High risk | No information about numbers or reasons for withdrawals during treatment. It seems that there was withdrawals only in the follow‐up: 44% at 18 months in RFHT group and 16% at 18 months in the SSG group. Losses to follow‐up were heterogeneous between groups and no ITT analyses were performed. |
| Selective reporting (reporting bias) | Low risk | Outcomes of interest were reported in results |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised single blind parallel clinical trial Setting/location: Leishmaniasis Center in Dadbin Health Care Clinic in Kerman, Iran Study period: 15 months. Participants recruitment: 8 months (December 2012 to August 2013) Sample size calculation: based on the data from previous study, and by considering the confidence interval of 95%, sample size was determined as 23 lesions per group. Regarding to a possible loss in follow‐up period, finally 32 lesions were allocated in each group | |
| Participants | Type of Leishmania: L amastigote (Leishman‐Donovan bodies) Inclusion criteria: positive direct smear or documented skin biopsy for L amastigote (Leishman‐Donovan bodies), > 2 years of age, no previous therapy for leishmaniasis, ulcerated lesions for those lesions that were included in Thio‐Ben + cryotherapy (TC) group Exclusion criteria: pregnancy, lesions on the eyelids and lips, having more than 5 lesions, positive history of confirmed immunodeficiency disorders or immunosuppression, disease duration for more than a year, positive history of allergy or hypersensitivity to thioxolone, benzoxonium chloride, or pentavalent antimony compounds. N randomised: 64 lesions of 47 participants, Thio‐Ben + cryotherapy (TC) group (32 lesions, 22 participants), ILMA (32 lesions, 25 participants) Withdrawals: 16 lesions of 9 participants (10 lesions from TC and 6 from ILMA group) were removed from the study arms because of their poor adherence to the trial protocol and lost to follow‐up. Additionally, one participant (with one lesion) was excluded because of developing a hypersensitive reaction to MA in the course of the treatment. Lesions assessed: 48 lesions in 47 participants. TC: 22, ILMA: 25 Mean age (SD): TC 23.5 years (16.4), ILMA 25.4 years (19.4) Sex (n (%)): TC: male 6 (27.2%), female: 16 (72.7%); ILMA: male 19 (76%), female: 6 (24%) Baseline data:
| |
| Interventions | Type of interventions:
Co‐intervention: in addition, at the beginning, and then every 2 weeks, cryotherapy with liquid nitrogen (−195°C) was performed for all lesions in both groups Duration of intervention: 3 months or until the lesion was cured, whichever came first Duration of follow‐up: 6 months after the termination of the treatment to evaluate the incidence of relapse (reported at 1 month, 2 months, 5 months) | |
| Outcomes | Clinical cure of the lesions:
Adverse effects Relapse: participants that developed with relapse of the lesions at the previously involved area Time points reported: clinical cure was reported when it occurs or for a maximum of 3 months. Adverse effects were assessed at follow‐up during therapy; they were the safety endpoints of the treatments, and 6 months after the termination of the treatment | |
| Notes | Study funding sources: this study was supported and funded by the Vice Chancellor for Research, Kerman University of Medical Sciences. The founder had no financial or proprietary interest in any material or method used in this study and had no role in study design, data collection and analysis, or preparation of the manuscript. Possible conflicts of interest: no conflict of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised allocation was performed by blocked randomisation method with block size of 2 |
| Allocation concealment (selection bias) | Low risk | Randomised allocation was performed by blocked randomisation method and was prepared by the analyst of the research team who had no clinical involvement in the trial. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding was impossible |
| Blinding of outcome assessment (detection bias) | Low risk | Assessing the outcomes and data analyst were blinded to group assignment. The photographs were reviewed by the dermatologist of the research team who was blinded to study groups. The photographs did not contain any indicator that could help differentiate the group of the lesion. |
| Incomplete outcome data (attrition bias) | High risk | The numbers of withdrawals were high in both groups: 31.25% (10/32) in TC group and 18.75 % (6/32) in the ILMA group. Participants were removed from the study arms because of their poor adherence to the trial protocol and lost to follow‐up. No intention‐to‐treat analysis was done. |
| Selective reporting (reporting bias) | Low risk | The study published reported our outcomes |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Aleppo, Syria Study period: June 2009 to December 2010 (19 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: not described Exclusion criteria: not described N randomised: 79 Withdrawals: 14 N assessed: 65. 46 participants (264 lesions) in the fluconazole group and 19 participants (102 lesions) in the placebo group Age (years): not described Sex: not described Baseline data: not described | |
| Interventions | Type of interventions:
Duration of follow‐up: not reported | |
| Outcomes | Healing rates: percentage of lesions 'cured' (follow‐up not reported) Adverse effects Time points reported: not described | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared This is an abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned to treatment" Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Quote: "randomly assigned to treatment" Comment: no further information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | No information about blinding was provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information about blinding was provided |
| Incomplete outcome data (attrition bias) | High risk | Quote: "Side effects were mild and similar in both groups" Comment: no further information on adverse effects was provided. Withdrawals: 14/79 (17.7%) and no ITT analyses were performed |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. Not possible to allocate to high or low risk. |
| Other bias | High risk | Sample size calculation and baseline comparability were not correctly reported |
| Methods | Study design: prospective randomised controlled trial Setting/location: dermatology clinic in Saadi Hospital, an academic center in Fars Province, Iran Study period: December 2008 to March 2010 (15 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: L major Inclusion criteria: participants that presented with skin lesions suspicious of CL, not receiving any previous treatment, positive for leishmaniasis with direct smears Exclusion criteria: pregnant and nursing women; children < 12 years old; lesions on the face; disease for more than 3 months; more than 5 active lesions; participants with any serious systemic disease or previous history of sensitivity to MA, allopurinol, or azithromycin; any difficulty in laboratory results before initial treatment (CBC diff, LFT, BUN, Cr); those who refused to sign the written informed consent form N randomised: 86 participants Withdrawals: 14 participants (6 in azithromycin + allopurinol group and 8 IMMA group) one lost follow‐up because of adverse effect N assessed: 71 participants (36 azithromycin + allopurinol group and 35 IMMA group) Mean age (SD; range): 38.2 years (12.6); range 16‐64. Azithromycin + allopurinol group: 39.7 years (12.6); IMMA: 36.8 years (12.8) Sex: 28 females and 53 males (azithromycin + allopurinol group: 13 females and 23 males; IMMA group: 15 females and 20 males Baseline data: most participants in azithromycin + allopurinol group had more than 3 lesions (72.3%) and in the IMMA group most participants also had more than 3 lesions (65.8%) | |
| Interventions | Type of interventions:
Duration of intervention: group 1, 2 months; group 2, 20 days. Co‐interventions: in case of any secondary bacterial infection, participants were with oral cephalexin for 10 days after which the antileishmanial was administered | |
| Outcomes | Cure rate, assessed as follows:
Adverse effects Time points reported: 2 months after completing treatment | |
| Notes | Study funding sources: funded by deputy of research, Shiraz University of Medical Sciences Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A total of 71 participants who met the inclusion criteria in the trial were randomly divided into two treatment groups according to simple even and odd number allocation" |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Unclear risk | Quote: "Fourteen of 86 patients dropped out due to poor compliance (six patients in the combination therapy and eight in the Glucantime group). The number and reason for their withdrawal were almost the same in both treatment groups. One patient also developed GI complications and headache while taking the combination therapy of azithromycin and allopurinol; therefore, overall 71 subjects completed the study." Comment: no ITT analyses were performed. However, withdrawals accounted for <20% and were homogeneous among the treatment groups. |
| Selective reporting (reporting bias) | Low risk | Our primary outcomes (cure and adverse effects) were described in Methods and reported in Results |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: India Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica in the area Inclusion criteria: participants with cutaneous Leishmania confirmed by the presence of L tropica bodies in the slit skin smear stained with Leishman stain. Exclusion criteria: women of child‐bearing age N randomised: 20 Withdrawals: 0 N assessed: 20 (100%). Intervention group: 15, control group: 5 Age: range 14‐56 years. Baseline data: single or multiple lesions, the duration of the lesions varied from 4 to 16 weeks | |
| Interventions | Type of interventions:
Duration of follow‐up: 6 weeks, but 3 months for relapses assessment | |
| Outcomes | Primary outcome: percentage of participants 'cured' at the end of treatment. The essential criteria for declaring the participant was cured was complete disappearance of the induration or redness in the nodular form and complete healing in the ulcerative form, accompanied by smear positivity conversion Secondary outcomes: duration of remission and percentage of people with treated lesions that recur within 3 months Adverse effects Tertiary outcomes: microbiological or histopathological cure of skin lesions Time points reported: clinical cure: 4 weeks, clinical and parasitological cure: 6 weeks | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Proportion of 2 to 4:1 Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgment |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to permit judgment |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to permit judgment |
| Selective reporting (reporting bias) | Unclear risk | All of the study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: India Study period: not described Sample size calculation: the number of subjects was determined by the standard method of Schork 1967 | |
| Participants | Type of Leishmania: L tropica in the area Inclusion criteria: demonstration of Leishmania from skin lesion by the slit smear technique. Exclusion criteria: pregnant women and children < 12 years old, suffering from any chronic illness, immunocompromised, allergic to sulphones, prior therapy for cutaneous Leishmania in any form, patients with scars of healed leishmanial lesions, lesions of > 4 months duration N randomised: 120. 60 in each group Withdrawals: 0 N assessed: 120 (100%), 60 in each group Age: range 15‐56 years Sex: 52 males/68 females Baseline data: the duration of the lesions ranged from 3 weeks to 3 months. Lesions were situated mainly on the exposed parts of the body (face, arms and feet). 46 participants (24 in dapsone group and 22 in placebo group) had a single lesion while 74 participants had multiple lesions (maximum 13). | |
| Interventions | Type of interventions:
Duration of intervention: every 12 h for 6 weeks Duration of follow‐up: 6 weeks | |
| Outcomes | Primary outcome: percentage of participants 'cured' at the end of treatment Secondary outcome: adverse effects Tertiary outcomes: microbiological or histopathological cure of skin lesions Time points reported: clinical response: days 15 and 45. Clinical and parasitological response: 6 weeks | |
| Notes | Informed consent obtained: yes Study funding sources: — Possible conflicts of interest: — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "... and was randomly allocated to receive either tablets of dapsone (100 mg) or placebo tablets which were identical in appearance" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "... and was randomly allocated to receive either tablets of dapsone (100 mg) or placebo tablets which were identical in appearance" Comment: no further information provided. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "double‐blind therapeutic trial" Comment: participants looks like blinded but no description about personnel blinding were provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "double‐blind therapeutic trial" Comment: no further information about blinding |
| Incomplete outcome data (attrition bias) | Low risk | All relevant outcome data were provided |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: India Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica in the area Inclusion criteria: participants with localised CL and only smear positive cases Exclusion criteria: not being smear positive N randomised: 60, 20 in each group Withdrawals: 0 N assessed: 60 (100%), 20 in each group Age (years): ≥ 15 years Sex: not described Severity of illness: 8, 11, and 12 participants had multiple lesions in the itraconazole, dapsone and placebo groups respectively. | |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks Duration of follow‐up: 6 weeks, but 3 months for assessment of relapses | |
| Outcomes | Healing rates: percentage of participants 'cured' at the end of treatment. Strict clinical and parasitological criteria were followed to asses cure. Adverse effects Time points reported: healing rates at the end of treatment | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: India Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania:L major and tropica in the area Inclusion criteria: participants with localised CL. Demonstration of parasites from skin lesions by slit smear examination Exclusion criteria: women of child‐bearing age, children < 18 years old, participants suffering from any chronic illness, immunocompromised, prior therapy for CLs in any form, scars of healed leishmanial lesions, lesions of 4 months or more duration, participants showing abnormality in liver function tests N randomised: 20 Withdrawals: 0 N assessed: 20 (100%) Age: range 19‐62 years Sex: 15 males/5 females Baseline data: the duration of the lesions ranged from 2 weeks to 16 weeks, they were mainly seen on exposed parts of the body. 9 had a single lesion and 11 participants had a multiple lesion. | |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks Duration of follow‐up: 3 months | |
| Outcomes | Primary outcome: percentage of participants 'cured' 3 months after treatment Secondary outcome: adverse effects Tertiary outcomes: microbiological or histopathological cure of skin lesions Time points reported: clinical response: day 15. Clinical and parasitological response: 6 weeks | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were allocated randomly to receive capsules of itraconazole 100 mg or identical placebo". Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were allocated randomly to receive capsules of itraconazole 100 mg or identical placebo". Comment: no further information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "double‐blind therapeutic trial" Comment: participants looks like blinded but no description about personnel blinding was provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "double‐blind therapeutic trial" Comment: participants looks like blinded but no description about assessment blinding was provided |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes were reported |
| Other bias | High risk | Sample size calculation, reporting of Leishmania spp involved and baseline comparability was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Pakistan at dermatology departments of Combined Military Hospital, Kharian Camtonment, Combines Military Hospital, Quetta and Combined Military Hospital, Muzaffarabad Study period: January 2008 to December 2010 (35 months) Sample size calculation: assuming equal‐sized groups, keeping the equivalence trial design, standardised difference of 0.05 and power at 90%, sample size was calculated as 150 participants in each arm using Altman nomogram. A total of 300 participants were needed for the study and 24 extra participants were recruited to cater for dropouts. | |
| Participants | Type of Leishmania: not described Inclusion criteria: men and women over 18 years of age having parasitologically proven CL requiring systemic therapy, willing for admission to hospital for the study and regular follow‐up visits, and consenting not to use any other treatment for CL during trial Exclusion criteria: pregnant, compromised immune system (i.e. diabetics or cancer patients), diffuse cutaneous or visceral leishmaniasis, complete or incomplete treatment with antimony compounds in the last 3 months, history of hepatic, renal, or cardiovascular disease N randomised: 324. Group 1: 151; group 2: 173 Withdrawals: not described N assessed: 324 (100%) Age: mean 27.9 years (SD 6.5), range 17‐48 years Sex: all were male soldiers Baseline data: most participants (39.2%) had a single lesion, but one participant had 15 lesions. Maximum lesions were found on exposed parts of body, arms and legs accounted for 42.3% and 47.2% of lesions respectively. Plaques were the most common morphological pattern seen (82.7%). Mean (SD) size of lesions at baseline was 28.8 mm (16.1). Group 1: 29.7 mm (16.4); group 2: 28 mm (15.8). Mean induration at baseline was 17.5 mm (11.6). Group 1: 17.7 mm (11.5); group 2: 18 mm (12.8) | |
| Interventions | Type of interventions:
Duration of intervention: 28 days maximum | |
| Outcomes | Successful treatment: was defined as complete re‐epithelialisation of the ulcer and disappearance of the induration, or reduction of more than 50% of the ulcer and the indurations areas in relation to the last clinical evaluation Adverse effects: serious adverse event was defined as life‐threatening, or prolongation of existing hospitalisation, or causing persistent or significant disability. Non‐serious adverse effects, not qualifying the above criteria were clinically judged by the investigator to be definitely related, probably related, possibly related, or not related to the trial medication. Time points reported: follow‐up phase lasted 6 months | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomisation through a random number table and allocation ratio being 1:1. |
| Allocation concealment (selection bias) | Unclear risk | "Randomisation sequence generation and allocation of medicine was done by lead investigators at the three research set ups" Comment: no information on the method of allocation concealment was provided |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded from the treatment groups; however, it is not clear how this was done. No placebo was provided. |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "There were 18 dropouts due to various complications, 9 belonging to each group" Comment: ITT analyses were performed. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. The trial was registered with www.anzctr.org.au and the registration number is ACTRN12607000295448. Some outcomes registered in the protocol were not reported: successful treatment; therapeutic failure; reactivation |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: the Saudi Hospital in Sanaa, Yemen Study period: 21 months; participants recruited from June 2006 to June 2007 Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania spp Inclusion criteria: all had the clinical signs of cutaneous leishmaniasis and a majority of their cutaneous lesions were found smear positive for mastigotes. 4 participants with a negative smear preparation were diagnosed by tissue culture using NNN (Novey, McNeal and Nicolle) medium Exclusion criteria: skin lesions of more than 8 weeks duration, allergic to antimonial drugs, lactating or pregnant N participants randomised (lesions): N = 30: ILSSG, n = 10 participants (12 lesions), ILSSG + IMSSG, n = 10 (15), ILSSG + oral ketoconazole: n = 10 (13) Withdrawals: no N assessed: 30 (100%) Age: range 12‐50 years (mean 23.5, SD 14). Group 1: 12‐50 (24.3, SD 15); group 2: 13‐48 years (22.5, SD 14); group 3: 12‐49 years (25.1, SD 12) Sex (male/female): group 1, 5/5; group 2, 7/3; group 3, 4/6 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: in all groups, treatment was continued until clearance or for a maximum of 3 treatment cycles at 4 week intervals (12 weeks) Follow‐up: performed monthly for 6 months after the last treatment | |
| Outcomes | Clinical cure: the cure was indicated by complete re‐epithelialisation, the disappearance of oedema, induration and other signs of inflammation and a negative Giemsa‐stained direct smear of a scraping of the skin at the lesion site. In the 4 participants diagnosed only by a positive culture before enrolment, the cure was indicated by a negative culture at the end of the 12 weeks. Adverse effects Time points reported: 4, 8, 13 weeks. Adverse effects: at the end of treatment | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "A follow‐up assessment was performed by the treating clinician, the patient and by comparing the serial photographs" Comment: open trial |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes were reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L major Inclusion criteria: PCR‐proven L major cutaneous infection, age > 12 years, not using anti‐Leishmania therapies during the past 2 months, duration of lesions < 4 moths Exclusion criteria: pregnancy, breastfeeding, presence of lesions on ears and/or face, number of lesions >10, history of liver or kidney disease N randomised: 120 participants (fluconazole 200 mg: 60; fluconazole 400 mg: 60) Withdrawals: 2 in the 400 mg group N assessed: 118 participants Mean (SD) age: fluconazole 200 mg, 36.45 years (15.34); fluconazole 400 mg, 35.38 years (13.81) Sex (male/female): 65/55 (fluconazole 200 mg, 30/30; fluconazole 400 mg, 35/25) Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks | |
| Outcomes | Complete healing: defined as complete re‐epithelialisation of the lesions at intervals of 2, 4 and 6 weeks Adverse effects Time points reported: 6 weeks | |
| Notes | Study funding sources: grant from Shiraz University of Medical Sciences, Shiraz, Iran Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were then randomized into two equal groups to receive either fluconazole 100 mg or 200 mg twice daily." Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | 2 dropouts were reported in the fluconazole 400 mg group. ITT analysis were performed. |
| Selective reporting (reporting bias) | Unclear risk | Our primary outcomes (Complete healing and adverse effects) were described in Methods and reported in Results. |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica in the area Inclusion criteria: positive direct smear or documented skin biopsy, not pregnant or nursing at the time of therapy, no serious systemic illness, no sensitivity to antimonial drugs or AL Exclusion criteria: not having received treatment for at least 2 months before entry into the study. N randomised: 150. 50 in each group Withdrawals: 0 N assessed: 150 (100%). 50 in each group Age: mean age 14 years. Group 1 (AL): 14, group 2 (IMMA): 14.5, group 3 (AL + IMMA): 14 Sex: male/female: 69/81. 23/27 in each group Baseline data: the common sites of involvement were the face and extremities. By groups were as follows: oral AL: face: 62%; upper limbs: 34%; lower limbs: 4%, and trunk: nil. IMMA: face: 48%; upper limbs: 38%; lower limbs: 14%, and trunk: nil. AL + IMMA: face: 78%; upper limbs: 15%; lower limbs: 6%, and trunk: 2%. Most participants had plaque‐type, papular, and nodular lesions. By groups: AL: plaque: 64%, papule: 29%, and nodule: 7%. IMMA: plaque: 71%, papule: 18%, and nodule: 11%. AL + IMMA: plaque: 77%, papule: 19%, and nodule: 4%. Mean number of lesions: group 1, 1.5; group 2, 1.8; group 3, 1.4. Most had multiple lesions (≤ 7 lesions) Mean duration of lesions: group 1, 8 months; group 2, 7.4 months; group 3, 8 months | |
| Interventions | Type of interventions:
Duration of follow‐up: one month | |
| Outcomes | Primary outcome: percentage of participants 'cured' at the end of treatment. The response to treatment was graded as excellent (reduction in the size of the lesion by at least 80% or complete clearance), good (reduction in the size of the lesion by 50%), and poor (minimal or no change in the lesion) Secondary outcome: adverse effects Time points reported: end of treatment and 2 and 4 weeks later | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the patients were randomly divided into three groups." Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "the patients were randomly divided into three groups." Comment: no further information provided |
| Blinding of participants and personnel (performance bias) | High risk | Comment: the treatment it is not possible to blind |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no reference to the outcome assessment blinding |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no missing outcome data |
| Selective reporting (reporting bias) | High risk | Comment: no reference to adverse effects |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Isfahan, Iran Study period: 15 months Sample size calculation: yes | |
| Participants | Type of Leishmania: L major is endemic in Isfahan Inclusion criteria: clinical and parasitological diagnosis of CL Exclusion criteria: pregnant or had > 3 lesions, ulcerative lesions, lesions with cartilage or lymphatic involvement or hypersensitivity to the drug N randomised: 96 participants, 48 in each group Withdrawals: 0 N assessed (lesions): 96 (190). 48 (95) in each group Age (years): age range 1‐48 years (mean age of 16 years old and a median of 14.5 years) Sex: male/female: 40/56 Baseline data: all lesions treated were papules or early nodules with mean diameter of about 4 mm. Mean number of lesions per person in each group: 1 | |
| Interventions | Type of interventions:
Duration of intervention: treatment was continued in both groups for 3 months or until complete recovery (return to the normal tissue texture without any atrophic changes or scar formation) Duration of follow‐up: one year | |
| Outcomes | Primary outcome: percentage of participants 'cured' within 2 months after treatment. Complete recovery or cure was defined as re‐epithelialisation and return to normal tissue texture in less than 2 months, with no residual scar or relapse after follow‐up of up to 1 year Secondary outcomes: duration of remission and percentage of people with treated lesions that recur within one year; prevention of scarring Time points reported: completely recovered (cured) (< 2 months). Healed (in 2–3 months) | |
| Notes | Study funding sources: Isfahan University of Medical Sciences (Pharmacy College and its Research Laboratory) and the Amin Leishmaniasis Research Group in Isfahan City Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "In the period of recruitment, […] they were randomised by fixed block random allocation". |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Treatment description do not appear as blinded |
| Blinding of outcome assessment (detection bias) | High risk | In statistical methods section, quote "There was no blinding method used." |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Afzalipour Hospital, Kerman University of Medical Sciences, Iran Study period: 1 year (2011‐12) Sample size calculation: a sample size of 40 participants per treatment group was planned, a probability of a type I error at alpha = 0.05 and beta = 0.1 to determine a 20% difference between topical terbinafine compared with control group | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: participants between 2‐60 years and without serious medical illness were included, not have received any other leishmanicidal treatment during last 3 months, duration of their lesions should be less than 6 months Exclusion criteria: cardiac, hepatic, renal and other systemic diseases; pregnant and nursing women; hypersensitivity to trial drugs N randomised: 80, 40 in each group Withdrawals: 0 N assessed: 80, 40 in each group Mean (SD) age: terbinafine: 16.3 years (14.8), IMMA: 20.74 years (19.4) Sex (n, %): terbinafine: male 18 (45); female 18 (45); the sex of 4 (10) participants was unknown. IMMA: male: 16 (40); female: 18 (45); the sex of 6 (15) participants was unknown Baseline data:
| |
| Interventions | Type of interventions:
Co‐interventions: Both groups received cryotherapy every 2 weeks for 4 weeks Duration of intervention: group 1: 4 weeks, group 2: 3 weeks Duration of follow up: patients were followed monthly for 3 months after the treatment. | |
| Outcomes | Clinical cure: clinical response was determined based on the following criteria:
Time to clinical cure: development of oartial and complete response to treatment in IMMA and terbinafine groups. Time points reported: the improving rate determined by measuring indurations at baseline, in the middle (day 10 for IMMA group and day14th for terbinafine group), and at the end of the study (day 21 for IMMA group and day 28 for terbinafine group) | |
| Notes | Study funding sources: Kerman University of Medical Sciences accepted the financial support of this study Possible conflicts of interest: the authors declare that there is no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was obtained by the use of a randomisation table. |
| Allocation concealment (selection bias) | Low risk | A simple block randomisation list with a block size of 4 was accumulated by a team member who was not involved in the enlistment and follow‐up of the participants. The randomisation allocation concealment was carried out by sending the randomisation numbers in envelopes to a dermatologist who was responsible for giving the assigned treatment after each participant was en‐rolled. |
| Blinding of participants and personnel (performance bias) | High risk | Different administration of treatments: oral terbinafine and IMMA. |
| Blinding of outcome assessment (detection bias) | Low risk | This study was an assessor blind trial in which the outcome assessor was unaware of the drugs used by the participants. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Selective reporting (reporting bias) | High risk | The study published does not report 2 primary outcomes: adverse effects and recurrence |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Afzalipour hospital affiliated to Kerman University of Medical Sciences and Dadbin Health Center, Kerman/Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: — Inclusion criteria: age over 7 years, positive smear or biopsy, providing informed consent Exclusion criteria: pregnant or lactating, lesions on face, more than 5 lesions, duration longer than one year, size larger than 3 cm, any treatment in past month, history of allergy to MA or dapsone, systemic diseases, taking immunosuppressive drugs in past 6 months, lupoid or sporotrichoid forms N randomised: 73 Withdrawals: 5 N assessed (lesions): 68 (73). Group 1: 33 (35); group 2: 35 (38) Mean (SD) age: 29.6 years (15.4) in group 1, 31.6 years (20.4) in group 2 Sex (male/female): intervention group: 17/16, group 2: 14/17 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: until complete healing or max 16 weeks | |
| Outcomes | Healing response: complete healing (100% epithelialisation and loss of induration), moderate healing (50‐99% epithelialisation and loss of induration), no response (less than 50% epithelialisation and loss of induration) Time points reported: 16 weeks after beginning intervention, 1 year later for recurrence | |
| Notes | Study funding sources: Kerman University of Medical Sciences Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgment |
| Blinding of participants and personnel (performance bias) | High risk | Open study |
| Blinding of outcome assessment (detection bias) | High risk | Open study |
| Incomplete outcome data (attrition bias) | High risk | No reasons for missing outcome data |
| Selective reporting (reporting bias) | High risk | One outcome of interest in the review is not reported: adverse effects, so that it cannot be entered in a meta‐analysis |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Isfahan, Iran Study period: 6 months Sample size calculation: not described | |
| Participants | Type of Leishmania: L major endemic in the area Inclusion criteria: the presence of parasitologically confirmed lesion(s) of CL, aged 12‐60 years, and otherwise healthy on the basis of medical history and physical examination Exclusion criteria: women of childbearing age without adequate effective contraception; pregnant or breastfeeding; duration of lesions > 8 weeks; the presence of lesions on face, joints or near the mucous membranes; the presence of > 5 lesions or any lesion with a diameter > 5 cm; history of any antileishmanial therapy in the past 4 weeks N participants randomised (lesions): 72 (106). 36 (53) treated with zinc sulphate (ZS) and 36 (53) treated with ILMA Withdrawals participants (lesions): 37 (56). ZS group 23 (34): unresponsive: 12, lost to follow‐up: 5, non‐medical events: 2, protocol deviation: 2, complications: 1, patient request: 1. ILMA 14 (22): unresponsive: 2, lost to follow‐up: 10, non‐medical events: 1, patient request: 1 N assessed (lesions): 35 (50). 13 (19) treated with ZS and 22 (31) treated with ILMA Mean (SD) age: 20.2. years (9.6). ZS group: 18.1 years (6.1); ILMA: 22.3 years (11.2) Sex (male/female): 33/39. ZS group: 19/17; ILMA group: 14/22. Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: up to 6 weeks Duration of follow‐up: 5 weeks | |
| Outcomes | Healing rates: percentage of lesions 'cured' 5 weeks after treatment. Complete re‐epithelialisation of each ulcer with marked reduction in induration with or without scarring was considered as the main efficacy parameter. Amount of injection into each lesion Adverse effects: the pain experienced by the participant (using a verbal analogue scale on a 0‐10 scale) was recorded Time points reported: 6 weeks | |
| Notes | Study funding sources: this study was supported by a grant from Chancellery of Research, Tehran University of Medical Sciences. Possible conflicts of interest: none declared The plot and the figures were not matched accordingly | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Low risk | The randomisation sequence was concealed from the investigators until the data entry was completed and the data bank was locked. |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Double‐blind" Comment: the preparation and coding of drugs were done by a pharmacist outside of the research team and investigators were blinded to them |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | High rate of dropouts (37/72, 54%). Missing outcome data imbalanced in numbers and reasons across intervention groups. ZS group: 23. ILMA group: 14. 'As‐treated' analysis done with substantial departure of the intervention received from that assigned at randomisation |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Mashad, Iran Study period: 18 months Sample size calculation: 45 participants per treatment group were needed to have 80% power to detect a significant difference in the expected cure rate of 50% in the vehicle group and the desired cure rate of 80% in the imiquimod‐treated group at week 8 with a type Ierror level of 0.05. To compensate for 20% estimated dropout, 54 participants would be required in each group. | |
| Participants | Type of Leishmania: L tropica endemic in the area Inclusion criteria: parasitologically proven cases of CL based on positive smear or culture, otherwise healthy participants Exclusion criteria: pregnant or lactating women, duration of the lesions > 6 months, number of lesions > 5, any lesions > 5 cm, history of any standard course of treatment with antimonials, history of allergy to antimonials, serious systemic illnesses, participation in any drug trials in the last 60 days N participants randomised (lesions): 119 (252). 59 (128) participants in the imiquimod group and 60 (124) in the vehicle group Withdrawals: 30 participants. Imiquimod group (n = 17): 9 lost to follow‐up, 4 inadequate efficacy, 3 protocol deviation, 1 consent withdrawal. Vehicle group (n = 13): 9 lost to follow‐up, 2 inadequate efficacy, 2 protocol deviation N assessed: 89. 42 participants in the imiquimod group and 47 in the vehicle group Mean (SD) age: 27.0 years (SD 1, range 12‐60). Imiquimod group: 7.4 years (13); vehicle group: 6.5 years (12) Sex: approximately 50%‐55% of the participants were female (35/59 in the imiquimod group, and 31/60 in the vehicle group) Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: imiquimod and vehicle 3 times per week for 28 days, IMMA 20 mg/kg/d for 14 days Duration of follow‐up: 20 weeks after initiation of treatment | |
| Outcomes | Primary outcome: percentage of participants 'cured' 3.5 months after treatment. Clinical cure of the participants, defined as more than 75% reduction in the size of lesions compared with baseline Secondary outcomes: the relapse rate (defined as a reappearance of lesions at the site or periphery of previously healed lesions or an increase in the size of lesions after initial improvement) was assessed 16 weeks after the end of treatment Adverse effects Time points reported: at the end of the treatment period (week 4) and 4 weeks later Intention‐to‐treat analysis of rates of complete re‐epithelialisation, clinical cure, and clinical improvement at weeks 4, 8,and 20 after initiation of treatment | |
| Notes | Study funding sources: this study was supported by the Small Grants Scheme for Operational Research in Tropical and Other Communicable Diseases from the Joint World Health Organization Eastern Mediterranean Region Division of Communicable Diseases and the Special Program for Research and Training in Tropical Diseases. Possible conflicts of interest: the funding source was involved in the study design, in the writing of the manuscript, and in the decision to submit the manuscript for publication, but not in the collection, analysis, or interpretation of data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly divided into 2 groups according to a list made by a simple randomisation block design" |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomisation allocation concealment was performed by sending the randomisation numbers in envelopes to a pharmacist who was responsible for giving the assigned treatment after each eligible patient was enrolled." |
| Blinding of participants and personnel (performance bias) | High risk | Treatment unlikely to be blinded. This study was a single‐blind trial. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "To keep the trial blinded, the physicians who were responsible for evaluation of patients were uninvolved in the process of allocation and drug dispensing and were unaware of the drug used by the patients." |
| Incomplete outcome data (attrition bias) | High risk | Withdrawals: 30/119 (25.2%); no ITT analyses performed |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Iran Study period: 24 months Sample size calculation: yes | |
| Participants | Type of Leishmania:L major Inclusion criteria: CL confirmed with direct smear, age 5‐50 years, maximum number of lesions 3, duration of disease < 100 days Exclusion criteria: previous treatment for leishmaniasis, use of immunosuppressives, history of chronic systemic disease, lesions on face, pregnancy or lactating, age < 5 years, duration of disease > 100 days N randomised: 197 Withdrawals: 26 N assessed: 171. 96 were treated with garlic 5% cream and 75 with vehicle Mean age: garlic, 18.5 years; vehicle, 23.7 years Sex (male/female): garlic, 51/45; placebo, 38/37 Baseline data: not reported | |
| Interventions | Type of interventions:
Duration of intervention: both applied twice daily under occlusion with sterile gauze for 3 hours, for 20 days Duration of follow‐up: 60 days (after the 3 week treatment, participants were followed for another period of 40 days) | |
| Outcomes | Healing rates: percentage of participants 'cured' one month (40 days) after treatment Time points reported: yes | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared We only have the abstract. The author (A Khamesipour) was contacted and kindly agreed to extract the data from the original paper written in Persian. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | List generated by a computer |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Low rates of dropouts (26/197; < 25%) |
| Selective reporting (reporting bias) | Unclear risk | All relevant outcomes reported |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Aleppo, Syria Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: up to 3 lesions diagnosed clinically and parasitologically as CL; absence of chronic or intercurrent systemic disease Exclusion criteria: pregnancy and no prior antimonial medication N randomised and withdrawals: not reported N participants assessed (lesions): 40 (75) ILMA: 20 (38); IFN‐γ: 20 (37) Mean age (range): ILMA: 21 years (6‐60); IFN‐γ: 27 years (12‐57) Sex (male/female): 17/23. ILMA: 9/11; IFN‐γ: 2/12 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: once weekly for 5 weeks Duration of follow‐up: 10 weeks | |
| Outcomes | Primary outcome: percentage of lesions 'cured' one month after treatment Secondary outcome: adverse effects Tertiary outcomes: microbiological or histopathological cure of skin lesions Time points reported: weeks 3, 6, 10 | |
| Notes | Study funding sources: none reported Possible conflicts of interest: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table method used |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information about allocation concealment |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: no information about blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no information about blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | No losses to follow‐up were reported. |
| Selective reporting (reporting bias) | Low risk | Comment: all relevant outcomes provided |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Department of Dermatology, Isfahan Medical University, Iran Study period: 10 months Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania spp: due to a previous study in the area, it was likely that participants were infected with L major Inclusion criteria: proven leishmaniasis based on typical lesions of ACL and a positive direct smear. Number of lesions < 4 and duration of lesion < 12 weeks Exclusion criteria: cases of reinfection, pregnant or nursing women, those who had lesion on the face or joints and participants with sporotrichoid or erysipeloid lesions N randomised: 104. ILMA: 55, zinc sulphate (ZS): 49 Withdrawals: 38. ILMA: 20, ZS: 18. 13 due to occurrence of new lesions: 7 from ILMA group and 6 from ZS group; 6 participants with sporotrichoid spread: 4 from the ILMA group and 2 from the ZS group; 19 participants lost to follow‐up: 9 from the ILMA group and 10 from the ZS group N assessed: 66. ILMA: 35, ZS: 31 Mean age (range): ILMA: 11 years (2‐67); ZS: 12 years (3‐64) Sex (male/female): 50/54. ILMA: 14/21; ZS: 17/14 Baseline imbalances: sex distribution in each group Severity of illness: Mean duration of lesions (SD) (weeks): ILMA: 6.73 ±0.53 ;ZS: 7.64±0.12 . | |
| Interventions | Type of interventions:
In cases where there was a slight to mild improvement, another injection was given after 2 weeks Duration of intervention: 2‐6 weeks Duration of follow‐up: 6 weeks | |
| Outcomes | Healing rates: percentage of participants 'cured' at the end of treatment. The results of treatment were graded according to the system of Sharquie 1997 slight = 1, mild = 2, moderate = 3, marked = 4, 5 = total clearance of the lesion and parasite not detected in the affected area by smear Adverse effects Time points reported: 2, 4, 6 weeks | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were treated randomly with intralesional injection of any of 2 similar 50‐mL vials marked A (MA) or B (ZS) by an independent physician. ZS solution was prepared by dissolving 2 g ZS (ZNSO4W 7H2O) per 100 mL of bidistilled deionised water. The blinding was unlikely to have been broken. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Low risk | The study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way |
| Other bias | High risk | Sample size calculation, reporting of Leishmania spp involved and baseline comparability was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Iran Study period: not described Sample size calculation: the required sample size, 40 in each treatment group, was estimated, assuming one in every 4 cases would not provide full data, using the formula n = [Z1 − (a/2) + Z1 − b] 2 × [P1(1 − P1) + P2(1 − P2)]/(P1 − P2)2, and setting P1 (the paromomycin efficacy) to 0.7, P2 (the vehicle efficacy) to 0.3, a to 0.05, b to 0.1, Z1 − (a/2) to 1.96, and Z(1 − b) to 1.64 | |
| Participants | Type of Leishmania: L tropica and L major are responsible for hyperendemic CL in rural areas and endemic CL in parts of many cities in Iran Inclusion criteria: had the clinical signs of CL and all of their cutaneous lesions were found smear‐positive for amastigotes Exclusion criteria: cases who had first noticed a skin lesion > 3 months previously, had lesions on their face, had lesions with diameter of > 3 cm, had received previous treatment, or who were lactating or pregnant N randomised: 80, 40 in each group Withdrawals: 15. Intervention group: 10; control group: 5 N assessed: 65. Intervention group: 30; control group: 35 Age: range 8‐55 years. Mean intervention group: 21.4 years; control group: 21.5 years Sex (male/female): 33/32. Intervention group: 19/11; control group: 14/21 Baseline data: mean duration of lesions (years): intervention group: 1.65; control group: 1.75 | |
| Interventions | Type of interventions:
Duration of intervention: 30 days Duration of follow‐up: for clinical and parasitological follow‐up on day 30 and for only parasitological follow‐up on day 60 | |
| Outcomes | Healing rates: percentage of participants 'cured' one month after treatment, clinical and parasitological cure
Adverse effects Time points reported: days 30 (clinical and parasitological follow‐up) and 60 (parasitological follow‐up) | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The cases enrolled were assigned to two treatment groups, placebo or paromomycin, using computer‐based randomisation." |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Study was described as "double blind" but no description about allocation method was given. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No blinding of outcome assessment described |
| Incomplete outcome data (attrition bias) | Unclear risk | No data about dropouts were given |
| Selective reporting (reporting bias) | Low risk | Relevant outcomes were reported |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Saudi Arabia (Bahrain) Study period: 12 months Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: proved positive for Leishmania parasites (amastigotes) on microscopic examination or biopsy Exclusion criteria: not described N randomised: 62. Rifampicin: 46; placebo: 16. Rifampicin: 2 groups were analysed; group 1a (children aged 3‐11 years ‐ mean age, 7.5 years), and group 1b (adults aged 12‐65 years ‐ mean age, 33 years). 32 participants enrolled in group 1a and 30 in group 1b. Out of these, 8 participants in each group (16 in total) served as control to receive the placebo. Withdrawals: 21 participants lost to follow‐up. Rifampicin: 12; placebo: 9 N assessed: 41. Rifampicin: 34; placebo: 7. Number participants imbalanced between groups Age: range 3‐65 years; mean 20 years Sex (male/female): 43/19 Baseline data: the duration of the lesions varied between 1 and 12 months (mean 2.6 months). The lesions of CL were single or multiple and were mostly over the extremities (upper limbs 51% and lower limbs 38%) and to a lesser extent on the face 30%. Most of the lesions were active being nodular, nodule‐ulcerative, or ulcerative. 2 of the participants were members of the same family. However, the rest of the participants had a negative family history. | |
| Interventions | Type of interventions:
Duration of intervention: 2 equally divided doses during meals for 4‐6 weeks Duration of follow‐up: 3 months | |
| Outcomes | Primary outcome: percentage of participants 'cured' 3 months after treatment Secondary outcomes: duration of remission and percentage of people with treated lesions that recur up to 3 months of follow‐up Adverse effects | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomized" Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Comment: "Randomized" but no further information was provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "Each subject in the control group was given placebo, which was supplied, in capsules/suspension identical in shape and colour to that given in the rifampicin group." Participants look blinded but no information about personnel were provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: "Double‐blinded" but no further information |
| Incomplete outcome data (attrition bias) | High risk | There is a 38.87% of follow‐up, the percentage is very different between the groups, and it isn't explained. |
| Selective reporting (reporting bias) | High risk | No adverse effects data available |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Skin Disease and Leishmaniasis Research Center of Isfahan (SDLRC), Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: not described Exclusion criteria: not described N randomised: 140 participants Withdrawals: 64 N assessed: 76 participants (47 with ILMA and topical Cassia fistula fruit gel and 29 participants in vehicle group) Age: not described Sex: not described Baseline data: not described | |
| Interventions | Type of interventions:
Duration of intervention: not described | |
| Outcomes | Cure: complete cure, partial cure and treatment failure Adverse effects (itching and erythema) Time points reported: 12 weeks | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared We only have the abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "140 patients with cutaneous leishmaniasis referring to Skin Diseases and Leishmaniasis Research Center of Isfahan (SDLRC) were randomly allocated in two groups" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Low risk | Comment: the vehicle came exactly in the same colour and shape as the drug and the application procedure was also the same. We think the outcome is unlikely to be influenced by lack of blinding of personnel. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Unclear risk | There is no information about withdrawals. |
| Selective reporting (reporting bias) | Low risk | Our primary outcomes (cured and adverse effects) were described in the Methods and reported in the text. |
| Other bias | High risk | Sample size calculation, inclusion criteria, reporting of Leishmania spp involved and baseline comparability was not correctly reported |
| Methods | Study design: double‐blind, randomised controlled study Setting/location: Isfahan, Iran Study period: January 2009 to February 2010 (13 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: met the histological criteria for presence of parasite, age > 5 years, acute leishmanial lesions smaller than 5 cm², fewer than 5 lesions, more than 3 months of disease duration Exclusion criteria: pregnancy, women of childbearing age, history of administration of immune suppressive drugs in the last 6 months or anti‐leishmanial drugs in the last month N randomised: 60 participants, 30 in each group Withdrawals: 0 N assessed: 60, 30 in each group Mean (SD) age: 25.29 years (4.01). Achillea millefolium 5%: 25.8 years (3.7); vehicle: 24.6 years (4.2). Sex: 15 (25%) female; 45 (75%) male. A millefolium: 7 (23.3%) female, 23 (76.6%) male; vehicle: 8 (26.6%) female, 22 (73.3%) male) Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 4 weeks Co‐interventions: all participants received 4 weekly an injections of MA (Glucantime, Paris, France) at a dose of 20 mg/kg | |
| Outcomes | Definition: complete or partial cure of lesions Time points reported: week 12 (visits months ‐ 3) | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "During this double‐blind randomised study, 60 patients were randomised into two treatment groups by using random allocation computer software." |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "During this double‐blind randomised study ..." Quote: "Both gels were identical in terms of the colour and consistency." |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No losses to follow‐up were reported, therefore ITT analyses performed |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised parallel clinical trial Setting/location: Skin Diseases and Leishmaniasis Research Center (SDLRC), Isfahan, Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: 6‐60 years old, with positive results of leishmaniasis smear test Exclusion criteria: size of lesion > 3 cm, > 5 lesions, lesion duration > 12 weeks, lesion located on the eyelid or < 2 cm away from the eye, pregnant or lactating N randomised: 165, 55 in each of 3 treatment groups Withdrawals: 7; 3 (5.5%), participants were in the concentrated boiled extract group and 2 (3.6%) participants in the other groups withdrew from the study due to the allergic reaction to the medications N assessed: 158. Concentrated boiled extract of Cassia fistula: 52; hydroalcoholic extract of C fistula: 53; ILMA: 53 Mean (SD) age: boiled extract of C fistula: 20.6 years (12.4); hydroalcoholic extract of C fistula: 19.8 years (11.5); ILMA: 22.9 years (13.6) Sex (n,(%)): boiled extract of C fistula: male: 35 (63.6), female: 20 (36.4); hydroalcoholic extract of C fistula: male: 29 (52.7), female: 26 (47.3); ILMA: male: 25 (45.5), female: 30 (54.5) Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: until complete resolution of the lesion (complete epithelialisation) or for a maximum duration of 4 weeks. Follow‐up: 3 months after completing the project, they were examined every month to assess the recurrence of the lesions | |
| Outcomes | Clinical and parasitological cure: lesions were considered completely cured (improvement), if the participants achieved both clinical and parasitological resolutions (negative results of direct smear). Participants were considered resistant to the treatment, if no clinical changes were observed in the lesion or it was worsened. Time to healing: comparison of complete cure time of the cutaneous Leishmaniasis lesions between 3 groups Adverse effects: allergic reaction to the medications Time points reported: week 1, 2, 3, 4, 16, complete cure | |
| Notes | Study funding sources: the study was self‐funded Possible conflicts of interest: there was no conflict of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The participants were randomly allocated to 3 groups using table of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Different administration of treatments: 2 groups: apply the extract‐soaked gauze; third group: ILMA |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons (allergic reaction to the medications) of withdrawals were similar and small in 2 of the groups 3.5% (3/28) in concentrated boiled group vs 3.6% (2/28) in the other groups. |
| Selective reporting (reporting bias) | Low risk | The study published reports our primary outcomes: cured and adverse effects |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Leishmania Clinic of the German Medical Service (GMS), Darwaze‐e‐Lahory, 1st district, Kabul, Afghanistan Study period: 36 months (2004‐7) Sample size calculation: sample size was calculated based on the primary outcome (i.e. complete wound healing). A number of 40 participants each was calculated to be necessary to obtain a power of 80% (significance level 5%). A presumed dropout rate of 20% led to a minimum total enrolment of 100 participants | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: male or female participants of the GMS Clinic; 5 years of age or older; with non‐ulcerated (papule/nodule) or ulcerated lesions (ulcer with or without crust); presence of at least one parasitologically confirmed CL lesion and no prior history of leishmaniasis and/or anti‐parasitic treatment Exclusion criteria: participants below age 5; with the presence of CL lesion(s) on or immediately adjacent to the nose, lips or eyes; pregnancy, or serious co morbidities N randomised: 135. Group 1: 73; group 2: 62 Withdrawals: due to protocol breach: group 1, n = 14; group 2, n = 8. Lost to follow‐up: group 1, n = 21; group 2, n = 22 N assessed: 113 (83.7%): group 1: 59 (80.82%); group 2: 54 (87.09%). Mean age (range): group 1: 18.62 years (5‐66); group 2: 18.16 years (6‐63) Sex (male/female): 93/42; group 1: n = 51/22; group 2: n = 42/20. Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: time to wound closure Co‐interventions: systemic antibiotics were only given if bacteria were detected and the wound infection was severe. Neither local nor systemic antifungal therapy was allowed to exclude anti‐protozoal effects on the Leishmania infection | |
| Outcomes | Primary outcome ‐ time to wound closure (days): the time needed for complete epithelialisation of the lesion wound was defined and photodocumented. Secondary outcome ‐ microbiological cure: the parasite load (Leishmania/g) of the lesions was taken prior to electrocauterisation (1st time), after wound closure (2nd) and after 6 months (3rd) Adverse effects: such as bacterial or fungal superinfections of the wounds, the formation or scars and the rate of re‐ulcerations were monitored during the treatment and follow‐up period | |
| Notes | Possible conflicts of interest: not described Study funding sources: this study was supported by the German‐Academic Exchange Service (travel grants to KWS, AFJ and FM), the Senior Expert Service (travel grants to KWS) and the Interdisciplinary Center of Clinical Research at the Universitätsklinikum Erlangen (IZKF, project A49 to US and CB). The founders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "subjects were randomly assigned with the help of a GMS computer at a ratio of 1:1" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "RS and KWS were responsible for the enrolment of the patients and their assignment to the treatment groups." Comment: not further information was provided regarding the method for allocation concealment. |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "The participants, the medical personnel treating and evaluating the patients, the investigators analysing the clinical course of treated lesions, as well as the lab members performing the parasitological analyses were blinded. The preparation of the two different gels (marked as jelly A and B), which could not be visually distinguished, was performed by a technician who was not involved in the treatment of patients". |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The participants, the medical personnel treating and evaluating the patients, the investigators analysing the clinical course of treated lesions, as well as the lab members performing the parasitological analyses were blinded. The preparation of the two different gels (marked as jelly A and B), which could not be visually distinguished, was performed by a technician who was not involved in the treatment of patients". |
| Incomplete outcome data (attrition bias) | Unclear risk | 14 participants of group 1 and 8 participants of group 2 were retrospectively excluded due to deviations from the study protocol. For the follow‐up analysis, 6 months after wound healing, only 70 participants could be included, as 21 participants of group I and 22 participants of group II did not observe their appointments. |
| Selective reporting (reporting bias) | Low risk | Main outcomes were included. Trial was registered at clinicaltrial.gov: NCT00947362 |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: double‐blind, randomised placebo‐controlled clinical trial Setting/location: south of Iran Study period: October 2007 to January 2009 (15 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: L major and L tropica Inclusion criteria: men and women aged at least 12 years old, positive smear and/or polymerase chain reaction (PCR) for CL, cutaneous lesions of less than 4 months' duration Exclusion criteria: pregnancy and lactation, facial lesions, lesions of more than 4 months' duration, complete or incomplete treatment with a systemic or topical medication within the previous month, drug sensitivity N randomised: 100 participants Withdrawals: 37 participants N assessed: 63 participants (36 in treatment and 27 in control group) Age: range 12‐62 years (mean 32.6 (SD 12) in the treatment group and 33.1 (14) in the vehicle group) Sex (male/female): 35/28 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 12 weeks Co‐interventions: simultaneously, cryotherapy once a week and aqueous cream containing 3% salicylic acid (emulsifying ointment 30 g, phenoxyethanol 1 g and freshly boiled and cooled water 69 g) | |
| Outcomes | Clinical response:
Adverse effects Time points reported: 12 weeks | |
| Notes | Study funding sources: not described Possible conflicts of interest: no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "This investigation was designed as a 12‐week, double blind, N randomised, placebo‐controlled study and its protocol was approved by the ethics committee of the vice chancellor of research affairs of Shiraz University." Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "The identically coded and packaged creams were applied two times daily." Quote: "The study was blinded to both the patients and the assessing physician." |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The study was blinded to both the patients and the assessing physician." |
| Incomplete outcome data (attrition bias) | High risk | 100 participants were enrolled but only 63 completed the study. Reasons for withdrawal were not reported. |
| Selective reporting (reporting bias) | Low risk | Our primary outcomes (cure and adverse effects) were described in Methods and reported in Results |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Center for Research & Training in Skin Diseases & Leprosy, Tehran University of Medical Sciences, Tehran, Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica and L major Inclusion criteria: the participants with CL who attended to Center for Research & Training in Skin Diseases & Leprosy, Tehran University of Medical Sciences, Tehran, Iran. The diagnosis was based on clinical findings and physical examination and confirmed by Giemsa‐stained direct smear of the lesion Exclusion criteria: ore than 5 lesions; lesions greater than 5 cm in diameter; received anti‐CL treatment during the previous month; lesions on the face and around vital organs; diabetic individuals; pregnant, lactating female participants; subjects with active infectious diseases N randomised: 85. Group 1: mesotherapy administration of meglumine antimonate: 41. Group 2: ILMA injection: 44 Withdrawals: 25. Group 1: 11 (7 lost to follow‐up, 3 inadequate efficacy, 1 allergic reaction). Group 2: 14 (10 lost to follow‐up, 2 inadequate efficacy, 2 allergic reaction) N assessed: 60 (70.59%). Group 1: 30 (73.17%), group 2: 30 (68.18%) Mean (SD) age: Group 1: 25.24 years (16), group 2: 24.32 years (15.26) Sex (male/female): Group 1: 19/11, group 2: 17/13 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks or until complete cure | |
| Outcomes | Clinical cure: 3 categories were defined for ulcer healing: complete cure: complete re‐epithelialisation of the ulcer with loss of induration; partial cure: 25 to 99% re‐epithelialisation of lesions; failure: less than 25% re‐epithelialisation of lesions. Improvement of the lesions: ulcer improvement (cm), induration improvement (cm), induration improvement (cm), speed of improvement (cm/week), speed of erythema improvement (cm/week), scare size (cm) Microbiological cure: Leismanian body: negative, positive. Pain severity during injection: visual analogue scale (VAS; 0 to 10). Amount of drug used (mL/cm²) and number of treatment sessions Adverse effects Time points reported: 3 months after treatment. Adverse effects: after the each treatment session. | |
| Notes | Study funding sources: this study was supported by a research grant from Center for Research & Training in Skin Diseases & Leprosy, Tehran University of Medical Sciences, Tehran, Iran Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible patients were randomised according to a computer generated simple randomisation list to be treated with intralesional injection of MA using either the classic method or mesotherapy gun." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | High risk | 14/44 participants with the conventional technique and 11/41 with mesotherapy gun withdrawn the study (29.4%) |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available; not registered in a trial registry; SD not provided for pain severity (VAS) Insufficient information to permit judgment |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Bam and Mashhad in Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: parasitologically proven cases of CL; otherwise healthy subjects on the basis of medical history, physical examination and results of blood tests; age 12–50 years; body weight >40 kg; willingness to participate in the trial and signing the informed consent Exclusion criteria: not described N randomised: 138 participants (75 in IMMA and 63 in miltefosine) Withdrawals: 33 in IMMA and 32 in miltefosine N assessed: 42 in IMMA arm and 31 in miltefosine Age (years): not described Sex: not described Baseline data: not described | |
| Interventions | Type of interventions: Group 1: oral miltefosine 2.5/kg/d for 28 days Group 2: IMMA 60 mg/kg/d for 14 days Duration of intervention: not described Co‐interventions: not described | |
| Outcomes | Healing of their lesions and occurrence Adverse effects Time points reported: participants were evaluated weekly for 28 days and then 1 month later | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote:"This open N randomised controlled trial was carried out in Bam and Mashhad in Iran …" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Quote:"This open N randomised controlled trial was carried out in Bam and Mashhad in Iran …" |
| Blinding of outcome assessment (detection bias) | High risk | Quote:"This open N randomised controlled trial was carried out in Bam and Mashhad in Iran…" |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up quite high (around 50%) Intervention group: 32/63= 50.8% Control group: 33/75= 44% |
| Selective reporting (reporting bias) | Unclear risk | It is an abstract. At least they reported complete cure of cases and adverse effects. |
| Other bias | High risk | Sample size calculation, reporting of Leishmania spp involved and baseline comparability was not correctly reported |
| Methods | Study design: randomised, assessor‐blind, controlled clinical trial Setting/location: Kashan, Tehran, Iran Study period: September 2008 to April 2010 (19 months) Sample size calculation: 56 lesions per treatment group were needed to have 80% power to detect a significant difference in the expected cure rate of 60% in the ILMA alone group and the desired cure rate of 85% in the ILMA and either silver or non‐silver dressing‐treated group at week 10 with a type I error level of 0.05. Compensating for a 20% loss‐to‐follow‐up, recruiting 68 (round up to 70) lesions per treatment group looked reasonable. | |
| Participants | Type of Leishmania: L major Inclusion criteria: parasitologically confirmed cases of CL based on positive smear and/or culture; otherwise healthy subjects on the basis of medical history; age of 12‐60 years; willingness to participate in the study and signing the informed consent form (by the participant or his/her parent/guardian in cases younger than 18 years). Exclusion criteria: pregnant or lactating women; duration of lesion more than 3 months; number of lesions more than 5; ulcer size greater than 5 cm in largest diameter; history of receiving full course standard treatment (antimonials); history of allergy to MA or silver; serious systemic illnesses (as judged by the physician); participation in any drug trials in the last 60 days; indication for systemic treatment with MA; presence of secondary bacterial infection of the lesion according to clinical appearance N randomised: 83 participants (158 lesions) ILMA: 26 participants (45 lesions); ILMA + non‐silver dressing: 26 participants (53 lesions); ILMA + silver dressing: 31 participants (60 lesions) Withdrawals: 10 participants (18 lesions) N assessed: 73 (140 lesions) Mean (SD) age: 28.81 years (14.45). ILMA: 32.88 years (12.92); ILMA + non‐silver dressing: 30.31 years (15.41); ILMA + silver dressing: 24.13 years (13.97) Sex: male 39; ILMA: male 8; ILMA + non‐silver dressing: male 11; ILMA + silver dressing: male 20 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks | |
| Outcomes | Clinical cure (complete healing defined as more than 75% reduction, clinical improvement defined as 50%–75% reduction, and no response to treatment defined as less than 50% reduction in the size of the lesion compared with baseline) Relapse: defined as a reappearance of lesions at the site or periphery of previously healed lesions or an increase in the size of lesions after initial improvement was assessed 5 months after the termination of treatment Adverse effects: itching and burning, exudation, oedema, and dermatitis Time points reported: oucomes were assessed at the end of the treatment period (end of week 6), then at 4 weeks and 5 months after the last treatment session | |
| Notes | Study funding sources: the budget of the research project has been provided by the Vice‐Chancellery of Research of Tehran University of Medical Sciences. Possible conflicts of interest: the authors have declared that no competing interests exist. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A random sequence generated by using the online software Random Sequence Generator, which is available at URL: www.random.org [22]. It was done by an investigator with no clinical involvement in the trial. R. Talaee was responsible for enrolment of the patients." |
| Allocation concealment (selection bias) | Low risk | Quote: "The method for randomisation concealment was to use sequentially numbered, opaque, sealed envelopes (SNOSE). The envelopes were kept in a safe box, which was only accessible to A. Khatami who was responsible for assigning the patients to the interventions." |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "An assessor who was blinded to the type of treatment visited the patients at weekly intervals during the treatment period and 1‐ month and 5 months after the last treatment session" |
| Incomplete outcome data (attrition bias) | Low risk | An intent‐to‐treat analysis was performed at 2 time points (end of the treatment period (day 42) and one month later (day 72)). The numbers of and the reasons for withdrawals were not significantly different between the 3 groups: 11% ILMA group; 19% ILMA + non‐silver and 6.45% ILMA + silver |
| Selective reporting (reporting bias) | Low risk | Comment: all relevant outcomes were reported |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: India Study period: 5 months Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: participants with a confirmed diagnosis of L tropica. The diagnosis was confirmed by demonstrations of L tropica bodies (amastigote stage of L tropica under oil immersion). Exclusion criteria: no mention about inclusion or exclusion criteria N randomised: 50. Rifampicin 1200 mg/d orally: 25; placebo: 25 Withdrawals: 4. Rifampicin 1: 2 (lost to follow‐up); placebo: 2 (withdrew due to exacerbation of lesions) N assessed: 46. Rifampicin: 23; placebo: 23 Mean (SD) age: rifampicin 29.54 years (17.34); placebo: 26.96 years (10.96) Sex (male/female): rifampicin: 10/13; placebo: 9/14 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 2 divided doses for 4 weeks Duration of follow‐up: 4 weeks Co‐interventions: the 2 withdrew due to exacerbation of lesions in placebo group and were treated by another therapeutic regimen | |
| Outcomes | Healing rates: percentage of participants 'cured' at the end of treatment: a cure was defined as complete healing and disappearance of the lesion or reversible hypopigmentation at the site of lesion. Incomplete or partial healing was defined as a reduction in the size of a lesion and the absence of parasites on smear. A treatment failure or non‐healing was defined as the absence of any change in the lesion and persistence of parasites on smear Adverse effects Tertiary outcomes: microbiological or histopathological cure of skin lesions Time points reported: at the end of the treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomized" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Comment: "Randomized" but no further information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: "Double‐blinded" but no further information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: "Double‐blinded" but no further information provided |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data balanced in numbers across intervention groups |
| Selective reporting (reporting bias) | Low risk | Comment: all relevant outcomes were reported |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: hospital, Bikaner, India Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: participants with a confirmed diagnosis of anthroponotic CL. Exclusion criteria: — N randomised: 50. Intervention group: 25, placebo group: 25 Withdrawals: 6 lost to follow‐up. Intervention group: 2, placebo group: 4 N assessed: 44. Intervention group: 23, placebo group: 21 Age: intervention group: n = 12, 16‐20 years; n = 5, 21‐30 years; n = 3, 31‐40 years; n = 2, 41‐50 years; n = 2, 51‐60 years; n = 0, 61‐70 years. Placebo group: n = 10, 16‐20 years; n = 4, 21‐30 years; n = 5, 31‐40 years; n = 3, 41‐50 years; n = 2, 51‐60 years; n = 1, 61‐70 years Sex (male/female): 34/16. Intervention group: 17/8; placebo group: 17/8 Male predominance was probably due to the habit of sleeping in open spaces outside the house without mosquito nets and improper clothing during night when the sandflies are active. Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks Duration of follow‐up: 6 weeks | |
| Outcomes | Healing rates: percentage of participants 'cured' at the end of treatment: complete healing; partial response; no response Time points reported: at the end of treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomized" Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Comment: "Randomized" but no further information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: "Double‐blinded" but no further information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: "Double‐blinded" but no further information provided |
| Incomplete outcome data (attrition bias) | Low risk | Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across group |
| Selective reporting (reporting bias) | High risk | Comment: no adverse effects information reported |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Saudi Arabia Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania:L major Inclusion criteria: only participants in whom parasites (amastigotes) were demonstrated were enrolled Exclusion criteria: pregnancy, chronic illness, immunocompromised or hyper allergic reaction to the trial drugs, treatment with regular medications such as antituberculous agents and steroids, which might have affected specific therapy, treatment with anti‐leishmanial drugs within the previous months, the presence of scars of previously treated lesions N randomised: 58. 2% miconazole cream: 27; 1% clotrimazole cream: 31 Withdrawals: 4: 2% miconazole cream: 4 (lost to follow‐up); 1% clotrimazole cream: 0 N participants assessed (lesions): 54 (151). 2% miconazole cream:n23 (62); 1% clotrimazole cream: 31 (89) Mean (SD) age: 2% miconazole cream: 19.5 years (15.4); 1% clotrimazole cream: 21.5 years (12.8) Sex (male/female): 42/12. 2% miconazole cream: 17/6; 1% clotrimazole cream: 25/6 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: twice daily for 30 consecutive days Duration of follow‐up: 30 days | |
| Outcomes | Healing rates: percentage of lesions 'cured' at the end of treatment. Response to treatment was based on results of repeated parasitologic evaluation and/or clinical changes using the same parameters as in the follow‐up. On this basis, response to treatment was graded into 4 categories:
Adverse effects Time points reported: at the end of treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was carried out by using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Patients admitted into the trial were given unlabeled tubes containing either 1% clotrimazole cream or 2% miconazole" Comment: we think that the outcome is unlikely to be influenced |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Of 27 participants treated with 2% miconazole, 4 defaulted and were lost to follow‐up; they were excluded from analysis" (4/27 = 14.28%) |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but he published reports probably include all expected outcomes. |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised, prospective Setting/location: dermatology department of Qaem University Hospital, Mashhad, Iran Study period: from October 2004 through November 2005 (13 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: not reported (although they reported that CLL is endemic and L tropica and, less commonly, L major are the most prevalent species) Inclusion criteria: aged > 2 years with CL of < 6‐months' duration; no treatment of the current infection during the last 3 months; and no history of a renal or liver disease Exclusion criteria: pregnant women; history of intolerance or allergy to Glucantime or macrolides; simultaneous use of antacids containing Al and Mg, theophyline, phenytoin, barbiturates, carbamazepine, and cyclosporin N randomised: 49: azithromycin: 22 (35 lesions), IMMA: 27 (58 lesions). Withdrawals: 2 (azithromycin group) N assessed: 47 participants; 20 (29 lesions) in the azithomicin group and 27 (58 lesions) in the IMMA group. Mean (SD) age: range 4‐70 years; azithromycin: 21.77 years (17.13) and IMMA: 22.78 years (13.17) Sex (male/female): 24/25; azithromycin: 8/14; IMMA: 16/11 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: up to 4 months (azithromicin) and 20 days (IMMA) Co‐interventions: participants showing no favourable response after 4 months of azithromycin therapy would receive IMMA at the same dose as the other group, at the end of the study. | |
| Outcomes | Clinical cure: clinical response was determined on the basis of the lesions' size, border, induration, and infiltration of papulonodular lesions; ulcerative lesions were evaluated on the basis of the ulcer depth, diameter, crusting, and the extent of re‐epithelialisation
Recurrence Adverse effects Time points reported: participants in the azithromycin group were evaluated monthly up to a maximum of 4 months, but participants in the IMMA group were evaluated both at the end of the treatment period (day 20) and 45 days later. Recurrence was reported after the 16‐week follow‐up period. | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The 49 patients who met our inclusion criteria were randomly divided into two groups." Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | 48 of 50 participants randomised completed the study. 2/20 participants of the azithromycin group withdrew because of adverse effects. Applications of study drugs were conducted according to the protocol |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Dermatology Clinic of Qaem Hospital in Mashad, Iran Study period: 10 months Sample size calculation: to detect a 22% difference in the cure rate between cryotherapy and ILMA groups and assuming a 57% cure rate in the cryotherapy group, with a 65% power and a 10% 2‐sided type I error, 40 persons were needed in each group. The 79 participants who met our criteria were randomly divided into 2 groups: 40 participants received cryotherapy and 39 participants received ILMA | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: positive direct skin smears for CL, were ≤ 13 years of age, had visited the dermatology clinic from September 2006 through June 2007, and had lesions with a duration of < 12 weeks to exclude any natural self‐healing during follow‐up Exclusion criteria: > 13 years of age, had a lesion history > 3 months, allergic to antimonial drugs, simultaneously using any other therapeutic method N randomised: 79. Cryotherapy: 40, ILMA: 39 Withdrawals: 7: cryotherapy group: 4, ILMA: 3 N assessed: 72 (91.14%): cryotherapy group: 36 (90%), ILMA: 36 (92.31%) Mean (SD) age: 6.8 years (3.4) in cryotherapy group and 6.2 years (3.4) in ILMA group Sex (male/female): cryotherapy: 18/22; ILMA: 20/19 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks | |
| Outcomes | Clinical cure: complete cure was defined as full re‐epithelialisation; disappearance of oedema, induration, and other signs of inflammation; and a negative direct skin smear result. Score:
Time to healing Adverse effects Time points reported: at the end of treatment and 6 months (clinical cure); at 4, 5 and 6 weeks (time to healing); at the end of treatment, after 6 weeks (adverse effects) | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Unclear risk | Open trial; lesions of all participants were photographed. |
| Incomplete outcome data (attrition bias) | Low risk | 4 participants in the cryotherapy group and 3 participants in the ILMA group were excluded because they received 2 medications simultaneously, did not complete the treatment course, did not visit the clinic for follow‐up 6 months later, or changed their address and were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Protocol not available; not registered; however, pre‐specified outcomes of the review were reported |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Dermatology Clinic of Ghaem Hospital, Mashhad, Iran Study period: March 2008 to September 2010 (30 months) Sample size calculation: to detect a 35% difference in the cure rate between the 2 groups of liposomal AmB and ILMA, assuming a 90% cure rate in liposomal AmB group with a 95% power and a 5% 2‐sided type I error, 36 subjects were required in each group. Also regarding a loss to follow‐up of 20%, this number was raised to 50 participants for each group | |
| Participants | Type of Leishmania: L tropica, L major Inclusion criteria: cutaneous leishmaniasis approved by either a direct smear stained with Giemsa or a positive skin biopsy of lesions with less than 6‐month duration, in cases with a previous history of anti‐leishmaniasis therapy, a 3‐month treatment‐free interval from the last treatment course Exclusion criteria: pregnancy, breastfeeding, taking any other specific treatment while participating in the study, past medical history of any local or systemic disease during the last 2 months, a significant underlying disease such as cardiac, renal, or liver dysfunction N randomised: 110. Group 1: 50; group 2: 60 Withdrawals: 34 did not adhere. Group 1: 11; group 2: 23 N assessed: group 1: 39 (78%); group 2: 37 (61.7%) Mean (SD) age: group 1: 20.54 years (18.72); group 2: 25.30 years (15.70) Sex (male/female): group 1: 23/27; group 2: 21/39 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 8 weeks | |
| Outcomes | Clinical response: determined on the basis of the lesion induration size of and the extent of re‐epithelialisation in ulcerative ones. Scales: clinical response:
Adverse effects Time points reported: at the end of treatment, and 6 months after termination. Adverse effects were reported at the end of treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The 110 patients who met our inclusion criteria were randomly divided into two groups." Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Unclear risk | ITT analyses performed Losses to follow‐up per group: Intervention group: 11/50 (22%) Control group: 23/60 (38.3%) |
| Selective reporting (reporting bias) | Unclear risk | Number of lesions higher in the liposomal ampB group (P < 0.05) whereas number of papule and plaque lesions where higher in the ILMA group (P = 0.011) Outcomes described in the methods were reported in the results section. However, only one time point was reported Protocol not available; not registered in a clinical trial registry |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: school children, Sudan Study period: 80 days Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania spp not specified but L major was presumed to be the causative parasite. Inclusion criteria: all positive smears Exclusion criteria: children who had received diminazene aceturate or previous treatment in hospital N randomised: 70. 35 in each group Withdrawals: 8. Berelin: 3; Savlon: 5. 2 children in Berelin group were not enrolled because they received diminazene aceturate before. 2 in Savlon group were excluded because they were treated for CL in the hospital N assessed: 62. Berelin: 32; Savlon: 30 Mean (SD) age: Berelin: 9.3 years (4.6); Savlon: 10.4 years (2.8) Sex (male/female): Berelin: 18/15; Savlon: 20/13 Baseline imbalances: comparability with regard to sex, age, number, size, duration and location of ulcer, and previous treatment taken
| |
| Interventions | Type of interventions:
Duration of treatment: 50 days Duration of follow‐up: one month | |
| Outcomes | Primary outcome: percentage of participants 'cured' at the end of treatment. Cure was defined when the skin lesion was completely closed and covered with scar tissue, without the possibility to evoke secretions on pressure and if this apparent cure was sustained for at least 2 weeks Secondary outcomes: duration of remission and percentage of people with treated lesions that recur 20 to 35 days after cure Adverse effects Time points reported: at the end of treatment and at the end of follow‐up. | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Unclear risk | A double‐blind study design was attempted, but could not be sustained as Savlon is a well‐known product and soapy on application |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Low rates of dropouts (8/70, < 2.5%) |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it is probably that the published reports include all expected outcomes |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Imam Reza Hospital in Mashhad, Iran Study period: March to September 2004 (7 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: confirmation of cutaneous leishmaniasis based on direct smear, ≤ 3 lesions, duration of the disease < 12 weeks, aged 7‐60 years, completion of informed consent form by participant or parents of minor participants, dry cutaneous leishmaniasis Exclusion criteria: pregnant or breastfeeding women; children < 7 years, lesions on ear, nose, joints, and near the eye; > 3 lesions; application of any kind of treatment for cutaneous leishmaniasis, duration of the disease longer than 12 weeks (to omit spontaneous healing cases during the follow‐up period), recurrent infection, wet cutaneous leishmaniasis N randomised: 45 participants Withdrawals: 11 N assessed: 34 participants (24, group 1; 10, group 2) Age: not described Sex: not described Baseline data: mean size of lesions (SD): group 1, 1.27 cm (0.81); group 2, 0.98 cm (0.61) | |
| Interventions | Type of interventions:
Duration of intervention: group 1, 2 weeks; group 2, 6 weeks | |
| Outcomes | Clinical response
Time points reported: 8 weeks | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "This N randomised controlled trial was performed from March to September 2004 on patients with cutaneous leishmaniasis admitted to Imam Reza Hospital in Mashhad" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | High risk | 45 participants were randomised into 2 groups. 11 were lost to follow‐up (24%). No ITT analyses were performed High imbalance between groups |
| Selective reporting (reporting bias) | High risk | No baseline data. Side effects not clearly reported (no statistical analyses performed either) |
| Other bias | High risk | Sample size calculation, reporting of Leishmania spp involved and baseline comparability was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Ahvaz city, southern Iran Study period: 12 months (2002) Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: clinically and parasitologically positive (Leishman bodies in Giemsa‐stained direct smear of the lesion scrapings), duration of lesions < 3 months, aged 15‐40 years, no evidence of secondary bacterial infections, no mucosal involvement, no history of previous treatment of cutaneous leishmaniasis, or of allergic reactions to MA or metronidazole Exclusion criteria: history of underlying disease (such as cardiac, renal, or pulmonary); pregnant or breastfeeding; cutaneous leishmaniasis localised on or near the joints N randomised: 36. Group 1: 18, group 2: 18 Withdrawals: 8. Group 1: 2, group 2: 6 N assessed: 28 (77.78%). Group 1: 16, group 2: 12 Age: mean 28.8 years (range 15‐40) Sex (male/female): 21/15 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 8 weeks | |
| Outcomes |
Time points reported: clinical cure: after 8 injections. Adverse effects: after the treatment. | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The method of randomisation was selecting a card among 36 cards with odd or even numbers |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | High risk | 28/36 participants completed the study (77.8%) |
| Selective reporting (reporting bias) | High risk | No protocol available. Adverse effects not reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: skin department of PNS Shifa, a naval hospital in Karachi. Endemic areas of Balochistan province, Pakistan Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania spp not mentioned Inclusion criteria: never received any treatment for their skin disease Exclusion criteria: very young and very old people, those who had received some treatment for the disease, people suffering from diffuse CL or leishmaniasis recidivans, people with some known cardiac, renal or hepatic disease N randomised: 40. 20 in each group Withdrawals: 0 Participants assessed: 40 (100%). 20 in each group Age: range 20‐40 Sex: 100% male Baseline data. Nodular, ulcerative and crusted forms were the most common morphological patterns seen. Most lesions were on hands and feet.
| |
| Interventions | Type of interventions:
Duration of intervention: 15 days Duration of follow‐up: 3 months | |
| Outcomes | Healing rates: percentage of participants 'cured' at the end of treatment Adverse effects Time points reported: at the end of treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it is probably that the published reports include all expected outcomes |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Golestan province, in northeastern Iran Study period: 20 November 2005 to 20 July 2006 (8 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: L major Inclusion criteria: observation of Leishman bodies (amastigotes) in dermal lesions, no previous use of anti‐leishmanial drugs, no previously confirmed leishmaniasis (by scar or clinically compatible history), no pregnant or lactating women, no acute or chronic medical condition and no history of allergy, female participants of childbearing age were included after giving consent for effective contraception during therapy and until 3 months thereafter Exclusion criteria: not explicitly reported, but can be inferred from the above inclusion criteria N randomised: 63. Group 1: 32; group 2: 31 Withdrawals: 5. Group 1: 4 (lost after first week because lack of gastrointestinal tolerance); group 2: 1 (lost to follow‐up after 3 months) N assessed: 63 (100%). Group 1: 28; group 2: 30 Mean age: group 1: 20.2 years; group 2: 16.8 years Sex (male/female): 35/28. Group 1: 19/13; group 2: 16/15 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: miltefosine: 28 days. IMMA: 14 days Duration of follow‐up: 6 months | |
| Outcomes | Healing rates: percentage of participants 'cured' 3 months after treatment Secondary outcomes: duration of remission and percentage of people with treated lesions that recur within 6 months Adverse effects Time points reported: 2 weeks, 3 months, 6 months | |
| Notes | Study funding sources: this study was financially supported by Medical Sciences/University of Tehran, Iran (from grant for full professor) Possible conflicts of interest: not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "For randomisation of patients into two groups, we used balanced block method" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "This study was an open‐label, N randomised comparison of miltefosine to meglumine antimonate in 63 patients" |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | Imbalance in numbers and reasons for missing data across intervention groups (4/32 = 12.5% miltefosine group; 1/31=3.22% IMMA group) Comment: the results for the dropouts were not excluded from the statistical analysis. We think missing outcome data likely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it is probably that the published reports include all expected outcomes |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Iran Study period: not described Sample size calculation: assuming a 30% spontaneous cure rate with placebo and the minimum usefulness of a 60% cure rate with itraconazole, and a 10% dropout rate, the sample size was calculated as 70 individuals in each group | |
| Participants | Type of Leishmania: L major Inclusion criteria: age > 12 years, diagnosis of CL confirmed by laboratory test results, no previous treatment for leishmaniasis, no serious concomitant medical problems Exclusion criteria: age < 12 years, pregnant and nursing women, patients who had lesions on the face, lesions lasting > 4 months N randomised: 140. Itraconazole: 70; placebo: 70 Withdrawals: itraconazole: 5 N assessed (lesions): 131. Itraconazole: 65 (219); placebo: 66 (262) Age: mean 26.3 years (range 12‐46) Sex (male/female): 90/41. Itraconazole: 44/21; placebo: 46/20 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 3 weeks Duration of follow‐up: 51 days | |
| Outcomes | Healing rates: percentage of participants 'cured' 51 days after treatment Adverse effects Time points reported: at the end of treatment (day 21); on day 51 (1 month after the end of treatment) | |
| Notes | Study funding sources: this work was supported by the World Health Organization Special Program for Research and Training in Tropical Diseases and the research programme of Isfahan University of the Medical Sciences. Possible conflicts of interest: not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Carried out by the WHO Special Programme for Research and Training in Tropical Diseases group in Geneva, Switzerland" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgment |
| Blinding of participants and personnel (performance bias) | Low risk | Identical capsules containing 100 mg of itraconazole or placebo were used in the study. The 2 treatment groups received either itraconazole as coded capsules for 21 days or placebo as coded capsules with the same dosages. Review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | Low risk | Reasons for missing outcome data unlikely to be related to true outcome |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. The study published reports our primary outcomes: 'cured' and adverse effects |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Skin Research Centre in Isfahan city. Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L major Inclusion criteria: age > 5 years, diagnosis of CL confirmed by laboratory test results, no previous treatment for leishmaniasis, no serious concomitant medical problems, signed written informed consent Exclusion criteria: pregnant and nursing women, age < 5 years, lesions lasting for > 4 months N randomised: 72. Group 1: 36; group 2: 36 Withdrawals: 6, lost to follow‐up. Group 1: 5; group 2: 1 N participants assessed (lesions): 66 (196). Group 1: 31 (91); group 2: 35 (105) Mean age (male/female): 21.9 years/17.6 years (range 5‐48 years). Group 1: 23.6 years/17.4 years; group 2: 20.2 years /18.1 years Sex (male/female): 50 (75.7%)/16 (24.3%). Group 1: 26/5; group 2: 24/11 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 20 days Duration of follow‐up: 51 days (1 month after the end of treatment) | |
| Outcomes | Healing rates: percentage of participants 'cured' 51 days after treatment. On day 21 (end of therapy), the clinical response to treatment was coded subjectively as: apparent cure, partial response, and failure. After 1 month of follow‐up (day 51), the participants were described as showing definitive cure if all the lesions had healed and direct smears of the lesions were negative Adverse effects Tertiary outcomes: microbiological or histopathological cure of skin lesions Time points reported: day 21, and 1 month after the end of treatment: day 51 | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Seventy‐two patients were assigned randomly to two groups." Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | Imbalance in numbers across intervention groups: 5/36 (13.89%), AL + IMMA group; 1/36 (2.78%), IMMAgroup. We think missing outcome data likely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: endemic areas in the north of Isfahan city, Iran Study period: not described Sample size calculation: sample size calculation was based on 90% significance and 90% power to detect a difference between vehicle and ketoconazole. Assuming a 15% spontaneous cure with placebo, a minimum usefulness of a 60% cure with ketoconazole cream and about a 10% dropout, the sample size was calculated as 45 individuals in each group. | |
| Participants | Type of Leishmania: Leishmania spp: L major and L tropica Inclusion criteria: age > 5 years, laboratory‐confirmed diagnosis of CL, no previous treatment for leishmaniasis, no serious concomitant medical problems Exclusion criteria: pregnant and nursing women, lesions on the face, lesions of > 4 months duration N randomised: 90 Withdrawals: 17 N assessed: 73 Age: mean 19.9 years (range 6‐60) Sex (male/female): 45/28 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: twice daily for 21 days. | |
| Outcomes | Healing rates: clinical response to treatment was coded subjectively as: apparent cure, partial response or failure. Definitive cure was defined if at day 51, the lesions were healed and direct smears of the lesions were negative. Adverse effects Time points reported: the clinical response of the lesions was reported on days 21 (end of therapy) and 51 | |
| Notes | Study funding sources: supported by a research programme of Isfahan University of Medical Sciences Possible conflicts of interest: not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study was designed as a double‐blind, N randomised, placebo‐controlled trial" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Placebo and ketoconazole creams were identical cream containing either 25 ketoconazole 2% or placebo were used in the study. The two treatment groups received either the ketoconazole cream or placebo twice daily for 21 days as coded tubes with the same dosage" |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: skin and CL clinic in Gaz in Isfahan, Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: size of ulcer less than 5 cm in diameter, ≤ 5 lesions, duration of disease < 3 months Exclusion criteria: patients who had lesions on the face near the eyes or on the nose or ears, pregnancy, lactation, lupoid or sporotrichoid lesions, use of immunosuppressor drugs in the past 6 months and severe adverse effects, exacerbation of the disease N randomised: 40 participants (19 in prepared gel group and 21 vehicle gel mask) Withdrawals: 1 participant in prepared gel group N assessed: 39. 21 (100%) in vehicle gel group, and 18 in prepared gel group Mean age: 28.2 years Sex (male/female): 25/15 Baseline data: not described | |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks Co‐interventions: all of the participants received the standard treatment including ILMA weekly and cryotherapy every 2 weeks for a maximum of 6 weeks | |
| Outcomes | Treatment outcome, defined as:
Time points reported: 2 months after the end of treatment for relapse | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly divided into two groups" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Unclear risk | Open trials. Photography was done from all the lesions both at the first visit and all the follow‐up visits |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | High risk | Protocol not available; not registered; in clinical trial registry; adverse effects not reported |
| Other bias | High risk | Sample size calculation, reporting of Leishmania spp involved and baseline comparability was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Pakistan Study period: around 4‐5 months Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania spp not mentioned Inclusion criteria: clinical diagnosis of CL and positive Giemsa‐stained smear of parasite Exclusion criteria: > 5 lesions and pregnant women N participants randomised (lesions): 104 (215). Group 1: n = 49 (111); group 2: n = 55 (104) Withdrawals: 8 N assessed: 96. group 1: n = 49; group 2, n = 47 Age:
Sex (male/female): 58/38 Baseline imbalances: comparability regarding age, sex, number, and site of lesions and duration of the disease
| |
| Interventions | Type of interventions:
Duration of intervention: until complete cure or up to 8 weeks | |
| Outcomes | Healing: complete cure (100%); partial (> 50%; < 50%); failure (nil) Speed of healing (time taken to be 'cured') Duration of remission and percentage of people with treated lesions that recur within 6 months and 1, 2, and3 years:time assessment not specified Prevention of scarring Adverse effects Time points reported: at 2, 4, 6 and 8 weeks of treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly divided into two treatment groups" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Patients in group A were treated with weekly and those in group B with fortnightly intralesional injections" Comment: we think the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Dropouts: 8/104: 7.6% lost to follow‐up Comment: the results for the defaulters were excluded from the statistical analysis. We think missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes. |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Iran Study period: October 2000 to February 2001 (5 months) Sample size calculation: to detect a clinically relevant difference of at least 25% between placebo (35% estimated response rate) and itraconazole (60% estimated response rate) in the primary outcome parameter with a power of 90% and a 2‐sided type I error of 5%, a total of 164 subjects (82 in each group) were required. To compensate for dropouts, 20% more participants were enrolled in each group (in total 200 participants). | |
| Participants | Type of Leishmania: L major Inclusion criteria: aged 12‐60 years; presence of parasitologically confirmed lesion(s) of CL; healthiness on the basis of physical examination, medical history, and the results of blood biochemistry and haematology, carried out < 2 weeks before the start of the trial Exclusion criteria: women of child‐bearing age without adequate effective contraception, pregnant or breastfeeding, duration of lesions > 45 days, presence of lesions on the face or near the mucous membranes, > 5 lesions, any lesion with a diameter > 3 cm, history of any systemic antileishmanial therapy, known hypersensitivity/allergy to itraconazole, receiving any drug with known interaction with itraconazole N randomised: 200 Withdrawals: 42 in total. 17 in the Itraconozale group and 25 in the placebo group N assessed: 158 Age: not described Baseline imbalances: comparable with regard to age, sex, and duration of the lesions
| |
| Interventions | Type of interventions:
Duration of intervention: 8 weeks | |
| Outcomes | Healing rates: for clinical assessment a 5‐point scoring system was employed: cure (complete re‐epithelialisation of all of the lesions), moderate improvement (more than 50% reduction in the size of the lesions), mild improvement (less than 50% reduction in the size of the lesions), no change, and worsening Adverse effects: at each visit, all of the participants were asked about any adverse effects. Time points reported: after completion of treatment (8 weeks), and at the end of the 3 months follow‐up (healing rates) | |
| Notes | Study funding sources: supported by a grant from Janssen‐Cilag Pharmaceuticals Inc. Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation sequence was generated from a random number table" |
| Allocation concealment (selection bias) | Low risk | Quote: "Concealed from the investigator until the data entry was completed and the data bank was locked" |
| Blinding of participants and personnel (performance bias) | Low risk | "Patients were randomly allocated to receive either itraconazole in the form of two 100‐mg capsules or identical placebo capsules once daily for 8 weeks." Comment: we think the outcome is unlikely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | Imbalance in numbers and reasons for missing data across intervention groups (17% itraconozale group; 25% placebo group). Comment: the results for the defaulters were not excluded from the statistical analysis. We think missing outcome data likely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes. |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: not mentioned Inclusion criteria: CL confirmed with direct smear, aged 1‐20 years, maximum number of lesions 3, maximum size of lesion 5 cm, duration of disease less than 8 weeks Exclusion criteria: history of allergy to MA, pregnancy or lactating N randomised: 210 Withdrawals: 53: 29/105 in group 1 and 24/105 in group 2 N assessed: 157. Group 1: 76, group 2: 81 Age: not described Baseline data: not described | |
| Interventions | Type of interventions:
Duration of intervention: 6 weeks | |
| Outcomes | Healing rates: percentage of participants 'cured' 2 weeks after treatment Adverse effects Time points reported: not described | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | High rates of dropouts: 53/210 (25.2%) |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes |
| Other bias | High risk | Sample size calculation, reporting of Leishmania spp involved and baseline comparability were not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Skin Disease and Leishmaniasis Research Center (SDLRC), Isfahan, Iran Study period: around 5 months Sample size calculation: not described | |
| Participants | Type of Leishmania: not mentioned Inclusion criteria: CL confirmed with direct smear Exclusion criteria: pregnant or nursing mothers, treated previously for CL, any known intercurrent illness or a history of allergy to MA, palpebral lesions, having > 5 lesions, lesion > 3 cm, duration of lesions was > 12 weeks N randomised: 80: 40 in each group Withdrawals: 7 N assessed: 73: 38 in group 1 and 35 in group 2 Age: range 5‐75 years Baseline data: the most common clinical type of the lesions in both groups was papule (50% in TCA and 44% in the ILMA group) and nodule (25% in TCA and 24% in the ILMA group). Mean number of lesions: TCA: 1.2; ILMA: 1.4 | |
| Interventions | Type of interventions:
Duration of intervention: up to 6 weeks | |
| Outcomes | Healing: complete cure was defined as complete healing and re‐epithelialisation of the lesion(s); partial care as partial clinical improvement with reduction in erythema, induration and size of the lesions; treatment failure as the absence of any change or worsening of the lesion(s) Duration of remission and percentage of people with treated lesions that recur after 3 months of follow‐up Adverse effects Microbiological or histopathological cure of skin lesions Time points reported: after the last treatment session, 1 and 3 months post‐treatment. Complete cure was reported at 4 and 6 weeks of the treatment period. Recurrence was assessed at 3 months follow‐up | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random digit table |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Unblindness is a limitation of this study" |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | Quote: "For 80 patients, which participated in the study, 73 cases completed the study" Comment: the results for the dropouts were excluded from the statistical analysis. We think missing outcome data likely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes. |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Skin Disease and Leishmaniasis Research Center (SDLRC), Isfahan, Iran Study period: 4 months Sample size calculation: not described | |
| Participants | Type of Leishmania: not mentioned Inclusion criteria: CL confirmed with direct smear, no history of systemic or topical therapy for CL, absence of the malnutrition or severe predisposing disease such as cardiac, renal or hepatic disease and other contraindication for MA Exclusion criteria: pregnant or lactating mothers, lesions > 3 months old and treated with the drugs that had interaction with MA N randomised: 100, 50 in each group Withdrawals: 23 (13 in the honey group and 10 in the ILMA group). However, in the abstract authors stated that 10 participants left the study. N assessed: 90 (45 in each group) Age: range 7‐70 years Baseline data: the most common clinical type of the lesions in both groups was plaque (60% in honey + ILMA and 55.6% in the ILMA‐alone group). Mean number of lesions: honey + ILMA: 1.3; ILMA: 1.7 | |
| Interventions | Type of interventions:
Duration of intervention: once weekly until complete healing of the ulcer or for maximum of 6 weeks | |
| Outcomes | Healing: complete healing was defined as disappearance of the induration and complete re‐epithelialisation of the ulcer. Complete healing of the lesions was defined as complete clinical and parasitological healing (negative direct smear); partial healing of the lesions was defined as the decrease of the size and indurations of the lesions; non‐responsive was defined as no clinical change or progression of the lesions Speed of healing (time taken to be 'cured'): expressed as mean healing time Adverse effects Time points reported: assessed weekly for 6 consecutive weeks and at the end of the 2nd, 3rd, and 4th month. Cure was assessed at the end of treatment and follow‐up | |
| Notes | Study funding sources: not reported Possible conflicts of interest: no competing interests | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random allocation software (ver 1.0, May 2004; Saghaei)" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | We think the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Balance in numbers and reasons for missing data across intervention groups (13/45 (28.8%) in honey + ILMA group; 10/45 (22.2%) in ILMA‐alone group) Comment: the results for the defaulters were excluded from the Kaplan‐Meyer analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: relevant outcomes were reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Skin Diseases and Leishmaniasis Research Center. Isfahan, Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica and L major Inclusion criteria: all the participants had positive smear for Leishmania body and had not received any topical or systemic therapy for leishmaniasis, aged 7‐70 years, lesion not more than 3 months Exclusion criteria: pregnant or lactating; history of cardiac, renal, hepatic diseases; any contraindication for the treatment N randomised: 150. Group 1: 50; group 2: 50; group 3: 50 Withdrawals: 26. Group 1: 7; group 2: 14; group 3: 5 N assessed: 124 (82.66%). Group 1: 43 (86%); group 2: 36 (72%); group 3: 45 (90%) Mean (SD) age: group 1: 33.1 years (17.5); group 2: 27.8 years (9.8); group 3: 29.1 years (14.7) Sex (male/female): 88 (70.97%)/36 (29.03%)
Baseline data:
| |
| Interventions | Type of interventions:
The oral placebo was identical in appearance to omeprazole capsules and was administered in the similar way Duration of intervention: 3 weeks | |
| Outcomes | Clinical cure: rate of complete response, 3 months (12 weeks) after starting treatment. Scale: complete healing of the lesions was regarded as complete clinical and parasitological healing (negative direct smear). Partial healing of the lesions was regarded as decrease of the size and indurations of the lesions, and no response was regarded as no clinical change or progression of the lesions. Time to healing: proportion of complete improvement in the 3 groups during the course of treatment Adverse effects: at the end of treatment Time points reported: clinical cure: 12 weeks. Time to healing: 2, 4, 6, 8, 12 weeks. Adverse effects: at the end of treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: they declared no competing interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were selected and randomised by random allocation software into 3 groups. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgment |
| Blinding of participants and personnel (performance bias) | Low risk | The oral placebo was completely similar to omeprazole capsules and was administered in the similar way; low dose of IMMA was prepared by addition of normal saline to IMMA Both the investigating physicians and the participants were blinded to the type of treatment and drug codes were revealed only at the end of the study. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | High risk | Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes. |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Isfahan University of Medical Science, Isfahan, Iran Study period: March 2008 to March 2009 (12 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: unclear Exclusion criteria: pregnant, children < 5 years, palpebral lesions (less than 20 mm from palpebral margin), > 5 lesions, > 12 weeks duration of leishmaniasis, history of any specific anti‐leishmaniasis therapy, significant underlying diseases N randomised: 80 lesions Withdrawals: 4 lesions N assessed: 76 lesions (38 lesions in each group) and 60 patients (30 patients in each group) Mean (SD) age: 5.11 years (13.3) (range 5‐50) Sex: unclear Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: non‐ablative radiofrequency + topical TCA 50%: 4 weeks; ILMA: 8 weeks | |
| Outcomes | Treatment responses:
Time points reported: 6 months of treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "This computer‐based randomised controlled trial was conducted from March 2008 to March 2009" |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The examinations and measurements were performed by the investigators who were blinded to the type of treatment." |
| Incomplete outcome data (attrition bias) | Unclear risk | Originally 80 lesions were studied and randomly assigned to the 2 groups. However, due to missing data, only 76 were finally included in the analysis. No ITT analysis |
| Selective reporting (reporting bias) | High risk | Complete cure was described in Methods and Results, but partial cure and treatment failure was not reported in the Results section. No adverse effects reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Cutaneous Leishmaniasis and Skin Diseases Research Center, Isfahan, Iran Study period: 2010 to 2011 (12 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: age older than 5 years, diameter less than 3 cm, the duration of disease less than 12 weeks, lesions with less than 2 cm distance from eyelid, < 5 lesions Exclusion criteria: pregnancy; lactation; colloid scar; lesions on cartilage, eyelids or joints; history of using other drugs against CL, treatment with immune system inhibitors N randomised: 90 (30 people in each group) Withdrawals: not described N assessed: 90 (30 people in each group) Mean (SD) age: 24.5years (14) Sex (male/female):21/9, 23/7 and 21/9 Baseline data: Number of lesions:single lesion in 53 (58.9%), 2 lesions in 29 (32.2%) and 3 lesions in 8 patients (8.9%). The type of lesion: plaque in 32 patients (35.6%), nodule in 44 (48.4%), plaque and nodule in 8 (8.9%), and papule in 6 patients (6.7%) Distribution of lesions: hand 43, foot 15, face 8, trunk 5, hand and trunk 4, hand and neck 4, neck 4, hand and foot 4, hand and face 2, ear 1 | |
| Interventions | Type of interventions:
All patients in three groups were followed weekly for 3 months and then after 4 and 6 months to assess improvement of lesions and size of scar. | |
| Outcomes | Clinical response, according to standard quartile grading:
The quantitative 4‐point scale used included:
Time points reported: 6 months | |
| Notes | Study funding sources: Isfahan University of Medical Sciences Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Impossible for blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Quote "Evaluation of patients were done by two physicians who were not aware of the treatment group. These two physicians did the evaluations separately. The reduction in this size of ulcer and the scar was compared with the same lesion" |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: prospective randomised controlled trial Setting/location: Central Research Center of Skin Diseases and Leishmaniasis and Novin Laser Center; Isfahan, Iran Study period: June 2010 to September 2011 (15 months) Sample size calculation: sample size was calculated as 60 cases in each group with further rate of 10% dropouts and exclusions | |
| Participants | Type of Leishmania: not described Inclusion criteria: leishmaniasis scar diagnosed clinically on participants by a dermatologist Exclusion criteria: pregnancy, lactation, colloid scar, treatment with immune system inhibitors, use of isotretinoin or fillers for the past 6 months, use of dermabrasion or skin resurfacing for the past 12 months, skin types of IV to V1 N randomised: 120 (60 people in case group and 60 in control group) Withdrawals: not described N assessed: not described Mean (SD) age: 27.21 years (11.52) (range 6‐45) Sex (male/female): 51%/49% Baseline imbalances: none Severity of illness: mean (SD) scar size: laser CO₂ group: 2.3 cm (0.3) and fractional CO₂ laser: 3.4 cm (0.4) | |
| Interventions | Type of interventions:
| |
| Outcomes | Clinical response, according to standard quartile grading:
The quantitative 4‐point scale used included:
Time points reported: 6 months | |
| Notes | Study funding sources: Isfahan University of Medical Sciences Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Low risk | Quotes: "A photo was taken from patients before and after treatment with a digital camera ... Evaluation of participants were done by 2 physicians who were not aware of the treatment group. These 2 physicians did the evaluations separately. The reduction in this size of ulcer and the scar was compared with the same lesion" |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Skin Disease and Leishmaniasis Research Center, Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: participants with positive direct smear for CL; 6‐60 years of age; without any previous history of systemic or topical therapy for CL; lesions < 3 cm, < 12 week duration, and not located within 2 cm distance of palpebral margin Exclusion criteria: pregnant and lactating women N randomised: 200 participants Withdrawals: not described N assessed: 187; group 1: 91; group 2: 96 Mean (SD) age: 10.7 years (22.04); group 1: 10 years (20.6); group 2: 11.3 years (23.3) Sex (male/female): 101/86 Baseline data: mean (SD) lesion area was 329 mm² (118.7) in group 1 and 359 mm² (55.6) in group 2 | |
| Interventions | Type of interventions:
Duration of intervention: complete resolution of the lesions or end of 8 weeks | |
| Outcomes | Clinical cure: complete re‐epithelialisation of the lesion and lack of induration. Clinical response was measured at the end of treatment and was defined as complete cure (negative direct smear and clinical healing), partial cure (partial clinical improvement with decreasing erythema, induration, and lesion size), non‐cure or treatment failure (no clinical change or worsening of the lesions) Time points reported: 8 weeks | |
| Notes | Study funding sources: the study is self‐funded Possible conflicts of interest: there is no conflict of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation software (version 1.0, May 2004, Saghaei) was used for randomisation |
| Allocation concealment (selection bias) | Low risk | Participants with confirmed cutaneous leishmaniasis referred to the Skin Diseases and Leishmaniasis Research Center were selected and randomised by random allocation software into 3 groups |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The measurements were done before treatment and at the end of eighth week by the investigators who were blinded to the type of treatment." Comment: Lesions were photographed before and after completion of the treatment course. Not clear how blinding was preserved |
| Incomplete outcome data (attrition bias) | Low risk | From a total of 200 randomised participants, 96 participants in ILMA group and 91 participants in the combination group completed the study Losses to follow‐up were below 25% and homogeneous between the groups |
| Selective reporting (reporting bias) | High risk | Protocol not available, not registered. Adverse effects not reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Anuradhapura Teaching Hospital, Anuradhapura, Sri Lanka Study period: 32 months. Participant selection: April 2006 to June 2007 (15 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: L donovani Inclusion criteria: participants with CL who attended to Anuradhapura Teaching Hospital, Anuradhapura, Sri Lanka from April 2006 to June 2007 Exclusion criteria: not described N randomised: a total of 154 participants with 229 lesions were included in the study. IL 7% HSCS: 67; ILSSG: 87 Withdrawals: (4.5%: 7/154). HSCS: 3, ILSSG: 4 N assessed: 147 (95.45%) CL participants with 222 lesions completed treatments. HSCS: 64 (95.52%); ILSSG: 83 (95.40%). Age: mean 32 years (range 16 months to 74 years) Sex (male/female): 99/55, M:F ratio of 1.8:1 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: HSCS: 1‐29 weeks, depending on the size and the duration of the lesions (mean 8.78 weeks). SSG: 1‐13 weeks, depending on the size and the duration of the lesions (mean 5.11 weeks) Participants were seen weekly for the first 3 injections; fortnightly for the fourth and fifth injections; then monthly until cure. | |
| Outcomes | Clinical cure: the percentage of lesions that were cured with SSG and HSCS Number of injections required per each lesion in total for cure (scales: 1‐10 injections) Adverse effects: systemic side effects with SSG or HSCS. Local side effects: pain during injection. Scarring after healing, postinflammatory hyperpigmentation Time points reported: at the end of treatment. Participants were followed‐up every 3 months after cure for 18 months to assess recurrences and evidence of visceralisation | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "double blind" Insufficient information to permit judgment |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double blind", "At each visit the patients were examined by the primary investigator who was blind to the therapy" Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | Low risk | 4.5% (7/154) did not complete the study |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available; not registered. Insufficient information to permit judgment SD not provided for duration of treatment and number of injections |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised double‐blind clinical trial Setting/location: Skin Clinic of Anuradhapura Teaching Hospital, Sri Lanka Study period: January 2012 to February 2013 (14 months) Sample size calculation: approximately 473 participants per group were required to enable the detection of a treatment difference of 5% with a lowest cure rate of one group of 90% | |
| Participants | Type of Leishmania: L donovani Inclusion criteria: the study recruited participants with suspected CL who consented to participation. Exclusion criteria: pregnant or lactating women, subjects with a history of cardiac, renal, or hepatic disease N participants randomised (lesions): 444 (643). 10% HSCS: 192 (297); 15% HSCS: 82 (101); ILSSG: 170 (245) Withdrawals (lesions): 17 (20) lost to follow‐up. 10% HSCS: 8 (7); 15% HSCS: 3 (3); ILSSG: 6 (10) N assessed (lesions): 427 (623); 10% HSCS: 79 (98); 15% HSCS: 184 (290); ILSSG: 164 (235) Age: mean 32.7 years (range 14 months to 88 years). Most (60.8%) were aged 16–45 years Sex (male/female): 286/158 Baseline data: the average delay in presentation was 8 months (range: 4 weeks to 5 years). 91% of lesions were located on exposed areas of the body. Most (69.8%) participants had a single lesion. | |
| Interventions | Type of interventions:
Duration of intervention: participants were seen weekly for the first 3 injections, fortnightly for the 4th and 5th injections, and then monthly until a cure was achieved. | |
| Outcomes | Clinical and parasitological cure: responses were graded as slight (10% improvement from the initial status of the lesion), mild (20%–30% improvement), moderate (50% improvement), marked (80%–90% improvement), or as total if the lesion had cleared and parasites were not detected in the affected area by smear or culture. Both marked improvements and total clearance were considered to represent a cure. Reported at the end of treatment. Duration of treatment: in weeks, mean (range) Time required to achieve the cure of the lesion: mean and median times taken for cure for the different treatments groups. Every 5 weeks until achieve 30 weeks. Injections per lesion, mean (range): number of injections for cure per lesion Relapse: L recidivans Adverse effects: local side effects: at the site of the lesion caused by the injections: pain during injections, postinflammatory hyperpigmentation, scarring, postinflammatory depigmentation, ulceration and necrosis, L recidivans. Systemic side effects: no systemic or significant local side effects with either SSG or 10% HSCS. Time points reported: participants were followed up every 3 months after cure for more than 6 months to assess recurrences and evidence of visceralisation | |
| Notes | Study funding sources: none reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The treatment options were documented separately and packed in opaque envelopes numbered consecutively according to the randomisation schedule at a ratio of 2: 2: 1 |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was concealed from the researcher who enrolled and assessed the participants by the use of sequentially numbered, opaque, sealed, and stapled envelopes that were impermeable even to intense light. |
| Blinding of participants and personnel (performance bias) | Low risk | The participants and the investigator (who assessed the participants for their clinical response) were blind to the type of therapy allocated. |
| Blinding of outcome assessment (detection bias) | Low risk | At each visit, the participant was examined by the primary investigator, who was blinded to the therapy. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers of withdrawals were similar and small in the 3 groups: 4.1% (8/192) in group 1, 3.6% (3/82) in group 2, and 3.5% (6/170) in group 3. |
| Selective reporting (reporting bias) | Low risk | The study published reports our primary outcome and adverse effects. |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Khair Khana Clinic; Kabul, Afghanistan Study period: 100 days Sample size calculation: to detect a 20% difference in the cure rate between the SSG and thermotherapy groups, assuming an 80% cure rate in the SSG groups, with a 90% power and a 5% 2‐sided type I error, 98 subjects were needed in each group. To compensate for anticipated loss to follow‐up, 40% more participants were enrolled in each group. | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: age > 5 years; the presence of a single, parasitologically confirmed CL lesion; no prior history of disease and/or antimonial treatment Exclusion criteria: the presence of a CL lesion located on or immediately adjacent to the nose, lips, or eyes; pregnancy; breastfeeding; major surgery in the previous 3 months; presence of any uncontrolled medical condition; anticipated unavailability for follow‐up N randomised: 431. Group 1: 148, group 2: 144, group 3: 139 Withdrawals: 172 in total: 30 decided to withdraw after allocation and 142 did not complete the 4 visits or the follow‐up N assessed: 259. Group 1: 93, group 2: 58, group 3: 108 Age: range 10‐20 years Sex (male/female): 200/201 Baseline data: the lesions were primarily located on the face (43.4% of participants), on the hands (38.2%), legs (15.9%) and arms (2.4%)
| |
| Interventions | Type of interventions:
Duration of intervention: not described | |
| Outcomes | Percentage of participants 'cured' at 100 days after treatment initiation and by time to cure: cure was defined as the complete re‐epithelialisation of the CL lesion, with no evidence of papules, inflammation, or induration Speed of healing (time taken to be 'cured') Adverse effects: the occurrence of adverse effects was evaluated blindly by means of participant interviews and physical examinations during follow‐up visits Time points reported: trial endpoint was 100 days after start of therapy | |
| Notes | Study funding sources: the HNI Malaria and Leishmaniasis Control Program is funded by the European Union. This study was supported by the United Nation Children's Fund/United Nation Development Program/WorldBank/World Health Organization Special Program for Research and Training in Tropical Diseases, the Afghan Research Evaluation Unit, and the Leveen Family Fund. Possible conflicts of interest: since March 2004, R Reithinger has been a part‐time employee of Thermosurgery Technologies. All other authors: no conflicts | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients then proceeded to pick 1 of 3 identical cardboard pieces out of a hat (the cardboard had been labelled with different treatment codes on one of its sides, the codes being non‐visible to the patient). After patients were randomly assigned to receive a treatment, the cardboard piece picked was returned to the hat." |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Comment: no blinding of participants and personnel seemed to be performed. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The occurrence of adverse effects was evaluated blindly by means of patient interviews and physical examinations during follow‐up visits", "Microscopic examination was performed blindly." Comment: microscopic examination and adverse effects were performed blindly but no description about clinical examination was given. |
| Incomplete outcome data (attrition bias) | Low risk | 172/431 (39.9%) withdrew from the study. However, ITT analyses were performed. Quote: "An intention‐to‐treat analysis of the data (... including the patients lost to follow‐up, who were considered to have had treatment failure) yielded similar results for the comparison of the odds of cure for the different treatments" |
| Selective reporting (reporting bias) | Low risk | Comment: relevant outcomes were reported |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Iran Study period: 3 months Sample size calculation: not described | |
| Participants | Type of Leishmania: L major Inclusion criteria: CL in whom the diagnosis was confirmed by laboratory demonstration of the parasite in the lesions by direct smear Exclusion criteria: allergic to antimonial drugs or pentoxifylline, lactating or pregnant, history of systemic illness N randomised: 64, 32 in each group Withdrawals: 1 participant withdrew from the MA + placebo group N participants assessed (lesions): 63. Group 1: 32 (143), group 2: 31 (164) Mean age: group 1: 27 years, group 2: 31 years Sex (male/female): 29/34 Baseline data: duration of the disease approximately 1.3 months.
| |
| Interventions | Type of interventions:
Duration of intervention: 20 days Duration of follow‐up: 3 months | |
| Outcomes | Healing rates:
Adverse effects Time points reported: after end of treatment and 3 months' follow‐up | |
| Notes | Study funding sources: not described Possible conflicts of interest: not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly divided into two groups" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Study was described as "double blind" but has no description about allocation method. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Study was described as "double blind" but has no description about the blinding method. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) | Low risk | One patient withdrew in the placebo group. Reasons for withdrawal were reported. However, no ITT analyses were performed. |
| Selective reporting (reporting bias) | Low risk | Comment: relevant outcomes were reported |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Skin Diseases and Leishmaniasis Research Center in Isfahan, Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania:L major endemic in the area. Inclusion criteria: participant with positive smear for Leishman bodies, of both sexes and > 5 years old who did not have indication for systemic therapy Exclusion criteria: facial lesions or lesions on joints, sporotrichoid type, lupoid leishmaniasis, erysipeloid type and other atypical forms of CL, pregnant women, history of cardiovascular and renal diseases N randomised: 72, 36 in each group Withdrawals: 0 N assessed: 72 Mean age: HSCS, 20.52 years; ILMA group, 18.67 years Baseline data: the most common site of lesions was on the extremities and the least common site was the trunk in both groups. The size range of lesions were from 0.5‐4 cm² (IL HSCL group) and from 0.5‐4 cm² (ILMA group) | |
| Interventions | Type of interventions:
Duration of intervention: weekly 6‐10 weeks Duration of follow‐up: 6 months | |
| Outcomes | Healing: complete improvement is defined as completely clinical re‐epithelialisation with no signs of induration and inflammation with negative smear for Leishman bodies at the end of the treatment period. Partial improvement is defined as the re‐epithelialising lesion has become smaller but not cured. If the lesion has become larger or has not been differed it will be called as no response to treatment. Time points reported: at 6 and 10 weeks of treatment and 6 months follow‐up | |
| Notes | Study funding sources: not described Possible conflicts of interest: not described | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "This N randomised controlled clinical trail study with simple sampling." "72 patients randomly divided in two equal groups". Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Selective reporting (reporting bias) | Low risk | Comment: relevant outcomes were reported |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Skin Diseases and Leishmaniasis Research Center, Iran Study period: 7 months Sample size calculation: not reported | |
| Participants | Type of Leishmania: not reported Inclusion criteria: smear from a suspected CL lesion was confirmed positive for Leishmania Exclusion criteria: pregnant women, children < 5 years of age, patients with facial lesions, those who had already received or were under other specific antileishmanial therapy, significant underlying diseases N randomised: 117 Withdrawals: 0 N participants assessed (lesions): 117: 57 (83) lesions in group 1 and 60 (94) in group 2 Mean age: group 1, 25.12 years; group 2, 22.6 years Sex (male/female): group 1, 37/20; group 2, 29/31 Baseline data: the shape of lesions was papule, nodule and plaque‐like. Lesions were located in the trunk and upper and lower limbs.
| |
| Interventions | Type of interventions:
Duration of intervention: once weekly for 4 consecutive weeks Duration of follow‐up: 6 months | |
| Outcomes | Percentage of participants 'cured':
Duration of remission and percentage of people with treated lesions that recur within 6 months Prevention of scarring Adverse effects Time points reported: at the end of treatment, and 6 months after | |
| Notes | Study funding sources: technical and financial support from the joint WHO Eastern Mediterranean Region (EMRO), Division of Communicable Diseases (DCD) and the WHO Special Program for Research and Training in Tropical Diseases (TDR): the EMRO/TDR Small Grant Scheme for Operational Research in Tropical and other Communicable Disease. Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly allocated to one of two treatment groups using a random number list generated by Epi Info (a software package designed to provide easy form and database construction, data entry, and analysis with epidemiologist statistics, map sand graphs)" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgment |
| Blinding of participants and personnel (performance bias) | High risk | Group 1 was treated with controlled localised heating using an RF heat generator. Group 2 was treated with ILMA |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Follow‐up evaluation was made by clinical assessment of treated lesions by a second dermatologist who was blinded to the method of treatment." |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes. |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Leishmaniasis clinic of the National Malaria and Leishmaniasis Control Program in Darul‐Aman District, Kabul City, Afghanistan Study period: not described Sample size calculation: to detect an 8% difference in the cure rate between the current standard therapy (ILMA) and thermotherapy by radio frequency groups, assuming 90% cure rate in the conventional therapy with an 80% power and a 5% type I error, 174 subjects were needed in each group. To compensate for anticipated loss to follow‐up, sample size inflated by 10%. Hence, the final sample size, figuring research design, rounded to nearest 10 turned out to be 390 subjects, with 195 assigned to each treatment group. | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: aged > 5 years; presence of a single, parasitologically confirmed CL lesion Exclusion criteria: history of previous infections from anthroponotic CL that was treated with antimonial medications, lesions located within 2 cm of the eyelids or on the lips or nose N randomised: 390 (195 assigned to each treatment group) Withdrawals: 8 participants (6 in group 1; 2 in group 2). N assessed: 382 (189 in group 1; 193 in group 2). Median (interval) age: group 1, 14 years (5‐70); group 2, 13 years (5‐75) Sex (male/female): group 1, 85/104; group 2, 92/101 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 5 weeks in ILMA group | |
| Outcomes | Cure was defined as complete re‐epithelialisation of the lesion with no inflammation and resolution of the papule and/or nodule. Failure was defined as no improvement, with the lesion unchanged or worse compared with its status at the start of treatment. Lesions that showed some improvement but did not meet the criteria for cure were considered treatment failures Adverse effects Time points reported: 6 months after treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were asked to pick one of two identical cardboard pieces out of a box (the cardboard had been labelled with different treatment codes on one of its sides) for their group assignment. After patients were assigned to a treatment group, the cardboard piece picked was returned to the box." |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Unclear risk | There were losses to follow‐up and no ITT analyses were performed. Also, the distribution of the lesions and the size was uneven between the 2 arms. Quote: "More papules (57.7%) were treated by thermotherapy compared to (42.3%) those which were treated by Glucantime. Nodules were mostly treated by Glucantime (58.9%), whereas all ulcers were treated by Glucantime. The lesion size interval was [1–4 cm²] with median of 1 cm² for thermotherapy by radio frequency and 2 cm² for Glucantime." This is important because the authors found out the following significant associations: Quote: "Type and size of lesion, were significantly associated with the outcome variable (cure/failure). Type of lesion was significantly associated with treatment outcome in this sample, taking papules as reference (Table V). Those who had nodules were 41% less likely and those with ulcers were 80% less likely to be cured compared with those with papules" |
| Selective reporting (reporting bias) | High risk | Adverse effects were described in Methods but not in Results. They mention them vaguely in the Discussion section. |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Iran Study period: 18 months Sample size calculation: not described | |
| Participants | Type of Leishmania:Leishmania spp: L tropica and L major Inclusion criteria: patient with CL confirmed parasitologically by direct skin smears or skin biopsies. Exclusion criteria: children < 3 years of age, pregnant and lactating women, cases with concomitant renal, liver or heart disease, and any event of any laboratory abnormality prior to initiation of treatment N randomised: 96 Withdrawals: 0 N assessed: 96 (100%): 64 in the ketoconazole group and 32 in the ILMA group Age: range 3‐64 years Sex (male/female): 44/52 Baseline data: In the ketoconazole group:
In the MA group:
| |
| Interventions | Type of interventions:
Duration of intervention: 30 days in the ketoconazole group. There is no mention about frequency of injections in MA group. | |
| Outcomes | Healing rates:
Adverse effects Time points reported: participants were followed every 2 weeks for the duration of the treatment and every 6 weeks after cessation of treatment up to 24 weeks | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated to two treatment groups using a simple randomisation method" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgment |
| Blinding of participants and personnel (performance bias) | High risk | Group 1, which included 64 participants, was designated as the group treated with oral ketoconazole. Group 2, which included 32 participants, was designated as the group that received ILMA. The outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | High risk | Imbalance in numbers and reasons for missing data across intervention groups: 7/57, ketoconazole; 9/23, ILMA |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgment |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Dermatology Clinic of Faghihi Hospital, Shiraz University of Medical Sciences, Shiraz, Iran Study period: unclear Sample size calculation: not reported | |
| Participants | Type of Leishmania: not reported Inclusion criteria: participant with CL confirmed Exclusion criteria: not described N randomised: 60 Withdrawals: 0 N assessed: 60 participants distributed into the 3 groups of equal number (n = 20) Age: not reported Sex: not reported Baseline data: lesions were located on the head, neck and lower and upper extremities. Lesion duration was divided in 2 groups: a duration of < 3 months and > 3 months. Regarding lesion size, the authors divided the sizes in 3 groups: < 1 cm, 1‐3 cm and > 3 cm. | |
| Interventions | Type of interventions:
Duration of intervention: weekly for a total of 6‐8 times for each case | |
| Outcomes | Healing rates: percentage of participants 'cured': timing not reported Adverse effects Time points reported: not reported | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgment |
| Blinding of participants and personnel (performance bias) | High risk | The outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) | High risk | No explanation was provided for missing outcome data. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports included all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Sample size calculation, reporting of Leishmania spp involved and baseline comparability were not correctly reported |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: dermatology clinic and leishmaniasis research centre of Afzalipour hospital of Kerman, province of Iran Study period: 21 months Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: aged 7–60 years, confirmed CL Exclusion criteria:chronic systemic disease (such as renal failure, myocarditis, hepatitis and pancreatitis), immune suppression, breastfeeding, pregnancy, sporotrichoid and lupoid forms, maximum diameter of lesions > 3 cm, disease duration more than 1 year, more than 2 lesions present, history of sensitisation to MA,facial and joint lesions, receiving other specific anti Leishmania therapies N randomised: 191. Group 1: 96, group 2: 95 Withdrawals: group 1: 16 (14: no follow‐up, 2 enrolled in other treatment), group 2: 15 (8 no follow‐up, 4 enrolled in other treatment, 3 did not adhere to treatment schedule) N assessed: 160 (83.77%). Group 1: participants: 80 (83.33%), group 2: participants: 80 (84.21%) Age: range 7‐60 years Sex (male/female): Randomised patients: group 1: 50(52%)/46 (48%), group 2 39 (41%)/56 (59%). Assessed patients: group 1: 42 (50%)/38 (46%); group 2: 31 (39%)/49 (61%) Baseline data (N lesions): group 1: 80, GB: 80 Locationof the target lesion:
Type of lesions:
Case type: New, group 1: 67 (83.3%); group 2: 69 (86.3%) Recurrence, group 1: 0 (0%); group 2: 1 (1.3%) Failure of previous treatment, group 1: 8 (10%); group 2: 0 (0%) Missed previous treatment, group 1: 5 (6.3%); group 2: 10 (12.5%) | |
| Interventions | Type of interventions:
Duration of intervention: 16 weeks | |
| Outcomes | Clinical cure of the lesions: defined as complete re‐epithelialisation of 100% (± scar), complete flattening of induration Laboratory cure of the lesions: negative smear of the lesions compared with baseline Cure rate based on weeks of follow‐up Adverse effects of 2 types of treatments Time points reported: weeks 2, 6, 12 and 16 | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was generated by the use of a randomisation Table. A simple block randomisation list with block size of 4 was prepared by a member of the study. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The randomisation allocation concealment was performed by sending the randomisation number in envelopes to a member who was responsible for giving the assigned treatment after each eligible patient was enrolled. The recruited patients were referred to this member to receive their assigned treatments." Comment: unclear because no mention of opaque and numbered envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | Unclear risk | There were 31 withdrawals (16/96 (16.7%) in the ILMA + cryotherapy and 15/95 (15.8%) in the CO₂ laser group) Comment: no ITT analyses were performed. However, withdrawals accounted for < 20% and were homogeneous among the treatment groups. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. Not registered. Some pre‐specified outcomes were reported. Data on individuals not presented. Conflicting data is presented between the abstract and the tables |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised double‐blind placebo‐controlled clinical trial Setting/location: Aleppo University Hospital Clinic, Aleppo, Syria Study period: 12 months (from July 2009 to July 2010) Sample size calculation: not described | |
| Participants | Type of Leishmania: not described Inclusion criteria: parasitological confirmation; aged 5–65 years; normal values of liver, kidney, and pancreas function tests and electrocardiogram before treatment Exclusion criteria: pregnant and lactating women; history of cardiac, renal, and hepatic diseases; treatment with other drugs during the month before commencement of the study N randomised: 90, 30 in each group Withdrawals: not described, but it seems that there were no dropouts N assessed: 90, 30 in each group Sex (male/female): group 1, 21 (70%)/9 (30%); group 2, 17 (56.7%)/13 (43.4%); group 3, 20 (66.7%)/10 (33.3%) Mean (SD) age: group 1, 26.3 years (11.2); group 2, 24.2 years (12.5); group 3, 25.1 years (12.4) Baseline data: Mean number of lesions (SD): group 1, 3.0 (1.92); group 2, 3.0 (1.92); group 3, 3.0 (1.92) | |
| Interventions | Type of interventions:
Duration of intervention: 3 weeks for 3 groups | |
| Outcomes | Clinical and parasitological cure: the effectiveness of the treatment was classified in 3 levels: complete response of the lesions was regarded as complete clinical and parasitological healing (negative direct smear). Partial response of the lesions was regarded as decrease of the size and indurations of the lesions, and no response was regarded as no clinical change or progression of the lesions Time to healing: proportion of complete response in 3 groups during the course of treatment Adverse effects: complications Time points reported: clinical and parasitological cure: 12 weeks. Adverse effects: 6, 8, 12 weeks | |
| Notes | Study funding sources: this project was funded by the University of Aleppo, Aleppo, Syria Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were recruited and randomised by random allocation software into 3 treatment groups of 30 subjects each. |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | Low risk | No blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding; the oral placebo was completely identical in appearance to the cimetidine tablet, they were the same colour, and drug codes were revealed only at the end of the study |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | High risk | The study report fails to include results for a key outcome that would be expected to have been reported for such a study. The adverse effects are not properly described, although questionnaires regarding response to treatment and drug side effects were completed and in Table 2 there are data, numbers (%). |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Baghdad, Iraq Study period: October 1994 to November 1995 (8 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania spp: L major and L tropica endemic in the area Inclusion criteria: confirmed cases of CL by smear or culture, or both; acute CL with a history of 12 weeks or less Exclusion criteria: cases of reinfection N randomised: 85 Withdrawals: 22 participants (participants who did not show up after the first or second injection were excluded). Losses were not reported by group N assessed: 63. Group 1, 19; group 2, 17; group 3, 18; group 4, 9 Age: range 3 months to 65 years Sex (male/female): 28/37 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: not described | |
| Outcomes | Healing: responses were graded according to scale (Sharquie 1988):
Speed of healing (time taken to be 'cured'); expressed in days Prevention of scarring Adverse effects Time points reported: participants were followed up every 10‐15 days for a period of 45 days. At the end of the 6 weeks follow‐up period, the lesions were reassessed and parasitological proof of cure or otherwise was sought by smear and/or culture | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information about the sequence generation process to permit judgment |
| Blinding of participants and personnel (performance bias) | Low risk | No blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | High risk | Of the 85 participants initially recruited, 63 participants were followed‐up for the full observation period. Participants who did not show up after the first or second injection were excluded. We do not know numbers of missing data across intervention groups |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported. |
| Methods | Study design: randomised controlled trial Setting/location: Iraq (outpatient department) Study period: October 1994 to May 1995 and November 1995 to May 1996 (15 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: L major and L tropica Inclusion criteria: CL confirmed by smear/culture; acute CL of ≤ 12 weeks duration (to exclude the possibility of self healing); those for whom systemic treatment was indicated including those for whom having multiple lesions ( > 5) or large lesions ( > 4 cm²), that could not be injected, or who had lesions near to critical areas such as the eye; very young children for whom no local injection was attempted; participants who refused local treatment (2%) Exclusion criteria: received antileishmanial treatment, either local or systemic, cases of reinfection N randomised: 130. Group 1, 39; group 2, 37; group 3, 39; group 4, 15 Withdrawals: 27. Group 1, 8; group 2, 8; group 3, 7; group 4, 3 N assessed: 104. Group 1, 31; group 2, 29; group 3, 32; group 4, 12 Mean (SEM) age: group 1, 20.57 years (3.20); group 2, 22.55 years (2.72); group 3, 13.83 years (2.45); group 4, 25.74 years (4.45) Sex (male/female): 62/68. Group 1, 13/18; group 2, 19/10; group 3, 11/21; group 4, 6/6 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: ZS groups one capsule every 8 hours Duration of follow‐up: 6 weeks | |
| Outcomes | Healing: responses were graded according to scale (Sharquie 1988):
Speed of healing (time taken to be 'cured'); expressed in days Prevention of scarring Adverse effects Time points reported: participants were followed up every 10‐15 days for a period of 45 days. At the end of the 6 weeks follow‐up period, the lesions were reassessed and parasitological proof of cure or otherwise was sought by smear and/or culture | |
| Notes | Study funding sources: none declared Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | High risk | Dropouts: 26/130 (25%) |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes. |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Military Base Clinic, Iran Study period: January to October 2001 (10 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: L major Inclusion criteria: proven cases of CL, healthy apart from CL, lesions not in close proximity to a vital organ or joint, number of lesions 1 to 3, ulcer size < 5 cm in diameter, onset of the lesions < 3 months, no previous standard anti‐Leishmania treatment, no history of allergy to the paromomycin family Exclusion criteria: not reported N randomised: 60, 30 in each group Withdrawals: 4. Group 1: 1; group 2: 3, N assessed: 36. Group 1: 29; group 2: 27 Age: Group 1: approx 20.6 years; group 2: approx 21.7 years Sex: all men Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: 20 days | |
| Outcomes | Healing rates:
Adverse effects Time points reported: follow‐up and clinical evaluation were performed at week 1 and 6 after completion of treatment. Participants were visited once at 6 months after treatment was completed. | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Study was described as open and no blinding was done |
| Blinding of outcome assessment (detection bias) | High risk | Study was described as open and no blinding was done |
| Incomplete outcome data (attrition bias) | Low risk | Comment: relevant outcomes were reported |
| Selective reporting (reporting bias) | Low risk | Comment: relevant outcomes were reported |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: single‐centre, 3‐armed, open label, randomised, controlled, phase IIb trial Setting/location: Leishmania and Malaria Centre (LMC) of the Provincial Balkh Civil Hospital Mazar‐e‐Sharif (Afghanistan) Study period: November 2010 to March 2011 (15 months) Sample size calculation: the sample size calculation was based on the per protocol (PP) analysis, defined as all participants evaluable with respect to the primary endpoint | |
| Participants | Type of Leishmania: in 44/69 participants analysed, 28 (64%) lesions were infected with L tropica and 16 (36%) with L major Inclusion criteria: CL lesions with Leishmania‐positive Giemsa smears without prior CL treatment Exclusion criteria: age < 12 years; more than one skin lesion (to exclude intra‐individual variations in this phase IIb analysis); lesion age > 3 months; lesions located on eye lids, lips or nose; drug addiction; coinfection with Mycobacterium tuberculosis, HIV, or diabetes N randomised: 87 participants: group 1, 24 (27.5%), group 2, 32 (36.8%), and group 3, 31 (35.6%) Withdrawals: lost after registration: group 2, 3; group 3, 3. Not followed up for the full treatment period: SSG, 1; group 2, 6; group 3, 3. Mixed treatment: group 3, 2 N assessed: 81 (93.10%). group 1: 24; group 2: 29; group 3: 28 Mean age: 29 years (95% CI 25–33) Sex (male/female): 32 (46%)/37 (54%) Baseline data: comparable in all 3 regimens | |
| Interventions | Type of interventions:
Duration of intervention: for all groups: daily treatments (with the exception of Fridays) during the first week, followed by topical treatments at the centre twice a week until the end of week 4 and thereafter once a week until wound closure In group 1, the SSG treatment was discontinued after week 4. In groups 2 and 3, participants dressed their lesion themselves after week 4 with the topical NaClO₂‐basic‐crème between their visits at the centre until lesion closure | |
| Outcomes | Primary outcome was the ratio of closed versus open wounds at day 75 (D75) in the PP analysis for each regimen Speed of healing: not reported in Methods Adverse effects: not reported in Methods 6 visits were scheduled in the first week, 2 visits per week from weeks 2 to 4, and 1 visit per week thereafter until complete wound closure. Follow‐up visits were required once a month until day 180 after treatment start | |
| Notes | The funders had no role in study design, data collection, data analysis, and interpretation, decision to publish, or preparation of the manuscript. KWS and HCS are members of the Board and CB is a member of the non‐profit NGO Waisenmedizin PACEM e.V. promoting access to essential medicine | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Each patient was randomly assigned to one of the 3 regimens by the random allocation generator in the computer‐based Leishmedoc system." |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Study was described as open and no blinding was done |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "the present trial could not be conducted as either a double or a single blinded trial due to the physical nature of the applied interventions" |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "The intention‐to‐treat analysis (ITT) is solely added as additional information. Patients that could not be evaluated were patients that were lost immediately after registration before treatment started. 81 out of 87 patients (93.1%) were suitable for the ITT and 69 (79.3%) for the PP analysis" |
| Selective reporting (reporting bias) | Low risk | Clinicaltrials.gov ID: NCT00996463. Registered: 15 October 2009 |
| Other bias | Low risk | Other items assessed correctly reported |
| Methods | Study design: randomised, prospective, double‐blind trial Setting/location: Dermatology Department, Ghaem Hospital, Mashhad University of Medical Sciences, Iran Study period: October 2006 to May 2008 (19 months) Sample size calculation: not described | |
| Participants | Type of Leishmania: L tropica Inclusion criteria: proven acute CL by a positive direct smear were selected for this study. Duration of lesions less than 6 months and no anti‐leishmaniasis treatment received during 2 months ago Exclusion criteria: pregnant or nursing women, participants with hepatic, renal, and heart diseases N randomised: 115. Group 1: 30, group 2: 85 Withdrawals: excluded because of side effects: group 2, 6. Not followed up for the full treatment period: group 1, 4; group 2, 5 N assessed: 100 (86.96%). Group 1: 26 (86.67%); group 2: 74 (87.06%) Mean (SD) age: group 1, 32 years (23), group 2: 25 years (19) Sex (male/female): group 1, 11/15, group 2: 39/35 Baseline data:
| |
| Interventions | Type of interventions:
Duration of intervention: group 1: 45 days, group 2: 20 days | |
| Outcomes | Decreased indurations of lesion (lesions were measured by palpation and ruler): in aspect of response to treatment in comparison with first visit participants graded as 4 improvement rate groups:
Decreased indurations of lesion after 45 days from completing treatment period: the same scale Adverse effects: severe muscular pain and topical reaction of inoculation site (severe erythema and pruritus) Time points reported: at the end of clinical treatment. After 45 days from completing treatment period. | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using simple randomisation". |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Open trial |
| Blinding of outcome assessment (detection bias) | High risk | Not done. At each visit all lesions were reexamined by the same dermatologist. The size and induration of lesions were measured by palpation and ruler. No photographs were taken |
| Incomplete outcome data (attrition bias) | Unclear risk | 100 out of 115 participants completed the study. 6 participants who received systemic MA were excluded because of side effects that included severe muscular pain and topical reaction of inoculation site (severe erythema and pruritus) |
| Selective reporting (reporting bias) | High risk | Protocol not available. Not registered. Alhtough most pre‐specified outcomes were reported, adverse effects were not clearly reported (only for those excluded from the analysis) |
| Other bias | Unclear risk | There was not enough information in the publication to assess if there were other biases present. |
| Methods | Study design: randomised controlled trial Setting/location: Fars province, Iran Study period: not described Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania spp: L major and L tropica in the area Inclusion criteria: diagnosed as having CL based on positive smears from lesions, and in some cases, cultures and histopathologic studies were also performed. Exclusion criteria: pregnant, nursing, or serious concomitant diseases. N randomised: 171 Withdrawals: 0 N assessed: 171 participants: 86 participants in the herbal extract Z‐HE group and 85 participants in the IMMA (15 to 20 mg/kg/d) Age: range 10 months to 69 years Sex (male/female): 84/87 Baseline data: the duration of the disease was < 4 months. Most participants had papular and papulonodular lesion(s), although other clinical forms including ulcerative, eczematoid, hyperkeratotic, and erysipeloid types were also present. Most participants had multiple lesions, and the most common sites were the face and the extremities. | |
| Interventions | Type of interventions:
Duration of intervention: 20 consecutive days | |
| Outcomes | Healing rates: complete cure was defined as clinical improvement with complete healing and re‐epithelialisation of the lesion(s), partial cure as partial clinical improvement with reduction in infiltration erythema, and size of the lesion(s), and failure as the absence of any changes in the lesion(s) or progression and worsening of the lesion(s) Adverse effects Time points reported: 6 weeks post‐treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information about the sequence generation process to permit judgment |
| Blinding of participants and personnel (performance bias) | Low risk | Blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to permit judgment |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgment |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
| Methods | Study design: randomised controlled trial Setting/location: Turkey Study period: around 8 weeks Sample size calculation: not described | |
| Participants | Type of Leishmania: Leishmania spp: L tropica in the area Inclusion criteria: confirmed diagnosis of CL Exclusion criteria: pregnant, nursing, or serious concomitant diseases N randomised: 72 Withdrawals: 0 N assessed: 72 (100%): 40 participants in group 1 and 32 participants in group 2 Age: most were children aged 10 years or younger Sex: both sexes Baseline data: the most common site of the lesion was the face and most of the participants had one papulonodular lesion, with duration of the lesions varying from 1 to 12 months
| |
| Interventions | Type of interventions:
Duration of intervention: 4 weeks | |
| Outcomes | Healing rates: percentage of participants 'cured' one month after treatment Adverse effects Time points reported: at the end of treatment and 4 weeks post‐treatment | |
| Notes | Study funding sources: not reported Possible conflicts of interest: none declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were divided randomly into two treatment groups" Comment: insufficient detail was reported about the method used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "An open‐labeled, N randomised controlled trial to evaluate the efficacy of paromomycin ointment as compared with ketoconazole" Comment: we think the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "No subjects withdrew because of this adverse effect" Comment: no dropouts, so ITT analyses were performed. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available, but it is clear that the published reports include all expected outcomes. |
| Other bias | High risk | Sample size calculation and reporting of Leishmania spp involved was not correctly reported |
ACL: anthroponotic cutaneous leishmaniasis; AL: allopurinol; CCR: complete clinical response; CL: cutaneous leishmaniasis; HF‐EC: high frequency electrocauterisation; HSCS: hypertonic sodium chloride solution; IL: intralesional; ILMA: intralesional meglumine antimoniate; ILSSG: intralesional sodium stibogluconate; IM: intramuscular; IMMA: intramuscular meglumine antimoniate; IQR: interquartile range; IV: intravenous; MA: meglumine antimoniate; MBCL: methyl benzethonium chloride; MDLBT: median duration of lesions before therapy; MNL: median number of lesions; MSL: median size of lesions; MWT: moist wound treatment; PDT: topical photodynamic therapy; PR: paromomycin; RF: radiofrequency; RFHT: radiofrequency heat therapy; SD: standard deviation, SEM: standard error of the mean; SSG: sodium stibogluconate; TCA: trichloroacetic acid; TM: ThermoMed; ZS: zinc sulphate;
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Review | |
| Inclusion criteria of the patients: patients with lupoid leishmaniasis, chronic recurrent leishmaniasis, that typically follows an acute form of cutaneus leishmaniasis | |
| Not an RCT. "Selected patients were categorised into two groups (groups A and B) of 110 persons each. Alternate patients were included in group A and B, respectively" | |
| They stated that participants were randomly selected for the study, but not randomly assigned to the treatment groups. | |
| They stated that participants were randomly selected for the study, but not randomly assigned to the treatment groups. | |
| Review | |
| Cross‐over study | |
| It measured immunity parameters but did not show any clinical results. | |
| This was a meta‐analysis. | |
| The method of generation of randomisation was inappropriate. The author was contacted and stated that after enrolling the participants, they did consecutively allocate ILMA for odd number participants and used topical paromomycin for even number participants. | |
| They stated that participants were randomly selected for the study, but not randomly assigned to the treatment groups. | |
| Included immunocompromised and chronically ill patients | |
| Only studied electrocardiogram and biochemical adverse effects of meglumine antimoniate | |
| They stated that participants in both groups were randomly selected. However, they did not have an initial population eligible for the study that was randomly divided in the 2 treatment groups. But rather one group of people that were randomly selected for one group and another group of participants that were also randomly selected to form part of the other group. Besides, the duration of treatments was not the same and the follow‐up was also different for both treatment groups. | |
| No clear data is available for multiple lesions. Only lesions from participants with multiple lesions were randomised. The lesions from participants with single lesions a cross‐over study was performed. |
RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Double‐blind randomised controlled trial This study was carried out in some clinics of Kerman University of Medical Sciences (Iran), from October 2008 to December 2010. Sample size calculation: a sample size of 40 participants per treatment group was planned, a probability of a type I error at alpha = 0.05 and beta = 0.1 to determine a 20% difference between intralesional injection of ZS 2 % solution with ILMA (Glucantime) |
| Participants | Type of Leishmania: L tropica Inclusion criteria: the presence of parasitological confirmed lesion(s) of CL and aged 5–60 years Exclusion criteria: disease duration more than 6 months, those with a history of hypersensitivity to MA (Glucantime) or ZS, pregnant or nursing women, those with more than 5 lesions, those with lesions with size of 5 cm or more, and a history of any anti‐leishmanial therapy during last 4 weeks N randomised: 80, 40 in each group Withdrawals: 34, 18 in the ZS‐treated group and 16 patients in the MA (Glucantime)‐treated group (lost to follow‐up in all of the participants except in one in the ZS‐treated group, who had severe necrosis) N assessed: 46; 22 patients in the ZS‐treated group and 24 patients in the MA (Glucantime)‐treated group There was no significant difference between compared groups' baseline characteristics |
| Interventions | Group 1: intralesional injection of ZS 2% vials once a week for 10 weeks or sooner in case of complete resolution of the lesions Group 2: ILMA once a week for 10 weeks or sooner in case of complete resolution of the lesions Co‐intervention: in both groups cryotherapy was performed once every other week for 10 weeks |
| Outcomes | Clinical response: no response to treatment was defined if the area of a lesion decreased less than 75%, partial treatment if decreased 75% to 99%, and complete treatment if decreased 100% compared to its baseline area Time to healing (partial/complete treatment) Adverse effects: there were no major side effects in either group. Pain was observed in all participants of both groups. In ZS group 4 participants developed necrosis of the site of the injection while this was not observed in MA (Glucantime) group at all Time points reported: on average, each participant was followed for 4.1 weeks (SD 2.6). |
| Notes | Study funding sources: none declared Possible conflicts of interest: there is no conflict of interest |
| Methods | Triple‐blind randomised controlled trial Performed in Shahid Dadbin Clinic of Leishmaniasis Research Center (Iran), at Kerman University of Medical Sciences, between 2008 and 2010 Sample size calculation: a sample size of 44 participants per treatment group was planned with a probability of a type I error at alpha = 0.05 and beta = 0.1 to determine a 20% difference between topical terbinafine and vehicle in outcome. |
| Participants | Type of Leishmania: L major and L tropica in the area Inclusion criteria: < 2 years of age; parasitological diagnosis of cutaneous leishmaniasis from all lesions with direct smear; ulcerative lesions with duration of less than one month that were not on exposed areas or joints; the size of lesions has to be < 3 cm; ≤ 3 lesions; no anti‐leishmanial therapy during last 2 weeks, and with no history of hypersensitivity to MA Exclusion criteria: pregnant or nursing women, patients with hepatic, renal, or heart diseases N randomised: 88, 44 in each group Withdrawals: 36 in topical terbinafine + MA; 29 in vehicle + MA N assessed (3 months): 9 in topical terbinafine + MA; 15 in vehicle + MA There are significant differences between participants' sex in intervention and control groups |
| Interventions | Group 1: IMMA 20 mg/kg/d + topical terbinafine for 20 days 3 months follow‐up after completing of the treatment phase Group 2: IMMA 20 mg/kg/d + vehicle (Mahan Vaseline) for 20 days Visited at days: 0, 14, 30 and 44 |
| Outcomes | Clinical cure, defined as:
Time to healing (partial/complete treatment) |
| Notes | Study funding sources: none declared Possible conflicts of interest: there is no conflict of interest. |
| Methods | Randomised controlled study Department of Dermatology, Sheikh Zayed Medical College/Hospital, Rahim Yar Khan, Pakistan, from November 2013 to June 2014 Sample size: was calculated by using a formula for 2 proportions; expected proportion for duration of treatment in one group was taken as 55, and in second group 51 days; power of study was taken as 80, and standard error of 5% |
| Participants | Type of Leishmania: not reported Inclusion criteria: patients of all age groups except neonates, with single or multiple parasitologically confirmed lesions of cutaneous leishmaniasis with no past history of disease and not previously treated with SSG or MA Exclusion criteria: retinal abnormality or visual field defects, pregnancy, hepatic dysfunction, known hypersensitivity to chloroquine and those having visceral leishmaniasis N randomised: 86; 48 intralesional chloroquine, 38 oral chloroquine Withdrawals: 0 N assessed: 86; 48 intralesional chloroquine, 38 oral chloroquine |
| Interventions | Intralesional and oral chloroquine administration Co‐interventions: lesions with secondary bacterial infection before, during, or after treatment were treated with topical antibiotics. If such infections required systemic treatment, an antibiotic that has no activity against Leishmania (e.g. erythromycin) was given. |
| Outcomes | Cure was defined as the complete re‐epithelialisation of the ulcerated lesions, with no evidence of papules, inflammation, or induration Quantitative variables like, duration, cost and total dose of treatment were calculated Adverse effects Time points reported: < 4 weeks, 5‐8 weeks, ≥ 9 weeks |
| Notes | Study funding sources: none declared Possible conflicts of interest: none declared |
| Methods | Interventional randomised controlled study was conducted in the Skin Disease and Leishmaniasis Research Center of Isfahan University of Medical Sciences, Isfahan, Iran, between April 2010 and May 2011 Sample size calculation: not described |
| Participants | Leishmania type: not described Inclusion criteria: patients older than 5 years with biopsy‐confirmed cutaneous leishmaniasis were eligible if they had the following criteria: lesion diameter < 3 cm, disease duration < 12 weeks, lesion‐to‐eyelid distance > 2 cm, and no history of systemic or topical therapy for cutaneous leishmaniasis Exclusion criteria: pregnancy, lactation, immunosuppressive therapy, and serious side effects of medication N randomised: 90. 30 in each group (ILMA (Glucantime) alone, ILMA + TCA 50%, or fractional CO₂ laser) Withdrawals: 14 N assessed: 76 participants (84.5%) completed treatment and were followed up for 60 days |
| Interventions | ILMA alone, ILMA + TCA 50% or fractional CO₂ laser for up to 8 weeks Participants in all 3 groups were followed up weekly for the next 6 months. |
| Outcomes | The clinical response was rated as complete improvement (complete re‐epithelialisation of the lesion with negative direct skin smear result), partial improvement (50%–75% improvement of the lesion size), and no change in the lesion appearance. Time to healing Adverse effects The improvement of scar was also evaluated according to the participant's satisfaction, the morphology of the lesion, the level of induration, and the level of atrophy and scored as follows: score of 1 (less than 5% improvement), score of 2 (25% to 50% improvement), score of 3 (51% to 75% improvement), and score of 4 (76% to 100% improvement) |
| Notes | Study funding sources: none declared Possible conflicts of interest: there is no conflict of interest. |
| Methods | Exploratory phase II, randomised, vehicle‐controlled, single‐centre (Ankober Health Center, North Shewa zone of Amhara region, Ethiopia) study Sample size calculation: not described |
| Participants | Leishamania type: not described Inclusion criteria: patients with localised cutaneous leishmaniasis (LCL) aged 18–65 years with a new, uncomplicated, localised, single lesion on the face or arms and positive parasite smear by microscopy Exclusion criteria: cutaneous leishmaniasis with secondary infection, concomitant diseases (mucocutaneous or visceral leishmaniasis), history of anti‐leishmanial treatment within the past 6 months, abnormality of biochemical and/or haematological laboratory tests, known hypersensitivity to any of the Shiunko components, or pregnancy (positive urine HCG test), breastfeeding, or possibility of becoming pregnant during the study N randomised: 40 were randomised to receive vehicle and Shiunko ointment (20 participants for each group) Withdrawals: 2 participants did not receive complete treatment, and 9 were not completely followed up. In the vehicle group, 2 and 5 cases did not have complete treatment and follow‐up, respectively. N assessed: 38 participants had complete treatment and 31, complete follow‐up. In the vehicle group, 18 and 15 cases had complete treatment and follow‐up, respectively. |
| Interventions | Group 1: the composition of Shiunko was as follows: 2.04 g shikon, 1.02 g tohki, 16.92 g sesame oil, and 6.76 g honeycomb wax Group 2: the vehicle contained 20 g wax Co‐interventions: cryotherapy was to be offered to all participants who were withdrawn or discontinued from the study for safety reasons Vehicle and Shiunko ointment applied on the lesion twice a day for 4 weeks Follow‐up: 16 weeks |
| Outcomes | Cure: complete cure was defined as complete wound closure and re‐epithelialisation without inflammation or infiltration and absence of parasite (amastigotes) within 12 weeks after the end of treatment. Partial response was defined as improvement of Leishmania signs (skin oedema, erythema, and/or hardening) and/or reduction in size but not total disappearance of the lesion and absence of parasite (amastigotes) within 12 weeks after the end of treatment. Treatment failure was defined as failure of the lesion size to decrease and/or lack of lesion sign improvement or re‐epithelialisation and/or presence of leishmanial amastigotes in the lesion 12 weeks after end of treatment (week 16) Adverse effects Clinical and parasitological assessments were performed before treatment, weekly for 4 weeks, and then 4, 8, and 12 weeks after the end of treatment |
| Notes | Study funding sources: the study was supported by the Institute of Tropical Medicine, Nagasaki University (Japan), ArmauerHansen Research Institute (Ethiopia), and Okusa Co., Ltd. (Japan). Possible conflicts of interest: there is no conflict of interest. |
| Methods | Clinical randomised trial conducted from March 2008 through 2009 in the dermatology department of Quaem University Hospital, Mashhad, Iran Sample size calculation: not described |
| Participants | Leishamania type: not described Inclusion criteria: positive smear for leishmaniasis with disease duration of less than 12 weeks, no treatment for the current condition before and volunteer to participate in the study Exclusion criteria: pregnancy, breastfeeding, history of simultaneous treatment with other methods before or during the trial, history of local cutaneous or systemic diseases in the past 2 months, history of intolerance or allergy to macrolides, severe underlying diseases such as cardiovascular, renal, or hepatic diseases N randomised: 96; 26 (43 lesions) azithromycin, 40 (54 lesions) MA (Glucantime) Withdrawals: 2 azithromycin group N assessed: 94; 24 (40 lesions) azithromycin, 40 (54 lesions) MA |
| Interventions | Group 1: topical liposomal form of azithromycin was administered for the first group twice daily. Clinical evaluations were performed every week during the treatment course (8 weeks) by a single dermatologist in both groups. The participants were followed up for recurrence or complications 6 and 12 months after the end of the treatment course. |
| Outcomes | Complete cure was defined as full re‐epithelialisation, disappearance of oedema, induration, and other signs of inflammation, and a negative direct skin smear result Improvement rate (%): complete improvement (full re‐epithelialisation of the lesions for ulcerative ones or disappearance of induration and erythema; significant improvement (decrease in induration size > 60%); moderate improvement (decrease in induration size between 30% and 60%; slight improvement (decrease in induration size of < 30%). Adverse effects |
| Notes | Study funding sources: none declared Possible conflicts of interest: none declared |
| Methods | Interventional randomised study Setting: Sri Lanka Sample size calculation: not described |
| Participants | Leishmania type:L donovani Inclusion criteria: Laboratory‐confirmed CL patients with single lesions Exclusion criteria: — N randomised: test group (n = 98); control group (n = 115) Withdrawals: — N assessed: — |
| Interventions | Group 1: single session of radiofrequency induced heat therapy (RFHT) at 50ºC for 30 s Group 2: received weekly ILSSG until cure or 10 doses Participants were followed up fortnightly for 12 weeks to assess clinical response and adverse effects. |
| Outcomes | Cure rate Adverse effects Time points reported: 8, 10, and 12 weeks |
| Notes | Poster |
| Methods | Randomised controlled trial |
| Participants | 40 participants (no more data described in abstract) |
| Interventions | Topical ointment prepared from the stem extract of Morinda citrifolia (no more data described in abstract) |
| Outcomes | Improvement (no more data described in abstract) |
| Notes | Article request to authors |
CL: cutaneous leishmaniasis; HCG: human chorionic gonadotropin; ILMA: intralesional meglumine antimoniate; IM: intramuscular; MA: meglumine antimoniate; SSG: sodium stibogluconate; ZS: zinc sulphate.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A clinical trial to assess the safety and effect of heat therapy in comparison to standard intra‐lesional sodium stibogluconate for cutaneous leishmaniasis |
| Methods | Randomised controlled trial |
| Participants | Inclusion criteria: suggestive skin lesions (papules, nodules, plaques, ulcers and nodule‐ulcers) who were clinically diagnosed by a consultant dermatologist and parasitologically confirmed as CL Exclusion criteria: non‐localised leishmaniasis (VL, MCL, leishmaniasis recidivans, diffuse cutaneous leishmaniasis and post‐kala‐azar dermal leishmaniasis); use of prior concomitant treatment for leishmaniasis including any traditional medicines; lesions close to nasal, oral, urogenital, anal areas (mucosae) and the eyes; multiple lesions; any chronic or concomitant illnesses and people on pace makers and any metallic devices; pregnancy and breastfeeding mothers; children < 12 years of age; immunocompromised states including HIV/AIDS and use of immunosuppressants like steroids; alcohol abuse; not capable of understanding and complying with the study protocol; known hypersensitivity or allergy to treatment Age: 12‐90 years |
| Interventions | The device used was the ThermoMed 1.8, ThermoSurgery Technologies portable battery operated device. The generator has received clearance by the US Food and Drug Administration for the treatment of CL. It delivers precisely controlled localised radiofrequency waves to selectively destroy diseased tissue. Heat therapy was administered as a single session. The lesion and surrounding normal skin was cleaned with normal saline. Then the area was anaesthetised with 2% lignocaine using a 1 cc syringe. The device was used in according to manufacturers instructions (ThermoMed 1.8; Thermosurgery). It generates a 6.78 mHz frequency applied with a hand set that is attached to 2 applicator electrodes which were placed on the diseased skin. A temperature of 50ºC was applied for 30 s to cover an area about 49‐73 mm², according to the size of electrodes (3 sizes are provided). Then the applicator is moved to another area of the lesion until the entire area is treated. Once treatment begins the temperature is measured by a thermistor embedded in the applicator which ensures that the applied temperature remains constant. After treatment the lesions were covered with gauze to prevent secondary infections and participants were given an antibiotic cream (soframycin 1% per 30 g depending on the size of lesion to cover the lesion) to be applied twice a day for 3 days. |
| Outcomes | Recurrence Treatment efficacy was measured by the percentage of participants clinically cured by 8 weeks, 10 weeks, 12 weeks and 16 weeks after initiation of treatment in both groups.
Any adverse effects like secondary bacterial infections, allergy to treatment or hypersensitivity and worsening of the lesion clinically was recorded during or after treatment with either therapy |
| Starting date | December 2014 |
| Contact information | Dr Fathima Wardha Refa PGIM address: No. 160, Professor Nandadasa Kodagoda Mawatha (Norris Canal Road), 00700, Colombo 7. 2.Department of Parasitology, Faculty of Medicine Colombo University of Colombo address: No 25, Kynsey Road, Colombo 8 0080, Sri Lanka. 7 MACLEOD ROAD COLOMBO 4, Sri Lanka +94 727800003 or +94 11 2580093 or+94 11 2699284 |
| Notes | — |
| Trial name or title | Comparison between the efficacy of intralesional placebo and nitric oxide releasing patch versus placebo patch and Glucantime in the treatment of cutaneous leishmaniasis |
| Methods | Randomised, placebo‐controlled trial |
| Participants | Inclusion criteria: diagnosis of acute zoonotic cutaneous leishmaniasis, proven parasitology by direct smear; aged 18‐50 years; lesion diameter ≤ 3 cm; 1 lesion, not located on the face near the eyes, joints, cartilage, on the nose and ears; < 3 months passed from diseases times Exclusion criteria: pregnancy and lactation; risk of presence or incidence of sporotrichoid or satellite lesions; history of hepatitis, heart, or kidney disorder; taking immunosuppressive medications (over the last 6 months); local or systemic treatment against leishmaniasis in the last 3 months; history of heart attack or high blood pressure; liver disease; anaemia; history of surgery for head and brain haemorrhage; taking blood pressure medications, antidepressants, or drugs used for angina |
| Interventions | Group 1: nitroglycerin patch (the pharmacy of Nour and Ali Asghar hospital in Isfahan) once a day covering 5.08 to 7.62 cm of lesion + intralesional injection of placebo (injection of distilled water) once a week (15‐30 mg) until whitening of base of the ulcer for 8 weeks or until complete cure Group 2: ILMA (Meglusan) from Avenue de Scheut company in Belium, once a week (15‐30 mg) until whitening of base of the ulcer + placebo patch (the pharmacy of Nour and Ali Asghar hospital in Isfahan) once a day covering 5.08 to 7.62 cm of lesion for 8 weeks or until complete cure |
| Outcomes | Improvement rate. Timepoint: 1, 2, 3, 4, 7, 8 weeks during treatment and 12, 16, 20 weeks after end of treatment. Method of measurement: observation and examination Induration. Timepoint: 1, 2, 3, 4, 7, 8, 12, 16, 20 weeks after end of treatment. Method of measurement: physical examination Lesion area. Timepoint: 8, 12, 20 weeks after end of treatment |
| Starting date | August 2013 |
| Contact information | Fariba Jaffary Skin Diseases and Leishmaniasis Research Center, Isfahan University of Medical Sciences, Sedigheh Tahereh (AS) Research Centers Complex, Khorram Ave., Isfahan, Iran Isfahan Iran, Islamic Republic Of Iran. 00983113373736 |
| Notes | — |
| Trial name or title | The effect of MJ1 (topical dairy extract) versus routine care for treatment of cutaneous leishmaniasis (rural) in Isfahan Iran:a randomised controlled clinical trial (RCTs) |
| Methods | Randomised controlled trial |
| Participants | Inclusion criteria: cutaneous leishmaniasis of parasitology confirmed that they have not been previously treated; any other medical problem (such as heart disease, renal, hepatic, or haematological); available for follow‐up; informed consent to participate in the study Exclusion criteria: secondary infections, history of allergic reactions |
| Interventions | Group 1: in this group patients apply MJ1 skin cream 3 times a day, they are trained to use it for a month with a diameter of 3 mm on the rub of the lesion without dressing Group 2: skin cream MJ1 ‐ 3 times a day ‐ for a month |
| Outcomes | Lesion size, lesion diameters measured Timepoint: 1, 2, 3, 4 and 8 weeks after starting treatment, participants are evaluated. Method of measurement: at each visit, the 2 dimensions are measured and the area calculated |
| Starting date | December 2013 |
| Contact information | Dr Mohsen Janghorbani Hezar jarib Street, School of Public Health, Isfahan University of Medical Sciences Isfahan Iran, Islamic Republic Of 00983117922774 |
| Notes | — |
| Trial name or title | Phase 2 study of the efficacy of daylight activated photodynamic therapy in the treatment of cutaneous leishmaniasis |
| Methods | Randomised, parallel assignment, open label |
| Participants | Age: ≥ 18 years |
| Interventions | Group 1: photodynamic therapy Application of Metvix 16% cream followed by exposure to daylight for 2.5 h Group 2: cryotherapy for 2 times 20 s |
| Outcomes | Eradiation of amastigotes |
| Starting date | September 2009 |
| Contact information | Prof Claes D. Enk, Hadassah Medical Organization |
| Notes | — |
| Trial name or title | Pilot study of efficacy of topical nano‐liposomal meglumine antimoniate (Glucantime) or paromomycin in combination with systemic Glucantime for the treatment of anthroponotic cutaneous leishmaniasis (ACL) caused by Leishmania tropica |
| Methods | Randomised, parallel assignment, double‐blind |
| Participants | Inclusion criteria: aged 12‐60 years; parasitologically proven CL due toL tropica; history of failure to at least one full course of systemic meglumine antimoniate (Glucantime); general good health based on history and physical examination; ≤ 4 lesions; lesion size < 3 cm; signed informed consent voluntarily and knowingly; guardian's signature for volunteer less than 18 years old Exclusion criteria: pregnant or lactating women and those who are planning to be pregnant in next 60 days; use of other types of treatment for CL; involvement in any other drug or vaccine trial during the study period; known heart, kidney, liver diseases based on history and physical exam; abnormal ECG Age: 12‐60 years |
| Interventions | Group 1: liposomal paromomycin (liposomes containing 10% paromomycin Group 2: liposomal MA (Glucantime) Group 3: placebo + liposomal MA |
| Outcomes | Complete cure equal to complete re‐epithelialisation of all lesions |
| Starting date | March 2011 |
| Contact information | Ali Khamesipour, Tehran University of Medical Sciences |
| Notes | — |
| Trial name or title | Randomised, double‐blind, controlled study on efficacy and safety of intralesional metronidazole vs intralesional sodium stibogluconate in L donovani cutaneous leishmaniasis |
| Methods | Randomised controlled trial |
| Participants | Inclusion criteria: > 12 years of age, positive slit skin smear and/or skin biopsy for Leishmania parasites Exclusion criteria: pregnancy, breastfeeding, known renal impairment, known liver impairment, congestive cardiac failure |
| Interventions | Group 1: intralesional metronidazole 0.2‐4 mL per lesion depending on the size of the lesion, weekly until cure or maximum of 10 injections Group 2: intralesional stibogluconate 0.2‐4 mL per lesion depending on the size of the lesion, weekly until cure or maximum of 10 injections |
| Outcomes | Rate of clinical cure Adverse effects – anticipated local side effects are pain, ulceration, scarring, postinflammatory hyperpigmentation or depigmentation. Systemic side effects are not anticipated as the drug is given intralesionally. |
| Starting date | November 2014 |
| Contact information | Ranthilaka R Ranawaka 0112855200 |
| Notes | — |
CL: cutaneous leishmaniasis; ECG: electrocardiogram; ILMA: intralesional meglumine antimoniate.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.1 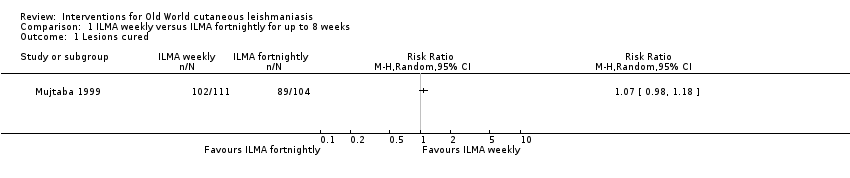 Comparison 1 ILMA weekly versus ILMA fortnightly for up to 8 weeks, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 ILMA (every other day) versus IMMA (6 d/week) for up to 4 weeks, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 IMMA (30 mg/kg/d for 3 weeks) + cimetidine versus IMMA (30 mg/kg/d for 3 weeks) + placebo, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 4.1 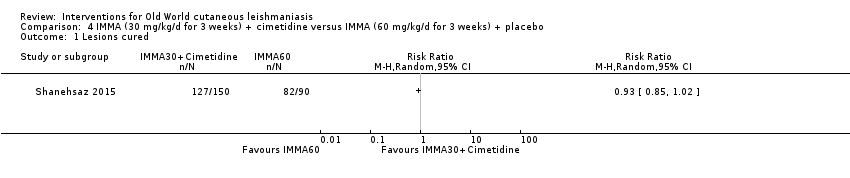 Comparison 4 IMMA (30 mg/kg/d for 3 weeks) + cimetidine versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 5.1  Comparison 5 IMMA (60 mg/kg/d for 3 weeks) + placebo versus IMMA (30 mg/kg/d for 3 weeks) + placebo, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 2 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.71, 0.96] |
| Analysis 6.1 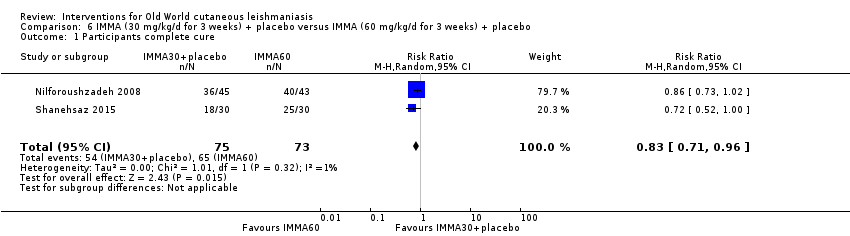 Comparison 6 IMMA (30 mg/kg/d for 3 weeks) + placebo versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 6.2  Comparison 6 IMMA (30 mg/kg/d for 3 weeks) + placebo versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 2 Adverse effects. | ||||
| 2.1 Serious adverse effects | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Skin reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Cardiac toxicity 'QT prolongation' | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 7.1  Comparison 7 IMMA (30 mg/kg/d for 3 weeks) + 40 mg omeprazole versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 8.1 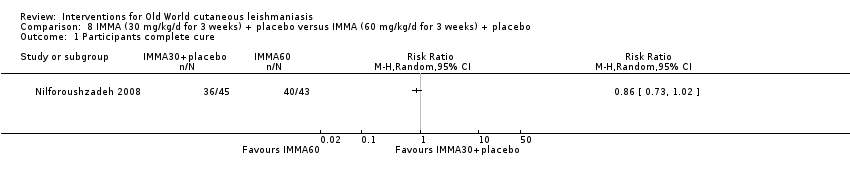 Comparison 8 IMMA (30 mg/kg/d for 3 weeks) + placebo versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 9.1  Comparison 9 IMMA (30 mg/kg/d for 3 weeks) + 40 mg omeprazole versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 10.1  Comparison 10 ILMA + non‐silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 1 Lesions cured. | ||||
| 2 Adverse effects (itching and burning) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 10.2  Comparison 10 ILMA + non‐silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 2 Adverse effects (itching and burning). | ||||
| 3 Adverse effects (oedema) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 10.3 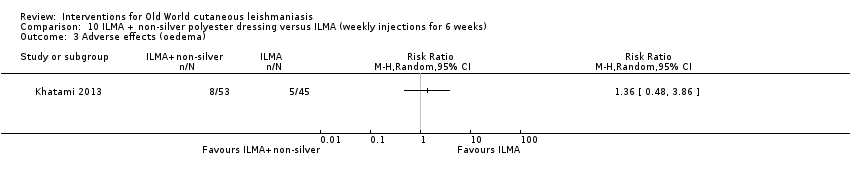 Comparison 10 ILMA + non‐silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 3 Adverse effects (oedema). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 11.1 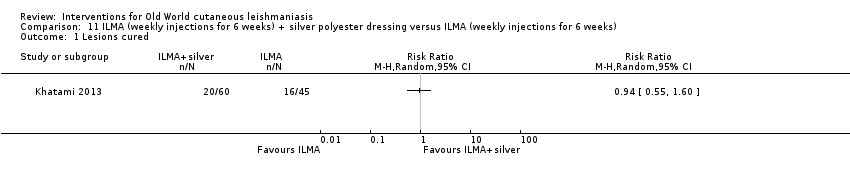 Comparison 11 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 1 Lesions cured. | ||||
| 2 Adverse effects (itching and burning) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 11.2  Comparison 11 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 2 Adverse effects (itching and burning). | ||||
| 3 Adverse effects (oedema) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 11.3 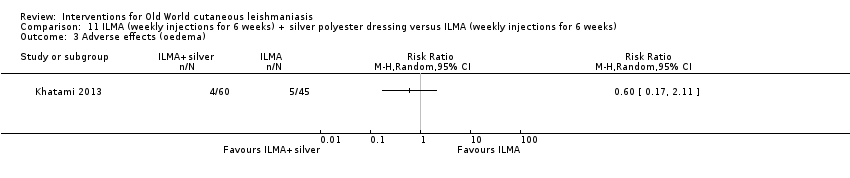 Comparison 11 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 3 Adverse effects (oedema). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 12.1 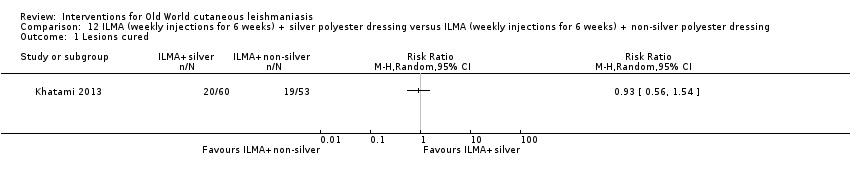 Comparison 12 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks) + non‐silver polyester dressing, Outcome 1 Lesions cured. | ||||
| 2 Adverse effects (itching and burning) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 12.2  Comparison 12 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks) + non‐silver polyester dressing, Outcome 2 Adverse effects (itching and burning). | ||||
| 3 Adverse effects (oedema) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 12.3  Comparison 12 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks) + non‐silver polyester dressing, Outcome 3 Adverse effects (oedema). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 13.1  Comparison 13 ILMA (weekly injections for 6 weeks) + gel mask twice a day versus ILMA (weekly injections for 6 weeks) + vehicle, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 14.1 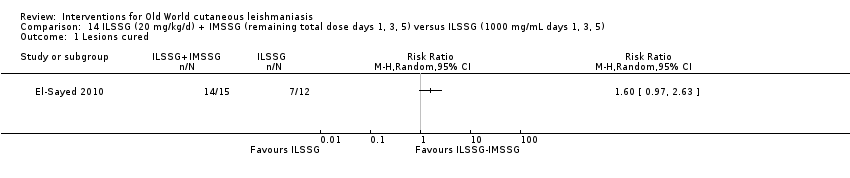 Comparison 14 ILSSG (20 mg/kg/d) + IMSSG (remaining total dose days 1, 3, 5) versus ILSSG (1000 mg/mL days 1, 3, 5), Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 15.1  Comparison 15 ILSSG (5 injections of 2 mL to 5 mL every 5 to 7 d for 29 days) versus IMSSG (20 mg/kg/d for 3 weeks), Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects (mild heart symptoms) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 15.2 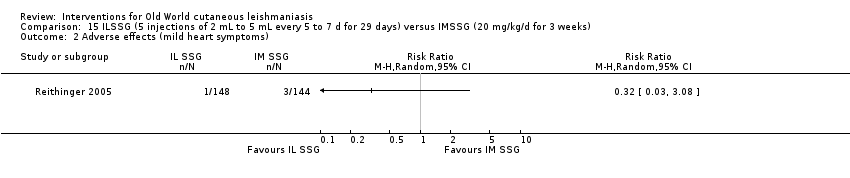 Comparison 15 ILSSG (5 injections of 2 mL to 5 mL every 5 to 7 d for 29 days) versus IMSSG (20 mg/kg/d for 3 weeks), Outcome 2 Adverse effects (mild heart symptoms). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 16.1  Comparison 16 Ketoconazole 600 mg/d for 6 weeks versus ketoconazole 800 mg/d for 6 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects (nausea and vomiting) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 16.2 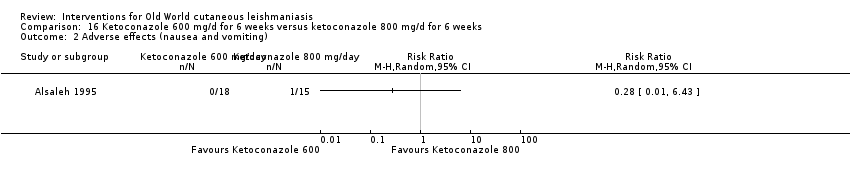 Comparison 16 Ketoconazole 600 mg/d for 6 weeks versus ketoconazole 800 mg/d for 6 weeks, Outcome 2 Adverse effects (nausea and vomiting). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 17.1  Comparison 17 Ketoconazole 600 mg/d for 30 d versus ILMA (6 to 8 biweekly injections), Outcome 1 Participants cured. | ||||
| 2 Adverse effect (liver enzymes increase) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 17.2  Comparison 17 Ketoconazole 600 mg/d for 30 d versus ILMA (6 to 8 biweekly injections), Outcome 2 Adverse effect (liver enzymes increase). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 18.1  Comparison 18 ILSSG (100 mg/mL days 1, 3, 5) + oral ketoconazole (600 mg/d for 4 weeks) versus ILSSG (100 mg/mL days 1, 3, 5), Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 19.1  Comparison 19 ILSSG (100 mg/mL days 1, 3, 5) + ketoconazole (600 mg/d for 4 weeks) versus ILSSG (20 mg/kg/d) + IMSSG (remaining total dose days 1, 3, 5), Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Analysis 20.1  Comparison 20 Itraconazole (200 mg for 6 weeks) versus placebo, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Analysis 21.1 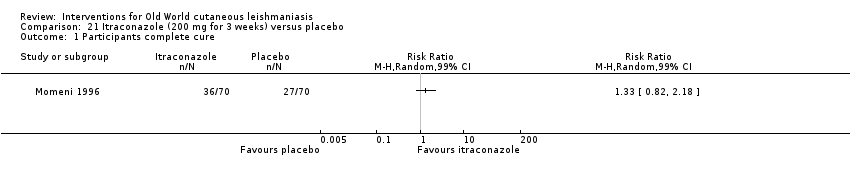 Comparison 21 Itraconazole (200 mg for 3 weeks) versus placebo, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 3 | 244 | Risk Ratio (M‐H, Random, 99% CI) | 3.70 [0.35, 38.99] |
| Analysis 22.1  Comparison 22 Itraconazole (200 mg for 6 to 8 weeks) versus placebo, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 22.2 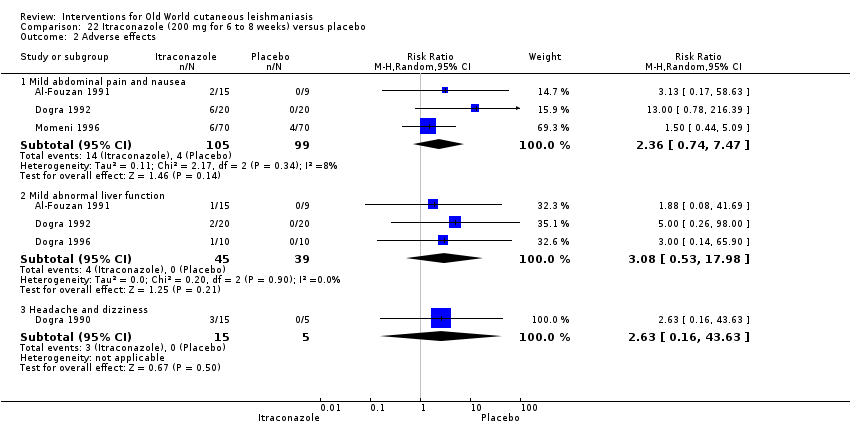 Comparison 22 Itraconazole (200 mg for 6 to 8 weeks) versus placebo, Outcome 2 Adverse effects. | ||||
| 2.1 Mild abdominal pain and nausea | 3 | 204 | Risk Ratio (M‐H, Random, 95% CI) | 2.36 [0.74, 7.47] |
| 2.2 Mild abnormal liver function | 3 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 3.08 [0.53, 17.98] |
| 2.3 Headache and dizziness | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 2.63 [0.16, 43.63] |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Analysis 22.3 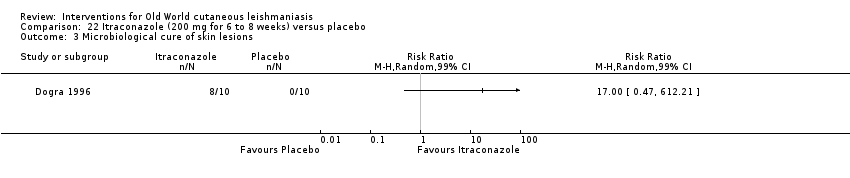 Comparison 22 Itraconazole (200 mg for 6 to 8 weeks) versus placebo, Outcome 3 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Analysis 23.1  Comparison 23 Itraconazole (200 mg for 6 to 8 weeks) versus no treatment, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects (headache and dizziness) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 23.2  Comparison 23 Itraconazole (200 mg for 6 to 8 weeks) versus no treatment, Outcome 2 Adverse effects (headache and dizziness). | ||||
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 23.3  Comparison 23 Itraconazole (200 mg for 6 to 8 weeks) versus no treatment, Outcome 3 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 24.1  Comparison 24 Fluconazole (200 mg for 6 weeks) versus placebo, Outcome 1 Lesions cured. | ||||
| 2 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 24.2 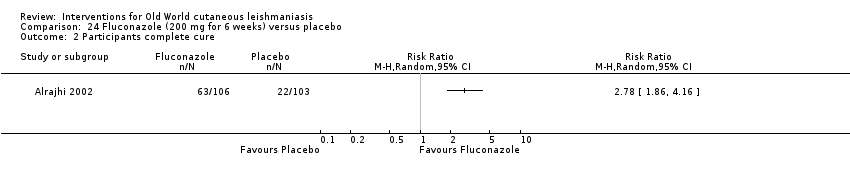 Comparison 24 Fluconazole (200 mg for 6 weeks) versus placebo, Outcome 2 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 25.1  Comparison 25 Fluconazole (400 mg/d for 6 weeks) versus fluconazole (200 mg/d for 6 weeks), Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 25.2 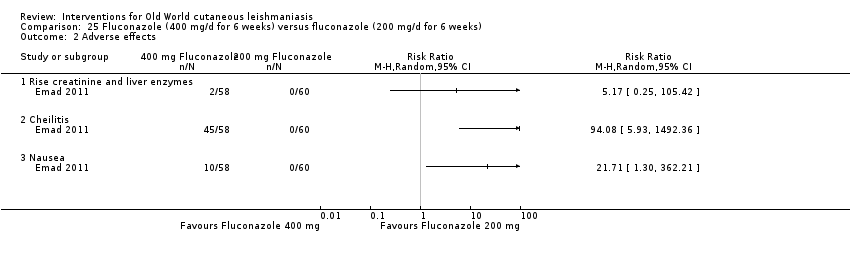 Comparison 25 Fluconazole (400 mg/d for 6 weeks) versus fluconazole (200 mg/d for 6 weeks), Outcome 2 Adverse effects. | ||||
| 2.1 Rise creatinine and liver enzymes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Cheilitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Nausea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete Cure Show forest plot | 2 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 24.08 [1.44, 403.43] |
| Analysis 26.1  Comparison 26 Oral dapsone (200 mg/d for 6 weeks) versus placebo, Outcome 1 Participants complete Cure. | ||||
| 2 Adverse effects Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 26.2  Comparison 26 Oral dapsone (200 mg/d for 6 weeks) versus placebo, Outcome 2 Adverse effects. | ||||
| 2.1 Nausea | 2 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 21.86 [3.04, 157.29] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 3.83 [1.71, 8.60] |
| Analysis 27.1  Comparison 27 Allopurinol (15 mg/kg/d for 3 weeks) + IMMA (20 mg/kg/d for 2 weeks) versus allopurinol (15 mg/kg/d for 3 weeks), Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 1.92 [1.08, 3.41] |
| Analysis 28.1  Comparison 28 Allopurinol (15mg/kg/d for 3 weeks)+ IMMA (20 mg/kg/d for 2 weeks) versus IMMA (20 mg/kg/d for 2 weeks), Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions Cured Show forest plot | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.35, 1.62] |
| Analysis 29.1  Comparison 29 Allopurinol (15 mg/kg/d for 3 weeks) versus IMMA (20 mg/kg/d for 2 weeks), Outcome 1 Lesions Cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 30.1  Comparison 30 Allopurinol (20 mg/kg/d for 3 weeks) + IMMA (30 mg/kg/d for 20 days) versus IMMA (60 mg/kg/d for 20 d), Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 30.2 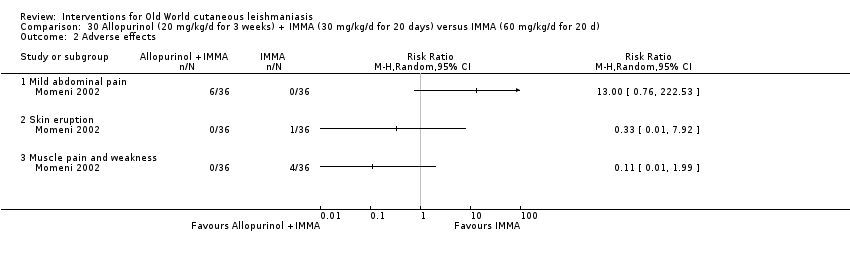 Comparison 30 Allopurinol (20 mg/kg/d for 3 weeks) + IMMA (30 mg/kg/d for 20 days) versus IMMA (60 mg/kg/d for 20 d), Outcome 2 Adverse effects. | ||||
| 2.1 Mild abdominal pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Skin eruption | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Muscle pain and weakness | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | 72 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.88, 1.41] |
| Analysis 30.3 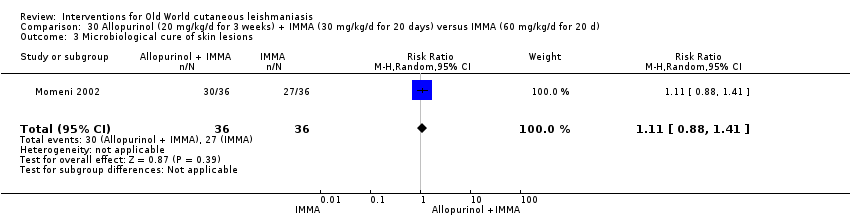 Comparison 30 Allopurinol (20 mg/kg/d for 3 weeks) + IMMA (30 mg/kg/d for 20 days) versus IMMA (60 mg/kg/d for 20 d), Outcome 3 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 31.1  Comparison 31 Allopurinol (20 mg/kg/d for 3 weeks)+ IMMA (10 mg/kg/d for 20 d) versus IMMA (20 mg/kg/d for 28 d), Outcome 1 Adverse effects. | ||||
| 1.1 Secondary infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Myalgia | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 ECG changes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Chest pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Pain injection site | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Abscess | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 32.1  Comparison 32 Allopurinol (20 mg/kg/d for 3 weeks) versus IVSSG (20 mg/kg/d for 15 d), Outcome 1 Participants complete cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 32.2 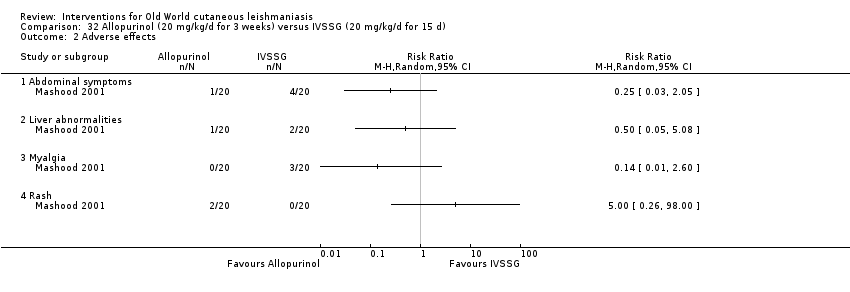 Comparison 32 Allopurinol (20 mg/kg/d for 3 weeks) versus IVSSG (20 mg/kg/d for 15 d), Outcome 2 Adverse effects. | ||||
| 2.1 Abdominal symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Liver abnormalities | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Myalgia | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Rash | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 33.1  Comparison 33 Oral rifampicin (10 mg/kg/d for 4 to 6 weeks) versus placebo, Outcome 1 Participants complete cure. | ||||
| 1.1 Evaluated 3 months after treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Evaluated after treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 33.2 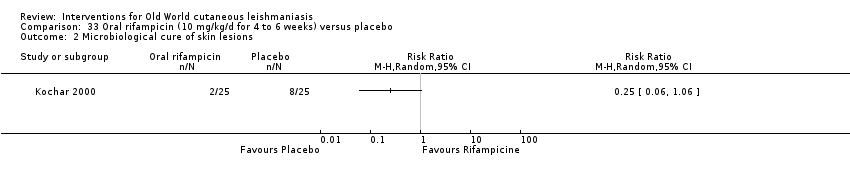 Comparison 33 Oral rifampicin (10 mg/kg/d for 4 to 6 weeks) versus placebo, Outcome 2 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 34.1 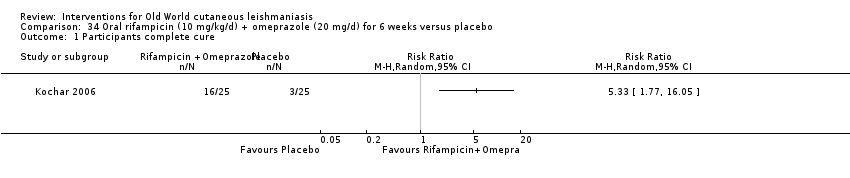 Comparison 34 Oral rifampicin (10 mg/kg/d) + omeprazole (20 mg/d) for 6 weeks versus placebo, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 35.1  Comparison 35 Azythromicin (500 mg/d for 5 d/month up to 4 months) versus IMMA (60 mg/kg/d for 20 d), Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 35.2  Comparison 35 Azythromicin (500 mg/d for 5 d/month up to 4 months) versus IMMA (60 mg/kg/d for 20 d), Outcome 2 Adverse effects. | ||||
| 2.1 Nausea and vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 36.1 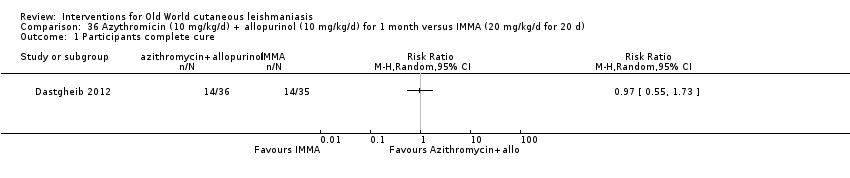 Comparison 36 Azythromicin (10 mg/kg/d) + allopurinol (10 mg/kg/d) for 1 month versus IMMA (20 mg/kg/d for 20 d), Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 36.2 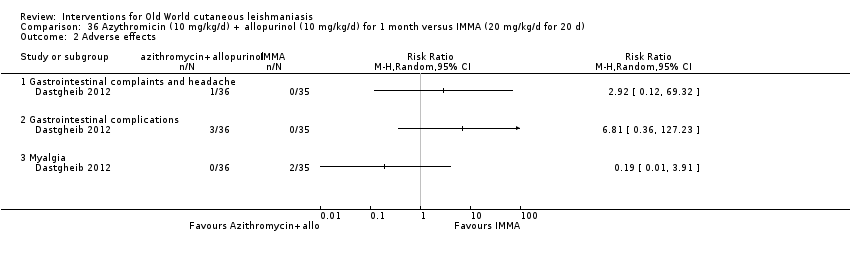 Comparison 36 Azythromicin (10 mg/kg/d) + allopurinol (10 mg/kg/d) for 1 month versus IMMA (20 mg/kg/d for 20 d), Outcome 2 Adverse effects. | ||||
| 2.1 Gastrointestinal complaints and headache | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Gastrointestinal complications | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Myalgia | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 37.1 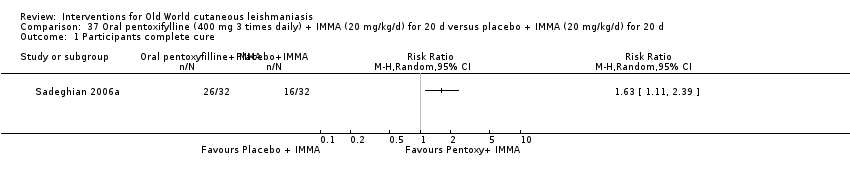 Comparison 37 Oral pentoxifylline (400 mg 3 times daily) + IMMA (20 mg/kg/d) for 20 d versus placebo + IMMA (20 mg/kg/d) for 20 d, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 37.2 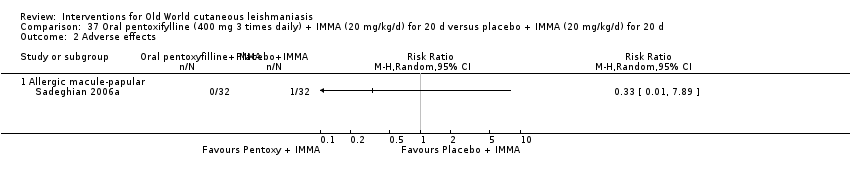 Comparison 37 Oral pentoxifylline (400 mg 3 times daily) + IMMA (20 mg/kg/d) for 20 d versus placebo + IMMA (20 mg/kg/d) for 20 d, Outcome 2 Adverse effects. | ||||
| 2.1 Allergic macule‐papular | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 38.1 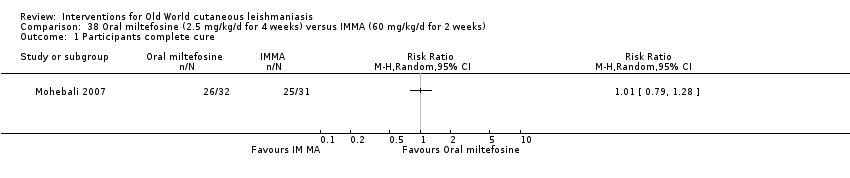 Comparison 38 Oral miltefosine (2.5 mg/kg/d for 4 weeks) versus IMMA (60 mg/kg/d for 2 weeks), Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 39.1  Comparison 39 Oral miltefosine (2.5 mg/kg/d for 4 weeks) versus IMMA (60 mg/kg/d for 2 weeks), Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 40.1  Comparison 40 Oral zinc sulphate 2.5 mg/kg/d for 45 days versus oral zinc sulphate 5 mg/kg/d for 45 d, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 40.2 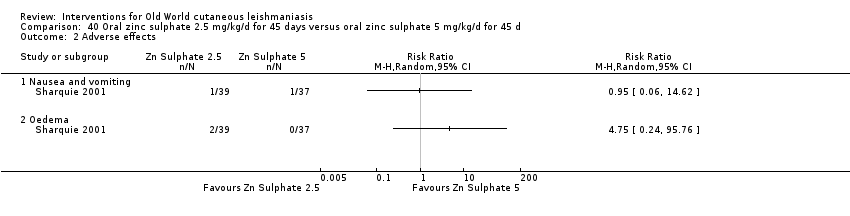 Comparison 40 Oral zinc sulphate 2.5 mg/kg/d for 45 days versus oral zinc sulphate 5 mg/kg/d for 45 d, Outcome 2 Adverse effects. | ||||
| 2.1 Nausea and vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 41.1 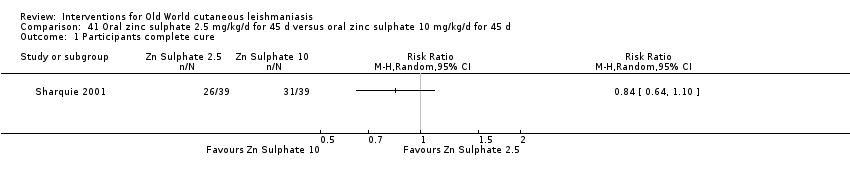 Comparison 41 Oral zinc sulphate 2.5 mg/kg/d for 45 d versus oral zinc sulphate 10 mg/kg/d for 45 d, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 41.2  Comparison 41 Oral zinc sulphate 2.5 mg/kg/d for 45 d versus oral zinc sulphate 10 mg/kg/d for 45 d, Outcome 2 Adverse effects. | ||||
| 2.1 Nausea and vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 42.1  Comparison 42 Oral zinc sulphate 5 mg/kg/d for 45 d versus oral zinc sulphate 10 mg/kg/d for 45 d, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 42.2  Comparison 42 Oral zinc sulphate 5 mg/kg/d for 45 d versus oral zinc sulphate 10 mg/kg/d for 45 d, Outcome 2 Adverse effects. | ||||
| 2.1 Nausea and vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 43.1  Comparison 43 Oral zinc sulphate (10 mg/kg/d for 45 d) versus IMMA (20 mg/kg/d for 20 d), Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 44.1 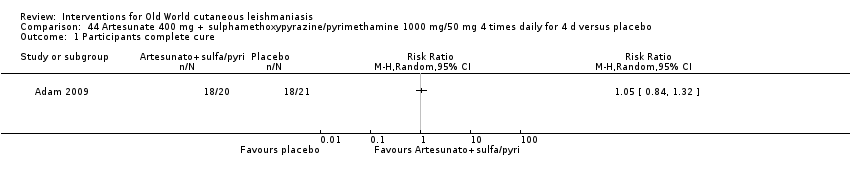 Comparison 44 Artesunate 400 mg + sulphamethoxypyrazine/pyrimethamine 1000 mg/50 mg 4 times daily for 4 d versus placebo, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 45.1  Comparison 45 Topical 2% miconazole (twice a day) versus topical 1% clotrimazole (twice a day) for 30 d, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 46.1  Comparison 46 Topical ketoconazole (twice a day) versus vehicle (twice a day) for 30 d, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure (ITT) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 47.1  Comparison 47 Topical amphotericin B (3 to 7 drops twice daily for 8 weeks) versus ILMA (max 2 mL) once a week for 8 weeks, Outcome 1 Participants complete cure (ITT). | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 47.2  Comparison 47 Topical amphotericin B (3 to 7 drops twice daily for 8 weeks) versus ILMA (max 2 mL) once a week for 8 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Hypersensitivity | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Mild pruritus | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Erithema and oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 48.1  Comparison 48 Paromomycin 15% + 12% MBCL (twice daily for 28 d) versus vehicle (twice daily for 28 d), Outcome 1 Lesions cured. | ||||
| 2 Scarring Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 48.2  Comparison 48 Paromomycin 15% + 12% MBCL (twice daily for 28 d) versus vehicle (twice daily for 28 d), Outcome 2 Scarring. | ||||
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 48.3  Comparison 48 Paromomycin 15% + 12% MBCL (twice daily for 28 d) versus vehicle (twice daily for 28 d), Outcome 3 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.25, 2.06] |
| Analysis 49.1  Comparison 49 Paromomycin (twice daily for 30 d) versus vehicle (twice daily for 30 d), Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 2 | 383 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.86, 1.17] |
| Analysis 50.1 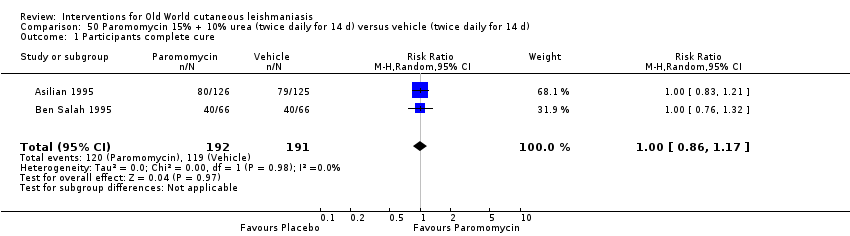 Comparison 50 Paromomycin 15% + 10% urea (twice daily for 14 d) versus vehicle (twice daily for 14 d), Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 50.2  Comparison 50 Paromomycin 15% + 10% urea (twice daily for 14 d) versus vehicle (twice daily for 14 d), Outcome 2 Adverse effects. | ||||
| 2.1 Skin/local reaction | 3 | 463 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.45, 1.93] |
| 3 Microbiological cure of skin lesions Show forest plot | 2 | 383 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.88, 1.20] |
| Analysis 50.3  Comparison 50 Paromomycin 15% + 10% urea (twice daily for 14 d) versus vehicle (twice daily for 14 d), Outcome 3 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 51.1  Comparison 51 Paromomycin 15% (daily for 20 d) versus vehicle, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 52.1  Comparison 52 Paromomycin 15% + gentamicin 0.5% (daily for 20 d) versus vehicle, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 53.1  Comparison 53 Paromomycin 15% + gentamicin 0.5% (daily for 20 d) versus paromomycin 15% alone (daily for 20 d), Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 54.1  Comparison 54 Paromomycin 15% + 10% urea (twice daily for 45 d) versus ILMA (weekly for up to 3 months), Outcome 1 Participants complete cure. | ||||
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 54.2 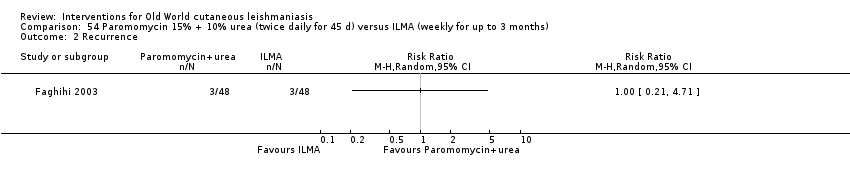 Comparison 54 Paromomycin 15% + 10% urea (twice daily for 45 d) versus ILMA (weekly for up to 3 months), Outcome 2 Recurrence. | ||||
| 3 Scarring Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 54.3  Comparison 54 Paromomycin 15% + 10% urea (twice daily for 45 d) versus ILMA (weekly for up to 3 months), Outcome 3 Scarring. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 55.1  Comparison 55 Paromomycin 15% + 10% urea (twice daily for 20 d) versus ILMA (weekly for up to 20 d), Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 55.2  Comparison 55 Paromomycin 15% + 10% urea (twice daily for 20 d) versus ILMA (weekly for up to 20 d), Outcome 2 Adverse effects. | ||||
| 2.1 Cutaneous reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 56.1 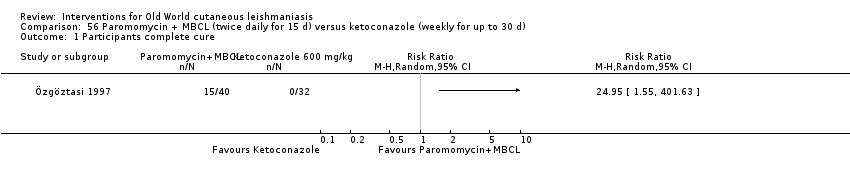 Comparison 56 Paromomycin + MBCL (twice daily for 15 d) versus ketoconazole (weekly for up to 30 d), Outcome 1 Participants complete cure. | ||||
| 2 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 56.2  Comparison 56 Paromomycin + MBCL (twice daily for 15 d) versus ketoconazole (weekly for up to 30 d), Outcome 2 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 57.1  Comparison 57 Paromomycin (15% + 12% MBCL twice daily for 28 days) versus PDT (weekly for 4 weeks), Outcome 1 Lesions cured. | ||||
| 2 Scarring Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Analysis 57.2 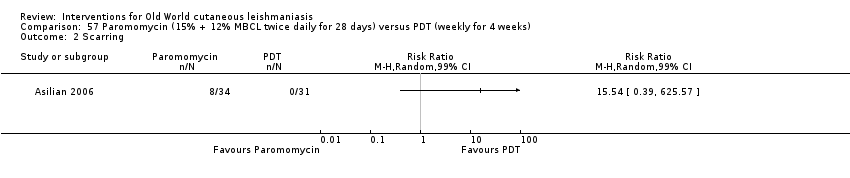 Comparison 57 Paromomycin (15% + 12% MBCL twice daily for 28 days) versus PDT (weekly for 4 weeks), Outcome 2 Scarring. | ||||
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 57.3  Comparison 57 Paromomycin (15% + 12% MBCL twice daily for 28 days) versus PDT (weekly for 4 weeks), Outcome 3 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 58.1 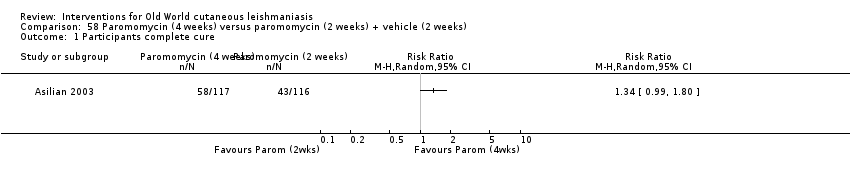 Comparison 58 Paromomycin (4 weeks) versus paromomycin (2 weeks) + vehicle (2 weeks), Outcome 1 Participants complete cure. | ||||
| 2 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 58.2  Comparison 58 Paromomycin (4 weeks) versus paromomycin (2 weeks) + vehicle (2 weeks), Outcome 2 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 59.1 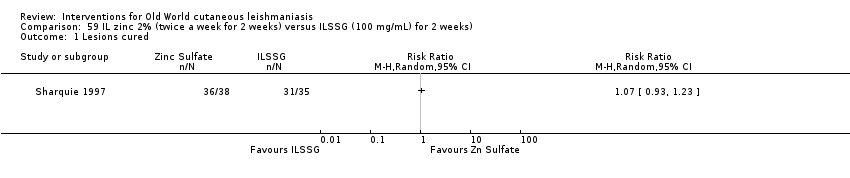 Comparison 59 IL zinc 2% (twice a week for 2 weeks) versus ILSSG (100 mg/mL) for 2 weeks), Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 60.1 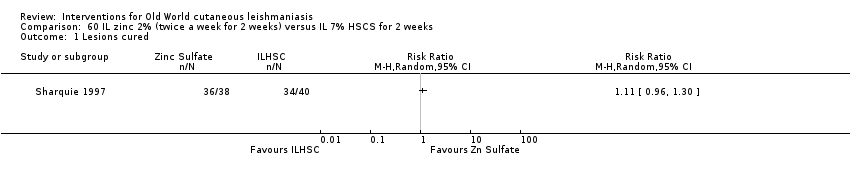 Comparison 60 IL zinc 2% (twice a week for 2 weeks) versus IL 7% HSCS for 2 weeks, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 61.1 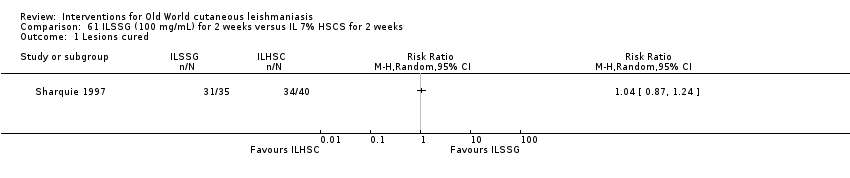 Comparison 61 ILSSG (100 mg/mL) for 2 weeks versus IL 7% HSCS for 2 weeks, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 62.1  Comparison 62 IL zinc 2% (weekly for up to 6 weeks) versus ILMA (max 2 mL weekly for up to 6 weeks), Outcome 1 Lesions cured. | ||||
| 2 Participants complete cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 62.2  Comparison 62 IL zinc 2% (weekly for up to 6 weeks) versus ILMA (max 2 mL weekly for up to 6 weeks), Outcome 2 Participants complete cured. | ||||
| 3 Adverse effects Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 62.3  Comparison 62 IL zinc 2% (weekly for up to 6 weeks) versus ILMA (max 2 mL weekly for up to 6 weeks), Outcome 3 Adverse effects. | ||||
| 3.1 Pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Burning | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Itching | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Inflammation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.5 Pruritus and erythema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.6 Severe pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 63.1 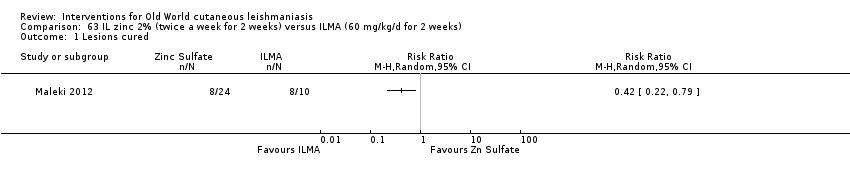 Comparison 63 IL zinc 2% (twice a week for 2 weeks) versus ILMA (60 mg/kg/d for 2 weeks), Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 63.2  Comparison 63 IL zinc 2% (twice a week for 2 weeks) versus ILMA (60 mg/kg/d for 2 weeks), Outcome 2 Adverse effects. | ||||
| 2.1 Inflammation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 64.1 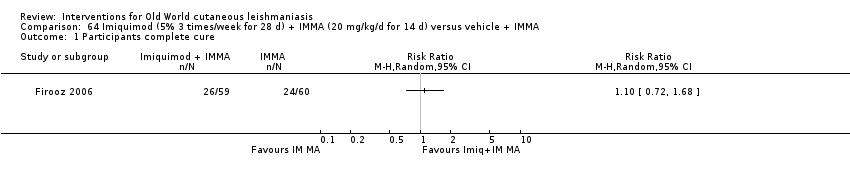 Comparison 64 Imiquimod (5% 3 times/week for 28 d) + IMMA (20 mg/kg/d for 14 d) versus vehicle + IMMA, Outcome 1 Participants complete cure. | ||||
| 2 Participants with treated lesions that recur Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 64.2  Comparison 64 Imiquimod (5% 3 times/week for 28 d) + IMMA (20 mg/kg/d for 14 d) versus vehicle + IMMA, Outcome 2 Participants with treated lesions that recur. | ||||
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 64.3  Comparison 64 Imiquimod (5% 3 times/week for 28 d) + IMMA (20 mg/kg/d for 14 d) versus vehicle + IMMA, Outcome 3 Adverse effects. | ||||
| 3.1 Itch and burning | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 65.1  Comparison 65 IL 7% HSCS (0.2 mL to 7 mL per lesion) versus ILSSG (max 2 mL) max 5 injections, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 66.1 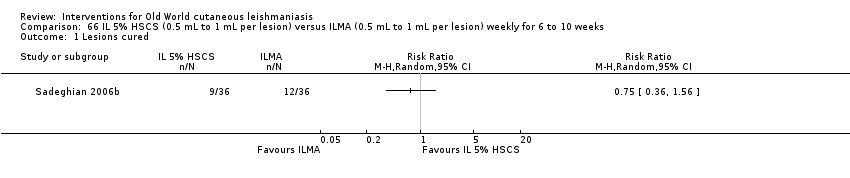 Comparison 66 IL 5% HSCS (0.5 mL to 1 mL per lesion) versus ILMA (0.5 mL to 1 mL per lesion) weekly for 6 to 10 weeks, Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 66.2  Comparison 66 IL 5% HSCS (0.5 mL to 1 mL per lesion) versus ILMA (0.5 mL to 1 mL per lesion) weekly for 6 to 10 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Sporotrichotic dissemination | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 67.1 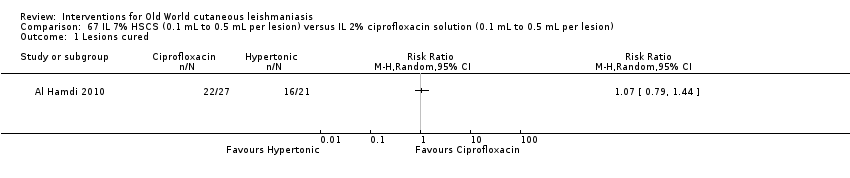 Comparison 67 IL 7% HSCS (0.1 mL to 0.5 mL per lesion) versus IL 2% ciprofloxacin solution (0.1 mL to 0.5 mL per lesion), Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 68.1  Comparison 68 IL 15% HSCS (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 1 Lesions cured. | ||||
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 68.2  Comparison 68 IL 15% HSCS (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 2 Recurrence. | ||||
| 3 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 68.3  Comparison 68 IL 15% HSCS (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 3 Speed of healing (weeks). | ||||
| 4 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 68.4  Comparison 68 IL 15% HSCS (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 4 Adverse effects. | ||||
| 4.1 Ulceration and necrosis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 69.1  Comparison 69 ILSSG (0.2 mL to 4 mL per lesion) max 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 1 Lesions cured. | ||||
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 69.2 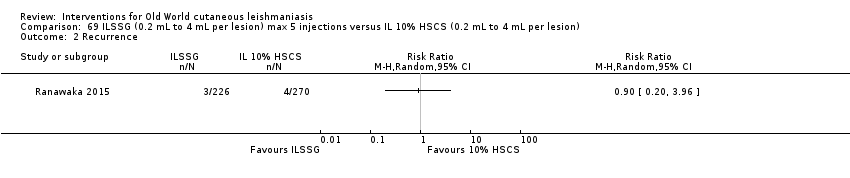 Comparison 69 ILSSG (0.2 mL to 4 mL per lesion) max 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 2 Recurrence. | ||||
| 3 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 69.3 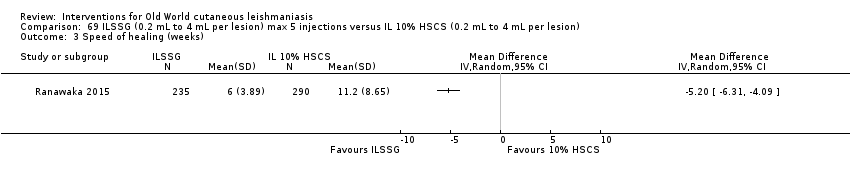 Comparison 69 ILSSG (0.2 mL to 4 mL per lesion) max 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 3 Speed of healing (weeks). | ||||
| 4 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 69.4  Comparison 69 ILSSG (0.2 mL to 4 mL per lesion) max 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 4 Adverse effects. | ||||
| 4.1 Ulceration and necrosis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 70.1 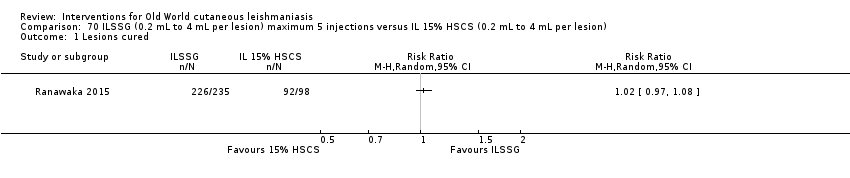 Comparison 70 ILSSG (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 15% HSCS (0.2 mL to 4 mL per lesion), Outcome 1 Lesions cured. | ||||
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Analysis 70.2 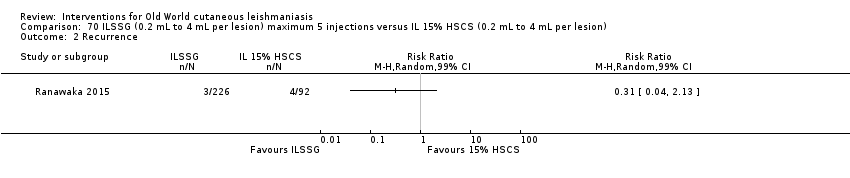 Comparison 70 ILSSG (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 15% HSCS (0.2 mL to 4 mL per lesion), Outcome 2 Recurrence. | ||||
| 3 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 70.3  Comparison 70 ILSSG (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 15% HSCS (0.2 mL to 4 mL per lesion), Outcome 3 Speed of healing (weeks). | ||||
| 4 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 70.4 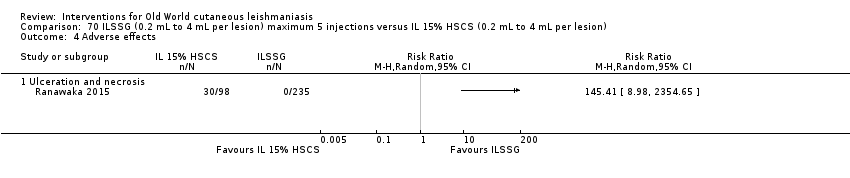 Comparison 70 ILSSG (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 15% HSCS (0.2 mL to 4 mL per lesion), Outcome 4 Adverse effects. | ||||
| 4.1 Ulceration and necrosis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 71.1 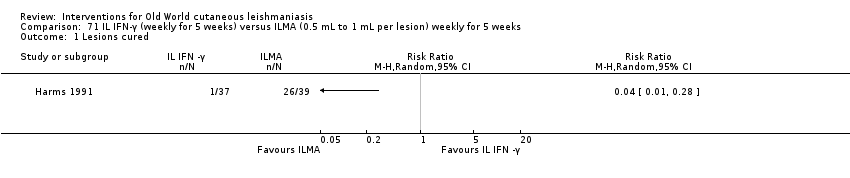 Comparison 71 IL IFN‐γ (weekly for 5 weeks) versus ILMA (0.5 mL to 1 mL per lesion) weekly for 5 weeks, Outcome 1 Lesions cured. | ||||
| 2 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 71.2 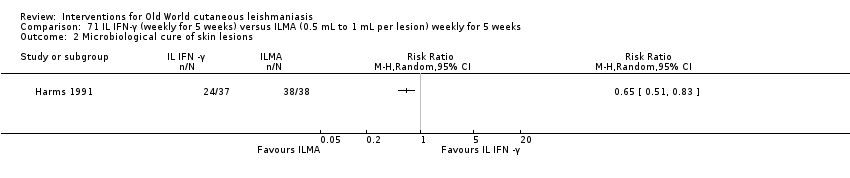 Comparison 71 IL IFN‐γ (weekly for 5 weeks) versus ILMA (0.5 mL to 1 mL per lesion) weekly for 5 weeks, Outcome 2 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 72.1  Comparison 72 WR279,396 (twice a day for 20 d) versus vehicle (twice a day for 20 d), Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 72.2  Comparison 72 WR279,396 (twice a day for 20 d) versus vehicle (twice a day for 20 d), Outcome 2 Adverse effects. | ||||
| 2.1 Erythema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Mild pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Hearing acuity problems | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 73.1  Comparison 73 IL metronidazole (2.5 mg to 10 mg each lesion) versus ILMA (150 mg to 600 mg each lesion) for up to 8 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 73.2  Comparison 73 IL metronidazole (2.5 mg to 10 mg each lesion) versus ILMA (150 mg to 600 mg each lesion) for up to 8 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Local inflammatory reactions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 74.1  Comparison 74 Topical miltefosine 6% (once daily) versus ILMA (twice a week) for up to 28 d, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 75.1  Comparison 75 Dapsone gel 5% (twice a day) + ILMA (weekly) versus cryotherapy (every 2 weeks) + IMMA (weekly) for up to 16 weeks, Outcome 1 Lesions cured. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 76.1 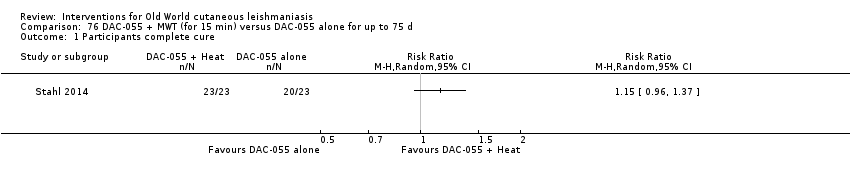 Comparison 76 DAC‐055 + MWT (for 15 min) versus DAC‐055 alone for up to 75 d, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 76.2 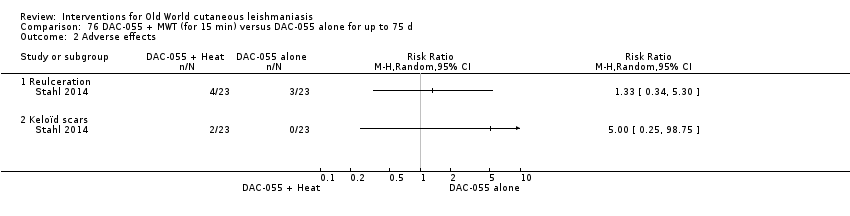 Comparison 76 DAC‐055 + MWT (for 15 min) versus DAC‐055 alone for up to 75 d, Outcome 2 Adverse effects. | ||||
| 2.1 Reulceration | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Keloïd scars | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 77.1 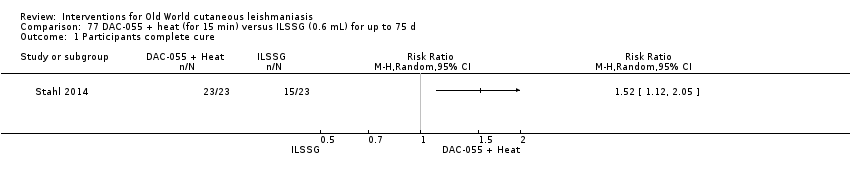 Comparison 77 DAC‐055 + heat (for 15 min) versus ILSSG (0.6 mL) for up to 75 d, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 77.2 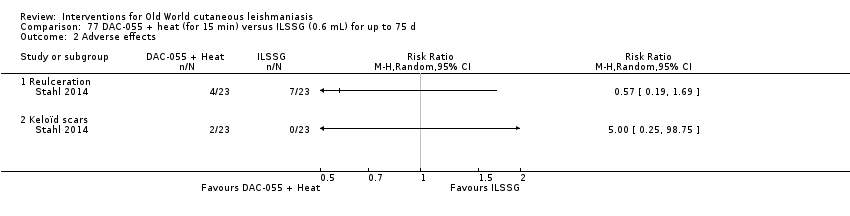 Comparison 77 DAC‐055 + heat (for 15 min) versus ILSSG (0.6 mL) for up to 75 d, Outcome 2 Adverse effects. | ||||
| 2.1 Reulceration | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Keloïd scars | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 78.1  Comparison 78 DAC‐055 alone (for 15 min) versus ILSSG (0.6 mL) for up to 75 d, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 78.2 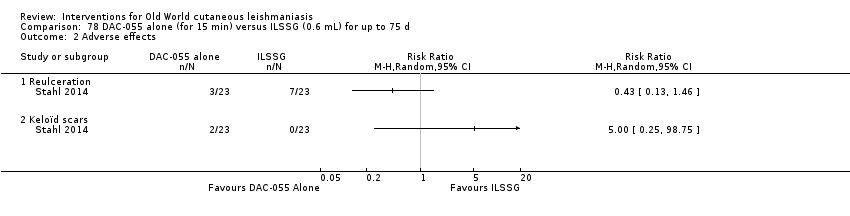 Comparison 78 DAC‐055 alone (for 15 min) versus ILSSG (0.6 mL) for up to 75 d, Outcome 2 Adverse effects. | ||||
| 2.1 Reulceration | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Keloïd scars | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 79.1  Comparison 79 Thio‐Ben (1 mL to 2 mL daily) + cryotherapy (fortnightly) versus ILMA (0.5 mL to 2 mL per lesions) weekly + cryotherapy (fortnightly) for up to 12 weeks, Outcome 1 Lesions cured. | ||||
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 79.2 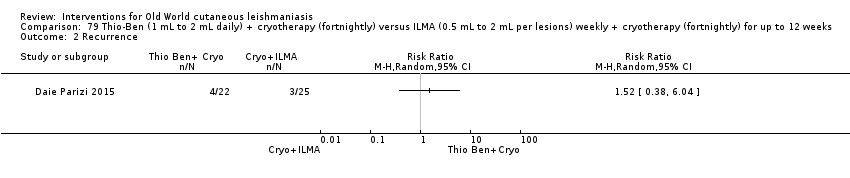 Comparison 79 Thio‐Ben (1 mL to 2 mL daily) + cryotherapy (fortnightly) versus ILMA (0.5 mL to 2 mL per lesions) weekly + cryotherapy (fortnightly) for up to 12 weeks, Outcome 2 Recurrence. | ||||
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 79.3 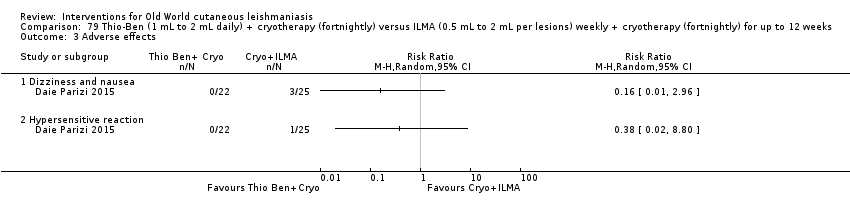 Comparison 79 Thio‐Ben (1 mL to 2 mL daily) + cryotherapy (fortnightly) versus ILMA (0.5 mL to 2 mL per lesions) weekly + cryotherapy (fortnightly) for up to 12 weeks, Outcome 3 Adverse effects. | ||||
| 3.1 Dizziness and nausea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Hypersensitive reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | 433 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.53, 1.55] |
| Analysis 80.1 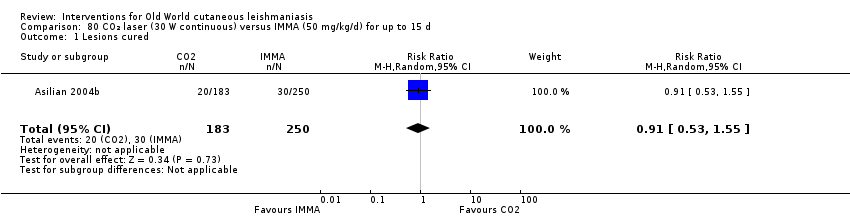 Comparison 80 CO₂ laser (30 W continuous) versus IMMA (50 mg/kg/d) for up to 15 d, Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 80.2  Comparison 80 CO₂ laser (30 W continuous) versus IMMA (50 mg/kg/d) for up to 15 d, Outcome 2 Adverse effects. | ||||
| 2.1 Hyperpigmentation and redness | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Hypertrophic scarring | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Systemic symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 81.1  Comparison 81 CO₂ laser (30 W continuous) versus cryotherapy (fortnightly) + ILMA (weekly) for up to 12 weeks, Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 81.2 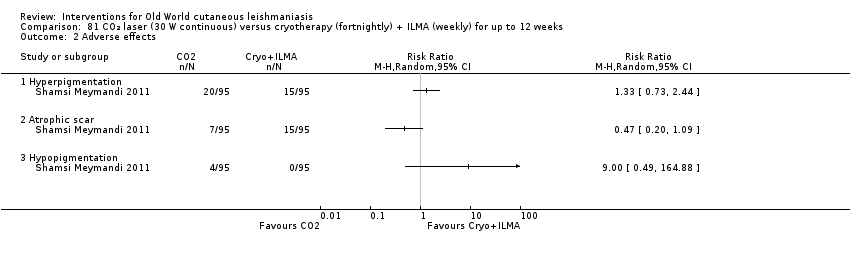 Comparison 81 CO₂ laser (30 W continuous) versus cryotherapy (fortnightly) + ILMA (weekly) for up to 12 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Hyperpigmentation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Atrophic scar | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Hypopigmentation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Partcipants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 82.1 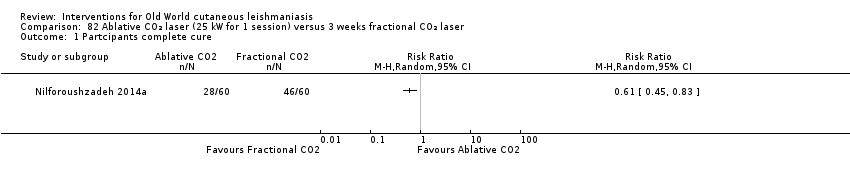 Comparison 82 Ablative CO₂ laser (25 kW for 1 session) versus 3 weeks fractional CO₂ laser, Outcome 1 Partcipants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 82.2 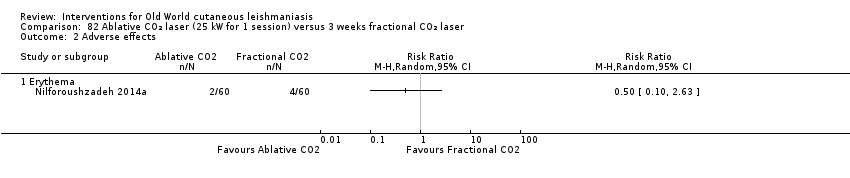 Comparison 82 Ablative CO₂ laser (25 kW for 1 session) versus 3 weeks fractional CO₂ laser, Outcome 2 Adverse effects. | ||||
| 2.1 Erythema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 83.1  Comparison 83 TCA (50% wt/vol) fortnightly up to 3 times versus ILMA alone (weekly for up to 6 weeks), Outcome 1 Participants complete cure. | ||||
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 83.2 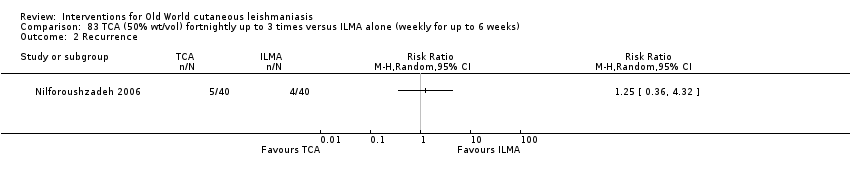 Comparison 83 TCA (50% wt/vol) fortnightly up to 3 times versus ILMA alone (weekly for up to 6 weeks), Outcome 2 Recurrence. | ||||
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 83.3  Comparison 83 TCA (50% wt/vol) fortnightly up to 3 times versus ILMA alone (weekly for up to 6 weeks), Outcome 3 Adverse effects. | ||||
| 3.1 Mild erythema and itch | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Microbiological cure of skin lesions Show forest plot | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.74, 1.26] |
| Analysis 83.4  Comparison 83 TCA (50% wt/vol) fortnightly up to 3 times versus ILMA alone (weekly for up to 6 weeks), Outcome 4 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 84.1 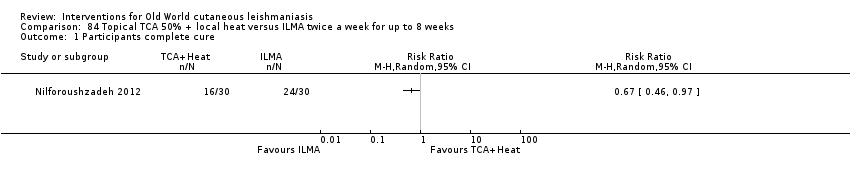 Comparison 84 Topical TCA 50% + local heat versus ILMA twice a week for up to 8 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Analysis 84.2  Comparison 84 Topical TCA 50% + local heat versus ILMA twice a week for up to 8 weeks, Outcome 2 Lesions cured. | ||||
| 2.1 Males | 1 | Risk Ratio (M‐H, Random, 99% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Females | 1 | Risk Ratio (M‐H, Random, 99% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 85.1  Comparison 85 TCA + ILMA (weekly for up to 8 weeks) versus ILMA alone (twice a week for up to 8 weeks), Outcome 1 Participants complete cure. | ||||
| 2 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 85.2 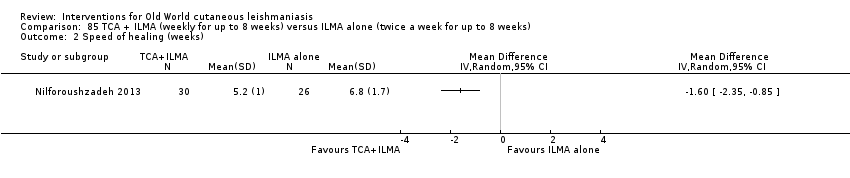 Comparison 85 TCA + ILMA (weekly for up to 8 weeks) versus ILMA alone (twice a week for up to 8 weeks), Outcome 2 Speed of healing (weeks). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 86.1 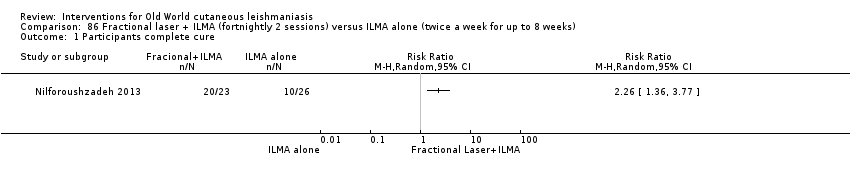 Comparison 86 Fractional laser + ILMA (fortnightly 2 sessions) versus ILMA alone (twice a week for up to 8 weeks), Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 87.1 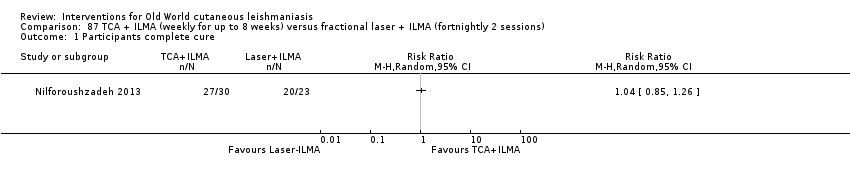 Comparison 87 TCA + ILMA (weekly for up to 8 weeks) versus fractional laser + ILMA (fortnightly 2 sessions), Outcome 1 Participants complete cure. | ||||
| 2 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 87.2 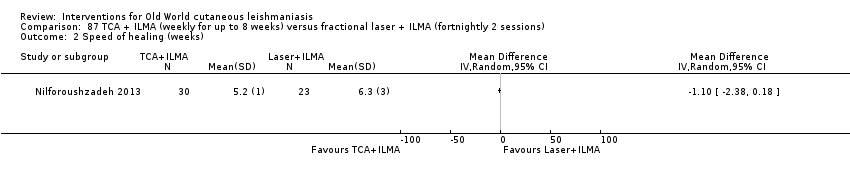 Comparison 87 TCA + ILMA (weekly for up to 8 weeks) versus fractional laser + ILMA (fortnightly 2 sessions), Outcome 2 Speed of healing (weeks). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 88.1  Comparison 88 TCA fortnightly up to 8 weeks + ILMA (twice a week) versus ILMA alone (weekly for up to 8 weeks), Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 89.1 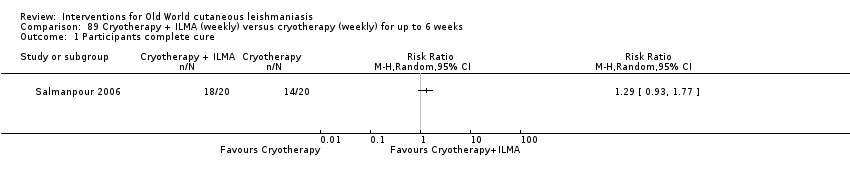 Comparison 89 Cryotherapy + ILMA (weekly) versus cryotherapy (weekly) for up to 6 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 89.2  Comparison 89 Cryotherapy + ILMA (weekly) versus cryotherapy (weekly) for up to 6 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Erythema and oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 90.1  Comparison 90 Cryotherapy + ILMA (weekly) versus ILMA (weekly) for up to 6 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 90.2 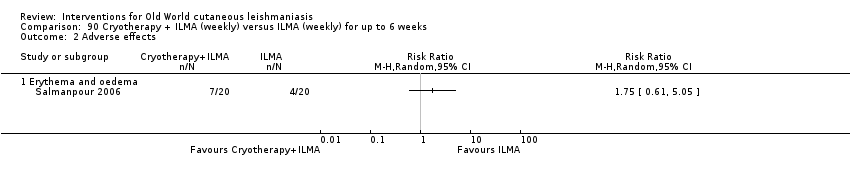 Comparison 90 Cryotherapy + ILMA (weekly) versus ILMA (weekly) for up to 6 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Erythema and oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 91.1 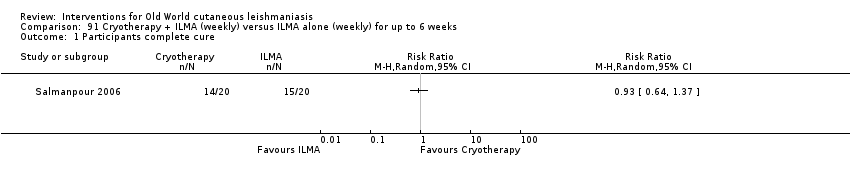 Comparison 91 Cryotherapy + ILMA (weekly) versus ILMA alone (weekly) for up to 6 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 91.2  Comparison 91 Cryotherapy + ILMA (weekly) versus ILMA alone (weekly) for up to 6 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Erythema and oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 92.1 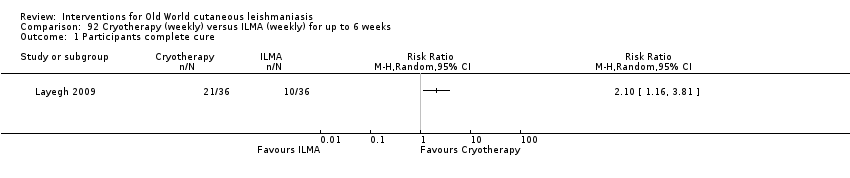 Comparison 92 Cryotherapy (weekly) versus ILMA (weekly) for up to 6 weeks, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 93.1 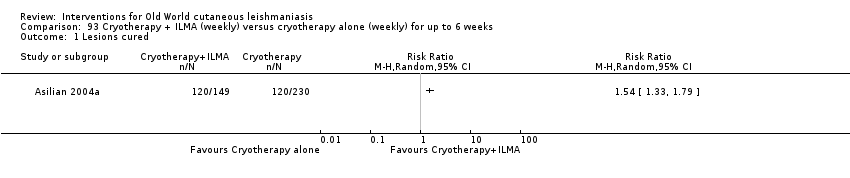 Comparison 93 Cryotherapy + ILMA (weekly) versus cryotherapy alone (weekly) for up to 6 weeks, Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 93.2  Comparison 93 Cryotherapy + ILMA (weekly) versus cryotherapy alone (weekly) for up to 6 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Hypopigmentation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 94.1 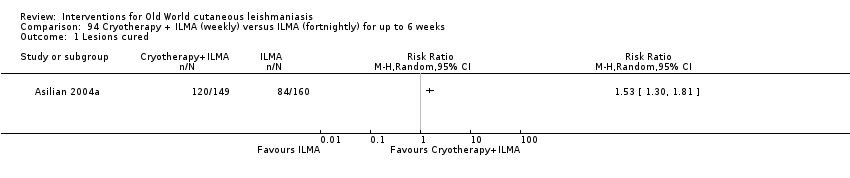 Comparison 94 Cryotherapy + ILMA (weekly) versus ILMA (fortnightly) for up to 6 weeks, Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 94.2  Comparison 94 Cryotherapy + ILMA (weekly) versus ILMA (fortnightly) for up to 6 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Hypopigmentation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 95.1 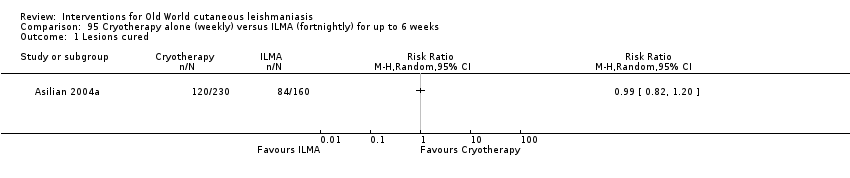 Comparison 95 Cryotherapy alone (weekly) versus ILMA (fortnightly) for up to 6 weeks, Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 14.64 [0.86, 247.99] |
| Analysis 95.2  Comparison 95 Cryotherapy alone (weekly) versus ILMA (fortnightly) for up to 6 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Hypopigmentation | 1 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 14.64 [0.86, 247.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 96.1 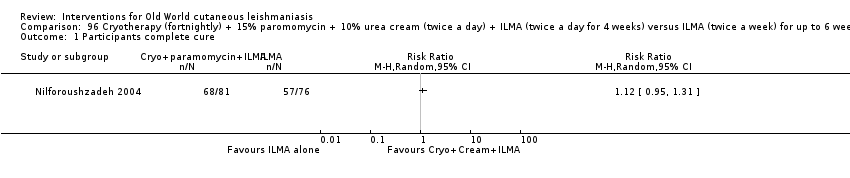 Comparison 96 Cryotherapy (fortnightly) + 15% paromomycin + 10% urea cream (twice a day) + ILMA (twice a day for 4 weeks) versus ILMA (twice a week) for up to 6 weeks, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 97.1 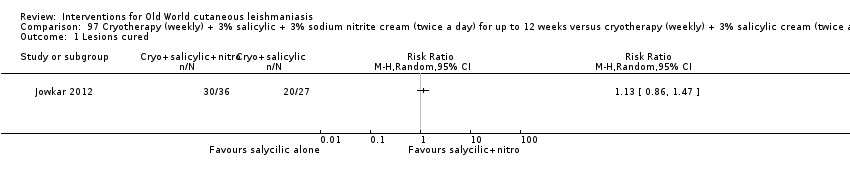 Comparison 97 Cryotherapy (weekly) + 3% salicylic + 3% sodium nitrite cream (twice a day) for up to 12 weeks versus cryotherapy (weekly) + 3% salicylic cream (twice a day), Outcome 1 Lesions cured. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 97.2  Comparison 97 Cryotherapy (weekly) + 3% salicylic + 3% sodium nitrite cream (twice a day) for up to 12 weeks versus cryotherapy (weekly) + 3% salicylic cream (twice a day), Outcome 2 Adverse effects. | ||||
| 2.1 Mild skin symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 98.1  Comparison 98 Radiofrequency waves versus ILMA (1 mL to 7 mL per lesion) weekly for 4 weeks, Outcome 1 Lesions cured. | ||||
| 2 Participants complete cure Show forest plot | 2 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.97, 1.55] |
| Analysis 98.2 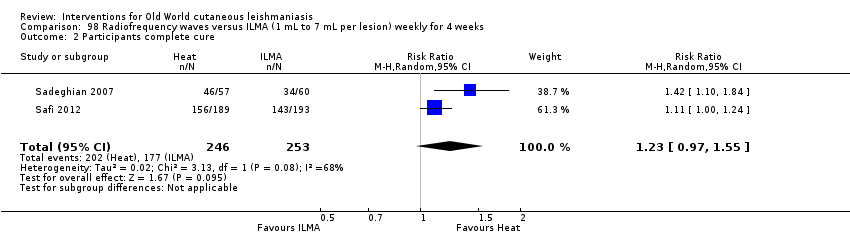 Comparison 98 Radiofrequency waves versus ILMA (1 mL to 7 mL per lesion) weekly for 4 weeks, Outcome 2 Participants complete cure. | ||||
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 98.3  Comparison 98 Radiofrequency waves versus ILMA (1 mL to 7 mL per lesion) weekly for 4 weeks, Outcome 3 Adverse effects. | ||||
| 3.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 99.1  Comparison 99 Radiofrequency waves (50 uCTM applied for 30 s) versus ILSSG (10 days of 20 mg/kg/d), Outcome 1 Lesions cured. | ||||
| 2 Adverse effects (serious) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 99.2  Comparison 99 Radiofrequency waves (50 uCTM applied for 30 s) versus ILSSG (10 days of 20 mg/kg/d), Outcome 2 Adverse effects (serious). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 100.1  Comparison 100 Radiofrequency waves (1 treatment of > 1 consecutive application at 50ºC for 30 s) versus IMSSG (20 mg/kg/d for 3 weeks), Outcome 1 Participants complete cure. | ||||
| 2 Adverse event (secondary infection) Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Analysis 100.2  Comparison 100 Radiofrequency waves (1 treatment of > 1 consecutive application at 50ºC for 30 s) versus IMSSG (20 mg/kg/d for 3 weeks), Outcome 2 Adverse event (secondary infection). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 101.1 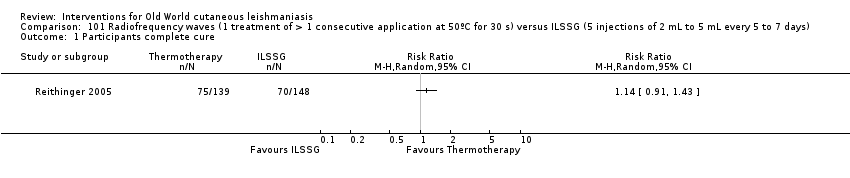 Comparison 101 Radiofrequency waves (1 treatment of > 1 consecutive application at 50ºC for 30 s) versus ILSSG (5 injections of 2 mL to 5 mL every 5 to 7 days), Outcome 1 Participants complete cure. | ||||
| 2 Adverse event (secondary infection) Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Analysis 101.2 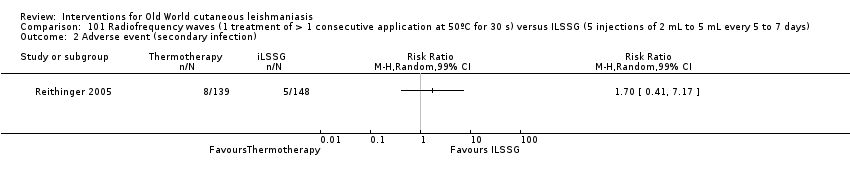 Comparison 101 Radiofrequency waves (1 treatment of > 1 consecutive application at 50ºC for 30 s) versus ILSSG (5 injections of 2 mL to 5 mL every 5 to 7 days), Outcome 2 Adverse event (secondary infection). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 102.1 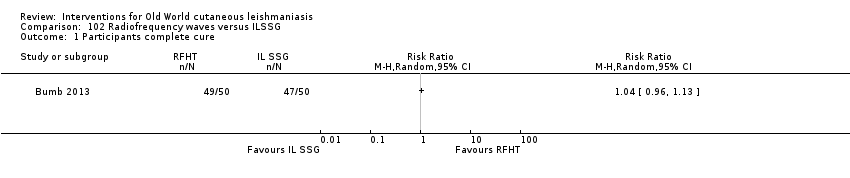 Comparison 102 Radiofrequency waves versus ILSSG, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 103.1 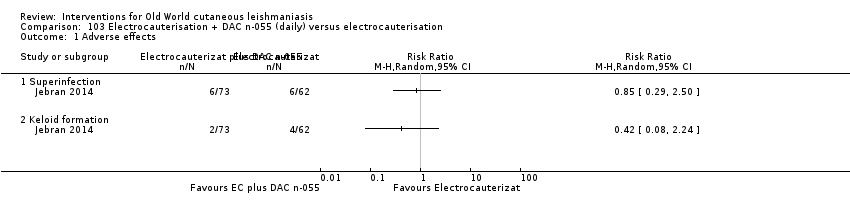 Comparison 103 Electrocauterisation + DAC n‐055 (daily) versus electrocauterisation, Outcome 1 Adverse effects. | ||||
| 1.1 Superinfection | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Keloid formation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 104.1  Comparison 104 PDT (weekly for 4 weeks) versus placebo (twice a day for 4 weeks), Outcome 1 Lesions cured. | ||||
| 2 Scarring Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 104.2  Comparison 104 PDT (weekly for 4 weeks) versus placebo (twice a day for 4 weeks), Outcome 2 Scarring. | ||||
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 104.3  Comparison 104 PDT (weekly for 4 weeks) versus placebo (twice a day for 4 weeks), Outcome 3 Microbiological cure of skin lesions. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 105.1 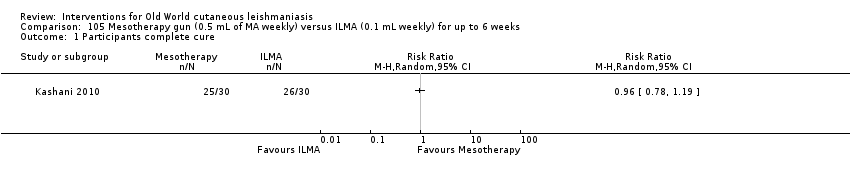 Comparison 105 Mesotherapy gun (0.5 mL of MA weekly) versus ILMA (0.1 mL weekly) for up to 6 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 105.2 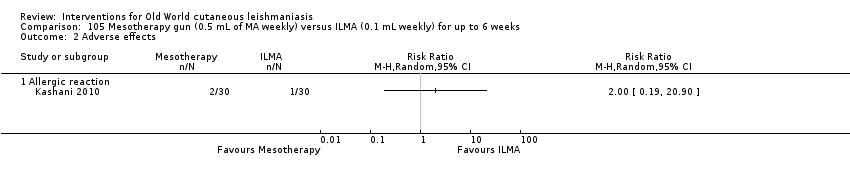 Comparison 105 Mesotherapy gun (0.5 mL of MA weekly) versus ILMA (0.1 mL weekly) for up to 6 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Development of cell‐mediated immunity Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 105.3 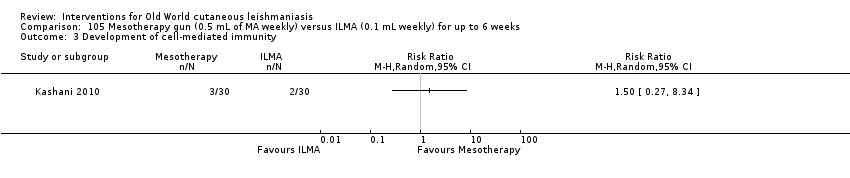 Comparison 105 Mesotherapy gun (0.5 mL of MA weekly) versus ILMA (0.1 mL weekly) for up to 6 weeks, Outcome 3 Development of cell‐mediated immunity. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 106.1 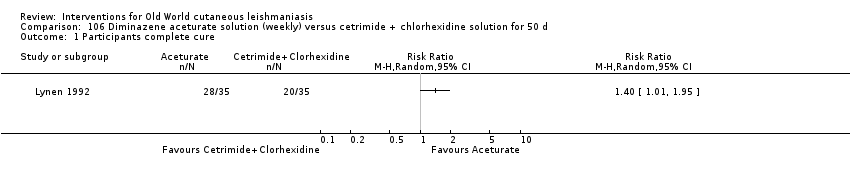 Comparison 106 Diminazene aceturate solution (weekly) versus cetrimide + chlorhexidine solution for 50 d, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 107.1  Comparison 107 Topical garlic (twice a day) versus vehicle for 3 weeks, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 108.1 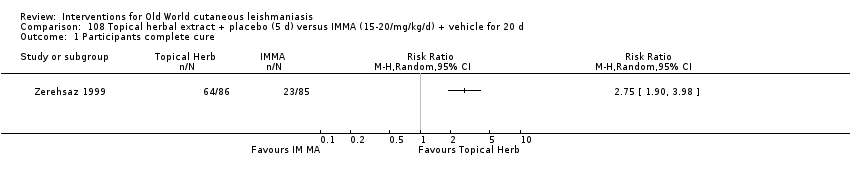 Comparison 108 Topical herbal extract + placebo (5 d) versus IMMA (15‐20/mg/kg/d) + vehicle for 20 d, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 109.1 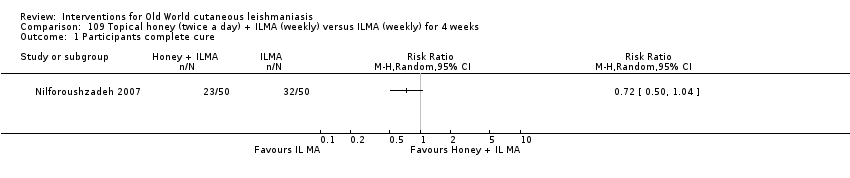 Comparison 109 Topical honey (twice a day) + ILMA (weekly) versus ILMA (weekly) for 4 weeks, Outcome 1 Participants complete cure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 110.1  Comparison 110 Cassia fistula (topical gel) + ILMA (0.5 mL to 2 mL), twice a week versus ILMA (0.5 mL to 2 mL), twice a week + vehicle, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 110.2 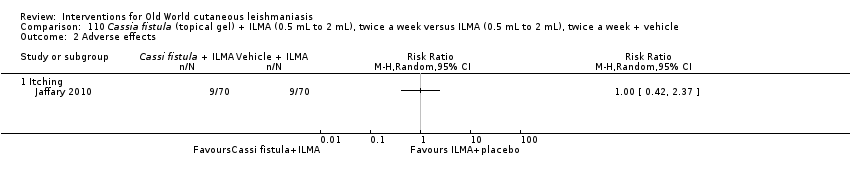 Comparison 110 Cassia fistula (topical gel) + ILMA (0.5 mL to 2 mL), twice a week versus ILMA (0.5 mL to 2 mL), twice a week + vehicle, Outcome 2 Adverse effects. | ||||
| 2.1 Itching | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 111.1 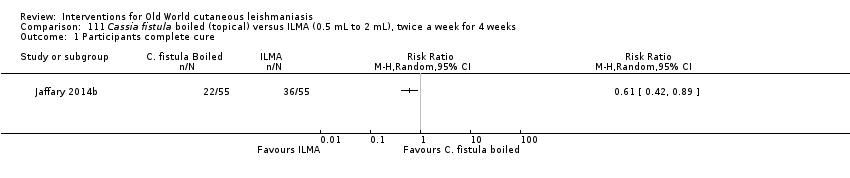 Comparison 111 Cassia fistula boiled (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 111.2 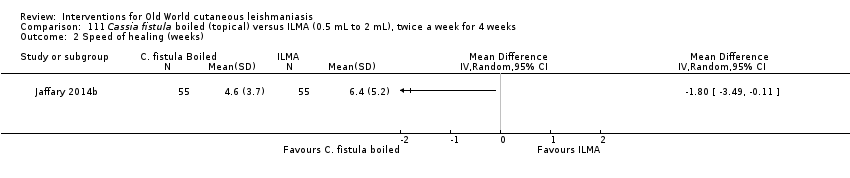 Comparison 111 Cassia fistula boiled (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 2 Speed of healing (weeks). | ||||
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 111.3 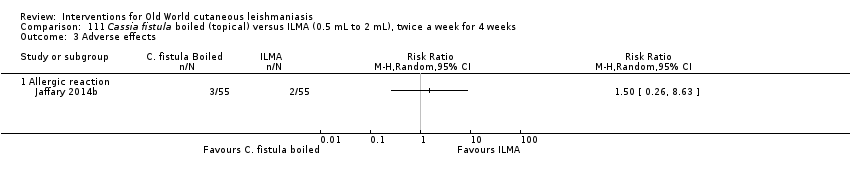 Comparison 111 Cassia fistula boiled (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 3 Adverse effects. | ||||
| 3.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 112.1 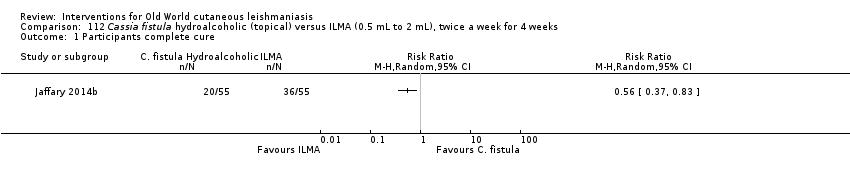 Comparison 112 Cassia fistula hydroalcoholic (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 112.2  Comparison 112 Cassia fistula hydroalcoholic (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 2 Speed of healing (weeks). | ||||
| 3 Adverse reaction Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 112.3 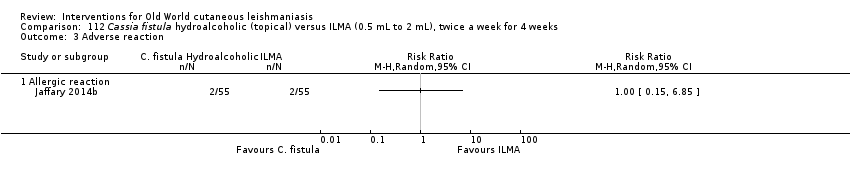 Comparison 112 Cassia fistula hydroalcoholic (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 3 Adverse reaction. | ||||
| 3.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 113.1 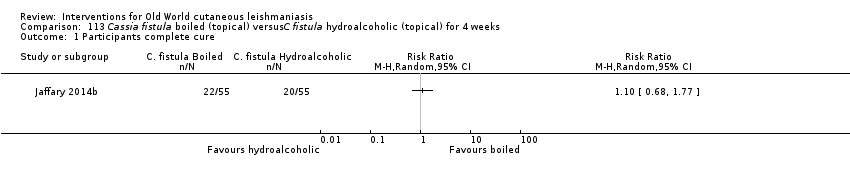 Comparison 113 Cassia fistula boiled (topical) versusC fistula hydroalcoholic (topical) for 4 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Speed of healing (days) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 113.2 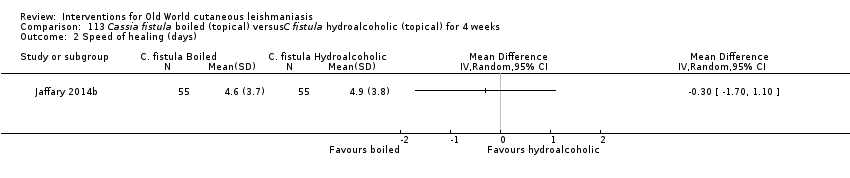 Comparison 113 Cassia fistula boiled (topical) versusC fistula hydroalcoholic (topical) for 4 weeks, Outcome 2 Speed of healing (days). | ||||
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 113.3  Comparison 113 Cassia fistula boiled (topical) versusC fistula hydroalcoholic (topical) for 4 weeks, Outcome 3 Adverse effects. | ||||
| 3.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 114.1 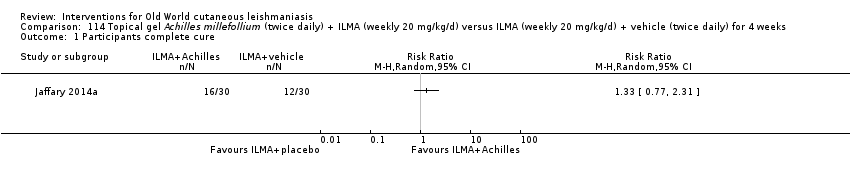 Comparison 114 Topical gel Achilles millefollium (twice daily) + ILMA (weekly 20 mg/kg/d) versus ILMA (weekly 20 mg/kg/d) + vehicle (twice daily) for 4 weeks, Outcome 1 Participants complete cure. | ||||
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 114.2  Comparison 114 Topical gel Achilles millefollium (twice daily) + ILMA (weekly 20 mg/kg/d) versus ILMA (weekly 20 mg/kg/d) + vehicle (twice daily) for 4 weeks, Outcome 2 Adverse effects. | ||||
| 2.1 Itching | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 114.3  Comparison 114 Topical gel Achilles millefollium (twice daily) + ILMA (weekly 20 mg/kg/d) versus ILMA (weekly 20 mg/kg/d) + vehicle (twice daily) for 4 weeks, Outcome 3 Microbiological cure of skin lesions. | ||||

Study flow diagram.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.

Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
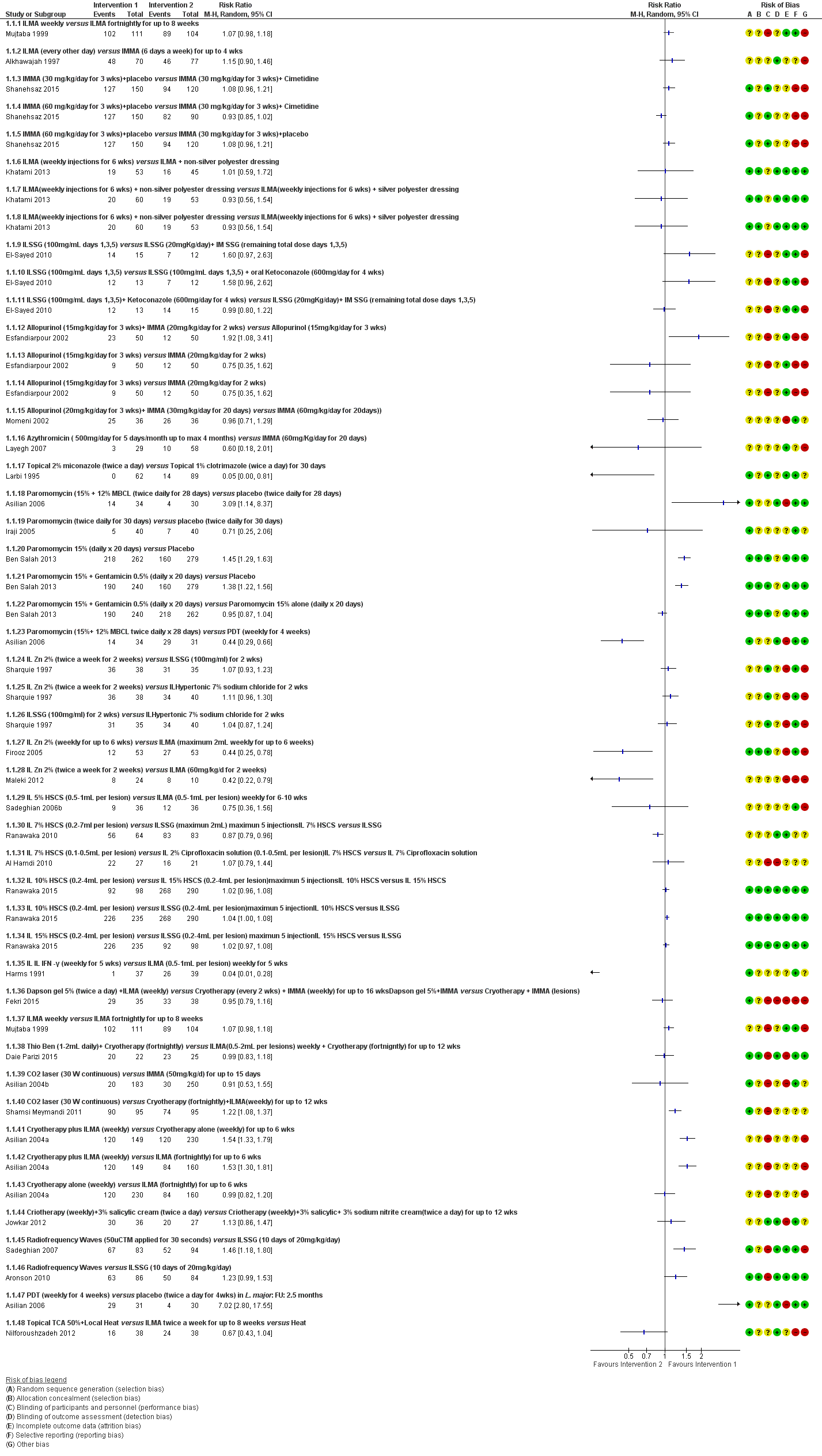
Forest Plot of Primary Outcome: Lesions Cured (Various comparisons)
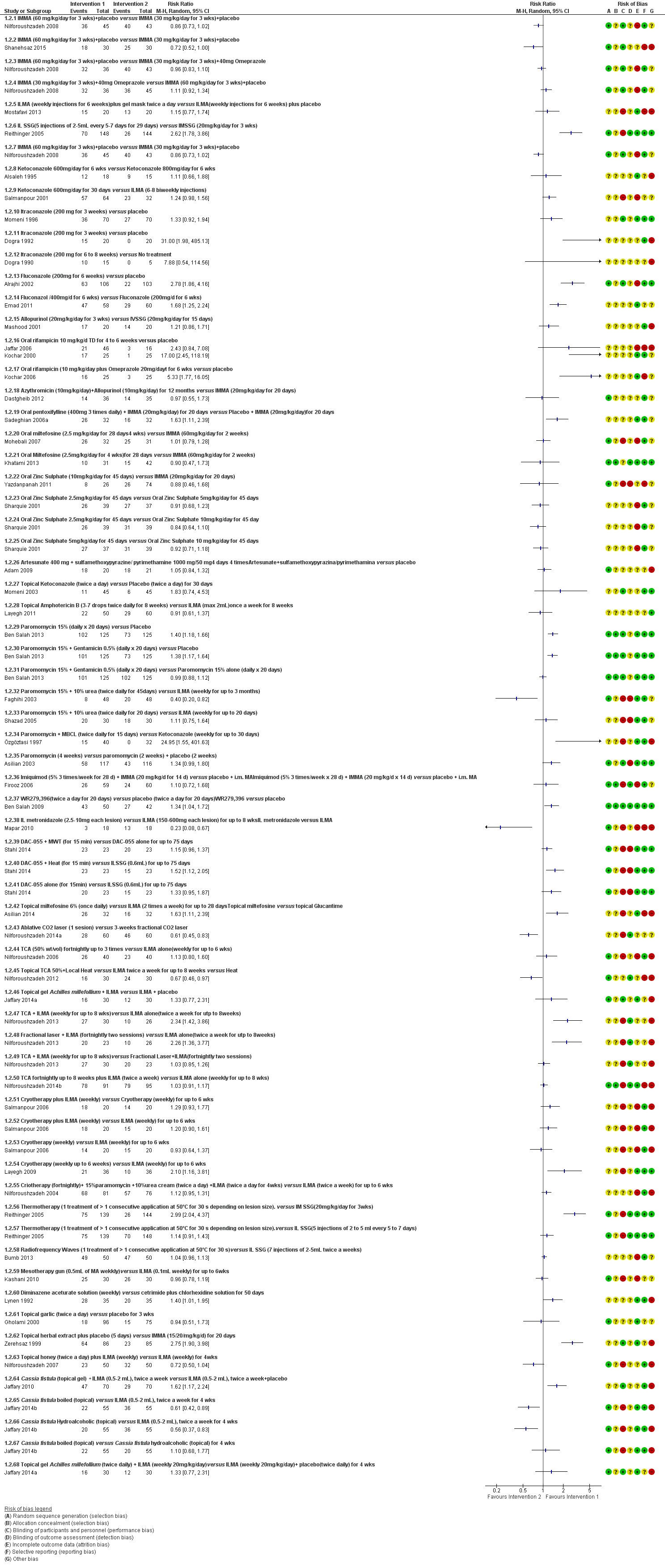
Forest plot of primary outcome: 1.2 Participants cured (Various comparisons)

Comparison 1 ILMA weekly versus ILMA fortnightly for up to 8 weeks, Outcome 1 Lesions cured.
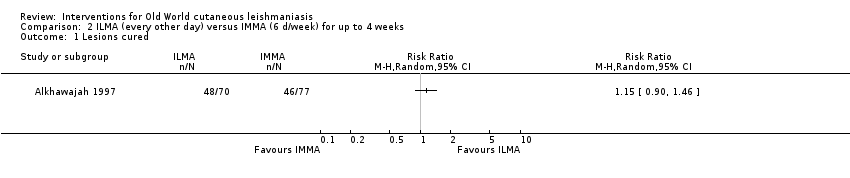
Comparison 2 ILMA (every other day) versus IMMA (6 d/week) for up to 4 weeks, Outcome 1 Lesions cured.
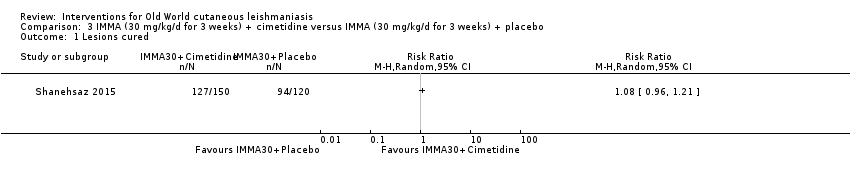
Comparison 3 IMMA (30 mg/kg/d for 3 weeks) + cimetidine versus IMMA (30 mg/kg/d for 3 weeks) + placebo, Outcome 1 Lesions cured.
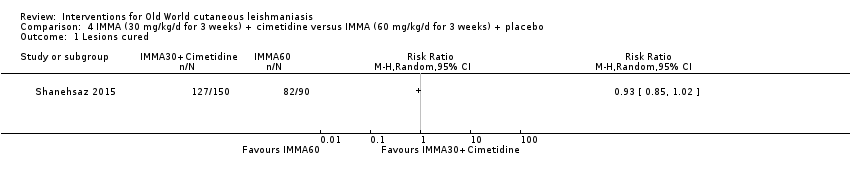
Comparison 4 IMMA (30 mg/kg/d for 3 weeks) + cimetidine versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Lesions cured.
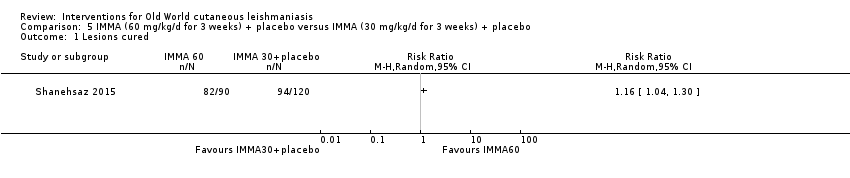
Comparison 5 IMMA (60 mg/kg/d for 3 weeks) + placebo versus IMMA (30 mg/kg/d for 3 weeks) + placebo, Outcome 1 Lesions cured.
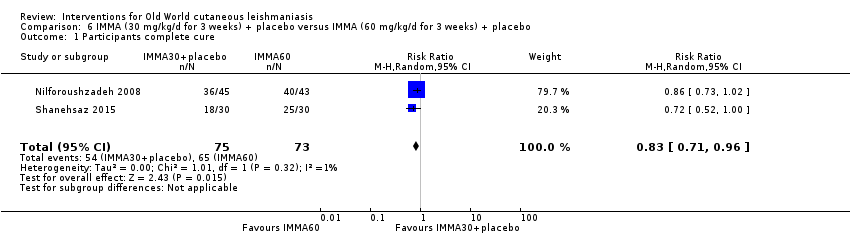
Comparison 6 IMMA (30 mg/kg/d for 3 weeks) + placebo versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Participants complete cure.
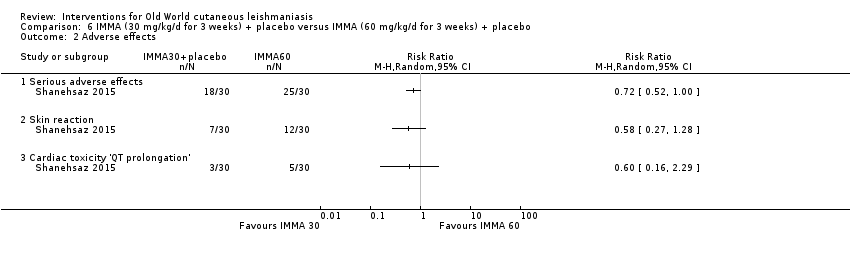
Comparison 6 IMMA (30 mg/kg/d for 3 weeks) + placebo versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 2 Adverse effects.
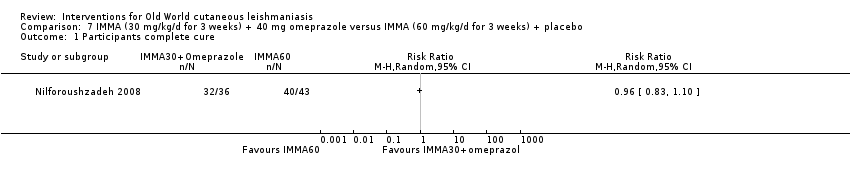
Comparison 7 IMMA (30 mg/kg/d for 3 weeks) + 40 mg omeprazole versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Participants complete cure.

Comparison 8 IMMA (30 mg/kg/d for 3 weeks) + placebo versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Participants complete cure.
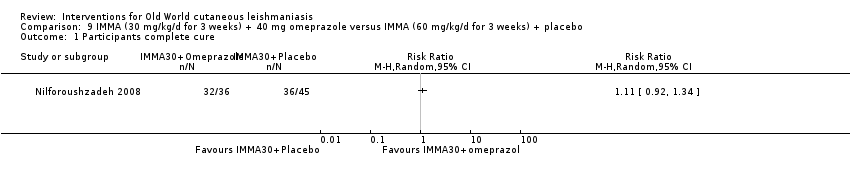
Comparison 9 IMMA (30 mg/kg/d for 3 weeks) + 40 mg omeprazole versus IMMA (60 mg/kg/d for 3 weeks) + placebo, Outcome 1 Participants complete cure.

Comparison 10 ILMA + non‐silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 1 Lesions cured.
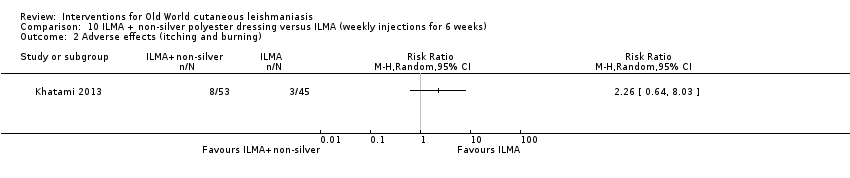
Comparison 10 ILMA + non‐silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 2 Adverse effects (itching and burning).

Comparison 10 ILMA + non‐silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 3 Adverse effects (oedema).
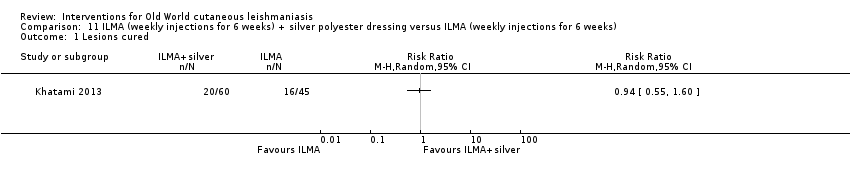
Comparison 11 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 1 Lesions cured.

Comparison 11 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 2 Adverse effects (itching and burning).
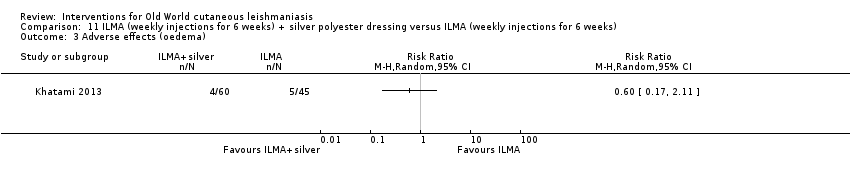
Comparison 11 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks), Outcome 3 Adverse effects (oedema).

Comparison 12 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks) + non‐silver polyester dressing, Outcome 1 Lesions cured.
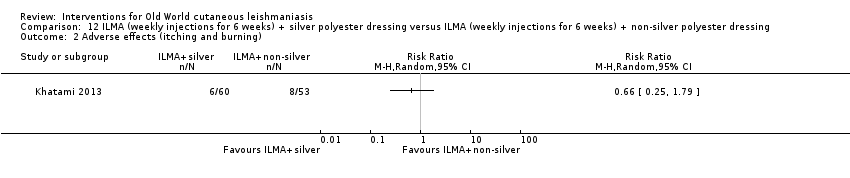
Comparison 12 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks) + non‐silver polyester dressing, Outcome 2 Adverse effects (itching and burning).

Comparison 12 ILMA (weekly injections for 6 weeks) + silver polyester dressing versus ILMA (weekly injections for 6 weeks) + non‐silver polyester dressing, Outcome 3 Adverse effects (oedema).
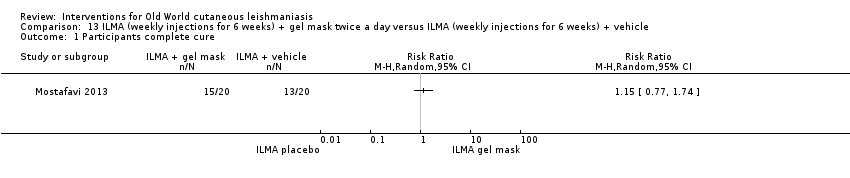
Comparison 13 ILMA (weekly injections for 6 weeks) + gel mask twice a day versus ILMA (weekly injections for 6 weeks) + vehicle, Outcome 1 Participants complete cure.

Comparison 14 ILSSG (20 mg/kg/d) + IMSSG (remaining total dose days 1, 3, 5) versus ILSSG (1000 mg/mL days 1, 3, 5), Outcome 1 Lesions cured.
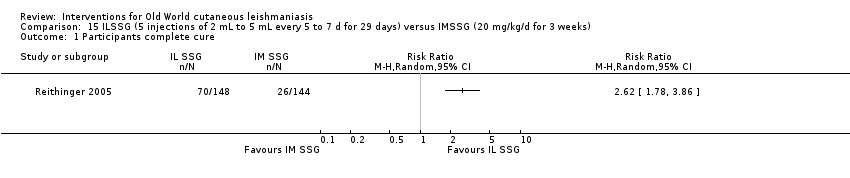
Comparison 15 ILSSG (5 injections of 2 mL to 5 mL every 5 to 7 d for 29 days) versus IMSSG (20 mg/kg/d for 3 weeks), Outcome 1 Participants complete cure.
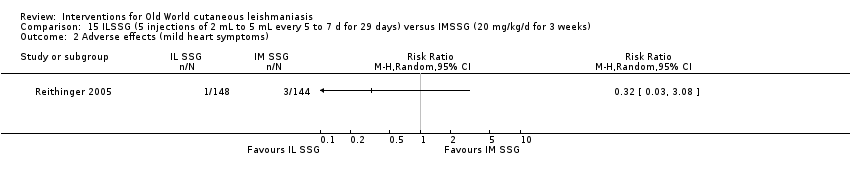
Comparison 15 ILSSG (5 injections of 2 mL to 5 mL every 5 to 7 d for 29 days) versus IMSSG (20 mg/kg/d for 3 weeks), Outcome 2 Adverse effects (mild heart symptoms).

Comparison 16 Ketoconazole 600 mg/d for 6 weeks versus ketoconazole 800 mg/d for 6 weeks, Outcome 1 Participants complete cure.
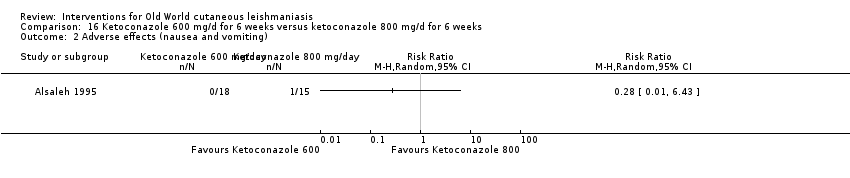
Comparison 16 Ketoconazole 600 mg/d for 6 weeks versus ketoconazole 800 mg/d for 6 weeks, Outcome 2 Adverse effects (nausea and vomiting).
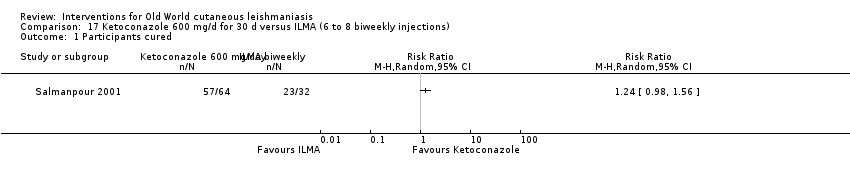
Comparison 17 Ketoconazole 600 mg/d for 30 d versus ILMA (6 to 8 biweekly injections), Outcome 1 Participants cured.

Comparison 17 Ketoconazole 600 mg/d for 30 d versus ILMA (6 to 8 biweekly injections), Outcome 2 Adverse effect (liver enzymes increase).

Comparison 18 ILSSG (100 mg/mL days 1, 3, 5) + oral ketoconazole (600 mg/d for 4 weeks) versus ILSSG (100 mg/mL days 1, 3, 5), Outcome 1 Lesions cured.
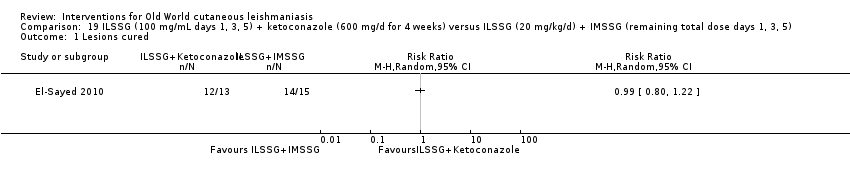
Comparison 19 ILSSG (100 mg/mL days 1, 3, 5) + ketoconazole (600 mg/d for 4 weeks) versus ILSSG (20 mg/kg/d) + IMSSG (remaining total dose days 1, 3, 5), Outcome 1 Lesions cured.

Comparison 20 Itraconazole (200 mg for 6 weeks) versus placebo, Outcome 1 Participants complete cure.

Comparison 21 Itraconazole (200 mg for 3 weeks) versus placebo, Outcome 1 Participants complete cure.
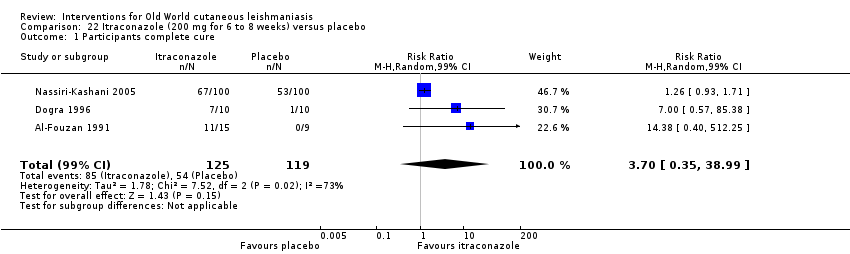
Comparison 22 Itraconazole (200 mg for 6 to 8 weeks) versus placebo, Outcome 1 Participants complete cure.
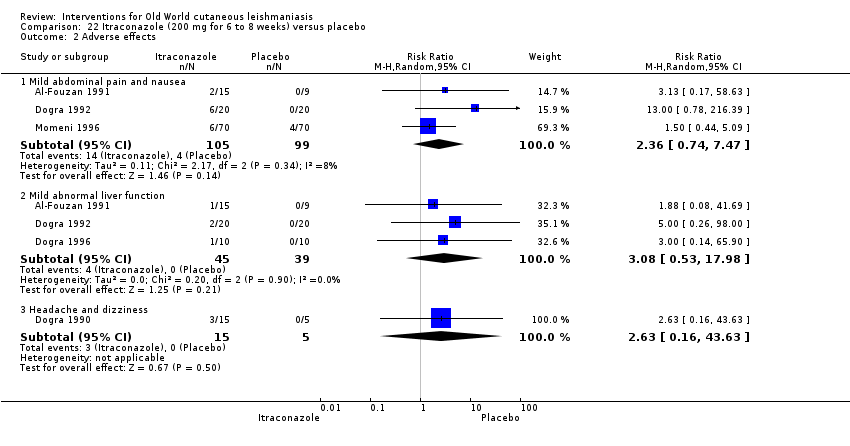
Comparison 22 Itraconazole (200 mg for 6 to 8 weeks) versus placebo, Outcome 2 Adverse effects.
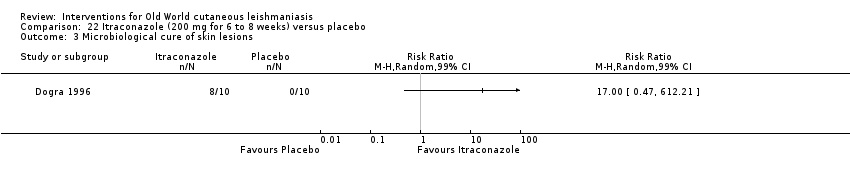
Comparison 22 Itraconazole (200 mg for 6 to 8 weeks) versus placebo, Outcome 3 Microbiological cure of skin lesions.
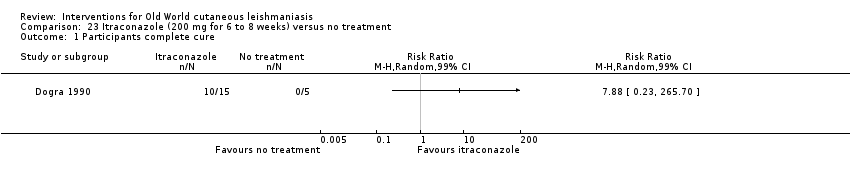
Comparison 23 Itraconazole (200 mg for 6 to 8 weeks) versus no treatment, Outcome 1 Participants complete cure.
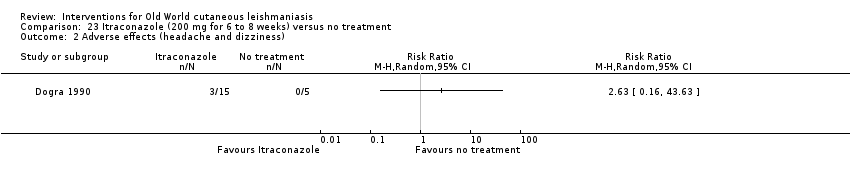
Comparison 23 Itraconazole (200 mg for 6 to 8 weeks) versus no treatment, Outcome 2 Adverse effects (headache and dizziness).
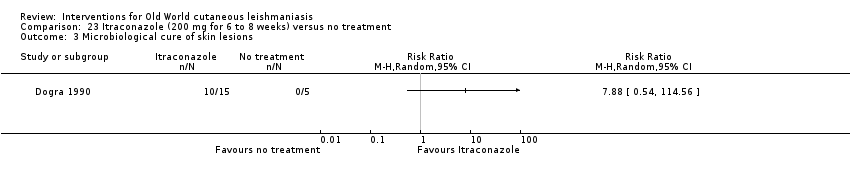
Comparison 23 Itraconazole (200 mg for 6 to 8 weeks) versus no treatment, Outcome 3 Microbiological cure of skin lesions.
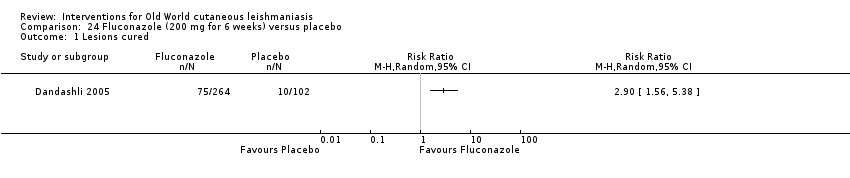
Comparison 24 Fluconazole (200 mg for 6 weeks) versus placebo, Outcome 1 Lesions cured.

Comparison 24 Fluconazole (200 mg for 6 weeks) versus placebo, Outcome 2 Participants complete cure.

Comparison 25 Fluconazole (400 mg/d for 6 weeks) versus fluconazole (200 mg/d for 6 weeks), Outcome 1 Participants complete cure.

Comparison 25 Fluconazole (400 mg/d for 6 weeks) versus fluconazole (200 mg/d for 6 weeks), Outcome 2 Adverse effects.
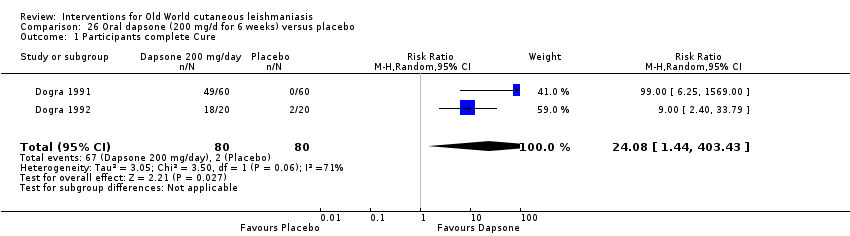
Comparison 26 Oral dapsone (200 mg/d for 6 weeks) versus placebo, Outcome 1 Participants complete Cure.

Comparison 26 Oral dapsone (200 mg/d for 6 weeks) versus placebo, Outcome 2 Adverse effects.

Comparison 27 Allopurinol (15 mg/kg/d for 3 weeks) + IMMA (20 mg/kg/d for 2 weeks) versus allopurinol (15 mg/kg/d for 3 weeks), Outcome 1 Lesions cured.

Comparison 28 Allopurinol (15mg/kg/d for 3 weeks)+ IMMA (20 mg/kg/d for 2 weeks) versus IMMA (20 mg/kg/d for 2 weeks), Outcome 1 Lesions cured.

Comparison 29 Allopurinol (15 mg/kg/d for 3 weeks) versus IMMA (20 mg/kg/d for 2 weeks), Outcome 1 Lesions Cured.

Comparison 30 Allopurinol (20 mg/kg/d for 3 weeks) + IMMA (30 mg/kg/d for 20 days) versus IMMA (60 mg/kg/d for 20 d), Outcome 1 Lesions cured.

Comparison 30 Allopurinol (20 mg/kg/d for 3 weeks) + IMMA (30 mg/kg/d for 20 days) versus IMMA (60 mg/kg/d for 20 d), Outcome 2 Adverse effects.

Comparison 30 Allopurinol (20 mg/kg/d for 3 weeks) + IMMA (30 mg/kg/d for 20 days) versus IMMA (60 mg/kg/d for 20 d), Outcome 3 Microbiological cure of skin lesions.

Comparison 31 Allopurinol (20 mg/kg/d for 3 weeks)+ IMMA (10 mg/kg/d for 20 d) versus IMMA (20 mg/kg/d for 28 d), Outcome 1 Adverse effects.
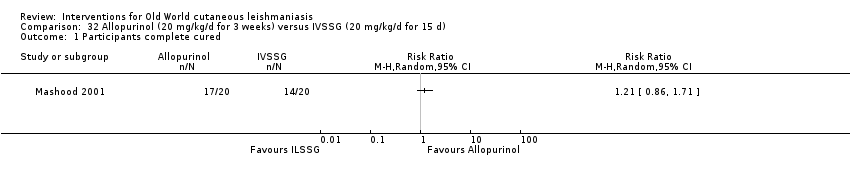
Comparison 32 Allopurinol (20 mg/kg/d for 3 weeks) versus IVSSG (20 mg/kg/d for 15 d), Outcome 1 Participants complete cured.
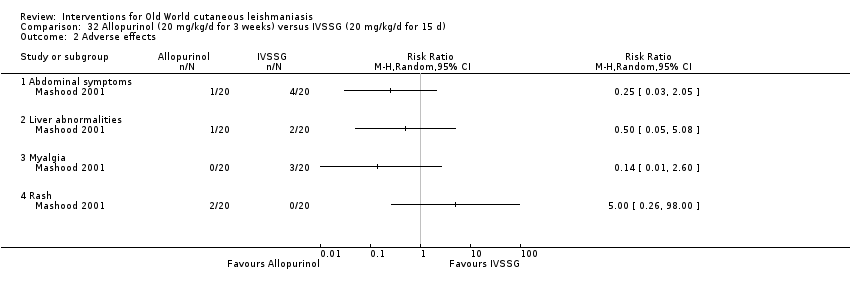
Comparison 32 Allopurinol (20 mg/kg/d for 3 weeks) versus IVSSG (20 mg/kg/d for 15 d), Outcome 2 Adverse effects.

Comparison 33 Oral rifampicin (10 mg/kg/d for 4 to 6 weeks) versus placebo, Outcome 1 Participants complete cure.

Comparison 33 Oral rifampicin (10 mg/kg/d for 4 to 6 weeks) versus placebo, Outcome 2 Microbiological cure of skin lesions.

Comparison 34 Oral rifampicin (10 mg/kg/d) + omeprazole (20 mg/d) for 6 weeks versus placebo, Outcome 1 Participants complete cure.

Comparison 35 Azythromicin (500 mg/d for 5 d/month up to 4 months) versus IMMA (60 mg/kg/d for 20 d), Outcome 1 Lesions cured.

Comparison 35 Azythromicin (500 mg/d for 5 d/month up to 4 months) versus IMMA (60 mg/kg/d for 20 d), Outcome 2 Adverse effects.
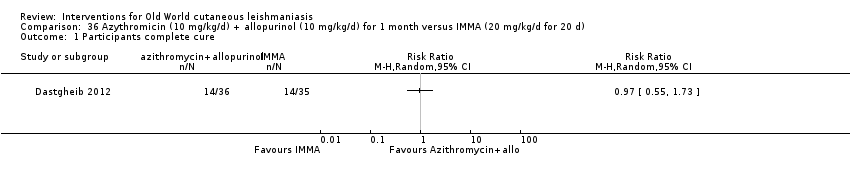
Comparison 36 Azythromicin (10 mg/kg/d) + allopurinol (10 mg/kg/d) for 1 month versus IMMA (20 mg/kg/d for 20 d), Outcome 1 Participants complete cure.
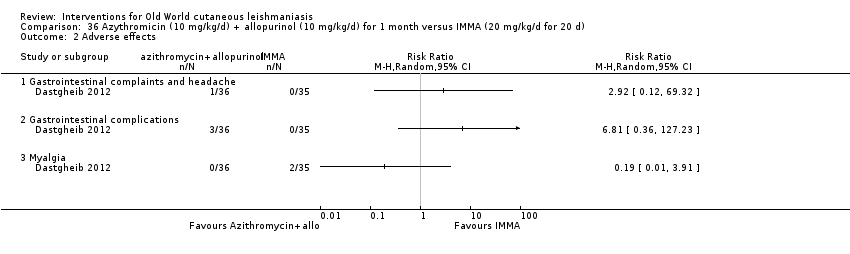
Comparison 36 Azythromicin (10 mg/kg/d) + allopurinol (10 mg/kg/d) for 1 month versus IMMA (20 mg/kg/d for 20 d), Outcome 2 Adverse effects.

Comparison 37 Oral pentoxifylline (400 mg 3 times daily) + IMMA (20 mg/kg/d) for 20 d versus placebo + IMMA (20 mg/kg/d) for 20 d, Outcome 1 Participants complete cure.

Comparison 37 Oral pentoxifylline (400 mg 3 times daily) + IMMA (20 mg/kg/d) for 20 d versus placebo + IMMA (20 mg/kg/d) for 20 d, Outcome 2 Adverse effects.

Comparison 38 Oral miltefosine (2.5 mg/kg/d for 4 weeks) versus IMMA (60 mg/kg/d for 2 weeks), Outcome 1 Participants complete cure.
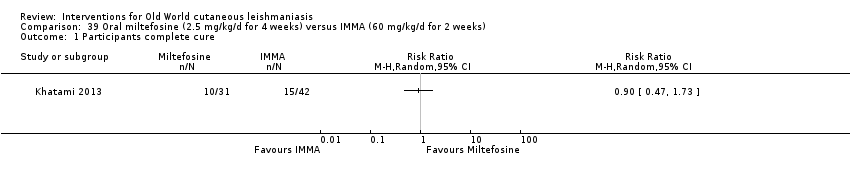
Comparison 39 Oral miltefosine (2.5 mg/kg/d for 4 weeks) versus IMMA (60 mg/kg/d for 2 weeks), Outcome 1 Participants complete cure.

Comparison 40 Oral zinc sulphate 2.5 mg/kg/d for 45 days versus oral zinc sulphate 5 mg/kg/d for 45 d, Outcome 1 Participants complete cure.
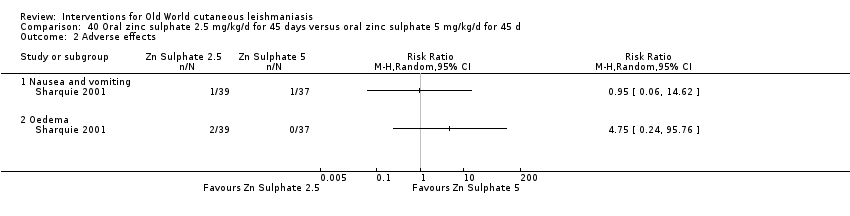
Comparison 40 Oral zinc sulphate 2.5 mg/kg/d for 45 days versus oral zinc sulphate 5 mg/kg/d for 45 d, Outcome 2 Adverse effects.

Comparison 41 Oral zinc sulphate 2.5 mg/kg/d for 45 d versus oral zinc sulphate 10 mg/kg/d for 45 d, Outcome 1 Participants complete cure.
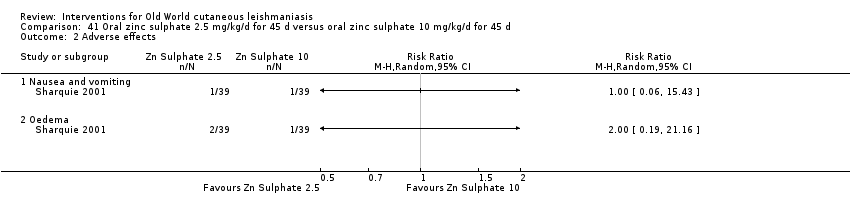
Comparison 41 Oral zinc sulphate 2.5 mg/kg/d for 45 d versus oral zinc sulphate 10 mg/kg/d for 45 d, Outcome 2 Adverse effects.
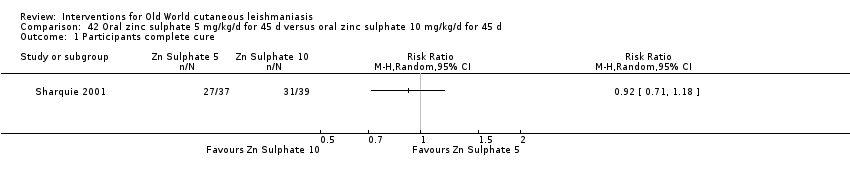
Comparison 42 Oral zinc sulphate 5 mg/kg/d for 45 d versus oral zinc sulphate 10 mg/kg/d for 45 d, Outcome 1 Participants complete cure.
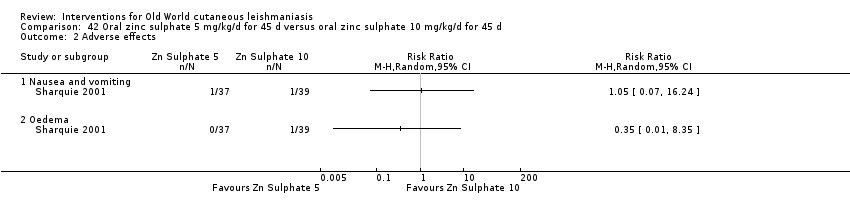
Comparison 42 Oral zinc sulphate 5 mg/kg/d for 45 d versus oral zinc sulphate 10 mg/kg/d for 45 d, Outcome 2 Adverse effects.
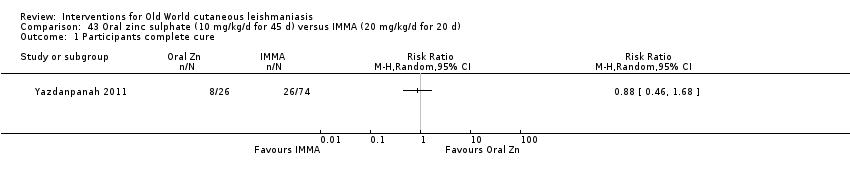
Comparison 43 Oral zinc sulphate (10 mg/kg/d for 45 d) versus IMMA (20 mg/kg/d for 20 d), Outcome 1 Participants complete cure.
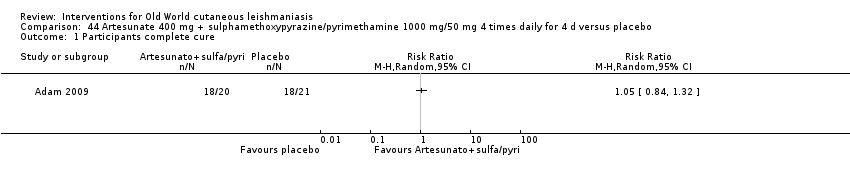
Comparison 44 Artesunate 400 mg + sulphamethoxypyrazine/pyrimethamine 1000 mg/50 mg 4 times daily for 4 d versus placebo, Outcome 1 Participants complete cure.
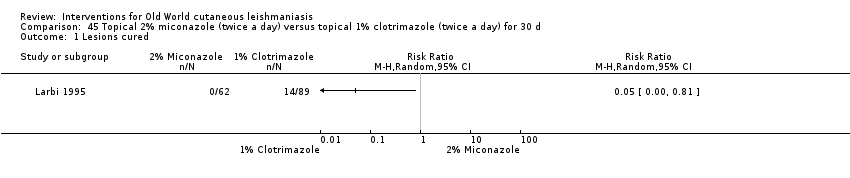
Comparison 45 Topical 2% miconazole (twice a day) versus topical 1% clotrimazole (twice a day) for 30 d, Outcome 1 Lesions cured.
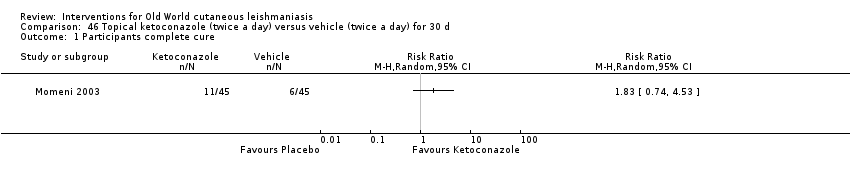
Comparison 46 Topical ketoconazole (twice a day) versus vehicle (twice a day) for 30 d, Outcome 1 Participants complete cure.

Comparison 47 Topical amphotericin B (3 to 7 drops twice daily for 8 weeks) versus ILMA (max 2 mL) once a week for 8 weeks, Outcome 1 Participants complete cure (ITT).

Comparison 47 Topical amphotericin B (3 to 7 drops twice daily for 8 weeks) versus ILMA (max 2 mL) once a week for 8 weeks, Outcome 2 Adverse effects.

Comparison 48 Paromomycin 15% + 12% MBCL (twice daily for 28 d) versus vehicle (twice daily for 28 d), Outcome 1 Lesions cured.

Comparison 48 Paromomycin 15% + 12% MBCL (twice daily for 28 d) versus vehicle (twice daily for 28 d), Outcome 2 Scarring.

Comparison 48 Paromomycin 15% + 12% MBCL (twice daily for 28 d) versus vehicle (twice daily for 28 d), Outcome 3 Microbiological cure of skin lesions.
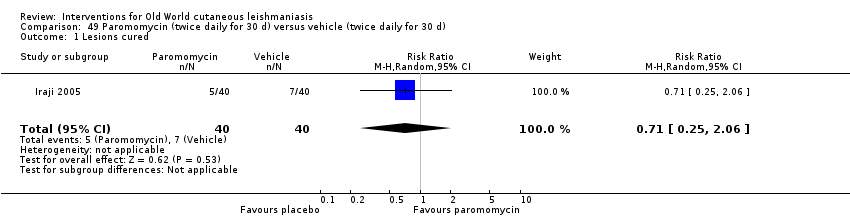
Comparison 49 Paromomycin (twice daily for 30 d) versus vehicle (twice daily for 30 d), Outcome 1 Lesions cured.
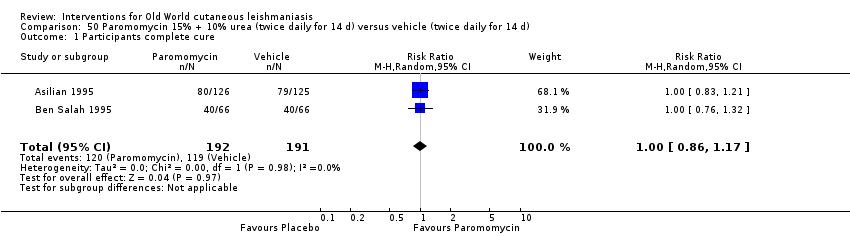
Comparison 50 Paromomycin 15% + 10% urea (twice daily for 14 d) versus vehicle (twice daily for 14 d), Outcome 1 Participants complete cure.
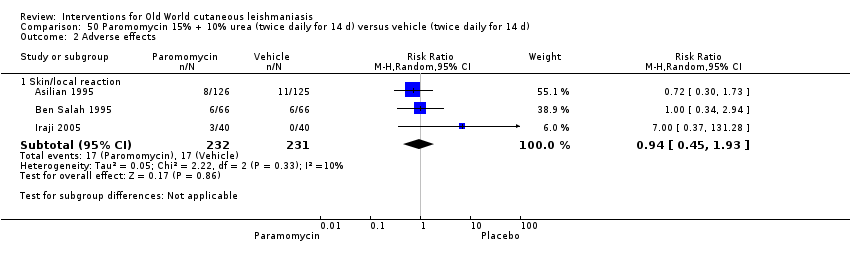
Comparison 50 Paromomycin 15% + 10% urea (twice daily for 14 d) versus vehicle (twice daily for 14 d), Outcome 2 Adverse effects.
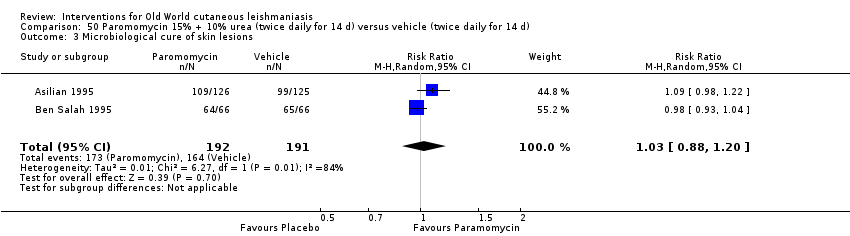
Comparison 50 Paromomycin 15% + 10% urea (twice daily for 14 d) versus vehicle (twice daily for 14 d), Outcome 3 Microbiological cure of skin lesions.
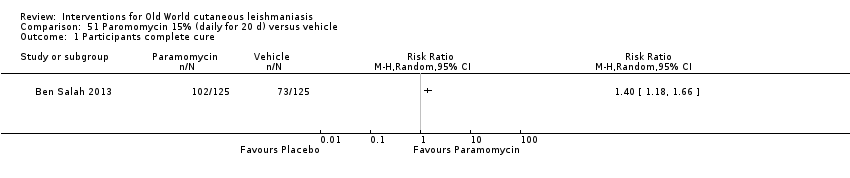
Comparison 51 Paromomycin 15% (daily for 20 d) versus vehicle, Outcome 1 Participants complete cure.

Comparison 52 Paromomycin 15% + gentamicin 0.5% (daily for 20 d) versus vehicle, Outcome 1 Participants complete cure.

Comparison 53 Paromomycin 15% + gentamicin 0.5% (daily for 20 d) versus paromomycin 15% alone (daily for 20 d), Outcome 1 Participants complete cure.

Comparison 54 Paromomycin 15% + 10% urea (twice daily for 45 d) versus ILMA (weekly for up to 3 months), Outcome 1 Participants complete cure.

Comparison 54 Paromomycin 15% + 10% urea (twice daily for 45 d) versus ILMA (weekly for up to 3 months), Outcome 2 Recurrence.
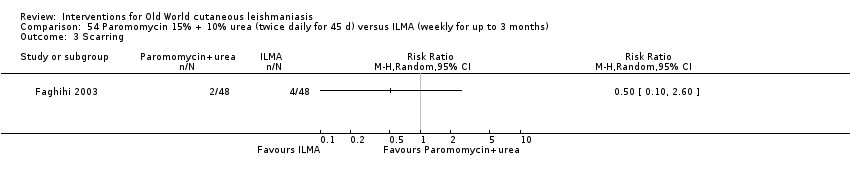
Comparison 54 Paromomycin 15% + 10% urea (twice daily for 45 d) versus ILMA (weekly for up to 3 months), Outcome 3 Scarring.
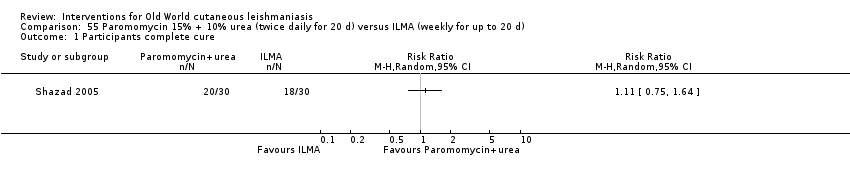
Comparison 55 Paromomycin 15% + 10% urea (twice daily for 20 d) versus ILMA (weekly for up to 20 d), Outcome 1 Participants complete cure.

Comparison 55 Paromomycin 15% + 10% urea (twice daily for 20 d) versus ILMA (weekly for up to 20 d), Outcome 2 Adverse effects.
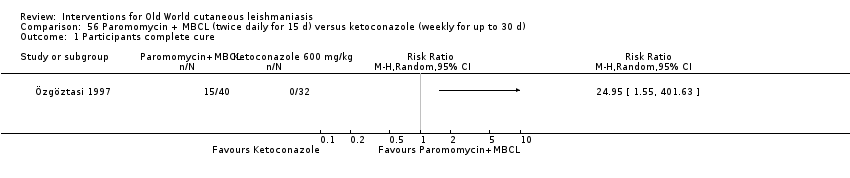
Comparison 56 Paromomycin + MBCL (twice daily for 15 d) versus ketoconazole (weekly for up to 30 d), Outcome 1 Participants complete cure.

Comparison 56 Paromomycin + MBCL (twice daily for 15 d) versus ketoconazole (weekly for up to 30 d), Outcome 2 Microbiological cure of skin lesions.
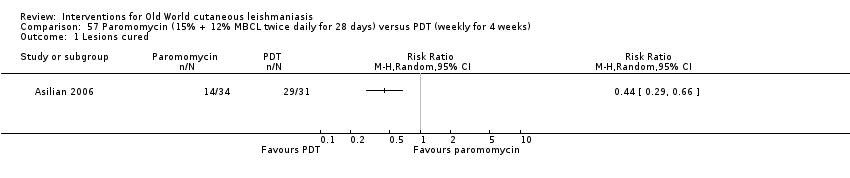
Comparison 57 Paromomycin (15% + 12% MBCL twice daily for 28 days) versus PDT (weekly for 4 weeks), Outcome 1 Lesions cured.
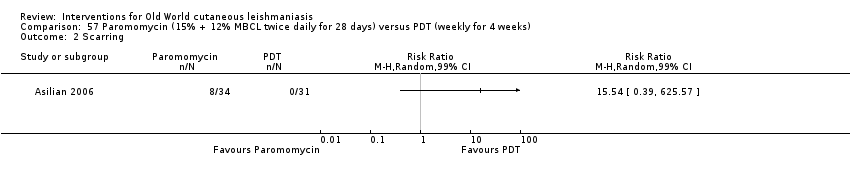
Comparison 57 Paromomycin (15% + 12% MBCL twice daily for 28 days) versus PDT (weekly for 4 weeks), Outcome 2 Scarring.

Comparison 57 Paromomycin (15% + 12% MBCL twice daily for 28 days) versus PDT (weekly for 4 weeks), Outcome 3 Microbiological cure of skin lesions.

Comparison 58 Paromomycin (4 weeks) versus paromomycin (2 weeks) + vehicle (2 weeks), Outcome 1 Participants complete cure.

Comparison 58 Paromomycin (4 weeks) versus paromomycin (2 weeks) + vehicle (2 weeks), Outcome 2 Microbiological cure of skin lesions.
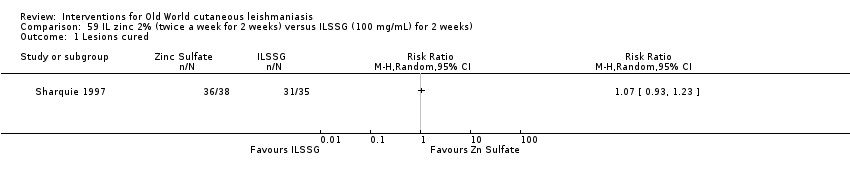
Comparison 59 IL zinc 2% (twice a week for 2 weeks) versus ILSSG (100 mg/mL) for 2 weeks), Outcome 1 Lesions cured.

Comparison 60 IL zinc 2% (twice a week for 2 weeks) versus IL 7% HSCS for 2 weeks, Outcome 1 Lesions cured.
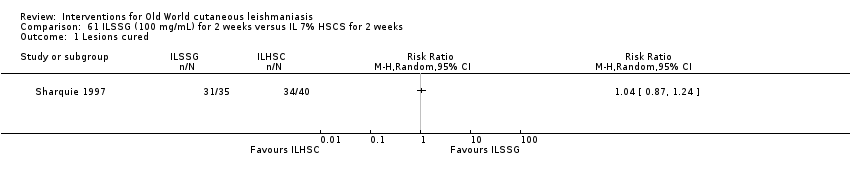
Comparison 61 ILSSG (100 mg/mL) for 2 weeks versus IL 7% HSCS for 2 weeks, Outcome 1 Lesions cured.
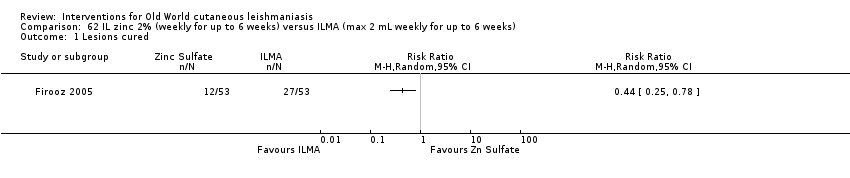
Comparison 62 IL zinc 2% (weekly for up to 6 weeks) versus ILMA (max 2 mL weekly for up to 6 weeks), Outcome 1 Lesions cured.

Comparison 62 IL zinc 2% (weekly for up to 6 weeks) versus ILMA (max 2 mL weekly for up to 6 weeks), Outcome 2 Participants complete cured.
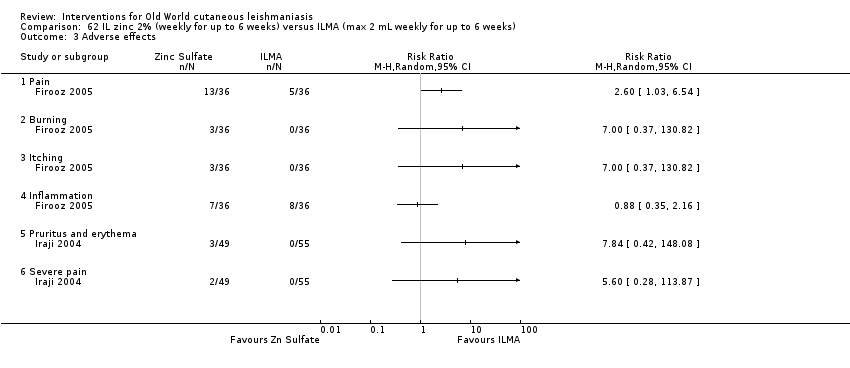
Comparison 62 IL zinc 2% (weekly for up to 6 weeks) versus ILMA (max 2 mL weekly for up to 6 weeks), Outcome 3 Adverse effects.
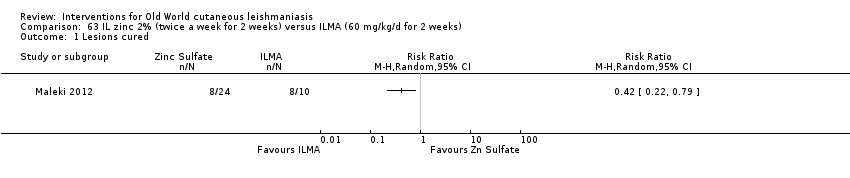
Comparison 63 IL zinc 2% (twice a week for 2 weeks) versus ILMA (60 mg/kg/d for 2 weeks), Outcome 1 Lesions cured.

Comparison 63 IL zinc 2% (twice a week for 2 weeks) versus ILMA (60 mg/kg/d for 2 weeks), Outcome 2 Adverse effects.
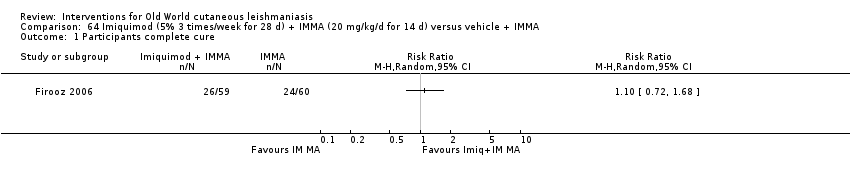
Comparison 64 Imiquimod (5% 3 times/week for 28 d) + IMMA (20 mg/kg/d for 14 d) versus vehicle + IMMA, Outcome 1 Participants complete cure.

Comparison 64 Imiquimod (5% 3 times/week for 28 d) + IMMA (20 mg/kg/d for 14 d) versus vehicle + IMMA, Outcome 2 Participants with treated lesions that recur.

Comparison 64 Imiquimod (5% 3 times/week for 28 d) + IMMA (20 mg/kg/d for 14 d) versus vehicle + IMMA, Outcome 3 Adverse effects.
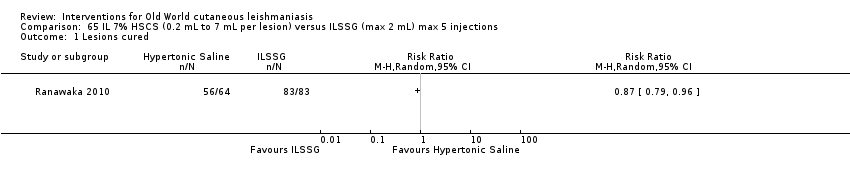
Comparison 65 IL 7% HSCS (0.2 mL to 7 mL per lesion) versus ILSSG (max 2 mL) max 5 injections, Outcome 1 Lesions cured.

Comparison 66 IL 5% HSCS (0.5 mL to 1 mL per lesion) versus ILMA (0.5 mL to 1 mL per lesion) weekly for 6 to 10 weeks, Outcome 1 Lesions cured.

Comparison 66 IL 5% HSCS (0.5 mL to 1 mL per lesion) versus ILMA (0.5 mL to 1 mL per lesion) weekly for 6 to 10 weeks, Outcome 2 Adverse effects.

Comparison 67 IL 7% HSCS (0.1 mL to 0.5 mL per lesion) versus IL 2% ciprofloxacin solution (0.1 mL to 0.5 mL per lesion), Outcome 1 Lesions cured.

Comparison 68 IL 15% HSCS (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 1 Lesions cured.
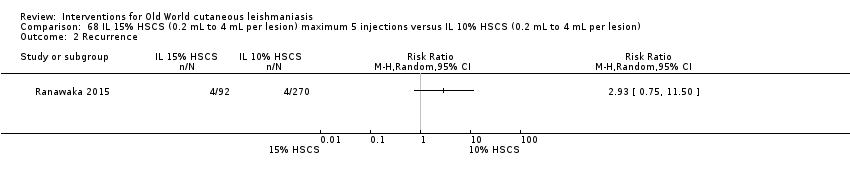
Comparison 68 IL 15% HSCS (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 2 Recurrence.

Comparison 68 IL 15% HSCS (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 3 Speed of healing (weeks).
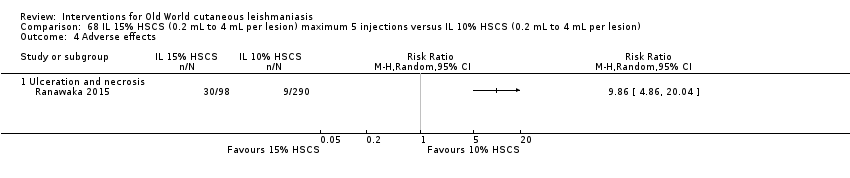
Comparison 68 IL 15% HSCS (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 4 Adverse effects.
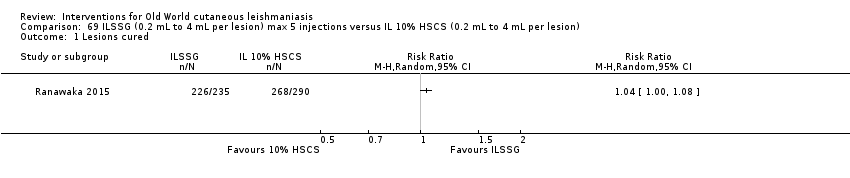
Comparison 69 ILSSG (0.2 mL to 4 mL per lesion) max 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 1 Lesions cured.

Comparison 69 ILSSG (0.2 mL to 4 mL per lesion) max 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 2 Recurrence.

Comparison 69 ILSSG (0.2 mL to 4 mL per lesion) max 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 3 Speed of healing (weeks).

Comparison 69 ILSSG (0.2 mL to 4 mL per lesion) max 5 injections versus IL 10% HSCS (0.2 mL to 4 mL per lesion), Outcome 4 Adverse effects.
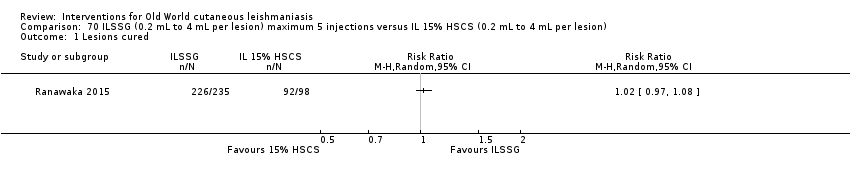
Comparison 70 ILSSG (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 15% HSCS (0.2 mL to 4 mL per lesion), Outcome 1 Lesions cured.

Comparison 70 ILSSG (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 15% HSCS (0.2 mL to 4 mL per lesion), Outcome 2 Recurrence.
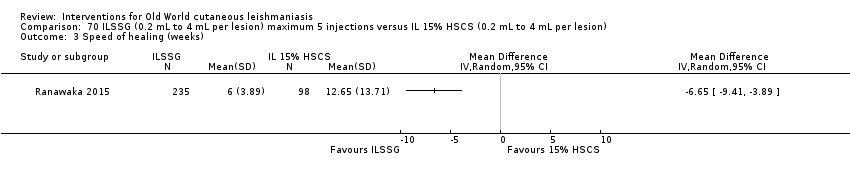
Comparison 70 ILSSG (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 15% HSCS (0.2 mL to 4 mL per lesion), Outcome 3 Speed of healing (weeks).

Comparison 70 ILSSG (0.2 mL to 4 mL per lesion) maximum 5 injections versus IL 15% HSCS (0.2 mL to 4 mL per lesion), Outcome 4 Adverse effects.

Comparison 71 IL IFN‐γ (weekly for 5 weeks) versus ILMA (0.5 mL to 1 mL per lesion) weekly for 5 weeks, Outcome 1 Lesions cured.
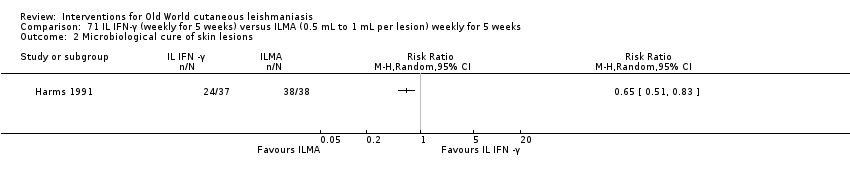
Comparison 71 IL IFN‐γ (weekly for 5 weeks) versus ILMA (0.5 mL to 1 mL per lesion) weekly for 5 weeks, Outcome 2 Microbiological cure of skin lesions.

Comparison 72 WR279,396 (twice a day for 20 d) versus vehicle (twice a day for 20 d), Outcome 1 Participants complete cure.

Comparison 72 WR279,396 (twice a day for 20 d) versus vehicle (twice a day for 20 d), Outcome 2 Adverse effects.

Comparison 73 IL metronidazole (2.5 mg to 10 mg each lesion) versus ILMA (150 mg to 600 mg each lesion) for up to 8 weeks, Outcome 1 Participants complete cure.
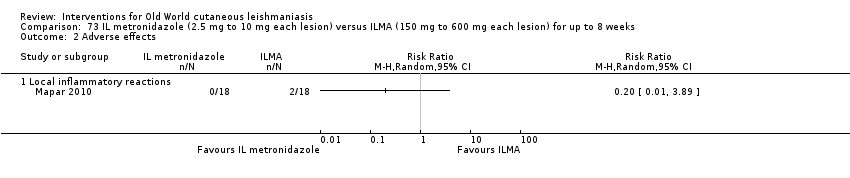
Comparison 73 IL metronidazole (2.5 mg to 10 mg each lesion) versus ILMA (150 mg to 600 mg each lesion) for up to 8 weeks, Outcome 2 Adverse effects.

Comparison 74 Topical miltefosine 6% (once daily) versus ILMA (twice a week) for up to 28 d, Outcome 1 Participants complete cure.

Comparison 75 Dapsone gel 5% (twice a day) + ILMA (weekly) versus cryotherapy (every 2 weeks) + IMMA (weekly) for up to 16 weeks, Outcome 1 Lesions cured.
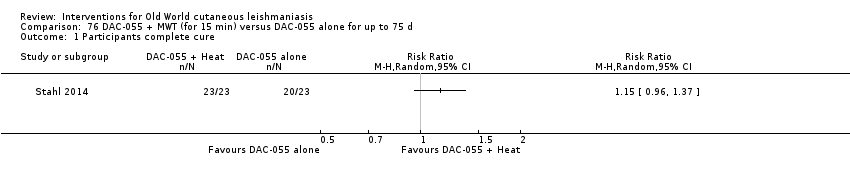
Comparison 76 DAC‐055 + MWT (for 15 min) versus DAC‐055 alone for up to 75 d, Outcome 1 Participants complete cure.
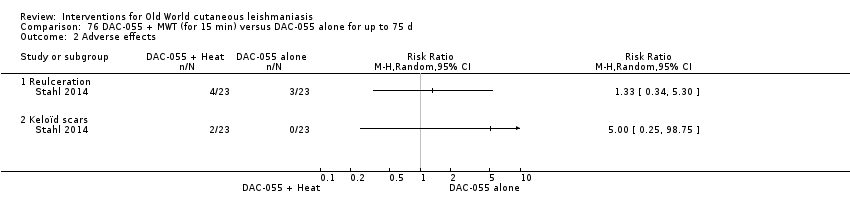
Comparison 76 DAC‐055 + MWT (for 15 min) versus DAC‐055 alone for up to 75 d, Outcome 2 Adverse effects.

Comparison 77 DAC‐055 + heat (for 15 min) versus ILSSG (0.6 mL) for up to 75 d, Outcome 1 Participants complete cure.
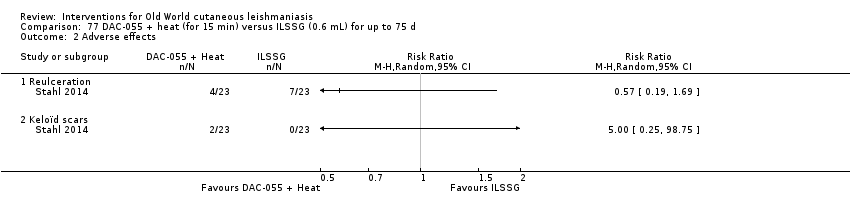
Comparison 77 DAC‐055 + heat (for 15 min) versus ILSSG (0.6 mL) for up to 75 d, Outcome 2 Adverse effects.

Comparison 78 DAC‐055 alone (for 15 min) versus ILSSG (0.6 mL) for up to 75 d, Outcome 1 Participants complete cure.

Comparison 78 DAC‐055 alone (for 15 min) versus ILSSG (0.6 mL) for up to 75 d, Outcome 2 Adverse effects.

Comparison 79 Thio‐Ben (1 mL to 2 mL daily) + cryotherapy (fortnightly) versus ILMA (0.5 mL to 2 mL per lesions) weekly + cryotherapy (fortnightly) for up to 12 weeks, Outcome 1 Lesions cured.
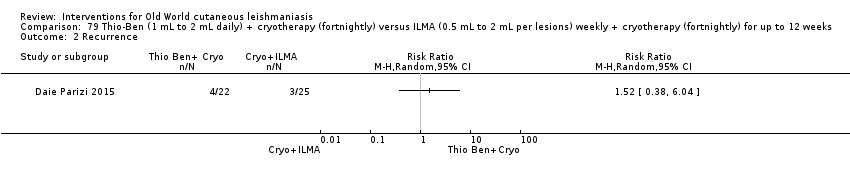
Comparison 79 Thio‐Ben (1 mL to 2 mL daily) + cryotherapy (fortnightly) versus ILMA (0.5 mL to 2 mL per lesions) weekly + cryotherapy (fortnightly) for up to 12 weeks, Outcome 2 Recurrence.
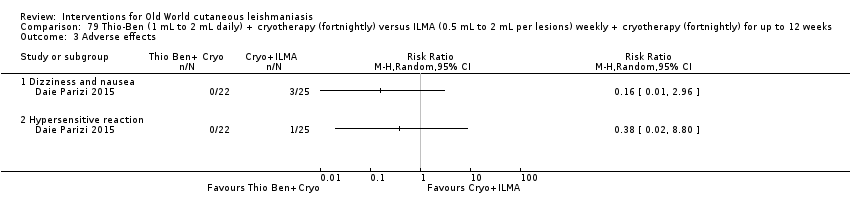
Comparison 79 Thio‐Ben (1 mL to 2 mL daily) + cryotherapy (fortnightly) versus ILMA (0.5 mL to 2 mL per lesions) weekly + cryotherapy (fortnightly) for up to 12 weeks, Outcome 3 Adverse effects.

Comparison 80 CO₂ laser (30 W continuous) versus IMMA (50 mg/kg/d) for up to 15 d, Outcome 1 Lesions cured.

Comparison 80 CO₂ laser (30 W continuous) versus IMMA (50 mg/kg/d) for up to 15 d, Outcome 2 Adverse effects.

Comparison 81 CO₂ laser (30 W continuous) versus cryotherapy (fortnightly) + ILMA (weekly) for up to 12 weeks, Outcome 1 Lesions cured.
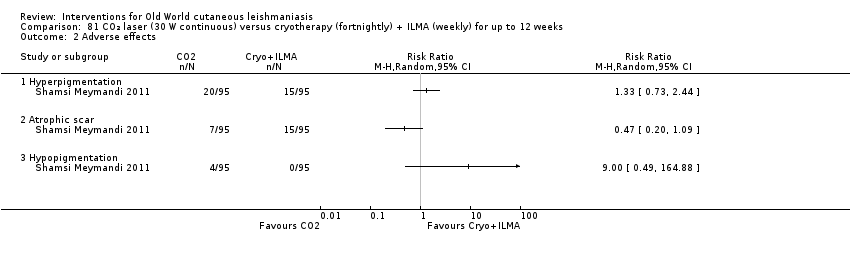
Comparison 81 CO₂ laser (30 W continuous) versus cryotherapy (fortnightly) + ILMA (weekly) for up to 12 weeks, Outcome 2 Adverse effects.
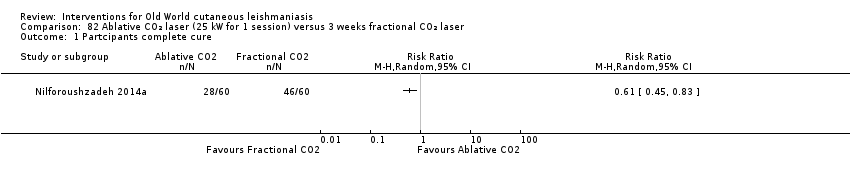
Comparison 82 Ablative CO₂ laser (25 kW for 1 session) versus 3 weeks fractional CO₂ laser, Outcome 1 Partcipants complete cure.
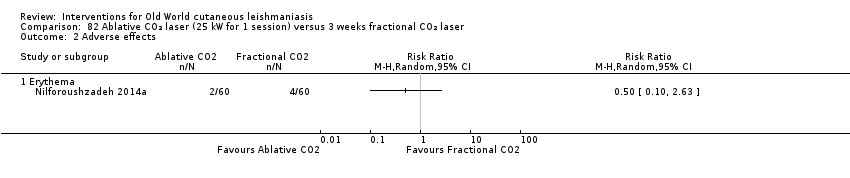
Comparison 82 Ablative CO₂ laser (25 kW for 1 session) versus 3 weeks fractional CO₂ laser, Outcome 2 Adverse effects.

Comparison 83 TCA (50% wt/vol) fortnightly up to 3 times versus ILMA alone (weekly for up to 6 weeks), Outcome 1 Participants complete cure.
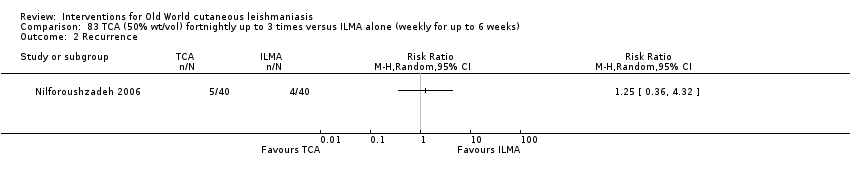
Comparison 83 TCA (50% wt/vol) fortnightly up to 3 times versus ILMA alone (weekly for up to 6 weeks), Outcome 2 Recurrence.

Comparison 83 TCA (50% wt/vol) fortnightly up to 3 times versus ILMA alone (weekly for up to 6 weeks), Outcome 3 Adverse effects.

Comparison 83 TCA (50% wt/vol) fortnightly up to 3 times versus ILMA alone (weekly for up to 6 weeks), Outcome 4 Microbiological cure of skin lesions.
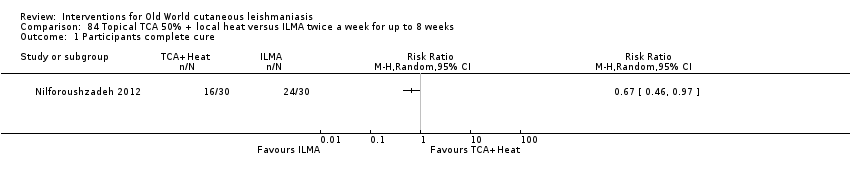
Comparison 84 Topical TCA 50% + local heat versus ILMA twice a week for up to 8 weeks, Outcome 1 Participants complete cure.
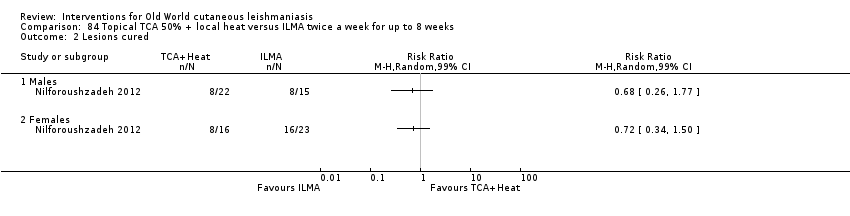
Comparison 84 Topical TCA 50% + local heat versus ILMA twice a week for up to 8 weeks, Outcome 2 Lesions cured.

Comparison 85 TCA + ILMA (weekly for up to 8 weeks) versus ILMA alone (twice a week for up to 8 weeks), Outcome 1 Participants complete cure.

Comparison 85 TCA + ILMA (weekly for up to 8 weeks) versus ILMA alone (twice a week for up to 8 weeks), Outcome 2 Speed of healing (weeks).
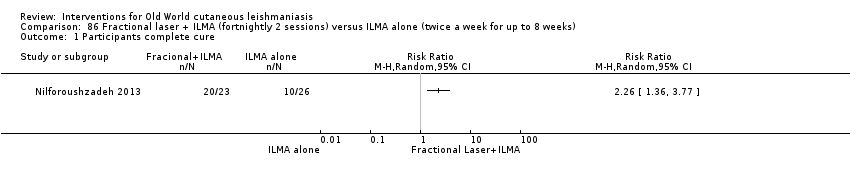
Comparison 86 Fractional laser + ILMA (fortnightly 2 sessions) versus ILMA alone (twice a week for up to 8 weeks), Outcome 1 Participants complete cure.

Comparison 87 TCA + ILMA (weekly for up to 8 weeks) versus fractional laser + ILMA (fortnightly 2 sessions), Outcome 1 Participants complete cure.

Comparison 87 TCA + ILMA (weekly for up to 8 weeks) versus fractional laser + ILMA (fortnightly 2 sessions), Outcome 2 Speed of healing (weeks).

Comparison 88 TCA fortnightly up to 8 weeks + ILMA (twice a week) versus ILMA alone (weekly for up to 8 weeks), Outcome 1 Participants complete cure.
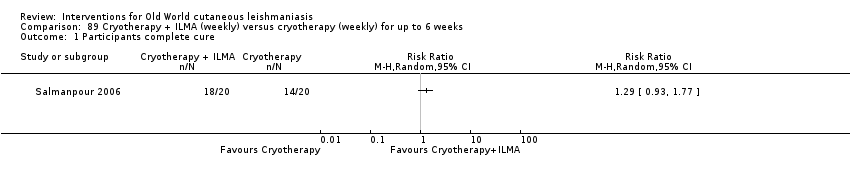
Comparison 89 Cryotherapy + ILMA (weekly) versus cryotherapy (weekly) for up to 6 weeks, Outcome 1 Participants complete cure.

Comparison 89 Cryotherapy + ILMA (weekly) versus cryotherapy (weekly) for up to 6 weeks, Outcome 2 Adverse effects.
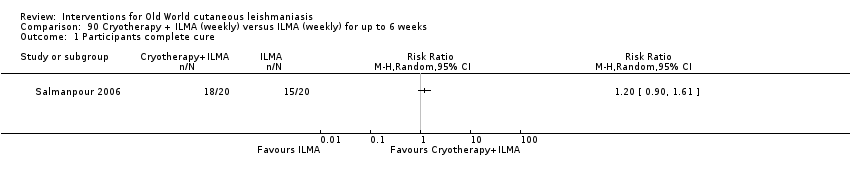
Comparison 90 Cryotherapy + ILMA (weekly) versus ILMA (weekly) for up to 6 weeks, Outcome 1 Participants complete cure.

Comparison 90 Cryotherapy + ILMA (weekly) versus ILMA (weekly) for up to 6 weeks, Outcome 2 Adverse effects.
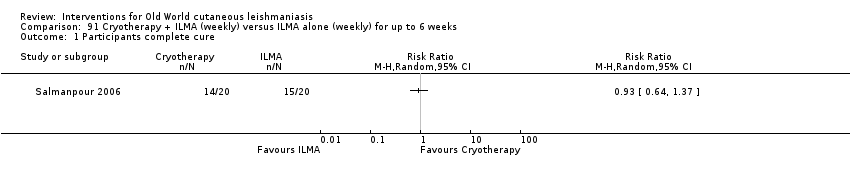
Comparison 91 Cryotherapy + ILMA (weekly) versus ILMA alone (weekly) for up to 6 weeks, Outcome 1 Participants complete cure.
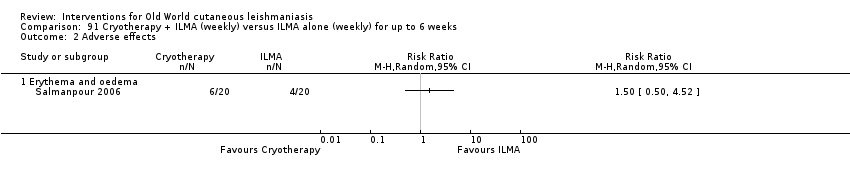
Comparison 91 Cryotherapy + ILMA (weekly) versus ILMA alone (weekly) for up to 6 weeks, Outcome 2 Adverse effects.

Comparison 92 Cryotherapy (weekly) versus ILMA (weekly) for up to 6 weeks, Outcome 1 Participants complete cure.
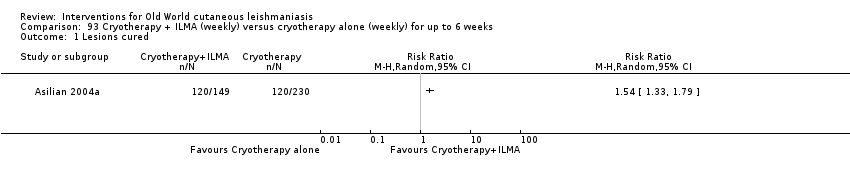
Comparison 93 Cryotherapy + ILMA (weekly) versus cryotherapy alone (weekly) for up to 6 weeks, Outcome 1 Lesions cured.

Comparison 93 Cryotherapy + ILMA (weekly) versus cryotherapy alone (weekly) for up to 6 weeks, Outcome 2 Adverse effects.

Comparison 94 Cryotherapy + ILMA (weekly) versus ILMA (fortnightly) for up to 6 weeks, Outcome 1 Lesions cured.

Comparison 94 Cryotherapy + ILMA (weekly) versus ILMA (fortnightly) for up to 6 weeks, Outcome 2 Adverse effects.
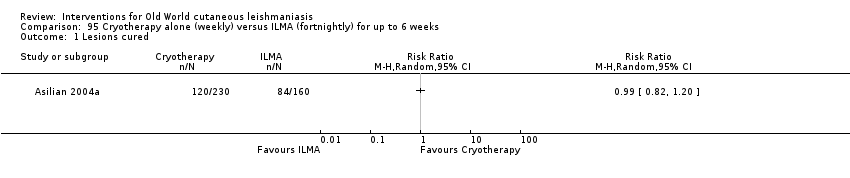
Comparison 95 Cryotherapy alone (weekly) versus ILMA (fortnightly) for up to 6 weeks, Outcome 1 Lesions cured.

Comparison 95 Cryotherapy alone (weekly) versus ILMA (fortnightly) for up to 6 weeks, Outcome 2 Adverse effects.

Comparison 96 Cryotherapy (fortnightly) + 15% paromomycin + 10% urea cream (twice a day) + ILMA (twice a day for 4 weeks) versus ILMA (twice a week) for up to 6 weeks, Outcome 1 Participants complete cure.

Comparison 97 Cryotherapy (weekly) + 3% salicylic + 3% sodium nitrite cream (twice a day) for up to 12 weeks versus cryotherapy (weekly) + 3% salicylic cream (twice a day), Outcome 1 Lesions cured.
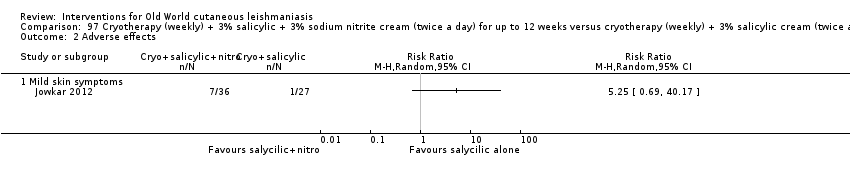
Comparison 97 Cryotherapy (weekly) + 3% salicylic + 3% sodium nitrite cream (twice a day) for up to 12 weeks versus cryotherapy (weekly) + 3% salicylic cream (twice a day), Outcome 2 Adverse effects.
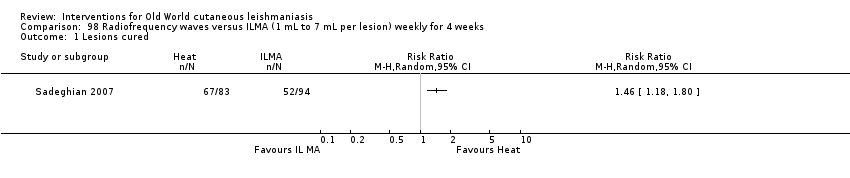
Comparison 98 Radiofrequency waves versus ILMA (1 mL to 7 mL per lesion) weekly for 4 weeks, Outcome 1 Lesions cured.
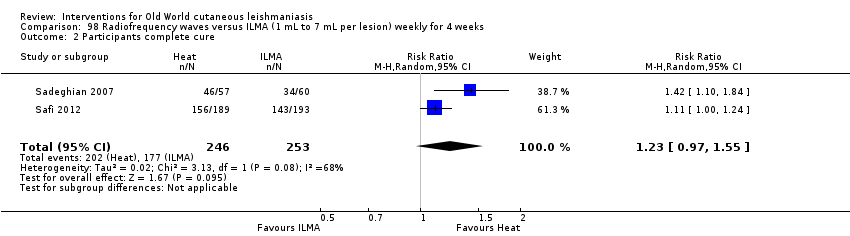
Comparison 98 Radiofrequency waves versus ILMA (1 mL to 7 mL per lesion) weekly for 4 weeks, Outcome 2 Participants complete cure.
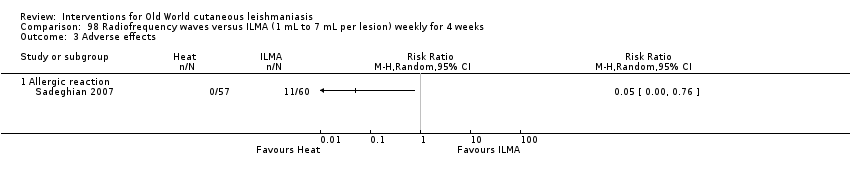
Comparison 98 Radiofrequency waves versus ILMA (1 mL to 7 mL per lesion) weekly for 4 weeks, Outcome 3 Adverse effects.

Comparison 99 Radiofrequency waves (50 uCTM applied for 30 s) versus ILSSG (10 days of 20 mg/kg/d), Outcome 1 Lesions cured.

Comparison 99 Radiofrequency waves (50 uCTM applied for 30 s) versus ILSSG (10 days of 20 mg/kg/d), Outcome 2 Adverse effects (serious).

Comparison 100 Radiofrequency waves (1 treatment of > 1 consecutive application at 50ºC for 30 s) versus IMSSG (20 mg/kg/d for 3 weeks), Outcome 1 Participants complete cure.

Comparison 100 Radiofrequency waves (1 treatment of > 1 consecutive application at 50ºC for 30 s) versus IMSSG (20 mg/kg/d for 3 weeks), Outcome 2 Adverse event (secondary infection).
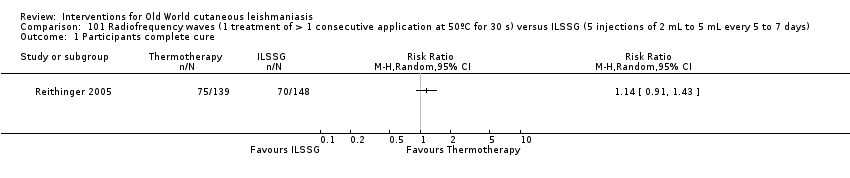
Comparison 101 Radiofrequency waves (1 treatment of > 1 consecutive application at 50ºC for 30 s) versus ILSSG (5 injections of 2 mL to 5 mL every 5 to 7 days), Outcome 1 Participants complete cure.

Comparison 101 Radiofrequency waves (1 treatment of > 1 consecutive application at 50ºC for 30 s) versus ILSSG (5 injections of 2 mL to 5 mL every 5 to 7 days), Outcome 2 Adverse event (secondary infection).

Comparison 102 Radiofrequency waves versus ILSSG, Outcome 1 Participants complete cure.
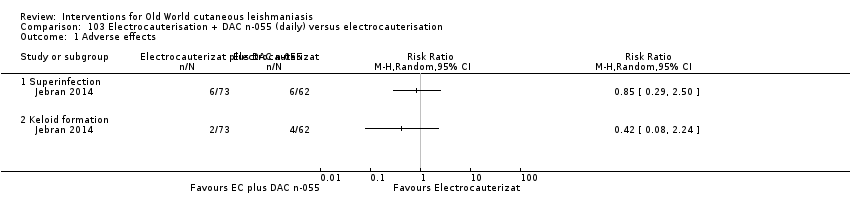
Comparison 103 Electrocauterisation + DAC n‐055 (daily) versus electrocauterisation, Outcome 1 Adverse effects.
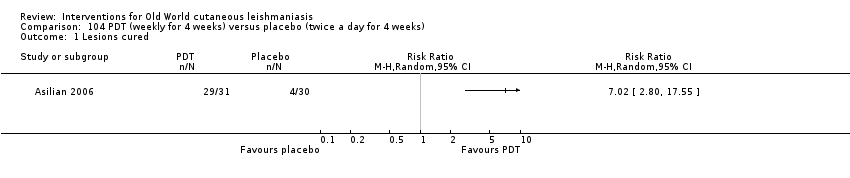
Comparison 104 PDT (weekly for 4 weeks) versus placebo (twice a day for 4 weeks), Outcome 1 Lesions cured.

Comparison 104 PDT (weekly for 4 weeks) versus placebo (twice a day for 4 weeks), Outcome 2 Scarring.

Comparison 104 PDT (weekly for 4 weeks) versus placebo (twice a day for 4 weeks), Outcome 3 Microbiological cure of skin lesions.

Comparison 105 Mesotherapy gun (0.5 mL of MA weekly) versus ILMA (0.1 mL weekly) for up to 6 weeks, Outcome 1 Participants complete cure.
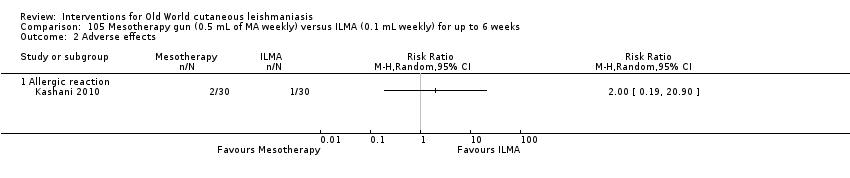
Comparison 105 Mesotherapy gun (0.5 mL of MA weekly) versus ILMA (0.1 mL weekly) for up to 6 weeks, Outcome 2 Adverse effects.

Comparison 105 Mesotherapy gun (0.5 mL of MA weekly) versus ILMA (0.1 mL weekly) for up to 6 weeks, Outcome 3 Development of cell‐mediated immunity.

Comparison 106 Diminazene aceturate solution (weekly) versus cetrimide + chlorhexidine solution for 50 d, Outcome 1 Participants complete cure.
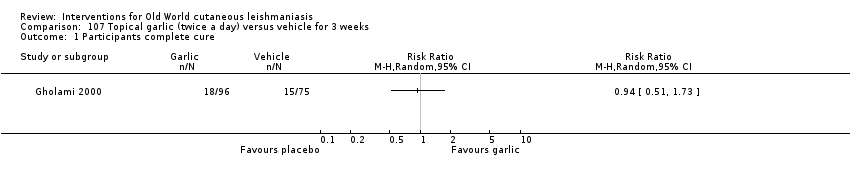
Comparison 107 Topical garlic (twice a day) versus vehicle for 3 weeks, Outcome 1 Participants complete cure.

Comparison 108 Topical herbal extract + placebo (5 d) versus IMMA (15‐20/mg/kg/d) + vehicle for 20 d, Outcome 1 Participants complete cure.
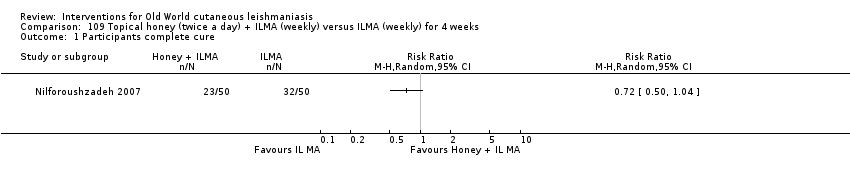
Comparison 109 Topical honey (twice a day) + ILMA (weekly) versus ILMA (weekly) for 4 weeks, Outcome 1 Participants complete cure.
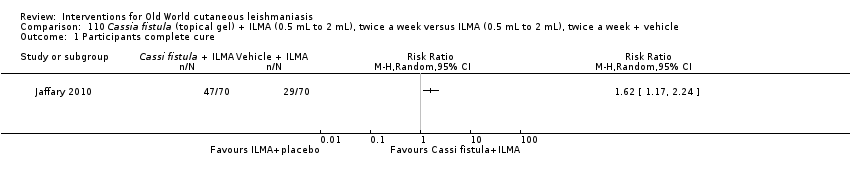
Comparison 110 Cassia fistula (topical gel) + ILMA (0.5 mL to 2 mL), twice a week versus ILMA (0.5 mL to 2 mL), twice a week + vehicle, Outcome 1 Participants complete cure.

Comparison 110 Cassia fistula (topical gel) + ILMA (0.5 mL to 2 mL), twice a week versus ILMA (0.5 mL to 2 mL), twice a week + vehicle, Outcome 2 Adverse effects.

Comparison 111 Cassia fistula boiled (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 1 Participants complete cure.

Comparison 111 Cassia fistula boiled (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 2 Speed of healing (weeks).

Comparison 111 Cassia fistula boiled (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 3 Adverse effects.
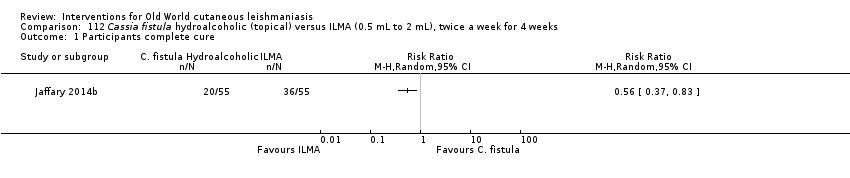
Comparison 112 Cassia fistula hydroalcoholic (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 1 Participants complete cure.

Comparison 112 Cassia fistula hydroalcoholic (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 2 Speed of healing (weeks).

Comparison 112 Cassia fistula hydroalcoholic (topical) versus ILMA (0.5 mL to 2 mL), twice a week for 4 weeks, Outcome 3 Adverse reaction.

Comparison 113 Cassia fistula boiled (topical) versusC fistula hydroalcoholic (topical) for 4 weeks, Outcome 1 Participants complete cure.
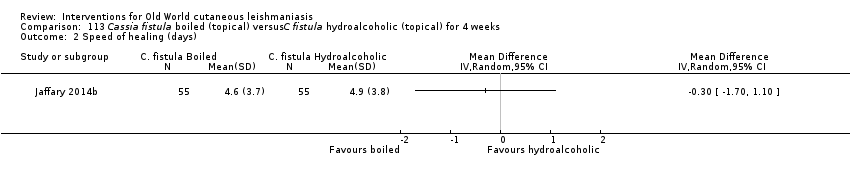
Comparison 113 Cassia fistula boiled (topical) versusC fistula hydroalcoholic (topical) for 4 weeks, Outcome 2 Speed of healing (days).

Comparison 113 Cassia fistula boiled (topical) versusC fistula hydroalcoholic (topical) for 4 weeks, Outcome 3 Adverse effects.
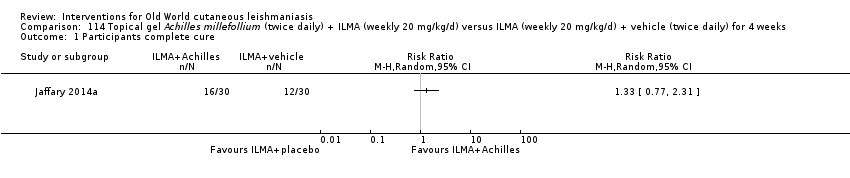
Comparison 114 Topical gel Achilles millefollium (twice daily) + ILMA (weekly 20 mg/kg/d) versus ILMA (weekly 20 mg/kg/d) + vehicle (twice daily) for 4 weeks, Outcome 1 Participants complete cure.

Comparison 114 Topical gel Achilles millefollium (twice daily) + ILMA (weekly 20 mg/kg/d) versus ILMA (weekly 20 mg/kg/d) + vehicle (twice daily) for 4 weeks, Outcome 2 Adverse effects.

Comparison 114 Topical gel Achilles millefollium (twice daily) + ILMA (weekly 20 mg/kg/d) versus ILMA (weekly 20 mg/kg/d) + vehicle (twice daily) for 4 weeks, Outcome 3 Microbiological cure of skin lesions.
| Itraconazole (200 mg for 6‐8 weeks) versus placebo for Old World cutaneous leishmaniasis | ||||||
| Patient or population: patients with Old World cutaneous leishmaniasis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Itraconazole (200 mg for 6‐8 weeks) | |||||
| Percentage of lesions cured after the end of treatment | Not measured in this comparison | |||||
| Percentage of participants with complete cure | Study population | RR 3.70 | 244 | ⊕⊝⊝⊝ | — | |
| 454 per 1000 | 1000 per 1000 | |||||
| Moderate | ||||||
| 100 per 1000 | 370 per 1000 | |||||
| Adverse effects Mild abdominal pain and nausea Adverse effects Mild abnormal liver function | 40 per 1000 0 per 1000 | 95 per 1000 0 per 1000 | RR 2.36 RR 3.08 | 204 84 | ⊕⊝⊝⊝ ⊕⊝⊝⊝ | — |
| Speed of healing (time taken to be 'cured') | Neither of the studies reported speed of healing (time taken to be 'cured') in this comparison. | |||||
| Microbiological or histopathological cure of skin lesions | Not estimable | Not estimable | RR 17.00 | 20 | ⊕⊝⊝⊝ | There were zero events in the placebo group |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded by 4 levels due to: risk of bias (2 RCTs have many uncertain items), inconsistency (there is considerable heterogeneity ‐ I² = 73%), and imprecision (2 levels due to wide 95% confidence intervals, crossing the line of no effect). | ||||||
| Paromomycin ointment versus matched vehicle for Old World cutaneous leishmaniasis | |||||
| Patient or population: patients with Old World cutaneous leishmaniasis | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Vehicle | Paromomycin ointment (15% + 10% urea) twice daily for 14 days | ||||
| Percentage of lesions cured after the end of treatment | Not measured in this comparison | ||||
| Percentage of participants with complete cure | Study population | RR 1.00 | 383 | ⊕⊝⊝⊝ | |
| 623 per 1000 | 623 per 1000 | ||||
| Moderate | |||||
| 619 per 1000 | 619 per 1000 | ||||
| Adverse effects Skin/local reactions | Study population | RR 1.42 | 713 | ⊕⊝⊝⊝ | |
| 96 per 1000 | 136 per 1000 | ||||
| Moderate | |||||
| 90 per 1000 | 128 per 1000 | ||||
| Speed of healing (time taken to be 'cured') | Not measured in this comparison | ||||
| Microbiological or histopathological cure of skin lesions | Study population | RR 1.03 | 383 | ⊕⊝⊝⊝ | |
| 859 per 1000 | 884 per 1000 | ||||
| Moderate | |||||
| 792 per 1000 | 816 per 1000 | ||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| aDowngraded by 4 levels due to risk of bias (1 RCT has many uncertain risks), indirectness (2 levels because one of the studies focused on young people), and imprecision (the confidence interval around the estimate risk ratio ranges from a 14% reduction to a 17% increase in the risk ratio for healing with paromomycin). | |||||
| Term | Definition |
| Antimonials | Pharmaceutical agents containing antimony. Antimony‐containing compounds (meglumine antimoniate and sodium stibogluconate) are the principal medications used to treat leishmaniases, an infection caused by a protozoan parasite. |
| Arthralgia | Pain in the joints. The causes of arthralgia are varied and range, from a joints perspective, from degenerative and destructive processes such as osteoarthritis and sports injuries to inflammation of tissues surrounding the joints, such as bursitis. |
| Cardiac arrhythmia | An arrhythmia is an abnormal heart rhythm. Many types of arrhythmia have no symptoms. When symptoms are present these may include palpitations or feeling a pause between heartbeats. More seriously there may be lightheadedness, passing out, shortness of breath, or chest pain. |
| Cutaneous necrosis | The death of living tissues in response to disease or injury. |
| Cytolysis | The degeneration or dissolution of cell caused by the disruption of cell membrane. |
| Exudate | A fluid with a high content of protein and cellular debris that has escaped from blood vessels and has been deposited in tissues or on tissue surfaces, usually as a result of inflammation. |
| Human monocytes | Monocytes are the biggest type of white blood cell in the immune system. Originally formed in the bone marrow, they are released into our blood and migrate into the connective tissue where they differentiate into macrophages. When certain germs enter the body, they quickly rush to the site of attack. |
| Hypotension | A systolic blood pressure reading (the top number) of 90 millimetres of mercury (mmHg) or less a diastolic blood pressure reading (the bottom number) of 60 mmHg or less is generally considered low blood pressure. The causes of low blood pressure can range from dehydration to serious medical or surgical disorders. |
| Immune response modifier | Any of a broad family of biomolecules that up‐ or down‐regulate, or restore immune responsiveness, which are generated after T cells recognise an antigen present on the surface of a self‐antigen‐presenting cell, which, once activated, produce multiple cytokines. |
| Immunolabeling | A biochemical process that enables the detection and localisation of an antigen to a particular site within a cell, tissue, or organ. Antigens are organic molecules, usually proteins, capable of binding to an antibody. These antigens can be visualised using a combination of antigen‐specific antibodies as well as a means of detection, called a tag, that is covalently linked to the antibody. If the immunolabeling process is meant to reveal information about a cell or its substructures, the process is called immunocytochemistry. Immunolabeling of larger structures is called immunohistochemistry. |
| In vitro | Biological processes or reactions made to occur outside the living organism in an artificial environment, such as a culture medium. |
| Intralesional meglumine antimoniate | Meglumine antimoniate (or Glucantime) is a medicine used for treating leishmaniasis. It belongs to a group of compounds known as the pentavalent antimonials. |
| Lymphadenopathies | Lymph nodes that have an abnormal in size, number or consistency; often used as a synonym for swollen or enlarged lymph nodes. Common causes of lymphadenopathy are infection, autoimmune disease, or malignancy. |
| Lymphatic channels | The vessels that transport lymph throughout the body. Lymph is a clear fluid that contains cells important for forming antibodies that fight infection. |
| Lymphokine | Any of various soluble protein mediators released by sensitised lymphocytes on contact with antigen, and believed to play a role in macrophage activation, lymphocyte transformation, and cell‐mediated immunity. They regulate immune responses through differentiation, amplification, and inhibition of cell functions. Lymphokines may also have a cytotoxic effector function. Used as biologic response modifiers in the treatment of cancer. |
| Macrophages | White blood cells (activated monocytes) that protect the body against infection and foreign substances by breaking them down into antigenic peptides recognised by circulating T cells. |
| Miltefosine | An oral alkyl phosphocholine analogue used to treat cutaneous and visceral leishmaniasis. Interacts with lipids and sterols in the Leishmania membrane resulting in inhibition of mitochondria and apoptotic cell death. |
| Mucous membranes | The mucous membranes (or mucosae or mucosas; singular mucosa) are linings of mostly endodermal origin, covered in epithelium, which are involved in absorption and secretion. They line cavities that are exposed to the external environment and internal organs. |
| Myalgia | Myalgia, or muscle pain, is a symptom of many diseases and disorders. The most common causes are the overuse or over‐stretching of a muscle or group of muscles. Myalgia without a traumatic history is often due to viral infections. Long‐term myalgias may be indicative of a metabolic myopathy, some nutritional deficiencies or chronic fatigue syndrome. |
| Nodular lymphangitis | Nodular lymphangitis is a distinct clinical entity, separate from lymphangitis. This disorder is characterised by inflammatory nodules along the lymphatics draining a primary skin infection |
| Papule | A solid, rounded growth that is elevated from the skin, usually inflammatory but nonsuppurative. A papule is usually less than 1 cm across. |
| Parenteral | Administration of a medicinal or therapeutic substance, other than through the gastrointestinal or respiratory tracts, e.g. by intravenous, intramuscular or subcuticular injection. |
| Pentamidine | Pentamidine (e.g. isethionate) is an antiprotozoal and antifungal agent of the class of aromatic diamidines, administered intravenously or intramuscularly in treatment of early African trypanosomiasis and leishmaniasis, and intravenously, intramuscularly, or by oral inhalation in treatment and prophylaxis of Pneumocystis carinii pneumonia. |
| Pentavalent antimony | Pentavalent antimonials are a group of compounds used for the treatment of leishmaniasis. The first pentavalent antimonial used was urea stibamine: first introduced in the 1930s, it fell out of favour in the 1950s due to higher toxicity compared to sodium stibogluconate. The compounds currently available for clinical use are: sodium stibogluconate (Pentostam; manufactured by GlaxoSmithKline; available in the USA and UK), which is administered by slow intravenous injection, intralesional or intramuscular injection, and meglumine antimoniate (Glucantime; manufactured by Aventis; available in Brazil, France and Italy), which is administered by intramuscular, intralesional, or intravenous injection. |
| Promastigotes | Term now generally used instead of 'leptomonad' or 'leptomonad stage' to avoid confusion with the flagellate genus Leptomonas. It denotes the flagellate stage of a trypanosomatid protozoan in which the flagellum arises from a kinetoplast in front of the nucleus and emerges from the anterior end of the organism; usually an extracellular phase, as in the insect intermediate host (or in culture) of Leishmania parasites. |
| Protozoan | Any of a group of single‐celled, usually microscopic, eukaryotic organisms, such as amoebas, ciliates, flagellates, and sporozoans. |
| ThermoMed device | The ThermoMed is a battery‐operated device that delivers precisely controlled localised current field radiofrequency heat to selectively destroy certain diseased tissue and is recommended by the World Health Organization as an alternative therapy for cutaneus leishmaniasis. |
| Thermotherapy | The treatment of disease by the application of heat. Thermotherapy may be administered as dry heat with heat lamps, diathermy machines, electric pads, or hot water bottles or as moist heat with warm compresses or immersion in warm water. Warm soaks or compresses may be used to treat local infections, relax muscles and relieve pain in patients with motor problems, and promote circulation in peripheral vascular disorders such as thrombophlebitis. |
| Drug | Doses |
| Systemic antimonials | |
| Sodium stibogluconate (Pentostam, Stibanate) Meglumine antimonate (Glucantime) Combined with pentoxifylline | 20 mgSb v+/kg/d intramuscularly or intravenously for 20‐30 days 400 mg orally 3 times a day for 10–20 days |
| Intralesional antimonials | |
| Sodium stibogluconate (Pentostam, Stibanate) Meglumine antimonate (Glucantime) | 1–5 mL per session every 3–7 days. Up to 10 sessions depending on the clinical response, but most patients require ≤ 5 sessions |
| Non‐antimonial systemic treatments | |
| Fluconazole | 200 mg orally daily for 6 weeks |
| Miltefosine | 50 mg orally three times daily for 28 days |
| Liposomal amphotericin B | 3 mg/kg/d IV on days 1‐5 and 10 (18 mg/kg total dose) |
| Non‐antimonial topical or intralesional therapies | |
| 15% paromomycin/12% methylbenzethonium chloride | Ointment twice daily for 10‐20 days |
| 15% paromomycin/0.5% gentamicin sulphate | Twice a day for 20 days |
| Physical therapies | |
| Cryotherapy with liquid nitrogen | Frozen for 10‐30 s and thaw applied locally 2‐3 times in each session, repeated every 1‐4 weeks to complete healing (usually 2‐4 sessions) |
| Local heat therapy | 50°‐55ºC for 30 s by: Infrared light Direct current electrical stimulation Ultrasound Laser Radiofrequency waves ThermoMed device |
| Study | Method of assessment | Timing | Interventions | Adverse effects |
| Quote: "Biochemical tests were done to detect any toxic effects of the drug." | Biochemical tests were done at the end of 1 week, 2 weeks and 4 weeks post‐ treatment. | I1: oral rifampicin 1200 mg/d I2: placebo | Intervention 23 participants evaluated for AEs. Quote: "The drug was well‐tolerated and no side‐effects were seen in any participant." Placebo 23 participants evaluated for AEs. Not reported | |
| Quote: "clinical examination, liver function tests, renal function tests" | Quote: "Before, during, and after completion of treatment" | I1: oral rifampicin 10 mg/kg/d I2: placebo | Intervention 46 participants evaluated for AEs. Elevation liver enzymes: 1 (2%) Placebo 16 participants evaluated for AEs. Not reported | |
| Haemoglobin, leukocyte count, and liver test | Biochemical tests were done at the end of 2 week, 4 weeks and 6 weeks post‐treatment | I1: oral rifampicin + omeprazole I2: placebo | Intervention 1 23 participants evaluated for AEs. Intervention 2 21 participants evaluated for AEs. Quote: "All participants tolerated the drug and placebo very well and no side effect was reported." | |
| Not described | Azythromycin group: monthly up to 4 months | I1: azithromycin 500 mg/d I2: IMMA 60 mg/kg/d | Intervention 1 22 participants evaluated for AEs (35 lesions). Nausea and vomiting: 2 (9%) Intervention 2 27 participants evaluated for AEs (58 lesions). Myalgia: 3 (11%); Erythema: 1 (3.7%). | |
| Quote: "Complete haemogram, including haemoglobin and liver and renal function tests Participants were questioned about expected adverse effects for 3 days (Days 5–7) following administration of the doses." | Haemogram: 1 and 2 months Clinical AEs: days 5‐7; 19‐21; 33‐35; 47‐19. | I1: artesunate I2: placebo | Intervention 1 20 participants evaluated for AEs. Placebo 21 participants evaluated for AEs. Skin rash with itching: 1 (4.7%) Quote: "There was no significant difference in biological tests (liver and renal function tests) in all the participants before and after treatment." | |
| Interview, physical examination, laboratory test, evaluation for pain, standardised questionnaire for the occurrence of systemic side effects (e.g. vertigo, tinnitus). Diminished hearing was verified with audiometer. Laboratory test. | Quote: "Investigators observed each participant each day that the topical creams were administered and at follow‐up study visits (days 50‐100‐180). Clinical and laboratory evidence of side effects was determined on D10 and D20." | I1: WR 279,396 I2: placebo | Intervention 50 participants evaluated for AEs. Erythema at the site of application: 15 (30%); mild pain within 30 minutes of application: 7 (14 %); mild increases and decreases in hearing acuity from baseline: 14 (28%); change hearing acuity: 14 (28%); vertigo: 0 (0%); Increase serum creatinine: 0 (0%); Death: 0 (0%) Placebo 42 participants evaluated for AEs. Erythema at the site of application: 10 (24%); mild pain within 30 minutes of application: 6 (14 %); mild increases and decreases in hearing acuity from baseline: 9 (21%); change hearing acuity: 9 (21%); vertigo: 0 (0%); increase serum creatinine: 0 (0%); death: 0 (0%) | |
| Quote: "Participants were interviewed and underwent laboratory tests three times" | Quote: "In Allopurinol group, the participants which were visited and received medication underwent laboratory tests three times (before, one month a2fter, and end of the treatment) | I1: azithromycin + allopurinol I2: IMMA | Intervention 1 36 participants evaluated for AEs. Gastrointestinal complaints and headache severe: 1 (2.7%); slight gastrointestinal complications (nausea, heartburn, and epigastric pain): 3 (8.3%) Intervention 2 35 participants evaluated for AEs. Myalgia: 2 (5.7%) | |
| AE: adverse effect; IMMA: intramuscular meglumine antimoniate. | ||||
| Study | Method of assessment | Timing | Interventions | Adverse effects |
| Clinical evaluation and laboratory tests | Days 15, 45 and 105 | I1: paromomycin I2: placebo | 126 participants evaluated for AEs. During treatment: oedema, local pain, vesiculation: 1 (0.7%) After treatment: redness, pain, vesiculation, and inflammation: 8 (6.3%) Quote: "There were no significant differences in four laboratory test results of safety (SGOT, BUN, Hb, and WBC) between the groups either before or after treatment." | |
| Clinical evaluation, physical examination, advice to participants, laboratory test: liver function, haemoglobin and white blood cell count | Days 15, 45 and 105 | I1: paromomycin I2: placebo | 57 participants evaluated for AEs. Quote: "A local reaction (inflammation, vesication, pain and/or red ness) was recorded for 12 participants, with no significant difference between the 2 groups." Laboratory test changes: 0 (0%) | |
| Not described | At the end of treatment (day 30) and 1 month post‐treatment | I1: paromomycin + MBCL I2: oral ketoconazole | 40 participants (62 lesions) evaluated for AEs Quote: "Treatment‐related adverse effects were only observed in the paromomycin group. The most common side‐effect was the development of irritant contact dermatitis. No subjects withdrew because of this adverse effect." | |
| Clinical evaluation | Days 15, 29, 45 and 105 | I1: paromomycin I2: placebo | 108 participants evaluated for AEs. Quote: "Treatment was well tolerated, and no adverse reactions to the ointment were observed or reported in either group." | |
| Not described | Quote "Clinical evaluation and follow‐up were performed fortnightly until 1 month post treatment and then monthly until 3 months post treatment, and finally every 3 months until 1 year post treatment" | I1: paromomycin + urea I2: ILMA weekly | Not described | |
| Not described | Week 1 and week 6 post‐treatment and at 6 months after treatment was completed | I1: paromomycin + urea I2: ILMA weekly | 30 participants evaluated for AEs. Cutaneous reactions (erythematosus, urticaria or lymphadenitis with pain): 1 (3%) Quote: "No systemic toxic reaction attributable to the drug was observed." | |
| Clinical evaluation | Days 7, 14, 21 and 30 | I1: paromomycin I2: placebo | 30 participants evaluated for AEs. Mild contact dermatitis: 3 (10%) | |
| Not described | Weekly during treatment and monthly for up 2 months | I1: photodynamic therapy I2: paromomycin I3: placebo | 19 participants (34 lesions) evaluated for AEs. Quote: "Adverse side‐effects seen in some participants in all groups were pruritus, burning, redness, discharge, oedema, and pain, but all were generally mild and tolerable." | |
| Quote: "Renal toxic effects and ototoxic effects from aminoglycoside exposure were ascertained by means of serum creatinine measurements at the end of therapy (at 20 days) and participants' daily reports of tinnitus and vertigo." | Quote: "Safety end points were assessed daily during therapy (20 days)." | I1:Paromomycin ‐Gentamicin I2: paromomycin Alone I3: vehicle Control | Intervention 1: 125 participants evaluated for AEs. Erythema: 6 (5%); local infection: 0 (0%); inflammation: 0 (0%); vesicles mild‐moderate: 31 (25%); mild oedema: 2 (2%); pain: 2 (2%); mild bronchitis: 5 (4%); paronychia: 2 (2%); superinfection: 3 (2%); upper respiratory tract infection: 0 (0%); oropharyngeal pain: 4 (3%); skin irritation: 3 (2%); tinnitus: 0 (0%); vertigo: 0 (0%); creatinine serum changes: 0 (0%) Intervention 2: 125 participants evaluated for AEs. Erythema: 7 (6%); local infection: 0 (0%); inflammation: 0 (0%); vesicles mild‐moderate: 32 (26%); mild‐moderate oedema: 3 (3%); pain: 2 (2%); bronchitis mild‐moderate: 3 (3%); paronychia: 0 (0%); superinfection: 0 (0%); upper respiratory tract infection: 2 (2%); oropharyngeal pain: 3 (2%); skin irritation: 9 (7%); tinnitus: 0 (0%); vertigo: 0 (0%); creatinine serum changes: 0 (0%) | |
| AE: adverse effect; BUN: blood urea nitrogen; Hb: haemoglobin; ILMA: intralesional meglumine antimoniate; SGOT: serum glutamic‐oxaloacetic transaminase; WBC: white blood cells. | ||||
| Study | Method of assessment | Timing | Interventions | Adverse effects |
| Not described | Quote: "Participants were seen at 10‐15 day intervals after injection, and at 6 weeks post treatment" | I1: IL 2% zinc sulphate I2: IL 7% sodium chloride I3: ILSSG 2‐5 mL per lesion | 19 participants evaluated for AEs. Quote: "Apart from pain at the time of injection, no appreciable side‐effect was noted." | |
| Not described | Not described | I1: IL zinc sulphate I2: ILMA weekly | 31 participants evaluated for AEs. Severe pain caused vasovagal shock: 2 (6.4%) | |
| Not described | Not described | I1: IL zinc sulphate I2: ILMA weekly | 36 participants evaluated for AEs. Pain: 13 (36.1%); burning at site injection: 3 (8.4%); itching: 3 (8.4%); inflammation: 7 (19.4%) | |
| Not described | 14, 28, 42, and 56 days after starting the treatment | I1: IL 2% zinc sulphate I2: ILMA weekly | 24 participants evaluated for AEs. Quote: "The side effects seen in both groups were pain after injection and hyperpigmentation." Burning after injection and necrosis of the lesions: 24 (100%); inflammation and swelling: 3 (12.5%) | |
| AE: adverse effect; IL: intralesional; ILMA: intralesional meglumine antimoniate; ILSSG: intralesional sodium stibogluconate. | ||||
| Study | Method of assessment | Timing | Interventions | Adverse effects |
| Not described | Quote: "Participants were seen at 10‐15 day intervals after injection, and at 6 week post treatment" | I1: IL 2% zinc sulphate I2: IL 7% HSCS I3: ILSSG 2‐5 mL per lesion | 17 participants evaluated for AEs. Quote: "No side‐effect other than pain at the time of injection was noted." | |
| Not described | Not described | I1: IL 5% HSCS I2: ILMA 0.5‐1 mL/week | 36 participants evaluated for AEs. Allergic reaction (erythema, oedema, and pruritus): 0 (0%); sporotrichoid dissemination: 3 (8.3%) | |
| Not described | Quote: "Participants were seen weekly for the first three injections; fortnightly for the fourth and fifth injections; then monthly until cure. Participants were followed‐up every 3 months after cure for 18 months to assess recurrences and evidence of visceralization." | I1: ILSSG I2: IL 7% HSCS | 67 participants evaluated for AEs. Leishmaniasis recidivans: 0 (0%) Quote: "There were no systemic side effects with SSG or HS. Pain during injection was the only local side effect noted with both therapies. After healing, scarring was minimal, but postinflammatory hyperpigmentation was observed in all participants for both treatments, which faded out over 6–8 months." | |
| AE: adverse effect; IL: intralesional; ILSSG: intralesional sodium stibogluconate; HSCS: hypertonic sodium chloride solution. | ||||
| Study | Method of assessment | Timing | Interventions | Adverse effects |
| Not described | 1, 3, 4, 8, 12 and 24 weeks after treatment | I1: CO₂ I2: IMMA 50 mg/kg/d | 123 participants evaluated for AEs. Quote: "Complications were seen in (4) 4.5% of participants and included hyperpigmentation, persistent redness." Hypertonic scars: 5 (4%) | |
| Quote: "Follow‐up was performed and any side‐effects were recorded." | Quote: "Follow‐up evaluation was performed by clinical assessment of treated lesions at weeks 2, 6, 12 and 16." | I1: CO₂ I2: cryotherapy + MA | 80 participants (95 lesions) evaluated for AEs. Hyperpigmentation + trivial scar: 20 (25%); atrophic scar: 7 (8.75%); hypertrophic scar: 1 (1.25%); sporotrichoid: 1 (1.25%); raised papular lesions: 1 (1.25%); persistent erythema: 3 (3.75%); hypopigmentation + trivial scar: 4 (5%) | |
| Not described | Quote: "Participants were followed in the first, third, and sixth months after treatment with the final evaluation in the sixth month." | I1: ablative CO₂ laser I2: fractional CO₂ laser | Intervention 1: 30 participants evaluated for AEs. Erythema: 2 (6.7%) Intervention 2: 30 participants evaluated for AEs. Erythema: 4 (13.3%) | |
| AE: adverse effect; IMMA: intramuscular meglumine antimoniate; MA: meglumine antimoniate. | ||||
| Study | Method of assessment | Timing | Interventions | Adverse effects |
| Not described | Fortnightly until 6 months post‐treatment and 2 weeks and 4 weeks post‐treatment | I1: cryotherapy + ILMA I2: cryotherapy alone I3: ILMA alone | Intervention 1: 100 participants evaluated for AEs. Postinflammatory hypopigmentation: 5 (5%) Intervention 2: 200 participants evaluated for AEs. Postinflammatory hypopigmentation: 10 (5%) | |
| Not described | Not described | I1: ILMA alone I2: cryotherapy alone I3: cryotherapy + ILMA | Intervention 2: 20 participants evaluated for AEs. Erythema and oedema of the lesions and perilesional area: (28%) Intervention 3: 20 participants evaluated for AEs. Erythema and oedema of the lesions and perilesional area: (33%) Quote: "There were no serious side‐effects in any of the treatment groups" | |
| Not described | Quote: "Weekly for up to six weeks of treatment and six months after." | I1: cryotherapy I2: ILMA | 36 participants evaluated for AEs. Hypopigmentation: 2 (5.5%); hyperpigmentation: 7 (19.4%). Quote: "the most common adverse reactions were erythema and oedema of the treated site, which appeared during the initial hours of treatment, and blistering of the treatment site, which became evident 1–2 days after treatment and responded well to local treatment." | |
| Quote: "Follow‐up was performed and any side‐effects were recorded." | Quote: "Follow‐up evaluation was performed by clinical assessment of treated lesions at weeks 2, 6, 12 and 16." | I1: CO₂ I2: cryotherapy + MA | 80 participants (95 lesions) evaluated for AEs. Hyperpigmentation + trivial scar: 15 (18.7%); atrophic scar: 6 (7.5%); hypertrophic scar: 0 (0%); sporotrichoid: 0 (0%); raised papular lesions: 0 (0%); persistent erythema: 0 (0%); hypopigmentation + trivial scar: 15 (18.8%) | |
| Quote: "During these visits the healing process of the ulcer, change of diameter and induration of lesions and complications were assessed." | Quote: "The participants were evaluated every 2 weeks up to 12 weeks." | I1: cryotherapy + 3% salicylic + 3% sodium nitrite I2: cryotherapy + 3% salicylic + placebo | Intervention 1: 36 participants evaluated for AEs. Erythema, a burning sensation and skin irritation: 7 (19.4%) Intervention 2: 27 participants evaluated for AEs. Erythema, a burning sensation and skin irritation: 1 (3.7%) | |
| AE: adverse effect; ILMA: intralesional meglumine antimoniate; MA: meglumine antimoniate. | ||||
| Study | Method of assessment | Timing | Interventions | Adverse effects |
| Quote: "The occurrence of adverse effects was evaluated blindly by means of participant interviews and physical examinations." | Quote: "The occurrence of adverse effects was evaluated … during follow‐up visits." | I1: ILSSG 2‐5 mL per lesion I2: IMSSG 20 mg/kg I3: thermotherapy | 138‐108 participants evaluated for AEs. Secondary infections: 8 (5.7%). Quote: "The original CL ulcer often increased in size immediately after and up to 2 weeks after treatment." | |
| Quote: "Appearance of lesions at subsequent follow‐up visits and occurrence of unwanted side‐effects were also recorded on the form." | Weekly 4 weeks and monthly up to 6 months | I1: thermotherapy I2: ILMA weekly | 57 participants (83 lesions) evaluated for AEs. Satellite lesions: 1 (1.7%) | |
| Quote: "Interview, physical examination, laboratory testing (complete blood count, creatine phosphokinase, amylase, lipase, complete metabolic profile), and electrocardiograms." | Quote: "Daily for the first 10 days and follow‐up at 2, 6, and 12–24 months post treatment" | I1: thermotherapy I2: ILSSG | 27 participants evaluated for AEs. Serious AE: 4 (15%); ECG changes: 10 (37%); abdominal discomfort: 1 (4%); wound infection: 5 (19%); musculoskeletal: 5 (19%); headache: 3 (11%); fatigue: 5 (19%); rash: 1 (4%); blister reaction: 25 (93%); erythema: 7 (26%); oozing: 21 (78%) | |
| Quote: "The occurrences of adverse effects were evaluated by means of participant interviews and physical examinations during follow‐up visits." | Quote: "During treatment, all participants were then followed for four visits at weekly intervals … After initial treatment, all participants were scheduled for four subsequent follow‐up visits: 10 days after baseline and 1‐month, 2 months and 6 months after treatment." | I1: thermotherapy I2: ILMA weekly | 189 participants evaluated for AEs Not reported | |
| Not described | Not described | I1: radiofrequency heat treatment I2: ILSSG | Quote: "RFHT was cosmetically acceptable because it was associated with less scarring and hyperpigmentation compared with intralesional SSG injections." | |
| Quote: "In case of clinical signs for a superinfection, a smear was taken, Gram stained and microscopically evaluated for the presence of bacteria and/or fungi." | Quote: "Adverse events such as bacterial or fungal superinfections of the wounds, the formation or scars and the rate of re‐ulcerations were monitored during the treatment and follow‐up period." | I1: electrocauterisation + DAC N‐055. I2: electrocauterisation + placebo. | Intervention 1: 38 participants evaluated for AEs. Bacterial and fungal superinfections: 3 (8.0%); Keloïd formation: 2 (5%) Intervention 2: 32 participants evaluated for AEs. Bacterial and fungal superinfections: 3 (9.0%); Keloïd formation: 2 (6%) | |
| AE: adverse effect; CL: cutaneous leishmaniasis; ILMA: intralesional meglumine antimoniate; ILSSG: intralesional sodium stibogluconate; IMSSG: intramuscular sodium stibogluconate. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 2 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.71, 0.96] |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Serious adverse effects | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Skin reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Cardiac toxicity 'QT prolongation' | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects (itching and burning) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Adverse effects (oedema) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects (itching and burning) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Adverse effects (oedema) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects (itching and burning) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Adverse effects (oedema) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects (mild heart symptoms) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects (nausea and vomiting) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effect (liver enzymes increase) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 3 | 244 | Risk Ratio (M‐H, Random, 99% CI) | 3.70 [0.35, 38.99] |
| 2 Adverse effects Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Mild abdominal pain and nausea | 3 | 204 | Risk Ratio (M‐H, Random, 95% CI) | 2.36 [0.74, 7.47] |
| 2.2 Mild abnormal liver function | 3 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 3.08 [0.53, 17.98] |
| 2.3 Headache and dizziness | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 2.63 [0.16, 43.63] |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| 2 Adverse effects (headache and dizziness) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Rise creatinine and liver enzymes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Cheilitis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Nausea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete Cure Show forest plot | 2 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 24.08 [1.44, 403.43] |
| 2 Adverse effects Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Nausea | 2 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 21.86 [3.04, 157.29] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 3.83 [1.71, 8.60] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 1.92 [1.08, 3.41] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions Cured Show forest plot | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.35, 1.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Mild abdominal pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Skin eruption | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Muscle pain and weakness | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | 72 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.88, 1.41] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Secondary infection | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Myalgia | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 ECG changes | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Chest pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Pain injection site | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Abscess | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Abdominal symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Liver abnormalities | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Myalgia | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Rash | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Evaluated 3 months after treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Evaluated after treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Nausea and vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Gastrointestinal complaints and headache | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Gastrointestinal complications | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Myalgia | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Allergic macule‐papular | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Nausea and vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Nausea and vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Nausea and vomiting | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure (ITT) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Hypersensitivity | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Mild pruritus | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Erithema and oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Scarring Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.25, 2.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 2 | 383 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.86, 1.17] |
| 2 Adverse effects Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Skin/local reaction | 3 | 463 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.45, 1.93] |
| 3 Microbiological cure of skin lesions Show forest plot | 2 | 383 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.88, 1.20] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Scarring Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Cutaneous reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Scarring Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Participants complete cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Adverse effects Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Burning | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Itching | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Inflammation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.5 Pruritus and erythema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.6 Severe pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Inflammation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Participants with treated lesions that recur Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Itch and burning | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Sporotrichotic dissemination | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Ulceration and necrosis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Ulceration and necrosis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| 3 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Ulceration and necrosis | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Erythema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Mild pain | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Hearing acuity problems | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Local inflammatory reactions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Reulceration | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Keloïd scars | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Reulceration | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Keloïd scars | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Reulceration | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Keloïd scars | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Dizziness and nausea | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Hypersensitive reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | 433 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.53, 1.55] |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Hyperpigmentation and redness | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Hypertrophic scarring | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Systemic symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Hyperpigmentation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Atrophic scar | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Hypopigmentation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Partcipants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Erythema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Recurrence Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Mild erythema and itch | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Microbiological cure of skin lesions Show forest plot | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.74, 1.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| 2.1 Males | 1 | Risk Ratio (M‐H, Random, 99% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Females | 1 | Risk Ratio (M‐H, Random, 99% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Erythema and oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Erythema and oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Erythema and oedema | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Hypopigmentation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Hypopigmentation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 14.64 [0.86, 247.99] |
| 2.1 Hypopigmentation | 1 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 14.64 [0.86, 247.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Mild skin symptoms | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Participants complete cure Show forest plot | 2 | 499 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.97, 1.55] |
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects (serious) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse event (secondary infection) Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse event (secondary infection) Show forest plot | 1 | Risk Ratio (M‐H, Random, 99% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Superinfection | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Keloid formation | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Lesions cured Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Scarring Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Development of cell‐mediated immunity Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Itching | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Speed of healing (weeks) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Adverse reaction Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Speed of healing (days) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Allergic reaction | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Participants complete cure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Adverse effects Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Itching | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Microbiological cure of skin lesions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |

