Técnicas para la asistencia de un parto difícil por cesárea
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised, unblinded trial. | |
| Participants | Women with prolonged obstructed labour, at full dilatation, arrest of descent greater than 1 hour and station +2, dystocia, vertex presentation. Exclusions: multiple pregnancies, fetal anomalies, previous caesarean delivery, premature delivery. | |
| Interventions | The pull method (reverse breech extraction) was compared to the push method (cephalic delivery with digital pressure via the vagina). | |
| Outcomes | Operative blood loss, uterine incision extension toward broad ligament/vagina, blood transfusion, wound infection, endometritis, bladder injury, ligation of hypogastric arteries and hysterectomy, urethral injury, prolonged hospital stay. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of randomisation process given. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) | Low risk | Anaesthetist blinded, responsible for assessment of estimated blood loss. |
| Incomplete outcome data (attrition bias) | Low risk | Nil loss apparent. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes described. |
| Other bias | Low risk | Nil other bias apparent. |
| Methods | Randomised unblinded trial, randomisation by envelope. | |
| Participants | 39 weeks' gestation, at least 1 previous caesarean delivery, cephalic presentation without fetopelvic engagement by vaginal examination, patient willingness to randomise to delivery technique. Exclusion criteria: fetal malpresentation (transverse or breech), serious maternal or fetal disease (maternal or fetal coagulopathy, fetal structural malformation or evidence of non‐reassuring fetal status), a deeply engaged fetal vertex or maternal unwillingness to undergo randomisation. | |
| Interventions | Random allocation to instrumental delivery (forceps or vacuum) or manual/fundal pressure delivery. | |
| Outcomes | Delivery as randomised, time to delivery, uterine incision extension, postoperative Hb, drop in Hb, pain scores, Apgars, cord artery pH, birthweight. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of randomisation process. |
| Allocation concealment (selection bias) | Low risk | Series of opaque manilla envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | Low risk | No loss apparent. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes described. |
| Other bias | Low risk | Nil other bias apparent. |
| Methods | Randomised, double‐blind, placebo‐controlled trial; randomisation involved computer‐generated random number sequence. | |
| Participants | Pregnant women 34‐42 weeks' gestation with singleton pregnancy and planned caesarean section. | |
| Interventions | Random allocation to 0.25 mg intravenous nitroglycerin, 0.5 mg intravenous nitroglycerin, or intravenous saline (placebo). | |
| Outcomes | Estimation of ease of fetal extraction (difficult, normal, easy); degree of uterine relaxation (none, minimal, strong, very strong); postpartum bleeding (decreased, normal, heavier); median blood loss; median change in systolic and diastolic blood pressure; median Apgar score; median cord pH; maternal side‐effects (headache, flushing, bradycardia). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Random‐number list kept away from clinical care area. |
| Blinding of participants and personnel (performance bias) | Low risk | Patients, surgical team and neonatologists were blinded, the anaesthetist was not. |
| Blinding of outcome assessment (detection bias) | Low risk | Surgeons were blinded, they performed assessment of primary outcome (ease of fetal extraction). |
| Incomplete outcome data (attrition bias) | Low risk | No loss apparent. |
| Selective reporting (reporting bias) | Low risk | No selective reporting apparent. |
| Other bias | Low risk | Nil other bias apparent. |
| Methods | Randomised unblinded trial, randomisation involved computer‐generated random number sequence. | |
| Participants | Patients with prolonged obstructed labour. Exclusion criteria: intrauterine fetal death, congenital fetal anomaly, multiple pregnancy, ruptured uterus, previous caesarean section, fetal head more than 2 finger‐breadths palpable per abdomen. | |
| Interventions | The pull method (reverse breech extraction) was compared to the push method (cephalic delivery with digital pressure via the vagina). | |
| Outcomes | Operation time, operative blood loss, degree of uterine incision extension either towards the broad ligament or vagina, Apgar scores, fetal outcome, neonatal admission rate, fetal injury during delivery, wound infection, endometritis, hospital stay and total hospital bill. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random sampling method. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | No blinding described. |
| Blinding of outcome assessment (detection bias) | Low risk | Anaesthetist blinded, responsible for assessment of estimated blood loss and operation duration. |
| Incomplete outcome data (attrition bias) | Low risk | Nil loss apparent. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes described. |
| Other bias | Low risk | Nil other bias apparent. |
| Methods | Randomised unblinded trial, no description of the randomisation process was given. | |
| Participants | Singleton, term, cephalic, obstructed labour, requiring abdominal delivery. Exclusion criteria: multiple pregnancy, non‐cephalic presentation, previous scar, preterm labour. | |
| Interventions | The pull method (reverse breech extraction) was compared to the push method (cephalic delivery with digital pressure via the vagina). | |
| Outcomes | Prespecified outcomes: frequency of uterine incision extension. Reported outcomes: uterine rupture, blood transfusion, operative time, PPH, endometritis, wound infection, mean hospital stay, mean fall in Hb, mean blood loss, Apgar score < 7, admission to nursery, stillbirth.
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Distribution of women to either group was made randomly based on 1:1 ratio', no other description given. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | No blinding described. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No blinding described. |
| Incomplete outcome data (attrition bias) | Low risk | Nil loss apparent. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes described. |
| Other bias | Low risk | Nil other bias apparent. |
| Methods | Randomised unblinded trial, randomisation involved computer‐generated consecutive numbered envelopes generated in blocks of 50. | |
| Participants | Pregnant, singleton gestation, caesarean delivery. Exclusion criteria: woman given fundal pressure in labour prior to caesarean delivery, failed operative vaginal delivery, breech presentation, known abruptios, placenta praevia, external cephalic version attempt within last 3 days. | |
| Interventions | Forceps was compared to manual delivery with fundal pressure. | |
| Outcomes | Prespecified ‐ per cent of umbilical cord blood placental alkaline phosphatase between the groups. Reported outcomes: conduction anaesthesia, low transverse uterine scar used, abdominal incision to uterine incision (minute), uterine incision to delivery (second), estimated blood loss, birthweight. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation using computer‐generated consecutive numbered envelopes generated in blocks of 50. |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes opened after consent. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No blinding described. |
| Incomplete outcome data (attrition bias) | Low risk | Nil loss apparent. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes described. |
| Other bias | Low risk | Nil other bias apparent. |
| Methods | Randomised unblinded trial, no description of the randomisation process was given. | |
| Participants | Women with singleton pregnancy at 37‐42 weeks, cephalic presentation with obstructed dystocia ‐ full cervical dilation and fetal head impacted in pelvis leading to caesarean delivery after failed attempt at operative vaginal delivery. Exclusion criteria ‐ suspected macrosomia > 4000 g, intrauterine fetal death, multiple pregnancy, previous caesarean or myomectomy, chorioamnionitis, third trimester haemorrhage. | |
| Interventions | The pull method (reverse breech extraction) was compared to the push method (cephalic delivery with digital pressure via the vagina). | |
| Outcomes | Operation time, estimated blood loss, incidence of extension of uterine incision, bladder injury, postpartum fever, postoperative wound complication. Neonatal ‐ 1 and 5 minute Apgar score, admission to NICU, fetal injury. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of randomisation process given. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not described. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No description of blinding given. |
| Incomplete outcome data (attrition bias) | Low risk | Nil loss apparent. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes described. |
| Other bias | Low risk | Nil other bias apparent. |
Hb: haemoglobin
NICU: neonatal intensive care unit
PPH: postpartum haemorrhage
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Study not yet published, contact made with author, awaiting data to be finalised. To be included next review | |
| Tocolysis used prior to caesarean section for fetal distress. | |
| Tocolysis used for intrauterine resuscitation prior to caesarean section for fetal distress. Trial used quasi‐randomised techniques (alternate month). | |
| Retrospective. | |
| Continuous tocolytic infusion used 2 hours prior to caesarean section to improve infant respiratory effort and metabolism. | |
| Assessment of anaesthetic duration, not tocolysis effect. | |
| Tocolytic agent used to prevent hypertension following intubation in hypertensive women. | |
| Not randomised. | |
| Tocolysis used prior to caesarean section for fetal distress. | |
| Tocolysis used for intrauterine resuscitation prior to caesarean section for fetal distress. | |
| Retrospective. | |
| Retrospective. | |
| Tocolysis used for intrauterine resuscitation prior to caesarean section for fetal distress. | |
| Not randomised. | |
| Tocolysis used appropriately but unable to contact author to obtain full data set. | |
| Not randomised. | |
| Email to RG Medical College in India to request data ‐ no response. | |
| Tocolysis used prior to caesarean section for fetal distress. | |
| Technique for facilitating delivery at elective caesarean section described, but unable to contact author to obtain full data set. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Maternal side‐effects (not prespecified) Show forest plot | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.1  Comparison 1 Tocolysis versus placebo, Outcome 1 Maternal side‐effects (not prespecified). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Infant birth trauma Show forest plot | 3 | 239 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.42, 5.73] |
| Analysis 2.1  Comparison 2 Reverse breech versus head push, Outcome 1 Infant birth trauma. | ||||
| 2 Extension of uterine incision Show forest plot | 4 | 357 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.13, 0.40] |
| Analysis 2.2  Comparison 2 Reverse breech versus head push, Outcome 2 Extension of uterine incision. | ||||
| 3 Blood loss > 500 mL Show forest plot | 1 | 118 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.18, 1.37] |
| Analysis 2.3  Comparison 2 Reverse breech versus head push, Outcome 3 Blood loss > 500 mL. | ||||
| 4 Mean blood loss Show forest plot | 3 | 298 | Mean Difference (IV, Random, 95% CI) | ‐294.92 [‐493.25, ‐96.59] |
| Analysis 2.4  Comparison 2 Reverse breech versus head push, Outcome 4 Mean blood loss. | ||||
| 5 Blood transfusion Show forest plot | 2 | 177 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.20, 1.66] |
| Analysis 2.5  Comparison 2 Reverse breech versus head push, Outcome 5 Blood transfusion. | ||||
| 6 Endometritis Show forest plot | 3 | 285 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.26, 1.05] |
| Analysis 2.6  Comparison 2 Reverse breech versus head push, Outcome 6 Endometritis. | ||||
| 7 Wound infection Show forest plot | 4 | 357 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.58, 1.59] |
| Analysis 2.7  Comparison 2 Reverse breech versus head push, Outcome 7 Wound infection. | ||||
| 8 Admission to neonatal special care or intensive care unit Show forest plot | 2 | 226 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.23, 1.22] |
| Analysis 2.8  Comparison 2 Reverse breech versus head push, Outcome 8 Admission to neonatal special care or intensive care unit. | ||||
| 9 Early neonatal death rate Show forest plot | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.23, 1.24] |
| Analysis 2.9  Comparison 2 Reverse breech versus head push, Outcome 9 Early neonatal death rate. | ||||
| 10 Mean fall in Hb (not prespecified) Show forest plot | 1 | 118 | Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.72, ‐0.16] |
| Analysis 2.10  Comparison 2 Reverse breech versus head push, Outcome 10 Mean fall in Hb (not prespecified). | ||||
| 11 Operative time (min) Show forest plot | 4 | 357 | Mean Difference (IV, Random, 95% CI) | ‐14.99 [‐27.67, ‐2.30] |
| Analysis 2.11  Comparison 2 Reverse breech versus head push, Outcome 11 Operative time (min). | ||||
| 12 Mean hospital stay (not prespecified) Show forest plot | 3 | 285 | Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐2.75, 0.48] |
| Analysis 2.12  Comparison 2 Reverse breech versus head push, Outcome 12 Mean hospital stay (not prespecified). | ||||
| 13 Average Apgar at 5 minutes (not prespecified) Show forest plot | 3 | 239 | Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.64, 1.36] |
| Analysis 2.13  Comparison 2 Reverse breech versus head push, Outcome 13 Average Apgar at 5 minutes (not prespecified). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Infant birth trauma Show forest plot | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 3.1  Comparison 3 Elective instrument versus fundal pressure, Outcome 1 Infant birth trauma. | ||||
| 2 Extension of uterine incision Show forest plot | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.7 [0.13, 3.73] |
| Analysis 3.2  Comparison 3 Elective instrument versus fundal pressure, Outcome 2 Extension of uterine incision. | ||||
| 3 Mean fall in Hb Show forest plot | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.53, 0.59] |
| Analysis 3.3  Comparison 3 Elective instrument versus fundal pressure, Outcome 3 Mean fall in Hb. | ||||

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Tocolysis versus placebo, Outcome 1 Maternal side‐effects (not prespecified).

Comparison 2 Reverse breech versus head push, Outcome 1 Infant birth trauma.
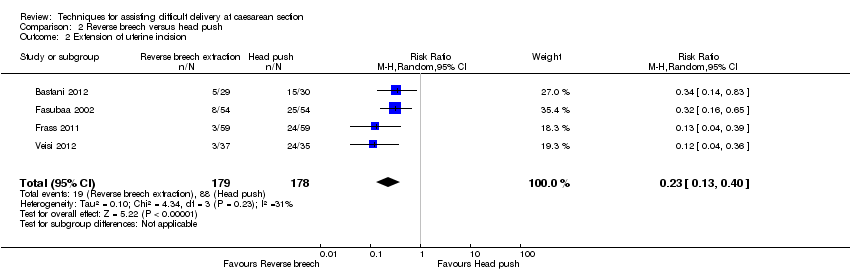
Comparison 2 Reverse breech versus head push, Outcome 2 Extension of uterine incision.
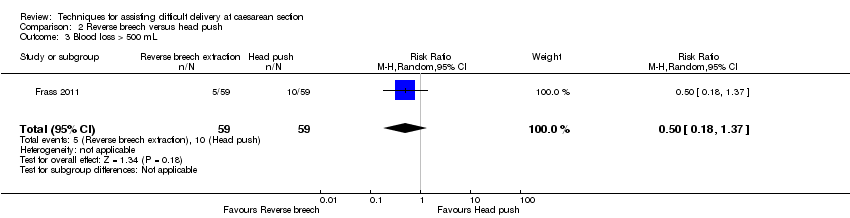
Comparison 2 Reverse breech versus head push, Outcome 3 Blood loss > 500 mL.

Comparison 2 Reverse breech versus head push, Outcome 4 Mean blood loss.

Comparison 2 Reverse breech versus head push, Outcome 5 Blood transfusion.

Comparison 2 Reverse breech versus head push, Outcome 6 Endometritis.

Comparison 2 Reverse breech versus head push, Outcome 7 Wound infection.

Comparison 2 Reverse breech versus head push, Outcome 8 Admission to neonatal special care or intensive care unit.
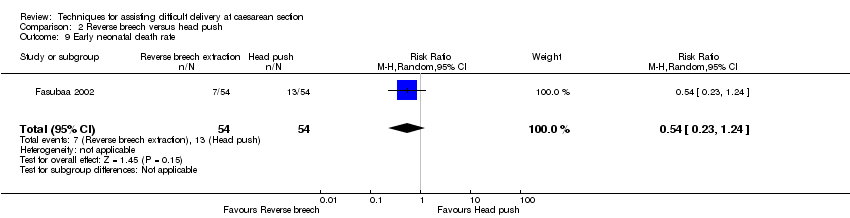
Comparison 2 Reverse breech versus head push, Outcome 9 Early neonatal death rate.

Comparison 2 Reverse breech versus head push, Outcome 10 Mean fall in Hb (not prespecified).
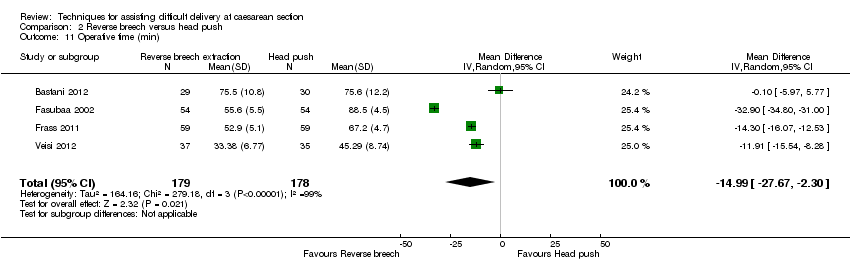
Comparison 2 Reverse breech versus head push, Outcome 11 Operative time (min).

Comparison 2 Reverse breech versus head push, Outcome 12 Mean hospital stay (not prespecified).
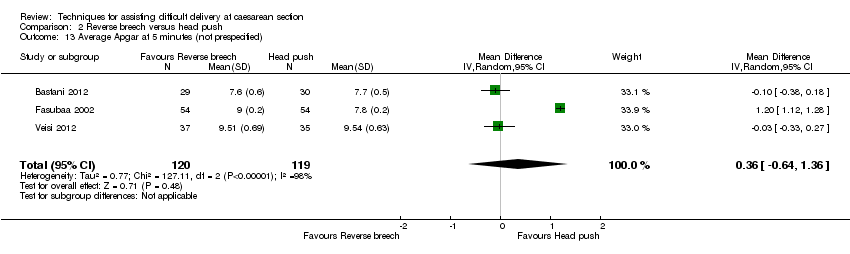
Comparison 2 Reverse breech versus head push, Outcome 13 Average Apgar at 5 minutes (not prespecified).
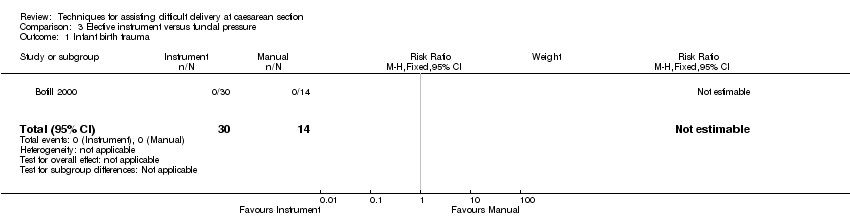
Comparison 3 Elective instrument versus fundal pressure, Outcome 1 Infant birth trauma.

Comparison 3 Elective instrument versus fundal pressure, Outcome 2 Extension of uterine incision.

Comparison 3 Elective instrument versus fundal pressure, Outcome 3 Mean fall in Hb.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Maternal side‐effects (not prespecified) Show forest plot | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Infant birth trauma Show forest plot | 3 | 239 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.42, 5.73] |
| 2 Extension of uterine incision Show forest plot | 4 | 357 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.13, 0.40] |
| 3 Blood loss > 500 mL Show forest plot | 1 | 118 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.18, 1.37] |
| 4 Mean blood loss Show forest plot | 3 | 298 | Mean Difference (IV, Random, 95% CI) | ‐294.92 [‐493.25, ‐96.59] |
| 5 Blood transfusion Show forest plot | 2 | 177 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.20, 1.66] |
| 6 Endometritis Show forest plot | 3 | 285 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.26, 1.05] |
| 7 Wound infection Show forest plot | 4 | 357 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.58, 1.59] |
| 8 Admission to neonatal special care or intensive care unit Show forest plot | 2 | 226 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.23, 1.22] |
| 9 Early neonatal death rate Show forest plot | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.23, 1.24] |
| 10 Mean fall in Hb (not prespecified) Show forest plot | 1 | 118 | Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.72, ‐0.16] |
| 11 Operative time (min) Show forest plot | 4 | 357 | Mean Difference (IV, Random, 95% CI) | ‐14.99 [‐27.67, ‐2.30] |
| 12 Mean hospital stay (not prespecified) Show forest plot | 3 | 285 | Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐2.75, 0.48] |
| 13 Average Apgar at 5 minutes (not prespecified) Show forest plot | 3 | 239 | Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.64, 1.36] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Infant birth trauma Show forest plot | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Extension of uterine incision Show forest plot | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.7 [0.13, 3.73] |
| 3 Mean fall in Hb Show forest plot | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.53, 0.59] |

