วัคซีนป้องกันไข้หวัดใหญ่ในผู้สูงอายุ
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Study characteristics | ||
| Methods | Case‐control study conducted in England, during the 1989 to 1990 influenza season, in the community. Data sources were: death certificates, general practitioner records. Follow‐up period was 4 November 1989 to 23 February 1990. Cases died from influenza during the 1989 epidemic; controls died in the same period a year later and were matched for age, sex, and residence | |
| Participants | 1092 people 16 years or older; 412 cases and 1256 controls were identified; 315 and 777 were included in the analysis, respectively | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched the circulating strain | |
| Outcomes | Certified influenza death | |
| Notes | 2 exposure definitions were used: current vaccinees and previous vaccinees (vaccinated between 1985 and 1989) the first was used; pneumococcal vaccination was very unlikely; circulating strain was A/England/308/89. The season was an epidemic one. The study controls for confounders in analysis: health status, previous vaccination. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Case‐control study conducted in England, during the 1989 to 1990 influenza season, in the community. Data sources were: hospital and general practitioner records. Follow‐up period was 1 December 1989 to 31 January 1990. Cases were hospitalised and their discharge diagnosis or cause of death was pneumonia, influenza, emphysema, or bronchitis; community controls were matched for age and sex. Specific controls were matched for cases who died; controls died 6 to 12 months later. | |
| Participants | 445 patients admitted to hospital (303 cases were identified; 156 cases and 289 controls were included in the analysis, respectively), 16 years of age or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia, influenza, emphysema, or bronchitis (ICD 466, 480.9 to 482.9, 485 to 492.8) | |
| Notes | 2 exposure definitions were used: current vaccinees and previous vaccinees (vaccinated between 1985 and 1989): the first was used; pneumococcal vaccination was very unlikely; circulating strain was A/England/308/89. The season was an epidemic one. The study controls for confounders in analysis: health status, previous vaccination. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Experimental study conducted in Liverpool, UK during the 1999 to 2000 influenza season, randomised, single‐blind, placebo controlled. Data sources were self administered questionnaire and medical records. Follow‐up period was the entire winter season. | |
| Participants | 729 community‐dwelling elderly without risk factors (552 treated and 177 controls, all included in the analysis), 65 to 74 years old | |
| Interventions | Parenteral influenza vaccine: A/Beijing/262/95, A/Sydney/5/97, B/Beijing/184/93. All participants also received pneumococcal vaccine. Vaccine strains matched the circulating strains. | |
| Outcomes | Clinically defined ILI (all of the following symptoms: sudden onset, fever, cough, prostration, weakness, myalgia, widespread aches), pneumonia, hospitalisation for any respiratory illness, death from all causes | |
| Notes | Vaccine contained the WHO recommended strains. The study was supposed to run for 2 influenza seasons: 99‐00 and 00‐01. After the first season, the UK's Department of Health changed the coverage policy for influenza vaccine, and recruitment to the placebo arm dwindled, affecting the validity of the trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random number generation |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes were sealed and serially numbered to assign participants to intervention. |
| Blinding (performance bias and detection bias) | Unclear risk | Described as placebo controlled, but no further details provided. |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information available to reliably assess. |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home, in Atlanta, USA, during the 1984 to 1985 influenza season; active surveillance; medical records were reviewed. Follow‐up period was 26 January 1985 to 1 February 1985. Pharyngeal swab and paired sera were collected to confirm diagnosis. | |
| Participants | 55 nursing home residents (31 treated and 24 controls, all included in the analysis), mean age 85 years | |
| Interventions | Parenteral influenza vaccine: A/Philippines/2/82, A/Chile/83, B/USSR/84. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever 38.7 °C or greater, cough, coryza, sore throat); hospitalisation from ILI; ILI severity (not extracted) | |
| Notes | 7 days after the outbreak started, all residents were given amantadine. Successive outcomes were not accounted for. The circulating strain was related to A/Philippines/2/82. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home, in Columbia, UK, during the 1982 to 1983 influenza season; active surveillance by home staff. Follow‐up period was 31 January 1983 to 25 February 1983. Pharyngeal swab and paired sera were collected to confirm diagnosis from 13 and 32 participants, respectively. | |
| Participants | 116 nursing home residents (26 treated and 90 controls, all included in the analysis) with underlying illnesses, 30 to 108 years old (mean age 71 years) | |
| Interventions | Parenteral influenza vaccine: A/Brazil/11/78; A/Bangkok/1/79; B/Singapore/79. Vaccine strains did not match circulating strains. | |
| Outcomes | ILI (any acute respiratory tract infection occurring during outbreak, with or without fever), pneumonia, death from respiratory disease | |
| Notes | 10 participants were given amantadine, not indicated if vaccinees or unvaccinated. The circulating strain was related to A/Philippines/2/82. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a geriatric hospital in France during the 1976 to 1977 influenza season. | |
| Participants | 100 nursing home residents (50 treated and 50 controls, all included in the analysis) | |
| Interventions | Bivalent parenteral vaccine: A/Vic/3/75; B/HK/1/72. Vaccine strains matched circulating strains. | |
| Outcomes | Disease and deaths without further specifications | |
| Notes | Part of a surveillance study conducted in several communities; poor description of methods; circulating strains were mostly A/Vic/3/75 like | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a geriatric hospital in France during the 1977 to 1978 influenza season. | |
| Participants | 155 nursing home residents (85 treated and 70 controls, all included in the analysis) | |
| Interventions | Bivalent parenteral vaccine: A/Vic/3/75; B/HK/1/73. Vaccine strains did not match circulating strains. | |
| Outcomes | Disease and deaths without further specifications. | |
| Notes | Part of a surveillance study conducted in several communities; poor description of methods; circulating strains were mostly A/Tex/1/77 like | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Italy during the 1990 to 1991 influenza season; medical charts, hospital records, and death certificate archives were reviewed. Follow‐up period was 1 December 1990 to 30 April 1991. 110 participants were tested for serological follow‐up. Throat swabs were obtained from ill residents. | |
| Participants | 242 nursing home residents (169 treated and 73 controls, all included in the analysis; 77 and 33 were tested for serological follow‐up, respectively), 55 to 99 years old | |
| Interventions | Parenteral influenza vaccine: A/Guizhou/54/89; A/Singapore/6/86; B/Yagamata/16/88. Vaccine strains matched the circulating strains. | |
| Outcomes | Clinically defined ILI (fever + at least 2 of the following: cough, coryza, sore throat, myalgia, headache, shivering), hospitalisation for ILI, hospitalisation for all respiratory illness, deaths from respiratory illness | |
| Notes | Circulating strain: B/Yagamata‐like. Vaccinated and control groups were roughly comparable as underlying disease: vaccinated participants had more chronic respiratory diseases. The influenza season was relatively mild. Data were reported by health status. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a skilled care nursing home, in Connecticut, USA, during the 1984 to 1985 influenza season; medical records were reviewed. Follow‐up period was 1 December 1984 to 15 January 1985. Paired sera specimens were obtained from some ill residents. | |
| Participants | 131 residents (96 treated and 48 controls, 96 and 35 included in the analysis respectively), 65 to 95 years old | |
| Interventions | Parenteral influenza vaccine: A/Philippines/2/82; A/Chile/83; B/USSR/100/82. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever 37.8 °C or greater, cough, coryza, sore throat); hospitalisation from ILI; deaths occurring within 2 weeks of ILI with no other explanation | |
| Notes | Amantadine was not used. There was serological evidence of A(H3N2) influenza infections. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a skilled nursing home, in Connecticut, USA, during the 1984 to 1985 influenza season; medical records were reviewed. Follow‐up period was 15 January 1985 to 15 February 1985. Throat swab and paired sera specimens were obtained from some ill residents. | |
| Participants | 85 residents (30 treated and 55 controls, all included in the analysis), 33 to 95 years old | |
| Interventions | Parenteral influenza vaccine: A/Philippines/2/82; A/Chile/83; B/USSR/100/83. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever 37.8 °C or greater, cough, coryza, sore throat); hospitalisation from ILI; deaths occurring within 2 weeks of ILI with no other explanation | |
| Notes | 9 days after the outbreak started amantadine prophylaxis was given to most of the remaining well residents. Successive outcomes were not accounted for. The circulating strain was related to A/Philippines/2/82. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a multiple‐level care facility in Connecticut, USA, during the 1984 to 1985 influenza season; medical records were reviewed. Follow‐up period was 1 February 1985 to 10 April 1985. Throat swab and paired sera specimens were obtained from some ill residents. | |
| Participants | 458 residents (332 treated and 151 controls, 332 and 126 included in the analysis respectively), 64 to 104 years old | |
| Interventions | Parenteral influenza vaccine: A/Philippines/2/82; A/Chile/83; B/USSR/100/84. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever 37.8 °C or greater, cough, coryza, sore throat); hospitalisation from ILI; deaths occurring within 2 weeks of ILI with no other explanation | |
| Notes | 42 days after the outbreak started amantadine prophylaxis was given to most of the remaining well residents. Successive outcomes were not accounted for. The circulating strain was related to A/Philippines/2/82. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Stockholm, Sweden during the 1998 to 1999 influenza season, in the community. Data sources were vaccination database and discharge diagnoses database. Follow‐up period was 1 December 1998 to 31 May 1999. 23% of vaccinees received flu vaccine alone; 76% of vaccinated received flu and pneumococcal vaccine. 841 participants had only pneumococcal vaccine. Only flu vaccinated were included in analysis. | |
| Participants | 182,609 community‐dwelling elderly (23,224 treated and 159,385 controls included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine: A/Beijing/262/95; A/Sydney/5/97; B/Harbin/7/94. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from influenza (ICD‐X: J10.0, J10.1, J10.8, J11.0, J11.1, J11.8), hospitalisation from pneumonia (ICD‐X: J12‐ J18, J69.0, A48.1); deaths from influenza and deaths from pneumonia were not available for this comparison | |
| Notes | Vaccinated people had higher education, more underlying diseases, and smoked less. Circulating strain was A/Sydney (H3N2). The season was probably an epidemic one. 6% of the population lived in a nursing home. The study controls for age in analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Stockholm, Sweden during the 1998 to 1999 influenza season in the community. Data sources were vaccination database and discharge diagnoses database. Follow‐up period was 1 December 1998 to 31 May 1999. 23% of vaccinees received flu vaccine alone; 76% of vaccinated received flu and pneumococcal vaccine. 841 participants had only pneumococcal vaccine. All data were included in a separate analysis. | |
| Participants | 259,627 community‐dwelling elderly (100,242 treated and 159,385 controls included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine: A/Beijing/262/95; A/Sydney/5/97; B/Harbin/7/94; pneumococcal vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from influenza (ICD‐X: J10.0, J10.1, J10.8, J11.0, J11.1, J11.8), deaths from influenza, hospitalisation from pneumonia (ICD‐X: J12‐ J18, J69.0, A48.1), deaths from pneumonia; all deaths | |
| Notes | Vaccinated people had higher education, more underlying diseases, and smoked less. Circulating strain was A/Sydney (H3N2). The season was probably an epidemic one. 6% of the population lived in a nursing home. The study controls for age in analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Stockholm, Sweden during the 1999 to 2000 influenza season, in the community. Data sources were vaccination database and discharge diagnoses database. Follow‐up period was December 1999 to November 2000. 23% of vaccinated received flu vaccine alone; 58% of vaccinated received flu and pneumococcal vaccine. 19% of vaccinated participants received pneumococcal vaccine alone. Only flu vaccinated were included in analysis. | |
| Participants | 163,391 community‐dwelling elderly (29,346 treated and 134,045 controls were included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine: A/Beijing/262/95; A/Sydney/5/97; B/Harbin/7/94. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from influenza (ICD‐X: J10.0, J10.1, J10.8, J11.0, J11.1, J11.8), in‐hospital deaths from influenza, hospitalisation from pneumonia (ICD‐X: J12‐ J18, J69.0, A48.1), in‐hospital deaths from pneumonia | |
| Notes | Vaccinated people had higher education, more underlying diseases, and smoked less. Circulating strain was A/Sydney (H3N2). The season was probably an epidemic one. 6% of the population lived in a nursing home. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Stockholm, Sweden during the 1999 to 2000 influenza season, in the community. Data sources were vaccination database and discharge diagnoses database. Follow‐up period was December 1999 to May 2000. 23% of vaccinees received flu vaccine alone; 58% of vaccinated received flu and pneumococcal vaccine. 19% of vaccinated received pneumococcal vaccine alone. All data were included in a separate analysis. | |
| Participants | 258,747 community‐dwelling elderly (124,702 treated and 134,045 controls were included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine: A/Beijing/262/95; A/Sydney/5/97; B/Harbin/7/94; pneumococcal vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from influenza (ICD‐X: J10.0, J10.1, J10.8, J11.0, J11.1, J11.8), hospitalisation from pneumonia (ICD‐X: J12‐ J18, J69.0, A48.1); in‐hospital deaths from influenza and in‐hospital deaths from pneumonia were not available for the 6‐month period. | |
| Notes | Vaccinated people had higher education, more underlying diseases, and smoked less. Circulating strain was A/Sydney (H3N2). The season was probably an epidemic one. 6% of the population lived in a nursing home. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a skilled nursing home, in New York, USA during the 1987 to 1988 influenza season; individual charts were reviewed. Follow‐up period was 26 December 1987 to 25 January 1988. Throat swab and paired sera specimens were obtained from some ill residents. | |
| Participants | 124 nursing home residents (112 treated and 12 controls, all included in the analysis), 20 to 100 years old (mean age 85 years). 105 participants had 1 or more underlying medical conditions. | |
| Interventions | Parenteral influenza vaccine: A/Taiwan/1/86; A/Leningrad/360/86; B/Ann Arbor/1/86. Vaccine strains did not match the circulating strain. | |
| Outcomes | Clinically defined ILI (fever 100 °F or greater, cough, coryza, sore throat, pneumonia); pneumonia; hospitalisation from ILI; flu‐related deaths | |
| Notes | Vaccinated and not vaccinated participants were similar as underlying conditions. The circulating strain was Shanghai/11/87. Only 1 participant received amantadine prophylaxis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Retrospective cohort study conducted in Italy during the 1991 to 1992 influenza season, in the community. Data sources were self administered questionnaire and vaccination registry. Follow‐up period was 1 December 1991 to 29 February 1992. Random samples of vaccinated and control participants were extracted from vaccination and population registries. | |
| Participants | 213 community‐dwelling elderly (150 treated and 63 controls; number of participants included in the analysis unknown), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Matching unknown, probably yes according to literature data. | |
| Outcomes | Clinically defined ILI (fever, cough, sore throat, myalgia, headache, weakness) | |
| Notes | Very poor description of methods, poor definitions, data extracted from percentages | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Italy during the 2002 to 2003 influenza season, in the community. Data sources were self administered questionnaire and phone interviews. Follow‐up period went from enrolment to April 2003. Ambulatory patients were enrolled at random to undergo either adjuvant or subunit influenza vaccine plus antipneumococcal vaccine. A control group of unvaccinated patients was also enrolled. Only flu vaccinated were included in analysis. | |
| Participants | 235 ambulatory patients (166 vaccinated with adjuvant vaccine, 69 controls; all included in analysis), 65 years or older | |
| Interventions | Adjuvant virosomal vaccine. Vaccine strains probably matched the circulating strain. | |
| Outcomes | Clinically defined ILI (fever 38 °C or more + at least 1 systemic symptom: headache, discomfort, myalgia, chills or sweating, weakness + at least 1 respiratory symptom: cough, sore throat, nasal congestion), hospitalisation for all respiratory diseases, all deaths. Acute respiratory infection was also defined. | |
| Notes | Vaccinated people had higher impairment. No information about flu activity; probably not epidemic year. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Italy during the 2002 to 2003 influenza season, in the community. Data sources were self administered questionnaire and phone interviews. Follow‐up period went from enrolment to April 2004. Ambulatory patients were enrolled at random to undergo either adjuvant or subunit influenza vaccine plus antipneumococcal vaccine. A control group of unvaccinated patients was also enrolled. All data were included in a separate analysis. | |
| Participants | 374 ambulatory patients (166 vaccinated with adjuvant vaccine, 139 vaccinated with flu + pneumo vaccine; 69 controls; all included in analysis), 66 years or older | |
| Interventions | Adjuvant virosomal vaccine; subunit influenza vaccine; antipneumococcal vaccine. Vaccine strains probably matched the circulating strain. | |
| Outcomes | Clinically defined ILI (fever 38 °C or more + at least 1 systemic symptom: headache, discomfort, myalgia, chills or sweating, weakness + at least 1 respiratory symptom: cough, sore throat, nasal congestion), hospitalisation for all respiratory diseases, all deaths. Acute respiratory infection was also defined. | |
| Notes | Vaccinated people had higher impairment. No information about flu activity; probably not epidemic year. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Case‐control study conducted in Italy during the 1994 to 1995 influenza season, in the community. Data sources were database discharge diagnoses and mailed questionnaire. Follow‐up period was 1 December 1994 to 31 March 1995. Cases were people discharged from hospital with pneumonia and influenza; community controls were matched for age, sex, and residence. | |
| Participants | 825 residents of the province of Florence (275 cases and 550 controls were included in analysis; non‐response rate was 15% in each group), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strains did not match the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487) | |
| Notes | Pneumococcal vaccination was very unlikely. The season was an epidemic one. The study controls for confounders in analysis: disability, socio‐economic factors, and smoking habits. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Italy during the 1978 to 1979 influenza season. Authors investigated an outbreak in a nursing home; individual cards were reviewed. Follow‐up period was 1 November 1978 to 31 May 1979. Throat swab and paired sera specimens were obtained from residents. | |
| Participants | 196 nursing home residents (86 treated and 110 controls, all included in the analysis), 60 years or older | |
| Interventions | Parenteral influenza vaccine: A/Texas/1/77; A/USSR/90/77; B/Hong Kong/8/73. Matching between vaccine and circulating strains is unknown. | |
| Outcomes | Positive culture or 4‐fold antibody titre increase with or without symptoms. Only symptomatic cases were included in the analysis. | |
| Notes | Poor reporting of methods; no confounders control. The circulating strain was related to B/Hong Kong/5/72. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in an intermediate and domiciliary care nursing home, in Maryland, USA during the 1987 to 1988 influenza season; medical records were reviewed. Follow‐up period was 8 January 1988 to 26 January 1988. Throat swabs and acute sera specimens were obtained from some ill residents. | |
| Participants | 126 nursing home residents (87 treated and 34 controls were included in the analysis; data on immunisation status for 5 residents were not available), mean age 87 years | |
| Interventions | Parenteral influenza vaccine: A/Taiwan/1/86; A/Leningrad/360/86; B/Ann Arbor/1/86. Vaccine strains did not match the circulating strain. | |
| Outcomes | Clinically defined ILI (fever 99.8 °F or greater + 1 of the following: cough, congestion, sore throat) or positive throat culture; pneumonia; deaths were also reported but not by immunisation status | |
| Notes | Vaccinated and not vaccinated participants were similar as underlying conditions, only senile dementia was more frequent in vaccinees. The circulating strain was A/Leningrad‐like. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective outbreak investigation study conducted in the USA during the 1967 to 1968 influenza season. Authors investigated an outbreak in a nursing home. Follow‐up period was December 1967 and January 1968. Throat swab and sera specimens were obtained from all ill residents and from an additional group of 27 residents with no illness. | |
| Participants | 176 nursing home residents (131 treated and 31 controls were included in the analysis, data on immunisation status for 14 residents were not available) | |
| Interventions | Parenteral influenza vaccine: A2/Japan/170/62; A2/Taiwan/1/64; B/Massachusetts/3/66. Matching between vaccine and circulating strains is unknown. | |
| Outcomes | Clinically defined ILI (fever 37.8 °C or greater, headache, cough, sore throat, myalgia, and prostration) | |
| Notes | Poor reporting; no confounders control. The circulating strain was A2/Wis/1/68. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Hawaii during the 1994 to 1995 influenza season, in the community. Data source was insurance claim records. Follow‐up period was 15 November 1994 to 31 March 1995. Only 10% of vaccinated participants and 3% of unvaccinated participants received pneumococcal vaccination. | |
| Participants | 77,951 person periods members of a medical care program (44,271 treated and 33,680 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strains probably did not match the circulating strain (literature data). | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from all respiratory conditions (ICD 460‐462, 465‐466, 480‐487, 500‐518), hospitalisation from congestive heart failure (ICD 428) | |
| Notes | Odds ratios were adjusted by age and health status. Frequencies data were not available. To perform quantitative analysis, adjusted data were used. The season had low epidemic levels. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Hawaii during the 1995 to 1996 influenza season, in the community. Data source was insurance claim records. Follow‐up period was 15 November 1995 to 31 March 1996. Only 10% of vaccinated participants and 3% of unvaccinated participants received pneumococcal vaccination. | |
| Participants | 77,951 person periods members of a medical care programme (44,271 treated and 33,680 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strains probably matched the circulating strain (literature data). | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from all respiratory conditions (ICD 460‐462, 465‐466, 480‐487, 500‐518), hospitalisation from congestive heart failure (ICD 428) | |
| Notes | Odds ratios were adjusted by age and health status. Frequencies data were not available. To perform quantitative analysis, adjusted data were used. The season was probably an epidemic one. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Hawaii during the 1996 to 1997 influenza season, in the community. Data source was insurance claim records. Follow‐up period was 15 November 1996 to 31 March 1997. Only 10% of vaccinated participants and 3% of unvaccinated participants received pneumococcal vaccination. | |
| Participants | 77,951 person periods members of a medical care programme (44,271 treated and 33,680 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strains probably matched the circulating strain (literature data). | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from all respiratory conditions (ICD 460‐462, 465‐466, 480‐487, 500‐518), hospitalisation from congestive heart failure (ICD 428) | |
| Notes | Odds ratios were adjusted by age and health status. Frequencies data were not available. To perform quantitative analysis, adjusted data were used. The season was probably an epidemic one. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Japan during the 1998 to 1999 influenza season. Follow‐up period was 1 November 1998 to 31 March 1999. 301 nursing homes were surveyed during an epidemic season; only a few residences had an outbreak of respiratory infections. Reports of illness were provided by study site staff. | |
| Participants | 22,462 residents in 301 nursing homes (10,739 treated and 11,723 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine: A/Beijing/262/95; A/Sydney/5/97; B/Mie/1/93. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinical ILI (any of the following symptoms: fever, runny nose, sore throat, cough, headache, muscle aches, chills, vomiting, decreased activity, irritability, wheezing, pulmonary congestion), hospitalisation due to severe illness, deaths due to influenza | |
| Notes | Poor description of methods, poor definitions; some cases were laboratory confirmed, but number of such cases was not indicated. Groups were comparable as age and gender. Health status was not investigated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Study characteristics | ||
| Methods | Experimental study conducted in Virginia, USA during the 1968 to 1969 influenza season. 4 arms: parenteral vaccine, aerosol vaccine, both, placebo. Methods are described in another article. | |
| Participants | 266 elderly psychiatric patients (90 in the parenteral arm, 89 in the aerosol arm, 88 in the arm with both administrations, 87 in the placebo arm) | |
| Interventions | Monovalent inactivated A2 Hong Kong influenza vaccine. Vaccine strains probably matched the circulating strains. | |
| Outcomes | Clinically defined ILI (fever + 1 or 2 respiratory symptoms or at least 2 systemic symptoms, lasting longer than 1 day; 3 respiratory symptoms or 2 respiratory symptoms + 2 systemic symptoms, lasting longer than 2 days); laboratory‐confirmed influenza | |
| Notes | The study year was an epidemic one; circulating strain was A2 HK. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient details provided. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient details provided. |
| Blinding (performance bias and detection bias) | Unclear risk | Insufficient details provided. |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient details provided. |
| Study characteristics | ||
| Methods | Case‐control study conducted in Manitoba, Canada during the 1982 to 1983 influenza season, in the community. Data source was insurance claim records. Follow‐up period was 1 December 1982 to 28 February 1983. Cases were admitted to the hospital with a lower respiratory tract condition as first diagnosis; community controls were matched for age, sex, and residence. | |
| Participants | 10,471 non‐institutionalised people, 70% were older than 65 years (2619 cases and 7828 controls, all included in analysis) | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from a lower respiratory tract condition (ICD 466, 480‐487, 490‐496, 500‐519), deaths from any respiratory condition, deaths from all causes. Data about deaths were not reported. | |
| Notes | Circulating strain: A/Bangkok/1/79‐like. The season was an epidemic one. The study controls for confounders in analysis: health status. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Case‐control study conducted in Manitoba, Canada during the 1985 to 1986 influenza season, in the community. Data source was insurance claim records. Follow‐up period was 1 December 1985 to 15 February 1986. Cases were admitted to the hospital with a lower respiratory tract condition as first diagnosis; community controls were matched for age, sex, and residence. | |
| Participants | 9666 non‐institutionalised people, 70% were older than 65 years (2417 cases and 7249 controls, all included in analysis) | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from a lower respiratory tract condition (ICD 466, 480‐487, 490‐496, 500‐519), deaths from any respiratory condition, deaths from all causes. Data about deaths were not reported. | |
| Notes | Circulating strain: A/Philippines/2/82‐like. The season was an epidemic one. The study controls for confounders in analysis: health status. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Melbourne, Australia during the 1976 influenza season. Authors investigated an outbreak in a nursing home. Follow‐up period was from mid‐April to mid‐August. Throat swabs and paired sera specimens were obtained from residents. | |
| Participants | 222 nursing home residents (154 treated and 68 controls, all included in the analysis); elderly | |
| Interventions | Parenteral influenza vaccine: A/Victoria/3/75; A/Scotland/840/74; B/Hong Kong/8/73. Vaccine strains matched circulating strains. | |
| Outcomes | Laboratory‐confirmed influenza, deaths from influenza | |
| Notes | Poor reporting; no confounders control. The circulating strain was A/Victoria/3/75. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Study characteristics | ||
| Methods | Retrospective cohort study conducted in UK during the 1989 to 1990 influenza season, in the community. Data source was the general practitioner database. Follow‐up period was 1 November 1989 to 15 January 1990. As vaccines used in 1988 and 1989 were antigenically closely related, 2 exposure definitions were used: recently vaccinated and previously vaccinated. | |
| Participants | 9391 people who had at least a general practitioner's consultation in previous months (599 treated and 8792 controls, all included in the analysis), 55 years or older | |
| Interventions | Parenteral influenza vaccine: A/Shanghai/1197‐like. Vaccine strains matched the circulating strain. | |
| Outcomes | Death, death or severe respiratory illness, death or any respiratory illness without further specification | |
| Notes | Important epidemic year. The study controls for confounders in analysis: age, gender, health status. Data were stratified by health status: people with minor underlying conditions are considered as healthy. People vaccinated during the previous year are considered as "non vaccinated". Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Case‐control study conducted in Michigan, USA during the 1989 to 1990 influenza season, in the community. Data sources were: discharge diagnoses, mailed questionnaire. Follow‐up period was 1 November 1989 to 30 April 1990. Cases were admitted to the hospital with pneumonia or influenza; community controls were randomly selected. | |
| Participants | 1907 non‐institutionalised people (1354 cases and 2389 controls were identified; 721 and 1786 were included in analysis, respectively), 65 years or older | |
| Interventions | Parenteral influenza vaccine; 35% of cases and 28% of controls received pneumococcal vaccination. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480.8‐483, 484.7‐487.1) | |
| Notes | Circulating strain: A/Shanghai/11/87. The season was an epidemic one. The study controls for confounders in analysis: health status, flu activity, pneumococcal vaccination, smoke. Peak data were used. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home in Canada during the 1982 to 1983 influenza season; active surveillance. Follow‐up period was 3 November 1982 to 17 January 1983. Throat swab and paired sera specimens were obtained from some residents. | |
| Participants | 545 chronically ill nursing home residents (321 treated and 224 controls, all included in the analysis); 18 to 103 years old, mean age 80 years | |
| Interventions | Parenteral influenza vaccine, whole and subvirion: A/Brazil/11/78; A/Bangkok/1/79; B/Singapore/222/79. Vaccine strains probably matched circulating strains. | |
| Outcomes | Acute respiratory symptoms: fever, congestion, cough, sore throat, general malaise, without a clear definition; death from pneumonia | |
| Notes | Poor reporting; no confounders control. Circulating strain: A/Bangkok/1/79‐like; no other viruses were identified | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home in Canada during the 1982 to 1983 influenza season; partial surveillance for delayed notification of outbreak. Follow‐up period was 30 November 1982 to 9 January 1983. Throat swab and paired sera specimens were obtained from some residents. | |
| Participants | 171 female, chronically ill nursing home residents (53 treated and 118 controls, all included in the analysis); 19 to 105 years old | |
| Interventions | Parenteral whole influenza vaccine: A/Brazil/11/78; A/Bangkok/1/79; B/Singapore/222/80. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined ILI without further specification; death from pneumonia | |
| Notes | Poor reporting; no confounders control. Circulating strain: A/Bangkok/1/79‐like | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Spain during the 1984 to 1985 influenza season, in the community. Data source was a questionnaire retrospectively applied by investigators in June to July 1985 (door‐to‐door survey). The whole population of a rural village was investigated. | |
| Participants | 268 community‐dwelling (188 treated and 80 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine: A/Philippines/2/82; A/Chile/1/83; B/USSR/100/83. Matching unknown. | |
| Outcomes | Clinically defined ILI (fever 39 °C or more, chills, general malaise, myalgia, headache, arthralgia, conjunctivitis, lasting 3 days or more) | |
| Notes | None of the observed deaths was due to flu‐related illness. The season had low epidemic levels. Subgroup analysis was performed but only for the whole population. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Spain during the 1988 to 1989 influenza season, in the community. Data sources were the health centre register, death certificate archives, hospital records. Follow‐up period was 1 November 1988 to 30 May 1989. In the first of the 4 health centres, all elderly people were enrolled; in the others only people approaching the centre for health reasons were enrolled. | |
| Participants | 4558 people enrolled at 4 health centres (1998 treated and 2560 controls, all included in the analysis), 65 years or older, mean age 74 years | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | All hospitalisations and hospitalisation from cardio‐respiratory causes (ICD 401‐414 and 460‐519); deaths from all causes. Only deaths from all causes are included in analysis. | |
| Notes | The season was an epidemic one. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home, in Atlanta, USA during the 1980 to 1981 influenza season; medical charts and hospital charts were reviewed. Follow‐up period was 12 December 1980 to 21 January 1981. Throat swab and paired sera specimens were obtained from some residents. | |
| Participants | 120 nursing home residents (36 treated and 84 controls, all included in the analysis), 47 to 95 years old (median age 80 years). Participants required intermediate and skilled nursing care. | |
| Interventions | Parenteral influenza vaccine: A/Bangkok/1/79; A/Brazil/11/78; B/Singapore/222/78. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever 37.7 °C or greater or cough in the outbreak period (12 December 1980 to 21 January 1981)), death from ILI. Hospitalisation and pneumonia were also accounted for, but results were not presented by immunisation status. | |
| Notes | No confounders control. The circulating strain was A/Bangkok/1/79‐like. Serological tests were negative for other pathogens. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Experimental study conducted in the Netherlands during the 1991 to 1992 influenza season, randomised, double‐blind, placebo controlled; randomisation scheme was stratified according to health status. Follow‐up period was 48 hours after vaccination. Adverse reactions were self reported on postal questionnaire completed 4 weeks after vaccination | |
| Participants | 1838 not known as belonging to a high‐risk group (927 treated and 911 controls; 23 and 9 dropped out, respectively), 60 years or older | |
| Interventions | Parenteral influenza recommended vaccine: A/Singapore/6/86; A/Beijing/357/89; B/Beijing/1/97; B/Panama/45/90 | |
| Outcomes | Local: swelling, itching, warm feeling, pain when touched, constant pain, discomfort. Systemic: fever, headache, malaise, other complaints | |
| Notes | Harms were reported for all participants and by risk condition. Data regarding all participants were included | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate description |
| Allocation concealment (selection bias) | Low risk | Adequate description |
| Blinding (performance bias and detection bias) | Low risk | Described as placebo controlled, but no additional information was available |
| Incomplete outcome data (attrition bias) | Low risk | Adequate description of follow up and attrition |
| Study characteristics | ||
| Methods | Experimental study conducted in the Netherlands during the 1991 to 1992 influenza season, in the community. Follow‐up period was 1 November 1991 to 30 April 1992. Randomised, double‐blind, placebo controlled; randomisation scheme was stratified according to health status. | |
| Participants | 1838 people not known as belonging to a high‐risk group (927 treated and 911 controls; 25 and 22 dropped out, respectively), 60 years or older | |
| Interventions | Parenteral influenza recommended vaccine: A/Singapore/6/86; A/Beijing/357/89; B/Beijing/1/97; B/Panama/45/90. Vaccine strains matched the circulating strains. | |
| Outcomes | Clinically defined ILI; laboratory‐confirmed ILI. Several definitions for clinical and laboratory ILI were tested; the Dutch Sentinel Stations definition is used (fever 37.8 °C or greater + cough or coryza or sore throat or headache or myalgia). | |
| Notes | The study year was an epidemic one; data were stratified by health status. Intention‐to‐treat analysis was performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate description |
| Allocation concealment (selection bias) | Low risk | Adequate description |
| Blinding (performance bias and detection bias) | Low risk | Adequate description |
| Incomplete outcome data (attrition bias) | Low risk | Adequate description |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in New York, USA during the 1982 to 1983 influenza season. Authors investigated an outbreak in a nursing home; independent blind assessment was conducted. Follow‐up period was 1 November 1982 to 30 April 1983. 305 of the 525 residents volunteered to participate in study; diagnosis was made without knowledge of vaccination status | |
| Participants | 305 nursing home residents, mostly ambulatory (181 treated and 124 controls; 138 and 94 had serological surveillance, respectively); groups were comparable for health status and drug use; mean age 85 years | |
| Interventions | Parenteral influenza vaccine: A/Bangkok/1/79; A/Brazil/11/78; B/Singapore/222/79. Vaccine strains matched circulating strains (slight drift) | |
| Outcomes | Laboratory‐confirmed influenza (4‐fold increase in antibody titre), X‐ray‐confirmed pneumonia, deaths from all causes | |
| Notes | Pneumococcal vaccine was rarely used. Amantadine was not used. The circulating strain was A/Arizona/80, closely related to A/Bangkok/1/79 Laboratory‐confirmed cases were analysed by intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in the USA during the 1996 to 1997 influenza season, in the community. Data source was a managed care organisation database. Follow‐up period was 5 October 1996 to 3 May 1997. | |
| Participants | 122,974 members of a medical care programme continuously enrolled for the 1‐year period (71,005 treated and 51,969 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine matched the circulating strain. | |
| Outcomes | Combined outcome: hospitalisation from influenza and pneumonia (ICD 480‐487) or death from all causes | |
| Notes | The study controls for confounders in analysis: age, gender, health status. Data were presented by health status. No information about pneumococcal vaccination. The season was an epidemic one. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in the USA during the 1997 to 1998 influenza season, in the community. Data source was a managed care organisation database. Follow‐up period was 23 November 1997 to 4 April 1998. | |
| Participants | 158,454 members of a medical care programme continuously enrolled for the 1‐year period (92,001 treated and 66,453 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine did not match the circulating strain. | |
| Outcomes | Combined outcome: hospitalisation from influenza and pneumonia (ICD 480‐487) or death from all causes | |
| Notes | The study controls for confounders in analysis: age, gender, health status. Data were presented by health status. No information about pneumococcal vaccination. The season was an epidemic one; circulating strain: A/Sydney‐like. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Saga, Japan. 10,000 community‐dwelling elderly were randomly selected from a population registry and were sent a letter explaining the study with a request for participation. Eligibility criteria were as follows: not being hospitalised, not being institutionalised, not having any long‐term absence, not living alone, and able to contact by telephone at least once a month. | |
| Participants | Among 10,000 elderly citizens, 7357 responded, and 4787 agreed to participate and matched our eligibility criteria. The vaccination status of the study participants was identified by self reporting verification and a list of recipients of partially funded vaccination; 3240 participants (3230 participants were self reported and 10 were known with verification) were vaccinated and 1547 non‐vaccinated. The vaccination coverage was 67.7%. | |
| Interventions | Influenza vaccination versus no vaccination | |
| Outcomes | ILI, clinical influenza, hospitalisation for all causes, hospitalisation for influenza or pneumonia, and total deaths | |
| Notes | The author concludes that influenza vaccination was associated with decreased ILI during the epidemic period in community‐dwelling elderly. The above risk reduction was greater under low‐risk conditions. The results were inconclusive for preventing hospitalisation and death, due to an inadequate sample size. However, our findings support the finding that all elderly individuals substantially benefit from vaccination even in a season of mild influenza activity, and also when the antigenic match between the vaccine strains and the circulating strains is not closely matched. | |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home in Maryland, USA during the 1980 to 1981 influenza season; residents' medical records were reviewed. Follow‐up period was 8 December 1980 to 13 January 1981. Throat swab and paired sera specimens were obtained from some residents. | |
| Participants | 159 nursing home residents, 62 to 100 years old (100 treated and 59 controls, all included in the analysis); most of the residents were chronically ill; risk status did not differ between vaccinees and unvaccinated. | |
| Interventions | Parenteral influenza vaccine: A/Brazil; A/Bangkok; B/Singapore. Vaccine strains matched circulating strains. | |
| Outcomes | Clinically defined ILI (2 case definitions; more specific definition was used: fever + cough or chest congestion), pneumonia without further specification, and case‐fatality rate | |
| Notes | Vaccination was not offered to staff. 36% of the observed deaths during the epidemic period occurred from causes other than flu. Circulating strains: A/Taiwan/1/79‐like, very similar to the vaccine strain A/Bangkok. Isolation attempts for other pathogens were unsuccessful. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Australia in 17 nursing homes during the 1983 influenza season. Follow‐up period was autumn to spring; blinded assessment of illness was performed. | |
| Participants | 326 residents in 17 nursing homes (229 treated and 97 controls, all included in the analysis), 44 to 99 years old | |
| Interventions | Parenteral influenza vaccine: A/Victoria/186/82; A/Philippines/2/82; B/Singapore/222/79. Vaccine strains matched circulating strains. | |
| Outcomes | Laboratory‐confirmed influenza (4‐fold increase in antibody titre) | |
| Notes | Poor description of methods; part of another study. The circulating strain was A/Philippines/2/82. No information about flu activity | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Australia in 17 nursing homes during the 1984 influenza season. Follow‐up period was autumn to spring; blinded assessment of illness was performed. | |
| Participants | 365 residents in 17 nursing homes (184 treated and 181 controls, all included in the analysis), 44 to 99 years old | |
| Interventions | Parenteral influenza vaccine: A/Dunedin/27/83; A/Philippines/2/82; B/Singapore/222/80. Vaccine strains matched circulating strains. | |
| Outcomes | Laboratory‐confirmed influenza (4‐fold increase in antibody titre) | |
| Notes | Poor description of methods; part of another study. The circulating strain was A/Philippines/2/82. No information about flu activity | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in the UK in several nursing homes during the 1971 to 1972 influenza season; all residents were under constant surveillance. Throat swab and paired sera specimens were obtained whenever possible. | |
| Participants | 490 nursing homes residents (134 treated and 356 controls, all included in the analysis), 60 years or older | |
| Interventions | Parenteral influenza vaccine: A2/HK/68; B/Vic.98926/70. Matching between vaccine and circulating strains is unknown. | |
| Outcomes | Respiratory illness and pneumonia without definition, deaths from pneumonia | |
| Notes | Very poor description of methods; groups were roughly comparable as age and general health. No information about flu activity and laboratory confirmation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in the UK in several nursing homes during the 1972 to 1973 influenza season; all residents were under constant surveillance. Throat swab and paired sera specimens were obtained whenever possible. | |
| Participants | 390 nursing homes residents (123 treated and 267 controls, all included in the analysis), 60 years or older | |
| Interventions | Parenteral influenza vaccine: A2/HK/68; B/Vic.98926/71. Matching between vaccine and circulating strains is unknown. | |
| Outcomes | Respiratory illness and pneumonia without definition, deaths from pneumonia | |
| Notes | Very poor description of methods; groups were roughly comparable as age and general health. No information about flu activity and laboratory confirmation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in the UK in several nursing homes during the 1973 to 1974 influenza season; all residents were under constant surveillance. Throat swab and paired sera specimens were obtained whenever possible. | |
| Participants | 470 nursing homes residents (183 treated and 287 controls, all included in the analysis), 60 years or older | |
| Interventions | Parenteral influenza vaccine: A/Eng/42/72; B/Vic.98926/71; B/Hong Kong/8/73. Matching between vaccine and circulating strains is unknown. | |
| Outcomes | Respiratory illness and pneumonia without definition, deaths from pneumonia | |
| Notes | Very poor description of methods; groups were roughly comparable as age and general health. No information about flu activity and laboratory confirmation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home in Ontario, Canada during the 1996 to 1997 influenza season. Follow‐up period was 1 January 1997 to 11 January 1997. Nasal swabs were obtained from 3 ill residents. | |
| Participants | 172 nursing home residents (149 treated and 23 controls, all included in the analysis) | |
| Interventions | Parenteral influenza vaccine. Vaccine strains probably matched circulating strains (other studies). | |
| Outcomes | Clinically defined ILI (fever 38 °C or greater, cough, sore throat, nasal congestion, muscle ache, lethargy, lasting 2 days or more) | |
| Notes | Amantadine was used in all residents. 1 positive result was obtained by rapid testing. Poor reporting | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Study characteristics | ||
| Methods | Case‐control study nested within a cohort of older people registered with 79 participating general practices in central England. People were included in the identified cohort if aged 65 to 89 years and if they consulted their general practitioner (or other emergency medical services) for an acute episode of respiratory infection or acute exacerbation of pre‐existing respiratory disease, between 1 October 2003 and 31 March 2004. People with simple upper respiratory tract infections were excluded. | |
| Participants | Cases were defined as all people admitted to hospital with acute respiratory disease. Only the first admission during the study period was included. Surviving cases were invited for interview. Controls were defined as people presenting with acute respiratory disease but who were managed in the community. 6 controls were invited per case to mitigate for a potential low uptake, in order to achieve 4 controls interviewed per case. Controls were matched to cases for age (within ± 5 years where possible), sex, and consultation date (within ± 7 days where possible). 3970 eligible participants were identified. 500 participants were admitted to hospital. Altogether 44.1% of invited cases and 54.5% of controls agreed to interview; 157 cases and 639 controls were finally interviewed. The proportion of cases vaccinated against influenza before entry to the study was 74.5% and in controls was 74.2%. | |
| Interventions | Influenza vaccination and admissions to hospital for acute respiratory disease | |
| Outcomes | — | |
| Notes | The authors conclude that in a winter typical of the current levels of circulating influenza, they were unable to demonstrate that influenza vaccination had a specific effect on preventing hospitalisation among elderly people clinically ill with acute respiratory disease, although there was a possible effect during the peak weeks of influenza activity. Relying solely on the influenza vaccine to control the annual winter bed pressures in hospitals is unlikely to be a sufficiently effective yearly strategy, and continuing attention to other factors (e.g. the effective vaccination of healthcare workers, treatment of comorbidities, indoor housing conditions) is essential. | |
| Study characteristics | ||
| Methods | Surveillance population‐based study conducted in the USA during the 1979 to 1980 and 1980 to 1981 influenza seasons. Case report for each case was obtained from neurologists. All case reports were included. Follow‐up period was 1 September 1979 to 31 March 1980 and 1 September 1980 to 31 March 1981. | |
| Participants | USA (minus Maryland) adult population, 18 years or older | |
| Interventions | Seasonal trivalent vaccine | |
| Outcomes | Cases of Guillain‐Barré syndrome. Vaccine‐associated cases were defined as those with onset within the 8‐week period after influenza vaccination. | |
| Notes | Vaccination rates in population were obtained from national immunisation survey. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Japan during the 2001 to 2002 period in the community. Data sources were the general practitioner database and self administered questionnaire. Follow‐up period was 31 December 2001 to 31 May 2002. Unvaccinated participants were matched as closely as possible for sex and age to the vaccinated participants. Laboratory confirmation was performed in 60% of cases. | |
| Participants | 4423 mostly community‐dwelling (3520 treated and 903 controls were included in the analysis), 65 to 104 years old | |
| Interventions | Parenteral influenza vaccine: A/New Caledonia/20/99; A/Panama/2007/99; B/Johannesburg/5/99. Vaccine strains matched the circulating strain. | |
| Outcomes | Clinically defined ILI (all of the following symptoms: sudden onset, fever 38 °C or more, cough) | |
| Notes | The influenza season was mild. The study controls for age, sex, and previous vaccinations in analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Experimental study conducted in Texas, USA during the 1994 to 1995 influenza season, randomised, placebo‐controlled trial; randomisation method and allocation concealment were not described. Participants were allocated to receive ascending doses (15 ug/45 ug/135 ug) of antigen. Only 15 ug vaccine was included in analysis. Follow‐up period was 48 hours after vaccination. | |
| Participants | 21 ambulatory, medically stable people, 65 years or older | |
| Interventions | Parenteral monovalent subvirion 15 ug (9 participants) and purified haemagglutinin 15 ug (12 participants) influenza vaccine: A/Singapore/6/86 | |
| Outcomes | Discomfort, erythema/induration, headache, malaise without further description | |
| Notes | Different vaccines (haemagglutinin and subvirion) were analysed as a single "treatment group". | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Surveillance population‐based study conducted in the USA (4 states: Illinois, Maryland, North Carolina, Washington) during the 1992 to 1993 and 1993 to 1994 influenza seasons. Discharge diagnoses database was used to identify cases. Hospital charts were reviewed to confirm diagnosis. Follow‐up period was 1 September 1992 to 28 February 1993 and 1 September 1993 to 28 February 1994. | |
| Participants | About 21 million people, 18 years or older | |
| Interventions | Seasonal trivalent vaccine | |
| Outcomes | Cases of Guillain‐Barré syndrome. Vaccine‐associated cases were defined a priori as those with onset within the 6‐week period after influenza vaccination. | |
| Notes | Results were stratified by age and adjusted by season and sex. Vaccination rates in population were estimated from a random‐digit dialling telephone survey. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Retrospective cohort study conducted in 46 elderly homes in Hong Kong, China to assess the effectiveness of influenza vaccination on influenza, pneumonia, hospitalisation for influenza, and death. People were eligible if they were age 65 years or above. The exposed group comprised people who had not received influenza vaccination, while the control group comprised people who had received influenza vaccination from the Department of Health or other healthcare providers in 2004. Information regarding vaccination was based on its documentation in the elderly home records. A resident having unknown history of influenza vaccination in the preceding calendar year was regarded as not being vaccinated. A standardised questionnaire was used to collect data from the elderly homes once an influenza outbreak was defined in the elderly home. The occurrence of influenza was identified by the self administered questionnaires. The occurrence of pneumonia, hospitalisation, and death were identified from the hospital records. | |
| Participants | 3177 residents participated in the study. The mean age was 83 years; 2133 were females and 1044 males. There were 2943 vaccinated (92.6%) and 234 (7.4%) unvaccinated participants. More females were vaccinated (67.7%) than males (59.8%). | |
| Interventions | Influenza vaccination versus no vaccination | |
| Outcomes | Influenza, pneumonia, hospitalisation, and death | |
| Notes | The authors conclude that this study failed to demonstrate a protective effect of influenza vaccine against influenza and its complications during outbreaks. | |
| Study characteristics | ||
| Methods | Retrospective cohort study conducted in Spain during the 1991 to 1992 influenza season, in the community. Data sources were: the health centre register, death certificate archives, hospital records. Follow‐up period was 7 months after vaccination. People were excluded if they did not approach the centre in the last 3 years. | |
| Participants | 1965 community‐dwelling elderly enrolled in a health centre (779 treated and 1186 controls, all included in the analysis), 65 years or older, mean age 73.5 years | |
| Interventions | Parenteral influenza vaccine. Vaccine strains probably matched the circulating strain. | |
| Outcomes | Hospitalisation from cardio‐respiratory causes, death from all causes. Only deaths from all causes are included in analysis. | |
| Notes | The study controls for confounders in analysis (age, health status, home care). The season had low epidemic levels. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Retrospective cohort study conducted in the UK during the 1990 to 1998 influenza season, in the community. Data source was a managed care organisation database. Follow‐up period was the epidemic period (period with consultation rate for ILI more than 50/100,000 person‐weeks). People were identified and included in the study if they were registered on the first day of the week that included 1 September each year. | |
| Participants | 692,819 person‐years in vaccine recipients and 1,534,280 person‐years in vaccine non‐recipients, 65 years or older | |
| Interventions | Parenteral influenza vaccine | |
| Outcomes | Hospitalisation for acute respiratory illness (ICD 466, 480‐487), respiratory‐related deaths | |
| Notes | Most of the seasons were epidemic, with vaccine strains matching the circulating strains. Data were presented by health status; other strata: year, flu activity, age. Data by health status were extracted by rates reported in tables. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | See Mangtani 2004a. Influenza season 1990 to 1991 | |
| Participants | See Mangtani 2004a | |
| Interventions | See Mangtani 2004a. Vaccine matched the epidemic strain. | |
| Outcomes | See Mangtani 2004a | |
| Notes | See Mangtani 2004a. Epidemic year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | See Mangtani 2004a. Influenza season 1991 to 1992 | |
| Participants | See Mangtani 2004a | |
| Interventions | See Mangtani 2004a. Vaccine matched the epidemic strain. | |
| Outcomes | See Mangtani 2004a | |
| Notes | See Mangtani 2004a. Epidemic year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | See Mangtani 2004a. Influenza season 1992 to 1993 | |
| Participants | See Mangtani 2004a | |
| Interventions | See Mangtani 2004a. Vaccine matched the epidemic strain. | |
| Outcomes | See Mangtani 2004a | |
| Notes | See Mangtani 2004a. Non‐epidemic year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | See Mangtani 2004a. Influenza season 1993 to 1994 | |
| Participants | See Mangtani 2004a | |
| Interventions | See Mangtani 2004a. Vaccine matched the epidemic strain. | |
| Outcomes | See Mangtani 2004a | |
| Notes | See Mangtani 2004a. Epidemic year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | See Mangtani 2004a. Influenza season 1994 to 1995 | |
| Participants | See Mangtani 2004a | |
| Interventions | See Mangtani 2004a. Vaccine matched the epidemic strain. | |
| Outcomes | See Mangtani 2004a | |
| Notes | See Mangtani 2004a. Non‐epidemic year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | See Mangtani 2004a. Influenza season 1995 to 1996 | |
| Participants | See Mangtani 2004a | |
| Interventions | See Mangtani 2004a. Vaccine matched the epidemic strain. | |
| Outcomes | See Mangtani 2004a | |
| Notes | See Mangtani 2004a. Epidemic year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | See Mangtani 2004a. Influenza season 1996 to 1997 | |
| Participants | See Mangtani 2004a | |
| Interventions | See Mangtani 2004a. Vaccine matched the epidemic strain. | |
| Outcomes | See Mangtani 2004a | |
| Notes | See Mangtani 2004a. Epidemic year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | See Mangtani 2004a. Influenza season 1997 to 1998 | |
| Participants | See Mangtani 2004a | |
| Interventions | See Mangtani 2004a. Vaccine did not match the epidemic strain. | |
| Outcomes | See Mangtani 2004a | |
| Notes | See Mangtani 2004a. Non‐epidemic year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | See Mangtani 2004a. Influenza season 1998 to 1999 | |
| Participants | See Mangtani 2004a | |
| Interventions | See Mangtani 2004a. Vaccine matched the epidemic strain. | |
| Outcomes | See Mangtani 2004a | |
| Notes | See Mangtani 2004a. Epidemic year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Experimental study conducted in Minneapolis, USA during the 1988 to 1989 influenza season, randomised, double‐blind, placebo‐controlled cross‐over trial. Follow‐up period was 7 days after vaccination. Symptoms were assessed by phone interview. | |
| Participants | 672 outpatients (336 treated and 336 controls were included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza recommended vaccine: A/Taiwan/1/86; A/Sichuan/2/87; B/Victoria/2/87 | |
| Outcomes | Cough, coryza, fatigue, malaise, myalgia, headache, nausea, sore arm, disability, feverish without further description | |
| Notes | Placebo was saline injection. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. |
| Blinding (performance bias and detection bias) | Low risk | Probably acceptable since placebo was a saline injection |
| Incomplete outcome data (attrition bias) | Unclear risk | Short‐term follow‐up for most outcomes was by phone, but unclear how complete data were for longer‐term outcomes. |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home in Wyoming, USA during the 1984 to 1985 influenza season. Follow‐up period was 2 January 1985 to 3 March 1985. Throat washing and convalescent sera were obtained from some residents. | |
| Participants | 55 nursing home residents (36 treated and 19 controls, all included in the analysis), 60 to 98 years old | |
| Interventions | Parenteral influenza vaccine: A/Philippines/82; A/Chile/83; B/USSR/84. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined URI (upper respiratory illness: fever, chills, myalgia, respiratory symptoms), radiologically confirmed pneumonia, hospitalisation, and death without further specification | |
| Notes | Amantadine was used in cases. The circulating strain that year was of A/Philippines type. No virus strain was isolated from participants, but serologic tests confirmed influenza A virus infections. Poor description of methods | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Michigan, USA during the 1991 to 1992 influenza season. Authors investigated 26 skilled nursing homes with evidence of flu activity; nursing homes with high rates of immunisation (herd immunity) were excluded from the study; data on ILI or pneumonia were recorded prospectively under supervision of a nurse co‐ordinator. Follow‐up period was 1 November 1991 to 29 February 1992. | |
| Participants | 2351 residents in 26 nursing homes (1728 treated and 623 controls, all included in the analysis), 65 years or older, for whom vaccination status was known | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever 37.8 °C or greater + cough, sore throat, or nasal congestion), clinical pneumonia, deaths occurring within 3 months of the onset of respiratory illness. Influenza was considered to have been introduced into a nursing home when a least 2% of residents developed ILI within a 7‐day period during community‐documented virus circulation or when virus was isolated from cases. | |
| Notes | Both influenza A (H3N2) and A (H1N1) co‐circulated with influenza A (H3N2) predominantly. The circulating strains were closely related to the vaccine strain. Rate ratio estimates were adjusted by sex, age, home size and presented by "peak period". Groups were comparable as age and chronic conditions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home in Honolulu, USA during the 1989 to 1990 influenza season; vaccination records, hospital records, resident records were reviewed. Follow‐up period was 15 December 1989 to 28 January 1990. Specimens for virus isolation were obtained from 9 ill residents, and paired sera specimens were obtained from 34 case and non‐case residents. | |
| Participants | 39 nursing home residents with multiple chronic conditions (36 treated and 3 controls, all included in the analysis), 36 to 102 years (mean age 80 years) | |
| Interventions | Parenteral influenza vaccine; pneumococcal vaccine was also used. Vaccine strains matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever 37.8 °C or greater + cough, coryza, or sore throat), laboratory‐confirmed influenza, pneumonia, deaths from ILI or pneumonia | |
| Notes | Amantadine was administered to all participants over a 1‐week period (January 4 to 12, 1990). The circulating strain was indistinguishable from the vaccine strain A/England/4/27/88. Lack of serologic evidence for other respiratory agents | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated outbreaks in 14 nursing homes in Wales, UK during the 1991 to 1992 influenza season. Follow‐up period was 15 December 1991 to 28 February 1992. Paired sera specimens were collected from 7 cases in 2 homes. | |
| Participants | 466 residents in 14 nursing homes (104 treated and 362 controls, all included in the analysis) | |
| Interventions | Parenteral influenza vaccine. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined URI (upper respiratory illness: fever, chills, myalgia, cough) | |
| Notes | Very poor reporting. Vaccine strain was assumed to match the circulating strain according to literature data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Case‐control study conducted in the USA during the 1981 to 1989 period, in the community. Data source was a managed care organisation database. Follow‐up period was the epidemic period according to surveillance data. Cases were admitted to services with pneumonia or influenza or died in hospital from pneumonia or influenza; community controls were matched for high‐risk status. | |
| Participants | 251,034 members of a medical care programme, 65 years or older | |
| Interventions | Parenteral influenza vaccine; participants also received pneumococcal vaccination. Vaccine strains matched the circulating strain. | |
| Outcomes | Pneumonia and influenza without hospitalisation, hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalised death | |
| Notes | Most of the seasons were epidemic, and vaccine strains did not match the circulating strains. The study controls for confounders in analysis (age, sex, pneumococcal vaccination). Data are stratified by health status, but allow only quantitative analysis. The odds ratio adjusted by risk status was obtained by pooling the data reported in the paper using Wolf method. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Authors investigated 2 consecutive outbreaks in the same nursing home in Japan during the 1996 to 1997 influenza season; patients' records were reviewed. Follow‐up period was 25 December 1996 to 14 January 1997 and 19 February 1997 to 26 February 1997. Throat swab and paired sera specimens were obtained from ill residents. | |
| Participants | 128 nursing home residents (60 treated and 68 controls, all included in the analysis), 70 years or older. None of the residents was previously vaccinated. | |
| Interventions | 2 doses of parenteral influenza vaccine: A/Yamagata/32/89; A/Wuhan/359/95; B/Mie/1/93. Vaccine strains matched circulating strains. | |
| Outcomes | ICHPP‐2 defined ILI (laboratory evidence or epidemiological criteria or 6 of the following symptoms: sudden onset, fever, cough, prostration, chills, weakness, myalgia, widespread aches), hospitalisations, and deaths without definition | |
| Notes | Epidemic reoccurrence of influenza A outbreak was observed. Both outbreaks were investigated; vaccinated and control groups were comparable as age or risk status. The circulating strain was A/Wuhan/359/95. Amantadine was not used. Other respiratory viruses were not isolated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Minneapolis, USA during the 1990 to 1991 influenza season, in the community. Data source was the managed care organisation database. Follow‐up period was 1 October 1990 to 31 March 1991. The rate was adjusted for age, sex, health status, pneumococcal vaccination. | |
| Participants | 25,532 members of a medical care programme continuously enrolled for the 1‐year period (11,483 treated and 14,049 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. 3% of vaccinees and 1% of unvaccinated received pneumococcal vaccination. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from all respiratory conditions (ICD 460, 462, 465‐466, 480‐487, 490‐96, 500‐518), hospitalisation from congestive heart failure (ICD 428), death from all causes (not reported) | |
| Notes | The season was an epidemic one. Data were extracted by rates reported in tables. Quantitative analysis with adjusted rates was not performed because data reported and statistical model used were not homogeneous to those reported in the other studies. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Minneapolis, USA during the 1991 to 1992 influenza season, in the community. Data source was the managed care organisation database. Follow‐up period was 1 October 1991 to 31 March 1992. The rate was adjusted for age, sex, health status, pneumococcal vaccination. | |
| Participants | 26,369 members of a medical care programme continuously enrolled for the 1‐year period (15,288 treated and 11,081 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. 5% of vaccinees and 2% of unvaccinated received pneumococcal vaccination. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from all respiratory conditions (ICD 460, 462, 465‐466, 480‐487, 490‐496, 500‐518), hospitalisation from congestive heart failure (ICD 428), death from all causes (not reported) | |
| Notes | The season was an epidemic one. Data were extracted by rates reported in tables. Quantitative analysis with adjusted rates was not performed because data reported and statistical model used were not homogeneous to those reported in the other studies. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Minneapolis, USA during the 1992 to 1993 influenza season, in the community. Data source was the managed care organisation database. Follow‐up period was 1 October 1992 to 31 March 1993. The rate was adjusted for age, sex, health status, pneumococcal vaccination. | |
| Participants | 26,626 members of a medical care programme continuously enrolled for the 1‐year period (14,647 treated and 11,979 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. 6% of vaccinees and 3% of unvaccinated received pneumococcal vaccination. Vaccine strains did not match the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from all respiratory conditions (ICD 460, 462, 465‐466, 480‐487, 490‐496, 500‐518), hospitalisation from congestive heart failure (ICD 428), death from all causes (not reported) | |
| Notes | The season was an epidemic one. Data were extracted by rates reported in tables. Quantitative analysis with adjusted rates was not performed because data reported and statistical model used were not homogeneous to those reported in the other studies. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Minneapolis, USA during the 1990 to 1995 period, in the community. Data source was the managed care organisation database. Follow‐up period was 15 November to 31 February. A subgroup analysis by health status was performed. The rate was adjusted for age, sex, health status, vaccination status. | |
| Participants | 147,551 members of a medical care programme continuously enrolled for the 1‐year period (87,898 treated and 59,653 controls included in the analysis), 64 years or older | |
| Interventions | Parenteral influenza vaccine. 11.3% of vaccinees and 4.5% of unvaccinated received pneumococcal vaccination, on average. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from all respiratory conditions, hospitalisation from congestive heart failure, death from all causes (deaths were not reported) | |
| Notes | Most of the seasons were epidemic, with vaccine strains matching the circulating strains. Data were extracted by rates reported in tables. Only data stratified by health status were included in the analysis. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Minneapolis, USA during the 1993 to 1995 period, in the community. Data source was the managed care organisation database. Follow‐up period was 15 November to 31 March. The rate was adjusted for age, sex, health status, vaccination status. | |
| Participants | 69,024 members of a medical care programme continuously enrolled for the 1‐year period (46,480 treated and 22,544 controls included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. 11.3% of vaccinees and 4.5% of unvaccinated received pneumococcal vaccination, on average. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from all respiratory conditions, hospitalisation from congestive heart failure, death from all causes (deaths were not reported) | |
| Notes | All the seasons were epidemic, with vaccine strains matching the circulating strains. Data were extracted by rates reported in tables and calculated by difference with data reported in previous studies. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in the USA, during the 1998 to 1999 influenza season, in the community. Data source was the managed care organisation database. Follow‐up period was 15 November to 31 February. The rate was adjusted for age, sex, health status. | |
| Participants | 140,055 members of a medical care programme continuously enrolled for the 1‐year period (77,738 treated and 62,317 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from cerebrovascular disease (ICD 431‐437), hospitalisation from heart disease (ICD 410‐414, 428), death from all causes | |
| Notes | The season probably was an epidemic one. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in the USA during the 1999 to 2000 influenza season, in the community. Data source was the managed care organisation database. Follow‐up period was 15 November to 31 March. The rate was adjusted for age, sex, health status. | |
| Participants | 146,328 members of a medical care programme continuously enrolled for the 1‐year period (87,357 treated and 58,971 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487), hospitalisation from cerebrovascular disease (ICD 431‐437), hospitalisation from heart disease (ICD 410‐414, 428), death from all causes | |
| Notes | The season probably was an epidemic one. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Leicester, UK during the 1993 to 1994 influenza season, in the community. Data source was weekly phone interviews. Follow‐up period was 18 October 1993 to 19 December 1993. The sample was randomly selected. Symptomatic participants were checked for laboratory confirmation. | |
| Participants | 427 community‐dwelling elderly (223 treated and 216 controls; 218 and 209 included in the analysis, respectively), 63 to 89 years old | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Laboratory‐confirmed influenza (4‐fold increase in antibody titre) | |
| Notes | The study was conducted throughout an outbreak of influenza. The study controls for age, health status, and smoking habits in analysis. Data are presented by smoking habits. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in the USA during the 1996 to 1997 influenza season, in the community. Data source was a 3 managed care organisation database. Follow‐up period was 5 October 1996 to 3 May 1997. | |
| Participants | 122,974 members of a medical care programme continuously enrolled for the 1‐year period (71,005 treated and 51,969 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine matched the circulating strain. | |
| Outcomes | Hospitalisation from influenza and pneumonia (ICD 480‐487), death from all causes | |
| Notes | Identical to Hak 1. Odds ratios adjusted for age, sex, site, health status were presented. Frequencies data were not available. To perform quantitative analysis adjusted data were used. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in the USA during the 1997 to 1998 influenza season, in the community. Data source was the managed care organisation database. Follow‐up period was 23 November 1997 to 4 April 1998. | |
| Participants | 158,454 members of a medical care programme continuously enrolled for the 1‐year period (92,001 treated and 66,453 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine did not match the circulating strain. | |
| Outcomes | Hospitalisation from influenza and pneumonia (ICD 480‐487), death from all causes | |
| Notes | Identical to Hak 2. Odds ratios adjusted for age, sex, site, health status were presented. Frequencies data were not available. To perform quantitative analysis adjusted data were used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Case‐control study conducted in Michigan, USA during the 1990 to 1991 influenza season, in the community. Data sources were: database discharge diagnoses, mailed questionnaire. Follow‐up period was 1 November 1990 to 30 April 1991. Cases were people discharged from hospital with pneumonia or influenza; community controls were matched for age, sex, and residence. | |
| Participants | 2197 non‐institutionalised elderly (860 cases and 1828 controls were identified; 667 and 1530 were included in analysis, respectively), 65 years or older | |
| Interventions | Parenteral influenza vaccine, participants were also offered pneumococcal vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487) | |
| Notes | 41% of cases and 28% of controls received pneumococcal vaccination. The season probably had low epidemic levels. The study controls for confounders in analysis: influenza activity, health status, age, sex, region. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Case‐control study conducted in Michigan, USA during the 1991 to 1992 influenza season, in the community. Data sources were: database discharge diagnoses, mailed questionnaire. Follow‐up period was 1 November 1991 to 30 April 1992. Cases were people discharged from hospital with pneumonia or influenza; community controls were matched for age, sex, and residence. | |
| Participants | 2761 non‐institutionalised elderly (1186 cases and 2345 controls were identified; 890 and 1871 were included in analysis, respectively), 65 years or older | |
| Interventions | Parenteral influenza vaccine, participants were also offered pneumococcal vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation from pneumonia and influenza (ICD 480‐487) | |
| Notes | 44% of cases and 32% of controls received pneumococcal vaccination. The season was probably an epidemic one. The study controls for confounders in analysis: influenza activity, health status, age, sex, region. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Case‐control study conducted in Michigan, USA during the 1989 to 1990 influenza season, in 23 nursing homes. Data sources were: patients specific logs, vaccination records. Follow‐up period was the epidemic period according to surveillance data. Cases developed ILI during the period of laboratory‐confirmed community influenza activity; controls resided in the same facility and were matched for age. | |
| Participants | 1198 residents in 23 nursing homes that experienced outbreaks or with virus isolation (361 cases and 837 controls, all included in analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine; 17% of cases and 17% of controls received pneumococcal vaccination. Vaccine strains matched the circulating strain. | |
| Outcomes | Clinically defined ILI (fever 37.8 °C or greater and 1 or more of the following: cough, sore throat, coryza) | |
| Notes | Circulating strain: A/Shanghai/11/87. The season was an epidemic one. The study controls for confounders in analysis: home size, vaccination level, sex, and age. Quantitative analysis was not performed, as the logistic model used by the authors did not control by health status. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Retrospective cohort study conducted in Michigan, USA during the 1982 to 1983 influenza season. Authors investigated 7 nursing homes with evidence of flu activity. Throat swab and paired sera specimens were obtained from some residents; medical records. Follow‐up period was 10 December 1982 to 4 March 1983. | |
| Participants | 1018 residents in 7 nursing homes with outbreak (548 treated and 470 controls, all included in the analysis) | |
| Interventions | Parenteral influenza vaccine: A/Bangkok/79; A/Brazil/78; B/Singapore/79. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever 37.8 °C or greater + cough, coryza, or sore throat), X‐ray‐confirmed pneumonia, hospitalisation for ILI, deaths occurring within 2 weeks of onset of ILI. An outbreak was defined by a number of ILI per week that exceeded 10% of the residents. | |
| Notes | Cohorts were comparable as age and level of nursing care. Amantadine was not used. The circulating strain was A/Bangkok/1/79‐like. Laboratory confirmation of influenza A infection was obtained in 3 homes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Retrospective cohort study conducted in Michigan, USA during the 1982 to 1983 influenza season, in 6 nursing homes. Throat swab and paired sera specimens were obtained from some residents; medical records were reviewed. Follow‐up period was 10 December 1982 to 4 March 1983. | |
| Participants | 458 residents in 6 nursing homes without outbreak (339 treated and 119 controls, all included in the analysis) | |
| Interventions | Parenteral influenza vaccine: A/Bangkok/79; A/Brazil/78; B/Singapore/79. Vaccine strains matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever 37.8 °C or greater + cough, coryza, or sore throat), deaths occurring within 2 weeks of onset of ILI | |
| Notes | Cohorts were comparable as age and level of nursing care. Amantadine was not used. The circulating strain in the community was A/Bangkok/1/79‐like, but laboratory confirmation was not available in the homes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Milan, Italy during the 2000 to 2001 influenza season, in the community. Data sources were: monthly phone interviews and self administered questionnaires. Follow‐up period was 30 November 2000 to 31 March 2001. | |
| Participants | 363 community‐dwelling elderly (264 treated and 99 controls; 184 and 79 included in the analysis, respectively), mean age 75 years | |
| Interventions | Adjuvant virosomal vaccine. Vaccine strains probably matched the circulating strain. | |
| Outcomes | Clinically defined ILI (fever + at least 1 systemic symptom: headache, myalgia, chills, weakness + at least 1 respiratory symptom: cough, sore throat, congestion); acute respiratory infection (respiratory symptoms without immediate fever); hospitalisation for pulmonary infection | |
| Notes | Low viral circulation. Cohorts were not significantly different as comorbidity. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Study characteristics | ||
| Methods | Case‐control study conducted in Spain during the 1994 to 1995 influenza season, in the community. Data sources were: hospital emergency logs and records; structured interview. Follow‐up period was 15 November 1994 to 31 March 1995. Cases were people admitted to hospital for pneumonia; controls were admitted to hospital in the same week for acute abdominal surgical condition or trauma. | |
| Participants | 249 non‐institutionalised people (94 cases and 166 controls were identified; 83 and 166 were included in analysis, respectively), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation for pneumonia; pneumonia was clinically defined and radiologically confirmed | |
| Notes | The study controls for confounders in analysis: health status, age, socio‐economic factors. The season probably had low epidemic levels. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Case‐control study conducted in Valencia, Spain during the 2002 to 2003 influenza season, in the community. Data sources were: hospital records; structured interview by trained field investigator. Follow‐up period was 15 November 2002 to 31 March 2003. Cases were people admitted to hospital for pneumonia; controls were admitted to hospital in the same week for acute abdominal surgical condition or trauma. | |
| Participants | 815 non‐institutionalised people (325 cases and 525 controls were identified; 290 and 525 were included in analysis, respectively), 65 years or older | |
| Interventions | Parenteral influenza MF59 adjuvant vaccine. 42% of cases and 34% of controls received pneumococcal vaccination. Vaccine strains matched the circulating strain. | |
| Outcomes | Hospitalisation for pneumonia (ICD‐9 code 480‐487); pneumonia was clinically defined and radiologically confirmed | |
| Notes | The study controls for confounders in analysis: health status, smoking habits, pneumococcal vaccination. The season had low epidemic levels. Quantitative analysis was also performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | 3 case‐control studies were performed in the elderly population (> 64 years of age) of 3 health districts in the Valencia Autonomous Region, Spain (total number of elderly residents in these districts: n = 105,454 at 31 December 2004), where MF59‐adjuvanted subunit influenza vaccine was used. The risk of hospitalisation for ACS, CVA, or pneumonia was evaluated for people who had received influenza vaccine and for those who had not received influenza vaccine. | |
| Participants | Description of cases Incident cases for each disease were identified from all consecutive emergency hospitalisations following their admission between 15 November 2004 and 31 March 2005. Diagnoses were made according to the International Classification of Diseases, 9th version, Clinical Modification for ACS (410‐411.89 and 413), CVA (431‐436), or pneumonia (480‐487). Only non‐institutionalised patients who were > 64 years of age, had lived in the hospital catchment area for the previous 6 months, were able to give informed consent, and remained in hospital for at least 72 hours were included in the study. After consideration of the exclusion criteria, 144 cases admitted for ACS, 134 for CVA, and 198 for pneumonia were included in the study. Description of controls Each case was paired with 1 or 2 controls, matched for hospital and gender. Controls were recruited based on the same inclusion criteria as cases, following emergency hospitalisations for an acute surgical process or trauma. The admission date for controls was matched to the case admission date, preferably being the same day, and with a maximum interval of 10 days. 258 controls were admitted for ACS, 246 for CVA, and 321 for pneumonia. A total of 75.2% and 78.1% of vaccinated cases and controls, respectively (P = 0.314) were vaccinated and on the population register. Of these, all cases and 99.73% of controls had received MF59‐adjuvanted subunit influenza vaccine. | |
| Interventions | Influenza vaccination and hospitalisation for ACS, CVA, and pneumonia | |
| Outcomes | — | |
| Notes | The authors conclude that the results suggest that MF59‐adjuvanted influenza vaccination is associated with a significant reduction in the risk of hospitalisation for ACS, CVA, and pneumonia during the period of influenza virus circulation. | |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home in California, USA during the 1972 to 1973 influenza season; independent blind assessment was conducted. Follow‐up period was 20 December 1972 to 28 January 1973. Throat swabs were obtained from ill residents. | |
| Participants | 392 nursing home residents (204 treated and 192 controls, all included in the analysis). Participants were both ambulatory and bedridden. | |
| Interventions | Parenteral influenza vaccine: A/Aichi/2/62; B/Mass/1/71. Vaccine strains did not match circulating strains. | |
| Outcomes | Clinically defined ILI (fever 37.7 °C + upper respiratory symptoms), laboratory‐confirmed ILI (positive swab culture), deaths from outbreak‐related respiratory illness | |
| Notes | Data stratified by nurse floor. The circulating strain was A/ENG/42/72. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Experimental study conducted in Russia during the 1996 to 1997 influenza season, randomised, double‐blind, placebo controlled; random sample stratified by age and underlying health conditions. Follow‐up period was 20 January 1997 to 2 March 1997 | |
| Participants | 602 nursing home residents (93 vaccinated with parenteral vaccine, 111 vaccinated with aerosol vaccine, and 109 controls); severely debilitated and immunosuppressed people were excluded; 41 to 95 years, median 73 years | |
| Interventions | Live cold‐adapted vaccine aerosol administered: A/Leningrad/134/17/57; B/Ann Arbor/60/69 parenteral vaccine: A/Texas/36/91; A/Nanchang/933/95; B/Harbin/7/94. Vaccine strains matched the circulating strains | |
| Outcomes | Laboratory‐confirmed influenza: positive swab or 4‐fold or greater increase in antibody titre | |
| Notes | No description of methods; 1 or 2 doses' efficacy was tested; data were extracted irrespective of the number of doses administered | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Random allocation sequence not described and the six groups have uneveven denominators |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | High risk | Unexplained attrition both for efficacy and serological outcomes. Harms are not mentioned at all in the report. This is a particular problem in the use of live attenuated vaccines in elderly or infirm people |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in New York, USA during the 1979 to 1980 influenza season. Authors investigated a nursing home with evidence of flu activity; medical records were reviewed. Comparability between cohorts was assessed by analysis of the underlying conditions of a sample of the population; 62 people with severe organic brain syndrome were excluded. Follow‐up period was 1 November 1979 to 30 April 1980. | |
| Participants | 453 residents in nursing home for healthy and ill elderly (219 treated and 234 controls, all included in the analysis); most patients required skilled nursing home care | |
| Interventions | Parenteral influenza vaccine: A/Brazil/78; A/Texas/77; B/Hong Kong/72. Matching between vaccine and circulating strains is unknown. | |
| Outcomes | Symptoms defined and radiologically confirmed pneumonia; death from pneumonia within 60 days from the onset of pneumonia | |
| Notes | Vaccinated participants had very slight excess of underlying conditions; smokers were rare; pneumococcal vaccine was rarely used. Specific viral diagnosis was not attempted, but the circulating strain in the community was B/Singapore/79‐like. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in New York, USA during the 1980 to 1981 influenza season. Authors investigated a nursing home with evidence of flu activity; medical records were reviewed. Comparability between cohorts was assessed by analysis of the underlying conditions of a sample of the population; 62 people with severe organic brain syndrome were excluded. Follow‐up period was 1 November 1980 to 30 April 1981. | |
| Participants | 458 residents in nursing home for healthy and ill elderly (244 treated and 214 controls, all included in the analysis); most patients required skilled nursing home care | |
| Interventions | Parenteral influenza vaccine: A/Brazil/78; A/Bangkok/79; B/Singapore/79. Vaccine strains matched circulating strains. | |
| Outcomes | Symptoms defined and radiologically confirmed pneumonia; death from pneumonia within 60 days from the onset of pneumonia | |
| Notes | Vaccinated participants had very slight excess of underlying conditions; smokers were rare; pneumococcal vaccine was rarely used. Specific viral diagnosis was not attempted, but the circulating strain in the community was A/Bangkok/79‐like. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in New York, USA during the 1981 to 1982 influenza season in 26 nursing homes. Comparability between cohorts was assessed by analysis of the underlying conditions of a sample of the population; 62 people with severe organic brain syndrome were excluded; medical records were reviewed. Follow‐up period was 1 November 1981 to 30 April 1982. | |
| Participants | 451 residents in nursing home for healthy and ill elderly (225 treated and 226 controls, all included in the analysis); most patients required skilled nursing home care | |
| Interventions | Parenteral influenza vaccine: A/Brazil/78; A/Bangkok/79; B/Singapore/80. Matching between vaccine and circulating strains is unknown. | |
| Outcomes | Symptoms defined and radiologically confirmed pneumonia; death from pneumonia within 60 days from the onset of pneumonia | |
| Notes | Vaccinated participants had very slight excess of underlying conditions; smokers were rare; pneumococcal vaccine was rarely used. The circulating strain was not identified. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Japan during the 1998 to 1999 influenza season in 9 nursing homes. Follow‐up period was the epidemic period. Efficacy assessment was also performed by vaccination rate in residents and HCWs, physical impairment, sex, age, and health status of residents. Throat swabs were obtained from ill individuals; medical charts were reviewed. | |
| Participants | 699 residents in 9 nursing homes (331 treated and 368 controls, all included in the analysis). The vaccinated group had more underlying diseases. | |
| Interventions | Parenteral influenza vaccine: A/Beijing/262/95; A/Sydney/5/97; B/Mie/1/93. Vaccine strains matched circulating strains (good match). | |
| Outcomes | Clinically defined ILI (fever + cough or coryza or sore throat) occurring during the epidemic period | |
| Notes | The circulating strain was A/Sydney. Influenza virus exposure was confirmed in all 9 facilities. Outbreaks were demonstrated in only 4 homes. No other respiratory viruses were isolated. Data were extracted by RRs reported in tables. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Prospective cohort study conducted in Japan during the 1999 to 2000 influenza season in 11 nursing homes. Follow‐up period was the epidemic period. Efficacy assessment was also performed by vaccination rate in residents and HCWs, physical impairment, sex, age, and health status of residents. Throat swabs were obtained from ill individuals; medical charts were reviewed. | |
| Participants | 930 residents in 11 nursing homes (743 treated and 187 controls, all included in the analysis). The vaccinated group had more physical impairment of daily living. | |
| Interventions | Parenteral influenza vaccine: A/Beijing/262/95; A/Sydney/5/97; B/Shandon/7/97. Vaccine strains matched circulating strains (good match). | |
| Outcomes | Clinically defined ILI (fever + cough or coryza or sore throat) occurring during the epidemic period | |
| Notes | The circulating strain was A/Sydney. Influenza virus exposure was confirmed in only 4/11 facilities. No outbreaks were detected. No other respiratory viruses were isolated. Data were extracted by RRs reported in tables. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Surveillance population‐based study conducted in the USA during the 1976 to 1977 influenza season. Neurologists were directly contacted; physician and hospital records were reviewed. Suspected cases reported to the Centers for Disease Control and Prevention directly by patients or medical personnel were included only if accepted by a state health department. Follow‐up period was 1 October 1976 to 31 January 1977. | |
| Participants | USA population | |
| Interventions | Monovalent A/New Jersey/76 or bivalent A/New Jersey/76 and A/Victoria/75 parenteral vaccine | |
| Outcomes | Cases of Guillain‐Barré syndrome | |
| Notes | Results were stratified by age group and vaccine type. Vaccination rates in population were obtained from national immunisation survey. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Study characteristics | ||
| Methods | Retrospective cohort study conducted in Israel during the 2000 to 2001 influenza season, in the community. Data source was managed care organisation database. Follow‐up period was the entire influenza season. | |
| Participants | 84,640 community‐dwelling elderly (36,596 treated and 48,044 controls included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strain probably matched the circulating strain (literature). | |
| Outcomes | Hospitalisation for any reason; deaths from all causes | |
| Notes | Very poor description of methods; no information about flu activity: probably not epidemic year. Data were presented by health status. Only deaths were included in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home in Los Angeles, USA during the 1982 to 1983 influenza season; patients records were reviewed. Follow‐up period was 1 February 1983 to 31 March 1983. Virus circulation was confirmed with throat swab from ill people. | |
| Participants | 87 nursing home residents, 59 to 94 years old, most of them suffering from dementia (65 treated and 19 controls were included in the analysis; vaccination status could not be determined for 3 residents) | |
| Interventions | Parenteral influenza vaccine: A/Bangkok/79; A/Brazil/78; B/Singapore/79. Vaccine strains probably matched circulating strains. | |
| Outcomes | Clinically defined ILI (fever or fever + respiratory symptoms) occurring during the epidemic period, deaths from ILI | |
| Notes | Age, sex ratio, and health status were similar in vaccinated and unvaccinated people. The circulating strain was A/Bangkok/79‐like. No other positive laboratory findings were found. Amantadine was not used. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Experimental study conducted in California, USA during the 1965 to 1966 influenza season; the control group received influenza B vaccine, placebo, or no vaccine; laboratory samples were obtained from ill people to confirm the infection active surveillance. Follow‐up period was 1 February 1966 to 30 April 1966. | |
| Participants | 4180 residents in the nursing home, healthy (1561 treated and 2619 controls were included in the analysis), 52 years or older | |
| Interventions | Monovalent A2 parenteral influenza vaccine: A2/Taiwan/1/64. Vaccine strains matched the circulating strains | |
| Outcomes | Clinically defined febrile illness (fever + cough or malaise or coryza or myalgia or headache), clinically defined afebrile illness, hospitalisation and deaths without definition. | |
| Notes | Participants randomised the previous year but not vaccinated (reason not explained) in the current year were added in the control group; the study year was an epidemic one | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient details available to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient details available to permit judgement |
| Blinding (performance bias and detection bias) | High risk | Open‐label design |
| Incomplete outcome data (attrition bias) | Low risk | Data available for most participants in the study |
| Study characteristics | ||
| Methods | Authors investigated an outbreak in a nursing home in Washington, USA during the 1988 to 1989 influenza season; residents' records and hospital charts were reviewed. Follow‐up period was 29 January 1989 to 1 March 1989. Throat swabs were obtained from a sample of acutely ill residents; paired sera were obtained from 63% of both ill and well residents. | |
| Participants | 109 nursing home residents (48 treated and 61 controls; 45 and 52 included in the analysis, respectively), 58 to 105 years old. Groups were similar in age, gender, and level of care required. | |
| Interventions | Parenteral influenza vaccine: A/Taiwan; A/Sichuan; B/Victoria. Vaccine strains probably matched circulating strains. | |
| Outcomes | Outbreak‐associated cases: clinically defined ILI (fever + cough) or laboratory‐confirmed influenza (4‐fold increase in antibody titre), pneumonia, hospitalisation from ILI or pneumonia, deaths from ILI or pneumonia | |
| Notes | Vaccination was not offered to staff. Positive specimens showed a diagnostic titre rise to A/Sichuan, but no virus was isolated; matching was only hypothetic. Amantadine was not used. Laboratory‐confirmed cases were analysed by intention‐to‐treat. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Study characteristics | ||
| Methods | Experimental study conducted in New York, USA during the 1990 to 1991 influenza season, randomised, double‐blind, placebo‐controlled study. 34 participants received live vaccine; 30 participants received trivalent vaccine; 11 participants received placebo. Follow‐up period was for 7 days after vaccination. Participants filled self administered diary card. | |
| Participants | 75 outpatients with chronic disease or elderly, mostly 65 years or older | |
| Interventions | Live cold‐adapted influenza B virus vaccine, aerosol administered; parenteral trivalent influenza vaccine | |
| Outcomes | Upper respiratory symptoms (coryza or sore throat), lower respiratory symptoms (cough, hoarseness, or dyspnoea), systemic symptoms (malaise and myalgia), sore arm, fever | |
| Notes | Participants experiencing symptoms within 1 week of vaccination were considered. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not described. |
| Blinding (performance bias and detection bias) | Unclear risk | Described as placebo controlled, but no further details available |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Study characteristics | ||
| Methods | Retrospective cohort study conducted in the Netherlands during the 1996 to 1997 influenza season, in the community. Data source was the managed care organisation database. Follow‐up period was 1 September 1996 to 1 June 1997. For every individual who had received an influenza vaccination, 1 age‐sex matched unvaccinated control participant was randomly selected. | |
| Participants | 17,822 community‐dwelling elderly with a permanent status in 1 of the practices (8911 treated and 8911 controls, all included in the analysis), 65 years or older | |
| Interventions | Parenteral influenza vaccine. Vaccine strain matched the circulating strain. | |
| Outcomes | Influenza as defined by International Classification of Primary Care (R80: proven influenza without pneumonia), pneumonia, deaths from all causes | |
| Notes | The influenza season was relatively mild. Data were stratified by age and health status. Quantitative analysis was also performed only for the outcome 'deaths from all causes'. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
ACS = acute coronary syndromes
CAP = community‐acquired pneumonia
CVA = cerebrovascular accident
HCWs = healthcare workers
ICD = International Classification of Diseases
ILI = influenza‐like illness
NI = neuroaminidase inhibitor
OR = odds ratio
RR = risk ratio
URI = upper respiratory infection
WHO = World Health Organization
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Elderly denominator 19 and no breakdown of cases by age groups is given | |
| See Allsup 2004 | |
| Comment | |
| No data presented. | |
| Cross‐sectional study | |
| Review | |
| Data presented cannot be used in the analysis; the statistical model is not comparable with that used in the other studies. | |
| Description of epidemic | |
| No data presented. | |
| No placebo/do nothing comparator: influenza + pneumococcus versus influenza vaccine | |
| Lack of a control group | |
| Cross‐sectional study | |
| No original data presented. | |
| Children and adults | |
| No placebo/do nothing comparator | |
| The study does not investigate the vaccine efficacy. | |
| Lack of a control group | |
| Data are not presented by vaccine condition. | |
| Retrospective paper looking at vaccination cover in > 65 and relations with effectiveness claimed as efficacy. Only 60 influenza‐like illness cases were tested out of a total of 2300. | |
| The study does not investigate the vaccine efficacy. | |
| This could be a cohort study to be considered for the adults review. | |
| Same cohorts of Christenson 2001 | |
| High‐risk groups | |
| Does not present original data | |
| Lack of a control group | |
| Same cohorts of Govaert 1994a | |
| Both arms administered influenza vaccine, no placebo/do nothing comparator. | |
| Healthy adults; lack of a control group | |
| Serological outcome only | |
| Same cohorts of Deguchi 2001 | |
| Same cohorts of Deguchi 2001 | |
| Same cohorts of Deguchi 2001 | |
| The study does not investigate the vaccine efficacy. | |
| Same data set as Skowronski ‐ high‐risk group | |
| Healthy adults | |
| Assessment of vitamins before vaccination as immunomodulators | |
| Frequency data are not reported; outcome is not clearly defined. | |
| The study does not investigate the vaccine efficacy. | |
| Comment | |
| Economic study without original data | |
| The study does not investigate the vaccine efficacy. | |
| Serological outcome only | |
| Data presented cannot be estimated for the analysis. | |
| Healthy adults | |
| Case report | |
| Only 16% of participants are over the age of 60. | |
| Economic study; data source not described | |
| Economic evaluation | |
| No original data presented. | |
| Unclear study design; probably retrospective cohort based only on individual recall of disease | |
| The study does not investigate the vaccine efficacy. | |
| The study does not investigate the vaccine efficacy. | |
| The study does not investigate the vaccine efficacy. | |
| Antibody outcomes only | |
| The study does not investigate the vaccine efficacy. | |
| Study population is children. | |
| Study population is children. | |
| Study population is children. | |
| Review | |
| Serological survey | |
| The study does not investigate the vaccine efficacy. | |
| Unclear study design; probably retrospective cohort based only on individual recall of disease; 1‐year follow‐up | |
| High‐risk groups | |
| The study does not investigate the vaccine efficacy. | |
| Economic review | |
| Redundant publication of Hara 2006 | |
| NI used | |
| Comment | |
| Same cohorts of Christenson 2001 | |
| Economic evaluation | |
| Cross‐sectional study | |
| The study does not investigate the vaccine efficacy. | |
| Same cohorts of Shapiro 2003 | |
| Healthy adults | |
| Study population is children. | |
| The study does not investigate the vaccine efficacy. | |
| Not elderly | |
| Non‐comparative data | |
| Unclear study design; probably cross‐sectional | |
| Poorly described study. Influenza‐like illness was defined only as "fever". Deaths from all causes referred to too long a period (from January to September). | |
| Poorly described study. Influenza‐like illness was defined only as "fever". Asymptomatic infections were indistinguishable from symptomatic ones. | |
| Inadequate comparator | |
| High‐risk groups | |
| High‐risk groups | |
| Economic evaluation | |
| Case report | |
| The study does not investigate the vaccine efficacy. | |
| Lack of a control group; high‐risk groups | |
| Non‐comparative design | |
| No data | |
| Comment | |
| Case report | |
| Cost‐of‐illness study | |
| Non‐comparative study | |
| 1‐year follow‐up in a population with important diseases | |
| Same data set as Landi 2003 | |
| No placebo/do nothing comparator, serological responses and age group? | |
| Frequency data not reported. | |
| Case report | |
| Case report | |
| Economic evaluation | |
| Lack of a control group | |
| Descriptive | |
| Case report | |
| Feasibility study of general practice reporting method to assess vaccine effectiveness | |
| No placebo/do nothing comparator | |
| Serological outcome only | |
| Serological outcome only | |
| Lack of a control group | |
| Comment | |
| Antibody only | |
| No data presented. | |
| No data presented. | |
| No data presented. | |
| No data presented. | |
| No data presented. | |
| No data presented. | |
| Interruption study | |
| Study population is children and adults. | |
| Comment | |
| Case report | |
| Lack of a control group | |
| Children | |
| No data presented. | |
| Non‐systematic review and meta‐analysis with metaviews back to front | |
| Lack of a control group | |
| No data presented. | |
| Unclear study design | |
| Same cohorts of Nichol 1994 | |
| No original effectiveness data presented. | |
| Same cohorts of Nichol 1994 | |
| High‐risk groups | |
| Adult population | |
| Same cohorts of Nichol 1998 | |
| Data already included in review from other publication by the same author | |
| No placebo/do nothing comparator | |
| Lack of a control group | |
| Unclear study design; symptomatic participants only | |
| No data presented. | |
| Unclear study design; symptomatic participants only | |
| No data presented. | |
| No data presented. | |
| Lack of a control group | |
| Lack of a control group | |
| Same population as Ohmit 1995 | |
| Data already included in the 2005 review; re‐analysis of the same data set | |
| Ecological study | |
| Case series | |
| No data | |
| Case report | |
| The study does not investigate the vaccine efficacy. | |
| Comment | |
| The study does not investigate the vaccine efficacy. | |
| Case report | |
| Review of economic evaluations | |
| Lack of a control group | |
| Serological outcomes | |
| Data are not presented by age. | |
| Lack of a control group | |
| Comment | |
| Study population is children. | |
| Not about vaccine effectiveness | |
| Review | |
| Data are not presented by vaccine condition. | |
| Serological outcome only | |
| Not about vaccine effectiveness | |
| The study does not investigate the vaccine efficacy. | |
| Serological outcome only | |
| Unclear study design | |
| Review | |
| Review | |
| Guideline | |
| Not about vaccines | |
| Does not report safety outcomes by age group | |
| Not about vaccines | |
| No outcome data by vaccine status, uncertain denominators | |
| Review | |
| Serological outcome only | |
| No data | |
| Review | |
| Children | |
| Only 1 participant was unvaccinated. | |
| Antibody titres and no placebo/do nothing comparator | |
| Not about vaccines | |
| Not about vaccines | |
| No placebo/do nothing comparator | |
| Not about vaccines | |
| Data only in graphs | |
| Antibody responses | |
| Not about vaccines | |
| Poor description; data do not fit the comparison of this review | |
| Comment | |
| Case report | |
| Very poor description; absence of definitions, incoherence between data reported in text and data reported in tables | |
| Not about vaccines | |
| Descriptive study | |
| No data | |
| Comment | |
| The study does not investigate the vaccine efficacy. | |
| Ecological study | |
| High‐risk groups | |
| Study assessing risk factors for community‐acquired pneumonia. Insufficient data presented for evaluation of influenza vaccine effectiveness. | |
| Ecological study | |
| Comment | |
| Lack of a control group | |
| Case report | |
| Case report | |
| Case report | |
| Healthy adults | |
| The study does not investigate the vaccine efficacy. | |
| No placebo/do nothing comparator | |
| Unclear study design | |
| Letter with no data | |
| Comment | |
| Review | |
| Lack of a control group | |
| Lack of a control group | |
| Model based on aspecific outcomes | |
| Descriptive study | |
| Antibody titres | |
| The study does not investigate the vaccine efficacy. | |
| No data presented. | |
| Not about effectiveness | |
| Insufficient data | |
| Serological outcomes | |
| Ethical study | |
| Insufficient data reported. | |
| Serological outcomes | |
| Lack of a control group | |
| Insufficient data reported (denominators are not reported). | |
| Review | |
| Lacks controls | |
| Comment | |
| The study does not investigate the vaccine efficacy. | |
| Comment | |
| 1‐year follow‐up | |
| Ecological study | |
| Review | |
| Review | |
| The study does not investigate the vaccine efficacy. | |
| Comment | |
| Comment | |
| Comment | |
| Survey of cases | |
| Healthy adults | |
| Review | |
| Methodological paper | |
| Vaccine and amantadine were used to control outbreak: amantadine acts as confounder. | |
| The study does not investigate the vaccine efficacy. | |
| Not about vaccine effectiveness | |
| Not about vaccine effectiveness | |
| Serological outcome only | |
| Serological outcome only | |
| Serological outcome only | |
| Serological outcome only |
NI: neuoraminidase inhibitors
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Influenza Show forest plot | 3 | 2217 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.27, 0.66] |
| Analysis 1.1  Comparison 1: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine, Outcome 1: Influenza | ||||
| 1.1.1 Outbreak ‐ vaccine matching ‐ community ‐ healthy and ill | 1 | 1838 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.23, 0.74] |
| 1.1.2 Outbreak ‐ vaccine matching ‐ psychiatric hospital | 1 | 177 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.12, 1.06] |
| 1.1.3 No outbreak ‐ vaccine matching ‐ nursing home ‐ healthy and ill | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.20, 1.25] |
| 1.2 Influenza‐like illness Show forest plot | 4 | 6894 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.47, 0.73] |
| Analysis 1.2  Comparison 1: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine, Outcome 2: Influenza‐like illness | ||||
| 1.2.1 Outbreak ‐ vaccine matching (circulating strains) ‐ community ‐ healthy | 2 | 2047 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.42, 0.79] |
| 1.2.2 Outbreak ‐ vaccine matching ‐ community ‐ risk groups | 1 | 490 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.49, 1.53] |
| 1.2.3 Outbreak ‐ vaccine matching ‐ nursing home ‐ healthy | 1 | 4180 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.37, 0.80] |
| 1.2.4 Outbreak ‐ vaccine matching ‐ psychiatric hospital | 1 | 177 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.13, 0.92] |
| 1.3 Pneumonia Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine, Outcome 3: Pneumonia | ||||
| 1.3.1 Outbreak ‐ vaccine matching ‐ community ‐ healthy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.4 All deaths Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine, Outcome 4: All deaths | ||||
| 1.4.1 Outbreak ‐ vaccine matching ‐ community ‐ healthy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 General malaise Show forest plot | 4 | 2560 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.87, 1.61] |
| Analysis 2.1  Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 1: General malaise | ||||
| 2.2 Nausea Show forest plot | 1 | 672 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.74, 4.12] |
| Analysis 2.2  Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 2: Nausea | ||||
| 2.3 Upper respiratory tract symptoms Show forest plot | 2 | 713 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.90, 2.01] |
| Analysis 2.3  Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 3: Upper respiratory tract symptoms | ||||
| 2.4 Headache Show forest plot | 3 | 2519 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.76, 1.58] |
| Analysis 2.4  Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 4: Headache | ||||
| 2.5 Fever Show forest plot | 3 | 2519 | Risk Ratio (M‐H, Random, 95% CI) | 1.57 [0.92, 2.71] |
| Analysis 2.5  Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 5: Fever | ||||
| 2.6 Local tenderness/sore arm Show forest plot | 4 | 2560 | Risk Ratio (M‐H, Random, 95% CI) | 3.56 [2.61, 4.87] |
| Analysis 2.6  Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 6: Local tenderness/sore arm | ||||
| 2.7 Swelling ‐ erythema ‐ induration Show forest plot | 2 | 1847 | Risk Ratio (M‐H, Random, 95% CI) | 8.23 [3.98, 17.05] |
| Analysis 2.7  Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 7: Swelling ‐ erythema ‐ induration | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Influenza Show forest plot | 1 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.40, 1.99] |
| Analysis 3.1  Comparison 3: Influenza vaccines versus placebo: randomised controlled trials ‐ inactivated aerosol vaccine, Outcome 1: Influenza | ||||
| 3.1.1 Outbreak ‐ vaccine matching ‐ psychiatric hospital | 1 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.40, 1.99] |
| 3.2 Influenza‐like illness Show forest plot | 1 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.41, 1.71] |
| Analysis 3.2  Comparison 3: Influenza vaccines versus placebo: randomised controlled trials ‐ inactivated aerosol vaccine, Outcome 2: Influenza‐like illness | ||||
| 3.2.1 Outbreak ‐ vaccine matching ‐ psychiatric hospital | 1 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.41, 1.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Influenza Show forest plot | 1 | 220 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.21, 1.17] |
| Analysis 4.1  Comparison 4: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine, Outcome 1: Influenza | ||||
| 4.1.1 No outbreak ‐ vaccine matching ‐ nursing home ‐ healthy and ill | 1 | 220 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.21, 1.17] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 General malaise Show forest plot | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 3.09 [0.18, 53.20] |
| Analysis 5.1  Comparison 5: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine ‐ adverse events, Outcome 1: General malaise | ||||
| 5.2 Fever Show forest plot | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 1.71 [0.09, 33.24] |
| Analysis 5.2  Comparison 5: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine ‐ adverse events, Outcome 2: Fever | ||||
| 5.3 Upper respiratory tract symptoms Show forest plot | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 1.62 [0.42, 6.29] |
| Analysis 5.3  Comparison 5: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine ‐ adverse events, Outcome 3: Upper respiratory tract symptoms | ||||
| 5.4 Lower respiratory tract symptoms Show forest plot | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 2.91 [0.41, 20.48] |
| Analysis 5.4  Comparison 5: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine ‐ adverse events, Outcome 4: Lower respiratory tract symptoms | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 Influenza Show forest plot | 8 | 1941 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.32, 1.29] |
| Analysis 6.1  Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 1: Influenza | ||||
| 6.1.1 Outbreak ‐ vaccine matching | 4 | 658 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.43, 2.51] |
| 6.1.2 Outbreak ‐ vaccine matching absent or unknown | 2 | 592 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.22, 1.04] |
| 6.1.3 No outbreak ‐ vaccine matching | 2 | 691 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.05, 1.03] |
| 6.1.4 No outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.2 Influenza‐like illness Show forest plot | 26 | 12388 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.66, 0.88] |
| Analysis 6.2  Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 2: Influenza‐like illness | ||||
| 6.2.1 Outbreak ‐ vaccine matching (circulating strains) | 16 | 5963 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.64, 0.94] |
| 6.2.2 Outbreak ‐ vaccine matching absent or unknown | 6 | 4096 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.60, 1.05] |
| 6.2.3 No outbreak ‐ vaccine matching | 4 | 2329 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.46, 0.98] |
| 6.2.4 No outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.3 Pneumonia Show forest plot | 17 | 10274 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.43, 0.66] |
| Analysis 6.3  Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 3: Pneumonia | ||||
| 6.3.1 Outbreak ‐ vaccine matching | 8 | 4482 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.42, 0.70] |
| 6.3.2 Outbreak ‐ vaccine matching absent or unknown | 5 | 3991 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.39, 1.21] |
| 6.3.3 No outbreak ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.3.4 No outbreak ‐ matching absent or unknown | 4 | 1801 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.18, 0.68] |
| 6.4 Hospitalisation for influenza‐like illness or pneumonia Show forest plot | 12 | 28032 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.32, 0.81] |
| Analysis 6.4  Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 4: Hospitalisation for influenza‐like illness or pneumonia | ||||
| 6.4.1 Outbreak ‐ vaccine matching | 8 | 2027 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.36, 0.84] |
| 6.4.2 Outbreak ‐ vaccine matching absent or unknown | 2 | 3301 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.43, 1.58] |
| 6.4.3 No outbreak ‐ vaccine matching | 2 | 22704 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.14, 0.76] |
| 6.4.4 No outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.5 Deaths from flu or pneumonia Show forest plot | 27 | 32179 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.33, 0.63] |
| Analysis 6.5  Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 5: Deaths from flu or pneumonia | ||||
| 6.5.1 Outbreak ‐ vaccine matching | 16 | 6127 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.41, 0.83] |
| 6.5.2 Outbreak ‐ vaccine matching absent or unknown | 4 | 1089 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.11, 1.02] |
| 6.5.3 No outbreak ‐ vaccine matching | 3 | 23162 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.09, 0.87] |
| 6.5.4 No outbreak ‐ vaccine matching absent or unknown | 4 | 1801 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.14, 0.67] |
| 6.6 All deaths Show forest plot | 1 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.21, 0.77] |
| Analysis 6.6  Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 6: All deaths | ||||
| 6.6.1 Outbreak ‐ vaccine matching | 1 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.21, 0.77] |
| 6.6.2 Outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.6.3 No outbreak ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.6.4 No outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.7 Influenza cases (clinically defined without clear definition) Show forest plot | 7 | 24238 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.27, 1.02] |
| Analysis 6.7  Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 7: Influenza cases (clinically defined without clear definition) | ||||
| 6.7.1 Outbreak ‐ vaccine matching | 2 | 271 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.11, 4.56] |
| 6.7.2 Outbreak ‐ vaccine matching absent or unknown | 1 | 155 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.09, 0.59] |
| 6.7.3 No outbreak ‐ vaccine matching | 1 | 22462 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.35, 0.46] |
| 6.7.4 No outbreak ‐ vaccine matching absent or unknown | 3 | 1350 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.41, 1.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Influenza‐like illness Show forest plot | 1 | 1198 | Odds Ratio (M‐H, Random, 95% CI) | 0.52 [0.40, 0.68] |
| Analysis 7.1  Comparison 7: Influenza and pneumococcal vaccines versus no vaccination: case‐control studies in nursing homes, Outcome 1: Influenza‐like illness | ||||
| 7.1.1 Outbreak ‐ vaccine matching | 1 | 1198 | Odds Ratio (M‐H, Random, 95% CI) | 0.52 [0.40, 0.68] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 8.1 Influenza Show forest plot | 2 | 18249 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.02, 2.01] |
| Analysis 8.1  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 1: Influenza | ||||
| 8.1.1 Epidemic year ‐ vaccine matching | 1 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 0.05 [0.01, 0.37] |
| 8.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 17822 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.27, 0.91] |
| 8.1.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.2 Influenza‐like illness Show forest plot | 4 | 9613 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.42, 1.33] |
| Analysis 8.2  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 2: Influenza‐like illness | ||||
| 8.2.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.2.3 Non‐epidemic year ‐ vaccine matching | 2 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.58, 2.03] |
| 8.2.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 268 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.16, 4.55] |
| 8.2.5 Epidemic year ‐ vaccine not matching | 1 | 4709 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.24, 0.81] |
| 8.3 Pneumonia Show forest plot | 2 | 18090 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.64, 1.20] |
| Analysis 8.3  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 3: Pneumonia | ||||
| 8.3.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.3.3 Non‐epidemic year ‐ vaccine matching | 1 | 17822 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.63, 1.19] |
| 8.3.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 268 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.16, 57.42] |
| 8.4 Hospitalisation for flu or pneumonia Show forest plot | 9 | 784643 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.62, 0.85] |
| Analysis 8.4  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 4: Hospitalisation for flu or pneumonia | ||||
| 8.4.1 Epidemic year ‐ vaccine matching | 6 | 727776 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.62, 0.88] |
| 8.4.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.4.3 Non‐epidemic year ‐ vaccine matching | 1 | 25532 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.37, 0.83] |
| 8.4.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 26626 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.54, 0.99] |
| 8.4.5 Epidemic year ‐ vaccine not matching | 1 | 4709 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.33, 2.40] |
| 8.5 Hospitalisation for any respiratory disease Show forest plot | 5 | 567299 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.54, 1.43] |
| Analysis 8.5  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 5: Hospitalisation for any respiratory disease | ||||
| 8.5.1 Epidemic year ‐ vaccine matching | 3 | 515141 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.37, 1.64] |
| 8.5.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.5.3 Non‐epidemic year ‐ vaccine matching | 1 | 25532 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.79, 1.12] |
| 8.5.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 26626 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [1.01, 1.34] |
| 8.6 Deaths from flu or pneumonia Show forest plot | 1 | 163391 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.70, 1.09] |
| Analysis 8.6  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 6: Deaths from flu or pneumonia | ||||
| 8.6.1 Epidemic year ‐ vaccine matching | 1 | 163391 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.70, 1.09] |
| 8.6.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.6.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.6.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.7 Deaths from respiratory disease Show forest plot | 1 | 426668 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.25, 1.39] |
| Analysis 8.7  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 7: Deaths from respiratory disease | ||||
| 8.7.1 Epidemic year ‐ vaccine matching | 1 | 426668 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.25, 1.39] |
| 8.8 All deaths Show forest plot | 8 | 409468 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.47, 0.80] |
| Analysis 8.8  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 8: All deaths | ||||
| 8.8.1 Epidemic year ‐ vaccine matching | 4 | 300332 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.50, 0.70] |
| 8.8.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.8.3 Non‐epidemic year ‐ vaccine matching | 3 | 104427 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.30, 1.39] |
| 8.8.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.8.5 Epidemic year ‐ vaccine not matching | 1 | 4709 | Risk Ratio (M‐H, Random, 95% CI) | 3.89 [0.90, 16.89] |
| 8.9 Hospitalisation for heart disease Show forest plot | 6 | 433934 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.67, 1.12] |
| Analysis 8.9  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 9: Hospitalisation for heart disease | ||||
| 8.9.1 Epidemic year ‐ vaccine matching | 4 | 381776 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.56, 0.97] |
| 8.9.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.9.3 Non‐epidemic year ‐ vaccine matching | 1 | 25532 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.81, 1.38] |
| 8.9.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 26626 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.07, 2.36] |
| 8.10 Combined outcome: all deaths or severe respiratory illness Show forest plot | 3 | 290819 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.58, 0.85] |
| Analysis 8.10  Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 10: Combined outcome: all deaths or severe respiratory illness | ||||
| 8.10.1 Epidemic year ‐ vaccine matching | 2 | 132365 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.42, 1.55] |
| 8.10.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | 158454 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.69, 0.80] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 9.1 Hospitalisation for influenza or pneumonia Show forest plot | 8 | Odds Ratio (IV, Random, 95% CI) | 0.73 [0.67, 0.79] | |
| Analysis 9.1  Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 1: Hospitalisation for influenza or pneumonia | ||||
| 9.1.1 Epidemic ‐ vaccine matching | 6 | Odds Ratio (IV, Random, 95% CI) | 0.71 [0.65, 0.77] | |
| 9.1.2 Non‐epidemic ‐ vaccine not matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.90 [0.58, 1.38] | |
| 9.1.3 Epidemic year ‐ vaccine matching absent or unknown | 1 | Odds Ratio (IV, Random, 95% CI) | 0.82 [0.68, 0.98] | |
| 9.2 Hospitalisation for any respiratory disease Show forest plot | 13 | Odds Ratio (IV, Random, 95% CI) | 0.78 [0.72, 0.85] | |
| Analysis 9.2  Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 2: Hospitalisation for any respiratory disease | ||||
| 9.2.1 Epidemic ‐ vaccine matching | 9 | Odds Ratio (IV, Random, 95% CI) | 0.71 [0.67, 0.74] | |
| 9.2.2 Non‐epidemic ‐ vaccine not matching | 2 | Odds Ratio (IV, Random, 95% CI) | 0.91 [0.76, 1.08] | |
| 9.2.3 Non‐epidemic year ‐ vaccine matching | 2 | Odds Ratio (IV, Random, 95% CI) | 0.94 [0.84, 1.06] | |
| 9.3 Hospitalisation for heart disease Show forest plot | 6 | Odds Ratio (IV, Random, 95% CI) | 0.76 [0.70, 0.82] | |
| Analysis 9.3  Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 3: Hospitalisation for heart disease | ||||
| 9.3.1 Epidemic year ‐ vaccine matching | 5 | Odds Ratio (IV, Random, 95% CI) | 0.75 [0.70, 0.82] | |
| 9.3.2 Non‐epidemic ‐ vaccine not matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.80 [0.55, 1.16] | |
| 9.4 All deaths Show forest plot | 7 | Odds Ratio (IV, Random, 95% CI) | 0.53 [0.46, 0.61] | |
| Analysis 9.4  Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 4: All deaths | ||||
| 9.4.1 Epidemic year ‐ vaccine matching | 5 | Odds Ratio (IV, Random, 95% CI) | 0.47 [0.42, 0.53] | |
| 9.4.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | Odds Ratio (IV, Random, 95% CI) | 0.65 [0.57, 0.75] | |
| 9.4.3 Non‐epidemic year ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.76 [0.60, 0.97] | |
| 9.5 Combined outcome: all deaths or severe respiratory illness Show forest plot | 1 | Odds Ratio (IV, Random, 95% CI) | 0.70 [0.37, 1.34] | |
| Analysis 9.5  Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 5: Combined outcome: all deaths or severe respiratory illness | ||||
| 9.5.1 Epidemic year ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.70 [0.37, 1.34] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 10.1 Influenza Show forest plot | 1 | 6423 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.14, 1.17] |
| Analysis 10.1  Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 1: Influenza | ||||
| 10.1.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 6423 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.14, 1.17] |
| 10.1.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.2 Pneumonia Show forest plot | 1 | 6423 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.76, 1.94] |
| Analysis 10.2  Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 2: Pneumonia | ||||
| 10.2.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.2.3 Non‐epidemic year ‐ vaccine matching | 1 | 6423 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.76, 1.94] |
| 10.2.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.3 Hospitalisation for influenza or pneumonia Show forest plot | 1 | 45932 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.63, 0.86] |
| Analysis 10.3  Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 3: Hospitalisation for influenza or pneumonia | ||||
| 10.3.1 Epidemic year ‐ vaccine matching | 1 | 45932 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.63, 0.86] |
| 10.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.3.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.3.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.4 Hospitalisation for any respiratory disease Show forest plot | 2 | 189004 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.80, 0.92] |
| Analysis 10.4  Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 4: Hospitalisation for any respiratory disease | ||||
| 10.4.1 Epidemic year ‐ vaccine matching | 2 | 189004 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.80, 0.92] |
| 10.4.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.4.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.4.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.5 Deaths from respiratory disease Show forest plot | 1 | 142464 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.86, 0.98] |
| Analysis 10.5  Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 5: Deaths from respiratory disease | ||||
| 10.5.1 Epidemic year ‐ vaccine matching | 1 | 142464 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.86, 0.98] |
| 10.6 All deaths Show forest plot | 3 | 68032 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.16, 0.97] |
| Analysis 10.6  Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 6: All deaths | ||||
| 10.6.1 Epidemic year ‐ vaccine matching | 1 | 2344 | Risk Ratio (M‐H, Random, 95% CI) | 0.13 [0.02, 0.92] |
| 10.6.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.6.3 Non‐epidemic year ‐ vaccine matching | 2 | 65688 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.17, 1.28] |
| 10.6.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.7 Hospitalisation for heart disease Show forest plot | 1 | 45932 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.83, 1.03] |
| Analysis 10.7  Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 7: Hospitalisation for heart disease | ||||
| 10.7.1 Epidemic year ‐ vaccine matching | 1 | 45932 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.83, 1.03] |
| 10.7.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.7.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.7.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.8 Combined outcome: all deaths or severe respiratory illness Show forest plot | 2 | 146248 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.49, 0.74] |
| Analysis 10.8  Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 8: Combined outcome: all deaths or severe respiratory illness | ||||
| 10.8.1 Epidemic year ‐ vaccine matching | 1 | 54438 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.49, 0.60] |
| 10.8.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | 91810 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.61, 0.72] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 11.1 Influenza Show forest plot | 1 | 11399 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.27, 1.17] |
| Analysis 11.1  Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 1: Influenza | ||||
| 11.1.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 11399 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.27, 1.17] |
| 11.1.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.2 Pneumonia Show forest plot | 1 | 11399 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.37, 0.92] |
| Analysis 11.2  Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 2: Pneumonia | ||||
| 11.2.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.2.3 Non‐epidemic year ‐ vaccine matching | 1 | 11399 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.37, 0.92] |
| 11.2.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.3 Hospitalisation for influenza or pneumonia Show forest plot | 1 | 101619 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.40, 0.63] |
| Analysis 11.3  Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 3: Hospitalisation for influenza or pneumonia | ||||
| 11.3.1 Epidemic year ‐ vaccine matching | 1 | 101619 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.40, 0.63] |
| 11.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.3.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.3.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.4 Hospitalisation for any respiratory disease Show forest plot | 2 | 376324 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.55, 1.27] |
| Analysis 11.4  Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 4: Hospitalisation for any respiratory disease | ||||
| 11.4.1 Epidemic year ‐ vaccine matching | 2 | 376324 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.55, 1.27] |
| 11.4.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.4.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.4.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.5 Deaths from respiratory disease Show forest plot | 1 | 281424 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [1.31, 1.53] |
| Analysis 11.5  Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 5: Deaths from respiratory disease | ||||
| 11.5.1 Epidemic year ‐ vaccine matching | 1 | 281424 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [1.31, 1.53] |
| 11.6 All deaths Show forest plot | 3 | 43821 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.33, 1.29] |
| Analysis 11.6  Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 6: All deaths | ||||
| 11.6.1 Epidemic year ‐ vaccine matching | 1 | 7047 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.26, 4.49] |
| 11.6.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.6.3 Non‐epidemic year ‐ vaccine matching | 2 | 36774 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.27, 1.30] |
| 11.6.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.7 Hospitalisation for heart disease Show forest plot | 1 | 101619 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.61, 1.01] |
| Analysis 11.7  Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 7: Hospitalisation for heart disease | ||||
| 11.7.1 Epidemic year ‐ vaccine matching | 1 | 101619 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.61, 1.01] |
| 11.7.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.7.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.7.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.8 Combined outcome: all deaths or severe respiratory illness Show forest plot | 2 | 135180 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.54, 0.70] |
| Analysis 11.8  Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 8: Combined outcome: all deaths or severe respiratory illness | ||||
| 11.8.1 Epidemic year ‐ vaccine matching | 1 | 68536 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.54, 0.78] |
| 11.8.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | 66644 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.48, 0.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 12.1 Influenza‐like illness Show forest plot | 1 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.16, 0.64] |
| Analysis 12.1  Comparison 12: Influenza and pneumococcal vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 1: Influenza‐like illness | ||||
| 12.1.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.16, 0.64] |
| 12.2 Hospitalisation for influenza or pneumonia or respiratory disease Show forest plot | 3 | 518748 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.64, 0.70] |
| Analysis 12.2  Comparison 12: Influenza and pneumococcal vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 2: Hospitalisation for influenza or pneumonia or respiratory disease | ||||
| 12.2.1 Epidemic year ‐ vaccine matching | 2 | 518374 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.63, 0.71] |
| 12.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.2.3 Non‐epidemic year ‐ vaccine matching | 1 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.10, 7.97] |
| 12.3 Deaths from influenza or pneumonia Show forest plot | 1 | 259627 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.33, 0.57] |
| Analysis 12.3  Comparison 12: Influenza and pneumococcal vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 3: Deaths from influenza or pneumonia | ||||
| 12.3.1 Epidemic year ‐ vaccine matching | 1 | 259627 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.33, 0.57] |
| 12.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.3.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.4 All deaths Show forest plot | 2 | 260001 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.41, 0.46] |
| Analysis 12.4  Comparison 12: Influenza and pneumococcal vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 4: All deaths | ||||
| 12.4.1 Epidemic year ‐ vaccine matching | 1 | 259627 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.41, 0.46] |
| 12.4.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.4.3 Non‐epidemic year ‐ vaccine matching | 1 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 1.60 [0.08, 30.65] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 13.1 Influenza‐like illness Show forest plot | 2 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.16, 0.56] |
| Analysis 13.1  Comparison 13: Influenza vaccines with adjuvant versus no vaccination: cohort studies in community‐dwellers, Outcome 1: Influenza‐like illness | ||||
| 13.1.1 Epidemic year ‐ vaccine matching | 1 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.07, 0.54] |
| 13.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.18, 0.82] |
| 13.2 Hospitalisation for influenza or pneumonia or respiratory disease Show forest plot | 2 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.02, 1.28] |
| Analysis 13.2  Comparison 13: Influenza vaccines with adjuvant versus no vaccination: cohort studies in community‐dwellers, Outcome 2: Hospitalisation for influenza or pneumonia or respiratory disease | ||||
| 13.2.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.2.3 Non‐epidemic year ‐ vaccine matching | 2 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.02, 1.28] |
| 13.3 All deaths Show forest plot | 1 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 2.10 [0.10, 43.10] |
| Analysis 13.3  Comparison 13: Influenza vaccines with adjuvant versus no vaccination: cohort studies in community‐dwellers, Outcome 3: All deaths | ||||
| 13.3.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.3.3 Non‐epidemic year ‐ vaccine matching | 1 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 2.10 [0.10, 43.10] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 14.1 Hospitalisations for influenza or pneumonia Show forest plot | 2 | 1074 | Odds Ratio (M‐H, Random, 95% CI) | 0.89 [0.69, 1.15] |
| Analysis 14.1  Comparison 14: Influenza vaccines versus no vaccination: case‐control studies in community, Outcome 1: Hospitalisations for influenza or pneumonia | ||||
| 14.1.1 Outbreak ‐ vaccine matching (circulating strains) | 0 | 0 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 14.1.2 Outbreak ‐ vaccine matching absent or unknown | 1 | 825 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.69, 1.22] |
| 14.1.3 No outbreak ‐ vaccine matching | 1 | 249 | Odds Ratio (M‐H, Random, 95% CI) | 0.82 [0.48, 1.40] |
| 14.2 Hospitalisations for any respiratory disease Show forest plot | 4 | 21378 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.95, 1.23] |
| Analysis 14.2  Comparison 14: Influenza vaccines versus no vaccination: case‐control studies in community, Outcome 2: Hospitalisations for any respiratory disease | ||||
| 14.2.1 Outbreak ‐ vaccine matching | 3 | 20582 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.92, 1.26] |
| 14.2.2 No outbreak ‐ not matching | 1 | 796 | Odds Ratio (M‐H, Random, 95% CI) | 1.02 [0.68, 1.52] |
| 14.3 Deaths from influenza or pneumonia Show forest plot | 1 | 1092 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.53, 1.04] |
| Analysis 14.3  Comparison 14: Influenza vaccines versus no vaccination: case‐control studies in community, Outcome 3: Deaths from influenza or pneumonia | ||||
| 14.3.1 Outbreak ‐ vaccine matching | 1 | 1092 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.53, 1.04] |
| 14.4 Pneumonia (no better defined) Show forest plot | 1 | 519 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.57, 1.33] |
| Analysis 14.4  Comparison 14: Influenza vaccines versus no vaccination: case‐control studies in community, Outcome 4: Pneumonia (no better defined) | ||||
| 14.4.1 Outbreak ‐ partially matching | 1 | 519 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.57, 1.33] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 15.1 Hospitalisations for influenza or pneumonia Show forest plot | 5 | Odds Ratio (IV, Random, 95% CI) | 0.59 [0.47, 0.74] | |
| Analysis 15.1  Comparison 15: Influenza vaccines versus no vaccination: case‐control studies in community ‐ adjusted rates, Outcome 1: Hospitalisations for influenza or pneumonia | ||||
| 15.1.1 Epidemic ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.55 [0.36, 0.85] | |
| 15.1.2 Non‐epidemic ‐ vaccine not matching | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 15.1.3 Epidemic year ‐ vaccine matching absent or unknown | 2 | Odds Ratio (IV, Random, 95% CI) | 0.68 [0.58, 0.79] | |
| 15.1.4 Non‐epidemic ‐ vaccine matching | 2 | Odds Ratio (IV, Random, 95% CI) | 0.37 [0.16, 0.87] | |
| 15.2 Hospitalisations for any respiratory disease Show forest plot | 3 | Odds Ratio (IV, Random, 95% CI) | 0.71 [0.56, 0.90] | |
| Analysis 15.2  Comparison 15: Influenza vaccines versus no vaccination: case‐control studies in community ‐ adjusted rates, Outcome 2: Hospitalisations for any respiratory disease | ||||
| 15.2.1 Epidemic ‐ vaccine matching | 3 | Odds Ratio (IV, Random, 95% CI) | 0.71 [0.56, 0.90] | |
| 15.2.2 Non‐epidemic ‐ vaccine matching | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 15.2.3 Non‐epidemic year ‐ vaccine matching | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 15.3 Deaths from pneumonia or influenza Show forest plot | 2 | Odds Ratio (IV, Random, 95% CI) | 0.74 [0.60, 0.92] | |
| Analysis 15.3  Comparison 15: Influenza vaccines versus no vaccination: case‐control studies in community ‐ adjusted rates, Outcome 3: Deaths from pneumonia or influenza | ||||
| 15.3.1 Epidemic year ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.76 [0.60, 0.97] | |
| 15.3.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | Odds Ratio (IV, Random, 95% CI) | 0.67 [0.42, 1.07] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 16.1 Hospitalisations for influenza or pneumonia Show forest plot | 4 | 6629 | Odds Ratio (M‐H, Random, 95% CI) | 0.97 [0.85, 1.09] |
| Analysis 16.1  Comparison 16: Influenza and pneumococcal vaccines versus no vaccination: case‐control studies in community, Outcome 1: Hospitalisations for influenza or pneumonia | ||||
| 16.1.1 Outbreak ‐ vaccine matching | 2 | 3617 | Odds Ratio (M‐H, Random, 95% CI) | 0.95 [0.69, 1.31] |
| 16.1.2 No outbreak ‐ vaccine matching | 2 | 3012 | Odds Ratio (M‐H, Random, 95% CI) | 0.93 [0.80, 1.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 17.1 Hospitalisations for influenza or pneumonia Show forest plot | 2 | Odds Ratio (IV, Random, 95% CI) | 0.68 [0.54, 0.86] | |
| Analysis 17.1  Comparison 17: Influenza and pneumococcal vaccines versus no vaccination: case‐control studies in community ‐ adjusted rates, Outcome 1: Hospitalisations for influenza or pneumonia | ||||
| 17.1.1 Epidemic ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.68 [0.50, 0.93] | |
| 17.1.2 Non‐epidemic ‐ vaccine not matching | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 17.1.3 Epidemic year ‐ vaccine matching absent or unknown | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 17.1.4 Non‐epidemic ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.69 [0.49, 0.97] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 18.1 Influenza‐like illness Show forest plot | 25 | 9211 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.65, 0.87] |
| Analysis 18.1  Comparison 18: Sensitivity analysis: comparison 01: subgroup analysis by study quality, Outcome 1: Influenza‐like illness | ||||
| 18.1.1 Quality A | 8 | 4502 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.65, 0.94] |
| 18.1.2 Quality B | 13 | 3854 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.65, 1.03] |
| 18.1.3 Quality C | 3 | 389 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.43, 1.00] |
| 18.1.4 Quality D | 1 | 466 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.35, 0.57] |

Study flow. We identified no new randomised controlled trials for the 2016 update and stabilisation.
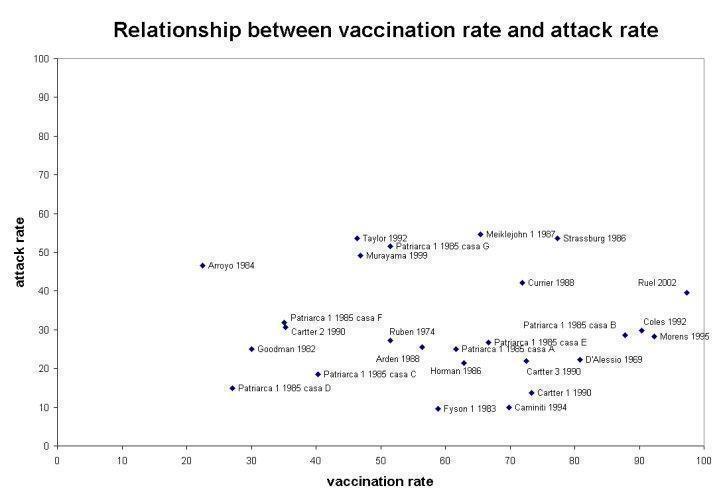
Relationship between vaccination rate and attack rate

Comparison 1: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine, Outcome 1: Influenza

Comparison 1: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine, Outcome 2: Influenza‐like illness

Comparison 1: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine, Outcome 3: Pneumonia

Comparison 1: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine, Outcome 4: All deaths

Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 1: General malaise

Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 2: Nausea

Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 3: Upper respiratory tract symptoms

Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 4: Headache

Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 5: Fever

Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 6: Local tenderness/sore arm

Comparison 2: Influenza vaccines versus placebo: randomised controlled trials ‐ parenteral vaccine ‐ adverse events, Outcome 7: Swelling ‐ erythema ‐ induration

Comparison 3: Influenza vaccines versus placebo: randomised controlled trials ‐ inactivated aerosol vaccine, Outcome 1: Influenza

Comparison 3: Influenza vaccines versus placebo: randomised controlled trials ‐ inactivated aerosol vaccine, Outcome 2: Influenza‐like illness

Comparison 4: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine, Outcome 1: Influenza

Comparison 5: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine ‐ adverse events, Outcome 1: General malaise

Comparison 5: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine ‐ adverse events, Outcome 2: Fever

Comparison 5: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine ‐ adverse events, Outcome 3: Upper respiratory tract symptoms

Comparison 5: Influenza vaccines versus placebo: randomised controlled trials ‐ live aerosol vaccine ‐ adverse events, Outcome 4: Lower respiratory tract symptoms

Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 1: Influenza

Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 2: Influenza‐like illness

Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 3: Pneumonia

Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 4: Hospitalisation for influenza‐like illness or pneumonia

Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 5: Deaths from flu or pneumonia

Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 6: All deaths

Comparison 6: Influenza vaccines versus no vaccination: cohort studies in nursing homes, Outcome 7: Influenza cases (clinically defined without clear definition)

Comparison 7: Influenza and pneumococcal vaccines versus no vaccination: case‐control studies in nursing homes, Outcome 1: Influenza‐like illness

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 1: Influenza

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 2: Influenza‐like illness

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 3: Pneumonia

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 4: Hospitalisation for flu or pneumonia

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 5: Hospitalisation for any respiratory disease

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 6: Deaths from flu or pneumonia

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 7: Deaths from respiratory disease

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 8: All deaths

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 9: Hospitalisation for heart disease

Comparison 8: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 10: Combined outcome: all deaths or severe respiratory illness

Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 1: Hospitalisation for influenza or pneumonia

Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 2: Hospitalisation for any respiratory disease

Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 3: Hospitalisation for heart disease

Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 4: All deaths

Comparison 9: Influenza vaccines versus no vaccination: cohort studies in community ‐ adjusted rates, Outcome 5: Combined outcome: all deaths or severe respiratory illness

Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 1: Influenza

Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 2: Pneumonia

Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 3: Hospitalisation for influenza or pneumonia

Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 4: Hospitalisation for any respiratory disease

Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 5: Deaths from respiratory disease

Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 6: All deaths

Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 7: Hospitalisation for heart disease

Comparison 10: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ risk groups, Outcome 8: Combined outcome: all deaths or severe respiratory illness

Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 1: Influenza

Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 2: Pneumonia

Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 3: Hospitalisation for influenza or pneumonia

Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 4: Hospitalisation for any respiratory disease

Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 5: Deaths from respiratory disease

Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 6: All deaths

Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 7: Hospitalisation for heart disease

Comparison 11: Influenza vaccines versus no vaccination: cohort studies in community‐dwellers ‐ no risk groups, Outcome 8: Combined outcome: all deaths or severe respiratory illness

Comparison 12: Influenza and pneumococcal vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 1: Influenza‐like illness

Comparison 12: Influenza and pneumococcal vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 2: Hospitalisation for influenza or pneumonia or respiratory disease

Comparison 12: Influenza and pneumococcal vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 3: Deaths from influenza or pneumonia

Comparison 12: Influenza and pneumococcal vaccines versus no vaccination: cohort studies in community‐dwellers, Outcome 4: All deaths

Comparison 13: Influenza vaccines with adjuvant versus no vaccination: cohort studies in community‐dwellers, Outcome 1: Influenza‐like illness

Comparison 13: Influenza vaccines with adjuvant versus no vaccination: cohort studies in community‐dwellers, Outcome 2: Hospitalisation for influenza or pneumonia or respiratory disease

Comparison 13: Influenza vaccines with adjuvant versus no vaccination: cohort studies in community‐dwellers, Outcome 3: All deaths

Comparison 14: Influenza vaccines versus no vaccination: case‐control studies in community, Outcome 1: Hospitalisations for influenza or pneumonia

Comparison 14: Influenza vaccines versus no vaccination: case‐control studies in community, Outcome 2: Hospitalisations for any respiratory disease

Comparison 14: Influenza vaccines versus no vaccination: case‐control studies in community, Outcome 3: Deaths from influenza or pneumonia

Comparison 14: Influenza vaccines versus no vaccination: case‐control studies in community, Outcome 4: Pneumonia (no better defined)

Comparison 15: Influenza vaccines versus no vaccination: case‐control studies in community ‐ adjusted rates, Outcome 1: Hospitalisations for influenza or pneumonia

Comparison 15: Influenza vaccines versus no vaccination: case‐control studies in community ‐ adjusted rates, Outcome 2: Hospitalisations for any respiratory disease

Comparison 15: Influenza vaccines versus no vaccination: case‐control studies in community ‐ adjusted rates, Outcome 3: Deaths from pneumonia or influenza

Comparison 16: Influenza and pneumococcal vaccines versus no vaccination: case‐control studies in community, Outcome 1: Hospitalisations for influenza or pneumonia

Comparison 17: Influenza and pneumococcal vaccines versus no vaccination: case‐control studies in community ‐ adjusted rates, Outcome 1: Hospitalisations for influenza or pneumonia

Comparison 18: Sensitivity analysis: comparison 01: subgroup analysis by study quality, Outcome 1: Influenza‐like illness
| Influenza vaccine compared to placebo for preventing influenza in the elderly | ||||||
| Patient or population: people aged over 65 years | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with placebo | Risk with influenza vaccine | |||||
| Influenza assessed with: laboratory confirmation Follow‐up was conducted over an influenza season. | Study population1 | RR 0.42 | 2217 | ⊕⊕⊝⊝ | ||
| 57 per 1000 | 24 per 1000 | |||||
| Influenza‐like illness Follow‐up was conducted over an influenza season. | Study population1 | RR 0.59 | 6894 | ⊕⊕⊕⊝ | ||
| 59 per 1000 | 35 per 1000 | |||||
| Pneumonia Follow‐up was conducted over an influenza season. | No events occurred in 1 study of 699 people. | ‐ | 699 | ⊕⊝⊝⊝ | ||
| Hospitalisations ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| All deaths Follow‐up was conducted over an influenza season. | Study population1 | RR 1.02 | 699 | ⊕⊝⊝⊝ | ||
| 6 per 1000 | 6 per 1000 | |||||
| Fever Follow‐up was conducted over an influenza season. | Study population1 | RR 1.57 | 2519 | ⊕⊕⊕⊝ | ||
| 16 per 1000 | 25 per 1000 | |||||
| Nausea Follow‐up was conducted over an influenza season. | Study population1 | RR 1.75 | 672 | ⊕⊕⊝⊝ | ||
| 24 per 1000 | 42 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Control group risk taken as aggregate of the study control group risks. | ||||||
| Review version (searches date) | Number of included trials (RCTs/CCTs) | Number of included observational studies | Estimates of effect (RCTs/CCTs only) | Conclusions (1 to 2 lines from abstract) |
|---|---|---|---|---|
| Version 1 (24 May 2006) | 9 | 621 | Influenza‐like illness LAIV = no data TIV = 41% (95% CI 27% to 53%) IAV = n.s. Influenza LAIV = n.s. TIV = 58% (95% CI 34% to 73%) IAV = n.s. | In long‐term care facilities, where vaccination is most effective against complications, the aims of the vaccination campaign are fulfilled, at least in part. However, according to reliable evidence the usefulness of vaccines in the community is modest. The apparent high effectiveness of the vaccines in preventing death from all causes may reflect a baseline imbalance in health status and other systematic differences in the 2 groups of participants. |
| Version 2 (20 January 2010) | 9 | 662 | Influenza‐like illness LAIV = no data TIV = 41% (95% CI 27% to 53%) IAV = n.s. Influenza LAIV = n.s. TIV = 58% (95% CI 34% to 73%) IAV = n.s. | The available evidence is of poor quality and provides no guidance regarding the safety, efficacy, or effectiveness of influenza vaccines for people aged 65 years or older. To resolve the uncertainty, an adequately powered publicly‐funded randomised, placebo‐controlled trial run over several seasons should be undertaken. |
| 1These include 49 cohort studies for efficacy/effectiveness (79 data sets); 10 case‐control studies for efficacy/effectiveness (12 data sets); 3 studies (cohorts) for Guillain‐Barré syndrome. Key: CCT = controlled clinical trial; CI = confidence interval; IAV = inactivated aerosol vaccines; LAIV = live attenuated vaccines; n.s. = not significant; RCT = randomised controlled trial; TIV = trivalent inactivated vaccines | ||||
| Study | Influenza season | Vaccine | Population | Age | RR (95% CI) |
|---|---|---|---|---|---|
| 1976 to 1977 | A/New Jersey/76 or A/New Jersey/76 and A/Victoria/75 swine vaccine | All the USA population | > 64 years | 5.2 (3.9 to 7.0) | |
| 1979 to 1980 | Inactivated trivalent | All the USA population | > 18 years | 0.6 (0.45 to 1.32) | |
| 1980 to 1981 | Inactivated trivalent | All the USA population | > 18 years | 1.4 (0.80 to 1.76) | |
| 1992 to 1994 | Inactivated trivalent | 21 million | > 64 years | 1.5 (0.7 to 3.3) | |
| Key: CI = confidence interval; RR = risk ratio | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Influenza Show forest plot | 3 | 2217 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.27, 0.66] |
| 1.1.1 Outbreak ‐ vaccine matching ‐ community ‐ healthy and ill | 1 | 1838 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.23, 0.74] |
| 1.1.2 Outbreak ‐ vaccine matching ‐ psychiatric hospital | 1 | 177 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.12, 1.06] |
| 1.1.3 No outbreak ‐ vaccine matching ‐ nursing home ‐ healthy and ill | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.20, 1.25] |
| 1.2 Influenza‐like illness Show forest plot | 4 | 6894 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.47, 0.73] |
| 1.2.1 Outbreak ‐ vaccine matching (circulating strains) ‐ community ‐ healthy | 2 | 2047 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.42, 0.79] |
| 1.2.2 Outbreak ‐ vaccine matching ‐ community ‐ risk groups | 1 | 490 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.49, 1.53] |
| 1.2.3 Outbreak ‐ vaccine matching ‐ nursing home ‐ healthy | 1 | 4180 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.37, 0.80] |
| 1.2.4 Outbreak ‐ vaccine matching ‐ psychiatric hospital | 1 | 177 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.13, 0.92] |
| 1.3 Pneumonia Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.3.1 Outbreak ‐ vaccine matching ‐ community ‐ healthy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.4 All deaths Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.4.1 Outbreak ‐ vaccine matching ‐ community ‐ healthy | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 General malaise Show forest plot | 4 | 2560 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.87, 1.61] |
| 2.2 Nausea Show forest plot | 1 | 672 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.74, 4.12] |
| 2.3 Upper respiratory tract symptoms Show forest plot | 2 | 713 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.90, 2.01] |
| 2.4 Headache Show forest plot | 3 | 2519 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.76, 1.58] |
| 2.5 Fever Show forest plot | 3 | 2519 | Risk Ratio (M‐H, Random, 95% CI) | 1.57 [0.92, 2.71] |
| 2.6 Local tenderness/sore arm Show forest plot | 4 | 2560 | Risk Ratio (M‐H, Random, 95% CI) | 3.56 [2.61, 4.87] |
| 2.7 Swelling ‐ erythema ‐ induration Show forest plot | 2 | 1847 | Risk Ratio (M‐H, Random, 95% CI) | 8.23 [3.98, 17.05] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Influenza Show forest plot | 1 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.40, 1.99] |
| 3.1.1 Outbreak ‐ vaccine matching ‐ psychiatric hospital | 1 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.40, 1.99] |
| 3.2 Influenza‐like illness Show forest plot | 1 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.41, 1.71] |
| 3.2.1 Outbreak ‐ vaccine matching ‐ psychiatric hospital | 1 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.41, 1.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Influenza Show forest plot | 1 | 220 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.21, 1.17] |
| 4.1.1 No outbreak ‐ vaccine matching ‐ nursing home ‐ healthy and ill | 1 | 220 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.21, 1.17] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 General malaise Show forest plot | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 3.09 [0.18, 53.20] |
| 5.2 Fever Show forest plot | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 1.71 [0.09, 33.24] |
| 5.3 Upper respiratory tract symptoms Show forest plot | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 1.62 [0.42, 6.29] |
| 5.4 Lower respiratory tract symptoms Show forest plot | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 2.91 [0.41, 20.48] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 Influenza Show forest plot | 8 | 1941 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.32, 1.29] |
| 6.1.1 Outbreak ‐ vaccine matching | 4 | 658 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.43, 2.51] |
| 6.1.2 Outbreak ‐ vaccine matching absent or unknown | 2 | 592 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.22, 1.04] |
| 6.1.3 No outbreak ‐ vaccine matching | 2 | 691 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.05, 1.03] |
| 6.1.4 No outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.2 Influenza‐like illness Show forest plot | 26 | 12388 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.66, 0.88] |
| 6.2.1 Outbreak ‐ vaccine matching (circulating strains) | 16 | 5963 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.64, 0.94] |
| 6.2.2 Outbreak ‐ vaccine matching absent or unknown | 6 | 4096 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.60, 1.05] |
| 6.2.3 No outbreak ‐ vaccine matching | 4 | 2329 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.46, 0.98] |
| 6.2.4 No outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.3 Pneumonia Show forest plot | 17 | 10274 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.43, 0.66] |
| 6.3.1 Outbreak ‐ vaccine matching | 8 | 4482 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.42, 0.70] |
| 6.3.2 Outbreak ‐ vaccine matching absent or unknown | 5 | 3991 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.39, 1.21] |
| 6.3.3 No outbreak ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.3.4 No outbreak ‐ matching absent or unknown | 4 | 1801 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.18, 0.68] |
| 6.4 Hospitalisation for influenza‐like illness or pneumonia Show forest plot | 12 | 28032 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.32, 0.81] |
| 6.4.1 Outbreak ‐ vaccine matching | 8 | 2027 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.36, 0.84] |
| 6.4.2 Outbreak ‐ vaccine matching absent or unknown | 2 | 3301 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.43, 1.58] |
| 6.4.3 No outbreak ‐ vaccine matching | 2 | 22704 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.14, 0.76] |
| 6.4.4 No outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.5 Deaths from flu or pneumonia Show forest plot | 27 | 32179 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.33, 0.63] |
| 6.5.1 Outbreak ‐ vaccine matching | 16 | 6127 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.41, 0.83] |
| 6.5.2 Outbreak ‐ vaccine matching absent or unknown | 4 | 1089 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.11, 1.02] |
| 6.5.3 No outbreak ‐ vaccine matching | 3 | 23162 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.09, 0.87] |
| 6.5.4 No outbreak ‐ vaccine matching absent or unknown | 4 | 1801 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.14, 0.67] |
| 6.6 All deaths Show forest plot | 1 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.21, 0.77] |
| 6.6.1 Outbreak ‐ vaccine matching | 1 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.21, 0.77] |
| 6.6.2 Outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.6.3 No outbreak ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.6.4 No outbreak ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 6.7 Influenza cases (clinically defined without clear definition) Show forest plot | 7 | 24238 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.27, 1.02] |
| 6.7.1 Outbreak ‐ vaccine matching | 2 | 271 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.11, 4.56] |
| 6.7.2 Outbreak ‐ vaccine matching absent or unknown | 1 | 155 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.09, 0.59] |
| 6.7.3 No outbreak ‐ vaccine matching | 1 | 22462 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.35, 0.46] |
| 6.7.4 No outbreak ‐ vaccine matching absent or unknown | 3 | 1350 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.41, 1.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Influenza‐like illness Show forest plot | 1 | 1198 | Odds Ratio (M‐H, Random, 95% CI) | 0.52 [0.40, 0.68] |
| 7.1.1 Outbreak ‐ vaccine matching | 1 | 1198 | Odds Ratio (M‐H, Random, 95% CI) | 0.52 [0.40, 0.68] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 8.1 Influenza Show forest plot | 2 | 18249 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.02, 2.01] |
| 8.1.1 Epidemic year ‐ vaccine matching | 1 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 0.05 [0.01, 0.37] |
| 8.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 17822 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.27, 0.91] |
| 8.1.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.2 Influenza‐like illness Show forest plot | 4 | 9613 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.42, 1.33] |
| 8.2.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.2.3 Non‐epidemic year ‐ vaccine matching | 2 | 4636 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.58, 2.03] |
| 8.2.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 268 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.16, 4.55] |
| 8.2.5 Epidemic year ‐ vaccine not matching | 1 | 4709 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.24, 0.81] |
| 8.3 Pneumonia Show forest plot | 2 | 18090 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.64, 1.20] |
| 8.3.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.3.3 Non‐epidemic year ‐ vaccine matching | 1 | 17822 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.63, 1.19] |
| 8.3.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 268 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.16, 57.42] |
| 8.4 Hospitalisation for flu or pneumonia Show forest plot | 9 | 784643 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.62, 0.85] |
| 8.4.1 Epidemic year ‐ vaccine matching | 6 | 727776 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.62, 0.88] |
| 8.4.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.4.3 Non‐epidemic year ‐ vaccine matching | 1 | 25532 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.37, 0.83] |
| 8.4.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 26626 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.54, 0.99] |
| 8.4.5 Epidemic year ‐ vaccine not matching | 1 | 4709 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.33, 2.40] |
| 8.5 Hospitalisation for any respiratory disease Show forest plot | 5 | 567299 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.54, 1.43] |
| 8.5.1 Epidemic year ‐ vaccine matching | 3 | 515141 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.37, 1.64] |
| 8.5.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.5.3 Non‐epidemic year ‐ vaccine matching | 1 | 25532 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.79, 1.12] |
| 8.5.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 26626 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [1.01, 1.34] |
| 8.6 Deaths from flu or pneumonia Show forest plot | 1 | 163391 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.70, 1.09] |
| 8.6.1 Epidemic year ‐ vaccine matching | 1 | 163391 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.70, 1.09] |
| 8.6.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.6.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.6.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.7 Deaths from respiratory disease Show forest plot | 1 | 426668 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.25, 1.39] |
| 8.7.1 Epidemic year ‐ vaccine matching | 1 | 426668 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.25, 1.39] |
| 8.8 All deaths Show forest plot | 8 | 409468 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.47, 0.80] |
| 8.8.1 Epidemic year ‐ vaccine matching | 4 | 300332 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.50, 0.70] |
| 8.8.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.8.3 Non‐epidemic year ‐ vaccine matching | 3 | 104427 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.30, 1.39] |
| 8.8.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.8.5 Epidemic year ‐ vaccine not matching | 1 | 4709 | Risk Ratio (M‐H, Random, 95% CI) | 3.89 [0.90, 16.89] |
| 8.9 Hospitalisation for heart disease Show forest plot | 6 | 433934 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.67, 1.12] |
| 8.9.1 Epidemic year ‐ vaccine matching | 4 | 381776 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.56, 0.97] |
| 8.9.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.9.3 Non‐epidemic year ‐ vaccine matching | 1 | 25532 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.81, 1.38] |
| 8.9.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 1 | 26626 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.07, 2.36] |
| 8.10 Combined outcome: all deaths or severe respiratory illness Show forest plot | 3 | 290819 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.58, 0.85] |
| 8.10.1 Epidemic year ‐ vaccine matching | 2 | 132365 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.42, 1.55] |
| 8.10.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | 158454 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.69, 0.80] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 9.1 Hospitalisation for influenza or pneumonia Show forest plot | 8 | Odds Ratio (IV, Random, 95% CI) | 0.73 [0.67, 0.79] | |
| 9.1.1 Epidemic ‐ vaccine matching | 6 | Odds Ratio (IV, Random, 95% CI) | 0.71 [0.65, 0.77] | |
| 9.1.2 Non‐epidemic ‐ vaccine not matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.90 [0.58, 1.38] | |
| 9.1.3 Epidemic year ‐ vaccine matching absent or unknown | 1 | Odds Ratio (IV, Random, 95% CI) | 0.82 [0.68, 0.98] | |
| 9.2 Hospitalisation for any respiratory disease Show forest plot | 13 | Odds Ratio (IV, Random, 95% CI) | 0.78 [0.72, 0.85] | |
| 9.2.1 Epidemic ‐ vaccine matching | 9 | Odds Ratio (IV, Random, 95% CI) | 0.71 [0.67, 0.74] | |
| 9.2.2 Non‐epidemic ‐ vaccine not matching | 2 | Odds Ratio (IV, Random, 95% CI) | 0.91 [0.76, 1.08] | |
| 9.2.3 Non‐epidemic year ‐ vaccine matching | 2 | Odds Ratio (IV, Random, 95% CI) | 0.94 [0.84, 1.06] | |
| 9.3 Hospitalisation for heart disease Show forest plot | 6 | Odds Ratio (IV, Random, 95% CI) | 0.76 [0.70, 0.82] | |
| 9.3.1 Epidemic year ‐ vaccine matching | 5 | Odds Ratio (IV, Random, 95% CI) | 0.75 [0.70, 0.82] | |
| 9.3.2 Non‐epidemic ‐ vaccine not matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.80 [0.55, 1.16] | |
| 9.4 All deaths Show forest plot | 7 | Odds Ratio (IV, Random, 95% CI) | 0.53 [0.46, 0.61] | |
| 9.4.1 Epidemic year ‐ vaccine matching | 5 | Odds Ratio (IV, Random, 95% CI) | 0.47 [0.42, 0.53] | |
| 9.4.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | Odds Ratio (IV, Random, 95% CI) | 0.65 [0.57, 0.75] | |
| 9.4.3 Non‐epidemic year ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.76 [0.60, 0.97] | |
| 9.5 Combined outcome: all deaths or severe respiratory illness Show forest plot | 1 | Odds Ratio (IV, Random, 95% CI) | 0.70 [0.37, 1.34] | |
| 9.5.1 Epidemic year ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.70 [0.37, 1.34] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 10.1 Influenza Show forest plot | 1 | 6423 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.14, 1.17] |
| 10.1.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 6423 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.14, 1.17] |
| 10.1.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.2 Pneumonia Show forest plot | 1 | 6423 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.76, 1.94] |
| 10.2.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.2.3 Non‐epidemic year ‐ vaccine matching | 1 | 6423 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.76, 1.94] |
| 10.2.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.3 Hospitalisation for influenza or pneumonia Show forest plot | 1 | 45932 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.63, 0.86] |
| 10.3.1 Epidemic year ‐ vaccine matching | 1 | 45932 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.63, 0.86] |
| 10.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.3.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.3.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.4 Hospitalisation for any respiratory disease Show forest plot | 2 | 189004 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.80, 0.92] |
| 10.4.1 Epidemic year ‐ vaccine matching | 2 | 189004 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.80, 0.92] |
| 10.4.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.4.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.4.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.5 Deaths from respiratory disease Show forest plot | 1 | 142464 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.86, 0.98] |
| 10.5.1 Epidemic year ‐ vaccine matching | 1 | 142464 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.86, 0.98] |
| 10.6 All deaths Show forest plot | 3 | 68032 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.16, 0.97] |
| 10.6.1 Epidemic year ‐ vaccine matching | 1 | 2344 | Risk Ratio (M‐H, Random, 95% CI) | 0.13 [0.02, 0.92] |
| 10.6.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.6.3 Non‐epidemic year ‐ vaccine matching | 2 | 65688 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.17, 1.28] |
| 10.6.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.7 Hospitalisation for heart disease Show forest plot | 1 | 45932 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.83, 1.03] |
| 10.7.1 Epidemic year ‐ vaccine matching | 1 | 45932 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.83, 1.03] |
| 10.7.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.7.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.7.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 10.8 Combined outcome: all deaths or severe respiratory illness Show forest plot | 2 | 146248 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.49, 0.74] |
| 10.8.1 Epidemic year ‐ vaccine matching | 1 | 54438 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.49, 0.60] |
| 10.8.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | 91810 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.61, 0.72] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 11.1 Influenza Show forest plot | 1 | 11399 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.27, 1.17] |
| 11.1.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 11399 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.27, 1.17] |
| 11.1.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.2 Pneumonia Show forest plot | 1 | 11399 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.37, 0.92] |
| 11.2.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.2.3 Non‐epidemic year ‐ vaccine matching | 1 | 11399 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.37, 0.92] |
| 11.2.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.3 Hospitalisation for influenza or pneumonia Show forest plot | 1 | 101619 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.40, 0.63] |
| 11.3.1 Epidemic year ‐ vaccine matching | 1 | 101619 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.40, 0.63] |
| 11.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.3.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.3.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.4 Hospitalisation for any respiratory disease Show forest plot | 2 | 376324 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.55, 1.27] |
| 11.4.1 Epidemic year ‐ vaccine matching | 2 | 376324 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.55, 1.27] |
| 11.4.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.4.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.4.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.5 Deaths from respiratory disease Show forest plot | 1 | 281424 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [1.31, 1.53] |
| 11.5.1 Epidemic year ‐ vaccine matching | 1 | 281424 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [1.31, 1.53] |
| 11.6 All deaths Show forest plot | 3 | 43821 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.33, 1.29] |
| 11.6.1 Epidemic year ‐ vaccine matching | 1 | 7047 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.26, 4.49] |
| 11.6.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.6.3 Non‐epidemic year ‐ vaccine matching | 2 | 36774 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.27, 1.30] |
| 11.6.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.7 Hospitalisation for heart disease Show forest plot | 1 | 101619 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.61, 1.01] |
| 11.7.1 Epidemic year ‐ vaccine matching | 1 | 101619 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.61, 1.01] |
| 11.7.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.7.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.7.4 Non‐epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 11.8 Combined outcome: all deaths or severe respiratory illness Show forest plot | 2 | 135180 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.54, 0.70] |
| 11.8.1 Epidemic year ‐ vaccine matching | 1 | 68536 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.54, 0.78] |
| 11.8.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | 66644 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.48, 0.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 12.1 Influenza‐like illness Show forest plot | 1 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.16, 0.64] |
| 12.1.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.16, 0.64] |
| 12.2 Hospitalisation for influenza or pneumonia or respiratory disease Show forest plot | 3 | 518748 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.64, 0.70] |
| 12.2.1 Epidemic year ‐ vaccine matching | 2 | 518374 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.63, 0.71] |
| 12.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.2.3 Non‐epidemic year ‐ vaccine matching | 1 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.10, 7.97] |
| 12.3 Deaths from influenza or pneumonia Show forest plot | 1 | 259627 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.33, 0.57] |
| 12.3.1 Epidemic year ‐ vaccine matching | 1 | 259627 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.33, 0.57] |
| 12.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.3.3 Non‐epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.4 All deaths Show forest plot | 2 | 260001 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.41, 0.46] |
| 12.4.1 Epidemic year ‐ vaccine matching | 1 | 259627 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.41, 0.46] |
| 12.4.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 12.4.3 Non‐epidemic year ‐ vaccine matching | 1 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 1.60 [0.08, 30.65] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 13.1 Influenza‐like illness Show forest plot | 2 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.16, 0.56] |
| 13.1.1 Epidemic year ‐ vaccine matching | 1 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.07, 0.54] |
| 13.1.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.1.3 Non‐epidemic year ‐ vaccine matching | 1 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.18, 0.82] |
| 13.2 Hospitalisation for influenza or pneumonia or respiratory disease Show forest plot | 2 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.02, 1.28] |
| 13.2.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.2.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.2.3 Non‐epidemic year ‐ vaccine matching | 2 | 498 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.02, 1.28] |
| 13.3 All deaths Show forest plot | 1 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 2.10 [0.10, 43.10] |
| 13.3.1 Epidemic year ‐ vaccine matching | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.3.2 Epidemic year ‐ vaccine matching absent or unknown | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 13.3.3 Non‐epidemic year ‐ vaccine matching | 1 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 2.10 [0.10, 43.10] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 14.1 Hospitalisations for influenza or pneumonia Show forest plot | 2 | 1074 | Odds Ratio (M‐H, Random, 95% CI) | 0.89 [0.69, 1.15] |
| 14.1.1 Outbreak ‐ vaccine matching (circulating strains) | 0 | 0 | Odds Ratio (M‐H, Random, 95% CI) | Not estimable |
| 14.1.2 Outbreak ‐ vaccine matching absent or unknown | 1 | 825 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.69, 1.22] |
| 14.1.3 No outbreak ‐ vaccine matching | 1 | 249 | Odds Ratio (M‐H, Random, 95% CI) | 0.82 [0.48, 1.40] |
| 14.2 Hospitalisations for any respiratory disease Show forest plot | 4 | 21378 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.95, 1.23] |
| 14.2.1 Outbreak ‐ vaccine matching | 3 | 20582 | Odds Ratio (M‐H, Random, 95% CI) | 1.08 [0.92, 1.26] |
| 14.2.2 No outbreak ‐ not matching | 1 | 796 | Odds Ratio (M‐H, Random, 95% CI) | 1.02 [0.68, 1.52] |
| 14.3 Deaths from influenza or pneumonia Show forest plot | 1 | 1092 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.53, 1.04] |
| 14.3.1 Outbreak ‐ vaccine matching | 1 | 1092 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.53, 1.04] |
| 14.4 Pneumonia (no better defined) Show forest plot | 1 | 519 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.57, 1.33] |
| 14.4.1 Outbreak ‐ partially matching | 1 | 519 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.57, 1.33] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 15.1 Hospitalisations for influenza or pneumonia Show forest plot | 5 | Odds Ratio (IV, Random, 95% CI) | 0.59 [0.47, 0.74] | |
| 15.1.1 Epidemic ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.55 [0.36, 0.85] | |
| 15.1.2 Non‐epidemic ‐ vaccine not matching | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 15.1.3 Epidemic year ‐ vaccine matching absent or unknown | 2 | Odds Ratio (IV, Random, 95% CI) | 0.68 [0.58, 0.79] | |
| 15.1.4 Non‐epidemic ‐ vaccine matching | 2 | Odds Ratio (IV, Random, 95% CI) | 0.37 [0.16, 0.87] | |
| 15.2 Hospitalisations for any respiratory disease Show forest plot | 3 | Odds Ratio (IV, Random, 95% CI) | 0.71 [0.56, 0.90] | |
| 15.2.1 Epidemic ‐ vaccine matching | 3 | Odds Ratio (IV, Random, 95% CI) | 0.71 [0.56, 0.90] | |
| 15.2.2 Non‐epidemic ‐ vaccine matching | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 15.2.3 Non‐epidemic year ‐ vaccine matching | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 15.3 Deaths from pneumonia or influenza Show forest plot | 2 | Odds Ratio (IV, Random, 95% CI) | 0.74 [0.60, 0.92] | |
| 15.3.1 Epidemic year ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.76 [0.60, 0.97] | |
| 15.3.2 Epidemic year ‐ vaccine matching absent or unknown | 1 | Odds Ratio (IV, Random, 95% CI) | 0.67 [0.42, 1.07] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 16.1 Hospitalisations for influenza or pneumonia Show forest plot | 4 | 6629 | Odds Ratio (M‐H, Random, 95% CI) | 0.97 [0.85, 1.09] |
| 16.1.1 Outbreak ‐ vaccine matching | 2 | 3617 | Odds Ratio (M‐H, Random, 95% CI) | 0.95 [0.69, 1.31] |
| 16.1.2 No outbreak ‐ vaccine matching | 2 | 3012 | Odds Ratio (M‐H, Random, 95% CI) | 0.93 [0.80, 1.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 17.1 Hospitalisations for influenza or pneumonia Show forest plot | 2 | Odds Ratio (IV, Random, 95% CI) | 0.68 [0.54, 0.86] | |
| 17.1.1 Epidemic ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.68 [0.50, 0.93] | |
| 17.1.2 Non‐epidemic ‐ vaccine not matching | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 17.1.3 Epidemic year ‐ vaccine matching absent or unknown | 0 | Odds Ratio (IV, Random, 95% CI) | Not estimable | |
| 17.1.4 Non‐epidemic ‐ vaccine matching | 1 | Odds Ratio (IV, Random, 95% CI) | 0.69 [0.49, 0.97] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 18.1 Influenza‐like illness Show forest plot | 25 | 9211 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.65, 0.87] |
| 18.1.1 Quality A | 8 | 4502 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.65, 0.94] |
| 18.1.2 Quality B | 13 | 3854 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.65, 1.03] |
| 18.1.3 Quality C | 3 | 389 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.43, 1.00] |
| 18.1.4 Quality D | 1 | 466 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.35, 0.57] |

