Akupunktur bei Nackenschmerzen
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT | |
| Participants | Myofascial neck pain lasting ≥ 6 months Participant recruitment: hospital‐based pain management centre, neurology clinic, public announcement | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT 1 COMPARISON TREATMENT 2 CO‐INTERVENTION Avoided Treatment schedule: 14 sessions over 12 weeks, with each session averaging 30 minutes in duration | |
| Outcomes | PAIN INTENSITY (VAS 0 to 10 scale) Reasons for drop‐out: 2 moved, 6 not specified, 2 lost to contact | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Low risk | Adequately described |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Participant blinded as outcome assessor of self reports |
| Incomplete outcome data (attrition bias) | Low risk | Described and acceptable |
| Incomplete outcome data (attrition bias) | High risk | Did not analyse; all randomised |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Each participant attended 14 sessions, twice weekly |
| Similar timing of outcome assessment? | Low risk | All assessed at 12 weeks |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Subacute and chronic WAD Participant recruitment: newspaper advertisement University Clinic, Sydney, Australia | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION Comparable between groups; included medication, physiotherapy and chiropractic therapy Treatment schedule: 2 sessions/wk over 6 weeks, with each session averaging 30 minutes in duration | |
| Outcomes | PAIN INTENSITY (VAS 10 cm scale) SMD ‐0.38 (95% CI random ‐0.73 to ‐0.02) at 3 months SMD ‐0.59 (95% CI random ‐0.95 to ‐0.23) at 6 months FUNCTION (NDI 50 point scale) Baseline mean: real EAP 15.6, simulated 18.7 End of study mean: real EAP 14.5, simulated 16.8 Absolute benefit: real EAP 1.1, simulated 1.9 Reported results: not significant SMD ‐0.22 (95% CI random ‐0.57 to 0.13) at 3 months SMD ‐0.31 (95% CI random ‐0.66 to 0.05) at 6 months Quality of life (SF‐36, Physical Component) Baseline mean: real EAP 43.6, simulated 41.3 End of study mean: real EAP 41.9, simulated 38.3 Absolute benefit: real EAP 1.7, simulated 3.0 Reported results: not significant Reasons for drop‐out: 8 in control group, no reasons given | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generated by random numbers table |
| Allocation concealment (selection bias) | Low risk | Numbered opaque envelopes |
| Blinding (performance bias and detection bias) | Low risk | Adequately blinded |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Adequately blinded participant as outcome assessor of self reports |
| Incomplete outcome data (attrition bias) | Low risk | Described and adequate |
| Incomplete outcome data (attrition bias) | High risk | Not all in control group analysed (52/60) |
| Selective reporting (reporting bias) | Low risk | Protocol provided by study author (grey literature) |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Reported as no evidence of imbalance but no results provided |
| Compliance acceptable? | Low risk | Reported and acceptable |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 and 6 months |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Chronic myofascial neck pain Participant recruitment: pain control clinic, Taiwan | |
| Interventions | INDEX TREATMENT Remote acupuncture group (RA) COMPARISON TREATMENT Sham acupuncture CO‐INTERVENTION Avoided Treatment schedule: 1 session | |
| Outcomes | PAIN INTENSITY (0 to 10 VAS scale) Drop‐outs: none | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence was generated from a computerised randomisation programme |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Low risk | Described in the report |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Described in the report |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Low risk | Avoided by design (pre/post) |
| Compliance acceptable? | Low risk | Acceptable by design (pre/post) |
| Similar timing of outcome assessment? | Low risk | Immediate post |
| Fatal Flaw | High risk | Main problem involves reporting errors and statistical analyses. No estimate of differences between groups, only percent changes between groups; only evidence of improvement in abstract results was noted within groups, not between groups; Table 1 P values are incorrect for pain duration and initial pain; no P values should be provided for % change data |
| Methods | RCT | |
| Participants | Chronic mechanical neck disorder with radicular symptoms or signs | |
| Interventions | INDEX TREATMENT Acupuncture (treatment group) Wait‐list (control group) Comparable between index and control groups for medication use only | |
| Outcomes | PAIN (VAS scale 0 to 10) End of study mean: acupuncture 3.6, control 5.4 SMD ‐0.74 (95% random CI ‐1.49 to 0.00) at 8 weeks | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Equally sized and folded papers in a box, half marked A, the other half B |
| Allocation concealment (selection bias) | High risk | Papers not concealed |
| Blinding (performance bias and detection bias) | High risk | Not blinded |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | High risk | Only medications reported, no other interventions mentioned |
| Compliance acceptable? | High risk | Not reported |
| Similar timing of outcome assessment? | Low risk | 8 weeks after treatment |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Chronic cervical spondylosis Participant recruitment: Acupuncture Department of Guangdong Provincial Traditional Chinese Medicine Hospital, China | |
| Interventions | INDEX TREATMENT Acupuncture group COMPARISON TREATMENT Sham Superficial insertion 1 cm apart laterally from acupuncture points. Remained for 20 minutes, no manipulation; infrared radiation CO‐INTERVENTION NR Treatment schedule: once every other day for 9 sessions over 18 days | |
| Outcomes | PAIN INTENSITY (0 to 10 VAS scale) SMD ‐0.53 (95% CI random ‐0.91 to ‐0.16) immediate post treatment SMD ‐0.59 (95% CI random ‐0.97 to ‐0.21) at 4 weeks SMD ‐0.23 (95% CI random ‐0.61 to 0.14) at 3 months Northwick Park Pain Questionnaire (NPQ) (0 to 100) Baseline mean: acupuncture 33.63, sham 33.21 Reported results: significant immediate post treatment favouring acupuncture but not over long term SMD ‐0.50 (95% CI random ‐0.88 to ‐0.12) at 4 weeks SMD ‐0.40 (95% CI random ‐0.78 to ‐0.03) at 3 months | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised sequence number and grouping address on a randomising card |
| Allocation concealment (selection bias) | Low risk | Use of sealed opaque envelopes |
| Blinding (performance bias and detection bias) | Low risk | Described adequately in the report |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Participant as outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | Described and acceptable 4.27% |
| Incomplete outcome data (attrition bias) | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Post, 4 weeks, 12 weeks |
| Fatal Flaw | High risk | No sample size justifications; multiple comparisons should have been done; analysis should have been stratified by syndrome type; time lines between points on graph are distorted |
| Methods | RCT | |
| Participants | Chronic neck pain Participant recruitment: selected from 5 large companies in Oslo by the company's occupational physician, Norway | |
| Interventions | INDEX TREATMENT Acupuncture COMPARISON TREATMENT Placebo 10 to 14 mm distal to real points or 4 to 6 mm for ear points; electrostimulation set up but no voltage CO‐INTERVENTION Reported, see 'Risk of bias' Treatment schedule: 3 times per week, over 3 to 4 weeks, for a total of 10 treatments, with each session averaging 45 minutes in duration | |
| Outcomes | PAIN INTENSITY (0 to 100 VAS scale) SMD ‐3.17 (95% CI random ‐4.44 to ‐1.90) immediate post treatment SMD ‐1.54 (95% CI random ‐2.47 to ‐0.61) at 6 months SMD ‐2.72 (95% CI random ‐3.89 to ‐1.56) at 3 years Drop‐outs: none | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by draw with replacement |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Low risk | Described in report |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Described in report |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Low risk | All participants randomised were analysed, described in report |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | High risk | Not similar with respect to PPT and duration of symptoms; also headache baseline information not provided |
| Co‐interventions avoided or similar? | High risk | 21% of the intervention group and 50% of the control group received other treatment |
| Compliance acceptable? | Low risk | All participants completed all 10 treatments |
| Similar timing of outcome assessment? | Low risk | All assessed immediate post, 6 months, 3 years |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Chronic neck pain Participant recruitment: selected from 5 large companies in Oslo by the company's occupational physician, Norway | |
| Interventions | INDEX TREATMENT Acupuncture COMPARISON TREATMENT Placebo 10 to 14 mm distal to real points or 4 to 6 mm for ear points; electrostimulation but no voltage CO‐INTERVENTION Reported, see 'Risk of bias' Treatment schedule: 3 times/wk over 3 to 4 weeks for a total of 10 treatments, with each session averaging 45 minutes in duration | |
| Outcomes | PAIN INTENSITY (0 to 100 VAS scale) SMD ‐3.17 (95% CI random ‐4.44 to ‐1.90) immediate post treatment SMD ‐1.75 (95% CI random ‐3.01 to ‐0.49) at 6 months SMD ‐3.33 (95% CI random ‐4.78 to ‐1.88) at 3 years Drop‐outs: none | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported adequately |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Low risk | Reported to be similar |
| Compliance acceptable? | Low risk | Each participant received 3 treatments/wk to a total of 10 |
| Similar timing of outcome assessment? | Low risk | All assessed at 6 months and 3 years |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Number analysed/randomised: 60/60 Intention‐to‐treat: NR | |
| Participants | Chronic myofascial pain syndrome | |
| Interventions | INDEX TREATMENT Dry needling (dn) upper trapezius COMPARISON TREATMENT Placebo laser CO‐INTERVENTION Paracetamol as needed Treatment schedule: dn once/wk over 4 weeks, placebo laser 3 sessions/wk over 4 weeks Duration of follow‐up: immediate post treatment and 6 months | |
| Outcomes | PAIN INTENSITY (VAS activity 10 cm scale) Baseline mean: dn 7.62, placebo 7.65 End of study mean: dn 4.24, placebo 4.22 Absolute benefit: dn 3.38, placebo 3.43 Reported results: significant differences favouring laser compared with dn and placebo post treatment only SMD ‐0.02 (95% CI random ‐0.64 to 0.60) immediate post treatment SMD 0.01 (95% CI random ‐0.61 to 0.63 at 6 months FUNCTION: Nottingham Health Profile Physical Activity Component (0 to 100) Baseline mean: dn 32.80, placebo 25.59 End of study mean: dn 13.68, placebo 16.08 Absolute benefit: dn 19.12, placebo 9.51 Reported results: significant differences favouring laser compared with dn and placebo SMD 0.22 (95% CI random ‐0.40 to 0.84) immediate post treatment SMD ‐0.14 (95% CI random ‐0.76 to 0.48) at 6 months Adverse effects: NR | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) | High risk | Not described, no n's in tables |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Followed medication use only |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | All assessed immediately post treatment and at 6 months |
| Fatal Flaw | High risk | Unclear randomisation, allocation concealment; drops‐outs not described; unclear whether ITT done |
| Methods | RCT | |
| Participants | Chronic mechanical neck disorder Participant recruitment: outpatient departments at the University of Munich | |
| Interventions | INDEX TREATMENT Acupuncture COMPARISON TREATMENT Sham laser acupuncture (control) CO‐INTERVENTION Not reported Treatment schedule: 5 sessions over 3 weeks, each session 30 minutes in duration | |
| Outcomes | PAIN INTENSITY (VAS 100‐point scale) for motion‐related pain Baseline mean: acupuncture 54.15, sham laser acupuncture 57.15 End of study mean: acupuncture 28.27, sham laser acupuncture 40.82 Absolute benefit: acupuncture 25.88, sham laser acupuncture 16.33 SMD ‐0.25 (95% CI random ‐0.62 to 0.13) at 1 week PAIN PRESSURE THRESHOLD (PPT kg/cm2) Baseline mean: acupuncture 1.07, sham laser acupuncture 1.05 End of study mean: acupuncture 0.19, sham laser acupuncture 0.03 Absolute benefit: acupuncture 0.88, sham laser acupuncture 1.02 Reported results: no significant differences between groups SMD 0.16 (95% CI random ‐0.21 to 0.54) immediate post treatment SMD 0.23 (95% CI random ‐0.15 to 0.61) at 3 months Reasons for drop‐out: withdrew, refused treatment, accident, diagnosed with other medical condition, lost to follow‐up | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation stratified for 2 centres |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant not blinded, then participant as outcome assessor would not be blinded either |
| Incomplete outcome data (attrition bias) | Low risk | Described and adequate |
| Incomplete outcome data (attrition bias) | Low risk | Reported in text |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment, 3 days after first treatment, 1 week and 3 months |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT, cross‐over | |
| Participants | Chronic neck disorder without radicular symptoms Participant recruitment: out‐patients from the Department of Physical Medicine and Rehabilitation and the Interdisciplinary Pain Unit at the University of Munich | |
| Interventions | INDEX TREATMENT 1 Non‐local needle acupuncture (NLA) at distant points according to the theory of channels of TCM and varied individually by therapist INDEX TREATMENT 2 Dry needling (dn) of local myofascial trigger points with strong manual stimulation of 'ah shi' points COMPARISON TREATMENT Sham laser acupuncture (SHAM) CO‐INTERVENTION Not reported Treatment schedule: each participant treated once with all interventions with a 1‐week wash‐out period and each session averaging 30 minutes in duration | |
| Outcomes | PAIN INTENSITY (VAS 100 mm scale) for motion‐related pain SMD 0.06 (95% CI random ‐0.42 to 0.54) dn group immediate post treatment Reasons for drop‐out: NA | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Cross‐over design, 6 possible sequences assigned to a number from 1 to 6, random list for 36 participants was then prepared by rolling dice |
| Allocation concealment (selection bias) | Low risk | Fully concealed |
| Blinding (performance bias and detection bias) | Low risk | Participant reported as blinded |
| Blinding (performance bias and detection bias) | High risk | Not possible for acupuncture group, only sham laser acupuncture had caregiver blinded |
| Blinding (performance bias and detection bias) | Low risk | Participant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | Reported and acceptable |
| Incomplete outcome data (attrition bias) | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Each participant received 1 treatment with each intervention with 1‐week wash‐out period between |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT Location: Japan Funding source: Japan Society of Acupuncture and Moxibustion | |
| Participants | Chronic neck pain, no radicular signs Participant recruitment: Participants were recruited from the Meiji University of Oriental Medicine Hospital | |
| Interventions | INDEX TREATMENT 1 Standard acupuncture (SA) Acupuncture points local: GB20, GB21, BL10, BL11, SI12, SI13; distal TE5, LI4, SI3 Inserted needles into the muscle (depth of 20 mm) using 'sparrow pecking' technique; manipulation stopped when participants reached Deqi, and needles were left in place for an additional 10 minutes INDEX TREATMENT 2 Trigger point acupuncture (TrP) Local needling of myofascial trigger points (mean number of insertions 2.3) Needles were inserted 20 mm into the skin over the trigger point by the 'sparrow pecking' technique. Manipulation was stopped when the local twitch response was elicited, and the needle was left in place for an additional 10 minutes INDEX TREATMENT 3: Non‐trigger point acupuncture (non‐TrP) Non‐TrP group received the same treatment as above but at non‐tender points (mean number of insertions 2.4). The non‐tender point chosen had no tenderness nor taut muscle band. However, the point was selected in the same muscle but away from the trigger point by 50 mm COMPARISON TREATMENT Sham acupuncture (SH) SH groups received treatment at trigger points. Similar stainless steel needles were used, but the tips had been cut off and smoothed to prevent penetration of the skin by the needle with the 'sparrow pecking' technique. Simulation of needle extraction was performed after 10 minutes (mean number of insertions 2.6) CO‐INTERVENTION Not specified Treatment schedule: 6 treatments within 10 weeks; applied in 2 phases of 3 treatments: 3 treatments within first 3 weeks, no treatment from week 4 to 7 and 3 treatments from week 7 to 10 Duration of follow‐up: 3 weeks | |
| Outcomes | Groups PAIN INTENSITY (VAS 0 to 100 mm) Baseline mean: SA 69.5, TrP 67.0, non‐TrP 70.9, SH 64.1 End of study mean: SA 51.6, TrP 11.0, non‐TrP 57.6, SH 53.9 Absolute benefit: SA 17.9, TrP 56.0, non‐TrP 13.3, SH 10.2 Reported results: statistically significant improvement in the TrP group only SA vs SH: SMD ‐0.24 (95% CI random ‐1.26 to 0.78) immediate post treatment SA vs SH: SMD ‐0.10 (95% CI random ‐1.11 to 0.92) at 3 weeks TrP vs SH: SMD ‐2.77 (95% CI random ‐4.31 to ‐1.24) immediate post treatment TrP vs SH: SMD ‐2.37 (95% CI random ‐3.78 to ‐0.95) at 3 weeks Non‐TrP vs SH: SMD 0.23 (95% CI random ‐0.79 to 1.25) immediate post treatment Non‐TrP vs SH: SMD ‐0.01 (95% CI random ‐1.03 to 1.00) at 3 weeks DISABILITY: NECK DISABILITY INDEX (NDI 0 to 50 point scale) Baseline mean: SA 12.6, TrP 13.0, non‐TrP 15.1, SH 12.0 End of study mean: SA 10.9, TrP 3.1, non‐TrP 12.0, SH 11.1 Absolute benefit: SA 1.7, TrP 9.9, non‐TrP 3.1, SH 0.9 Reported results: TrP group demonstrated greatest improvement SA vs SH: SMD ‐0.19 (95% CI random ‐1.21 to 0.83) immediate post treatment SA vs SH: SMD ‐0.03 (95% CI random ‐1.05 to 0.98) at 3 weeks TrP vs SH: SMD ‐2.81 (95% CI random ‐4.36 to ‐1.26) immediate post treatment TPA vs SH: SMD ‐1.82 (95% CI random ‐3.09 to ‐0.56) at 3 weeks Non‐TrP vs SH: SMD 0.38 (95% CI random ‐0.65 to 1.41) immediate post treatment Non‐TrP vs SH: SMD 0.18 (95% CI random ‐0.84 to 1.20) at 3 weeks Drop‐outs due to no response to treatment: SA 1, TPA 1, NTPA 1, SH 1 Drop‐outs due to adverse effects: deterioration of symptoms, not specified SA 1, TPA 1, NTPA 0, SH 1 Costs of care: NR | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Participants not adequately blinded |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant as outcome assessor not blinded adequately |
| Incomplete outcome data (attrition bias) | High risk | Discrepancy between Table 2, Figure 3 and text |
| Incomplete outcome data (attrition bias) | High risk | n's in Figure 3 do not add up |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Unclear risk | Table 2 gives only baseline info on those who completed the trial, not those randomised |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Assessed immediately post treatment |
| Fatal Flaw | High risk | Numbers in flow charts and tables do not add up |
| Methods | RCT Number analysed/randomised: 40/40 Funding source: University of Tsukuba, Japan | |
| Participants | WAD symptoms 3 months or longer Participant recruitment: through advertisements in local newspapers and on the homepage of the Kyung Hee Medical Center | |
| Interventions | INDEX TREATMENT Acupuncture Acupuncture points from the gallbladder (GB), small intestine (SI), bladder (BL), triple energiser (TE) and large intestine (LI) meridian systems located on shoulder, neck, head and upper limbs. Needles (length 40 mm; diameter 0.16 mm, SEIRIN Co. Ltd) were inserted perpendicularly to a depth of 1.0 to 2.0 cm in place for 15 minutes COMPARISON Wait‐list CO‐INTERVENTION Both groups maintained their usual care, including physiotherapy, exercise and sufficient rest Treatment schedule: Treatment consisted of 6 sessions, 3×/wk for 2 weeks No follow‐up | |
| Outcomes | PAIN INTENSITY (0 to 10 VAS scale) Drop‐outs: none No serious side effects reported | |
| Notes | Unable to reach study author to obtain necessary data for abstraction | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised number table generated random sequences |
| Allocation concealment (selection bias) | Unclear risk | Envelopes sealed but not sequentially numbered (numbers inside) |
| Blinding (performance bias and detection bias) | High risk | Not possible because of design |
| Blinding (performance bias and detection bias) | High risk | Not possible because of design |
| Blinding (performance bias and detection bias) | Unclear risk | Participant was the outcome assessor with self reports |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Low risk | Acceptable |
| Selective reporting (reporting bias) | Low risk | See registration |
| Similarity of baseline characteristics | Low risk | Reported as similar in Tables 2, 3, 5 |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline and 2 weeks |
| Fatal Flaw | High risk | Flawed; wrong analysis was used; Figure 2 should use independent t‐test, not paired t‐test |
| Methods | RCT Funding source: NR | |
| Participants | Chronic neck disorder associated with degenerative changes ‐ cervical spondylosis Participant recruitment: Guangdong Provincial Hospital of TCM | |
| Interventions | INDEX TREATMENT Routine acupuncture Treated with routine acupuncture at GV 14, Ex‐HN 15 and SI 15 with 40 mm long needles (diameter of 0.30 mm). Needles were retained for 20 minutes after Deqi was achieved COMPARISON TREATMENT Sham acupuncture Sham acupuncture. Needled at 1 cm lateral to Ex‐HN 15 and SI 15 (needles were 40 mm long with a diameter of 0.22 mm). Needles were retained for 20 minutes CO‐INTERVENTION Infrared radiation as adjuvant treatment, comparable between index and control groups Treatment schedule: Treatment consisted of 9 sessions, applied 3 times a week (every other day) over a period of 3 weeks No follow‐up | |
| Outcomes | QUALITY OF LIFE: Northwick Park Neck Pain Questionnaire (up to 100, low score = better) Baseline mean: routine acupuncture 35.32, sham acupuncture 31.96 End of study mean: routine acupuncture 19.16, sham acupuncture 23.76 Absolute benefit: routine acupuncture 16.16, sham acupuncture 8.2 Reported results: Both groups showed improvement SMD ‐0.39 (95% CI random ‐0.77 to ‐0.00) immediate post treatment Adverse effects: NR | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Low risk | As described |
| Selective reporting (reporting bias) | Low risk | None reported |
| Similarity of baseline characteristics | Unclear risk | Not described |
| Co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Similar at baseline and 3 weeks |
| Fatal Flaw | High risk | Reporting flaws |
| Methods | RCT, pilot | |
| Participants | Chronic mechanical neck disorder Participant recruitment: outpatient clinic of Guangdong Provincial Hospital of Chinese Medicine in Guangzhou, China | |
| Interventions | INDEX TREATMENT Acupuncture group COMPARISON TREATMENT Sham CO‐INTERVENTION NR Treatment schedule: 3 weeks, total 9 sessions, with each session averaging 20 minutes in duration | |
| Outcomes | PAIN INTENSITY (VAS 10 cm scale) SMD ‐0.40 (95% CI random ‐0.69 to ‐0.10) at 4 weeks SMD ‐0.20 (95% CI random ‐0.50 to 0.09) at 3 months NECK DISABILITY: NPQ Baseline mean: acupuncture 32.73, sham 33.04 End of study mean: acupuncture 19.09, sham 23.53 Absolute benefit: acupuncture 13/64, sham 9.51 Reported results: significant favouring acupuncture SMD ‐0.28 (95% CI random ‐0.57 to 0.02) immediate post treatment SMD ‐0.37 (95% CI random ‐0.67 to ‐0.07) at 4 weeks SMD ‐0.37 (95% CI random ‐0.67 to ‐0.07) at 3 months QUALITY OF LIFE: SF‐36 (Physical Component ‐ higher = better) Baseline mean: acupuncture 80.79, sham 79.22 End of study mean: acupuncture 84.26, sham 85.88 Absolute benefit: 3.47, sham 6.66 Reported results: no significant differences between groups SMD 0.38 (95% CI random 0.08 to 0.68) immediate post treatment SMD ‐0.05 (95% CI random ‐0.35 to 0.24) at 4 weeks SMD ‐0.11 (95% CI random ‐0.40 to 0.18) at 3 months | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers were generated by computer software |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding (performance bias and detection bias) | Low risk | Reported as blinded |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Participant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | Reported in text and acceptable |
| Incomplete outcome data (attrition bias) | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment, 4 weeks, 3 months |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Chronic neck pain, no radicular signs Participant recruitment: students from an acupuncture school in Japan | |
| Interventions | Treatment was provided to 'tender points' on the posterior aspect of the neck and upper back "All tender points were carefully detected where the subjects felt dull pain and stiffness (neck, shoulder, and back) and were used for the acupuncture treatment. All tender points were treated in each group” INDEX TREATMENT 'Sparrow pecking' acupuncture Disposable stainless needles (0.2 mm × 40 mm) were inserted into the muscle to a depth of about 20 mm, and the ‘sparrow pecking’ technique was applied. When the participant felt Deqi, the manipulation was stopped and the needle was retained for 5 more minutes COMPARISON TREATMENT Simulated 'sparrow pecking' acupuncture with no needle insertion For sham acupuncture, similar stainless needles (0.2 mm × 40 mm) were used, but the tips had previously been cut off to prevent the needle from penetrating the skin. The cut ends were smoothed with sandpaper manually under clean conditions. The acupuncturist pretended to insert the needle and to use the sparrow pecking technique, then removed the needles. Simulation of needle extraction was performed after 5 minutes CO‐INTERVENTION Not specified Duration of treatment: once/wk for 3 weeks Duration of follow‐up: 9 days | |
| Outcomes | PAIN INTENSITY: VAS Baseline mean: acupuncture 60.5, sham 48.8 End of study mean: acupuncture 43.3, sham 46.8 Absolute benefit: acupuncture 17.2, sham 2.0 Reported results: significant favouring acupuncture SMD ‐0.15 (95% CI random ‐0.82 to 0.52) at 9 days Reasons for drop‐out: NR | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation programme |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Low risk | Reported as blinded |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Participant as outcome assessor was blinded |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar but baseline VAS different by 11.7 |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | High risk | Some participants did not receive all treatment |
| Similar timing of outcome assessment? | Low risk | 9 days |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Chronic mechanical neck disorder with radicular signs or symptoms Participant recruitment: out‐patients from Addenbrooke's Hospital, Cambridge, UK | |
| Interventions | INDEX TREATMENT Acupuncture group COMPARISON Placebo TNS group CO‐INTERVENTION Comparable between index and control groups Treatment schedule: 4 weeks (2 times/wk), with each session averaging 20 minutes | |
| Outcomes | PAIN INTENSITY: pain relief score (5 point scale) Reasons for drop‐out: NA | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reported only as randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Appears similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | All participants treated twice weekly for 4 weeks |
| Similar timing of outcome assessment? | Low risk | Assessed immediately post treatment |
| Fatal Flaw | High risk | Randomisation and allocation concealment details not reported |
| Methods | RCT | |
| Participants | Chronic mechanical neck disorder Participant recruitment: hospitalised patients from Queen Elizabeth Hospital, Palmersion North, New Zealand | |
| Interventions | INDEX TREATMENT Acupuncture group COMPARISON TREATMENT Sham TNS CO‐INTERVENTION Analgesics comparable between groups Treatment schedule: 2 sessions/wk for 4 weeks, with each session averaging 20 minutes in duration | |
| Outcomes | PAIN INTENSITY (4 item VAS scale) | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Drop‐outs described and acceptable |
| Incomplete outcome data (attrition bias) | High risk | All randomised participants were not analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | High risk | Acupuncture group had more daily use of NSAIDs and pain scores with statistically significant differences |
| Co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | High risk | Not all participants received the scheduled 8 treatments |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment |
| Fatal Flaw | High risk | Due to inadequate reporting |
| Methods | RCT | |
| Participants | Chronic myofascial neck pain Participant recruitment: patients recruited from the clinic of the Department of Physical Medicine and Rehabilitation in Turkey | |
| Interventions | INDEX TREATMENT Electroacupuncture group (EAP) COMPARISON TREATMENT Sham EAP CO‐INTERVENTION NR Treatment schedule: 10 sessions over 3 weeks, with each session averaging 30 minutes in duration | |
| Outcomes | PAIN INTENSITY (10 point VAS (movement) scale) Reported results: not significant, including pain at rest SMD ‐0.56 (95% CI random ‐1.31 to 0.19) immediate post treatment SMD 0.00 (95% CI random ‐0.73 to 0.73) at 3 months | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not described |
| Allocation concealment (selection bias) | High risk | Names sealed in opaque envelopes. Envelopes were then allocated randomly into 2 groups. After the doctor examined participants, she gave the names of those who were included in the study to someone else, who prepared the envelopes |
| Blinding (performance bias and detection bias) | Low risk | Reported as blinded |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Participant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | Described and acceptable |
| Incomplete outcome data (attrition bias) | High risk | All randomised participants not analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | High risk | VAS pain scores > 10% difference |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Assessed immediate post treatment and 3 months |
| Fatal Flaw | High risk | Randomisation not performed properly; planned to recruit 80 participants but enrolled only 31 |
| Methods | RCT | |
| Participants | Chronic mechanical neck disorder: cervical tendomyosis Participant recruitment: NR | |
| Interventions | INDEX TREATMENT Conventional meridian acupuncture (Acu) 15 minutes per session; maximum 15 needles per session. Option of 15 acupuncture points was available. Seirin needles 7, 0.3 × 30 mm and 0.2 × 15 mm. Insertion until the Deqi response was achieved COMPARISON TREATMENT Placebo LASER (LLLT0) Outcome power: 0 mV, Meridian acupuncture points same as acupuncture group CO‐INTERVENTION Avoided in trial design Treatment schedule: 4 weeks, 2 sessions per week ‐ total 8 sessions Duration of follow‐up: 4 weeks | |
| Outcomes | PAIN INTENSITY: VAS (mm) Baseline mean: Acu 39.3, LLLT0 34.1 End of study mean: Acu 7.0, LLLT0 25.2 Absolute benefit: Acu 32.3, LLLT0 8.9 SMD ‐0.86 (95% CI random ‐1.70 to ‐0.02) at immediate post SMD ‐0.46 (95% CI random ‐1.27 to 0.35) at 4 week follow‐up Reported results: statistically significant favouring acupuncture immediate post treatment and at 4 week follow‐up TENDERNESS (pressure pain threshold ‐ PPT) Baseline mean: Acu 4.13, LLLT0 5.05 End of study mean: Acu 5.75, LLLT0 6.12 Absolute benefit: Acu 1.62, LLLT0 1.07 Reported results: not significant SMD ‐0.14 (95% CI random ‐0.95 to 0.66) at immediate post SMD ‐0.22 (95% CI random ‐1.02 to 0.58) at 4 week follow‐up Reasons for drop‐out: NR Adverse effects: reported for control and for index treatment; not specified Costs of care: NR | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Reported randomised double‐blinded |
| Allocation concealment (selection bias) | Unclear risk | Possibly adequate |
| Blinding (performance bias and detection bias) | Low risk | Reported as blinded |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Paticipant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | Reported and acceptable |
| Incomplete outcome data (attrition bias) | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Low risk | Avoided |
| Compliance acceptable? | High risk | Not acceptable |
| Similar timing of outcome assessment? | Low risk | Assessed at 4 weeks |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Myofascial neck pain syndrome (MPS) Participant recruitment: Department of Neurology at Nantou Hospital, Department of Health | |
| Interventions | INDEX TREATMENT Acupuncture group COMPARISON TREATMENT Sham acupuncture CO‐INTERVENTION NR Treatment schedule: 2 sessions/wk for 3 consecutive weeks, with each session averaging 20 minutes in duration | |
| Outcomes | PAIN INTENSITY (100 point VAS (movement) scale) SMD ‐0.54 (95% CI random ‐1.22 to 0.15) at 4 weeks | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not clear if adequately done |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Unclear risk | Some participant were not naive to acupuncture |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear whether participant was blinded and was also the outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | Reported and acceptable |
| Incomplete outcome data (attrition bias) | Unclear risk | Appears 1 randomised participant may not have been analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not specifically and clearly reported |
| Similar timing of outcome assessment? | Low risk | Assessed after 6 treatments, 4 weeks, 12 weeks |
| Fatal Flaw | High risk | Randomisation not clearly done properly; participants do not appear to have been blinded; ITT not done; missing data handled by last observation carried forward; all P values in Table 2 within‐group changes; scores in Table 3 do not look credible |
| Methods | RCT cross‐over Funding source: NR | |
| Participants | Chronic mechanical neck disorder, cervical osteoarthritis Participant recruitment: Sweden | |
| Interventions | INDEX TREATMENT Instructed to take no pain medication 24 hours before trials | |
| Outcomes | PAIN INTENSITY (VAS 0 to 10) vs placebo acupuncture: SMD 0.17 (95% CI random ‐0.25 to 0.59) immediate post treatment vs placebo diazepam: SMD 0.09 (95% CI random ‐0.33 to 0.51) immediate post treatment | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only described as randomised to order |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant not blinded as outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Each participant received all treatments |
| Co‐interventions avoided or similar? | Low risk | Avoided |
| Compliance acceptable? | Low risk | All participants received all treatments |
| Similar timing of outcome assessment? | Low risk | Immediate post treatment |
| Fatal Flaw | High risk | Improper error terms for analysis (SD should not be used for within‐patient analysis); randomisation and concealment not described; no adjustments made for order; balancing not apparent |
| Methods | RCT pilot/feasibility study Number analysed/randomised: 34/41 | |
| Participants | WAD myofascial pain (injury of 2 to 16 week duration) Participant recruitment: Derriford Hospital Physiotherapy Department, UK | |
| Interventions | INDEX TREATMENT Acupuncture group Trigger point needling using 0.25 mm × 30 to 40 mm length, 6 to 7 sparrow pecking into each MTrP (muscles treated not described) COMPARISON Sham acupuncture CO‐INTERVENTION Participant education, heat, analgesics and exercise (home therapy) Treatment schedule: 1 session/wk, total 2 to 6 treatments depending on participant response | |
| Outcomes | PAIN INTENSITY (SF‐McGill Pain Questionnaire, VAS component 10 cm scale) Absolute benefit: acupuncture 3.2, sham acupuncture 1.8 DISABILITY: NECK DISABILITY INDEX (NDI 0 to 50 point scale) Baseline mean: acupuncture 18.6, sham acupuncture 20.5 End of study mean: acupuncture 8.4, sham acupuncture 11.9 Absolute benefit: acupuncture 10.2, sham acupuncture 8.6 Reported results: not significant SMD ‐0.41 (95% CI random ‐1.09 to 0.27) at 6 weeks Reasons for drop‐out: increased pain (stopped attending: 3 acupuncture, 4 sham) Costs of care: NR | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Reported as random allocation sequence, computer‐generated using block size of 4 |
| Allocation concealment (selection bias) | Low risk | Held centrally by the pharmacy department at the research site; allocation concealed from the investigator until after participant enrolment |
| Blinding (performance bias and detection bias) | Unclear risk | Unclear whether sham was indistinguishable |
| Blinding (performance bias and detection bias) | High risk | Not possible because of design |
| Blinding (performance bias and detection bias) | Unclear risk | Participant was the outcome assessor with self reports |
| Incomplete outcome data (attrition bias) | Low risk | Acceptable at 17% |
| Incomplete outcome data (attrition bias) | High risk | Only participants who completed the study were included; ITT done only for P value |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics | Low risk | Reported as similar Tables 1 and 2 |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Exercise booklet given; unsure whether participants received all acupuncture treatment prescribed |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 and 6 weeks |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Chronic myofascial neck pain Participant recruitment: teaching hospital, Taiwan | |
| Interventions | INDEX TREATMENT Acupuncture group Dry needling, used a 25‐hypodermic needle (0.5 mm in diameter). Manual stimulation of the needle to the MTrP region of the extensor carpi radialis longus muscle to elicit a local twitch response. 1 to 2 minutes COMPARISON Sham acupuncture CO‐INTERVENTION Avoided Treatment schedule: 1 session | |
| Outcomes | PAIN INTENSITY (0 to 10 VAS scale) Absolute benefit: acupuncture 2.1, sham acupuncture 0.8 PRESSURE PAIN THRESHOLD (PPT, kg/cm2) Baseline mean: acupuncture 2.3, sham acupuncture 2.5 Absolute benefit: acupuncture 1.5, sham acupuncture 0.4 SMD ‐1.25 (95% CI random ‐0.52 to ‐1.98) immediate post treatment | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation programme |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Low risk | Reported in text |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Participant blinded as outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | No drop‐outs |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Low risk | Avoided by pre/post design |
| Compliance acceptable? | Low risk | Acceptable by design |
| Similar timing of outcome assessment? | Low risk | Immediate post treatment |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Non‐specific cervical disorder, uncomplicated Participant recruitment: Participants were referred to the Pain Treatment Unit at a Primary Attention Healthcare Centre in Spain by general practitioners in the municipality | |
| Interventions | INDEX TREATMENT Points were selected according to pain characteristics and accompanying symptoms on the basis of traditional Chinese treatment methods. Puncture was bilateral, with sterile, single‐use needles (25 mm × 0.25 mm or 40 mm × 0.25 mm). Puncture was effected by determining the Deqi. Needles were kept in place for 30 minutes and were manually stimulated every 10 minutes. After the needles were removed, Vaccaria seeds were applied in the ear auricle and were taped there until the following treatment session. Participants were told to apply pressure to each ear point for a series of 10 repeats 3 times per day COMPARISON TREATMENT TENS placebo Applied using TRANSMED 911 transcutaneous nerve stimulation units that had been adjusted beforehand to prevent current through the electrodes. Electrodes were placed at Jianjing (GB 21) bilateral acupuncture point for 30 minutes. Participant's state was checked every 10 minutes, and the TENS‐placebo potentiometer adjusted CO‐INTERVENTION Not avoided but comparable; both groups were provided with analgesic rescue medications once weekly Duration of treatment: 3 weeks Treatment consisted of 5 sessions over 3 weeks (2 in each of first 2 weeks and once in the third week) Duration of follow‐up: 6 months | |
| Outcomes | PAIN INTENSITY (VAS 100 mm scale related to motion) Baseline mean: acupuncture 68.7, placebo TENS 72.3 End of study mean: acupuncture 27.6, placebo TENS 45.5 Absolute benefit: acupuncture 41.1, placebo TENS 26.8 SMD ‐1.50 (95% CI random ‐1.91 to ‐1.10) at 1 week SMD ‐0.54 (95% CI random ‐0.97 to ‐0.10) at 6 months FUNCTION (DISCAPACITY): Northwick Park Pain Questionnaire (NPQ 0 to 100 scale) Baseline mean: acupuncture 52.7, placebo TENS 56.5 End of study mean: acupuncture 22.5, placebo TENS 43.8 Absolute benefit: acupuncture 30.2, placebo TENS 12.7 Reported results: significant at 1 week after final treatment SMD ‐1.22 (95% CI random ‐1.60 to ‐0.83) at 1 week 6 month follow‐up for this outcome: NR QUALITY OF LIFE: SF‐36 (Physical Component ‐ higher = better) Baseline mean: acupuncture 36.7, placebo TENS 37.6 End of study mean: acupuncture 27.4, placebo TENS 32.3 Absolute benefit: acupuncture 9.3, placebo TENS 5.3 Results: significant difference at 1 week favouring acupuncture but not at 6 months SMD ‐0.57 (95% CI random ‐0.93 to ‐0.21) at 1 week SMD 0.41 (95% CI random ‐0.02 to 0.84) at 6 months Reasons for drop‐out: personal reasons, pregnancy, fear Reported for control: increase in symptoms Reported for index treatment: swelling or bruising of the hand | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Opaque envelopes not reported as sequentially numbered |
| Blinding (performance bias and detection bias) | Low risk | Reported in text as participant blinded |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | Low risk | Blinded participant as outcome assessor |
| Incomplete outcome data (attrition bias) | High risk | Drop‐out approximately 35% at long term |
| Incomplete outcome data (attrition bias) | High risk | Not reported for long term |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | High risk | Reported only on medication use |
| Compliance acceptable? | Unclear risk | Unsure whether ear seed protocol was followed by each participant |
| Similar timing of outcome assessment? | Low risk | Assessed at 1 week and 6 months |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT/cross‐over | |
| Participants | Chronic mechanical neck disorder, degenerative changes Participant recruitment: Eugene McDermott Centre for Pain Management, Department of Anesthesiology and Pain Management, University of Texas Southwestern Medical Centre, Dallas, Texas | |
| Interventions | INDEX TREATMENT 1 Local dermatomal stimulation COMPARISON TREATMENT 1 Remote dermatomal stimulation COMPARISON TREATMENT 2 Control needles only CO‐INTERVENTION Analgesics comparable between groups Treatment schedule: 3 times/wk for 3 consecutive weeks, with 1 week off between modalities and each session averaging 30 minutes in duration | |
| Outcomes | PAIN INTENSITY (10 cm VAS scale) Reasons for drop‐out: NA | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Inadequate description |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear whether all analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | High risk | Means given as 1 group in total |
| Co‐interventions avoided or similar? | High risk | Medication use not similar |
| Compliance acceptable? | Low risk | Acceptable |
| Similar timing of outcome assessment? | Low risk | Immediate post treatment |
| Fatal Flaw | High risk | Inadequate reporting |
| Methods | RCT | |
| Participants | Chronic mechanical neck disorder Participant recruitment: out‐patient departments of Southampton General Hospital and Salisbury District Hospital, United Kingdom | |
| Interventions | INDEX TREATMENT Acupuncture with single‐use needles, points based on individualised western acupuncture techniques previously reported as effective in neck pain, 6 points on average, with each session averaging 20 minutes in duration. Manual stimulation to Deqi. 8 treatments over 4 weeks provided by physiotherapists with 7 years of experience COMPARISON TREATMENT Mock TENS electroacupuncture stimulator; up to 8 points could be stimulated at 1 time; session time not reported CO‐INTERVENTION Comparable between index and control groups Treatment schedule: Both groups received 8 sessions over 4 weeks | |
| Outcomes | PAIN INTENSITY (100 mm VAS scale) DISABILITY (NDI 0 to 50 point scale) SMD ‐0.08 (95% CI random ‐0.43 to 0.27) at 1 week SMD ‐0.24 (95% CI random ‐0.60 to 0.12) at 8 weeks SMD ‐0.09 (95% CI random ‐0.47 to 0.28) at 6 months SMD ‐0.23 (95% CI random ‐0.61 to 0.15) at 1 year QUALITY OF LIFE (SF‐36, Physical Component) SMD 0.07 (95% CI random ‐0.28 to 0.42) at 1 week SMD ‐0.13 (95% CI random ‐0.49 to 0.23) at 8 weeks Time points at 6 months and 1 year not reported for this outcome | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes; unclear whether opaque and sequentially numbered |
| Blinding (performance bias and detection bias) | High risk | Interventions perceivably different |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Acceptable |
| Incomplete outcome data (attrition bias) | High risk | Not all randomised participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | High risk | Medication use not similar |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | 6 months and 1 year |
| Fatal Flaw | Low risk | Acceptable |
| Methods | RCT | |
| Participants | Chronic neck pain Participant recruitment: Participants with neck pain asked a participating physician for acupuncture, or physician considered acupuncture to be adequate treatment | |
| Interventions | INDEX TREATMENT Immediate acupuncture treatment plus additional conventional treatment as needed Participants could be treated individually, and numbers of needles and acupuncture points used were chosen at the discretion of physicians. Only needle acupuncture (with disposable 1‐time needles) and manual stimulation were allowed, whereas other forms of acupuncture treatment were not allowed COMPARISON TREATMENT Conventional treatment; delayed acupuncture treatment 3 months after study onset Control group was not allowed to use any kind of acupuncture during first 3 months CO‐INTERVENTION Comparable between index and control groups. Participants were free to use conventional routine medical care as offered by German social health insurance funds Treatment schedule: Each participant in the randomised acupuncture group received up to 15 acupuncture sessions during first 3 months and no acupuncture sessions between 3 and 6 months Duration of treatment: 3 months Duration of follow‐up: 3 months after treatment | |
| Outcomes | HEALTH AND WELL‐BEING Neck and pain disability assessed by validated neck and pain disability scale developed by Wheeler Baseline mean: 55.0 immediate acupuncture (randomised), 56.0 (immediate acupuncture non‐randomised), 53.9 delayed acupuncture % reduction in neck pain and disability Time 1 (3 months): 28.9 immediate acupuncture (randomised), 31.7 immediate acupuncture (non‐randomised), 5.8 delayed acupuncture Time 2 (6 months): 28.0 immediate acupuncture (randomised), 30.6 immediate acupuncture (non‐randomised), 25.1 delayed acupuncture Reported results: significant at time 1 SMD ‐35.53 (95% CI random ‐36.37 to ‐34.69) at 3 month follow‐up SMD 4.14 (95% CI random 4.02 to 4.26) at 6 month follow‐up SF‐36 PHYSICAL COMPONENT SCORE Baseline mean: 37.6 immediate acupuncture (randomised), 36.7 immediate acupuncture (non‐randomised), 38.1 delayed acupuncture Time 1 (3 months): 5.8 immediate acupuncture (randomised), 6.8 immediate acupuncture (non‐randomised), 4.7 delayed acupuncture Time 2 (6 months): 5.6 immediate acupuncture (randomised), 6.8 immediate acupuncture (non‐randomised), 0.7 delayed acupuncture SMD 22.99 (95% CI random 22.45 to 23.54) at 3 month follow‐up SMD 3.00 (95% CI random 2.90 to 3.10) at 6 month follow‐up SF‐36 MENTAL COMPONENT SCORE Baseline mean: 43.1 immediate acupuncture (randomised), 42.8 immediate acupuncture (non‐randomised), 43.8 delayed acupuncture Time 1 (3 months): 4.2 immediate acupuncture (randomised), 4.7 immediate acupuncture (non‐randomised), 3.1 delayed acupuncture Time 2 (6 months): 4.0 immediate acupuncture (randomised), 4.8 immediate acupuncture (non‐randomised), 3.1 delayed acupuncture SMD 12.80 (95% CI random 12.49 to 13.11) at 3 month follow‐up SMD 3.00 (95% CI random 2.90 to 3.10) at 6 month follow‐up Reasons for drop‐out: 315 participants could not be included in the ITT analysis because the study office did not receive the consent form Adverse effects: 8.9% of cases (n = 1005); 1216 side effects were reported: 57% minor local bleeding or hematoma, 10% pain (e.g. needling pain), 4% vegetative symptoms, 29% other Costs of care: acupuncture treatment associated with higher costs (€925.53 ± 1551.06 vs €648.06 ± 1459.13); however according to assumed threshold values beyond 3 month follow‐up, acupuncture appears cost‐effective. Also, over‐the‐counter medications were not included in the cost of routine care | |
| Notes | ‐‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using a central telephone randomisation procedure |
| Allocation concealment (selection bias) | Low risk | Study office included participants into the study |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Not possible |
| Blinding (performance bias and detection bias) | High risk | Participant as outcome assessor not blinded |
| Incomplete outcome data (attrition bias) | High risk | Drop‐outs not adequately described |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear whether ITT was done correctly |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics | Low risk | Reported to be similar |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Most participants (77.3%) received 5 to 10 sessions, whereas 17.7% received more than 10 sessions and 5% fewer than 5 sessions |
| Similar timing of outcome assessment? | Low risk | Assessed at 3 and 6 months |
| Fatal Flaw | Low risk | Acceptable |
Abbreviations:
BL = bladder
CI = confidence interval
cm = centimetre
dn = dry needling
EAP = electroacupuncture
g = gauge
GB = gallbladderITT = intention‐to‐treat
LI = large intestine
LLLT0 = placebo intestine
mg = milligram
mm = millimetreMPS = myofascial neck pain syndrome
MTrP = muscles treated not described
NA = not applicable
NDI = Neck Disability Index
NLA = non‐local needle electroacupuncture
NPQ = Northwick Park Pain Questionnaire
NR = not reported
NSAID = non‐steroidal anti‐inflammatory drug
NTPA = non‐trigger point acupuncture
OD = daily
PPT = pain pressure threshold
RA = remote acupuncture
RCT = randomised controlled trial
SA = standard acupuncture
SD = standard deviation
SF‐36 = Short Form‐36
SH = sham treatment
SI = small intestine
SMD = standardised mean difference
TCM = Traditional Chinese Medicine
TE = triple energiser
TENS = transcutaneous electrical nerve stimulation
TNS = transcutaneous nerve stimulation
TPA = trigger point acupuncture
TrP = trigger point acupuncture
VAS = visual analogue scale
WAD = whiplash‐associated disorder
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Comparison: acupuncture vs active treatment (ultrasound) | |
| Intervention: auto‐acupressure, not acupuncture Comparison: active treatment (paracetamol and/or ibuprofen and tetrazepam) | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: 3 acupuncture doses compared | |
| Comparison: acupuncture vs active treatment (NSAID) | |
| Intervention (EMG needle) | |
| Population: migraine and tension‐type headaches, others not specified as cervicogenic Comparison: acupuncture vs active treatment (medical management) | |
| Intervention: acupuncture portion of multi‐modal treatment | |
| Comparison: acupuncture vs active treatment (mobilisation) | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: multi‐modal treatment acupuncture vs active treatment (stretching) | |
| Population: ankylosing spondylitis | |
| Comparison: acupuncture vs active treatment (lidocaine injection or oral flurbiprofen) | |
| Comparison: acupuncture portion of multi‐modal treatment vs active treatment (usual care) | |
| Comparison: acupuncture received in both groups as control | |
| Comparison: acupuncture vs active treatment (exercise) | |
| Comparison: acupuncture vs active treatment (lidocaine) | |
| Comparison: 1 acupuncture insertion direction vs another | |
| Comparison: electroacupuncture vs active treatment (traction and low‐frequency therapy) | |
| Design: quasi‐RCT Comparison: acupuncture vs active treatment (lidocaine) | |
| Comparison: acupuncture vs active treatment (lidocaine) | |
| Population: tendomyotonic cervical and lumbar syndrome; unable to separate data | |
| Population: rheumatoid arthritis | |
| Intervention: acupuncture combined with manual therapy; not a stand‐alone treatment | |
| Population: pain in many areas; unable to separate data | |
| Intervention: individual vs group acupuncture | |
| Comparison: acupuncture vs active treatment (medication) | |
| Population: neck and low back; unable to split data | |
| Comparison: included other treatments with acupuncture; the effect of acupuncture could not be isolated | |
| Comparison: acupuncture portion of the control | |
| Comparison: sham acupuncture vs lidocaine injection (no real acupuncture compared) | |
| Comparison: acupuncture may be part of multi‐modal treatment vs epidural steroid injections (ESI) with depo‐methylprednisolone | |
| Comparison: electroacupuncture vs active treatment (bloodletting and cupping ‐ CAM intervention) | |
| Design: quasi‐RCT Comparison: electroacupuncture portion of control | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: acupuncture vs active treatment (traction, magnetic therapy) Outcome: blood flow; no participant‐specific outcomes | |
| Comparison: acupuncture portion of multi‐modal usual care active treatment (2 participants) | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: 1 acupuncture type vs another | |
| Abstract; did not appear to be RCT; unable to contact study author | |
| Comparison: 1 acupuncture type vs another | |
| Population: neck and shoulder pain; cannot split data | |
| Comparison: 1 acupuncture type vs another | |
| Population: spinal cord stenosis Comparison: acupuncture vs active treatment (manipulation/traction) | |
| Comparison: acupuncture received in both groups as control | |
| Intervention: scalpel technique | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: acupuncture vs active treatment (intravenous drip with 5% glucose 250 mL and compound Salvia miltiorrhiza injection and mechanical traction) | |
| Comparison: acupuncture vs acupuncture with moxibustion | |
| Comparison: acupuncture vs active treatment (trigger point manual therapy) | |
| Design: quasi‐RCT Comparison: acupuncture vs active treatment (traction and shortwave diathermy) | |
| Comparison: 1 acupuncture type vs another | |
| Population: head and neck pain included; unable to obtain split data | |
| Comparison: multi‐modal; effects of acupuncture unknown | |
| Design: non‐RCT | |
| Intervention: mini‐scalpel | |
| Comparison: acupuncture vs active treatment (Alexander lessons, postural awareness, usual care) | |
| Comparison: acupuncture portion of multi‐modal usual care active treatment (4 participants) | |
| Comparison: see excluded Giles 2003; this is LT follow‐up | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: 1 type of acupuncture vs another | |
| Design: quasi‐RCT Population: occipital neuralgia | |
| Comparison: 1 acupuncture type vs another | |
| Design: non‐RCT | |
| Comparison: acupuncture vs active treatment (physiotherapy including heat, TENS, ultrasound, passive and self stretching) | |
| Comparison: acupuncture vs active treatment (GP care in both groups) | |
| Population: individuals with latent trigger points in upper trapezius, no neck pain | |
| Comparison: 1 acupuncture type vs another | |
| Intervention: bee venom acupuncture (BVA) injected with syringe Comparison: acupuncture vs active treatment (NSAID) | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: multi‐modal; effects of acupuncture unknown | |
| Comparison: acupuncture vs electroacupuncture (protocol) | |
| Population: individuals with functional neck stiffness without pain | |
| Abstract; did not appear to be RCT; unable to obtain further information | |
| Comparison: active treatment (relaxation therapy) | |
| Population: tension‐type and/or migraine headaches Comparison: acupuncture vs active treatment (lidocaine) | |
| Population: tension‐type and/or migraine headaches Comparison: active treatment (lidocaine or Botox) | |
| Comparison: 1 acupuncture type vs another vs active treatment (oral Jing fukang granule) | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: acupuncture in both groups as control | |
| Comparison: 1 acupuncture type vs another | |
| Design: quasi‐RCT Comparison: 1 acupuncture type vs another | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: acupuncture vs active treatment (Chinese manipulation) | |
| Comparison: 3 types of acupuncture needles compared | |
| Comparison: acupuncture vs active treatment (TENS) | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: 1 acupuncture type vs another | |
| Design: appeared to be before/after study or case series report Population: included myelopathy | |
| Comparison: acupuncture vs active treatment (traction) | |
| Comparison: electroacupuncture vs active treatment (laser) | |
| Comparison: acupuncture received in both groups as control | |
| Intervention: 1 acupuncture type vs another | |
| Comparison: acupuncture with moxibustion | |
| Intervention: mini‐scalpel acupuncture Comparison: 1 acupuncture type vs another | |
| Intervention: injection‐type needle | |
| Comparison; acupuncture vs active treatment (moxibustion) | |
| Outcome: no between‐group comparison analysed | |
| Comparison: acupuncture vs needle‐knife therapy | |
| Comparison: 1 acupuncture type vs another | |
| Comparison: acupuncture vs active treatment (massage) |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Abstract for RCT |
| Participants | 67 acute neck and back pain |
| Interventions | Acupuncture vs sham acupuncture plus standard ER care (medication not described) |
| Outcomes | Numeric Rating Scale (NRS), ROM, Symptom Checklist (SCL) questionnaire and overall satisfaction |
| Notes | Await full study, contact study author |
| Methods | RCT |
| Participants | 65 patients with acute or subacute/chronic simple back or neck pain |
| Interventions | Acupuncture vs placebo acupuncture vs no treatment |
| Outcomes | Pain (NPS) |
| Notes | clinicaltrials.gov |
| Methods | RCT |
| Participants | 44 patients with myofascial neck pain |
| Interventions | Acupuncture + stretching vs same stretching |
| Outcomes | Pain (VAS), pressure pain threshold |
| Notes | clinicaltrials.gov |
| Methods | RCT |
| Participants | 40 patients with whiplash‐associated disorder |
| Interventions | Acupuncture vs wait‐list |
| Outcomes | Pain (VAS), post‐needling pain, pressure pain threshold, range of motion, quality of life (SF‐36), Depression Scale, Cornell Medical Index (CMI) |
| Notes | clinicaltrials.gov |
| Methods | Guo Y |
| Participants | 154 with unspecific duration of neck pain |
| Interventions | Acupuncture vs sham acupuncture |
| Outcomes | Pain (NPQ, VAS), quality of life (SF‐36), participant satisfaction |
| Notes | http://apps.who.int/trialsearch/AdvSearch.aspx |
| Methods | Abstract for RCT |
| Participants | 60 patients with unilateral cervicobrachialgia |
| Interventions | Abdominal acupuncture vs sham abdominal acupuncture |
| Outcomes | VAS for pain and hypomobility (ROM) |
| Notes | Await full study, contact study author |
| Methods | RCT |
| Participants | 17 patients with acute mechanical idiopathic unilateral neck pain |
| Interventions | Dry needling of trigger points vs no treatment control |
| Outcomes | Numeric Pain Rating Scale (NPRS), pressure pain threshold (PPT) for pain, range of motion |
| Notes | ‐‐ |
| Methods | RCT |
| Participants | 23 patients with acute symptoms of craniomandibular disorder |
| Interventions | Acupuncture vs sham laser |
| Outcomes | Pain intensity (VAS), functional muscle test, ability to open the mouth, axiographic evaluation |
| Notes | German; awaiting translation |
| Methods | Protocol for double‐blind RCT |
| Participants | 120 participants with chronic whiplash, grade II |
| Interventions | Dry needling, advice and exercise vs sham dry needling, advice and exercise |
| Outcomes | Neck Disability Index (NDI), participant‐perceived recovery |
| Notes | ‐‐ |
| Methods | RCT, cross‐over design |
| Participants | 19 patients with myofascial neck pain |
| Interventions | Acupuncture, acupuncture plus stretching vs placebo laser acupuncture |
| Outcomes | Mechanical pain threshold, motion‐related pain (visual analogue scale ‐ VAS) and cervical range of motion, range of motion |
| Notes | ‐‐ |
| Methods | RCT |
| Participants | 206 patients with chronic neck pain |
| Interventions | Electroacupuncture vs sham laser acupuncture |
| Outcomes | Neck Pain Disability Northwick Park Neck Pain Questionnaire (NPQ), Quality of Life SF‐36 health survey, use of medication for neck pain, sick leave |
| Notes | ‐‐ |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Evaluation of immediate effect of acupuncture on pain, cervical range of motion and electromyographic activity of the upper trapezius muscle in patients with non‐specific neck pain: study protocol for a randomised controlled trial |
| Methods | Protocol for RCT cross‐over design, 1 week wash‐out period |
| Participants | 12 participants with neck pain, 12 healthy participants |
| Interventions | Acupuncture vs placebo acupuncture |
| Outcomes | EMG activity of upper trapezius, NPRS for neck pain and cervical range of motion (CROM) |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | ‐‐ |
| Trial name or title | Acupuncture as analgesia for non‐emergent acute non‐specific neck pain, ankle sprain and primary headache in an emergency department setting: a protocol for a parallel‐group, randomised, controlled pilot trial |
| Methods | Protocol for RCT |
| Participants | 40 patients with non‐emergent acute neck pain, ankle sprain or primary headache |
| Interventions | Acupuncture + standard emergency department care vs same |
| Outcomes | Numeric Rating Scale for pain (NRS), Neck Disability Index (NDI), participant‐reported overall improvement |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | To be determined if number of participants with neck pain is sufficient and extractable data are available and/or if primary headaches are of cervical origin |
| Trial name or title | Optimised acupuncture treatment for neck pain caused by cervical spondylosis: a study protocol of a multi‐centre randomised controlled trial |
| Methods | Protocol for RCT |
| Participants | 945 patients with cervical spondylosis |
| Interventions | Acupuncture vs sham acupuncture vs shallow acupuncture |
| Outcomes | Northwick Park Pain Questionnaire (NPQ), McGill Pain Questionnaire (MPQ) and SF‐36 for pain and disability |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | ‐‐ |
| Trial name or title | Effectiveness of acupuncture intervention for neck pain caused by cervical spondylosis: study protocol for a randomised controlled trial |
| Methods | Protocol for RCT |
| Participants | 456 patients with neck pain caused by cervical spondylosis |
| Interventions | Acupuncture vs sham acupuncture |
| Outcomes | NPQ, MPQ and SF‐36 for pain and disability |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | ‐‐ |
| Trial name or title | Acupuncture at Houxi (SI 3) acupoint for acute neck pain caused by stiff neck: study protocol for a pilot randomised controlled trial. |
| Methods | Protocol for pilot RCT |
| Participants | 36 patients with acute neck pain and stiffness |
| Interventions | Acupuncture + massage vs massage |
| Outcomes | NPQ, SF‐MPQ |
| Starting date | ‐‐ |
| Contact information | ‐‐ |
| Notes | ‐‐ |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity (VAS) immediate post treatment Show forest plot | 11 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Acupuncture versus sham treatment, Outcome 1 Pain intensity (VAS) immediate post treatment. | ||||
| 1.1 Chronic MPS 1 treatment session | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Chronic MND 3 to 4 wk treatment | 4 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Chronic MPS 12 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Chronic MND SA group 10 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Cervical osteoarthritis 1 treatment session | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Chronic MPS 3 wk treatment, pain with movement scale | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain intensity (VAS) short term Show forest plot | 8 | 560 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.40, ‐0.07] |
| Analysis 1.2  Comparison 1 Acupuncture versus sham treatment, Outcome 2 Pain intensity (VAS) short term. | ||||
| 2.1 Chronic MPS 3 wk treatment, 3 mo follow‐up, pain with movement scale | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.67, 0.67] |
| 2.2 Chronic MND 3 to 4 wk treatment, 1 to 4 wk follow‐up | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.82, 0.52] |
| 2.3 Chronic MND 3 to 4 wk treatment, 3 mo follow‐up | 3 | 319 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.40, 0.04] |
| 2.4 Subacute/chronic WAD 6 wk treatment, 3 mo follow‐up | 1 | 124 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.73, ‐0.02] |
| 2.5 WAD myofascial 2 to 6 sessions, 6 wk follow‐up | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.29, 0.09] |
| 2.6 Chronic MND SA group 10 wk treatment, 3 wk follow‐up | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐1.11, 0.92] |
| 3 Pain intensity (VAS) intermediate term Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 Acupuncture versus sham treatment, Outcome 3 Pain intensity (VAS) intermediate term. | ||||
| 3.1 Chronic MPS ESNS 3 to 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Chronic WAD 6 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain intensity (VAS) long term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.4 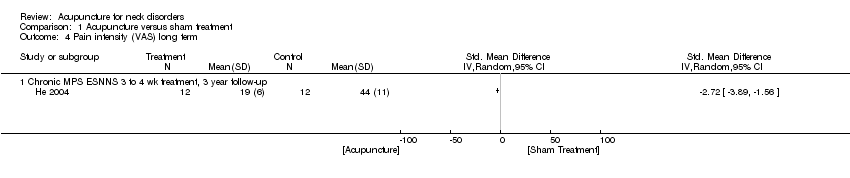 Comparison 1 Acupuncture versus sham treatment, Outcome 4 Pain intensity (VAS) long term. | ||||
| 4.1 Chronic MPS ESNNS 3 to 4 wk treatment, 3 year follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Disability (NDI) immediate post treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 Acupuncture versus sham treatment, Outcome 5 Disability (NDI) immediate post treatment. | ||||
| 5.1 Chronic MND SA group 10 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Disability (NPQ) immediate post treatment Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.6 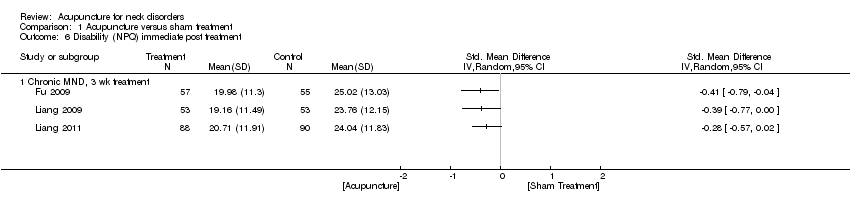 Comparison 1 Acupuncture versus sham treatment, Outcome 6 Disability (NPQ) immediate post treatment. | ||||
| 6.1 Chronic MND, 3 wk treatment | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Disability (NPQ) short term Show forest plot | 2 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.62, ‐0.15] |
| Analysis 1.7 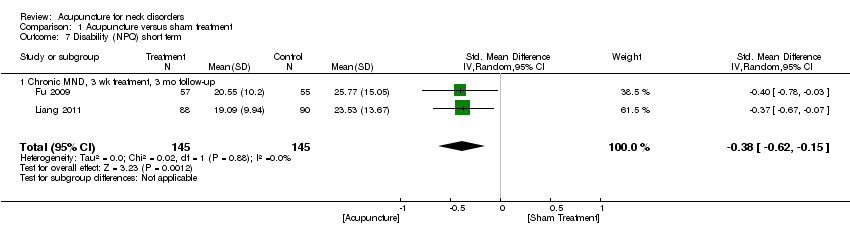 Comparison 1 Acupuncture versus sham treatment, Outcome 7 Disability (NPQ) short term. | ||||
| 7.1 Chronic MND, 3 wk treatment, 3 mo follow‐up | 2 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.62, ‐0.15] |
| 8 Disability (NDI) short term Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.8 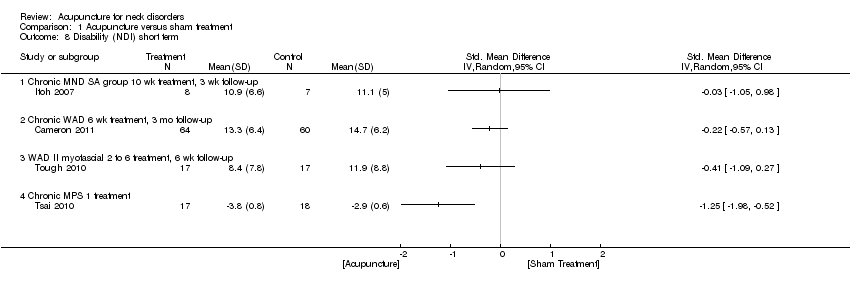 Comparison 1 Acupuncture versus sham treatment, Outcome 8 Disability (NDI) short term. | ||||
| 8.1 Chronic MND SA group 10 wk treatment, 3 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Chronic WAD 6 wk treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 WAD II myofascial 2 to 6 treatment, 6 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Chronic MPS 1 treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Disability (NDI) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.9  Comparison 1 Acupuncture versus sham treatment, Outcome 9 Disability (NDI) intermediate term. | ||||
| 9.1 Chronic WAD 6 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Quality of life (SF‐36) immediate post treatment Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.10  Comparison 1 Acupuncture versus sham treatment, Outcome 10 Quality of life (SF‐36) immediate post treatment. | ||||
| 10.1 Chronic MND, 3 wk treatment | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Quality of life (SF‐36) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.11  Comparison 1 Acupuncture versus sham treatment, Outcome 11 Quality of life (SF‐36) short term. | ||||
| 11.1 Chronic MND, 3 wk treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity (VAS) immediate post treatment Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.1 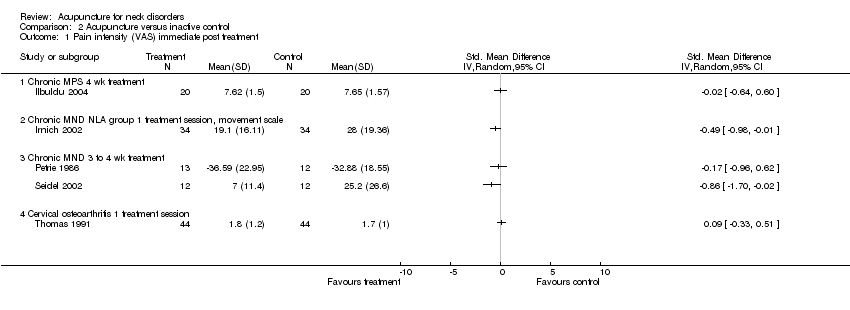 Comparison 2 Acupuncture versus inactive control, Outcome 1 Pain intensity (VAS) immediate post treatment. | ||||
| 1.1 Chronic MPS 4 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Chronic MND NLA group 1 treatment session, movement scale | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Chronic MND 3 to 4 wk treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Cervical osteoarthritis 1 treatment session | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain intensity (VAS) short term Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Acupuncture versus inactive control, Outcome 2 Pain intensity (VAS) short term. | ||||
| 2.1 Chronic MND 3 to 4 wk treatment, 1 to 4 wk follow‐up | 5 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain intensity (VAS) intermediate term Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.3 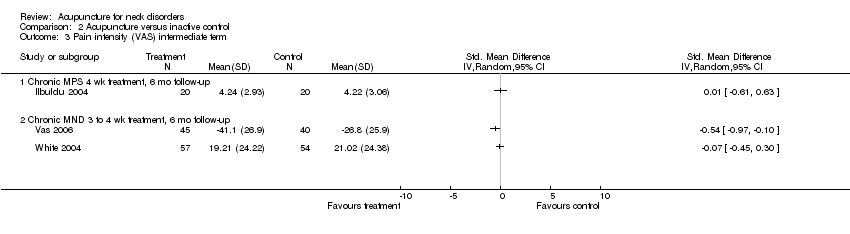 Comparison 2 Acupuncture versus inactive control, Outcome 3 Pain intensity (VAS) intermediate term. | ||||
| 3.1 Chronic MPS 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Chronic MND 3 to 4 wk treatment, 6 mo follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain intensity (VAS) long term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.4  Comparison 2 Acupuncture versus inactive control, Outcome 4 Pain intensity (VAS) long term. | ||||
| 4.1 Chronic MND 3 to 4 wk treatment, 12 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pain pressure threshold immediate post treatment Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.5  Comparison 2 Acupuncture versus inactive control, Outcome 5 Pain pressure threshold immediate post treatment. | ||||
| 5.1 Chronic MND 3 to 4 wk treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Pain pressure threshold short term Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.6 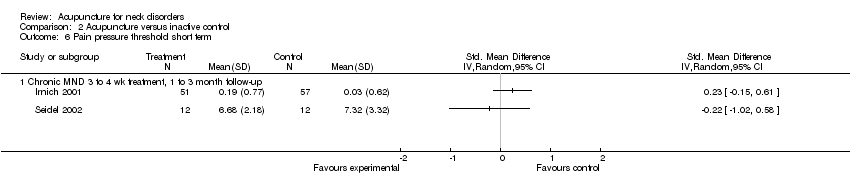 Comparison 2 Acupuncture versus inactive control, Outcome 6 Pain pressure threshold short term. | ||||
| 6.1 Chronic MND 3 to 4 wk treatment, 1 to 3 month follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain intensity (proportion pain relief) immediate post treatment Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 2.7  Comparison 2 Acupuncture versus inactive control, Outcome 7 Pain intensity (proportion pain relief) immediate post treatment. | ||||
| 7.1 Chronic MND 4 wk treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Disability (NDI) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.8 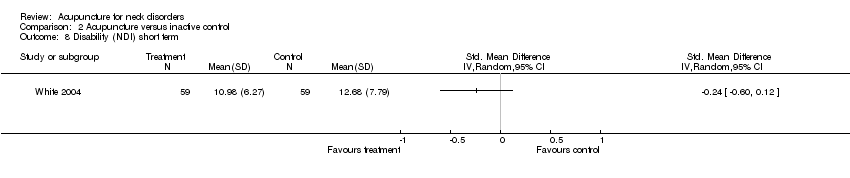 Comparison 2 Acupuncture versus inactive control, Outcome 8 Disability (NDI) short term. | ||||
| 9 Disability (NDI) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.9  Comparison 2 Acupuncture versus inactive control, Outcome 9 Disability (NDI) intermediate term. | ||||
| 9.1 Chronic MND 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Disability (NDI) long term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.10  Comparison 2 Acupuncture versus inactive control, Outcome 10 Disability (NDI) long term. | ||||
| 10.1 Chronic MND 4 wk treatment, 12 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Function (NHP) immediate post treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.11 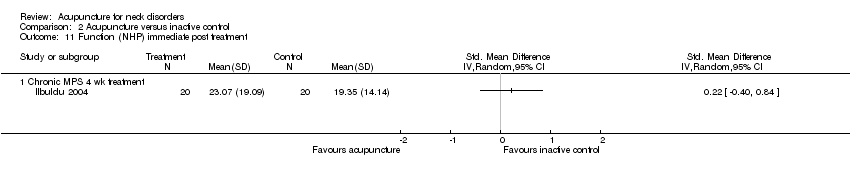 Comparison 2 Acupuncture versus inactive control, Outcome 11 Function (NHP) immediate post treatment. | ||||
| 11.1 Chronic MPS 4 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Function (NHP) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.12  Comparison 2 Acupuncture versus inactive control, Outcome 12 Function (NHP) intermediate term. | ||||
| 12.1 Chronic MPS 4 wk treatment 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Function (NPQ) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.13  Comparison 2 Acupuncture versus inactive control, Outcome 13 Function (NPQ) short term. | ||||
| 13.1 Chronic MND 1 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Quality of life (SF‐36, Functional Component) short term Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.14 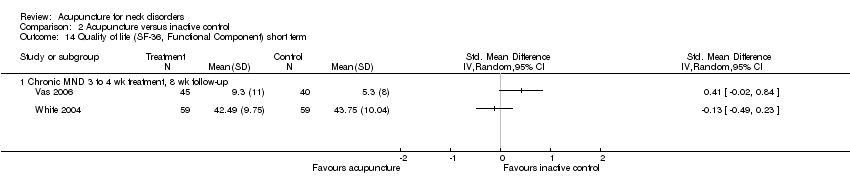 Comparison 2 Acupuncture versus inactive control, Outcome 14 Quality of life (SF‐36, Functional Component) short term. | ||||
| 14.1 Chronic MND 3 to 4 wk treatment, 8 wk follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity (VAS) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 3.1 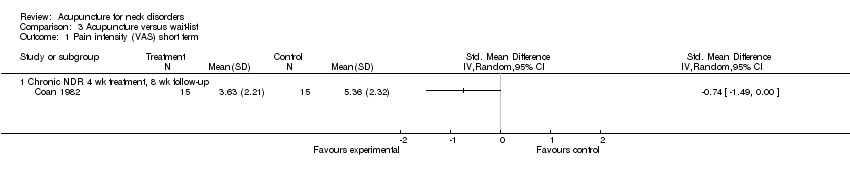 Comparison 3 Acupuncture versus wait‐list, Outcome 1 Pain intensity (VAS) short term. | ||||
| 1.1 Chronic NDR 4 wk treatment, 8 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Disability (neck and pain disability scale) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 3.2  Comparison 3 Acupuncture versus wait‐list, Outcome 2 Disability (neck and pain disability scale) short term. | ||||
| 2.1 Chronic MND 3 mo treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Disability (neck and pain disability scale) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 3.3 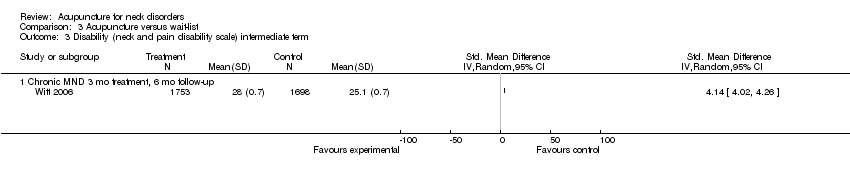 Comparison 3 Acupuncture versus wait‐list, Outcome 3 Disability (neck and pain disability scale) intermediate term. | ||||
| 3.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Quality of life (SF‐36 mental score) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 3.4  Comparison 3 Acupuncture versus wait‐list, Outcome 4 Quality of life (SF‐36 mental score) short term. | ||||
| 4.1 Chronic MND 3 mo treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Quality of life (SF‐36 mental score) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 3.5  Comparison 3 Acupuncture versus wait‐list, Outcome 5 Quality of life (SF‐36 mental score) intermediate term. | ||||
| 5.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Quality of life (SF‐36 physical score) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 3.6  Comparison 3 Acupuncture versus wait‐list, Outcome 6 Quality of life (SF‐36 physical score) intermediate term. | ||||
| 6.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |

Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Acupuncture versus sham treatment, Outcome 1 Pain intensity (VAS) immediate post treatment.

Comparison 1 Acupuncture versus sham treatment, Outcome 2 Pain intensity (VAS) short term.

Comparison 1 Acupuncture versus sham treatment, Outcome 3 Pain intensity (VAS) intermediate term.
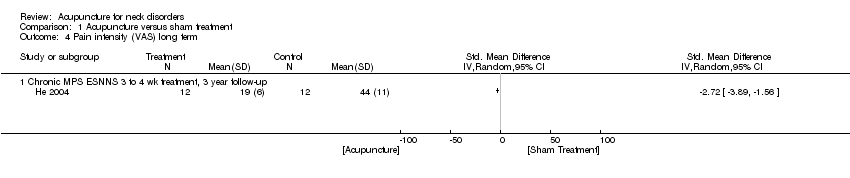
Comparison 1 Acupuncture versus sham treatment, Outcome 4 Pain intensity (VAS) long term.
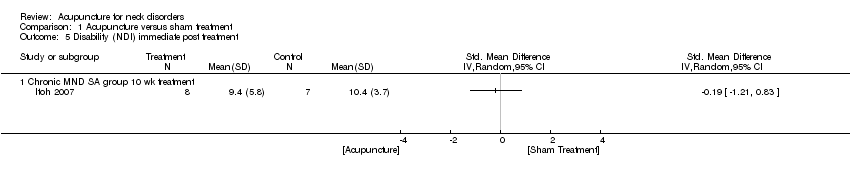
Comparison 1 Acupuncture versus sham treatment, Outcome 5 Disability (NDI) immediate post treatment.

Comparison 1 Acupuncture versus sham treatment, Outcome 6 Disability (NPQ) immediate post treatment.

Comparison 1 Acupuncture versus sham treatment, Outcome 7 Disability (NPQ) short term.

Comparison 1 Acupuncture versus sham treatment, Outcome 8 Disability (NDI) short term.

Comparison 1 Acupuncture versus sham treatment, Outcome 9 Disability (NDI) intermediate term.

Comparison 1 Acupuncture versus sham treatment, Outcome 10 Quality of life (SF‐36) immediate post treatment.

Comparison 1 Acupuncture versus sham treatment, Outcome 11 Quality of life (SF‐36) short term.

Comparison 2 Acupuncture versus inactive control, Outcome 1 Pain intensity (VAS) immediate post treatment.
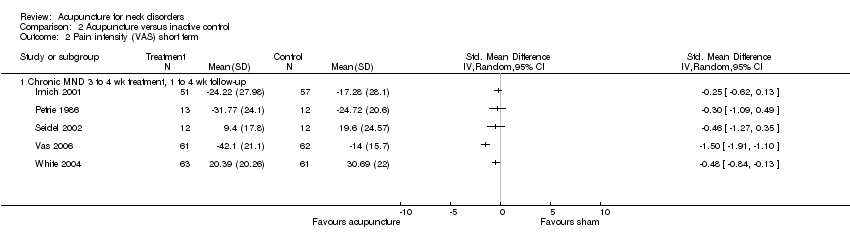
Comparison 2 Acupuncture versus inactive control, Outcome 2 Pain intensity (VAS) short term.

Comparison 2 Acupuncture versus inactive control, Outcome 3 Pain intensity (VAS) intermediate term.
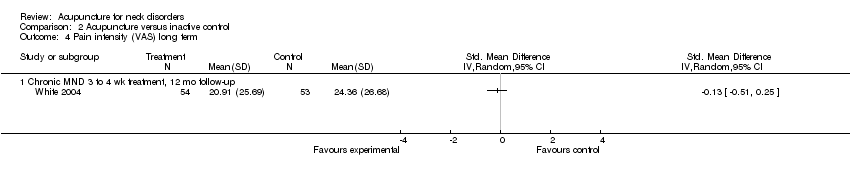
Comparison 2 Acupuncture versus inactive control, Outcome 4 Pain intensity (VAS) long term.

Comparison 2 Acupuncture versus inactive control, Outcome 5 Pain pressure threshold immediate post treatment.
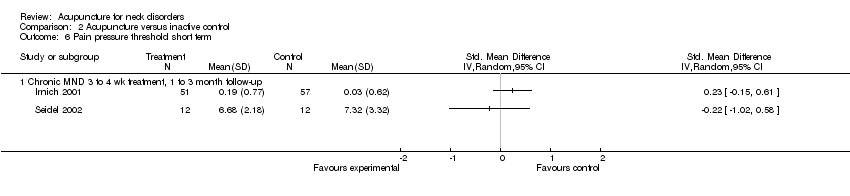
Comparison 2 Acupuncture versus inactive control, Outcome 6 Pain pressure threshold short term.
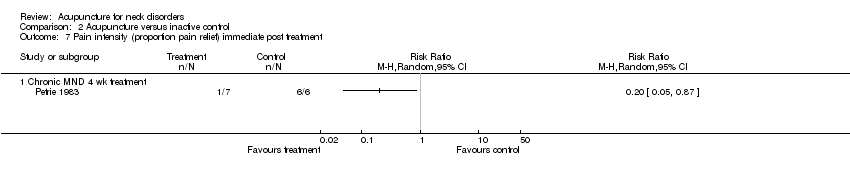
Comparison 2 Acupuncture versus inactive control, Outcome 7 Pain intensity (proportion pain relief) immediate post treatment.
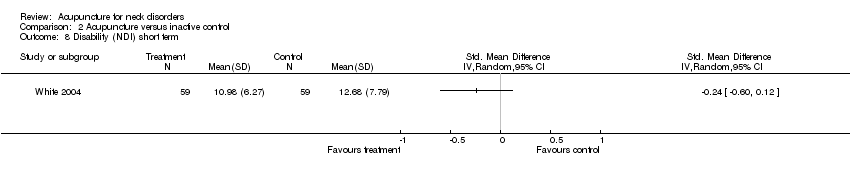
Comparison 2 Acupuncture versus inactive control, Outcome 8 Disability (NDI) short term.

Comparison 2 Acupuncture versus inactive control, Outcome 9 Disability (NDI) intermediate term.

Comparison 2 Acupuncture versus inactive control, Outcome 10 Disability (NDI) long term.
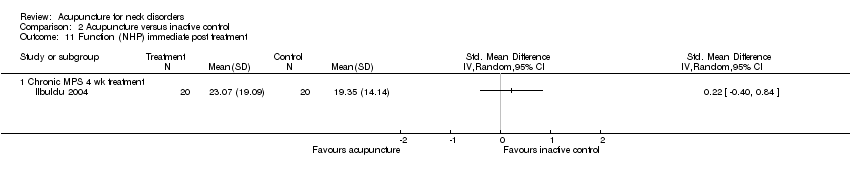
Comparison 2 Acupuncture versus inactive control, Outcome 11 Function (NHP) immediate post treatment.

Comparison 2 Acupuncture versus inactive control, Outcome 12 Function (NHP) intermediate term.
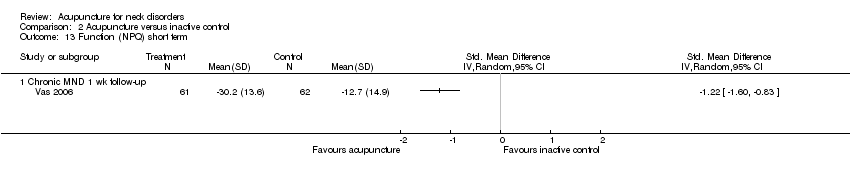
Comparison 2 Acupuncture versus inactive control, Outcome 13 Function (NPQ) short term.

Comparison 2 Acupuncture versus inactive control, Outcome 14 Quality of life (SF‐36, Functional Component) short term.

Comparison 3 Acupuncture versus wait‐list, Outcome 1 Pain intensity (VAS) short term.
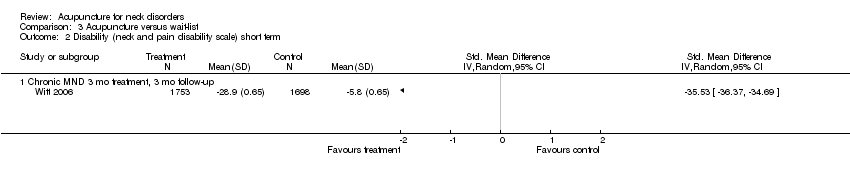
Comparison 3 Acupuncture versus wait‐list, Outcome 2 Disability (neck and pain disability scale) short term.

Comparison 3 Acupuncture versus wait‐list, Outcome 3 Disability (neck and pain disability scale) intermediate term.
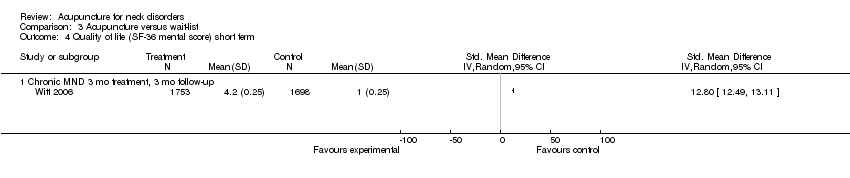
Comparison 3 Acupuncture versus wait‐list, Outcome 4 Quality of life (SF‐36 mental score) short term.

Comparison 3 Acupuncture versus wait‐list, Outcome 5 Quality of life (SF‐36 mental score) intermediate term.

Comparison 3 Acupuncture versus wait‐list, Outcome 6 Quality of life (SF‐36 physical score) intermediate term.
| Acupuncture compared with sham for chronic neck pain | ||||||
| Patient or population: patients with chronic mechanical neck pain (pain for more than 90 days) Settings: varied, mostly at university or hospital clinics Intervention: acupuncture Comparison: sham | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Sham | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity ranged across sham groups from 3 points on a 0 to 10 scale to 47 points on a 0 to 100 scale | Mean pain intensity in intervention groups was 0.23 standard deviations lower (0.20 to 0.07 higher) | ‐0.23 (‐0.20 to ‐0.07) | 560 (8 studies) | ⊕⊕⊕⊝ Limitations: ‐1 Inconsistency: 0 Indirectness: 0 Imprecision: 0 Other: 0 | Statistical pooling was appropriate in this instance because of statistical homogeneity. Results of the meta‐analysis favoured acupuncture |
| Disability (NPQ) short term | Mean disability ranged across control groups from 24 points on a 0 to 100 scale to 26 points on a 0 to 100 scale | Mean disability in intervention groups was | ‐0.38 (‐0.62 to ‐0.15) | 290 (2 studies) | ⊕⊕⊝⊝ Limitations: ‐1 Inconsistency: 0 Indirectness: 0 Imprecision: ‐1 Other: 0 | Two small trials were in favour of acupuncture. On the basis of the GRADE scale, quality level of evidence was downgraded to low because only 1 of the 2 studies (50%) was at low risk with small sample size |
| Disability (NDI) short term | Mean disability ranged across control groups from | Mean disability in intervention groups ranged from | ‐‐ | 173 | N/A | All 3 studies, 2 with low risk of bias, did not show a statistically significant result in favour of acupuncture |
| Quality of life (SF‐36) short term | Mean quality of life across control groups ranged from 86 points on a 0 to 100 scale to 86 points on a 0 to 100 scale | Mean quality of life in intervention groups ranged from 84 points on a 0 to 100 scale to 85 points on a 0 to 100 scale | ‐‐ | 178 (1 study) | ⊕⊕⊝⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: ‐1 Other: 0 | One study with low risk of bias favoured acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies. GRADE Working Group grades of evidence | ||||||
| Acupuncture compared with inactive treatments for chronic neck pain | ||||||
| Patient or population: patients with chronic neck pain (pain for more than 90 days) Settings: primary care, general practitioners' clinics to secondary care, outpatient pain clinics or speciality clinics Intervention: acupuncture Comparison: inactive treatments | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Inactive treatment | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity ranged across control groups from 17 points on a 0 to 100 scale to 31 points on a 0 to 100 scale | Mean pain intensity in intervention groups was 17 points on a 0 to 100 scale to 9 points on a 0 to 10 scale | ‐‐ | 404 (5 studies) | ⊕⊕⊕⊝ Limitations: 0 Inconsistency: 0 Indirectness: 0 Imprecision: ‐1 Other: 0 | Five studies (n = 461) assessed participants with mechanical neck disorders. Four were at low risk of bias. Statistical pooling was inappropriate in this instance because of statistical heterogeneity. Four of these studies favoured acupuncture |
| Pain pressure threshold short term | Mean pain pressure threshold ranged across control groups from 0 points on a 0 to 10 scale to 7 points on a 0 to 10 scale | Mean pain pressure threshold in intervention groups ranged from 0.2 points on a 0 to 10 scale to 7 points on a 0 to 10 scale | ‐‐ | 132 (2 studies) | N/A | Two studies with low risk of bias did not favour acupuncture |
| Disability (NDI) short term Function (NPQ) short term | Mean disability ranged across control groups from 12 points on a 0 to 100 scale to 13 points on a 0 to 100 scale Mean function across control groups was 13 points on a 0 to 100 scale | Mean disability in intervention groups ranged from Mean function in intervention groups was 30 points on a 0 to 100 scale | ‐‐ | 118 (1 study) 123 (1 study) | N/A ⊕⊕⊝⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: ‐1 Other: 0 | One study with low risk of bias did not favour acupuncture One study with low risk of bias favoured acupuncture |
| Quality of life (SF‐36, Functional Component) short term | Mean function ranged across control groups from 0.7 points on a 0 to 10 scale to 5 points on a 0 to 10 scale | Mean function in intervention groups ranged from 41 points on a 0 to 100 scale to 9 points on a 0 to 10 scale | ‐‐ | 143 (2 studies) | N/A | Two studies with low risk of bias did not favour acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies. GRADE Working Group grades of evidence | ||||||
| Acupuncture compared with wait‐list control for chronic neck pain | ||||||
| Patient or population: patients with chronic neck pain (pain for more than 90 days) Settings: primary care newspaper advertisement or recruited through participating physicians Intervention: acupuncture Comparison: wait‐list control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Wait‐list control | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity across control groups was 5 points on a 0 to 10 scale | Mean pain intensity in intervention groups was | ‐‐ | 30 (1 study) | ⊕⊕⊕⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: 0 Other: 0 | One trial with low risk of bias showed a small reduction in pain. Moderate evidence supporting acupuncture is helpful |
| Disability (neck and pain disability scale) short term | Mean disability across control groups was | Mean disability in intervention groups was 29 points on a 0 to 100 scale | ‐‐ | 3451 (1 study) | ⊕⊕⊕⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: 0 Other: 0 | One large study with low risk of bias favoured acupuncture |
| Quality of life (SF‐36 mental score) short term | Mean quality of life score across control groups was | Mean quality of life score in intervention groups was 4 points on a 0 to 10 scale | ‐‐ | 3451 (1 study) | N/A | One large study showed no statistically significant findings in favour of acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies Cost of care was calculated in 1 study, which found that acupuncture treatment was cost‐effective GRADE Working Group grades of evidence | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity (VAS) immediate post treatment Show forest plot | 11 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Chronic MPS 1 treatment session | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Chronic MND 3 to 4 wk treatment | 4 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Chronic MPS 12 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Chronic MND SA group 10 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Cervical osteoarthritis 1 treatment session | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Chronic MPS 3 wk treatment, pain with movement scale | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain intensity (VAS) short term Show forest plot | 8 | 560 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.40, ‐0.07] |
| 2.1 Chronic MPS 3 wk treatment, 3 mo follow‐up, pain with movement scale | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.67, 0.67] |
| 2.2 Chronic MND 3 to 4 wk treatment, 1 to 4 wk follow‐up | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.82, 0.52] |
| 2.3 Chronic MND 3 to 4 wk treatment, 3 mo follow‐up | 3 | 319 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.40, 0.04] |
| 2.4 Subacute/chronic WAD 6 wk treatment, 3 mo follow‐up | 1 | 124 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.73, ‐0.02] |
| 2.5 WAD myofascial 2 to 6 sessions, 6 wk follow‐up | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.29, 0.09] |
| 2.6 Chronic MND SA group 10 wk treatment, 3 wk follow‐up | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐1.11, 0.92] |
| 3 Pain intensity (VAS) intermediate term Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Chronic MPS ESNS 3 to 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Chronic WAD 6 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain intensity (VAS) long term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Chronic MPS ESNNS 3 to 4 wk treatment, 3 year follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Disability (NDI) immediate post treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chronic MND SA group 10 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Disability (NPQ) immediate post treatment Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Chronic MND, 3 wk treatment | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Disability (NPQ) short term Show forest plot | 2 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.62, ‐0.15] |
| 7.1 Chronic MND, 3 wk treatment, 3 mo follow‐up | 2 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.62, ‐0.15] |
| 8 Disability (NDI) short term Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Chronic MND SA group 10 wk treatment, 3 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Chronic WAD 6 wk treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 WAD II myofascial 2 to 6 treatment, 6 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Chronic MPS 1 treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Disability (NDI) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Chronic WAD 6 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Quality of life (SF‐36) immediate post treatment Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Chronic MND, 3 wk treatment | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Quality of life (SF‐36) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Chronic MND, 3 wk treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity (VAS) immediate post treatment Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Chronic MPS 4 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Chronic MND NLA group 1 treatment session, movement scale | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Chronic MND 3 to 4 wk treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Cervical osteoarthritis 1 treatment session | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain intensity (VAS) short term Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Chronic MND 3 to 4 wk treatment, 1 to 4 wk follow‐up | 5 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain intensity (VAS) intermediate term Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Chronic MPS 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Chronic MND 3 to 4 wk treatment, 6 mo follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain intensity (VAS) long term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Chronic MND 3 to 4 wk treatment, 12 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pain pressure threshold immediate post treatment Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chronic MND 3 to 4 wk treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Pain pressure threshold short term Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Chronic MND 3 to 4 wk treatment, 1 to 3 month follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain intensity (proportion pain relief) immediate post treatment Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Chronic MND 4 wk treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Disability (NDI) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9 Disability (NDI) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Chronic MND 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Disability (NDI) long term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Chronic MND 4 wk treatment, 12 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Function (NHP) immediate post treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Chronic MPS 4 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Function (NHP) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Chronic MPS 4 wk treatment 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Function (NPQ) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 Chronic MND 1 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Quality of life (SF‐36, Functional Component) short term Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Chronic MND 3 to 4 wk treatment, 8 wk follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity (VAS) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Chronic NDR 4 wk treatment, 8 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Disability (neck and pain disability scale) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Chronic MND 3 mo treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Disability (neck and pain disability scale) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Quality of life (SF‐36 mental score) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Chronic MND 3 mo treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Quality of life (SF‐36 mental score) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Quality of life (SF‐36 physical score) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |

