목 통증의 침 치료
초록
배경
목 통증은 3대 근골격계 질환 중 하나로 꼽힌다. 목 통증 치료법은 다양하며, 각 치료법의 효과에 대한 인식 역시 편차가 크다. 침 치료는 근골격계 통증의 기존 치료법에 대한 대안으로 사용되어 왔다. 이 리뷰에서는 급성, 아급성, 만성 목 통증의 침 치료 효과에 대한 가장 최신의 과학적 근거를 요약하였다. 이번 리뷰는 동일한 주제에 대한 2006년의 코크란 리뷰를 갱신한 것이다.
목적
목 통증이 있는 성인 환자를 대상으로 통증 경감과 장애 또는 기능 측정, 환자 만족도 그리고 환자가 느낀 전반적인 효과에 대한 침 치료 효과를 알아보기 위함.
검색 전략
6개의 데이터베이스 (센트럴(CENTRAL), 메드라인(MEDLINE), 엠베이스(EMBASE), 맨티스(MANTIS), 시날(CINAHL), 아이씨엘(ICL)) (최초 자료 등록일부터 2015년 8월까지의 자료)과 참고문헌 목록, 2개의 임상시험 등록부, 중국의 침 치료 데이터베이스인 TCMLARS (2005년까지의 자료)를 검색하였다.
선정 기준
전문 또는 초록 형태로 보고된 무작위 대조 연구를 분석대상으로 하였다. 유사‐무작위 대조 연구는 연구 대상에서 제외하였다.
자료 수집 및 분석
두 명의 리뷰 저자가 연구 선정, 자료 추출, 연구 방법론의 품질 평가 측면에서 각각 독립적 분석을 수행하였다. 코크란 허리 리뷰 그룹의 ‘바이어스 위험’ 도구를 이용하여 연구의 품질을 평가하였다. 리뷰 저자들의 의견이 엇갈릴 경우 합의 과정을 거쳤다. 임상적 이질성이 없을 경우, 변량 효과 모형을 이용하여 연구들을 메타‐분석하였다.
주요 결과
27건의 임상시험 중 3건은 급성과 만성 환자(참가자 205명)를 포함한 편타 손상 관련 질환 에 대한 연구였으며, 5건은 만성의 근막 목 통증 (참가자 186명)에 대한 연구였고, 5건은 관절 변화가 동반된 만성 통증 (참가자 542명), 6건은 만성 단순 목 통증 (참가자 4011명), 2건은 방사통이 있는 목 통증 (참가자 43명), 6건은 아급성 또는 만성 기계적 목 통증(참가자 5111명) 에 대한 연구였다.
기계적 원인의 목 통증의 경우, 침 치료를 아래와 같은 경우와 비교하였을 때 더 효과가 좋았다.
1) 일련의 치료 과정을 마친 직후 거짓 침 치료와 비교하였을 때 통증 강도 면에서.
2) 단기간 추적 관찰에서 거짓 또는 비활성 치료와 비교하였을 때 통증 강도 면에서.
3) 단기간 추적 관찰에서 거짓 침 치료와 비교하였을 때 장애 면에서.
4)단기간 추적 관찰에서 치료를 하지 않는 것과 비교하였을 때 통증 강도와 목의 장애 개선 면에서. 침 치료를 거짓 침 치료와 비교하였을 때 단기간의 결과 지표에 대하여 통계적인 이질성은 발견되지 않아, 결과의 통계적 합성은 가능했다 (P value = 0.83; I2 = 20%). 메타 분석 결과는 침 치료가 효과 있음을 보여주었다 (SMD ‐0.23, 95% CI ‐0.20 to ‐0.07; P value = 0.0006). 이 효과는 장기간 관찰에서는 지속되지 않는 것으로 보인다.순차적인 반복 치료가 성공적일지에 대해 조사한 임상시험은 없었다.
이상 반응이 경미하였기에, 침 치료는 안전한 치료 기법으로 보인다. 보고된 이상반응으로는 통증 증가, 멍, 실신, 증상 악화, 국소적 부기, 그리고 어지럼이 있었다. 모든 임상시험에서 치명적인 이상반응은 보고되지 않았으며, 침 치료가 비용‐대비 효과적이었다고 보고했다.
첫 번째 리뷰 출간 이후, 무작위 대조 연구의 품질이 개선되었으며, 이들 중 많은 연구들은 바이어스 위험이 낮았다. 그러나 높은 품질의 증거에 기여할 수 있는 대규모 임상시험은 거의 수행되지 않았다.
연구진 결론
침 치료가 거짓 침 치료에 비해 치료 완료 직후 및 단기간 추적 관찰 시 통증 경감에 효과적이며, 침 치료를 받은 환자가 치료 받지 않은 환자들에 비해 단기간 추적 관찰에서 통증과 장애가 덜하다는 중간 품질의 증거가 있다. 또한 단기간 추적 관찰에서 침 치료가 비활성 치료에 비해 통증 경감에 더 효과적이라는 중간 품질의 증거가 있다.
쉬운 말 요약
목 통증의 침 치료
연구 질문
목 통증과 관련된 기능, 장애, 환자 만족도, 환자가 느끼는 전반적인 효과 측면에서 침 치료의 효과에 대한 증거를 분석했다.
연구 배경
목 통증은 3대 근골격계 질환 중 하나로 꼽힌다. 치료법은 다양하며, 각 치료법의 효과에 대한 인식 역시 편차가 크다. 침 치료는 근골격계 통증의 기존 치료법에 대한 대안으로 종종 사용되어 왔다. 이 연구에서 침 치료란 몸의 특정 지점에 침을 꽂아 자극하여 치료 효과를 나타내기 위한 방법을 말한다. 침은 보통 손으로 자극하지만, 전기자극이나 온침 자극 (침 손잡이에 쑥을 붙여 태워 뜸 치료를 병행하는 방법) 등의 응용법도 흔히 사용된다. 한약 추출물을 경혈에 주입하는 약침도 때때로 활용한다.
연구의 특징
이 연구에서는 며칠 지속되거나 또는 적어도 3개월 이상 된 급성 또는 만성 목 통증에 대한 침 치료 효과를 연구한 27개 임상시험 (참가자 5,462명) 을 분석하였다. 침 치료는 거짓 침, 치료를 제공하지 않는 경과 관찰, 거짓 레이저와 같은 다른 형태의 비활성 치료 등과 비교되었다. 2015년 8월까지 수집된 증거를 분석했다.
핵심 연구 결과
각 임상시험에 참여한 환자 특성, 사용된 침 치료 기법, 결과 평가 방식의 차이 때문에, 결과 합성을 통한 침 치료 효과의 개괄은 하지 못했다. 따라서, 이 연구에서는 제한적인 결론을 낼 수 밖에 없었다.
만성 목 통증 환자 중 침 치료를 받은 사람은 거짓 침 치료를 받은 사람에 비해, 치료 직후 및 치료 후 짧은 기간 동안 통증이 더 많이 완화되었다. 또한 치료를 받지 않은 사람에 비해, 치료 후 짧은 기간 동안 더 많은 통증 완화와 장애 개선을 보였다.
침 치료는 안전한 것으로 보이며, 임상시험 연구자들은 단지 경미하고 짧게 나타나는 부작용을 보고했다.
증거의 품질
침 치료가 도움이 되는지 판단하기 위한 증거는 낮음 또는 중간 품질이었다. 적은 참가자 수, 임상시험에서 탈락한 이들에 대해 추적하지 않는 경향, 연구 참여자의 무작위 배정이 제대로 이루어졌음을 확실히 하지 않은 점 등이 증거의 제한점이다. 이와 같은 결점들은 연구에 바이어스를 유발하며 결과의 신뢰성에 영향을 미친다.
Authors' conclusions
Summary of findings
| Acupuncture compared with sham for chronic neck pain | ||||||
| Patient or population: patients with chronic mechanical neck pain (pain for more than 90 days) Settings: varied, mostly at university or hospital clinics Intervention: acupuncture Comparison: sham | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Sham | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity ranged across sham groups from 3 points on a 0 to 10 scale to 47 points on a 0 to 100 scale | Mean pain intensity in intervention groups was 0.23 standard deviations lower (0.20 to 0.07 higher) | ‐0.23 (‐0.20 to ‐0.07) | 560 (8 studies) | ⊕⊕⊕⊝ Limitations: ‐1 Inconsistency: 0 Indirectness: 0 Imprecision: 0 Other: 0 | Statistical pooling was appropriate in this instance because of statistical homogeneity. Results of the meta‐analysis favoured acupuncture |
| Disability (NPQ) short term | Mean disability ranged across control groups from 24 points on a 0 to 100 scale to 26 points on a 0 to 100 scale | Mean disability in intervention groups was | ‐0.38 (‐0.62 to ‐0.15) | 290 (2 studies) | ⊕⊕⊝⊝ Limitations: ‐1 Inconsistency: 0 Indirectness: 0 Imprecision: ‐1 Other: 0 | Two small trials were in favour of acupuncture. On the basis of the GRADE scale, quality level of evidence was downgraded to low because only 1 of the 2 studies (50%) was at low risk with small sample size |
| Disability (NDI) short term | Mean disability ranged across control groups from | Mean disability in intervention groups ranged from | ‐‐ | 173 | N/A | All 3 studies, 2 with low risk of bias, did not show a statistically significant result in favour of acupuncture |
| Quality of life (SF‐36) short term | Mean quality of life across control groups ranged from 86 points on a 0 to 100 scale to 86 points on a 0 to 100 scale | Mean quality of life in intervention groups ranged from 84 points on a 0 to 100 scale to 85 points on a 0 to 100 scale | ‐‐ | 178 (1 study) | ⊕⊕⊝⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: ‐1 Other: 0 | One study with low risk of bias favoured acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies. GRADE Working Group grades of evidence | ||||||
| Acupuncture compared with inactive treatments for chronic neck pain | ||||||
| Patient or population: patients with chronic neck pain (pain for more than 90 days) Settings: primary care, general practitioners' clinics to secondary care, outpatient pain clinics or speciality clinics Intervention: acupuncture Comparison: inactive treatments | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Inactive treatment | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity ranged across control groups from 17 points on a 0 to 100 scale to 31 points on a 0 to 100 scale | Mean pain intensity in intervention groups was 17 points on a 0 to 100 scale to 9 points on a 0 to 10 scale | ‐‐ | 404 (5 studies) | ⊕⊕⊕⊝ Limitations: 0 Inconsistency: 0 Indirectness: 0 Imprecision: ‐1 Other: 0 | Five studies (n = 461) assessed participants with mechanical neck disorders. Four were at low risk of bias. Statistical pooling was inappropriate in this instance because of statistical heterogeneity. Four of these studies favoured acupuncture |
| Pain pressure threshold short term | Mean pain pressure threshold ranged across control groups from 0 points on a 0 to 10 scale to 7 points on a 0 to 10 scale | Mean pain pressure threshold in intervention groups ranged from 0.2 points on a 0 to 10 scale to 7 points on a 0 to 10 scale | ‐‐ | 132 (2 studies) | N/A | Two studies with low risk of bias did not favour acupuncture |
| Disability (NDI) short term Function (NPQ) short term | Mean disability ranged across control groups from 12 points on a 0 to 100 scale to 13 points on a 0 to 100 scale Mean function across control groups was 13 points on a 0 to 100 scale | Mean disability in intervention groups ranged from Mean function in intervention groups was 30 points on a 0 to 100 scale | ‐‐ | 118 (1 study) 123 (1 study) | N/A ⊕⊕⊝⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: ‐1 Other: 0 | One study with low risk of bias did not favour acupuncture One study with low risk of bias favoured acupuncture |
| Quality of life (SF‐36, Functional Component) short term | Mean function ranged across control groups from 0.7 points on a 0 to 10 scale to 5 points on a 0 to 10 scale | Mean function in intervention groups ranged from 41 points on a 0 to 100 scale to 9 points on a 0 to 10 scale | ‐‐ | 143 (2 studies) | N/A | Two studies with low risk of bias did not favour acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies. GRADE Working Group grades of evidence | ||||||
| Acupuncture compared with wait‐list control for chronic neck pain | ||||||
| Patient or population: patients with chronic neck pain (pain for more than 90 days) Settings: primary care newspaper advertisement or recruited through participating physicians Intervention: acupuncture Comparison: wait‐list control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Wait‐list control | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity across control groups was 5 points on a 0 to 10 scale | Mean pain intensity in intervention groups was | ‐‐ | 30 (1 study) | ⊕⊕⊕⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: 0 Other: 0 | One trial with low risk of bias showed a small reduction in pain. Moderate evidence supporting acupuncture is helpful |
| Disability (neck and pain disability scale) short term | Mean disability across control groups was | Mean disability in intervention groups was 29 points on a 0 to 100 scale | ‐‐ | 3451 (1 study) | ⊕⊕⊕⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: 0 Other: 0 | One large study with low risk of bias favoured acupuncture |
| Quality of life (SF‐36 mental score) short term | Mean quality of life score across control groups was | Mean quality of life score in intervention groups was 4 points on a 0 to 10 scale | ‐‐ | 3451 (1 study) | N/A | One large study showed no statistically significant findings in favour of acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies Cost of care was calculated in 1 study, which found that acupuncture treatment was cost‐effective GRADE Working Group grades of evidence | ||||||
Background
Description of the condition
Neck pain is a common health impairment among individuals of all ages in the general population (Cote 2004; Haldeman 2008; Hogg‐Johnson 2008; Miller 2010). In fact, according to Haldeman 2008, “most people can expect to experience some degree of neck pain in their lifetime”. The prevalence of neck pain in adults over a 12‐month period ranges from 30% to 50% (Carroll 2008; Hogg‐Johnson 2008). Furthermore, neck pain is a commonly recurring condition. Neck pain appears to be episodic in nature and therefore frequently recurs in 50% to 80% of people one to five years after a prior incident (Carroll 2008; Cote 2004). Symptoms of neck pain range from mildly discomforting to severely disabling and can interfere with daily activities and quality of life. Moreover, incidents of neck pain can be associated with headache, arm pain or even neurological or sensory deficits (Haldeman 2008). Neck pain has a substantial impact on healthcare costs; the economic burden of neck pain is widespread because it affects patients, insurers, governments and employers through sick leave, disability, visits to healthcare providers and loss of productivity (Haldeman 2008; Haraldsson 2006; Miller 2010).
Description of the intervention
A variety of conventional treatments are used to address neck pain, including massage, physiotherapy, exercise, muscle relaxants and steroid injections (Fu 2009SR; Haraldsson 2006; Irnich 2001). Acupuncture has been used increasingly as an alternative to more conventional treatment for musculoskeletal pain. It is defined as stimulation of a certain point or points on the body by insertion of needles to achieve a therapeutic effect. Acupuncture typically includes manual stimulation of needles, but variations are commonly used, such as electrical and heat stimulation of needles, which is called moxibustion (the moxa herb Artemisia vulgaris is burned at the handle end of the needle).
How the intervention might work
Research evidence indicates that acupuncture involves the release of neurotransmitters and hormones such as endorphins (Han 2004), serotonin (Zhang 2012) and adenosine triphosphate (ATP) (Goldman 2010).
Best evidence suggests that the release of β‐endorphin triggered by acupuncture acts both as a neurotransmitter involved in central descending pain inhibitory pathways and as a hormone released into the blood flow. In addition, evidence indicates that central release of dynorphines and the expression level of the opioid antagonist cholecystokinin octapeptide (CCK‐8) (Tang 1997) may play a role in central mechanisms of acupuncture‐induced analgesia. In the peripheral nervous system, β‐endorphin seems to be released from keratinocytes when activated by increased extracellular endocannabinoid concentrations after acupuncture in an inflammatory pain model (Chen 2009).
Likewise, serotonin is known to be involved in the analgesic effect of acupuncture by affecting transmission of pain signals at central and peripheral levels. Similar to oestrogen, serotonin seems to be indirectly involved in the antinociceptive effect of acupuncture by sensitising peripheral afferents and thereby activating endogenous pain control. In contrast, an increase in extracellular ATP concentration may act directly on afferent neurons expressing purinergic receptors, leading to nerve fibre activation, which in turn causes antinociceptive spinal or supraspinal reactions.
Such mechanisms of endogenous pain control triggered by Aδ‐ and C‐fiber activation are generally distinguished according to the respective neural structures and neurotransmitters involved and are termed diffuse noxious inhibitory control (DNIC), segmental inhibition and descending pain control pathways (Zhao 2008).
Effects of acupuncture on muscles and fascia have also been described (Langevin 2006). When effects of acupuncture are approached from the perspective of mechanical tissue manipulation, it can be concluded that existing evidence shows effects of acupuncture on structure and alignment of connective tissue or fasciae (Langevin 2006). Conversely, a reduction in muscle tone through acupuncture has been proposed, but this proposal is based mainly on observations of clinical improvement after acupuncture, such as increased cervical range of motion in patients with neck pain (Irnich 2001). Moreover, recent brain imaging studies have revealed that acupuncture alters brain activation patterns in areas associated with pain processing (Huang 2012SR).
Why it is important to do this review
According to several existing reviews, including our own (Trinh 2006), moderate‐quality evidence indicates that acupuncture is effective in the short term for relieving neck pain (Fu 2009; Furlan 2012; Graham 2013; Gross 2007; Vernon 2009). Randomised controlled trials (RCTs) included in these reviews were based on small population samples (Irnich 2011; Linde 2007), and more recent studies are likely to have used improved methods.
Given the heavy public health and economic burden caused by neck pain and the fact that many sufferers consult complementary and alternative medicine practitioners for relief of their symptoms, a systematic review with new and updated evidence of these practices was justified. The purpose of this review was to include more recent studies in an effort to reveal updated evidence for the use of acupuncture to relieve neck pain and to examine long‐term effects that were absent from previous studies. This review summarises the most current scientific evidence on the effectiveness of acupuncture for acute, subacute and chronic neck pain.
Objectives
To determine the effects of acupuncture for adults with neck pain, with focus on pain relief, disability or functional measures, patient satisfaction and global perceived effect.
Methods
Criteria for considering studies for this review
Types of studies
We included published randomised controlled trials (RCTs) in full text or abstract form. We included abstracts if sufficient information for analyses could be obtained from study authors. We excluded quasi‐RCTs and clinical controlled trials (CCTs) because we found numerous RCTs for this update. This is different from the approach presented in the protocol.
Types of participants
Participants were adults (18 years or older) with the following neck disorders.
-
Mechanical neck disorders (MNDs), including whiplash‐associated disorders (WADs) categories 1 and 2 (Spitzer 1987; Spitzer 1995), myofascial pain syndrome (MPS) and degenerative changes (DCs) (Schumacher 1993).
-
Neck disorder with headache (Olesen 1988; Olesen 1997; Sjaastad 1990).
-
Neck disorders with radicular symptoms (NDRs), including WAD category 3 (Spitzer 1987; Spitzer 1995).
For the purposes of this review, we defined symptom duration as acute (< 30 days), subacute (30 days to 90 days) or chronic (≥ 90 days).
We excluded studies if they investigated neck disorders with:
-
definite or possible long tract signs (e.g. myelopathies);
-
neck pain caused by other pathological entities (Schumacher 1993);
-
neck pain related to neurological disease (e.g. spasmodic torticollis);
-
neck pain related to fracture and dislocation;
-
headache not of cervical origin;
-
co‐existing headache when neck pain was not dominant or when headache was not provoked by neck movement or sustained neck posture; or
-
'mixed' headache.
Types of interventions
Studies must have used acupuncture techniques involving insertion of needles. Stimulation of needles may involve manual, electrical, heat, laser or other forms of stimulation. Control groups were treated with sham acupuncture (some form of mock or pretend), wait‐list control or inactive treatment control (e.g. sham transcutaneous electrical nerve stimulation (TENS)).
Types of outcome measures
Primary outcomes
Pain relief (e.g. visual analogue scale (VAS), numerical rating scale (NRS)), disability or functional measures (e.g. Neck Disability Index (NDI), quality of life (e.g. Short Form (SF)‐36), activities of daily living (ADLs)), patient satisfaction questionnaires and global perceived effect were the outcomes of interest.
Secondary outcomes
When available, we examined adverse effects and costs of treatment.
The duration of the follow‐up period was defined as:
-
immediately post treatment: up to one day;
-
short‐term follow‐up: between one day and three months;
-
intermediate‐term follow‐up: longer than three months to less than one year; or
-
long‐term follow‐up: one year and longer.
Search methods for identification of studies
Electronic searches
We searched the following databases from their inception to August 2015.
-
Cochrane Central Register of Controlled Trials (CENTRAL, which includes the Cochrane Back Review Group (CBRG) Trials Register; Ovid, August 2015).
-
MEDLINE (Ovid, 1950 to August 2015 week 4).
-
EMBASE (Ovid, 1980 to August 2015).
-
Manual, Alternative and Natural Therapy Indexing System (MANTIS; Ovid, 1980 to November 2013 last available access date).
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCO, 1982 to August 2015).
-
Index to Chiropractic Literature (ICL; August 2015).
-
ClinicalTrials.gov (August 2015).
-
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (August 2015).
The Chinese Cochrane Centre searched the Traditional Chinese Medical Literature Analysis and Retrieval System (TCMLARS) in China in September 2005. We did not further update the TCMLARS search, as this search yielded no RCTs previously.
See Appendix 1 for the search strategies used for CENTRAL, MEDLINE, EMBASE, MANTIS, CINAHL and ICL. Subject headings (MeSHs) and keywords included anatomical terms, disorder or syndrome terms, treatment terms and methodological terms consistent with those advised by the CBRG (Furlan 2009).
Searching other resources
We also screened references, communicated with the Trials Search Co‐ordinator of the CBRG, contacted identified content experts and reviewed our own personal files.
Data collection and analysis
We used standard methodological procedures as expected by The Cochrane Collaboration and the CBRG.
Selection of studies
At least two review authors independently identified citations, selected studies and abstracted data. We resolved disagreements through consensus.
If additional information was required to assess the appropriateness of a study for selection, we contacted study authors for clarification. If this was not forthcoming, we allowed a consensus process to determine selection status. If the article or citation posting was written in a non‐English language, one investigator and a translator with a health sciences background conducted study selection in an unblinded manner.
Data extraction and management
Two review authors independently extracted raw data for demographics, descriptions of treatment and all outcomes from full manuscripts onto pre‐designed forms.
Using the Chi2 test, we calculated agreement between investigators for study identification, selection and validity processes before reaching consensus (Graham 2012). We used the quadratic weighted kappa statistic (Kw) (Cicchetti 1976) to measure agreement.
Assessment of risk of bias in included studies
At least two review authors independently assessed each selected study for methodological quality using pre‐piloted forms based on the CBRG risk of bias (RoB) assessment tool (12 criteria) (Furlan 2009). See Appendix 2 for operationalisation of the RoB tool. We rated each item as having high, low or unclear risk and entered ratings into the RoB table. A consensus team met to reach a final assessment based on an overview of RoB items; we used no pre‐defined cutoff score for the RoB assessment. We deemed an RCT acceptable for inclusion if we found no fatal methodological flaws (e.g. randomisation, allocation concealment, drop‐outs, intention‐to‐treat (ITT) analyses were done appropriately and were well reported).
Measures of treatment effect
We used descriptive statistics to provide a summary description of groups, interventions, outcomes, adverse effects of treatment and costs of care. We reported results on the basis of the sample size analysed.
We calculated standardised mean differences (SMDs) and 95% confidence intervals (95% CIs) for outcomes reported in a continuous data format. We used the SMD because different measures were frequently used to address the same clinical outcome. Effect size (SMD) is a unitless measure reported in standard deviation units. Generally, effect size can be interpreted as small (‐0.20), medium (‐0.50) or large (‐0.80), as defined by Cohen (Cohen 1988).
For dichotomous outcomes, we calculated risk ratios (RRs) and 95% CIs for outcome rates in the treatment versus control group. For undesirable outcomes, RR less than one represents a beneficial treatment.
When neither continuous nor dichotomous data were available, we extracted findings and statistical significance as reported by authors of the original study and noted them in the Characteristics of included studies tables.
Unit of analysis issues
For clinical trials using a simple parallel‐group design, we collected from each participant and analysed a single measurement for each outcome. For clinical trials using a cross‐over design, we collected from each participant and analysed measurements of each outcome for each participant from each of the interventions. We analysed only the first phase of the cross‐over study and included no cluster‐randomised trials in this review.
Dealing with missing data
When data were not extractable, we contacted the primary authors.
When neither continuous nor dichotomous data were available, we extracted findings and presented statistical significance as reported by study authors.
Assessment of heterogeneity
We considered the following possible sources of heterogeneity: symptom duration (acute vs chronic); subtype of neck pain (e.g. WAD); intervention type (traditional acupuncture vs trigger point needling); characteristics of treatment (e.g. dosage, technique); and outcomes (pain relief, measures of function and disability, patient satisfaction, quality of life).
A P value for the Chi2 test (test of heterogeneity) less than 0.05 or an I2 value greater than 25% would indicate significant statistical heterogeneity. However, because an acupuncture review includes few studies, the test of heterogeneity might not have the power to detect a difference even when one exists; therefore, we determined that subgroups were statistically heterogeneous if I2 values were greater than 25% despite failure to reject the null hypothesis with the Chi2 test.
Assessment of reporting biases
When a published protocol was available, we compared outcomes reported a priori with outcomes of interest in the RCT.
Data synthesis
Before calculating a pooled effect measure, we assessed the appropriateness of pooling on clinical grounds. We planned to combine outcome measures from individual trials by performing a meta‐analysis when possible (clinical comparability of populations, interventions and outcomes between trials). We planned to use a random‐effects model for these meta‐analyses.
We considered each subgroup (e.g. 1.1) to be clinically homogeneous. We meta‐analysed each subgroup unless we noted statistical heterogeneity. When a meta‐analysis was not possible, we described qualitatively in the text the results of clinically comparable trials.
Regardless of whether available data were sufficient for use in quantitative analyses to summarise the data, we assessed the overall quality of the evidence for each outcome. To accomplish this, we used the GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) approach, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) and adapted in the updated CBRG method guidelines (Furlan 2009). We considered that the following factors may decrease the quality of the evidence, study design and risk of bias, inconsistency of results, indirectness (not generalisable), imprecision (sparse data) and other factors (e.g. reporting bias). We reduced our rating of the quality of the evidence for a specific outcome by one level according to the performance of studies against these five factors.
-
High‐quality evidence: Findings are consistent among at least 75% of RCTs with low risk of bias; consistent, direct and precise data; and no known or suspected publication bias. Further research is unlikely to change the estimate or our confidence in the results.
-
Moderate‐quality evidence: One of the domains is not met. Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
-
Low‐quality evidence: Two domains are not met. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
-
Very low‐quality evidence: Three domains are not met. We are very uncertain about the results.
-
No evidence: We identified no RCTs that addressed this outcome.
Subgroup analysis and investigation of heterogeneity
We did not plan to perform a subgroup analysis.
Sensitivity analysis
We planned to conduct a sensitivity analysis on risks of bias or meta‐regression by type of neck pain and duration of symptoms. However, we did not find sufficient data for any of these categories.
Results
Description of studies
We selected 27 trials (N = 5462) for inclusion in this review (Figure 1). Duration of the disorder and disorder subtypes were as follow.

Study flow diagram.
-
Acute and subacute WAD (n = 1) (Tough 2010).
-
Subacute and chronic WAD (n = 2) (Cameron 2011; Kwak 2012).
-
Chronic myofascial neck pain (n = 5) (Birch 1998; Chou 2009; Ilbuldu 2004; Sun 2010; Tsai 2010).
-
Chronic pain due to osteoarthritic cervical degenerative changes (n = 5) (Fu 2009; Liang 2009; Thomas 1991; White 2000; White 2004).
-
Chronic non‐specific neck pain (n = 6) (He 2004; He 2005; Itoh 2007; Nabeta 2002; Vas 2006; Witt 2006).
-
Neck pain with radicular findings (n = 2) (Coan 1982; Petrie 1983).
-
Subacute or chronic mechanical neck pain (n = 6) (Irnich 2001; Irnich 2002; Liang 2011; Petrie 1986; Sahin 2010; Seidel 2002).
Results of the search
We identified and screened 1562 citation postings and retrieved 154 studies for more detailed evaluation. We included 27 RCTs in this review (Figure 1). We identified no RCTs through the Chinese language search. Additionally, five studies were protocols (Calamita 2015; Kim 2014; Liang 2012; Que 2013; Sun 2014) and two were conference proceeding abstracts (Amos 2012; Liguori 2012) that are awaiting assessment. One study is awaiting translation (Simma‐Kletscha 2009), and four further studies are awaiting completion (Bar‐Haim 2012; Cerezo‐Tellez 2014; Choi 2011; Guo 2014). We found three studies that provided additional analyses for the primary study (see Witt 2006). We found four studies after analysis was complete; these are also awaiting assessment (Mejuto‐Vázquez 2014; Sterling 2015; Wilke 2014; Zhang SP 2013).
See Characteristics of included studies tables for additional details on study design, numbers randomised/analysed, treatments selected, co‐interventions provided, absolute benefits noted, results reported, SMDs, RRs, ITT analyses, side effects and costs of care. Agreement between pairs of independent review authors from diverse professional backgrounds regarding inclusion of studies was excellent, with an estimated Kw = 0.9425 (standard error 0.020).
Included studies
Of the 27 included studies, three represented individuals with WAD (205 participants), five chronic myofascial neck pain (186 participants), five chronic pain due to arthritic changes (n = 506), six chronic non‐specific neck pain (4011 participants), two neck pain with radicular signs (43 participants) and six subacute or chronic mechanical neck pain (511 participants).
Excluded studies
We excluded 103 trials after reviewing the full report. Of these, we excluded 13 studies on the basis of participant characteristics: Two RCTs included participants with a neck disorder excluded from this review (i.e. ankylosing spondylitis) (Emery 1986) and spinal cord stenosis (Li 2006); three included headaches not of cervical origin (Coeytaux 2005; Venancio 2008; Venancio 2009); seven included participants with pain from other areas as well (head, shoulder or back) (Gallacchi 1981; Gallacchi 1983; Gaw 1975; Giles 2003; Kisiel 1996; Lundeburg 1988; Muller 2005); and one included participants who did not have neck pain (Sato 2014). Furthermore, we excluded two abstracts (Johnson 2000; Teng 1973) because they did not appear to describe RCTs. We excluded 64 studies on the basis of the comparison performed: Six studies included acupuncture as the control (Fernandez‐Carnero 2014; Guo 2013; Harvey 2015; Li 2013; Wang G 2014; Zhang J 2013); 31 compared acupuncture types (Ceccherelli 2006; Ceccherilli 2014; Dong 2012; Fu 2007; Gil 2015; Huang 2008; Jia 2007; Jin 2012; Kai 2008; Li 2004; Liu 2008; Lixing 2000; Lu 2006; Myburgh 2012; Nakajima 2015; Pecos‐Martin 2015; Sator‐Katzenschlager 2003; Shang 2002; Shuangquan 2003; Sun 2013; Wan 2013; Wang 2007; Wang 2008; Xu 2012; Yang 2009; Yoon 2009; Yu 2003; Zeng 2005; Zhao 2004; Zhu 2006; Zhuang 2004); 27 compared acupuncture versus active treatment (Bahadir 2009; Cho 2014; David 1998; Edwards 2003; Eroglu 2013; Falkenberg 2007; Franca 2008; Fu 2005; Fu 2014; Ga 2007b; Giles 1999; Hu 2014; Huang 2012; Hudson 2010; Li 2006; Liu 2013; MacPherson 2013; McLean 2013; Rayegani 2014; Salter 2006; Tobbackx 2013; Yang 2013; Yoshimizu 2012; Zhang 2003; Zhang J 2008; Zhou 2014; Ziaeifar 2014). In addition, we excluded 15 RCTs on the basis of the intervention provided: eight by type (i.e. EMG needle, mini‐scalpel, injection needle) (Calvo‐Trujillo 2013; Chu 1997; Lin 2004; Ma 2010; Seo 2014; Zhang X‐Z 2013; Zheng 2014; Zhi 2008) and seven additional studies that used acupuncture as part of a multi‐modal approach (Cohen 2014; Gallego Sendarrubias 2015; Guanygue 2001; Hayek 2014; Hudson 2010; Lundeburg 1991; Soderlund 2001) and could not isolate the acupuncture effect. We excluded eight studies because they were not randomised or were quasi‐randomised (Ga 2007a; Hua 2009; Loy 1983; Luo 2010; Pan 2008; Peng 1987; Xue 2007; Zhang 1996). We excluded one study because investigators did not perform between‐group comparisons (Zhu 2002). (See Characteristics of excluded studies tables.)
Risk of bias in included studies
We assessed methodological quality using CBRG guidelines (Furlan 2009). Please see Figure 2 for these results. We assessed 12 of the 27 included studies (44%) as having fatal flaws, including selection, performance, attrition (related to lack of ITT principles) and reporting biases. Other potential sources of bias included inadequate reporting of co‐interventions and participant compliance.
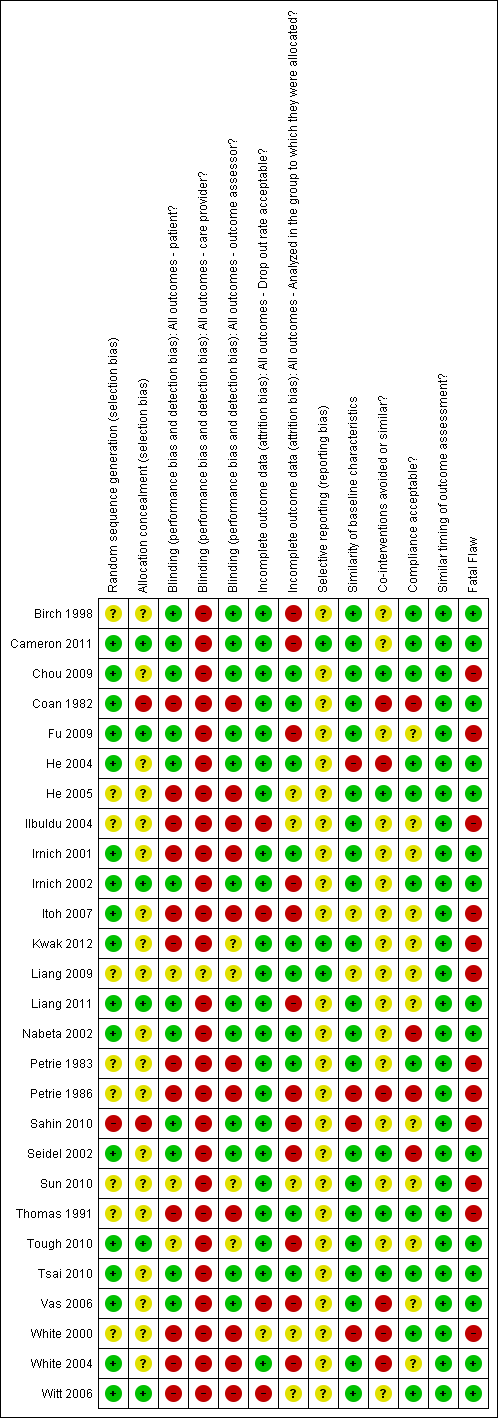
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We found that six of the 27 included studies had low risk of bias on the basis of allocation; 19 had uncertain risk of bias; and two had high risk of bias. We discussed effects of risks of bias on review results for each subgroup separately under Effects of interventions.
Blinding
We found that 12 of the 27 included studies had low risk of bias on blinding of participants; 12 studies had uncertain risk of bias, and three had high risk of bias. We discussed effects of risks of bias on review results for each subgroup separately under Effects of interventions.
Incomplete outcome data
We found that two of the 27 included studies had low risk of bias on drop‐out rate; four studies had uncertain risk of bias, and one had high risk of bias. We discussed effects of risks of bias on review results for each subgroup separately under Effects of interventions.
Selective reporting
We found that three of the 27 included studies had low risk of bias; 24 studies had uncertain risk of bias, and no study had high risk of bias. We discussed effects of risks of bias on review results for each subgroup separately under Effects of interventions.
Other potential sources of bias
We assessed 12 of the 27 included studies (44%) as having fatal flaws, including selection, performance, attrition (related to lack of ITT principles) and reporting biases. Other potential sources of bias included inadequate reporting of co‐interventions and participant compliance.
Effects of interventions
See: Summary of findings for the main comparison ; Summary of findings 2 ; Summary of findings 3
Acupuncture versus sham acupuncture
Pain intensity (VAS) post treatment
Eleven studies (n = 712) included participants with mechanical neck disorders or myofascial pain syndrome. Eight of these eleven studies favoured acupuncture over sham acupuncture. One study (Sahin 2010) did not favour acupuncture. However, this study had a fatal methodological flaw involving randomisation issues and the small number of participants recruited compared with the number of participants needed for its sample size calculation. This study was terminated early and is considered to have high risk of bias. Itoh 2007 studied two methods of acupuncture compared with sham acupuncture. The trigger point treatment was significantly different from sham, and the standard acupuncture treatment was not significantly different from sham. We considered this study to have high risk of bias. Thomas 1991, a study with high risk of bias, also did not favour acupuncture for individuals with osteoarthritis.
These studies involved various methods of sham acupuncture or pretend acupuncture treatments. In some studies, sham group needles did not penetrate the skin (Chou 2009; Itoh 2007). Some studies defined their sham treatments as superficial needle insertions (Fu 2009; Sun 2010; Thomas 1991; Tsai 2010); three studies use a sham control group for whom needles were placed at some distance (1 to 2 cm) from the acupuncture points (He 2004; Liang 2011; Sahin 2010) or in a remote dermatome (White 2000). Birch 1998 used predetermined irrelevant points in his control group.
We considered five of these 11 studies to have low risk of bias (Birch 1998; Chou 2009; He 2004; Liang 2011; Tsai 2010) and six studies to have high risk of bias (Fu 2009; Itoh 2007; Sahin 2010; Sun 2010; Thomas 1991; White 2000).
Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.00001; I2 = 83%). Moderate‐quality evidence suggests that acupuncture is beneficial for individuals with chronic mechanical neck pain for pain intensity immediately following treatment. (Please see Analysis 1.1.) On the basis of the GRADE scale, we downgraded the quality level of evidence to moderate because only five of the 11 studies (46%) presented low risk.
Pain intensity (VAS) short term
We assigned eight studies (n = 560) (Cameron 2011; Fu 2009; Liang 2011; Nabeta 2002; Sahin 2010; Sun 2010; Tough 2010; Itoh 2007) to this category. (Please see Analysis 1.2.) Statistical pooling was appropriate in this instance because of statistical homogeneity (P value = 0.83; I2 = 0%). Results of the meta‐analysis favoured acupuncture (P value = 0.006). We considered four studies (Fu 2009; Itoh 2007; Sahin 2010; Sun 2010) to have high risk of bias. On the basis of the GRADE scale, we downgraded the quality level to moderate because only four of the eight studies (50%) presented low risk.
Pain intensity (VAS) intermediate term
Two studies (n = 158) presented low risk of bias: one involving participants with whiplash (Cameron 2011) and the other involving participants with mechanical neck disorders (He 2004). Both studies favoured acupuncture. (Please see Analysis 1.3.) Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.06; I2 = 71%). On the basis of the GRADE scale, we downgraded the quality level of evidence to moderate as the result of imprecision.
Pain intensity (VAS) long term
One study (n = 24) with low risk of bias involved participants with mechanical neck disorders (He 2004). This study favoured acupuncture. (Please see Analysis 1.4.)
Disability and quality of life
No convincing evidence favoured acupuncture in all other measures such as disability (NDI) or quality of life over the short term, the intermediate term or the long term. (Please see Analysis 1.5, Analysis 1.6, Analysis 1.7, Analysis 1.8, Analysis 1.9, Analysis 1.10, and Analysis 1.11.) Statistical pooling for Analysis 1.6 and Analysis 1.8 were inappropriate in this instance because of heterogeneity.
Some evidence suggests that acupuncture may be more beneficial than sham acupuncture for disability (Northwick Park Pain Questionnaire (NPQ)). Two studies (n = 290) involved participants with mechanical neck disorders, one with low risk of bias (Liang 2011) and the other with high risk of bias (Fu 2009). Meta‐analysis favoured acupuncture (P value = 0.001). (Please see Analysis 1.7.) Statistical pooling was appropriate in this instance because of statistical homogeneity (P value = 0.88; I2 = 0%). On the basis of the GRADE scale, we downgraded the quality level of evidence to moderate because only one of the two studies (50%) presented low risk.
Acupuncture versus inactive treatment
Pain intensity (VAS) immediate post treatment
We assigned five studies (n = 245) to this category (Ilbuldu 2004; Irnich 2002; Petrie 1986; Seidel 2002; Thomas 1991). We considered two of these studies (Irnich 2002; Seidel 2002) to have low risk of bias and three to have high risk of bias (Ilbuldu 2004; Petrie 1986; Thomas 1991). Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.20; I2 = 33%). Most of these studies ‐ four of the five ‐ did not favour acupuncture (Ilbuldu 2004; Petrie 1986; Seidel 2002; Thomas 1991). (Please see Analysis 2.1.)
Pain intensity (VAS) short term
Five studies (n = 404) (Irnich 2001; Petrie 1986; Seidel 2002; Vas 2006; White 2004) assessed participants with mechanical neck disorders. Petrie 1986 found no differences between groups (Petrie 1986). Another study compared acupuncture versus sham laser and reported no differences (Irnich 2001). However, Vickers 2004 used regression analysis and adjusted for baseline pain in re‐analysing this study (Vickers 2004) and showed that acupuncture resulted in a 9.4‐point greater reduction in pain over sham laser (0.9 to 18.0 points; P value = 0.031). Another study compared acupuncture versus sham laser (Seidel 2002) and showed statistically significant results favouring acupuncture at four‐week follow‐up. One study compared acupuncture versus sham electroacupuncture stimulator and yielded positive results at one‐week follow‐up, but these results were not sustained at eight‐week follow‐up (White 2004). Vas and colleagues also favoured acupuncture over inactive treatment (Vas 2006).
Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.0001; I2 = 83%). We considered four of these studies (Irnich 2001; Seidel 2002; Vas 2006; White 2004) to have low risk of bias and one study (Petrie 1986) (n = 26) to have high risk of bias.
On the basis of the GRADE scale, we determined that evidence should be rated as high quality because criteria such as design, limitations, inconsistency of results, indirectness, imprecision and other factors were met. However, because of the small sample size of these studies, it is highly possible that future research may change the estimate or our confidence in the results. Therefore, we downgraded the quality level of evidence to moderate. Moderate‐quality evidence suggests that acupuncture is beneficial for individuals with chronic mechanical neck pain for pain intensity at short‐term follow‐up. (Please see Analysis 2.2.)
Pain intensity (VAS) intermediate term
Three studies (n = 318) assessed participants with mechanical neck disorders (Vas 2006; White 2004) or myofascial pain syndrome (Ilbuldu 2004). One of these studies favoured acupuncture over inactive treatment (Vas 2006). We considered two of these studies (Vas 2006; White 2004) to have low risk of bias. Statistical pooling was inappropriate in this instance because of statistical heterogeneity (P value = 0.21; I2 = 36%).
Low‐quality evidence suggests that acupuncture is beneficial for individuals with chronic mechanical neck pain for pain intensity at intermediate‐term follow‐up. We downgraded the quality of evidence because of risk of bias (< 75% of the studies presented low risk) and inconsistency of results. (Please see Analysis 2.3.)
Pain intensity (VAS) long term
We considered White 2004 (n = 124) to have low risk of bias; this study did not favour acupuncture treatment. No evidence suggests that acupuncture is effective for long‐term pain relief. (Please see Analysis 2.4.)
Disability and quality of life
No convincing evidence favoured acupuncture in all other measures such as disability (NDI) and quality of life over the short term, the intermediate term or the long term. (Please see Analysis 2.5, Analysis 2.6, Analysis 2.7, Analysis 2.8, Analysis 2.9, Analysis 2.10, Analysis 2.11, Analysis 2.12, Analysis 2.13 and Analysis 2.14.) Statistical pooling for Analysis 2.5, Analysis 2.6 and Analysis 2.14 were inappropriate in this instance because of heterogeneity.
Acupuncture versus wait‐list control
Pain intensity (VAS) at short‐term follow‐up
One study (n = 30) involving participants with mechanical neck disorders with radicular symptoms (Coan 1982) favoured acupuncture for short‐term pain relief. This study had low risk of bias. However, no evidence suggests that this improvement was sustained to intermediate follow‐up. (Please see Analysis 3.1.)
Disability and quality of life
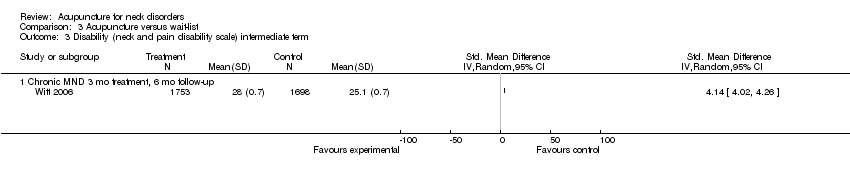
One study (n = 3766) involving participants with mechanical neck disorders (Witt 2006) favoured acupuncture for short‐term NDI improvement. This study had low risk of bias, but no evidence suggests that this improvement was sustained to intermediate follow‐up. (Please see Analysis 3.2.)
No convincing evidence favoured acupuncture in all other measures such as quality of life over the short term or the intermediate term regarding physical or mental scores (SF‐36). In fact, some evidence suggests that results favoured control on the basis of a single study in each category. (Please see Analysis 3.3, Analysis 3.4, Analysis 3.5 and Analysis 3.6.)
Fourteen studies reported adverse effects (Cameron 2011; Fu 2009; Irnich 2001; Irnich 2002; Itoh 2007; Kwak 2012; Liang 2011; Nabeta 2002; Seidel 2002; Sun 2010; Tough 2010; Vas 2006; White 2004; Witt 2006), which included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. (See Characteristics of included studies table for full details.) These studies noted no life‐threatening adverse effects.
One large multi‐centre trial reported costs of care (Witt 2006) and indicated that acupuncture is cost‐effective.
For a summary of results, please see summary of findings Table for the main comparison, summary of findings Table 2 and summary of findings Table 3.
Discussion
Summary of main results
For mechanical neck pain, we found that acupuncture is more beneficial at immediate‐term follow‐up compared with sham treatments for pain intensity; at short‐term follow‐up compared with sham treatments and inactive treatments for pain intensity; at short term follow‐up compared with sham treatments for disability (Northwick Park Pain Questionnaire (NPQ)) and at short‐term follow‐up compared with wait‐list control for pain intensity and Neck Disability Index (NDI) improvement. Effects do not seem sustainable over the long term. Our primary studies did not examine whether subsequent repeated sessions will be successful.
Overall completeness and applicability of evidence
In this review, we limited our trials to include acupuncture interventions in the experimental arm and no acupuncture interventions in the control arm. Control arms could be given sham acupuncture, an inactive treatment or no treatment. In this way, we could better study the effects of acupuncture. Our challenge remains determining what constitutes acupuncture treatments. In other Cochrane reviews such as acupuncture for back pain, acupuncture is defined as treatment that uses some type of standardised acupuncture points, whereas dry needling is treatment that uses acupuncture needles over trigger points. We found insufficient studies on dry needling alone to justify separating this needling treatment method for examination in a separate review.
We found that the number of acupuncture treatment sessions was associated with outcomes (Ezzo 2000). Ideally, treatment should consist of six or more acupuncture sessions. One study (Irnich 2002) intentionally studied the effects of a single treatment. Five studies provided underdosing with fewer than six treatment sessions (Chou 2009; Ilbuldu 2004; Nabeta 2002; Tsai 2010; Vas 2006). All remaining studies were adequately dosed on the basis of this variable alone.
Quality of the evidence
The most difficult challenge faced in this review was clinical heterogeneity, which appeared at many levels, as in sample group included, acupuncture interventions provided and outcomes measured. Acupuncture interventions and sham therapies were quite varied. Among sham therapies, treatment varied from a non‐insertion type of inactivated transcutaneous electrical nerve stimulation (TENS) or laser to insertion of needles at different locations or at different depths. The qualitative method of synthesising evidence has its limitations. We determined consistency of evidence by group consensus, but this method is sensitive to how studies are categorised because meeting the criteria for a certain level of evidence depends on the number of studies included within a category.
Fortunately, the quality of acupuncture studies for neck pain seems to have improved over time. We classified many studies identified in the latest update of our search as having low risk of bias.
Potential biases in the review process
Weaknesses of this review rest with limitations in the primary studies. Furthermore, many studies did not report details of drop‐outs. We avoided language bias by including all languages during study selection; however, we did not search non‐English language databases, and we did not search Chinese databases beyond 2005.
Our approach to summarising the literature has several strengths. We used a comprehensive, librarian‐assisted search of multiple databases. We relied on teams of healthcare professionals to decide on article relevance and to assess study quality. At least two review authors extracted data, and the principal investigator verified data entry. We used a group consensus approach, coupled with the Cochrane Back Review Group risk of bias assessment tool. We avoided professional bias inherent in having members of a single profession evaluate the literature for that profession.
Agreements and disagreements with other studies or reviews
Our findings are similar to those of our past review in 2006 (Trinh 2006) and to those of Fu et al in 2009 (Fu 2009). This is consistent with other reviews on acupuncture for migraine headache prophylaxis (Linde 2009), elbow pain (Trinh 2004), tension headache (Linde 2009a) and back pain (Furlan 2005). The result is not surprising. The findings of our review of other therapies for neck disorders were disappointing. It appears that the effect size of treatments for neck disorders is small even for therapies (such as injections) believed to have a large clinical effect. It is likely that in a clinical setting, both specific and non‐specific effects of treatments are evident, whereas in a randomised controlled trial (RCT), investigators observe non‐specific effects of treatments in both experimental and control groups. Therefore, the difference is seen in the specific effects of treatment, and these effects may be smaller than those observed clinically.
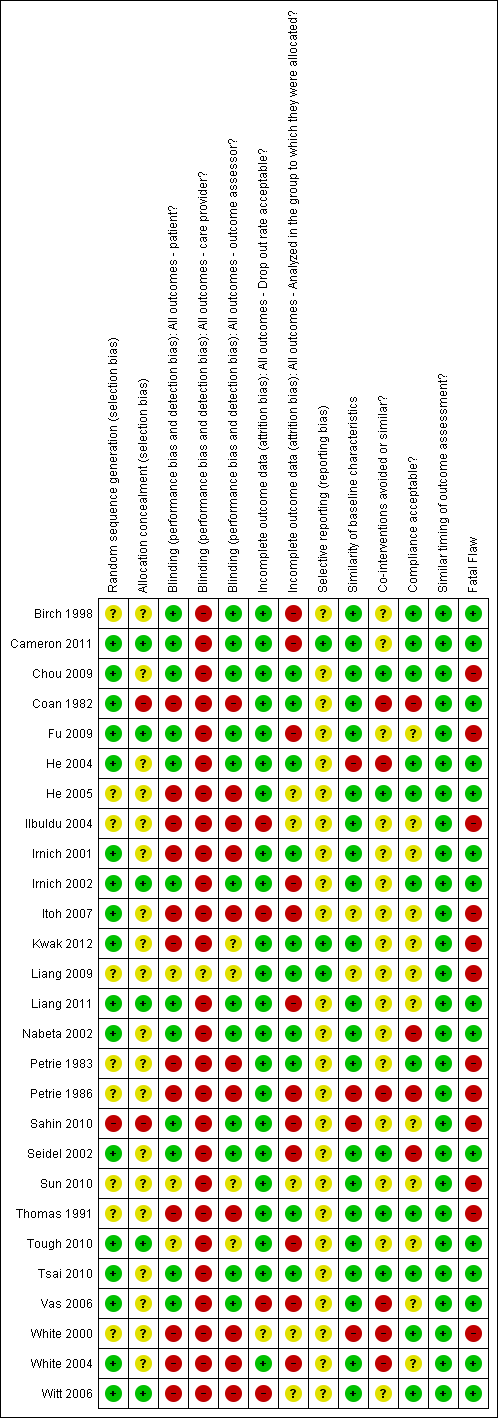
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Acupuncture versus sham treatment, Outcome 1 Pain intensity (VAS) immediate post treatment.

Comparison 1 Acupuncture versus sham treatment, Outcome 2 Pain intensity (VAS) short term.

Comparison 1 Acupuncture versus sham treatment, Outcome 3 Pain intensity (VAS) intermediate term.
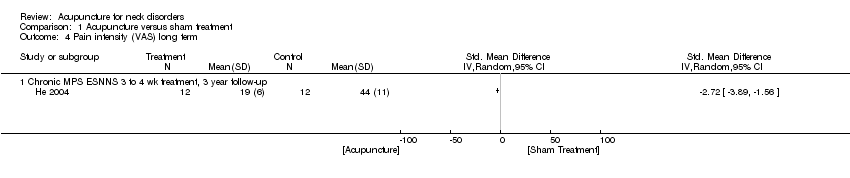
Comparison 1 Acupuncture versus sham treatment, Outcome 4 Pain intensity (VAS) long term.

Comparison 1 Acupuncture versus sham treatment, Outcome 5 Disability (NDI) immediate post treatment.
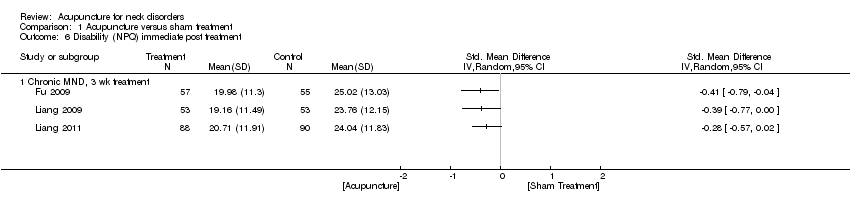
Comparison 1 Acupuncture versus sham treatment, Outcome 6 Disability (NPQ) immediate post treatment.
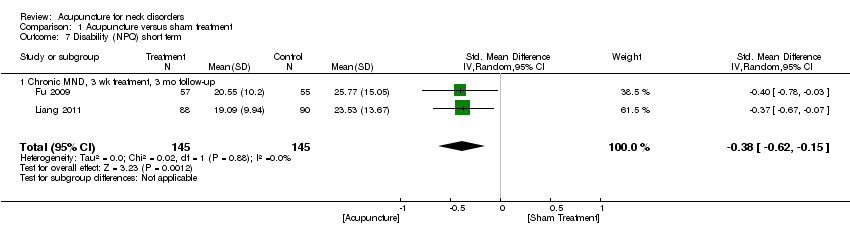
Comparison 1 Acupuncture versus sham treatment, Outcome 7 Disability (NPQ) short term.
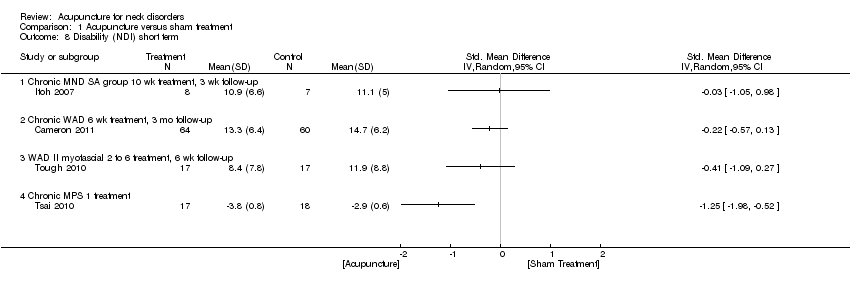
Comparison 1 Acupuncture versus sham treatment, Outcome 8 Disability (NDI) short term.

Comparison 1 Acupuncture versus sham treatment, Outcome 9 Disability (NDI) intermediate term.

Comparison 1 Acupuncture versus sham treatment, Outcome 10 Quality of life (SF‐36) immediate post treatment.

Comparison 1 Acupuncture versus sham treatment, Outcome 11 Quality of life (SF‐36) short term.
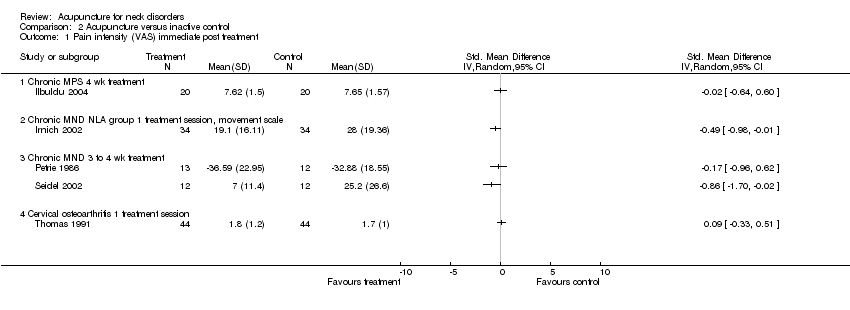
Comparison 2 Acupuncture versus inactive control, Outcome 1 Pain intensity (VAS) immediate post treatment.

Comparison 2 Acupuncture versus inactive control, Outcome 2 Pain intensity (VAS) short term.
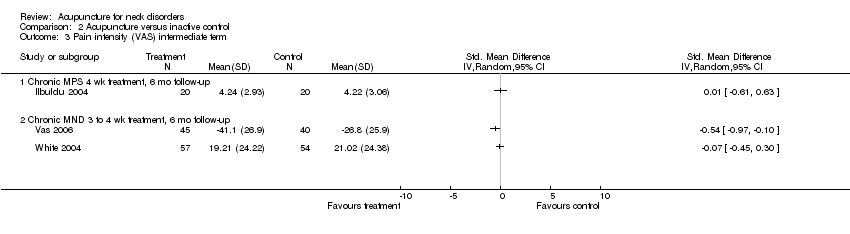
Comparison 2 Acupuncture versus inactive control, Outcome 3 Pain intensity (VAS) intermediate term.

Comparison 2 Acupuncture versus inactive control, Outcome 4 Pain intensity (VAS) long term.

Comparison 2 Acupuncture versus inactive control, Outcome 5 Pain pressure threshold immediate post treatment.
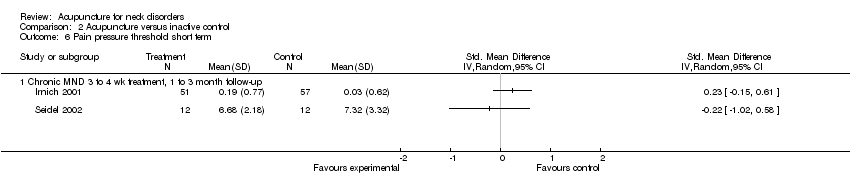
Comparison 2 Acupuncture versus inactive control, Outcome 6 Pain pressure threshold short term.

Comparison 2 Acupuncture versus inactive control, Outcome 7 Pain intensity (proportion pain relief) immediate post treatment.
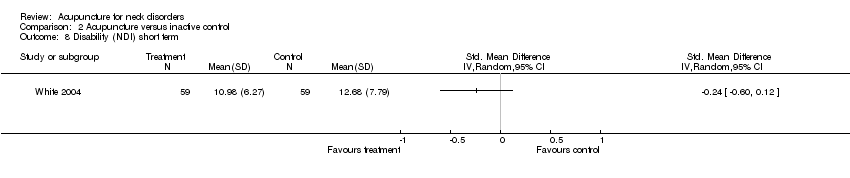
Comparison 2 Acupuncture versus inactive control, Outcome 8 Disability (NDI) short term.

Comparison 2 Acupuncture versus inactive control, Outcome 9 Disability (NDI) intermediate term.

Comparison 2 Acupuncture versus inactive control, Outcome 10 Disability (NDI) long term.
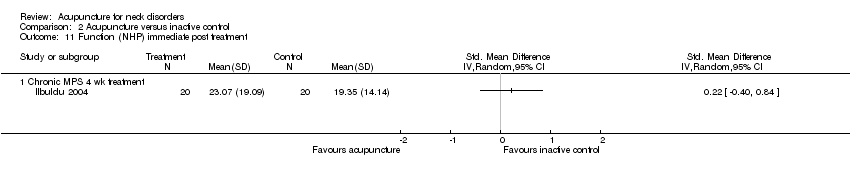
Comparison 2 Acupuncture versus inactive control, Outcome 11 Function (NHP) immediate post treatment.

Comparison 2 Acupuncture versus inactive control, Outcome 12 Function (NHP) intermediate term.

Comparison 2 Acupuncture versus inactive control, Outcome 13 Function (NPQ) short term.
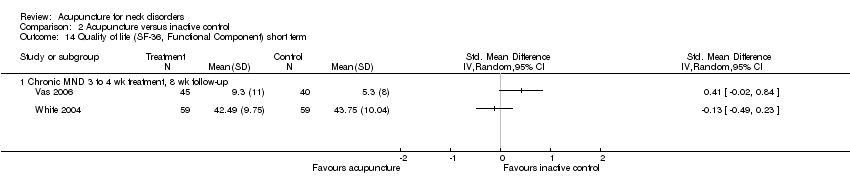
Comparison 2 Acupuncture versus inactive control, Outcome 14 Quality of life (SF‐36, Functional Component) short term.
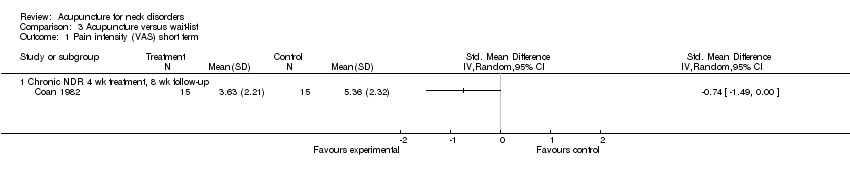
Comparison 3 Acupuncture versus wait‐list, Outcome 1 Pain intensity (VAS) short term.

Comparison 3 Acupuncture versus wait‐list, Outcome 2 Disability (neck and pain disability scale) short term.
Comparison 3 Acupuncture versus wait‐list, Outcome 3 Disability (neck and pain disability scale) intermediate term.

Comparison 3 Acupuncture versus wait‐list, Outcome 4 Quality of life (SF‐36 mental score) short term.

Comparison 3 Acupuncture versus wait‐list, Outcome 5 Quality of life (SF‐36 mental score) intermediate term.

Comparison 3 Acupuncture versus wait‐list, Outcome 6 Quality of life (SF‐36 physical score) intermediate term.
| Acupuncture compared with sham for chronic neck pain | ||||||
| Patient or population: patients with chronic mechanical neck pain (pain for more than 90 days) Settings: varied, mostly at university or hospital clinics Intervention: acupuncture Comparison: sham | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Sham | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity ranged across sham groups from 3 points on a 0 to 10 scale to 47 points on a 0 to 100 scale | Mean pain intensity in intervention groups was 0.23 standard deviations lower (0.20 to 0.07 higher) | ‐0.23 (‐0.20 to ‐0.07) | 560 (8 studies) | ⊕⊕⊕⊝ Limitations: ‐1 Inconsistency: 0 Indirectness: 0 Imprecision: 0 Other: 0 | Statistical pooling was appropriate in this instance because of statistical homogeneity. Results of the meta‐analysis favoured acupuncture |
| Disability (NPQ) short term | Mean disability ranged across control groups from 24 points on a 0 to 100 scale to 26 points on a 0 to 100 scale | Mean disability in intervention groups was | ‐0.38 (‐0.62 to ‐0.15) | 290 (2 studies) | ⊕⊕⊝⊝ Limitations: ‐1 Inconsistency: 0 Indirectness: 0 Imprecision: ‐1 Other: 0 | Two small trials were in favour of acupuncture. On the basis of the GRADE scale, quality level of evidence was downgraded to low because only 1 of the 2 studies (50%) was at low risk with small sample size |
| Disability (NDI) short term | Mean disability ranged across control groups from | Mean disability in intervention groups ranged from | ‐‐ | 173 | N/A | All 3 studies, 2 with low risk of bias, did not show a statistically significant result in favour of acupuncture |
| Quality of life (SF‐36) short term | Mean quality of life across control groups ranged from 86 points on a 0 to 100 scale to 86 points on a 0 to 100 scale | Mean quality of life in intervention groups ranged from 84 points on a 0 to 100 scale to 85 points on a 0 to 100 scale | ‐‐ | 178 (1 study) | ⊕⊕⊝⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: ‐1 Other: 0 | One study with low risk of bias favoured acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies. GRADE Working Group grades of evidence | ||||||
| Acupuncture compared with inactive treatments for chronic neck pain | ||||||
| Patient or population: patients with chronic neck pain (pain for more than 90 days) Settings: primary care, general practitioners' clinics to secondary care, outpatient pain clinics or speciality clinics Intervention: acupuncture Comparison: inactive treatments | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Inactive treatment | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity ranged across control groups from 17 points on a 0 to 100 scale to 31 points on a 0 to 100 scale | Mean pain intensity in intervention groups was 17 points on a 0 to 100 scale to 9 points on a 0 to 10 scale | ‐‐ | 404 (5 studies) | ⊕⊕⊕⊝ Limitations: 0 Inconsistency: 0 Indirectness: 0 Imprecision: ‐1 Other: 0 | Five studies (n = 461) assessed participants with mechanical neck disorders. Four were at low risk of bias. Statistical pooling was inappropriate in this instance because of statistical heterogeneity. Four of these studies favoured acupuncture |
| Pain pressure threshold short term | Mean pain pressure threshold ranged across control groups from 0 points on a 0 to 10 scale to 7 points on a 0 to 10 scale | Mean pain pressure threshold in intervention groups ranged from 0.2 points on a 0 to 10 scale to 7 points on a 0 to 10 scale | ‐‐ | 132 (2 studies) | N/A | Two studies with low risk of bias did not favour acupuncture |
| Disability (NDI) short term Function (NPQ) short term | Mean disability ranged across control groups from 12 points on a 0 to 100 scale to 13 points on a 0 to 100 scale Mean function across control groups was 13 points on a 0 to 100 scale | Mean disability in intervention groups ranged from Mean function in intervention groups was 30 points on a 0 to 100 scale | ‐‐ | 118 (1 study) 123 (1 study) | N/A ⊕⊕⊝⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: ‐1 Other: 0 | One study with low risk of bias did not favour acupuncture One study with low risk of bias favoured acupuncture |
| Quality of life (SF‐36, Functional Component) short term | Mean function ranged across control groups from 0.7 points on a 0 to 10 scale to 5 points on a 0 to 10 scale | Mean function in intervention groups ranged from 41 points on a 0 to 100 scale to 9 points on a 0 to 10 scale | ‐‐ | 143 (2 studies) | N/A | Two studies with low risk of bias did not favour acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies. GRADE Working Group grades of evidence | ||||||
| Acupuncture compared with wait‐list control for chronic neck pain | ||||||
| Patient or population: patients with chronic neck pain (pain for more than 90 days) Settings: primary care newspaper advertisement or recruited through participating physicians Intervention: acupuncture Comparison: wait‐list control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Wait‐list control | Acupuncture | |||||
| Pain intensity (VAS) short term | Mean pain intensity across control groups was 5 points on a 0 to 10 scale | Mean pain intensity in intervention groups was | ‐‐ | 30 (1 study) | ⊕⊕⊕⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: 0 Other: 0 | One trial with low risk of bias showed a small reduction in pain. Moderate evidence supporting acupuncture is helpful |
| Disability (neck and pain disability scale) short term | Mean disability across control groups was | Mean disability in intervention groups was 29 points on a 0 to 100 scale | ‐‐ | 3451 (1 study) | ⊕⊕⊕⊝ Limitations: 0 Inconsistency: 0 Indirectness: ‐1 Imprecision: 0 Other: 0 | One large study with low risk of bias favoured acupuncture |
| Quality of life (SF‐36 mental score) short term | Mean quality of life score across control groups was | Mean quality of life score in intervention groups was 4 points on a 0 to 10 scale | ‐‐ | 3451 (1 study) | N/A | One large study showed no statistically significant findings in favour of acupuncture |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| Adverse effects were reported in 14 studies and included increased pain, bruising, fainting, worsening of symptoms, local swelling and dizziness. No life‐threatening adverse effects were noted by these studies Cost of care was calculated in 1 study, which found that acupuncture treatment was cost‐effective GRADE Working Group grades of evidence | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity (VAS) immediate post treatment Show forest plot | 11 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Chronic MPS 1 treatment session | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Chronic MND 3 to 4 wk treatment | 4 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Chronic MPS 12 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Chronic MND SA group 10 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Cervical osteoarthritis 1 treatment session | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Chronic MPS 3 wk treatment, pain with movement scale | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain intensity (VAS) short term Show forest plot | 8 | 560 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.40, ‐0.07] |
| 2.1 Chronic MPS 3 wk treatment, 3 mo follow‐up, pain with movement scale | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.67, 0.67] |
| 2.2 Chronic MND 3 to 4 wk treatment, 1 to 4 wk follow‐up | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.82, 0.52] |
| 2.3 Chronic MND 3 to 4 wk treatment, 3 mo follow‐up | 3 | 319 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.40, 0.04] |
| 2.4 Subacute/chronic WAD 6 wk treatment, 3 mo follow‐up | 1 | 124 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.73, ‐0.02] |
| 2.5 WAD myofascial 2 to 6 sessions, 6 wk follow‐up | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.29, 0.09] |
| 2.6 Chronic MND SA group 10 wk treatment, 3 wk follow‐up | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐1.11, 0.92] |
| 3 Pain intensity (VAS) intermediate term Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Chronic MPS ESNS 3 to 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Chronic WAD 6 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain intensity (VAS) long term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Chronic MPS ESNNS 3 to 4 wk treatment, 3 year follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Disability (NDI) immediate post treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chronic MND SA group 10 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Disability (NPQ) immediate post treatment Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Chronic MND, 3 wk treatment | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Disability (NPQ) short term Show forest plot | 2 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.62, ‐0.15] |
| 7.1 Chronic MND, 3 wk treatment, 3 mo follow‐up | 2 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.62, ‐0.15] |
| 8 Disability (NDI) short term Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Chronic MND SA group 10 wk treatment, 3 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Chronic WAD 6 wk treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 WAD II myofascial 2 to 6 treatment, 6 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Chronic MPS 1 treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Disability (NDI) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Chronic WAD 6 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Quality of life (SF‐36) immediate post treatment Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Chronic MND, 3 wk treatment | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Quality of life (SF‐36) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Chronic MND, 3 wk treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity (VAS) immediate post treatment Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Chronic MPS 4 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Chronic MND NLA group 1 treatment session, movement scale | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Chronic MND 3 to 4 wk treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Cervical osteoarthritis 1 treatment session | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain intensity (VAS) short term Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Chronic MND 3 to 4 wk treatment, 1 to 4 wk follow‐up | 5 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain intensity (VAS) intermediate term Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Chronic MPS 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Chronic MND 3 to 4 wk treatment, 6 mo follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain intensity (VAS) long term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Chronic MND 3 to 4 wk treatment, 12 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pain pressure threshold immediate post treatment Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chronic MND 3 to 4 wk treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Pain pressure threshold short term Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Chronic MND 3 to 4 wk treatment, 1 to 3 month follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain intensity (proportion pain relief) immediate post treatment Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Chronic MND 4 wk treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Disability (NDI) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9 Disability (NDI) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Chronic MND 4 wk treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Disability (NDI) long term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Chronic MND 4 wk treatment, 12 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Function (NHP) immediate post treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Chronic MPS 4 wk treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Function (NHP) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Chronic MPS 4 wk treatment 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Function (NPQ) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 Chronic MND 1 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Quality of life (SF‐36, Functional Component) short term Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Chronic MND 3 to 4 wk treatment, 8 wk follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity (VAS) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Chronic NDR 4 wk treatment, 8 wk follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Disability (neck and pain disability scale) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Chronic MND 3 mo treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Disability (neck and pain disability scale) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Quality of life (SF‐36 mental score) short term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Chronic MND 3 mo treatment, 3 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Quality of life (SF‐36 mental score) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Quality of life (SF‐36 physical score) intermediate term Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Chronic MND 3 mo treatment, 6 mo follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |

