Модели непрерывного акушерского контроля в сравнении с другими моделями оказания помощи женщинам детородного возраста
Appendices
Appendix 1. Search methods used in previous versions of this review
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co‐ordinator (January 2008).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
-
quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
-
weekly searches of MEDLINE;
-
handsearches of 30 journals and the proceedings of major conferences;
-
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL and MEDLINE, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
In addition, we searched the Cochrane Effective Practice and Organisation of Care Group's Trials Register (January 2008), Current Contents (1994 to January 2008), CINAHL (1982 to August 2006), Web of Science, BIOSIS Previews, ISI Proceedings, (1990 to 2008), and the WHO Reproductive Health Library (WHO‐RHL), No. 9. Through WHO‐RHL we obtained unpublished studies from the System for Information on Grey Literature In Europe (SIGLE). We used the search strategy detailed below, modifying it for each database as appropriate by checking each thesaurus for relevant subject headings and replacing them with text‐word search terms when a subject heading was not available.
We did not apply any language restrictions.
1 exp Pregnancy/
2 exp Prenatal Care/
3 exp Intrapartum Care/
4 exp Obstetric Care/
5 exp Postnatal Care/
6 exp Midwifery/
7 exp Midwifery Service/
8 exp Obstetric Service/
9 exp Home Childbirth/
10 exp Alternative Birth Centers/
11 or/1‐10
12 exp Continuity of Patient Care/
13 exp Nursing Care Delivery Systems/
14 (midwif$ adj2 team$).tw.
15 (midwif$ adj model$).tw.
16 (multidisciplinary adj team$).tw.
17 (share$ adj care).tw.
18 (midwif$ adj led).tw.
19 (midwif$ adj manag$).tw.
20 (medical$ adj led).tw.
21 (medical adj manag$).tw.
22 or/12‐21
23 exp Clinical Trials/
24 11 and 22 and 23
Appendix 2. Methods used to assess trials included in previous versions of this review
We developed the methods of the review in consideration of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2005).
Selection of studies
We considered all trials that compared midwife‐led models of care with other models of care for childbearing women and their infants for inclusion. We assessed for inclusion all potential studies identified as a result of the search strategy. We resolved any disagreement through discussion. We obtained potentially eligible trials identified by the search strategy as full‐text papers and two authors independently assessed each for inclusion. There were no studies where eligibility was hampered by requirement for translation or missing information.
Data extraction and management
We designed a form to extract data. At least two review authors extracted the data using the agreed form. We resolved discrepancies through discussion. We used the Review Manager software (RevMan 2003) to double enter all the data or a subsample. When information regarding any of the above was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of methodological quality of included studies
We assessed the validity of each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2005). Methods used for generation of the randomisation sequence were described for each trial. Two review authors independently assessed the quality of each included trial using the criteria outlined in Higgins 2005. Quality assessment was based on the criteria of selection (allocation concealment).
(1) Selection bias (allocation concealment)
We assigned a quality score for each trial, using the following criteria:
(A) adequate concealment of allocation: such as telephone randomisation, consecutively‐numbered, sealed opaque envelopes;
(B) unclear whether adequate concealment of allocation: such as list or table used, sealed envelopes, or study does not report any concealment approach;
(C) inadequate concealment of allocation: such as open list of random‐number tables, use of case record numbers, dates of birth or days of the week.
(2) Attrition bias (loss of participants, eg withdrawals, dropouts, protocol deviations)
We assessed completeness to follow‐up using the following criteria:
(A) less than 5% loss of participants;
(B) 5% to 9.9% loss of participants;
(C) 10% to 19.9% loss of participants;
(D) more than 20% loss of participants.
Any outcome for a given study was excluded from analyses where loss to follow‐up was greater than 20%.
(3) Performance bias (blinding of participants, researchers and outcome assessment)
It was not possible to blind participants to the model of care they receive. Therefore lack of blinding was not considered as part of the quality assessment of included trials.
Measures of treatment effect
We carried out statistical analysis using the Review Manager software (RevMan 2003).
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we used the mean difference if outcomes were measured in the same way between trials. If necessary, we planned to use the standardised mean difference to combine trials that measured the same outcome, but used different methods. If there was evidence of skewness according to the test suggested by Altman 1996, we have reported this.
Unit of analysis issues
Cluster‐randomised trials
We included one cluster‐randomised trial in the analyses along with the other individually‐randomised trials. We adjusted the sample size using the methods described by Gates 2005 using an estimate of the intracluster correlation coefficient (ICC) derived from the trial. This trial estimated the ICC to be zero, so for the main analysis we used this estimate and did not adjust the sample sizes. We also conducted a sensitivity analysis, to investigate the effects of variation in the ICC. The analysis was repeated using values of 0.001 and 0.01 for the ICC.
Dealing with missing data
We analysed data on all participants with available data in the group to which they were allocated, regardless of whether or not they received the allocated intervention. If in the original reports participants were not analysed in the group to which they were randomised, and there was sufficient information in the trial report, we restored them to the correct group. Denominators were the number of women randomised minus the number of participants known to have missing data. Women with miscarriages and termination of pregnancy were included in the denominators for maternal and neonatal outcomes. This denominator was also used for perineal outcomes. Where data was available on twin births, these were added to the neonatal denominator. Where detailed denominator outcome data were available, these were used in the analysis. Any outcome for a given study was excluded from analyses where loss to follow‐up was greater than 20%.
Assessment of heterogeneity
We used the I² statistic to assess heterogeneity between the trials in each analysis. An I² value of 30% suggests mild heterogeneity and a value of more than 50% indicates substantial heterogeneity. High levels of heterogeneity (exceeding 50%) were explored by prespecified subgroup analysis, and a random‐effects meta‐analysis was used for an overall summary.
Data synthesis (meta‐analysis)
We used fixed‐effect meta‐analysis for combining data in the absence of significant heterogeneity if trials were sufficiently similar.
Subgroup analyses
We conducted the planned subgroup analyses to investigate the effects of greater continuity in caseload models, variations in maternal risk status and of less medicalised environments provided by community settings.
(1) Variations in the model of midwife‐led care (caseload versus team)
(2) Variations in maternal risk status (low‐risk versus mixed‐risk status)
(3) Variations in practice setting: community based (antenatal and/or intrapartum and/or postnatal care provided in the community) or hospital based (all care provided in a hospital setting).
All of these subgroup analyses investigate potential sources of heterogeneity, as differences in the type of intervention, risk profile of the population or setting may affect the treatment effects. Subgroup analyses were conducted by interaction tests as described by Deeks 2001.
Sensitivity analyses
We performed sensitivity analysis based on quality comparing high‐quality trials with trials of lower quality. Given that study reports on attrition after allocation have not been found to be consistently related to bias, 'high quality' was, for the purposes of this sensitivity analysis, defined as a trial having allocation concealment classified as 'A' (adequate). We excluded studies that did not achieve an 'A' rating in the sensitivity analysis in order to assess for any substantive difference to the overall result.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

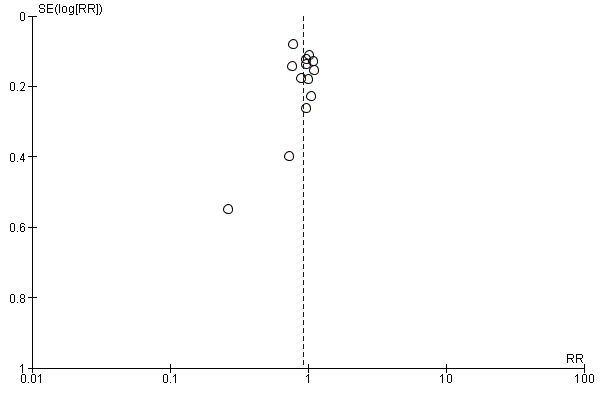
Funnel plot of comparison: 1 Midwife‐led versus other models of care for childbearing women and their infants (all), outcome: 1.1 Regional analgesia (epidural/spinal).
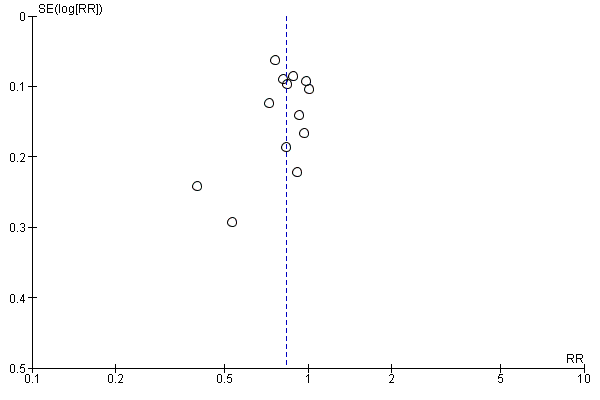
Funnel plot of comparison: 1 Midwife‐led versus other models of care for childbearing women and their infants (all), outcome: 1.2 Caesarean birth.
Funnel plot of comparison: 1 Midwife‐led versus other models of care for childbearing women and their infants (all), outcome: 1.16 Episiotomy.
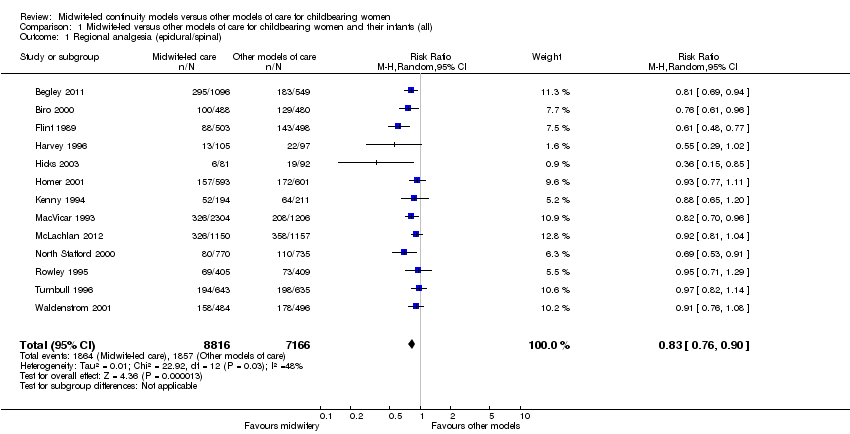
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 1 Regional analgesia (epidural/spinal).

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 2 Caesarean birth.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 3 Instrumental vaginal birth (forceps/vacuum).

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 4 Spontaneous vaginal birth (as defined by trial authors).
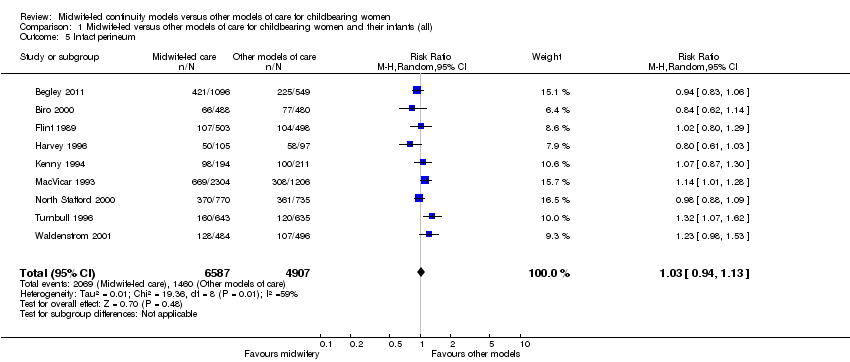
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 5 Intact perineum.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 6 Preterm birth (< 37 weeks).
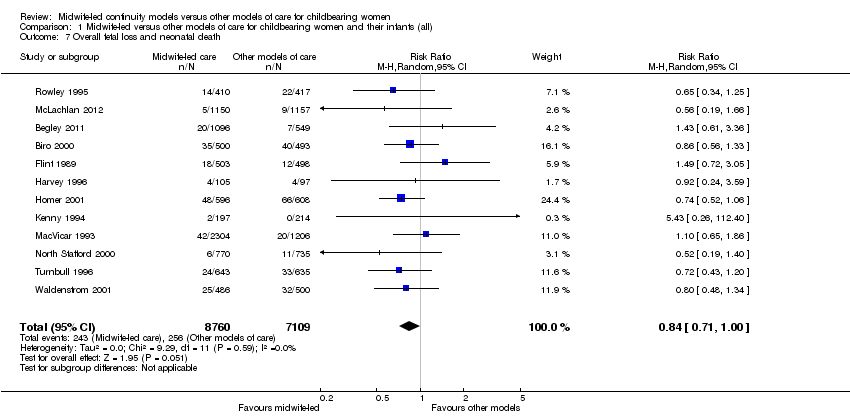
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 7 Overall fetal loss and neonatal death.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 8 Antenatal hospitalisation.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 9 Antepartum haemorrhage.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 10 Induction of labour.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 11 Amniotomy.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 12 Augmentation/artificial oxytocin during labour.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 13 No intrapartum analgesia/anaesthesia.
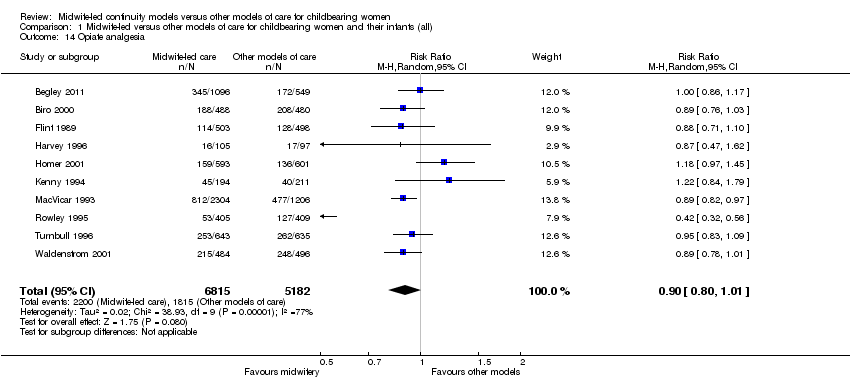
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 14 Opiate analgesia.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 15 Attendance at birth by known midwife.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 16 Episiotomy.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 17 Perineal laceration requiring suturing.
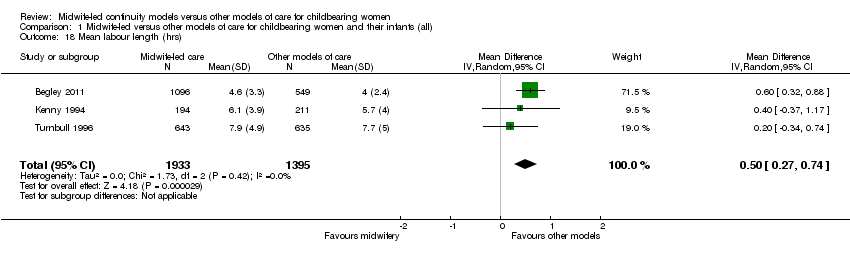
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 18 Mean labour length (hrs).

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 19 Postpartum haemorrhage (as defined by trial authors).
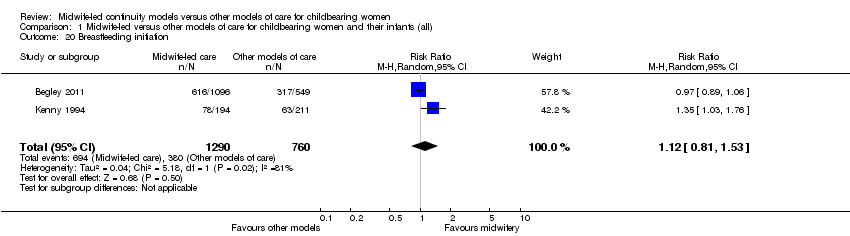
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 20 Breastfeeding initiation.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 21 Duration of postnatal hospital stay (days).
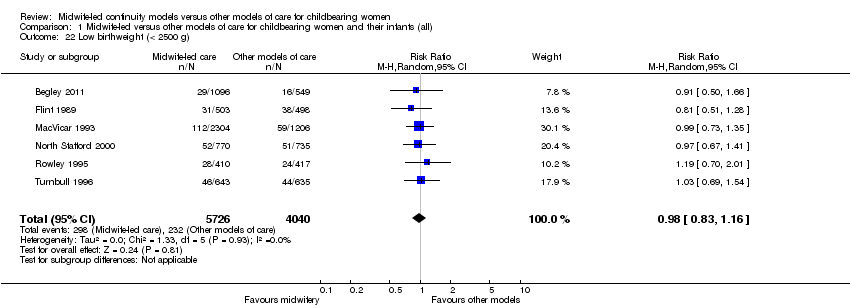
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 22 Low birthweight (< 2500 g).

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 23 5‐minute Apgar score below or equal to 7.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 24 Neonatal convulsions (as defined by trial authors).
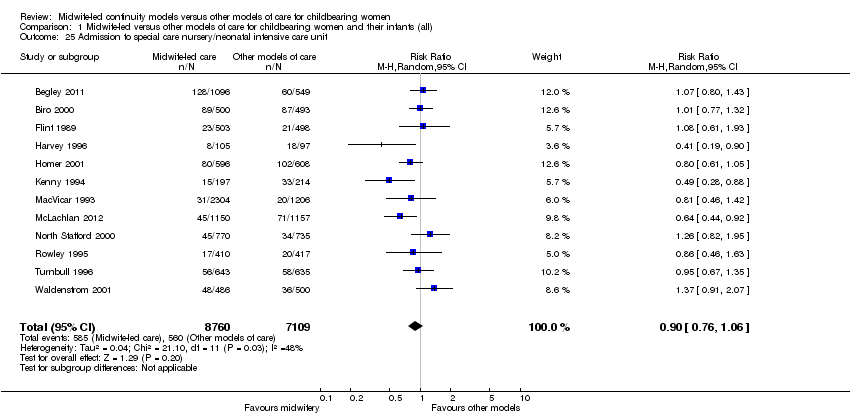
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 25 Admission to special care nursery/neonatal intensive care unit.

Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 26 Mean length of neonatal hospital stay (days).
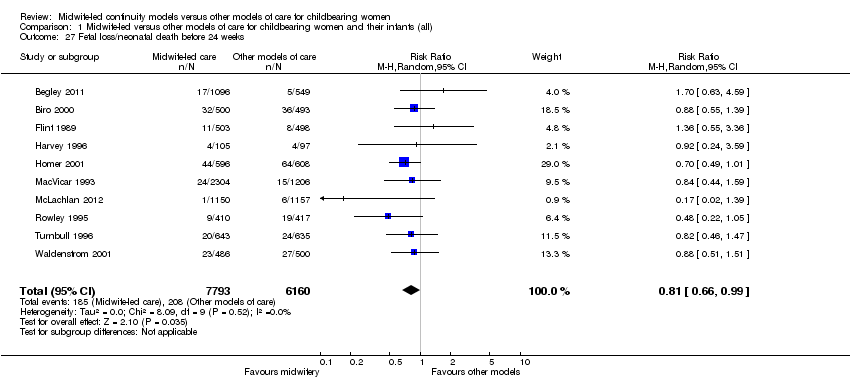
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 27 Fetal loss/neonatal death before 24 weeks.
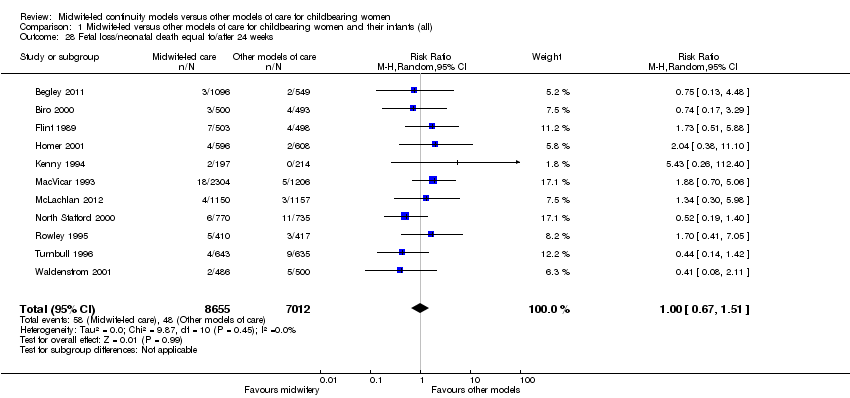
Comparison 1 Midwife‐led versus other models of care for childbearing women and their infants (all), Outcome 28 Fetal loss/neonatal death equal to/after 24 weeks.

Comparison 2 Midwife‐led versus other models of care: variation in midwifery models of care (caseload/one‐to‐one or team), Outcome 1 Regional analgesia (epidural/spinal).

Comparison 2 Midwife‐led versus other models of care: variation in midwifery models of care (caseload/one‐to‐one or team), Outcome 2 Caesarean birth.

Comparison 2 Midwife‐led versus other models of care: variation in midwifery models of care (caseload/one‐to‐one or team), Outcome 3 Instrumental vaginal birth (forceps/vacuum).
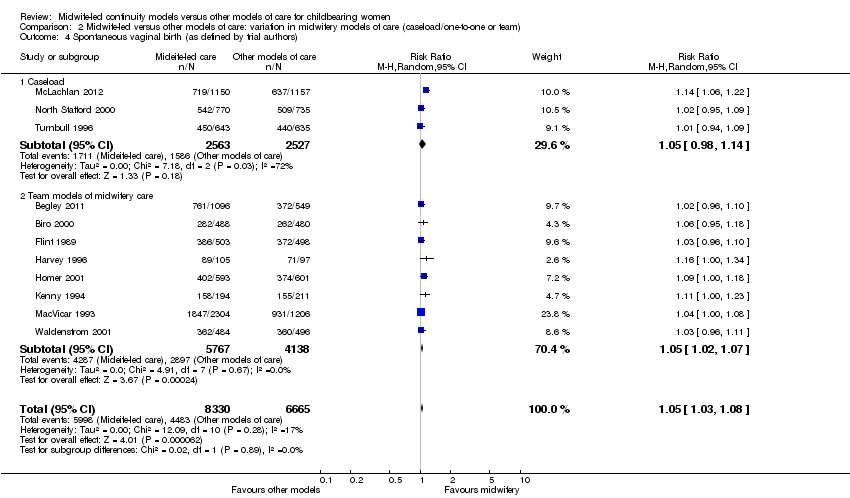
Comparison 2 Midwife‐led versus other models of care: variation in midwifery models of care (caseload/one‐to‐one or team), Outcome 4 Spontaneous vaginal birth (as defined by trial authors).

Comparison 2 Midwife‐led versus other models of care: variation in midwifery models of care (caseload/one‐to‐one or team), Outcome 5 Intact perineum.
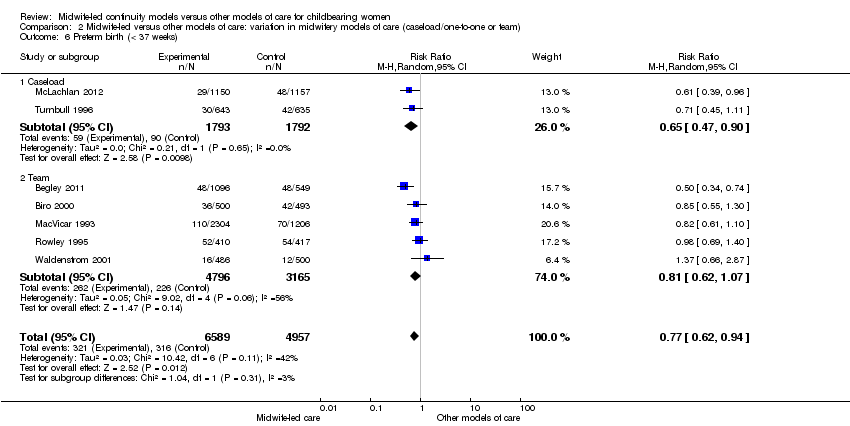
Comparison 2 Midwife‐led versus other models of care: variation in midwifery models of care (caseload/one‐to‐one or team), Outcome 6 Preterm birth (< 37 weeks).

Comparison 2 Midwife‐led versus other models of care: variation in midwifery models of care (caseload/one‐to‐one or team), Outcome 7 Overall fetal loss and neonatal death.

Comparison 3 Midwife‐led versus other models of care: variation in risk status (low versus mixed), Outcome 1 Regional analgesia (epidural/spinal).

Comparison 3 Midwife‐led versus other models of care: variation in risk status (low versus mixed), Outcome 2 Caesarean birth.

Comparison 3 Midwife‐led versus other models of care: variation in risk status (low versus mixed), Outcome 3 Instrumental vaginal birth (forceps/vacuum).

Comparison 3 Midwife‐led versus other models of care: variation in risk status (low versus mixed), Outcome 4 Spontaneous vaginal birth (as defined by trial authors).

Comparison 3 Midwife‐led versus other models of care: variation in risk status (low versus mixed), Outcome 5 Intact perineum.
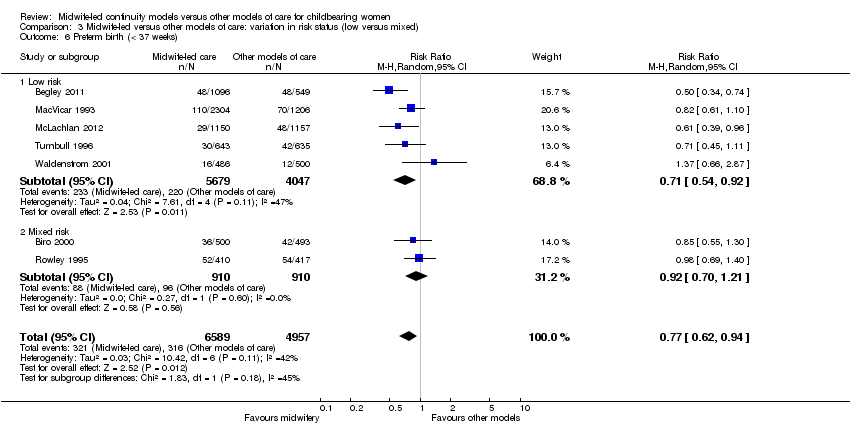
Comparison 3 Midwife‐led versus other models of care: variation in risk status (low versus mixed), Outcome 6 Preterm birth (< 37 weeks).

Comparison 3 Midwife‐led versus other models of care: variation in risk status (low versus mixed), Outcome 7 Overall fetal loss and neonatal death.
| Satisfaction | Intervention (n/N) | Control (n/N) | Relative rate | 95% CI | Statistical test | P value |
| Staff in labour (very caring) | 252/275 (92%) | 208/256 (81%) | 1.1 | 1.0‐1.2 | ||
| Experience of labour (wonderful/enjoyable) | 104/246 (42%) | 72/223 (32%) | 1.3 | 1.0‐1.8 | ||
| Satisfaction with pain relief (very satisfied) | 121/209 (58%) | 104/205 (51%) | 1.1 | 0.9‐1.4 | ||
| Very well prepared for labour | 144/275 (52%) | 102/254 (40%) | 1.3 | 1.0‐1.7 | ||
| N = 1663 | N = 826 | Difference | ||||
| Very satisfied with antenatal care | 52% | 44% | 8.3% | 4.1‐12.5 | ||
| Very satisfied with care during labour | 73% | 60% | 12.9% | 9.1‐16.8 | ||
| N = 213 | N = 233 | |||||
| Carer skill, attitude and communication (antenatal care) | 57.1/60 | 47.7/60 | t = 12.4 | 0.0001 | ||
| Convenience and waiting (antenatal care) | 14.8/20 | 10.9/20 | t = 10.1 | 0.0001 | ||
| Expectation of labour/birth (antenatal care) | 9.8/18 | 9.3/18 | t = 1.4 | 0.16 | ||
| Asking questions (antenatal care) | 8.5/12 | 6.9/12 | t = 6.6 | 0.0001 | ||
| Information/communication (labour and birth) | 28.3/30 | 24.8/30 | t = 7.48 | 0.0001 | ||
| Coping with labour (labour and birth) | 20.9/30 | 19.3/30 | t = 2.83 | 0.005 | ||
| Midwife skill/caring (labour and birth) | 22.7/24 | 21.3/24 | t = 3.44 | 0.0007 | ||
| Help and advice (postnatal care) | 21.0/24 | 19.7/24 | t = 1.88 | 0.06 | ||
| Midwife skill and communication (postnatal care) | 16.6/18 | 15.4/18 | t = 4.48 | 0.0001 | ||
| Managing baby (postnatal care) | 8.7/12 | 8.5/12 | t = 0.77 | 0.77 | ||
| Self‐rated health (postnatal care) | 7.5/12 | 7.1/12 | t = 1.67 | 0.10 | ||
| OR | ||||||
| Encouraged to ask questions | N/A | 4.22 | 2.72‐6.55 | |||
| Given answers they could understand | N/A | 3.03 | 1.33‐7.04 | |||
| Able to discuss anxieties | N/A | 3.60 | 2.28‐5.69 | |||
| Always had choices explained to them | N/A | 4.17 | 1.93‐9.18 | |||
| Participation in decision making | N/A | 2.95 | 1.22‐7.27 | |||
| Midwives interested in woman as a person | N/A | 7.50 | 4.42‐12.80 | |||
| Midwives always friendly | N/A | 3.48 | 1.92 ‐ 6.35 | |||
| n/N | n/N | Mean difference ‐ satisfaction score | ||||
| Antenatal care | 534/648 | 487/651 | 0.48 | 0.55‐0.41 | ||
| Intrapartum care | 445/648 | 380/651 | 0.28 | 0.37‐0.18 | ||
| Hospital‐based postnatal care | 445/648 | 380/651 | 0.57 | 0.70‐0.45 | ||
| Home‐based postnatal care | 445/648 | 380/651 | 0.33 | 0.42‐0.25 | ||
| % | % | OR | ||||
| Overall antenatal care was very good (strongly agree) | 58.2% | 39.7% | 2.22 | 1.66‐2.95 | < 0.001 | |
| Happy with the physical aspect of intrapartum care (strongly agree) | 58.6% | 42.5% | 1.94 | 1.46‐2.59 | < 0.001 | |
| Happy with the emotional aspect of intrapartum care (strongly agree) | 58.8% | 44.0% | 1.78 | 1.34‐2.38 | < 0.001 | |
| Overall postnatal care was very good (strongly agree) | 37.6% | 33.2% | 1.27 | 0.97‐1.67 | 0.08 | |
| Care and sensitivity of staff (antenatal) | 1.32 | 1.77 | Mean difference? | 0.0000 | ||
| Care and sensitivity of staff (labour and delivery) | 1.26 | 1.58 | Mean difference? | 0.008 | ||
| Care and sensitivity of staff (postpartum at home) | 1.24 | 1.57 | Mean difference? | 0.0000 | ||
| Labour and Delivery Satisfaction Index + | 211 | 185 | 26 | 18.8‐33.1 | 0.001 | |
| Satisfaction with antenatal care (very good) | 195/344 (57%) | 100/287 (35%) | 1.24 | 1.13‐1.36 | 0.001 | |
| Satisfaction with intrapartum care (very good) | 215/241 (63%) | 134/282 (47%) | 1.11 | 1.03‐1.20 | 0.01 | |
| Satisfaction with postpartum care in hospital (very good) | 141/344 (41%) | 102/284 (31%) | 0.92 | 0.82‐1.04 | 0.22 | |
| *: 99% Confidence interval (CI) for Flint study was reported | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Regional analgesia (epidural/spinal) Show forest plot | 13 | 15982 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.76, 0.90] |
| 2 Caesarean birth Show forest plot | 13 | 15982 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.02] |
| 3 Instrumental vaginal birth (forceps/vacuum) Show forest plot | 12 | 15809 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.81, 0.96] |
| 4 Spontaneous vaginal birth (as defined by trial authors) Show forest plot | 11 | 14995 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [1.03, 1.08] |
| 5 Intact perineum Show forest plot | 9 | 11494 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.94, 1.13] |
| 6 Preterm birth (< 37 weeks) Show forest plot | 7 | 11546 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.62, 0.94] |
| 7 Overall fetal loss and neonatal death Show forest plot | 12 | 15869 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.71, 1.00] |
| 8 Antenatal hospitalisation Show forest plot | 6 | 6039 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.83, 1.05] |
| 9 Antepartum haemorrhage Show forest plot | 4 | 3654 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.57, 1.40] |
| 10 Induction of labour Show forest plot | 12 | 15809 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.86, 1.03] |
| 11 Amniotomy Show forest plot | 4 | 3253 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.66, 0.98] |
| 12 Augmentation/artificial oxytocin during labour Show forest plot | 11 | 13502 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.79, 1.01] |
| 13 No intrapartum analgesia/anaesthesia Show forest plot | 6 | 8807 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [1.04, 1.31] |
| 14 Opiate analgesia Show forest plot | 10 | 11997 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.80, 1.01] |
| 15 Attendance at birth by known midwife Show forest plot | 6 | 5225 | Risk Ratio (M‐H, Random, 95% CI) | 7.83 [4.15, 14.80] |
| 16 Episiotomy Show forest plot | 13 | 15982 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.76, 0.92] |
| 17 Perineal laceration requiring suturing Show forest plot | 9 | 13412 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.95, 1.10] |
| 18 Mean labour length (hrs) Show forest plot | 3 | 3328 | Mean Difference (IV, Random, 95% CI) | 0.50 [0.27, 0.74] |
| 19 Postpartum haemorrhage (as defined by trial authors) Show forest plot | 9 | 12522 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.84, 1.11] |
| 20 Breastfeeding initiation Show forest plot | 2 | 2050 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.81, 1.53] |
| 21 Duration of postnatal hospital stay (days) Show forest plot | 3 | 3593 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.29, 0.09] |
| 22 Low birthweight (< 2500 g) Show forest plot | 6 | 9766 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.83, 1.16] |
| 23 5‐minute Apgar score below or equal to 7 Show forest plot | 10 | 10854 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.70, 1.41] |
| 24 Neonatal convulsions (as defined by trial authors) Show forest plot | 2 | 2923 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.14, 5.74] |
| 25 Admission to special care nursery/neonatal intensive care unit Show forest plot | 12 | 15869 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.76, 1.06] |
| 26 Mean length of neonatal hospital stay (days) Show forest plot | 2 | 1979 | Mean Difference (IV, Random, 95% CI) | ‐3.63 [‐7.57, 0.30] |
| 27 Fetal loss/neonatal death before 24 weeks Show forest plot | 10 | 13953 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.66, 0.99] |
| 28 Fetal loss/neonatal death equal to/after 24 weeks Show forest plot | 11 | 15667 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.67, 1.51] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Regional analgesia (epidural/spinal) Show forest plot | 13 | 15982 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.76, 0.90] |
| 1.1 Caseload | 3 | 5090 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.76, 1.03] |
| 1.2 Team models of midwifery care | 10 | 10892 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.73, 0.89] |
| 2 Caesarean birth Show forest plot | 13 | 15966 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.02] |
| 2.1 Caseload | 3 | 5090 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.75, 1.17] |
| 2.2 Team models of midwifery care | 10 | 10876 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.84, 1.05] |
| 3 Instrumental vaginal birth (forceps/vacuum) Show forest plot | 12 | 16273 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.82, 0.96] |
| 3.1 Caseload | 3 | 5090 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.80, 1.04] |
| 3.2 Team models of midwifery care | 9 | 11183 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.79, 0.97] |
| 4 Spontaneous vaginal birth (as defined by trial authors) Show forest plot | 11 | 14995 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [1.03, 1.08] |
| 4.1 Caseload | 3 | 5090 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.98, 1.14] |
| 4.2 Team models of midwifery care | 8 | 9905 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [1.02, 1.07] |
| 5 Intact perineum Show forest plot | 9 | 11494 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.94, 1.13] |
| 5.1 Caseload | 2 | 2783 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.83, 1.50] |
| 5.2 Team | 7 | 8711 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.91, 1.13] |
| 6 Preterm birth (< 37 weeks) Show forest plot | 7 | 11546 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.62, 0.94] |
| 6.1 Caseload | 2 | 3585 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.47, 0.90] |
| 6.2 Team | 5 | 7961 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.62, 1.07] |
| 7 Overall fetal loss and neonatal death Show forest plot | 12 | 15835 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.70, 1.00] |
| 7.1 Caseload | 3 | 5090 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.43, 0.99] |
| 7.2 Team | 9 | 10745 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.73, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Regional analgesia (epidural/spinal) Show forest plot | 13 | 15982 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.76, 0.90] |
| 1.1 Low risk | 8 | 11096 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.73, 0.92] |
| 1.2 Mixed risk | 5 | 4886 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.75, 0.95] |
| 2 Caesarean birth Show forest plot | 13 | 15982 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.02] |
| 2.1 Low risk | 8 | 11096 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.79, 1.06] |
| 2.2 Mixed risk | 5 | 4886 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.84, 1.09] |
| 3 Instrumental vaginal birth (forceps/vacuum) Show forest plot | 12 | 15809 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.81, 0.96] |
| 3.1 Low risk | 7 | 10923 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.81, 0.99] |
| 3.2 Mixed risk | 5 | 4886 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.65, 1.03] |
| 4 Spontaneous vaginal birth (as defined by trial authors) Show forest plot | 11 | 14995 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [1.03, 1.08] |
| 4.1 Low risk | 7 | 10923 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [1.02, 1.08] |
| 4.2 Mixed risk | 4 | 4072 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [1.01, 1.10] |
| 5 Intact perineum Show forest plot | 9 | 11494 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.94, 1.13] |
| 5.1 Low risk | 6 | 8616 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.93, 1.21] |
| 5.2 Mixed risk | 3 | 2878 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.90, 1.07] |
| 6 Preterm birth (< 37 weeks) Show forest plot | 7 | 11546 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.62, 0.94] |
| 6.1 Low risk | 5 | 9726 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.54, 0.92] |
| 6.2 Mixed risk | 2 | 1820 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.70, 1.21] |
| 7 Overall fetal loss and neonatal death Show forest plot | 12 | 15835 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.70, 1.00] |
| 7.1 Low risk | 7 | 10895 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.73, 1.20] |
| 7.2 Mixed risk | 5 | 4940 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.59, 0.97] |

