Détartrage et polissage de routine pour la santé parodontale chez l'adulte
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised controlled trial conducted in: UK Number of centres: 3 dental practices Recruitment period: Not stated Design: Parallel group 3‐arm RCT | |
| Participants | Adults (18‐60 years) attending practice for scheduled dental check‐up appointment. Generally fit and well with minimum of 20 natural teeth. All participants had scale and polish at baseline Number of participants: 369 allocated, 305 analysed | |
| Interventions | Group 1: Scale and polish every 6 months Group 2: Scale and polish every 12 months n = 122 allocated; n = 100 in analysis Group 3: No scale and polish n = 122 allocated; n = 99 in analysis 9 hygienists and therapists performed the interventions in this study Oral hygiene advice was given every 6 months to all participants | |
| Outcomes | See Additional Table 1 for further details of indices used to measure outcomes Outcomes measured at 24‐month follow‐up | |
| Notes | Sample size calculation: Yes Funding source: Oral Health Unit, The University of Manchester Consort flow diagram recording reasons for loss to follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomised, 3 arm parallel clinical trial" Quote: "Treatment allocation was by minimization and carried out by the trial manager using MINIM, an MS‐DOS program" Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Comment: Central method of randomisation Comment: Probably adequate |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Participants were asked not to disclose their allocation group to their dentist or to the outcome examiner" Quote: "the same two examiners carried out all of the follow‐up examinations blind to the allocation" Comment: Possibility of accidental disclosure by patient |
| Incomplete outcome data (attrition bias) | Low risk | 369 patients were randomised. Consort diagram and text explanation of withdrawals/drop‐outs |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the methods presented in the results |
| Other bias | Unclear risk | Patients who had BPE > 3 at any interim exam were withdrawn and the outcome data for these patients not collected (total numbers varied in months 15, 17 and 19, but more in the no scale and polish group). Authors note an overall deterioration in gingival health of the trial population, which the authors suggest may be a result of inter‐examiner variation |
| Methods | Randomised controlled trial conducted in: USA Number of centres: 1 US Air Force Academy Recruitment period: 1965/1966 Design: Parallel group 4‐arm RCT | |
| Participants | Young male US Air Force Academy cadets (mean age at final examination was 22 years) Number of participants: 713 recruited, 470 in analysis | |
| Interventions | Group 1: Scale and polish every 12 months without OHI Subdivided further into Groups 1A and 1B. 1 50‐minute preventive treatment (scale and polish) per year with no instruction in toothbrushing. Groups (1A and 1B) were treated 1 month apart. In this review when testing for treatment effects, a single group mean was employed for Groups 1A and 1B. Number of participants in analysis is 108 Group 2: Scale and polish every 12 months with OHI 1 preventive treatment per year given in 2 30‐minute appointments, 5 to 11 days apart and 10 minutes of toothbrushing instruction at each of their 2 appointments. Number of participants in analysis is 121 Group 3: Scale and polish every 6 months with OHI 2 scale and polish treatments per year, given 6 months apart: the first given in 2 30‐minute appointments, 5 to 11 days apart, with an additional 10 minutes of toothbrushing instruction at each session; the second given in 1 30‐minute appointment, plus 10 minutes of brushing instruction. Number of participants in analysis is 110 Group 4A: Scale and polish every 3 months with OHI Group 4B: Scale and polish every 3 months without OHI Individuals in groups receiving toothbrushing instruction received the instruction at each appointment prior to preventive treatment. Disclosing solution was used to disclose plaque. If only small plaque accumulation was noted, patients were instructed how to modify their technique to clean teeth effectively. If patient had no effective technique, they were instructed to use modified Roll technique in all areas, with the exception of the lingual surface of the mandibular molars, for which they were instructed to use the Bass technique Toothbrushes were provided to all participants throughout the course of the study. Each participant received 2 brushes every 90 days, either at a scheduled appointment or via postal delivery Due to graduation of participants in June 1969, the treatment schedule for the final year of the study had to be revised for Groups 3, 4A and 4B. However, the participants in Group 1A, 1B and 2 received their regular treatments at the customary times. Participants in Group 3 received their second preventive treatment after only 4 months instead of 6 months. The participants in Groups 4A and 4B received 3 instead of 4 preventive treatments. Number of participants in analysis is 64 in 4A and 67 in 4B All treatment was provided by 3 dental hygienists | |
| Outcomes | See Additional Table 1 for further details of indices used to measure outcomes Plaque: 0‐3 scale | |
| Notes | Sample size calculation: Not stated Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned to one of four treatment groups" Comment: Random component not described |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "the dentist was unaware of the treatment groups to which the participants were assigned" Comment: Dentist unaware of treatment allocations at initial and follow‐up examinations. Probably done |
| Incomplete outcome data (attrition bias) | Unclear risk | 712 participants entered the trial and 121, 74 and 42 participants lost in years 1, 2 and 3 respectively. Patients withdrew because they were moved to a different airbase. Total rate of withdrawal was 33%. However, this was unlikely to be related to intervention group |
| Selective reporting (reporting bias) | Low risk | Planned outcomes of plaque, gingivitis and calculus reported |
| Other bias | Unclear risk | Baseline imbalance: Calculus scores at baseline were lower in the control group |
| Methods | Randomised controlled study conducted in: USA Number of centres: 1 (the Dental Hygiene Clinic at the University of Pennsylvania School of Dental Medicine) Recruitment period: Not stated Design: Parallel group 2‐arm RCT | |
| Participants | Healthy adults, at least 18 years of age, in good general health, recruited from the Dental Hygiene Clinic at the University of Pennsylvania School of Dental Medicine Sex: All subjects had at least 5 teeth per quadrant, but no periodontal pockets probable to a depth of 6 mm or more. They had varying degrees of gingivitis but no evidence of alveolar bone loss. Some, but not all subjects, had been receiving periodontal prophylaxes at intervals of 3 to 6 months (no further information given in the report on the latter point) Number of participants: 69 randomised, 61 in analysis | |
| Interventions | Group 1: Scale and polish every 6 months Clinical examination (every 6 months), periodontal prophylaxis every 6 months (after every examination). Number of participants in analysis is 31 Clinical examination (every 6 months). Prophylaxes administered according to a variable schedule, based on the outcome of differential dark‐field microscopy (DDFM) tests. For negative DDFM tests (less than 15% spirochetes or motile rods, or less than 20% spirochetes plus motile rods) recall intervals were gradually increased from 1 to 2, to 3, to 6, to 12, to 24 months. 1 month after the baseline examination, the test was negative the recall interval was extended to 2 months and no prophylaxis was given. If at that time the test was still negative the interval was increased to 3 months, and so on. By the time a 12‐month interval was assigned, a subject may already have gone 12 months without a prophylaxis. If at a given recall (e.g. 3 months) a test was positive, a prophylaxis was given and the patient kept on the same recall interval (in this case, 3 months). If 3 months later the test was still positive, the prophylaxis was repeated and the patients recall interval reduced to the next lower interval, in this case 2 months. No patients were assigned recall intervals of less than 1 month. (Note: the latter description of the DDFM test was given in an earlier paper by the authors (Listgarten 1982 (for full reference see 'Additional references')). In the experimental group, the authors state that 25 out of 30 subjects achieved recall intervals of 12 to 24 months within the 3‐year experimental period. 11 subjects in the experimental group reached the end of the study without receiving a single prophylaxis over the 3‐year duration of the trial. Number of participants in analysis is 30 | |
| Outcomes | See Additional Table 1 for further details of indices used to measure outcomes | |
| Notes | Funding source: NIDR grant DE‐02623 to the Centre for Oral Health Research and a grant from the Colgate‐Palmolive company Sample size calculation: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Assignment to the C or T group was randomised" Comment: Random component not described |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) | Unclear risk | 69 patients randomised. 61 patients completed the study (31 in the intervention arm and 30 in the control arm). No reasons given for withdrawal or drop‐outs |
| Selective reporting (reporting bias) | Low risk | Plaque index, gingival index, probing depth recession, recall interval and microbiology outcomes planned and reported |
| Other bias | Unclear risk | Quote: "despite randomisation of the patients... into two groups some differences were observed at baseline" Comment: Baseline imbalances |
BPE = Basic Periodontal Examination; mm = millimetre; OHI = oral hygiene instruction; RCT = randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| None of the primary outcomes specified in our review were measured in this study. This study evaluated the effectiveness of professional tooth cleaning once a week for 24 months in a group of elderly subjects living in 2 nursing homes. Outcomes: fevers of 37.8º C >, prevalence of aspiration pneumonia, numbers of Staphylococcus species and Candida albicans in oral swab samples and the amount of methylmercaptan exhaled. | |
| Not routine scale and polish. Antimicrobial strips were used in 3 out of 4 treatment groups. The remaining treatment group received root planing. | |
| Length of follow‐up less than 6 months. Data from 2 studies presented in this paper. In study 1, 41 patients were randomly allocated to receive oral hygiene instruction (small loop flossing, Bass technique brushing, scaling and adjustment of restorative margins) or no treatment. Patients in the intervention group returned for re‐enforcement 1 month later. This study was excluded as it employed less than 6 months follow‐up (follow‐up was 2 months). In study 2, 23 patients were randomised to receive non‐surgical treatment (Bass technique brushing, flossing, scaling and root planing under local anaesthesia) or no‐treatment control. This study was excluded due to the use of root planing (not routine scale and polish). | |
| Children with mixed dentition at baseline. This study recruited schoolgirls aged between 11 and 12 years old at baseline. Girls in the intervention arm were randomly assigned by class to visit the hygienist every 2 weeks during term time for 3 years for oral hygiene reinforcement and professional prophylaxis. Girls in the control group received the oral hygiene instruction normally given at the school. | |
| Unclear if randomised. This study examined the effect of fluoride on caries in a programme involving meticulous plaque control. 82 patients of both genders were recruited (41 in each arm). Prophylactic treatment was administered once every 2 weeks. During these sessions an abrasive paste containing 5% sodium monofluorophosphate was used in the control group. While in the test group, a paste which did not contain fluoride was used. | |
| Children with mixed dentition at baseline. In this study 216 Swedish schoolchildren aged between 7 and 14 years old were divided into test and control groups. Once monthly children in the control group brushed their teeth with a 0.2% sodium fluoride solution under the supervision of a dental nurse. While patients in the treatment group received detailed information on the prevention of gingivitis, periodontitis and caries. During the first 2 years of the trial, patients in the treatment group also received detailed oral hygiene instruction and professional prophylaxis (including the application of sodium monoflurophosphate) at a dental nurse clinic every 2 weeks. | |
| Not a randomised controlled trial. 90 patients referred for treatment of advanced periodontal disease were recruited by the authors. For the first 2 months after surgery (Widman flap technique), the patients were recalled once every 2 weeks for professional tooth cleaning. Every third patient was then referred back to the care of their dentist for maintenance. While the remaining 2 out of 3 were enrolled in a maintenance care programme at a university clinic (patients were recalled every 2‐months and received oral health instruction, scaling and tooth cleaning). Patients were re‐examined 3 years and 6 years after baseline examination. | |
| Not routine scale and polish. This study involved 2 treatment groups (Groups 1 and 2) and 1 control group (Group 3). Group 1: received oral hygiene instruction, professional mechanical tooth cleaning including tongue scraping and chlorhexidine mouthrinse followed by application of 1% chlorhexidine gel (excluded from review due to adjunctive use of chlorhexidine). The entire prophylactic regimen was performed on days 1, 3, 5 and 8, followed by 1 single treatment every 6 months throughout the experimental period. Group 2 received only oral hygiene instructions ‐ given on days 1, 3, 5 and 8 for approximately 10 minutes on each occasion (excluded from review as no scale and polish provided). The instructions were repeated every 6 months. The 'control' group (Group 3) did not receive any treatment additional to the one based on individual needs given by the local dental health officers. | |
| Not a randomised controlled trial. The authors refer to an earlier paper (Axelsson 1978) for further details of the study participants. This paper was retrieved by the review team. Participants were recruited using the recall list of 3 general private practitioners and the waiting list of 3 large public dental health clinics. Potential participants for the test group were informed by letter of the purpose of the study and asked to volunteer for the trial. Potential members for the control group were informed that if they agreed to receive a very detailed oral examination they would be recalled for dental treatment to the public dental health clinic once a year during the next 3 years. Only those volunteers who had sought and received dental treatment annually during the last 5 years were selected. | |
| Unclear if randomised. In this study the incisors, cuspids and premolars received plaque control and supra and subgingival debridement using hand or ultrasonic scaling in a split‐mouth design. | |
| Children with mixed dentition at baseline. This study examined the effect of monthly professional tooth cleaning on gingivitis in children aged between 7 and 11 years old. | |
| Not routine scale and polish. Study compared 2 different methods of scaling (manual versus ultrasonic scaling). | |
| Not routine scale and polish. This study evaluated the effects of routine and intensified dental care and disease prevention in persons with human immunodeficiency virus (HIV). Study involved 1 control group ('standard care group') and 1 treatment group ('enhanced care group'). The standard care group received free professional dental treatment as needed and desired, including semi‐annual professional prophylaxes and checkups (3 per subject, at baseline, 6 months and 1 year). The enhanced care group received standard care plus additional free professional prophylaxes (every 2 months) and twice‐daily chlorhexidine antiseptic mouthrinses (excluded from review due to adjunctive use of chlorhexidine). | |
| Not a randomised controlled trial. Study examined the effects of an oral health programme on the occurrence of oral candidosis in residents in a long‐term care facility. 2 groups of residents were formed in this study. The authors state that random allocation was 'ruled out' and all the residents of each ward were assigned to 1 of the 2 groups. The study appears to have been carried out in the same long‐term care facility as Mojon 1998. | |
| Not routine scale and polish. Split‐mouth design: full power versus half power ultrasonic scaling. | |
| Randomisation not mentioned. One of the study authors was contacted by the review team but failed to respond to a second e‐mail request for further information. | |
| Not a randomised controlled trial. This study was a field trial of a community‐based periodontal disease prevention programme in a developing nation. The authors state that allocation of villages to periodontal disease prevention programmes was on an 'arbitrary basis' and was also dependent on the facilities available. | |
| Not a randomised controlled trial. This study examined the long‐term impact of 2 dental delivery systems on children's oral health. It was not possible to determine any differences in the provision of scale and polish treatments to both groups. On reviewing an earlier paper (Bentley 1983) describing the procedure for forming the 2 study groups, it became evident that the randomisation procedure used was compromised. After first siblings were randomly assigned, their brothers or sisters or both were removed from the subsequent assignment process and given the same assignment. | |
| Study included periodontal patients in maintenance phase. | |
| Not routine scale and polish. Patients randomised to receive the intervention were taught to self scale using a dentiscope, a large plane mouth mirror and a scaler. The control group received scaling and oral hygiene instruction limited to 3 hours over 4 or 5 visits. | |
| Not routine scale and polish. This study compared the effectiveness of 2 oral hygiene regimens ('Keyes' method' versus 'conventional oral hygiene instruction'). | |
| Not a randomised controlled trial. In this study the treatment and control groups were formed according to the age of participants. | |
| Not a randomised controlled trial. This study was a 3‐phase prospective study examining the effects of a long‐term preventive programme for mothers and children starting during pregnancy ‐ there were no randomised comparison groups. | |
| All patients received a scale and polish. No control group. | |
| Not routine scale and polish. In this study each quadrant of a participating patient's dentition was randomly assigned to 1 of 4 treatment types: Quadrant 1 (surgical pocket elimination); Quadrant 2 (modified Widman flap surgery); Quadrant 3 (subgingival curettage); Quadrant 4 (thorough scaling and root planing by the periodontist as a principally 'non‐surgical' control area). | |
| Not routine scale and polish. This study compared the use of a Vector™ scaling system and a piezo‐electric scaler. | |
| Not a randomised controlled trial. In this study only 1 group of patients was formed and all received the same level of treatment (ultrasonic scaling and root planing). | |
| Not a randomised controlled trial. Study used a split‐mouth experimental design. However, allocation to 'test' and 'control' sides was not random. | |
| Interventions confounded by other things. 1 group had a scale and polish on 2 quadrants so a split‐mouth design. | |
| Not routine scale and polish. In this study coronal scaling was used as a 'control' in 1 quadrant (Quadrant A) for 3 'treatment' quadrants: Quadrant B: coronal and subgingival scaling and root planing; Quadrant C: coronal and subgingival scaling and root planing followed by modified Widman surgery; Quadrant D: coronal and subgingival scaling and root planing followed by flap with osseous resection surgery. | |
| Patients had partial dentures. | |
| Not a randomised controlled trial. In this study participants were assigned (not a random assignment) either to 'individualised recall' or to 'annual recall' examinations. | |
| Not routine scale and polish. In this study participants were randomised to 4 treatment groups: 1) scaling and root planing alone, 2) scaling and root planing plus antimicrobial therapy (minocycline gel), 3) scaling and root planing plus antimicrobial therapy (tetracycline fibres), and 4) scaling and root planing plus antimicrobial therapy (metronidazole gel). | |
| Not a randomised controlled trial. This study examined the cost and effectiveness of various types and combinations of school‐based preventive dental care procedures. Schools (rather than individual children) were assigned to regimens in a way that balanced baseline decay level, numbers of children and racial mix across treatment regimens. | |
| Not routine scale and polish. This study compared scaling and root planing to full mouth scaling in a sample of 37 male subjects with moderate chronic periodontitis. | |
| Not routine scale and polish. This study compared oral hygiene instructions alone or in combination with metronidazole 25% gel or subgingival scaling with or without metronidazole gel in the treatment of new, residual or recurrent periodontal pockets in patients previously treated for periodontitis. | |
| Not a randomised controlled trial. Pseudo‐randomised: order of outpatient visits used to randomly assign patients to intervention and control groups. | |
| Randomised split‐mouth design on contralateral quadrants, single intervention given once. | |
| Unclear if randomised. 550 employees of both sexes aged between 25 and 44 were selected using "stratified random sampling criteria". Patients were then "divided" into 4 groups. Group A: oral hygiene group (n = 195), group B: scaling (n = 148), Group C: scaling and oral hygiene (n = 145), group D: control (n = 62). | |
| Study included patients with treated periodontal disease and were on different maintenance schedules. | |
| Not routine scale and polish. Patients were randomly assigned (following debridement) to receive either metronidazole or doxycycline or placebo. | |
| Not routine scale and polish. This study randomised 870 pregnant women with gingivitis to periodontal treatment before 28 weeks gestation or a control group who received periodontal treatment after delivery. Periodontal therapy consisted of plaque control, scaling and daily rinsing with 0.12% chlorhexidine. Maintenance therapy was provided every 2 or 3 weeks until delivery. Excluded due to the use of chlorhexidine. | |
| Not a randomised controlled trial. Participants were allocated to treatment (18‐month recall) and control (12‐month recall) groups alphabetically according to their surname. Authors also state that "when allocating the children into the 2 groups geography and caries‐activity was taken into consideration." | |
| Not routine scale and polish. Split‐mouth. Scale and polish versus waterjet. | |
| Randomisation not mentioned (abstract). This study divided patients into 2 groups. Group 1 received prophylaxis and maintained usual oral hygiene while group 2 carried out usual oral hygiene only. | |
| Not a randomised controlled trial. The aim of this study was to evaluate the effectiveness of a comprehensive oral health programme for residents of a long‐term care facility. 2 groups were formed: 1 group comprised of residents from 5 wards; the other group comprised of residents from 7 wards. The assignment of wards to each group took into account the location of the ward. 1 of the groups was then randomly selected as the experimental group. The study appears to have been carried out in the same long‐term care facility as Budtz‐Jorgensen 2000. | |
| Not routine scale and polish. This study compared the subgingival application of amino acid glycerine powder to scaling and root planing. | |
| Study included patients post‐periodontal surgery. | |
| Children with mixed dentition at baseline. This study randomised 7‐year old children to 2 groups: the intervention group received mechanical tooth cleaning every 2 weeks while the control group were untreated. | |
| Not routine scale and polish. In this study subjects were randomly assigned to 1 of 4 experimental groups or a control group. The control group (Group 1) received 'usual care' from a public health department or private practitioner. Group 2 received an educational programme of 2 hours duration implemented twice a year. Group 3 received the educational programme plus a chlorhexidine rinse weekly. Group 4 received the education and chlorhexidine interventions and a fluoride varnish application by a dental hygienist twice a year. Group 5 received all of the above interventions as well as scaling and root planing by a dental hygienist every 6 months throughout the 3‐year study. | |
| Interventions not relevant. This randomised controlled trial was designed to test the effectiveness (in high caries risk patients) of an intensified preventative regimen. The effects of scaling and polishing were not examine in this trial. | |
| Not a randomised controlled trial. In this study, following the initial examination, 391 subjects were divided into 4 experimental groups. First, 3 age groups were formed and within each of these age groups equal numbers of individuals were matched into the 4 experimental groups based on the number of remaining teeth, number of decayed and filled tooth surfaces, number of decayed surfaces, full mouth plaque scores and mean probing depth. | |
| Study included patients with advanced periodontal disease. | |
| Not routine scale and polish. 2 studies. In study 1 (2‐year clinical study), 75 patients were randomly distributed into intervention (professional cleaning) and control groups. Patients were additionally randomly distributed to receive 1 of 5 surgical procedures: the apically repositioned flap operation including elimination of bony fragments, the apically repositioned flap operation including curettage of bony defects but without removal of bone, the Widman flap technique including elimination of bony defects, the Widman flap technique including curettage of bony defects but without removal of bone and gingivectomy. After surgery, the teeth of patients in the intervention arm were professionally cleaned once a fortnight during a 2‐year period. The patients in the control arm were recalled once a year for supragingival scaling and polishing. No data from this study are reported in this article. Only the 50 patients in the treatment arm of the 2‐year clinical study progressed to the 6‐year clinical study, while the 25 control patients were withdrawn. | |
| Randomisation not mentioned (abstract). In this study 45 schoolchildren were divided into 3 groups. Group A received toothbrushing and dental floss use under supervision. Group B received professional prophylaxis. Group C received non‐supervised toothbrushing. | |
| Unclear if study was randomised (paper in German). This study was partially translated (Material and methods section) with a view to determining its eligibility. However, we were unable to ascertain if it was a randomised trial. The authors state that "2 comparable groups of 18 or 20 patients were studied. A year ago those patients were treated with cast removable partial dentures at the department of Stomatology of the medical academy Erfurt." | |
| No scale and polish. This study compared professional oral care performed by a hygienist (15 minutes of instructions on mouth cleaning and on Bass toothbrushing method) with toothbrushing and mouth rinsing by patients themselves. | |
| Not routine scale and polish. The purpose of this study was to evaluate the effect of subgingival scaling versus subginigival pocket irrigation with 0.1% chlorhexidine or saline controls. | |
| Unclear if study was randomised. Unable to contact authors to determine if the study was a randomised controlled trial (paper in German). | |
| Not routine scale and polish. The purpose of this study was to compare three protocols for non‐surgical periodontal therapy. Patients were randomised to receive either scaling and root planing quadrant by quadrant at weekly intervals (control group), full mouth scaling and root planing performed over 2 consecutive days (FM group), or full mouth scaling and root planing performed over 2 consecutive days combined with the administration of antibiotics (FMa group). | |
| 4 centres randomised to 4 interventions. Cluster randomised controlled trial with single cluster per intervention so unable to use data at all. | |
| Not routine scale and polish. Patients were randomised to 4 groups. Group 1 received initial scaling and daily polishing, group 2 received daily polishing without initial scaling, group 3 received initial scaling without daily polishing and group 4 received no treatment. | |
| Not a randomised controlled trial. This study was carried out "to test the hypothesis that the development and progression of gingival inflammation and destructive periodontal disease are retarded in an oral environment in which high levels of hygiene are maintained." 2 groups (experimental and control) were matched on the basis of periodontal and oral hygiene status, past caries experience, age and sex. The experimental group were given a series of frequent oral prophylaxes combined with oral hygiene instruction and dental health education. Subjects in the control groups received no attention from the study team except for annual examinations. | |
| Unclear how groups were formed, unlikely to be randomised. | |
| Follow‐up less than 6 months. In this study 120 Dutch army recruits in 2 camps were randomised to receive no treatment (group A), professional prophylaxis (group B), dental health instruction (group C) or both prophylaxis and dental health instruction (group D). Patients were examined at initiation of the study, after 1 month and 3 months. | |
| Not a randomised controlled trial (after translation from Japanese). | |
| No scale and polish. This study looked at the effect of pre‐experimental maintenance on the development of gingivitis. | |
| Interventions not relevant. In this randomised controlled trial participants were randomly allocated to recall examination at either 12 months or 24 months. Scale and polish treatments (if any) provided at recall were not reported in this paper. Outcomes reported were clinical examination time, treatment time and the DMFS increment during the 2‐year study period. | |
| Not routine scale and polish. This study compared air polishing to ultrasonic instruments in a split‐mouth study. | |
| Included patients had periodontal surgery. | |
| Not routine scale and polish. Split‐mouth study. 2 quadrants of each patient were designated test group, while the other 2 were identified as control. Patients in the test arm received supragingival plaque control. While patients in the control arm received subgingival scaling and root planing. | |
| Length of follow‐up less than 6 months. Single episode of scaling. Participant characteristics not presented. This study examined the efficiency of 2 professionals (1 dentist, 1 dental hygienist) in removing supragingival calculus. Participants were concomitantly participating in a tartar control dentifrice trial. Outcomes: total developed force, average force per stroke, total strokes and Volpe‐Manhold‐Index (VMI) grading. | |
| Length of follow‐up less than 6 months. Split‐mouth study. 67 patients received supragingival scaling on the 6 mandibular teeth. Quadrants were then randomly selected to be polished or not with a rubber cup and pumice. Outcomes assessed at 1, 2 and 3 weeks post‐treatment. | |
| Not routine scale and polish. Split‐mouth study. Active treatment included subgingival scaling, metronidazole 25% gel and subgingival scaling plus metronidazole 25% gel. A control group was also employed. | |
| All patients received scale and polish.This study examined the effectiveness of 1 versus 2 preventive advice sessions. Both treatment and control groups were given 30‐minute scale and polish treatments. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | IQUAD: Improving the Quality of Dentistry |
| Methods | A 5‐year multicentre, randomised, open trial with blinded outcome evaluation based in dental primary care in Scotland and the North East of England. Dental practices are cluster randomised to provide routine oral hygiene advice or personalised oral hygiene advice. Both dentists and DCPs will undertake the scale and polish treatments. To test the effects of Periodontal Instrumentation each participant will be randomised to 1 of 3 groups: no periodontal instrumentation, 6‐monthly periodontal instrumentation (current practice), or 12‐monthly periodontal instrumentation |
| Participants | Dentate adults with BPE <= 3 |
| Interventions | No periodontal instrumentation, 6‐monthly periodontal instrumentation (current practice), or 12‐monthly periodontal instrumentation |
| Outcomes | Primary outcomes: Clinical: gingival inflammation/bleeding on probing at the gingival margin measured by the Gingival Index of Loe. Patient‐centred: oral hygiene self efficacy Economic: net benefits (mean willingness to pay minus mean costs). Measured at 3 years |
| Starting date | 2012 |
| Contact information | |
| Notes | HTA funded ISRCTN56465715. A multicentre randomised controlled trial comparing oral hygiene advice and periodontal instrumentation for the prevention and management of periodontal disease in dentate adults attending dental primary care |
BPE = Basic Periodontal Examination; DCPs = dental care professionals
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingivitis at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1 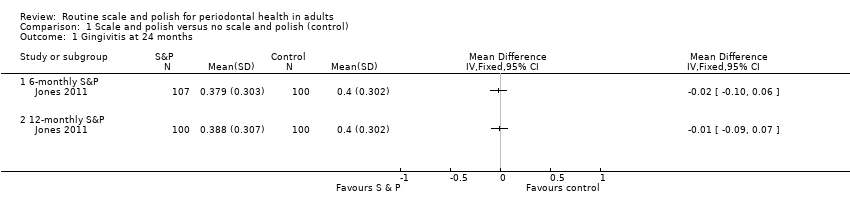 Comparison 1 Scale and polish versus no scale and polish (control), Outcome 1 Gingivitis at 24 months. | ||||
| 1.1 6‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 12‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Calculus at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Scale and polish versus no scale and polish (control), Outcome 2 Calculus at 24 months. | ||||
| 2.1 6‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 12‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Plaque at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 Scale and polish versus no scale and polish (control), Outcome 3 Plaque at 24 months. | ||||
| 3.1 6‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 12‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingivitis at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Scale and polish at a fixed interval versus scale and polish in response to the signs and/or symptoms of perio, Outcome 1 Gingivitis at 24 months. | ||||
| 2 Plaque at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2 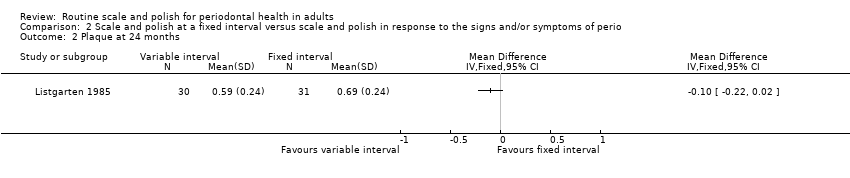 Comparison 2 Scale and polish at a fixed interval versus scale and polish in response to the signs and/or symptoms of perio, Outcome 2 Plaque at 24 months. | ||||
| 3 Pocket depth at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 Scale and polish at a fixed interval versus scale and polish in response to the signs and/or symptoms of perio, Outcome 3 Pocket depth at 24 months. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 S&P: 3‐monthly versus 6‐monthly (with OHI) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1 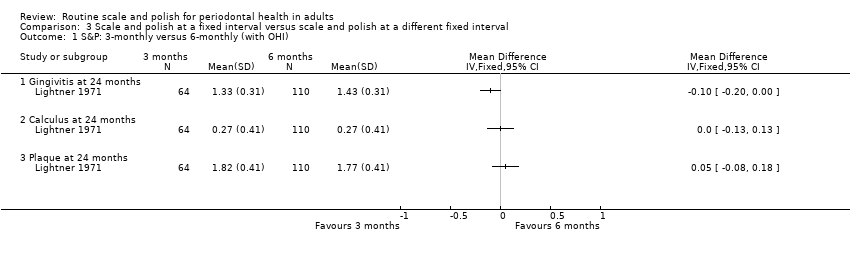 Comparison 3 Scale and polish at a fixed interval versus scale and polish at a different fixed interval, Outcome 1 S&P: 3‐monthly versus 6‐monthly (with OHI). | ||||
| 1.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 S&P: 3‐monthly versus 12‐monthly (with OHI) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.2  Comparison 3 Scale and polish at a fixed interval versus scale and polish at a different fixed interval, Outcome 2 S&P: 3‐monthly versus 12‐monthly (with OHI). | ||||
| 2.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 S&P: 3‐monthly versus 12‐monthly (without OHI) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.3  Comparison 3 Scale and polish at a fixed interval versus scale and polish at a different fixed interval, Outcome 3 S&P: 3‐monthly versus 12‐monthly (without OHI). | ||||
| 3.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 S&P: 6‐monthly versus 12‐monthly (with OHI) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.4  Comparison 3 Scale and polish at a fixed interval versus scale and polish at a different fixed interval, Outcome 4 S&P: 6‐monthly versus 12‐monthly (with OHI). | ||||
| 4.1 Gingivitis at 24 months | 2 | 438 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.27, 0.10] |
| 4.2 Calculus at 24 months | 2 | 438 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐0.44, ‐0.06] |
| 4.3 Plaque at 24 months | 2 | 438 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.35, 0.03] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 S&P every 3 months with OHI versus without OHI Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.1  Comparison 4 Scale and polish at a fixed interval with OHI versus scale and polish without OHI at the same fixed interval, Outcome 1 S&P every 3 months with OHI versus without OHI. | ||||
| 1.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 S&P every 12 months with OHI versus without OHI Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.2 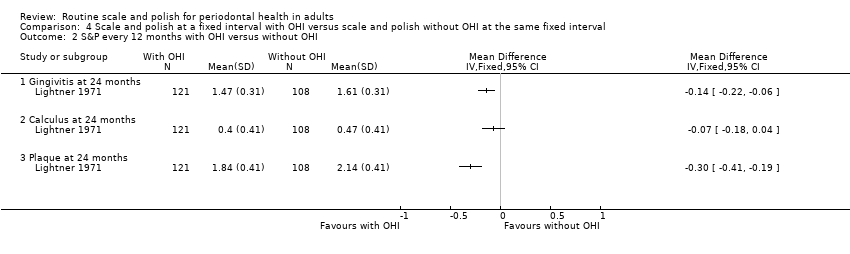 Comparison 4 Scale and polish at a fixed interval with OHI versus scale and polish without OHI at the same fixed interval, Outcome 2 S&P every 12 months with OHI versus without OHI. | ||||
| 2.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Scale and polish versus no scale and polish (control), Outcome 1 Gingivitis at 24 months.

Comparison 1 Scale and polish versus no scale and polish (control), Outcome 2 Calculus at 24 months.

Comparison 1 Scale and polish versus no scale and polish (control), Outcome 3 Plaque at 24 months.
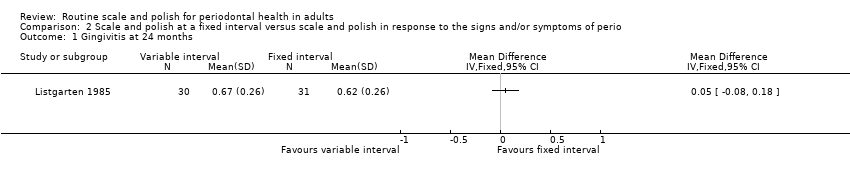
Comparison 2 Scale and polish at a fixed interval versus scale and polish in response to the signs and/or symptoms of perio, Outcome 1 Gingivitis at 24 months.

Comparison 2 Scale and polish at a fixed interval versus scale and polish in response to the signs and/or symptoms of perio, Outcome 2 Plaque at 24 months.

Comparison 2 Scale and polish at a fixed interval versus scale and polish in response to the signs and/or symptoms of perio, Outcome 3 Pocket depth at 24 months.
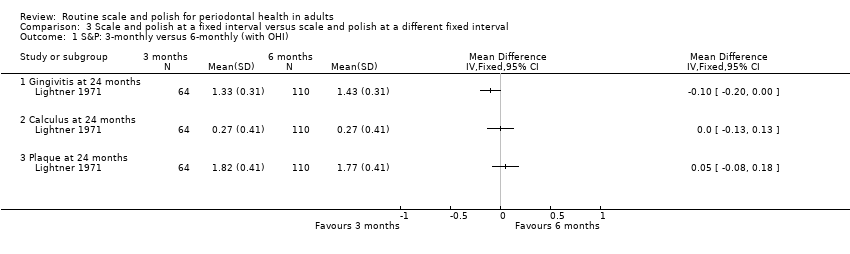
Comparison 3 Scale and polish at a fixed interval versus scale and polish at a different fixed interval, Outcome 1 S&P: 3‐monthly versus 6‐monthly (with OHI).

Comparison 3 Scale and polish at a fixed interval versus scale and polish at a different fixed interval, Outcome 2 S&P: 3‐monthly versus 12‐monthly (with OHI).
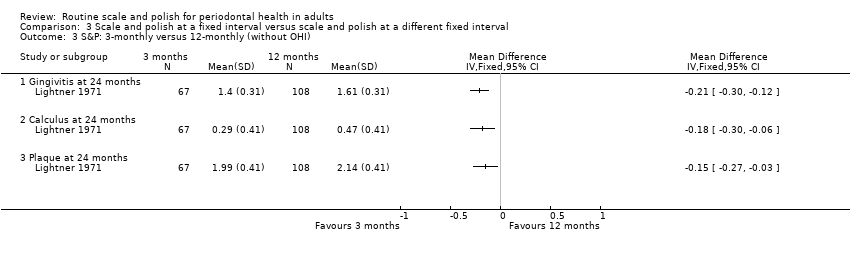
Comparison 3 Scale and polish at a fixed interval versus scale and polish at a different fixed interval, Outcome 3 S&P: 3‐monthly versus 12‐monthly (without OHI).

Comparison 3 Scale and polish at a fixed interval versus scale and polish at a different fixed interval, Outcome 4 S&P: 6‐monthly versus 12‐monthly (with OHI).

Comparison 4 Scale and polish at a fixed interval with OHI versus scale and polish without OHI at the same fixed interval, Outcome 1 S&P every 3 months with OHI versus without OHI.

Comparison 4 Scale and polish at a fixed interval with OHI versus scale and polish without OHI at the same fixed interval, Outcome 2 S&P every 12 months with OHI versus without OHI.
| Routine scale and polish compared with no treatment for periodontal health | ||||
| Patient or population: Healthy dentate adults Settings: General dental practice Intervention: Routine scale and polish (either 6‐monthly or 12‐monthly) Comparison: No treatment | ||||
| Outcomes | Relative effect | No of participants | Quality of the evidence | Comments |
| Gingivitis (proportion of index sites bleeding) at 24 months 6‐monthly scale and polish Mean proportion in control group is 0.40 sites | MD ‐0.02 (‐0.10 to 0.06) | 1 study1 (207 participants) | ⊕⊕⊝⊝ | The results for 12‐monthly scale and polish were similar and also not significant |
| Calculus (mean depth in mm at index sites) at 24 months 6‐monthly scale and polish Mean in control group is 0.95 mm | MD ‐0.24 (‐0.51 to 0.03) | 1 study1 (207 participants) | ⊕⊕⊝⊝ | The results for 12‐monthly scale and polish were similar and also not significant |
| Plaque (proportion of index sites with plaque) at 24 months 6‐monthly scale and polish Mean proportion in control group is 0.44 sites | MD ‐0.04 (‐0.13 to 0.05) | 1 study1 (207 participants) | ⊕⊕⊝⊝ | The results for 12‐monthly scale and polish were similar and also not significant |
| CI: confidence interval; MD: mean difference | ||||
| GRADE Working Group grades of evidence | ||||
| 1Single study at unclear risk of bias | ||||
| Routine scale and polish at different frequencies for periodontal health | ||||
| Patient or population: Healthy dentate young adults Settings: Air Force Academy Intervention: Routine scale and polish every 6 months with oral hygiene instruction Comparison: Routine scale and polish every 12 months with oral hygiene instruction | ||||
| Outcomes | Relative effect | No of participants | Quality of the evidence | Comments |
| Gingivitis different indices used | SMD ‐0.08 (‐0.27 to 0.10) | 2 studies1 (438 participants) | ⊕⊕⊝⊝ | The results for comparing 3 versus 12 months are significant but based on only 1 study |
| Calculus different indices used | SMD ‐0.25 (‐0.44 to ‐0.06) | 2 studies1 (438 participants) | ⊕⊕⊝⊝ | The results for comparing 3 versus 12 months are significant but based on only 1 study |
| Plaque different indices used | SMD ‐0.16 (‐0.35 to 0.03) | 2 studies1 (438 participants) | ⊕⊕⊝⊝ | The results for comparing 3 versus 12 months are generally not significant |
| CI: confidence interval; MD: mean difference; SMD: standardised mean difference | ||||
| GRADE Working Group grades of evidence | ||||
| 12 studies at unclear risk of bias | ||||
| Routine scale and polish with and without oral hygiene instruction for periodontal health | ||||
| Patient or population: Healthy dentate young adults Settings: Air Force Academy Intervention: Routine scale and polish with oral hygiene instruction Comparison: Routine scale and polish without oral hygiene instruction | ||||
| Outcomes | Relative effect | No of participants | Quality of the evidence | Comments |
| Gingivitis (mean on 0‐3 scale) at 24 months 3‐monthly scale and polish Mean gingivitis score (0‐3 scale) in control group is 1.40 | MD ‐0.07 (‐0.18 to 0.04) | 1 study1 (131 participants) | ⊕⊕⊝⊝ | Results for 12‐monthly scale and polish was significant |
| Calculus (mean on 0‐3 scale) at 24 months 3‐monthly scale and polish Mean calculus score (0‐3 scale) in control group is 0.29 mm | MD ‐0.02 (‐0.16 to 0.12) | 1 study1 (131 participants) | ⊕⊕⊝⊝ | Results for 12‐monthly scale and polish was similar |
| Plaque (mean on 0‐3 scale) at 24 months 3‐monthly scale and polish Mean plaque score (0‐3 scale) in control group is 1.99 | MD ‐0.17 (‐0.31 to ‐0.03) | 1 study1 (131 participants) | ⊕⊕⊝⊝ | Results for 12‐monthly scale and polish was not significant |
| CI: confidence interval; MD: mean difference | ||||
| GRADE Working Group grades of evidence | ||||
| 1Single study at unclear risk of bias | ||||
| Routine scale and polish undertaken by dentist or dental care professional for periodontal health | ||||
| Patient or population: Healthy dentate adults Settings: General dental practice Intervention: Routine scale and polish by dental professional Comparison: Routine scale and polish by dentist | ||||
| Outcomes | Relative effect | No of participants | Quality of the evidence | Comments |
| Gingivitis | No studies | |||
| Calculus | No studies | |||
| Plaque | No studies | |||
| GRADE Working Group grades of evidence | ||||
| Study | Notes/references | Plaque | Calculus | Gingivitis/bleeding | Pocket depth | Attachment change | Periodontal indices |
| Jones 2011 | For references to index teeth used in trial seeRamfjord 1959 | Visual presence of any plaque on the 6 (Ramfjord) index teeth according to a dichotomous scale: plaque present/not present | Measurement of calculus in mm: 1 measurement, | Bleeding from the gingival margin of 6 (Ramfjord) index teeth. Bleeding was detected by running a blunt‐ended (PCP‐10) probe gently around the gingival margin of the tooth at a 60° | Not reported | Not reported | Not reported |
| Lightner 1971 | For references to indices used in trial seeO' Leary 1967. The examination system used was the Periodontal Screening Examination (O' Leary 1967). The mouth is divided into 6 segments. The highest score found for any tooth in a segment is recorded as the score for the segment | Plaque index (no description of the precise criteria used). Plaque scores range from 0 to 3. Data reported as mean plaque index scores | Hard deposit index. Hard deposit scores range from 0 to 3 (precise criteria not described). Data presented as mean hard deposit index scores | Gingival index (precise criteria not described). Gingival scores range from 0 to 3. Data reported as mean gingival index scores | Not reported | Loss of epithelial attachment. Data reported as mean attachment loss (mm). Reported data not used in this review as no standard deviations provided | Periodontal index. Possible scores of 0, 4, 5 or 6 (criteria described in full in the paper). To simplify the statistical handling of data, scores 4, 5 and 6 were transformed to 1, 2 and 3 respectively. Reported data were not used in this review as presented in an inappropriate format |
| Listgarten 1985 | For references to indices used in trial seeLoe 1967 | Modified plaque index. Index based on a 0‐3 score (Loe 1967). Each tooth was scored on the mid‐buccal and mid‐lingual surfaces as well as on the mesial buccal surface. The mean values for the whole mouth obtained by adding all mid‐buccal and mid‐lingual and the doubled value of the mesial buccal scores and dividing by the number of surfaces at risk. Data reported as mean plaque index scores for control and test groups | Not reported | Modified gingival index (Loe 1967). Index is based on a 0‐3 score. Data reported as mean gingival index scores for control and test groups for all surfaces measured at each examination | Probing depth. Data reported as mean probing depth (mm). Probing depth recorded to the nearest mm with uniform probes calibrated in mm, with a tip diameter of 0.35 mm | Recession recorded to the nearest mm as the distance from the gingival margin to the cemento‐enamel junction (only when a distinct cemento‐enamel junction was identifiable) | Not reported |
| mm = millimetre | |||||||
| Frequency of scale and polish | Data points | Plaque | Calculus | Gingivitis/bleeding | Pocket depth | Attachment change |
| 6 months | 24 | Jones 2011 | Jones 2011 | Jones 2011 | ||
| 12 months | 24 | Jones 2011 | Jones 2011 | Jones 2011 |
| Frequency of scale and polish | Data points | Plaque | Calculus | Gingivitis/bleeding | Pocket depth | Attachment change |
| 6 months | 6 | Listgarten 1985 | Listgarten 1985 | Listgarten 1985 | ||
| 12 | Listgarten 1985 | Listgarten 1985 | Listgarten 1985 | |||
| 18 | Listgarten 1985 | Listgarten 1985 | Listgarten 1985 | |||
| 24 | Listgarten 1985 | Listgarten 1985 | Listgarten 1985 | |||
| 30 | Listgarten 1985 | Listgarten 1985 | Listgarten 1985 | |||
| 36 | Listgarten 1985 | Listgarten 1985 | Listgarten 1985 |
| Frequency of scale and polish | Data points | Plaque | Calculus | Gingivitis/bleeding | Pocket depth | Attachment change | Periodontal indices |
| 3 months versus 6 months | 12 | Lightner 1971 | Lightner 1971 | Lightner 1971 | |||
| 24 | Lightner 1971 | Lightner 1971 | Lightner 1971 | ||||
| 36 | Lightner 1971 | Lightner 1971 | Lightner 1971 | ||||
| 46 | Lightner 1971 | Lightner 1971 | Lightner 1971 | ||||
| 3 months versus 12 months | 24 | Lightner 1971 | Lightner 1971 | Lightner 1971 | |||
| 36 | Lightner 1971 | Lightner 1971 | Lightner 1971 | ||||
| 46 | Lightner 1971 | Lightner 1971 | Lightner 1971 | ||||
| 6 months versus 12 months | 24 | Lightner 1971 Jones 2011 | Lightner 1971 Jones 2011 | Lightner 1971 Joners 2011 | |||
| 36 | Lightner 1971 | Lightner 1971 | Lightner 1973 | ||||
| 46 | Lightner 1971 | Lightner 1971 | Lightner 1971 | ||||
| Outcome measured | Variable interval | Fixed interval | ||||||
| Mean | SD | n | Mean | SD | n | MD (95% CI) | P value | |
| Gingivitis | ||||||||
| 6 months | 0.3 | 0.26 | 30 | 0.29 | 0.26 | 31 | 0.01 (‐0.12, 0.14) | 0.88 |
| 12 | 0.4 | 0.26 | 30 | 0.42 | 0.26 | 31 | ‐0.02 (‐0.15, 0.11) | 0.76 |
| 18 | 0.52 | 0.26 | 30 | 0.59 | 0.26 | 31 | ‐0.07 (‐0.20, 0.06) | 0.29 |
| 24 | 0.67 | 0.26 | 30 | 0.62 | 0.26 | 31 | 0.05 (‐0.08, 0.18) | 0.45 |
| 30 | 0.7 | 0.26 | 30 | 0.7 | 0.26 | 31 | 0.00 (‐0.13, 0.13) | 1.00 |
| 36 | 0.63 | 0.26 | 30 | 0.67 | 0.26 | 31 | ‐0.04 (‐0.17, 0.09) | 0.55 |
|
| ||||||||
| Plaque |
|
| ||||||
| 6 months | 0.43 | 0.24 | 30 | 0.53 | 0.24 | 31 | ‐0.10 (‐0.22, 0.02) | 0.10 |
| 12 | 0.55 | 0.24 | 30 | 0.62 | 0.24 | 31 | ‐0.07 (‐0.19, 0.05) | 0.25 |
| 18 | 0.6 | 0.24 | 30 | 0.7 | 0.24 | 31 | ‐0.10 (‐0.22, 0.02) | 0.10 |
| 24 | 0.59 | 0.24 | 30 | 0.69 | 0.24 | 31 | ‐0.10 (‐0.22, 0.02) | 0.10 |
| 30 | 0.68 | 0.24 | 30 | 0.74 | 0.24 | 31 | ‐0.06 (‐0.18, 0.06) | 0.33 |
| 36 | 0.6 | 0.24 | 30 | 0.68 | 0.24 | 31 | ‐0.08 (‐0.20, 0.04) | 0.19 |
|
| ||||||||
| Pocket depth |
|
|
|
|
|
|
|
|
| 6 months | 1.65 | 0.19 | 30 | 1.7 | 0.19 | 31 | ‐0.05 (‐0.15, 0.05) | 0.19 |
| 12 | 1.65 | 0.19 | 30 | 1.7 | 0.19 | 31 | ‐0.05 (‐0.15, 0.05) | 0.19 |
| 18 | 1.65 | 0.17 | 30 | 1.7 | 0.17 | 31 | ‐0.05 (‐0.14, 0.04) | 0.17 |
| 24 | 1.65 | 0.17 | 30 | 1.7 | 0.17 | 31 | ‐0.05 (‐0.14, 0.04) | 0.17 |
| 30 | 1.65 | 0.18 | 30 | 1.7 | 0.17 | 31 | ‐0.05 (‐0.14, 0.04) | 0.18 |
| 36 | 1.65 | 0.17 | 30 | 1.7 | 0.17 | 31 | ‐0.05 (‐0.14, 0.04) | 0.17 |
| CI = confidence interval; MD = mean difference; SD = standard deviation | ||||||||
| Comparison | Outcome measured | Variable interval | Fixed interval | MD (95% CI) | P value | ||||
| 3 versus 6 months | Gingivitis | Mean | SD | n | Mean | SD | n |
|
|
| Lightner 1971 | 12 | 1.58 | 0.31 | 64 | 1.63 | 0.31 | 110 | ‐0.05 (‐0.15, 0.05) | 0.30 |
| Lightner 1971 | 24 | 1.33 | 0.31 | 64 | 1.43 | 0.31 | 110 | ‐0.10 (‐0.20, ‐0.00) | 0.04 |
| Lightner 1971 | 36 | 1.27 | 0.31 | 64 | 1.34 | 0.31 | 110 | ‐0.07 (‐0.17, 0.03) | 0.15 |
| Lightner 1971 | 48 | 1.25 | 0.31 | 64 | 1.34 | 0.31 | 110 | ‐0.09 (‐0.19, 0.01) | 0.06 |
|
| |||||||||
|
| Calculus |
|
|
|
|
|
|
|
|
| Lightner 1971 | 12 | 0.26 | 0.41 | 64 | 0.3 | 0.41 | 110 | ‐0.04 (‐0.17, 0.09) | 0.53 |
| Lightner 1971 | 24 | 0.27 | 0.41 | 64 | 0.27 | 0.41 | 110 | 0.00 (‐0.13, 0.13) | 1.00 |
| Lightner 1971 | 36 | 0.22 | 0.41 | 64 | 0.23 | 0.41 | 110 | ‐0.01 (‐0.14, 0.12) | 0.88 |
| Lightner 1971 | 48 | 0.13 | 0.41 | 64 | 0.15 | 0.41 | 110 | ‐0.02 (‐0.15, 0.11) | 0.76 |
|
| Plaque |
|
|
|
|
|
|
|
|
| Lightner 1971 | 12 | 1.85 | 0.41 | 64 | 1.84 | 0.41 | 110 | 0.01 (‐0.12, 0.14) | 0.88 |
| Lightner 1971 | 24 | 1.82 | 0.41 | 64 | 1.77 | 0.41 | 110 | 0.05 (‐0.08, 0.18) | 0.44 |
| Lightner 1971 | 36 | 1.53 | 0.41 | 64 | 1.58 | 0.41 | 110 | ‐0.05 (‐0.18, 0.08) | 0.44 |
| Lightner 1971 | 48 | 1.48 | 0.41 | 64 | 1.47 | 0.41 | 110 | 0.01 (‐0.12, 0.14) | 0.88 |
|
| |||||||||
| 3 versus 12 months (with OHI) | Gingivitis |
|
|
|
|
|
|
|
|
| Lightner 1971 | 24 | 1.33 | 0.31 | 64 | 1.47 | 0.31 | 121 | ‐0.14 (‐0.23, ‐0.05) | 0.003 |
| Lightner 1971 | 36 | 1.27 | 0.31 | 64 | 1.39 | 0.31 | 121 | ‐0.12 (‐0.21, ‐0.03) | 0.01 |
| Lightner 1971 | 48 | 1.25 | 0.31 | 64 | 1.4 | 0.31 | 121 | ‐0.15 (‐0.24, ‐0.06) | 0.002 |
|
| |||||||||
|
| Calculus |
|
|
|
|
|
|
|
|
| Lightner 1971 | 24 | 0.27 | 0.41 | 64 | 0.4 | 0.41 | 121 | ‐0.13 (‐0.25, ‐0.01) | 0.04 |
| Lightner 1971 | 36 | 0.22 | 0.41 | 64 | 0.32 | 0.41 | 121 | ‐0.10 (‐0.22, 0.02) | 0.11 |
| Lightner 1971 | 48 | 0.13 | 0.41 | 64 | 0.26 | 0.41 | 121 | ‐0.13 (‐0.25, ‐0.01) | 0.04 |
|
| |||||||||
|
| Plaque |
|
|
|
|
|
|
|
|
| Lightner 1971 | 24 | 1.82 | 0.41 | 64 | 1.84 | 0.41 | 121 | ‐0.02 (‐0.14, 0.10) | 0.75 |
| Lightner 1971 | 36 | 1.53 | 0.41 | 64 | 1.68 | 0.41 | 121 | ‐0.15 (‐0.27, ‐0.03) | 0.02 |
| Lightner 1971 | 48 | 1.48 | 0.41 | 64 | 1.53 | 0.41 | 121 | ‐0.05 (‐0.17, 0.07) | 0.43 |
|
|
|
|
|
|
|
|
|
|
|
| 3 versus 12 months (without OHI) | Gingivitis |
|
|
|
|
|
|
|
|
| Lightner 1971 | 24 | 1.4 | 0.31 | 67 | 1.61 | 0.31 | 108 | ‐0.21 (‐0.30, ‐0.12) | < 0.001 |
| Lightner 1971 | 36 | 1.41 | 0.31 | 67 | 1.56 | 0.31 | 108 | ‐0.15 (‐0.24, ‐0.06) | 0.002 |
| Lightner 1971 | 48 | 1.34 | 0.31 | 67 | 1.55 | 0.31 | 108 | ‐0.21 (‐0.30, ‐0.12) | < 0.001 |
|
| |||||||||
|
| Calculus |
|
|
|
|
|
|
|
|
| Lightner 1971 | 24 | 0.29 | 0.41 | 67 | 0.47 | 0.41 | 108 | ‐0.18 (‐0.30, ‐0.06) | 0.005 |
| Lightner 1971 | 36 | 0.29 | 0.41 | 67 | 0.45 | 0.41 | 108 | ‐0.16 (‐0.28, ‐0.04) | 0.01 |
| Lightner 1971 | 48 | 0.19 | 0.41 | 67 | 0.33 | 0.41 | 108 | ‐0.14 (‐0.26, ‐0.02) | 0.03 |
|
| |||||||||
|
| Plaque |
|
|
|
|
|
|
|
|
| Lightner 1971 | 24 | 1.99 | 0.41 | 67 | 2.14 | 0.41 | 108 | ‐0.15 (‐0.27, ‐0.03) | 0.02 |
| Lightner 1971 | 36 | 1.9 | 0.41 | 67 | 2.04 | 0.41 | 108 | ‐0.14 (‐0.26, ‐0.02) | 0.03 |
| Lightner 1971 | 48 | 1.75 | 0.41 | 67 | 1.93 | 0.41 | 108 | ‐0.18 (‐0.30, ‐0.06) | 0.005 |
|
| |||||||||
| 6 versus 12 months | Gingivitis |
|
|
|
|
|
|
|
|
| Jones 2011 | 24 | 0.379 | 0.303 | 107 | 0.388 | 0.307 | 100 | ‐0.01 (‐0.09, 0.07) | 0.03 |
| Lightner 1971 | 24 | 1.43 | 0.31 | 110 | 1.47 | 0.31 | 121 | ‐0.04 (‐0.12, 0.04) | 0.33 |
| Lightner 1971 | 36 | 1.34 | 0.31 | 110 | 1.39 | 0.31 | 121 | ‐0.05 (‐0.13, 0.03) | 0.22 |
| Lightner 1971 | 48 | 1.34 | 0.31 | 110 | 1.4 | 0.31 | 121 | ‐0.06 (‐0.14, 0.02) | 0.14 |
|
| |||||||||
|
| Calculus |
|
|
|
|
|
|
|
|
| Jones 2011 | 24 | 0.71 | 1.0 | 107 | 0.89 | 0.99 | 100 | ‐0.18 (‐0.45, 0.09) | 0.19 |
| Lightner 1971 | 24 | 0.27 | 0.41 | 110 | 0.4 | 0.41 | 121 | ‐0.13 (‐0.24, ‐0.02) | 0.02 |
| Lightner 1971 | 36 | 0.23 | 0.41 | 110 | 0.32 | 0.41 | 121 | ‐0.09 (‐0.20, 0.02) | 0.10 |
| Lightner 1971 | 48 | 0.15 | 0.41 | 110 | 0.26 | 0.41 | 121 | ‐0.11 (‐0.22, ‐0.00) | 0.04 |
|
| |||||||||
|
| Plaque |
|
|
|
|
|
|
|
|
| Jones 2011 | 24 | 0.394 | 0.342 | 107 | 0.435 | 0.347 | 100 | ‐0.04 (‐0.13, 0.05) | 0.39 |
| Lightner 1971 | 24 | 1.77 | 0.41 | 110 | 1.84 | 0.41 | 121 | ‐0.07 (‐0.18, 0.04) | 0.19 |
| Lightner 1971 | 36 | 1.58 | 0.41 | 110 | 1.68 | 0.41 | 121 | ‐0.10 (‐0.21, 0.01) | 0.06 |
| Lightner 1971 | 48 | 1.47 | 0.41 | 110 | 1.53 | 0.41 | 121 | ‐0.06 (‐0.17, 0.05) | 0.27 |
| CI = confidence interval; MD = mean difference; OHI = oral hygiene instruction; SD = standard deviation | |||||||||
| Comparison | Outcome measured (months) | OHI | Without OHI | MD (95% CI) | P value | ||||
| Scale and polish every 3 months | Gingivitis | Mean | SD | n | Mean | SD | n |
|
|
| Lightner 1971 | 12 | 1.58 | 0.31 | 64 | 1.65 | 0.31 | 67 | ‐0.07 (‐0.18, 0.04) | 0.20 |
| Lightner 1971 | 24 | 1.33 | 0.31 | 64 | 1.4 | 0.31 | 67 | ‐0.07 (‐0.18, 0.04) | 0.20 |
| Lightner 1971 | 36 | 1.27 | 0.31 | 64 | 1.41 | 0.31 | 67 | ‐0.14 (‐0.25, ‐0.03) | 0.01 |
| Lightner 1971 | 48 | 1.25 | 0.31 | 64 | 1.34 | 0.31 | 67 | ‐0.09 (‐0.20, 0.02) | 0.10 |
|
| |||||||||
|
| Calculus |
|
|
|
|
|
|
|
|
| Lightner 1971 | 12 | 0.26 | 0.41 | 64 | 0.31 | 0.41 | 67 | ‐0.05 (‐0.19, 0.09) | 0.49 |
| Lightner 1971 | 24 | 0.27 | 0.41 | 64 | 0.29 | 0.41 | 67 | ‐0.02 (‐0.16, 0.12) | 0.78 |
| Lightner 1971 | 36 | 0.22 | 0.41 | 64 | 0.29 | 0.41 | 67 | ‐0.07 (‐0.21, 0.07) | 0.33 |
| Lightner 1971 | 48 | 0.13 | 0.41 | 64 | 0.19 | 0.41 | 67 | ‐0.06 (‐0.20, 0.08) | 0.40 |
|
| |||||||||
|
| Plaque |
|
|
|
|
|
|
|
|
| Lightner 1971 | 12 | 1.85 | 0.41 | 64 | 2.12 | 0.41 | 67 | ‐0.27 (‐0.41, ‐0.13) | < 0.001 |
| Lightner 1971 | 24 | 1.82 | 0.41 | 64 | 1.99 | 0.41 | 67 | ‐0.17 (‐0.31, ‐0.03) | 0.02 |
| Lightner 1971 | 36 | 1.53 | 0.41 | 64 | 1.9 | 0.41 | 67 | ‐0.37 (‐0.51, ‐0.23) | < 0.001 |
| Lightner 1971 | 48 | 1.48 | 0.41 | 64 | 1.75 | 0.41 | 67 | ‐0.27 (‐0.41, ‐0.13) | < 0.001 |
|
| |||||||||
| Scale and polish every 12 months | Gingivitis |
|
|
|
|
|
|
|
|
| Lightner 1971 | 24 | 1.47 | 0.31 | 121 | 1.61 | 0.31 | 108 | ‐0.14 (‐0.22, ‐0.06) | < 0.001 |
| Lightner 1971 | 36 | 1.39 | 0.31 | 121 | 1.56 | 0.31 | 108 | ‐0.17 (‐0.25, ‐0.09) | < 0.001 |
| Lightner 1971 | 48 | 1.4 | 0.31 | 121 | 1.55 | 0.31 | 108 | ‐0.15 (‐0.23, ‐0.07) | < 0.001 |
|
| Calculus |
|
|
|
|
|
|
|
|
| Lightner 1971 | 24 | 0.4 | 0.41 | 121 | 0.47 | 0.41 | 108 | ‐0.07 (‐0.18, 0.04) | 0.20 |
| Lightner 1971 | 36 | 0.32 | 0.41 | 121 | 0.45 | 0.41 | 108 | ‐0.13 (‐0.24, ‐0.02) | 0.02 |
| Lightner 1971 | 48 | 0.26 | 0.41 | 121 | 0.33 | 0.41 | 108 | ‐0.07 (‐0.18, 0.04) | 0.20 |
|
| |||||||||
|
| Plaque |
|
|
|
|
|
|
|
|
| Lightner 1971 | 24 | 1.84 | 0.41 | 121 | 2.14 | 0.41 | 108 | ‐0.30 (‐0.41, ‐0.19) | < 0.001 |
| Lightner 1971 | 36 | 1.68 | 0.41 | 121 | 2.04 | 0.41 | 108 | ‐0.36 (‐0.47, ‐0.25) | < 0.001 |
| Lightner 1971 | 48 | 1.53 | 0.41 | 121 | 1.93 | 0.41 | 108 | ‐0.40 (‐0.51, ‐0.29) | < 0.001 |
| CI = confidence interval; MD = mean difference; OHI = oral hygiene instruction; SD = standard deviation | |||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingivitis at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 6‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 12‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Calculus at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 6‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 12‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Plaque at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 6‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 12‐monthly S&P | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingivitis at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Plaque at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Pocket depth at 24 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 S&P: 3‐monthly versus 6‐monthly (with OHI) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 S&P: 3‐monthly versus 12‐monthly (with OHI) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 S&P: 3‐monthly versus 12‐monthly (without OHI) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 S&P: 6‐monthly versus 12‐monthly (with OHI) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Gingivitis at 24 months | 2 | 438 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.27, 0.10] |
| 4.2 Calculus at 24 months | 2 | 438 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐0.44, ‐0.06] |
| 4.3 Plaque at 24 months | 2 | 438 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.35, 0.03] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 S&P every 3 months with OHI versus without OHI Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 S&P every 12 months with OHI versus without OHI Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Gingivitis at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Calculus at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Plaque at 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

