| Study ID | Intervention | Strength | Dose and frequency | Duration | Ear Toilet | Concurrent meds |
| Do topical antibiotic eardrops work? | | | | | | |
| Quinolone versus placebo: | | | | | | |
| Kasemsuwan 1997 | 1) Quinolone: ciprofloxacin in saline solution
2) Placebo: normal saline solution | 1) Ciprofloxacin: 250 microgram/mL
2) Saline: n/a | Both treatments:
5 drops three times daily. | Both treatments:
At least 7 days. | Both groups:
Ear cleaning at each visit (treatment days 1, 4 and 7). | Excluded if received antibiotics in the previous two weeks or during the study. |
| van Hasselt 2002 | 1) Quinolone: ofloxacin in HPMC
2) Placebo: HPMC
HPMC = hydroxypropyl methyl‐cellulose (hypromellose) ‐ a treatment delivery vehicle. | 1) 0.075% Ofloxacin in 1.5% HPMC
2) 1.5% HPMC | All treatments:
1 single topical application after suction cleaning. | Both treatments:
Once only. | Both groups:
Suction cleaning once. | Not reported. |
| Which antibiotic eardrops work best? | | | | | | |
| Non‐quinolone versus non‐quinolone | | | | | | |
| Gyde 1978 | 1) Non‐quinolone: trimethoprim‐sulfacetamide‐polymyxin B (TSP) (Burroughs Wellcome Ltd).
2) Non‐quinolone: gentamicin sulphate (Garamycine) | 1) 0.1% TSP
(Trimethoprim 1 mg/mL; Polymyxin B 10,000 U/mL; Sulfacetamide 5mg/mL).
2) 0.3% gentamycin sulphate | Both treatments:
8 drops twice daily (morning and evening). | Both treatments:
Depended on clinical and bacteriological response:
Up to 3 weeks initially, plus 3 weeks if required.
Failed ears or not dry at 6 months crossed over to the other treatment for 3 weeks; 6 month follow‐up as before: 11 participants (12 ears; 7 CSOM ears).
Average duration (including crossovers) (days):
All successfully treated ears:
TSP 19.3 days (range 7 to 32) (N = 46);
gentamicin 21.7 days (range 10 to 37) (N = 51).
CSOM: TSP 16.4, gentamicin 22.8;
Post‐operative or mastoid infections: TSP 24.0, gentamicin 24.3;
Subacute otitis media: TSP 21.3, gentatmicin 22.7
Otitis externa: TSP 17.1, gentamicin 17.5. | Both groups:
Suction and dry mopping before each treatment application.
Pneumatic otoscope sometimes also used to ensure the eardrops reached the middle ear and mastoid cavity. | Two‐week washout period if used any antibiotics before study entry.
Excluded if used high doses of ototopical corticosteroids, or ever used ototoxic drug therapy. |
| Gyde 1981 | 1) Non‐quinolone: Trimethoprim‐ sulfacetamide‐ polymyxin B (TSP)
2) Non‐quinolone: Trimethoprim‐ polymyxin B (TP) | 1) 0.1% TSP
2) 0.1% TP
Concentrations of treatment components: Trimethoprim 1 mg/mL; Polymyxin B 10,000 U/mL; Sulfacetamide 5 mg/mL. | Both treatments:
8 drops twice daily (morning and night). | Both treatments:
Up to 14 days maximum, depending on response to treatment and bacterial culture results. | Both groups:
Suction and dry mopping before each treatment application.
Pneumatic otoscope sometimes also used to ensure the eardrops reached the middle ear and mastoid cavity. | Two week washout period if used any antibiotics before inclusion.
Excluded if used extensive ototopical corticosteroids within 4 weeks, or ever used ototoxic drug therapy.
Concurrent medications such as analgesics and decongestants etc were allowed. |
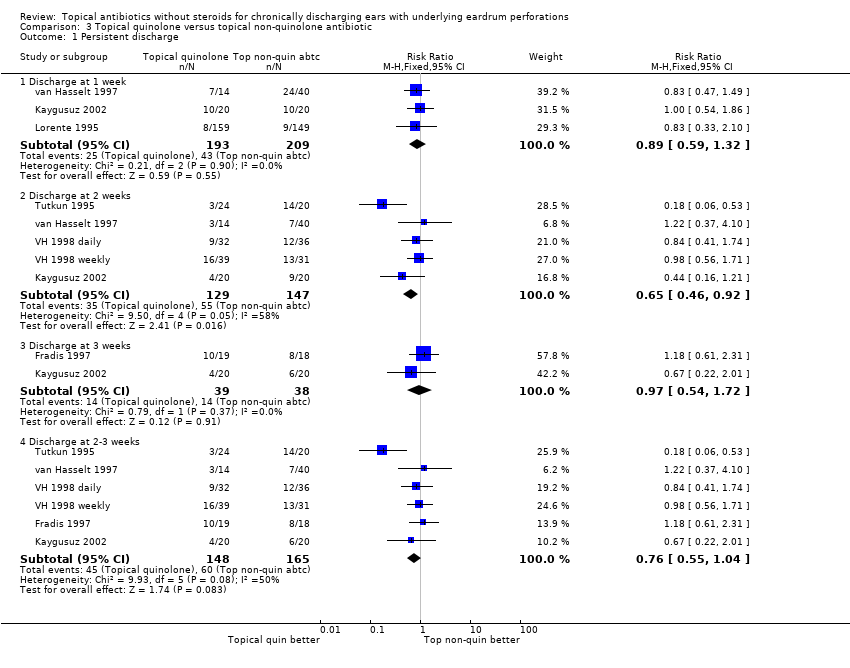
| Quinolone versus non‐quinolone | | | | | | |
| Fradis 1997 | 1) Quinolone: ciprofloxacin hydrochloride solution
2) Non‐quinolone: tobramycin | 1) Ciprofloxacin: Not specified
2) Tobramycin: Not specified | All treatments:
5 drops, 3 time daily. | All treatments:
3 weeks. | Not specified. | All other medication discontinued two weeks before study entry.
(34 participants previously received systemic antibiotics; 12 had used neomycin‐polymyxin B eardrops without success). |
| Kaygusuz 2002 | 1) Quinolone: ciprofloxacin hydrochloride
2) Non‐quinolone: tobramycin | 1) 0.3% Ciprofloxacin hydrochloride
2) 0.3% Tobramycin | All treatments:
2 drops 3 times daily. | All treatments:
3 weeks. | All groups:
Aspiration once daily. | Not reported. |
| Lorente 1995 | 1) Quinolone: ciprofloxacin
2) Non‐quinolone: gentamicin | 1) 0.3% Ciprofloxacin
2) 0.3% Gentamicin | Both treatments:
5 drops (0.75 mg) 3 times daily. | Both treatments:
8 days (awaiting confirmation that this was not continued to day 30). | Not specified. | Excluded if received antibiotic treatment (topical or systemic) in the last 48 hours. |
| Tutkun 1995 | 1) Quinolone: ciprofloxacin hydrochloride
2) Non‐quinolone: gentamicin sulfate | 1) Ciprofloxacin hydrochloride: 200 microgram/mL
2) Gentamicin sulfate: 5 mg/mL | Both treatments:
5 drops 3 times daily. | Both treatments:
10 days. | Not specified. | All other medication stopped at least 10 days prior to treatment.
Excluded if used any other medication during the study. |
| van Hasselt 1997 | 1) Quinolone: ofloxacin (Exocin R from Allergan)
2) Non‐quinolone: neomycin‐polymyxin B | 1) 0.3% Ofloxacin;
2) 0.5% Neomycin, 0.1% polymyxin B | All treatments:
3 drops, 3 times daily. | All treatments:
2 weeks. | All groups:
Suction cleaning at the beginning of the trial, and at weeks 1 and 2 visits. | Not reported. |
| VH 1998 daily | 1) Quinolone: ofloxacin
2) Non‐quinolone: neomycin‐ polymyxin B | 1) 0.3% Ofloxacin
2) Neomycin‐ polymyxin B: not specified | Both treatments:
6 drops twice daily. | All treatments:
2 weeks. | All groups:
Once weekly suction cleaning. | Not reported. |
| VH 1998 weekly | 1) Quinolone: ofloxacin
2) Non‐quinolone: neomycin‐ polymyxin B | 1) 0.3% Ofloxacin
2) Neomycin‐ polymyxin B: not specified | Both treatments:
Once weekly. | All treatments:
2 weeks. | All groups:
Once weekly suction cleaning. | Not reported. |
| Do topical antibiotics work better than topical antiseptics? | | | | | | |
| Non‐quinolone versus antiseptic | | | | | | |
| Browning 1983a | 1) Non‐quinolone: chloramphenicol (Chloromycetin), or gentamicin (Genticin) (self treated).
Choice of antibiotics depended on sensitivity of bacterial isolated at baseline.
2) Antiseptics: insufflation of boric acid and iodine powder after aural toilet (otologist treated). | 1) Antibiotics: not specified
2) Antiseptic: not specified | 1) Topical Antibiotics (self treat):
a) Chloramphenicol: 1 or 2 drops, 3 times daily;
b) gentamicin: 3 or 4 drops, 4 times daily.
2) Antiseptic: once weekly (insufflation after aural toilet, by otologist) (dose not reported). | All treatments:
4 weeks. | All groups:
Weekly aural toilet by otologist, using microscopic vision and suction aspiration when necessary. | Not reported. |
| Clayton 1990 | 1) Non‐quinolone: gentamicin sulphate
2) Antiseptic: aluminium acetate | 1) 0.3% Gentamicin sulphate
2) 8% Aluminium acetate | All treatments:
5 drops, 3 times daily. | All treatments:
3 weeks. | All groups:
Self mopping before each treatment administration. | No antibiotics in the preceding 3 weeks. |
| Fradis 1997 | 2) Non‐quinolone: tobramycin
3) Antiseptic: Burow aluminium acetate solution | 2) Tobramycin: Not specified
3) 1% Aluminium acetate
(weak antiseptic, used as a "placebo" by the trialists). | All treatments:
5 drops, 3 times daily. | All treatments:
3 weeks. | Not specified. | All other medication discontinued two weeks before study entry. (34 participants previously received systemic antibiotics; 12 had used neomycin‐polymyxin B eardrops without success). |
| van Hasselt 1997 | 2) Non‐quinolone: neomycin‐polymyxin B
3) Antiseptic: acetic acid in spirit and glycerin | 2) 0.5% Neomycin, 0.1% polymyxin B
3) 2% Acetic acid in 25% spirit and 30% glycerin | All treatments: 3 drops, 3 times daily. | All treatments:
2 weeks. | All groups: Suction cleaning at the beginning of the trial, and at weeks 1 & 2 visits. | Not reported. |
| Quinolone versus antiseptic | | | | | | |
| Fradis 1997 | 1) Quinolone: ciprofloxacin hydrochloride solution
3) Antiseptic: Burow aluminium acetate solution | 1) Ciprofloxacin: Not specified
3) 1% Aluminium acetate (weak antiseptic, designated as the "placebo group" by the trialists). | All treatments:
5 drops, 3 time daily. | All treatments:
3 weeks. | Not specified. | All other medication discontinued two weeks before study entry. (34 participants previously received systemic antibiotics; 12 had used neomycin‐polymyxin B eardrops without success). |
| Jaya 2003 | 1) Quinolone: ciprofloxacin hydrochloride
2) Antiseptic: povidone (polyvinyl pyrrolidone)‐ iodine (PVP‐I, Betadine) | 1) 0.3% Ciprofloxacin hydrochloride
2) 5% Povidone iodine | All treatments:
3 drops three times daily. | All treatments:
10 days. | Both groups:
Dry mopping before each treatment occasion.
Aural suctioning performed before initial treatment for all participants, and at subsequent weekly visits if discharge was present. | No prior systemic or topical antibiotic therapy within 10 days of study entry. |
| Macfadyen 2005 | 1) Quinolone: ciprofloxacin hydrochloride (Ciloxan, from Alcon)
2) Antiseptic: boric acid in alcohol
(powder from UK but manufactured locally) | 1) 0.3% Ciprofloxacin hydrochloride
2) 2% Boric acid in 45% alcohol | Both treatments:
Drops given twice daily (morning registration and lunch time).
Child‐to‐child treatment: older children trained to clean and treat infected ears (at school), under supervision of trained teachers. | Both treatments:
10 consecutive school days (ie excluding weekends). | Both groups:
Dry mopping before each treatment administration.
Dry mop only for weeks 2‐4 if persistent discharge at week 2. | Excluded if treated for ear infection or received antibiotics for any other disorder in the previous 2 weeks. |
| van Hasselt 1997 | 1) Quinolone: ofloxacin (Exocin R, from Allergan)
3) Antiseptic: acetic acid in spirit and glycerin | 1) 0.3% Ofloxacin
3) 2% Acetic acid in 25% spirit and 30% glycerin | All treatments: 3 drops, 3 times daily. | All treatments:
2 weeks. | All groups: Suction cleaning at the beginning of the trial, and at weeks 1 & 2 visits. | Not reported. |
| van Hasselt 2002 | 1) Quinolone: ofloxacin in HPMC
2) Antiseptic: povidone iodine in HPMC
HPMC = hydroxypropyl methyl‐cellulose (hypromellose) ‐ a treatment delivery vehicle. | 1) 0.075% Ofloxacin in 1.5% HPMC
2) 1% Povidone iodine in 1.5% HPMC | All treatments: 1 single topical application after suction cleaning. | Both treatments:
Once only. | All groups:
Suction cleaning once. | Not reported. |