Frühe versus späte orale Flüssigkeits‐ und Nahrungsaufnahme zur Reduktion von Komplikationen nach großen abdominalen gynäkologischen Operationen
Appendices
Appendix 1. MDSG search strategy
MDSG Search strategy for KC813 15.06.11
Keywords CONTAINS "gynecologic surgical procedure"or "salpingectomy"or"salpingo‐oopherectomy" or "*Salpingostomy‐" or "salpingotomy" or "surgery" or "surgery‐gynaecological" or"Surgical"or "myomectomy"or "Hysterectomy,abdominal"or "total abdominal hysterectomy" or "abdominal myomectomy"or"abdominal hysterectomy"or"abdominal myomectomy" or Title CONTAINS "gynecologic surgical procedure"or "salpingectomy"or"salpingo‐oopherectomy" or "*Salpingostomy‐" or "salpingotomy" or "surgery" or "surgery‐gynaecological" or"Surgical"or "myomectomy"or "Hysterectomy,abdominal"or "total abdominal hysterectomy" or "abdominal myomectomy"or"abdominal hysterectomy"or"abdominal myomectomy"
AND
Keywords CONTAINS "Food intake"or "early feeding"or"starved state" or Title CONTAINS "Food intake"or "early feeding"or"starved state" or"starved state"
Appendix 2. CENTRAL search strategy
1 (surgery or surgical).tw. (67324)
2 exp General Surgery/ (227)
3 exp Postoperative Complications/ (24734)
4 postoperative.tw. (35065)
5 exp Gynecologic Surgical Procedures/ (3154)
6 or/1‐5 (86713)
7 (gynecol$ or gynaecol$).tw. (4596)
8 exp Gynecology/ (87)
9 (abdomin$ or abdomen$).tw. (11988)
10 exp Abdomen/ (2194)
11 exp Pelvis/ (538)
12 pelvi$.tw. (4062)
13 intraabdominal.tw. (308)
14 hysterectom$.tw. (2321)
15 or/7‐14 (21207)
16 exp eating/ or exp gastrointestinal motility/ (4623)
17 exp Food/ (29667)
18 exp Feeding Methods/ or exp Feeding Behavior/ (7376)
19 feeding.tw. (5096)
20 food.tw. (9126)
21 fluid$.tw. (10387)
22 oral.tw. (55828)
23 water.tw. (10191)
24 solid$.tw. (3058)
25 eating.tw. (3105)
26 eat.tw. (725)
27 or/16‐26 (111186)
28 early.tw. (41225)
29 exp Time Factors/ (45655)
30 (time or timing).tw. (113194)
31 day one.tw. (762)
32 day two.tw. (740)
33 or/28‐32 (173700)
34 6 and 15 and 27 and 33 (606)
35 limit 34 to yr="2012 ‐Current" (51)
Appendix 3. MEDLINE search strategy
1 (surgery or surgical).tw. (1204744)
2 exp General Surgery/ (33397)
3 exp Postoperative Complications/ (411947)
4 postoperative.tw. (303965)
5 exp Gynecologic Surgical Procedures/ (63349)
6 or/1‐5 (1586874)
7 (gynecol$ or gynaecol$).tw. (71639)
8 exp Gynecology/ (13214)
9 (abdomin$ or abdomen$).tw. (244185)
10 exp Abdomen/ (80147)
11 exp Pelvis/ (18399)
12 pelvi$.tw. (98306)
13 intraabdominal.tw. (6783)
14 hysterectom$.tw. (26049)
15 or/7‐14 (460798)
16 exp eating/ or exp gastrointestinal motility/ (88490)
17 exp Food/ (1038694)
18 exp Feeding Methods/ or exp Feeding Behavior/ (152611)
19 feeding.tw. (134574)
20 food.tw. (248095)
21 fluid$.tw. (348392)
22 oral.tw. (419172)
23 water.tw. (491988)
24 solid$.tw. (218823)
25 eating.tw. (44448)
26 eat.tw. (12050)
27 or/16‐26 (2648763)
28 early.tw. (1029482)
29 exp Time Factors/ (989633)
30 (time or timing).tw. (2037094)
31 day one.tw. (2125)
32 day two.tw. (1070)
33 or/28‐32 (3546350)
34 6 and 15 and 27 and 33 (4855)
35 randomized controlled trial.pt. (368553)
36 controlled clinical trial.pt. (87954)
37 randomized.ab. (288824)
38 randomised.ab. (57687)
39 placebo.tw. (156289)
40 clinical trials as topic.sh. (168882)
41 randomly.ab. (209520)
42 trial.ti. (123979)
43 (crossover or cross‐over or cross over).tw. (59999)
44 or/35‐43 (931125)
45 exp animals/ not humans.sh. (3907798)
46 44 not 45 (858747)
47 34 and 46 (768)
48 (2012$ or 2013$ or 2014$).ed. (2212373)
49 (2012$ or 2013$ or 2014$).dp. (2164044)
50 48 or 49 (2713731)
51 47 and 50 (132)
Appendix 4. EMBASE search strategy
1 gynecologic surgery/ or uterine tube surgery/ or salpingoplasty/ or salpingostomy/ or uterus surgery/ or hysterectomy/ or abdominal hysterectomy/ or hysterotomy/ or radical hysterectomy/ (53972)
2 ovariectomy/ or salpingooophorectomy/ (32953)
3 ((gynecolog$ or gynaecolog$) adj5 surg$).tw. (11122)
4 ((gynecolog$ or gynaecolog$) adj5 operat$).tw. (2627)
5 (hysterectomy or ovariectomy or salpingostomy or salpingooophorectomy).tw. (41333)
6 exp Uterus Tumor/su [Surgery] (25970)
7 exp Ovary Tumor/su [Surgery] (14387)
8 or/1‐7 (116284)
9 food intake/ or drinking/ or eating/ (108665)
10 feeding/ (26586)
11 feeding behavior/ (52426)
12 (oral adj5 intak$).tw. (8436)
13 (intake adj5 (food or drink or fluid$)).tw. (50060)
14 (postoperat$ adj5 feed$).tw. (1071)
15 (tradition$ adj5 feed$).tw. (460)
16 (tradition$ adj5 intake$).tw. (306)
17 (early adj5 feed$).tw. (4248)
18 (early adj5 intake$).tw. (1386)
19 (delay$ adj5 feed$).tw. (2130)
20 (delay$ adj5 intake$).tw. (503)
21 (timing adj4 intake).tw. (242)
22 (timing adj4 feed$).tw. (403)
23 fasting.tw. (94474)
24 nil per mouth.tw. (7)
25 nil per os.tw. (100)
26 or/9‐25 (294313)
27 8 and 26 (1103)
28 Clinical Trial/ (829495)
29 Randomized Controlled Trial/ (338330)
30 exp randomization/ (61474)
31 Single Blind Procedure/ (18001)
32 Double Blind Procedure/ (112268)
33 Crossover Procedure/ (38288)
34 Placebo/ (236087)
35 Randomi?ed controlled trial$.tw. (95686)
36 Rct.tw. (13359)
37 random allocation.tw. (1288)
38 randomly allocated.tw. (19758)
39 allocated randomly.tw. (1894)
40 (allocated adj2 random).tw. (707)
41 Single blind$.tw. (13923)
42 Double blind$.tw. (137961)
43 ((treble or triple) adj blind$).tw. (351)
44 placebo$.tw. (193373)
45 prospective study/ (244428)
46 or/28‐45 (1338033)
47 case study/ (25023)
48 case report.tw. (253523)
49 abstract report/ or letter/ (882948)
50 or/47‐49 (1156030)
51 46 not 50 (1300837)
52 27 and 51 (137)
53 (2012$ or 2013$ or 2014$).em. (3244058)
54 52 and 53 (27)
Appendix 5. CINAHL search strategy
KC813 CINAHL search strategy 01.04.14
| # | Query | Results |
| S34 | S18 AND S32 | 8 |
| S33 | S18 AND S32 | 72 |
| S32 | S19 OR S20 or S21 or S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 | 880,148 |
| S31 | TX allocat* random* | 3,851 |
| S30 | (MH "Quantitative Studies") | 11,743 |
| S29 | (MH "Placebos") | 8,683 |
| S28 | TX placebo* | 31,261 |
| S27 | TX random* allocat* | 3,851 |
| S26 | (MH "Random Assignment") | 36,901 |
| S25 | TX randomi* control* trial* | 70,671 |
| S24 | TX ( (singl* n1 blind*) or (singl* n1 mask*) ) or TX ( (doubl* n1 blind*) or (doubl* n1 mask*) ) or TX ( (tripl* n1 blind*) or (tripl* n1 mask*) ) or TX ( (trebl* n1 blind*) or (trebl* n1 mask*) ) | 707,698 |
| S23 | TX ( (trebl* n1 blind*) or (trebl* n1 mask*) ) | 103 |
| S22 | TX ( (trebl* n1 blind*) or (trebl* n1 mask*) ) | 0 |
| S21 | TX clinic* n1 trial* | 161,901 |
| S20 | PT Clinical trial | 75,662 |
| S19 | (MH "Clinical Trials+") | 172,920 |
| S18 | S7 AND S17 | 288 |
| S17 | S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 | 200,933 |
| S16 | TX eat* | 32,854 |
| S15 | (MH "Food Intake+") | 5,373 |
| S14 | TX drink* | 28,560 |
| S13 | TX feed* | 47,112 |
| S12 | TX "food" | 98,420 |
| S11 | TX "oral intake" | 645 |
| S10 | TX "fasting" | 10,669 |
| S9 | TX "nil by mouth" | 62 |
| S8 | TX fluids | 5,646 |
| S7 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 | 9,613 |
| S6 | TX Hysterectomy | 4,816 |
| S5 | TX Oophorectomy | 1,898 |
| S4 | TX gyn?ecolog* surg* | 432 |
| S3 | (MM "Oophorectomy") | 590 |
| S2 | (MH "Hysterectomy+") | 3,860 |
| S1 | (MH "Surgery, Gynecologic+") | 8,310 |
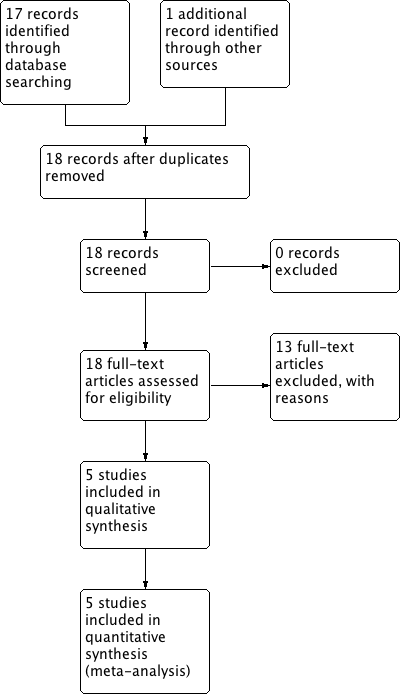
Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
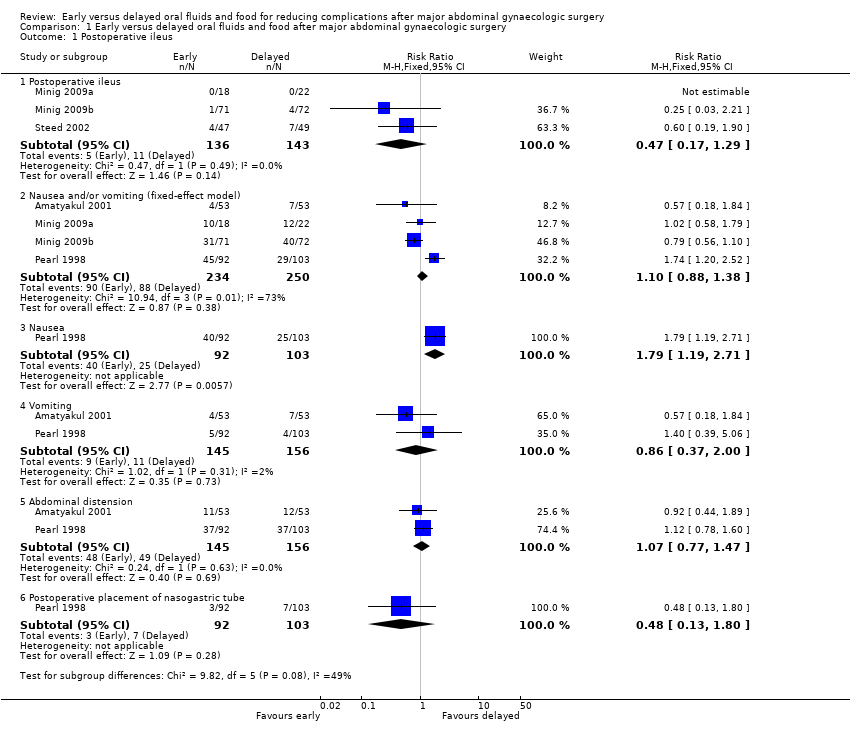
Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 1 Postoperative ileus.
![Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 2 Time intervals (fixed‐effect model) [days].](/es/cdsr/doi/10.1002/14651858.CD004508.pub4/media/CDSR/CD004508/image_n/nCD004508-CMP-001-02.png)
Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 2 Time intervals (fixed‐effect model) [days].

Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 3 Other major postoperative complications.
![Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 4 Satisfaction visual analog scale [mm].](/es/cdsr/doi/10.1002/14651858.CD004508.pub4/media/CDSR/CD004508/image_n/nCD004508-CMP-001-04.png)
Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 4 Satisfaction visual analog scale [mm].
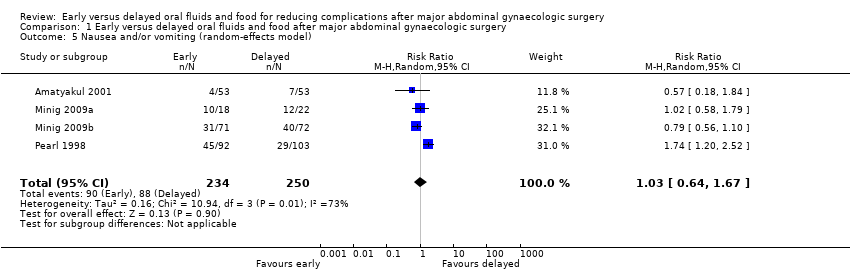
Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 5 Nausea and/or vomiting (random‐effects model).
![Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 6 Time to the presence of bowel sound (random‐effects model) [days].](/es/cdsr/doi/10.1002/14651858.CD004508.pub4/media/CDSR/CD004508/image_n/nCD004508-CMP-001-06.png)
Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 6 Time to the presence of bowel sound (random‐effects model) [days].
![Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 7 Time to the first solid diet (random‐effects model) [days].](/es/cdsr/doi/10.1002/14651858.CD004508.pub4/media/CDSR/CD004508/image_n/nCD004508-CMP-001-07.png)
Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 7 Time to the first solid diet (random‐effects model) [days].
![Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 8 Hospital stay (random‐effects model) [days].](/es/cdsr/doi/10.1002/14651858.CD004508.pub4/media/CDSR/CD004508/image_n/nCD004508-CMP-001-08.png)
Comparison 1 Early versus delayed oral fluids and food after major abdominal gynaecologic surgery, Outcome 8 Hospital stay (random‐effects model) [days].
| Early oral feeding compared to delayed oral feeding for women who had major abdominal gynaecologic surgery | ||||||
| Patient or population: Women who had major abdominal gynaecologic surgery | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed oral feeding | Early oral feeding | |||||
| Postoperative ileus | 77 per 1000 | 36 per 1000 | RR 0.47 | 279 | ⊕⊕⊕⊝ | |
| Nausea or vomiting or both | 352 per 1000 | 363 per 1000 | RR 1.03 | 484 | ⊕⊕⊕⊝ | Random effects model, deployed because of substantial heterogeneity between studies (I2> 50%) |
| Time to bowel sounds [days] | The mean time to the presence of bowel sound [days] in the intervention groups was | 338 | ⊕⊕⊕⊝ | Random effects model, deployed because of substantial heterogeneity between studies (I2> 50%) | ||
| Time to the passage of flatus [days] | The mean time to the passage of flatus [days] in the intervention groups was | 444 | ⊕⊕⊕⊕ | |||
| Time to the first solid diet [days] | The mean time to the first solid diet [days] in the intervention groups was | 301 | ⊕⊕⊕⊝ | Random effects model, deployed because of substantial heterogeneity between studies (I2> 50%) | ||
| Time to first passage of stool [days] | The mean time to first passage of stool [days] in the intervention groups was | 249 | ⊕⊕⊕⊝ | |||
| Hospital stay [days] | The mean hospital stay [days] in the intervention groups was | 484 | ⊕⊕⊕⊝ | Random effects model, deployed because of substantial heterogeneity between studies (I2> 50%) | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 For the three studies contributing data, all were at high risk of performance bias, two were at unclear risk of detection bias, and one was at high risk of selection bias (no allocation concealment). 4 This outcome may be influenced by the high risk of performance bias in all studies that provided data. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postoperative ileus Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Postoperative ileus | 3 | 279 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.17, 1.29] |
| 1.2 Nausea and/or vomiting (fixed‐effect model) | 4 | 484 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.88, 1.38] |
| 1.3 Nausea | 1 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.79 [1.19, 2.71] |
| 1.4 Vomiting | 2 | 301 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.37, 2.00] |
| 1.5 Abdominal distension | 2 | 301 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.77, 1.47] |
| 1.6 Postoperative placement of nasogastric tube | 1 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.13, 1.80] |
| 2 Time intervals (fixed‐effect model) [days] Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Time to the presence of bowel sound (fixed‐effect model) [days] | 2 | 338 | Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.48, ‐0.11] |
| 2.2 Time to the passage of flatus [days] | 3 | 444 | Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.40, ‐0.01] |
| 2.3 Time to the first solid diet (fixed‐effect model) [days] | 2 | 301 | Mean Difference (IV, Fixed, 95% CI) | ‐1.19 [‐1.34, ‐1.05] |
| 2.4 Time to the first passage of stool [days] | 2 | 249 | Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐0.58, 0.09] |
| 2.5 Hospital stay (fixed‐effect model) [days] | 4 | 484 | Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐0.83, ‐0.35] |
| 3 Other major postoperative complications Show forest plot | 4 | 1286 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.63, 1.01] |
| 3.1 Febrile morbidity | 1 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.76, 1.27] |
| 3.2 Infectious complications | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.05, 0.73] |
| 3.3 Wound complications | 4 | 474 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.50, 1.35] |
| 3.4 Pneumonia | 3 | 434 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.07, 1.73] |
| 4 Satisfaction visual analog scale [mm] Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5 Nausea and/or vomiting (random‐effects model) Show forest plot | 4 | 484 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.64, 1.67] |
| 6 Time to the presence of bowel sound (random‐effects model) [days] Show forest plot | 2 | 338 | Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.61, ‐0.03] |
| 7 Time to the first solid diet (random‐effects model) [days] Show forest plot | 2 | 301 | Mean Difference (IV, Random, 95% CI) | ‐1.47 [‐2.26, ‐0.68] |
| 8 Hospital stay (random‐effects model) [days] Show forest plot | 4 | 484 | Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.53, ‐0.31] |

