Aspiración simple versus drenaje con tubo intercostal para el neumotórax espontáneo primario en adultos
Información
- DOI:
- https://doi.org/10.1002/14651858.CD004479.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 07 septiembre 2017see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Atención crítica y de emergencia
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Kristin Carson‐Chahhoud ‐ updated the protocol, reviewed the literature, identified studies for inclusion, extracted data, entered and analysed data, completed editorial amendments, and updated the text of the manuscript.
Joseph van Agteren ‐ updated the protocol, reviewed the literature, identified studies for inclusion, extracted data, entered and analysed data, and updated the text of the manuscript.
Abel Wakai ‐ authored the original review, updated the text of the manuscript, and supervised the update.
Brian Smith ‐ updated the text of the manuscript and supervised the latest update.
Grainne McCabe ‐ authored the original review and identified studies for inclusion in the update.
Malcolm Brinn ‐ updated search and identified studies for inclusion.
Ronan O'Sullivan ‐ authored the original review.
Sources of support
Internal sources
-
Department of Emergency Medicine, St. Vincent's University Hospital, Dublin, Ireland.
External sources
-
Higher Specialist Training Scheme in Emergency Medicine, Ireland.
Declarations of interest
Kristin Carson‐Chahhoud: no conflicts of interest to declare.
Abel Wakai: no conflicts of interest to declare.
Joseph van Agteren: no conflicts of interest to declare.
Brian Smith: no conflicts of interest to declare.
Grainne McCabe: no conflicts of interest to declare.
Malcolm Brinn: no conflicts of interest to declare.
Ronan O'Sullivan: no conflicts of interest to declare.
Acknowledgements
We wish to acknowledge and thank Frédérique Noble for translating the Desmettre 2010 publication into English. For their tireless efforts, we wish to thank all staff and editors of the Cochrane Anaesthesia, Crticial and Emergency Care Group, in particular Jane Cracknell, who aided review completion and provided valuable feedback and suggestions.
We would like to thank Harald Herkner (Content Editor); Jing Xie (Sophia) (Statistical Editor); Nick Maskell and Teresa Williams (Peer Reviewers); Janne Vendt (Information Specialist); and Brian Stafford (Consumer Referee) for help and editorial advice provided during preparation of this updated systematic review.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Sep 07 | Simple aspiration versus intercostal tube drainage for primary spontaneous pneumothorax in adults | Review | Kristin V Carson‐Chahhoud, Abel Wakai, Joep EM van Agteren, Brian J Smith, Grainne McCabe, Malcolm P Brinn, Ronan O'Sullivan | |
| 2007 Jan 24 | Simple aspiration versus intercostal tube drainage for primary spontaneous pneumothorax in adults | Review | Abel Wakai, Ronan O'Sullivan, Grainne McCabe | |
| 2003 Oct 20 | Simple aspiration versus intercostal tube drainage for primary spontaneous pneumothorax in adults | Protocol | Abel Wakai, Ronan G. O'Sullivan, Conor Deasy, Grainne McCabe | |
Differences between protocol and review
-
We have changed the review author line since the protocol (Wakai 2003) and the original review (Wakai 2007) were prepared, by adding Kristin Carson‐Chahhoud, Joseph van Agteren, Malcolm Brinn, and Brian Smith.
-
We used the GRADE approach to assess the quality of the evidence in this update.
-
We reduced the number of secondary outcomes to adhere to Cochrane recommendations to include as small a total number of outcomes as possible, while keeping them clinically relevant (went from 13 to 7 secondary outcomes).
-
We incorporated a 'Summary of findings' table into the review.
-
We changed the analysis method from a fixed‐effect to a random‐effects model for all outcomes.
-
We included in the review studies investigating participants with a recurrent pneumothorax and conducted a sensitivity analysis to examine potential biases.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans;
PICO

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Simple aspiration versus intercostal tube drainage, outcome: 1.1 Immediate success rate of procedure as defined by study authors.

Comparison 1 Simple aspiration versus intercostal tube drainage, Outcome 1 Immediate success rate of procedure as defined by study authors.

Comparison 1 Simple aspiration versus intercostal tube drainage, Outcome 2 Early failure rate of procedure (incomplete lung expansion after the procedure).
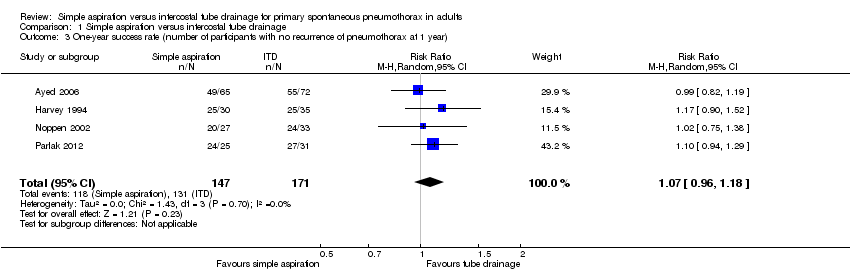
Comparison 1 Simple aspiration versus intercostal tube drainage, Outcome 3 One‐year success rate (number of participants with no recurrence of pneumothorax at 1 year).
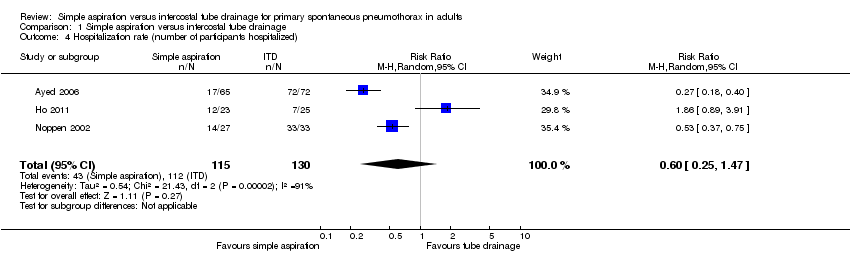
Comparison 1 Simple aspiration versus intercostal tube drainage, Outcome 4 Hospitalization rate (number of participants hospitalized).

Comparison 1 Simple aspiration versus intercostal tube drainage, Outcome 5 Duration of hospital stay in days.
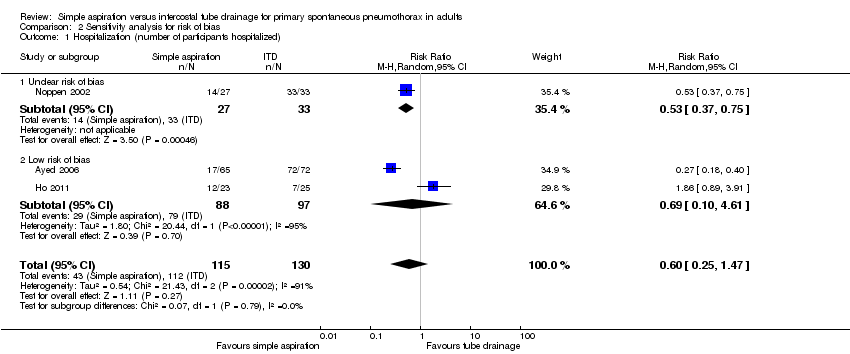
Comparison 2 Sensitivity analysis for risk of bias, Outcome 1 Hospitalization (number of participants hospitalized).
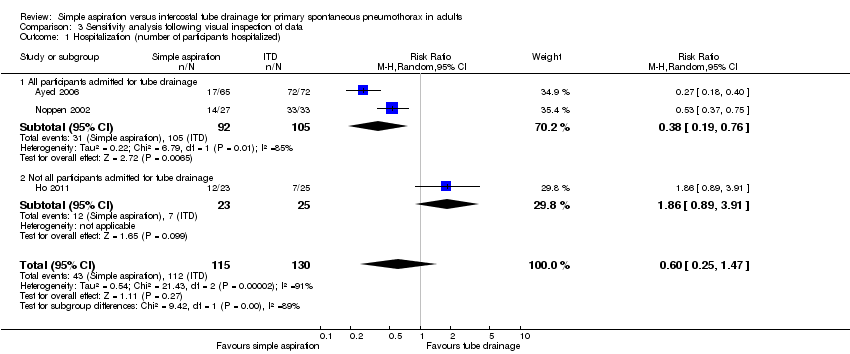
Comparison 3 Sensitivity analysis following visual inspection of data, Outcome 1 Hospitalization (number of participants hospitalized).

Comparison 4 Sensitivity analysis for studies with recurrent pneumothorax, Outcome 1 Immediate success rate of procedure as defined by study authors.

Comparison 4 Sensitivity analysis for studies with recurrent pneumothorax, Outcome 2 Early failure rate of procedure (incomplete lung expansion after the procedure).
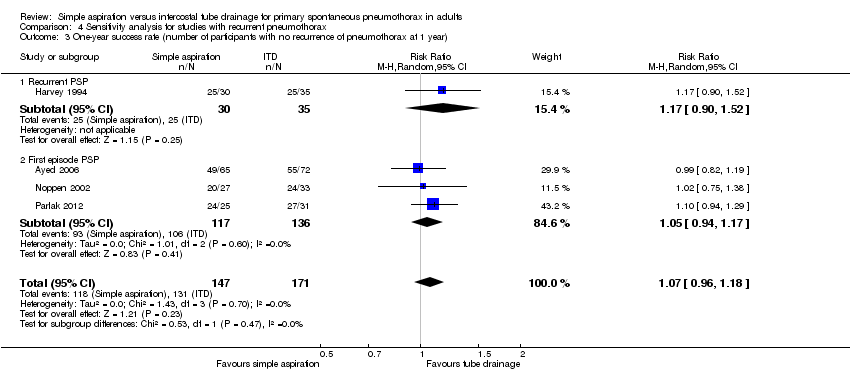
Comparison 4 Sensitivity analysis for studies with recurrent pneumothorax, Outcome 3 One‐year success rate (number of participants with no recurrence of pneumothorax at 1 year).

Comparison 4 Sensitivity analysis for studies with recurrent pneumothorax, Outcome 4 Duration of hospital stay in days.
| Simple aspiration compared with intercostal tube drainage for primary spontaneous pneumothorax | ||||||
| Patient or population: adults with primary spontaneous pneumothorax Settings: university teaching hospitals, tertiary care hospitals, and general hospitals | ||||||
| Outcomes | Illustrative comparative risks (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Intercostal tube drainage | Simple aspiration | |||||
| Immediate success rate | 714 per 1000 | 557 per 1000 | RR 0.78 | 435 | ⊕⊕⊕⊝ | |
| One‐year success rate | 766 per 1000 | 820 per 1000 | RR 1.07 | 318 | ⊕⊕⊕⊝ | |
| Hospitalization rate | 862 per 1000 | 517 per 1000 | RR 0.60 | 245 | ⊕⊝⊝⊝ | |
| Duration of hospital stay | Mean duration of hospital stay ranged across control groups from 4.04 to 7 days. | Mean duration of hospital stay in the intervention groups was 1.66 lower (‐2.28 to ‐1.04). | — | 387 | ⊕⊕⊕⊝ | |
| Adverse events | Overall, fewer adverse events occurred when patients were treated by simple aspiration than by tube drainage, including lesser perceived pain and lower pain scores, reduced need for thoracoscopic pleurodesis, and fewer technical adverse events (e.g. tube blockage when treated by tube drainage). | Not estimable | 245 | ⊕⊕⊝⊝ | ||
| Cost‐effectiveness | See comment. | See comment. | Not estimable | ‐ | See comment. | No studies reported cost‐effectiveness data. |
| Patient satisfaction | Median patient satisfaction among those treated with intercostal tube drainage was 8 on a visual analogue scale of 1 to 10 (Interquartile range 6.25 to 9.00), and median patient satisfaction among those treated by simple aspiration was 0.5 points lower (Interquartile range 5.00 to 9.00). | 48 | ⊕⊕⊝⊝ | |||
| CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence | ||||||
| aResults for all outcomes downgraded one level as a result of study and/or reporting limitations, specifically, the large number of unclear or high risks of bias in the presented studies. bDowngraded one level as a result of significant heterogeneity (I² = 91%). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Immediate success rate of procedure as defined by study authors Show forest plot | 6 | 435 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.69, 0.89] |
| 2 Early failure rate of procedure (incomplete lung expansion after the procedure) Show forest plot | 6 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.91, 1.68] |
| 3 One‐year success rate (number of participants with no recurrence of pneumothorax at 1 year) Show forest plot | 4 | 318 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.96, 1.18] |
| 4 Hospitalization rate (number of participants hospitalized) Show forest plot | 3 | 245 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.25, 1.47] |
| 5 Duration of hospital stay in days Show forest plot | 5 | 387 | Mean Difference (IV, Random, 95% CI) | ‐1.66 [‐2.28, ‐1.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hospitalization (number of participants hospitalized) Show forest plot | 3 | 245 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.25, 1.47] |
| 1.1 Unclear risk of bias | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.37, 0.75] |
| 1.2 Low risk of bias | 2 | 185 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.10, 4.61] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hospitalization (number of participants hospitalized) Show forest plot | 3 | 245 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.25, 1.47] |
| 1.1 All participants admitted for tube drainage | 2 | 197 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.19, 0.76] |
| 1.2 Not all participants admitted for tube drainage | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 1.86 [0.89, 3.91] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Immediate success rate of procedure as defined by study authors Show forest plot | 6 | 435 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.69, 0.89] |
| 1.1 Recurrent primary spontaneous pneumothorax (PSP) | 2 | 134 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.58, 0.82] |
| 1.2 First episode PSP | 4 | 301 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.75, 1.06] |
| 2 Early failure rate of procedure (incomplete lung expansion after the procedure) Show forest plot | 6 | 427 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.91, 1.68] |
| 2.1 Recurrent PSP | 2 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 2.20 [0.11, 42.99] |
| 2.2 First episode PSP | 4 | 301 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.93, 1.77] |
| 3 One‐year success rate (number of participants with no recurrence of pneumothorax at 1 year) Show forest plot | 4 | 318 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.96, 1.18] |
| 3.1 Recurrent PSP | 1 | 65 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.90, 1.52] |
| 3.2 First episode PSP | 3 | 253 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.94, 1.17] |
| 4 Duration of hospital stay in days Show forest plot | 5 | 387 | Mean Difference (IV, Random, 95% CI) | ‐1.66 [‐2.28, ‐1.04] |
| 4.1 Recurrent PSP | 2 | 134 | Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐3.31, 0.67] |
| 4.2 First episode PSP | 3 | 253 | Mean Difference (IV, Random, 95% CI) | ‐1.69 [‐2.40, ‐0.98] |

