Incisiones quirúrgicas abdominales para la operación cesárea
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomisation to Mouchel incision or Pfannenstiel incision. Method of randomisation unclear. | |
| Participants | 58 women undergoing caesarean section by Mouchel or Pfannenstiel incision. The study also included 61 women undergoing gynaecological surgery in Grenoble, France. | |
| Interventions | Mouchel (muscle‐cutting) incision (n = 28) versus Pfannenstiel incision (n = 30). | |
| Outcomes | Extraction time. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Potential risk of bias in assessment of extraction time and Apgar scores. intraoperative maternal variables studied. Cord pH estimated for all babies. Postoperative maternal assessment by single observer unaware of allocation. |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information. |
| Other bias | Unclear risk | Insufficient information. |
| Methods | Multicentre study. Sealed envelopes containing computer‐generated random codes. | |
| Participants | Women over 18 years, singleton pregnancy with indication for caesarean delivery in Varese, Italy and Berne, Switzerland. Exclusion criteria were: gestation less than 32 weeks, previous myomectomy, previous longitudinal abdominal incision, previous caesarean section prior to 32 weeks, 2 or more caesarean sections, maternal diseases requiring long‐term medical treatment. 2 women in Joel‐Cohen group were excluded after randomisation because they required caesarean hysterectomy. | |
| Interventions | Joel‐Cohen incision (n = 154) versus Pfannenstiel incision (n = 158) for laparotomic access. | |
| Outcomes | Extraction time defined as interval from skin incision to the clamping of the umbilical cord. | |
| Notes | Abdominal wound infection was graded with a 6‐grade score. Febrile morbidity was defined as temperature elevation to 38 deg C on 2 occasions 4 h apart, excluding the first 24 h and in the absence of known operative or non‐operative site infection. Puerperal endometritis was defined as postpartum temperature elevation to 38 deg C on 2 occasions 4 h apart with uterine tenderness, foul‐smelling lochia, and no other apparent sources of fever. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation. |
| Allocation concealment (selection bias) | Unclear risk | Envelopes used but unclear if sequentially numbered, opaque and sealed. |
| Blinding of participants and personnel (performance bias) | High risk | Since surgical team was aware of allocated intervention, assessment of intraoperative variables (secondary outcomes) may have been subject to bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unclear if women and health workers providing postoperative newborn care and assessments were adequately blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Data from 1 woman in each group excluded after randomisation because of caesarean hysterectomy. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information. |
| Other bias | Unclear risk | Insufficient information. |
| Methods | Consecutively‐numbered, sealed envelopes containing allocation code. | |
| Participants | Women (n = 120) more than 18 years old and at gestation more than 37 weeks undergoing elective or emergency caesarean delivery in Montpelier, France. Excluded were women with scarred abdominal wall, previous caesarean delivery, hernia, multifetal gestation, grand multiparity, diabetes mellitus, myopathy, corticosteroid therapy during pregnancy, on anticoagulants or having haemostatic disorder, having general anaesthesia. Mother was not asked to participate when neonate was at risk of transfer to neonatal unit. Postoperative questionnaires and outcome variables were available for 97 (87%). Postoperative isokinetic assessment was performed on 54 of these women only. | |
| Interventions | Maylard (muscle‐cutting) incision (n = 43) versus Pfannenstiel incision (n = 54) for laparotomic access. | |
| Outcomes | Intraoperative and postoperative morbidity. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table used. |
| Allocation concealment (selection bias) | Low risk | Consequently numbered, sealed envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Since surgical team was aware of allocated intervention, assessment of intraoperative variables may have been subject to bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Women and health workers providing postoperative care and assessment were unaware of allocation. |
| Incomplete outcome data (attrition bias) | High risk | Postoperative questionnaires and outcome variables available for only 81% of women with fewer women in intervention arm. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information. |
| Other bias | Unclear risk | Insufficient information. |
| Methods | Sealed, consecutively‐numbered envelopes containing randomisation code. Block randomisation to 1 of 2 interventions. | |
| Participants | Women (n = 105) with singleton pregnancies at longitudinal lie at term requiring cesarean delivery under spinal anaesthesia in Vellore, India. Excluded were those with multiple pregnancy, any previous abdominal surgery, conditions where midline or paramedian incisions were planned, and where spinal anaesthesia was contraindicated. Spinal anaesthesia was ineffective in 1 in each group. 2 women in Joel Cohen group (1 underwent caesarean hysterectomy; 1 had vaginal delivery prior to caesarean section). | |
| Interventions | Joel‐Cohen incision (n = 51) versus Pfannenstiel incision (n = 50) for laparotomic access. | |
| Outcomes | Analgesia on demand within the first 4 h after surgery. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Since surgical team was aware of allocated intervention, assessment of intraoperative variables (secondary outcomes) may have been subject to bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Women and health workers providing postoperative care were not aware of allocation. |
| Incomplete outcome data (attrition bias) | Low risk | 4 exclusions after randomisation ‐ 1 in each group due to ineffective spinal analgesia; 1 in intervention group following caesarean hysterectomy for PPH; 1 in control group delivered vaginally before caesarean section. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information. |
| Other bias | Unclear risk | Insufficient information. |
deg: degree
h: hour
PPH: postpartum haemorrhage
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Alternate allocation, not randomised. | |
| Treatment allocation based on hospital number. | |
| Not enough data provided in abstract for assessment. | |
| Not enough data provided in abstract for assessment. | |
| Comparison of abdominal incisions along with different combinations of other steps of surgery. | |
| Comparison of abdominal incisions along with different combinations of other steps of surgery. | |
| Comparison of abdominal incisions along with different combinations of other steps of surgery. | |
| Not enough data provided in abstract for assessment. | |
| Not enough data provided in abstract for assessment. | |
| Not a randomised controlled trial. | |
| Comparison of abdominal incisions along with different combinations of other steps of surgery. | |
| Comparison of abdominal incisions along with different combinations of other steps of surgery. | |
| Treatment allocation by year of birth. | |
| Not enough data provided in abstract for assessment. | |
| Comparison of abdominal incisions along with different combinations of other steps of surgery. | |
| Not a comparison of abdominal incisions. | |
| Not a comparison of abdominal incisions. | |
| Not enough data provided in abstract for assessment. | |
| Not enough data provided in abstract for assessment. | |
| Comparison of abdominal incisions along with different combinations of other steps of surgery. | |
| Not a comparison of abdominal incisions | |
| Treatment allocation by first letter of surname. | |
| Comparison of abdominal incisions along with different combinations of other steps of surgery. | |
| Not enough data provided in abstract for assessment. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | The Coronis Trial. |
| Methods | International multicentre study of caesarean section surgical techniques: a randomised fractional, factorial trial. |
| Participants | Women undergoing their first or second caesarean section through a transverse abdominal incision. |
| Interventions | Five comparisons using a 2 x 2 x 2 x 2 x 2 fractional factorial design:
|
| Outcomes | Primary outcome: death or maternal infectious morbidity (one or more of the following: antibiotic use for maternal febrile morbidity during postnatal hospital stay, antibiotic use for endometritis, wound infection or peritonitis) or further operative procedures; or blood transfusion. |
| Starting date | Not stated in reports. |
| Contact information | The CORONIS Trial Collaborative Group, Peter Brocklehurst: [email protected] |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postoperative febrile morbidity Show forest plot | 2 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.14, 0.87] |
| Analysis 1.1  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 1 Postoperative febrile morbidity. | ||||
| 1.1 Joel‐Cohen versus Pfannenstiel incision | 2 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.14, 0.87] |
| 2 Postoperative analgesia on demand Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.40, 0.76] |
| Analysis 1.2  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 2 Postoperative analgesia on demand. | ||||
| 3 Time between surgery and first dose of analgesic (hours) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [0.12, 1.48] |
| Analysis 1.3  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 3 Time between surgery and first dose of analgesic (hours). | ||||
| 4 Total dose of analgesics in 24 hours Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐0.89 [‐1.19, ‐0.59] |
| Analysis 1.4  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 4 Total dose of analgesics in 24 hours. | ||||
| 5 Number of analgesic injections required | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Duration of analgesics (hours) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of analgesic doses required | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Estimated blood loss (mL) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐58.0 [‐108.51, ‐7.49] |
| Analysis 1.8  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 8 Estimated blood loss (mL). | ||||
| 9 Change in pre‐ and postoperative haemoglobin levels (g) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Blood transfusion Show forest plot | 1 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.10  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 10 Blood transfusion. | ||||
| 11 Wound infection as defined by trial authors Show forest plot | 1 | 310 | Risk Ratio (M‐H, Random, 95% CI) | 1.56 [0.45, 5.42] |
| Analysis 1.11  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 11 Wound infection as defined by trial authors. | ||||
| 12 Wound haematoma | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Postoperative pain absent on day 1 | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Postoperative pain absent on day 2 | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 "Significant" postoperative pain by visual analogue score | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Time (hours) from surgery to start of breastfeeding Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐5.5 [‐13.62, 2.62] |
| Analysis 1.16  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 16 Time (hours) from surgery to start of breastfeeding. | ||||
| 17 Total operative time (minutes) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐11.40 [‐16.55, ‐6.25] |
| Analysis 1.17  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 17 Total operative time (minutes). | ||||
| 18 Need for re‐laparotomy Show forest plot | 1 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.18  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 18 Need for re‐laparotomy. | ||||
| 19 Long‐term "significant" wound pain assessed by visual analogue score | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Not satisfied with wound | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Delivery time (minutes) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐1.90 [‐2.53, ‐1.27] |
| Analysis 1.21  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 21 Delivery time (minutes). | ||||
| 22 5‐minute Apgar score less than 7 | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Admissions to special care baby unit ‐ all types Show forest plot | 1 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.44, 3.20] |
| Analysis 1.23  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 23 Admissions to special care baby unit ‐ all types. | ||||
| 24 Admission to special care baby unit ‐ emergency caesarean section Show forest plot | 1 | 98 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.54, 3.86] |
| Analysis 1.24  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 24 Admission to special care baby unit ‐ emergency caesarean section. | ||||
| 25 Postoperative hospital stay for mother (days) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐2.16, ‐0.84] |
| Analysis 1.25  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 25 Postoperative hospital stay for mother (days). | ||||
| 26 Stay in special care nursery (days) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.95, 0.03] |
| Analysis 1.26  Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 26 Stay in special care nursery (days). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postoperative febrile morbidity Show forest plot | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.08, 19.50] |
| Analysis 2.1  Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 1 Postoperative febrile morbidity. | ||||
| 2 Blood transfusion Show forest plot | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.02, 9.98] |
| Analysis 2.2  Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 2 Blood transfusion. | ||||
| 3 Wound infection as defined by trial authors Show forest plot | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.27, 5.91] |
| Analysis 2.3  Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 3 Wound infection as defined by trial authors. | ||||
| 4 Long‐term complication ‐ physical test at 3 months (Janda's test) Show forest plot | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.73, 0.93] |
| Analysis 2.4  Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 4 Long‐term complication ‐ physical test at 3 months (Janda's test). | ||||
| 5 Postoperative hospital stay for mother (days) Show forest plot | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | 0.40 [‐0.34, 1.14] |
| Analysis 2.5  Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 5 Postoperative hospital stay for mother (days). | ||||
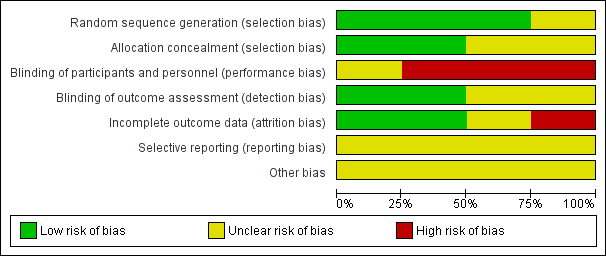
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 1 Postoperative febrile morbidity.

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 2 Postoperative analgesia on demand.

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 3 Time between surgery and first dose of analgesic (hours).

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 4 Total dose of analgesics in 24 hours.

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 8 Estimated blood loss (mL).

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 10 Blood transfusion.
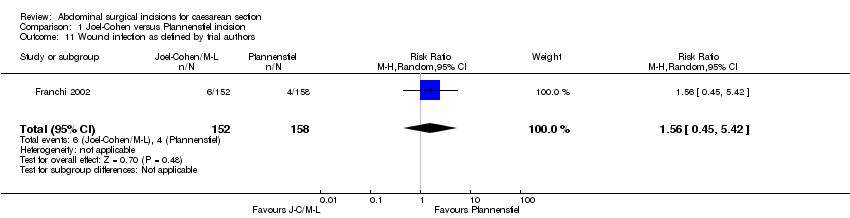
Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 11 Wound infection as defined by trial authors.

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 16 Time (hours) from surgery to start of breastfeeding.
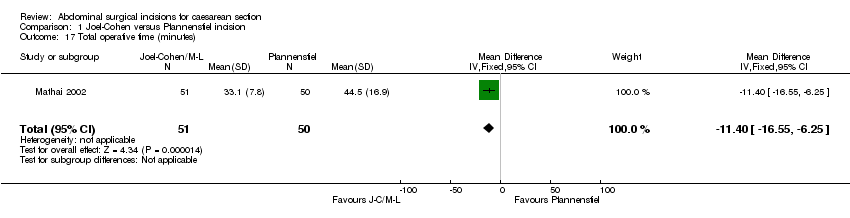
Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 17 Total operative time (minutes).
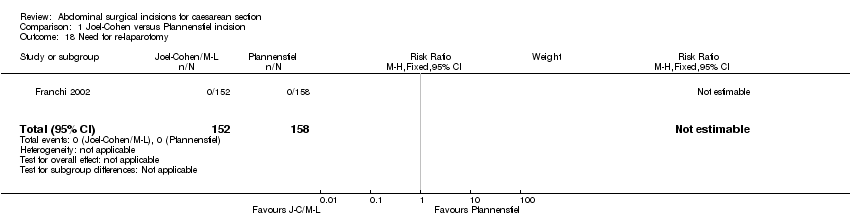
Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 18 Need for re‐laparotomy.

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 21 Delivery time (minutes).

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 23 Admissions to special care baby unit ‐ all types.
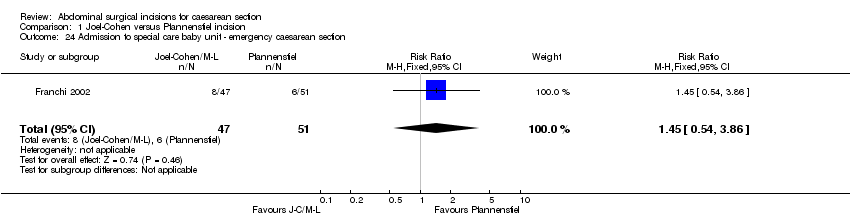
Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 24 Admission to special care baby unit ‐ emergency caesarean section.

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 25 Postoperative hospital stay for mother (days).

Comparison 1 Joel‐Cohen versus Pfannenstiel incision, Outcome 26 Stay in special care nursery (days).

Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 1 Postoperative febrile morbidity.
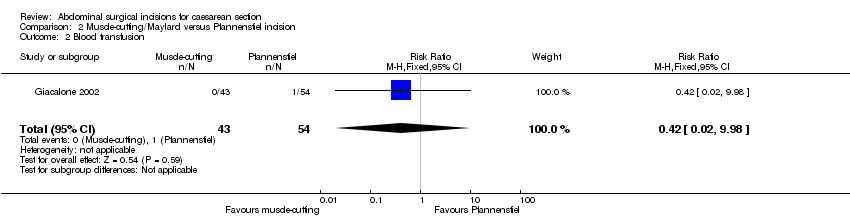
Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 2 Blood transfusion.

Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 3 Wound infection as defined by trial authors.

Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 4 Long‐term complication ‐ physical test at 3 months (Janda's test).
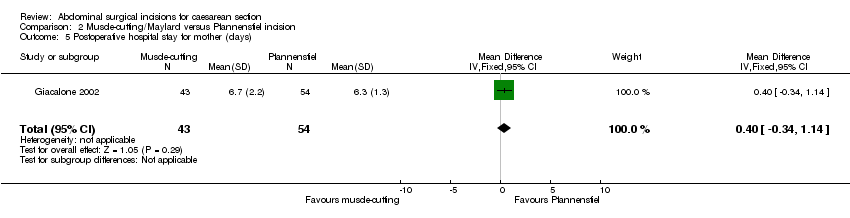
Comparison 2 Muscle‐cutting/Maylard versus Pfannenstiel incision, Outcome 5 Postoperative hospital stay for mother (days).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postoperative febrile morbidity Show forest plot | 2 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.14, 0.87] |
| 1.1 Joel‐Cohen versus Pfannenstiel incision | 2 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.14, 0.87] |
| 2 Postoperative analgesia on demand Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.40, 0.76] |
| 3 Time between surgery and first dose of analgesic (hours) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [0.12, 1.48] |
| 4 Total dose of analgesics in 24 hours Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐0.89 [‐1.19, ‐0.59] |
| 5 Number of analgesic injections required | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Duration of analgesics (hours) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number of analgesic doses required | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Estimated blood loss (mL) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐58.0 [‐108.51, ‐7.49] |
| 9 Change in pre‐ and postoperative haemoglobin levels (g) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Blood transfusion Show forest plot | 1 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Wound infection as defined by trial authors Show forest plot | 1 | 310 | Risk Ratio (M‐H, Random, 95% CI) | 1.56 [0.45, 5.42] |
| 12 Wound haematoma | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Postoperative pain absent on day 1 | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Postoperative pain absent on day 2 | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 "Significant" postoperative pain by visual analogue score | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Time (hours) from surgery to start of breastfeeding Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐5.5 [‐13.62, 2.62] |
| 17 Total operative time (minutes) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐11.40 [‐16.55, ‐6.25] |
| 18 Need for re‐laparotomy Show forest plot | 1 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Long‐term "significant" wound pain assessed by visual analogue score | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Not satisfied with wound | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Delivery time (minutes) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐1.90 [‐2.53, ‐1.27] |
| 22 5‐minute Apgar score less than 7 | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Admissions to special care baby unit ‐ all types Show forest plot | 1 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.44, 3.20] |
| 24 Admission to special care baby unit ‐ emergency caesarean section Show forest plot | 1 | 98 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.54, 3.86] |
| 25 Postoperative hospital stay for mother (days) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐2.16, ‐0.84] |
| 26 Stay in special care nursery (days) Show forest plot | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.95, 0.03] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Postoperative febrile morbidity Show forest plot | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.08, 19.50] |
| 2 Blood transfusion Show forest plot | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.02, 9.98] |
| 3 Wound infection as defined by trial authors Show forest plot | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.27, 5.91] |
| 4 Long‐term complication ‐ physical test at 3 months (Janda's test) Show forest plot | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.73, 0.93] |
| 5 Postoperative hospital stay for mother (days) Show forest plot | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | 0.40 [‐0.34, 1.14] |

