Servicios de enfermería especializada en el domicilio para niños con enfermedades agudas y crónicas
Resumen
Antecedentes
Se ha sugerido que los servicios de enfermería pediátrica especializada en el domicilio constituyen un medio rentable para disminuir el estrés que resulta de los ingresos hospitalarios, al tiempo que mejoran la atención primaria y reducen la estancia hospitalaria. Esta revisión es una actualización de la revisión original, que fue publicada en 2006.
Objetivos
Evaluar servicios de enfermería especializada en el domicilio para niños con enfermedades agudas y crónicas.
Métodos de búsqueda
Se realizaron búsquedas en las siguientes bases de datos en febrero 2012: Reg¡stro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL) en The Cochrane Library 2012, número 2, Ovid MEDLINE, EMBASE, PsycINFO, CINAHL y en Sociological Abstracts. También se hicieron búsquedas en ClinicalTrials.gov y en la WHO International Clinical Trials Registry Platform. No se aplicaron restricciones en cuanto al idioma.
Criterios de selección
Ensayos controlados aleatorios (ECA) en niños desde el nacimiento hasta los 18 años de edad con enfermedades agudas o crónicas asignados a los servicios de enfermería especializada en el domicilio en comparación con la asistencia sanitaria convencional. Los resultados fueron: uso de los servicios de salud, salud física y mental, satisfacción, resultados de salud adversos y costos.
Obtención y análisis de los datos
Dos autores de la revisión extrajeron los datos de los estudios de forma independiente y resolvieron las discrepancias recurriendo a un tercer autor. El metanálisis no fue apropiado debido a la diversidad clínica de los estudios y a la ausencia de medidas de resultado comunes.
Resultados principales
Se examinaron 4226 títulos, lo cual produjo siete ECA con un total de 840 participantes. Los participantes, las intervenciones y los resultados fueron diversos. No se informaron diferencias significativas en los resultados de salud; dos estudios informaron una reducción de la estancia hospitalaria sin diferencias en las tasas de reingreso al hospital. Tres estudios informaron una reducción de la ansiedad paterna y tres estudios observaron una mejoría en el comportamiento de los niños. Se informó un aumento general de la satisfacción paterna en tres estudios. Además, se informó una mejoría en el afrontamiento paterno y el funcionamiento familiar en un estudio. Por el contrario, un estudio no observó un impacto sobre la carga de atención paterna y otro no informó un efecto sobre el estado funcional de los niños. Se informó que la atención domiciliaria fue más costosa para los proveedores del servicio con reducciones apreciables de los costos para la familia en dos estudios, mientras que un estudio no reveló beneficios significativos en los costos para la familia.
Conclusiones de los autores
La investigación actual no aporta pruebas para apoyar una reducción en el acceso a los servicios hospitalarios o una reducción de la tasa de reingresos al hospital para los niños con enfermedades agudas y crónicas mediante el uso de los servicios de enfermería especializada en el domicilio; sin embargo, el único hallazgo resumido a través de unos pocos estudios fue que existe una disminución significativa en la estancia hospitalaria. Los resultados preliminares no muestran un impacto adverso sobre los resultados de salud física y varios documentos informaron una mejoría en la satisfacción con la atención domiciliaria. Se requieren ensayos adicionales que midan la salud, la satisfacción, el uso de servicios y los costos a largo plazo.
PICO
Resumen en términos sencillos
Servicios de enfermería especializada en el domicilio para niños con enfermedades agudas y crónicas
El objetivo de esta revisión fue estudiar si los servicios de enfermería especializada en el domicilio para niños y adolescentes con enfermedades agudas y crónicas reducen el número de ingresos y la estancia hospitalaria, mejoran la asistencia sanitaria en la comunidad y reducen el estrés para las familias motivado por la enfermedad de sus hijos. Ésta es una actualización de la revisión original publicada en 2006. Se encontraron siete ensayos controlados aleatorios (ECA) relevantes con un total de 840 niños desde el nacimiento hasta 18 años de edad que presentaban enfermedades agudas o crónicas y que estaban recibiendo servicios de enfermería especializada en el domicilio o asistencia sanitaria convencional. Los resultados fueron: uso de los servicios de salud, salud física y mental, satisfacción, resultados de salud adversos y costos. Se decidió no combinar los resultados de estos ECA debido a la variedad en los tipos de servicios proporcionados, los tipos de participantes y las medidas de resultado utilizadas. El análisis de los resultados de los ECA individuales muestra un incremento de la satisfacción con la atención domiciliaria, sin repercusiones adversas sobre los resultados de salud física para los pacientes. Hay algunas pruebas de que los servicios de enfermería especializada en el domicilio reducen la estancia hospitalaria; sin embargo, no existen pruebas de que resulten en una reducción en el uso de los servicios hospitalarios. Se requieren ensayos adicionales que midan la salud, la satisfacción, el uso de servicios y los costos a largo plazo.
Authors' conclusions
Background
Description of the condition
The illness of a child leading to hospitalisation is a stressful event for the family (Kai 1996). It can be distressing for children, as in some emergency departments they may be separated from their families and the security of their own home (Farquahar 1990; Lenihan 1985). While not every child who presents to a hospital is admitted (Cooper 2000), many such children spend several hours in the emergency department (ED) while being observed or assessed (Browne 1996); in addition, children may wait while their carers are provided with education on how to manage the child's illness.
Children presenting at EDs frequently have a non‐urgent problem (Bowling 1987; Halfon 1996; Jones 1999; Worsley 1985) and no usual care provider (Beebe 1993; Grover 1994). Many parents take their child to an ED seeking reassurance (Boyle 2000). These presentations, and subsequent admissions, may provide opportunities to give carers the confidence to support and care for their child, as well as to provide education about the disease process and its management. Admission of children is not always determined by the severity of their illness; it can also be influenced by previous medical consultations for the illness as well as parental expectations that the child will not be discharged from the ED (Cooper 2003).
In the current era, the necessity to explore alternative models of service delivery such as home‐based nursing services has become more important, based on increasing survival of children with complex conditions, and also as it has become more feasible to provide high‐technology interventions at home (Parker 2012). Thus, there is a shift towards parents being more responsible for complex care for children children with chronic illnesses in the home settings with educational as well as clinical management support.
Description of the intervention
The need to reduce hospital admission rates and shorten the length of hospital stay has prompted the development of specialist home‐based nursing services for children with acute and chronic illnesses. The home‐based nursing care substitutes for acute hospital review and/or admission by providing clinical review, support, education and management of the acutely or chronically unwell child in their own home. If the child requires it, they are provided with streamlined access to hospital services. It has been postulated that these services have the potential to reduce the number of hospital admissions (Meates 1997; Smith 1986), to reduce the length of stay (Meates 1997; Whiting 1997) and to facilitate early discharge by providing a continuum of care from the hospital into the home (Meates 1997). They also provide opportunities to enhance primary care in the community through liaison with general practitioners (GPs) and through links with other community‐based health services (Fradd 1994).
Why it is important to do this review
The development of specialist home‐based nursing services for children with acute and chronic illnesses has been determined by local circumstance and enthusiastic individuals rather than strategic planning based on evidence (While 2000), resulting in a diverse range of service models. Much of the literature comprises accounts of service development (Box 1993) or descriptive studies of parent or professional views (Madigan 1997; Sartain 2001). Literature related to the safety of models of care is limited (McConnochie 1998; Montalto 1998) and concerns are rapidly increasing about the impact of changes in delivery and financing mechanisms on quality of care (Kelly 1994). Empirical data are needed about the effects of specialist home‐based nursing services for children with acute and chronic illnesses, to explore the strengths and weaknesses of different service models, as well as general efficacy.
The literature search for this review was completed in 2005 prior to its first publication (Cooper 2006). Subsequently, a systematic review was published in the UK about international evidence for the effectiveness and costs of paediatric home care. The Parker 2012 review was produced because there had not been a substantial growth in this kind of service despite advocacy by policy makers and professionals over the past few decades. We have conducted this update on a similar basis, to explore the available international evidence regarding specialist home‐based nursing services for children and adolescents.
Objectives
To evaluate the impact of specialist home‐based nursing services for children with acute and chronic illnesses.
Methods
Criteria for considering studies for this review
Types of studies
Trials were eligible for inclusion in the review if:
-
The assignment of study participants to the intervention or control group was random or quasi‐random, for example, by alternate allocation;
-
The study intervention had paediatric nursing outreach services as its major focus;
-
There was at least one objective measure, for example, hospital admission data and/or a standardised measure such as a behaviour checklist, and that such measures were used for both intervention and control groups.
Types of participants
Children aged from birth to 18 years with acute and or chronic illnesses. In this review, terms such as 'chronic illness' and 'long‐term illness' are used interchangeably.
Types of interventions
Specialist home‐based nursing services provided to children with acute illnesses and/or chronic and complex conditions, compared with conventional health care (for example, hospital admission) as the control group. We excluded studies where nurses provided planned illness educational support independent of clinical review and management of children with acute and/or chronic diseases.
Types of outcome measures
-
Physical health of participants;
-
Mental health of participants;
-
Utilisation of emergency departments (EDs);
-
Hospital admissions;
-
Length of stay in hospital;
-
Parental, child and referrer satisfaction;
-
Quality of life of children and their carers;
-
Cost of treatment for the family and to the service providers.
The study outcomes were measured using the following.
-
Hospital data on service utilisation, admissions, length of stay.
-
Questionnaires, for example, quality of life questionnaires, health outcome rating scales.
-
Satisfaction surveys.
Search methods for identification of studies
Electronic searches
This update is based on database searches run in February 2012 (Appendix 1), which cover the period since the search date of the previous version of this review in August 2005. We used the most recent version of the Cochrane highly sensitive search strategy for identifying randomised trials in Ovid MEDLINE (Lefebvre 2008) and searched two additional sources (ClinicalTrials.gov and International Clinical Trials Registry Platform).
We searched the following databases with no language restrictions.
The Cochrane Central Register of Controlled Trials (CENTRAL), part of the The Cochrane Library, 2012 Issue 2, last searched 9 February 2012;
Ovid MEDLINE (1946 to January Week 4 2012), last searched 8 February 2012;
CINAHL (1937 to current), last searched 9 February 2012;
EMBASE (1980 to 2012 Week 05), last searched 9 February 2012
PsycINFO (1806 to Feb Week 1 2012), last searched 9 February 2012;
Sociological Abstracts (Sociofile) (1952 to current), last searched 9 February 2012;
ClinicalTrials.gov, all available years searched 10 February 2012;
International Clinical Trials Registry Platform, all available years searched 10 February 2012.
Searching other resources
The archives of abstracts from the Pediatric Academic Societies (incorporating the American Ambulatory Pediatric Association and the Society for Pediatric Research) Annual Scientific Meetings from 2000 to 2012 did not yield any unpublished data from randomised trials evaluating specialist home‐based nursing services for children. We had no responses to emails to the Ambulatory Care Australia email list and the 'Hospital in the Home' electronic exchange.
Data collection and analysis
Selection of studies
Three review authors working independently (CC, DW, SW) screened titles and abstracts from the searches for the original review and two authors (CP, CC) screened results for this update. We resolved disagreements by consensus. We obtained potentially relevant articles for assessment of the full text and for data extraction.
Data extraction and management
We input data using Review Manager 5.1 (Cochrane Handbook). Data extraction forms were developed a priori and included information about study location, methods, participants, type of ambulatory paediatric intervention, and outcomes. Two review authors (CC, SW) independently performed data extraction for the initial phase of the review and two (CP, CC) for the next phase. We resolved disagreements by negotiation with a third review author (DW for the first phase and SW for the second phase).
Assessment of risk of bias in included studies
We assessed the risk of bias for the five previously included studies and the two newly added studies using the domain‐based evaluation tool described in the Cochrane Handbook. Each study was assessed as being at low, high or unclear risk of bias for allocation concealment, blinding, incomplete outcome data and other sources of bias.
Measures of treatment effect
We report mean differences and 95% confidence intervals for continuous variables, where they were available. For binary outcomes, we report the risk ratio and 95% confidence interval. For meta‐analysis, where possible in future updates, we will use mean differences for continuous variables, with standardised mean differences if different scales measure the same construct in different studies, and risk ratios for binary outcomes.
Dealing with missing data
We analysed data where possible on an intention‐to‐treat basis, i.e. with all participants randomised in their original groups. We contacted trial authors to obtain missing or additional information.
Assessment of reporting biases
The tool described in the Cochrane Handbook was used to assess the risk of bias in included studies. Two authors (CP, CC) independently carried out this assessment and there was an agreement among both for conclusions.
Data synthesis
Due to the clinical diversity of the participants' illnesses and the services offered, as well as a lack of common outcome measures, we decided against meta‐analysis and statistical assessment of heterogeneity (the I² statistic; Higgins 2002), and we therefore provide a narrative summary. In future updates, we intend to include any available data in meta‐analyses if it proves feasible.
Subgroup analysis and investigation of heterogeneity
We stratified the results to determine any differences in treatment effects according to age and type of intervention:
-
Clinically different interventions, for example, hospital‐based versus community‐based services;
-
Clinically relevant differences between groups of participants:
-
children with acute illness, children with chronic illness, children with chronic haematological illnesses;
-
children under 10 years, children between 10 and 18 years.
We present results according to the above subgroups. However, statistical subgroup analysis was not possible for the current version of this review.
Sensitivity analysis
Sensitivity analysis (to evaluate the impact of study quality on outcome) was not possible. If a meta‐analysis can be undertaken in future updates, we will use sensitivity analyses to determine the impact of risk of bias on our findings.
Results
Description of studies
Results of the search
The original review included five studies. The search was run again from August 2005 until February 2012. A total of 2570 new titles were screened and 152 duplicates were identified. Of the 2418 titles screened, 2347 were not relevant to the review. We read the remaining 71 articles to obtain further information and only two studies (Stevens 2006; Tie 2009) were suitable for inclusion, giving a total of seven studies in this update. See the study flow diagrams Figure 1 and Figure 2.
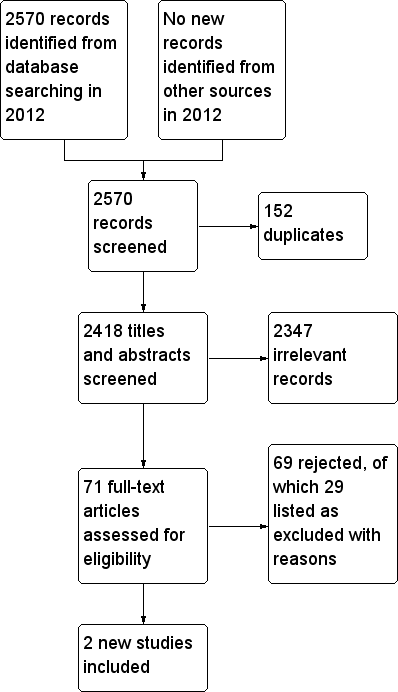
Study flow diagram for records found during 2012 update searches

Study flow diagram incorporating all records for lifetime of review
Included studies
Please see Characteristics of included studies table for more detailed information.
The number of participants in the seven included studies ranged from 29 (Stevens 2006) to 399 (Sartain 2001). The total number of participants across all the included studies was 840. Participants in these studies ranged from three months of age through to 17 years of age. Specialist home‐based nursing outreach services were provided as an intervention in each study. However, studies differed in respect of the qualifications of the nurses and their availability, including hours of service and number of visits. This is detailed in Table 1, 'Characteristics of Interventions'. No two studies examined the same intervention. In addition, treatments and outcomes varied considerably. Included studies broadly fell under the following categories.
| Study | Study settings | Type of illness ‐ intervention | Hours Available | No. visits possible | Staff Qualifications | Information provided |
| Queen's University, University of Toronto, Ontario, Canada | Children with chronic conditions ‐ stress‐point intervention for parents | Not reported. | Not reported. | "master's prepared nurse". | Mailed summaries and reminders of families own stress points and coping strategies. | |
| The Montreal Children's Hospital, Montreal, Quebec, Canada | Newly diagnosed children with IDDM ‐ Home based treatment | 24 hour telephone consultation. | Home visits once/twice daily for first 2 ‐ 3 days, teaching visit at clinic after 2 weeks, follow‐up outpatient visits at 2 ‐ 3 months. | Diabetes treatment nurse, as part of a team of diabetes‐specialist physician, psychologist and social worker. | Teaching session, instruction and supervision in practical and theoretical aspects of treatment. | |
| Arrow Park Hospital, Upton, Wirral, UK | Acute illness (breathing difficulty, diarrhoea and vomiting or fever) ‐ Hospital at home scheme treatment | 24 hours, 7 days. Service until 2300, on‐call overnight. | 1 ‐ 4 daily | Not specified. | Patient information booklets detailing possible course of illness, signs and symptoms of potential deterioration, appropriate treatment, contact information. | |
| Paediatric Ambulatory Care Division, Albert Einstein College of Medicine, Bronx, New York | Heterogenous group of children with chronic illnesses ‐ Paediatric home care | Not specified. | Minimum package: initial home visit, one contact (by person or by telephone) each month for 6 months. Most participants received more. | Team of generalist paediatricians, paediatric nurse practitioners and social worker. | "Teach child and family about condition and train them in self‐care skills". | |
| University of Toronto and Sick Kid's Hospital, Toronto, Canada | Children with acute lymphoblastic leukemia ‐ Home chemotherapy | Not specified. | Home visits for administration of chemotherapy as per the protocol. | Trained nurse from a community health services agency administered chemotherapy, routine contact by community nurse to the oncologist if concerns. | Parents encouraged to contact primary nurse at the oncology clinic at the hospital as required | |
| The Montreal Children's Hospital, Montreal, Quebec, Canada | Management of bleeding in hemophilic children | 24‐hour service when incident (bleeding in children with haemophilia) occurred. | Not specified. | Specially trained nurse. | No educational intervention reported. | |
| Department of General Paediatrics, Princess Margaret Hospital for children, Perth, Western Australia | Acute bronchiolitis ‐ home oxygen therapy | Not specified | "Hospital in the home (HiTH)" nurse home visit within 12 hours of hospital discharge, minimum of 2 home visits, one phone contact with parents in every 24‐hour period. | Not specified. | Parents were educated on home oxygen use and instructed on how to observe their children for signs of clinical deterioration. |
Study design
Five trials used parallel study designs while two had a cross‐over study design. Participants were allocated to the intervention versus usual posthospitalisation care in two studies (Burke 1997; Stein 1984) and to traditional inpatient care in the other three (Dougherty 1998; Sartain 2001; Tie 2009). Strawczynski 1973 was a cross‐over study with participants spending a year in each of the intervention and control (hospital care) groups. Another cross‐over study was Stevens 2006, with participants receiving each of hospital (standard care) or home (intervention) chemotherapy alternately over a period of six months in succession.
Interventions for children with acute paediatric illnesses
There were only two studies that evaluated home‐based nursing intervention for children with acute illnesses. Sartain 2001 focused on children with acute paediatric illness with breathing difficulty, diarrhoea and vomiting or fever. The intervention, home care, was defined as clinical nursing care in a patient's own home, as an alternative to hospital admission. Treatment in this study was between one and four home visits per day, with the number of days and visits determined by health professionals in conjunction with parents. This study examined readmission rates and length of stay data as outcomes. The second study (Tie 2009) compared home oxygen therapy with traditional inpatient hospital care for children with acute bronchiolitis. The children in the home care group continued with oxygen therapy at home following initial hospitalisation and were supported by the nurse home visiting programme accompanied by parental education. The outcomes assessed were readmission to hospital within seven days of discharge home and the total duration of hospitalisation.
Interventions for children with a range of chronic conditions
Stein 1984 examined home care provided to children with chronic conditions through traditional clinics, inpatient units or a home care office. The minimum package was an initial assessment, one home visit and one monthly contact thereafter for at least six months. Involvement in home care was reassessed every six months by the treating staff. This study measured outcomes related to psychological adjustment and functional status.
Another study (Burke 1997) examined a community‐based stress‐point intervention provided by nursing staff to children with chronic illness. The intervention began two weeks before a planned hospital admission and continued until two weeks postdischarge. This study collected data throughout the intervention period using various scales to assess outcomes including stress and behavioural responses.
Interventions for children with newly diagnosed insulin‐dependent diabetes mellitus (IDDM)
Dougherty 1998 examined home‐based care provided by nursing staff over an extended period to newly diagnosed diabetic children, as an alternative to inpatient care. Nursing staff initially provided twice‐daily home visits in the first few days after diagnosis, with transition to diminishing visits or phone calls to the family over two weeks, but remained available to the family for telephone contact for the next 24 months. This study focused on outcomes of diabetic management including metabolic control and diabetes‐related adverse events.
Interventions for children with chronic haematological illnesses
Strawczynski 1973 defined home care as the availability of access to a 24‐hour nursing service to treat acute bleeds at home or at school for children with haemophilia, as soon as possible after they occurred. It did not report on the number of days or visits for individual children. This study reported the number of bleeds and reduction in procrastination time for haemophilia as its outcomes.
Another study (Stevens 2006) compared a hospital‐based and a home‐based programme for children with acute lymphoblastic leukaemia (ALL). Some of the chemotherapy treatment was delivered by the hospital pharmacy to children's homes and was then administered by a trained nurse from a community health service agency. The option of contacting a hospital oncology nurse was available to parents as required. The study outcomes were child's quality of life, the burden on parental caregivers, adverse effects and costs.
Excluded studies
Please see Characteristics of excluded studies table for details of the 41 excluded studies.
Risk of bias in included studies
The risk of bias for seven included studies was assessed using the Cochrane domain‐based evaluation tool (Cochrane Handbook: Chapter 8) and is summarised below in Figure 3 and Figure 4.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
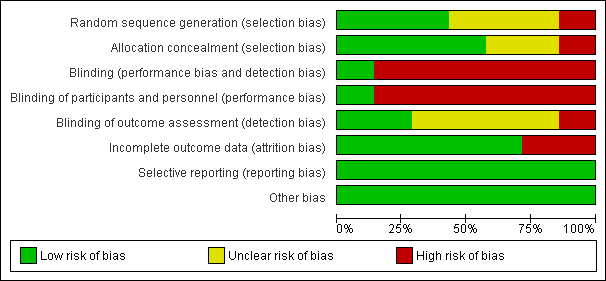
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
While all seven studies stated that participants were randomised, only three gave information about the methods of randomisation or allocation concealment, and details were not reported for two studies (Dougherty 1998; Tie 2009). Opaque sealed numbered envelopes were used in one study (Sartain 2001) and a dice roll with opaque sealed envelopes in another (Stein 1984). A table of random numbers was used in a third study (Stevens 2006), but with no mention of the allocation concealment. Another study (Burke 1997) used randomisation by a secretary blinded to the study details but the method of allocation concealment was not clarified. Quasi‐randomisation was used in one study with alternate allocation (Strawczynski 1973).
Where necessary, we contacted study authors for clarification or missing information, but received no replies.
Blinding
Outcome assessors were reported to be blind to the intervention groups in two of the included studies. Burke 1997 used study nurses to administer the pretest to participants. Research assistants blinded to study group membership administered post‐test questionnaires. Study nurses did not have contact with hospital staff during the study. In Dougherty 1998, the principal investigators were not blinded to the intervention; however, results for the intervention and control groups were not disclosed before the end of the trial. Stein 1984 made no attempt to blind interviewers to the intervention status, but there was no direct contact between the clinicians and interviewers. Strawczynski 1973 was not able to blind clinical staff to intervention status or outcome measures. Sartain 2001 had the same researcher conduct all interviews in the participant's home within two weeks of discharge. It was not stated that the interviewer was blind to group allocation; however, the allocation is likely to have been disclosed during the interview. Stevens 2006 and Tie 2009 did not mention details of blinding, but the study methodology implies that blinding of neither participants nor clinicians was possible.
Incomplete outcome data
The number of participants lost to follow‐up varied. Three studies (Dougherty 1998; Sartain 2001; Tie 2009) reported no withdrawal of participants. Burke 1997 recruited 50 children and two were lost to extended follow‐up (4% loss). Loss to follow‐up was 15% for Stein 1984 at six months and 17% at one year. Strawczynski 1973 enrolled 40 patients with four (10%) lost to follow‐up. Of these, one died of an intracranial haemorrhage; one developed a circulating anticoagulant, and two moved away from the study city. Stevens 2006 randomised 29 children and two from each group withdrew at the start of the study due to relapse. Throughout the study, at four data collection stages, data were not available for analysis on one or two participants from each group. Only one study (Sartain 2001) conducted an intention‐to‐treat analysis.
Selective reporting
All studies appear to have reported on all measured outcomes.
Other potential sources of bias
There were no other potential sources of bias in the included studies.
Effects of interventions
Meta‐analysis was not appropriate in this review because of the range of outcome measures being reported. In addition, interventions were diverse and complex involving multidisciplinary teams, different hours of service and variable inclusion of educational components (see Table 1). Participants were also diverse: some had chronic illnesses such as diabetes, haemophilia, acute lymphoblastic leukaemia (ALL), and others had an acute presentation. Results are therefore presented as a written summary of individual studies only, without data synthesis.
Physical health of participants (including harmful effects)
Stein 1984 reported presentations for concurrent illness during the period of the study and found no significant difference in general health between the intervention and control groups of children with a range of chronic conditions.
Burke 1997 identified improved parental ability to cope with illness in a chronically ill child three months postintervention (P < 0.001).
Dougherty 1998 reported on metabolic control and diabetes‐related adverse events in children with newly diagnosed insulin‐dependent diabetes mellitus (IDDM). At 24 months, the home care group had lower mean HbA1c levels (biological measure of diabetic control), 6.1% versus 6.8% (P < 0.02). There was no difference between the two groups for adverse diabetes‐related clinical events.
Strawczynski 1973 reported on the number of bleeds and procrastination time in children with haemophilia presenting with a bleed. Overall, significantly more bleeding episodes were reported in the home care programme, with the majority of these being mild to moderate bleeds. Severe bleeds were significantly more likely in the hospital programme (P value not reported). Procrastination time was defined as the time elapsed between the bleed occurring and reporting for treatment. Reported procrastination time decreased in the intervention group (mean 17 hours, compared to 29 hours in the control group; P value and significance not reported).
Stevens 2006 used Pediatric Oncology Quality of Life Scale (POQOLS) to assess quality of life, and reported no significant long‐term difference between the hospital and home treatment groups in values for sensitivity to restrictions in physical functioning and the ability to maintain a normal physical routine.
Mental health of participants
Stein 1984 reported on psychological adjustment for children with a range of chronic conditions. For children five years and older, there was a significant improvement in the child's psychological adjustment at six months postintervention (P < 0.05), with some diminution by 12 months postintervention (P < 0.10). Mothers in the home care group showed improvement in mental health symptoms compared to those in the control group (P = 0.07).
Burke 1997 reported on the behaviour and anxiety of children with a range of chronic conditions. There was no significant difference between the two groups for child behaviour. However, at three months postintervention, intervention group parents were less anxious, with this difference being statistically significant. The intervention group had significantly less discrepancy between desired and actual family functioning at the end of three months of intervention.
Stevens 2006 used Child Behavior Checklist scores to identify behavioural problems and social competence among the study participants and reported no significant difference between intervention and control groups at any of the follow‐up periods.
The utilisation of emergency departments (EDs)
No studies offered data for this outcome.
Hospital admissions
Sartain 2001 reported that there were no significant differences between home care and hospital care readmissions over 90 days, at 21 (10.0%) and 15 (7.9%) respectively (P = 0.49). Of those in home care, 14 were readmitted once (7%), two were readmitted twice (1%) and one child was readmitted three times (1%). For hospital care, 13 (7%) were readmitted once and one (< 1%) twice. No child was readmitted more than twice. No other studies reported on this outcome.
Tie 2009 reported that hospital readmission rates were the same for children with acute bronchiolitis within seven days of discharge for traditional hospital care versus home care. One child from each group of 22 participants required readmission.
Length of stay in hospital
Four studies reported on length of service provision. This was reported in several ways, including bed days, inpatient stay and use of hospital‐based services. Sartain 2001 reported that children with acute illnesses who were in the control group, i.e. usual hospital treatment, were more likely to have a longer stay than those in the home care group, with mean bed stay of 2.37 versus 1.37 days (P < 0.0001).
Dougherty 1998 reported that there was no difference between both groups in the mean days spent in the intensive care unit at diagnosis. However, mean hospital inpatient stay was lower with home‐based care (2.2 +/‐ 1.6 nights, 70 total) compared to hospital‐based care (4.7 +/‐ 1.6 nights, 147 total). The use of services while hospitalised was lower for the home‐based group, logistically because of shorter initial hospital stay. However, they did report that children receiving home care used more diabetes nursing hours during the 24‐month period, 58.9 hours per child compared with 17.3 hours for standard care (P value and significance not stated), which implies that the intervention required more intensive nursing support.
Strawczynski 1973 reported the total number of treatment days for children with haemophilia in the home care group was 2030 compared with 1644 for the hospital‐based group. However, only 241 from the home care group needed hospitalisation during the treatment period (P value and significance not reported).
Tie 2009 reported that children in the 'hospital in the home' treatment group spent significantly less time in a hospital bed (55.2 hours) than those in the hospital group (96.9 hours) (P = 0.001).
Parental, child and referrer satisfaction
Sartain 2001 collected parent‐reported data for children with acute paediatric illnesses from a subset of the intervention group, which found that 36 of 40 (90%) parents and 7 of 11 (66%) children would prefer to access a 'Hospital at Home' service. There was a perception that children receiving the 'Hospital at Home' service recovered more quickly in their own environment and that there was less social disruption and financial burden for the family.
Stein 1984 identified overall greater satisfaction from respondents, with medical care provided in the home care group (P < 0.05) for children with a range of chronic conditions.
Quality of life of children and their carers
At three months post‐intervention, Burke 1997 reported that for children with chronic illnesses, the home care group had greater satisfaction in family functioning (P < 0.001); greater parental ability to cope (P < 0.001); greater family ability to cope (P < 0.001); a greater ability in personal and social care coping (P < 0.01); and a greater perception of helpfulness from healthcare providers and institutional sources (P < 0.001).
Stein 1984 did not observe a significant difference for the impact of chronic illness on families between those receiving home care and those in the control group (P = 0.14).
Strawczynski 1973 reported significantly better school attendance (P value not stated) in the home care group, with an average of 2.5 school days missed compared to six days in the hospital programme for children with haemophilia.
Stevens 2006 reported no evidence of an effect of the location (i.e. home or hospital) where chemotherapy was administered in relation to parental burden of care using Caregiving Burden Scale (CBS) at different stages during the study period. Another important finding was that the age of the child was a significant predictor, with inverse effect being observed on quality of life, caregiver burden and adverse events.
Costs
Sartain 2001 assessed costs for children with acute paediatric illnesses in a separate paper (Bagust 2002). A number of parents thought that hospital care was more costly for them, with 20% of parents in the home care programme commenting on savings resulting from remaining at home and 30% of parents in the hospital care group commenting on the financial cost of the child staying in hospital.
Dougherty 1998 found that for children with newly diagnosed IDDM, there were social cost savings. This means that there were savings across hospital, physicians, tax payers and families. There were also parental cost savings (difference between out‐of‐pocket expenses and the value of their time diverted to care for their child from other activities) of CAD 188 for each child on the home care programme (P < 0.001) and an increased cost to the hospital of CAD 87 per child on the home care programme (P < 0.001).
Strawczynski 1973 reported total costs for providing both the home care and the hospital programme but did not give separate information on costs for the intervention and control groups.
Stevens 2006 did not find any significant difference between costs for the family (societal perspective) associated with home chemotherapy and standard care (P = 0.79).
Discussion
Summary of main results
Two studies of children with acute paediatric illnesses (Sartain 2001; Tie 2009) reported a statistically significant reduction in the duration of hospital stay, with no significant difference in readmission rates
A variety of assessment tools were used in the studies included in this review to measure the functional impact or quality of life. Burke 1997 found that home‐care parents postintervention had better coping skills, family functioning and a reduction in anxiety than those in the traditional care group. No differences in child behaviour were reported in either group. A similar finding of no significant differences in child behaviour was reported in two other studies (Dougherty 1998; Stevens 2006) which used Child Behaviour Checklist (CBCL) for the assessment. A reduction in parental anxiety was noted in two other studies, with Burke 1997 and Stein 1984 reporting an improvement in mental health symptoms for mothers in the study group. Another study (Strawczynski 1973) reported better school attendance in the home‐care children. Stein 1984 did not detect any significant impact of the intervention on the functional status of the participating children; Stevens 2006 reported that neither home or hospital location for treatment affected the parental burden of care. Overall, parental satisfaction with the home‐based nursing care was reported in three studies (Sartain 2001; Stein 1984; Strawczynski 1973) which included semi‐structured parental interviews.
Cost effectiveness was not comprehensively addressed by any of the included studies. Three studies presented limited cost data. Dougherty 1998 suggested that the financial cost to the hospital of providing the home‐based care programme may cost more than the hospital‐based care, but suggested that there are substantial cost savings for the family from the home‐care programme. This view was supported by Sartain 2001, who presented qualitative data on cost savings for families in the home‐care programme versus increased expenditure for families in the hospital‐care group. Interestingly, Stevens 2006 did not find any difference in family costs from a societal perspective in either home‐ or hospital‐based treatment groups.
Overall completeness and applicability of evidence
There was wide clinical diversity between studies due to differences in participants, disease or condition requiring care, interventions and outcomes measured. There was also variation in the statistical methods used by studies. For these reasons, we did not conduct meta‐analyses, which should be taken into consideration when drawing conclusions from this review. Few benefits of home‐based nursing care were evident in the included studies. However, current studies (Dougherty 1998; Sartain 2001; Stevens 2006) do not take into account the original set‐up costs of traditional inpatient services, or the long‐term cost savings for children and families achieved by a less disruptive model of care. Further research is required that examines the long‐term costs to both service providers and families before an economic rationalisation of home care can be attempted.
Quality of the evidence
This systematic review included seven randomised controlled trials with 840 participants ranging from three months to 17 years. Only one study (Burke 1997) blinded participants and personnel while only two blinded the process of outcome assessment (Burke 1997; Dougherty 1998). The risks of performance and detection bias should be considered when interpreting results of the relevant studies. Also, some studies have a limited sample size which impacts on the statistical power of the study.
Potential biases in the review process
The authors followed the process of systematic review as detailed in the Cochrane Handbook and have tried to minimise the likelihood of potential biases in the review process.
Agreements and disagreements with other studies or reviews
The findings of reduction of hospital stay and hospital readmission rates with home‐based nursing care are consistent with some findings from the previously published literature (Meates 1997; Smith 1986; Whiting 1997). A recent systematic review (Parker 2012) on the paediatric home care services reported some evidence of reduced burden and costs for families, particularly in relation to acute admission avoidance. This is consistent with some of the cost‐effectiveness findings in the studies included in this review. A mixed‐methods study based in the UK (Spiers 2012 ) enumerates the diversity and complexity as well as variable clinical coverage of the service delivery models which are categorised as 'care closer to home'. This is consistent with the diverse clinical settings of the included studies in this review.

Study flow diagram for records found during 2012 update searches

Study flow diagram incorporating all records for lifetime of review

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
| Study | Study settings | Type of illness ‐ intervention | Hours Available | No. visits possible | Staff Qualifications | Information provided |
| Queen's University, University of Toronto, Ontario, Canada | Children with chronic conditions ‐ stress‐point intervention for parents | Not reported. | Not reported. | "master's prepared nurse". | Mailed summaries and reminders of families own stress points and coping strategies. | |
| The Montreal Children's Hospital, Montreal, Quebec, Canada | Newly diagnosed children with IDDM ‐ Home based treatment | 24 hour telephone consultation. | Home visits once/twice daily for first 2 ‐ 3 days, teaching visit at clinic after 2 weeks, follow‐up outpatient visits at 2 ‐ 3 months. | Diabetes treatment nurse, as part of a team of diabetes‐specialist physician, psychologist and social worker. | Teaching session, instruction and supervision in practical and theoretical aspects of treatment. | |
| Arrow Park Hospital, Upton, Wirral, UK | Acute illness (breathing difficulty, diarrhoea and vomiting or fever) ‐ Hospital at home scheme treatment | 24 hours, 7 days. Service until 2300, on‐call overnight. | 1 ‐ 4 daily | Not specified. | Patient information booklets detailing possible course of illness, signs and symptoms of potential deterioration, appropriate treatment, contact information. | |
| Paediatric Ambulatory Care Division, Albert Einstein College of Medicine, Bronx, New York | Heterogenous group of children with chronic illnesses ‐ Paediatric home care | Not specified. | Minimum package: initial home visit, one contact (by person or by telephone) each month for 6 months. Most participants received more. | Team of generalist paediatricians, paediatric nurse practitioners and social worker. | "Teach child and family about condition and train them in self‐care skills". | |
| University of Toronto and Sick Kid's Hospital, Toronto, Canada | Children with acute lymphoblastic leukemia ‐ Home chemotherapy | Not specified. | Home visits for administration of chemotherapy as per the protocol. | Trained nurse from a community health services agency administered chemotherapy, routine contact by community nurse to the oncologist if concerns. | Parents encouraged to contact primary nurse at the oncology clinic at the hospital as required | |
| The Montreal Children's Hospital, Montreal, Quebec, Canada | Management of bleeding in hemophilic children | 24‐hour service when incident (bleeding in children with haemophilia) occurred. | Not specified. | Specially trained nurse. | No educational intervention reported. | |
| Department of General Paediatrics, Princess Margaret Hospital for children, Perth, Western Australia | Acute bronchiolitis ‐ home oxygen therapy | Not specified | "Hospital in the home (HiTH)" nurse home visit within 12 hours of hospital discharge, minimum of 2 home visits, one phone contact with parents in every 24‐hour period. | Not specified. | Parents were educated on home oxygen use and instructed on how to observe their children for signs of clinical deterioration. |

