مقایسه مراقبت پرستار‐محور در برابر مراقبت پزشک‐محور در برونشکتازی
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Country: United Kingdom Design: randomised controlled trial, single centre, cross‐over study. No washout phase Study objective: to assess feasibility and safety of nurse‐led outpatient clinic and to compare cost‐effectiveness of nurse‐led vs doctor‐led care Methods of analysis: paired student's t tests, means, confidence intervals Exacerbation and admission: Poisson distribution and modes of care comparison using likelihood ratios Patient satisfaction: Wilcoxon signed rank test, McNemar test Cost analysis: paired non‐parametric bootstrap analysis Clustering adjustments made: not relevant | |
| Participants | Eligible for study: 80 Randomised: 39 nurse‐led care, 41 doctor‐led care Completed: 37 nurse‐led care, 40 doctor‐led care Age, years: nurse/doctor 63.7, doctor/nurse 53.1; mean age 58.3 ± 13.3 years Gender: male/female 25/55 Bronchiectasis diagnosis: confirmed by high‐resolution computed tomography Recruitment: outpatient clinic attendance with established management plan Comorbidities: no detail provided regarding comorbid conditions Exclusion criteria: life expectancy < 2 years, need for transplant listing within 2 years, FEV1 < 30% predicted, other significant pathology that would modify the management of bronchiectasis | |
| Interventions | Intervention description: nurse specialist‐led care Control description: doctor‐led care Duration of intervention: two 1‐year care blocks Setting: outpatient | |
| Outcomes | Prespecified outcomes: FEV1, FVC, exacerbation rates, hospital admissions, quality of life, cost‐effectiveness, exercise capacity, 12MWT, withdrawals and dropouts, nurse autonomy, participant and GP satisfaction; consultation: type, length, and venue; participant compliance Follow‐up period: 1 year, then cross‐over | |
| Notes | Funding: NHS R&D Health Technology Assessment Programme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation mentioned but methods not described |
| Allocation concealment (selection bias) | Low risk | Numbered opaque envelopes used |
| Blinding of participants and personnel (performance bias) | Unclear risk | Blinding did not occur; blindness was not possible, given it is part of the intervention. Impact of knowing group assignment is unclear. Carryover effects from first year of study may have occurred when crossed‐over. |
| Blinding of outcome assessment (detection bias) | High risk | Blinding did not occur. |
| Incomplete outcome data (attrition bias) | Low risk | High level of completion; attrition reported with reasons |
| Selective reporting (reporting bias) | High risk | Changes between time periods were tested; however effects were observed in the economic analysis during the second time period; post hoc analyses occurred for carryover of clinical outcomes but were not reported. Selection effect cannot be ruled out, given that 6 participants did not cross‐over to nurse‐led care. |
| Other bias | Low risk | No other biases identified |
12MWT: 12‐minute walk test; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; GP: general practitioner; NHS: National Health Service; R&D: Research and Development.
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Randomised controlled trial ‐ participants had a confirmed diagnosis of chronic obstructive pulmonary disease | |
| Randomised controlled trial ‐ participants with chronic obstructive airways disease were recruited | |
| Randomised controlled trial of specialist nurse education in asthma | |
| Randomised trial of nurse in complementary alternative medicine role utilising acupressure as treatment for participants with bronchiectasis |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Infective exacerbations (per patient per year) Show forest plot | 1 | Rate Ratio (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1 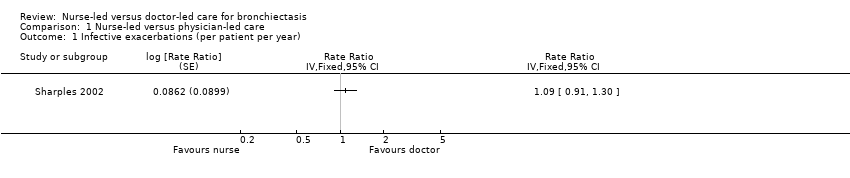 Comparison 1 Nurse‐led versus physician‐led care, Outcome 1 Infective exacerbations (per patient per year). | ||||
| 2 Admissions per patient per year Show forest plot | 1 | Rate Ratio (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Nurse‐led versus physician‐led care, Outcome 2 Admissions per patient per year. | ||||
| 3 SGRQ ‐ symptoms Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3 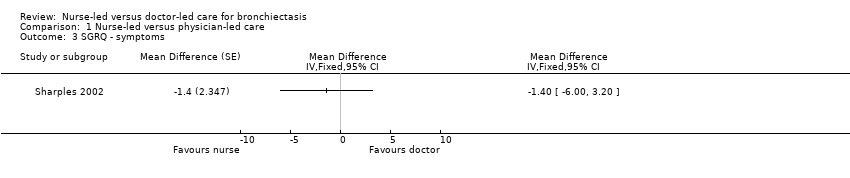 Comparison 1 Nurse‐led versus physician‐led care, Outcome 3 SGRQ ‐ symptoms. | ||||
| 4 SGRQ ‐ control Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4 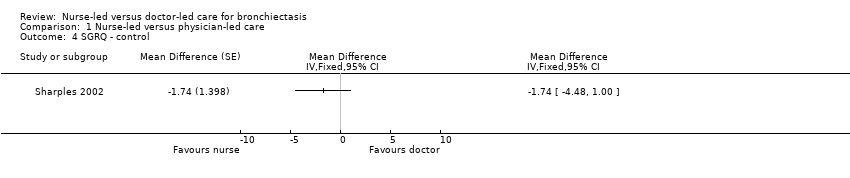 Comparison 1 Nurse‐led versus physician‐led care, Outcome 4 SGRQ ‐ control. | ||||
| 5 SGRQ ‐ impact Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 Nurse‐led versus physician‐led care, Outcome 5 SGRQ ‐ impact. | ||||
| 6 SGRQ ‐ total scores Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.6 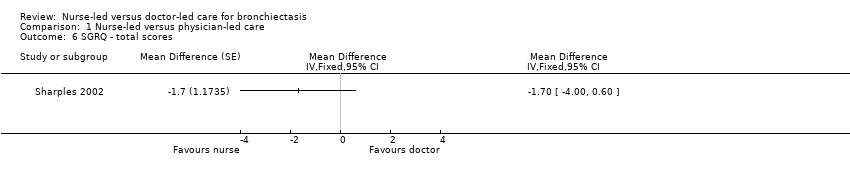 Comparison 1 Nurse‐led versus physician‐led care, Outcome 6 SGRQ ‐ total scores. | ||||
| 7 Exercise capacity: 12‐minute walk distance, metres Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.7  Comparison 1 Nurse‐led versus physician‐led care, Outcome 7 Exercise capacity: 12‐minute walk distance, metres. | ||||
| 8 FEV1 (% predicted) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.8  Comparison 1 Nurse‐led versus physician‐led care, Outcome 8 FEV1 (% predicted). | ||||
| 9 FVC (% predicted) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| Analysis 1.9 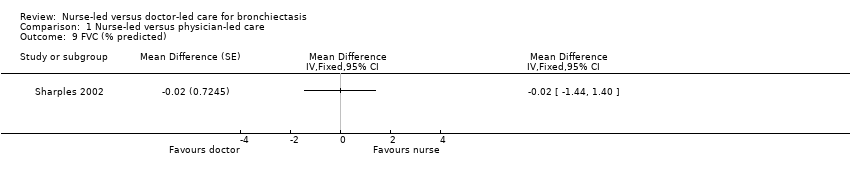 Comparison 1 Nurse‐led versus physician‐led care, Outcome 9 FVC (% predicted). | ||||
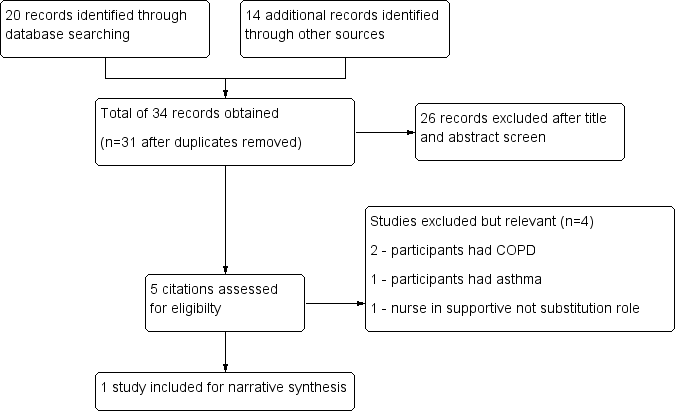
Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
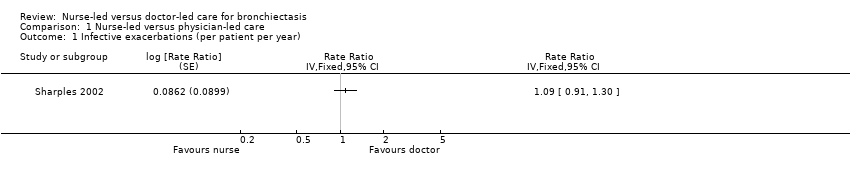
Comparison 1 Nurse‐led versus physician‐led care, Outcome 1 Infective exacerbations (per patient per year).

Comparison 1 Nurse‐led versus physician‐led care, Outcome 2 Admissions per patient per year.

Comparison 1 Nurse‐led versus physician‐led care, Outcome 3 SGRQ ‐ symptoms.
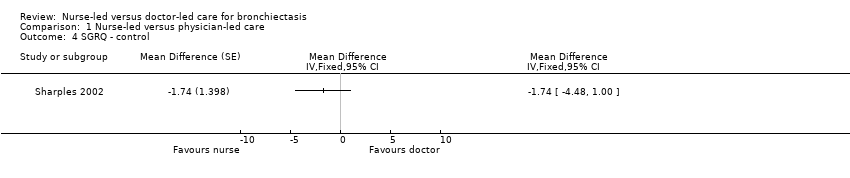
Comparison 1 Nurse‐led versus physician‐led care, Outcome 4 SGRQ ‐ control.

Comparison 1 Nurse‐led versus physician‐led care, Outcome 5 SGRQ ‐ impact.
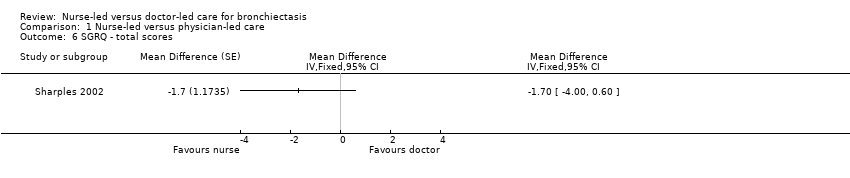
Comparison 1 Nurse‐led versus physician‐led care, Outcome 6 SGRQ ‐ total scores.
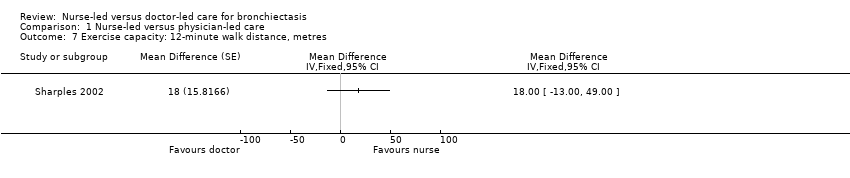
Comparison 1 Nurse‐led versus physician‐led care, Outcome 7 Exercise capacity: 12‐minute walk distance, metres.
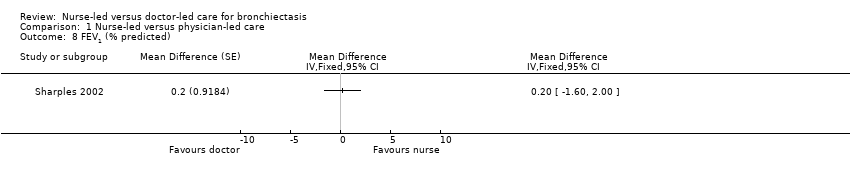
Comparison 1 Nurse‐led versus physician‐led care, Outcome 8 FEV1 (% predicted).
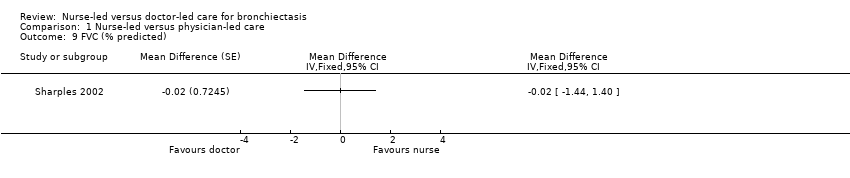
Comparison 1 Nurse‐led versus physician‐led care, Outcome 9 FVC (% predicted).
| Nurse‐led care compared with doctor‐led care for management of bronchiectasis | ||||||
| Patient or population: management of bronchiectasis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
| Risk with doctor‐led care | Risk with nurse‐led care | |||||
| Exacerbations Assessed by clinician identified or participant self‐reported Follow‐up: 12 months | Mean rate of infective exacerbations was 3.1 per patient per year. | 0.28 per patient per year higher | 1.09 (95% CI 0.91 to 1.30) | 80 | ⊕⊕⊝⊝ | |
| Hospital admissions (per patient per year). | Mean admission per patient per year was 1.02. | 1.55 per patient per year higher | 1.52 (95% CI 1.03 to 2.23) | 80 | ⊕⊕⊝⊝ | More admissions in nurse‐led care. All nurse‐led care admissions approved by consultant. Protocol followed by nurse regarding management |
| Emergency department attendance | See comment. | See comment. | See comment. | See comment. | See comment. | Not reported |
| Mortality | Two participants died ‐ 1 from each care group ‐ after 12‐month assessment. | See comment. | ⊕⊕⊝⊝ | |||
| Cost‐effectiveness Total cost for duration of study and difference in cost for first and second years Cost scale: £ per participant | Total costs £5428 Cost difference £274 higher in second year | Total costs £8464 Cost difference £1940 lower in second year | ⊕⊕⊝⊝ | Costs may be reduced over time through a learning effect. | ||
| Quality of life, measured with SGRQ ‐ total scores | Unreported | MD 1.7 higher | 79 | ⊕⊕⊝⊝ | Participants reported fewer symptoms and less impact on daily life with nurse‐led care, but data show no clinical or statistically significant differences between nurse‐led and doctor‐led care. | |
| Exercise capacity: 12MWT | Mean exercise capacity: 12MWT was 746 m. | MD 18 m greater | 80 | ⊕⊕⊝⊝ | No significant differences in distance walked between nurse‐led and doctor‐led care | |
| FEV1 | Mean FEV1 was 69.5% predicted. | MD 0.2% predicted higher | 80 | ⊕⊕⊝⊝ | Nil significant differences in percentage predicted FEV1 between nurse‐led and doctor‐led care | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aCannot rule out carryover effects from cross‐over trial. No reported information at first 12‐month time period before cross‐over. May have had a learned effect that resulted in fewer exacerbations and hospitalisations and better quality of life. This may have led to better lung function and exercise capacity. Marked down one point for risk of bias. bAge of study, small number of participants, and uncertainty, with some results based on wide confidence intervals. Marked down one point for imprecision. cCannot rule out selective reporting with the decision not to cross‐over 6 participants after first 12 months. No longer considered stable bronchiectasis. Already marked down for risk of bias previously, so not downgraded again based on this reason. | ||||||
| Resource | Nurse‐led care (mean visits per participant) | Nurse‐led care (mean cost per participant, £) | Doctor‐led care (mean visits per participant) | Doctor‐led care (mean cost per participant, £) | Difference (SD, £) |
| Nurse‐led clinics | 4.61 | 180 | 0 | 0 | 180 (158) |
| Doctor‐led clinics | 0.45 | 25 | 4.48 | 217 | ‐192 (199) |
| Procedures | 0.13 | 61 | 0.11 | 54 | 7 (376) |
| Imaging | 1.14 | 47 | 0.76 | 45 | 1 (112) |
| Other tests | 24.58 | 260 | 18.94 | 222 | 37 (257) |
| Antibiotics (intravenous) | 23 (days) | 879 | 16 (days) | 523 | 356 (1452) |
| Antibiotics (oral) | 222 (days) | 684 | 201 (days) | 524 | 161 (695) |
| Bronchodilators | 461 (days) | 213 | 435 (days) | 193 | 20 (179) |
| Corticosteroids | 238 (days) | 278 | 219 (days) | 258 | 20 (181) |
| Other drugs | 212 (days) | 180 | 190 (days) | 155 | 25 (194) |
| Inpatient | 6.46 (days) | 1338 | 2.36 (days) | 477 | 861 (2755) |
| Day case | 0.11 | 43 | 0.05 | 16 | 27 (170) |
| GP visits | 1.11 | 20 | 1.40 | 26 | ‐6 (33) |
| Total | 4208 | 2711 | 1498 (688 to 2674) | ||
| SD: standard deviation. | |||||
| Comments | Nurse practitioner better, number, (%) | Doctor better, number (%) | P value |
| It was sometimes difficult to discuss your problems with the doctor/nurse practitioner. | 11/76 (14.5) | 1/76 (1.3) | 0.006 |
| The doctor/nurse practitioner explained clearly what is wrong. | 7/74 (9.5) | 0/74 (0) | 0.016 |
| The doctor/nurse practitioner examined you thoroughly when necessary. | 6/70 (8.6) | 0/70 (0) | 0.031 |
| The doctor/nurse practitioner should tell you more about your illness/condition and treatment. | 7/59 (11.9) | 3/59 (5.1) | 0.344 |
| The doctor/nurse practitioner made you feel at ease. | 2/75 (2.7) | 1/75 (1.3) | 1.000 |
| There was not enough time to discuss your problems with the doctor/nurse. | 10/74 (13.5) | 1/74 (1.4) | 0.012 |
| You felt confident the doctor/nurse practitioner knew about your medical history and your care. | 7/74 (9.5) | 1/74 (1.4) | 0.070 |
| Sometimes you felt that the doctor/nurse practitioner should listen more to what you said. | 5/69 (7.2) | 2/69 (2.9) | 0.453 |
| The doctor/nurse practitioner gave clear explanation about any tests that you needed. | 4/75 (5.3) | 1/75 (1.3) | 0.375 |
| You often came away from your appointment wishing you'd asked more questions. | 13/72 (18.1) | 9/72 (12.5) | 0.523 |
| You felt you were given a chance to have an active part when discussing your illness/condition. | 4/73 (5.5) | 0/73 (0.0) | 0.125 |
| There were frequent interruptions during your consultation. | 6/73 (8.2) | 3/73 (4.1) | 0.508 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Infective exacerbations (per patient per year) Show forest plot | 1 | Rate Ratio (Fixed, 95% CI) | Totals not selected | |
| 2 Admissions per patient per year Show forest plot | 1 | Rate Ratio (Fixed, 95% CI) | Totals not selected | |
| 3 SGRQ ‐ symptoms Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 4 SGRQ ‐ control Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 5 SGRQ ‐ impact Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 6 SGRQ ‐ total scores Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 7 Exercise capacity: 12‐minute walk distance, metres Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 8 FEV1 (% predicted) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |
| 9 FVC (% predicted) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | Totals not selected | |

