Intervalos de visita para la salud oral en pacientes de atención primaria
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Trial design: parallel‐group RCT (2 arms) Number of centres: 1 | |
| Participants | Inclusion criteria: children and adolescents who received regular dental care in one public dental clinic in Norway; participants entering the trial were either 3, 16 or 18 years of age Exclusion criteria: children classified as 'at risk'. Criteria for classification of 'risk patients': Baseline caries (DMFS) (mean and SD): 3‐year olds (12‐month group: 0 ± 0; 24‐month group: 0 ± 0); 16‐year olds (12‐month group: 10.6 ± 7.7; 24‐month group: 11.4 ± 5.7); 18‐year olds (12‐month group: 11.9 ± 6.7; 24‐month group: 13.7 ± 6.8) Age at baseline: stratified into 3‐, 16‐, and 18‐year olds Gender: not reported Number randomised: 241; 3‐year olds (12‐month group: 35; 24‐month group: 35); 16‐year olds (12‐month group: 50; 24‐month group: 51); 18‐year olds (12‐month group: 35; 24‐month group: 35) Number evaluated: 185; 3‐year olds (12‐month group: 27; 24‐month group: 31); 16‐year olds (12‐month group: 43; 24‐month group: 35); 18‐year olds (12‐month group: 23; 24‐month group: 26) | |
| Interventions | Comparison: 12‐month recall versus 24‐month recall 1 dentist and 1 hygienist provided all dental care. The hygienist examined 3‐year old patients at the initial, intermediate and final visits. The dentist examined the 16 and 18‐year olds and provided operative treatment for all the children Duration of study: 24 months | |
| Outcomes | DMFS increment; total time (the sum of clinical examination time, operative treatment, acute visits (unscheduled extra visits initiated by the participant) and minutes wasted when the participant did not show up) | |
| Notes | Funding source: not reported Sample size calculation: not reported Adverse effects: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The participating children were randomly allocated to two groups" Comment: insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The participating children were randomly allocated to two groups" Comment: insufficient information |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Blinding of personnel was not mentioned |
| Blinding of outcome assessment (detection bias) | High risk | 1 dentist and 1 dental hygienist provided all dental care and examined the participants. Therefore blinding of outcome assessment was not carried out |
| Incomplete outcome data (attrition bias) | Low risk | 22% dropped out from the 12‐month group; 24% dropped out from the 24‐month group; all drop‐outs were due to leaving the area |
| Selective reporting (reporting bias) | Low risk | Outcomes stated in the methods section were reported in full |
| Other bias | Low risk | No other apparent biases |
DMFS = decayed, missing, filled surfaces; DMFT/dmft = decayed, missing, filled teeth; RCT = randomised controlled trial; SD = standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not a randomised controlled trial. In this study treatment and control groups were formed according to the age of participants | |
| Unable to contact authors to determine if this study was a randomised controlled trial (paper in German) |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | INTERVAL Dental Recalls Trial |
| Methods | Multicentre, 3‐arm, parallel‐group, randomised controlled trial |
| Participants | Adult patients (18 years of age or older) in the United Kingdom, who are dentate, have visited their dentist in the previous 2 years, and receive all or part of their dental care as an National Health Service patient |
| Interventions | 6‐month fixed‐period recall versus risk‐based recall versus 24‐month fixed‐period recall |
| Outcomes | Primary 1. Health‐related quality of life measured using an annual, self administered patient questionnaire. Questionnaire will include a global assessment of quality of life using short form Oral Health Impact Profile, a standardised measure of health outcome (EQ‐5D) and a specially developed, context‐specific, health‐related quality of life measure Secondary |
| Starting date | 01/09/2011 |
| Contact information | |
| Notes | Funding source: NIHR Health Technology Assessment Programme ‐ HTA (UK) Sample size: In total, 2288 participants will be recruited in order to retain 1735 at 4 years Anticipated end date: 28/02/2017 |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Caries (dmfs/DMFS increment) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Clinical examination at 12 months versus clinical examination at 24 months, Outcome 1 Caries (dmfs/DMFS increment). | ||||
| 1.1 3‐5 year olds (primary teeth) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 16‐20 year olds (permanent teeth) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Total time (minutes) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Clinical examination at 12 months versus clinical examination at 24 months, Outcome 2 Total time (minutes). | ||||
| 2.1 3‐5 year olds (primary teeth) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 16‐20 year olds (permanent teeth) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
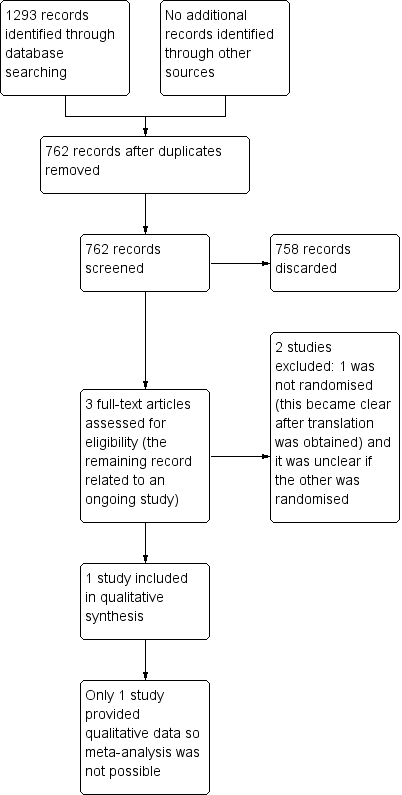
Study flow diagram.
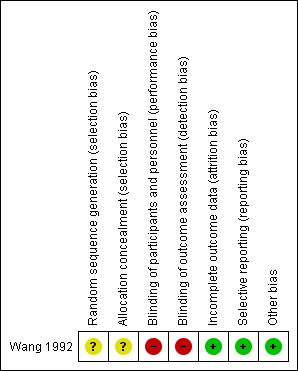
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
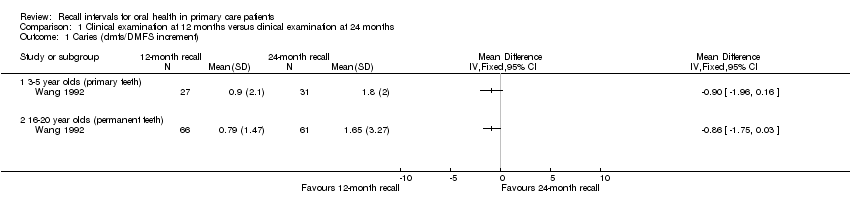
Comparison 1 Clinical examination at 12 months versus clinical examination at 24 months, Outcome 1 Caries (dmfs/DMFS increment).
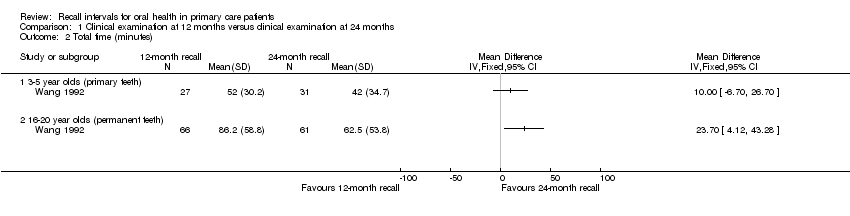
Comparison 1 Clinical examination at 12 months versus clinical examination at 24 months, Outcome 2 Total time (minutes).
| Clinical examination at 12 months compared with clinical examination at 24 months for oral health | ||||
| Patient or population: children and adults Settings: public dental clinic Intervention: clinical examination at 12 months Comparison: clinical examination at 24 months | ||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | |||
| 12‐month recall | 24‐month recall | |||
| Caries (dmfs/DMFS increment) ‐ 3‐5 year olds (primary teeth) Higher values represent worse caries Follow‐up: 2 years | The mean caries score in the 12‐month group was 0.9 | The mean caries score in the 24‐month group was 0.9 higher (1.96 higher to 0.16 lower) | 58 | ⊕⊝⊝⊝ |
| Caries (dmfs/DMFS increment) ‐ 16‐20 year olds (permanent teeth) Higher values represent worse caries Follow‐up: 2 years | The mean caries score in the 12‐month group was 0.79 | The mean caries score in the 24‐month group was 0.86 higher (1.75 higher to 0.03 lower) | 127 | ⊕⊝⊝⊝ |
| Total time (minutes) ‐ 3‐5 year olds (primary teeth) Higher values represent worse time/cost outcomes Follow‐up: 2 years | The mean total time used by each participant in the 12‐month group was 52 minutes | The mean total time used by each participant in the 24‐month group was 10 minutes lower (6.7 higher to 26.7 lower) | 58 | ⊕⊝⊝⊝ |
| Total time (minutes) ‐ 16‐20 year olds (permanent teeth) Higher values represent worse time/cost outcomes Follow‐up: 2 years | The mean total time used by each participant in the 12‐month group was 86.2 minutes | The mean total time used by each participant in the 24‐month group was 23.7 minutes lower (4.12 lower to 43.28 lower) | 127 | ⊕⊝⊝⊝ |
| CI: confidence interval; dmfs/DMFS: decayed, missing, filled surfaces | ||||
| GRADE Working Group grades of evidence | ||||
| 1 Single study at high risk of performance and detection bias with unclear methods of sequence generation and allocation concealment 2 Only low risk participants who had previously received regular dental care, including health promotion and preventive services were included 3 Low sample size | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Caries (dmfs/DMFS increment) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 3‐5 year olds (primary teeth) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 16‐20 year olds (permanent teeth) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Total time (minutes) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 3‐5 year olds (primary teeth) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 16‐20 year olds (permanent teeth) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

