Rehabilitación multidisciplinaria para la lesión cerebral adquirida en adultos en edad laboral
Resumen
Antecedentes
Las pruebas derivadas de revisiones sistemáticas demuestran que la rehabilitación multidisciplinaria es efectiva en los pacientes que han presentado un accidente cerebrovascular, una población constituida predominantemente por personas de edad avanzada. Sin embargo, no se ha establecido la base de pruebas sobre la efectividad de la rehabilitación después de la lesión cerebral adquirida (LCA) en adultos más jóvenes, quizás porque en estos casos existen diversos desafíos metodológicos para la investigación.
Objetivos
Evaluar los efectos de la rehabilitación multidisciplinaria después de la LCA en adultos entre 16 y 65 años de edad.
Métodos de búsqueda
Se realizó la búsqueda más reciente el 14 de septiembre de 2015. Se hicieron búsquedas en el registro especializado del Grupo Cochrane de Lesiones (Cochrane Injuries Group), The Cochrane Library, Ovid MEDLINE(R), Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid OLDMEDLINE(R), Embase Classic+Embase (OvidSP), Web of Science (ISI WOS) databases, registros de ensayos clínicos y se examinaron las listas de referencias.
Criterios de selección
Ensayos controlados aleatorios (ECA) que compararon la rehabilitación multidisciplinaria con los servicios locales disponibles habitualmente o con niveles inferiores de intervención; o ensayos que compararon una intervención en diferentes ámbitos, de diferentes intensidades o de diferente momento de inicio. Se incluyeron ensayos clínicos controlados, siempre que cumplieran los criterios metodológicos predefinidos.
Obtención y análisis de los datos
Tres autores de la revisión seleccionaron de forma independiente los ensayos y evaluaron su calidad metodológica. Un cuarto autor de la revisión hubiera arbitrado si no se hubiera alcanzado el consenso mediante discusión, pero en realidad, esto no ocurrió. Al igual que en las versiones anteriores de esta revisión, se utilizó el método descrito por Van Tulder 1997 para calificar la calidad de los ensayos y para realizar la síntesis de las "mejores pruebas", al atribuir los niveles de las pruebas sobre la base de la calidad metodológica. Las evaluaciones del riesgo de sesgo se realizaron en paralelo mediante la metodología estándar Cochrane. Sin embargo, el sistema Van Tulder proporcionó una evaluación más discriminatoria de los ensayos de rehabilitación, de manera que se ha mantuvo su uso para la síntesis primaria de las pruebas. Los ensayos se subdividieron con respecto a la gravedad de la lesión cerebral y el ámbito, el tipo y el momento de la rehabilitación ofrecida.
Resultados principales
Se identificó un total de 19 estudios con 3480 pacientes. Según el sistema de calificación Van Tulder, 12 estudios fueron de buena calidad metodológica y siete fueron de calidad inferior. Dentro del subgrupo de lesión cerebral predominantemente leve, "pruebas sólidas" indicaron que la mayoría de los individuos tuvo una buena recuperación cuando se proporcionó información apropiada, sin la necesidad de intervenciones específicas adicionales. Para la lesión moderada a grave, existen "pruebas sólidas" que muestran efectos beneficiosos de la intervención formal y "pruebas limitadas" que indican que el comienzo temprano de la rehabilitación después de la lesión da lugar a mejores resultados. Para los pacientes con LCA de moderada a grave y en rehabilitación, existen "pruebas sólidas" de que los programas más intensivos se asocian con logros funcionales más tempranos, y "pruebas moderadas" indicaron que el tratamiento ambulatorio continuo podría ayudar a mantener los logros obtenidos en la rehabilitación temprana posaguda. El contexto de rehabilitación multidisciplinaria parece influir en los resultados. "Pruebas sólidas" apoyan el uso de un modelo adaptado al medio en los pacientes con lesión cerebral grave, en el cual la rehabilitación cognitiva integral tiene lugar en un ambiente terapéutico e incluye a compañeros de los pacientes. Existen "pruebas limitadas" de que la rehabilitación hospitalaria especializada y la rehabilitación comunitaria multidisciplinaria especializada pueden dar lugar a logros funcionales adicionales; sin embargo, los estudios indican los obstáculos éticos y prácticos de la asignación al azar de pacientes con lesiones graves, para los cuales no se dispone de alternativas realistas a la intervención especializada.
Conclusiones de los autores
Después de una LCA se presentan diversos problemas. Por lo tanto, se requieren diferentes intervenciones y combinaciones de intervenciones para satisfacer las necesidades de los pacientes con diferentes problemas. Los pacientes que se presentan de manera aguda al hospital con una lesión cerebral leve se benefician del seguimiento y la información y el asesoramiento apropiados. Los pacientes con lesión cerebral moderada a grave se benefician del seguimiento habitual, por lo que sus necesidades de rehabilitación se pueden evaluar. La intervención intensiva parece dar lugar a logros más tempranos y la intervención inmediata, incluso aún en la atención de urgencia y de casos agudos, ha sido apoyada por pruebas limitadas. Aún debe determinarse el equilibrio entre la intensidad y la relación costo‐efectividad. Los pacientes a los que se les ha dado de alta de la rehabilitación hospitalaria se benefician con el acceso a servicios comunitarios o ambulatorios adecuados a sus necesidades. La rehabilitación grupal en un medio terapéutico (donde los pacientes reciben la rehabilitación neuropsicológica en un ambiente terapéutico con compañeros que enfrentan retos similares) representa un enfoque efectivo para los pacientes que requieren rehabilitación neuropsicológica después de una lesión cerebral grave. No todos los aspectos en la rehabilitación se pueden abordar mediante ensayos controlados aleatorios u otros enfoques experimentales. Por ejemplo, la bibliografía basada en ensayos no dice qué tratamientos funcionan mejor en qué pacientes a largo plazo ni qué modelos de servicio presentan un valor acorde en el contexto de la atención de toda la vida. En el futuro será necesario considerar dichas preguntas junto con las pruebas basadas en la práctica obtenidas de los estudios de cohortes longitudinales sistemáticos grandes realizados en el contexto de la práctica clínica habitual.
PICO
Resumen en términos sencillos
Rehabilitación para adultos en edad laboral que presentan una lesión cerebral
Antecedentes: Los estudios muestran que la rehabilitación multidisciplinaria tiene efectos beneficiosos en los pacientes con daño cerebral debido a un accidente cerebrovascular. Algunos programas multidisciplinarios están dirigidos a los adultos en edad laboral que presentan lesión cerebral posterior a traumatismo u otras causas. Estos pacientes tienden a ser más jóvenes que la mayoría de los pacientes con accidente cerebrovascular y pueden tener distintos objetivos de tratamiento, como el regreso al trabajo o el cuidado de los hijos. Los pacientes con lesiones cerebrales pueden presentar dificultades diversas que incluyen problemas con las funciones físicas, la comunicación, los procesos de pensamiento, el comportamiento o las emociones. La importancia de los problemas puede variar de leve a grave. La rehabilitación multidisciplinaria se dirige a una o más de estas áreas en lugar de centrarse en un único aspecto como la función física (motora).
Pregunta de la revisión: Los autores de esta revisión Cochrane buscaron los estudios de rehabilitación multidisciplinaria en adultos de 16 a 65 años de edad, con lesión cerebral adquirida (LCA) por cualquier causa.
Características de los estudios: Los estudios elegibles para inclusión en esta revisión fueron los ensayos controlados en los que un grupo de pacientes recibieron tratamiento (como rehabilitación multidisciplinaria) y se comparó con un grupo similar que recibió un tratamiento diferente. Se encontraron 19 estudios relevantes con un total de 3480 pacientes.
Fecha de la búsqueda: Se realizaron búsquedas en la literatura médica en todo el mundo el 14 de septiembre de 2015.
Métodos de la revisión: Se utilizó el sistema Van Tulder para calificar la fortaleza de las pruebas ya que distinguió mejor entre los ensayos de calidad diferente con respecto a criterios que son importantes en el contexto de la rehabilitación, en comparación con el sistema estándar GRADE.
Resultados clave: Para la lesión cerebral leve, la información y el asesoramiento fueron generalmente más apropiados que la rehabilitación intensiva. En general, los estudios indican que los pacientes con lesión cerebral moderada a grave que recibieron rehabilitación más intensiva mostraron una mejoría más temprana, y que la rehabilitación inmediata fue mejor que el tratamiento tardío. Pruebas sólidas apoyan la provisión de rehabilitación cognitiva en un "medio" terapéutico, o sea, un ambiente en el cual los pacientes reciben principalmente rehabilitación grupal junto a compañeros que se enfrentan con retos similares. La bibliografía basada en ensayos aporta pocas pruebas relacionadas con otros aspectos de la rehabilitación multidisciplinaria, de manera que los revisores recomiendan que se deben realizar estudios de investigación adicionales. La rehabilitación para la lesión cerebral es un proceso tan individualizado y a largo plazo que los estudios de investigación no facilitan necesariamente establecer conclusiones generales.
Calidad de la evidencia: En general, los estudios incluidos eran de buena calidad; 12 de 19 estudios se calificaron de alta calidad según el sistema de calificación Van Tulder. Los otros estudios tuvieron riesgo de sesgo debido a elementos del diseño, por ejemplo, en un estudio el tratamiento dependió de la disponibilidad de una cama en la unidad de rehabilitación. La disponibilidad de la cama es una manera irregular de asignar el tratamiento a los pacientes, y hace que los resultados del estudio sean propensos a sesgo.
Conclusiones de los autores
Antecedentes
Los servicios de rehabilitación de lesiones cerebrales se definen cada vez más por las necesidades de los pacientes, en lugar de por la patología de base (es decir, la enfermedad o el diagnóstico). Se han desarrollado servicios de rehabilitación multidisciplinaria especializada en el Reino Unido para atender las necesidades de los adultos más jóvenes y en edad laboral (16 a 65 años de edad). Esta separación de los servicios para "adultos de edad avanzada" no es sólo una cuestión de edad, sino que surge por los distintos objetivos de rehabilitación de los pacientes más jóvenes (como el regreso al trabajo o el cuidado de los hijos), que pueden ser menos importantes en pacientes de mayor edad, en su mayoría jubilados. Además, los adultos más jóvenes podrían mantener el aprendizaje y la adaptación durante un tiempo más largo. Debido a que es posible que ellos y la sociedad tengan que vivir con las consecuencias de la discapacidad por muchos años, la oportunidad de lograr una recuperación adicional de la independencia después de una rehabilitación más larga o más intensiva, o ambas, puede ser económicamente valiosa (Turner‐Stokes 2006; Turner‐Stokes 2007). Existen pruebas que indican que los individuos más jóvenes responden mejor en ambientes diferentes que los pacientes de edad avanzada (Gladman 1993; Kalra 1994). Las guías clínicas para el accidente cerebrovascular del Royal College of Physicians incluyen la siguiente recomendación: "Los adultos más jóvenes que han presentado un accidente cerebrovascular se deben atender en servicios médicos y de rehabilitación especializados que (1) reconozcan y traten las necesidades físicas, psicológicas y sociales particulares de los pacientes más jóvenes con accidente cerebrovascular (p.ej. rehabilitación profesional, actividades para el cuidado de los niños) y (2) se proporcionen en un ambiente conveniente a sus necesidades sociales específicas" (Royal College of Physicians 2008).
Se mencionan a continuación las principales causas de lesión cerebral adquirida (LCA) en este grupo de adultos más jóvenes.
-
Traumatismo craneoencefálico (TCE): la lesión resultante de traumatismo en la cabeza y sus consecuencias directas tales como hipoxia, hipotensión, hemorragia intracraneal y presión intracraneal elevada.
-
Lesión cerebral adquirida difusa: daño difuso que surge de un TCE o una variedad de otros incidentes agudos, entre ellos hipoxia (p.ej. debido a ahogamiento, electrocución, accidente anestésico), hipoglucemia y encefalitis viral.
-
Accidente cerebrovascular: puede ser isquémico o hemorrágico, pero incluye una proporción mayor de hemorragia subaracnoidea (de aneurismas o malformaciones arteriovenosas) que los accidentes cerebrovasculares en la población de edad avanzada.
-
Otras causas como cirugías neuroquirúrgicas (p.ej. extracción de un meningioma), radioterapia, absceso cerebral, meningitis bacteriana y heridas de arma de fuego.
Por lo tanto, es pertinente considerar las pruebas sobre la efectividad de la rehabilitación de forma separada para el grupo más joven de adultos en edad laboral y utilizar una definición amplia de "lesión cerebral adquirida (LCA)" que abarque todas las afecciones anteriores y represente al grupo de pacientes que habitualmente acude a la rehabilitación después de una lesión neurológica única. Este enfoque concuerda con el National Service Framework (NSF) for Long‐term Conditions del Reino Unido, que se basa en las características comunes de las enfermedades neurológicas categorizadas por su patrón de progresión (lesión única aguda, variación impredecible, progresión inevitable), en lugar de por diagnósticos patológicos específicos. La presente revisión contribuyó a la base de pruebas para corroborar las National Clinical Guidelines for Rehabilitation following Acquired Brain Injury (RCP/BSRM 2003) del Reino Unido y el NSF for Long‐term Conditions del Reino Unido (Department of Health 2005), que también destacan las necesidades particulares del adulto en edad laboral.
Los pacientes con LCA experimentan una variedad amplia de déficits, según la naturaleza y la ubicación de la lesión. Se pueden presentar a la rehabilitación con diversas combinaciones de problemas físicos, comunicativos, cognitivos, conductuales, psicosociales y ambientales. En concordancia con el vocabulario utilizado en la World Health Organization's International Classification of Functioning (WHO ICF) expandida (Wade 2000; Wade 2003; Wade 2004), demuestran heterogeneidad en cada nivel, ya que:
-
presentan diversas enfermedades;
-
experimentan una gran variedad de deficiencias, y cada paciente tiene una combinación única en cuanto a la gravedad y la naturaleza de la deficiencia;
-
también experimentan varias limitaciones, o restricciones, en las actividades (discapacidades) y la participación (previamente conocida como "incapacidad"); y
-
acuden a la rehabilitación desde una variedad de contextos diferentes: personal, social y físico.
Esto significa que cada individuo tiene un conjunto único de necesidades. Diferentes individuos necesitan diferentes programas de rehabilitación; además, el mismo paciente necesitará diferentes programas de rehabilitación en diferentes estadios de la recuperación. Por ejemplo:
-
después de los estadios iniciales de recuperación de una lesión aguda, algunos pacientes necesitarán un período de rehabilitación intensiva en el hospital para regresar a la independencia funcional y para hacer la transición desde el hospital nuevamente a la comunidad; los resultados de estos programas para casos agudos o subagudos tienden a centrarse en la reducción de la deficiencia y la discapacidad; y
-
una vez de vuelta en la comunidad, la atención se dirige más hacia la integración social, con retorno al trabajo y a la independencia económica si fuera posible; los programas de rehabilitación comunitaria que apoyan estas actividades se centran correctamente en medidas de resultado que reflejan la mejor participación y el ajuste psicosocial.
La variación amplia en los servicios es evidente entre y dentro de los países.
La heterogeneidad de los pacientes, los servicios de rehabilitación y los resultados plantean un desafío a la intervención tradicional o a los métodos basados en los ensayos controlados aleatorios (DeJong 2005; Horn 2005; Whyte 2002), así como a la asimilación de los resultados mediante el metanálisis. Estos problemas no son únicos de la rehabilitación sino que se enfrentan de igual manera en muchas especialidades médicas (Shiel 2008) y han sido reconocidos por el Medical Research Council (MRC) en su enfoque para la evaluación de intervenciones complejas (Craig 2008).
La revisión actual sirve para:
-
identificar las pruebas existentes basadas en ensayos para la rehabilitación multidisciplinaria en la LCA en adultos en edad laboral;
-
tratar explícitamente las cuestiones para la expansión futura de la base de pruebas con métodos de investigación tradicionales; e
-
identificar brechas en el conocimiento y sugerir métodos apropiados mediante los cuales se podrían explorarse en el futuro.
El método descrito a continuación tiene en cuenta el asesoramiento ofrecido por Greener y Langhorne (Greener 2002) con respecto a la aplicación de las revisiones sistemáticas en el campo de la rehabilitación.
Objetivos
Evaluar los efectos de la rehabilitación multidisciplinaria después de la LCA en adultos entre 16 y 65 años de edad.
Las preguntas específicas que se abordarán en esta revisión incluyen las siguientes:
-
¿La rehabilitación multidisciplinaria organizada logra mejores resultados que la ausencia de dichos servicios para este grupo de pacientes?
-
¿Una mayor intensidad (tiempo, pericia, o ambos) o el inicio más temprano de la rehabilitación da lugar a logros mayores?
-
¿Qué tipo de programas son efectivos y en qué ámbito?
-
¿Qué resultados específicos se ven influenciados (dependencia, integración social, estado de ánimo, retorno al trabajo, etc.)?
-
¿Con la rehabilitación multidisciplinaria se asocian costos‐beneficios demostrables?
Métodos
Criterios de inclusión de estudios para esta revisión
Tipos de estudios
Se incluyeron todos los ensayos controlados aleatorios (ECA) y los ensayos clínicos controlados (ECC) que compararon la rehabilitación multidisciplinaria versus los servicios locales disponibles habitualmente o versus niveles inferiores de intervención; y los ensayos que compararon una intervención proporcionada en diferentes ámbitos o a diferentes niveles de intensidad. Los ensayos controlados fueron elegibles para inclusión siempre que incluyeran un gran elemento de probabilidad en la disponibilidad de un lugar dentro de un servicio determinado versus la posibilidad de derivación a otro sitio.
Tipos de participantes
Se incluyeron los ensayos en los que la población estudiada estaba predominantemente en edad laboral (es decir, media de edad entre 16 y 65 años) y los sujetos presentaban una lesión cerebral adquirida (LCA) por cualquier causa (como traumatismo craneoencefálico [TCE], lesión cerebral difusa, accidente cerebrovascular, hemorragia subaracnoidea, hemorragia intracraneana, o poblaciones mixtas con LCA). También se planificó clasificar como elegibles para inclusión los ensayos que incluyeron todas las edades pero presentaron un subanálisis separado de la población de 16 a 65 años de edad, por lo que los resultados de los adultos dentro de este grupo etario fueran identificables por separado. Todavía no se han identificado ensayos en esta categoría.
Los programas de rehabilitación diseñados principalmente para satisfacer las necesidades de los pacientes de edad avanzada pueden incluir una minoría de pacientes más jóvenes porque se carece de los servicios más apropiados para ellos, pero en la práctica estos programas a menudo no logran hacer frente a los objetivos de rehabilitación más amplios de los individuos más jóvenes (Kersten 2002; Roding 2003). Por este motivo, no se estableció contacto con los autores de los estudios para obtener información sobre los adultos más jóvenes dentro de grupos de estudio con pacientes predominantemente de edad avanzada, a menos que hubiera pruebas claras de que se habían identificado y tratado como un grupo aparte. Nuevamente, no se ha identificado este tipo de ensayos.
La clasificación de los pacientes con LCA es compleja porque, como se señaló anteriormente, los individuos pueden tener una o más de una amplia variedad de deficiencias, cada una de diferente gravedad. Sin embargo, la naturaleza y la gravedad de los déficits neurológicos tienden a determinar el tipo de programa de rehabilitación ofrecido, así como los objetivos del tratamiento y las medidas de resultado utilizadas. Por ejemplo, a modo de generalización amplia, los pacientes con LCA leve tienden a presentar principalmente pérdidas cognitivas, y los objetivos para su rehabilitación tienden a centrarse en mejorar la participación, mientras que es más probable que los pacientes en la categoría grave a moderada tengan objetivos centrados en la mejoría a nivel de deficiencia y actividad (discapacidad). Los estudios no se incluyeron ni excluyeron sobre la base de la gravedad, pero se subagruparon sobre esta base para los objetivos del análisis y la discusión.
Tipos de intervenciones
La rehabilitación se define ampliamente como "proceso educativo de solución de problemas dirigido a reducir la discapacidad y la incapacidad que experimenta una persona como resultado de enfermedades o lesiones (Wade 1992). Para esta revisión, la rehabilitación multidisciplinaria se ha definido como cualquier intervención proporcionada por dos o más disciplinas que trabajan en un esfuerzo coordinado para alcanzar estos objetivos.
No se ha alcanzado acuerdo con respecto a la clasificación de las intervenciones y los programas de rehabilitación. Nuevamente, y en términos generales, los programas se pueden describir en cuanto al ámbito y el contenido.
Los ámbitos de rehabilitación incluyen:
-
ámbitos hospitalarios, en los que la rehabilitación se realiza en un contexto de 24 horas de atención y se puede desarrollar en una sala hospitalaria o en una unidad de rehabilitación especializada en casos agudos o subagudos;
-
ámbitos ambulatorios o de tratamiento de día, nuevamente se puede realizar en un ambiente hospitalario o en un ámbito comunitario local (p.ej. centro social de atención); y
-
ámbitos domiciliarios o domésticos, centrados en el propio domicilio del paciente y la comunidad local.
Los términos actuales encontrados en la literatura con respecto al contenido del programa incluyen:
-
rehabilitación física;
-
terapia cognitiva y conductual;
-
terapia profesional y recreativa; y
-
apoyo psicológico y psicosocial.
Sin embargo, es probable que el contenido real de dos programas cualesquiera dentro de la misma categoría haya variado enormemente y también que programas similares hayan recibido diferentes términos.
En consecuencia, se incluyó cualquier estudio que declaró o indicó la inclusión de un programa de rehabilitación multidisciplinaria o interdisciplinaria o que utilizó cualquiera de los términos anteriores, siempre que comparara la intervención mencionada con alguna forma de control.
Por las mismas razones, es igualmente difícil describir el control. Para esta revisión, se consideró lo siguiente:
-
Un nivel inferior o un tipo diferente de intervención como servicios locales disponibles habitualmente o intervención mínima, como solamente información o tratamiento de una sola sesión.
-
Control con lista de espera.
-
Intervenciones proporcionadas en diferentes ámbitos (como rehabilitación hospitalaria versus comunitaria).
-
Programa de tratamiento de intensidad inferior.
Se excluyeron los estudios que evaluaron los efectos de los siguientes:
-
Tratamiento de una disciplina sola (p.ej. fisioterapia), incluidos estudios de intensidad del tratamiento dentro de esa sola disciplina.
-
Dos formas diferentes de tratamiento, sin definir claramente la intervención ni el control.
-
Una intervención o modalidad unidisciplinaria sola (p.ej. ejercicio físico).
-
Programas para despertar del coma (porque ya se trataron en una revisión Cochrane [Lombardi 2002]), excepto cuando estos programas se proporcionaron como parte de un enfoque multidisciplinario coordinado.
Tipos de medida de resultado
El interés se centró en los resultados que reflejan la carga de la enfermedad invalidante sobre los pacientes y sus familias, y en los servicios que se les prestan. Se excluyeron los estudios que informaron solamente los resultados en cuanto a la deficiencia.
La medición de los resultados después de la rehabilitación se puede describir en dos ejes principales.
-
Tiempo de la medición ‐ desde el inicio de la enfermedad o desde el inicio de la rehabilitación.
-
Nivel de la medición dentro de WHO ICF.
Muchos de estos estudios se realizaron cuando la WHO classification of Impairment, Disability and Handicap previa estaba activa; por lo tanto, estos términos se han incluido entre paréntesis al lado de los términos actuales.
Para los propósitos de esta revisión:
-
"corto plazo" se refiere al tiempo desde la evaluación en el ingreso hasta el alta del programa de rehabilitación (independientemente de su duración) y hasta seis meses después; y
-
"largo plazo", a cualquier momento después de pasados seis meses del final de la intervención, generalmente un año o más.
Una vez más, no se ha alcanzado acuerdo sobre la clasificación de las medidas de resultado para la investigación en la rehabilitación después de la LCA, pero para esta revisión los resultados se han categorizado en general del siguiente modo.
-
Medidas de resultado centradas en los objetivos al nivel de la deficiencia y la actividad (discapacidad), por ejemplo:
-
síntomas residuales (amnesia postraumática [APT], síntomas poscontusión);
-
independencia funcional incluida la movilidad, el funcionamiento cognitivo y la capacidad para realizar las actividades cotidianas (AC) básicas (p.ej. Barthel Index, Functional Independence Measure [FIM] or Functional Assessment Measure [FIM+FAM], Glasgow Outcome Scale [GOS]); y
-
carga y estrés para el cuidador (p.ej. Caregiver Strain Index, Caregiver Burden Scale).
-
-
Medidas de resultado centradas en los objetivos a nivel de la participación (previamente conocida como "incapacidad") y el contexto personal (ajuste psicosocial, calidad de vida) (Langhorne 1995), por ejemplo:
-
destino del alta (p.ej. el hogar/ una institución);
-
retorno al trabajo;
-
integración o actividades sociales (p.ej. Rivermead Head Injury Follow‐Up Questionnaire [RHFUQ]);
-
actividades cotidianas ampliadas (ACA) (p.ej. Community Integration Questionnaire [CIQ]);
-
calidad de vida relacionada con la salud del paciente y el cuidador (p.ej. General Health Questionnaire [GHQ], Short‐Form‐36 [SF‐36]); y
-
estado de ánimo del paciente y el cuidador (p.ej. Hospital Anxiety and Depression Scale [HADS]) y satisfacción con los servicios.
-
Cuando se proporcionaron, también se incluyeron los resultados que reflejaron el uso de los recursos. Estos resultados incluyeron la duración de la estancia hospitalaria o el tratamiento, el reingreso posterior al hospital, la necesidad de atención, que incluyó el nivel de atención y el grado de apoyo necesario después del alta.
Tiempo
Resultados
Results
Description of studies
From the 30 articles selected at stage 2, we identified 20 that met the eligibility criteria for consideration (Figure 1).
In the previous update of this review in 2008, 16 trials met the criteria for consideration, as described in a total of 24 articles.
-
Two trials were excluded because of fatal flaws ‐ Relander 1972 on the basis of > 40% attrition, and Bjorkdahl 2007 for the reasons given below.
-
Six articles were supplementary papers providing additional details of programme content (Braverman 1999 and Warden 2000 for Salazar 2000), subgroup or specific analyses (King 1997 and Wenden 1998 for Wade 1997; Kwakkel 2002 for Kwakkel 1999) or follow‐up data (Paniak 2000 for Paniak 1998).
-
Two trials (Wade 1997; Wade 1998) reported data from the same programme but in different (sequential) cohorts of participants, so we treated these two papers as separate trials.
-
The paper by Zhu 2007 presented findings from the completed study from which Zhu 2001 had presented preliminary findings (which were included in the original review).
-
The trial by Björkdahl and colleagues was presented in two papers: Björkdahl 2006 reported main trial findings, and Bjorkdahl 2007 presented a subgroup analysis of carer burden. However, we excluded the latter analysis on the basis of fatal flaws (small numbers with high chance of type II error and poorly matched groups at baseline).
The latest updated search (2008 to 2015) yielded the six trials that met the eligibility criteria for consideration. We excluded two on the basis of fatal flaws.
-
Browne 2013 ‐ excluded on account of overall low quality (unclear matching of groups due to lack of functional outcome measures performed at baseline) and a considerable attrition rate of 30%.
-
Ownsworth 2008 ‐ excluded on the basis of very small participant numbers and high chance of type II error; also, no evidence of outcome comparisons between intervention and control groups.
We discussed at length but eventually excluded a third trial (Vanderploeg 2008). Although this high‐quality trial compared two approaches to rehabilitation, investigators did not identify a clearly hypothesised intervention and control, and so the study did not fit our pre‐defined criteria. Instead we have referred to it in the Discussion section.
Therefore, we selected three new trials for inclusion in this review update (Cicerone 2008; Andelic 2012; Bai 2012), yielding a total of 19 trials, including:
-
10 single‐blinded RCTs (Bai 2012; Björkdahl 2006; Cicerone 2008; Kwakkel 1999; Paniak 1998; Powell 2002; Slade 2002; Wade 1997; Wade 1998; Zhu 2007);
-
four unblinded RCTs (Elgmark 2007; Salazar 2000; Shiel 2001; Smith 1981);
-
five controlled clinical trials (CCTs) (Andelic 2012; Bowen 2001; Ozdemir 2001; Semlyen 1998; Werner 1996). (Andelic 2012 included a supplementary article (Andelic 2014) that described a cost‐effectiveness analysis.)
Types of brain injuries
Twelve of the 19 trials studied patients with traumatic brain injury (TBI), five studied stroke patients and one (Slade 2002) studied a mixed population with acquired brain injury (ABI).
Participants
The trials covered a range of severities of ABI. Three studies (Cicerone 2008; Wade 1997; Wade 1998) recruited people with brain injury of all severities, two (Elgmark 2007; Paniak 1998) recruited only people with mild TBI and the remainder recruited people with moderate to severe ABI. Between them, trials recruited 2729 patients and 132 carers.
Interventions
The interventions studied also varied. However, trials could be divided broadly into the following categories.
-
Five trials (Elgmark 2007; Paniak 1998; Salazar 2000; Wade 1997; Wade 1998) enrolled all patients presenting acutely to hospital with TBI and included populations predominantly in the milder ambulatory category. The intervention was targeted primarily at increasing participation (social integration, return to work, etc.) and reducing post‐concussional symptoms.
-
Two trials (Andelic 2012; Bai 2012) enrolled patients with moderate to severe TBI during acute stages of recovery. In these trials, participants received some form of very early rehabilitation alongside their acute medical management. As a result of the severity of their injuries, rehabilitation emphasised reducing disability.
-
Twelve trials (Björkdahl 2006; Bowen 2001; Cicerone 2008; Kwakkel 1999; Ozdemir 2001; Powell 2002; Semlyen 1998; Shiel 2001; Slade 2002; Smith 1981; Werner 1996; Zhu 2007) enrolled patients (following TBI or stroke) who were already presenting to rehabilitation services. This group, therefore, had greater levels of motor impairment and dependence on personal activities of daily living (ADLs), and interventions were targeted at improving function in ADLs (reduced disability), although measures of participation (reduced handicap) sometimes were also included.
Within this third group, trials covered a range of different interventions in different settings.
-
Two trials assessed the impact of out‐patient rehabilitation programmes, with one testing programmes of different intensity (Smith 1981), and the other testing therapy offered late after treatment (Werner 1996).
-
Three trials assessed the benefits of a co‐ordinated community‐based multi‐disciplinary team approach for patients (Powell 2002) and carers (Bowen 2001). Björkdahl 2006 compared a short programme of home‐based rehabilitation versus out‐patient (day clinic) rehabilitation following a period of in‐patient stroke rehabilitation.
-
Two trials assessed the benefits of a specialist in‐patient rehabilitation programme as opposed to local services (Semlyen 1998) or home‐based advice (Ozdemir 2001).
-
Four trials compared programmes of higher intensity versus treatment of lower (standard) intensity: two with a view towards assessing impact on length of stay (Shiel 2001; Slade 2002), and two (Kwakkel 1999; Zhu 2007) with focus on improving functional outcomes.
-
Two trials (Cicerone 2008 and also a subgroup analysis within Salazar 2000) assessed the benefits of holistic neuropsychological rehabilitation programmes delivered in a ‘therapeutic milieu’ model for patients requiring cognitive rehabilitation following moderate to severe brain injury. Salazar 2000 compared this approach versus a limited home‐based rehabilitation programme, and Cicerone 2008 compared it against a standard neurorehabilitation programme.
Outcomes
Within these groups, studies used different outcomes measured at different intervals over follow‐up periods of various lengths. As anticipated, we found insufficient concordance between outcome measures, time points and types of interventions to allow pooling of data for meta‐analysis.
Adverse effects
Rehabilitation can certainly have 'adverse effects', but in clinical practice this has often been considered unlikely; the absence of adverse effects, therefore, is hardly ever specifically recorded. Because adverse effects can and do occur, they should be recorded. We looked for information on adverse effects, but none of the included studies explicitly reported on them.
Risk of bias in included studies
According to the van Tulder scoring system of methodological quality, the maximum achievable score is 19. Results of scoring are shown in Table 3. Re‐scoring of all studies has led to minor changes in the order of quality.
| Study ID | Internal validity | Descriptive criteria | Statistical criteria | Total score | Positive criteria |
| Kwakkel 1999 | 8 | 5 | 2 | 15 | a,bi,bii,c,d,f,g,j,l,mi,mii,n,o,p,q. |
| Wade 1997 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,f,g,i,j,l,mi,n,o,q. |
| Wade 1998 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,f,g,i,j,l,mi,n,o,q. |
| Powell 2002 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,f,g,i,j,l,mii,n,o,q. |
| Cicerone 2008 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,g,i,j,l,mi,n,o,p,q |
| Smith 1982 | 7 | 5 | 2 | 14 | a,bi,c,d,f,g,i,j,l,mi,mii,n,o. |
| Salazar 2000 | 7 | 5 | 2 | 14 | a,bi,c,d,f,g,j,l,mi,mii,n,o,p,q. |
| Paniak 1998 | 6 | 5 | 2 | 13 | a,c,d,f,g,j,l,mi,mii,n,o,p,q. |
| Slade 2002 | 7 | 3 | 2 | 12 | a,bi,bii,c,d,f,g,j,l,mi,o,p,q |
| Shiel 2001 | 7 | 3 | 2 | 12 | a,bi,d,g,h,i,j,l,mi,o,q. |
| Zhu 2007 | 6 | 4 | 2 | 12 | a.bi,bii,c,d,i,j,l,mi,mii,n,o,p,q |
| Elgmark 2007 | 6 | 4 | 2 | 12 | a,bi,bii,c,d,i,j,l,mii,n,o,p,q |
| Bowen 2001 | 4 | 4 | 2 | 10 | a,c,d,f,j,l,mi,n,o,p,q. |
| Bjorkdahl 2006 | 5 | 3 | 2 | 10 | d,i,j,l,mi,mii,n,o,p,q |
| Bai 2012 | 5 | 3 | 1 | 9 | a,c,g,i,j,l,mi,n,o |
| Werner 1996 | 4 | 4 | 1 | 9 | a,bi,d,i,j,mi,mii,n,o. |
| Semlyen 1998 | 4 | 4 | 1 | 9 | a,d,f,g,j,l,mi,mii,n,o. |
| Andelic 2012 | 4 | 4 | 1 | 9 | a,c,d,g,j,l,mii,n,o |
| Ozdemir 2001 | 3 | 4 | 2 | 9 | a,c,d,f,g,j,mi,o,q. |
We identified 12 RCTs of high methodological quality according to the criteria given above. Wade 1997 noted that only 478 of 1156 originally randomly assigned participants (41%) could be traced to attend an interview. However, this is not unexpected in the often‐itinerant group of people who suffer head injuries. The trial was in part a feasibility study, and the inability to trace a larger proportion of these patients is a clinical reality and is itself an important finding of this particular trial. A detailed analysis of baseline characteristics was offered and demonstrated no significant differences between interviewed and non‐interviewed groups. Therefore, we rated this study as having high quality. Two RCTs (Bai 2012; Björkdahl 2006) were of lower quality, as they were lacking in some aspects of methodological detail. Björkdahl 2006 was also small and was probably underpowered for comparisons of the two groups.
We identified three controlled studies which had low methodological quality (Bowen 2001; Ozdemir 2001; Werner 1996).
-
Werner 1996 started off as a randomised trial, with a weighted 2:1 chance that participants would be allocated to active intervention (by picking a number of 666 or less from a sample of 1 to 1000); but after nine of the 16 original controls dropped out, trialists added five additional non‐randomised control participants. In addition, the trial report did not include measures of variability or point estimates.
-
Bowen 2001 and Ozdemir 2001 reported unblinded trials with only short‐term follow‐up.
The two remaining low‐scoring trials had a haphazard allocation procedure.
-
Andelic 2012 involved patients with severe traumatic brain injury. Treatment allocation was dependent on availability of beds on the rehabilitation unit.
-
Semlyen 1998 was a controlled study in which patients were admitted to a specialist multi‐disciplinary (MD) rehabilitation programme or were passed back to their standard local services (LS), depending on geography and the availability of a vacancy in the specialist programme. Although an element of chance was present in this allocation, patients with the most severe brain injuries, whose needs could not be met by their local services, in fact had no alternative option and remained on the acute ward for longer periods until a specialist bed became available. Therefore, the multi‐disciplinary rehabilitation group was significantly more disabled to start with, and participants were in hospital longer than the group referred to local services. This paper illustrates some of the important practical and methodological issues considered in the Discussion.
We also assessed included studies for methodological quality against the Cochrane risk of bias tool (Higgins 2011), and our summary of judgements can be seen in Figure 2 and Figure 3. As expected, there was a broad relationship between risk of bias and trial quality as rated by the van Tulder 2003 method, but not a close one. This is because van Tulder 2003 system includes a wider range of quality criteria, including reporting, duration of follow‐up and co‐interventions, which are important in the context of rehabilitation.
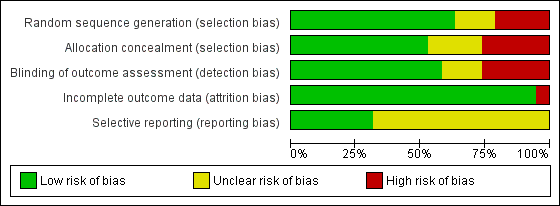
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. Nineteen studies are included in this review.
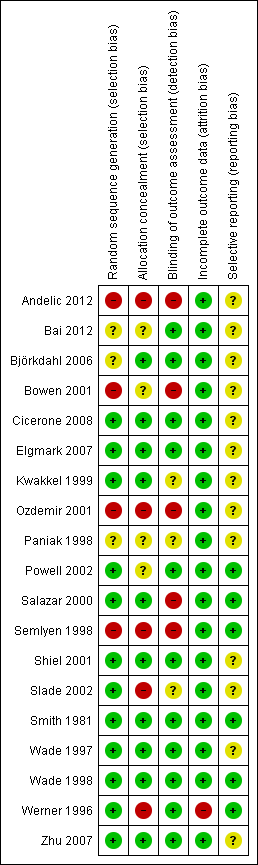
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
Milder ambulatory patients
Five trials predominantly addressed the milder ambulatory group (see Table 4).
| Paniak 1998 and 2000 | Participant and group comparisons | Patients with TBI admitted to hospital (all severities); mean age 33 y Intervention: ‘treatment as needed’ (TAN) (n = 58) Control: single session (SS) of education and advice (n = 53) | |||
| Primary outcomes | Impairment: Problem Checklist (PCL) Participation: Community Integration Questionnaire (CIQ) Health status: Short‐Form 36 (SF‐36) Work status: socio‐economic status (SES) | ||||
| Assessment points | 3 to 4 months (n = 111) and 1 year (n = 105) | ||||
| Summary of results | Participation (CIQ) did not change significantly for either group Impairment (PCL) and health status (SF‐36): Repeated measures MANOVA showed significant effects for time in both groups, which were maintained at 1 year Results showed no significant group interaction or time by group for any of the primary outcomes at either time point | ||||
| Vocational status (SES) | Intervention Mean (SD) | Control Mean (SD) | Difference in mean | P value (MANOVA) | |
| Pre‐injury | 37.2 (18.7) | 34.3 (18.5) | 2.9 | N/S | |
| Baseline | 26.9 (20.7) | 23.2 (19.9) | 0.8 | N/S | |
| 3 to 4 mo | 32.5 (20.2) | 32.8 (19.7) | 0.3 | N/S | |
| 1 y | 34.8 (19.7) | 36.7 (21.0) | 1.9 | N/S | |
| Authors' conclusions |
Interventions appear to be equally effective | ||||
| Salazar 2000 | Participant and group comparisons | Active duty military personnel with moderate to severe TBI; mean age 25 y Intervention: 8‐week intensive in‐patient cognitive‐behavioural programme (n = 67) Control: limited home programme of weekly telephone support from psychiatric nurse (educational material, counselling and suggested home exercises) (n = 53) | |||
| Primary outcomes | Work status: return to work return to fitness for military duty | ||||
| Assessment points | 1 year | ||||
| Summary of results | No overall differences in outcomes between groups Post hoc analysis demonstrated significant group interaction (in favour of the intervention group) for ‘fitness for military duty’ at 1 year for the more severe subgroup, who were unconscious for > 1 h | ||||
| Vocational status at 1 y | Intervention % achieved | Control % achieved | Difference | P value (Fisher's exact) | |
| Return to work | 90% | 94% | 4% (‐5.14) | N/S | |
| Fit for military duty | 73% | 66% | 7% (‐10.24) | N/S | |
| Post hoc analysis of subgroup unconscious for > 1 h (n = 75) | |||||
|
| (n = 35) | (n = 40) | Difference | P value | |
| Fit for military duty | 80% | 58% | 22% | 0.05 | |
| Authors' conclusions | Overall benefit of in‐patient cognitive rehabilitation programme similar to that of limited home rehabilitation, although institutional therapy may be beneficial for selected patients with severe TBI | ||||
| Wade 1997 | Participant and group comparisons | All patients presenting to Accident and Emergency following TBI; age 16 to 65 y Intervention: telephone follow‐up at 7 to 10 days with advice and referral as required (n = 252) Control: no specific intervention (standard services only) (n = 226) (NB: Despite major efforts to trace and contact patients, follow‐up interview at 6 months could be achieved in only 478 of 1156 (41%) participants randomly assigned) | |||
| Primary outcomes | Social disability: Rivermead Head Injury Follow‐Up Questionnaire (RFUQ) Symptoms: Rivermead Post‐concussion Symptoms Questionnaire (RPQ) | ||||
| Assessment points | 6 months | ||||
| Summary of results | No overall differences between intervention and control groups Post hoc analysis revealed significant group interaction (in favour of the active intervention group) with respect to social disability in a subgroup of individuals with more severe injury (>1 h PTA) | ||||
| Health status at 6 mo | Intervention Mean (SD) | Control Mean (SD) | P value (Mann‐Whitney) | ||
| RFUQ | 3.6 (6.0) | 3.3 (6.3) | N/S | ||
| RPQ | 7.7 (10.9) | 6.8 (10.0) | N/S | ||
| Post hoc analysis of subgroup with PTA > 1 h (n = 121) | |||||
| (n = 71) | (n = 53) | ||||
| RFUQ | 0.85 (0.89) | 1.17 (1.07) | 0.003 | ||
| RPQ | 2.03 (0.85) | 2.21 (0.89) | N/S | ||
| Authors' conclusions | Routine follow‐up does not appear to be necessary for all patients presenting with head injury, but a subgroup of patients with more severe TBI may benefit from such intervention | ||||
| Wade 1998 | Participant and group comparisons | All patients admitted to hospital following TBI (i.e. a more severe group than the total group reported in Wade 1997); age 16 to 65 y Intervention: telephone follow‐up at 7 to 10 days with advice and referral as required (n = 132) Control: no specific intervention (standard services only) (n = 86) (NB: follow‐up data obtained in 218 (69%) of 314 participants randomly assigned) | |||
| Primary outcomes | Social disability: Rivermead Head Injury Follow‐Up Questionnaire (RFUQ) Symptoms: Rivermead Post‐concussion Symptoms Questionnaire (RPQ) | ||||
| Assessment points | 6 months | ||||
| Summary of results | Significant group interaction (in favour of the active intervention group) with respect to social disability and post‐concussion symptoms. Subgroup analysis demonstrated that the main benefit appeared in the group with PTA < 7 days | ||||
| Health status at 6 mo | Intervention Mean (SD) | Control Mean (SD) | P value (Mann‐Whitney U test) | ||
| RFUQ | 5.36 (7.81) | 8.23 (8.75) | 0.01 | ||
| RPQ | 9.8 (11.7) | 13.9 (13.6) | 0.02 | ||
| Authors’ conclusions | Early intervention by a specialist service significantly reduced social morbidity and severity of post‐concussion symptoms 6 months after head injury, in the group of patients who required admission to hospital. Possibly most beneficial for the moderate to severe group, some of whom may not present without pro‐active intervention | ||||
| Elgmark 2007 | Participant and group comparisons | All patients aged 16 to 60 with mild traumatic brain injury according to American Congress of Rehabilitation medicine criteria Intervention: follow‐up at 2 to 8 weeks by telephone or letter with advice and referral as required (n = 264 ‐ 96 received intervention; 150 declined); 18 lost to follow‐up Control: no specific intervention (regular care) (n = 131); 22 lost to follow‐up 246 treatment and 109 control included in intention‐to‐treat analysis | |||
| Primary outcomes | Symptoms: change in post‐concussion symptoms ‐ Swedish Post‐concussion Symptoms Questionnaire (PCSQ) Social disability: Community Integration Questionnaire (CIQ), Life Satisfaction Questionnaire, Short‐Form Health Survey (SF‐36) | ||||
| Assessment points | 1 y post injury | ||||
| Summary of results | No statistically significant differences were found between intervention and control groups. Participants who experienced few PCS 2 to 8 weeks post injury declined rehabilitation and returned to work. Those who suffered several PCS and accepted rehabilitation did not recover after 1 y | ||||
| Health status at 6 mo | Intervention Mean (SD) | Control Mean (SD) | Significance
| ||
| Total PCSQ | 5.2 (5.3) | 4.4 (5.3) | N/S | ||
| CIQ | 20.3 (4.0) | 19.8 (4.0) | 0.02 | ||
| Authors’ conclusions | In this particular study of MTBI, active rehabilitation did not change outcomes to a significant degree. Additional studies should focus on patients who remain symptomatic during the first 1 to 3 months and should test various types of interventions | ||||
PTA = post‐traumatic amnesia; TBI = traumatic brain injury.
Four trials (Elgmark 2007; Paniak 1998; Wade 1997; Wade 1998) compared a programme of treatment as needed (which consisted largely of community‐based rehabilitation) versus a lesser intervention (Paniak: information only; Wade: standard follow‐up arrangements, which usually meant no further input). We rated all as high‐quality RCTs on the basis of all assessment criteria, and together they recruited a total of 1180 patients.
Salazar 2000 addressed a specific model of milieu‐based neuropsychological rehabilitation in comparison with weekly telephone counselling and advice given at home, recruiting 120 patients with mild TBI. A subgroup analysis also demonstrated benefits in the more severe group (unconscious > 1 hour) with respect to rate of return to military duty (80% vs 58%), as is discussed further below.
The general conclusion derived from all these studies was that intervention provided to a totally unselected group of patients with mild TBI was not effective. Both treatment and control intervention groups made substantial gains in terms of reduced post‐concussion symptoms and enhanced participation, including return to work. No significant differences between groups were recorded.
In the trial by Wade 1997, a post hoc subgroup analysis demonstrated that those admitted to hospital or with post‐traumatic amnesia (PTA) > 1 hour (n = 121) demonstrated significant gains with treatment. They demonstrated these gains as fewer difficulties with everyday activities (increased participation) as measured by the Rivermead Head Injury Follow‐Up Questionnaire (RHFUQ) (P value < 0.03).
A subsequent trial (Wade 1998) (218 completing participants) was undertaken. This trial prospectively selected the group admitted to hospital and again demonstrated improved outcomes for the treatment as needed group, with significantly fewer post‐concussive symptoms (Rivermead Post‐concussion Questionnaire (RPQ)) (Mann‐Whitney U: z = ‐2.27; P value < 0.02) and improved participation (RHFUQ) (z = ‐2.54; P value < 0.01). The impact of proactive intervention appeared to be most marked for participants with PTA < 7 days; these patients may be less likely than those more severely affected to present for services by themselves.
From the van Tulder 2003 'best evidence' synthesis of these studies, we concluded that 'strong evidence' suggests that:
-
most patients with mild TBI make a good recovery;
-
patients with PTA of less than one hour, usually not admitted to hospital, need no specific intervention;
-
patients with PTA of one hour or longer do benefit from routine follow‐up contact to receive information and advice; and
-
a subgroup of patients with moderate to severe injury benefit from a higher level of intervention and may not present themselves unless routine follow‐up is provided.
Patients with greater limitations on activities, with generally more severe brain damage and generally requiring greater multi‐disciplinary rehabilitation input
The effectiveness of combined out‐patient physiotherapy and occupational therapy was investigated by two trials in stroke patients (see Table 5).
| Smith 1981 | Participant and group comparisons | Patients suitable for out‐patient rehabilitation following discharge from hospital after acute stroke (n = 133); mean age 63 y Intervention: out‐patient physiotherapy and occupational therapy for 6 months at 2 levels of intensity:
Control: no routine rehabilitation, health visitor encourages home exercises as learned in hospital (n = 44) | |||
| Primary outcomes | Dependency for ADL: Northwick Park ADL score | ||||
| Assessment points | 3 and 12 months | ||||
| Summary of results | Significantly greater decrease in ADL scores in intNervention groups compared with controls at 3 months. Difference is sustained at 1 y follow‐up with greater number of control group participants (NB: trend towards better results from intensive rehabilitation than from conventional regimen not tested statistically) | ||||
| Decrease in ADL score | Intensive rehabilitation | Conventional rehabilitation | Control | P value | |
| Mean change 0 to 3 m | 3.54 (n = 41) | 2.87 (n = 40) | 1.50 (n = 42) | 1 vs 3: P value < 0.01 1/2 vs 3: P value < 0.01 | |
| Mean change 0 to 12 m | 3.50 (n = 36) | 2.89 (n = 36) | 0.60 (n = 35) | 1 vs 3: P value < 0.05 | |
| Authors’ conclusions | Out‐patient rehabilitation following stroke appears to be effective. Decreasing intensity of rehabilitation was associated with an increase in both the proportion of participants who deteriorated and the extent to which they deteriorated | ||||
| Werner 1996 | Participant and group comparisons | Patients discharged from in‐patient rehabilitation and ≥ 1 y (mean 2.9 y) after stroke (n = 49); mean age 63 y Intervention: out‐patient physiotherapy and occupational therapy (2 hours, 4 times per week, for 3 months) (n = 33) Control: no specific intervention (n = 16) (NB: 28% (5/33 intervention group and 9/16 control group) did not complete follow‐up: 5 non‐randomised controls were subsequently recruited to make control numbers up to 12) | |||
| Primary outcomes | Activity: Functional Independence Measure ‐ Motor (FIM‐MM) Limitation of participation: Sickness Impact Profile (SIP) Depression: Beck Depression Inventory (BDI) | ||||
| Assessment points | 3 and 9 months | ||||
| Summary of results | Significant changes in FIM and SIP at 3 months maintained at 9 months. Trend towards improved mood did not reach significance | ||||
| Mean change in score | Intervention (n = 28) | Control (n = 12) | Difference in mean | P value (t‐tests) | |
| FIM‐MM (0 to 3 mo) | 6.6 | 1.5 | 5.1 | 0.03 | |
| FIM‐MM (3 to 9 mo) | 0.7 | ‐1.0 | 1.7 | N/S | |
| SIP (0 to 3 mo) | ‐5.2 | 2.6 | 7.8 | 0.04 | |
| BDI (0 to 3 mo) | ‐2.6 | 0.2 | 2.8 | N/S | |
| BDI (3 to 9 mo) | 0.7 | 0.5 | 0.2 | N/S | |
| Authors’ conclusions | Significant gains can still be attained in the post‐acute stroke survivor, despite prior in‐patient rehabilitation services | ||||
ADLs = activities of daily living.
-
Smith 1981 reported a good quality, unblinded RCT (n = 133) that demonstrated improved functional ability (Northwick Park ADL Index) for groups attending as out‐patients as compared with a no‐treatment control group (P value < 0.01). A trend towards greater improvement with the more intense of two out‐patient programmes was not tested for significance. However, gains for both treated groups were maintained at one‐year follow‐up, while the control group was seen to deteriorate (P value < 0.05).
-
Werner 1996 reported a single‐blind CCT (n = 49) that was of much lower quality (see Table 3). This study assessed the benefits of late out‐patient intervention (offered at least one year after a stroke). The treatment group demonstrated significant gains in function (an increase in FIM motor score of 6.6 vs 1.5; P value < 0.03) and socialisation (sickness impact profile ‐5.2 vs an increase of 2.6 in the control group; P value < 0.04) at three months, which were maintained at nine months. However, no significant change in mood (Beck Depression Inventory) was observed.
In summary, from the van Tulder 2003 synthesis, 'moderate evidence' shows that outpatient therapy improves outcomes of stroke rehabilitation; 'limited evidence' suggests that more intensive treatment regimens are associated with better outcomes; and 'indicative evidence' reveals that this type of intervention may be effective even late (at least one year) after stroke.
Effectiveness of community‐based co‐ordinated multi‐disciplinary rehabilitation
This question was addressed by three trials (see Table 6).
| Powell 2002 | Participant and group comparisons | Patients (16 to 65 y) with severe traumatic brain injury 3 mo to 20 y previously (n = 110 allocated: 94 (85%) completed follow‐up) Intervention: inter‐disciplinary team interventions: 2 sessions per week for mean 27.3 (SD 19.1) weeks in community settings (home, work or day centres) (n = 48) Control: written information only (n = 46) | |||
| Primary outcomes | Activity: Barthel Index (BI) Participation: Brain Injury Community Rehabilitation Outcome (BICRO‐39) | ||||
| Assessment points | Approximately 2 y (median 23 mo) (IQR 18 to 40) | ||||
| Summary of results | Intervention group made significantly greater gains on both BI and BICRO scales. Median changes were small, reflecting the diversity of the population, but 40% of intervention group and only 20% of controls made a clinically significant improvement of 2+ points on ≥ 1 BICRO subscale | ||||
| Change scores from baseline | Intervention | Control | P value | ||
| BI: % improving Median (IQR) change | 35.4% 0 (‐5, 5) | 19.6% 0 (‐5, 4) | < 0.05 | ||
| BICRO‐39: % Median (IQR) change | 80% 2.5 (‐1.7, 6.2) | 70% 0.9 (‐4.1, 6.8) | < 0.05 | ||
| Authors’ conclusions | Multi‐disciplinary community rehabilitation, even years after injury, can make clinically significant gains which outlive the active treatment period. | ||||
| Bowen 2001 | Participant and group comparisons | Carers of young adult (16 to 65 y) TBI survivors with hospital stay ≥ 3 days (n = 96) Intervention: active intervention from Head Injury Neurorehabilitation Team (HINT)
Control: no specific intervention ‐ existing services only (n = 27) (NB: 20/96 (21%) received service other than that allocated ‐ only 56% allocated to early intervention actually received it) | |||
| Primary outcomes | Information received: carer perceptions of how well informed they are ‐ 7 questions Emotional state: Wimbledon Self‐report Scale (WSS) | ||||
| Assessment points | 6 mo post injury | ||||
| Summary of results | Analyses adjusted for potential confounding factors confirmed a clinically plausible superior outcome for both treatment groups compared with controls, but none of the results reached significance (set at P value < 0.01) | ||||
| Mean change from baseline | Early (n = 41) | Late (n = 28) | Control (n = 27) | P value (t‐tests) | |
| % poorly informed | 46%‐64% | 46%‐81% | 63%‐89% | N/S | |
| WSS, median (IQR) | 3 (0‐9) | 2 (0‐6) | 8 (1‐15) | N/S | |
| Authors' conclusions | Hypothesis not confirmed, but absence of effect cannot be proven with these data, which may reflect type II error in view of mixing of groups. Longer‐term follow‐up data also required | ||||
| Bjorkdahl 2006 | Participant and group comparisons | Stroke patients (mean age 53 y) discharged from an in‐patient rehabilitation programme
| |||
| Primary outcomes | Functional assessment: Motor and Process Skills (AMPS); secondary measures: mobility (30 m walking test); FIM, instrumental activity measure Impairment: NIH scale | ||||
| Assessment points | End of intervention (3 wk post discharge), 3 and 12 mo | ||||
| Summary of results | Both groups improved significantly from discharge to 1‐y follow‐up. No significant differences between groups for any of the 4 assessments, at any time point, although trends show earlier gains in the home‐rehabilitation group. Only the day clinic group changed ‘significantly’ on the FIM, but degree of change was small (5 FIM points over 1 y). Costs of home rehabilitation programme were less than half those of the day clinic | ||||
| Rasch transformed AMPS data (logits) | Home (n = 30) Mean (SD) | Day clinic (n = 39) Mean (SD) | |||
| Motor | Process | Motor | Process | ||
| Discharge 3 wk 3 mo 1 y | 1.45 1.71 2.02 2.18 | 1.00 1.26 1.23 1.55 | 1.42 1.52 1.88 2.28 | 1.18 1.37 1.54 1.59 | |
| Authors’ conclusions | Both rehabilitation programmes could be recommended, but additional studies are required to define patients who may benefit specifically from home rehabilitation. Costs should be taken into consideration | ||||
-
Powell 2002 reported a good quality, single‐blind RCT (n = 110) of a multi‐disciplinary community outreach service providing a home‐based goal‐oriented programme of two to six hours of intervention per week versus standard treatment. This group was more severely affected than the group studied by Wade 1998 (91% with PTA for seven days vs only 7%). Follow‐up was variable but averaged approximately two years. Gains for the intervention group were reported as reduced disability (35.4% showing improvement in Barthel Index vs 19.6% in the control group; P value < 0.05) and increased participation (significant changes on self organisation and psychological scales of the Brain Injury Community Rehabilitation Outcome Scales (BICRO)‐39; P value < 0.05), but no gains were observed for secondary outcomes, which included FIM+FAM and mood (Hospital Anxiety and Depression Scales (HADS)). Global disability scales such as FIM and FIM+FAM were noted to be insensitive, as most items did not change. A maximal gain index was calculated, which selected the subscales with maximal change. Rated in this way, changes in both disability (FIM+FAM) and participation (BICRO‐39) reached a greater level of significance (P value < 0.025).
-
Bowen 2001 reported an unblinded CCT of lower quality in which carer outcomes were evaluated following input from a multi‐disciplinary head injury specialist rehabilitation team in addition to standard services. An 'early' arm (n = 41) started the intervention before discharge, and a 'late' arm (n = 28) started after discharge. However, despite best intentions, only 23 of 41 (56%) actually received early intervention and 19 or 28 (67%) received late intervention, with some mixing noted between groups and with 14 participants receiving neither intervention. Nevertheless, intention‐to‐treat analysis revealed that the early intervention group still received significantly earlier treatment (median five days; P value < 0.001) than the late intervention group (median 40 days) post injury. At six months, after adjustment for confounding factors, a clinically plausible, superior outcome was reported for both intervention groups when compared with controls with regard to emotional status (Wimbledon Self Report Scale) and knowledge about brain injury. However, this finding did not reach Bonferroni‐adjusted clinical significance (P value < 0.01). Logistical difficulties with recruitment and service provision led to significant underpowering of this study and may have interfered with demonstration of a clinically significant effect.
-
Björkdahl 2006 reported a small single‐blinded RCT (n = 59) that compared a short programme of home‐based rehabilitation with one of out‐patient day rehabilitation following a period of in‐patient stroke rehabilitation. Although neither group changed significantly in terms of impairment, both were reported to make significant gains in Assessment of Motor and Process Skills (AMPS) and in mobility over a one‐year follow‐up period. Although a trend toward earlier gains was observed in the home rehabilitation group, researchers noted no significant differences at any time point. Only the day clinic group changed significantly on functional measures (Functional Independence Measure), but the degree of change was small (5 FIM points over one year). Despite an a priori power calculation, the trial was probably underpowered to distinguish between groups and had a moderately high chance of a type II error. On the basis of this evidence, neither programme could be said to be better than the other, although the cost of the home‐based programme was noted to be half that of the day clinic programme.
In summary, this group of studies provided 'limited evidence' that multi‐disciplinary, community‐based rehabilitation can improve functional outcomes for individuals at the level of 'activity' (disability) on the WHO ICF (especially when targeted towards specific goals).
Specialist in‐patient rehabilitation
Two studies addressed the benefits of specialist in‐patient rehabilitation in comparison with those of local services (Semlyen 1998) (n = 51) or a home‐based advisory service (Ozdemir 2001) (n = 60) (see Table 7). Both studies were small and exhibited low methodological quality.
| Semlyen 1998 | Participant and group comparisons | Consecutive patients in‐hospital with severe TBI and referred for in‐patient rehabilitation within 4 weeks of injury; age 16 to 62 y Intervention: multi‐disciplinary specialist rehabilitation service ‐ Hunter’s Moor (HM) (n = 33) Control: ‘Other rehabilitation’ (OR) in local non‐specialist services in district hospitals (n = 18) | ||
| Primary outcomes | Activity and independence: Barthel Index, FIM and Newcastle Independence Assessment Form (NIAF) Care‐givers' Health: GHQ‐28 | |||
| Assessment points | 1, 2, 3, 6, 12 and 24 mo after injury | |||
| Summary of results | Only Z values (BI) and t‐values (FIM and NIAF) are given HM intervention group was significantly more disabled at outset (as indicated by FIM up to 3 mo, BI up to 6 mo and NIAF up to 12 mo). By 12 mo, therefore, the HM group had caught up with the OR group in level of activity OR group made significant gains only up to 12 wk on NIAF and FIM cognitive scales, but none on the FIM motor or BI (already at ceiling). By contrast, HM continued to make significant gains up to 24 mo, as assessed by NIAF and BI Significant improvements in carer distress for the HM group were sustained at 2 y, whereas the OR group showed evidence of deterioration between 6 and 12 mo No differences in length of stay between groups | |||
| Authors’ conclusions | Results support the efficiency of specialist rehabilitation services in achieving lasting gains for patients with more severe disability over similar lengths of stay | |||
| Ozedemir 2001 | Participant and group comparisons | Stroke patients referred for rehabilitation after medical stabilisation (n = 60); mean age 59.1 y (SD 5.9) Group 1: in‐patient rehabilitation (n = 30) ‐ ≥ 2 h/d of formal therapy, 5 d/wk Group 2: home‐based rehabilitation (n = 30) ‐ team visited home for 2 h/wk and instructed family in home exercises ‐ family provided therapy ≥ 2 h/d, 7 d/wk Mean duration of rehabilitation 64 d in both groups | ||
| Primary outcomes | Impairment: Brunnstrom score, Ashworth (spasticity) Activity: FIM, Mini‐Mental State Examination (MMSE) | |||
| Assessment points | Before and after rehabilitation | |||
| Summary of results | Significant group differences in favour of in‐patient group for change in Brunnstrom, FIM and MMSE scores, but no differences in spasticity | |||
| Change scores | Group 1 Mean (SD) | Group 2 Mean (SD) | P value (t‐tests) | |
| Ashworth UE | 0.5 (1.2) | 0.2 (0.5) | N/S | |
| Ashworth LE | 0.2 (1.2) | 0.1 (0.3) | N/S | |
| Brunnstrom (UE) | 2.0 (1.2) | 0.3 (0.6) | < 0.001 | |
| Brunnstrom (LE) | 2.4 (1.2) | 0.8 (0.6) | < 0.001 | |
| FIM | 59.6 (14.2) | 12.3 (13.4) | < 0.001 | |
| MMSE | 4.8 (5.0) | 2.0 (2.1) | < 0.001 | |
| Authors' conclusions | Intensive in‐patient rehabilitation provided significantly more favourable functional and cognitive outcomes than home‐based rehabilitation programme | |||
-
Methodological problems of Semlyen 1998 (n = 51) have already been highlighted. The 'multi‐disciplinary (MD) rehabilitation' group was significantly more disabled at the outset. Thus, significantly greater gains evident at each measurement point up to 24 months may have reflected this lower starting point and the fact that many of the 'other rehabilitation' groups were already at ceiling levels on some scores. Carer distress was assessed using the General Health Questionnaire, which identified a higher proportion of 'cases' in the MD rehabilitation group at the outset, which fell between six and 12 months. By contrast, the proportion of cases in the 'other rehabilitation' groups started from a lower point but rose progressively throughout the follow‐up period. By 12 months, carers in the 'other rehabilitation' group had significantly higher levels of distress than those in the MD rehabilitation group.
-
Ozdemir 2001 reported an unblinded CCT in 60 stroke patients. Groups were well matched to start with. The treatment group made a five‐fold greater gain in FIM score (mean 59.6 4.8 ± 14.1 vs mean 12.3 4.8 ± 13.4; P value < 0.001) and a two‐fold change in Mini‐Mental State Examination (MMSE) (mean 4.8 ± 5.0 vs mean 2.0 4.8 ± 2.1; P value < 0.025) compared with the control group.
In summary, 'limited evidence' at the current time suggests that specialist in‐patient rehabilitation services can improve functional outcomes in terms of both activity (reduced disability) and carer distress when compared with controls. However, this reflects in part the practical and ethical difficulties associated with allocating individuals with severe brain injury no opportunity for co‐ordinated multi‐disciplinary rehabilitation. This problem is elaborated in the Discussion section.
Increased intensity of rehabilitation
Four trials addressed the benefits of increased intensity of rehabilitation (see Table 8).
| Kwakkel 1999 | Participant and | Stroke patients within 2 wk of onset (n = 101) All groups received 15 min arm training plus 15 min leg training daily, plus 1.5 h ADL training per wk In addition, for 30 min 5 d/wk, groups received: Group 1: intensive arm training (n = 33) Group 2: intensive leg training (n = 31) Group 3 (control): inflatable splint (n = 37) | |||
| Primary outcomes | ADL ability: Barthel Index (BI) Walking ability: functional ambulation categories (FAC) Dexterity: Action Research Arm Test (AR Arm Test) | ||||
| Assessment points | 0, 6, 12, 20, 26, 38, 52 wk | ||||
| Median (IQR) at 20 wk | Arm training | Leg training | Control | P value (K‐W test) | |
| BI | 17 (14‐20) | 19 (16‐20) | 16 (10‐19) | < 0.05 | |
| FAC | 4 (3‐5) | 4 (3‐5) | 3 (1‐4) | < 0.05 | |
| AR Arm Test | 9 (0‐39) | 2 (0‐56) | 0 (0‐2) | < 0.01 | |
| Authors’ conclusions | Greater intensity of leg training improves early functional recovery; whereas greater intensity of arm training improves only dexterity, providing further evidence that therapy primarily induces effects on abilities at which training is specifically aimed. Functional gains maintained up to 1 y | ||||
| Zhu 2001
| Participant and | Patients aged 12 to 65 y with moderate to severe TBI up to 6 mo post injury (n = 68) Interventions: multi‐disciplinary rehabilitation at 2 intensities:
| |||
| Primary outcomes | Global outcome: Glasgow Outcome Scale (GOS) Activity (disability): FIM, Neurobehavioural Cognitive Status Examination (NCSE) | ||||
| Assessment points | 0, 1, 2, 3, 4, 5, 8, 10 and 12 mo | ||||
| Summary of results | No statistically significant differences in FIM or NSCE between groups. However, significantly greater number of participants achieved maximal FIM and GOS scores within 3 mo, although no differences were noted at later time points and up to 1 year | ||||
| Outcome | Intensive (n = 36) | Conventional (n = 32) | P value (Chi2) | ||
| % good GOS 3 mo | 38
| 14
| Chi2 3.9, df 1, P value = 0.044 P value = 0.483 | ||
| % full FIM 3 mo | 47
| 19
| Chi2 5.8, df 1, P value = 0.015 P value = 0.242 | ||
| Authors’ conclusions | Early intensive rehabilitation can improve functional outcomes of patients with TBI in the early months post injury, and hence may increase the chance of their early return to work Intensive rehabilitation in this study speeded up recovery rather than changing final outcomes | ||||
| Shiel 2001
| Participant and | Patients with moderate to severe TBI (age 16 to 70 y) admitted for rehabilitation (n = 51); stratified and randomly assigned on age and GCS Intervention groups
(NB: study conducted across 2 centres, which had very different structures and processes, 1 offering significantly more routine therapy than the other. Participants at each centre were randomly assigned to received standard and enhanced therapy according to their practice | |||
| Primary outcomes | Activity (disability): FIM+FAM | ||||
| Assessment points | Admission and discharge | ||||
| Summary of results | Despite procedural differences between centres, no significant differences in FIM+FAM change scores were reported between centres. Significant differences were observed between intensive and routine intervention groups and were greatest in the domains of self care, continence, locomotion and psychosocial function. No significant difference in length of stay overall, but possibly skewed by very prolonged LOS for intervention group at 1 centre | ||||
| Change scores during admission | Enhanced intensity Median (IQR)
| Routine Median (IQR) | P (Mann‐Whitney) | ||
| FIM+FAM Motor | 74 (47‐95)
| 21 (2‐48) | < 0.01 | ||
| FIM+FAM Cognitive | 40 (14‐45)
| 12 (5‐22) | < 0.01 | ||
| Authors’ conclusions | Increased intensity of rehabilitation is associated with enhanced function recovery | ||||
| Slade 2001
| Participant and | Patients with acquired brain injury (stroke, TBI or MS) aged 16 to 65 y admitted for rehabilitation (n = 131) Interventions: multi‐disciplinary rehabilitation at 2 intensities:
(NB: Although in theory the intensive group should have received 67% more therapy than controls, in reality, they received only 30% more) | |||
| Primary outcomes | Length of stay (LOS) ADL ability: Modified Barthel Index | ||||
| Assessment points | Admission and discharge | ||||
| Summary of results | No significant differences in discharge Barthel scores were reported (data not given), but this is expected, as patients are discharged at the point at which they are sufficiently independent to manage in the community. This question is then whether more intensive therapy reaches that point earlier Mean LOS for all participants was 84.6 d. Straightforward comparison showed no significant group interactions However, a multiple regression model was applied to take account of confounders of experimental design that could not be controlled for (impairment mix, community delays, missed treatment, etc.); this demonstrated a 14‐d reduction for the intensive group | ||||
| Authors’ conclusions | Intensive rehabilitation has the potential to reduce length of stay, but concurrently, LOS in both groups was increased by 16 d as the result of external delays in discharge | ||||
-
Kwakkel 1999 reported a good quality, single‐blinded RCT for 101 severely disabled stroke patients that compared a group with emphasis on arm training (n = 33), a group with emphasis on leg‐training (n = 31) and a control group (n = 37), whose arms and legs were immobilised in an inflatable splint. Each treatment was applied for 30 minutes, five days a week, for the first 20 weeks after stroke; this was over and above a consistent basic level of intervention for all groups. Post hoc analysis by the Kruskal‐Wallis test showed that leg training resulted in significantly greater independence (Barthel Index) and mobility (functional ambulation categories) than could be seen in the control group up to the first 20 weeks, and better dexterity (Action Research Arm Test) in the ‘arm training’ group from week 12 onwards. Effects of treatment appeared to be maintained at one year, but no significant differences were demonstrated between groups beyond six months.
-
Shiel 2001 reported a two‐centre RCT (n = 51 completing participants) for patients with moderate to severe traumatic brain injury. At each centre, participants were randomly assigned to receive routine treatment with or without input from an additional experienced staff member acting in a transdisciplinary capacity to supplement the rehabilitation programme. Those with added intensity of input made more rapid gains in independence (FIM+FAM) at both centres, with no evidence of any ceiling effect of therapeutic intensity beyond which no further response was observed. However, investigators reported marked differences between the two centres in terms of staffing levels and intensity of the routine programme. This led to substantially shorter lengths of stay at one centre, so that no significant reduction in length of stay was observed for the trial as a whole despite more rapid gains in independence.
-
Slade 2002 conducted a good quality, single‐blind RCT (n = 131) for a group with mixed ABI that compared two rehabilitation programmes in the same setting ‐ one more intensive than the other. Records of therapy input demonstrated that individuals were able to tolerate increased input with no adverse effects. Although investigators intended for the intensive group to receive 67% more therapy than the control group, the intensive group in fact received only 30% more. The intention to demonstrate reduced length of stay as a result of more intensive therapy was confounded by external delays in discharge. Analysis by a regression model was undertaken to account for confounding variables including impairment mix and factors that could not be controlled for in the study design (community delays and missed treatment). This revealed a significant reduction in length of stay (14 days; P value < 0.001) for the intensive group. Similar Barthel scores between groups at admission and at discharge confirmed that this reduced length of stay did not occur at the expense of poorer functional outcomes.
-
Zhu 2007 reported a small but good quality single‐blind RCT for individuals with moderate to severe traumatic brain injury (n = 68) that compared different intensities of treatment (two vs four hours per day for up to six months). Analysis of time utilisation, presented in a preliminary report (Zhu 2001), showed that after the second week, most participants could tolerate therapy lasting longer than two hours per day. Functional and overall outcome status FIM and Glasgow Outcome Scale (GOS) scores were recorded monthly to every six months, then bi‐monthly to each year. No significant differences were found between the two treatment groups beyond three months, but significantly more patients in the high‐intensity group achieved a maximum FIM score at three months (47% vs 19%) and GOS score at two months (28% vs 8%), although these early functional gains did not appear to have a significant impact on length of stay. This study provides evidence that intensive rehabilitation may speed up recovery rather than changing final outcomes. Study authors concluded that early intensive rehabilitation can improve functional outcomes of individuals with TBI in the early months post injury and may (theoretically) increase their chances of early return to work, although actual return to work and job retention were not recorded as outcomes in this study. As most individuals did not remain in the programme beyond 90 days, it is not possible to know whether more prolonged intervention, or treatment targeted at goals beyond simple activities of daily living, could have capitalised on these earlier gains to produce higher‐level gains in participation and in social integration.
In summary, from the van Tulder 2003 synthesis, 'strong evidence' shows that more intensive rehabilitation programmes are associated with earlier function gains once patients are fit to engage. No evidence showed a ceiling effect on therapeutic intensity in any of these studies. However, for intensive intervention to be cost‐effective, it is necessary to demonstrate that it is associated with potential cost savings farther down the line (e.g. reduction in length of stay, long‐term dependency) that might offset the additional costs of providing the initial programme. None of these studies undertook a direct analysis of cost‐effectiveness, and at the current time, only 'moderate evidence' indicates that more intensive rehabilitation leads to reduced length of stay. On the other hand, length of stay is frequently affected by external confounders (such as lack of a suitable place to discharge the patient, or lack of community support for a patient otherwise ready for discharge) that may need to be controlled before this benefit can be demonstrated.
Early versus delayed rehabilitation
Two trials addressed the question of whether starting rehabilitation earlier after injury could result in better patient outcomes (see Table 9).
| Andelic 2012 | Participant and group comparisons | Patients with severe TBI; mean age 29.4 y Intervention:continuous chain of rehabilitation from specialist on ITU directly into specialist subacute rehabilitation post discharge from ITU (n = 33). | ||
| Primary outcomes | Disability: Glasgow Outcome Scale Extended (GOSE) | |||
| Secondary outcomes | Disability: Disability Rating Score (DRS) Employment status: return to work Living situation: at home with or without care, or in a nursing home | |||
| Assessment points | 12 months post injury (n = 61) | |||
| Summary of results | Disability (GOSE) at 12 mo significantly less in the early rehabilitation group than in the control group Significantly higher percentage of participants in the early rehabilitation group were living at home when compared with controls Non‐significant trend towards higher rate of return to work in the early rehabilitation group than in the control group Non‐significant trend towards shorter overall length of stay (acute hospital and rehabilitation unit) in the early rehabilitation group | |||
| Outcomes | Intervention | Control | P value | |
| Favourable GOSE (6‐8) | 71% | 37% | 0.007 | |
| % living at home | 81 | 53 | 0.06 | |
| Authors' conclusions | Early comprehensive rehabilitation in a continuous chain leads to better functional outcomes at 12 months post injury among patients with severe TBI | |||
| Bai 2012 | Participant and group comparisons | Patients with moderate to severe intracerebral haemorrhage; mean age 61 y Intervention: early rehabilitation commencing in the Emergency Department and continuing for 6 mo (n = 181) Controls: standard medical care (n = 183) | ||
| Primary outcomes | Impairment: Fugl‐Meyer Assessment (FMA) Disability: Modified Barthel Index (MBI) | |||
| Assessment points | Outcome measures administered at 1, 3 and 6 mo | |||
| Summary of results | At baseline, post hoc testing showed no significant differences between FMA and MBI scores in the 2 groups At 1, 3 and 6 mo, intervention group had significantly higher FMA and MBI scores | |||
| Authors' conclusions | Early rehabilitation can significantly improve ADLs and motor recovery in patients with intracranial haemorrhage | |||
-
Andelic 2012 was a controlled study involving patients with severe TBI (n = 61 completing participants). Participants received early comprehensive rehabilitation (1 hour and 45 minutes per day involving motor, sensory and facial components) starting immediately after admission to a dedicated rehabilitation section of the ICU (n = 33) or awaited eventual subacute rehabilitation on an in‐patient brain injury unit (n = 31). In fact, some of the latter group received no rehabilitation at all. Treatment allocation was dependent on availability of beds in the rehabilitation section of the ITU. The early rehabilitation group showed significantly better functional outcomes with lower scores on GOSE and the Disability Rating Scale (DRS). In addition, participants in the early rehabilitation group showed increased independence (81% living at home) compared with controls (23% living at home; P value = 0.06). As a result of its design, this study is subject to clear quality flaws as a result of lack of randomisation and blinding. In addition, functional measures were taken only at 12 months; therefore, no estimate of functional change or of functional similarity in intervention and control groups could be made at baseline. A subsequent cost‐effectiveness analysis (Andelic 2014) used a decision tree model to compare hospitalisation costs, health effects and incremental cost‐effectiveness ratios of a continuous chain versus a broken chain of rehabilitation. Across five years, the continuous chain of rehabilitation resulted in lower costs and better health effects. By replacing the broken chain with the continuous chain, Norwegian Krone 37.000 could be saved and 4.06 DRS points gained. (The study report gives an exchange rate of USD 1 = NOK 6.09, so approximately $6,000 in US dollars in 2012 could be saved.)
-
Bai 2012 reported a single‐blinded randomised controlled trial involving individuals with moderate to severe intracerebral haemorrhage (n = 345 completing participants). Participants were randomly assigned to an ‘early rehabilitation’ group (n = 181) or to a control group receiving standard ward care (n = 183). Participants in the early rehabilitation group received a six‐month programme of rehabilitation in three stages, beginning in the Emergency or Neurology Department during the first month after admission, and continuing into the community. Individuals in the control group received only routine medical care. The intervention group showed significantly higher Fugl‐Meyer Assessment (FMA) and Modified Barthel Index (MBI) scores than were reported in controls at one, three and six months post stroke (all P values < 0.05). Study authors concluded that early rehabilitation can improve functional recovery among individuals with intracerebral haemorrhage. The quality of the paper is limited by the fact that very little information is provided on the processes of randomisation, treatment allocation and blinding. Moreover, no explanation is provided as to why the paper was published eight years after data were collected.
In spite of clear limitations in the quality of these two studies, taken together they provide ‘limited evidence’ to support commencing comprehensive rehabilitation acutely in patients with moderate to severe injury.
Therapeutic milieu‐based rehabilitation
Two trials investigated use of a ‘therapeutic milieu’ model of rehabilitation (see Table 10). On the basis of models described by Ben‐Yishay 1990 and Prigatano 1994, this approach comprises intensive holistic neuropsychological rehabilitation delivered as a largely group‐based intervention in a residential setting.
| Cicerone 2008 | Participant and group comparisons | Mixed severity traumatic brain injury; mean age 36.6 y Intervention: intensive cognitive rehabilitation provided in a therapeutic environment (n = 34) with a focus on group work Control: standard neurorehabilitation; mostly individual, discipline‐specific therapy (n = 34) | |||
| Primary outcomes | Community integration: Community Integration Questionnaire (CIQ) Life satisfaction: Perceived Quality of Life Scale (PQOL) | ||||
| Secondary outcomes | Neuropsychological functioning Perceived self‐efficacy Vocational outcome: Vocational Integration Scale (VIS) | ||||
| Assessment points | 2 wk before treatment, 2 wk post treatment and 6 mo follow‐up | ||||
| Summary of results | Treatment arm showed significantly improved community integration and quality of life scores ‐ not seen in control arm Self efficacy was significantly improved in the treatment arm – another improvement not seen in the control arm Additionally, treatment group had a significantly higher rate of employment compared with control group | ||||
| Standard neurorehabilitation | |||||
| Outcome measures | Pre‐Tx | Post‐Tx | Follow‐up | P value | |
| CIQ | 12.1 | 11.7 | 12.9 | > 0.05 | |
| PQOL | 61.2 | 62.2 | 59.6 | > 0.05 | |
| Authors' conclusions | This trial demonstrates that an intensive cognitive rehabilitation programme can produce significantly better outcomes when compared with standard neurorehabilitation | ||||
| Salazar 2000 | Participant and group comparisons | Active duty military personnel with moderate to severe TBI; mean age 25 y Intervention: 8‐week intensive in‐patient cognitive‐behavioural programme (n = 67) Control: limited home programme of weekly telephone support from psychiatric nurse (educational material, counselling and suggested home exercises) (n = 53) | |||
| Primary outcomes | Work status: return to work return to fitness for military duty | ||||
| Assessment points | 1 y | ||||
| Summary of results | No overall differences in outcomes between groups Post hoc analysis demonstrated significant group interaction (in favour of the intervention group) for ‘fitness for military duty’ at 1 y for members of the more severe subgroup, who were unconscious for >1 h | ||||
| Vocational status at 1 y | Intervention % achieved | Control % achieved | Difference | P value (Fisher's exact) | |
| Return to work | 90% | 94% | 4% (‐5,14) | N/S | |
| Fit for military duty | 73% | 66% | 7% (‐10.24) | N/S | |
| Post hoc analysis of subgroup unconscious for > 1 h (n = 75) | |||||
| (n = 35) | (n = 40) | Difference | P value | ||
| Fit for military duty | 80% | 58% | 22% | 0.05 | |
| Authors' conclusions | Overall benefit of in‐patient cognitive rehabilitation programme similar to that of limited home rehabilitation, although institutional therapy may be beneficial for selected patients with more severe TBI | ||||
-
Cicerone 2008 reported a high‐quality, single‐blinded RCT for patients with TBI of mixed severity (n = 62 completing participants). Participants were randomly assigned to receive intensive cognitive rehabilitation (treatment arm n = 34) or standard neurorehabilitation (control arm n = 34). Approximately 15 hours per week of both interventions was delivered at the same centre, but treatment orientation and programme structure varied. The cognitive group received ‘intensive neurospsychological’ rehabilitation based on the milieu model, with more group‐based interventions provided in a therapeutic environment. The standard rehabilitation group consisted primarily of individual discipline‐specific out‐patient interventions. Study authors hypothesised that the intensive neuropsychological programme would result in greater improvement in community integration, productivity and life satisfaction than was provided by the standard programme. Participants in the treatment arm of this trial showed a statistically significant improvement on both the Community Integration Questionnaire (CIQ) and the Perceived Quality of Life Scale (PQOL) between pre‐treatment and post‐treatment assessment, and improvements were maintained at six‐month follow‐up compared with no significant change in the control arm. With respect to secondary outcomes, both treatment and control arms improved significantly on neuropsychological testing. Self efficacy was significantly improved in the treatment arm immediately post treatment, and improvement was maintained at follow‐up, whereas the control arm demonstrated no significant change.
-
Salazar 2000 compared an eight‐week intensive in‐patient cognitive rehabilitation programme modelled on the milieu‐based approach versus a home‐based programme of weekly telephone contact providing counselling and advice from a psychiatric nurse for active military personnel with moderate to severe TBI. Although main results showed no significant differences between groups overall, post hoc analysis of participants in the more severe subgroup (i.e. those who were unconscious > 1 hour at the time of injury; n = 75) showed that individuals in the intervention group were more likely than controls to be 'fit for military duty' at one year (80% in intervention group vs 58% in control group; P value = 0.05). As the trial pre‐dated the requirement for pre‐registration, it is not known whether this sub‐group analysis was pre‐planned. However, brain injury severity is an anticipated confounding factor for rehabilitation outcome, and the findings resonate with other studies (e.g. Wade 1997 and Wade 1998) suggesting that it is the more severely injured patients who have most to gain from organised rehabilitation programmes.
In summary, from the van Tulder 2003 synthesis, these two high‐quality studies have provided reasonably ‘strong evidence’ that a milieu‐based approach to in‐patient rehabilitation is effective for individuals with moderate to severe ABI.
Discusión
Esta revisión indica que la rehabilitación multidisciplinaria con servicios de rehabilitación neurológica especializada mejora los resultados después de la lesión cerebral aguda (LCA) en adultos de en edad laboral, y que es probable que una mayor intensidad dé lugar a una recuperación más rápida y posiblemente mejor. También indica que los pacientes con traumatismo craneoencefálico (TCE) relativamente leve que no ingresan al hospital, o que no presentan un período de amnesia postraumática mayor de 30 minutos, se recuperarán sin el seguimiento y la rehabilitación especializados habituales.
De esta actualización han surgido nuevos hallazgos.
-
Las pruebas de dos ensayos controlados aleatorios (ECA) de alta calidad muestran que en la LCA moderada a grave, los programas residenciales basados en el medio (mediante los cuales los pacientes reciben rehabilitación neuropsicológica en un ambiente terapéutico con compañeros que enfrentan retos similares) pueden ser más efectivos que las intervenciones individuales de nivel inferior.
-
Existen pruebas limitadas que indican que iniciar la rehabilitación más temprano después de la lesión, mientras los pacientes todavía están en ámbitos de atención de urgencia o de casos agudos, puede dar lugar a mejores resultados en los pacientes con LCA moderado a grave.
Esta revisión destaca la necesidad de estudios de investigación adicionales para confirmar la conclusión general, investigar la relación entre costo y efectividad e identificar qué componentes del paquete de rehabilitación son de especial importancia.
Contexto
Esta revisión necesita colocarse en el contexto de otros estudios y revisiones que investigan la rehabilitación especializada (neurológica). Varias revisiones Cochrane han presentado conclusiones similares con respecto a otros programas de rehabilitación para el accidente cerebrovascular (Stroke Unit Trialists Collaboration 2007) después del reemplazo la articulación de la cadera o la rodilla (Khan 2008), en pacientes con esclerosis múltiple (Khan 2007) y en pacientes con enfermedad pulmonar obstructiva crónica (Lacasse 2006).
Por lo tanto, no sorprende que esta revisión indique que la rehabilitación es una intervención efectiva.
Sin embargo, se debe recalcar que estos estudios han investigado principalmente el proceso de rehabilitación, y no una intervención específica (terapia o tratamiento) o un grupo de intervenciones. Los investigadores han mostrado que la participación en un servicio que incluya un equipo multidisciplinario de personas con pericia en la rehabilitación neurológica y que se centre en la reducción de la discapacidad y en aumentar la participación social mediante un proceso de solución de problemas, generalmente mejora los resultados de los pacientes.
Las pruebas de la rehabilitación de un accidente cerebrovascular, utilizadas para formular una recomendación relevante (3.2.1B) en la tercera edición de National Clinical Guideline for Stroke del Reino Unido (Royal College of Physicians 2008), indican que las características clave de un servicio de rehabilitación especializada exitoso incluyen las siguientes.
-
Equipo multidisciplinario.
-
Todos los miembros del equipo con pericia relevante.
-
Programas educacionales para el personal, los pacientes y los familiares.
-
Base o ubicación geográfica específica.
-
Acordar protocolos basados en pruebas para tratar los problemas comunes, cuando sea posible.
Limitaciones de esta revisión
Esta revisión siguió un enfoque inclusivo para un área amplia de la práctica clínica y un grupo de gran variedad de afecciones bajo el estandarte colectivo de "lesión cerebral adquirida". Este enfoque planteó retos para la evaluación y la asimilación de las pruebas disponibles.
Primero, la calidad de los estudios incluidos puede haber sido demasiado baja para permitir establecer conclusiones útiles por sí solos. Sin embargo, la síntesis presentada mediante el enfoque de las "mejores pruebas", que incluye una medida de calidad metodológica, ha facilitado una comparación útil de varios estudios disponibles. También ha permitido el reconocimiento público de las pruebas limitadas proporcionadas por estos estudios más deficientes, que no obstante, son las mejores actualmente disponibles (o, de hecho, es probable que estén disponibles en algunas áreas) por las razones analizadas a continuación.
Segundo, un enfoque menos sistemático, al realizar muchas revisiones separadas de los diversos modelos de práctica, quizás haya sido más fácil de interpretar y analizar. Sin embargo, los pacientes rara vez se presentan con un problema único, y los estudios sobre soluciones individuales no necesariamente son útiles o utilizables. Tienen sus propias deficiencias al reclutar a pacientes muy seleccionados o incluir muchas otras variables que pueden afectar los resultados. Por lo tanto, aunque algunos países planifican u organizan la prestación de servicios alrededor de programas específicos de rehabilitación para grupos con diagnósticos específicos, un enfoque más amplio condicionado por las necesidades de prestación de servicios a grupos más mixtos de pacientes es probablemente más apropiado y es lo que se ha evaluado. Los estudios en la unidad de accidentes cerebrovasculares son el ejemplo más sólido de la investigación centrada en un enfoque amplio, no un enfoque poco sistemático, y estos investigadores han sido claros en los resultados e influyentes en el campo.
Tercero, para mantener la revisión a un tamaño manejable, los estudios considerados se restringieron cuidadosamente a los que clasificaban dentro del alcance del protocolo. No se incluyeron los estudios que investigaron el proceso de rehabilitación dentro de una única profesión o en pacientes de edad avanzada. En esta actualización se excluyó a Vanderploeg 2008 después de mucha deliberación. Este estudio del Defense and Veterans Brain Injury Center Study Group de los EE.UU. (el mismo grupo de Salazar 2000) es un estudio de alta calidad bien realizado que comparó dos enfoques para la rehabilitación, un enfoque "cognitivo‐didáctico" y un enfoque "funcional‐experimental", dentro de un ambiente compartido. Aunque los investigadores no mostraron diferencias estadísticamente significativas entre los dos enfoques, destacaron la importancia de estudios de investigación adicionales sobre diferentes enfoques para la rehabilitación multidisciplinaria, lo que está más allá del alcance de esta revisión.
Por último, esta revisión se centró en las afecciones de inicio agudo, pero el proceso de rehabilitación y los tipos de problemas enfrentados por los pacientes con otros tipos de enfermedades son similares. Se observaron con interés los resultados del ensayo controlado con lista de espera Khan 2014 en supervivientes de cáncer cerebral, que demostró que la rehabilitación multidisciplinaria puede mejorar la función, con logros mantenidos hasta seis meses. Los participantes se asignaron a los grupos de tratamiento o control sobre la base de la necesidad, por razones que son completamente comprensibles en esta población. Sin embargo, este estudio no cumplió los criterios de inclusión para esta revisión, ya que no se cumplió el requisito de "un gran elemento de probabilidad" en la asignación al tratamiento.
Se decidió limitar el alcance de esta revisión, en parte para llenar un vacío en el grupo más amplio de revisiones de rehabilitación y en parte porque los comisionados de servicio (compradores) perciben a los adultos con lesión cerebral adquirida como una población específica que necesita un grupo específico de pruebas. Otras revisiones Cochrane se han centrado en la rehabilitación multidisciplinaria en afecciones como la esclerosis múltiple (Khan 2007), la enfermedad de la motoneurona (Ng 2009) y el síndrome de Guillain‐Barré (Khan 2010).
En resumen, se considera que estas limitaciones se deben colocar en el contexto del conjunto completo de la investigación en la rehabilitación especializada y que no restan mérito a las conclusiones.
Implicaciones
Los resultados directos de esta revisión tienen algunas implicaciones para la solicitud y la prestación de servicios, que en gran parte apoyan el desarrollo y el uso de los servicios de rehabilitación neurológica especializada en los pacientes en edad laboral con problemas residuales poco después de la lesión cerebral de aparición aguda, independientemente de cómo se adquirió.
Las otras lecciones importantes a aprender se relacionan con la naturaleza de la rehabilitación y las maneras en que se realiza la investigación en la rehabilitación.
Los ensayos controlados aleatorios son el medio principal para demostrar la eficacia del tratamiento, sobre todo por su capacidad de controlar los factores de confusión desconocidos, muchos de los cuales se encuentran en la rehabilitación. Son adecuados para intervenciones únicas fácilmente identificadas, como fármacos o procedimientos específicos.
Sin embargo, la rehabilitación es una intervención compleja que tiene muchos componentes interdependientes e interrelacionados. Los cambios que se producen durante la rehabilitación se deben evaluar contra el telón de fondo de la recuperación espontánea, pero las relaciones previstas bien pueden ser no lineales e imprevisibles individualmente. Lo anterior se ha reconocido cada vez con mayor frecuencia en muchas otras áreas de la investigación en asistencia sanitaria.
En el contexto de la investigación en el proceso de rehabilitación y en intervenciones (tratamientos) de rehabilitación más específicas, esta revisión ha destacado varios desafíos.
-
Los números de pacientes son relativamente pequeños.
-
La heterogeneidad es notable entre las características clínicas relevantes, las intervenciones, los contextos y los resultados.
-
Los recursos requeridos para asignar al azar sistemas completos de atención a diferentes grupos de tratamiento son mucho mayores que los requeridos para la administración de fármacos o procedimientos específicos.
-
El período de tiempo durante el cual la rehabilitación puede tener efectos (siempre muchos meses y habitualmente varios años) es habitualmente más prolongado que cualquier proyecto de investigación financiado.
Además, el grupo de pruebas en expansión de la efectividad de la rehabilitación multidisciplinaria en otras afecciones (en particular el accidente cerebrovascular) hace cada vez más difícil (ética y prácticamente) asignar al azar a los participantes de los estudios a la rehabilitación no especializada, ya que no se puede argumentar "equipoise" clínico.
Es decir, la realidad es que los servicios de rehabilitación neurológica especializada no están disponibles para muchos pacientes, incluso en los países ricos (como el Reino Unido y EE.UU.), por lo que en teoría todavía debe ser posible realizar estudios aleatorios que comparen la rehabilitación por un equipo de rehabilitación neurológica multidisciplinaria especializada versus la rehabilitación no especializada, poco sistemática y no coordinada, que actualmente reciben muchas personas. Además, los diseños como los ensayos aleatorios grupales (en los que un servicio completo se puede asignar al azar, en contraposición con participantes individuales) pueden ayudar a abordar algunos de los retos, aunque traen consigo sus propios retos en cuanto a la complejidad del diseño y el análisis y en que requieren números mayores para producir el poder estadístico requerido.
Por lo tanto, se recomienda que dichos estudios se deben realizar cuando sea posible adquirir un grupo de pruebas equivalentes a las adquiridas en las unidades de accidente cerebrovascular, siempre que se puedan superar las diversas barreras prácticas y logísticas.
Los estudios identificados en esta revisión proporcionan algunas revelaciones útiles sobre problemas prácticos asociados con los estudios de investigación en esta área que será necesario analizar en los estudios futuros.
Reclutamiento y retención de los participantes
Cuando el consentimiento completamente informado se obtiene antes de la participación (como debe ser), el reclutamiento y la retención pueden ser problemáticos, especialmente para el brazo control. Por ejemplo, Werner 1996 comenzó como un estudio aleatorio ponderado. Sin embargo, una vez reclutados, muchos participantes del grupo control demostraron renuencia a asistir a las evaluaciones, ya que se sentían desilusionados por no pertenecer al grupo de tratamiento. Después de que más de la mitad del grupo control abandonara el seguimiento, los investigadores se vieron obligados a reclutar otros cinco controles más de manera no aleatoria.
Diferencias entre centros
Se necesitan estudios multicéntricos debido al reducido número de pacientes disponibles en cualquier centro. Sin embargo, la heterogeneidad adicional así introducida puede superar los beneficios de mayores números en el análisis. Este problema estuvo bien ilustrado en el estudio Shiel 2001, en el que los dos centros, elegidos inicialmente por su semejanza en el servicio, resultaron tener diferencias críticas en los niveles de personal y, por consiguiente, en la intensidad de la rehabilitación habitual ofrecida. Lo anterior dio lugar a diferentes estancias hospitalarias que fueron suficientes para confundir este resultado crítico en el análisis estadístico.
Escala de tiempo e interpretación
Los efectos beneficiosos de la rehabilitación neurológica habitualmente se acumulan durante de varios años, en lugar de durante semanas o meses. Generalmente los ECA se realizan por un tiempo mucho más corto. Se deben financiar ECA definitivos en esta área para incluir un seguimiento de tres a cinco años. Lo anterior rara vez es posible con los programas existentes de financiamiento para ECA.
Medidas de resultado
Las medidas comunes (compartidas) son un prerrequisito necesario para la asimilación de los datos. Se han desarrollado varias evaluaciones de resultado global, como el Barthel Activities of Daily Living (ADL) Index y la Functional Independence Measure (FIM) con la intención de crear bases de datos comparables, y son ampliamente utilizadas. Desafortunadamente, estas medidas plantean problemas adicionales.
-
Homogeneidad: Las mismas medidas pueden ser menos homogéneas de lo que se suponía anteriormente. El análisis indica que incluso los instrumentos más consistentemente aplicados se comportan de otro modo en diferentes culturas y ámbitos (Tennant 2002), y actualmente se usan varias versiones diferentes del Barthel Index (Turner‐Stokes 1997).
-
Sensibilidad a los cambios previstos: La rehabilitación se proyecta cada vez más hacia objetivos específicos fijados para el paciente y su familia. Estos instrumentos globales abordan una variedad de dimensiones diferentes, muchas de las cuales pueden no cambiar en respuesta a dichos esfuerzos dirigidos. Por tanto, es poco probable que las puntuaciones generales reflejen los verdaderos efectos beneficiosos de la intervención. Powell 2002 intentó superar este problema al registrar solamente las dimensiones que demostraron logros máximos (máximo índice de logro). Lo anterior mejoró las diferencias estadísticas entre los brazos de tratamiento y control, pero se podría considerar que representa una manipulación excesiva de los datos, especialmente porque estas dimensiones seleccionadas no se identificaron como áreas objetivo antes de comenzar el tratamiento.
-
Interpretación: Semlyen 1998 ilustra un dilema para la interpretación de los datos. Los participantes que recibieron rehabilitación multidisciplinaria presentaban más discapacidad al inicio pero a los 12 meses lograron el mismo nivel de función (Barthel Index) que los otros grupos de rehabilitación. Este hecho se puede interpretar como un sesgo inverso para el brazo de tratamiento que, por lo tanto, demostró significativamente mayores logros durante la rehabilitación, a pesar de este punto de partida inferior. De manera alternativa, se puede alegar que este punto de partida inferior ofrece una ventaja estadística a fuerza de una mayor oportunidad para el cambio en una escala con efectos de techo reconocidos.
-
Efectos de techo: Los efectos de techo posibles de la FIM, que se utiliza habitualmente como una medida de resultado para la rehabilitación de las lesiones cerebrales, se observaron en Zhu 2007. Los mismos porcentajes de participantes del grupo de tratamiento y control al final alcanzaron la puntuación máxima de la FIM al año de la lesión. Sin embargo, el grupo de tratamiento alcanzó puntuaciones altas más rápidamente, con diferencias significativas detectables a los tres meses. No es posible determinar si el retorno más temprano a la independencia total les permitió a los pacientes extender sus horizontes más allá de las actividades cotidianas básicas, ya que el estudio no registró medidas de las actividades cotidianas ampliadas ni de la participación.
Los estudios incluidos en esta revisión utilizaron una variedad amplia de medidas para explorar la función psicosocial (p.ej. el Community Integration Questionnaire [CIQ], la Perceived Quality of Life Scale [PQOL], la Canadian Occupational Performance Measure [COPM], las escalas Brain Injury Community Rehabilitation Outcome (BICRO‐39)). Sin embargo, la falta de consenso sobre qué medidas utilizar impide el análisis de los datos agrupados.
Estas limitaciones en la medición de los resultados también subrayan la necesidad de obtener medidas más centradas en el paciente, como el alcance gradual de los logros obtenidos, para registrar si el programa de rehabilitación alcanzó los objetivos concebidos para ese individuo y destacar la necesidad del desarrollo adicional de medidas estandarizadas que registren los logros a diversos niveles de deficiencia, actividad y participación. Además, debido a la diversidad de las necesidades reales de rehabilitación, los resultados se deben interpretar según las necesidades de rehabilitación y según el grado en que se han cumplido estas necesidades. En los aproximadamente diez años en los que esta revisión ha estado activa, se han introducido mecanismos más complejos para captar las necesidades, las contribuciones y los resultados (Turner‐Stokes 2012), así como las necesidades no atendidas (Turner‐Stokes 2013). Éstos y otros desarrollos deben mejorar la posibilidad de evaluación de los resultados ajustados a la mezcla de casos de rehabilitación en el futuro, para guiar la interpretación de los resultados de los estudios.
Como en otras áreas complejas del ejercicio de la medicina, puede ser necesario desarrollar la base de pruebas para un tratamiento efectivo mediante la triangulación de una serie de diferentes métodos de investigación. En esta revisión se han incluido estudios controlados, siempre que cumplieran los criterios predeterminados. Se acepta que estos diseños de investigación estén abiertos a un cierto nivel de sesgo. Sin embargo, debido a los problemas observados anteriormente, los revisores aceptaron que en el contexto de la práctica clínica real, este nivel de "aleatoriedad" puede ser el más alcanzable en el contexto de la lesión cerebral grave. En el futuro, estos diseños experimentales deberán considerarse junto con las pruebas basadas en la práctica (Horn 2007) obtenidas de estudios de cohortes longitudinales sistemáticos grandes, realizados en el contexto de la práctica clínica habitual para abordar preguntas que no se pueden responder mediante ECA, como qué tratamientos funcionan mejor en qué pacientes a largo plazo y qué modelos de servicio presentan un valor acorde en el contexto de la atención de toda la vida (Turner‐Stokes 2008).

Study flow diagram. The numbers for identification, screening and eligibility are from updated searches in 2013, 2014 and 2015.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. Nineteen studies are included in this review.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Criterion | Score positive if: |
| Eligibility criteria specified | A list of inclusion/exclusion criteria was explicitly stated. |
| Method of randomisation | A random (unpredictable) assignment sequence was used. |
| Treatment allocation concealment | Assignment was concealed from investigators. Assignment was generated by an independent person not responsible for determining the eligibility of patients. This person has no information about individuals included in the trial and has no influence on the assignment sequence nor on the decision about eligibility of patients. |
| Similarity of baseline characteristics | Study groups were comparable at baseline for important prognostic parameters. To receive a 'yes', groups had to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of patients with neurological symptoms and value of main outcome measure(s). |
| Treatment and control interventions specifically described | Details are given of the programme, including disciplines involved and treatment duration. |
| Care provider blinded to the intervention | Treating team is blinded regarding the intervention (NB: rarely possible in this context). |
| Co‐interventions avoided or equal | Co‐interventions should be avoided in the trial design or similar between index and control. |
| Compliance | Compliance was measured and satisfactory in all study groups. |
| Participant blinded to the intervention | Participant was blinded regarding the intervention (NB: rarely possible in this context if consent procedures are properly applied). |
| Outcome assessor blinded to the intervention | Outcome assessor was blinded regarding treatment allocation, and standardised assessment measures were used to structure the interviews. Scored negative if only self reported (questionnaire) outcomes were used and no observer outcomes were provided. |
| Outcome measures relevant | Outcome measures reflected disability (activity) or participation as relevant to the intervention. |
| Adverse effects described | Any adverse effects of the intervention are described. |
| Withdrawal rate described and acceptable | Number of participants included in the study who did not complete the observation period or were not included in the analysis must be described and reasons given. If percentage of withdrawals and dropouts does not exceed 20% for immediate‐ and short‐term follow‐up or 30% for intermediate‐ and long‐term follow‐up, and does not lead to substantial bias, 'yes' is scored. |
| Short‐term outcome measurement | Outcomes were measured at the end of treatment (e.g. admission to discharge) or within 6 months of the end of treatment. |
| Long‐term outcome measurement | Outcomes were measured at 1 year or longer. |
| Timing of outcome assessment in both groups comparable | Timing of outcome assessment should be identical for all intervention groups and for all important outcome assessments. |
| Sample size described for each group | Number of participants was stated for each group. |
| Intention‐to‐treat analysis | All randomly assigned participants were included in the analysis (minus missing values), irrespective of non‐compliance and co‐interventions. If loss to follow‐up was substantial (≥ 20%), an intention‐to‐treat analysis as well as an alternative analysis that accounts for missing values (e.g. a worst‐case analysis) should have been performed. |
| Point estimates and measures of variability | A mean or median figure was given for each important outcome parameter, together with a measure of variability such as standard deviation, standard error of the mean or 95% confidence intervals. |
| Category of evidence | Criteria |
| Strong evidence | Consistent statistically significant findings in outcome measures in ≥ 2 high‐quality RCTs. |
| Moderate evidence | Consistent statistically significant findings in outcome measures in ≥ 1 high‐quality RCT and ≥ 1 controlled study. |
| Limited evidence | Consistent statistically significant findings in outcome measures in ≥ 1 high‐quality RCT, or |
| Indicative findings | Consistent statistically significant findings in process or outcome measures in ≥ 1 controlled studies. |
| No evidence | Conflicting results between trials or in cases of insufficient data. |
| Study ID | Internal validity | Descriptive criteria | Statistical criteria | Total score | Positive criteria |
| Kwakkel 1999 | 8 | 5 | 2 | 15 | a,bi,bii,c,d,f,g,j,l,mi,mii,n,o,p,q. |
| Wade 1997 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,f,g,i,j,l,mi,n,o,q. |
| Wade 1998 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,f,g,i,j,l,mi,n,o,q. |
| Powell 2002 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,f,g,i,j,l,mii,n,o,q. |
| Cicerone 2008 | 8 | 4 | 2 | 14 | a,bi,bii,c,d,g,i,j,l,mi,n,o,p,q |
| Smith 1982 | 7 | 5 | 2 | 14 | a,bi,c,d,f,g,i,j,l,mi,mii,n,o. |
| Salazar 2000 | 7 | 5 | 2 | 14 | a,bi,c,d,f,g,j,l,mi,mii,n,o,p,q. |
| Paniak 1998 | 6 | 5 | 2 | 13 | a,c,d,f,g,j,l,mi,mii,n,o,p,q. |
| Slade 2002 | 7 | 3 | 2 | 12 | a,bi,bii,c,d,f,g,j,l,mi,o,p,q |
| Shiel 2001 | 7 | 3 | 2 | 12 | a,bi,d,g,h,i,j,l,mi,o,q. |
| Zhu 2007 | 6 | 4 | 2 | 12 | a.bi,bii,c,d,i,j,l,mi,mii,n,o,p,q |
| Elgmark 2007 | 6 | 4 | 2 | 12 | a,bi,bii,c,d,i,j,l,mii,n,o,p,q |
| Bowen 2001 | 4 | 4 | 2 | 10 | a,c,d,f,j,l,mi,n,o,p,q. |
| Bjorkdahl 2006 | 5 | 3 | 2 | 10 | d,i,j,l,mi,mii,n,o,p,q |
| Bai 2012 | 5 | 3 | 1 | 9 | a,c,g,i,j,l,mi,n,o |
| Werner 1996 | 4 | 4 | 1 | 9 | a,bi,d,i,j,mi,mii,n,o. |
| Semlyen 1998 | 4 | 4 | 1 | 9 | a,d,f,g,j,l,mi,mii,n,o. |
| Andelic 2012 | 4 | 4 | 1 | 9 | a,c,d,g,j,l,mii,n,o |
| Ozdemir 2001 | 3 | 4 | 2 | 9 | a,c,d,f,g,j,mi,o,q. |
| Paniak 1998 and 2000 | Participant and group comparisons | Patients with TBI admitted to hospital (all severities); mean age 33 y Intervention: ‘treatment as needed’ (TAN) (n = 58) Control: single session (SS) of education and advice (n = 53) | |||
| Primary outcomes | Impairment: Problem Checklist (PCL) Participation: Community Integration Questionnaire (CIQ) Health status: Short‐Form 36 (SF‐36) Work status: socio‐economic status (SES) | ||||
| Assessment points | 3 to 4 months (n = 111) and 1 year (n = 105) | ||||
| Summary of results | Participation (CIQ) did not change significantly for either group Impairment (PCL) and health status (SF‐36): Repeated measures MANOVA showed significant effects for time in both groups, which were maintained at 1 year Results showed no significant group interaction or time by group for any of the primary outcomes at either time point | ||||
| Vocational status (SES) | Intervention Mean (SD) | Control Mean (SD) | Difference in mean | P value (MANOVA) | |
| Pre‐injury | 37.2 (18.7) | 34.3 (18.5) | 2.9 | N/S | |
| Baseline | 26.9 (20.7) | 23.2 (19.9) | 0.8 | N/S | |
| 3 to 4 mo | 32.5 (20.2) | 32.8 (19.7) | 0.3 | N/S | |
| 1 y | 34.8 (19.7) | 36.7 (21.0) | 1.9 | N/S | |
| Authors' conclusions |
Interventions appear to be equally effective | ||||
| Salazar 2000 | Participant and group comparisons | Active duty military personnel with moderate to severe TBI; mean age 25 y Intervention: 8‐week intensive in‐patient cognitive‐behavioural programme (n = 67) Control: limited home programme of weekly telephone support from psychiatric nurse (educational material, counselling and suggested home exercises) (n = 53) | |||
| Primary outcomes | Work status: return to work return to fitness for military duty | ||||
| Assessment points | 1 year | ||||
| Summary of results | No overall differences in outcomes between groups Post hoc analysis demonstrated significant group interaction (in favour of the intervention group) for ‘fitness for military duty’ at 1 year for the more severe subgroup, who were unconscious for > 1 h | ||||
| Vocational status at 1 y | Intervention % achieved | Control % achieved | Difference | P value (Fisher's exact) | |
| Return to work | 90% | 94% | 4% (‐5.14) | N/S | |
| Fit for military duty | 73% | 66% | 7% (‐10.24) | N/S | |
| Post hoc analysis of subgroup unconscious for > 1 h (n = 75) | |||||
|
| (n = 35) | (n = 40) | Difference | P value | |
| Fit for military duty | 80% | 58% | 22% | 0.05 | |
| Authors' conclusions | Overall benefit of in‐patient cognitive rehabilitation programme similar to that of limited home rehabilitation, although institutional therapy may be beneficial for selected patients with severe TBI | ||||
| Wade 1997 | Participant and group comparisons | All patients presenting to Accident and Emergency following TBI; age 16 to 65 y Intervention: telephone follow‐up at 7 to 10 days with advice and referral as required (n = 252) Control: no specific intervention (standard services only) (n = 226) (NB: Despite major efforts to trace and contact patients, follow‐up interview at 6 months could be achieved in only 478 of 1156 (41%) participants randomly assigned) | |||
| Primary outcomes | Social disability: Rivermead Head Injury Follow‐Up Questionnaire (RFUQ) Symptoms: Rivermead Post‐concussion Symptoms Questionnaire (RPQ) | ||||
| Assessment points | 6 months | ||||
| Summary of results | No overall differences between intervention and control groups Post hoc analysis revealed significant group interaction (in favour of the active intervention group) with respect to social disability in a subgroup of individuals with more severe injury (>1 h PTA) | ||||
| Health status at 6 mo | Intervention Mean (SD) | Control Mean (SD) | P value (Mann‐Whitney) | ||
| RFUQ | 3.6 (6.0) | 3.3 (6.3) | N/S | ||
| RPQ | 7.7 (10.9) | 6.8 (10.0) | N/S | ||
| Post hoc analysis of subgroup with PTA > 1 h (n = 121) | |||||
| (n = 71) | (n = 53) | ||||
| RFUQ | 0.85 (0.89) | 1.17 (1.07) | 0.003 | ||
| RPQ | 2.03 (0.85) | 2.21 (0.89) | N/S | ||
| Authors' conclusions | Routine follow‐up does not appear to be necessary for all patients presenting with head injury, but a subgroup of patients with more severe TBI may benefit from such intervention | ||||
| Wade 1998 | Participant and group comparisons | All patients admitted to hospital following TBI (i.e. a more severe group than the total group reported in Wade 1997); age 16 to 65 y Intervention: telephone follow‐up at 7 to 10 days with advice and referral as required (n = 132) Control: no specific intervention (standard services only) (n = 86) (NB: follow‐up data obtained in 218 (69%) of 314 participants randomly assigned) | |||
| Primary outcomes | Social disability: Rivermead Head Injury Follow‐Up Questionnaire (RFUQ) Symptoms: Rivermead Post‐concussion Symptoms Questionnaire (RPQ) | ||||
| Assessment points | 6 months | ||||
| Summary of results | Significant group interaction (in favour of the active intervention group) with respect to social disability and post‐concussion symptoms. Subgroup analysis demonstrated that the main benefit appeared in the group with PTA < 7 days | ||||
| Health status at 6 mo | Intervention Mean (SD) | Control Mean (SD) | P value (Mann‐Whitney U test) | ||
| RFUQ | 5.36 (7.81) | 8.23 (8.75) | 0.01 | ||
| RPQ | 9.8 (11.7) | 13.9 (13.6) | 0.02 | ||
| Authors’ conclusions | Early intervention by a specialist service significantly reduced social morbidity and severity of post‐concussion symptoms 6 months after head injury, in the group of patients who required admission to hospital. Possibly most beneficial for the moderate to severe group, some of whom may not present without pro‐active intervention | ||||
| Elgmark 2007 | Participant and group comparisons | All patients aged 16 to 60 with mild traumatic brain injury according to American Congress of Rehabilitation medicine criteria Intervention: follow‐up at 2 to 8 weeks by telephone or letter with advice and referral as required (n = 264 ‐ 96 received intervention; 150 declined); 18 lost to follow‐up Control: no specific intervention (regular care) (n = 131); 22 lost to follow‐up 246 treatment and 109 control included in intention‐to‐treat analysis | |||
| Primary outcomes | Symptoms: change in post‐concussion symptoms ‐ Swedish Post‐concussion Symptoms Questionnaire (PCSQ) Social disability: Community Integration Questionnaire (CIQ), Life Satisfaction Questionnaire, Short‐Form Health Survey (SF‐36) | ||||
| Assessment points | 1 y post injury | ||||
| Summary of results | No statistically significant differences were found between intervention and control groups. Participants who experienced few PCS 2 to 8 weeks post injury declined rehabilitation and returned to work. Those who suffered several PCS and accepted rehabilitation did not recover after 1 y | ||||
| Health status at 6 mo | Intervention Mean (SD) | Control Mean (SD) | Significance
| ||
| Total PCSQ | 5.2 (5.3) | 4.4 (5.3) | N/S | ||
| CIQ | 20.3 (4.0) | 19.8 (4.0) | 0.02 | ||
| Authors’ conclusions | In this particular study of MTBI, active rehabilitation did not change outcomes to a significant degree. Additional studies should focus on patients who remain symptomatic during the first 1 to 3 months and should test various types of interventions | ||||
| PTA = post‐traumatic amnesia; TBI = traumatic brain injury. | |||||
| Smith 1981 | Participant and group comparisons | Patients suitable for out‐patient rehabilitation following discharge from hospital after acute stroke (n = 133); mean age 63 y Intervention: out‐patient physiotherapy and occupational therapy for 6 months at 2 levels of intensity:
Control: no routine rehabilitation, health visitor encourages home exercises as learned in hospital (n = 44) | |||
| Primary outcomes | Dependency for ADL: Northwick Park ADL score | ||||
| Assessment points | 3 and 12 months | ||||
| Summary of results | Significantly greater decrease in ADL scores in intNervention groups compared with controls at 3 months. Difference is sustained at 1 y follow‐up with greater number of control group participants (NB: trend towards better results from intensive rehabilitation than from conventional regimen not tested statistically) | ||||
| Decrease in ADL score | Intensive rehabilitation | Conventional rehabilitation | Control | P value | |
| Mean change 0 to 3 m | 3.54 (n = 41) | 2.87 (n = 40) | 1.50 (n = 42) | 1 vs 3: P value < 0.01 1/2 vs 3: P value < 0.01 | |
| Mean change 0 to 12 m | 3.50 (n = 36) | 2.89 (n = 36) | 0.60 (n = 35) | 1 vs 3: P value < 0.05 | |
| Authors’ conclusions | Out‐patient rehabilitation following stroke appears to be effective. Decreasing intensity of rehabilitation was associated with an increase in both the proportion of participants who deteriorated and the extent to which they deteriorated | ||||
| Werner 1996 | Participant and group comparisons | Patients discharged from in‐patient rehabilitation and ≥ 1 y (mean 2.9 y) after stroke (n = 49); mean age 63 y Intervention: out‐patient physiotherapy and occupational therapy (2 hours, 4 times per week, for 3 months) (n = 33) Control: no specific intervention (n = 16) (NB: 28% (5/33 intervention group and 9/16 control group) did not complete follow‐up: 5 non‐randomised controls were subsequently recruited to make control numbers up to 12) | |||
| Primary outcomes | Activity: Functional Independence Measure ‐ Motor (FIM‐MM) Limitation of participation: Sickness Impact Profile (SIP) Depression: Beck Depression Inventory (BDI) | ||||
| Assessment points | 3 and 9 months | ||||
| Summary of results | Significant changes in FIM and SIP at 3 months maintained at 9 months. Trend towards improved mood did not reach significance | ||||
| Mean change in score | Intervention (n = 28) | Control (n = 12) | Difference in mean | P value (t‐tests) | |
| FIM‐MM (0 to 3 mo) | 6.6 | 1.5 | 5.1 | 0.03 | |
| FIM‐MM (3 to 9 mo) | 0.7 | ‐1.0 | 1.7 | N/S | |
| SIP (0 to 3 mo) | ‐5.2 | 2.6 | 7.8 | 0.04 | |
| BDI (0 to 3 mo) | ‐2.6 | 0.2 | 2.8 | N/S | |
| BDI (3 to 9 mo) | 0.7 | 0.5 | 0.2 | N/S | |
| Authors’ conclusions | Significant gains can still be attained in the post‐acute stroke survivor, despite prior in‐patient rehabilitation services | ||||
| ADLs = activities of daily living. | |||||
| Powell 2002 | Participant and group comparisons | Patients (16 to 65 y) with severe traumatic brain injury 3 mo to 20 y previously (n = 110 allocated: 94 (85%) completed follow‐up) Intervention: inter‐disciplinary team interventions: 2 sessions per week for mean 27.3 (SD 19.1) weeks in community settings (home, work or day centres) (n = 48) Control: written information only (n = 46) | |||
| Primary outcomes | Activity: Barthel Index (BI) Participation: Brain Injury Community Rehabilitation Outcome (BICRO‐39) | ||||
| Assessment points | Approximately 2 y (median 23 mo) (IQR 18 to 40) | ||||
| Summary of results | Intervention group made significantly greater gains on both BI and BICRO scales. Median changes were small, reflecting the diversity of the population, but 40% of intervention group and only 20% of controls made a clinically significant improvement of 2+ points on ≥ 1 BICRO subscale | ||||
| Change scores from baseline | Intervention | Control | P value | ||
| BI: % improving Median (IQR) change | 35.4% 0 (‐5, 5) | 19.6% 0 (‐5, 4) | < 0.05 | ||
| BICRO‐39: % Median (IQR) change | 80% 2.5 (‐1.7, 6.2) | 70% 0.9 (‐4.1, 6.8) | < 0.05 | ||
| Authors’ conclusions | Multi‐disciplinary community rehabilitation, even years after injury, can make clinically significant gains which outlive the active treatment period. | ||||
| Bowen 2001 | Participant and group comparisons | Carers of young adult (16 to 65 y) TBI survivors with hospital stay ≥ 3 days (n = 96) Intervention: active intervention from Head Injury Neurorehabilitation Team (HINT)
Control: no specific intervention ‐ existing services only (n = 27) (NB: 20/96 (21%) received service other than that allocated ‐ only 56% allocated to early intervention actually received it) | |||
| Primary outcomes | Information received: carer perceptions of how well informed they are ‐ 7 questions Emotional state: Wimbledon Self‐report Scale (WSS) | ||||
| Assessment points | 6 mo post injury | ||||
| Summary of results | Analyses adjusted for potential confounding factors confirmed a clinically plausible superior outcome for both treatment groups compared with controls, but none of the results reached significance (set at P value < 0.01) | ||||
| Mean change from baseline | Early (n = 41) | Late (n = 28) | Control (n = 27) | P value (t‐tests) | |
| % poorly informed | 46%‐64% | 46%‐81% | 63%‐89% | N/S | |
| WSS, median (IQR) | 3 (0‐9) | 2 (0‐6) | 8 (1‐15) | N/S | |
| Authors' conclusions | Hypothesis not confirmed, but absence of effect cannot be proven with these data, which may reflect type II error in view of mixing of groups. Longer‐term follow‐up data also required | ||||
| Bjorkdahl 2006 | Participant and group comparisons | Stroke patients (mean age 53 y) discharged from an in‐patient rehabilitation programme
| |||
| Primary outcomes | Functional assessment: Motor and Process Skills (AMPS); secondary measures: mobility (30 m walking test); FIM, instrumental activity measure Impairment: NIH scale | ||||
| Assessment points | End of intervention (3 wk post discharge), 3 and 12 mo | ||||
| Summary of results | Both groups improved significantly from discharge to 1‐y follow‐up. No significant differences between groups for any of the 4 assessments, at any time point, although trends show earlier gains in the home‐rehabilitation group. Only the day clinic group changed ‘significantly’ on the FIM, but degree of change was small (5 FIM points over 1 y). Costs of home rehabilitation programme were less than half those of the day clinic | ||||
| Rasch transformed AMPS data (logits) | Home (n = 30) Mean (SD) | Day clinic (n = 39) Mean (SD) | |||
| Motor | Process | Motor | Process | ||
| Discharge 3 wk 3 mo 1 y | 1.45 1.71 2.02 2.18 | 1.00 1.26 1.23 1.55 | 1.42 1.52 1.88 2.28 | 1.18 1.37 1.54 1.59 | |
| Authors’ conclusions | Both rehabilitation programmes could be recommended, but additional studies are required to define patients who may benefit specifically from home rehabilitation. Costs should be taken into consideration | ||||
| Semlyen 1998 | Participant and group comparisons | Consecutive patients in‐hospital with severe TBI and referred for in‐patient rehabilitation within 4 weeks of injury; age 16 to 62 y Intervention: multi‐disciplinary specialist rehabilitation service ‐ Hunter’s Moor (HM) (n = 33) Control: ‘Other rehabilitation’ (OR) in local non‐specialist services in district hospitals (n = 18) | ||
| Primary outcomes | Activity and independence: Barthel Index, FIM and Newcastle Independence Assessment Form (NIAF) Care‐givers' Health: GHQ‐28 | |||
| Assessment points | 1, 2, 3, 6, 12 and 24 mo after injury | |||
| Summary of results | Only Z values (BI) and t‐values (FIM and NIAF) are given HM intervention group was significantly more disabled at outset (as indicated by FIM up to 3 mo, BI up to 6 mo and NIAF up to 12 mo). By 12 mo, therefore, the HM group had caught up with the OR group in level of activity OR group made significant gains only up to 12 wk on NIAF and FIM cognitive scales, but none on the FIM motor or BI (already at ceiling). By contrast, HM continued to make significant gains up to 24 mo, as assessed by NIAF and BI Significant improvements in carer distress for the HM group were sustained at 2 y, whereas the OR group showed evidence of deterioration between 6 and 12 mo No differences in length of stay between groups | |||
| Authors’ conclusions | Results support the efficiency of specialist rehabilitation services in achieving lasting gains for patients with more severe disability over similar lengths of stay | |||
| Ozedemir 2001 | Participant and group comparisons | Stroke patients referred for rehabilitation after medical stabilisation (n = 60); mean age 59.1 y (SD 5.9) Group 1: in‐patient rehabilitation (n = 30) ‐ ≥ 2 h/d of formal therapy, 5 d/wk Group 2: home‐based rehabilitation (n = 30) ‐ team visited home for 2 h/wk and instructed family in home exercises ‐ family provided therapy ≥ 2 h/d, 7 d/wk Mean duration of rehabilitation 64 d in both groups | ||
| Primary outcomes | Impairment: Brunnstrom score, Ashworth (spasticity) Activity: FIM, Mini‐Mental State Examination (MMSE) | |||
| Assessment points | Before and after rehabilitation | |||
| Summary of results | Significant group differences in favour of in‐patient group for change in Brunnstrom, FIM and MMSE scores, but no differences in spasticity | |||
| Change scores | Group 1 Mean (SD) | Group 2 Mean (SD) | P value (t‐tests) | |
| Ashworth UE | 0.5 (1.2) | 0.2 (0.5) | N/S | |
| Ashworth LE | 0.2 (1.2) | 0.1 (0.3) | N/S | |
| Brunnstrom (UE) | 2.0 (1.2) | 0.3 (0.6) | < 0.001 | |
| Brunnstrom (LE) | 2.4 (1.2) | 0.8 (0.6) | < 0.001 | |
| FIM | 59.6 (14.2) | 12.3 (13.4) | < 0.001 | |
| MMSE | 4.8 (5.0) | 2.0 (2.1) | < 0.001 | |
| Authors' conclusions | Intensive in‐patient rehabilitation provided significantly more favourable functional and cognitive outcomes than home‐based rehabilitation programme | |||
| Kwakkel 1999 | Participant and | Stroke patients within 2 wk of onset (n = 101) All groups received 15 min arm training plus 15 min leg training daily, plus 1.5 h ADL training per wk In addition, for 30 min 5 d/wk, groups received: Group 1: intensive arm training (n = 33) Group 2: intensive leg training (n = 31) Group 3 (control): inflatable splint (n = 37) | |||
| Primary outcomes | ADL ability: Barthel Index (BI) Walking ability: functional ambulation categories (FAC) Dexterity: Action Research Arm Test (AR Arm Test) | ||||
| Assessment points | 0, 6, 12, 20, 26, 38, 52 wk | ||||
| Median (IQR) at 20 wk | Arm training | Leg training | Control | P value (K‐W test) | |
| BI | 17 (14‐20) | 19 (16‐20) | 16 (10‐19) | < 0.05 | |
| FAC | 4 (3‐5) | 4 (3‐5) | 3 (1‐4) | < 0.05 | |
| AR Arm Test | 9 (0‐39) | 2 (0‐56) | 0 (0‐2) | < 0.01 | |
| Authors’ conclusions | Greater intensity of leg training improves early functional recovery; whereas greater intensity of arm training improves only dexterity, providing further evidence that therapy primarily induces effects on abilities at which training is specifically aimed. Functional gains maintained up to 1 y | ||||
| Zhu 2001
| Participant and | Patients aged 12 to 65 y with moderate to severe TBI up to 6 mo post injury (n = 68) Interventions: multi‐disciplinary rehabilitation at 2 intensities:
| |||
| Primary outcomes | Global outcome: Glasgow Outcome Scale (GOS) Activity (disability): FIM, Neurobehavioural Cognitive Status Examination (NCSE) | ||||
| Assessment points | 0, 1, 2, 3, 4, 5, 8, 10 and 12 mo | ||||
| Summary of results | No statistically significant differences in FIM or NSCE between groups. However, significantly greater number of participants achieved maximal FIM and GOS scores within 3 mo, although no differences were noted at later time points and up to 1 year | ||||
| Outcome | Intensive (n = 36) | Conventional (n = 32) | P value (Chi2) | ||
| % good GOS 3 mo | 38
| 14
| Chi2 3.9, df 1, P value = 0.044 P value = 0.483 | ||
| % full FIM 3 mo | 47
| 19
| Chi2 5.8, df 1, P value = 0.015 P value = 0.242 | ||
| Authors’ conclusions | Early intensive rehabilitation can improve functional outcomes of patients with TBI in the early months post injury, and hence may increase the chance of their early return to work Intensive rehabilitation in this study speeded up recovery rather than changing final outcomes | ||||
| Shiel 2001
| Participant and | Patients with moderate to severe TBI (age 16 to 70 y) admitted for rehabilitation (n = 51); stratified and randomly assigned on age and GCS Intervention groups
(NB: study conducted across 2 centres, which had very different structures and processes, 1 offering significantly more routine therapy than the other. Participants at each centre were randomly assigned to received standard and enhanced therapy according to their practice | |||
| Primary outcomes | Activity (disability): FIM+FAM | ||||
| Assessment points | Admission and discharge | ||||
| Summary of results | Despite procedural differences between centres, no significant differences in FIM+FAM change scores were reported between centres. Significant differences were observed between intensive and routine intervention groups and were greatest in the domains of self care, continence, locomotion and psychosocial function. No significant difference in length of stay overall, but possibly skewed by very prolonged LOS for intervention group at 1 centre | ||||
| Change scores during admission | Enhanced intensity Median (IQR)
| Routine Median (IQR) | P (Mann‐Whitney) | ||
| FIM+FAM Motor | 74 (47‐95)
| 21 (2‐48) | < 0.01 | ||
| FIM+FAM Cognitive | 40 (14‐45)
| 12 (5‐22) | < 0.01 | ||
| Authors’ conclusions | Increased intensity of rehabilitation is associated with enhanced function recovery | ||||
| Slade 2001
| Participant and | Patients with acquired brain injury (stroke, TBI or MS) aged 16 to 65 y admitted for rehabilitation (n = 131) Interventions: multi‐disciplinary rehabilitation at 2 intensities:
(NB: Although in theory the intensive group should have received 67% more therapy than controls, in reality, they received only 30% more) | |||
| Primary outcomes | Length of stay (LOS) ADL ability: Modified Barthel Index | ||||
| Assessment points | Admission and discharge | ||||
| Summary of results | No significant differences in discharge Barthel scores were reported (data not given), but this is expected, as patients are discharged at the point at which they are sufficiently independent to manage in the community. This question is then whether more intensive therapy reaches that point earlier Mean LOS for all participants was 84.6 d. Straightforward comparison showed no significant group interactions However, a multiple regression model was applied to take account of confounders of experimental design that could not be controlled for (impairment mix, community delays, missed treatment, etc.); this demonstrated a 14‐d reduction for the intensive group | ||||
| Authors’ conclusions | Intensive rehabilitation has the potential to reduce length of stay, but concurrently, LOS in both groups was increased by 16 d as the result of external delays in discharge | ||||
| Andelic 2012 | Participant and group comparisons | Patients with severe TBI; mean age 29.4 y Intervention:continuous chain of rehabilitation from specialist on ITU directly into specialist subacute rehabilitation post discharge from ITU (n = 33). | ||
| Primary outcomes | Disability: Glasgow Outcome Scale Extended (GOSE) | |||
| Secondary outcomes | Disability: Disability Rating Score (DRS) Employment status: return to work Living situation: at home with or without care, or in a nursing home | |||
| Assessment points | 12 months post injury (n = 61) | |||
| Summary of results | Disability (GOSE) at 12 mo significantly less in the early rehabilitation group than in the control group Significantly higher percentage of participants in the early rehabilitation group were living at home when compared with controls Non‐significant trend towards higher rate of return to work in the early rehabilitation group than in the control group Non‐significant trend towards shorter overall length of stay (acute hospital and rehabilitation unit) in the early rehabilitation group | |||
| Outcomes | Intervention | Control | P value | |
| Favourable GOSE (6‐8) | 71% | 37% | 0.007 | |
| % living at home | 81 | 53 | 0.06 | |
| Authors' conclusions | Early comprehensive rehabilitation in a continuous chain leads to better functional outcomes at 12 months post injury among patients with severe TBI | |||
| Bai 2012 | Participant and group comparisons | Patients with moderate to severe intracerebral haemorrhage; mean age 61 y Intervention: early rehabilitation commencing in the Emergency Department and continuing for 6 mo (n = 181) Controls: standard medical care (n = 183) | ||
| Primary outcomes | Impairment: Fugl‐Meyer Assessment (FMA) Disability: Modified Barthel Index (MBI) | |||
| Assessment points | Outcome measures administered at 1, 3 and 6 mo | |||
| Summary of results | At baseline, post hoc testing showed no significant differences between FMA and MBI scores in the 2 groups At 1, 3 and 6 mo, intervention group had significantly higher FMA and MBI scores | |||
| Authors' conclusions | Early rehabilitation can significantly improve ADLs and motor recovery in patients with intracranial haemorrhage | |||
| Cicerone 2008 | Participant and group comparisons | Mixed severity traumatic brain injury; mean age 36.6 y Intervention: intensive cognitive rehabilitation provided in a therapeutic environment (n = 34) with a focus on group work Control: standard neurorehabilitation; mostly individual, discipline‐specific therapy (n = 34) | |||
| Primary outcomes | Community integration: Community Integration Questionnaire (CIQ) Life satisfaction: Perceived Quality of Life Scale (PQOL) | ||||
| Secondary outcomes | Neuropsychological functioning Perceived self‐efficacy Vocational outcome: Vocational Integration Scale (VIS) | ||||
| Assessment points | 2 wk before treatment, 2 wk post treatment and 6 mo follow‐up | ||||
| Summary of results | Treatment arm showed significantly improved community integration and quality of life scores ‐ not seen in control arm Self efficacy was significantly improved in the treatment arm – another improvement not seen in the control arm Additionally, treatment group had a significantly higher rate of employment compared with control group | ||||
| Standard neurorehabilitation | |||||
| Outcome measures | Pre‐Tx | Post‐Tx | Follow‐up | P value | |
| CIQ | 12.1 | 11.7 | 12.9 | > 0.05 | |
| PQOL | 61.2 | 62.2 | 59.6 | > 0.05 | |
| Authors' conclusions | This trial demonstrates that an intensive cognitive rehabilitation programme can produce significantly better outcomes when compared with standard neurorehabilitation | ||||
| Salazar 2000 | Participant and group comparisons | Active duty military personnel with moderate to severe TBI; mean age 25 y Intervention: 8‐week intensive in‐patient cognitive‐behavioural programme (n = 67) Control: limited home programme of weekly telephone support from psychiatric nurse (educational material, counselling and suggested home exercises) (n = 53) | |||
| Primary outcomes | Work status: return to work return to fitness for military duty | ||||
| Assessment points | 1 y | ||||
| Summary of results | No overall differences in outcomes between groups Post hoc analysis demonstrated significant group interaction (in favour of the intervention group) for ‘fitness for military duty’ at 1 y for members of the more severe subgroup, who were unconscious for >1 h | ||||
| Vocational status at 1 y | Intervention % achieved | Control % achieved | Difference | P value (Fisher's exact) | |
| Return to work | 90% | 94% | 4% (‐5,14) | N/S | |
| Fit for military duty | 73% | 66% | 7% (‐10.24) | N/S | |
| Post hoc analysis of subgroup unconscious for > 1 h (n = 75) | |||||
| (n = 35) | (n = 40) | Difference | P value | ||
| Fit for military duty | 80% | 58% | 22% | 0.05 | |
| Authors' conclusions | Overall benefit of in‐patient cognitive rehabilitation programme similar to that of limited home rehabilitation, although institutional therapy may be beneficial for selected patients with more severe TBI | ||||

