Noninvasive positive pressure ventilation as a weaning strategy for intubated adults with respiratory failure
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Pseudo‐randomized | |
| Participants | Patients admitted with an acute exacerbation of COPD. Patients were invasively ventilated through a nasotracheal tube for 48 to 60 hours | |
| Interventions | Patients were randomized by alternating day of the month to receive either noninvasive ventilation in PS mode or to continued weaning with invasive PS. PS and PEEP were gradually decreased to facilitate liberation from mechanical support. Ventilation was discontinued after completion of a 3 hour SBT and meeting discontinuation criteria. | |
| Outcomes | 1. Mortality | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment | Unclear risk | D ‐ Not used |
| Methods | RCT 2 centres | |
| Participants | Patients with ARF and persistent weaning failure requiring MV for at least 72 hours and failing a two hour T‐piece trial on three consecutive days. Patients were identified by daily screening. | |
| Interventions | Patients were randomized to bilevel positive airway pressure in ST mode or invasive weaning with AC or PS. Daily T‐piece trials were conducted until extubation in the IPPV group. Periods of SB of increasing duration were used to wean NPPV. IPPV was discontinued after successful completion of a two hour SBT. | |
| Outcomes | 1. ICU mortality, | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment | Low risk | A ‐ Adequate |
| Methods | RCT | |
| Participants | Patients with acute on chronic respiratory failure (COPD, restrictive, mixed) failing a two hour T‐piece trial after invasive mechanical ventilation for at least 48 hours. Patients were identified using daily screening. | |
| Interventions | Participants were randomized to receive invasive pressure support or NPPV delivered in flow or pressure mode. NPPV was delivered intermittently following extubation, separated by periods of SB of increasing duration. Invasive PS was titrated by 3 to 5 cm H2O according to tolerance. Discontinuation of support followed successful completion of two periods of observation during SB (NPPV) or during PS weaning with optional SBTs (IPPV). Extubation was performed when PS was less than 8 cm H2O in the IPPV group. | |
| Outcomes | 1. 90 day mortality | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment | Low risk | A ‐ Adequate |
| Methods | RCT (abstract) | |
| Participants | Patients with acute respiratory failure admitted to a medical intensive care unit and failing a 30 minute T‐piece trial were eligible. Patients were identified using daily screening. | |
| Interventions | Patients were randomized to receive VPAP using PS, delivered in ST mode, or invasive PS. In both arms mechanical support was titrated to RR and tidal volume. Whereas T‐piece trials were permitted to discontinue IPPV support in the IPPV group, at least one period of SB of gradually increasing duration per day was permitted between NPPV trials in the NPPV group. | |
| Outcomes | 1. Mortality | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment | Low risk | A ‐ Adequate |
| Methods | RCT 3 centres | |
| Participants | Patients admitted with an acute exacerbation of COPD requiring intubation and MV for at least 36 to 48 hours. Relapse was defined by pH less than 7.33, PaO2 less than 45 mm Hg, severe dyspnoea in the absence of pneumonia or 1 of 11 non‐operative diagnoses. Patients who met permissive criteria and failed a one hour T‐piece trial were eligible for inclusion. | |
| Interventions | Patients were intubated, sedated and paralysed for the first 6 to 8 hours. Those failing a one hour T‐piece trial were randomized to weaning with either NPPV or IPPV. NPPV was delivered continuously with at least two periods of SB per day of increasing duration. PS was decreased by 2 to 4 cm H2O/d in the NPPV group. In the IPPV group, PS was titrated to a RR of less than 25 b/min and twice daily SBT were permitted. Discontinuation occurred after successful completion of a three hr period of SB (NPPV) or SBT (IPPV) and when discontinuation criteria were met. | |
| Outcomes | 1. 60 day mortality 2. Incidence of VAP 3. Successful weaning at 60 days 4. Total duration of MV 5. ICU LOS 6. Adverse events 7. Tracheostomy | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment | Low risk | A ‐ Adequate |
RCT; randomized controlled trial, COPD; chronic obstructive pulmonary disease, b/min; breaths per minute, PaO2; arterial partial pressure of oxygen, PaCO2; arterial partial pressure of carbon dioxide, RR; respiratory rate, ARF; acute respiratory failure, MV; mechanical ventilation, AC; assist control, PS; pressure support, PEEP; positive end‐expiratory pressure, NPPV; noninvasive positive pressure ventilation, IPPV; invasive positive pressure ventilation, VPAP; ventilator (delivered) positive airway pressure, SB, spontaneous breathing, SBT; spontaneous breathing trial, ST; spontaneous timed, LOS; length of stay, VAP; ventilator associated pneumonia, ETMV; endotracheal mechanical ventilation, ICU; intensive care unit.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This non randomized study assessed the role of BIPAP in the management of respiratory failure following cardiovascular surgery. Twenty patients who required respiratory support for greater than 72 hours were studied. BiPAP (n=8) was compared to unassisted, oxygen treatment (n=12) in the control group. Outcomes reported included the respiratory index, alveolar arterial oxygen difference and shunt fraction. This study was excluded as it was not a RCT. In addition, NPPV was not used to facilitate weaning and physiologic end points alone were reported. | |
| This RCT evaluated early application of NPPV on extubation outcome in 93 patients following elective (n=56) or unplanned (n=37) extubation. Following extubation patients were randomly assigned to receive either NPPV or oxygen therapy. This study did not assess the role of NPPV as a weaning modality. | |
| This RCT evaluated 572 patients who underwent median sternotomy and hypothermic cardiac arrest for cardiopulmonary bypass. Participants were randomized to receive either BiPAP (n=280) or SIMV with PS (n=292). Outcomes reported included the duration of intubation (reported in hours), proportion of patients extubated within six hours, requirement for post operative analgesia and reintubation rate. This study did not assess the role of NPPV as a weaning strategy in postoperative patients with respiratory failure. | |
| This RCT evaluated 32 patients with COPD requiring intubation for hypercapneic respiratory failure. Participants were randomized to receive either BiPAP (n=19) or conventional therapy (n=13). Outcomes reported included gas exchange at 45 minutes and 12 hours following extubation and rates of reintubation. This study did not assess the role of NPPV as a weaning strategy. | |
| This was a prospective, randomized study in which patients received either BIPAP or PS following aortocoronary bypass surgery in the early postoperative period (7 plus or minus 1 h). Criteria for eligibility included an awake patient with neuromuscular activity. The population studied represent a cohort of patients in the post‐acute care setting that did not require formal weaning. | |
| This prospective RCT allocated patients requiring MV for greater than 72 hours to receive either NPPV or supplemental oxygen, by mask, after achieving criteria for extubation. The proportion of successful extubations, length of ICU stay and hospital mortality were reported. This study did not assess the role of NPPV as a weaning strategy as the comparative group received unassisted oxygen alone. |
BiPAP; Bilevel positive airway pressure, RCT; randomized controlled trial, NPPV; noninvasive positive pressure ventilation, SIMV; synchronized intermittent mandatory ventilation, PS; pressure support, ARF; acute respiratory failure, ICU; intensive care unit, COPD; chronic obstructive pulmonary disease, MV; mechanical ventilation.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Prospective multicenter randomized study of noninvasive ventilation for weaning from mechanical ventilation in acute on chronic respiratory failure |
| Methods | |
| Participants | 17 MICUs in Europe. Inclusion criteria: Exclusion criteria: |
| Interventions | Randomization between three strategies after failure of a T‐piece weaning trial. |
| Outcomes | 1. 28 day mortality |
| Starting date | October 2002 |
| Contact information | Christope Girault, Service Reanimation Medicale, |
| Notes |
MV, mechanical ventilation; GCS, Glasgow Coma Scale; PaO2/FiO2, ratio of arterial partial pressure of oxygen to fractional concentration of inspired oxygen; PEEP, positive end‐expiratory pressure; SBT, spontaneous breathing trial; PS, pressure support; NPPV, noninvasive positive pressure ventilation; VAP, ventilator associated pneumonia; ICU, intensive care unit; LOS, length of stay.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 mortality Show forest plot | 5 | 171 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.22, 0.76] |
| Analysis 1.1  Comparison 1 noninvasive versus invasive weaning, Outcome 1 mortality. | ||||
| 1.1 COPD | 2 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.07, 0.91] |
| 1.2 mixed | 3 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.23, 0.96] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 weaning failure Show forest plot | 3 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.29, 2.32] |
| Analysis 2.1  Comparison 2 noninvasive versus invasive weaning, Outcome 1 weaning failure. | ||||
| 1.1 COPD | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.11, 1.25] |
| 1.2 mixed | 2 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.45, 3.60] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 nosocomial pneumonia Show forest plot | 4 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.09, 0.85] |
| Analysis 3.1  Comparison 3 noninvasive versus invasive weaning, Outcome 1 nosocomial pneumonia. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 LOS ICU Show forest plot | 3 | 126 | Mean Difference (IV, Random, 95% CI) | ‐6.88 [‐12.60, ‐1.15] |
| Analysis 4.1  Comparison 4 noninvasive versus invasive weaning, Outcome 1 LOS ICU. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 LOS hospital Show forest plot | 3 | 100 | Mean Difference (IV, Random, 95% CI) | ‐7.33 [‐14.05, ‐0.61] |
| Analysis 5.1  Comparison 5 noninvasive versus invasive weaning, Outcome 1 LOS hospital. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 average total duration of mechanical ventilatory support Show forest plot | 2 | 93 | Mean Difference (IV, Random, 95% CI) | ‐7.33 [‐11.45, ‐3.22] |
| Analysis 6.1  Comparison 6 noninvasive versus invasive weaning, Outcome 1 average total duration of mechanical ventilatory support. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 average duration of ventilation related to weaning Show forest plot | 3 | 92 | Mean Difference (IV, Random, 95% CI) | ‐2.72 [‐15.58, 10.14] |
| Analysis 7.1  Comparison 7 noninvasive versus invasive weaning, Outcome 1 average duration of ventilation related to weaning. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 duration of endotracheal mechanical ventilation Show forest plot | 3 | 97 | Mean Difference (IV, Random, 95% CI) | ‐6.32 [‐12.12, ‐0.52] |
| Analysis 8.1  Comparison 8 noninvasive versus invasive weaning, Outcome 1 duration of endotracheal mechanical ventilation. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
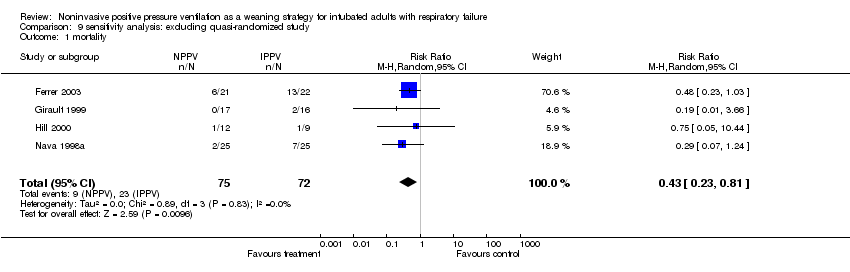
| 1 mortality Show forest plot | 4 | 147 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.23, 0.81] |
| Analysis 9.1  Comparison 9 sensitivity analysis: excluding quasi‐randomized study, Outcome 1 mortality. | ||||
| 2 nosocomial pneumonia Show forest plot | 3 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.15, 0.93] |
| Analysis 9.2  Comparison 9 sensitivity analysis: excluding quasi‐randomized study, Outcome 2 nosocomial pneumonia. | ||||
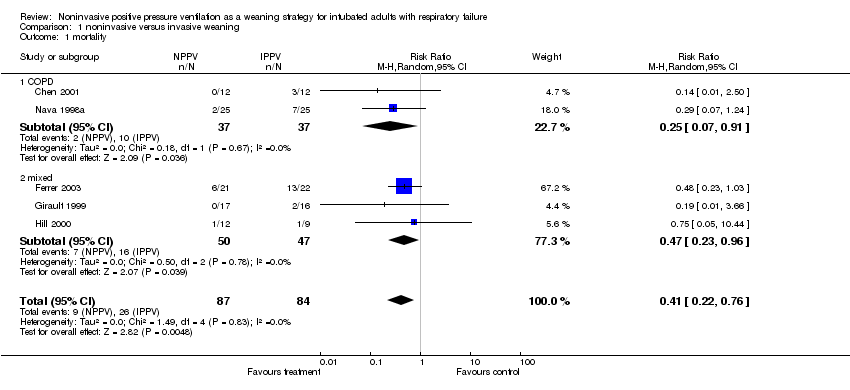
Comparison 1 noninvasive versus invasive weaning, Outcome 1 mortality.

Comparison 2 noninvasive versus invasive weaning, Outcome 1 weaning failure.

Comparison 3 noninvasive versus invasive weaning, Outcome 1 nosocomial pneumonia.
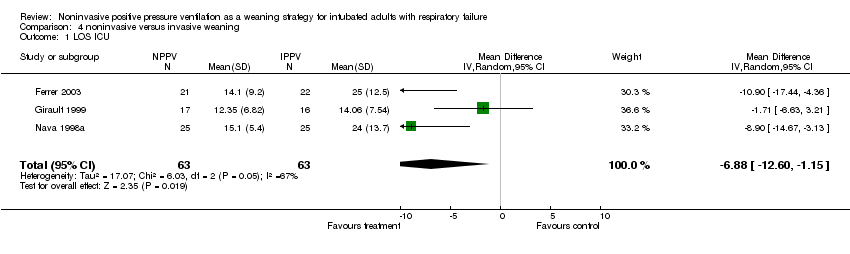
Comparison 4 noninvasive versus invasive weaning, Outcome 1 LOS ICU.

Comparison 5 noninvasive versus invasive weaning, Outcome 1 LOS hospital.
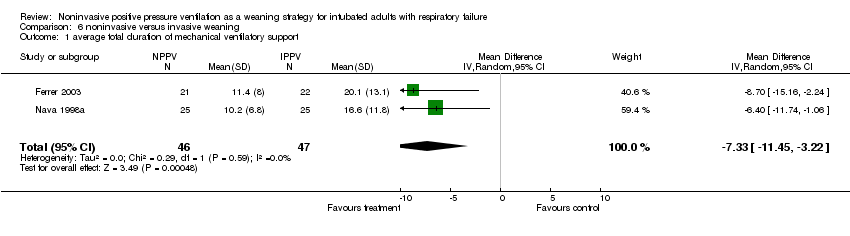
Comparison 6 noninvasive versus invasive weaning, Outcome 1 average total duration of mechanical ventilatory support.
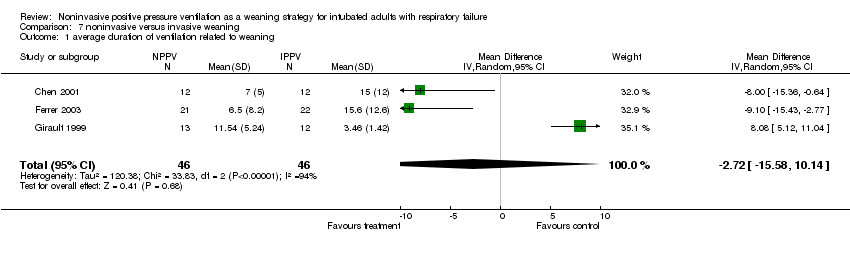
Comparison 7 noninvasive versus invasive weaning, Outcome 1 average duration of ventilation related to weaning.

Comparison 8 noninvasive versus invasive weaning, Outcome 1 duration of endotracheal mechanical ventilation.
Comparison 9 sensitivity analysis: excluding quasi‐randomized study, Outcome 1 mortality.

Comparison 9 sensitivity analysis: excluding quasi‐randomized study, Outcome 2 nosocomial pneumonia.
| Outcome | Number of trials | Number of patients | Test of homogeneity | Summary estimate | Significance |
| Mortality | 5 | 171 | p=0.83 | RR 0.41 [0.22, 0.76] | p=0.005 |
| VAP | 4 | 150 | p=0.27 | RR 0.28 [0.09, 0.85] | p=0.03 |
| Weaning failure | 3 | 104 | p=0.20 | RR 0.82 [0.29, 2.32] | p=0.71 |
| ICU LOS | 3 | 126 | p=0.05 | WMD ‐6.88 [‐12.60, ‐1.15] | p=0.02 |
| Hospital LOS | 3 | 100 | p=0.20 | WMD ‐7.33 [‐14.05, ‐0.61] | p=0.03 |
| Total duration MV | 2 | 93 | p=0.59 | WMD ‐7.33 [‐11.45, ‐3.22] | p=0.0005 |
| Duration related to weaning | 3 | 92 | p<0.00001 | WMD ‐2.72 [‐15.58, 10.14) | p=0.68 |
| Duration ETMV | 3 | 97 | p=0.08 | WMD ‐6.32 [‐12.12, ‐0.52] | p=0.03 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 mortality Show forest plot | 5 | 171 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.22, 0.76] |
| 1.1 COPD | 2 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.07, 0.91] |
| 1.2 mixed | 3 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.23, 0.96] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 weaning failure Show forest plot | 3 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.29, 2.32] |
| 1.1 COPD | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.11, 1.25] |
| 1.2 mixed | 2 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.45, 3.60] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 nosocomial pneumonia Show forest plot | 4 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.09, 0.85] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 LOS ICU Show forest plot | 3 | 126 | Mean Difference (IV, Random, 95% CI) | ‐6.88 [‐12.60, ‐1.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 LOS hospital Show forest plot | 3 | 100 | Mean Difference (IV, Random, 95% CI) | ‐7.33 [‐14.05, ‐0.61] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 average total duration of mechanical ventilatory support Show forest plot | 2 | 93 | Mean Difference (IV, Random, 95% CI) | ‐7.33 [‐11.45, ‐3.22] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 average duration of ventilation related to weaning Show forest plot | 3 | 92 | Mean Difference (IV, Random, 95% CI) | ‐2.72 [‐15.58, 10.14] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 duration of endotracheal mechanical ventilation Show forest plot | 3 | 97 | Mean Difference (IV, Random, 95% CI) | ‐6.32 [‐12.12, ‐0.52] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 mortality Show forest plot | 4 | 147 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.23, 0.81] |
| 2 nosocomial pneumonia Show forest plot | 3 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.15, 0.93] |

