Berufliche, strukturelle und organisatorische Interventionen in der Primärversorgung zur Reduktion von Medikationsfehlern
Abstract
Background
Medication‐related adverse events in primary care represent an important cause of hospital admissions and mortality. Adverse events could result from people experiencing adverse drug reactions (not usually preventable) or could be due to medication errors (usually preventable).
Objectives
To determine the effectiveness of professional, organisational and structural interventions compared to standard care to reduce preventable medication errors by primary healthcare professionals that lead to hospital admissions, emergency department visits, and mortality in adults.
Search methods
We searched CENTRAL, MEDLINE, Embase, three other databases, and two trial registries on 4 October 2016, together with reference checking, citation searching and contact with study authors to identify additional studies. We also searched several sources of grey literature.
Selection criteria
We included randomised trials in which healthcare professionals provided community‐based medical services. We also included interventions in outpatient clinics attached to a hospital where people are seen by healthcare professionals but are not admitted to hospital. We only included interventions that aimed to reduce medication errors leading to hospital admissions, emergency department visits, or mortality. We included all participants, irrespective of age, who were prescribed medication by a primary healthcare professional.
Data collection and analysis
Three review authors independently extracted data. Each of the outcomes (hospital admissions, emergency department visits, and mortality), are reported in natural units (i.e. number of participants with an event per total number of participants at follow‐up). We presented all outcomes as risk ratios (RRs) with 95% confidence intervals (CIs). We used the GRADE tool to assess the certainty of evidence.
Main results
We included 30 studies (169,969 participants) in the review addressing various interventions to prevent medication errors; four studies addressed professional interventions (8266 participants) and 26 studies described organisational interventions (161,703 participants). We did not find any studies addressing structural interventions. Professional interventions included the use of health information technology to identify people at risk of medication problems, computer‐generated care suggested and actioned by a physician, electronic notification systems about dose changes, drug interventions and follow‐up, and educational interventions on drug use aimed at physicians to improve drug prescriptions. Organisational interventions included medication reviews by pharmacists, nurses or physicians, clinician‐led clinics, and home visits by clinicians.
There is a great deal of diversity in types of professionals involved and where the studies occurred. However, most (61%) of the interventions were conducted by pharmacists or a combination of pharmacists and medical doctors. The studies took place in many different countries; 65% took place in either the USA or the UK. They all ranged from three months to 4.7 years of follow‐up, they all took place in primary care settings such as general practice, outpatients' clinics, patients' homes and aged‐care facilities. The participants in the studies were adults taking medications and the interventions were undertaken by healthcare professionals including pharmacists, nurses or physicians. There was also evidence of potential bias in some studies, with only 18 studies reporting adequate concealment of allocation and only 12 studies reporting appropriate protection from contamination, both of which may have influenced the overall effect estimate and the overall pooled estimate.
Professional interventions
Professional interventions probably make little or no difference to the number of hospital admissions (risk ratio (RR) 1.24, 95% confidence interval (CI) 0.79 to 1.96; 2 studies, 3889 participants; moderate‐certainty evidence). Professional interventions make little or no difference to the number of participants admitted to hospital (adjusted RR 0.99, 95% CI 0.92 to 1.06; 1 study, 3661 participants; high‐certainty evidence). Professional interventions may make little or no difference to the number of emergency department visits (adjusted RR 0.71, 95% CI 0.50 to 1.02; 2 studies, 1067 participants; low‐certainty evidence). Professional interventions probably make little or no difference to mortality in the study population (adjusted RR 0.98, 95% CI 0.82 to 1.17; 1 study, 3538 participants; moderate‐certainty evidence).
Organisational interventions
Overall, it is uncertain whether organisational interventions reduce the number of hospital admissions (adjusted RR 0.85, 95% CI 0.71 to 1.03; 11 studies, 6203 participants; very low‐certainty evidence). Overall, organisational interventions may make little difference to the total number of people admitted to hospital in favour of the intervention group compared with the control group (adjusted RR 0.92, 95% CI 0.86 to 0.99; 13 studies, 152,237 participants; low‐certainty evidence. Overall, it is uncertain whether organisational interventions reduce the number of emergency department visits in favour of the intervention group compared with the control group (adjusted RR 0.75, 95% CI 0.49 to 1.15; 5 studies, 1819 participants; very low‐certainty evidence. Overall, it is uncertain whether organisational interventions reduce mortality in favour of the intervention group (adjusted RR 0.94, 95% CI 0.85 to 1.03; 12 studies, 154,962 participants; very low‐certainty evidence.
Authors' conclusions
Based on moderate‐ and low‐certainty evidence, interventions in primary care for reducing preventable medication errors probably make little or no difference to the number of people admitted to hospital or the number of hospitalisations, emergency department visits, or mortality. The variation in heterogeneity in the pooled estimates means that our results should be treated cautiously as the interventions may not have worked consistently across all studies due to differences in how the interventions were provided, background practice, and culture or delivery of the interventions. Larger studies addressing both professional and organisational interventions are needed before evidence‐based recommendations can be made. We did not identify any structural interventions and only four studies used professional interventions, and so more work needs to be done with these types of interventions. There is a need for high‐quality studies describing the interventions in more detail and testing patient‐related outcomes.
PICO
Laienverständliche Zusammenfassung
Maßnahmen zur Reduktion von Medikationsfehlern bei Erwachsenen in der Primärversorgung
Was ist das Ziel dieses Reviews?
Ziel dieses Cochrane Reviews war herauszufinden, wie Medikationsfehler bei erwachsenen Patienten, die zu Aufnahmen in ein Krankenhaus, zu Besuchen in der Notaufnahme und zum Tod führen, von medizinischem Fachpersonal (Primärversorger), am besten reduziert werden können. Wir wollten herausfinden, ob entweder Maßnahmen, die sich direkt an Fachpersonen im Gesundheitswesen richten (z.B. in Form von Schulungsmaterialien und Erinnerungshilfen zur Arzneimitteldosierung, etc.), organisatorische Veränderungen der Primärversorgung (z.B. veränderte berufliche Rollen, wie etwa Verschreibungen durch Pflegende oder Pharmazeuten etc.) oder strukturelle Maßnahmen, wie etwa die Einführung von Qualitätskontrollen, zu einer Verringerung von Medikationsfehlern durch Primärversorger führen. Wir sammelten und analysierten relevante Studien zur Beantwortung dieser Frage und fanden 30 Studien.
Hauptaussagen
In den 30 Studien (169.969 Teilnehmer) dieses Cochrane Reviews zeigte sich, dass Maßnahmen, die darauf abzielten Medikationsfehler zu verringern, wie etwa Medikamentenreviews durch Pharmazeuten oder Mediziner, vermutlich nur einen kleinen oder keinen Unterschied in Bezug auf die Anzahl der Personen, die ins Krankenhaus aufgenommen werden, die Anzahl der Krankenhausaufnahmen, die Anzahl der Besuche in der Notaufnahme oder Todesfälle ausmachen. Insgesamt zeigte sich, dass der Nutzen für alle im Review dargestellten Maßnahmen unklar ist. Wir fanden keine Studien, die den Kriterien einer strukturellen Maßnahme entsprachen. Die größte Einschränkung dieses Reviews liegt in der geringen Anzahl an Studien zu den jeweiligen Maßnahmen und der niedrigen Vertrauenswürdigkeit der Evidenz.
Was wurde in diesem Review untersucht?
Die Verschreibung von Medikamenten ist für Allgemeinmediziner eines der wichtigsten Werkzeuge in der Vorbeugung und Behandlung von Krankheiten. Medikationsbedingte unerwünschte Ereignisse können in Form von unerwünschten Arzneimittelwirkungen auftreten (für gewöhnlich nicht vermeidbar) oder aus Medikationsfehlern (für gewöhnlich vermeidbar) entstehen. Wir untersuchten die Wirksamkeit von beruflichen und organisatorischen Maßnahmen im Vergleich zur Standardversorgung in Settings der Primärversorgung (Beispiele für Settings der Primärversorgung sind Hausarztpraxen, Apotheken, Pflegeheime, Kommunen, Ambulanzen und Einrichtungen für Senioren), um vermeidbare Medikationsfehler zu reduzieren, die bei erwachsenen Patienten, die in der Primärversorgung Arzneimittel verschrieben bekommen, zu Krankenhausaufnahmen, Besuchen der Notaufnahme oder Tod führen.
Was sind die Hauptergebnisse des Reviews?
Wir schlossen 30 Studien in unsere Analyse ein. Wir klassifizierten 26 Studien als organisatorische und die verbleibenden vier als berufliche Maßnahmen. Wir fanden keine strukturellen Maßnahmen in unserer Suche. Basierend auf einer moderaten und niedrigen Vertrauenswürdigkeit der Evidenz zeigten die in diesen Cochrane‐Review eingeschlossenen Studien, dass Maßnahmen zur Reduktion von vermeidbaren Medikationsfehlern in der Primärversorgung vermutlich nur einen kleinen oder keinen Unterschied auf die Anzahl an Menschen, die in ein Krankenhaus aufgenommen werden oder die Anzahl an Krankenhausaufnahmen, Besuche der Notaufnahme oder Todesfälle ausmachen. Die meisten Studien wurden in Großbritannien (UK) und den USA durchgeführt. Studien aus Ländern mit hohem Einkommen mit benachteiligten Bevölkerungsgruppen sowie Studien aus Ländern mit mittlerem und geringem Einkommen waren unterrepräsentiert. Dies könnte einen Einfluss auf die Übertragbarkeit der Ergebnisse haben.
Vertrauenswürdigkeit der Evidenz
Wir fanden heraus, dass sich die gesamte Vertrauenswürdigkeit der Evidenz für die beruflichen Maßnahmen erheblich zwischen den berichteten Endpunkten unterscheidet: moderate Vertrauenswürdigkeit für die Anzahl der Krankenhausaufnahmen, hohe Vertrauenswürdigkeit für die Anzahl an Personen, die in ein Krankenhaus aufgenommen wurden, niedrige Vertrauenswürdigkeit für Besuche der Notaufnahme und moderate Vertrauenswürdigkeit für Todesfälle. Die Vertrauenswürdigkeit der Evidenz für organisatorische Maßnahmen unterscheidet sich weniger: sehr niedrige Vertrauenswürdigkeit für die Anzahl an Krankenhausaufnahmen, niedrige Vertrauenswürdigkeit für die Anzahl an Personen, die in ein Krankenhaus aufgenommen wurden und sehr niedrige Vertrauenswürdigkeit für Besuche der Notaufnahme und Todesfälle.
Zur Verbesserung der Qualität der Studien sollte hinsichtlich der Auswahl der Studienteilnehmer und angemessener Verblindung der Studienteilnehmer sowie der Endpunktbeurteilung mehr getan werden. Der Abbruch der Studie durch Studienteilnehmer war ein weiteres Problem hinsichtlich der Vertrauenswürdigkeit der Evidenz. Die Finanzierung der eingeschlossenen Studien stammte aus unterschiedlichen Förderquellen und es ist schwer einzuschätzen, ob die Förderung einen Einfluss auf die Ergebnisse der Studien hatte.
Wie aktuell ist dieser Review?
Wir suchten nach Studien, die bis zum 4. Oktober 2016 veröffentlicht wurden.
Authors' conclusions
Summary of findings
| Professional interventions compared to standard/usual care for prevention of medication errors | ||||||
| Patient or population: adults receiving medication in primary care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with standard/usual care | Risk with professional interventions | |||||
| Number of hospital admissions | Study population | RR 1.24 | 3889 | ⊕⊕⊕⊝ | The two studies had wide confidence intervals. | |
| 17 per 1000 | 21 per 1000 | |||||
| Number of people admitted to hospital | Study population | RR 0.99 | 3661 | ⊕⊕⊕⊕ | ||
| 448 per 1000 | 443 per 1000 | |||||
| Number of emergency department visits | Study population | RR 0.71 | 1067 | ⊕⊕⊝⊝ | The two studies had wide confidence intervals and selection bias. | |
| 118 per 1000 | 85 per 1000 | |||||
| Mortality | Study population | RR 0.98 | 3538 | ⊕⊕⊕⊝ | ||
| 122 per 1000 | 119 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1We downgraded one level due to imprecision. | ||||||
| Organisational interventions compared to standard/usual care for prevention of medication errors | ||||||
| Patient or population: adults receiving medication in primary care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with standard/usual care | Risk with organisational interventions | |||||
| Number of hospital admissions | Study population | RR 0.85 | 6203 | ⊕⊝⊝⊝ | Some studies had unclear risk of bias (selection and attrition), high heterogeneity and wide confidence intervals. | |
| 274 per 1000 | 233 per 1000 | |||||
| Number of people admitted to hospital | Study population | RR 0.92 | 152,237 | ⊕⊕⊝⊝ | Some studies had unclear risk of bias (selection, attrition and performance bias) and wide confidence intervals. | |
| 13 per 1000 | 13 per 1000 | |||||
| Number of emergency department visits | Study population | RR 0.75 | 1819 | ⊕⊝⊝⊝ | Studies had unclear risk of bias (selection, performance and attrition bias), high heterogeneity and wide confidence intervals. | |
| 234 per 1000 | 176 per 1000 | |||||
| Mortality | Study population | RR 0.94 | 154,962 | ⊕⊝⊝⊝ | Studies had high risk of selection, attrition and performance bias and wide confidence intervals. | |
| 50 per 1000 | 47 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1We downgraded one level for unclear risk of bias (selection and attrition bias). | ||||||
Background
Description of the condition
Medication‐related (drug‐related) adverse events in primary care represent an important cause of hospital admissions and mortality (Howard 2003). Medication‐related adverse events could be the result of people either experiencing adverse drug reactions (not usually preventable) or as a result of medication errors (usually preventable) (Bates 1995; Ioannidis 2001).
According to Edwards 2000, adverse drug reactions can be defined as "an appreciably harmful or unpleasant reaction resulting from an intervention related to the use of a medicinal product." Medication errors on the other hand, are mostly preventable. A medication error is defined by Ferner 2006 as "a failure in the treatment process that leads to, or has the potential to lead to, harm to the patient." They are mainly due to prescribing or medication management errors. A reduction of these types of prescribing/medication errors has been a high priority for healthcare policy in order to improve the safety profile of the healthcare delivery system (Howard 2003; Soe 2013).
A prospective cohort study has shown that within four weeks of receiving a primary care prescription, 25% of participants experienced an adverse drug event, 11% of which were judged preventable (Gandhi 2003). A systematic review and meta‐analysis by Winterstein 2002 reported that a median 7.1% (inter‐quartile range 5.7% to 16.2%) of hospital admissions resulted from drug‐related problems, of which 59% were considered preventable (i.e. attributable to error), while Howard 2007 reported that a median of 3.7% of hospital admissions were preventable and drug‐related. Improving patient safety is, as a consequence, now a government priority in many high‐income and middle‐ and low‐income countries, including the UK, USA and five African countries; Egypt, South Africa, Morocco, Tanzania and Zimbabwe (Brown 2008; WHO 2004).
Description of the intervention
In this review we examined interventions in primary care to reduce preventable medication errors that resulted in hospital admissions, emergency department visits, and mortality. The three main types of interventions that we examined included professional, organisational, and structural interventions as described by Cochrane Effective Practice and Organisation of Care (EPOC) (Appendix 1). Professional interventions included quality assurance tools that provided educational interventions for practitioners or participants, such as teaching the use of structured assessments with general practitioners (GPs). Organisational interventions included revision of professional roles (e.g. nurse‐ or pharmacist‐led chronic disease clinics and nurse prescribing) and revision of clinical multidisciplinary teams (e.g. pharmacist‐managed medication reviews). Structural interventions included the organisation of quality monitoring services. We used these interventions for any type of primary care‐based population, irrespective of their characteristics. The comparator was no intervention or standard or usual care. The selected outcomes included in the review were the number of hospital admissions, emergency department visits, and mortality. These outcomes were selected as they are tangible and mostly reported in primary studies. We did not consider patient‐oriented or patient‐mediated outcomes in this review due to the complexity of the included interventions. We will consider these outcomes in the updated review.
How the intervention might work
The three main interventions, mentioned above, used different approaches to achieve a reduction in medication errors that led to hospital admissions, emergency department visits, and mortality.
Professional interventions included continuing education and quality assurance that provided educational interventions for practitioners or participants, such as teaching the use of structured assessments with GPs. Other examples of professional interventions included drug education programmes for physicians that were run by physicians, electronic health record systems that provided information about drugs and gave recommendations about changing doses, health technology that identified care home residents at risk of falls, and computer‐based drug‐ordering systems that gave suggestions to physicians and pharmacists.
Organisational interventions included revision of professional roles (e.g. nurse‐ or pharmacist‐led chronic disease clinics and nurse prescribing) and revision of clinical multidisciplinary teams (e.g. pharmacist‐managed medication reviews). Organisational interventions may have included telephone consultations along with home‐based medication reviews by pharmacists or nurses. Such interventions aimed at engaging workers in the management of risk to increase patient safety.
Structural interventions included the organisation of quality monitoring services. Examples of these interventions included structural approaches such as social, economic, and political interventions that could improve public health outcomes by increasing the willingness and ability of individuals to practice prevention. An example of the latter would be the introduction of financial incentives to healthcare workers to reduce medication errors. By looking at all of these interventions in the current review, we can begin to address the multiple perspectives of various stakeholders who provide health care to individuals in primary care (Benning 2011).
Why it is important to do this review
Prescribing medications is one of the most powerful tools available to GPs in the prevention and treatment of disease, and alleviation of symptoms (Spencer 2014). However, medication‐related adverse events arising as a result of primary care prescribing are an important source of participant morbidity, much of which could be prevented by higher‐quality prescribing and medicines management (Howard 2007). To date, there is little information on the interventions mentioned above, aimed at reducing preventable medication‐related adverse events in primary care due to errors. A review undertaken by Ioannidis 2001, addressed interventions of all types of medical errors in both primary and secondary care. It highlighted the complexity in studying those types of interventions aimed at minimising errors in healthcare delivery. Other reviews by Durieux 2012 and O'Brien 2008 focused on interventions to improve professional practice and healthcare outcomes, including prescribing. A review by Royal 2006 found that there was weak evidence to support pharmacist‐led medication interventions being effective in reducing hospital admissions. However, none of these reviews have focused on other types of interventions at the professional, organisational or structural level that could possibly reduce medication errors in the primary care setting.
Given that preventable medication errors in primary care are associated with hospital admissions, emergency department visits, and mortality, it is important to know whether there are any interventions that have been found to be effective in reducing the occurrence of these outcomes. While members of our team published a related systematic review on this topic (Royal 2006), there has been no Cochrane Review of interventions aimed at reducing the incidence of preventable medication errors that lead to hospital admissions, emergency department visits, and mortality.
Objectives
To determine the effectiveness of professional, organisational and structural interventions compared to standard care to reduce preventable medication errors by primary healthcare professionals that lead to hospital admissions, emergency department visits, and mortality in adults.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised trials in this review. We excluded controlled before‐after studies and other non‐randomised designs as they provided much weaker evidence due to the non‐randomisation of participants to experimental and control groups. We did not impose any restriction on the language or country in which studies were carried out.
Types of participants
We included studies directed at healthcare professionals and organisations involved in the provision of primary care in the community setting who were authorised to prescribe, sell or administer medications, including primary care physicians (general practitioners (GPs), family doctors, family physicians, family practitioners), dental practitioners, community nurses, nurse practitioners, community pharmacists, dispensers in community pharmacies and any other relevant healthcare providers. We included all adult participants who were receiving a medication through the intervention of the aforementioned primary healthcare professionals.
Examples of community settings included general practice, community pharmacies, and nursing and residential homes. We excluded studies of interventions for outpatients in a clinic attached to a hospital or a day hospital unless these were specifically described as primary care clinics.
Types of interventions
Using the taxonomy of interventions developed by EPOC, we categorised interventions that improved patient safety by reducing hospital admissions, emergency department visits, and mortality (Appendix 1). We compared the interventions with inactive control interventions such as no treatment, or standard or conventional care. We divided interventions into the following categories.
Professional interventions
Professional interventions included the use of health information technology to identify people at risk of medication problems, computer‐generated care suggested and actioned by a physician, electronic notification systems about dose changes, drug interventions and follow‐up, and educational interventions on drug use aimed at physicians to improve drug prescriptions.
Organisational interventions
Examples of organisational interventions included medication reviews by pharmacists, nurses or physicians, clinician‐led clinics, and home visits by clinicians.
Structural interventions
Structural interventions included the organisation of quality monitoring services. Structural approaches included social, economic, and political interventions that could improve public health outcomes by increasing the willingness and ability of individuals to practice prevention. An example of the latter would be the introduction of financial incentives to healthcare workers to reduce medication errors.
Types of outcome measures
We included studies that addressed preventable medication errors with the following outcomes. All the outcomes below are included in summary of findings Table 1 and summary of findings Table 2.
Primary outcomes
-
Number of hospital admissions (this outcome takes into account that one patient can have multiple admissions)
-
Number of people admitted to hospital (this outcome reports on the number of people admitted to hospital irrespective of the number of times they were admitted during the study period)
Secondary outcomes
-
Number of emergency department visits
-
Mortality
Search methods for identification of studies
EPOC's Information Specialist, Paul Miller, developed the search strategies in consultation with the review authors. The Information Specialist searched the Cochrane Database of Systematic Reviews and the Database of Abstracts of Reviews of Effects (DARE) for related systematic reviews, and the databases listed below for primary studies.
Electronic searches
We searched the following databases on 4 October 2016.
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2016, Issue 9), in the Cochrane Library.
-
MEDLINE Ovid (including epub ahead of print, in‐process and other non‐indexed citations) (1946 to 4 October 2016).
-
Embase, Ovid (1974 to 3 October 2016).
-
Health Technology Assessment Database (NHSEED; 2015, Issue 2), in the Cochrane Library.
-
NHS Economic Evaluation Database (NHSEED; 2015, Issue 2), in the Cochrane Library.
-
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature; 1981 to 4 October 2016).
Search strategies are comprised of keywords and controlled vocabulary terms. We applied no language or time limits. We searched all databases from database start date to date of search. All search strategies used are provided in Appendix 2.
Searching other resources
Grey literature
On 4 October 2016 we conducted a grey literature search to identify studies not indexed in the databases listed above. Sources included the sites listed below. We documented additional sources, if any, in the review.
-
Open Grey (opengrey.eu).
-
Grey Literature Report (New York Academy of Medicine) (greylit.org).
-
Agency for Healthcare Research and Quality (AHRQ) (ahrq.gov).
-
Joanna Briggs Institute (joannabriggs.edu.au).
-
National Institute for Health and Care Excellence (NICE) (nice.org.uk).
Trial registries
We searched the following trial registries on 4 October 2016.
-
International Clinical Trials Registry Platform (ICTRP), Word Health Organization (WHO) (who.int/ictrp).
-
ClinicalTrials.gov, US National Institutes of Health (NIH) (clinicaltrials.gov).
We undertook the following.
-
Screened individual journals and conference proceedings (e.g. handsearch).
-
Reviewed reference lists of all included studies, relevant systematic reviews/primary studies/other publications.
-
Contacted authors of relevant studies or reviews to clarify reported published information/seek unpublished results/data.
-
Contacted researchers with expertise relevant to the review topic/EPOC interventions.
-
Conducted cited reference searches for all included studies in citations indexes.
Data collection and analysis
Selection of studies
Three review authors (HK, HC and BB) independently screened the titles and abstracts to assess studies against the inclusion criteria. We obtained full‐text copies of all papers considered to be of potential relevance and we contacted first authors of studies for clarification, where necessary. We resolved disagreements about relevance by discussion between the review authors. We entered all included studies in Review Manager 5 software (Review Manager 2014).
Data extraction and management
Three review authors (HK, HC and BB) independently completed data extraction using a customised version of the EPOC data collection checklist (EPOC 2017a). All three review authors met frequently to discuss progress, with discrepancies resolved by discussion between the review authors. We grouped studies together on the basis of similar interventions and common outcomes and used Review Manager 5 software to manage and pool data (Review Manager 2014), as mentioned in chapter 7 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We documented the selection process in sufficient detail to complete a PRISMA flow chart (Liberati 2009), and a Characteristics of excluded studies table.
Assessment of risk of bias in included studies
Three review authors (HK, HC and BB) independently assessed the risk of bias of all included studies using the criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). We resolved differences through discussion.
We assessed seven parameters including random sequence generation, allocation concealment, blinding of participants and outcome assessors, incomplete outcome data, selective reporting, and other bias including protection against contamination and publication bias. We discussed the inclusion of the selected studies in the meta‐analysis based on their risk of bias. We assessed studies on the basis of having low, unclear or high risk of bias. We included all trials in the final meta‐analysis.
Measures of treatment effect
For each of the primary outcomes listed above, we reported outcomes for each study in natural units (i.e. number of participants with an event per total number of participants at follow‐up). We examined funnel plots for evidence of publication bias and analysed data using Review Manager 5 (Review Manager 2014). We presented results with 95% confidence intervals (CIs) and estimates for dichotomous data (number of people admitted to hospital) as risk ratios (RRs).
Unit of analysis issues
We examined the methods of analysis of all study types critically. All randomised trials were appropriately analysed. We analysed cluster‐randomised trials at the same level as the allocation, thereby avoiding unit‐of‐analyses errors (Alvarez 2001; Coleman 1999; Gernant 2016; Kaczorowski 2011; Lapane 2011; Lowrie 2012; Malet‐Larrea 2016; Roberts 2001). Therefore, we did not need to reanalyse the results and it was appropriate to combine them with other randomised trials.
Dealing with missing data
We did not exclude any studies from the meta‐analysis due to a differential loss to follow‐up or missing data. Most studies had adequate reporting of the participants in their samples. We were able to extract all the data needed for analysis from the included studies. We did not need to contact any study authors for more information.
Assessment of heterogeneity
Because trials may not have been carried out according to a common protocol, there were usually variations in participant groups, clinical settings, concomitant care, etc. Therefore, we assessed heterogeneity between trial results. We considered trial data to be heterogeneous where the I2 statistic was greater than 40% (Higgins 2003). For analyses, we used the random‐effects method. We attempted to explain the differences between studies on the basis of the characteristics of interventions in the included studies.
Assessment of reporting biases
We carefully assessed all studies for reporting bias. Reporting bias was especially likely with outcomes that used participant self‐reports or self‐administered surveys.
Data synthesis
We carried out statistical analysis using Review Manager 5 software (Review Manager 2014). We used a random‐effects meta‐analysis for combining data due to the clinical and methodological heterogeneity between studies. We grouped studies based on the two main interventions (i.e. professional and organisational). Where appropriate, we carried out meta‐analyses to establish the effects of interventions on medication‐related hospital admissions, emergency department visits, and mortality. We found no studies addressing structural interventions and hence no analysis was undertaken.
'Summary of findings table' and GRADE
We included two 'Summary of findings' tables for the main intervention comparisons: 'professional interventions compared to usual care' (summary of findings Table 1); and 'organisational interventions compared to usual care' (summary of findings Table 2). The 'Summary of findings' tables include the justification for our decisions to downgrade or upgrade the evidence for an outcome, along with comments to help the reader understand the process. We included the following outcomes in the 'Summary of findings' tables: number of hospital admissions, number of people admitted to hospital, number of emergency department visits, and mortality.
Three review authors (HK, HC and BB) used the GRADE tool to independently judge the certainty of the evidence (high, moderate, low, and very low) with respect to five criteria (risk of bias, inconsistency, indirectness, imprecision, and publication bias), with disagreements resolved through discussion (Guyatt 2008). We used methods and recommendations described in Section 8.5 and Chapter 11 of the Cochrane Handbook for Systematic Reviews of interventions and GRADEpro GDT software (GRADE pro GDT 2015; Higgins 2011b; Schünemann 2011). In addition, we used the EPOC worksheets to write plain language statements to report these findings in the review (EPOC 2017b).
Subgroup analysis and investigation of heterogeneity
We conducted the analyses based on the types of interventions (professional, organisational, structural) as described by Deeks 2011. We undertook analyses for the following interventions.
-
Professional interventions, such as provision of educational interventions for practitioners or participants.
-
Organisational interventions, including revision of professional roles (e.g. nurse‐ or pharmacist‐led chronic disease clinics, nurse prescribing) and clinical multidisciplinary teams (e.g. pharmacist‐managed medication reviews).
We found no studies addressing structural interventions and therefore, we did not include this type of intervention in our review. There was no other subgroup analysis undertaken in the review.
Sensitivity analysis
We used a sensitivity analysis to explore the influence of the following on effect size: repeating the analysis; and excluding any high risk of bias studies to see how they influenced the results. We did this in order to help understand whether the results of the review are robust.
Results
Description of studies
Results of the search
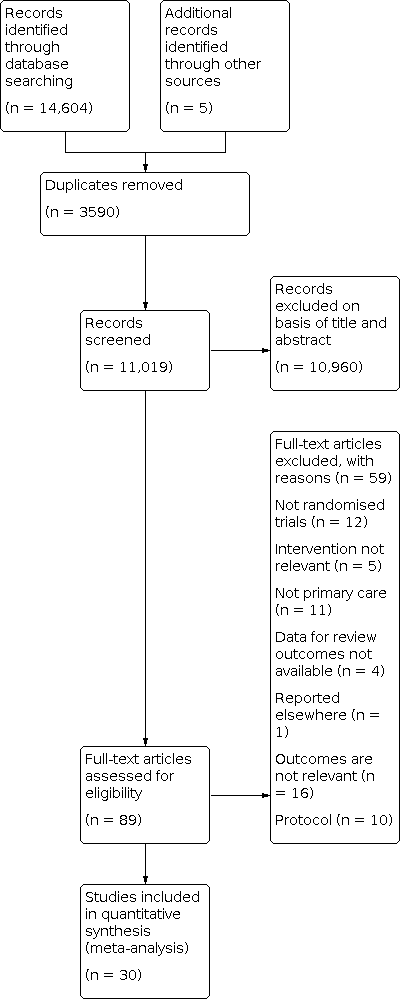
Searches of the main electronic databases led to identification of 14,604 titles. A search of the grey literature and of trial registries yielded a total of five articles that did not make it in the final included studies. Handsearching of the references listed did not yield new studies.
We identified a total of 11,019 references after removal of duplicates. From reading titles and abstracts, we eliminated 10,960 as being not relevant to the review. Reasons for exclusions included irrelevant interventions, study designs and populations (i.e. not primary care settings). We obtained full papers for 89 references. From these 89 papers, we excluded 59 papers for reasons such as study design, study reported elsewhere and study not conducted in a primary care setting, irrelevant outcomes and protocols (see Characteristics of excluded studies). We included a total of 30 papers reporting on 30 trials (see Characteristics of included studies). We have provided an overview of the selection process in a PRISMA flow diagram, Figure 1 (Liberati 2009).
Study flow diagram
Included studies
Method (design)
We included a total of 30 studies (169,969 participants) in this review. Four studies addressed professional interventions (8266 participants) and 26 studies described organisational interventions (161,703 participants). Overall, there were eight cluster‐randomised trials (Alvarez 2001; Coleman 1999; Gernant 2016; Kaczorowski 2011; Lapane 2011; Lowrie 2012; Malet‐Larrea 2016; Roberts 2001), and 22 randomised trials (Bernsten 2001; Campins 2016; Frankenthal 2014; Garcia‐Gollarte 2014; Gurwitz 2014; Hawes 2014; Holland 2005; Ibrahim 2013; Korajkic 2011; Krska 2001; Lenaghan 2007; Malone 2000; Moertl 2009; Murray 2004; Nabagiez 2013; Okamoto 2001; Olesen 2014; Pai 2009; Rytter 2010; Triller 2007; Zermansky 2001; Zermansky 2006. They all ranged from three months to 4.7 years of follow‐up. A full description of the interventions of each study is included in the 'Characteristics of included studies', Table 1 and Table 2. All cluster‐randomised trials were appropriately analysed. Alvarez 2001 reported randomisation at the pharmacy level. They used adjusted Pearson's Chi2 to compare means. Coleman 1999 used statistical techniques that accounted for potential within‐practice correlation that results from randomisation of practices. For continuous variables, they used a mixed model analysis of covariance and regression analysis and for binary values, they used generalised estimating equations. They derived P values from a t‐distribution rather than a normal distribution. Gernant 2016 used a multivariable logistic regression model using generalised estimating equations to examine the effect of the intervention on the probability of 60‐day all‐cause emergency department utilisation. The analysis was approved by the Purdue University Institutional Review Board. Kaczorowski 2011 fitted linear regression models by using the Poisson distribution. Lapane 2011 analysed their results using a Poisson regression model and accounted for the cluster trial design to provide estimates adjusted for potential confounders. In contrast, Lowrie 2012 compared the main outcomes between the intervention and control groups using a Cox proportional hazards frailty model, which accounted for the cluster‐randomisation design. Malet‐Larrea 2016 included a random intercept for pharmacies nested within a group, to account for clustering of participants within pharmacies, and was adjusted by covariate that could affect hospital admissions (age, gender and number of health problems). Differences between groups in hospital costs were analysed by hospital admission and by participant, and the latter ones adjusted by analysis of covariance (ANCOVA) for the number of health problems. Roberts 2001 used robust variance estimation techniques (SUDAAN 2012), in which the effect of clustering within nursing homes on the variance was accounted for.
| Study | Name | Theory | Materials | Procedures | Who provided intervention | Modes of delivery |
|---|---|---|---|---|---|---|
| Pharmaceutical care | Pharmaceutical care is the provision of drug therapy for the purpose of achieving outcomes that improve a person’s quality of life. | Pharmacies in the intervention group provided pharmaceutical care, which consisted of offering the pharmaceutical care service to participants and to their corresponding GPs. | An Initial interview and assessment of the therapeutic plan was undertaken, registration of data during the subsequent visits to allow the identification of medication‐related problems, and an intervention to solve the problem. The intervention involved proposing changes in the medication participants received, which had to be communicated to the patient’s GP. | Pharmacists provided the intervention. | Individual and face‐to‐face | |
| Pharmaceutical care | Pharmaceutical care is the provision of drug therapy for the purpose of achieving outcomes that improve a person's quality of life, although little research has been conducted in community‐based pharmaceutical care with elderly people. | Training of pharmacists was done with a study manual. The manual contained an overview of the concept of pharmaceutical care and its provision to elderly people. No reference was provided for the study manual. | The intervention group of pharmacists identified actual and potential drug‐related problems using a structured approach. These pharmacists utilised a number of data sources in this assessment including the participant, the participant's GP, and pharmacy records. Following this assessment, pharmacists were instructed to formulate an intervention and monitoring plan. | Community pharmacists were trained to provide the structured pharmaceutical care intervention. A study manual helped facilitate this process. It contained an overview of the concept of pharmaceutical care, its provision to elderly people, information on the therapeutic management of a number of disease states common in the elderly, together with other issues pertinent to drug therapy in the elderly. | Individual face‐to‐face | |
| Drug evaluation and recommendation | Several instruments, criteria, and algorithms have been developed to enable more rational and appropriate use of medication, but limited evidence exists with regard to the outcomes that were investigated. | The Good Palliative‐Geriatric Practice algorithm Garfinkel 2007) and the STOPP/START criteria were used (O'Mahony 2015). Both of these tools assess the appropriate use of medication in older people. | The intervention was composed of 3 phases. In the first phase, an experienced pharmacist evaluated all prescriptions using the GP‐GP algorithm and based their decision about appropriateness on the STOPP/START criteria. In the second phase, the pharmacist discussed recommendations for each drug with the participant's physician in order to come up with a final list of recommendations. Finally, the recommendations were discussed with the participant and a final decision was agreed by physicians and participants. | The intervention was delivered by a trained and experienced pharmacist. No details are provided concerning what is a "trained and experienced" pharmacist. | Individual and face‐to‐face | |
| Chronic care clinics | Chronic care clinics redesign the structure and content of primary care services through the delivery of scheduled visits devoted to chronic disease management. This mode of service delivery has the potential to improve outcomes for elderly people. | The chronic care clinics included an extended visit with the physician and nurse dedicated to planning chronic disease management, a pharmacist visit that emphasised reduction of polypharmacy and high‐risk medications, and a patient self‐management group. | Frail older people were invited to participate in visits with the primary care team. During these visits, a shared treatment plan was developed, a session was conducted with the pharmacist that addressed polypharmacy and medications associated with functional decline, patient self‐management group sessions were conducted, and the provision of health status assessment information was provided to the practice team. | The team that provided the intervention consisted of the participant’s physician, a team nurse, and a pharmacist. Physicians and team nurses received training in population‐based medicine and management strategies of geriatric syndromes. Team nurses received on‐the‐job coaching from study staff. | The intervention was delivered individually and in groups in a face‐to‐face format. | |
| Medication review and drug recommendations | Potentially inappropriate prescriptions are prevalent in older people and are associated with adverse drug events. The STOPP/START criteria are designed to detect potentially inappropriate prescriptions in elderly people. However, little is known about the effects of an intervention involving the application of the STOPP/START criteria on clinical outcomes. | The STOPP/START criteria were used to deliver the intervention (Gallagher 2008). The STOPP criteria focus on avoiding the use of drugs that are potentially inappropriate for older people and the START criteria identify undertreatment or prescribing omissions in older people. | Medication reviews were conducted by the study pharmacist for all residents. Recommendations made by the pharmacist were discussed with the chief physician. The physician then decided whether to accept these recommendations and implement prescribing changes. | The intervention was conducted by the study pharmacist who applied the STOPP/START criteria during the medication review. The pharmacist also discussed the recommendations from the intervention with the chief physician, who decided whether to accept these recommendations and implement prescribing changes. | Intervention was delivered individually and face‐to‐face. | |
| Structured educational intervention | Inappropriate drug prescription is a common problem in people living in nursing homes and is linked to adverse health outcomes. This study assessed the effect of an educational intervention directed to nursing home physicians in reducing inappropriate prescription and improving health outcomes and resource utilisation. | Educational material and references were given to physicians and two 1‐h workshops were used to review cases and promote practice changes. The STOPP/START criteria were reviewed with a random sample of 10 residents cared for by each physician (Gallagher 2008). The content of the educational intervention is provided in an appendix (Garcia‐Gollarte 2014). | The educational intervention included general aspects of prescription and drug use in geriatric patients, how to reduce the number of drugs, to perform a regular review of medications, to avoid inappropriate drug use, to discontinue drugs that do not show benefits, and to avoid under treatment with drugs that have shown benefits. It also discussed some drugs frequently related to adverse drug reactions in older people. | A nursing home physician delivered the structured educational intervention. | Face‐to‐face intervention delivered in a group and individual format. | |
| Medicine reconciliation and action plan | Emergency department overcrowding has been linked to increased mortality, costs, and length of stay. This study evaluated the effectiveness of a telephone‐based, medicines‐management service on reducing emergency department utilisation. | Medication therapy management was provided to participants (APA 2008). A pharmacy technician completed telephonic medication reconciliation, after which a trained pharmacist consulted with the participant or caregiver via telephone to complete a scheduled, comprehensive medication therapy review to identify and resolve any medication‐related problems. The pharmacist constructed a personal medication record and a medication‐related action plan for the participant. The action plan was a participant‐centred document that assisted participants, caregivers, and the pharmacist in the resolution of identified medication‐related problems. | The intervention commenced with a pharmacy technician completing medication reconciliation with the participant over the telephone. Then, a pharmacist consulted with the participant by telephone for an average of 30 min to complete a comprehensive medication review to identify and resolve medication‐related problems. The pharmacist constructed a person medication‐related action plan and followed‐up with the participant's prescriber. | A pharmacy technician delivered the initial medicine reconciliation with the participant. A trained pharmacist conducted the medication therapy review, constructed a personal medication record, and a medication‐related action plan. The pharmacist also followed up with the participant's prescriber for resolution of problems that could not be resolved with the participant. | The intervention was conducted individually on the telephone. | |
| Automated system to facilitate flow of information and provide warnings, alerts, and recommendations | Transitions between the impatient and outpatient setting is a period of high risk for older adults. Most approaches to improving transitions require a substantial commitment of resources but automating these processes may improve the quality and safety of care. | An automated system was used to facilitate the flow of information to the medical group's primary care providers about individuals who were discharged to home from the hospital (Field 2012). | An automated system was developed to facilitate the flow of information to the medical group's primary care providers. A computer interface linked the primary care provider's electronic health records to the hospital records, which provided information about admissions and discharges. The system also provided information about new drugs at discharge, warnings about drug‐drug interactions, recommendations about dose changes and laboratory monitoring of high‐risk medications, and alerts to the provider's support staff to schedule a post‐hospitalisation office visit within 1 week of discharge if not already scheduled. | The automated system delivered the intervention. | The intervention was delivered electronically. | |
| Care transitions clinic visit | Medication errors related to hospital discharge result in rehospitalisations and emergency department visits, which may be reduced by pharmacist involvement during postdischarge transitions of care. This study evaluated the impact of a transitional care clinic visit conducted by a pharmacist. | The Best Possible Medication Discharge List was used to identify medication discrepancies (Wong 2008). It served as the gold standard for the list of medications that the participant should take after discharge. | Participants in the intervention group were scheduled for a care transitions clinic visit approximately 72 h after hospital discharge. The visit involved performing a complete medication history, identifying and resolving medication discrepancies, creating a current medication list, and counselling on appropriate medication use. | Clinical pharmacists provided the intervention. They collaborated with the inpatient medical team to create the Best Possible Medication Discharge List. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist home visits | Older people often have trouble adhering to their medications. This study evaluated the effectiveness of a home‐based medication review on hospital admissions among elderly people. | A standardised visit form was used to record the home visit but no reference was provided. | Pharmacists arranged home visits with the participant during which they assessed the participant's ability to self‐medicate and drug adherence. They educated the participant, removed out‐of‐date drugs, reported drug reactions or interactions to the physician, and reported the need for a compliance aid. | Pharmacists conducted the home visits. Pharmacists held a postgraduate qualification in pharmacy practice or had recent continuing professional development in therapeutics. The pharmacists participated in a 2‐day training course, which included lectures on adverse drug reactions, prescribing in elderly people, improving concordance, and communication skills. | The intervention was delivered individually and face‐to‐face. | |
| Telephone consultation with home visits | Adherence to warfarin treatment and monitoring guidelines may be suboptimal among patients and staff. This study assessed the improvement in adherence to warfarin therapy with telephone and home visits. | A predesigned set of questions was used in the telephone consultation, but no reference or any additional details were provided. | The intervention group was counselled with once‐a‐week telephone consultations and 2 home visits per month by either a nurse or a pharmacist that dealt with warfarin use. | A pharmacist or a nurse provided the home visits. The telephone consultation was conducted by a pharmacist. | The intervention was delivered individually using a face‐to‐face format and telephone calls. | |
| Cardiovascular risk assessment and education sessions | Strategies for managing blood pressure are essential as high blood pressure is the leading risk factor for death. The study authors evaluated the effectiveness of a community‐based cardiovascular health promotion and disease prevention programme in reducing morbidity. | The Cardiovascular Health Awareness Program was a standardised intervention that consisted of 10 weeks of cardiovascular risk assessment, blood pressure measurements, and education sessions (CHAP 2017). | The intervention consisted of 10 weeks of cardiovascular risk factor assessment and educational sessions. Volunteers were recruited to help participants measure their blood pressure and supported self‐management by providing participants with their risk profile, risk‐specific educational materials and information about access to local services. At the end of the 10‐week programme and 6 months after the programme ended, the results were forwarded to family physicians who rank‐ordered their participants by their most recent systolic blood pressure reading. | Volunteers were recruited and trained to carry out the intervention. The volunteers were trained according to a standardised curriculum developed by a public health nurse and delivered by nurses working in the intervention community. | The intervention was conducted individually in a face‐to‐face manner. | |
| Educational intervention with pharmacist | Few studies have examined a pharmacist's contribution to improving diuretic compliance and reducing rehospitalisation and health care use. This study aimed to determine the impact of a pharmacist‐led intervention on patient‐guided diuretic dose adjustment. | The intervention group adjusted their diuretic dose using a flexible frusemide dose‐adjustment guide that was provided in the paper. | The intervention consisted of a 30‐min educational session and focused on improving participant self‐care, recognising symptoms of fluid retention, measuring weight daily, self‐adjusting the diuretic dose and improving knowledge of heart failure and heart failure medications. | A pharmacist provided the intervention. The frusemide dose‐adjustment guide was developed in collaboration with cardiologists. | Conducted individually in a face‐to‐face fashion. | |
| Pharmaceutical care plan | Regular medication reviews can reduce the risk of medication‐related problems. This study aimed to evaluate the effect of a pharmacist‐led medication review on pharmaceutical care issues and hospitalisations. | Clinically‐trained pharmacists completed a detailed profile for each participant using medical notes and computer records. All participants were interviewed in their home about their use of and responses to medication and their use of health and social services. No references provided | A pharmaceutical care plan was drawn up listing all pharmaceutical care issues together with all the actions planned to achieve the outcomes of any pharmaceutical care issue. Copies of the plan were given to the GP who was asked to agree, after which the pharmacist implemented the plan. | The pharmacist performed the medication review. The participants' GP indicated their level of agreement with each pharmaceutical care issue and with the actions taken. | The mode of delivery was individual and face‐to‐face. | |
| Use of health information technology to identify people at risk for delirium and falls, implement monitoring plans, and provide reports to pharmacists | Falls and delirium pose the greatest threats to resident safety in nursing homes and contributes to further functional decline. Medication use is associated with greater risk of delirium and falls. Therefore, this study used health information technology to identify residents at risk for delirium and falls due to adverse drug events. | A Geriatric Risk Assessment MedGuide was a database designed to identify medications that potentially contributed to delirium and fall risk (Tobias 1999). It also facilitated early recognition of signs and symptoms indicative of potential medication‐related problems. Training was provided to nursing staff and pharmacists in how to use the reports generated by the Geriatric Risk Assessment MedGuide. | Health information technology was used to identify residents at risk for delirium and falls, implement monitoring plans, and provide reports to pharmacists in conducting medication reviews. The consultant pharmacist shared the reports with the nurse contact at the facility and used the reports in their monthly drug review. | The intervention was an automated system that provided reports to pharmacists and nurses, who were trained to use these reports. The training for nurses provided information regarding medications that cause, aggravate, or contribute to the risk of falls and delirium. The course also reviewed symptoms and signs of adverse medication effects and reinforced the importance of the early observation of symptoms and signs of adverse medication effects. Pharmacists were trained to provide a targeted drug review for all participants who experienced delirium and falls. | The intervention was delivered individually and face‐to‐face. | |
| Home‐based medication review | Home‐based medication reviews are convenient for the patient and provide an opportunity to understand their medication‐taking in their home environment. Therefore, this study looked at whether home‐based medication reviews with elderly people could reduce hospital admissions. | The intervention comprised 2 home visits by a community pharmacist who educated the participant/carer about their medicines, noted any pharmaceutical care issues and assessed the need for an adherence aid. | At the home visit, the pharmacist educated the participant, removed out‐of‐date drugs, and assessed the need for an adherence aid. The pharmacist held regular meetings with the GP where changes to the participant's medications were discussed and amendments were implemented by the GP. | A pharmacist with a post‐graduate qualification in pharmacy practice conducted the home‐based medication review. They had regular meetings with the lead GP. Possible changes to the participant's medication were discussed and agreed amendments were implemented by the GP. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Although angiotensin‐converting enzyme inhibitors and beta‐blockers reduce morbidity and mortality in people with heart failure, these treatments are underused. Pharmacists may improve treatment through medication review. This study investigated whether a pharmacist intervention would reduce hospital admission and death for people with heart problems. | Pharmacists received training covering the aetiology, symptoms, and evidence‐based management of heart failure. They also participated in monthly discussions of specific cases. The pharmacist used guidelines to optimise treatment for participants with left ventricular systolic dysfunction. All of these materials are available at onlinelibrary.wiley.com/journal | Participants were offered a 30‐min appointment with the pharmacist If there was agreement between the pharmacist and the participant, and subsequently with the doctor, medications were initiated, discontinued, or modified by the pharmacist during 3‐4 weekly or fortnightly consultations. | The pharmacists, who delivered the medication review, had between 3 and 16 years of post‐qualification experience, had experience delivering primary care‐based medication review clinics for people receiving multiple‐drug treatment and attended an in‐house training day covering the aetiology, symptoms, and evidence‐based management of heart failure. An additional session covered the methods of the trial. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Aging and the use of polypharmacy are risk factors for drug‐related problems and medication‐related hospital admissions. Therefore, this study assessed the impact of a community pharmacist‐led medication review on hospital admissions in older people. | Pharmacists in the intervention group received a training course that covered the clinical management of older people and the medication review method. No reference was provided. | The medication review consisted of the pharmacist collecting information about the participant's health problems, medication use, lifestyle habits, and concerns about diseases and medications. The pharmacist then identified negative clinical outcomes related to medicines and drug‐related problems. Subsequently, an action plan was agreed upon which focused on participant outcomes and the medication use process. | Pharmacists provided the medication review. They received a 3‐day training course covering clinical management of elderly people, the medication review with follow‐up method, communication with participants and doctors, study protocol and documentation forms. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist visits | Pharmacists have adopted pharmaceutical care, which is the provision of drug therapy to improve a person's quality of life, to reduce morbidity and mortality. Unlike previous studies that did not focus on people who were most likely to benefit, this study examined veterans who were at high risk for a medication‐related problem. | Contacts between the pharmacist and participant were recorded on a data collection form, which contained the method of contact, time spent, medical problems addressed, drug‐related problems addressed, and drug‐related problems resolved. This form was not referenced. | The intervention participants received consultation and follow‐up care from a clinical pharmacist. | Pharmacists conducted the intervention. Most had a Doctor of Pharmacy degree and over 70% were either receiving or had completed postgraduate training. | The intervention was delivered individually and face‐to‐face. | |
| Home‐based nurse care | Home‐based nurse care can reduce adverse events in people with chronic heart failure. High levels of natriuretic peptides in people with heart failure are predictors of death and hospitalisations. The study authors looked at whether high levels of these peptides can predict whether people with heart failure benefit from a home‐based nurse intervention. | The nurse checked for and, in co‐ordination with the treating physician, implemented guideline‐based medication (Remme 1997; Remme 2001). | At home visits, the nurse checked and recorded weight, recorded symptoms and signs of heart failure as well as heart rate and blood pressure, and organised and reviewed blood analyses on demand. The nurse also gave the patient education and self‐management skills. | Nurses who specialised in caring for people with heart failure provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Computerised care suggestions | Hypertension is associated with cardiovascular morbidity and mortality, but is difficult to control. Guidelines on hypertension are complicated and can become outdated quickly, so this study investigated the benefits of evidence‐based treatment for hypertension using a computerised system. | This study used the pharmacist intervention recording system, which was used to document all pharmaceutical care interventions (Overhage 1999). This system gave the pharmacist care suggestions, which they could pass on to the physician. The physician used an order writing workstation to write orders for drugs, tests, nursing activities, and consultations (McDonald 1999). The workstation gave the physician care suggestions for the treatment of hypertension. | The pharmacist intervention recording system was used by intervention pharmacists to receive care suggestions. The pharmacist could fill the prescription as written, discuss the suggestions with the participant and encourage discussions between the participant and physician, or contact the ordering physician. The physician intervention used an order‐writing workstation to write orders for drugs, tests, nursing activities and consultations and display care suggestions. All hypertension care suggestions were displayed as suggested orders along with possible actions and a brief explanation of the rationale for the suggestion. | Pharmacists and physicians provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Home visits by physician assistants | Studies suggest that people who have undergone coronary artery bypass graft surgery benefit from a home intervention, but there are few studies of home visits by physicians or physician assistants. Therefore, this study examined the hospital readmissions of people who received home visits by physician assistants. | A physician assistant home care form/checklist was used to record all findings from the home visit. A copy of this form was provided in the paper. | Cardiothoracic physician assistants conducted home visits during which they performed a physical examination and reviewed the participant's medications. Adjustments were made to the participant's medications and new medications were prescribed as needed. The surgical wounds were examined and participant concerns were addressed. Prescriptions were written for antibiotics, blood work, or imaging studies. | Physician assistants provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist‐managed hypertension clinic | Hypertension can be controlled, but this study investigated whether it can be managed at a reasonable cost with minimal adverse effects by pharmacists. | Sitting blood pressure was measured with a Datascope Accutorr automated sphygmomanometer (Datascope Corporation Montvale, NJ, USA). 2 readings were taken for each participant and the average of the 2 readings was recorded (Datascope Patient Monitoring 1996). | Participants were counselled by a pharmacist who told them that efforts would be made to decrease the number of antihypertensive drugs or alter their therapy by giving more appropriate or less expensive drugs to achieve similar or improved blood pressure control. The pharmacist determined the most appropriate antihypertensive regimen for each participant, ordered laboratory tests as needed, and provided education on nonpharmacological ways to control blood pressure. | Clinical pharmacists provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Pharmacists work with participants in designing, implementing and monitoring therapeutic plans, but elderly people may have problems with adhering to their medication. This study looked at treatment adherence, as well as hospitalisations and mortality, in elderly people who received a home visit by a pharmacist along with telephone follow‐up. | Pharmacists adhered to a manual to deliver the intervention (Medication Review‐Managing Medicine Manual, Danmarks Apotekerforening, Pharmakon. Medicingennemgang 2004). This manual helps pharmacists identify and resolve drug‐related problems (Danmarks 2004). | Participants were visited at home by a pharmacist who examined the medicines list with regard to side‐effects, interactions and administration. The pharmacist tried to make the regime less complex, informed participants, and motivated adherence. | Pharmacists who had some practical experience or courses in medication review provided the intervention. | The intervention was delivered individually. It was conducted by telephone and face‐to‐face. | |
| Pharmacist medication review | People with end‐stage renal disease take multiple drugs and experience multiple co morbidities, which places them at greater risk of drug‐related problems. This paper looked at the effects of a pharmacist‐led intervention on drug‐related problems and hospitalisations in ambulatory patients undergoing haemodialysis. | Drug‐related problems were recorded, evaluated and assigned to 10 possible categories (Hepler 1990). The drug‐related problems were also categorised into therapeutic drug classes and the outcome related to the drug‐related problem intervention was captured. | Participants assigned to pharmaceutical care had drug therapy reviews conducted by a nephrology‐trained pharmacist. The pharmacist conducted a participant interview, generated a drug therapy profile, identified and addressed drug‐related problems, and provided healthcare‐provider and participant education. The pharmacist also provided consultative services that focused on optimising drug therapy. | The clinical pharmacists who conducted the intervention were either nephrology‐trained or completing postdoctoral training in nephrology pharmacotherapy. | The intervention was delivered individually and face‐to‐face. | |
| Medication review, nurse education, and development of professional relationships | Pharmacist‐conducted medication reviews and nurse education about medication use may have an impact on drug use in nursing homes. This study looked at the effect of medication review and nurse education on mortality and hospitalisations in nursing homes. | Problem‐based educational sessions were provided to nurses and addressed basic geriatric pharmacology and some common problems in long‐term care. No referenced documentation is provided for these sessions. | The intervention introduced a new professional role to stakeholders with relationship building, nurse education, and a medication review by pharmacists. Professional contact between nursing home staff and pharmacists on issues such as drug policy and resident problems was conducted along with problem‐based educational sessions for nurses. These sessions addressed geriatric pharmacology and problems in long‐term care. The medication reviews highlighted adverse drug effects, ceasing or adding drugs, better use of specific drug therapy, non‐drug interventions, and adverse effect and drug response monitoring. | Clinical pharmacists delivered the intervention. | The intervention was delivered individually and in groups over the phone and face‐to‐face. | |
| Structured home visits by GP and nurse | Many hospital admissions are due to inappropriate medical treatment, and the discharge of fragile elderly patients is associated with a high risk of readmission. This study examined whether home visits by GPs and district nurses reduced the risk of readmission of discharged elderly patients. | The joint home visits were guided by an agenda. During the structured home visit the agenda included checking the discharge letter for recommended follow‐up, checking the need for adjustment of medication, checking if social and personal support was arranged, and checking the family’s medicine cabinet. This agenda was provided in the article. | There was a joint home visit by the GP and district nurse approximately one week after discharge from the hospital. 2 more contacts were conducted by the GP in the GP's clinic or as a home visit. These visits included checking the discharge letter, checking the need for adjustment of medication, checking if social and personal support was arranged, and checking the family's medicine cabinet. | GPs and district nurses provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication reviews | Adverse drug events are frequently caused by cardiovascular drugs. Pharmacists can identify and resolve drug‐related problems for people at home and reduce re‐hospitalisation rates. This study investigated whether a pharmacist‐led intervention could reduce re‐hospitalisations and death in people with heart failure. | Using a predefined checklist, the pharmacist tried to reduce the use of inappropriate mediations, encourage smoking cessation, suggest improvements in the participant’s diet, and promote medication adherence, self‐monitoring, and vaccination. The checklist is not provided in the paper. | The pharmacist in the intervention group conducted an in‐home medication assessment and 2 follow‐up visits. This involved assessing and reviewing physician notes and laboratory test values and interacting with prescribers on behalf of the participants. The pharmacist catalogued all medications and interviewed the participant regarding medication use. | A clinical pharmacist, who had over 20 years of combined experience as a hospital and community pharmacist and had received a doctor of pharmacy degree and completed a 1‐year clinical residency in home care, provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Repeat prescribing is poorly managed in the UK, which puts people at risk. Pharmacists could review these prescriptions and reduce the pressure on GPs. This study tested whether pharmacists can review repeat prescriptions to reduce hospital admissions and deaths. | The process for reviewing repeat prescriptions involved discussing each condition with the participant and asking about symptoms (Lowe 2000). If clinical or pathological monitoring was due, the pharmacist directed the participant to the practice nurse or doctor. Participants with new clinical problems were referred to the doctor. | The pharmacists conducted a medication review during which they evaluated the therapeutic efficacy of each drug and the progress of the conditions being treated. Compliance, actual and potential adverse effects, interactions, and the participant’s understanding of the condition and its treatment were considered. The outcome of the review was a decision about the continuation of the treatment. | A pharmacist provided the medication review. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Elderly people take multiple medicines, which increases the risk of adverse drug events. Pharmacists can improve medicine management for elderly people in the community. In this study, the authors looked at whether a pharmacist‐led review would reduce hospitalisations and deaths among elderly people in nursing homes. | The clinical medication review (Lowe 2000), which was conducted by the pharmacist, comprised a review of the GP clinical record, and a consultation with the participant and carer. The pharmacist made recommendations and passed them on a written proforma to the GP for acceptance and recommendation. | The pharmacist conducted a medication review in which the pharmacist identified the drugs that were taken, identified the original indication for each drug, assessed adherence to medication, and identified unaddressed medical problems. They also considered the continuing need for each drug, identified side effects, identified drug interactions or contraindications, and considered costs. Finally, the pharmacist implemented and documented any changes. | The study pharmacist provided the intervention. | The intervention was delivered individually and face‐to‐face. |
GP: general practitioner
| Study | Location of intervention | When and how much of the intervention was delivered | Tailoring | Modifications | Adherence planning | Adherence assessment |
|---|---|---|---|---|---|---|
| 83 community pharmacies in the provinces of Asturias, Barcelona, Madrid and Biscay | The intervention was delivered once. | There was no tailoring made to the intervention. | Two additional seminars were given to the intervention group on real cases in order to approve the intervention. | Not undertaken | Not undertaken | |
| Community pharmacies in 7 European countries; Denmark, Germany, The Netherlands, Northern Ireland (co‐ordinating centre), Portugal, Republic of Ireland and Sweden. A minimum of 12 sites per country were chosen according to specific criteria set within each participating country relating to the population of elderly people who visited the pharmacy, staffing levels within the pharmacy and working relationships with local GPs. | The intervention was delivered at least once according to the study manual. However, Each site was free to provide as much information as possible to the intervention group as per the study manual. | A study manual describing the intervention was developed for all the participating countries. Each country translated the manual into their own language. | Each country adapted the manual, translating and modifying sections where appropriate, according to differing national practices. | Not undertaken | Not undertaken | |
| 7 Primary Health care clinics in Mataró and Argentona | The intervention included 3 phases and the participants were followed up for 12 months. It is not clear if the intervention was repeated more than once. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| 9 primary care physician practices in Washington State. Clinics were allowed to select their target condition of focus: frail older adults or people with diabetes. The physicians were board certified in Family Practice and did not have formal training or certification in geriatric medicine. | The intervention was undertaken once. However there was variability in the frequency of one of its components. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | A priori process of care measures for each of the geriatric syndromes were developed with decision rules for acceptable documentation by the study reviewers for the interventions. | The chart abstraction of assessing the documentation for the interventions was performed by one member of the study team along with an additional reviewer blinded to knowledge of the study group and study hypothesis. The overall level of agreement between the 2 reviewers was acceptable based on published ranges (kappas for geriatric syndrome process measures 0.75 to 0.85) | |
| Chronic care geriatric facilities in Central Israel | The intervention was done once at 6 months and 12 months later. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| A private organisation of 37 nursing homes in Spain | It is unclear how many times the intervention was given as the educator offered further on‐demand advice on prescription for the next 6 months. | There was no tailoring made to the intervention. | There was no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| Home health patients within a medicare insured home health population in Canada | The intervention was undertaken at least once however, some participants received more than one phone call as additional telephone follow‐up was provided as needed per the pharmacists' discretion during the first 30 days of the 60‐day home healthcare episode. | Some participants received additional follow‐up depending on their conditions. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| Large multispecialty group practice employing 265 physicians, including 66 primary care providers caring for adults in the outpatient setting | Daily records generated by the computer system were examined. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| 804‐bed academic medical centre in North Carolina, USA | The intervention took place once. | There was no tailoring made to the intervention. | Only hospitalisations and ED visits at the study institution were included for those participants who were not able to be contacted after 3 phone call attempts. | Not undertaken | Not undertaken | |
| Home‐based medication review after discharge from acute or community hospitals in Norfolk and Suffolk, UK. | The intervention was performed once. | It is possible that a small number of participants in both groups may have had their medication reviewed during the follow‐up period by their GP or community pharmacist. | There were no modifications made to the intervention during the study. | Not undertaken. No data on adherence were collected. | Not undertaken | |
| Telephone consultation with home visits | The intervention was performed once. | Any additional contact as requested by the participant in the intervention group was undertaken. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| Community‐based pharmacies in Canada | The intervention was performed once as planned. | The local lead organisations used several strategies to recruit volunteer peer health educators. These strategies included using the local lead organisation's existing volunteer base, advertising in the local media, and giving presentations at local seniors’ clubs. | When required, Cardiovascular Health Awareness Program support staff produced and mailed invitation letters on behalf of participating physicians (CHAP 2017). | Feedback of results was given to primary healthcare providers. | Evaluation data collected for the purpose of ongoing evaluation and quality improvement: 1. Success of different advertising/invitation strategies 2. Attendance, consent, completed assessments 3. Nurse assessments, pharmacist consults, fax/call to family physician the same day. Feedback to family physicians, pharmacists, and participants | |
| Outpatients clinic in Melbourne, Australia | The intervention was performed once as planned. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | There were written instructions on how to adjust the dose of frusemide per weight increase. | Data on dosage adjustment of frusemide were collected and compared against the initial criteria. | |
| General medical practices in the Grampian region of Scotland | The intervention was performed once as planned. | In the control group, when pharmacists considered a review to be serious and beneficial to the participants, an independent medical assessor decided on the need to withdraw the participants on clinical grounds. | There were no modifications made to the intervention during the study. | Any outstanding care issues in both groups were communicated to the participant's GP. | Not undertaken | |
| 25 nursing homes serviced by 2 long‐term care pharmacies in Northern Ireland | It is unclear the number of times the reports were generated and used by the pharmacists for every resident. | The Geriatric Risk Assessment MedGuide database software for falls and delirium was integrated into the pharmacies’ commercial pharmacy software system (Rescot LTCP System) for the intervention homes (Tobias 1999). | It is unclear if there were any modifications to the interventions. | The computer system did not capture if the recommendations done by the pharmacist were accepted. | Not undertaken | |
| A GP setting in Norfolk, UK | It is unclear how many times the pharmacist and the GP met to discuss participant's care plan. | A follow‐up visit with the participant occurred 6‐8 weeks later to reinforce the original advice, and assess whether there were any further pharmaceutical care issues to address with the GP. | It is unclear if there were any modifications to the interventions. | Not undertaken | Not undertaken | |
| The study was conducted within the NHS which provides free health care to the population of the UK. 27 primary care‐based pharmacists employed by the NHS to work with family doctors | It is unclear how many times the pharmacist met the participant and the GP. | If there was agreement between the pharmacist and the participant during the consultation and subsequently with the family doctor, medications were initiated, discontinued, or modified by the pharmacist during 3‐4 subsequent weekly or fortnightly consultations. | It is unclear if there were any modifications to the interventions. | Not undertaken | Not undertaken | |
| The study was conducted in 178 community pharmacies in Spain | It is unclear how many times the intervention was undertaken. | A specifically trained pharmacist called a practice change facilitator helped pharmacists of the intervention group in the provision of the medication review with follow‐up service, identifying barriers specific to each pharmacy and providing solutions. | It is unclear if there were any modifications to the interventions. | The practice change facilitator ensured fidelity to the intervention and supported pharmacists of both study groups on queries about documentation forms. | The experts were requested to answer individually for each case and the degree of agreement between them was later established. Inter‐rater reliability was measured using Fleiss's kappa. | |
| 9 Veterans Affairs medical centres in the USA | It is unclear how many times participants were seen by the pharmacist in the intervention group as the protocol indicated that each participant should have at least 3 visits with the clinical pharmacist during the study, but participants could be seen as frequently as deemed necessary to ensure appropriate care. | To prevent contamination, some sites marked medical records of intervention and control participants to alert clinical pharmacists that participants were in the study. Other sites noted this distinction in electronic medical records. One site distributed a list of participants enrolled in the study to all pharmacists providing primary care. | Clinical pharmacist intervention, however, occurred in one control participant; this participant was withdrawn from the study and his data were not included in the results. | Each contact with the participant was recorded on a standard data collection form that contained information about the method of contact, estimated time spent with the participant, medical problems addressed, drug‐related problems addressed, and drug‐related problems resolved. | Each month after enrolment the co‐ordinating centre received electronic data on each participant's prescription drugs dispensed in the preceding month. When participants either completed the study or died, data on resource use from enrolment to termination were retrieved. | |
| Ambulatory patients participating in the EuroHeart Failure Survey programme in Vienna | It is unclear how many times the nurse visited the intervention participants as more visits were made optional for participants. | More frequent contacts such as visits or telephone calls between the nurse and the participants were optional in case the participant or the nurse considered them necessary. | The nurse was in charge of individualised participant and caregiver education and enhancement of self‐management. If the nurse noted any deterioration in the participant's status, she reported to the treating physician or advised the participant to visit the treating physician. | Not undertaken | Not undertaken | |
| Academic primary care internal medicine practice in the USA | It is unclear how many times the intervention was undertaken. | There was no tailoring made to the intervention. | There were no modifications made to the interventions. | Data necessary to generate care suggestions were derived from the computer programme. Treatment suggestions fell into 5 major categories. | Not undertaken | |
| Ambulatory patients discharged from a large 702‐bed hospital in Staten University Hospital, USA | It is unclear how many times the physician visited each participant in the home after their discharge. | There was no tailoring made to the intervention. | There were some modifications done to the intervention due to the participants not being available at the weekend. Participants were not seen directly after discharge as per the study protocol. | All findings were documented on the intervention visit form. | It is unclear if this was undertaken. | |
| Managed care organisation in California, USA | It is unclear how many times participants were seen by the pharmacist in the intervention group as additional follow‐up was organised by the pharmacists for some participants. | Additional follow‐up was organised by the pharmacists for some participants. | The intervention was not modified. | Not undertaken | Not undertaken | |
| Patients living at home in the municipality of Aarhus, Denmark | The intervention was performed at the intended follow‐up. | Pharmacists could consult the project physician if they considered a participant's medication problems to be life‐threatening. | The intervention was not modified. | Adherence to the medications were assessed by a pill‐count in all participants during 1 year. | Pill count was undertaken | |
| The study took place in a non‐profit university‐affiliated dialysis clinic in Albany, USA. | It is unclear if all participants received the same number of follow‐up visits by the pharmacist or the physician in the intervention group. | It is unclear if there was any tailoring made to the intervention. | The intervention was not modified. | Not undertaken | Not undertaken | |
| 52 nursing homes located in south‐east Queensland and north‐east New South Wales, Australia | There was variability in the number of educational sessions provided to staff in each nursing home as well as the number of visits by the intervention pharmacists. | It is unclear if there was any tailoring made to the intervention. | It is unclear if the intervention was modified. | Validation of prescription claim data with participants' medications profiles. | To validate prescription claims data, a sample of 1328 cross‐sectional medication profiles were collected for 8 nursing home clusters for control and intervention homes at post‐intervention. An audit, comparing original post‐intervention medication data with the same data recollected up to 6 weeks later for a 6%, random sample, showed an overall reproducibility of 97% (range 92% to 100%) | |
| Patients discharged from Glostrup Hospital, Denmark. | The intervention was performed as prescribed. | There was no tailoring made to the intervention. | There was no modification made to the intervention. | Not undertaken | Not undertaken | |
| Heart failure patients discharged from hospital in Albany, Scotland | The intervention was performed as prescribed. | The clinical pharmacist accessed and reviewed all pertinent physician notes and laboratory test values via the National Endowment for the Humanities data system and interacted with prescribers on behalf of the participants, as necessary. | There was no modification made to the intervention. | Not undertaken | Not undertaken | |
| 4 GPs in Leeds, UK | It is unclear how many times the pharmacist visited the participant. | Immobile participants were visited at home. Non‐attenders were invited once more by telephone. | The study authors agreed with each practice the level of intervention that the pharmacist could make without seeking prior approval | It is unclear if this was undertaken. | It is unclear if this was undertaken. | |
| 65 care homes for the elderly in Leeds, UK | It is unclear how many times the pharmacist reviewed each participant. | There was no tailoring made to the intervention. | There was no modification made to the intervention. | Pharmacists filled in a proforma sheet including their recommendations. | GP acceptance of the recommendations was signified by ticking a box on the proforma. |
ED: emergency department; GP: general practitioner; NHS: National Health Service
Participants and study setting
There is a great deal of diversity in types of professionals involved and where the studies occurred. However, most (61%) of the interventions were conducted by pharmacists or a combination of pharmacists and medical doctors. The studies took place in many different countries; 65% took place in either the USA or the UK. The study settings included general practices (Coleman 1999; Gurwitz 2014; Krska 2001; Lowrie 2012; Murray 2004;Zermansky 2001), community pharmacies (Alvarez 2001; Bernsten 2001; Malet‐Larrea 2016), patient homes or community settings (Campins 2016; Gernant 2016; Kaczorowski 2011; Holland 2005; Ibrahim 2013; Lenaghan 2007; Olesen 2014; Rytter 2010; Triller 2007), outpatient clinics (Hawes 2014; Korajkic 2011; Malone 2000; Moertl 2009; Okamoto 2001;Pai 2009), and aged care facilities (Frankenthal 2014; Garcia‐Gollarte 2014; Lapane 2011; Roberts 2001; Triller 2007;Zermansky 2006).
Interventions
We included a total of 30 studies (169,969 participants) in this review.
Four studies (8266 participants) reported on professional interventions (Garcia‐Gollarte 2014; Gurwitz 2014; Lapane 2011; Murray 2004). Two of these studies (3889 participants) reported on the number of hospital admissions (Lapane 2011; Murray 2004), one study (3661 participants) reported on the number of people admitted to hospital (Gurwitz 2014), one study (3538 participants) reported on mortality (Lapane 2011), and two studies (1067 participants) reported on the number of emergency department visits (Garcia‐Gollarte 2014; Murray 2004).
A total of 26 studies (161,703 participants) reported on organisational interventions (Alvarez 2001; Bernsten 2001; Campins 2016; Coleman 1999; Frankenthal 2014; Gernant 2016; Hawes 2014; Holland 2005; Ibrahim 2013; Kaczorowski 2011; Korajkic 2011; Krska 2001; Lenaghan 2007; Lowrie 2012; Malet‐Larrea 2016; Malone 2000; Moertl 2009; Nabagiez 2013; Okamoto 2001; Olesen 2014; Pai 2009; Roberts 2001; Rytter 2010; Triller 2007; Zermansky 2001; Zermansky 2006). Eleven trials (6203 participants) reported on number of hospital admissions (Coleman 1999; Holland 2005; Ibrahim 2013; Krska 2001; Lenaghan 2007; Lowrie 2012; Malone 2000; Moertl 2009; Nabagiez 2013; Okamoto 2001;Rytter 2010). A total of 13 studies (152,237 participants) reported on the number of people admitted to hospital (Alvarez 2001; Bernsten 2001; Campins 2016; Frankenthal 2014; Hawes 2014; Kaczorowski 2011; Korajkic 2011; Malet‐Larrea 2016; Nabagiez 2013; Olesen 2014; Triller 2007; Zermansky 2001; Zermansky 2006). Five studies (1819 participants) reported on emergency department visits (Alvarez 2001; Coleman 1999; Gernant 2016; Hawes 2014; Ibrahim 2013), and 12 studies (154,962 participants) reported on mortality (Campins 2016; Holland 2005; Kaczorowski 2011; Lenaghan 2007; Lowrie 2012; Moertl 2009; Olesen 2014; Pai 2009; Roberts 2001; Triller 2007; Zermansky 2001; Zermansky 2006).
We did not find any studies that fitted the criteria of structural interventions. This was in concordance with the EPOC taxonomy of interventions (Appendix 1).
The 'Characteristics of included studies' tables provide a summary of the interventions and comparisons. The interventions varied. Professional interventions included the use of health information technology to identify people at risk of medication problems: computer‐generated care suggested and actioned by physicians; electronic notification system about dose changes, drug interventions and follow‐up; and educational interventions on drug use aimed at physicians to improve drug prescriptions. Organisational interventions included medication reviews by pharmacists, nurses or physicians, clinician‐led clinics and home visits by clinicians.
Outcomes
The primary outcomes were number of hospital admissions and number of people admitted to hospital. A total of 13 studies (10,092 participants) reported on number of hospital admissions (Coleman 1999; Holland 2005; Ibrahim 2013; Krska 2001; Lapane 2011; Lenaghan 2007; Lowrie 2012; Malone 2000; Moertl 2009; Murray 2004; Nabagiez 2013; Okamoto 2001; Rytter 2010); and 14 studies (155,898 participants) reported on number of people admitted to hospital (Alvarez 2001; Bernsten 2001; Campins 2016; Frankenthal 2014; Kaczorowski 2011; Gurwitz 2014; Hawes 2014; Korajkic 2011; Malet‐Larrea 2016; Nabagiez 2013; Olesen 2014; Triller 2007; Zermansky 2001;Zermansky 2006).
The secondary outcomes were the number of emergency department visits and mortality. Seven studies (2886 participants) reported on the number of emergency department visits (Alvarez 2001; Coleman 1999; Garcia‐Gollarte 2014; Gernant 2016; Hawes 2014; Ibrahim 2013; Murray 2004); and 13 studies (158,500 participants) reported on mortality (Campins 2016; Holland 2005; Kaczorowski 2011; Lenaghan 2007; Lapane 2011; Lowrie 2012; Moertl 2009; Olesen 2014; Pai 2009; Roberts 2001; Triller 2007; Zermansky 2001; Zermansky 2006).
Excluded studies
We have summarised the 59 excluded studies, with the reasons for their exclusion in the 'Characteristics of excluded studies' table. We excluded studies with an unsuitable design (Furniss 2000; Graffen 2004; Hugtenburg 2009; Lee 1996; Leendertse 2011; Leendertse 2013; Mills 2001; Montero‐Balosa 2016; Moreno 2016; Ni 2016; Safran 1993; Saltzberg 2011). Other reasons for exclusion were studies that did not occur in a primary care setting (Alassaad 2014; Barker 2012; Bell 2016; Bonnet‐Zamponi 2013; Briggs 2015; Gorgas 2012; Hanlon 1996; Keane 2014; Naunton 2003; Neven 2016; Xin 2014); results reported elsewhere (Sturgess 2003); data for outcomes not available (Cowper 1998; Knowlton 1994; Liu 2010; Yuan 2003); interventions not relevant to the review (Al‐Arifi 2014; Benard‐Laribiere 2015; Carrington 2013; Fredericks 2013; Pinnock 2013); outcomes not relevant to the review (Barker 2016; Barnes 2014; Basheti 2016; Billington 2015; Clyne 2015; Clyne 2016; Dhalla 2014; Geurts 2016; Guthrie 2016; Hallsworth 2016; Huiskes 2014; Malin 2016; Perula 2014; Setter 2009; Sinnott 2015; Wolf 2015); and 10 studies were published protocols (Alicic 2016; Bhatt 2014; Clyne 2013; Desveaux 2016; Elliott 2014; Forster 2015; Phung 2013; Przytula 2015; Stingl 2016; Wooster 2016), as described in the PRISMA diagram (see Figure 1).
Risk of bias in included studies
We have presented details of risk of bias in Figure 2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
A total of 21 studies reported adequate sequence generation (Bernsten 2001; Campins 2016; Frankenthal 2014; Garcia‐Gollarte 2014; Gernant 2016; Gurwitz 2014; Hawes 2014; Holland 2005; Kaczorowski 2011; Krska 2001; Lowrie 2012; Malet‐Larrea 2016; Malone 2000; Okamoto 2001; Olesen 2014; Pai 2009; Roberts 2001; Rytter 2010; Triller 2007; Zermansky 2001; Zermansky 2006); and 18 reported adequate concealment of allocation (Bernsten 2001; Campins 2016; Frankenthal 2014; Gernant 2016; Gurwitz 2014; Hawes 2014; Holland 2005; Kaczorowski 2011; Lenaghan 2007; Lowrie 2012; Malone 2000; Malet‐Larrea 2016; Murray 2004; Pai 2009; Roberts 2001; Rytter 2010; Triller 2007;Zermansky 2001).
Blinding
Thirteen studies adequately blinded measurements of participants and personnel delivering the intervention (Bernsten 2001; Campins 2016; Coleman 1999; Garcia‐Gollarte 2014; Gernant 2016; Gurwitz 2014; Kaczorowski 2011; Krska 2001; Lapane 2011; Lowrie 2012; Murray 2004; Pai 2009; Triller 2007), whereas adequate blinding of outcome assessment was undertaken in 19 studies (Bernsten 2001; Campins 2016; Frankenthal 2014; Garcia‐Gollarte 2014; Gurwitz 2014; Hawes 2014; Holland 2005; Kaczorowski 2011; Korajkic 2011; Krska 2001; Malet‐Larrea 2016; Murray 2004; Nabagiez 2013; Olesen 2014; Pai 2009; Roberts 2001; Rytter 2010; Triller 2007;Zermansky 2006). Eleven studies reported an unclear risk of detection bias (Alvarez 2001; Coleman 1999; Gernant 2016; Ibrahim 2013; Lapane 2011; Lenaghan 2007; Lowrie 2012; Malone 2000; Moertl 2009; Okamoto 2001;Zermansky 2001).
Incomplete outcome data
A total of five studies had high risk of attrition bias (Alvarez 2001; Bernsten 2001; Hawes 2014; Nabagiez 2013; Pai 2009). Twenty‐two studies adequately addressed problems with incomplete outcomes (Campins 2016; Frankenthal 2014; Gernant 2016; Gurwitz 2014; Holland 2005; Ibrahim 2013; Kaczorowski 2011; Korajkic 2011; Krska 2001; Lapane 2011; Lenaghan 2007; Lowrie 2012; Malet‐Larrea 2016; Malone 2000; Moertl 2009; Okamoto 2001; Olesen 2014; Roberts 2001; Rytter 2010; Triller 2007; Zermansky 2001; Zermansky 2006), that is, these studies reported complete outcome data or they replaced any missing outcome data using a recognised statistical method, such as last observation carried forward with participants remaining in the group to which they had been allocated.
Selective reporting
There was no selective reporting in the included studies. All studies assessed their predefined primary and secondary outcomes.
Other potential sources of bias
Other potential sources of bias included protection against contamination, publication bias and other bias.
Protection against contamination bias
A total of 12 studies adequately protected against contamination bias (Bernsten 2001; Coleman 1999; Gernant 2016; Lapane 2011; Lowrie 2012; Murray 2004; Nabagiez 2013; Olesen 2014; Pai 2009; Roberts 2001; Rytter 2010; Triller 2007); whereas 16 studies, had unclear risk of protection against contamination (Alvarez 2001; Campins 2016; Frankenthal 2014; Gurwitz 2014; Hawes 2014; Holland 2005; Ibrahim 2013; Kaczorowski 2011; Korajkic 2011; Lenaghan 2007; Malet‐Larrea 2016; Malone 2000; Moertl 2009; Okamoto 2001; Zermansky 2001; Zermansky 2006), and two studies clearly did not adequately protect against contamination bias (Garcia‐Gollarte 2014; Krska 2001). Contamination bias occurs when members of the control group are inadvertently exposed to the intervention, thus potentially minimising the difference in outcomes between the two groups (Higgins 2011b).
Publication bias
Publication bias did not take place amongst the professional interventions due to the small number of studies included in the review. We have shown funnel plots of the main outcomes for the organisational interventions as follows: number of hospital admissions (Figure 3); number of people admitted to hospital (Figure 4); number of emergency department visits (Figure 5); and mortality (Figure 6). There was no evidence of publication bias.

Funnel plot of comparison: 2 Organisational interventions, outcome: 2.1 Number of hospital admissions

Funnel plot of comparison: 2 Organisational interventions, outcome: 2.2 Number of people admitted to hospital

Funnel plot of comparison: 2 Organisational interventions, outcome: 2.3 Number of emergency department visits

Funnel plot of comparison: 2 Organisational interventions, outcome: 2.4 Mortality
Other bias
A total of 22 studies had an unclear risk of 'other bias' (Bernsten 2001; Campins 2016; Coleman 1999; Gernant 2016; Gurwitz 2014; Hawes 2014; Ibrahim 2013; Korajkic 2011; Krska 2001; Lapane 2011; Lowrie 2012; Malet‐Larrea 2016; Malone 2000; Murray 2004; Nabagiez 2013; Okamoto 2001; Olesen 2014; Pai 2009; Roberts 2001; Rytter 2010; Zermansky 2001;Zermansky 2006). Seven studies had a high risk of 'other bias' (Alvarez 2001; Frankenthal 2014; Garcia‐Gollarte 2014; Kaczorowski 2011; Lenaghan 2007; Moertl 2009;Triller 2007), while only one study had a low risk of 'other bias' (Holland 2005). Other biases included inappropriate administration of the intervention, such as the method of training used to deliver the intervention or level of knowledge of the health professional delivering the intervention. Short length of the intervention was a bias in some studies (Kaczorowski 2011;Triller 2007), with the level of knowledge of the pharmacist or health professional delivering the intervention a bias in other studies. For example, in the study by Lenaghan 2007, research was carried out in one rural general practice with a single experienced review pharmacist, which may have had a bearing on the generalisability of the results.
In Bernsten 2001, one aspect of the study that was not rigorously controlled was the training of participating pharmacists. A study manual was provided to each participating pharmacist, followed by a one‐day training session. Further training was provided in individual countries; however, the extent of this was driven by available resources. Other biases include small sample sizes in the intervention arms; with 48 participants in Moertl 2009 and 77 participants in Triller 2007, and poor pharmacist‐prescriber communication, which may have reduced the efficacy of the intervention (Triller 2007). Alvarez 2001 did not report on any pre‐intervention data for most of the outcome measures. Garcia‐Gollarte 2014 had a short intervention of a six‐month period and a short follow‐up of three months. Frankenthal 2014 conducted the study in only one geriatric centre.
There was a total of eight cluster‐randomised studies included in the review (Alvarez 2001; Coleman 1999; Gernant 2016; Kaczorowski 2011; Lapane 2011; Lowrie 2012; Malet‐Larrea 2016; Roberts 2001). Cluster‐randomised studies include other potential biases such as recruitment bias and complete loss of a cluster in a trial. The extent of this type of bias was not fully reported and therefore we considered it under this section.
Effects of interventions
See: Summary of findings 1 Professional interventions compared to standard/usual care for prevention of medication errors; Summary of findings 2 Organisational interventions compared to standard/usual care for prevention of medication errors
Professional interventions
We performed a meta‐analysis on the number of hospital admissions and the number of emergency department visits, as they were the only outcomes reported by more than one study. We have presented effect estimates and certainty of evidence for each outcome in summary of findings Table 1 (see Appendix 3 for the full GRADE evidence profile). We obtained all reported data from the published papers.
Primary outcomes
We measured hospital admissions as either the number of hospital admissions or the number of people admitted to hospitals.
1. Number of hospital admissions
Two studies (3889 participants) reported on the number of hospital admissions (Lapane 2011; Murray 2004). Overall, professional interventions in health information technology to identify people at risk of medication problems in the case of Lapane 2011, or the computer‐generated care suggested and actioned by the physician described by Murray 2004, reported an increase in the number of hospital admissions, but the 95% confidence interval (CI) indicates that it probably makes little or no difference (risk ratio (RR) 1.24, 95% CI 0.79 to 1.96; moderate‐certainty evidence). There was no significant heterogeneity (I2 = 0%, P = 0.44) across the studies, as shown in summary of findings Table 1.
2. Number of people admitted to hospital
One study (3661 participants) reported on number of people admitted to hospital (Gurwitz 2014). The study authors found that the intervention, which included an electronic notification system about dose changes, drug interactions, and follow‐up, made little or no difference to the number of people admitted to hospital (adjusted RR 0.99, 95% CI 0.92 to 1.06; high‐certainty evidence).
Secondary outcomes
1. Number of emergency department visits
Two studies (1067 participants) reported on this outcome (Garcia‐Gollarte 2014; Murray 2004). Garcia‐Gollarte 2014 described an educational intervention on drug use aimed at physicians to improve drug prescriptions. Murray 2004 described an intervention including computer‐generated care suggested and actioned by the physician. Both professional interventions described by the study authors may make little or no difference to the number of emergency department visits (adjusted RR 0.71, 95% CI 0.50 to 1.02; low‐certainty evidence). There was no significant heterogeneity among the two studies (I2 = 0%, P = 0.64).
2. Mortality
One study (3538 participants) reported on the number of deaths (Lapane 2011). The health information technology to identify people at risk of medication problems probably makes little or no difference to the number of deaths in the study population (adjusted RR 0.98, 95% CI 0.82 to 1.17; moderate‐certainty evidence).
Organisational interventions
We performed a meta‐analysis on the number of hospital admissions, number of people admitted to hospital, the number of emergency department visits, and mortality. We have presented effect estimates and certainty of evidence for each outcome in summary of findings Table 2 (see Appendix 4 for the full GRADE evidence profile). We obtained all reported data from the published papers.
Primary outcome
1. Number of hospital admissions
Eleven trials (6203 participants) reported on the number of hospital admissions (Coleman 1999; Holland 2005; Ibrahim 2013; Krska 2001; Lenaghan 2007; Lowrie 2012; Malone 2000; Moertl 2009; Nabagiez 2013; Okamoto 2001; Rytter 2010). The organisational interventions included medication reviews by pharmacists, nurses or physicians, clinician‐led clinics, and home visits by clinicians. Most interventions included optimisation of the medications that participants were taking or home visits by healthcare practitioners, or both. Overall, it is uncertain whether organisational interventions (which included pharmaceutical care or medication reviews by a doctor, a pharmacist, or a nurse, home visits, educational interventions with a pharmacist) reduce the number of hospital admissions (adjusted RR 0.85, 95% CI 0.71 to 1.03; very low‐certainty evidence. There was significant heterogeneity (I2 = 75%, P < 0.0001) across the studies (Analysis 2.1). The direction of the effect was consistent in 10 out of 11 trials. Holland 2005 reported an increase in the total number of hospital admissions (adjusted RR 1.31, 95% CI 1.13 to 1.50; based on very low‐certainty evidence. The study authors explained these findings by indicating that their study was not statistically powered to detect changes in hospital admissions and new admissions. The study authors explained the unusual increase in hospital admissions among participants by concluding that the participants were better informed about adverse events through the pharmacist intervention, and this promoted help‐seeking behaviour, which resulted in an admission.
We undertook a sensitivity analysis by removing studies at high risk of bias (Holland 2005; Krska 2001; Moertl 2009; Nabagiez 2013), and again it is uncertain whether organisational interventions (which included pharmacist home visits, pharmaceutical care plan, home‐based nurse care and home visits by physician assistants) reduce the number of hospital admissions (adjusted RR 0.86, 95% CI 0.72 to 1.03). Ibrahim 2013, Moertl 2009 and Rytter 2010 showed a reduction in hospital admissions with a relatively narrow confidence interval: adjusted RR 0.40, 95% CI 0.22 to 0.74 (Ibrahim 2013); RR 0.38, 95% CI 0.19 to 0.72 (Moertl 2009); and RR 0.76, 95% CI 0.61 to 0.95 (Rytter 2010), in favour of the interventions. These three studies were characterised by frequent follow‐up by the clinical pharmacists. In the case of Ibrahim 2013, there was a three‐month follow‐up and a once‐a‐week telephone conversation; Moertl 2009 had frequent follow‐up by the clinical pharmacists at three, six, nine, and 12 months; and Rytter 2010 also had three follow‐up contacts by GPs and district nurses.
2. Number of people admitted to hospital
A total of 13 studies (152,237 participants) reported on the number of people admitted to hospital (Alvarez 2001; Bernsten 2001; Campins 2016; Frankenthal 2014; Hawes 2014; Kaczorowski 2011; Korajkic 2011; Malet‐Larrea 2016; Nabagiez 2013; Olesen 2014; Triller 2007; Zermansky 2001; Zermansky 2006). Most of the organisational interventions described included medication reviews by pharmacists, nurses or physicians, clinician‐led clinics, and home visits by clinicians. Overall, organisational interventions may make little or no difference to the total number of people admitted to hospital in favour of the intervention group compared with the control group (adjusted RR 0.92, 95% CI 0.86 to 0.99; low‐certainty evidence) with significant heterogeneity (I2 = 47%, P = 0.03). Three studies showed that the organisational interventions reduced the total number of people admitted to hospital, as the RR was less than 1 (Bernsten 2001; Hawes 2014; Malet‐Larrea 2016).
We undertook a sensitivity analysis by removing studies at high risk of bias (Alvarez 2001; Bernsten 2001; Frankenthal 2014; Hawes 2014; Kaczorowski 2011; Malet‐Larrea 2016; Nabagiez 2013; Triller 2007), and again, the intervention made little or no difference to the number of people admitted to hospital (adjusted RR 0.98, 95% CI 0.85 to 1.13) with low, non‐significant heterogeneity between studies (I2 = 28%, P = 0.23).
Secondary outcomes
1. Number of emergency department visits
Five studies (1819 participants) reported on emergency department visits (Alvarez 2001; Coleman 1999; Gernant 2016; Hawes 2014; Ibrahim 2013). Overall, it is uncertain whether organisational interventions including medication reviews by pharmacists, nurses or physicians, clinician‐led clinics, and home visits by clinicians reduce emergency department visits in favour of the intervention group compared with the control group (adjusted RR 0.75, 95% CI 0.49 to 1.15; very low‐certainty evidence). Please refer to summary of findings Table 2.
There was also significant heterogeneity between the studies (I2 = 73%, P = 0.005). We undertook a sensitivity analysis by removing studies at high risk of bias (Alvarez 2001; Hawes 2014). Pharmaceutical care and care transition clinic interventions may make little or no difference in emergency department visits (adjusted RR 0.68, 95% CI 0.37 to 1.27) with significant heterogeneity between studies (I2 = 79%, P = 0.009).
All studies showed wide confidence intervals, and although Alvarez 2001 showed an increase in the number of emergency department visits in favour of the intervention, this study had high risk of bias as there was a high proportion of incomplete data in the outcomes measured.
2. Mortality
A total of 12 studies (154,962 participants) reported on mortality (Campins 2016; Holland 2005; Kaczorowski 2011; Lenaghan 2007; Lowrie 2012; Moertl 2009; Olesen 2014; Pai 2009; Roberts 2001; Triller 2007; Zermansky 2001; Zermansky 2006). Overall, it is uncertain whether organisational interventions, which included medication reviews by pharmacists, nurses or physicians, clinician‐led clinics, and home visits by clinicians reduce mortality in favour of the intervention group (adjusted RR 0.94, 95% CI 0.85 to 1.03; very low‐certainty evidence) with non‐significant heterogeneity (I2 = 37%, P = 0.10). Please refer to summary of findings Table 2.
We undertook sensitivity analysis by removing studies at high risk of bias (Holland 2005; Kaczorowski 2011; Lenaghan 2007; Moertl 2009; Olesen 2014; Roberts 2001), and we found that interventions addressing home visits by pharmacists, educational sessions to assess cardiovascular risk, medication reviews, home‐based nurse care, and nurse education probably made little or no difference to mortality (adjusted RR 1.02, 95% CI 90 to 1.17). There was no significant heterogeneity between studies after the removal of the six studies (I2 = 0%, P = 0.45).
Structural interventions
We did not find any studies that fitted the criteria of structural interventions.
Discussion
Summary of main results
The studies included in this Cochrane Review showed that, based on moderate‐ and low‐certainty evidence, interventions in primary care for reducing preventable medication errors probably make little or no difference to the number of people admitted to hospital or the number of hospitalisations, emergency department visits, or mortality. Most of the interventions took place in the UK and the USA; studies undertaken in high‐income countries with disadvantaged populations, and in low‐ and middle‐income countries, were underrepresented. This might affect the generalisability of the results. We undertook sensitivity analysis by removing studies at high risk of bias and detecting whether there was any difference on the overall effect size. Overall, there is no evidence of an effect in any of the outcomes.
Overall completeness and applicability of evidence
The types of interventions included in this review were based on the taxonomy of interventions developed by Cochrane EPOC (Appendix 1); four studies used professional interventions and 26 studies used organisational interventions. The professional interventions included the use of health information technology to identify people at risk of medication problems: computer‐generated care suggested and actioned by a physician; electronic notification systems about dose changes, drug interventions and follow‐up; and educational interventions on drug use aimed at physicians to improve drug prescriptions. Organisational interventions consisted of medication reviews by pharmacists, nurses or physicians, clinician‐led clinics and home visits by clinicians.
The interventions described in the review were complex and generally multifaceted, which resulted in significant heterogeneity. The variation in heterogeneity in the pooled estimates means that our results should be treated cautiously as the interventions may not have worked consistently across all studies due to differences in how the interventions were provided, background practice, setting, healthcare system, or delivery of the interventions. Another potential limitation is the quality of the studies. The methods sections of the studies provided varying levels of detail on how complex interventions were developed, the design of the trials or how staff were trained to deliver the interventions. There was also evidence of potential bias in some studies, with only 18 studies reporting adequate concealment of allocation and only 12 studies reporting appropriate protection from contamination, both of which may have influenced the overall effect estimate and the overall pooled estimate.
Certainty of the evidence
The certainty of the evidence obtained from the 'Summary of findings' tables using the GRADE system highlights the very low to high certainty of the evidence reported by the studies. The primary outcomes of number of hospital admissions and number of people admitted to hospital were reported to have very low‐ to high‐certainty evidence, respectively. Mortality was reported in 13 studies (1 study involving professional interventions, moderate‐certainty evidence; and 12 studies involving organisational interventions, very low‐certainty evidence), with the main type of biases being detection and performance bias. We considered studies reporting on emergency department visits to have low‐certainty evidence for professional interventions and very low‐certainty evidence for organisational interventions using the GRADE system, due to study design and heterogeneity. Further research and better study designs are likely to change the overall estimate reported using these outcomes.
The Methods sections provided few details about study methodology and how complex interventions were delivered. The overall quality of the evidence presented in this review is either at high risk or unclear risk of bias. The main limitations were the heterogeneity between studies, the imprecision in results due to the wide confidence intervals amongst studies, unclear selection bias, performance and detection bias, and attrition bias.
Potential biases in the review process
The number of studies that we were able to combine in the meta‐analysis was somewhat small due to subclassification of the interventions and because not all studies reported on all the outcomes of interest mentioned in the review. We did not place any language restrictions on the search strategy. The review included one study written in Spanish (Alvarez 2001). We were able to pool the data from this study with the help of a Spanish‐speaking colleague. Despite the limited number of studies that were included, funnel plots of studies reporting the outcomes of interest showed no apparent publication bias (Figure 3; Figure 4; Figure 5; Figure 6). Another limitation of the review included the definitions of 'pharmaceutical care' and 'pharmaceutical review' described in the studies, which may have led to different interventions. We also did not consider studies where participants were treated in the emergency department of hospitals, although we are aware that at times people could receive treatment in the emergency department without being admitted to hospital. We will consider these types of studies in our updated review. Finally, a sensitivity analysis with a separate comparison of cluster‐ and individual randomised trials may have yielded different results, and we will consider including this in our updated review.
Agreements and disagreements with other studies or reviews
Few studies have examined whether the types of interventions that were investigated in this review lead to reductions in hospital admissions, emergency department visits, or mortality. One of the few reviews that studied this problem (Royal 2006), found that pharmacist‐led medication reviews were effective in reducing hospital admissions, although restricting the analysis to randomised trials did not produce a significant benefit.
Previous observational studies addressing similar interventions also provide limited evidence of their effectiveness. A controlled study by Hugtenburg 2009, which included 37 community pharmacists and 715 participants, and examined the impact of medication reviews and participant counselling at discharge from the hospital by community pharmacists, found that the intervention was not effective at reducing mortality. Another open controlled study, conducted by Leendertse 2013, examined the effect of reviewing medications in primary care by pharmacists. They found that the intervention did not significantly reduce medication‐related hospital admissions. Moreover, a study by Safran 1993 examined the effect of an electronic medical record used by physicians to care for people with HIV on hospitalisation, emergency visits and mortality. The study authors found that the intervention was significant for emergency department visits, but not for mortality or hospitalisations. Our study mirrors these findings in that the interventions investigated in this review had little or no effect on the number of people admitted to hospital, number of hospital admissions, number of emergency department visits, or mortality.

Study flow diagram

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Funnel plot of comparison: 2 Organisational interventions, outcome: 2.1 Number of hospital admissions

Funnel plot of comparison: 2 Organisational interventions, outcome: 2.2 Number of people admitted to hospital

Funnel plot of comparison: 2 Organisational interventions, outcome: 2.3 Number of emergency department visits

Funnel plot of comparison: 2 Organisational interventions, outcome: 2.4 Mortality

Comparison 1: Professional interventions versus standard care, Outcome 1: Number of hospital admissions

Comparison 1: Professional interventions versus standard care, Outcome 2: Number of people admitted to hospital

Comparison 1: Professional interventions versus standard care, Outcome 3: Number of emergency department visits

Comparison 1: Professional interventions versus standard care, Outcome 4: Mortality

Comparison 2: Organisational interventions versus standard care, Outcome 1: Number of hospital admissions

Comparison 2: Organisational interventions versus standard care, Outcome 2: Number of people admitted to hospital

Comparison 2: Organisational interventions versus standard care, Outcome 3: Number of emergency department visits

Comparison 2: Organisational interventions versus standard care, Outcome 4: Mortality
| Professional interventions compared to standard/usual care for prevention of medication errors | ||||||
| Patient or population: adults receiving medication in primary care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with standard/usual care | Risk with professional interventions | |||||
| Number of hospital admissions | Study population | RR 1.24 | 3889 | ⊕⊕⊕⊝ | The two studies had wide confidence intervals. | |
| 17 per 1000 | 21 per 1000 | |||||
| Number of people admitted to hospital | Study population | RR 0.99 | 3661 | ⊕⊕⊕⊕ | ||
| 448 per 1000 | 443 per 1000 | |||||
| Number of emergency department visits | Study population | RR 0.71 | 1067 | ⊕⊕⊝⊝ | The two studies had wide confidence intervals and selection bias. | |
| 118 per 1000 | 85 per 1000 | |||||
| Mortality | Study population | RR 0.98 | 3538 | ⊕⊕⊕⊝ | ||
| 122 per 1000 | 119 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1We downgraded one level due to imprecision. | ||||||
| Organisational interventions compared to standard/usual care for prevention of medication errors | ||||||
| Patient or population: adults receiving medication in primary care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with standard/usual care | Risk with organisational interventions | |||||
| Number of hospital admissions | Study population | RR 0.85 | 6203 | ⊕⊝⊝⊝ | Some studies had unclear risk of bias (selection and attrition), high heterogeneity and wide confidence intervals. | |
| 274 per 1000 | 233 per 1000 | |||||
| Number of people admitted to hospital | Study population | RR 0.92 | 152,237 | ⊕⊕⊝⊝ | Some studies had unclear risk of bias (selection, attrition and performance bias) and wide confidence intervals. | |
| 13 per 1000 | 13 per 1000 | |||||
| Number of emergency department visits | Study population | RR 0.75 | 1819 | ⊕⊝⊝⊝ | Studies had unclear risk of bias (selection, performance and attrition bias), high heterogeneity and wide confidence intervals. | |
| 234 per 1000 | 176 per 1000 | |||||
| Mortality | Study population | RR 0.94 | 154,962 | ⊕⊝⊝⊝ | Studies had high risk of selection, attrition and performance bias and wide confidence intervals. | |
| 50 per 1000 | 47 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1We downgraded one level for unclear risk of bias (selection and attrition bias). | ||||||
| Study | Name | Theory | Materials | Procedures | Who provided intervention | Modes of delivery |
|---|---|---|---|---|---|---|
| Pharmaceutical care | Pharmaceutical care is the provision of drug therapy for the purpose of achieving outcomes that improve a person’s quality of life. | Pharmacies in the intervention group provided pharmaceutical care, which consisted of offering the pharmaceutical care service to participants and to their corresponding GPs. | An Initial interview and assessment of the therapeutic plan was undertaken, registration of data during the subsequent visits to allow the identification of medication‐related problems, and an intervention to solve the problem. The intervention involved proposing changes in the medication participants received, which had to be communicated to the patient’s GP. | Pharmacists provided the intervention. | Individual and face‐to‐face | |
| Pharmaceutical care | Pharmaceutical care is the provision of drug therapy for the purpose of achieving outcomes that improve a person's quality of life, although little research has been conducted in community‐based pharmaceutical care with elderly people. | Training of pharmacists was done with a study manual. The manual contained an overview of the concept of pharmaceutical care and its provision to elderly people. No reference was provided for the study manual. | The intervention group of pharmacists identified actual and potential drug‐related problems using a structured approach. These pharmacists utilised a number of data sources in this assessment including the participant, the participant's GP, and pharmacy records. Following this assessment, pharmacists were instructed to formulate an intervention and monitoring plan. | Community pharmacists were trained to provide the structured pharmaceutical care intervention. A study manual helped facilitate this process. It contained an overview of the concept of pharmaceutical care, its provision to elderly people, information on the therapeutic management of a number of disease states common in the elderly, together with other issues pertinent to drug therapy in the elderly. | Individual face‐to‐face | |
| Drug evaluation and recommendation | Several instruments, criteria, and algorithms have been developed to enable more rational and appropriate use of medication, but limited evidence exists with regard to the outcomes that were investigated. | The Good Palliative‐Geriatric Practice algorithm Garfinkel 2007) and the STOPP/START criteria were used (O'Mahony 2015). Both of these tools assess the appropriate use of medication in older people. | The intervention was composed of 3 phases. In the first phase, an experienced pharmacist evaluated all prescriptions using the GP‐GP algorithm and based their decision about appropriateness on the STOPP/START criteria. In the second phase, the pharmacist discussed recommendations for each drug with the participant's physician in order to come up with a final list of recommendations. Finally, the recommendations were discussed with the participant and a final decision was agreed by physicians and participants. | The intervention was delivered by a trained and experienced pharmacist. No details are provided concerning what is a "trained and experienced" pharmacist. | Individual and face‐to‐face | |
| Chronic care clinics | Chronic care clinics redesign the structure and content of primary care services through the delivery of scheduled visits devoted to chronic disease management. This mode of service delivery has the potential to improve outcomes for elderly people. | The chronic care clinics included an extended visit with the physician and nurse dedicated to planning chronic disease management, a pharmacist visit that emphasised reduction of polypharmacy and high‐risk medications, and a patient self‐management group. | Frail older people were invited to participate in visits with the primary care team. During these visits, a shared treatment plan was developed, a session was conducted with the pharmacist that addressed polypharmacy and medications associated with functional decline, patient self‐management group sessions were conducted, and the provision of health status assessment information was provided to the practice team. | The team that provided the intervention consisted of the participant’s physician, a team nurse, and a pharmacist. Physicians and team nurses received training in population‐based medicine and management strategies of geriatric syndromes. Team nurses received on‐the‐job coaching from study staff. | The intervention was delivered individually and in groups in a face‐to‐face format. | |
| Medication review and drug recommendations | Potentially inappropriate prescriptions are prevalent in older people and are associated with adverse drug events. The STOPP/START criteria are designed to detect potentially inappropriate prescriptions in elderly people. However, little is known about the effects of an intervention involving the application of the STOPP/START criteria on clinical outcomes. | The STOPP/START criteria were used to deliver the intervention (Gallagher 2008). The STOPP criteria focus on avoiding the use of drugs that are potentially inappropriate for older people and the START criteria identify undertreatment or prescribing omissions in older people. | Medication reviews were conducted by the study pharmacist for all residents. Recommendations made by the pharmacist were discussed with the chief physician. The physician then decided whether to accept these recommendations and implement prescribing changes. | The intervention was conducted by the study pharmacist who applied the STOPP/START criteria during the medication review. The pharmacist also discussed the recommendations from the intervention with the chief physician, who decided whether to accept these recommendations and implement prescribing changes. | Intervention was delivered individually and face‐to‐face. | |
| Structured educational intervention | Inappropriate drug prescription is a common problem in people living in nursing homes and is linked to adverse health outcomes. This study assessed the effect of an educational intervention directed to nursing home physicians in reducing inappropriate prescription and improving health outcomes and resource utilisation. | Educational material and references were given to physicians and two 1‐h workshops were used to review cases and promote practice changes. The STOPP/START criteria were reviewed with a random sample of 10 residents cared for by each physician (Gallagher 2008). The content of the educational intervention is provided in an appendix (Garcia‐Gollarte 2014). | The educational intervention included general aspects of prescription and drug use in geriatric patients, how to reduce the number of drugs, to perform a regular review of medications, to avoid inappropriate drug use, to discontinue drugs that do not show benefits, and to avoid under treatment with drugs that have shown benefits. It also discussed some drugs frequently related to adverse drug reactions in older people. | A nursing home physician delivered the structured educational intervention. | Face‐to‐face intervention delivered in a group and individual format. | |
| Medicine reconciliation and action plan | Emergency department overcrowding has been linked to increased mortality, costs, and length of stay. This study evaluated the effectiveness of a telephone‐based, medicines‐management service on reducing emergency department utilisation. | Medication therapy management was provided to participants (APA 2008). A pharmacy technician completed telephonic medication reconciliation, after which a trained pharmacist consulted with the participant or caregiver via telephone to complete a scheduled, comprehensive medication therapy review to identify and resolve any medication‐related problems. The pharmacist constructed a personal medication record and a medication‐related action plan for the participant. The action plan was a participant‐centred document that assisted participants, caregivers, and the pharmacist in the resolution of identified medication‐related problems. | The intervention commenced with a pharmacy technician completing medication reconciliation with the participant over the telephone. Then, a pharmacist consulted with the participant by telephone for an average of 30 min to complete a comprehensive medication review to identify and resolve medication‐related problems. The pharmacist constructed a person medication‐related action plan and followed‐up with the participant's prescriber. | A pharmacy technician delivered the initial medicine reconciliation with the participant. A trained pharmacist conducted the medication therapy review, constructed a personal medication record, and a medication‐related action plan. The pharmacist also followed up with the participant's prescriber for resolution of problems that could not be resolved with the participant. | The intervention was conducted individually on the telephone. | |
| Automated system to facilitate flow of information and provide warnings, alerts, and recommendations | Transitions between the impatient and outpatient setting is a period of high risk for older adults. Most approaches to improving transitions require a substantial commitment of resources but automating these processes may improve the quality and safety of care. | An automated system was used to facilitate the flow of information to the medical group's primary care providers about individuals who were discharged to home from the hospital (Field 2012). | An automated system was developed to facilitate the flow of information to the medical group's primary care providers. A computer interface linked the primary care provider's electronic health records to the hospital records, which provided information about admissions and discharges. The system also provided information about new drugs at discharge, warnings about drug‐drug interactions, recommendations about dose changes and laboratory monitoring of high‐risk medications, and alerts to the provider's support staff to schedule a post‐hospitalisation office visit within 1 week of discharge if not already scheduled. | The automated system delivered the intervention. | The intervention was delivered electronically. | |
| Care transitions clinic visit | Medication errors related to hospital discharge result in rehospitalisations and emergency department visits, which may be reduced by pharmacist involvement during postdischarge transitions of care. This study evaluated the impact of a transitional care clinic visit conducted by a pharmacist. | The Best Possible Medication Discharge List was used to identify medication discrepancies (Wong 2008). It served as the gold standard for the list of medications that the participant should take after discharge. | Participants in the intervention group were scheduled for a care transitions clinic visit approximately 72 h after hospital discharge. The visit involved performing a complete medication history, identifying and resolving medication discrepancies, creating a current medication list, and counselling on appropriate medication use. | Clinical pharmacists provided the intervention. They collaborated with the inpatient medical team to create the Best Possible Medication Discharge List. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist home visits | Older people often have trouble adhering to their medications. This study evaluated the effectiveness of a home‐based medication review on hospital admissions among elderly people. | A standardised visit form was used to record the home visit but no reference was provided. | Pharmacists arranged home visits with the participant during which they assessed the participant's ability to self‐medicate and drug adherence. They educated the participant, removed out‐of‐date drugs, reported drug reactions or interactions to the physician, and reported the need for a compliance aid. | Pharmacists conducted the home visits. Pharmacists held a postgraduate qualification in pharmacy practice or had recent continuing professional development in therapeutics. The pharmacists participated in a 2‐day training course, which included lectures on adverse drug reactions, prescribing in elderly people, improving concordance, and communication skills. | The intervention was delivered individually and face‐to‐face. | |
| Telephone consultation with home visits | Adherence to warfarin treatment and monitoring guidelines may be suboptimal among patients and staff. This study assessed the improvement in adherence to warfarin therapy with telephone and home visits. | A predesigned set of questions was used in the telephone consultation, but no reference or any additional details were provided. | The intervention group was counselled with once‐a‐week telephone consultations and 2 home visits per month by either a nurse or a pharmacist that dealt with warfarin use. | A pharmacist or a nurse provided the home visits. The telephone consultation was conducted by a pharmacist. | The intervention was delivered individually using a face‐to‐face format and telephone calls. | |
| Cardiovascular risk assessment and education sessions | Strategies for managing blood pressure are essential as high blood pressure is the leading risk factor for death. The study authors evaluated the effectiveness of a community‐based cardiovascular health promotion and disease prevention programme in reducing morbidity. | The Cardiovascular Health Awareness Program was a standardised intervention that consisted of 10 weeks of cardiovascular risk assessment, blood pressure measurements, and education sessions (CHAP 2017). | The intervention consisted of 10 weeks of cardiovascular risk factor assessment and educational sessions. Volunteers were recruited to help participants measure their blood pressure and supported self‐management by providing participants with their risk profile, risk‐specific educational materials and information about access to local services. At the end of the 10‐week programme and 6 months after the programme ended, the results were forwarded to family physicians who rank‐ordered their participants by their most recent systolic blood pressure reading. | Volunteers were recruited and trained to carry out the intervention. The volunteers were trained according to a standardised curriculum developed by a public health nurse and delivered by nurses working in the intervention community. | The intervention was conducted individually in a face‐to‐face manner. | |
| Educational intervention with pharmacist | Few studies have examined a pharmacist's contribution to improving diuretic compliance and reducing rehospitalisation and health care use. This study aimed to determine the impact of a pharmacist‐led intervention on patient‐guided diuretic dose adjustment. | The intervention group adjusted their diuretic dose using a flexible frusemide dose‐adjustment guide that was provided in the paper. | The intervention consisted of a 30‐min educational session and focused on improving participant self‐care, recognising symptoms of fluid retention, measuring weight daily, self‐adjusting the diuretic dose and improving knowledge of heart failure and heart failure medications. | A pharmacist provided the intervention. The frusemide dose‐adjustment guide was developed in collaboration with cardiologists. | Conducted individually in a face‐to‐face fashion. | |
| Pharmaceutical care plan | Regular medication reviews can reduce the risk of medication‐related problems. This study aimed to evaluate the effect of a pharmacist‐led medication review on pharmaceutical care issues and hospitalisations. | Clinically‐trained pharmacists completed a detailed profile for each participant using medical notes and computer records. All participants were interviewed in their home about their use of and responses to medication and their use of health and social services. No references provided | A pharmaceutical care plan was drawn up listing all pharmaceutical care issues together with all the actions planned to achieve the outcomes of any pharmaceutical care issue. Copies of the plan were given to the GP who was asked to agree, after which the pharmacist implemented the plan. | The pharmacist performed the medication review. The participants' GP indicated their level of agreement with each pharmaceutical care issue and with the actions taken. | The mode of delivery was individual and face‐to‐face. | |
| Use of health information technology to identify people at risk for delirium and falls, implement monitoring plans, and provide reports to pharmacists | Falls and delirium pose the greatest threats to resident safety in nursing homes and contributes to further functional decline. Medication use is associated with greater risk of delirium and falls. Therefore, this study used health information technology to identify residents at risk for delirium and falls due to adverse drug events. | A Geriatric Risk Assessment MedGuide was a database designed to identify medications that potentially contributed to delirium and fall risk (Tobias 1999). It also facilitated early recognition of signs and symptoms indicative of potential medication‐related problems. Training was provided to nursing staff and pharmacists in how to use the reports generated by the Geriatric Risk Assessment MedGuide. | Health information technology was used to identify residents at risk for delirium and falls, implement monitoring plans, and provide reports to pharmacists in conducting medication reviews. The consultant pharmacist shared the reports with the nurse contact at the facility and used the reports in their monthly drug review. | The intervention was an automated system that provided reports to pharmacists and nurses, who were trained to use these reports. The training for nurses provided information regarding medications that cause, aggravate, or contribute to the risk of falls and delirium. The course also reviewed symptoms and signs of adverse medication effects and reinforced the importance of the early observation of symptoms and signs of adverse medication effects. Pharmacists were trained to provide a targeted drug review for all participants who experienced delirium and falls. | The intervention was delivered individually and face‐to‐face. | |
| Home‐based medication review | Home‐based medication reviews are convenient for the patient and provide an opportunity to understand their medication‐taking in their home environment. Therefore, this study looked at whether home‐based medication reviews with elderly people could reduce hospital admissions. | The intervention comprised 2 home visits by a community pharmacist who educated the participant/carer about their medicines, noted any pharmaceutical care issues and assessed the need for an adherence aid. | At the home visit, the pharmacist educated the participant, removed out‐of‐date drugs, and assessed the need for an adherence aid. The pharmacist held regular meetings with the GP where changes to the participant's medications were discussed and amendments were implemented by the GP. | A pharmacist with a post‐graduate qualification in pharmacy practice conducted the home‐based medication review. They had regular meetings with the lead GP. Possible changes to the participant's medication were discussed and agreed amendments were implemented by the GP. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Although angiotensin‐converting enzyme inhibitors and beta‐blockers reduce morbidity and mortality in people with heart failure, these treatments are underused. Pharmacists may improve treatment through medication review. This study investigated whether a pharmacist intervention would reduce hospital admission and death for people with heart problems. | Pharmacists received training covering the aetiology, symptoms, and evidence‐based management of heart failure. They also participated in monthly discussions of specific cases. The pharmacist used guidelines to optimise treatment for participants with left ventricular systolic dysfunction. All of these materials are available at onlinelibrary.wiley.com/journal | Participants were offered a 30‐min appointment with the pharmacist If there was agreement between the pharmacist and the participant, and subsequently with the doctor, medications were initiated, discontinued, or modified by the pharmacist during 3‐4 weekly or fortnightly consultations. | The pharmacists, who delivered the medication review, had between 3 and 16 years of post‐qualification experience, had experience delivering primary care‐based medication review clinics for people receiving multiple‐drug treatment and attended an in‐house training day covering the aetiology, symptoms, and evidence‐based management of heart failure. An additional session covered the methods of the trial. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Aging and the use of polypharmacy are risk factors for drug‐related problems and medication‐related hospital admissions. Therefore, this study assessed the impact of a community pharmacist‐led medication review on hospital admissions in older people. | Pharmacists in the intervention group received a training course that covered the clinical management of older people and the medication review method. No reference was provided. | The medication review consisted of the pharmacist collecting information about the participant's health problems, medication use, lifestyle habits, and concerns about diseases and medications. The pharmacist then identified negative clinical outcomes related to medicines and drug‐related problems. Subsequently, an action plan was agreed upon which focused on participant outcomes and the medication use process. | Pharmacists provided the medication review. They received a 3‐day training course covering clinical management of elderly people, the medication review with follow‐up method, communication with participants and doctors, study protocol and documentation forms. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist visits | Pharmacists have adopted pharmaceutical care, which is the provision of drug therapy to improve a person's quality of life, to reduce morbidity and mortality. Unlike previous studies that did not focus on people who were most likely to benefit, this study examined veterans who were at high risk for a medication‐related problem. | Contacts between the pharmacist and participant were recorded on a data collection form, which contained the method of contact, time spent, medical problems addressed, drug‐related problems addressed, and drug‐related problems resolved. This form was not referenced. | The intervention participants received consultation and follow‐up care from a clinical pharmacist. | Pharmacists conducted the intervention. Most had a Doctor of Pharmacy degree and over 70% were either receiving or had completed postgraduate training. | The intervention was delivered individually and face‐to‐face. | |
| Home‐based nurse care | Home‐based nurse care can reduce adverse events in people with chronic heart failure. High levels of natriuretic peptides in people with heart failure are predictors of death and hospitalisations. The study authors looked at whether high levels of these peptides can predict whether people with heart failure benefit from a home‐based nurse intervention. | The nurse checked for and, in co‐ordination with the treating physician, implemented guideline‐based medication (Remme 1997; Remme 2001). | At home visits, the nurse checked and recorded weight, recorded symptoms and signs of heart failure as well as heart rate and blood pressure, and organised and reviewed blood analyses on demand. The nurse also gave the patient education and self‐management skills. | Nurses who specialised in caring for people with heart failure provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Computerised care suggestions | Hypertension is associated with cardiovascular morbidity and mortality, but is difficult to control. Guidelines on hypertension are complicated and can become outdated quickly, so this study investigated the benefits of evidence‐based treatment for hypertension using a computerised system. | This study used the pharmacist intervention recording system, which was used to document all pharmaceutical care interventions (Overhage 1999). This system gave the pharmacist care suggestions, which they could pass on to the physician. The physician used an order writing workstation to write orders for drugs, tests, nursing activities, and consultations (McDonald 1999). The workstation gave the physician care suggestions for the treatment of hypertension. | The pharmacist intervention recording system was used by intervention pharmacists to receive care suggestions. The pharmacist could fill the prescription as written, discuss the suggestions with the participant and encourage discussions between the participant and physician, or contact the ordering physician. The physician intervention used an order‐writing workstation to write orders for drugs, tests, nursing activities and consultations and display care suggestions. All hypertension care suggestions were displayed as suggested orders along with possible actions and a brief explanation of the rationale for the suggestion. | Pharmacists and physicians provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Home visits by physician assistants | Studies suggest that people who have undergone coronary artery bypass graft surgery benefit from a home intervention, but there are few studies of home visits by physicians or physician assistants. Therefore, this study examined the hospital readmissions of people who received home visits by physician assistants. | A physician assistant home care form/checklist was used to record all findings from the home visit. A copy of this form was provided in the paper. | Cardiothoracic physician assistants conducted home visits during which they performed a physical examination and reviewed the participant's medications. Adjustments were made to the participant's medications and new medications were prescribed as needed. The surgical wounds were examined and participant concerns were addressed. Prescriptions were written for antibiotics, blood work, or imaging studies. | Physician assistants provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist‐managed hypertension clinic | Hypertension can be controlled, but this study investigated whether it can be managed at a reasonable cost with minimal adverse effects by pharmacists. | Sitting blood pressure was measured with a Datascope Accutorr automated sphygmomanometer (Datascope Corporation Montvale, NJ, USA). 2 readings were taken for each participant and the average of the 2 readings was recorded (Datascope Patient Monitoring 1996). | Participants were counselled by a pharmacist who told them that efforts would be made to decrease the number of antihypertensive drugs or alter their therapy by giving more appropriate or less expensive drugs to achieve similar or improved blood pressure control. The pharmacist determined the most appropriate antihypertensive regimen for each participant, ordered laboratory tests as needed, and provided education on nonpharmacological ways to control blood pressure. | Clinical pharmacists provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Pharmacists work with participants in designing, implementing and monitoring therapeutic plans, but elderly people may have problems with adhering to their medication. This study looked at treatment adherence, as well as hospitalisations and mortality, in elderly people who received a home visit by a pharmacist along with telephone follow‐up. | Pharmacists adhered to a manual to deliver the intervention (Medication Review‐Managing Medicine Manual, Danmarks Apotekerforening, Pharmakon. Medicingennemgang 2004). This manual helps pharmacists identify and resolve drug‐related problems (Danmarks 2004). | Participants were visited at home by a pharmacist who examined the medicines list with regard to side‐effects, interactions and administration. The pharmacist tried to make the regime less complex, informed participants, and motivated adherence. | Pharmacists who had some practical experience or courses in medication review provided the intervention. | The intervention was delivered individually. It was conducted by telephone and face‐to‐face. | |
| Pharmacist medication review | People with end‐stage renal disease take multiple drugs and experience multiple co morbidities, which places them at greater risk of drug‐related problems. This paper looked at the effects of a pharmacist‐led intervention on drug‐related problems and hospitalisations in ambulatory patients undergoing haemodialysis. | Drug‐related problems were recorded, evaluated and assigned to 10 possible categories (Hepler 1990). The drug‐related problems were also categorised into therapeutic drug classes and the outcome related to the drug‐related problem intervention was captured. | Participants assigned to pharmaceutical care had drug therapy reviews conducted by a nephrology‐trained pharmacist. The pharmacist conducted a participant interview, generated a drug therapy profile, identified and addressed drug‐related problems, and provided healthcare‐provider and participant education. The pharmacist also provided consultative services that focused on optimising drug therapy. | The clinical pharmacists who conducted the intervention were either nephrology‐trained or completing postdoctoral training in nephrology pharmacotherapy. | The intervention was delivered individually and face‐to‐face. | |
| Medication review, nurse education, and development of professional relationships | Pharmacist‐conducted medication reviews and nurse education about medication use may have an impact on drug use in nursing homes. This study looked at the effect of medication review and nurse education on mortality and hospitalisations in nursing homes. | Problem‐based educational sessions were provided to nurses and addressed basic geriatric pharmacology and some common problems in long‐term care. No referenced documentation is provided for these sessions. | The intervention introduced a new professional role to stakeholders with relationship building, nurse education, and a medication review by pharmacists. Professional contact between nursing home staff and pharmacists on issues such as drug policy and resident problems was conducted along with problem‐based educational sessions for nurses. These sessions addressed geriatric pharmacology and problems in long‐term care. The medication reviews highlighted adverse drug effects, ceasing or adding drugs, better use of specific drug therapy, non‐drug interventions, and adverse effect and drug response monitoring. | Clinical pharmacists delivered the intervention. | The intervention was delivered individually and in groups over the phone and face‐to‐face. | |
| Structured home visits by GP and nurse | Many hospital admissions are due to inappropriate medical treatment, and the discharge of fragile elderly patients is associated with a high risk of readmission. This study examined whether home visits by GPs and district nurses reduced the risk of readmission of discharged elderly patients. | The joint home visits were guided by an agenda. During the structured home visit the agenda included checking the discharge letter for recommended follow‐up, checking the need for adjustment of medication, checking if social and personal support was arranged, and checking the family’s medicine cabinet. This agenda was provided in the article. | There was a joint home visit by the GP and district nurse approximately one week after discharge from the hospital. 2 more contacts were conducted by the GP in the GP's clinic or as a home visit. These visits included checking the discharge letter, checking the need for adjustment of medication, checking if social and personal support was arranged, and checking the family's medicine cabinet. | GPs and district nurses provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication reviews | Adverse drug events are frequently caused by cardiovascular drugs. Pharmacists can identify and resolve drug‐related problems for people at home and reduce re‐hospitalisation rates. This study investigated whether a pharmacist‐led intervention could reduce re‐hospitalisations and death in people with heart failure. | Using a predefined checklist, the pharmacist tried to reduce the use of inappropriate mediations, encourage smoking cessation, suggest improvements in the participant’s diet, and promote medication adherence, self‐monitoring, and vaccination. The checklist is not provided in the paper. | The pharmacist in the intervention group conducted an in‐home medication assessment and 2 follow‐up visits. This involved assessing and reviewing physician notes and laboratory test values and interacting with prescribers on behalf of the participants. The pharmacist catalogued all medications and interviewed the participant regarding medication use. | A clinical pharmacist, who had over 20 years of combined experience as a hospital and community pharmacist and had received a doctor of pharmacy degree and completed a 1‐year clinical residency in home care, provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Repeat prescribing is poorly managed in the UK, which puts people at risk. Pharmacists could review these prescriptions and reduce the pressure on GPs. This study tested whether pharmacists can review repeat prescriptions to reduce hospital admissions and deaths. | The process for reviewing repeat prescriptions involved discussing each condition with the participant and asking about symptoms (Lowe 2000). If clinical or pathological monitoring was due, the pharmacist directed the participant to the practice nurse or doctor. Participants with new clinical problems were referred to the doctor. | The pharmacists conducted a medication review during which they evaluated the therapeutic efficacy of each drug and the progress of the conditions being treated. Compliance, actual and potential adverse effects, interactions, and the participant’s understanding of the condition and its treatment were considered. The outcome of the review was a decision about the continuation of the treatment. | A pharmacist provided the medication review. | The intervention was delivered individually and face‐to‐face. | |
| Pharmacist medication review | Elderly people take multiple medicines, which increases the risk of adverse drug events. Pharmacists can improve medicine management for elderly people in the community. In this study, the authors looked at whether a pharmacist‐led review would reduce hospitalisations and deaths among elderly people in nursing homes. | The clinical medication review (Lowe 2000), which was conducted by the pharmacist, comprised a review of the GP clinical record, and a consultation with the participant and carer. The pharmacist made recommendations and passed them on a written proforma to the GP for acceptance and recommendation. | The pharmacist conducted a medication review in which the pharmacist identified the drugs that were taken, identified the original indication for each drug, assessed adherence to medication, and identified unaddressed medical problems. They also considered the continuing need for each drug, identified side effects, identified drug interactions or contraindications, and considered costs. Finally, the pharmacist implemented and documented any changes. | The study pharmacist provided the intervention. | The intervention was delivered individually and face‐to‐face. | |
| GP: general practitioner | ||||||
| Study | Location of intervention | When and how much of the intervention was delivered | Tailoring | Modifications | Adherence planning | Adherence assessment |
|---|---|---|---|---|---|---|
| 83 community pharmacies in the provinces of Asturias, Barcelona, Madrid and Biscay | The intervention was delivered once. | There was no tailoring made to the intervention. | Two additional seminars were given to the intervention group on real cases in order to approve the intervention. | Not undertaken | Not undertaken | |
| Community pharmacies in 7 European countries; Denmark, Germany, The Netherlands, Northern Ireland (co‐ordinating centre), Portugal, Republic of Ireland and Sweden. A minimum of 12 sites per country were chosen according to specific criteria set within each participating country relating to the population of elderly people who visited the pharmacy, staffing levels within the pharmacy and working relationships with local GPs. | The intervention was delivered at least once according to the study manual. However, Each site was free to provide as much information as possible to the intervention group as per the study manual. | A study manual describing the intervention was developed for all the participating countries. Each country translated the manual into their own language. | Each country adapted the manual, translating and modifying sections where appropriate, according to differing national practices. | Not undertaken | Not undertaken | |
| 7 Primary Health care clinics in Mataró and Argentona | The intervention included 3 phases and the participants were followed up for 12 months. It is not clear if the intervention was repeated more than once. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| 9 primary care physician practices in Washington State. Clinics were allowed to select their target condition of focus: frail older adults or people with diabetes. The physicians were board certified in Family Practice and did not have formal training or certification in geriatric medicine. | The intervention was undertaken once. However there was variability in the frequency of one of its components. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | A priori process of care measures for each of the geriatric syndromes were developed with decision rules for acceptable documentation by the study reviewers for the interventions. | The chart abstraction of assessing the documentation for the interventions was performed by one member of the study team along with an additional reviewer blinded to knowledge of the study group and study hypothesis. The overall level of agreement between the 2 reviewers was acceptable based on published ranges (kappas for geriatric syndrome process measures 0.75 to 0.85) | |
| Chronic care geriatric facilities in Central Israel | The intervention was done once at 6 months and 12 months later. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| A private organisation of 37 nursing homes in Spain | It is unclear how many times the intervention was given as the educator offered further on‐demand advice on prescription for the next 6 months. | There was no tailoring made to the intervention. | There was no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| Home health patients within a medicare insured home health population in Canada | The intervention was undertaken at least once however, some participants received more than one phone call as additional telephone follow‐up was provided as needed per the pharmacists' discretion during the first 30 days of the 60‐day home healthcare episode. | Some participants received additional follow‐up depending on their conditions. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| Large multispecialty group practice employing 265 physicians, including 66 primary care providers caring for adults in the outpatient setting | Daily records generated by the computer system were examined. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| 804‐bed academic medical centre in North Carolina, USA | The intervention took place once. | There was no tailoring made to the intervention. | Only hospitalisations and ED visits at the study institution were included for those participants who were not able to be contacted after 3 phone call attempts. | Not undertaken | Not undertaken | |
| Home‐based medication review after discharge from acute or community hospitals in Norfolk and Suffolk, UK. | The intervention was performed once. | It is possible that a small number of participants in both groups may have had their medication reviewed during the follow‐up period by their GP or community pharmacist. | There were no modifications made to the intervention during the study. | Not undertaken. No data on adherence were collected. | Not undertaken | |
| Telephone consultation with home visits | The intervention was performed once. | Any additional contact as requested by the participant in the intervention group was undertaken. | There were no modifications made to the intervention during the study. | Not undertaken | Not undertaken | |
| Community‐based pharmacies in Canada | The intervention was performed once as planned. | The local lead organisations used several strategies to recruit volunteer peer health educators. These strategies included using the local lead organisation's existing volunteer base, advertising in the local media, and giving presentations at local seniors’ clubs. | When required, Cardiovascular Health Awareness Program support staff produced and mailed invitation letters on behalf of participating physicians (CHAP 2017). | Feedback of results was given to primary healthcare providers. | Evaluation data collected for the purpose of ongoing evaluation and quality improvement: 1. Success of different advertising/invitation strategies 2. Attendance, consent, completed assessments 3. Nurse assessments, pharmacist consults, fax/call to family physician the same day. Feedback to family physicians, pharmacists, and participants | |
| Outpatients clinic in Melbourne, Australia | The intervention was performed once as planned. | There was no tailoring made to the intervention. | There were no modifications made to the intervention during the study. | There were written instructions on how to adjust the dose of frusemide per weight increase. | Data on dosage adjustment of frusemide were collected and compared against the initial criteria. | |
| General medical practices in the Grampian region of Scotland | The intervention was performed once as planned. | In the control group, when pharmacists considered a review to be serious and beneficial to the participants, an independent medical assessor decided on the need to withdraw the participants on clinical grounds. | There were no modifications made to the intervention during the study. | Any outstanding care issues in both groups were communicated to the participant's GP. | Not undertaken | |
| 25 nursing homes serviced by 2 long‐term care pharmacies in Northern Ireland | It is unclear the number of times the reports were generated and used by the pharmacists for every resident. | The Geriatric Risk Assessment MedGuide database software for falls and delirium was integrated into the pharmacies’ commercial pharmacy software system (Rescot LTCP System) for the intervention homes (Tobias 1999). | It is unclear if there were any modifications to the interventions. | The computer system did not capture if the recommendations done by the pharmacist were accepted. | Not undertaken | |
| A GP setting in Norfolk, UK | It is unclear how many times the pharmacist and the GP met to discuss participant's care plan. | A follow‐up visit with the participant occurred 6‐8 weeks later to reinforce the original advice, and assess whether there were any further pharmaceutical care issues to address with the GP. | It is unclear if there were any modifications to the interventions. | Not undertaken | Not undertaken | |
| The study was conducted within the NHS which provides free health care to the population of the UK. 27 primary care‐based pharmacists employed by the NHS to work with family doctors | It is unclear how many times the pharmacist met the participant and the GP. | If there was agreement between the pharmacist and the participant during the consultation and subsequently with the family doctor, medications were initiated, discontinued, or modified by the pharmacist during 3‐4 subsequent weekly or fortnightly consultations. | It is unclear if there were any modifications to the interventions. | Not undertaken | Not undertaken | |
| The study was conducted in 178 community pharmacies in Spain | It is unclear how many times the intervention was undertaken. | A specifically trained pharmacist called a practice change facilitator helped pharmacists of the intervention group in the provision of the medication review with follow‐up service, identifying barriers specific to each pharmacy and providing solutions. | It is unclear if there were any modifications to the interventions. | The practice change facilitator ensured fidelity to the intervention and supported pharmacists of both study groups on queries about documentation forms. | The experts were requested to answer individually for each case and the degree of agreement between them was later established. Inter‐rater reliability was measured using Fleiss's kappa. | |
| 9 Veterans Affairs medical centres in the USA | It is unclear how many times participants were seen by the pharmacist in the intervention group as the protocol indicated that each participant should have at least 3 visits with the clinical pharmacist during the study, but participants could be seen as frequently as deemed necessary to ensure appropriate care. | To prevent contamination, some sites marked medical records of intervention and control participants to alert clinical pharmacists that participants were in the study. Other sites noted this distinction in electronic medical records. One site distributed a list of participants enrolled in the study to all pharmacists providing primary care. | Clinical pharmacist intervention, however, occurred in one control participant; this participant was withdrawn from the study and his data were not included in the results. | Each contact with the participant was recorded on a standard data collection form that contained information about the method of contact, estimated time spent with the participant, medical problems addressed, drug‐related problems addressed, and drug‐related problems resolved. | Each month after enrolment the co‐ordinating centre received electronic data on each participant's prescription drugs dispensed in the preceding month. When participants either completed the study or died, data on resource use from enrolment to termination were retrieved. | |
| Ambulatory patients participating in the EuroHeart Failure Survey programme in Vienna | It is unclear how many times the nurse visited the intervention participants as more visits were made optional for participants. | More frequent contacts such as visits or telephone calls between the nurse and the participants were optional in case the participant or the nurse considered them necessary. | The nurse was in charge of individualised participant and caregiver education and enhancement of self‐management. If the nurse noted any deterioration in the participant's status, she reported to the treating physician or advised the participant to visit the treating physician. | Not undertaken | Not undertaken | |
| Academic primary care internal medicine practice in the USA | It is unclear how many times the intervention was undertaken. | There was no tailoring made to the intervention. | There were no modifications made to the interventions. | Data necessary to generate care suggestions were derived from the computer programme. Treatment suggestions fell into 5 major categories. | Not undertaken | |
| Ambulatory patients discharged from a large 702‐bed hospital in Staten University Hospital, USA | It is unclear how many times the physician visited each participant in the home after their discharge. | There was no tailoring made to the intervention. | There were some modifications done to the intervention due to the participants not being available at the weekend. Participants were not seen directly after discharge as per the study protocol. | All findings were documented on the intervention visit form. | It is unclear if this was undertaken. | |
| Managed care organisation in California, USA | It is unclear how many times participants were seen by the pharmacist in the intervention group as additional follow‐up was organised by the pharmacists for some participants. | Additional follow‐up was organised by the pharmacists for some participants. | The intervention was not modified. | Not undertaken | Not undertaken | |
| Patients living at home in the municipality of Aarhus, Denmark | The intervention was performed at the intended follow‐up. | Pharmacists could consult the project physician if they considered a participant's medication problems to be life‐threatening. | The intervention was not modified. | Adherence to the medications were assessed by a pill‐count in all participants during 1 year. | Pill count was undertaken | |
| The study took place in a non‐profit university‐affiliated dialysis clinic in Albany, USA. | It is unclear if all participants received the same number of follow‐up visits by the pharmacist or the physician in the intervention group. | It is unclear if there was any tailoring made to the intervention. | The intervention was not modified. | Not undertaken | Not undertaken | |
| 52 nursing homes located in south‐east Queensland and north‐east New South Wales, Australia | There was variability in the number of educational sessions provided to staff in each nursing home as well as the number of visits by the intervention pharmacists. | It is unclear if there was any tailoring made to the intervention. | It is unclear if the intervention was modified. | Validation of prescription claim data with participants' medications profiles. | To validate prescription claims data, a sample of 1328 cross‐sectional medication profiles were collected for 8 nursing home clusters for control and intervention homes at post‐intervention. An audit, comparing original post‐intervention medication data with the same data recollected up to 6 weeks later for a 6%, random sample, showed an overall reproducibility of 97% (range 92% to 100%) | |
| Patients discharged from Glostrup Hospital, Denmark. | The intervention was performed as prescribed. | There was no tailoring made to the intervention. | There was no modification made to the intervention. | Not undertaken | Not undertaken | |
| Heart failure patients discharged from hospital in Albany, Scotland | The intervention was performed as prescribed. | The clinical pharmacist accessed and reviewed all pertinent physician notes and laboratory test values via the National Endowment for the Humanities data system and interacted with prescribers on behalf of the participants, as necessary. | There was no modification made to the intervention. | Not undertaken | Not undertaken | |
| 4 GPs in Leeds, UK | It is unclear how many times the pharmacist visited the participant. | Immobile participants were visited at home. Non‐attenders were invited once more by telephone. | The study authors agreed with each practice the level of intervention that the pharmacist could make without seeking prior approval | It is unclear if this was undertaken. | It is unclear if this was undertaken. | |
| 65 care homes for the elderly in Leeds, UK | It is unclear how many times the pharmacist reviewed each participant. | There was no tailoring made to the intervention. | There was no modification made to the intervention. | Pharmacists filled in a proforma sheet including their recommendations. | GP acceptance of the recommendations was signified by ticking a box on the proforma. | |
| ED: emergency department; GP: general practitioner; NHS: National Health Service | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Number of hospital admissions Show forest plot | 2 | 3889 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.79, 1.96] |
| 1.2 Number of people admitted to hospital Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.3 Number of emergency department visits Show forest plot | 2 | 1067 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.50, 1.02] |
| 1.4 Mortality Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Number of hospital admissions Show forest plot | 11 | 6203 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.71, 1.03] |
| 2.2 Number of people admitted to hospital Show forest plot | 13 | 152237 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.86, 0.99] |
| 2.3 Number of emergency department visits Show forest plot | 5 | 1819 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.49, 1.15] |
| 2.4 Mortality Show forest plot | 12 | 154962 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.85, 1.03] |

