| Study | Anaesthetic technique | Titrating strategies |
| Ahmad 2003 | Endotracheal GA. Induction: sevoflurane
Maintenance: sevoflurane‐sufentanil‐nitrous oxide‐a relaxant | Sevoflurane/sufentanil titrated for increased blood pressure/heart rate > 20%, despite a BIS value of 50‐60 or end tidal sevoflurane concentration 2% |
| Aime 2006 | Endotracheal GA, Induction: propofol‐sufentanil Intubation: atracurium Maintenance: sevoflurane and nitrous oxide in oxygen, sufentanil, atracurium | BIS group: intermittent bolus dose of sufentanil despite BIS or Entropy values within the recommended range Control group (CS group): increased sevoflurane concentration or intermittent bolus doses of intravenous sufentanil for signs of inadequate anaesthesia, i.e. hypertension and bradycardia |
| Anez 2001 | LMA GA. Induction: propofol‐alfentanil
Maintenance: propofol‐rocuronium | NA |
| Assare 2002 | LMA GA. Induction: propofol‐fentanyl
Lidocaine infiltration prior to incision
Maintenance: sevoflurane‐nitrous oxide (no muscle relaxant) | NA |
| Basar 2003 | Endotracheal GA. Induction: fentanyl‐thiopentone
Intubation: rocuronium
Maintenance: sevoflurane‐nitrous oxide | Inadequate analgesia in both groups managed by increased concentration of sevoflurane (no supplemental fentanyl) |
| Boztug 2006 | Endotracheal GA. Induction: fentanyl‐thiopentone
Intubation: cis‐atracurium
Maintenance: 50% O2/air mixture and 0.8%–1.5% sevoflurane, fentanyl, and cis‐atracurium | BIS group: additional fentanyl was administered in 0.1mg doses when the BIS value rose to 55. With inadequate decreases in the haemodynamic values, sevoflurane concentration was increased by 20%.
Control (CS) group: fentanyl was also administered in 0.1‐mg doses if MAP increased by 20% from baseline values, and in the event of inadequate decreases in the haemodynamic values, the sevoflurane concentration was increased by 20%. |
| Bruhn 2005 | Endotracheal GA. Induction: remifentanil‐propofol
Intubation: cis‐atracurium
Maintenance: desflurane in O2/air mixture and remifentanil (no more neuromuscular blocking agents) | BIS group: desflurane during maintenance was continuously adjusted according to a target value of ‘50’. In case anaesthesia was judged inadequate despite the BIS target value, the infusion rate of remifentanil could be increased.
Control (CS) group: if anaesthesia was inadequate, the desflurane concentration was increased in steps of 0.5 vol%. If this was judged insufficient, the infusion rate of remifentanil could be increased. |
| Chiu 2007 | Endotracheal GA. Induction: fentanyl‐propofol
Intubation:rocuronium
Maintenance: Before cardiopulmonary bypass
‐sevoflurane (end tidal concentration 0.5‐1.5%) with oxygen in air + infusion atracurium: during cardiopulmonary bypass
‐propofol starting TCI from 2 µg/ml in both arms | BIS group: adjustment of the propofol infusion to achieve BIS 40 to 50
Control (CS) group: titrating of TCI propofol according to perfusion pressure (70 to 90 mmHg) |
| Gan 1997 | Endotracheal/LMA anaesthesia
Induction: propofol alfentanil
Maintenance: 50%nitrous in oxygen‐propofol‐alfentanil‐relaxants | BIS group: increasing alfentanil if BIS was within the recommended range (45‐60)
SP group: increasing doses of either propofol, alfentanil or antihypertensive agents |
| Hachero 2001 | Endotracheal GA. Induction: propofol
Intubation: mivacurium Maintenance: propofol‐fentanyl‐mivacurium | Signs of inadequate anaesthesia managed in both groups by fentanyl |
| Ibraheim 2008 | Endotracheal GA. Induction: fentanyl‐propofol Intubation: succinylcholine. Maintenance: sevoflurane, nitrous oxide in oxygen, fentanyl, and atracurium | Any instances of inadequate anaesthesia were managed by increasing the concentration of sevoflurane |
| Kreuer 2003 | Endotracheal GA. Induction: propofol‐remifentanil
Intubation: cisatracurium. Maintenance: propofol (TCI)‐ remifentanil (constant infusion) | Remifentanil infusion was given in both groups for signs of inadequate anaesthesia despite achieving propofol target concentration or a target value of 50 for BIS |
| Kreuer 2005 | Endotracheal GA, Induction: propofol‐remifentanil
Intubation: cis‐atracurium
Maintenance: desflurane in O2/air mixture and remifentanil ( no more neuromuscular blocking agents) | BIS group: desflurane during maintenance was continuously adjusted according to a target value of ‘50’. In case anaesthesia was judged inadequate despite the BIS target value, the infusion rate of remifentanil could be increased.
Control (CS) group: if anaesthesia was inadequate, the desflurane concentration was increased in steps of 0.5 vol%. If this was judged insufficient, the infusion rate of remifentanil could be increased. |
| Leslie 2005a | Relaxant general anaesthesia. Induction: midazolam‐propofol or thiopentone Intubation: nondepolarizing muscle relaxants. Maintenance: propofol or volatiles‐nitrous oxide‐opioids. Hypnotic drugs. Combined general and regional anaesthesia | Narcotic analgesics on the discretion of the attending anaesthesiologists |
| Luginbuhl 2003 | Endotracheal GA
Induction: propofol and fentanyl. Intubation: vecuronium
Maintenance: propofol‐fentanyl or desflurane‐fentanyl | BIS group: propofol or desflurane to keep BIS 45‐55 and opioids according clinical criteria
CS group: propofol or desflurane and opioids according to haemodynamic and vital sign criteria (within 20% of the baseline value) |
| Masuda 2002 | Endotracheal GA
Induction: propofol‐fentanyl
Intubation: vecuronium
Maintenance: propofol‐nitrous oxide ‐ fentanyl‐vecuronium | NA |
| Mayer 2007 | Endotracheal anaesthesia combined with thoracic epidural analgesia Induction: propofol 2 mg/kg, fentanyl 1–2 g/kg Intubation: cisatracurium 0.15 mg/kg Maintenance: propofol‐cisatracurium‐thoracic epidural rovivacaine and sufentanil | BIS group: additional epidural ropivacaine/sufentanil mixture plus intravenous fentanyl (a small bolus dose) for increased blood pressure despite adequate hypnosis. Control group (CS group): increased propofol infusion for increased blood pressure, and a small fentanyl bolus along with an additional epidural bolus injection of ropivacaine/sufentanil for insufficient blood pressure control by propofol. |
| Morimoto 2002 | Endotracheal GA
Induction:thiopentone, Intubation: vecuronium
Maintenance: sevoflurane‐nitrous oxide‐ fentanyl‐vecuronium | Managed by fentanyl 50‐100 µg, despite 2% in sevoflurane in both groups. |
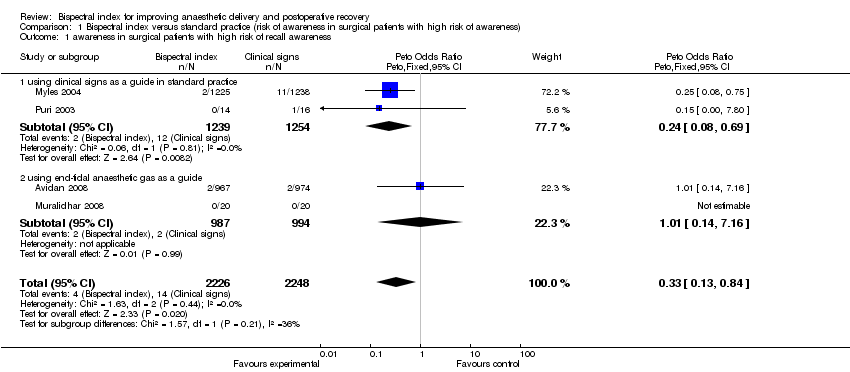
| Myles 2004 | Relaxant general anaesthesia. Induction: midazolam‐propofol or thiopentone Intubation: nondepolarizing muscle relaxants. Maintenance: Propofol or volatiles‐nitrous oxide‐opioids. Hypnotic drugs. Combined general and regional anaesthesia | Narcotic analgesics on the discretion of the attending anaesthesiologists |
| Nelskyla 2001 | Endotracheal GA. Induction:propofol Intubation: rocuronium
Maintenance: Sevoflurane (0.94%‐1.4%)‐Nitrous oxide‐rocuronium | Supplemental alfentanil given for haemodynamic variables >25% of the preanaesthetic value, despite BIS of 50‐60 in BIS group or sevoflurane concentration of 1.4% in CP group |
| Paventi 2001 | Endotracheal GA. Induction: remifentanil ‐ thiopentone Intubation: vecuronium Maintenance: sevoflurane‐nitrous oxide‐remifentanil‐vecuronium. | Remifentanil infusion (0.4 µg/kg/min) for both groups |
| Puri 2003 | Endotracheal GA. Induction: midazolam‐morphine‐thiopentone
Intubation:vecuronium. Maintenance: isoflurane‐nitrous oxide‐morphine | Signs of inadequate analgesia (tachycardia, hypertension, sweating, lacrimation etc) in both groups managed by morphine before vasodilators or beta‐blocker |
| Recart 2003 | Endotracheal GA Premedication: Induction: propofol‐fentanyl
Intubation: rocuronium Maintenance: desflurane‐fentanyl | Intermittent intravenous fentanyl 0.5 mg/kg as needed to maintain haemodynamic variables within 15% of the baseline value
Labetalol to control sympathetic responses as needed (in the presence of adequate hypnotic and analgesic states)
Intermittent intravenous fentanyl 0.5 mg/kg as needed to maintain haemodynamic variables within 15% of the baseline value
Labetalol to control sympathetic responses as needed (in the presence of adequate hypnotic and analgesic states) |
| Song 1997 | Endotracheal GA. Induction: fentanyl‐propofol. Intubation:succinylcholine Maintenance: desflurane or sevoflurane‐nitrous‐fentanyl‐mivacurium (at least 1‐2 TOF) | Inadequate analgesia (haemodynamic variables >20%of baseline) managed by supplemental doses of fentanyl (25‐30 µg) |
| Struys 2001 | Endotracheal GA. Induction: remifentanil, propofol .Intubation: rocuronium. Maintenance: remifentanil infusion (0.5 µg/kg/min)‐propofol infusion | Remifentanil infusion |
| Tufano 2000 | Endotracheal GA. Induction: Propofol. Intubation: Cis‐atracurium. Maintenance: propofol infusion or sevoflurane‐nitrous oxide‐cisatracurium‐fentanyl | NA |
| White 2004 | Endotracheal GA. Induction: propofol and fentanyl Intubation: succinylcholine. Maintenance: desflurane‐nitrous‐cisatracurium | Esmolol to treat sustained increased heart rate |
| Wong 2002 | Endotracheal GA. Induction: propofol‐fentanyl‐midazolam
Intubation: rocuronium. Maintenance: isoflurane‐nitrous oxide‐fentanyl‐rocuronium‐fentanyl | BIS group: BIS > 60 increasing isoflurane concentration; BIS = 50‐60 giving supplemental fentanyl; BIS < 50 decreasing isoflurane concentration and supplementing fentanyl (signs of inadequate anaesthesia) or labetalol (no sign of inadequate anaesthesia)
Control(CS) group: increasing isoflurane concentration or supplemental fentanyl or labetalol for management of hypertension (>25%) or tachycardia (>90 beats per minute). |
| Zohar 2006 | LMA GA. Induction: propofol‐fentanyl
Maintenance: sevoflurane‐nitrous oxide (no muscle relaxant) | In both groups, the sevoflurane concentration was increased in response to signs of an inadequate “depth of anaesthesia” (e.g. movement in response to surgical stimulation). |