Flúor para la prevención de la caries dental temprana (lesiones blancas desmineralizadas) durante el tratamiento con aparatología fija
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Trial design: 2‐arm parallel‐group RCT Unit of randomisation: Participants Location: Leeds, UK Number of centres: 1 Recruitment period: December 1998 to December 1999 Funding source: BDA Research Foundation Shirley Glasstone Hughes Memorial Prize Fund and the Listerine Preventive Care Award | |
| Participants | Inclusion criteria: Participants with upper incisors and canines developing and at least 3 upper permanent incisors and 1 upper permanent canine erupted, prior to commencement of orthodontic treatment with fixed upper appliances 40 F/28 M (sic) Exclusion criteria: Participants with grossly damaged, restored or defective upper permanent canines or incisors, participants living in areas with fluoridated water supply, physically or mentally handicapped individuals, those with comorbidities or requiring antibiotic cover and pregnant or nursing females Mean age at baseline, years: 15.7 (range 11 to 45) Number randomised: 70 (34 F‐releasing glass bead and 36 F rinse) Number evaluated: 37 (18 F‐releasing glass bead and 19 F rinse) | |
| Interventions | Comparison: Fluoride‐releasing glass beads versus fluoride rinse Group A (n = 18): Fluoride‐releasing glass bead (containing 13.3% F) attached to appliance Group B (n = 19): Fluoride rinse (Endekay 0.05% NaF). Participants instructed to use 5 drops in 10 ml of water and to rinse once daily Duration of treatment: Approximately 19 months (recruitment ended December 1999; final data collection September 2002) | |
| Outcomes | Before and after cross‐polarised images of 6 upper anterior teeth, assessed by a masked individual using image analysis, salivary fluoride levels | |
| Notes | Background exposure to fluoride not reported: Unclear whether participants used fluoride toothpaste Power calculation reported that 28 participants/group would be needed to show the expected 75% difference; it was planned to recruit 35 per group to allow for drop‐outs Large numbers of participants both withdrawing or dropping out (total 14: 6 control, 8 experimental), as well as insufficient data for analysis (total 19: 11 control, 8 experimental). Null findings should be interpreted with caution, as investigators lost so many in their sample, which means that it is likely that this study lacks statistical power | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A random number table was generated on an Excel spreadsheet by the trial’s statistical advisor" |
| Allocation concealment (selection bias) | Low risk | Quote: "Each time a patient agreed to take part in the study, a dental nurse who was not involved in the running of the study accessed the concealed table and crossed off the next number, informing the operator of the treatment to be used i.e. whether the patient had been allocated to the fluoride rinse or FGB group" |
| Blinding ‐ Patients & Operators | High risk | Not possible to blind participants or operators to allocated intervention |
| Blinding ‐ Outcome assessors | Low risk | Quote: "Analysis was undertaken blind by one operator, who was unaware of which group the teeth being analysed came from" |
| Incomplete outcome data addressed | High risk | 14 participants (8 F‐releasing glass bead and 6 rinse) dropped out ‐ reasons not given. Further 19 (8 F‐releasing glass bead and 11 rinse) excluded from analysis because of insufficient data, and reasons not explained. 47% of randomised participants not included in the analysis. High rate of breakage of F‐releasing glass beads. Substantial risk of bias due to attrition |
| Free of selective reporting | Unclear risk | Numbers of participants and teeth with DWLs reported at the beginning and at the end of the trial, but denominators were unclear. No indication of mean size of lesions in each group. Salivary fluoride levels not reported |
| Free of other bias | Unclear risk | Number of breakages of F‐releasing glass beads reported, but no indication of level of compliance in fluoride rinse group. No information on duration of trial and therefore duration of exposure to fluoride in each group |
| Methods | Trial design: Parallel RCT Unit of randomisation: Individuals Location: Skelleftea & Lycksele, Sweden Number of centres: 2 Recruitment period: Not stated Funding source: Grants from the County Council of Vasterbotten & Swedish Dental Society, with varnishes supplied by Ivoclar Vivadent and brackets by 3M Unitek | |
| Participants | Inclusion criteria: Children 12 to 15 years of age scheduled for maxillary treatment with fixed orthodontic appliances for an expected duration of at least 6 months Exclusion criteria: None stated Mean age at baseline, years: 14.3 ± 1.6 Number randomised: 273 (137 and 136) Number evaluated: 257 (132 and 125) | |
| Interventions | Comparison: Fluoride varnish (Fluor Protector) versus placebo Group A (n = 137): Fluor Protector (0.1% F difluorosilane in polyurethane base) varnish applied after bonding and at each checkup (approximately every 6 weeks) until debonding Group B (n = 136): Placebo varnish, identical in appearance to active, applied after bonding and at the end of each check‐up (every 6 weeks) until debonding In both groups, after removal of visible plaque with an explorer, 0.2 to 0.3 ml varnish was applied around the bracket bases in a thin layer with a minibrush and was allowed to dry for 2 minutes. Participants were instructed to avoid all eating and drinking for 2 hours and to not brush teeth until the following day Duration of treatment: Not given, but mean number of applications of varnish was 10, and assuming they were seen every 6 weeks, the mean duration was 60 weeks or just over 1 year (which is quite short) All children strongly advised to brush teeth with 1000 to 1500 ppm fluoride toothpaste at least twice daily Fluoride in piped drinking water in these communities was < 0.2 ppm | |
| Outcomes | Before and after clinical photographs assessed for presence and severity of DWLs by 2 experienced and calibrated judges | |
| Notes | Sample size calculation reported. Estimated requirement for 132 participants per group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (author): "The patients were assigned to one of the two groups on the basis of odd and even numbers from a dice" Comment: The corresponding author was asked how investigators obtained equal numbers in all groups but does not seem to have answered this |
| Allocation concealment (selection bias) | Low risk | Quote (author): "The study was coordinated from the Department of Paediatric Dentistry and the randomization was performed there by an independent technician not involved in the clinical work and collection of data" |
| Blinding ‐ Patients & Operators | Low risk | Quote (author): "The placebo varnish applied had an identical composition but without fluoride. Both varnishes were uncoloured and obtained from the producer in identical bottles coded by colour. Neither clinicians nor patients knew whether they were treated with fluoride or placebo varnish" Comment: The study was double‐blind |
| Blinding ‐ Outcome assessors | Low risk | Quote: The two "experienced and calibrated" judges who scored the photographs for presence/absence and severity of DWLs "were not involved in the treatment of the patients and blinded for group assignment" |
| Incomplete outcome data addressed | Low risk | Comment: Flow diagram provided and withdrawals and drop‐outs reported (5/137 or 4% experimental; 11/136 or 8% controls). Reasons given and similar in each group. Unlikely to have introduced a bias |
| Free of selective reporting | Low risk | Planned outcome was white spot lesions at debonding in each group. Reported as % prevalence with P value for difference between groups. No apparent evidence of selective reporting |
| Free of other bias | Low risk | No other sources of bias identified |
| Methods | Trial design: 2‐arm double‐blind parallel‐group RCT Unit of randomisation: Individual Location: Sweden Number of centres: 2 Recruitment period: Starting orthodontic treatment in1999 Funding source: The study was supported by GABA International, Basel, Switzerland | |
| Participants | Inclusion criteria: Participants were those starting orthodontic treatment in 1999 with fixed appliances in both arches Exclusion criteria: None stated Age at baseline: Not stated Number randomised: 115 Number evaluated: 97 | |
| Interventions | Comparison: 2 different fluoride toothpastes and mouthrinses Group A (n = 50): Participants were instructed to brush twice daily with toothpaste containing amine fluoride and stannous fluoride combination (AmF/SnF2 140 ppm, pH 4.5) and to rinse every evening after toothbrushing with a solution containing amine fluoride and stannous fluoride Group B (n = 47): Participants were instructed to brush twice daily with toothpaste containing neutral sodium fluoride (NaF 1400 ppm, pH 6.7) and to rinse every evening after toothbrushing with a solution containing NaF (250 ppm, pH 6.3) Duration of treatment: Fluoride treatments were continued for the whole duration of orthodontic treatment with fixed appliances | |
| Outcomes | White spot lesion index, visible plaque index, gingival bleeding index, measured at baseline and at debonding | |
| Notes | Background exposure to fluoride: Not reported Power calculation: Not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "allocated to two groups at bonding according to a randomized table" Comment: Assumed this refers to random number table |
| Allocation concealment (selection bias) | Unclear risk | Not described Comment: Assumed not done |
| Blinding ‐ Patients & Operators | Low risk | Double‐blind. Quote: "Neither the subjects nor the research team were informed about which group each participant belonged to" |
| Blinding ‐ Outcome assessors | Low risk | Double‐blind. Quote: "Neither the subjects nor the research team were informed about which group each participant belonged to" |
| Incomplete outcome data addressed | Low risk | 18 of the patients invited to participate were not included in the evaluation. Not stated which groups they were from, but it seems likely that number was similar in each group. Reason given was moving house |
| Free of selective reporting | Low risk | Planned outcomes reported in full |
| Free of other bias | Low risk | No other sources of bias identified |
DWL = demineralised white lesion; F = fluoride; ppm = parts per million; RCT = randomised controlled trial.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Clinical assessment carried out 1 month after debonding not immediately after | |
| Abstract only. Insufficient information to include in review. Contacted author. Unable to provide sufficient data for analysis. No subsequent publication identified | |
| Split‐mouth study | |
| CCT with alternate allocation to fluoride or non‐fluoride elastomeric ligatures | |
| "Patients chosen at random" and divided into 2 groups. Report is unclear about the details of allocation to each group, groups are unequal in size, no baseline characteristics, and no outcome data presented per participant. Unable to contact authors and unable to include this study based on available information | |
| Demineralisation assessed 3 months after debonding rather than immediately | |
| Demineralisation assessed 3 months after debonding rather than immediately | |
| Not RCT | |
| Split‐mouth study | |
| Split‐mouth study | |
| Split‐mouth study | |
| Outcomes were DMFT and DMFS not demineralised white lesions | |
| Split‐mouth study | |
| Not RCT | |
| Assessed DMFS not white spot lesions | |
| Assessed DMFS not white spot lesions | |
| Assessed DMFS not white spot lesions | |
| Not RCT | |
| Not RCT | |
| Not RCT | |
| Not RCT | |
| Not RCT | |
| Not RCT | |
| Split‐mouth study | |
| Ex vivo study ‐ outcomes measured on extracted teeth | |
| Not RCT | |
| Appears to be allocation based on study number (odd or even) and teeth allocated alternately. CCT. No reply to emails sent to contact author | |
| Not RCT | |
| Split‐mouth study | |
| Duration of intervention 12 months but outcomes assessed at end of treatment period not at the end of treatment with fixed orthodontic appliances | |
| Split‐mouth RCT | |
| Split‐mouth study, allocation of each side to treatment by alternation. Not RCT | |
| Split‐mouth study, allocation of each side to treatment by alternation.Not RCT | |
| Split‐mouth study, no random allocation. Author contacted | |
| Abstract only. Insufficient data, no subsequent publication identified | |
| Ex vivo study ‐ outcomes measured on extracted teeth | |
| Ex vivo study ‐ outcomes measured on extracted teeth | |
| Duration of intervention 12 months but outcomes assessed at end of treatment period not at the end of treatment with fixed orthodontic appliances | |
| Abstract only. No subsequent publication identified | |
| Split‐mouth study | |
| Allocation method not stated. Unable to contact the authors | |
| Allocation method not stated. Unable to contact the authors | |
| Intervention period was short (12 weeks) and assessments were not undertaken at the start and end of orthodontic treatment | |
| Not RCT | |
| Split‐mouth study. All participants had the same product used in the same quadrants. Not RCT.Contacted author (LR Dermaut). Unable to provide further data for statistical analysis | |
| Split‐mouth study | |
| Split‐mouth study | |
| Both groups had fluoride mouthrinse. The experimental group had in addition an antimicrobial mouthrinse, therefore the study looks at the efficacy of the antimicrobial mouthrinse rather than the fluoride mouthrinse | |
| Random allocation not mentioned. Brackets on alternate teeth bonded with each adhesive. Not RCT | |
| Split‐mouth study | |
| Split‐mouth study | |
| Not RCT | |
| Ex vivo study ‐ outcomes measured on extracted teeth | |
| Random allocation to treatment not mentioned. Author contacted | |
| Not RCT. Author contacted | |
| Effect of fluoride confounded by co‐intervention. Both groups had fluoride varnish. The experimental group had in addition an antimicrobial varnish therefore the study looks at the efficacy of the antimicrobial varnish rather than the fluoride varnish | |
| Effect of fluoride confounded by co‐intervention. 2 randomised groups and 1 non‐randomised control group. Both randomised groups received fluoride varnish every 12 weeks, fluoride exposure was not different between the 2 randomised groups |
CCT = controlled clinical trial; DMFS/DMFT = decayed, missing and filled surfaces/teeth.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Phase 4 study on prevention of incipient carious lesions (white spot lesions) in patients with fixed orthodontic appliances following the application of Elmex gel |
| Methods | Parallel‐group, double‐blind RCT |
| Participants | 314 healthy participants between 10 and 60 years of age, undergoing orthodontic treatment |
| Interventions | Toothbrushing with Elmex gel or placebo product once weekly during the entire study (12 to 30 months) plus tray application of test or control product 4 times per year |
| Outcomes | Visually detected white spot lesions |
| Starting date | April 2006 |
| Contact information | Principal Investigators Dr Meir Radlich ([email protected]) and Prof Paul George Jost‐Brinkman (paul‐g.jost‐[email protected]) |
| Notes | Email sent to Jost‐Brinkmann to request results 19/7/2012. Email reply 19/7/2012 stating that last participant now finished and data analysis about to start |
| Trial name or title | Caries‐preventive effectiveness of a dentifrice containing 5000 ppm fluoride ‐ a randomised controlled trial in adolescents with fixed orthodontic appliances |
| Methods | Parallel‐group single‐blind RCT |
| Participants | 420 healthy participants 11 to 16 years old, undergoing orthodontic treatment |
| Interventions | High‐dose (5000 ppm) fluoride toothpaste versus usual‐dose (1450 ppm) fluoride toothpaste |
| Outcomes | Incidence and severity of white spot lesions over the duration of orthodontic treatment (18 to 24 months) |
| Starting date | January 2008. Data collection expected to be complete July 2012 |
| Contact information | Professor SHA Twetman, University of Copenhagen ([email protected] ) |
| Notes | Email sent to Prof Twetman 24 June 2013. Reply 25 June 2013: "The study is completed and the manuscript was submitted for publication about one month ago. We have not yet received any response from the journal but if we are lucky, it will appear "on line" later this year." Abstract presented at European Orthodontic Society meeting, Reykjvik, Iceland, June 2013 |
| Trial name or title | Resin‐modified glass ionomer or composite for orthodontic bonding? A multicentre, randomised, single‐blinded clinical trial |
| Methods | A multicentre randomised single‐blinded controlled clinical trial with 2 parallel groups |
| Participants | 206 orthodontic patients requiring upper and/or lower preadjusted edgewise fixed appliance therapy, 11 years of age or older |
| Interventions | Brackets will be bonded to all teeth in front of the first permanent molars with either a resin‐modified glass ionomer cement (Fuji Ortho LC) or a light cured composite control (Transbond) |
| Outcomes | Primary: Incidence and severity of demineralisation at the end of treatment. Secondary: Incidence of first time bond failures |
| Starting date | February 2009 |
| Contact information | Dr Philip Benson, University of Sheffield ([email protected]) |
| Notes |
ppm = parts per million; RCT = randomised controlled trial.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DWLs Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Fluoride varnish versus placebo varnish, Outcome 1 Number of participants with new DWLs. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 White spot index Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Amine fluoride/stannous fluoride toothpaste/mouthrinse combination versus sodium fluoride toothpaste/mouthrinse combination, Outcome 1 White spot index. | ||||
| 2 Visible plaque index Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Amine fluoride/stannous fluoride toothpaste/mouthrinse combination versus sodium fluoride toothpaste/mouthrinse combination, Outcome 2 Visible plaque index. | ||||
| 3 Gingival bleeding index Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 Amine fluoride/stannous fluoride toothpaste/mouthrinse combination versus sodium fluoride toothpaste/mouthrinse combination, Outcome 3 Gingival bleeding index. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DWLs Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 Intraoral fluoride‐releasing glass bead device versus mouthrinse‐only control, Outcome 1 Number of participants with new DWLs. | ||||
| 1.1 Fluoride‐releasing intraoral device versus fluoride mouthrinse | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Fluoride varnish versus placebo varnish, Outcome 1 Number of participants with new DWLs.

Comparison 2 Amine fluoride/stannous fluoride toothpaste/mouthrinse combination versus sodium fluoride toothpaste/mouthrinse combination, Outcome 1 White spot index.

Comparison 2 Amine fluoride/stannous fluoride toothpaste/mouthrinse combination versus sodium fluoride toothpaste/mouthrinse combination, Outcome 2 Visible plaque index.

Comparison 2 Amine fluoride/stannous fluoride toothpaste/mouthrinse combination versus sodium fluoride toothpaste/mouthrinse combination, Outcome 3 Gingival bleeding index.
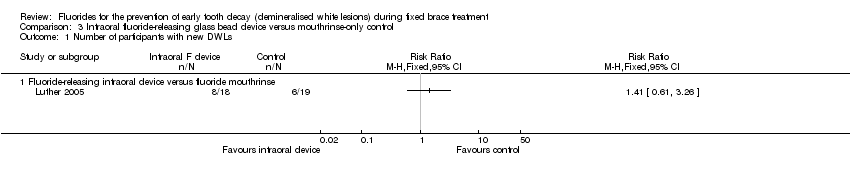
Comparison 3 Intraoral fluoride‐releasing glass bead device versus mouthrinse‐only control, Outcome 1 Number of participants with new DWLs.
| Fluoride varnish versus placebo varnish for the prevention of demineralised white lesions on teeth during fixed brace treatment | ||||||
| Patient or population: Participants undergoing orthodontic treatment with fixed appliances Comparison: Placebo varnish | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo varnish | Fluoride varnish | |||||
| Number of patients with new demineralised white lesions | Study population | RR 0.31 | 253 | ⊕⊕⊕⊝ | ||
| 640 per 1000 | 198 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| 1 A single study with 253 participants evaluated this outcome. Risk of bias was assessed as low. However, this finding should be interpreted with caution until the study has been replicated. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DWLs Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 White spot index Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Visible plaque index Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Gingival bleeding index Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DWLs Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Fluoride‐releasing intraoral device versus fluoride mouthrinse | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

