Fluorides for preventing early tooth decay (demineralised lesions) during fixed brace treatment
Abstract
Background
Early dental decay or demineralised lesions (DLs, also known as white spot lesions) can appear on teeth during fixed orthodontic (brace) treatment. Fluoride reduces decay in susceptible individuals, including orthodontic patients. This review compared various forms of topical fluoride to prevent the development of DLs during orthodontic treatment. This is the second update of the Cochrane Review first published in 2004 and previously updated in 2013.
Objectives
The primary objective was to evaluate whether topical fluoride reduces the proportion of orthodontic patients with new DLs after fixed appliances.
The secondary objectives were to examine the effectiveness of different modes of topical fluoride delivery in reducing the proportions of orthodontic patients with new DLs, as well as the severity of lesions, in terms of number, size and colour. Participant‐assessed outcomes, such as perception of DLs, and oral health‐related quality of life data were to be included, as would reports of adverse effects.
Search methods
Cochrane Oral Health's Information Specialist searched the following databases: Cochrane Oral Health's Trials Register (to 1 February 2019), the Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 1) in the Cochrane Library (searched 1 February 2019), MEDLINE Ovid (1946 to 1 February 2019), and Embase Ovid (1980 to 1 February 2019). The US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform were searched for ongoing trials. No restrictions were placed on the language or date of publication when searching the electronic databases.
Selection criteria
Parallel‐group, randomised controlled trials comparing the use of a fluoride‐containing product versus a placebo, no treatment or a different type of fluoride treatment, in which the outcome of enamel demineralisation was assessed at the start and at the end of orthodontic treatment.
Data collection and analysis
At least two review authors independently, in duplicate, conducted risk of bias assessments and extracted data. Authors of trials were contacted to obtain missing data or to ask for clarification of aspects of trial methodology. Cochrane's statistical guidelines were followed.
Main results
This update includes 10 studies and contains data from nine studies, comparing eight interventions, involving 1798 randomised participants (1580 analysed). One report contained insufficient information and the authors have been contacted.
We assessed two studies as at low risk of bias, six at unclear risk of bias, and two at high risk of bias.
Two placebo (non‐fluoride) controlled studies, at low risk of bias, investigated the professional application of varnish (7700 or 10,000 parts per million (ppm) fluoride (F)), every six weeks and found insufficient evidence of a difference regarding its effectiveness in preventing new DLs (risk ratio (RR) 0.52, 95% confidence interval (CI) 0.14 to 1.93; 405 participants; low‐certainty evidence). One placebo (non‐fluoride) controlled study, at unclear risk of bias, provides a low level of certainty that fluoride foam (12,300 ppm F), professionally applied every two months, may reduce the incidence of new DLs (12% versus 49%) after fixed orthodontic treatment (RR 0.26, 95% CI 0.11 to 0.57; 95 participants).
One study, at unclear risk of bias, also provides a low level of certainty that use of a high‐concentration fluoride toothpaste (5000 ppm F) by patients may reduce the incidence of new DLs (18% versus 27%) compared with a conventional fluoride toothpaste (1450 ppm F) (RR 0.68, 95% CI 0.46 to 1.00; 380 participants).
There was no evidence for a difference in the proportions of orthodontic patients with new DLs on the teeth after treatment with fixed orthodontic appliances for the following comparisons:
‐ an amine fluoride and stannous fluoride toothpaste/mouthrinse combination versus a sodium fluoride toothpaste/mouthrinse,
‐ an amine fluoride gel versus a non‐fluoride placebo applied by participants at home once a week and by professional application every three months,
‐ resin‐modified glass ionomer cement versus light‐cured composite resin for bonding orthodontic brackets,
‐ a 250 ppm F mouthrinse versus 0 ppm F placebo mouthrinse,
‐ the use of an intraoral fluoride‐releasing glass bead device attached to the brace versus a daily fluoride mouthrinse.
The last two comparisons involved studies that were assessed at high risk of bias, because a substantial number of participants were lost to follow‐up.
Unfortunately, although the internal validity and hence the quality of the studies has improved since the first version of the review, they have compared different interventions; therefore, the findings are only considered to provide low level of certainty, because none has been replicated by follow‐up studies, in different settings, to confirm external validity.
A patient‐reported outcome, such as concern about the aesthetics of any DLs, was still not included as an outcome in any study. Reports of adverse effects from topical fluoride applications were rare and unlikely to be significant. One study involving fluoride‐containing glass beads reported numerous breakages.
Authors' conclusions
This review found a low level of certainty that 12,300 ppm F foam applied by a professional every 6 to 8 weeks throughout fixed orthodontic treatment, might be effective in reducing the proportion of orthodontic patients with new DLs. In addition, there is a low level of certainty that the patient use of a high fluoride toothpaste (5000 ppm F) throughout orthodontic treatment, might be more effective than a conventional fluoride toothpaste. These two comparisons were based on single studies. There was insufficient evidence of a difference regarding the professional application of fluoride varnish (7700 or 10,000 ppm F). Further adequately powered, randomised controlled trials are required to increase the certainty of these findings and to determine the best means of preventing DLs in patients undergoing fixed orthodontic treatment. The most accurate means of assessing adherence with the use of fluoride products by patients and any possible adverse effects also need to be considered. Future studies should follow up participants beyond the end of orthodontic treatment to determine the effect of DLs on patient satisfaction with treatment.
PICO
Plain language summary
Fluorides for preventing early tooth decay (demineralised lesions) during fixed brace treatment
Review question
Ugly white or brown marks sometimes appear on the teeth during treatment with braces to straighten teeth. These are due to early tooth decay and usually occur with fixed, glued‐on 'train track', braces, which make it more difficult to clean the teeth.
We know that fluoride in toothpaste helps to prevent tooth decay and think that if extra fluoride is given to people wearing fixed braces, it will protect them from getting these marks. The aim of this Cochrane Oral Health's review was to look at how well fluorides help to prevent early tooth decay during fixed brace treatment and to find out the best way to get fluoride to the teeth.
Background
Wearing a fixed brace makes it harder for people to keep their teeth clean and may also cause pain. Pain can make it more difficult for people to brush their teeth. This can lead to a build‐up of dental plaque around the brackets that attach the fixed brace to the teeth, and if the plaque stays on the tooth for long enough, it will cause early tooth decay, which looks like white or brown marks (demineralised lesions, also known as white spot lesions). People often wear braces for 18 months or longer and if the decay is left to progress, it can cause holes, which are sometimes bad enough to need fillings to be done in the teeth.
Fluoride helps the tooth to heal, reducing tooth decay in people who are at risk of developing it. People receiving fixed brace treatment may be given different forms of fluoride treatment. It is important to think about how the fluoride gets to the teeth. Does the fluoride need to be placed by a dentist or dental nurse, or can people having treatment with braces apply the fluoride to their own teeth?
Study characteristics
This review is up‐to‐date as of 1 February 2019. The review includes 10 studies but we could only use the information from nine studies involving 1798 randomised people. We have asked for more information about one study. The review looks at eight different ways of applying fluoride to the teeth. People taking part in the studies were all having treatment with fixed braces. The number of people with new decay on the teeth at end of fixed brace treatment, as well as the amount of decay in each person, were measured and counted.
We compared the following treatments:
‐ dentist or nurse‐applied fluoride e.g. varnish, gel or foam,
‐ patient‐applied/used fluoride e.g. toothpaste, mouthwash, gel or foam, and
‐ materials that release fluoride over time e.g. glues, elastic bands.
Key results
One study showed that when the dentist applies a foam with a high level of fluoride in it onto the teeth every time the patient is seen, this might reduce the risk of new decay. Another study found that if patients use a toothpaste with a higher level of fluoride than normal, then this might also reduce the risk of new marks on their teeth.
No studies have shown that other ways of giving the teeth extra fluoride reduced the number and/or size of new decay on teeth in people wearing fixed braces. Harmful effects of the different ways of giving the teeth more fluoride were not reported in any of the included studies.
Certainty of the evidence
The level of belief we have in these findings is low, due to the lack of studies testing the same fluorides and showing the same results. We suggest that more, well‐conducted studies should be done in this area.
Authors' conclusions
Summary of findings
| Fluoride varnish compared to non‐fluoride (placebo) varnish for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With non‐fluoride (placebo) varnish | With fluoride varnish | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: pre‐treatment and day of debond clinical intraoral photographs Follow‐up: 1.7 years | 28.80% | 15% | 13.80% fewer | RR 0.52 | 405 | ⊕⊕⊝⊝ | The evidence that professional application of fluoride varnish (7700 or 10,000 ppm F) every 6 weeks to the teeth of patients wearing fixed orthodontic braces reduces the number of new DLs is equivocal |
| Number of participants with more severe DLs (severity of DLs) (score 3 or 4 versus score 1 or 2) Follow‐up: 1.7 years | 26% | 12% | 14.10% fewer | RR 0.46 | 148 | ⊕⊕⊝⊝ | The evidence suggests that when a dentist or nurse applies 7700 ppm F (ammonium fluoride) varnish every 6 weeks to a patient wearing a fixed orthodontic brace there may a reduction in the number of orthodontic patients with more severe DLs (score 3 or 4 versus score 1 or 2) |
| Number of participants with adverse effects (adverse effects) Follow‐up: 1.7 years | No evidence that the intervention had adverse effects | 148 | ⊕⊕⊝⊝ | Only 1 participant with an adverse event and not clear if this was directly related to the intervention | |||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 1 level for indirectness (evidence from only 2 studies) (Stecksén‐Blicks 2007; Sonesson 2019). | |||||||
| 12,300 ppm F APF foam compared to 0 ppm F placebo foam for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Certainty of the evidence | Number of participants (studies) | Comments | ||
| With 0 ppm F placebo foam | With 12,300 ppm F APF foam | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: clinical assessment Follow‐up: mean 18 months | 48.90% | 12.70% | 36.20% fewer | RR 0.26 | ⊕⊕⊝⊝ | 95 | The evidence suggests that when foam, containing 12,300 ppm F, is applied by a dentist or a nurse, every 2 months, to the teeth of patients wearing fixed orthodontic appliances there might be a reduction in the number of patients who have at least 1 new DL |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) | None of the trials reported this outcome | ||||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aAlthough effect size is large this was only for 1 study at unclear risk of bias and therefore downgraded 1 level (Jiang 2013). | |||||||
| 5000 ppm F toothpaste compared to 1450 ppm F toothpaste for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With 1450 ppm F toothpaste | With 5000 ppm F toothpaste | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: pre‐treatment and post‐treatment clinical intraoral photographs Follow‐up: 1.8 years | 26.60% | 18.10% | 8.50% fewer | RR 0.68 | 380 | ⊕⊕⊝⊝ | The evidence suggests that in patients wearing an orthodontic fixed brace use of a daily 5000 ppm F toothpaste compared with a daily 1450 ppm F toothpaste throughout treatment may lead to a reduction in the number of orthodontic patients with new DLs |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) | None of the trials reported this outcome | ||||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 1 level due to single study at unclear risk of bias (Sonesson 2014). | |||||||
| 250 ppm F mouthrinse (100 ppm amine F/150 ppm NaF) compared to 0 ppm F placebo mouthrinse for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With 0 ppm F placebo mouthrinse | With 250 ppm F mouthrinse (100 ppm amine F/150 ppm NaF) | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: QLF Follow‐up: 24.5 months | 46.70% | 30.30% | 16.30% fewer | RR 0.65 | 81 | ⊕⊝⊝⊝ | The evidence is very uncertain about the effect of a daily 250 ppm F mouthrinse (100 ppm amine F/150 ppm NaF) compared with a daily 0 ppm F placebo mouthrinse on the number of patients wearing a fixed orthodontic brace with new DLs |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) | None of the trials reported this outcome | ||||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 2 levels: single study with a relatively small number of participants (81), at high risk of bias due to high attrition (33%) (van der Kaaij 2015). | |||||||
| Resin‐modified glass ionomer cement compared to light‐cured composite resin for bonding orthodontic brackets for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With light‐cured composite resin | With resin‐modified glass ionomer cement | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: before and day of debond clinical intraoral photographs Follow‐up: 17.6 months | 22.40% | 26.20% | 3.80% more | RR 1.17 | 173 | ⊕⊕⊝⊝ | The evidence suggests that resin‐modified glass ionomer cement for bonding orthodontic brackets compared with light‐cured composite resin results in little to no difference in the number of orthodontic patients with new DLs |
| Number of participants with more severe DLs of aesthetic concern (severity of DLs) Assessed with: pre‐treatment and day of debond clinical intraoral photographs Follow‐up: 17.6 months | 8.00% | 9.40% | 1.40% more | RR 1.18 | 173 | ⊕⊕⊝⊝ | The evidence suggests that using resin‐modified glass ionomer cement for bonding orthodontic brackets compared with light‐cured composite resin results in little to no difference in the number of orthodontic patients with more severe DLs of aesthetic concern |
| Number of participants with adverse effects (adverse effects) Follow‐up: 17.6 months | No evidence that either intervention had adverse effects | 173 | ⊕⊕⊝⊝ | ‐ | |||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 1 level: single study at unclear risk of bias (Benson 2019). | |||||||
Background
Description of the condition
During orthodontic treatment with fixed appliances, brackets are attached to the teeth to hold the wires that provide the forces to straighten the teeth. One of the adverse effects of fixed braces is that dental plaque collects around the attachments, leading to accumulation of the types of bacteria that cause dental disease (Naranjo 2006). Build‐up of dental plaque around orthodontic brackets is associated with increased risk of demineralised lesions (DLs, also known as white spot lesions), which can be visible within six months (Tufekci 2011). Demineralisation is an early, but reversible, stage in the development of dental decay (caries). Cariogenic bacteria present in the dental plaque change sugar in the diet into organic acids, which start to damage the tooth enamel. Effective removal of plaque will prevent DLs from occurring; however, the presence of orthodontic appliances in the mouth and associated dental pain may make it more difficult for individuals to adequately clean their teeth and braces. DLs developing on the labial and buccal surfaces of teeth during orthodontic treatment can become a significant problem over the course of treatment, which may last for 18 months or longer, resulting in a poor appearance of the teeth following straightening (Maxfield 2012). In severe cases the caries can make a hole in the tooth that will require a filling (restoration), which may be both painful and costly.
Enaia and colleagues (Enaia 2011) used clinical photographs of the teeth taken before and after fixed brace treatment to show that whereas 32% of people in their study had DLs before the brace was fitted, this rose to 74% after their braces had been taken off. Most of the DLs were minor, but a significant minority of participants (10%) had holes in their teeth, which may have required a filling. Although DLs tend to fade with time as they heal, one study has shown that, even five years after treatment, a significant proportion of people who had worn fixed braces showed some evidence of DLs caused by the braces compared with a control group of people who had not had a fixed brace (Ogaard 1989).
Description of the intervention
Orthodontists are keen to prevent the development of DLs so their patients may have the best possible appearance after orthodontic treatment ‐ straight teeth with no marks. Fluoride is important in the prevention of dental decay (ten Cate 2013). Marinho and colleagues (Marinho 2016) found a definite reduction in dental decay in children and adolescents who performed regular supervised rinsing with a fluoride mouthwash. It has also been shown that fluoride may reduce the number of DLs that develop during brace treatment. When orthodontic participants used a mouthrinse, Geiger et al (Geiger 1992) found a 30% reduction in the number of participants with DLs and a 25% reduction in the incidence of teeth affected by DLs. Many orthodontists recommend the use of a daily fluoride mouthrinse throughout brace treatment to prevent DLs (Kerbusch 2012).
Several methods (in addition to fluoridated toothpaste) are used to deliver fluoride to teeth in patients during orthodontic treatment. These include the following:
-
topical fluorides (e.g. mouthrinse, gel, varnish or foam) that are applied by the dentist or nurse when the orthodontic patient is seen to adjust their brace;
-
topical fluorides (e.g. toothpaste, mouthrinse, gel or foam) that the orthodontic patient can apply themselves at home;
-
fluoride‐releasing materials (e.g. glues used to bond the brackets onto the teeth and orthodontic elastics that are impregnated with fluoride);
-
dietary fluoride supplementation (e.g. fluoridated milk).
How the intervention might work
Fluoride present in the mouth reduces caries development via three mechanisms: inhibition of the demineralisation of dental enamel, enhancement of the remineralisation of dental enamel producing a remineralised layer that is resistant to acid attack, and inhibition of the bacterial enzymes that produce the acid (Lynch 2006; ten Cate 2013).
Most children undergoing orthodontic treatment will be exposed to some fluoride ‐ low concentrations in the water supply, higher concentrations from fluoridated toothpaste, or both. Use of other topical fluorides or fluoride sources designed to deliver additional fluoride to the at‐risk area, or both, near orthodontic brackets, are likely to further reduce the risk of DL development. Topical fluorides include fluoride toothpastes, mouthrinses, gels, varnishes and dietary sources (e.g. fluoridated milk). Specific orthodontic sources of fluoride include bracket adhesives and orthodontic elastic bands (elastomeric ligatures), which slowly release fluoride into the mouth. All of these fluoride sources release fluoride into saliva that is distributed throughout the mouth.
Why it is important to do this review
Several systematic reviews have concluded that the use of topical fluoride in various forms reduce the prevalence and incidence of dental caries in children and adolescents (Marinho 2003a; Marinho 2003b; Marinho 2004; Marinho 2016). Orthodontists have, therefore, routinely recommended the use of topical fluoride mouthrinses to their patients wearing fixed appliances or apply fluoride in the form of varnish, gel or foam to reduce the risk of orthodontic patients developing dental caries. Others use fluoride‐releasing materials to attach the brackets or bands to the teeth. Clear evidence is lacking, regarding the optimum concentration of topical fluoride, the optimum frequency of use and the effects of topical fluorides and fluoride‐releasing materials over the whole length of orthodontic treatment.
This Cochrane Review was first published in 2004 (Benson 2004). It was updated in 2013 with an amended protocol to only include appropriately designed randomised studies, using parallel groups and measuring relevant outcomes over the full length of orthodontic treatment (Benson 2013). This is the second update.
Objectives
The primary objective of this review was to evaluate whether topical fluoride reduces the proportion of orthodontic patients with new demineralised lesions (DLs) after fixed appliances.
The secondary objectives were to examine the effectiveness of different modes of fluoride delivery in reducing the proportions of orthodontic patients with new DLs, as well as the severity of lesions, in terms of number, size and colour. Participant‐assessed outcomes, such as perception of DLs, and oral health‐related quality of life data were to be included, as would reports of adverse effects.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) in which fluoride was delivered by any method to prevent the development of new enamel demineralised lesions (DLs) during fixed orthodontic treatment. As topical fluorides are distributed throughout the mouth by saliva, the use of a within‐person or split‐mouth study design to evaluate these interventions is inappropriate, due to potential carry‐across effects (Pandis 2013) and any study using this design was excluded. Studies involving multiple arms would be examined and only comparisons between two fluoride interventions or fluoride versus no fluoride interventions would be included in the pairwise analysis.
Types of participants
Included were participants of any age who had orthodontic treatment with fixed braces in situations where DLs were assessed on teeth remaining in the mouth at the end of orthodontic treatment (at debonding, immediately after the active fixed brace is removed). We excluded studies that evaluated demineralisation of extracted teeth (ex vivo) or that were undertaken over short periods of time i.e. less than the whole time the fixed brace was in the mouth.
Types of interventions
-
Topical fluoride in the form of toothpaste, mouthrinse, gel, varnish, foam or dietary sources at any dose, frequency, duration or method of administration, and with any of the following active agents/ingredients: NaF (sodium fluoride), SMFP (sodium monofluorophosphate), SnF (stannous fluoride), APF (acidulated phosphate fluoride) and amine F (amine fluoride) applied either by a professional in the dental surgery or office, or used by the patient at home.
-
Materials containing fluoride that is potentially released during treatment, including fluoride‐releasing composite resin‐bonding materials, compomers, glass ionomer cements and resin‐modified glass ionomers for bonding or banding, slow‐release fluoride beads/devices and fluoride‐releasing elastomeric ligatures.
-
The control group comprising of individuals not subjected to the fluoride intervention, but instead treated with a placebo, such as a non‐fluoride toothpaste and mouthrinse, or given no intervention. Studies involving a control subjected to an alternative fluoride intervention were also included.
Types of outcome measures
Primary outcomes
-
The primary outcome was the difference in the proportion of participants in the experimental and comparison groups with new DLs on the day the fixed appliance was removed.This could be assessed directly from the participant (clinically) or preferably from start and finish photographs or fluorescent images of the teeth immediately after the active fixed brace was removed. If the number of DLs was not recorded at the start of treatment, the outcome was the presence or absence of DLs at the end of orthodontic treatment, again assessed directly from the participant or indirectly from photographs or fluorescent images of the teeth. It is important that the assessment was carried out on the day the appliance was removed (or as close to this as possible), because the white marks will tend to heal (remineralise) after the brace is removed. The rate at which the DLs remineralise can be variable between individuals and is another potential confounding factor.
Secondary outcomes
-
Differences in the severity of the new DLs, as assessed by number, size and colour between experimental and control groups at the end of orthodontic treatment.
-
Any quantitative assessment of enamel mineral loss, such as fluorescent light techniques or microradiography, used with in situ caries models (Benson 2010) at the end of treatment.
-
Any participant‐assessed outcomes, such as perception of DLs and oral health‐related quality of life data.
-
Adverse effects.
Search methods for identification of studies
Electronic searches
Cochrane Oral Health's Information Specialist conducted systematic searches in the following databases for randomised controlled trials and controlled clinical trials. There were no language, publication year or publication status restrictions:
-
Cochrane Oral Health's Trials Register (searched 1 February 2019) (Appendix 1);
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 1) in the Cochrane Library (searched 1 February 2019) (Appendix 2);
-
MEDLINE Ovid (1946 to 1 February 2019) (Appendix 3);
-
Embase Ovid (1980 to 1 February 2019) (Appendix 4).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 6 (Lefebvre 2011).
Searching other resources
The following trial registries were searched for ongoing studies (see Appendix 5 for details of the search terms used):
-
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 1 February 2019);
-
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 1 February 2019).
We searched the reference lists of included studies and relevant systematic reviews for further studies.
We checked that none of the included studies in this review were retracted due to error or fraud.
We did not perform a separate search for adverse effects of interventions used, we considered adverse effects described in included studies only.
Data collection and analysis
Selection of studies
The search was designed to be sensitive and include controlled clinical trials, these were filtered out early in the selection process if they were not randomised.
Two review authors independently examined the title, keywords and abstract of reports identified through electronic searching for evidence of three criteria.
-
A randomised clinical trial of participants undergoing orthodontic treatment with fixed appliances.
-
A trial comparing the use of a fluoride‐containing product versus a non‐fluoride control or an alternative fluoride product.
-
A trial that assessed the prevalence or incidence of DLs either at the start and at the end of orthodontic treatment or just at the end of treatment, where the end was defined as the day of removal of the fixed appliance or as soon as possible thereafter.
For studies that appeared to meet the inclusion criteria, or for which data in the title and abstract were insufficient to allow a clear decision, the full report was obtained. We resolved disagreements by discussion.
No language restrictions were applied. Translations of foreign language articles were produced by contacts within Cochrane Oral Health.
Data extraction and management
Two review authors extracted data independently, in duplicate, using specially designed data extraction forms. The data extraction forms were piloted on several papers and were modified as required before use. Any disagreement was discussed, and a third review author was consulted when necessary. We contacted all study authors for clarification of missing information. Data from studies in which the reporting was incomplete were not included in the analysis until the corresponding author of the study had supplied adequate clarification. If agreement could not be reached, data were excluded from the review. All studies that met the inclusion criteria underwent an assessment of the risk of bias. We extracted data from the published report; however if the report was unclear or lacking in important information then the corresponding author of the article was contacted by e‐mail. We recorded studies rejected at this or subsequent stages, along with reasons for exclusion, in the 'Characteristics of excluded studies' tables.
For each trial, we recorded the following data.
-
Year of publication and country of origin.
-
Study design.
-
Unit of randomisation.
-
Details of participants, including demographic characteristics and criteria for inclusion.
-
Details of types of interventions (method of delivery of fluoride, dose, duration of use).
-
Details of outcomes reported (number, size and severity of DLs), including method of assessment and mean duration of the study.
Assessment of risk of bias in included studies
This assessment was conducted by using the recommended approach for assessing risk of bias in studies included in Cochrane Reviews (Higgins 2011). We used the two‐part tool to address the six specific domains (namely, sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and other bias). Each domain includes one or more specific entries in a 'Risk of bias' table. Within each entry, the first part of the tool involves describing what was reported to have happened in the study. The second part of the tool involves assigning a judgement relating to the risk of bias for that entry: either low risk, unclear risk or high risk.
The domains of sequence generation, allocation concealment, incomplete outcome data and selective outcome reporting are addressed in the tool by a single entry for each study. For blinding, two entries were used because assessments need to be made separately for (1) participants and operators/orthodontists and (2) outcome assessors. When the operator/orthodontist assessed the outcome of the trial, this was noted. The final domain ('other sources of bias') was assessed as a single entry for studies as a whole.
Two review authors undertook the risk of bias assessment independently and in duplicate as part of the data extraction process. We resolved disagreements by discussion.
After taking into account additional information provided by the authors of the trials, review authors grouped studies into the following categories.
| Risk of bias | Interpretation | Within a study | Across studies |
| Low risk of bias | Plausible bias unlikely to seriously alter the results | Low risk of bias for all key domains | Most information comes from studies at low risk of bias |
| Unclear risk of bias | Plausible bias that raises some doubt about the results | Unclear risk of bias for one or more key domains | Most information comes from studies at low or unclear risk of bias |
| High risk of bias | Plausible bias that seriously weakens confidence in the results | High risk of bias for one or more key domains | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results |
We completed a 'Risk of bias' table for each included study. We also presented the results graphically (Figure 1).

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Measures of treatment effect
For dichotomous outcomes, we expressed the estimate of effect of an intervention as risk ratios (RRs) together with 95% confidence intervals (CIs). For continuous outcomes, we estimated mean differences (MDs) and 95% CIs.
Unit of analysis issues
In parallel‐group trials in which participants are randomly assigned to intervention or to control and a single outcome measure per participant is reported, the analysis is straightforward. When individuals are randomly assigned to treatment, each individual has a number of teeth exposed to the intervention or to the control. When the outcome is reported per number of teeth, the data should be adjusted for clustering within the mouth of each individual to avoid unit of analysis errors. If it was unclear from the reports of included trials whether clustering had been considered, authors were contacted to clarify how this dependence had been accounted for in the analysis.
Dealing with missing data
When data were not available in the printed report, or when data were unclear, we contacted the corresponding author of the study to obtain the missing data. The analysis generally includes only available data (ignoring missing data); we would, however, have used methods of estimating missing standard deviations as provided in Section 7.7.3 of theCochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), if appropriate. Otherwise, we did not undertake any imputations or use statistical methods to allow for missing data.
Assessment of heterogeneity
Pooling of data and meta‐analysis were carried out only if sufficient similarities were noted between studies in types of participants, interventions and outcomes, including the time of the outcome measurement. If any trials were pooled, the significance of discrepancies in the estimates of treatment effects from the different trials was to be assessed by using Cochran's test for heterogeneity, by which heterogeneity was considered significant if P < 0.1 (Higgins 2011).
The I2 statistic, which describes the percentage total variation across studies that is due to heterogeneity rather than to chance, was used to quantify heterogeneity, with I2 greater than 50% considered to show substantial heterogeneity (Higgins 2011: Section 9.5.2).
Assessment of reporting biases
Only a proportion of research projects conducted are ultimately published in an indexed journal and become easily identifiable for inclusion in systematic reviews. Reporting biases arise when reporting of research findings is influenced by the nature and direction of the findings of the research. We investigated and attempted to minimise in this review potential reporting biases, including publication bias, time lag bias, multiple (duplicate) publication bias and language bias.
If more than ten studies were included for one outcome, we would have constructed a funnel plot. Any asymmetry in the funnel plot indicating possible publication bias would have been investigated by statistical analysis using the methods introduced by Egger 1997 (continuous outcome) and Rücker 2008 (dichotomous outcome) (such analysis would have been done in STATA 11.0). However, insufficient trials were included in this review to enable the review authors to investigate publication bias.
Data synthesis
A meta‐analysis was to be conducted only if studies of similar comparisons reported the same outcome measures. Risk ratios would have been combined for dichotomous data and mean differences for continuous data, using random‐effects models, provided more than three studies were included in the meta‐analysis.
Subgroup analysis and investigation of heterogeneity
We planned to investigate clinical heterogeneity by examining the different sources of fluoride. Provided sufficient studies were identified for each intervention and outcome, we planned a priori to conduct subgroup analyses for different sources of fluoride (mouthrinse, gel, varnish dentifrice, bracket adhesive, elastomeric ligature).
Sensitivity analysis
It was planned to undertake sensitivity analyses to examine the effects of quality assessment items on the assessment of overall estimates of effect. In addition, the effect on findings of the review of including unpublished literature was to be examined. However, insufficient trials were included in the review for a sensitivity analysis to be undertaken.
Summary of findings
We developed 'Summary of findings' tables for the comparisons that were considered most important for decision makers and the outcomes number of participants with new DLs on the day the fixed appliance was removed, number of participants with more severe DLs, and number of participants with adverse effects using GRADEpro GDT software (GRADEpro GDT 2015). We assessed the level of certainty in the findings with reference to the risk of bias assessments, the directness of the evidence, the inconsistency of the results, the precision of the estimates, and the risk of publication bias. The level of certainty for each of the comparisons was categorised as high, moderate, low, or very low.
Results
Description of studies
Results of the search
Searches were originally done in July 2003, then repeated in May 2012, January 2013, December 2016, January 2018 and February 2019.
The first version of this review included 14 trials, involving 613 participants. The review protocol was amended for the 2013 update to include only randomised studies (excluding quasi‐randomised or controlled clinical trials), using parallel groups and measuring relevant outcomes over the full length of orthodontic treatment. This resulted in the exclusion of all included studies from the first version, for the following reasons: five were quasi‐randomised (Banks 2000; Dyer 1982; Hirschfield 1978; Millett 2000; Sonis 1989), five were within‐person or split‐mouth designs (Chung 1998; Czochrowska 1998; Gillgrass 2001; Marcusson 1997; Twetman 1997) and three had ex vivo outcomes on extracted teeth (Gorton 2003; Ogaard 1986; Pascotto 2004). Ogaard 2001 was excluded because investigators compared fluoride versus fluoride plus an antiseptic solution.
The 2013 update included three studies (Luther 2005; Ogaard 2006; Stecksén‐Blicks 2007), involving 458 randomised participants (391 analysed). For the 2019 update a further seven studies were identified for inclusion (Benson 2019; He 2010; Jiang 2013; Jost‐Brinkman 2017; Sonesson 2014; Sonesson 2019; van der Kaaij 2015). Three ongoing studies were also identified (DRKS00012533; DRKS00012540; IRCT2016122531558N1).
For details of the studies examined and reasons for inclusion or exclusion, please see Characteristics of included studies and Characteristics of excluded studies tables. The search process and results are presented as a flow chart in Figure 2.

Study flow diagram.
Included studies
Characteristics of the trial participants and settings
Seven of the included studies were conducted in Europe, involving Sweden (Ogaard 2006; Sonesson 2014; Sonesson 2019; Stecksén‐Blicks 2007), the UK (Luther 2005), the UK and Republic of Ireland (Benson 2019), and the Netherlands (van der Kaaij 2015). One study was undertaken in Germany and Israel (Jost‐Brinkman 2017) and two in China (He 2010; Jiang 2013). Participant age ranged from 10 years at the start of treatment (Jost‐Brinkman 2017) to 60 years (Jost‐Brinkman 2017). All participants in the included trials were recruited at the start of their orthodontic treatment with fixed appliances and were followed until their fixed appliances were removed.
Characteristics of the interventions
We have grouped the included trials into three broad comparisons.
-
Dentist or nurse‐applied fluoride in the form of varnish (He 2010; Sonesson 2019; Stecksén‐Blicks 2007), foam (Jiang 2013), and gel (Jost‐Brinkman 2017), both home use once a week and professional application every three months.
-
Patient‐applied/used fluoride in the form of toothpaste/mouthrinse combinations (Ogaard 2006; Sonesson 2014; van der Kaaij 2015).
-
Fluoride‐releasing materials in the form of intraoral fluoride‐releasing glass beads device (Luther 2005) and resin‐modified glass ionomer cement for bonding orthodontic brackets (Benson 2019).
One study (Jost‐Brinkman 2017) investigated both a dentist/nurse‐applied and a patient‐applied fluoride intervention in the same participants. Adherence to home use is more difficult to assess than adherence to dentist or nurse‐applied therefore it was categorised in the latter. There were no studies investigating dietary fluoride supplementation.
Five studies were placebo‐controlled, comparing a fluoride‐containing product with the same product not containing fluoride, where participant, clinician/operator and assessor were all masked as to group allocation (Jiang 2013; Jost‐Brinkman 2017; Sonesson 2019; Stecksén‐Blicks 2007; van der Kaaij 2015). In four studies just the assessor was masked for group allocation, due to differences in the nature of the interventions. One study was a comparison of fluoride varnish versus placebo (He 2010). One study was a comparison of two products containing fluoride (Sonesson 2014), one was a comparison of two methods of delivering fluoride (Luther 2005) and one study compared one fluoride and one non‐fluoride containing bonding material (Benson 2019). One study compared two fluoride products, but the masking was unclear (Ogaard 2006).
Characteristics of the outcomes
Seven studies reported our primary outcome of number of participants in each group with new demineralised lesions (DLs) (Benson 2019; Jost‐Brinkman 2017; Luther 2005; Sonesson 2014; Sonesson 2019; Stecksén‐Blicks 2007; van der Kaaij 2015). One study reported the number of teeth in each group with new DLs (Jiang 2013), one study reported a mean index score (Ogaard 2006), and in one study the outcome was unclear (He 2010).
All reported some outcomes on the severity of DLs in terms of differences in the number, size, colour, or quantitative measurement of mineral loss. None of the included studies reported outcomes of participant perception of their DLs or oral health‐related quality of life, and only one study reported adverse effects (Sonesson 2019).
Excluded studies
The details and reasons for exclusion are outlined in the Characteristics of excluded studies table. The main reasons for exclusion were that participants were not followed to the end of their orthodontic treatment and an inappropriate research methodology was used (within‐person or split‐mouth design).
Risk of bias in included studies
Overall risk of bias assessments for all included studies are shown in Figure 1. Two studies were assessed at low risk of bias for all domains (Sonesson 2019; Stecksén‐Blicks 2007). Two studies were assessed as at unclear risk of bias in one or two domains (Benson 2019; Sonesson 2014) and four in more than two domains (He 2010; Jiang 2013; Jost‐Brinkman 2017; Ogaard 2006). Two studies were assessed as at high risk of bias in one domain (Luther 2005; van der Kaaij 2015) due to a high proportion of participants withdrawing or dropping out of the studies. The authors of the studies have been contacted for further information, but at the time of publication we are awaiting clarification from the authors of two studies (Jost‐Brinkman 2017; Ogaard 2006) and one is currently uncontactable (He 2010).
Allocation
We assessed six of the included studies at low risk of bias, because the method of sequence generation and clear allocation concealment were considered adequate from either the description in the reported or following further clarification from the study authors (Benson 2019; Luther 2005; Sonesson 2014; Sonesson 2019; Stecksen‐Blicks 2007; van der Kaaij 2015).
Three studies (He 2010; Jiang 2013; Ogaard 2006) reported the method of sequence generation (randomisation table), but did not mention how they achieved equal numbers of participants in each group (since clarified for Jiang 2013) or method of allocation concealment. One study described the method of allocation concealment, but did not report the method of sequence generation (Jost‐Brinkman 2017). They were all assessed as at unclear risk of selection bias.
Blinding
In five studies the participant, clinician and assessor were all considered masked to group allocation, because the authors reported that the substances provided to the active and control groups were identical in presentation, taste, appearance and consistency (Jiang 2013; Jost‐Brinkman 2017; Sonesson 2019; Stecksén‐Blicks 2007; van der Kaaij 2015). Due to the nature of the materials used in three studies it was not possible to mask the clinician as to group allocation and the participant could have guessed (Benson 2019; Luther 2005; Sonesson 2014). It is not clear how knowledge of group allocation might affect the behaviour of the clinician and participant, so these were judged to be an unclear risk of performance bias. In one study the masking was not clear (Ogaard 2006) and the author has been contacted. In one study, the participants received different preventative regimens, at different times, therefore neither participants or operators could be masked (He 2010).
Nine studies reported that the outcome assessors were masked as to group allocation. In four of these studies more than one expert judge was involved in assessing before treatment and day of debond or close to debond photographs for new DLs (Benson 2019; Sonesson 2014; Sonesson 2019; Stecksén‐Blicks 2007). In two studies only one assessor was involved, but using relatively objective measures of demineralisation (image analysis (Luther 2005), and quantitative light‐induced fluorescence (QLF) (van der Kaaij 2015)). These were judged to be at low risk of detection bias.
We are still awaiting clarification from Jost‐Brinkman 2017 about who and how many undertook the clinical assessments, whether they were calibrated and whether any assessment of reproducibility was undertaken.
Jiang 2013 reported that assessments were undertaken clinically by one masked assessor. Although the assessor was described as having participated in the 'initial calibration trial' and intraexaminer agreement was assessed before the start of the trial, it is not clear if the repeatability was good for the full length of the trial and whether the assessor agreed with other calibrated assessors. This study was therefore assessed to be an unclear risk of detection bias.
Ogaard 2006 indicates that clinical assessments and colour photographs were obtained prior to bonding and at debond, but does not state that the photographs were used in the assessment. There are no details about who carried out the assessments or whether they were calibrated. No repeatability or reproducibility assessments are reported and this study was therefore judged to be an unclear risk of detection bias.
In He 2010 the number of assessors was unclear. It was also judged to be an unclear risk of detection bias.
Incomplete outcome data
The proportion of post‐randomisation exclusions was reported as zero in one study (He 2010), and low in four studies (Benson 2019; Jiang 2013; Sonesson 2019; Stecksén‐Blicks 2007). The numbers and reasons for exclusion were similar for each group and the risk of attrition bias and the effect of this on the interpretation of the findings is outlined in the 'Risk of bias' tables for each study. The report by Benson 2019 had a flow diagram and fully reported the reasons for withdrawal or dropout, which were about equal in the two groups. Two studies were assessed as an unclear risk of attrition bias (Ogaard 2006; Sonesson 2014). The reasons for this are given in the 'Risk of bias' tables for each study. The report by Ogaard 2006 had neither a flow diagram, nor a detailed explanation of the reasons for withdrawal or dropout. Sonesson 2014 had a flow diagram and reported the reasons for withdrawal or dropout, however it reports that a number of participants "did not comply with the study protocol" and were excluded from the analysis, but the definition of non‐compliance is unclear. Due to inconsistencies on the number of exclusions from analyses and lack of clarity on non‐compliance Jost‐Brinkman 2017 was also assessed as at unclear risk of attrition bias. Two studies were assessed as at high risk of attrition bias, because a significant proportion of the participants who were randomised were not included in the analysis (47% (Luther 2005), 33% (van der Kaaij 2015)).
Selective reporting
Ogaard 2006 reported the change in the mean Gorelick Index scores, as well as the numbers of teeth with new DLs and was assessed as at unclear risk of reporting bias. The report by Luther 2005 had some information missing and the denominators were not stated, so this study was assessed at unclear risk of reporting bias. In He 2010 the definition of incidence is unclear (difference between start and finish) and it does not state how they took into account the clustering of teeth within the mouth, therefore the study was also assessed at unclear risk of reporting bias.
Other potential sources of bias
Four studies reported data for the number of participants with new DLs at or near the date of debond (Benson 2019; Sonesson 2014; Sonesson 2019; Stecksén‐Blicks 2007). All these studies assessed the number of new DLs (incidence) by comparing pre‐treatment and at or near debond photographs and were considered to be at low risk of other potential sources of bias. Other potential sources of bias are discussed for these studies, but they were assessed at low potential risk of bias, as was the study by Ogaard 2006. Luther 2005 was assessed at unclear risk of other bias, because of possible differences between the groups in terms of compliance, duration of orthodontic treatment and exposure to topical fluorides. van der Kaaij 2015 was also assessed as at unclear risk of bias, because it is unclear if all the QLF images were collected and analysed from the day of debond. The authors state that the "WSL assessments were made at an average of 52 d (days) after debonding (with a range of 0‐156 d)." Those undertaken at five months following debond might have undergone quite extensive remineralisation unrelated to mouthrinse use. Jiang 2013 was also assessed as unclear risk of bias in this domain, because it was not clear from the report how many operators were involved in the study and how the investigators controlled for other sources of fluoride. We are still awaiting clarification about other sources of bias from Jost‐Brinkman 2017 and were not able to contact the authors of He 2010.
Effects of interventions
See: Summary of findings for the main comparison Dentist/nurse‐applied fluoride: fluoride varnish compared to non‐fluoride (placebo) varnish for preventing early tooth decay (demineralised lesions) during fixed brace treatment; Summary of findings 2 Dentist/nurse‐applied fluoride: 12,300 ppm F APF foam compared to 0 ppm F placebo foam for preventing early tooth decay (demineralised lesions) during fixed brace treatment; Summary of findings 3 Patient‐applied/used fluoride: 5000 ppm F toothpaste compared to 1450 ppm F toothpaste for preventing early tooth decay (demineralised lesions) during fixed brace treatment; Summary of findings 4 Patient‐applied/used fluoride: 250 ppm F mouthrinse (100 ppm F amine F/150 ppm NaF) compared to 0 ppm F placebo mouthrinse for preventing early tooth decay (demineralised lesions) during fixed brace treatment; Summary of findings 5 Fluoride‐releasing materials: resin‐modified glass ionomer cement compared to light‐cured composite resin for bonding orthodontic brackets for preventing early tooth decay (demineralised lesions) during fixed brace treatment
The 10 studies included in this review evaluated different modes of fluoride application, which we have categorised into three broad methods.
-
Professionally‐applied (dentist or nurse‐applied) fluoride in the form of varnish (He 2010; Sonesson 2019; Stecksén‐Blicks 2007), foam (Jiang 2013) and gel (Jost‐Brinkman 2017), both home use once a week and professional application every three months.
-
Patient‐applied/used fluoride in the form of toothpaste/mouthrinse combinations (Ogaard 2006; Sonesson 2014; van der Kaaij 2015).
-
Fluoride‐releasing materials in the form of intraoral fluoride‐releasing glass bead device (Luther 2005) and resin‐modified glass ionomer cement for bonding orthodontic brackets (Benson 2019).
Although the study by Jost‐Brinkman and colleagues (Jost‐Brinkman 2017) investigated both a dentist/nurse‐applied and a patient‐applied fluoride intervention in the same participants, we have placed this in the dentist or nurse‐applied category for the reasons explained previously. Summaries of the methods, participants, interventions and outcomes for each study are provided in the Characteristics of included studies tables.
Dentist or nurse‐applied fluoride
Primary outcome
Stecksén‐Blicks 2007 reported a prevalence of DLs before treatment of 4.3% in participants who received the professionally‐applied fluoride varnish (experimental group) and 4.0% in those receiving the professionally‐applied non–fluoride placebo varnish (control group). At debond the proportions of participants with DLs was 11.7% in the experimental group and 29.7% in the control group, which the authors state as an incidence of 7.4% and 25.7% respectively. The authors report a risk reduction or preventive fraction (1‐RR) of 0.69 for new DLs. The authors calculated that nearly 6 (5.5) individuals would need to receive the fluoride varnish every orthodontic visit (approximately every six weeks) to prevent one patient from having a new DL (number needed to treat or NNT). This result should be treated with caution, because another trial by Sonesson and colleagues (Sonesson 2019) using a slightly lower concentration of fluoride varnish (7000 parts per million (ppm) fluoride) had different findings. They reported a prevalence of DLs before treatment of 8.0% (6 out of 75) in participants who received the professionally‐applied fluoride varnish (experimental group) and 9.6% (7 out of 73) in those receiving the professionally‐applied non‐fluoride placebo varnish (control group). At debond the proportions of participants with DLs (index scores of 2 and above) was 41.3% (31 out of 75) in the experimental group and 43.8% (32 out of 73) in the control group. Combining the data from these two studies the calculated risk ratio (RR) for the development of new lesions with professionally‐applied fluoride varnish was 0.52 (95% confidence interval (CI) 0.14 to 1.93; 405 participants; Analysis 1.1), which is a non‐significant reduction.
Jost‐Brinkman 2017, who applied fluoride gel every three months (as well as home‐used gel), found no difference in the development of DLs between those who were allocated to the fluoride gel and those to the placebo gel (RR 0.99, 95% CI 0.76 to 1.27; 312 participants; Analysis 2.1).
Jiang 2013 found that applying a fluoride‐containing foam professionally every two months reduces the incidence of new DLs after fixed orthodontic treatment (RR 0.26, 95% CI 0.11 to 0.57; 95 participants analysed; Analysis 3.1).
As previously stated we were not able to contact the authors of He 2010.
Secondary outcomes
Stecksén‐Blicks 2007 stated that they calculated a "progression score" by "subtracting the debond score from that registered at baseline." The progression scores were mean 0.8 (standard deviation (SD) 2.0) for participants who received the fluoride varnish and mean 2.6 (SD 2.8) for those who received the placebo varnish. We interpret this as the control group having a greater number of teeth with lesions, as well as a greater incidence. In terms of severity Figure 2 in the study shows that the great majority of new lesions were minor (Gorelick Index score 2: slight white spot formation, thin rim) and the aesthetic impact of the new DLs was not assessed.
Sonesson 2019 reported a reduction in the number of participants with the more severe DLs (index score of 3 or 4) at debond in the experimental group who received the fluoride varnish (12%, 9 out of 75), compared with the non‐fluoride control (26%, 19 out of 73). This is a RR of 0.46 (95% CI 0.22 to 0.95) and a number needed to treat of 7 (but with a wide confidence interval 3.80 to 71.10).
Jiang 2013 reported that the "mean net increment" in the scores was 0.7 (SD 2.8) for those who received the fluoride foam and 4.4 (SD 5.4) for those who received the non‐fluoride foam. This is a large increase, which we interpret as those not receiving the fluoride foam having a greater number of teeth affected by DLs. The authors cite a NNT, but we believe this is calculated on the number of teeth with new DLs, not participants, which is not appropriate. Again, the severity scores (Figure 2) were mostly minor (Gorelick Index 2) and the aesthetic impact is uncertain.
There were no data reported from any of the studies about participant perception of their DLs or any measure of oral health‐related quality of life. Only Sonesson 2019 reported adverse effects and that one participant who received the fluoride varnish withdrew from their study, due to a feeling of slight nausea during the trial.
Patient‐applied/used various fluoride toothpaste/mouthrinse combinations
Primary outcome
Sonesson 2014 found that the proportions of participants with DLs before orthodontic treatment were 17% in the high concentration fluoride (5000 ppm) toothpaste group and 19% in the standard concentration fluoride (1450 ppm) toothpaste group. These proportions increased to 35% and 45% respectively, on the day of debond. The calculated RR of developing a new DL is 0.68 (95% CI 0.46 to 1.00; 380 participants; Analysis 4.1). Although the upper confidence interval contacts the line of no difference, we believe that this provides evidence that the use of high fluoride toothpaste by patients wearing fixed orthodontic appliances does provide some protection against new DLs, with a risk reduction or preventive fraction (1‐RR) of 0.32 and a NNT of 12. As with the trial by Stecksén‐Blicks 2007, however, the results of this trial should be interpreted with caution until further clinical trials confirm this finding.
van der Kaaij 2015 states that none of their participants had DLs before the start of treatment. They report that 11 of 36 participants in the fluoride mouthrinse group developed at least one new DL, compared with 21 of 45 participants in the non‐fluoride mouthrinse group. However, the calculated RR is 0.65 (95% CI 0.37 to 1.17; 81 participants; Analysis 5.1) and the confidence interval crosses the line of no difference. The lack of statistical significance could be due to the small number of participants and the large proportion of withdrawals and dropouts.
Ogaard 2006 reported the outcome of new DLs at the tooth level with no indication of correction for clustering of teeth within the mouth. The author has been contacted to provide these data at the participant level.
Secondary outcomes
Sonesson 2014 reported that the mean numbers of DLs before the start of treatment were 0.3 (SD 1.0) in the high concentration fluoride (5000 ppm) toothpaste group and 1.0 (SD 1.8) in the standard concentration fluoride (1450 ppm) toothpaste group. These increased to 0.4 (SD 1.0) and 1.2 (SD 1.8) respectively, at debond. They also stated that the "vast majority of all new WSL were thin rims (score 2) in both groups," with only 1.2% in the high fluoride toothpaste group and 2.3% in the standard fluoride toothpaste group having teeth affected with the more severe Gorelick Index scores of 3 or 4. The aesthetic impact of the DLs is, therefore, unclear. Like most studies they report that lateral incisors were the most frequently affected teeth in both groups, followed by the canines and premolars.
van der Kaaij 2015 reported that the number of new DLs ranged from 1 to 5 in participants who received the fluoride mouthrinse (experimental group) and 1 to 15 in those receiving the non‐fluoride mouthrinse (control group). The quantitative light‐induced fluorescence (QLF) measurements revealed a mean fluorescence loss (delta F; DL – sound enamel) of 11.6% (SD 5.0) in the experimental group and 10.3% (SD 3.0) in the control group. The lesion depths were 0.9 mm2 (SD 0.6) and 1.3 mm2 (SD 1.6 mm) respectively. Neither were reported as statistically significant and there is no indication in the report how these QLF measurements can be interpreted in terms of aesthetic impact.
Ogaard 2006 found a greater mean change in the 'white spot lesion index' from baseline in a group of participants using a neutral sodium fluoride toothpaste (1400 ppm, pH 6.7) twice daily and a sodium fluoride mouthrinse (250 ppm fluoride (F), pH 6.3) at night compared with a group using amine fluoride/stannous fluoride toothpaste (Meridol 140 ppm F, pH 4.5) twice daily and an amine fluoride/stannous fluoride mouthrinse (250 ppm F, pH 4.0) after toothbrushing at bedtime (97 participants; Analysis 6.1). This suggest that the sodium fluoride combination was less effective than the amine fluoride/stannous fluoride. They also found a slightly larger increase in both the visible plaque index and the gingival bleeding index over the duration of treatment in the group exposed to sodium fluoride (97 participants; Analysis 6.2; Analysis 6.3). These differences, however, should be interpreted cautiously until the results can be independently replicated.
There were no data reported from any of the studies about participant perception of their DLs, any measure of oral health‐related quality of life, and/or reports of adverse effects.
Fluoride‐releasing materials
Primary outcome
Benson 2019 did not assess the number of DLs at baseline, rather the assessors were asked to look concurrently at the before treatment and day of debond images and determine if they saw new DLs. On this basis 23 out of 88 participants who received the fluoride‐containing bonding material (resin‐modified glass ionomer cement) were assessed as having new DLs versus 19 out of 85 who received the material containing no fluoride (light‐cured composite resin). The calculated RR was 1.17 (95% CI 0.69 to 1.99; 173 participants; Analysis 7.1); therefore, there was no difference statistically or clinically in the proportion of participants with new DLs between the two groups.
Luther 2005 reported that, of those participants completing the trial, 10 of the 18 receiving the fluoride‐containing glass beads developed DLs, compared with 7 out 19 receiving the fluoride mouthrinse. The calculated RR was 1.51 (95% CI 0.73 to 3.10; 37 participants; Analysis 8.1), which is not statistically significant.
Secondary outcomes
Unlike any of the other studies, Benson 2019 undertook an assessment of the aesthetic impact of the new DLs. They found that in only 15 of the 42 participants with new DLs were the lesions judged to be of aesthetic concern by a majority of the expert and lay assessors. Therefore, the incidence of aesthetically displeasing new DLs was 9% compared with the overall incidence of 24% and there was no difference between the groups (fluoride material 8 out of 23; non‐fluoride material 7 out of 19). Like other studies they found that upper lateral incisors were affected most, followed by upper central incisors and upper canines. This study also reported the proportion of bond failures, which was not an outcome in this review.
Luther 2005 reported that, for those participants who completed their trial, there was no statistically significant difference in the numbers of teeth affected by DLs between the two groups (fluoride‐releasing beads 17 out of 108 teeth; fluoride mouthrinse 19 out of 114).
There were no data reported from any of the studies about adverse effects, participant perception of their DLs and/or any measures of oral health‐related quality of life.
Discussion
Summary of main results
There is insufficient evidence of a difference from two trials, judged to be at a low risk of bias, on the effectiveness of fluoride varnish applied, by a professional, every six weeks in reducing new demineralised lesions (DLs) during fixed orthodontic treatment (summary of findings Table for the main comparison). Evidence from one trial judged to be at unclear risk of bias, provides a low level of certainty that fluoride foam (12,300 parts per million (ppm) fluoride), professionally applied every two months, reduces the incidence of new DLs after fixed orthodontic treatment (summary of findings Table 2). Similarly, one trial, assessed as at unclear risk of bias, provides a low level of certainty that use of a high‐concentration fluoride toothpaste by patients throughout their fixed orthodontic treatment reduces the incidence of new DLs, compared with a conventional concentration of fluoride toothpaste (summary of findings Table 3).
Evidence is insufficient to show whether the use of a professionally‐applied amine fluoride gel reduces new DLs (Additional Table 1), or patient use of a sodium fluoride/amine fluoride mouthrinse (summary of findings Table 4) or amine fluoride and stannous fluoride toothpaste/mouthrinse combination (Additional Table 2) is more or less effective than a non‐fluoride mouthrinse or a sodium fluoride toothpaste/mouthrinse combination respectively. Finally, there is no evidence that either a fluoride‐containing material to bond brackets (summary of findings Table 5) or an intraoral fluoride‐releasing glass bead device (Additional Table 3) reduces the incidence of new DLs.
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With 0 ppm F placebo gel | With 12,500 ppm F (NaF/olaflur/dectaflur) fluoride gel | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: clinical examination Follow‐up: mean 16.6 months | 42.90% | 42.50% | 0.40% fewer | RR 0.99 | 312 | ⊕⊝⊝⊝ | The evidence is very uncertain about the effect of an amine fluoride gel compared with a placebo gel on the number of patients wearing fixed orthodontic braces with new DLs |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) Follow‐up: mean 16.6 months | 0.60% | 0.00% | 0.60% fewer | Not estimable | 312 | ⊕⊝⊝⊝ | Authors write "Most AEs (96.4%) were unrelated to the study treatment. Only a single AE (hay fever) was considered related to the study treatment (placebo)." They go on to state "The use... for a maximum of 32.5 months was not associated with any unexpected ARs or AEs. Thus, there are no safety issues to be considered for long‐term use of elmex® gel" |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
aDowngraded 1 level due to single study at unclear risk of bias (Jost‐Brinkman 2017).
bDowngraded 1 level for imprecision (insufficient number of participants with new DLs (guidance 300 to 400 events)).
cDowngraded 1 level for publication bias (data collection for the trial was completed in 2011. The results were obtained from the study report that was published in 2016, but not yet submitted to a peer‐reviewed journal).
dDowngraded 1 level for imprecision (insufficient number with adverse events).
| Patient or population: orthodontic patients (any age) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Risk with 1400 ppm/250 ppm F (NaF) toothpaste/mouthrinse | Risk with 1400 ppm/250 ppm F (amineF/SnF) toothpaste/mouthrinse | |||||
| Number of participants with new DLs (new DLs) Follow‐up: 1.5 years | Outcome not reported. White spot lesion index, visible plaque index and gingival bleeding index reported instead: MD 0.05 lower (0.10 lower to 0) white spot index, MD 0.09 lower (0.18 lower to 0) visible plaque index, MD 0.07 lower (0.15 lower to 0.01 higher) gingival bleeding index for 1400 ppm/250 ppm F (amine F/SnF) toothpaste/mouthrinse | ‐ | 97 | ⊕⊝⊝⊝ | The evidence is very uncertain about the effect of daily 1400 ppm/250 ppm F (amine F/SnF) versus 1400 ppm/250 ppm F (NaF) toothpaste/mouthrinse combinations on the white spot index, visible plaque index and on the gingival bleeding index in patients wearing fixed orthodontic braces | |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | |||||
| Number of participants with adverse effects (adverse effects) | None of the trials reported this outcome | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
aDowngraded 1 level due to single study assessed at unclear risk of bias (Ogaard 2006).
bDowngraded 1 level for indirectness (outcomes assessed were not the most useful for answering this question).
cDowngraded 1 level for imprecision (insufficient number of participants with new DLs (guideline 300 to 400)).
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With 250 ppm F mouthrinse | With intraoral fluoride‐releasing glass bead device | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: clinical intraoral photographs Follow‐up: 19 months | 36.80% | 55.60% | 18.80% more | RR 1.51 | 37 | ⊕⊝⊝⊝ | The evidence is very uncertain about the effect of intraoral fluoride‐releasing glass bead devices compared with daily 250 ppm F mouthrinses on the number of patients wearing a fixed orthodontic brace with new DLs |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) Follow‐up: 19 months | ‐ | ‐ | ‐ | ‐ | 37 | ⊕⊝⊝⊝ | Current design of fluoride glass bead inadequate. The authors write "an improved method of attachment is needed before it can be established whether FGBs (fluoride glass beads) are more effective than FR (fluoride mouthrinse)."c |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
aDowngraded 2 levels due to single study at high risk of bias (high attrition (47%)) (Luther 2005).
bDowngraded 1 level for imprecision (insufficient number of participants with new DLs (guidance 300 to 400 events)).
cHigh attrition partly due to breaks of the glass beads. The authors write "Some patients in the FGB (fluoride glass bead) group experienced a large number of bead breakages, resulting in a number of patients requesting to leave the trial." Numbers not supplied.
Overall completeness and applicability of evidence
As with the last version, the update of this review has included only parallel‐group trials, in which the individual participant is the unit of randomisation. This was decided upon because of the possibility of cross‐contamination between experimental and control teeth in the same mouth, either between upper and lower arches or between sides of the mouth, which might lead to under‐estimation of the effectiveness of any fluoride products.
Interventions that rely on the patient for delivery, including fluoride mouthrinse and toothpaste, will work only if they are used regularly. They rely greatly on patient compliance to succeed; however, evidence suggests that compliance with mouthrinsing is poor among orthodontic patients. One study (Geiger 1992) found that only 42% of participants rinsed with a sodium fluoride mouthrinse at least every other day. Results also showed that those who complied least with fluoride rinsing regimens tended to have more DLs. It is important to consider the acceptability of interventions to both adolescents and adults with a view toward increasing compliance with recommended dental hygiene practices.
Interventions that are professionally applied and deliver fluoride 'passively', such as fluoride varnish, fluoride‐releasing bracket cements and fluoride‐releasing elastics, avoid the need for patient compliance. In addition, these materials deliver fluoride close to the bracket, where it is most needed. Many fluoridated materials release large amounts of fluoride initially, but the level drops rapidly and might not be sufficient to prevent decay over the whole course of orthodontic treatment. Reapplication of fluoride varnish and frequent replacement of fluoride‐releasing elastics are likely to be required. In the parallel‐group trial of a fluoride varnish intervention included in this review, varnish was reapplied every six weeks at each orthodontic check‐up appointment. We found no parallel‐group trials of fluoride‐releasing cements or elastics that met the inclusion criteria for this review.
An interesting addition, since the initial review was carried out, is the further development of materials that produce a slow and sustained release of fluoride (Luther 2005). This trial was small and at high risk of bias, and evidence was insufficient to reveal whether these devices are more or less effective than a mouthrinse in reducing the development of DLs. It is possible, that with further refinement, this technique could potentially be effective. Intraoral fluoride‐releasing devices should be evaluated by parallel‐group randomised controlled trials with appropriate masking of participants, clinicians/operators and assessors.
When examining the effectiveness of a fluoride product in preventing dental decay, one should consider two aspects: first, whether the fluoride product reduces the number of DLs appearing during treatment, and second, whether it reduces the severity of DLs in terms of the size or area of the tooth surface affected, the amount of mineral lost or the depth of decay. Banks et al (Banks 2000) developed the Enamel Decalcification Index, which is an ordinal index that includes an assessment of the area covered. Assessment of the size of the lesion is a useful outcome measure, but none of the studies included in this review reported this outcome.
Ideally the appearance of the tooth should be recorded before and after orthodontic treatment, so that the change in appearance of the tooth is measured (incidence), not just its appearance at the end (prevalence). There are many different causes of coloured marks on the teeth, many of which occur during their development. It is important that these development lesions, as well as decay that has occurred before the brace is fitted, are excluded from the analysis, hence the need for the clinical photographs or fluorescent images taken before treatment. Measurement of both incidence and severity will depend on the method used to record DLs. Two main methods may be used: visual inspection and clinical images. Both methods are associated with problems. One problem with visual inspection is that the examiner or examiners will require calibration at the start and regular recalibration throughout the experimental period to ensure consistency of measurement. The duration of the experiment, including the recruitment and data collection will be long because, as discussed later, the product should be tested over the entire length of orthodontic treatment. This can take between 18 and 30 months ‐ sometimes longer. Another problem with visual recording clinically involves masking of the assessor to the allocated intervention. To reduce bias, the examiner should not know whether the participant has received a fluoride product and this will complicate the way the experiment is run.
Images have the advantage of providing a permanent record of the appearance of the tooth. Assessments can be carried out by several people independently or in groups, whereby a consensus is achieved. The images can be placed in a random order and the judges masked to group allocation. In addition, because the assessment can be performed over a short period of time the problem of examiner drift, whereby an assessor might subtly change his or her assessment over time, is reduced. The challenge of using clinical photographs consists of achieving consistency in lighting and reducing reflections that can mask or mimic DLs. When a careful photographic technique is applied, however, the advantages of photographs outweigh their potential disadvantages. Several optical and fluorescent methods are available for measuring lesions on the teeth (Angmar‐Mansson 1996). These methods require specialised equipment, which would add considerably to the cost of a clinical study, but they provide an objective measurement of the amount of decay in terms of mineral loss or lesion depth or both.
Quality of the evidence
Two studies included in this review were judged to be at low risk of bias in all domains; however clarification over some issues was required from some of the authors before these judgements could be confirmed. Both the design and the reporting of trials of fluorides for preventing DLs have improved since the first version of this review and we hope that this may continue. Undoubtedly the increasing use of the CONSORT guidelines for the reporting of randomised controlled trials has been a factor.
Several of the studies were assessed at some risk of bias as a result of the proportion of participants randomised to the intervention not been included in the analysis following withdrawal or dropout. It is inevitable that some patients will move away during a course of orthodontic treatment, but every effort should be made to collect records and data at the appropriate times, even if the treatment is finished early.
Another issue in orthodontic research is that it is often not possible to mask the clinician/operator to the allocated intervention. In these situations the participant can also usually work out to which group they have been allocated and, therefore, triple‐blinding is difficult, if not impossible to achieve. It is, however, not clear how much this will affect the behaviour of the clinician and the participant. It is known that patients respond favourably to simply being part of a clinical trial, irrespective of whether they have received the active intervention or the control (McCarney 2007). This is the so‐called Hawthorne effect, named after a Chicago electrical company works, whose workers were subjected to a series of experiments during the 1920s and 1930s. The investigators noticed that no matter how they changed the working conditions of the workers their productivity improved and concluded it was because they knew they were part of an experiment. We believe that it would be harsh to judge all trials that are not triple‐blind as a potentially high risk of bias when the effects are not known and perhaps this should be an area of research in the future.
Potential biases in the review process
We undertook a sensitive search of several electronic sources, supplemented by searches of references lists. We placed no restriction on language or publication status. The review authors have tried, as far as possible, to identify all possible studies that might meet the inclusion criteria for this review. Study authors have been contacted, and many have replied; however, some were not able to supply the requested information, as their records have been destroyed or lost.
When a product, such as a bonding material, can be applied to single teeth, it is tempting to use an experimental design whereby the material being tested is used in two quadrants of the mouth and the control material is used in the other two quadrants. This is called a split‐mouth design. The main advantage of the split‐mouth design over a conventional parallel‐group study design, in which the two materials are tested in two separate groups of individuals, is that the experimental material is tested in the same mouth, under the same conditions as the control material. In theory, any differences in outcome between the two materials are due only to their properties ‐ not to other factors, such as differences in oral hygiene and diet between participants (with a parallel design) or even differences in oral hygiene and diet over time within the same participants (with a cross‐over design).
Unfortunately, when one is examining the ability of fluoride products to reduce decay, it is highly unlikely that the fluoride released will be confined to only the quadrants/teeth in which the experimental material has been placed, and some contamination of the 'untreated' teeth is inevitable. This contamination will reduce the difference in outcomes between treated and untreated teeth. The previous version of this review included split‐mouth studies, which failed to show any difference between treated and untreated teeth; this may be due to cross‐over contamination between control and experimental sides and may reflect our contention of contamination. For this reason, we have decided to exclude split‐mouth studies from the previous update of our review.
Agreements and disagreements with other studies or reviews
Three other systematic reviews gathering evidence for the most effective means of preventing caries/demineralisation during fixed orthodontic appliance treatment have been reported in the literature. Derks et al (Derks 2004) examined all preventive measures for preventing demineralisation ‐ not just fluoride products. These review authors had to exclude many published studies as well, because of inappropriate research design or poor reporting and were unable to provide firm, evidence‐based recommendations as to the prevention of DLs during fixed orthodontic treatment.
A second systematic review (Chadwick 2005) investigated the effectiveness of topical fluorides used alone in preventing demineralisation during orthodontic treatment. These review authors included seven studies in their review; these studies, however, were excluded from our review, because the outcomes were not appropriate (DMFT/DMFS (decayed, missing, and filled teeth/surfaces)), or the participants were not examined immediately after removal of the fixed appliance(s). Although they suggest that according to their outcome measure (preventive fraction), some evidence shows that the addition of a topical fluoride preparation helps in the prevention of demineralisation during fixed orthodontic treatment, this conclusion must be viewed with caution, because these review authors were not able to calculate confidence intervals. We support their request that researchers design and report their studies using standard outcomes, so that in the future, data may be pooled and overall recommendations on preventive measures may be provided.
Rogers et al (Rogers 2010) included 10 studies in their systematic review investigating the effectiveness of fluoride‐containing bonding adhesives used in orthodontics to prevent demineralisation. Five of these studies were excluded from our review because they were not randomised, and a further three studies were excluded because data in the report were insufficient, and the study authors, when contacted, were unable to provide requested data. Rogers' conclusions are consistent with ours with regard to the design of trials and the quality of reporting and statistical analyses.
Wang 2013 included 20 studies (19 articles) in their review, which is written in Chinese and only includes data from Chinese studies. They included studies with quasi‐randomised designs and it is not clear if they included studies with a within‐person (split‐mouth) design and those not following patients for the full length of orthodontic treatment.
The following reviews were also examined: Höchli 2017; Lapenaite 2016; Lopatiene 2016; Nascimento 2016; Rahimi 2017; Sardana 2019a; Sardana 2019b; Tasios 2019. These reviews either investigated interventions other than fluoride to prevent DLs, such as casein phosphopeptide‐amorphous calcium phosphate (CCP‐ACP), treatment of DLs after the appliance was removed or included quasi‐ and non‐randomised studies, studies with short follow‐up or outcomes that are not particularly relevant to patients and clinicians. No new studies were identified from the references in these articles to include in this review.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Study flow diagram.
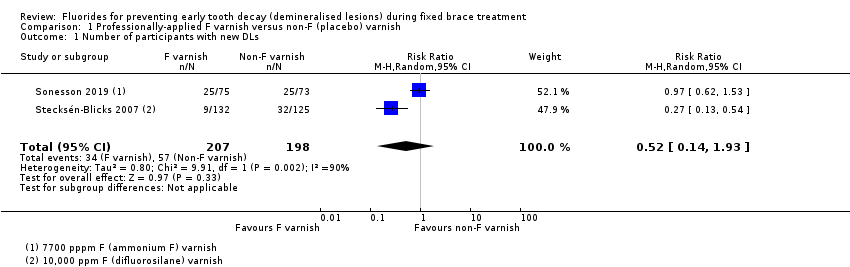
Comparison 1 Professionally‐applied F varnish versus non‐F (placebo) varnish, Outcome 1 Number of participants with new DLs.
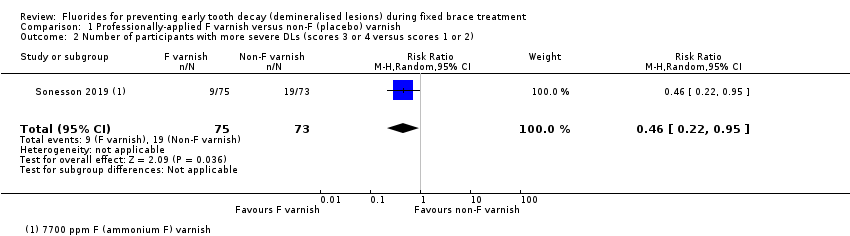
Comparison 1 Professionally‐applied F varnish versus non‐F (placebo) varnish, Outcome 2 Number of participants with more severe DLs (scores 3 or 4 versus scores 1 or 2).

Comparison 2 12,500 ppm F (NaF/olaflur/dectaflur) gel versus 0 ppm F placebo gel, Outcome 1 Number of participants with new DLs.

Comparison 3 12,300 ppm F APF foam versus 0 ppm F placebo foam, Outcome 1 Number of participants with new DLs.

Comparison 4 5000 ppm F toothpaste versus 1450 ppm F toothpaste, Outcome 1 Number of participants with new DLs.

Comparison 5 250 ppm F mouthrinse (100 ppm AmF/150 ppm NaF) versus 0 ppm F placebo mouthrinse, Outcome 1 Number of participants with new DLs.

Comparison 6 1400 ppm/250 ppm F (AmF/SnF) versus 1400 ppm/250 ppm F (NaF) toothpaste/mouthrinse combinations, Outcome 1 White spot index.
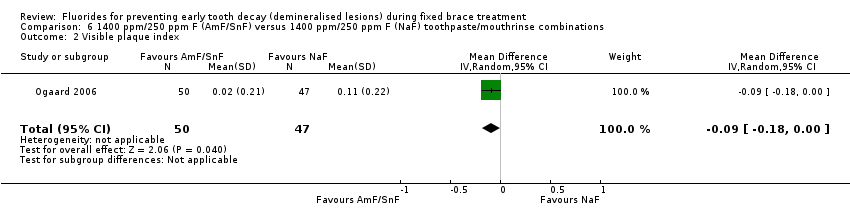
Comparison 6 1400 ppm/250 ppm F (AmF/SnF) versus 1400 ppm/250 ppm F (NaF) toothpaste/mouthrinse combinations, Outcome 2 Visible plaque index.

Comparison 6 1400 ppm/250 ppm F (AmF/SnF) versus 1400 ppm/250 ppm F (NaF) toothpaste/mouthrinse combinations, Outcome 3 Gingival bleeding index.

Comparison 7 Resin‐modified glass ionomer cement (RM‐GIC) versus light‐cured composite resin (LCC), Outcome 1 Number of participants with new DLs.

Comparison 7 Resin‐modified glass ionomer cement (RM‐GIC) versus light‐cured composite resin (LCC), Outcome 2 Number of participants with more severe DLs of aesthetic concern.
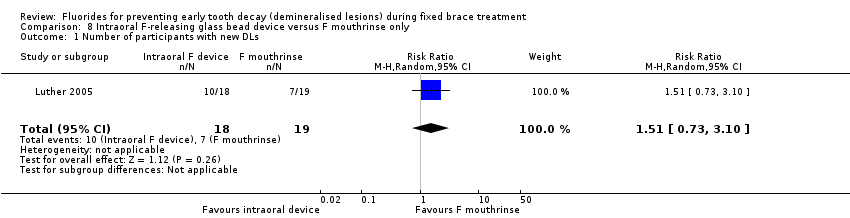
Comparison 8 Intraoral F‐releasing glass bead device versus F mouthrinse only, Outcome 1 Number of participants with new DLs.
| Fluoride varnish compared to non‐fluoride (placebo) varnish for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With non‐fluoride (placebo) varnish | With fluoride varnish | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: pre‐treatment and day of debond clinical intraoral photographs Follow‐up: 1.7 years | 28.80% | 15% | 13.80% fewer | RR 0.52 | 405 | ⊕⊕⊝⊝ | The evidence that professional application of fluoride varnish (7700 or 10,000 ppm F) every 6 weeks to the teeth of patients wearing fixed orthodontic braces reduces the number of new DLs is equivocal |
| Number of participants with more severe DLs (severity of DLs) (score 3 or 4 versus score 1 or 2) Follow‐up: 1.7 years | 26% | 12% | 14.10% fewer | RR 0.46 | 148 | ⊕⊕⊝⊝ | The evidence suggests that when a dentist or nurse applies 7700 ppm F (ammonium fluoride) varnish every 6 weeks to a patient wearing a fixed orthodontic brace there may a reduction in the number of orthodontic patients with more severe DLs (score 3 or 4 versus score 1 or 2) |
| Number of participants with adverse effects (adverse effects) Follow‐up: 1.7 years | No evidence that the intervention had adverse effects | 148 | ⊕⊕⊝⊝ | Only 1 participant with an adverse event and not clear if this was directly related to the intervention | |||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 1 level for indirectness (evidence from only 2 studies) (Stecksén‐Blicks 2007; Sonesson 2019). | |||||||
| 12,300 ppm F APF foam compared to 0 ppm F placebo foam for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Certainty of the evidence | Number of participants (studies) | Comments | ||
| With 0 ppm F placebo foam | With 12,300 ppm F APF foam | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: clinical assessment Follow‐up: mean 18 months | 48.90% | 12.70% | 36.20% fewer | RR 0.26 | ⊕⊕⊝⊝ | 95 | The evidence suggests that when foam, containing 12,300 ppm F, is applied by a dentist or a nurse, every 2 months, to the teeth of patients wearing fixed orthodontic appliances there might be a reduction in the number of patients who have at least 1 new DL |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) | None of the trials reported this outcome | ||||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aAlthough effect size is large this was only for 1 study at unclear risk of bias and therefore downgraded 1 level (Jiang 2013). | |||||||
| 5000 ppm F toothpaste compared to 1450 ppm F toothpaste for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With 1450 ppm F toothpaste | With 5000 ppm F toothpaste | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: pre‐treatment and post‐treatment clinical intraoral photographs Follow‐up: 1.8 years | 26.60% | 18.10% | 8.50% fewer | RR 0.68 | 380 | ⊕⊕⊝⊝ | The evidence suggests that in patients wearing an orthodontic fixed brace use of a daily 5000 ppm F toothpaste compared with a daily 1450 ppm F toothpaste throughout treatment may lead to a reduction in the number of orthodontic patients with new DLs |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) | None of the trials reported this outcome | ||||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 1 level due to single study at unclear risk of bias (Sonesson 2014). | |||||||
| 250 ppm F mouthrinse (100 ppm amine F/150 ppm NaF) compared to 0 ppm F placebo mouthrinse for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With 0 ppm F placebo mouthrinse | With 250 ppm F mouthrinse (100 ppm amine F/150 ppm NaF) | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: QLF Follow‐up: 24.5 months | 46.70% | 30.30% | 16.30% fewer | RR 0.65 | 81 | ⊕⊝⊝⊝ | The evidence is very uncertain about the effect of a daily 250 ppm F mouthrinse (100 ppm amine F/150 ppm NaF) compared with a daily 0 ppm F placebo mouthrinse on the number of patients wearing a fixed orthodontic brace with new DLs |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) | None of the trials reported this outcome | ||||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 2 levels: single study with a relatively small number of participants (81), at high risk of bias due to high attrition (33%) (van der Kaaij 2015). | |||||||
| Resin‐modified glass ionomer cement compared to light‐cured composite resin for bonding orthodontic brackets for preventing early tooth decay (demineralised lesions) during fixed brace treatment | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With light‐cured composite resin | With resin‐modified glass ionomer cement | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: before and day of debond clinical intraoral photographs Follow‐up: 17.6 months | 22.40% | 26.20% | 3.80% more | RR 1.17 | 173 | ⊕⊕⊝⊝ | The evidence suggests that resin‐modified glass ionomer cement for bonding orthodontic brackets compared with light‐cured composite resin results in little to no difference in the number of orthodontic patients with new DLs |
| Number of participants with more severe DLs of aesthetic concern (severity of DLs) Assessed with: pre‐treatment and day of debond clinical intraoral photographs Follow‐up: 17.6 months | 8.00% | 9.40% | 1.40% more | RR 1.18 | 173 | ⊕⊕⊝⊝ | The evidence suggests that using resin‐modified glass ionomer cement for bonding orthodontic brackets compared with light‐cured composite resin results in little to no difference in the number of orthodontic patients with more severe DLs of aesthetic concern |
| Number of participants with adverse effects (adverse effects) Follow‐up: 17.6 months | No evidence that either intervention had adverse effects | 173 | ⊕⊕⊝⊝ | ‐ | |||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 1 level: single study at unclear risk of bias (Benson 2019). | |||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With 0 ppm F placebo gel | With 12,500 ppm F (NaF/olaflur/dectaflur) fluoride gel | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: clinical examination Follow‐up: mean 16.6 months | 42.90% | 42.50% | 0.40% fewer | RR 0.99 | 312 | ⊕⊝⊝⊝ | The evidence is very uncertain about the effect of an amine fluoride gel compared with a placebo gel on the number of patients wearing fixed orthodontic braces with new DLs |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) Follow‐up: mean 16.6 months | 0.60% | 0.00% | 0.60% fewer | Not estimable | 312 | ⊕⊝⊝⊝ | Authors write "Most AEs (96.4%) were unrelated to the study treatment. Only a single AE (hay fever) was considered related to the study treatment (placebo)." They go on to state "The use... for a maximum of 32.5 months was not associated with any unexpected ARs or AEs. Thus, there are no safety issues to be considered for long‐term use of elmex® gel" |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 1 level due to single study at unclear risk of bias (Jost‐Brinkman 2017). | |||||||
| Patient or population: orthodontic patients (any age) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Risk with 1400 ppm/250 ppm F (NaF) toothpaste/mouthrinse | Risk with 1400 ppm/250 ppm F (amineF/SnF) toothpaste/mouthrinse | |||||
| Number of participants with new DLs (new DLs) Follow‐up: 1.5 years | Outcome not reported. White spot lesion index, visible plaque index and gingival bleeding index reported instead: MD 0.05 lower (0.10 lower to 0) white spot index, MD 0.09 lower (0.18 lower to 0) visible plaque index, MD 0.07 lower (0.15 lower to 0.01 higher) gingival bleeding index for 1400 ppm/250 ppm F (amine F/SnF) toothpaste/mouthrinse | ‐ | 97 | ⊕⊝⊝⊝ | The evidence is very uncertain about the effect of daily 1400 ppm/250 ppm F (amine F/SnF) versus 1400 ppm/250 ppm F (NaF) toothpaste/mouthrinse combinations on the white spot index, visible plaque index and on the gingival bleeding index in patients wearing fixed orthodontic braces | |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | |||||
| Number of participants with adverse effects (adverse effects) | None of the trials reported this outcome | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded 1 level due to single study assessed at unclear risk of bias (Ogaard 2006). | ||||||
| Patient or population: orthodontic patients (any age) | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | ||
| With 250 ppm F mouthrinse | With intraoral fluoride‐releasing glass bead device | Difference | |||||
| Number of participants with new DLs (new DLs) Assessed with: clinical intraoral photographs Follow‐up: 19 months | 36.80% | 55.60% | 18.80% more | RR 1.51 | 37 | ⊕⊝⊝⊝ | The evidence is very uncertain about the effect of intraoral fluoride‐releasing glass bead devices compared with daily 250 ppm F mouthrinses on the number of patients wearing a fixed orthodontic brace with new DLs |
| Number of participants with more severe DLs (severity of DLs) | None of the trials reported this outcome | ||||||
| Number of participants with adverse effects (adverse effects) Follow‐up: 19 months | ‐ | ‐ | ‐ | ‐ | 37 | ⊕⊝⊝⊝ | Current design of fluoride glass bead inadequate. The authors write "an improved method of attachment is needed before it can be established whether FGBs (fluoride glass beads) are more effective than FR (fluoride mouthrinse)."c |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| aDowngraded 2 levels due to single study at high risk of bias (high attrition (47%)) (Luther 2005). | |||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DLs Show forest plot | 2 | 405 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.14, 1.93] |
| 2 Number of participants with more severe DLs (scores 3 or 4 versus scores 1 or 2) Show forest plot | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.22, 0.95] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DLs Show forest plot | 1 | 312 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.76, 1.27] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DLs Show forest plot | 1 | 95 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.11, 0.57] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DLs Show forest plot | 1 | 380 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.46, 1.00] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DLs Show forest plot | 1 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.37, 1.17] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 White spot index Show forest plot | 1 | 97 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.10, 0.00] |
| 2 Visible plaque index Show forest plot | 1 | 97 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.18, ‐0.00] |
| 3 Gingival bleeding index Show forest plot | 1 | 97 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.15, 0.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DLs Show forest plot | 1 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.69, 1.99] |
| 2 Number of participants with more severe DLs of aesthetic concern Show forest plot | 1 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.45, 3.12] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of participants with new DLs Show forest plot | 1 | 37 | Risk Ratio (M‐H, Random, 95% CI) | 1.51 [0.73, 3.10] |

