Apoio contínuo para mulheres em trabalho de parto
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT. | |
| Participants | 3 trials are reported separately, within 1 publication. Participants were nulliparous, healthy, in spontaneous labour, term, with singleton vertex presentations. | |
| Interventions | Permanent presence of a midwife compared to varying degrees of presence. Fathers were allowed to be present. | |
| Outcomes | Oxytocin, epidural analgesia, labour length, mode of birth, Apgar scores, mothers' views of their experiences. | |
| Notes | Epidural analgesia was available and it is not known whether EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women were 'randomly assigned'. The envelopes were prepared by the co‐ordinating centre. No mention of the process of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No mention if they were opaque or consecutively numbered. The process of how the envelopes were opened was not described. |
| Blinding (performance bias and detection bias) | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) | Low risk | Completion rate for medical record data and in‐hospital questionnaire were 99.2% and 91.0% respectively. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | See Breart ‐ Belgium. | |
| Participants | See Breart ‐ Belgium. | |
| Interventions | See Breart ‐ Belgium. Fathers were allowed to be present. | |
| Outcomes | See Breart ‐ Belgium. | |
| Notes | Epidural analgesia was available and it is unknown whether EFM was routine. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women were 'randomly assigned'. The envelopes were prepared by the co‐ordinating centre. No mention of the process of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No mention if they were opaque or consecutively numbered. The process of how the envelopes were opened was not described. |
| Blinding (performance bias and detection bias) | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) | Low risk | Completion rate for medical record data and in‐hospital questionnaire was > 95%. There were some discrepancies in the total number enrolled. 2 reports show 656 in the permanent support group and 664 in the control group for a total of 1320. The table of results in 1 report shows 654 in the permanent support and 666 in control. The in‐hospital questionnaire results are shown for 654 and 664 women (total 1318) but the authors state this is 95% of the sample, meaning the total is 1386. The n reported with each outcome was the one used in the data tables in this review. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | See Breart ‐ Belgium. | |
| Participants | See Breart ‐ Belgium. Trial in Greece: n = 569 (295 permanent support; 274 control). | |
| Interventions | See Breart ‐ Belgium. Fathers/family members were not permitted to be present. | |
| Outcomes | See Breart ‐ Belgium, except that mothers' views were not reported. | |
| Notes | Epidural analgesia was not available. Not stated if EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women were 'randomly assigned'. The envelopes were prepared by the co‐ordinating centre. No mention of the process of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No mention if they were opaque or consecutively numbered. The process of how the envelopes were opened was not described. |
| Blinding (performance bias and detection bias) | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) | Low risk | Completion rate for medical record data was 97%. No in‐hospital questionnaire data were available. |
| Selective reporting (reporting bias) | Low risk | All medical record outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 212 nulliparous women in active labour at term (105 support group, 107 control group) at a University‐affiliated hospital in Sao Paulo, Brazil. To be eligible a companion of the woman's choosing had to be available. 49.5% of the companions were present at enrolment and the others were phoned and asked to come to the hospital (4 failed to make it before delivery). | |
| Interventions | Support was 'presence of a chosen companion during labour and delivery'. 'The companions received verbal and written information on the activities involved in providing support, expected behaviour when confronted with signs of tiredness, anxiety, concern, crying, screaming and/or the woman's feelings of inability to cope, compliance with regulations and the possibility of requesting information from staff'. in 47.6% of the sample the woman's companion was her partner, for 29.5% it was her mother. The control group received usual care where a companion during labour and delivery was not permitted. For both groups labour and delivery care was provided 'according to the routine protocol including active management of labour (early amniotomy, use of oxytocin, intermittent EFM and systematic analgesia)'. | |
| Outcomes | Satisfaction with labour and delivery, perinatal and breastfeeding outcome in the 12 hours post delivery. | |
| Notes | All women in labour at this hospital received epidural analgesia as a routine practice. Therefore, we did not include epidural analgesia data in the review. EFM was not used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Computer generated sequence of random numbers.' |
| Allocation concealment (selection bias) | High risk | 'Individual assignment numbers were all placed in an opaque container to assure the concealment. The eligible women who had agreed to participate selected one of the numbers once, and were therefore allocated to either intervention group or control according to the list.' This process was open to selection bias as women could have re‐picked another number from the container. No audit process is possible with this system of randomisation. |
| Blinding (performance bias and detection bias) | High risk | Data collection by author, who knew group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Medical record data were collected and in‐hospital questionnaires were completed for 100% of sample. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 600 nulliparous, low‐income, under‐insured pregnant women (300 doula group, 300 control group) booked for delivery at a hospital in New Jersey, USA were enrolled between 12 and 38 weeks' gestation. They were considered low risk, with no contraindications to labour and had a female friend or relative willing to act as their lay doula. The doula was in addition to support people of their own choosing. | |
| Interventions | Intervention: continuous support by a female friend or relative who had had 2, 2‐hour sessions about labour support. The training sessions were conducted for nearly all of the lay caregivers when the participants were 34‐36 weeks' gestation. Control group: support people of their own choosing. | |
| Outcomes | Labour length, epidural analgesia, oxytocin augmentation, cervical dilation at epidural insertion, length of second stage labour, caesarean birth, 1‐min Apgar score > 6, 5‐min Apgar score > 6. | |
| Notes | Epidural analgesia was available and EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Computer generated randomization scheme.' |
| Allocation concealment (selection bias) | Low risk | Consecutively‐numbered, sealed opaque envelopes contained treatment assignments. After obtaining consent, a research assistant opened the next envelope. It was unclear whether the research assistant enrolling the woman was the same one that opened the envelope. |
| Blinding (performance bias and detection bias) | High risk | Medical record abstraction was done by the author who was not blinded. The 6‐week questionnaire data collection was not blinded. |
| Incomplete outcome data (attrition bias) | High risk | Medical record information was completed for 97.7% of the sample (82.3% in the intervention group and 94.3% in the control group). The differential rates are due to withdrawals from the intervention group for doula related reasons (incomplete training and not being present during labour). The 6‐week questionnaire was completed for 82.3% of the sample. Only those women included in the study at delivery had the opportunity to complete the questionnaire and thus the differential completion rate between groups remained (76.3% in the intervention group and 88.3% in the control group). The differential withdrawals could introduce selection bias. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Unclear risk | The training of the doulas giving the intervention was done by the research assistant, who was herself a doula. This same research assistant enrolled all study participants. |
| Methods | RCT. | |
| Participants | 34 women (primigravidas and multigravidas) at 26‐37 weeks' gestation in 2 Texas hospitals (20 to supported group and 14 to usual care). They were in early, uncomplicated preterm labour. | |
| Interventions | Intervention: support provided by a Lamaze childbirth preparation instructor. Support included continuous presence, acting as a liaison with hospital staff, providing information, and teaching relaxation and breathing measures. Usual care: intermittent nursing care. Family members allowed to be present. | |
| Outcomes | Fetal distress, caesarean birth, artificial oxytocin, labour length, Apgar scores, neonatal intensive care. | |
| Notes | Not stated if epidural analgesia was available or if EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Randomly assigned.' No further details provided. |
| Allocation concealment (selection bias) | Unclear risk | Admitting nurse telephoned research assistant to obtain treatment allocation. No details about whether the research assistant had foreknowledge of the treatment allocation scheme. |
| Blinding (performance bias and detection bias) | Low risk | Medical record information collected by 'research assistants who did not know the group membership of the women'. |
| Incomplete outcome data (attrition bias) | High risk | Withdrawals occurred before analysis (6 (30%) in support group and 3 (21%) in control). This resulted in a follow‐up rate of 73.5%. The withdrawals were done differentially in the support group, i.e. some women were withdrawn because of an event that occurred before the support person arrived. Women in the control group with the same event were not withdrawn. We were able to re‐create the original study groups for 1 outcome only, caesarean birth, and therefore it is included in the analysis table. |
| Selective reporting (reporting bias) | Unclear risk | No outcomes were stated a priori. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT, stratified by induced or spontaneous labour at trial entry. | |
| Participants | 992 nulliparous women at term (499 to continuous support and 493 to control), cephalic fetal presentation, cervical dilatation < 5 cm, in a hospital in Perth, Western Australia. | |
| Interventions | Group 1: continuous physical and emotional support by midwifery staff, and women were encouraged to use pharmacologic and nonpharmacologic alternatives to epidural analgesia. | |
| Outcomes | Labour length (expressed as median and interquartile range), epidural analgesia, mode of delivery, 5 min Apgar score < 7, arterial cord pH. | |
| Notes | The stated purpose was to compare the effects of intrapartum analgesic techniques on labour outcomes. Continuous midwifery support was conceptualised as an analgesic technique. Both groups had access to opioids and nitrous oxide. No data were presented about the number of women who used no pharmacologic analgesia. Because the type of analgesia used was a measure of compliance rather than an outcome, no data on analgesic outcomes are included in this review. It was not stated if other support person was allowed. epidural analgesia was available and EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details about how the blocks of treatment allocations were produced. |
| Allocation concealment (selection bias) | Unclear risk | Randomisation on presentation in the labour and delivery unit, "by selection from a blocked group of eight sealed opaque envelopes, replenished from blocks of 12". No further details about process. |
| Blinding (performance bias and detection bias) | Unclear risk | Not noted. |
| Incomplete outcome data (attrition bias) | Low risk | There was 100% follow‐up for medical record data and in‐hospital survey. A 6‐month questionnaire was completed by 64.7% of the sample and these data were not used. |
| Selective reporting (reporting bias) | Low risk | All main outcomes were reported. Effects on breastfeeding were not analysed by treatment group and thus the results could not be included in the review. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 413 women admitted to an intrapartum unit at a tertiary care teaching hospital in Montreal, Canada, were randomly allocated to experimental (n = 209) or control (n = 204) groups. All but 3 in the experimental group and 6 in the control group were accompanied by a spouse, relative or friend during labour. All participants were nulliparous, with singleton fetuses, > 37 weeks' gestation, and in labour. | |
| Interventions | Experimental: 1‐to‐1 nursing care from randomisation until 1 hour postbirth. Care was provided by on‐call nurses who were hired specifically for the study and had received a 30‐hour training program and quarterly refresher workshops. The training program included critical reviews of the literature concerning the effects of intrapartum medical and nursing practices, as well as discussions of stress and pain management techniques. The nurse provided the usual nursing care plus physical comfort, emotional support, and instruction on relaxation and coping techniques. The nurse took meal breaks and brief rest breaks. Women in the comparison group received usual nursing care by the regular unit staff, consisting of intermittent support and monitoring. | |
| Outcomes | Caesarean birth, caesarean birth for cephalopelvic disproportion or failure to progress, post‐randomisation artificial oxytocin augmentation, post‐randomisation analgesia/anaesthesia, instrumental vaginal delivery (forceps or vacuum extraction), NICU admission, perineal trauma, mean duration of labour post‐randomisation, postpartum urinary catheterisation. | |
| Notes | The participants had been admitted to the unit for an average of 5 hours (SD = 4 hours) prior to randomisation. 36 women in the experimental group and 41 in the control group had epidural analgesia prior to randomisation. 55 women in the experimental group and 45 in the control group had intravenous oxytocin augmentation of labour prior to randomisation. Mean duration of labour post‐randomisation was 9.2 hours (SD = 4.3). Epidural analgesia was available but it was not stated if EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Randomized using a list of computer generated random numbers.' |
| Allocation concealment (selection bias) | Low risk | 'Randomized in blocks of eight.' 'Group assignments were placed in sequentially numbered, sealed, opaque envelopes.' |
| Blinding (performance bias and detection bias) | High risk | Data collectors were not blinded as they read nurses notes to collect data. |
| Incomplete outcome data (attrition bias) | Low risk | 100% follow‐up. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | 2 RCTs reported in the same publication. The Zelen method was used: only those participants randomised to the experimental group were told the true purpose of the trial and asked for consent. The participants in the control group were told about the study in the introduction letter for the postpartum questionnaire and they were told it was 'a study on factors influencing birth'. | |
| Participants | Healthy nulliparous and parous women in labour at a hospital in Finland. 86 women were enrolled in Trial A. The actual number enrolled to each group was not noted but medical record data were collected for 79 women (41 in the support group and 38 in the control group). These 79 women represented 91.9% of the total sample. | |
| Interventions | Trial A: in 1987, the intervention was 1:1 support by midwifery students from enrolment until transfer to the postpartum ward. The midwifery students volunteered, were not specially trained in support and responsible for the other routine intrapartum care. The control group 'was cared for according to the normal routine of the midwife and by a medical student, if s(he) was on duty'. Over 70% of fathers were present. | |
| Outcomes | Labour length, medical interventions, complications (mother and baby), pharmacologic pain relief, method of birth, mothers' evaluations of their experiences. | |
| Notes | Not stated if epidural analgesia was available or if EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention of how the allocation sequence was produced. |
| Allocation concealment (selection bias) | Unclear risk | 'Randomization coding was done in blocks of 6 and put into non‐transparent envelopes. The envelope was opened at the reception ward when it was decided to transfer mother to labour ward.' It was not stated if the envelopes were consecutively numbered. |
| Blinding (performance bias and detection bias) | High risk | Medical record outcome were collected unblinded. |
| Incomplete outcome data (attrition bias) | Low risk | Medical record data were collected on 91.9% of the sample. A questionnaire was administered at 2‐3 days postpartum. This was completed by only 70% of the sample and thus the data were not used. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | High risk | Mothers were told the purpose of the study differentially (see methods for Trial A above). |
| Methods | See Hemminki 1990a. | |
| Participants | See Hemminki 1990a. 161 women were enrolled in Trial B (81 in the support group and 80 in control). | |
| Interventions | Trial B: in 1988, the intervention was support by a new group of midwifery students. All students were involved in the trial, not just volunteers. The students were permitted to leave their participants to witness other interventions and deliveries. The control group 'was cared for according to the normal routine of the midwife' and by a medical student as enrolment was limited to days when medical students were on duty. Slightly less than 70% of fathers were present. | |
| Outcomes | See Hemminki 1990a. | |
| Notes | Not stated if epidural analgesia was available or if EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided. |
| Allocation concealment (selection bias) | Unclear risk | The block size was reduced from the first study. 'To lessen the frustration resulting from opening a code for a control mother, randomisation envelopes contained a maximum of two similar codes in sequence (not told in advance)'. 'Put into non‐transparent envelopes'. The envelope was opened in the labour ward. It was not stated if the envelopes were consecutively numbered. |
| Blinding (performance bias and detection bias) | High risk | Medical record outcome were collected unblinded. |
| Incomplete outcome data (attrition bias) | Low risk | Medical record data were collected on 100% of the sample. A questionnaire was administered at 2‐3 days postpartum and completed by 93.7% of the sample. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | High risk | Mothers were told the purpose of the study differentially (see methods for Trial A above). |
| Methods | RCT, stratified by type of prenatal classes (Lamaze vs general). | |
| Participants | 145 nulliparous women (72 to support group and 73 to control) in the last trimester of a healthy pregnancy, booked for delivery at a Toronto, Canada, hospital. | |
| Interventions | Support provided by a monitrice (community 'lay' midwife or midwifery apprentice) compared with usual hospital care, defined as the intermittent presence of a nurse. Support described as including physical comfort measures, continuous presence, information, emotional support, and advocacy. The monitrice met with the woman twice in the latter weeks of pregnancy, to discuss her birth plans. Comparable prenatal attention was provided to the controls. All but 1 woman also had husbands or partners present during labour. Support began in early labour at home or in hospital and continued through delivery. | |
| Outcomes | Intrapartum interventions, perceived control, method of delivery. | |
| Notes | Epidural analgesia was available and EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated table of random numbers. |
| Allocation concealment (selection bias) | Low risk | Randomisation done over the phone by a third party who had no knowledge of the participant, but used the open table of random numbers. |
| Blinding (performance bias and detection bias) | Low risk | All participants blinded to the intervention. Control participants received prenatal and postpartum support (after the end of data collection); experimental participants received prenatal and intrapartum support. Initial collection of medical record data was not blinded. 'Duplicate abstraction was done by a second research assistant blind to the subject's study group assignment, on a random sample of 20 records. Interrater agreement of over 95% was obtained for all categories of intervention and physical outcomes.' In‐home interview at 2‐4 weeks postpartum was blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Method of delivery outcome available on 88.3% of sample. Other outcomes collected on only 71% of the sample and thus not used. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | Multi‐centre RCT with prognostic stratification for parity and hospital. | |
| Participants | 6915 nulliparous and parous women in labour at 13 hospitals in the USA and Canada (3454 to continuous labour support and 3461 to usual care). Eligibility criteria: live singleton fetus or twins, no contraindications to labour, in labour. Women were excluded if gestational age was < 34 weeks or if they were so high risk that a 1:1 patient‐nurse ratio was medically necessary. | |
| Interventions | Experimental: continuous support from staff labour and delivery nurses who had volunteered for and received a 2‐day training workshop in labour support. Prior to the trial, the support nurses had opportunities to practice their skills. They also had opportunities to continue learning from each other and the labour support trainer, throughout the trial. The nurses with training were part of the regular staffing complement of the unit and they provided care to the continuous support group but not to the usual care group. Usual care: intermittent support from a nurse who had not received labour support training. | |
| Outcomes | Intrapartum interventions, method of birth, immediate complications (mother or baby), complications (mother or baby) in the first 6‐8 weeks postpartum, perceived control, postpartum depression, breastfeeding at 6‐8 weeks, relationship with partner and with baby, likes and dislikes about birth experience and future preferences for labour support. | |
| Notes | Other support person(s) were allowed, epidural analgesia was available and EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation program. |
| Allocation concealment (selection bias) | Low risk | 'Randomization was centrally controlled with the use of a computerized randomization program at the data co‐ordinating centre, accessible by means of a touch‐tone telephone.' |
| Blinding (performance bias and detection bias) | Low risk | Data collectors were not blinded as they read nurses' notes to collect data about type of nursing care provided. However random chart audits yielded no errors in reporting study outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | Medical record data were collected on 100% of the sample. In‐hospital questionnaires were completed by 96.4% and 6‐8 week questionnaires by 81% of the sample. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 189 nulliparous women (92 to support and 97 to control) in active labour at a community hospital serving low‐income women in South Africa. | |
| Interventions | Intervention group: support by carefully trained, volunteer lay women, for at least several hours (supporters not expected to remain after dark). Control group: intermittent care on a busy ward. Husbands/family members were not permitted. | |
| Outcomes | Intrapartum interventions, method of birth, complications (mother and baby), anxiety, pain, mothers' perceptions of labour, breastfeeding. | |
| Notes | Epidural analgesia was not available and EFM was not used routinely. While scores on an instrument measuring postpartum depression were reported in categories of "low", "moderate," and 'high", the authors stated that categorization was not appropriate as a clinical diagnostic definition of depression. To achieve the latter, the change in score must be reported, and these data were not collected. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random. |
| Allocation concealment (selection bias) | Unclear risk | "Randomly ordered cards in sealed opaque envelopes". Not stated if consecutively numbered. |
| Blinding (performance bias and detection bias) | High risk | Data collectors were not blinded as they asked questions about support received in labour. |
| Incomplete outcome data (attrition bias) | Low risk | Medical record data were collected on 100% of the sample and questionnaires within 24 hours postpartum were completed by 99%. The 6‐week follow‐up interviews were completed by 78.8% of the sample, no imbalances existed between groups and thus the data were included in the analysis. At 1‐year interviews were complete for 46% of the sample and data from these were not used. Nikodem reported on a larger sample of women with 1‐year follow‐ups but the completion rate was still only 50% of the original number enrolled. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 100 nulliparous women at term (50 to support and 50 to routine care) in active labour at a university hospital in Tehran, Iran from March to September 2003. | |
| Interventions | 'Women allocated to the intervention group were shown to an isolated room and were supported by an experienced midwife. The women were free to choose their position, and able to eat and walk about freely. During labor, the midwife explained the process of labor and the importance of body relaxation. Midwife‐led support included close physical proximity, touch, and eye contact with the labouring women, and teaching, reassurance, and encouragement. The midwife remained with the woman throughout labor and delivery, and applied warm or cold packs to the woman's back, abdomen, or other parts of the body, as well as performing massage according to each woman's request.' 'Women allocated to the routine care group were admitted to the labor ward (where 5‐7 women labour in the same room), did not receive continuous support, and followed the routine orders of the ward. They did not have a private room, did not receive one‐to‐one care,were not permitted food, and did not receive education and explanation about the labor process. The only persons allowed in the delivery room were nurses, midwives, and doctors.' | |
| Outcomes | Duration of labour, caesarean delivery, oxytocin use, Apgar score at 5 mins. | |
| Notes | EFM was not used routinely and epidural analgesia was not available. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | From personal communication ‐ equal numbers of envelopes were produced for each letter (see below) and put into a box. No list of treatment allocations was created. |
| Allocation concealment (selection bias) | High risk | 'Allocated to one of two groups using 4‐part, block randomization'. Used 'sealed envelopes labelled A, B, C, and D: envelopes A and C (intervention group) and B and D (routine care group). Patients then chose an envelope, which was opened by the investigator'. Further details from personal communication ‐ the women picked from all the envelopes produced. Once an envelope was picked it was discarded. This process was open to selection bias as women previously in the trial may have shared knowledge of which envelope contained which group with women not yet enrolled in the study. |
| Blinding (performance bias and detection bias) | Low risk | From personal communication ‐ 'The co worker of investigator collected the outcome data and she was blind for the study group.' |
| Incomplete outcome data (attrition bias) | Low risk | Medical record information was collected on 100% of the sample. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT of continuous support vs usual care with an 'inconspicuous observer' plus a retrospective non‐random control group. This review is restricted to comparisons of the outcomes of the participants who were randomly assigned. | |
| Participants | 412 nulliparous women (212 in support group and 200 in observed group) were part of the RCT. They were aged 13‐34, with singleton, term, healthy pregnancies, many not English‐speaking, in active labour at a public hospital in Texas which provides care for low‐income patients. | |
| Interventions | The description of the setting, the participants, and the type of care echo developing world conditions. All women laboured in a large 12‐bed room. For the women in the support group a doula stayed by their bedside and gave continuous support. For those in the observed group they had the routine intermittent presence of a nurse and continuous presence of an 'inconspicuous observer' who 'kept a record of staff contact, interaction and procedures'. The observer was away from the beside and never spoke to the labouring woman. | |
| Outcomes | Analgesia/anaesthesia, labour length, artificial oxytocin use, method of birth, complications (mother and baby), neonatal health, number of women who rated their experience as negative. | |
| Notes | In instances in which outcome data (such as analgesia/anaesthesia use) in the published report were only provided for subgroups, the primary author was contacted and he provided complete outcome data for all women who were originally randomised. Family members were not allowed to be present. Epidural analgesia was available and EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as random. |
| Allocation concealment (selection bias) | Low risk | 'Randomly assigned' is stated in the report. In the protocol for the trial it states 'numbered opaque envelopes' would be used. The envelopes 'would contain the random assignments of the women to control or treatment groups and would be numbered sequentially'. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | There is some discrepancy in the number of women enrolled in the study. The report states 412 were enrolled and reports outcome data on all 412 women. But it also states that '14 women that agreed to participate were not included in the study.' The reasons for not including them seem to be events that would happen after randomisation ‐ e.g. transferred due to staffing limitations, withdrew, undetected breech, interrupted observations, etc., and thus the sample appears to have numbered 426. Data are reported for 412 women (96.7% of 426). |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. Purposefully enrolled more women to the control group. See 'Risk of bias' table below. | |
| Participants | 465 healthy nulliparous women (186 to support group and 279 to control) in labour at the Social Security Hospital in Guatemala. | |
| Interventions | Support group: continuous emotional and physical support by a doula. Control group: usual hospital routines (described as no consistent support). | |
| Outcomes | Labour length, use of artificial oxytocin, method of birth, problems during labour and birth, fetal distress, Apgar scores, transfer to neonatal intensive care nursery. | |
| Notes | No family members permitted to be present. epidural analgesia was not available and EFM was not used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Enrolled using randomised design'. 'Pool of envelopes contained more control group to ensure similar sized groups with uncomplicated labours and deliveries.' They anticipated more complications in control group based on an earlier study (Sosa 1980). No information on how allocation sequence was generated. |
| Allocation concealment (selection bias) | Low risk | 'Randomly assigned according to contents of a sealed opaque envelope. Each envelope was numbered sequentially.' |
| Blinding (performance bias and detection bias) | Unclear risk | Not noted. |
| Incomplete outcome data (attrition bias) | Low risk | 'Mother‐infant pairs were excluded when the mother developed a complication during labour, delivery, or post partum that required special care, if the baby's weight was below 5.5 lbs or above 8 lbs, if there were twins or congenital malformations.' This occurred for about 10% of cases in both groups resulting in reported outcomes for 89.6% of those randomised. Unpublished data on the excluded women were provided by the author. Labour length data were only available for 48.4% of the sample (225 of 465) and thus not included. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported on. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 724 women (361 to support and 363 to control) admitted for delivery at a large social security hospital in Mexico City, who met the following criteria: singleton fetus, no previous vaginal delivery, < 6 cm cervical dilatation, and no indications for an elective caesarean delivery. | |
| Interventions | Support group: continuous support from 1 of 10 women who had received doula training (6 were retired nurses), throughout labour, birth, and the immediate postpartum period. Support included: emotional support, information, physical comfort measures, social communication, ensuring immediate contact between mother and baby after birth, and offering advice about breastfeeding during a single brief session postnatally. Control group: women received 'routine care'. | |
| Outcomes | The main outcomes were exclusive and full breastfeeding at 1 month postpartum. Other outcomes included labour length, epidural anaesthesia, forceps birth, caesarean birth, meconium staining, and Apgar scores, as well as mothers' perceived control during childbirth, anxiety, pain, satisfaction, and self‐esteem. | |
| Notes | Partners and family members were not permitted. Epidural analgesia was available but it was not stated if EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'Computer generated random number list'. 'The treatment sequence was kept at a central level.' |
| Allocation concealment (selection bias) | Unclear risk | 'Opaque envelopes with the assignment were locked in a cabinet to which only a social worker exclusively in charge of randomisation and the principal investigator had access. An envelope with a paper inside showing to which group each woman was assigned was opened by the social worker immediately after recruitment in the labour and delivery unit. Not stated if envelopes were sequentially numbered. |
| Blinding (performance bias and detection bias) | Low risk | Data were collected by 2 'blinded social workers'. |
| Incomplete outcome data (attrition bias) | Low risk | Medical record data and in‐hospital interview data were collected for 100% of the sample. A in‐home interview was completed at 1 month postpartum for 92.2% of the sample. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 109 Black women from Botswana (53 in support group and 56 in usual care group), mean age 19 years, 80% unmarried, mostly students, who had met the following criteria: nulliparous, in labour, pregnancy at term, no history of pregnancy complications, cephalic presentation, normal spontaneous labour with cervical dilation 1‐6 cm, female relative present who was willing to remain with the woman for the duration of labour. | |
| Interventions | Support group: continuous presence of female relative (usually her mother) in addition to usual hospital care. Congrol group: usual hospital care, which involved staff:patient ratios of 1:4, and no companions permitted during labour. | |
| Outcomes | Spontaneous vaginal birth, vacuum extraction, caesarean birth, analgesia, amniotomy, artificial oxytocin during labour, Apgar scores (1‐ and 5‐min). | |
| Notes | Epidural analgesia was not available and it was not stated whether EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Randomly allocated.' No other details provided. |
| Allocation concealment (selection bias) | Low risk | 'Selection of an opaque, numbered, sealed envelope from a box of envelopes that were shuffled in the woman's presence. When opened the envelope revealed a code indicating her group.' An assistant that was not involved in the recruitment process shuffled the envelopes. |
| Blinding (performance bias and detection bias) | High risk | The researcher, who was involved in the recruitment of participants, collected the medical record data. |
| Incomplete outcome data (attrition bias) | Low risk | Medical record data were collected on 100% of the sample. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. Enrollment occurred at childbirth education classes and randomisation occurred when the woman arrived at hospital in labour. | |
| Participants | 420 nulliparous middle and upper class women (224 on doula group and 196 in control group) were enrolled in the third trimester of an uncomplicated pregnancy in Cleveland, Ohio. All women expected to be accompanied during labour by their male partner. | |
| Interventions | Experimental group: a doula met the couple at the hospital as soon as possible after random assignment (typically within an hour of their arrival at the hospital) and remained with them throughout labour and delivery. The central component of doula support was the doula’s continuous bedside presence during labour and delivery, although her specific activities were individualised to the needs of the labouring woman. Doula support included close physical proximity, touch, and eye contact with the labouring woman, and teaching, reassurance, and encouragement of the woman and her male partner. All doulas completed training requirements that were equivalent to the DONA International doula certification. Control group: routine obstetric and nursing care which included the presence of a male partner or other support person. | |
| Outcomes | Caesarean delivery, epidural anaesthesia, oxytocin use, labour length, mode of delivery, fever during labour, satisfaction at 6 weeks postpartum. | |
| Notes | Epidural analgesia was available and EFM was used routinely. The author has been contacted for data split by study group and questionnaire data for the control group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details stated. |
| Allocation concealment (selection bias) | Low risk | 'When the research co‐ordinator was informed that an enrolled woman had arrived at the hospital in early active labor, she opened the next sequentially numbered opaque envelope to determine random assignment to the doula or control group'. The research co‐ordinator was off‐site and called by the staff or the study participant. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | Medical record data were collected on 100% of the sample. The in‐hospital and 6‐week questionnaires were completed by 87.9% and 87.5% of the doula group. No information was provided for the control group. |
| Selective reporting (reporting bias) | Low risk | The primary outcomes of caesarean birth and epidural anaesthesia were reported for each study group. Other labour and delivery outcomes were reported for the full sample only (not split by group). The in‐hospital and 6‐week questionnaire data were only reported for the doula group. The author has been contacted for these missing details. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT. | |
| Participants | 603 women from Ibadan, Nigeria with anticipated vaginal delivery were enrolled between 30 and 32 weeks' gestation at an antenatal clinic (305 to intervention and 298 to control) from November 2006 to March 2007. | |
| Interventions | Those in the experimental group were informed to bring someone of their choice to act as a companion during labour. On arrival in labour the accompanying companions were provided with an information leaflet that explained their responsibilities. These included: gentle massage of the woman’s back during contraction, reassuring words, spiritual support inform of prayers and also acting as intermediary between the woman and healthcare team. After studying the leaflets, they were allowed to seek clarifications. The information leaflet was also interpreted for those that are not literate. The attending midwife allowed and ensured companions performed their expected duties throughout. The companions were told to offer continuous support – they were to be by the patient’s side except for feeding and use of toilet until two hours after childbirth. Husbands were the most common support person (65.4%). The women in the control group had only routine care where relatives of patients are usually barred from the labour ward. | |
| Outcomes | Caesarean section rate, active phase of labour duration, pain score, need for analgesia, need for oxytocin augmentation, time from delivery to initiation of breastfeeding and the emotional experience during labour. | |
| Notes | Epidural analgesia was not available and it was not stated whether EFM was used routinely. We have requested further details from the authors. The randomisation process was well done, but resulted in an imbalance in socioeconomic status between the groups. Women in the experimental group tended to be more educated (82% vs 48% with tertiary level) and skilled workers (78% vs 39%). This imbalance was noted and discussed by the authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'The randomisation sequence was generated using a table of random numbers'. |
| Allocation concealment (selection bias) | Low risk | 'Random permuted blocks of size four were used to ensure a balanced design.' 'Based on the sequence of treatments generated using this method, treatment groups (A and B) were written on pieces of cardboard paper and put into sealed opaque envelopes. Each of the opaque envelopes had a serial number on it.' 'Two trained research assistants (RAs) non‐medical staff, supervised the randomisation procedure at every clinic. On each clinic day, consented women that met the inclusion criteria were given serial numbers with allotted treatment group based on their arrival time. Only the statistician and RAs had access to the list of numbers used to prevent clinicians’ influence on the randomisation. Each participant opened the opaque envelope in the presence of an RA, and the assigned treatment group was recorded on the woman’s medical record file.' |
| Blinding (performance bias and detection bias) | High risk | How data collection was done was not noted. The treatment group was noted in the chart so it is likely that the data collectors were unblinded. |
| Incomplete outcome data (attrition bias) | Low risk | Follow‐up was completed for 97% of the sample. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT, no details regarding method of random assignment. | |
| Participants | 144 'healthy' women having their first baby booked for delivery at a Swedish hospital (72 to doula group and 72 to usual care). Participants were enrolled at 36 weeks' gestation. | |
| Interventions | Continuous presence by a doula who had met the woman during pregnancy, compared to usual care. | |
| Outcomes | Emergency caesarean birth and epidural analgesia. | |
| Notes | The trial author reported that the information about randomisation method and outcomes of those lost to follow‐up are no longer available. Epidural analgesia was available. It was not stated if other support person(s) were allowed or if EFM was used routinely. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomized' ‐ no further details provided or available. |
| Allocation concealment (selection bias) | Unclear risk | No details provided or obtained. |
| Blinding (performance bias and detection bias) | Unclear risk | Not noted. |
| Incomplete outcome data (attrition bias) | High risk | Medical record data collected on 70.1% of sample. No usable outcome data, due to serious risk of attrition bias. Outcomes are reported for 55/72 (76%) of the intervention group and 46/72 (64%) of the control group. Reason for the 41 “dropouts” were preterm birth, induction, or caesarean section “for medical reasons”, and participant withdrawal. No numbers are given for individual reasons, or by group, but it is clear that some “dropouts” were prior to labour and others were during labour. Numbers in the report show the number of dropouts was actually 43. |
| Selective reporting (reporting bias) | Unclear risk | Sample size was based on caesarean section rate. The only outcome reported was emergency caesarean. |
| Other bias | High risk | Trial was stopped early for 'a range of largely organizational issues' when only 1/4 of the original sample size had been enrolled. |
| Methods | RCT. | |
| Participants | 435 women (217 in companion group, 218 in control group) with a singleton pregnancy and considered to be low‐risk at University Hospital in Santiago, Chile. Enrolled at 34‐36 weeks' gestation. | |
| Interventions | Intervention group: psychosocial support during labour from a companion chosen by the pregnant woman. The companions were trained by trial staff to provide emotional support, promote physical comfort and encourage progress of labour, without interfering with the activities of the obstetricians or midwives. They were with the labouring woman continuously from admission to delivery. Women were encouraged to pick a companion who had experienced a vaginal birth. Control group did not have companion. Both groups laboured in a room with other women where curtains were pulled for privacy. | |
| Outcomes | Caesarean section, exclusive breastfeeding, duration of labour, mode of delivery, use of oxytocics, presence of meconium, regional anaesthesia, birth asphyxia, Apgar scores, level of neonatal care, maternal satisfaction. | |
| Notes | Epidural analgesia was available. It was not stated if EFM was used routinely. Authors have been contacted for further details. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers. |
| Allocation concealment (selection bias) | Low risk | Used blocks of 6. Group assignment used sealed opaque envelopes numbered consecutively. A member of the trial team enrolled women and did not know in advance the content of each envelope. |
| Blinding (performance bias and detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | Medcial record data were collected for 100% of the sample and in‐hospital surveys were completed by 95.8%. A 6‐week phone interview was completed for 71.2% of the sample and thus these data were not used. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
| Methods | RCT | |
| Participants | 120 nulliparous women, ages 18‐30, at least 36 weeks' gestation, singleton fetus with cephalic presentation, able and willing to have a close female relative with them during labour and birth, booked to give birth at a regional teaching hospital in Thailand. | |
| Interventions | Experimental group: close female relative who attended a 2‐hour preparation class on labour routines and supportive actions, and provided continuous support during the active portion of hospital labour. The institution required that the researcher remain in order to monitor the relative's activities. Control group: usual care by health professionals, which included intermittent support. Family members were not permitted to stay with the woman. | |
| Outcomes | Oxytocin during labour, analgesia, labour length, spontaneous birth, assisted vaginal birth, caesarean birth, Apgar Scores, perceived control. | |
| Notes | Epidural analgesia was not available and continuous EFM was not used. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number sequence generated by a software program. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were used. Envelopes were consecutively‐numbered on the outside. |
| Blinding (performance bias and detection bias) | Low risk | Women, investigator, and providers could not be blinded to the presence of the female relative. Research assistant blinded to group assignment collected satisfaction data. |
| Incomplete outcome data (attrition bias) | Low risk | 5% lost to follow‐up: 2 in the experimental group and 4 in the control group. |
| Selective reporting (reporting bias) | Low risk | Appears complete. |
| Other bias | Low risk | 6 women (10%) in experimental group did not receive continuous support. |
EFM: electronic fetal monitoring
min: minutes
NICU: neonatal intensive care unit
RCT: randomised controlled trial
SD: standard deviation
vs: versus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| 2 studies are reported, n = 12 in the first study and n = 30 in the second. Neither one was an RCT. Both employed alternate allocation that was neither centrally controlled nor concealed. The researcher delivered the intervention and collected outcome data. In the first study the researcher also enrolled participants. No usable outcome data are reported. | |
| The intervention was not continuous labour support. It was a short nursing intervention (taking approximately 1 hour) administered in early labour for women undergoing Misoprostol induction. | |
| The intervention was not continuous labour support. It was an educational intervention to promote childbirth companions in hospital deliveries. A cluster‐RCT was undertaken at 10 South African state maternity hospitals. | |
| Not an RCT. 100 randomly‐selected mothers who had a birth companion were compared with 50 randomly‐selected mothers who did not have one. Mothers were matched for age and socioeconomic status. | |
| 30% of those enrolled were excluded post‐randomisation, 73/232 in the doula group and 69/246 in the control group. A letter was sent to the first author, asking for data on the excluded participants that would permit an intent‐to‐treat analysis. If and when a response is received, we will evaluate the trial report again. | |
| Third study in the same report as Hemminki 1990aand Hemminki 1990b. This was a small pilot RCT of support by laywomen that was 'stopped for economic and other practical reasons'. 31 women were enrolled but 7 dropped out (all from the intervention group). Very little data were reported and it was not separated by treatment group and thus unusable. | |
| Support was not continuous, and was quite brief in duration. 16 women in active labour were randomised to either 1 hour with a supportive companion or 1 hour without. The only outcome was maternal oxytocin level for 16 minutes post‐support or control period. | |
| An abstract outlining a study of 531 women in Houston, Texas. Insufficient details to permit evaluation of the quality of the trial, and insufficient details regarding results. Thus far, attempts to locate a full report of the trial have been unsuccessful. | |
| Not a randomised trial. Women chose to either have a doula or have Lamaze preparation for childbirth. | |
| An abstract of a paper presented at the Xth World Congress of Psychiatry in Madrid, 1996. Preliminary results were reported. Efforts to locate a published report of the full trial have been unsuccessful. The abstract provides insufficient details regarding methods, to permit evaluation of the quality of the trial. The purpose was to compare the effectiveness of female vs male doulas vs routine care without doulas. The doulas were medical and psychology students. | |
| Not an RCT. Translated personal communication from the author stated "I randomly sampling allocated the patient, did not use any random tool". | |
| Not a trial. A review of selected studies of intrapartum support. | |
| Strong evidence of selection bias. "A woman was removed from the study if labor was false or prolonged; if fetal distress necessitated an intervention such as oxytocin, caesarean delivery, or forceps"; or if the infant was asphyxiated or ill at birth, etc. "If a woman was removed, her group assignment was inserted at random into the pool of unused assignments. Women were enrolled in the study until there were 20 in the control group and 20 in the experimental group." The total study sample of 127 mothers includes 95 in the control group and 32 in the experimental group. Thus assignment was not random. | |
| Direct contact with investigator revealed that randomisation was not used. On arrival at the hospital, women were asked if they wanted to have a doula. If they accepted, a doula was assigned to them. Also support was not continuous throughout active labour for most women, since admission to the labour ward (and assignment of a doula) did not usually occur until 8 cm. | |
| Not an RCT. "After a random start, the matched groups were alternately assigned to experimental and control groups." Women who developed severe complications in labour (number not specified), such as fetal distress, were dropped from the study. | |
| Not a trial of continuous 1‐to‐1 support. On admission to the labour ward, women received instruction about normal labour, non‐pharmacological methods to ease pain, and how to push in second stage, from a team of physicians and nurses. Support was continuous, depending on the women's needs, but not 1‐to‐1. |
EFM: electronic fetal monitoring
RCT: randomised controlled trial
vs: versus
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract ‐ insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Unclear. |
| Outcomes | Insufficient details. |
| Notes | Communication sent to author regarding details of randomisation process, the nature of the intervention, and information to allow classification for analysis subgroups. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract ‐ insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract ‐ insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract ‐ insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract ‐ insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract ‐ insufficient details to permit classification. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Notes | Abstract ‐ insufficient details to permit classification. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Janssen. |
| Methods | Insufficient details. |
| Participants | Insufficient details. |
| Interventions | Insufficient details. |
| Outcomes | Insufficient details. |
| Starting date | Insufficient details. |
| Contact information | Insufficient details. |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | 12283 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.84, 0.96] |
| Analysis 1.1  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 1 Any analgesia/anaesthesia. | ||||
| 2 Regional analgesia/anaesthesia Show forest plot | 9 | 11444 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.99] |
| Analysis 1.2  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 2 Regional analgesia/anaesthesia. | ||||
| 3 Synthetic oxytocin during labour Show forest plot | 15 | 12620 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.91, 1.04] |
| Analysis 1.3 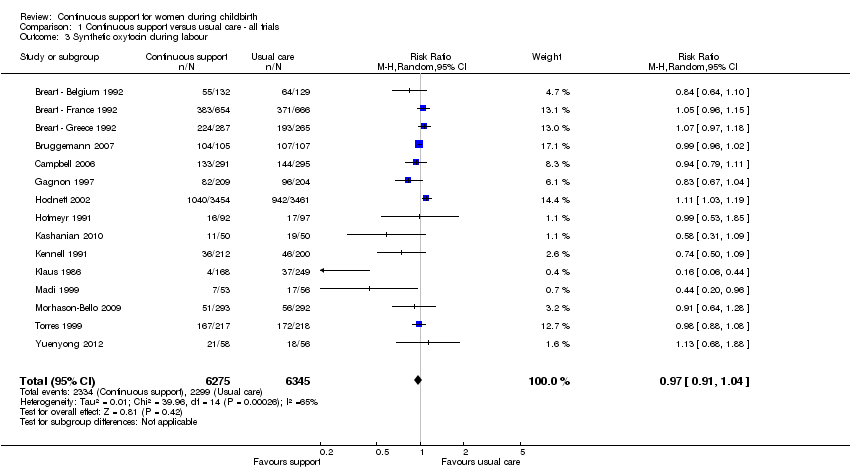 Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 3 Synthetic oxytocin during labour. | ||||
| 4 Labour length Show forest plot | 12 | 5366 | Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐0.85, ‐0.31] |
| Analysis 1.4  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 4 Labour length. | ||||
| 5 Spontaneous vaginal birth Show forest plot | 19 | 14119 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [1.04, 1.12] |
| Analysis 1.5 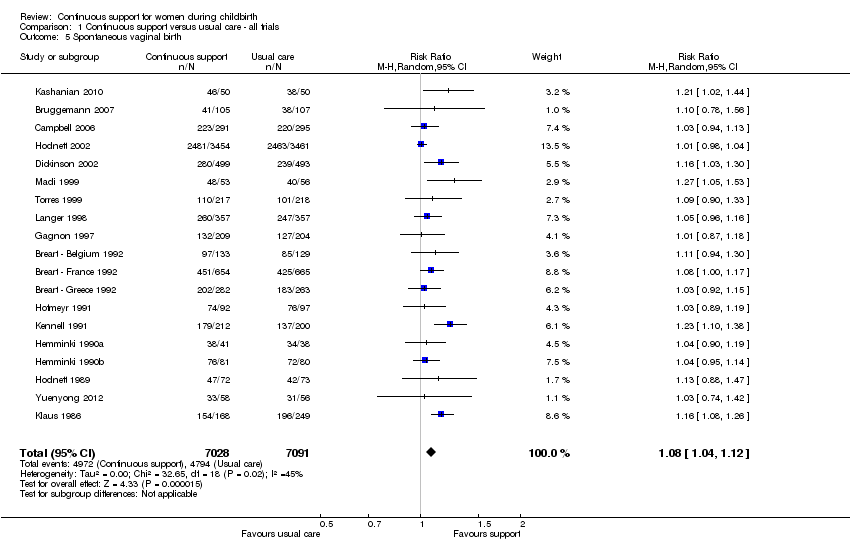 Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 5 Spontaneous vaginal birth. | ||||
| 6 Instrumental vaginal birth Show forest plot | 19 | 14118 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.85, 0.96] |
| Analysis 1.6  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 6 Instrumental vaginal birth. | ||||
| 7 Caesarean birth Show forest plot | 22 | 15175 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.67, 0.91] |
| Analysis 1.7 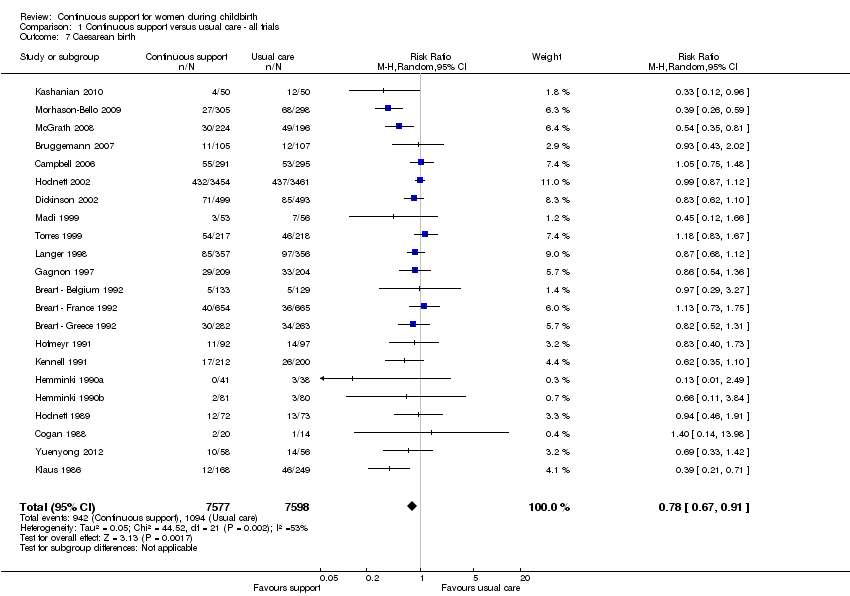 Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 7 Caesarean birth. | ||||
| 8 Perineal trauma Show forest plot | 4 | 8120 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.92, 1.01] |
| Analysis 1.8  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 8 Perineal trauma. | ||||
| 9 Low 5‐minute Apgar score Show forest plot | 13 | 12515 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.50, 0.95] |
| Analysis 1.9  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 9 Low 5‐minute Apgar score. | ||||
| 10 Admission to special care nursery Show forest plot | 7 | 8897 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.76, 1.25] |
| Analysis 1.10  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 10 Admission to special care nursery. | ||||
| 11 Prolonged neonatal hospital stay Show forest plot | 3 | 1098 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.42, 1.65] |
| Analysis 1.11  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 11 Prolonged neonatal hospital stay. | ||||
| 12 Postpartum report of severe labour pain Show forest plot | 4 | 2456 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.83, 1.21] |
| Analysis 1.12  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 12 Postpartum report of severe labour pain. | ||||
| 13 Negative rating of/negative feelings about birth experience Show forest plot | 11 | 11133 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.59, 0.79] |
| Analysis 1.13 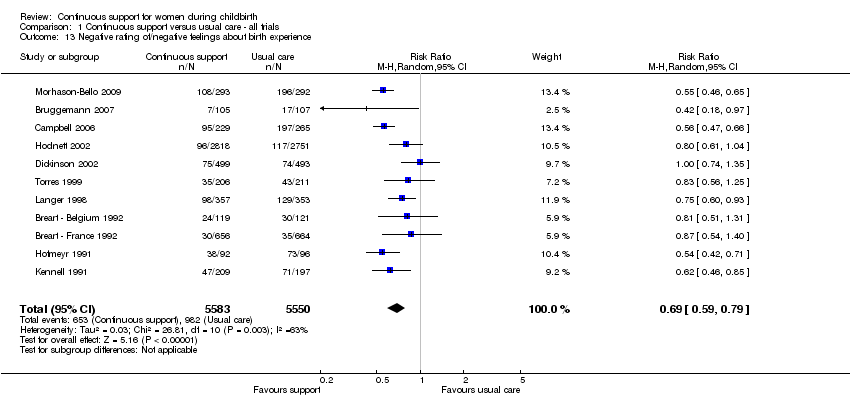 Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 13 Negative rating of/negative feelings about birth experience. | ||||
| 14 Difficulty mothering Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.14  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 14 Difficulty mothering. | ||||
| 15 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | 5363 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.94, 1.09] |
| Analysis 1.15  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 15 Breastfeeding at 1‐2 months postpartum. | ||||
| 16 Postpartum depression Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.16  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 16 Postpartum depression. | ||||
| 17 Low postpartum self‐esteem Show forest plot | 1 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.77, 1.30] |
| Analysis 1.17  Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 17 Low postpartum self‐esteem. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 1 Any analgesia/anaesthesia. | ||||
| 1.1 Other support permitted | 7 | 9752 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.99] |
| 1.2 Other support not permitted | 7 | 2598 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.85, 0.96] |
| 2 Synthetic oxytocin during labour Show forest plot | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 2 Synthetic oxytocin during labour. | ||||
| 2.1 Other support permitted | 5 | 9495 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [0.99, 1.10] |
| 2.2 Other support not permitted | 10 | 3125 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.97, 1.02] |
| 3 Spontaneous vaginal birth Show forest plot | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 3 Spontaneous vaginal birth. | ||||
| 3.1 Other support permitted | 9 | 10889 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [1.00, 1.05] |
| 3.2 Other support not permitted | 10 | 3329 | Risk Ratio (IV, Fixed, 95% CI) | 1.11 [1.07, 1.16] |
| 4 Caesarean birth Show forest plot | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.4  Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 4 Caesarean birth. | ||||
| 4.1 Other support permitted | 11 | 11326 | Risk Ratio (IV, Fixed, 95% CI) | 0.94 [0.85, 1.03] |
| 4.2 Other support not permitted | 11 | 3849 | Risk Ratio (IV, Fixed, 95% CI) | 0.75 [0.65, 0.86] |
| 5 Admission to special care nursery Show forest plot | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 5 Admission to special care nursery. | ||||
| 5.1 Other support permitted | 2 | 7328 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.84, 1.17] |
| 5.2 Other support not permitted | 5 | 1569 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.71, 1.17] |
| 6 Postpartum depression Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.6  Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 6 Postpartum depression. | ||||
| 6.1 Other support permitted | 1 | 5567 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.73, 1.02] |
| 6.2 Other support not permitted | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.18 [0.09, 0.36] |
| 7 Negative rating of/negative feelings about birth experience Show forest plot | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.7  Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 7 Negative rating of/negative feelings about birth experience. | ||||
| 7.1 Other support permitted | 5 | 8639 | Risk Ratio (IV, Fixed, 95% CI) | 0.70 [0.62, 0.78] |
| 7.2 Other support not permitted | 6 | 2539 | Risk Ratio (IV, Fixed, 95% CI) | 0.62 [0.56, 0.69] |
| 8 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.8  Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 8 Breastfeeding at 1‐2 months postpartum. | ||||
| 8.1 Other support permitted | 1 | 4559 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.92, 1.02] |
| 8.2 Other support not permitted | 2 | 804 | Risk Ratio (IV, Fixed, 95% CI) | 1.05 [0.98, 1.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.1 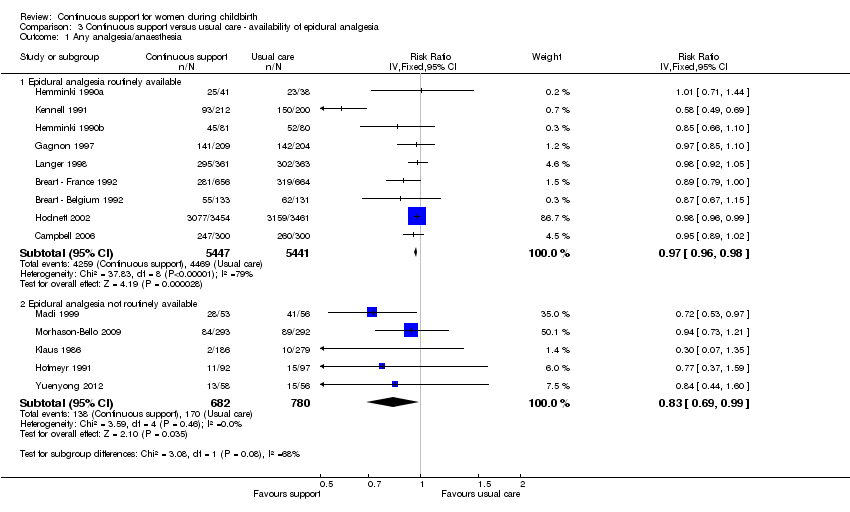 Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 1 Any analgesia/anaesthesia. | ||||
| 1.1 Epidural analgesia routinely available | 9 | 10888 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.98] |
| 1.2 Epidural analgesia not routinely available | 5 | 1462 | Risk Ratio (IV, Fixed, 95% CI) | 0.83 [0.69, 0.99] |
| 2 Synthetic oxytocin during labour Show forest plot | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 2 Synthetic oxytocin during labour. | ||||
| 2.1 Epidural analgesia routinely available | 8 | 10568 | Risk Ratio (IV, Fixed, 95% CI) | 1.00 [0.98, 1.02] |
| 2.2 Epidural analgesia not routinely available | 7 | 2066 | Risk Ratio (IV, Fixed, 95% CI) | 1.02 [0.93, 1.11] |
| 3 Spontaneous vaginal birth Show forest plot | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.3 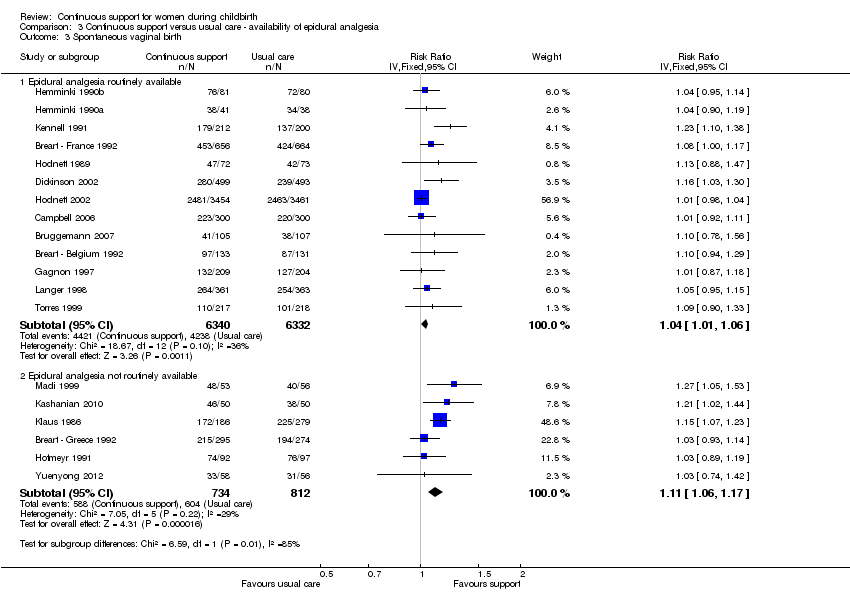 Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 3 Spontaneous vaginal birth. | ||||
| 3.1 Epidural analgesia routinely available | 13 | 12672 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [1.01, 1.06] |
| 3.2 Epidural analgesia not routinely available | 6 | 1546 | Risk Ratio (IV, Fixed, 95% CI) | 1.11 [1.06, 1.17] |
| 4 Caesarean birth Show forest plot | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.4  Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 4 Caesarean birth. | ||||
| 4.1 Epidural analgesia routinely available | 14 | 13064 | Risk Ratio (IV, Fixed, 95% CI) | 0.93 [0.86, 1.02] |
| 4.2 Epidural analgesia not routinely available | 7 | 2077 | Risk Ratio (IV, Fixed, 95% CI) | 0.54 [0.43, 0.68] |
| 4.3 Unknown availability of epidural analgesia | 1 | 34 | Risk Ratio (IV, Fixed, 95% CI) | 1.4 [0.14, 13.98] |
| 5 Admission to special care nursery Show forest plot | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.5  Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 5 Admission to special care nursery. | ||||
| 5.1 Epidural analgesia routinely available | 5 | 8380 | Risk Ratio (IV, Fixed, 95% CI) | 0.98 [0.85, 1.13] |
| 5.2 Epidural analgesia not routinely available | 2 | 517 | Risk Ratio (IV, Fixed, 95% CI) | 0.26 [0.08, 0.88] |
| 6 Postpartum depression Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.6 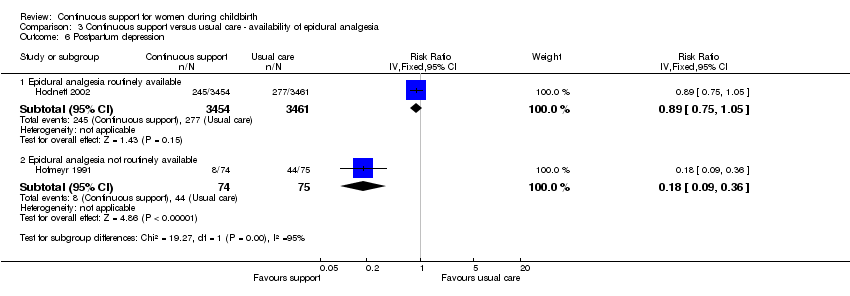 Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 6 Postpartum depression. | ||||
| 6.1 Epidural analgesia routinely available | 1 | 6915 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.75, 1.05] |
| 6.2 Epidural analgesia not routinely available | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.18 [0.09, 0.36] |
| 7 Negative rating of/negative feelings about birth experience Show forest plot | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.7  Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 7 Negative rating of/negative feelings about birth experience. | ||||
| 7.1 Epidural analgesia routinely available | 9 | 10404 | Risk Ratio (IV, Fixed, 95% CI) | 0.70 [0.64, 0.77] |
| 7.2 Epidural analgesia not routinely available | 2 | 774 | Risk Ratio (IV, Fixed, 95% CI) | 0.55 [0.48, 0.63] |
| 8 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.8 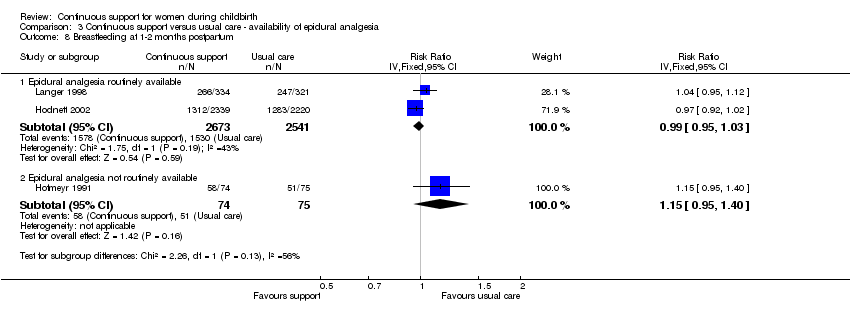 Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 8 Breastfeeding at 1‐2 months postpartum. | ||||
| 8.1 Epidural analgesia routinely available | 2 | 5214 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.95, 1.03] |
| 8.2 Epidural analgesia not routinely available | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 1.15 [0.95, 1.40] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.1  Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 1 Any analgesia/anaesthesia. | ||||
| 1.1 Setting had routine EFM | 6 | 8580 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.99] |
| 1.2 Setting did not have routine EFM | 6 | 2186 | Risk Ratio (IV, Fixed, 95% CI) | 0.96 [0.90, 1.02] |
| 1.3 Policy about routine EFM not known | 2 | 1579 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.80, 0.99] |
| 2 Synthetic oxytocin during labour Show forest plot | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.2  Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 2 Synthetic oxytocin during labour. | ||||
| 2.1 Setting had routine EFM | 4 | 8340 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [0.98, 1.11] |
| 2.2 Setting did not have routine EFM | 7 | 1726 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.96, 1.01] |
| 2.3 Policy about routine EFM not known | 4 | 2568 | Risk Ratio (IV, Fixed, 95% CI) | 1.02 [0.97, 1.08] |
| 3 Spontaneous vaginal birth Show forest plot | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.3 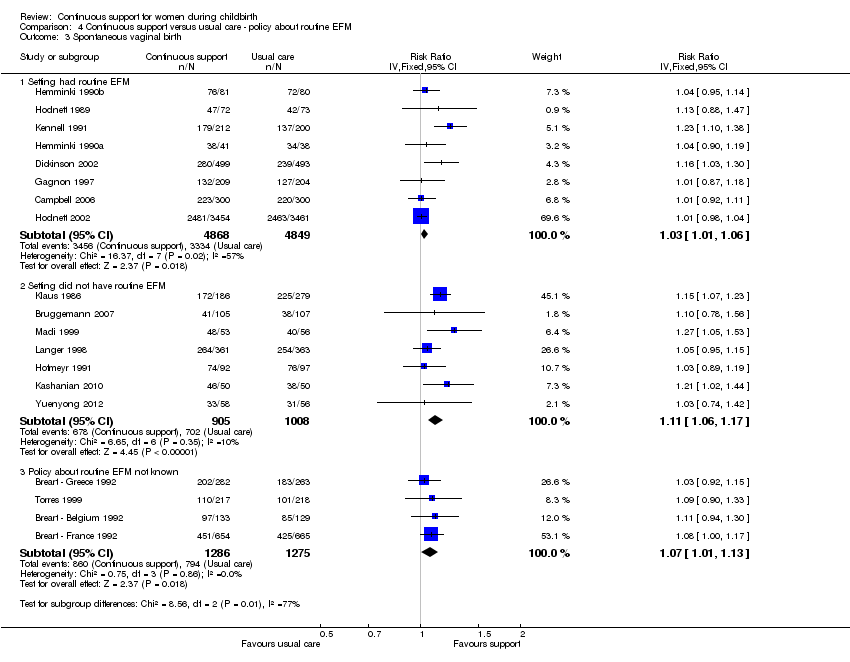 Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 3 Spontaneous vaginal birth. | ||||
| 3.1 Setting had routine EFM | 8 | 9717 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [1.01, 1.06] |
| 3.2 Setting did not have routine EFM | 7 | 1913 | Risk Ratio (IV, Fixed, 95% CI) | 1.11 [1.06, 1.17] |
| 3.3 Policy about routine EFM not known | 4 | 2561 | Risk Ratio (IV, Fixed, 95% CI) | 1.07 [1.01, 1.13] |
| 4 Caesarean birth Show forest plot | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.4  Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 4 Caesarean birth. | ||||
| 4.1 Setting had routine EFM | 9 | 10123 | Risk Ratio (IV, Fixed, 95% CI) | 0.92 [0.83, 1.01] |
| 4.2 Setting did not have routine EFM | 8 | 2457 | Risk Ratio (IV, Fixed, 95% CI) | 0.66 [0.55, 0.79] |
| 4.3 Policy about routine EFM not known | 5 | 2595 | Risk Ratio (IV, Fixed, 95% CI) | 1.06 [0.84, 1.33] |
| 5 Admission to special care nursery Show forest plot | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.5  Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 5 Admission to special care nursery. | ||||
| 5.1 Setting had routine EFM | 3 | 7740 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.84, 1.11] |
| 5.2 Setting did not have routine EFM | 3 | 729 | Risk Ratio (IV, Fixed, 95% CI) | 0.48 [0.21, 1.12] |
| 5.3 Policy about routine EFM not known | 1 | 428 | Risk Ratio (IV, Fixed, 95% CI) | 1.98 [0.76, 5.18] |
| 6 Postpartum depression Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.6  Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 6 Postpartum depression. | ||||
| 6.1 Setting had routine EFM | 1 | 6915 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.75, 1.05] |
| 6.2 Setting did not have routine EFM | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.18 [0.09, 0.36] |
| 7 Negative rating of/negative views about birth experience Show forest plot | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.7 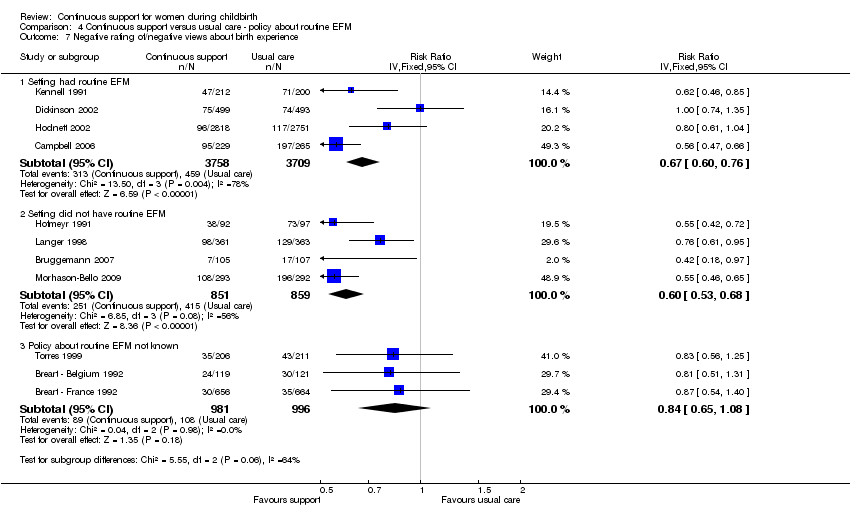 Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 7 Negative rating of/negative views about birth experience. | ||||
| 7.1 Setting had routine EFM | 4 | 7467 | Risk Ratio (IV, Fixed, 95% CI) | 0.67 [0.60, 0.76] |
| 7.2 Setting did not have routine EFM | 4 | 1710 | Risk Ratio (IV, Fixed, 95% CI) | 0.60 [0.53, 0.68] |
| 7.3 Policy about routine EFM not known | 3 | 1977 | Risk Ratio (IV, Fixed, 95% CI) | 0.84 [0.65, 1.08] |
| 8 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.8 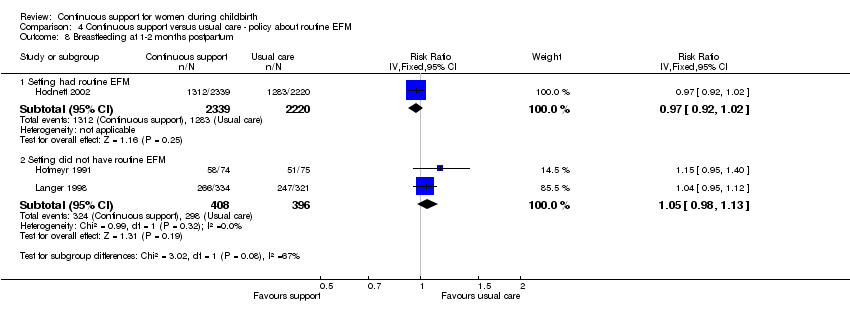 Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 8 Breastfeeding at 1‐2 months postpartum. | ||||
| 8.1 Setting had routine EFM | 1 | 4559 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.92, 1.02] |
| 8.2 Setting did not have routine EFM | 2 | 804 | Risk Ratio (IV, Fixed, 95% CI) | 1.05 [0.98, 1.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.1  Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 1 Any analgesia/anaesthesia. | ||||
| 1.1 Support people were hospital staff | 6 | 9152 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.99] |
| 1.2 Support people were not hospital staff and not chosen by woman | 4 | 1790 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.86, 0.97] |
| 1.3 Support people were not hospital staff and were chosen by woman | 4 | 1408 | Risk Ratio (IV, Fixed, 95% CI) | 0.94 [0.88, 1.00] |
| 2 Synthetic oxytocin during labour Show forest plot | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.2 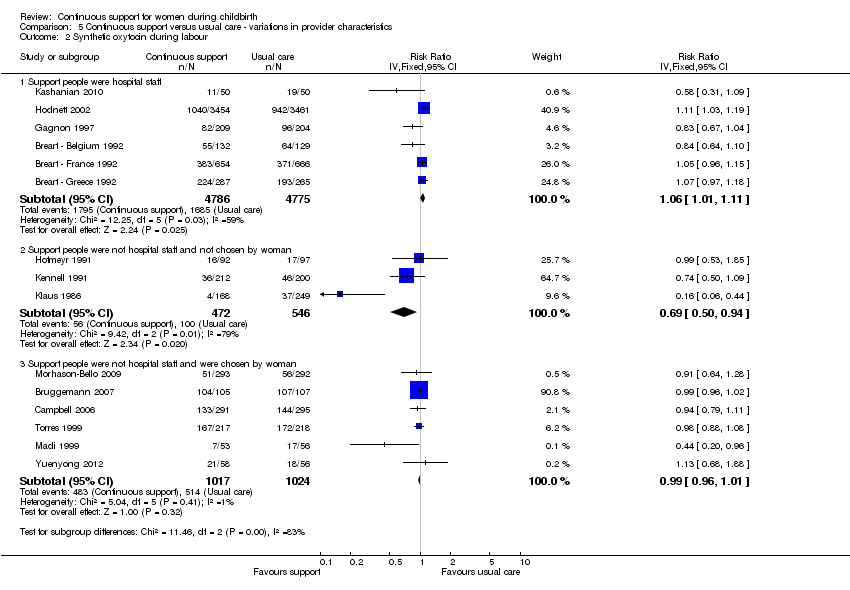 Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 2 Synthetic oxytocin during labour. | ||||
| 2.1 Support people were hospital staff | 6 | 9561 | Risk Ratio (IV, Fixed, 95% CI) | 1.06 [1.01, 1.11] |
| 2.2 Support people were not hospital staff and not chosen by woman | 3 | 1018 | Risk Ratio (IV, Fixed, 95% CI) | 0.69 [0.50, 0.94] |
| 2.3 Support people were not hospital staff and were chosen by woman | 6 | 2041 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.96, 1.01] |
| 3 Spontaneous vaginal birth Show forest plot | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.3 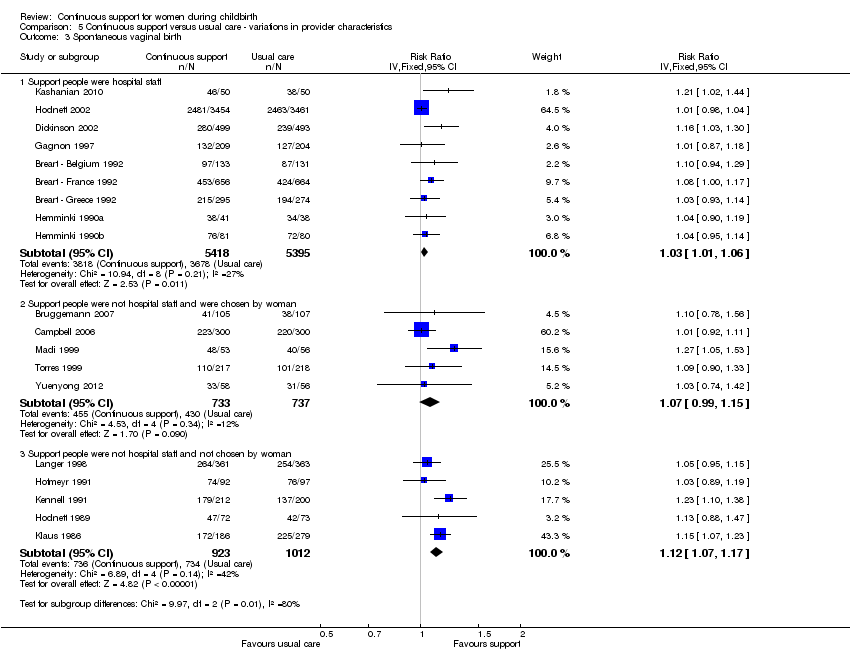 Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 3 Spontaneous vaginal birth. | ||||
| 3.1 Support people were hospital staff | 9 | 10813 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [1.01, 1.06] |
| 3.2 Support people were not hospital staff and were chosen by woman | 5 | 1470 | Risk Ratio (IV, Fixed, 95% CI) | 1.07 [0.99, 1.15] |
| 3.3 Support people were not hospital staff and not chosen by woman | 5 | 1935 | Risk Ratio (IV, Fixed, 95% CI) | 1.12 [1.07, 1.17] |
| 4 Caesarean birth Show forest plot | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.4  Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 4 Caesarean birth. | ||||
| 4.1 Support people were hospital staff | 9 | 10786 | Risk Ratio (IV, Fixed, 95% CI) | 0.95 [0.85, 1.05] |
| 4.2 Support people were not hospital staff and not chosen by woman | 7 | 2330 | Risk Ratio (IV, Fixed, 95% CI) | 0.72 [0.60, 0.86] |
| 4.3 Support people were not hospital staff and were chosen by woman | 6 | 2059 | Risk Ratio (IV, Fixed, 95% CI) | 0.83 [0.69, 1.01] |
| 5 Admission to special care nursery Show forest plot | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.5  Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 5 Admission to special care nursery. | ||||
| 5.1 Support people were hospital staff | 3 | 7428 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.84, 1.17] |
| 5.2 Support people were not hospital staff and not chosen by woman | 2 | 829 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.66, 1.12] |
| 5.3 Support people were not hospital staff and were chosen by woman | 2 | 640 | Risk Ratio (IV, Fixed, 95% CI) | 1.40 [0.67, 2.93] |
| 6 Postpartum depression Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.6  Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 6 Postpartum depression. | ||||
| 6.1 Support people were hospital staff | 1 | 5567 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.73, 1.02] |
| 6.2 Support people were not hospital staff and not chosen by woman | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.17 [0.09, 0.33] |
| 6.3 Support people were not hospital staff and were chosen by woman | 0 | 0 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Negative rating of/negative feelings about birth experience Show forest plot | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.7  Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 7 Negative rating of/negative feelings about birth experience. | ||||
| 7.1 Support people were hospital staff | 4 | 8145 | Risk Ratio (IV, Fixed, 95% CI) | 0.87 [0.73, 1.03] |
| 7.2 Support people were not hospital staff and not chosen by woman | 3 | 1325 | Risk Ratio (IV, Fixed, 95% CI) | 0.66 [0.57, 0.77] |
| 7.3 Support people were not hospital staff and were chosen by woman | 4 | 1708 | Risk Ratio (IV, Fixed, 95% CI) | 0.57 [0.51, 0.64] |
| 8 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.8  Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 8 Breastfeeding at 1‐2 months postpartum. | ||||
| 8.1 Support people were hospital staff | 1 | 4559 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.92, 1.02] |
| 8.2 Support people were not hospital staff and not chosen by woman | 2 | 804 | Risk Ratio (IV, Fixed, 95% CI) | 1.05 [0.98, 1.13] |
| 8.3 Support people were not hospital staff and were chosen by woman | 0 | 0 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
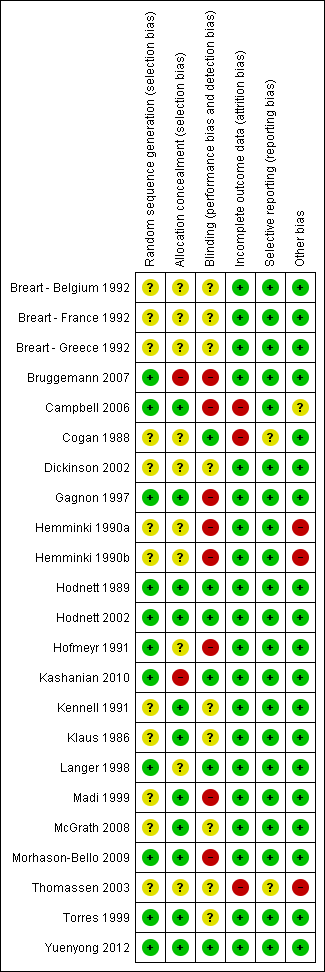
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
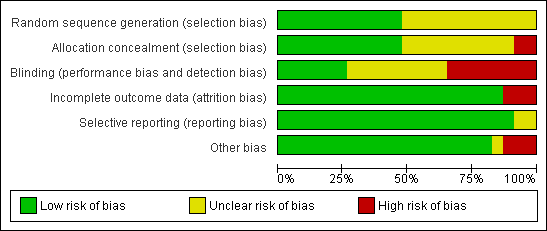
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies

Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 1 Any analgesia/anaesthesia.
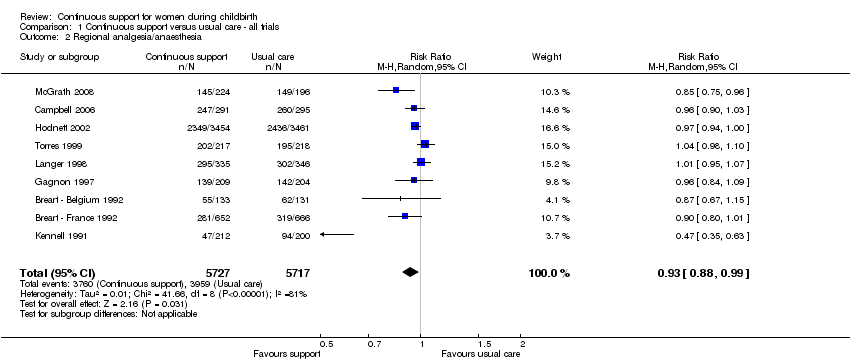
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 2 Regional analgesia/anaesthesia.
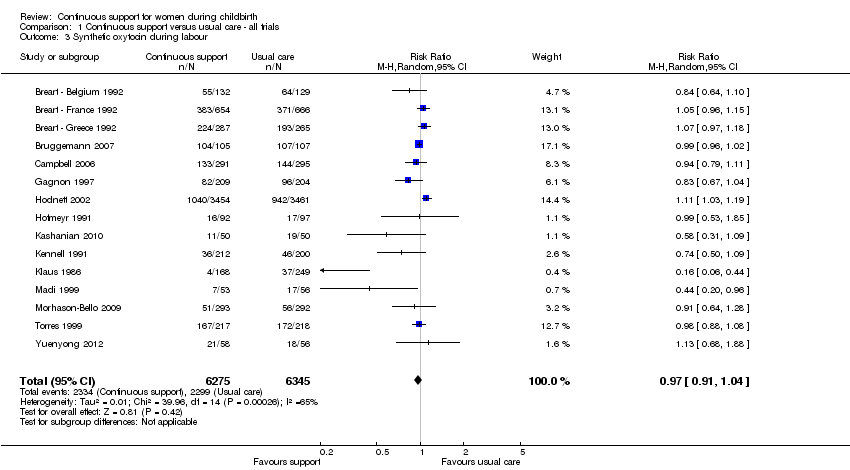
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 3 Synthetic oxytocin during labour.
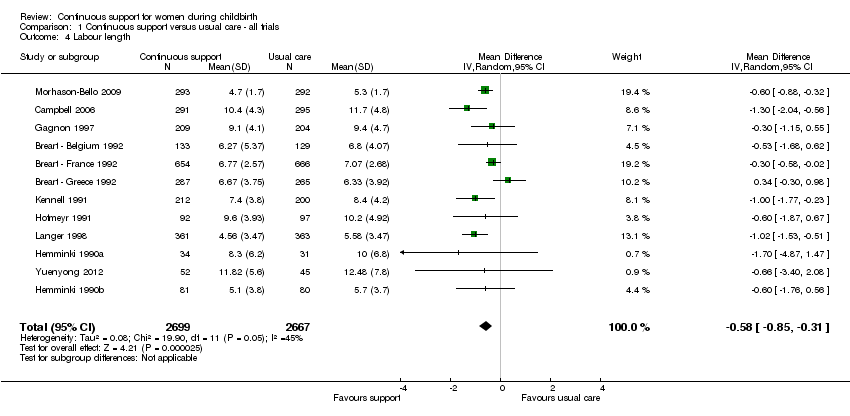
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 4 Labour length.
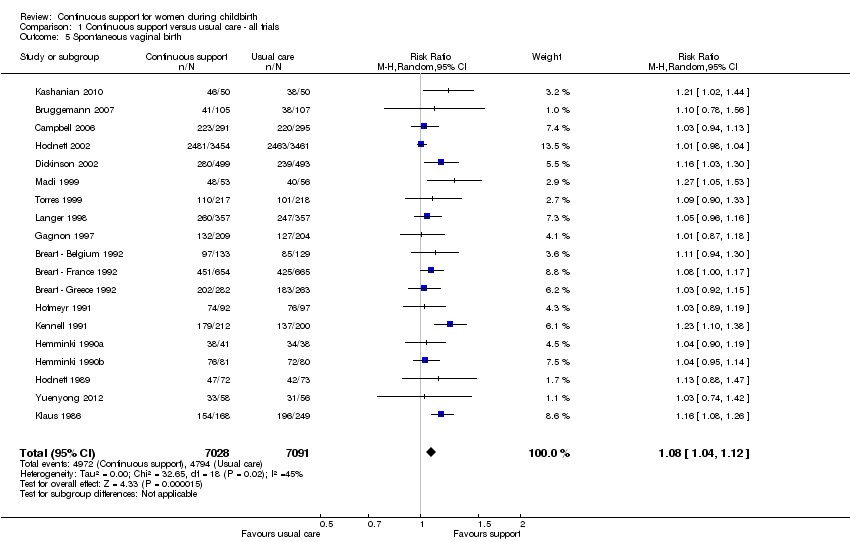
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 5 Spontaneous vaginal birth.

Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 6 Instrumental vaginal birth.

Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 7 Caesarean birth.
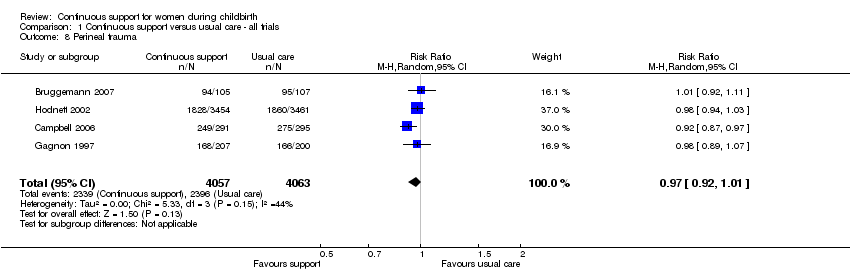
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 8 Perineal trauma.
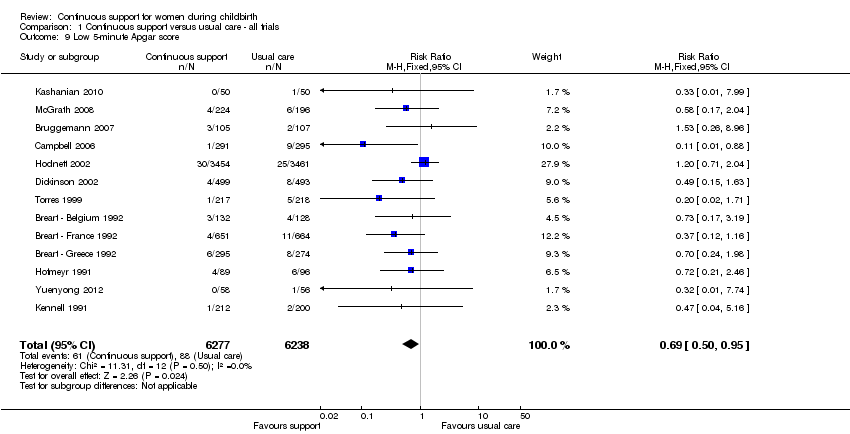
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 9 Low 5‐minute Apgar score.

Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 10 Admission to special care nursery.
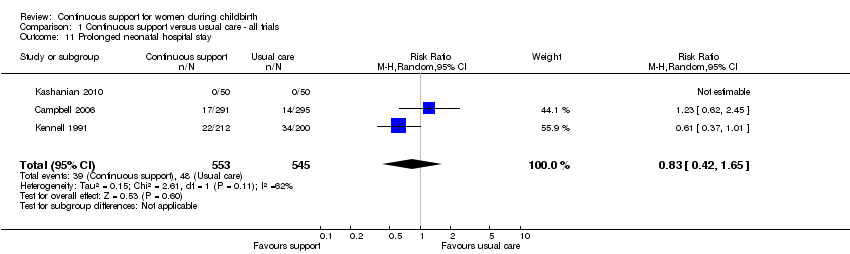
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 11 Prolonged neonatal hospital stay.
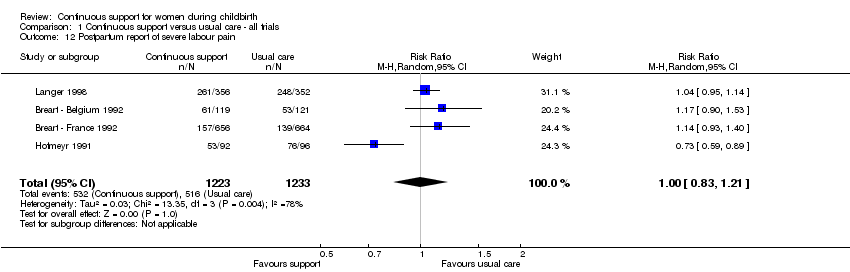
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 12 Postpartum report of severe labour pain.
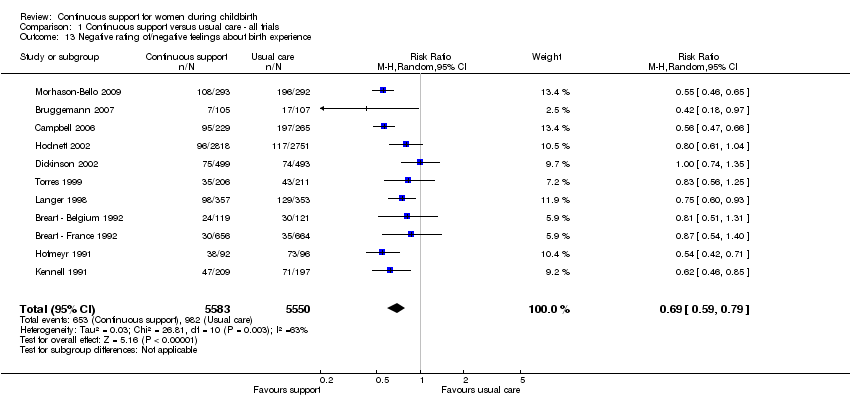
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 13 Negative rating of/negative feelings about birth experience.

Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 14 Difficulty mothering.
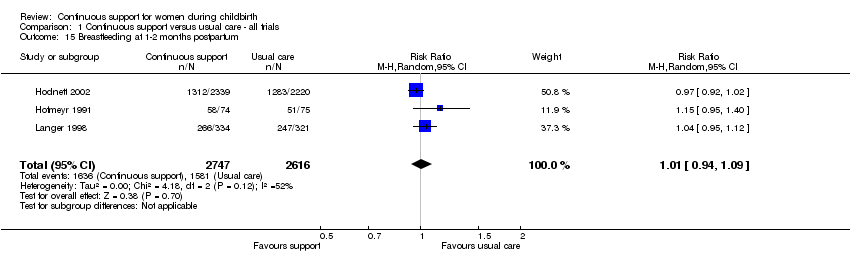
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 15 Breastfeeding at 1‐2 months postpartum.

Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 16 Postpartum depression.
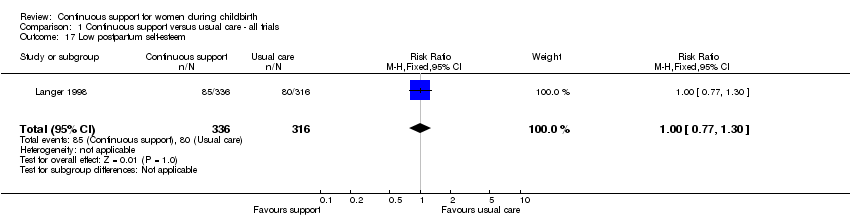
Comparison 1 Continuous support versus usual care ‐ all trials, Outcome 17 Low postpartum self‐esteem.
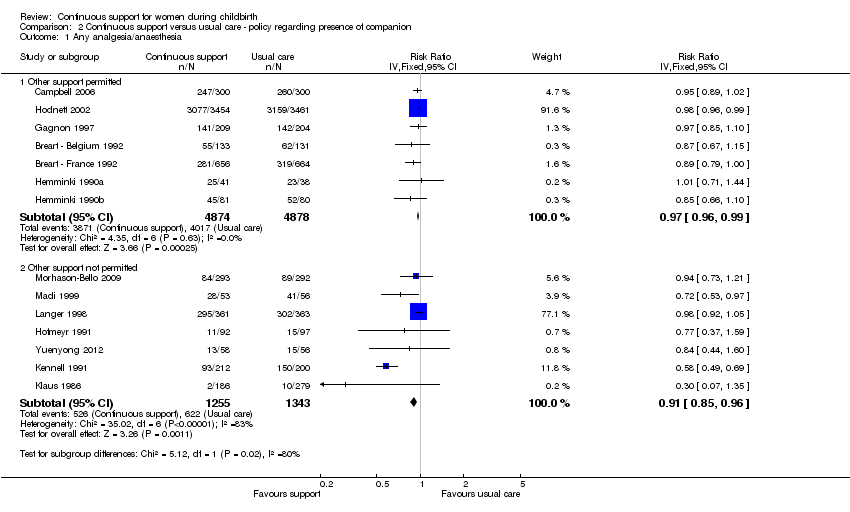
Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 1 Any analgesia/anaesthesia.

Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 2 Synthetic oxytocin during labour.
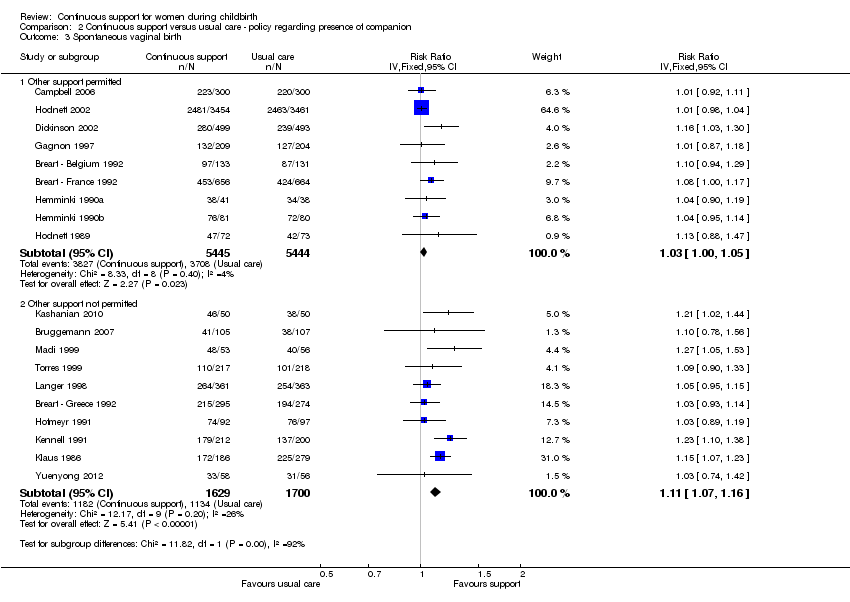
Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 3 Spontaneous vaginal birth.

Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 4 Caesarean birth.

Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 5 Admission to special care nursery.
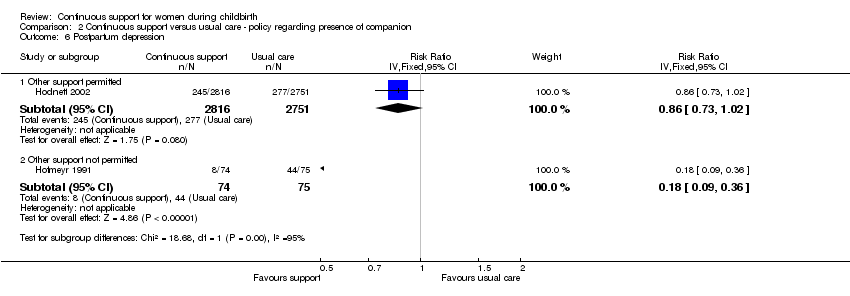
Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 6 Postpartum depression.

Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 7 Negative rating of/negative feelings about birth experience.

Comparison 2 Continuous support versus usual care ‐ policy regarding presence of companion, Outcome 8 Breastfeeding at 1‐2 months postpartum.
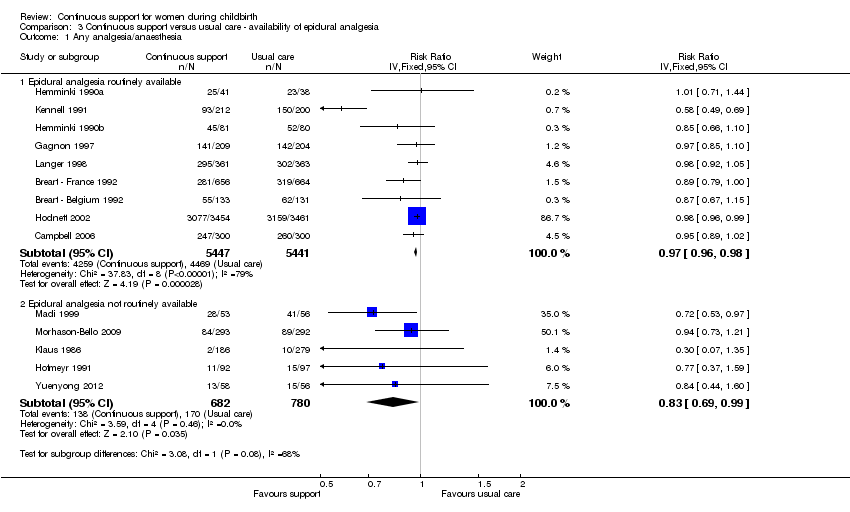
Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 1 Any analgesia/anaesthesia.

Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 2 Synthetic oxytocin during labour.

Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 3 Spontaneous vaginal birth.
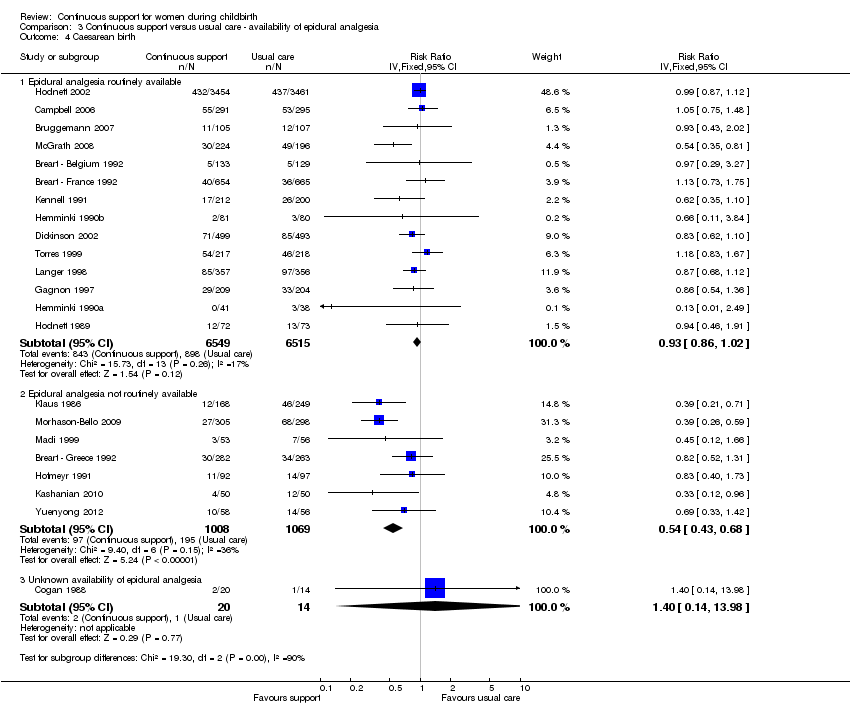
Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 4 Caesarean birth.

Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 5 Admission to special care nursery.

Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 6 Postpartum depression.

Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 7 Negative rating of/negative feelings about birth experience.
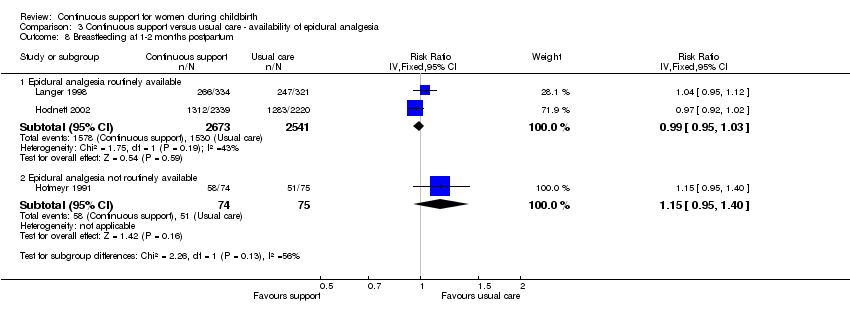
Comparison 3 Continuous support versus usual care ‐ availability of epidural analgesia, Outcome 8 Breastfeeding at 1‐2 months postpartum.
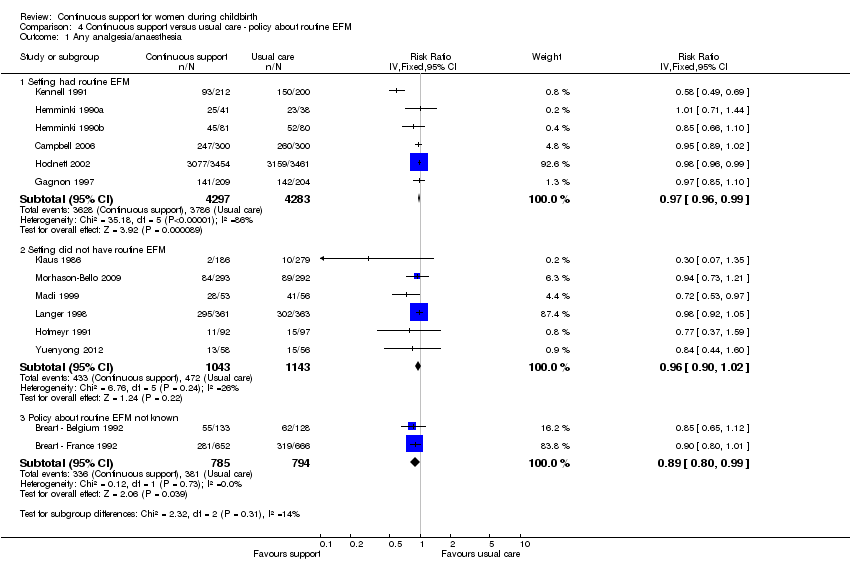
Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 1 Any analgesia/anaesthesia.
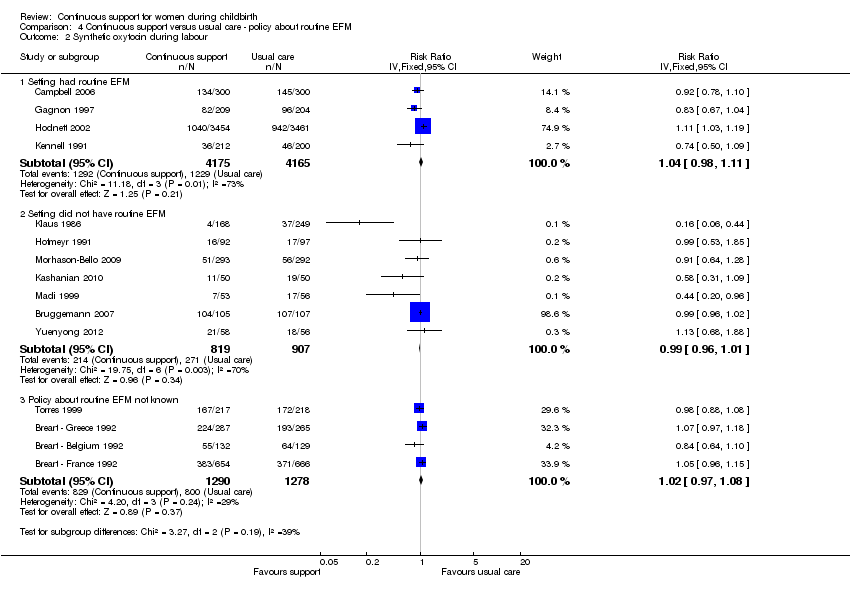
Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 2 Synthetic oxytocin during labour.
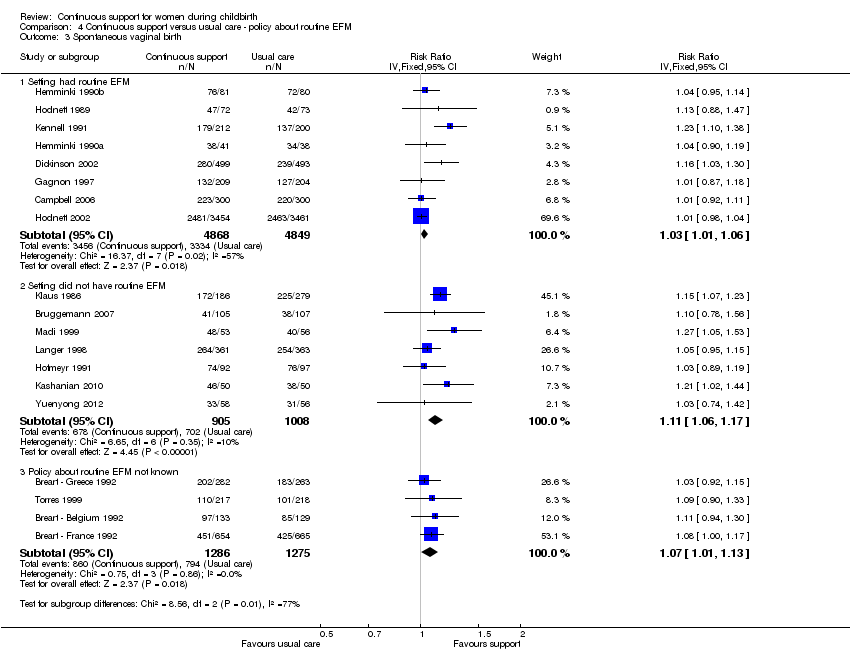
Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 3 Spontaneous vaginal birth.

Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 4 Caesarean birth.

Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 5 Admission to special care nursery.

Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 6 Postpartum depression.

Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 7 Negative rating of/negative views about birth experience.
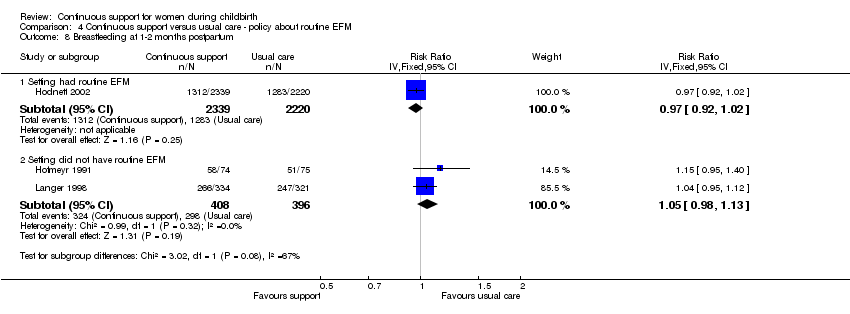
Comparison 4 Continuous support versus usual care ‐ policy about routine EFM, Outcome 8 Breastfeeding at 1‐2 months postpartum.
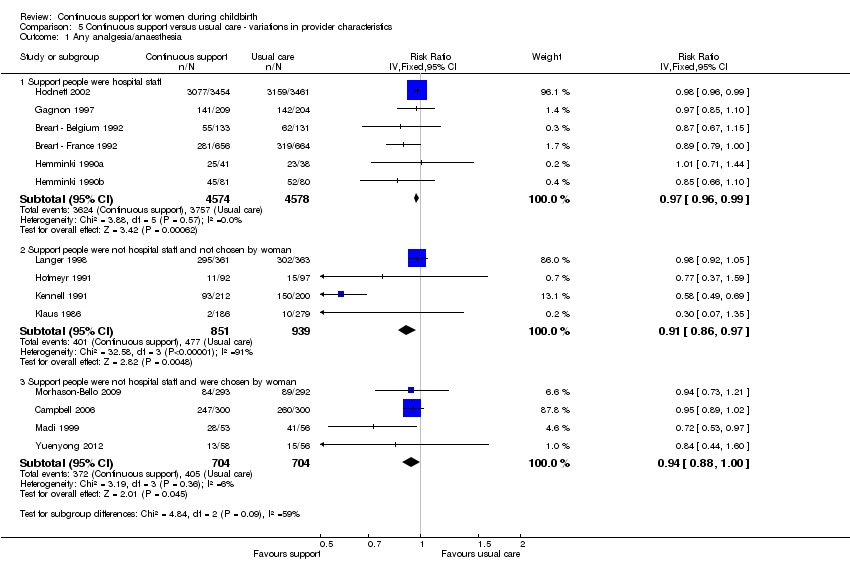
Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 1 Any analgesia/anaesthesia.
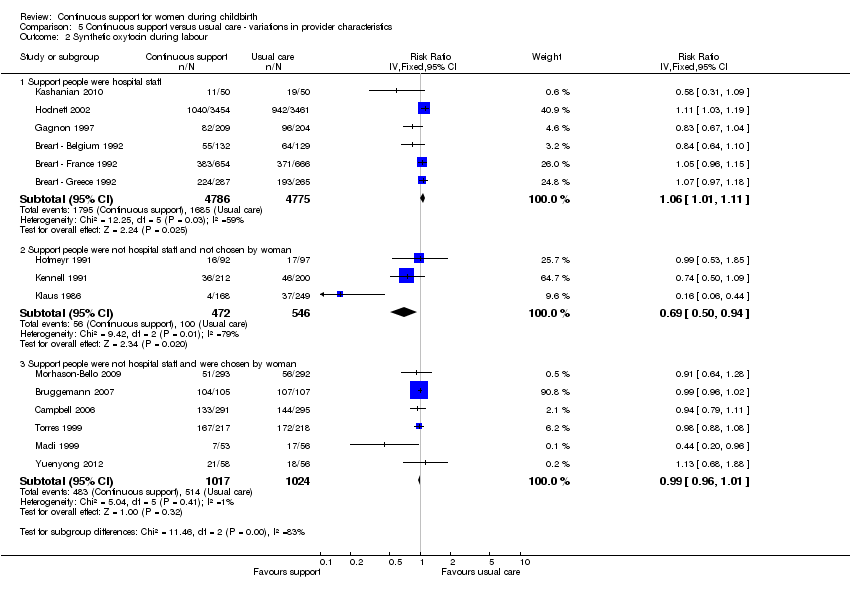
Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 2 Synthetic oxytocin during labour.
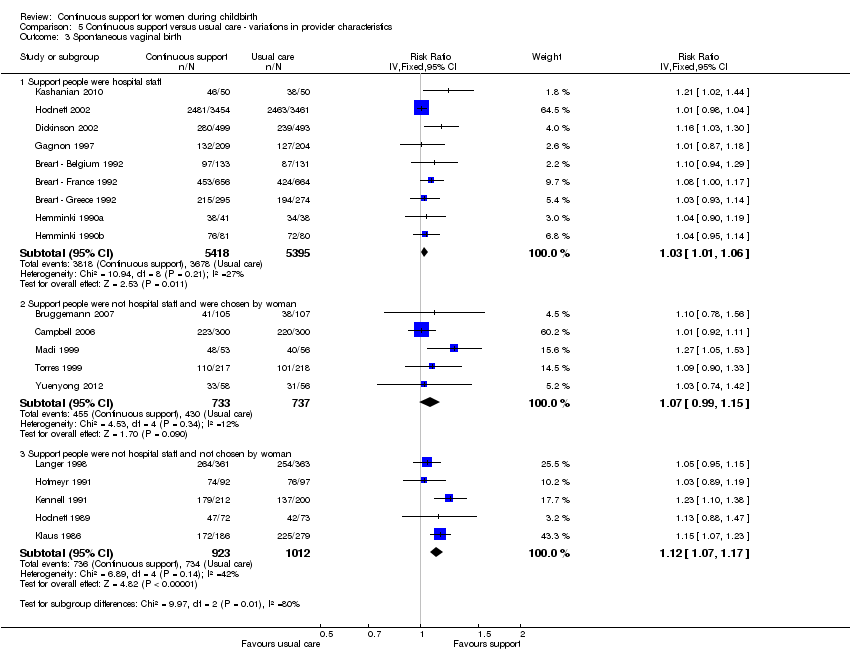
Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 3 Spontaneous vaginal birth.

Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 4 Caesarean birth.
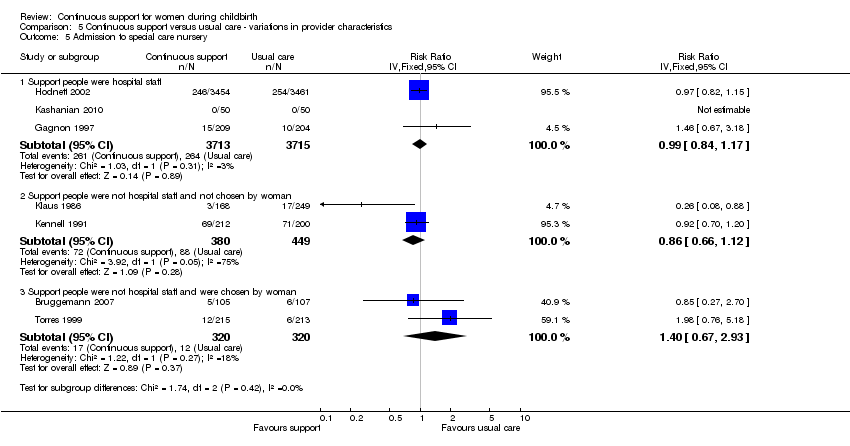
Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 5 Admission to special care nursery.

Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 6 Postpartum depression.

Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 7 Negative rating of/negative feelings about birth experience.
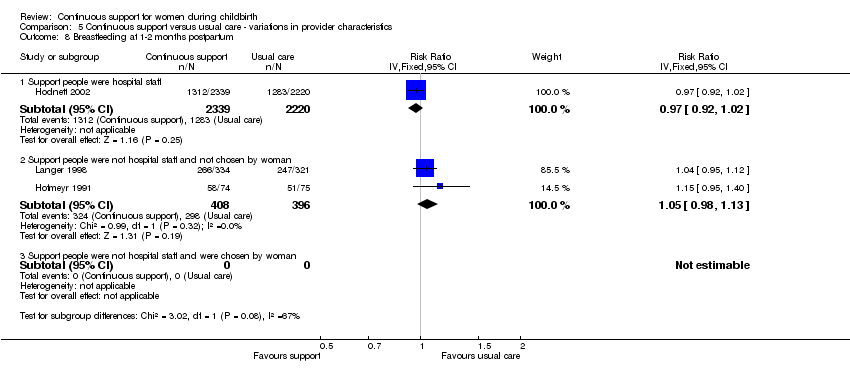
Comparison 5 Continuous support versus usual care ‐ variations in provider characteristics, Outcome 8 Breastfeeding at 1‐2 months postpartum.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | 12283 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.84, 0.96] |
| 2 Regional analgesia/anaesthesia Show forest plot | 9 | 11444 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.99] |
| 3 Synthetic oxytocin during labour Show forest plot | 15 | 12620 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.91, 1.04] |
| 4 Labour length Show forest plot | 12 | 5366 | Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐0.85, ‐0.31] |
| 5 Spontaneous vaginal birth Show forest plot | 19 | 14119 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [1.04, 1.12] |
| 6 Instrumental vaginal birth Show forest plot | 19 | 14118 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.85, 0.96] |
| 7 Caesarean birth Show forest plot | 22 | 15175 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.67, 0.91] |
| 8 Perineal trauma Show forest plot | 4 | 8120 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.92, 1.01] |
| 9 Low 5‐minute Apgar score Show forest plot | 13 | 12515 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.50, 0.95] |
| 10 Admission to special care nursery Show forest plot | 7 | 8897 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.76, 1.25] |
| 11 Prolonged neonatal hospital stay Show forest plot | 3 | 1098 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.42, 1.65] |
| 12 Postpartum report of severe labour pain Show forest plot | 4 | 2456 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.83, 1.21] |
| 13 Negative rating of/negative feelings about birth experience Show forest plot | 11 | 11133 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.59, 0.79] |
| 14 Difficulty mothering Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | 5363 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.94, 1.09] |
| 16 Postpartum depression Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17 Low postpartum self‐esteem Show forest plot | 1 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.77, 1.30] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Other support permitted | 7 | 9752 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.99] |
| 1.2 Other support not permitted | 7 | 2598 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.85, 0.96] |
| 2 Synthetic oxytocin during labour Show forest plot | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Other support permitted | 5 | 9495 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [0.99, 1.10] |
| 2.2 Other support not permitted | 10 | 3125 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.97, 1.02] |
| 3 Spontaneous vaginal birth Show forest plot | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Other support permitted | 9 | 10889 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [1.00, 1.05] |
| 3.2 Other support not permitted | 10 | 3329 | Risk Ratio (IV, Fixed, 95% CI) | 1.11 [1.07, 1.16] |
| 4 Caesarean birth Show forest plot | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Other support permitted | 11 | 11326 | Risk Ratio (IV, Fixed, 95% CI) | 0.94 [0.85, 1.03] |
| 4.2 Other support not permitted | 11 | 3849 | Risk Ratio (IV, Fixed, 95% CI) | 0.75 [0.65, 0.86] |
| 5 Admission to special care nursery Show forest plot | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Other support permitted | 2 | 7328 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.84, 1.17] |
| 5.2 Other support not permitted | 5 | 1569 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.71, 1.17] |
| 6 Postpartum depression Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Other support permitted | 1 | 5567 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.73, 1.02] |
| 6.2 Other support not permitted | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.18 [0.09, 0.36] |
| 7 Negative rating of/negative feelings about birth experience Show forest plot | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Other support permitted | 5 | 8639 | Risk Ratio (IV, Fixed, 95% CI) | 0.70 [0.62, 0.78] |
| 7.2 Other support not permitted | 6 | 2539 | Risk Ratio (IV, Fixed, 95% CI) | 0.62 [0.56, 0.69] |
| 8 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Other support permitted | 1 | 4559 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.92, 1.02] |
| 8.2 Other support not permitted | 2 | 804 | Risk Ratio (IV, Fixed, 95% CI) | 1.05 [0.98, 1.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Epidural analgesia routinely available | 9 | 10888 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.98] |
| 1.2 Epidural analgesia not routinely available | 5 | 1462 | Risk Ratio (IV, Fixed, 95% CI) | 0.83 [0.69, 0.99] |
| 2 Synthetic oxytocin during labour Show forest plot | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Epidural analgesia routinely available | 8 | 10568 | Risk Ratio (IV, Fixed, 95% CI) | 1.00 [0.98, 1.02] |
| 2.2 Epidural analgesia not routinely available | 7 | 2066 | Risk Ratio (IV, Fixed, 95% CI) | 1.02 [0.93, 1.11] |
| 3 Spontaneous vaginal birth Show forest plot | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Epidural analgesia routinely available | 13 | 12672 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [1.01, 1.06] |
| 3.2 Epidural analgesia not routinely available | 6 | 1546 | Risk Ratio (IV, Fixed, 95% CI) | 1.11 [1.06, 1.17] |
| 4 Caesarean birth Show forest plot | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Epidural analgesia routinely available | 14 | 13064 | Risk Ratio (IV, Fixed, 95% CI) | 0.93 [0.86, 1.02] |
| 4.2 Epidural analgesia not routinely available | 7 | 2077 | Risk Ratio (IV, Fixed, 95% CI) | 0.54 [0.43, 0.68] |
| 4.3 Unknown availability of epidural analgesia | 1 | 34 | Risk Ratio (IV, Fixed, 95% CI) | 1.4 [0.14, 13.98] |
| 5 Admission to special care nursery Show forest plot | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Epidural analgesia routinely available | 5 | 8380 | Risk Ratio (IV, Fixed, 95% CI) | 0.98 [0.85, 1.13] |
| 5.2 Epidural analgesia not routinely available | 2 | 517 | Risk Ratio (IV, Fixed, 95% CI) | 0.26 [0.08, 0.88] |
| 6 Postpartum depression Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Epidural analgesia routinely available | 1 | 6915 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.75, 1.05] |
| 6.2 Epidural analgesia not routinely available | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.18 [0.09, 0.36] |
| 7 Negative rating of/negative feelings about birth experience Show forest plot | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Epidural analgesia routinely available | 9 | 10404 | Risk Ratio (IV, Fixed, 95% CI) | 0.70 [0.64, 0.77] |
| 7.2 Epidural analgesia not routinely available | 2 | 774 | Risk Ratio (IV, Fixed, 95% CI) | 0.55 [0.48, 0.63] |
| 8 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Epidural analgesia routinely available | 2 | 5214 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.95, 1.03] |
| 8.2 Epidural analgesia not routinely available | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 1.15 [0.95, 1.40] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Setting had routine EFM | 6 | 8580 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.99] |
| 1.2 Setting did not have routine EFM | 6 | 2186 | Risk Ratio (IV, Fixed, 95% CI) | 0.96 [0.90, 1.02] |
| 1.3 Policy about routine EFM not known | 2 | 1579 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.80, 0.99] |
| 2 Synthetic oxytocin during labour Show forest plot | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Setting had routine EFM | 4 | 8340 | Risk Ratio (IV, Fixed, 95% CI) | 1.04 [0.98, 1.11] |
| 2.2 Setting did not have routine EFM | 7 | 1726 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.96, 1.01] |
| 2.3 Policy about routine EFM not known | 4 | 2568 | Risk Ratio (IV, Fixed, 95% CI) | 1.02 [0.97, 1.08] |
| 3 Spontaneous vaginal birth Show forest plot | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Setting had routine EFM | 8 | 9717 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [1.01, 1.06] |
| 3.2 Setting did not have routine EFM | 7 | 1913 | Risk Ratio (IV, Fixed, 95% CI) | 1.11 [1.06, 1.17] |
| 3.3 Policy about routine EFM not known | 4 | 2561 | Risk Ratio (IV, Fixed, 95% CI) | 1.07 [1.01, 1.13] |
| 4 Caesarean birth Show forest plot | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Setting had routine EFM | 9 | 10123 | Risk Ratio (IV, Fixed, 95% CI) | 0.92 [0.83, 1.01] |
| 4.2 Setting did not have routine EFM | 8 | 2457 | Risk Ratio (IV, Fixed, 95% CI) | 0.66 [0.55, 0.79] |
| 4.3 Policy about routine EFM not known | 5 | 2595 | Risk Ratio (IV, Fixed, 95% CI) | 1.06 [0.84, 1.33] |
| 5 Admission to special care nursery Show forest plot | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Setting had routine EFM | 3 | 7740 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.84, 1.11] |
| 5.2 Setting did not have routine EFM | 3 | 729 | Risk Ratio (IV, Fixed, 95% CI) | 0.48 [0.21, 1.12] |
| 5.3 Policy about routine EFM not known | 1 | 428 | Risk Ratio (IV, Fixed, 95% CI) | 1.98 [0.76, 5.18] |
| 6 Postpartum depression Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Setting had routine EFM | 1 | 6915 | Risk Ratio (IV, Fixed, 95% CI) | 0.89 [0.75, 1.05] |
| 6.2 Setting did not have routine EFM | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.18 [0.09, 0.36] |
| 7 Negative rating of/negative views about birth experience Show forest plot | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Setting had routine EFM | 4 | 7467 | Risk Ratio (IV, Fixed, 95% CI) | 0.67 [0.60, 0.76] |
| 7.2 Setting did not have routine EFM | 4 | 1710 | Risk Ratio (IV, Fixed, 95% CI) | 0.60 [0.53, 0.68] |
| 7.3 Policy about routine EFM not known | 3 | 1977 | Risk Ratio (IV, Fixed, 95% CI) | 0.84 [0.65, 1.08] |
| 8 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Setting had routine EFM | 1 | 4559 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.92, 1.02] |
| 8.2 Setting did not have routine EFM | 2 | 804 | Risk Ratio (IV, Fixed, 95% CI) | 1.05 [0.98, 1.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any analgesia/anaesthesia Show forest plot | 14 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Support people were hospital staff | 6 | 9152 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.96, 0.99] |
| 1.2 Support people were not hospital staff and not chosen by woman | 4 | 1790 | Risk Ratio (IV, Fixed, 95% CI) | 0.91 [0.86, 0.97] |
| 1.3 Support people were not hospital staff and were chosen by woman | 4 | 1408 | Risk Ratio (IV, Fixed, 95% CI) | 0.94 [0.88, 1.00] |
| 2 Synthetic oxytocin during labour Show forest plot | 15 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Support people were hospital staff | 6 | 9561 | Risk Ratio (IV, Fixed, 95% CI) | 1.06 [1.01, 1.11] |
| 2.2 Support people were not hospital staff and not chosen by woman | 3 | 1018 | Risk Ratio (IV, Fixed, 95% CI) | 0.69 [0.50, 0.94] |
| 2.3 Support people were not hospital staff and were chosen by woman | 6 | 2041 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.96, 1.01] |
| 3 Spontaneous vaginal birth Show forest plot | 19 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Support people were hospital staff | 9 | 10813 | Risk Ratio (IV, Fixed, 95% CI) | 1.03 [1.01, 1.06] |
| 3.2 Support people were not hospital staff and were chosen by woman | 5 | 1470 | Risk Ratio (IV, Fixed, 95% CI) | 1.07 [0.99, 1.15] |
| 3.3 Support people were not hospital staff and not chosen by woman | 5 | 1935 | Risk Ratio (IV, Fixed, 95% CI) | 1.12 [1.07, 1.17] |
| 4 Caesarean birth Show forest plot | 22 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Support people were hospital staff | 9 | 10786 | Risk Ratio (IV, Fixed, 95% CI) | 0.95 [0.85, 1.05] |
| 4.2 Support people were not hospital staff and not chosen by woman | 7 | 2330 | Risk Ratio (IV, Fixed, 95% CI) | 0.72 [0.60, 0.86] |
| 4.3 Support people were not hospital staff and were chosen by woman | 6 | 2059 | Risk Ratio (IV, Fixed, 95% CI) | 0.83 [0.69, 1.01] |
| 5 Admission to special care nursery Show forest plot | 7 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Support people were hospital staff | 3 | 7428 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.84, 1.17] |
| 5.2 Support people were not hospital staff and not chosen by woman | 2 | 829 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.66, 1.12] |
| 5.3 Support people were not hospital staff and were chosen by woman | 2 | 640 | Risk Ratio (IV, Fixed, 95% CI) | 1.40 [0.67, 2.93] |
| 6 Postpartum depression Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Support people were hospital staff | 1 | 5567 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.73, 1.02] |
| 6.2 Support people were not hospital staff and not chosen by woman | 1 | 149 | Risk Ratio (IV, Fixed, 95% CI) | 0.17 [0.09, 0.33] |
| 6.3 Support people were not hospital staff and were chosen by woman | 0 | 0 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Negative rating of/negative feelings about birth experience Show forest plot | 11 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Support people were hospital staff | 4 | 8145 | Risk Ratio (IV, Fixed, 95% CI) | 0.87 [0.73, 1.03] |
| 7.2 Support people were not hospital staff and not chosen by woman | 3 | 1325 | Risk Ratio (IV, Fixed, 95% CI) | 0.66 [0.57, 0.77] |
| 7.3 Support people were not hospital staff and were chosen by woman | 4 | 1708 | Risk Ratio (IV, Fixed, 95% CI) | 0.57 [0.51, 0.64] |
| 8 Breastfeeding at 1‐2 months postpartum Show forest plot | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Support people were hospital staff | 1 | 4559 | Risk Ratio (IV, Fixed, 95% CI) | 0.97 [0.92, 1.02] |
| 8.2 Support people were not hospital staff and not chosen by woman | 2 | 804 | Risk Ratio (IV, Fixed, 95% CI) | 1.05 [0.98, 1.13] |
| 8.3 Support people were not hospital staff and were chosen by woman | 0 | 0 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

