Cuidado cardiaco rápido para pacientes adultos sometidos a cirugía cardíaca
Información
- DOI:
- https://doi.org/10.1002/14651858.CD003587.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 12 septiembre 2016see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Anestesia
- Copyright:
-
- Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Designing the update for the review: Wai‐Tat Wong (WTW), Veronica Ka Wai Lai (VKWL), Yee Eot Chee (YEC), Anna Lee (AL).
Co‐ordinating the review: AL.
Screening search results: WTW, AL.
Organizing retrieval of papers: VKWL, AL.
Screening retrieved papers against inclusion criteria: WTW, AL.
Appraising quality of papers: VKWL, AL.
Abstracting data from papers: VKWL, AL.
Writing to authors of papers for additional information: AL.
Managing data for the review: VKWL, AL.
Entering data into Review Manager (RevMan 5.3): VKWL.
Checking data entry in Review Manager (RevMan 5.3): WTW, AL.
Analysing RevMan statistical data: VKWL, AL.
Performing there statistical analyses not using RevMan: VKWL, AL.
Interpreting data: all review authors.
Making statistical inferences: all review authors.
Writing the review: all review authors.
Providing guidance on the review: AL.
Securing funding for the review: not applicable.
Sources of support
Internal sources
-
Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Hong Kong.
External sources
-
No sources of support supplied
Declarations of interest
WTW, VKWL and YEC declare no potential conflict of interests in this review. AL co‐authored a previous related systematic review (Myles 2003), along with Professor Paul Myles; two of his trials are included in this updated review (Myles 1997; Myles 2002). As AL was also co‐author of a trial included in this updated review (Zhu 2015), WTW and VKWL independently performed data extraction.
Acknowledgements
We would like to thank Rodrigo Cavallazzi (Content Editor), Nathan Pace (Statistical Editor) Janet Wale (Consumer Editor) and Jane Cracknell (Managing Editor) for help and editorial advice provided during preparation of this updated systematic review.
Thanks to Dr John Carlisle, Prof Nathan Pace, Dr Karen Hovhannisyan, Dr R Peter Alston, Prof Paul Myles, Dr Vesna Svircevic and Ms Jane Cracknell for help and editorial advice provided during the previous update (Zhu 2012). Thanks to Dr Zhirajr Mokini for translating a study (Nougarede 2004) from French to English.
We would like to acknowledge the work done in the original Cochrane review by Claire Hawkes, Srinivasan Dhileepan and David Foxcroft (Hawkes 2003), and in the previous update by Fang Zhu (Zhu 2012).
Version history
| Published | Title | Stage | Authors | Version |
| 2016 Sep 12 | Fast‐track cardiac care for adult cardiac surgical patients | Review | Wai‐Tat Wong, Veronica KW Lai, Yee Eot Chee, Anna Lee | |
| 2012 Oct 17 | Fast‐track cardiac care for adult cardiac surgical patients | Review | Fang Zhu, Anna Lee, Yee Eot Chee | |
| 2003 Oct 20 | Early extubation for adult cardiac surgical patients | Review | Claire A Hawkes, Srinivasan Dhileepan, David R Foxcroft | |
Differences between protocol and review
Inclusion criteria and mortality time points in this updated systematic review are different from those in the original review by Hawkes et al (Hawkes 2003). This update and our previous updated review (Zhu 2012) includes more types of postoperative adverse outcomes, health‐related quality of life and healthcare costs. These patient‐centred outcomes are important for clinical decision making.
Notes
None.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Adult; Humans;
PICO
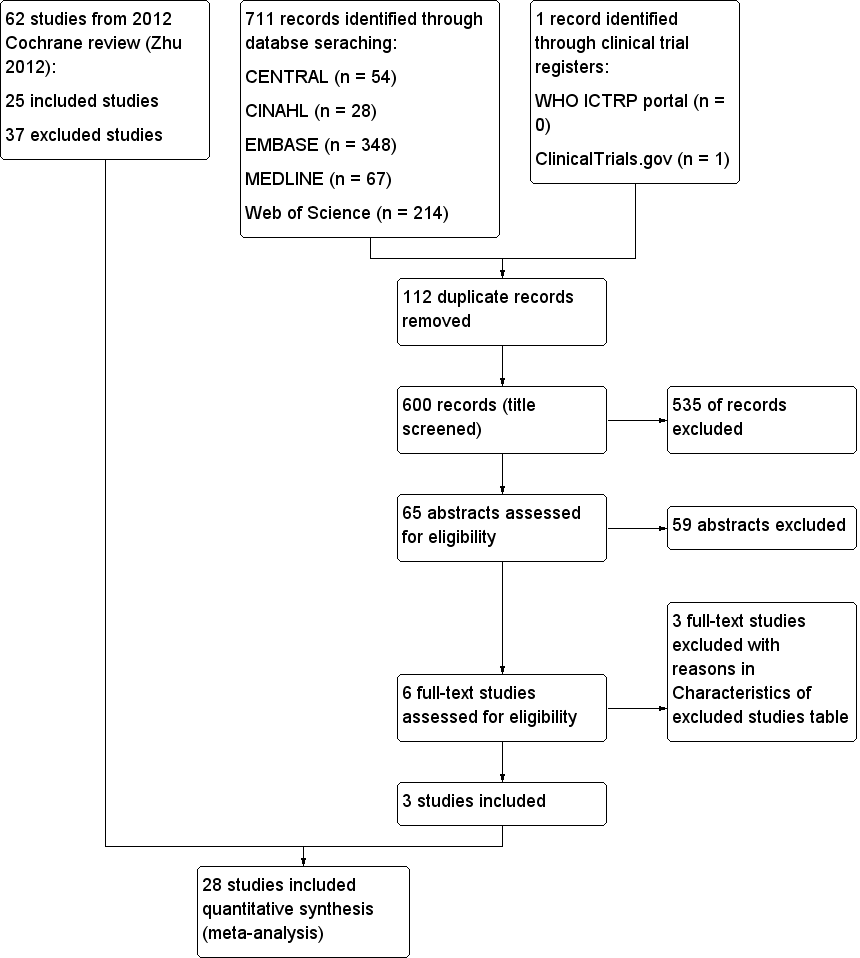
Study flow diagram.
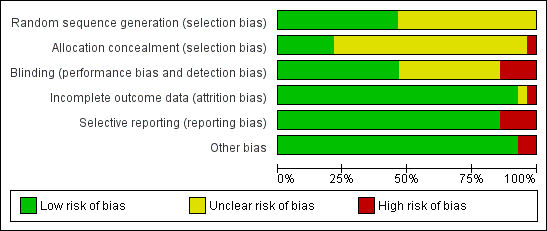
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
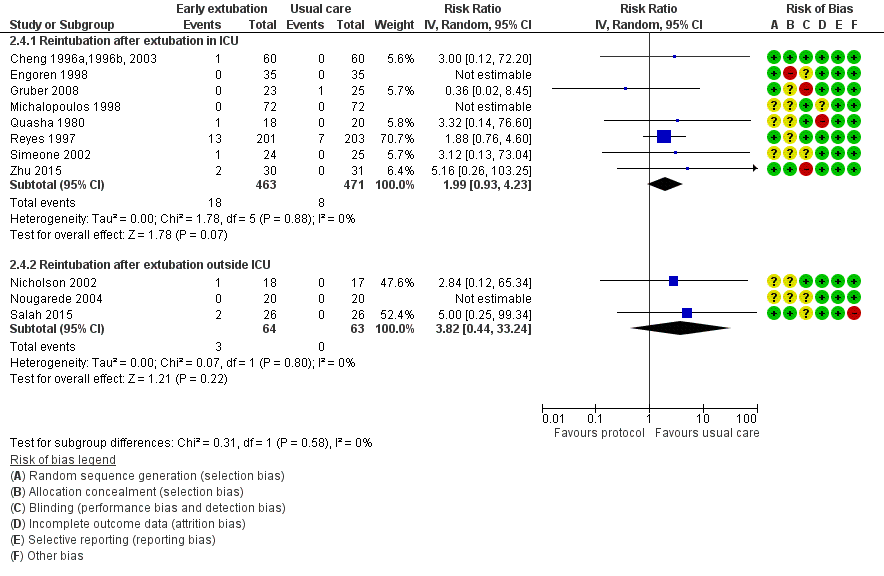
Forest plot of comparison: 2 Time‐directed extubation protocols, outcome: 2.4 Subgroup analysis.

Comparison 1 Dose of opioid‐based cardiac anaesthesia, Outcome 1 Mortality.

Comparison 1 Dose of opioid‐based cardiac anaesthesia, Outcome 2 Postoperative complications.
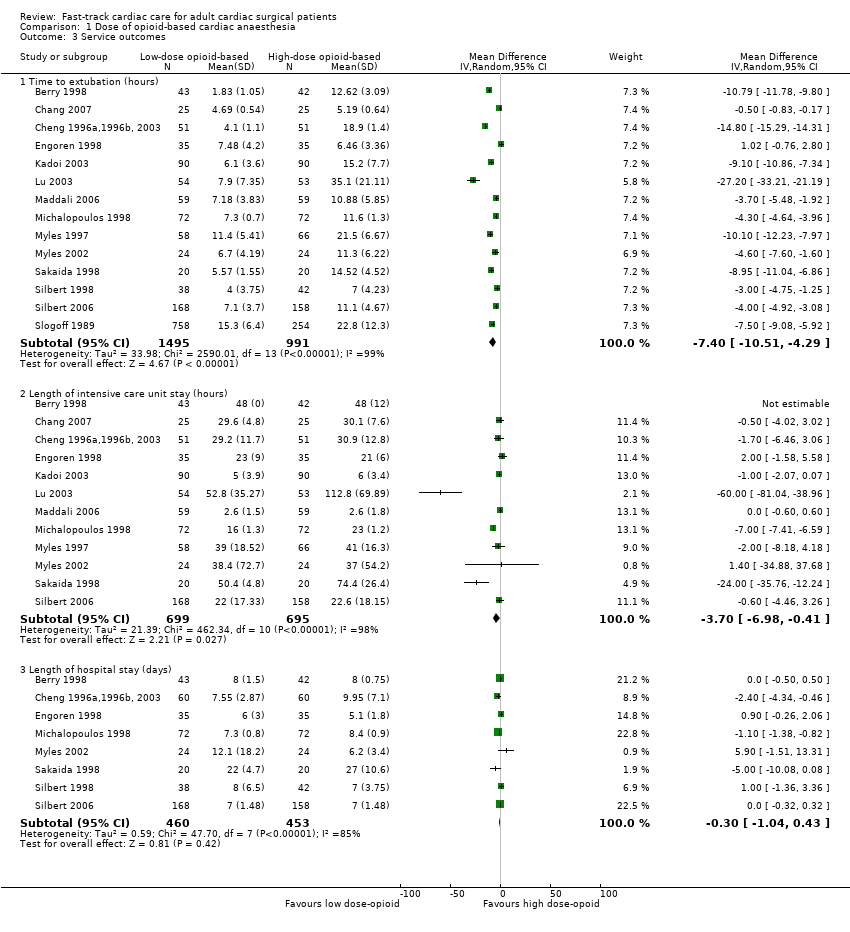
Comparison 1 Dose of opioid‐based cardiac anaesthesia, Outcome 3 Service outcomes.

Comparison 2 Time‐directed extubation protocol, Outcome 1 Mortality.
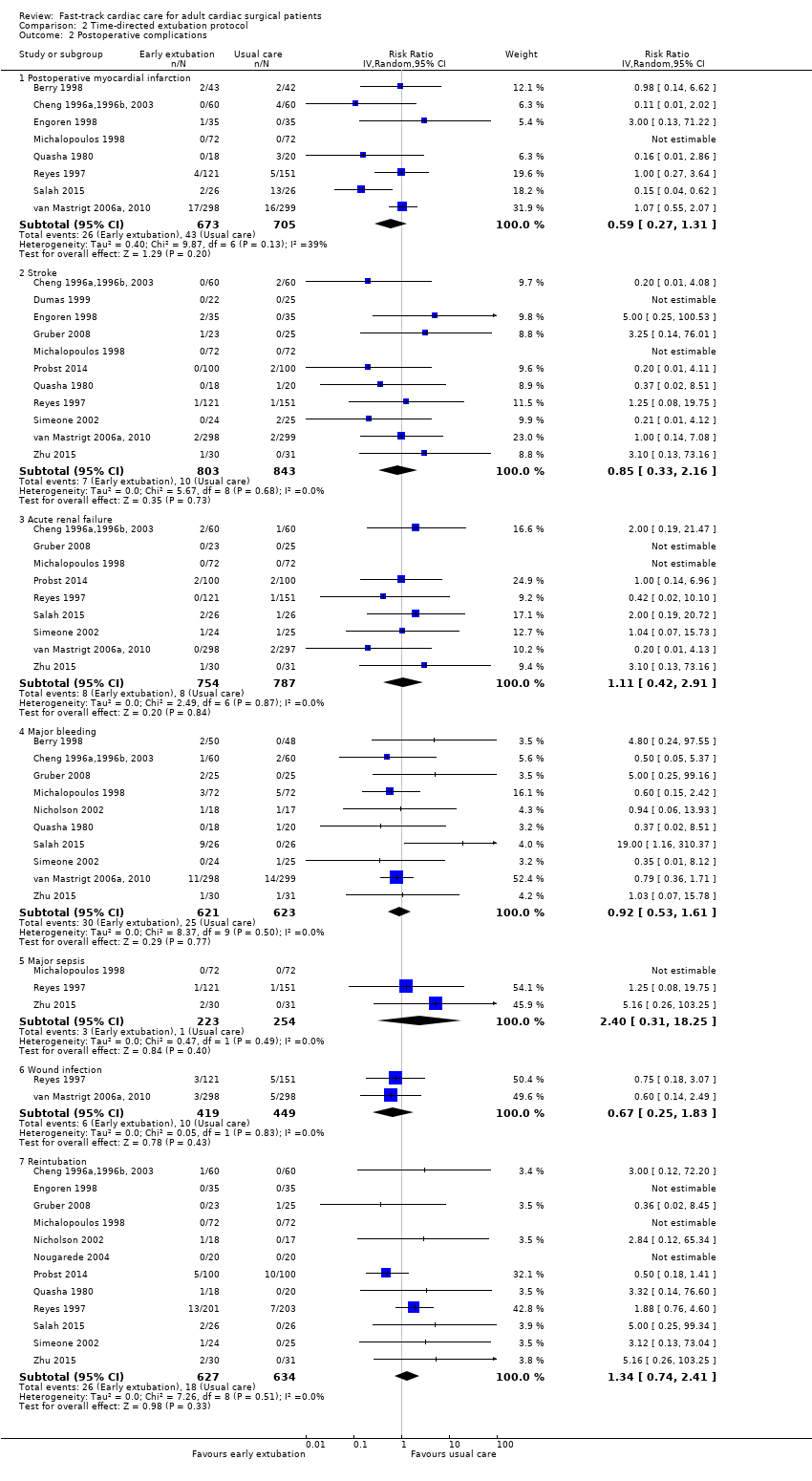
Comparison 2 Time‐directed extubation protocol, Outcome 2 Postoperative complications.

Comparison 2 Time‐directed extubation protocol, Outcome 3 Service outcomes.
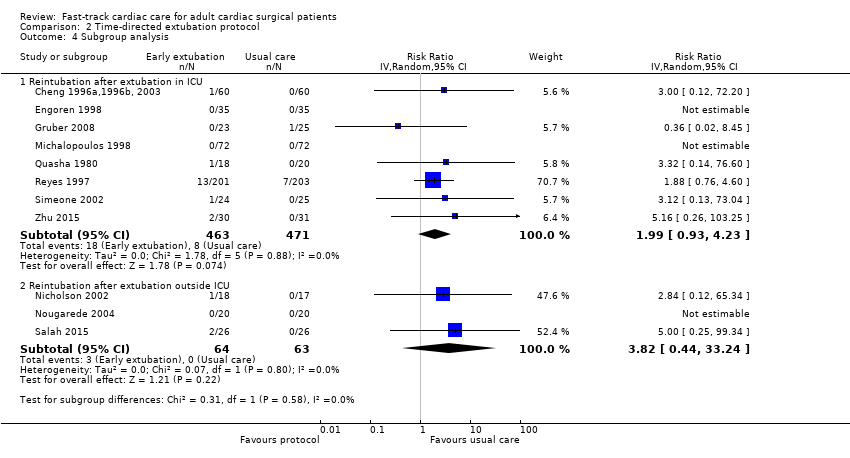
Comparison 2 Time‐directed extubation protocol, Outcome 4 Subgroup analysis.
| Low‐dose opioid‐based general anaesthesia compared with high‐dose opioid‐based general anaesthesia for adults undergoing cardiac surgery | ||||||
| Patient or population: adult cardiac surgical patients Intervention: low‐dose opioid‐based general anaesthesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with high‐dose opioid‐based general anaesthesia | Risk with low‐dose opioid‐based general anaesthesia | |||||
| Mortality ‐ Death at any time after surgery | Low | OR 0.53 | 1994 | ⊕⊕⊝⊝ | No death recorded in 3 trials | |
| 10 per 1000 | 5 per 1000 | |||||
| Moderate | ||||||
| 30 per 1000 | 16 per 1000 | |||||
| High | ||||||
| 110 per 1000 | 61 per 1000 | |||||
| Postoperative myocardial infarction | Study population | RR 0.98 | 1683 | ⊕⊕⊝⊝ | No postoperative myocardial infarction recorded in 2 trials | |
| 30 per 1000 | 30 per 1000 | |||||
| Postoperative stroke | Study population | RR 1.17 | 562 | ⊕⊕⊝⊝ | No stroke recorded in 1 trial | |
| 18 per 1000 | 21 per 1000 | |||||
| Postoperative tracheal reintubation | Study population | RR 1.77 | 594 | ⊕⊕⊝⊝ | No reintubation recorded in 3 trials | |
| 7 per 1000 | 12 per 1000 | |||||
| Time to extubation (hours) | Mean time to extubation (hours) was 5.2 to 35.1 | Mean time to extubation (hours) in the intervention group was 7.4 lower (10.51 lower to 4.29 lower). | ‐ | 2486 | ⊕⊕⊝⊝ | |
| Length of intensive care unit stay (hours) | Mean length of intensive care unit stay (hours) was 2.6 to 112.8. | Mean length of intensive care unit stay (hours) in the intervention group was 3.7 lower (6.98 lower to 0.41 lower). | ‐ | 1394 | ⊕⊕⊝⊝ | |
| Length of hospital stay (days) | Mean length of hospital stay (days) was 5.1 to 27.0. | Mean length of hospital stay (days) in the intervention group was 0.3 lower (1.04 lower to 0.43 higher). | ‐ | 913 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group using the EuroSCORE risk classification (Michel 2003) and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aOf the 8 trials, 2 had ≥ 1 high risk of bias domain (downgrade 1 point owing to study limitations). bOptimal information size not met (downgrade 1 point owing to imprecision). cOf the 5 trials, 1 had ≥ 1 high risk of bias domain (downgrade 1 point owing to study limitations). dOf the 5 trials, 2 had ≥ 1 high risk of bias domain (downgrade 1 point owing to study limitations). eOf the 14 trials, 4 had ≥ 1 high risk of bias domain (downgrade 1 point owing to study limitations). fUnexplained reasons for high heterogeneity. gOf the 12 trials, 3 had ≥ 1 high risk of bias domain (downgrade 1 point owing to study limitations). hOf the 8 trials, 3 had ≥ 1 high risk of bias domain (downgrade 1 point owing to study limitations). | ||||||
| Time‐directed extubation protocol compared with usual care for adults undergoing cardiac surgery | ||||||
| Patient or population: adult cardiac surgical patients | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with time‐directed extubation protocol | |||||
| Mortality ‐ Death at any time after surgery | Low | OR 0.80 | 1802 | ⊕⊕⊝⊝ | No deaths recorded in 4 trials. Low to moderate heterogeneity (I2 = 37%) may be explained by the inclusion of a trial (Reyes 1997) that had the highest rate of mortality of all trials considered. When excluded, the OR changed to 0.31 (95% CI 0.11 to 0.90, P = 0.03, I2 = 0%). | |
| 10 per 1000 | 8 per 1000 | |||||
| Moderate | ||||||
| 30 per 1000 | 24 per 1000 | |||||
| High | ||||||
| 110 per 1000 | 90 per 1000 | |||||
| Postoperative myocardial infarction | Study population | RR 0.59 | 1378 | ⊕⊕⊝⊝ | No postoperative myocardial infarction was recorded in 1 trial. | |
| 61 per 1000 | 36 per 1000 | |||||
| Postoperative stroke | Study population | RR 0.85 | 1646 | ⊕⊕⊝⊝ | No stroke was recorded in 2 trials. | |
| 12 per 1000 | 10 per 1000 | |||||
| Postoperative reintubation | Study population | RR 1.34 | 1261 | ⊕⊕⊝⊝ | No reintubation was recorded in 3 trials. | |
| 28 per 1000 | 38 per 1000 | |||||
| Time to extubation (hours) | Mean time to extubation (hours) was 3.4 to 18.9. | Mean time to extubation (hours) in the intervention group was 6.25 lower (8.84 lower to 3.67 lower). | ‐ | 2024 | ⊕⊕⊝⊝ | No variation in time to extubation in the early extubation group in 1 trial |
| Length of intensive care unit stay (hours) | Mean length of intensive care unit stay (hours) was 17.9 to 95.0. | Mean length of intensive care unit stay (hours) in the intervention group was 7.16 lower (10.45 lower to 3.88 lower). | ‐ | 1888 | ⊕⊕⊝⊝ | No variation in length of ICU stay in early extubation group in 1 trial |
| Length of hospital stay (days) | Mean length of hospital stay (days) was 5.1 to 13.0. | Mean length of hospital stay (days) in the intervention group was 0.44 lower (1.04 lower to 0.16 higher). | ‐ | 1334 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group using the EuroSCORE risk classification (Michel 2003) and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aOf the 10 trials, 3 had 1 high risk of bias domain (downgrade 1 point owing to study limitations). bOptimal information size not met (downgrade 1 point owing to imprecision). cOf the 8 trials, 3 had 1 high risk of bias domain (downgrade 1 point owing to study limitations). dOf the 11 trials, 5 had 1 high risk of bias domain (downgrade 1 point owing to study limitations). dOf the 12 trials, 5 had 1 high risk of bias domain (downgrade 1 point owing to study limitations). fUnexplained reasons for high heterogeneity. gOf the 16 trials, 6 had 1 high risk of bias domain (downgrade 1 point owing to study limitations). hOf the 13 trials, 5 had 1 high risk of bias domain (downgrade 1 point owing to study limitations). iOf the 8 trials, 2 had 1 high risk of bias domain (downgrade 1 point owing to study limitations). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 8 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 1.1 Death in hospital after surgery | 7 | 1896 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.58 [0.24, 1.39] |
| 1.2 Death at 1 year after surgery | 2 | 446 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.55 [0.17, 1.82] |
| 1.3 Death at any time after surgery | 8 | 1994 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.53 [0.25, 1.12] |
| 2 Postoperative complications Show forest plot | 10 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Postoperative myocardial infarction | 8 | 1683 | Risk Ratio (IV, Random, 95% CI) | 0.98 [0.48, 1.99] |
| 2.2 Stroke | 5 | 562 | Risk Ratio (IV, Random, 95% CI) | 1.17 [0.36, 3.78] |
| 2.3 Acute renal failure | 4 | 492 | Risk Ratio (IV, Random, 95% CI) | 1.19 [0.33, 4.33] |
| 2.4 Major bleeding | 4 | 469 | Risk Ratio (IV, Random, 95% CI) | 0.48 [0.16, 1.44] |
| 2.5 Reintubation | 5 | 594 | Risk Ratio (IV, Random, 95% CI) | 1.77 [0.38, 8.27] |
| 3 Service outcomes Show forest plot | 14 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Time to extubation (hours) | 14 | 2486 | Mean Difference (IV, Random, 95% CI) | ‐7.40 [‐10.51, ‐4.29] |
| 3.2 Length of intensive care unit stay (hours) | 12 | 1394 | Mean Difference (IV, Random, 95% CI) | ‐3.70 [‐6.98, ‐0.41] |
| 3.3 Length of hospital stay (days) | 8 | 913 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.04, 0.43] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 10 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 1.1 Death in the intensive care unit | 2 | 370 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.19, 3.88] |
| 1.2 Death in hospital after surgery | 5 | 582 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.23 [0.05, 1.04] |
| 1.3 Death at 1 month after surgery | 4 | 1122 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.13 [0.59, 2.19] |
| 1.4 Death at any time after surgery | 10 | 1802 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.80 [0.45, 1.45] |
| 2 Postoperative complications Show forest plot | 15 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Postoperative myocardial infarction | 8 | 1378 | Risk Ratio (IV, Random, 95% CI) | 0.59 [0.27, 1.31] |
| 2.2 Stroke | 11 | 1646 | Risk Ratio (IV, Random, 95% CI) | 0.85 [0.33, 2.16] |
| 2.3 Acute renal failure | 9 | 1541 | Risk Ratio (IV, Random, 95% CI) | 1.11 [0.42, 2.91] |
| 2.4 Major bleeding | 10 | 1244 | Risk Ratio (IV, Random, 95% CI) | 0.92 [0.53, 1.61] |
| 2.5 Major sepsis | 3 | 477 | Risk Ratio (IV, Random, 95% CI) | 2.40 [0.31, 18.25] |
| 2.6 Wound infection | 2 | 868 | Risk Ratio (IV, Random, 95% CI) | 0.67 [0.25, 1.83] |
| 2.7 Reintubation | 12 | 1261 | Risk Ratio (IV, Random, 95% CI) | 1.34 [0.74, 2.41] |
| 3 Service outcomes Show forest plot | 16 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Time to extubation (hours) | 16 | 2024 | Mean Difference (IV, Random, 95% CI) | ‐6.25 [‐8.84, ‐3.67] |
| 3.2 Length of intensive care unit stay (hours) | 13 | 1888 | Mean Difference (IV, Random, 95% CI) | ‐7.16 [‐10.45, ‐3.88] |
| 3.3 Length of hospital stay (days) | 8 | 1334 | Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐1.04, 0.16] |
| 4 Subgroup analysis Show forest plot | 11 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Reintubation after extubation in ICU | 8 | 934 | Risk Ratio (IV, Random, 95% CI) | 1.99 [0.93, 4.23] |
| 4.2 Reintubation after extubation outside ICU | 3 | 127 | Risk Ratio (IV, Random, 95% CI) | 3.82 [0.44, 33.24] |

